- 1Department of Pharmacy, College of Health Sciences, Debre Berhan University, Debre Berhan, Ethiopia
- 2Department of Midwifery, School of Nursing and Midwifery, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
- 3Clinical Pharmacy Unit and Research Team, Department of Pharmacy, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Background: Globally, about 18 million people died from cardiovascular diseases (CVDs) in 2019, over three-quarters in developing countries. Non-adherence to medication in CVD patients causes hospitalization, worsened symptoms, higher healthcare costs, and more emergency visits. Hence, this study aimed to assess treatment satisfaction and medication adherence and predictors in heart failure (HF) patients attending Debre Berhan Comprehensive Specialized Hospital (DBCSH), Ethiopia.
Methods: A hospital-based cross-sectional study was undertaken at the medical referral clinic of DBCSH. A total of 344 ambulatory HF patients who visited the medical care of the DBCSH medical referral clinic during the study period were included. Treatment satisfaction was assessed using a self-administered Medicine Questionnaire (SATMED-Q). Relationships between predictor variables and treatment satisfaction were determined using one-way analysis of variance (ANOVA) and an independent t-test. Medication adherence was determined using the Morisky Green Levin Medication Adherence Scale (MGLS).
Results: Participants with drug-drug interactions (DDIs) were approximately 38% less likely to adhere to medication compared to their counterparts (AOR = 0.62, 95% CI: 0.54–0.71). Additionally, participants who had taken five or more drugs were approximately 68% less likely to adhere to medication compared to those who had taken only one drug (AOR = 0.32, 95% CI: 0.2–0.51). The correlation between medication adherence and drug-drug interactions remains a possible pseudo-correlation via the number of medications taken. There was a noteworthy positive correlation (rs = 0.34, p = 0.027) between participants’ treatment adherence and treatment satisfaction.
Conclusion: The rate of treatment satisfaction and treatment adherence among HF patients was 67.6% and 60.9%, respectively. The presence of DDI and the number of drugs were identified as predictors to medication adherence.
Introduction
Cardiovascular diseases (CVDs) cause 17.9 million deaths occurred in developing nations (WHO, 2021). In Sub-Saharan African (SSA) countries, poor access to high-quality and inaccessible healthcare contributes to an increase in CVD morbidity and death (Mensah et al., 2015; Meyer et al., 2017; Schultz et al., 2018; Rosengren et al., 2019). The prevalence of CVD in Ethiopia was 5,534 per 100,000 people (Ali et al., 2020).
Globally, heart failure (HF) constitutes a significant medical and economic challenge (Lesyuk et al., 2018). It results from changes in cardiac structure or function that impair the ability of the ventricle to fill with or eject blood (Parker et al., 2020). The incidence and prevalence of HF are increasing; approximately 6.5 million Americans currently have HF, with 1,000,000 new cases diagnosed each year and annual expenditures exceeding 30 billion US dollars (Benjamin et al., 2018). Based on the phenotypes of the disease, HF can be classified as HF with reduced ejection fraction (EF) (HFrEF) and HF with preserved EF (HFpEF) (Mann et al., 2018).
Managing HF remains challenging due to co-existing co-morbidities (Chiatti et al., 2012). In addition, prescribing a higher number of medications for HF patients results in non-adherence to medication and more frequent hospital stays (Page et al., 2016). To achieve favorable clinical outcomes, HF guidelines emphasize the paramount importance of adhering to prescribed treatment regimens (Riegel et al., 2011; Ponikowski et al., 2016). Maximizing treatment results depends critically on adherence to HF medications (Pallangyo et al., 2020).
Studies conducted in various countries indicated that HF patients adhering to their medication experienced fewer emergency department visits, improved clinical survival, fewer HF exacerbations, and lower healthcare costs (Hope et al., 2004; Murray et al., 2009; Wu et al., 2009). However, medication non-adherence was associated with increased hospitalization (Knafl and Riegel, 2014a; Aggarwal et al., 2015), worsening symptoms, disease progression, an overall increase in healthcare costs (Aggarwal et al., 2015), and frequent emergency department visits (Davis et al., 2014). Heart failure medication adherence often falls below optimal levels in global investigations using various adherence evaluation methods (Fitzgerald et al., 2011; Lee et al., 2015; Shah et al., 2015; Amininasab et al., 2018; Fernandez-Lazaro et al., 2019; Rehman et al., 2019; Pallangyo et al., 2020).
Patient satisfaction with prescriptions or services influences treatment outcomes, the duration of pharmacological care, optimal service utilization, clinical compliance, and treatment plan adherence (Langebeek et al., 2014).
Patients satisfied with their treatment adhere more to prescribed therapeutic regimens, take an active role in their self-care, and improve their quality of life compared to those dissatisfied with their therapy (Asadi-Lari et al., 2003; Liberato et al., 2016). Individuals treated satisfactorily with services are more likely to remain members of the healthcare facility and adhere to prescribed medication regimens (Holsclaw et al., 2005). Medication non-adherence in HF patients ranged from 18% (Simpson et al., 2021) to 92% (Chang et al., 2018). While the rate of treatment satisfaction among HF patients was 4.2 mean score out of 5 best scores (Bjertnaes et al., 2012). However, no study has assessed treatment adherence and patient satisfaction among HF patients at DBCSH, Ethiopia. Hence, this study aims to evaluate treatment satisfaction and medication adherence and their predictors, which influence treatment outcomes in HF care.
Material and methods
Study setting and participants
A cross-sectional study was conducted on ambulatory HF patients who visited the DBCSH medical referral clinic for HF care from 30 January 2021, to 30 April 2021. The medical referral clinic, one of the specialty clinics in DBCSH, provides cardiac care.
Eligibility criteria
Inclusion criteria
Patients with HF receiving follow-up at an adult ambulatory medical referral clinic of DBCSH, aged 18 years or older, and those with complete medical records were included in the current study.
Exclusion criteria
Study participants who refuses to give informed consent, too sick patient during the interview, admitted patients and those missing their appointment data were excluded from the current study.
Sample size determination and sampling technique
The sample size was estimated using a single population proportion formula. Taking treatment satisfaction proportion in HF patients was 50% to get the possible minimum sample size.
Where n - is the minimum sample size required for a large population (≥10,000)
Z α/2 - is the critical value for a 95% confidence interval (1.96 from Z-table)
p - Prevalence = 50% (0.5)
d - Degree of accuracy desired (the margin of error 5% = 0.05); then the sample size is
The expected number of source population in the study period (N), based on the average number of patients coming to the clinic 3 days a week with a total of 16 weeks was 1,680 (16 × 3 × 35). The corrected sample size, using the following correction formula was 312.6 ≈ 313, Corrected sample size =
Then 10% contingency was added on 313: 313% × 10% = 32.
The final sample size included in the current study was 344.
A systematic random sampling technique was used to select study participants from the Health Management Information Systems (HMIS) list of HF patients at the medical referral clinic of DBCSH.
Data collection procedures and tools
Two nurses and one clinical pharmacist underwent training for data collection, with pharmacists handling clinical data review and nurses conducting patient interviews.
Clinical and demographic data of study participants were collected using pre-tested data abstraction tools and structured questionnaires.
Drug-drug interactions were assessed using Micromedex drug interaction checkers, drugs.com, and up-to-date.
Treatment satisfaction was assessed using the self-administered Medicines Questionnaire (SATMED-Q), consisting of 17 items across six domains: treatment effectiveness (3 items), undesirable side effects (3 items), impact on daily activity (3 items), medical care (2 items), convenience of use (3 items), and global satisfaction (3 items). Each item in a specific domain received an ordinal score on a five-point Likert scale: not at all (0), a little bit (WHO, 2021) point, somewhat satisfied (Schultz et al., 2018) points, quite a bit (Mensah et al., 2015) points, and very much satisfied (Rosengren et al., 2019) points. The sum of the items ranged from 0 to 68 points, with higher scores indicating greater patient treatment satisfaction with the drug therapy. This score was transformed into a more intuitive and easily understandable metric, ranging from a minimum of 0 to a maximum of 100, using the following formula:
Where Ymax is 68 (maximum total score); Ymin is 0 (minimum total score); Yobs is the total score obtained by the patient; and Y′ is the transformed score. A similar expression can be used to change the metric of each domain (Ruiz et al., 2008; Rejas et al., 2011).
Medication adherence was determined using the Morisky Green Levin Medication Adherence Scale (MGLS). It has four items focusing on past medication use patterns with closed dichotomies (yes/no). Each ‘yes’ response was rated as 0 and each ‘no’ response was rated as 1. The total summed score ranges from 0 to 4 and was grouped as good adherence to medication (0–2 points scored) and non-adherence to medication (≥3 points scored) (Beyhaghi et al., 2016).
Data analysis and interpretations
Data entry was conducted using Epidata version 4.2.0, while data analysis was performed using Statistical Package for Social Sciences (SPSS) version 25 software. Descriptive statistics, including frequency, mean, and percentage, were employed to summarize study participant characteristics.
The relationships between predictor variables and treatment satisfaction were assessed using one-way analysis of variance (ANOVA) with post hoc analysis for mean values of more than two continuous variables. For the mean values of two continuous variables, an independent t-test was employed. Binary logistic regression analysis was used to examine the association between predictor variables and medication adherence.
The relationship between the treatment adherence score and total treatment satisfaction scores was elucidated using Spearman’s correlation coefficient.
Ethics approval
The study (P009/01/2021) received ethical clearance from the Debre Berhan University Institutional Review Board. Written informed consent was obtained from all study participants who accepted the invitation to participate. All methods were conducting in accordance with the relevant guidelines and regulations (we followed the declaration of Helenski).
Results
Clinical characteristics and demographic features
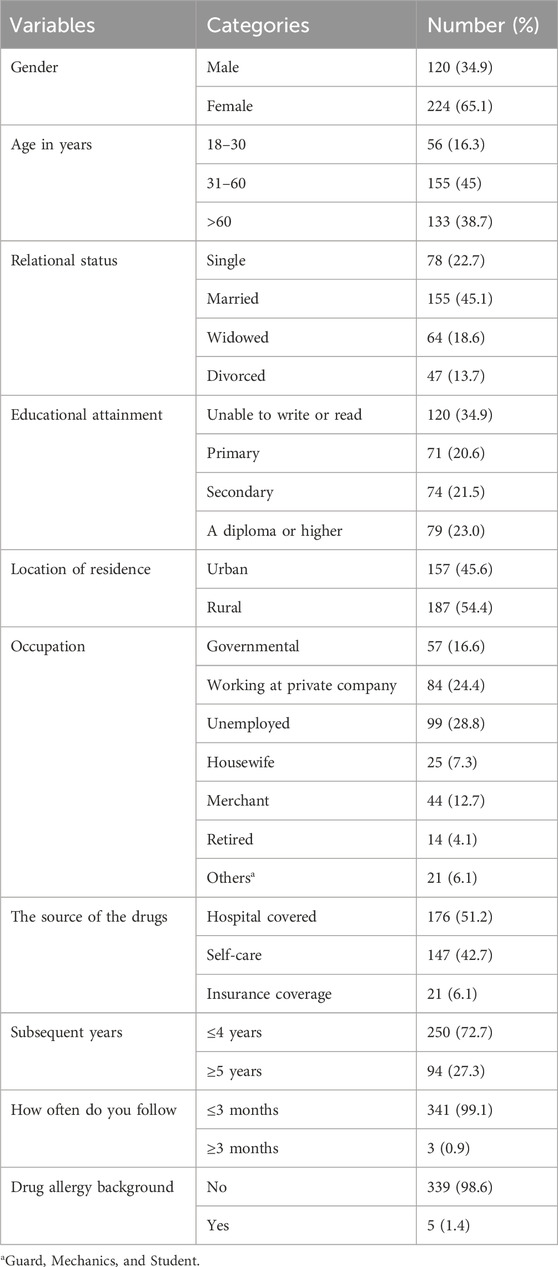
Study participants had a mean age of 53.38 (SD, 18.84) years, and most (45%) were in the age range of 31–60 years. Most of them were females (65.1%), married (45.1%), and residents of rural areas (54.4%). A drug allergy history was not found in 98.6% of study participants. Most study participants (72.7%) had less than 4 years of follow-up with DBCSH (Table 1).
Treatment satisfaction of HF patients
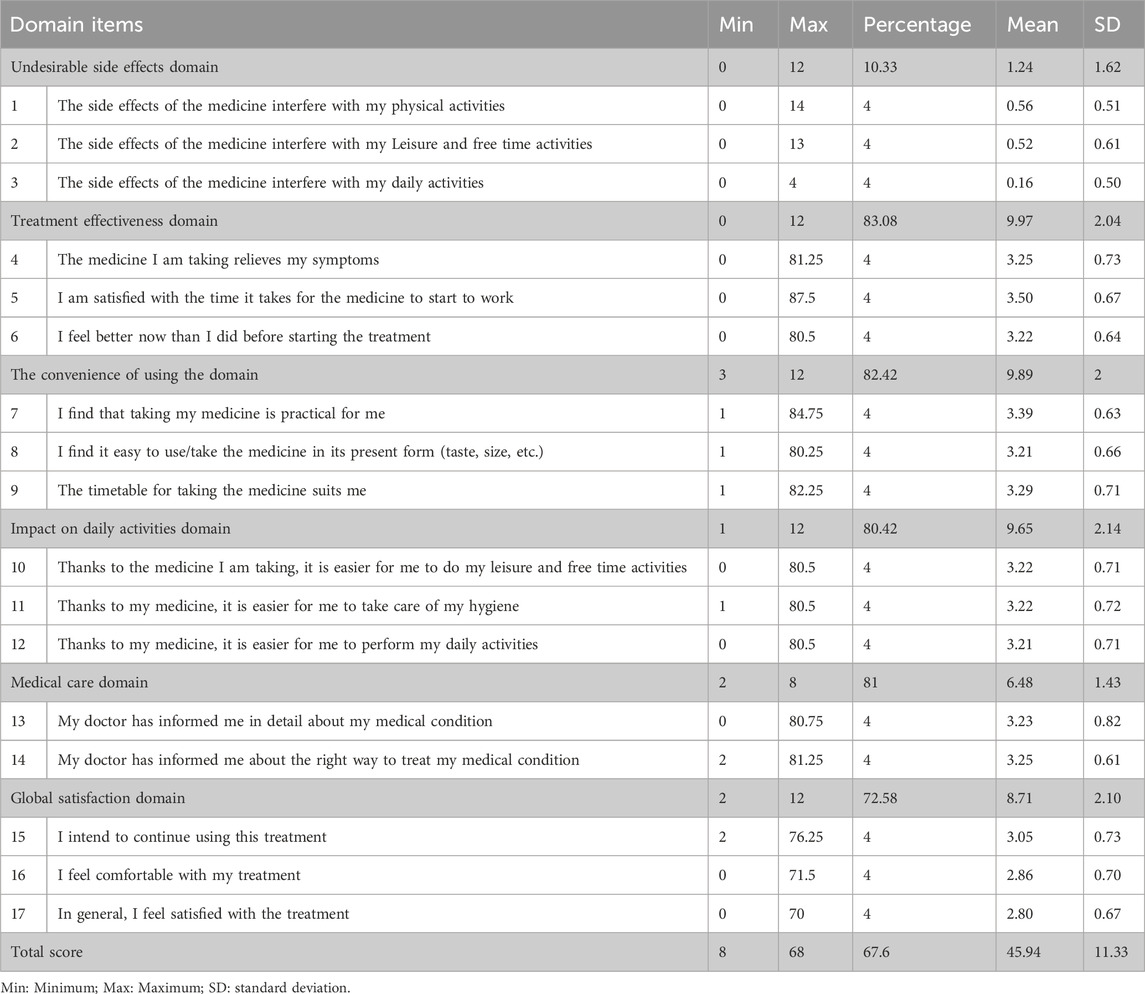
Considering that the scores of the SATMED-Q ranged from 0 to 100 in each domain, the higher the score, the greater the treatment satisfaction with the medicine. The overall treatment satisfaction score of the study participant was 67.6(SD, 11.33). The highest scores were found in the treatment effectiveness 83.08 (SD, 2.04) domain, and the lower scores were reported in the impact on daily activities 80.42 (SD, 2.14) and global satisfaction 72.58 (SD, 2.10) domains. The lowest scores were reported in the side effects 10.33 (SD, 1.62) domain (Table 2).
Treatment satisfaction of HF patients’ relationship with different characteristics of study participants
Participants with a diploma and above education level (mean = 68.73, SD = 5.82), those with comorbidities (mean = 67.82, SD = 6.12), those took one drug, individuals not adhering to salt restrictions (mean = 68.45, SD = 6.52), and participants who had no drug-drug interaction (mean = 68.1, SD = 5.23) exhibited notably higher treatment satisfaction scores than their counterparts (p < 0.05). No significant relationship was observed between treatment satisfaction and the other reported demographic and clinical characteristics (p > 0.05) (Table 3).
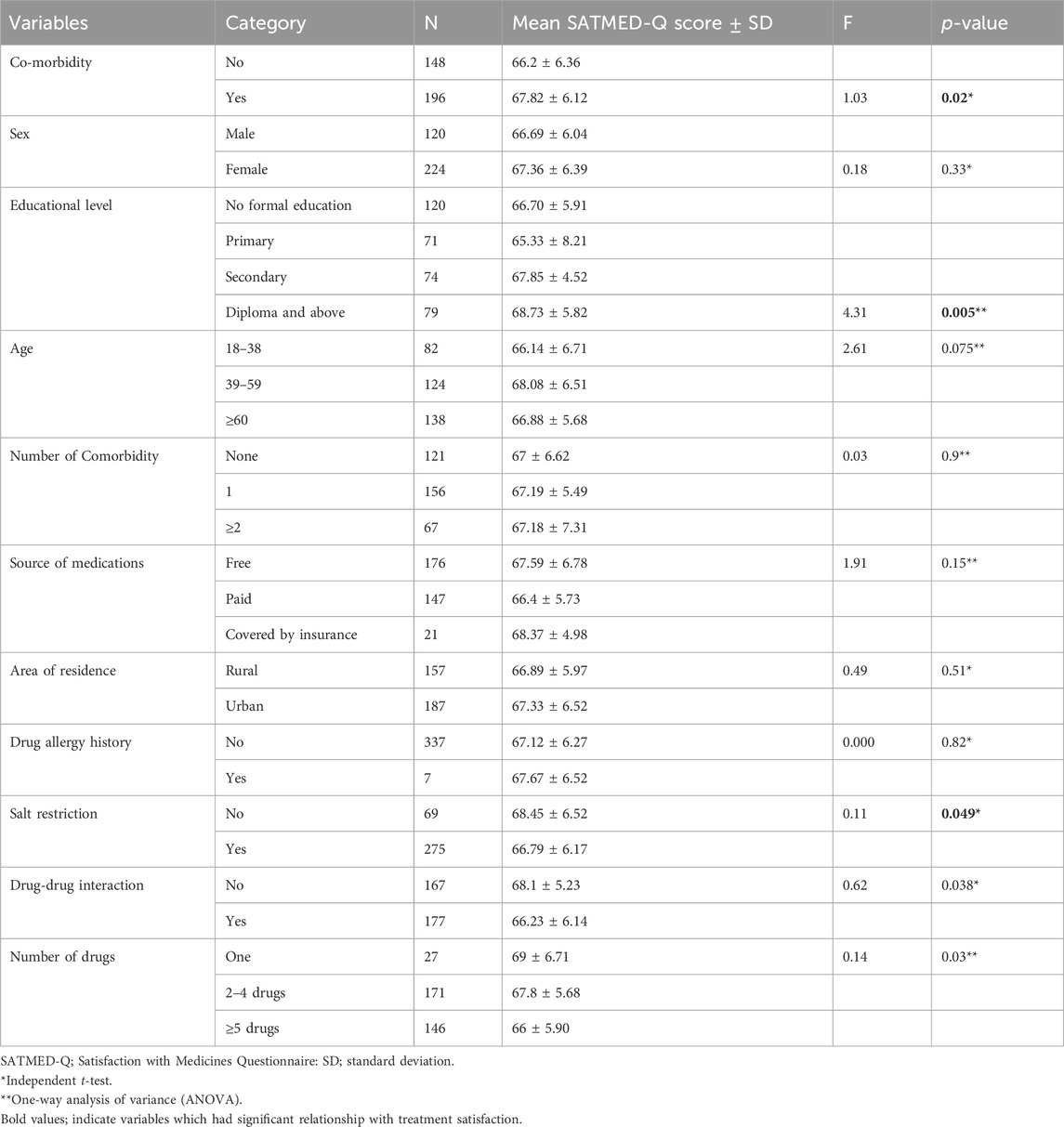
Table 3. Relationship between treatment satisfaction and different demographic and clinical characteristics of patients with HF.
Rates of study participants’ medication adherence
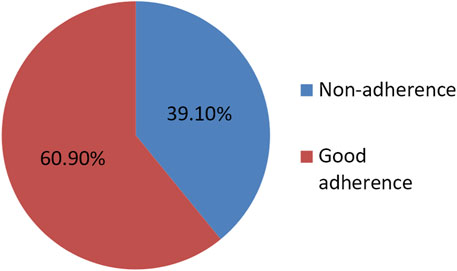
Nearly two-thirds of the study participants exhibited good treatment adherence, with 217 individuals (60.9%), while 127 participants (39.1%) showed low treatment adherence levels (Figure 1).
Contributing factors for medication adherence
In the binary logistic regression analysis, the number of prescribed drugs and occurrences of DDIs were significantly associated with treatment adherence. Study participants who had drug-drug interactions were about 38% less likely to be on medication adherence than participants who did not have drug-drug interactions (AOR = 0.62, 95% CI: 0.54–0.71). In addition, study participants who had taken more than or equal to five drugs were about 68% less likely to adhere to medication than study participants who had taken one drug (AOR = 0.32, 95% CI: 0.2–0.51) (Table 4). The number of medications and drug-drug interactions correlate with medication adherence, respectively, but did not have a causal relationship.
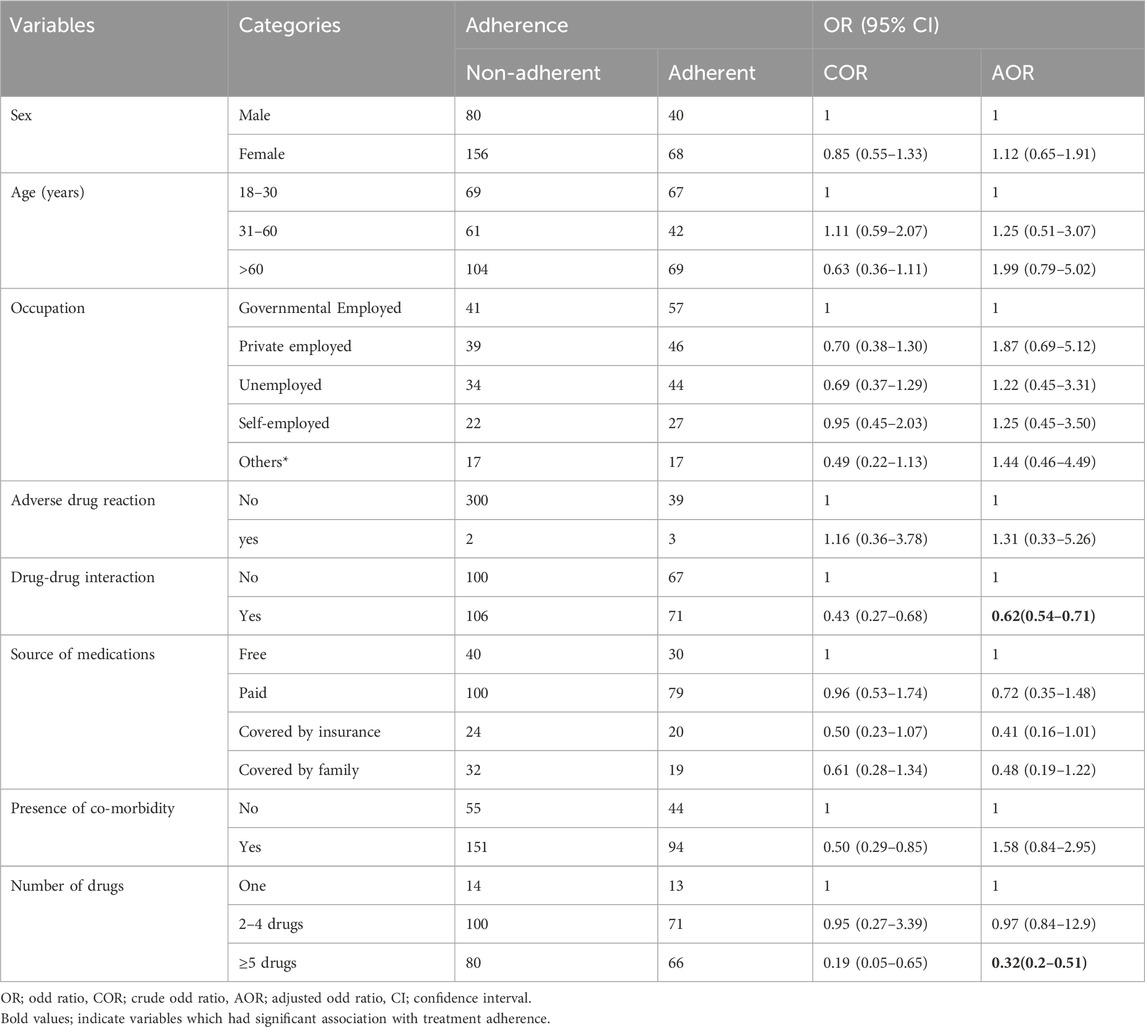
Table 4. Univariable and multivariable analysis of factors associated with treatment adherence in heart failure patients.
The relationship between treatment satisfaction and treatment adherence
There was a significant positive correlation between treatment satisfaction and medication adherence (rs (342) = 0.34, p = 0.027).
Discussion
The study revealed that a treatment satisfaction rate of 67.6% and a medication adherence rate of 60.9% among HF patients.
In medical studies, knowing how satisfied patients are with their treatment is essential to understanding their perspective on care. It is also shown that improving clinical outcomes is connected to increasing patient satisfaction with their care (Al-Jabi et al., 2015).
In this study, most participants were aged 30–59, with an average age of 53.4 years. This was lower than a study in Brazil (average age 60.2, range 28–87) (), but similar to a study in Nigeria (average age 52, range 32–83) (Iloh and Amadi, 2017). But, the study conducted in Greek reported that 74% of participants found in the age range of 18–59 years (Geitona et al., 2008). Age among HF patients was linked to both treatment satisfaction and medication adherence.
More than two-thirds of participants had a co-morbid illness, a finding similar to a Palestinian study (63.2%) (Al-Jabi et al., 2015). Almost three-fourths of the study subjects had received treatment for 4 years or less, in contrast to research in Palestine (Al-Jabi et al., 2015), where the majority had been treated for more than 4 years (69.7%). The variations could be differences in the study participants’ clinical characteristics.
In the current study, participants had an overall treatment satisfaction score was 67.6%. This finding was similar with a study done in Brazil (69.2%) (). However, this result was lower to studies conducted among cancer patients in Greece (85.6%) (Pini et al., 2014), Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia (80.81) (Demoz et al., 2019), Nigeria (78.6%) (Iloh and Amadi, 2017), Greek (more than 80%) (Geitona et al., 2008) but higher than studies from Australia (nearly 65% fully satisfied only) (Candlish et al., 1998) and Addis Ababa, Ethiopia (Seid et al., 2020). These differences may be variations in the definition of treatment satisfaction between studies. Patient satisfaction with therapy is the most reliable indicator of continued medication use, impacting the effectiveness and efficiency of medical care (Zyoud et al., 2013; Iloh and Amadi, 2017). So, satisfaction with medication constitutes a quality indicator that can be used for improving healthcare of chronic patients like HF. The findings imply that barriers to treatment satisfaction of HF patients must be addressed.
The satisfaction scores of the study participants regarding medication side effects were relatively low (10.33%) compared to other domains. This result contrasts with a study in Addis Ababa, Ethiopia (79.3%) (Seid et al., 2020), a study in Palestine (86.0%) (Hope et al., 2004), Brazil (93.5%) (), . The discrepancy may be attributed to differences in the study setting, the number of comorbidities the study participant has, number and types of medication study participants take, severity of illness or the side effect items are being measured incorrectly. The Addis Ababa study by Seid et al. was conducted at a tertiary hospital, where patients might have multiple comorbidities and take multiple drugs, potentially leading to more drug side effects among participants. In addition, it is possible that the patients who participated in this study have different understanding of side effects, different perception of side effects, different perception of the severity of side effects, and different interpretation of the SATMED-Q questions.
The global treatment satisfaction domain score was 72.6% in the current study compared to other dimensions. This result was consistent with a study conducted in Palestine (72.1%) (Al-Jabi et al., 2015), but this finding was greater than a study done in Brazil (69.2%) (). The score in the medical care domain was 81%. This finding was higher than a study done in Estonia (68%) (Polluste et al., 2000). A possible reason for this variation could be the treatment satisfaction assessment tools used.
The occurrence of comorbidity, individuals with a diploma or higher educational level, and those with no salt reduction showed a statistically significant relationship with treatment satisfaction. However, other clinical and socio-demographic characteristics did not exhibit a statistically significant relationship with treatment satisfaction. Additionally, our result was inconsistent with studies reported from China (Fang et al., 2019) and Saudi Arabia (Ammo et al., 2014). Primary factors associated with low satisfaction with healthcare services include waiting time, extensive administrative procedures, appointments, and the attitudes of medical personnel toward patients (Zyoud et al., 2013; Lazarevik and Kasapinov, 2015). Our finding was contradicted with a web-based survey conducted in Macedonia, Serbia, and Bulgaria (Lazarevik and Kasapinov, 2015).
In the current study, most heart failure (HF) patients showed good treatment adherence (60.9%). This result was higher than a study in Yemen (45.8%) (Alakhali et al., 2013) but lower than in the Brazil (77%) (Da Silva et al., 2015).
It also aligned with findings from other studies (Murray et al., 2007; Bisharat et al., 2012; Zhao et al., 2015). These variations could be due to differences in how treatment adherence is measured, the patient-care strategies used by pharmacists, and differences in the definition of adherence. For example, our study was conducted at DBCSH, a referral hospital in a resource-limited setting, with participants dealing with complex medical conditions and multiple medications, leading to a lower treatment adherence rate compared to other study locations. Low adherence among patients with HF is adversely affecting clinical results and leading to greater HF exacerbations, lower physical activity, and a greater likelihood of hospitalization and mortality. Our study found that study participants had a low medication adherence rate; thus, effective interventions are needed to increase medication adherence and achieve improved medical outcomes.
Participants taking five or more drugs were 68% less likely to adhere to treatment compared to those using only one drug. This finding aligns with studies conducted in the United States of America and Iran, emphasizing that a higher pill burden could decrease treatment adherence (Knafl and Riegel, 2014b).
Strengths and limitations of the study
This study has several limitations and strengths. The cross-sectional nature of the study precludes establishing a causal relationship between the demographic and clinical characteristics of study participants and the outcome variable. However, there is possibility of pseudo-correlation remains for drug-drug interactions, and it is not clear whether there is a causal relationship or not. The collected data was primarily obtained from study participants’ self-reports during interviews. Skipping essential information and recall bias may impact the study’s overall treatment satisfaction and adherence. Despite these limitations, this study suggests that healthcare personnel should prioritize counseling HF patients about symptoms, and non-pharmacological and pharmacological treatment to enhance treatment satisfaction and medication adherence.
Conclusion
In conclusion, the study revealed a treatment satisfaction rate of 67.6% and a medication adherence rate of 60.9% among HF patients. The statistically significant association between drug-drug interactions (DDI) and the number of drugs used highlights the importance of addressing these factors for improving treatment adherence. The correlation between medication adherence and drug-drug interactions remains a possible pseudo-correlation via the number of medications taken. Therefore, it is imperative for medical facilities to ensure the provision of quality services and all necessary resources to enhance treatment satisfaction and medication adherence among heart failure patients. This may involve optimizing healthcare processes, reducing drug interactions, and promoting comprehensive patient care.
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Debre Berhan University Institutional Review Board (P009/01/2021). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AT: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing–original draft, Writing–review and editing. BE: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing–original draft, Writing–review and editing. HH: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing–original draft, Writing–review and editing. YW: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing–original draft, Writing–review and editing. SA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing–original draft, Writing–review and editing. BK: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing–original draft, Writing–review and editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We truly thank all the study participants who volunteered for this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aggarwal, B., Pender, A., Mosca, L., and Mochari-Greenberger, H. (2015). Factors associated with medication adherence among heart failure patients and their caregivers. J. Nurs. Educ. Pract. 5 (3), 22–27. doi:10.5430/jnep.v5n3p22
Alakhali, K. M., Daniel, P. S., Noohu, A. M., and Sirajudeen, S. A. (2013). Patient medication adherence and physician prescribing among congestive heart failure patients of Yemen. Indian J. Pharm. Sci. 75, 557–562.
Ali, S., Misganaw, A., Worku, A., Destaw, Z., Negash, L., Bekele, A., et al. (2020). The burden of cardiovascular diseases in Ethiopia from 1990 to 2017: evidence from the Global Burden of Disease Study. Int. Health 13, 318–326. doi:10.1093/inthealth/ihaa069
Al-Jabi, S. W., Zyoud, S. H., Sweileh, W. M., Wildali, A. H., Saleem, H. M., Aysa, H. A., et al. (2015). Relationship of treatment satisfaction to health-related quality of life: findings from a cross-sectional survey among hypertensive patients in Palestine. Health Expect. 18 (6), 3336–3348. doi:10.1111/hex.12324
Amininasab, S., Lolaty, H., Moosazadeh, M., and Shafipour, V. (2018). Medication adherence and its predictors among patients with heart failure. Nurs. Midwifery Stud. 7 (2), 81–86. doi:10.4103/nms.nms_9_17
Ammo, M. A., Abu-Shaheen, A. K., Kobrosly, S., and Al-Tannir, M. A. (2014). Determinants of patient satisfaction at tertiary care centers in Lebanon. Open J. Nurs. 4 (13), 939–946. doi:10.4236/ojn.2014.413100
Asadi-Lari, M., Packham, C., and Gray, D. (2003). Patients' satisfaction and quality of life in coronary artery disease. Health Qual. life outcomes 1, 57. doi:10.1186/1477-7525-1-57
Benjamin, E. J., Virani, S. S., Callaway, C. W., Chamberlain, A. M., Chang, A. R., Cheng, S., et al. (2018). Heart disease and stroke statistics-2018 update: a report from the American heart association USA. Report No.: 0009-7322 Contract No.: 12.
Beyhaghi, H., Reeve, B. B., Rodgers, J. E., and Stearns, S. C. (2016). Psychometric properties of the four-item Morisky green levine medication adherence scale among atherosclerosis risk in communities (ARIC) study participants. Value Health 19 (8), 996–1001. doi:10.1016/j.jval.2016.07.001
Bisharat, B., Hafi, L., Baron-Epel, O., Armaly, Z., and Bowirrat, A. (2012). Pharmacist counseling to cardiac patients in Israel prior to discharge from hospital contribute to increasing patient's medication adherence closing gaps and improving outcomes. J. Transl. Med. 10, 34. doi:10.1186/1479-5876-10-34
Bjertnaes, O. A., Sjetne, I. S., and Iversen, H. H. (2012). Overall patient satisfaction with hospitals: effects of patient-reported experiences and fulfilment of expectations. BMJ Qual. Saf. 21 (1), 39–46. doi:10.1136/bmjqs-2011-000137
Candlish, P., Watts, P., Redman, S., Whyte, P., and Lowe, J. (1998). Elderly patients with heart failure: a study of satisfaction with care and quality of life. Int. J. Qual. Health Care 10 (2), 141–146. doi:10.1093/intqhc/10.2.141
Chang, L. L., Xu, H., DeVore, A. D., Matsouaka, R. A., Yancy, C. W., Fonarow, G. C., et al. (2018). Timing of postdischarge follow-up and medication adherence among patients with heart failure. J. Am. Heart Assoc. 7 (7), e007998. doi:10.1161/JAHA.117.007998
Chiatti, C., Bustacchini, S., Furneri, G., Mantovani, L., Cristiani, M., Misuraca, C., et al. (2012). The economic burden of inappropriate drug prescribing, lack of adherence and compliance, adverse drug events in older people: a systematic review. Drug Saf. 35 (Suppl. 1), 73–87. doi:10.1007/BF03319105
Da Silva, A. F., Cavalcanti, A. C., Malta, M., Arruda, C. S., Gandin, T., da Fé, A., et al. (2015). Treatment adherence in heart failure patients followed up by nurses in two specialized clinics. Rev. Lat. Am. Enferm. 23, 888–894. doi:10.1590/0104-1169.0268.2628
Davis, E. M., Packard, K. A., and Jackevicius, C. A. (2014). The pharmacist role in predicting and improving medication adherence in heart failure patients. J. Manag. care & specialty Pharm. 20 (7), 741–755. doi:10.18553/jmcp.2014.20.7.741
Demoz, G. T., Berha, A. B., Alebachew Woldu, M., Yifter, H., Shibeshi, W., and Engidawork, E. (2019). Drug therapy problems, medication adherence and treatment satisfaction among diabetic patients on follow-up care at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. PLOS ONE 14, e0222985. doi:10.1371/journal.pone.0222985
Fang, J., Liu, L., and Fang, P. (2019). What is the most important factor affecting patient satisfaction–A study based on gamma coefficient. Patient Prefer. adherence 13, 515–525. doi:10.2147/PPA.S197015
Fernandez-Lazaro, C. I., García-González, J. M., Adams, D. P., Fernandez-Lazaro, D., Mielgo-Ayuso, J., Caballero-Garcia, A., et al. (2019). Adherence to treatment and related factors among patients with chronic conditions in primary care: a cross-sectional study. BMC Fam. Pract. 20 (1), 132. doi:10.1186/s12875-019-1019-3
Fitzgerald, A. A., Powers, J. D., Ho, P. M., Maddox, T. M., Peterson, P. N., Allen, L. A., et al. (2011). Impact of medication nonadherence on hospitalizations and mortality in heart failure. J. cardiac Fail. 17 (8), 664–669. doi:10.1016/j.cardfail.2011.04.011
Geitona, M., Kyriopoulos, J., Zavras, D., Theodoratou, T., and Alexopoulos, E. C. (2008). Medication use and patient satisfaction: a population-based survey. Fam. Pract. 25 (5), 362–369. doi:10.1093/fampra/cmn068
Holsclaw, S. L., Olson, K. L., Hornak, R., and Denham, A. M. (2005). Assessment of patient satisfaction with telephone and mail interventions provided by a clinical pharmacy cardiac risk reduction service. J. Manag. Care Pharm. 11 (5), 403–409. doi:10.18553/jmcp.2005.11.5.403
Hope, C. J., Wu, J., Tu, W., Young, J., and Murray, M. D. (2004). Association of medication adherence, knowledge, and skills with emergency department visits by adults 50 years or older with congestive heart failure. Am. J. health-system Pharm. AJHP official J. Am. Soc. Health-System Pharm. 61 (19), 2043–2049. doi:10.1093/ajhp/61.19.2043
Iloh, G. U. P., and Amadi, A. N. (2017). Treatment satisfaction, medication adherence, and blood pressure control among adult Nigerians with essential hypertension. Int. J. Health & Allied Sci. 6 (2), 75.
Knafl, GJRB, and Riegel, B. (2014a). What puts heart failure patients at risk for poor medication adherence? Patient Prefer. adherence 8, 1007–1018. doi:10.2147/PPA.S64593
Knafl, GJRB., and Riegel, B. (2014b). What puts heart failure patients at risk for poor medication adherence? Patient Prefer Adherence 8, 1007–1018. doi:10.2147/PPA.S64593
Langebeek, N., Sprenger, H. G., Gisolf, E. H., Reiss, P., Sprangers, M. A., Legrand, J., et al. (2014). A simplified combination antiretroviral therapy regimen enhances adherence, treatment satisfaction and quality of life: results of a randomized clinical trial. HIV Med. 15 (5), 286–290. doi:10.1111/hiv.12112
Lazarevik, V., and Kasapinov, B. (2015). Predictors of patients' satisfaction with health care services in three Balkan countries (Macedonia, Bulgaria and Serbia): a cross country survey. Acta Inf. Med. 23 (1), 53–56. doi:10.5455/aim.2015.23.53-56
Lee, D., Mansi, I., Bhushan, S., and Parish, R. (2015). Non-adherence in at-risk heart failure patients: characteristics and outcomes;1(5).
Lesyuk, W., Kriza, C., and Kolominsky-Rabas, P. (2018). Cost-of-illness studies in heart failure: a systematic review 2004–2016. BMC Cardiovasc. Disord. 18 (1), 74. doi:10.1186/s12872-018-0815-3
Liberato, A. C. S., Rodrigues, R. C. M., São-João, T. M., Alexandre, N. M. C., and Gallani, MCBJ (2016). Satisfaction with medication in coronary disease treatment: psychometrics of the Treatment Satisfaction Questionnaire for Medication. Rev. latino-americana Enferm. 24, e2705. doi:10.1590/1518-8345.0745.2705
Mann, D. L., and Chakinala, M. (2018). “Heart failure: pathophysiology and diagnosis,” in Harrison's principles of internal medicine. Editors J. L. Jameson, A. S. Fauci, D. L. Kasper, S. L. Hauser, D. L. Longo, and J. Loscalzo 20e. (New York, NY: McGraw-Hill Education).
Mensah, G. A., Roth, G. A., Sampson, U. K., Moran, A. E., Feigin, V. L., Forouzanfar, M. H., et al. (2015). Mortality from cardiovascular diseases in sub-Saharan Africa, 1990-2013: a systematic analysis of data from the Global Burden of Disease Study 2013. Cardiovasc. J. Afr. 26 (2 Suppl. 1), S6–S10. doi:10.5830/CVJA-2015-036
Meyer, J. C., Schellack, N., Stokes, J., Lancaster, R., Zeeman, H., Defty, D., et al. (2017). Ongoing initiatives to improve the quality and efficiency of medicine use within the public healthcare system in South Africa; A preliminary study. Front. Pharmacol. 8 (751), 751. doi:10.3389/fphar.2017.00751
Murray, M. D., Tu, W., Wu, J., Morrow, D., Smith, F., and Brater, D. C. (2009). Factors associated with exacerbation of heart failure include treatment adherence and health literacy skills. Clin. Pharmacol. Ther. 85 (6), 651–658. doi:10.1038/clpt.2009.7
Murray, M. D., Young, J., Hoke, S., Tu, W., Weiner, M., Morrow, D., et al. (2007). Pharmacist intervention to improve medication adherence in heart failure: a randomized trial. Ann. Intern Med. 146, 714–725. doi:10.7326/0003-4819-146-10-200705150-00005
Page, R. L., O’Bryant, C. L., Cheng, D., Dow, T. J., Ky, B., Stein, C. M., et al. (2016). Drugs that may cause or exacerbate heart failure: a scientific statement from the American Heart Association. Circulation 134 (6), e32–e69. doi:10.1161/CIR.0000000000000426
Pallangyo, P., Millinga, J., Bhalia, S., Mkojera, Z., Misidai, N., Swai, H. J., et al. (2020). Medication adherence and survival among hospitalized heart failure patients in a tertiary hospital in Tanzania: a prospective cohort study. BMC Res. Notes 13 (1), 89. doi:10.1186/s13104-020-04959-w
Parker, R. B., Nappi, J. M., and Cavallari, L. H. (2020). “Chronic heart failure,” in Pharmacotherapy: a pathophysiologic approach. 11th edn, Editors J. T. DiPiro, G. C. Yee, L. M. Posey, S. T. Haines, T. D. Nolin, and V. Ellingrod (New York, NY: McGraw-Hill Education).
Pini, A., Sarafis, P., Malliarou, M., Tsounis, A., Igoumenidis, M., Bamidis, P., et al. (2014). Assessment of patient satisfaction of the quality of health care provided by outpatient services of an oncology hospital. Glob. J. health Sci. 6 (5), 196–203. doi:10.5539/gjhs.v6n5p196
Polluste, K., Kalda, R., and Lember, M. (2000). Primary health care system in transition: the patient's experience. Int. J. Qual. Health Care 12 (6), 503–509. doi:10.1093/intqhc/12.6.503
Ponikowski, P., Voors, A. A., Anker, S. D., Bueno, H., Cleland, J. G. F., Coats, A. J. S., et al. (2016). 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 37 (27), 2129–2200. doi:10.1093/eurheartj/ehw128
Rehman, Z. U., Siddiqui, A. K., Karim, M., Majeed, H., and Hashim, M. (2019). Medication non-adherence among patients with heart failure. Cureus 11 (8), e5346. doi:10.7759/cureus.5346
Rejas, J., Ruiz, M. A., Pardo, A., and Soto, J. (2011). Minimally important difference of the treatment satisfaction with Medicines questionnaire (SATMED-Q). BMC Med. Res. Methodol. 11 (1), 142–149. doi:10.1186/1471-2288-11-142
Riegel, B., Lee, C. S., and Dickson, V. V.Medscape (2011). Self-care in patients with chronic heart failure. Nat. Rev. Cardiol. 8 (11), 644–654. doi:10.1038/nrcardio.2011.95
Rosengren, A., Smyth, A., Rangarajan, S., Ramasundarahettige, C., Bangdiwala, S. I., AlHabib, K. F., et al. (2019). Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: the Prospective Urban Rural Epidemiologic (PURE) study. Lancet Glob. Health 7 (6), e748–e760. doi:10.1016/S2214-109X(19)30045-2
Ruiz, M. A., Pardo, A., Rejas, J., Soto, J., Villasante, F., and Aranguren, J. L. (2008). Development and validation of the "treatment satisfaction with Medicines questionnaire" (SATMED-Q). Value health J. Int. Soc. Pharmacoeconomics Outcomes Res. 11 (5), 913–926. doi:10.1111/j.1524-4733.2008.00323.x
Schultz, W. M., Kelli, H. M., Lisko, J. C., Varghese, T., Shen, J., Sandesara, P., et al. (2018). Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation 137 (20), 2166–2178. doi:10.1161/CIRCULATIONAHA.117.029652
Seid, E., Engidawork, E., Alebachew, M., Mekonnen, D., and Berha, A. B. (2020). Evaluation of drug therapy problems, medication adherence, and treatment satisfaction among heart failure patients on follow-up at a tertiary care hospital in Ethiopia. PloS one 15 (8), e0237781. doi:10.1371/journal.pone.0237781
Shah, D., Simms, K., Barksdale, D. J., and Wu, J.-R. (2015). Improving medication adherence of patients with chronic heart failure: challenges and solutions. Res. Rep. Clin. Cardiol. 6, 87–95. doi:10.2147/rrcc.s50658
Simpson, J., Jackson, C. E., Haig, C., Jhund, P. S., Tomaszewski, M., Gardner, R. S., et al. (2021). Adherence to prescribed medications in patients with heart failure: insights from liquid chromatography-tandem mass spectrometry-based urine analysis. Eur. Heart J. Cardiovasc. Pharmacother. 7 (4), 296–301. doi:10.1093/ehjcvp/pvaa071
WHO (2021). Cardiovascular diseases. Available at: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (Accessed October 5, 2021).
Wu, J.-R., Moser, D. K., De Jong, M. J., Rayens, M. K., Chung, M. L., Riegel, B., et al. (2009). Defining an evidence-based cutpoint for medication adherence in heart failure. Am. Heart J. 157 (2), 285–291. doi:10.1016/j.ahj.2008.10.001
Zhao, S. J., Zhao, H. W., Du, S., and Qin, Y. H. (2015). The impact of clinical pharmacist support on patients receiving multi-drug therapy for coronary heart disease in China. Indian J. Pharm. Sci. 77, 306–311. doi:10.4103/0250-474x.159632
Keywords: treatment satisfaction, medication adherence, heart failure, Ethiopia, Debre Berhan comprehensive specialized hospital
Citation: Tsige AW, Endalifer BL, Habteweld HA, Wondmkun YT, Ayele SG and Kefale B (2024) Treatment satisfaction and medication adherence and predictors among patients with heart failure in Ethiopia: a hospital-based cross-sectional study. Front. Pharmacol. 15:1399177. doi: 10.3389/fphar.2024.1399177
Received: 13 March 2024; Accepted: 02 July 2024;
Published: 29 July 2024.
Edited by:
Tomoya Tachi, Nagoya City University, JapanReviewed by:
Ebere Emilia Ayogu, University of Nigeria, Nsukka, NigeriaHirofumi Tamaki, Gifu Pharmaceutical University, Japan
Copyright © 2024 Tsige, Endalifer, Habteweld, Wondmkun, Ayele and Kefale. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abate Wondesen Tsige, YWJhdGV3b25kZXNlbkBkYnUuZWR1LmV0
 Abate Wondesen Tsige
Abate Wondesen Tsige Bedilu Linger Endalifer
Bedilu Linger Endalifer Habtemariam Alekaw Habteweld
Habtemariam Alekaw Habteweld Yehualashet Teshome Wondmkun
Yehualashet Teshome Wondmkun Siraye Genzeb Ayele
Siraye Genzeb Ayele Belayneh Kefale
Belayneh Kefale