- 1Department of Family Medicine, China Medical University Hospital, China Medical University, Taichung, Taiwan
- 2Department of Health Policy and Management, Chung Shan Medical University, Taichung, Taiwan
- 3Department of Medical Management, Chung Shan Medical University Hospital, Taichung, Taiwan
- 4Department of Healthcare Administration, Asia University, Taichung, Taiwan
- 5Department of Medical Research, China Medical University Hospital, China Medical University, Taichung, Taiwan
- 6Department of Health Services Administration, China Medical University, Taichung, Taiwan
Introduction: Cancer prevention and treatment, particularly lung cancer, remain major healthcare challenges in Taiwan and globally. This study investigates factors and healthcare utilization patterns associated with adjunctive Chinese herbal medicine (CHM) therapy in non-small cell lung cancer (NSCLC) patients.
Methods: Using Taiwan’s National Health Insurance Research Database and the Taiwan Cancer Registry, we conducted a retrospective cohort study of non-small cell lung cancer patients diagnosed between 2007 and 2013. Descriptive analysis, propensity score matching, and regression models were employed to assess CHM therapy utilization and its impact on emergency department visits and hospitalization days.
Results: Among 43,122 non-small cell lung cancer patients, 5.76% received adjunctive CHM therapy, with the majority at stage IV cancer. Factors such as cancer stage, age, gender, marital status, education level, monthly salary, degree of urbanization, severity of comorbidity, comorbid diseases, hospital ownership, experience of using Chinese medicine, chemotherapy status, and years of diagnosis are significantly associated with whether NSCLC patients receive adjunctive CHM therapy. Patients receiving adjunctive CHM therapy for 181–365 days reduced emergency department visits by 16% (OR = 0.84, 95%CI: 0.74-0.95) and shortened hospitalization days by 17% (Ratio = 0.83, 95%CI: 0.75-0.91).
Conclusion: Prolonged adjunctive CHM therapy, particularly for 181–365 days, is associated with decreased healthcare utilization among non-small cell lung cancer patients. These findings suggest a potential role for extended CHM therapy in managing NSCLC and warrant consideration by clinical teams.
Introduction
Cancer has been the leading cause of death among the Taiwanese population for 40 years now. In 2022, the cancer mortality rate was 222.7 per 100,000 population. The top three cancer mortality rates were (1) tracheal, bronchus, and lung cancer; (2) liver and intrahepatic bile duct cancer; and (3) colorectal and anal cancer (Ministry of Health and Welfare, 2023). In March 2021, the World Health Organization (WHO) reported that cancer was the leading cause of global deaths in 2020, resulting in nearly ten million deaths. The three most common types of cancer by incidence in the same year were breast cancer (2.26 million), lung cancer (2.21 million), and colorectal cancer (1.93 million). The top three cancers causing death were lung cancer (1.80 million), colorectal cancer (935,000), and liver cancer (830,000) (Cancer Organization, 2021). Looking at both Taiwan and globally, cancer prevention and treatment are major healthcare priorities, with lung cancer being particularly significant. The most common primary malignant tumor in the lungs is epithelial carcinoma, which can be broadly categorized into small cell lung carcinoma (SCLC) and non-small cell lung carcinoma (NSCLC). Non-small cell lung carcinoma accounts for approximately 85% of lung cancers. Histologically, it is divided into adenocarcinoma, squamous cell carcinoma (SCC), and large cell carcinoma (Medscape, 2021). The main treatment modalities include surgical resection, chemotherapy, radiation therapy, targeted therapy, and immunotherapy. Early-stage lung cancer often responds well to treatment, but the mortality rate remains high in advanced stages (Hirsch et al., 2017).
Cancer patients endure significant physical and psychological distress during the treatment process. The side effects of medications and the fear of cancer recurrence often diminish the effectiveness of treatments. As a result, cancer patients often seek alternative therapies in addition to conventional Western medicine. These may include acupuncture and moxibustion, qigong therapy, herbal medicine, dietary therapy, and other approaches that aim to alleviate symptoms and improve overall wellbeing. Complementary and Alternative Medicine (CAM) is embraced by some cancer patients, with research indicating that, on average, patients use one to two types of CAM, which can enhance their quality of life (Kuo et al., 2018). Given that Traditional Chinese Medicine (TCM) therapy is covered by Taiwan’s National Health Insurance, 62.5% of the population seeks Traditional Chinese Herbal Medicines (TCHM) as part of their treatment regimen (Chen et al., 2007). In today’s world, where Western medicine dominates, TCM is recognized as an important form of CAM. Of course, in many countries in Asia, TCM is one of the mainstream medical systems.
In 2009, a study conducted in Hong Kong surveyed 786 cancer patients regarding their use of TCM therapy. The study found that 57.1% of cancer patients utilized a combination of Chinese and Western medicine. Among patients undergoing chemotherapy, a higher proportion sought TCM therapy compared to those undergoing other forms of Western medical treatment (Lam et al., 2009). In 2018, a cross-sectional survey conducted in mainland China involving 590 cancer patients revealed that younger patients (aged less than 60) and those in the early stages of cancer significantly sought TCM therapy (Sun et al., 2018). In 2020, a study conducted in China involving 1950 cancer patients from the southern region examined the use of TCM therapy. The results indicated that cancer patients with higher levels of education (more than 12 years) tended to opt for TCM therapy. Among those who used TCM, 54.61% primarily used Chinese herbal medicine. Additionally, the majority of TCM users (54.51%) underwent treatment for more than 6 months (Xiong et al., 2020).
Previous studies on healthcare utilization among lung cancer patients have often focused on palliative care in the terminal stages, outpatient, inpatient, and intensive care unit (ICU) utilization rates, as well as the proportions of different treatment modalities. Research conducted in Australia on patients with advanced non-small cell lung cancer found that 83% sought palliative care and 82% sought psychosocial support care. However, seeking both types of care did not provide any survival benefit (Duggan et al., 2019). Research comparing healthcare utilization in the last 6 months of life between lung cancer patients and those with chronic obstructive pulmonary disease (COPD) found that COPD patients had higher rates of outpatient visits and ICU admissions, while lung cancer patients had higher utilization of palliative care (Au et al., 2006). American scholars have studied the healthcare utilization of terminally ill lung cancer patients and found that women are more likely than men to use hospitalization, nursing homes, home care, and end-of-life care (Shugarman et al., 2008). Research conducted in mainland China on lung cancer patients has shown an association between comorbidities and healthcare utilization. Comorbidities increase the annual outpatient and inpatient visits among lung cancer patients, increase the probability of choosing chemotherapy and radiotherapy, but decrease the probability of choosing surgery (Ding et al., 2020). Most studies using TCM and CHM in NSCLC were mainly based on survival analysis and treatment effect. The combined-treatment group had better physical function and role function than the Western medicine group at 6 months (p < 0.05) (Tang et al., 2016). The use of CHM as an adjunctive therapy may reduce the mortality hazard ratio of lung cancer patients (Li et al., 2018).
The above literature suggests that past studies on healthcare utilization among lung cancer patients have lacked discussion on the impact of adjunctive TCM therapy and on the research regarding emergency department visits and length of hospitalization. Emergency department utilization and length of hospitalization are important indicators of medical care. Previous studies have pointed out the factors that cancer patients tend to receive adjunctive TCM therapy, including those who have received chemotherapy, those under the age of 60, those with early-stage cancer, and those with higher education levels (Lam et al., 2009; Sun et al., 2018; Xiong et al., 2020). This study would like to explore the factors associated with NSCLC patients receiving adjunctive TCM treatments in Taiwan.
The purpose of this study is to investigate the factors influencing NSCLC patients' acceptance of adjunctive TCM therapy and to explore the difference in emergency medical utilization and length of hospitalization among NSCLC patients based on the duration of adjunctive TCM therapy.
Materials and methods
Data sources
This study adopted a retrospective study design. Data were sourced from the National Health Insurance research databases (NHIRD) from the Health and Welfare Data Science Center of the Ministry of Health and Welfare, covering the period from 2000 to 2018, as well as the Cancer Registry issued by the Health Promotion Administration, the Cause of Death Data issued by the Department of Statistics of the Ministry of Health and Welfare, and the Household Registration Database from the Ministry of the Interior. Currently, the national health insurance coverage rate in Taiwan is 99.82%, making it a representative evidence-based medical database.
Research participants
The inclusion criteria for the study participants were newly diagnosed NSCLC patients, obtained from the Cancer Registry from 2007 to 2013, with observation follow-up until the end of 2018. The lung cancer codes in the Cancer Registry are based on the International Classification of Diseases for Oncology third edition (ICD-O-3 code): C33∼C34. A total of 76,232 individuals were identified. Exclusion criteria were: (1) unclear cancer diagnosis date and time; (2) small cell carcinoma (ICD-O-3 codes: 8041, 8042, 8043, 8044, 8045); (3) in situ carcinoma/lung cancer stage 0; (4) unspecified stage; (5) prior history of other cancers before lung cancer diagnosis because this study focused on NSCLC; (6) age less than 20 years old; (7) no active treatment within 1 year, to avoid interference from patients who did not actively seek treatment; (8) unspecified level of the main treatment institution; (9) death within 3 months (90 days) of diagnosis, because it was impossible to track and observe. After exclusions, a total of 43,122 individuals were included in the study.
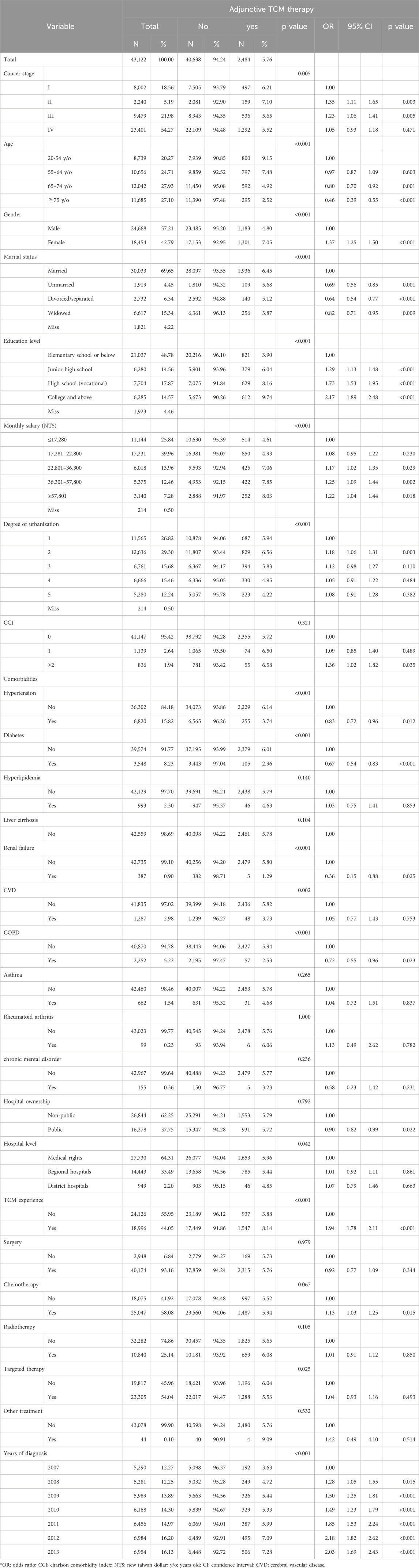
In order to mitigate the influence of individual characteristics, cancer stage, and disease severity on whether lung cancer patients received adjunctive TCHM therapy, this study employed Propensity Score Matching (PSM) at a ratio of 1:5, taking into account the different personal characteristics, socioeconomic status, comorbidities, and severity of cancer. The matching controlled for variables including cancer stage, gender, age, monthly income, education level, marital status, severity of comorbidity, medical history (diabetes, cirrhosis, renal failure, cerebrovascular disease, chronic obstructive pulmonary disease), cancer diagnosis year, and whether surgery was performed within 90 days. Precise matching was conducted for lung cancer patients who received adjunctive TCHM therapy and those who did not, based on cancer stage, gender, age, and severity of comorbidity. After matching, there were a total of 2,308 lung cancer patients who received adjunctive TCHM therapy and 11,540 lung cancer patients who did not, resulting in a total of 13,848 individuals included in the study analysis (Figure 1; Table 1).
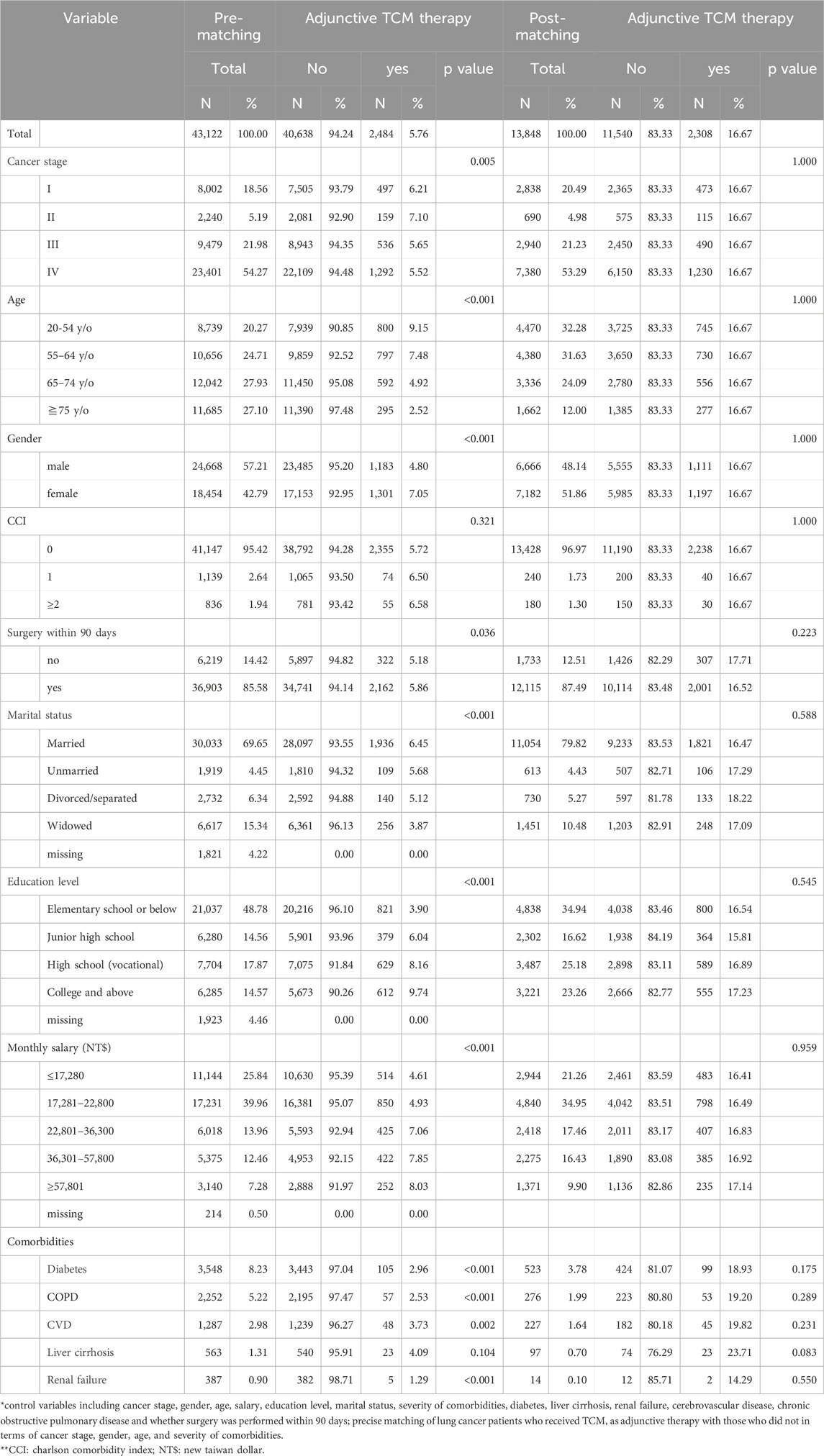
Table 1. Descriptive analysis before and after matching whether patients with NSCLC receive adjunctive TCM therapy.
Variable definition and explanation
The inclusion criteria for receiving adjunctive TCHM therapy were defined as follows: The first diagnosis code for lung cancer during the visit to a Chinese medicine practitioner must be lung cancer. Patients who used adjunctive TCHM therapy for less than 30 days within 1 year after diagnosis were defined as non-users of adjunctive TCHM therapy, while those who used adjunctive TCHM therapy for 30 days or more within 1 year after diagnosis were defined as users (Lin et al., 2015). Subsequently, the use of adjunctive TCHM therapy within 1 year after diagnosis was further divided into three groups: <30 days, 30–180 days, and 181–365 days. The experience of using Chinese medicine referred to whether patients had visited a Chinese medicine department in the 2 years before being diagnosed with NSCLC. Emergency department utilization by patients referred to whether NSCLC patients visited the emergency department within 1 year after diagnosis. The total number of hospitalization days for patients referred to the total number of hospitalization days within 1 year after diagnosis of NSCLC. When we analyzed the emergency department utilization of patients with NSCLC, regardless of whether the diagnosis of the emergency department visits was lung cancer, if there were emergency department visits, they had been counted. Because NSCLC and its treatment have many complications, any emergency visits may be related to NSCLC or treatments.
Basic personal information includes gender, age, marital status, and education level. Gender is divided into male and female. Age is divided into five age groups: 20–54 years old, 55–64 years old, 65–74 years old, ≥75 years old (Huang et al., 2014). Marital status is categorized as married, divorced/separated, widowed, or unmarried. Education level is classified as elementary school or below, junior high school, high school (including vocational), and college or above. Economic status is grouped based on monthly salary, ranging from high to low: ≥57,801 NT dollars, 36,301–57800 NT dollars, 22,801–36300 NT dollars, 17,281–22800 NT dollars, and ≤17,280 NT dollars. Environmental factors are differentiated by the degree of urbanization in the residential area, categorized according to the urbanization levels proposed by Liu (2006) et al., which divided Taiwan into seven levels of urbanization, from the highest urbanization level (Level 1) to the lowest (Level 7) (Liu et al., 2006). Due to the small number of individuals in Level 6 and Level 7, this study combined them with Level 5.
The comorbidities were based on whether the primary or secondary diagnosis codes in the medical records of patients in the 2 years before the diagnosis of NSCLC include the following disease codes, with the disease diagnosis occurring two or more times. Hypertension (ICD-9 codes 401-405; ICD-10 codes I10-I15), diabetes (ICD-9 code 250; ICD-10 codes E08-E13), hyperlipidemia (ICD-9 code 272; ICD-10 codes E78), liver cirrhosis (ICD-9 code 571; ICD-10 codes K70, K73-K76), renal failure (ICD-9 codes 584-586; ICD-10 codes N17-N19), cerebral vascular disease (ICD-9 codes 430-438; ICD-10 codes I60-I69), chronic obstructive pulmonary disease (ICD-9 codes 491, 492, and 496; ICD-10 codes J41-J44), asthma (ICD-9 codes 493; ICD-10 codes J45), rheumatoid arthritis (ICD-9 codes 714; ICD-10 codes M05-M06), and chronic mental disorder (ICD-9 codes 295, 296; ICD-10 codes F20, F30-F34, F39). The severity of comorbidities adopts the Charlson Comorbidity Index (CCI) as defined by Deyo et al. (1992). The original disease categories of the CCI are defined based on the diagnosis or procedure codes of ICD-9-CM, where a higher score indicates a more severe comorbidity level. The CCI score is calculated by converting the primary or secondary diagnosis codes from medical visits in the 2 years before diagnosis into scores, and the cumulative score represents the comorbidity level.
Hospital attributes refer to the institution where the first treatment (surgery, chemotherapy, radiotherapy, targeted therapy) for lung cancer diagnosis within 6 months is received. For those without treatment, it refers to the institution where the primary diagnosis first occurred. Hospital ownership is classified as public and non-public institutions. Hospital levels include medical centers, regional hospitals, and district hospitals. Cancer staging follows the TNM (tumor-node-metastasis) system and is categorized into stages I, II, III, and IV (Kay et al., 2017). Staging data is primarily obtained from the Cancer Registry. Treatment modalities include surgery, chemotherapy, radiotherapy, targeted therapy, surgery combined with other treatments, chemotherapy combined with other treatments, and other treatment combinations. NSCLC diagnosis years range from 2007 to 2013.
Statistical analysis
This study utilized statistical software SAS 9.4 (SAS Institute Inc., Cary, NC, USA) to analyze and process the data, conducting both descriptive and inferential statistics. All statistical analyses were considered significant at the p < 0.05 level and described as follows. Descriptive statistics were used to describe frequencies, percentages, means, etc. Specifically, descriptive analysis was conducted before and after matching on whether NSCLC patients received adjunctive TCHM therapy. It included the proportions of NSCLC patients with and without adjunctive TCHM therapy across different demographic variables, socioeconomic status, environmental factors, health conditions, cancer stages, hospital attributes, treatment modalities, year of diagnosis, etc.
Inferential statistics include exploring the factors influencing whether NSCLC patients receive adjunctive TCHM therapy and investigating the differences in emergency department visits and hospitalization days among NSCLC patients receiving adjunctive TCHM therapy. The Chi-Square test was employed to compare the differences in receiving or not receiving adjunctive TCHM therapy with gender, age, marital status, education level, monthly salary, degree of urbanization of residential area, severity of comorbidities, comorbid diseases, cancer stage, hospital level, ownership, treatment modalities, and year of diagnosis. Logistic regression analysis was conducted to investigate the factors influencing whether NSCLC patients receive adjunctive TCHM therapy. The dependent variable was the receipt of adjunctive TCHM therapy, and the independent variables included gender, age, marital status, education level, monthly salary, degree of urbanization of residential area, comorbid diseases, cancer stage, hospital level, ownership, treatment modalities, and year of diagnosis.
For the analysis of the association between adjunctive TCHM therapy and emergency department visits, conditional logistic regression can be employed. To analyze the association between hospitalization days of NSCLC patients and receiving adjunctive TCHM therapy, multiple regression analysis with Generalized Estimating Equations (GEE) was utilized. Since the distribution of hospitalization days for NSCLC patients within 1 year is not normally distributed, the hospitalization days of the study subjects will be transformed using a natural logarithm to approximate a normal distribution before conducting the GEE multiple regression analysis.
This study was reviewed and approved by the Research Ethics Center of China Medical University Hospital (IRB No. CMUH110-REC2-244). This research used unidentifiable data obtained from government legal databases (e.g., NHIRD, Cancer Registry). Therefore, patient consent is not required to access the NHIRD. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Results
This study included 43,122 patients with NSCLC, of whom 2,484 received adjunctive TCHM therapy, accounting for only 5.76% of the total. Among the cancer stages, the highest number of patients was in stage IV, with 23,401 individuals (54.27%). In terms of age distribution, the majority were aged 65–74 years (27.93%) and those aged 75 years and above (27.10%). Among the patients, there were 24,668 males (57.21%) and 18,454 females (42.79%). Regarding marital status, the majority were married, accounting for 69.65%, while in terms of education level, the highest proportion had education up to or below elementary school (48.78%). Among the patients, 41,147 individuals (95.42%) had a CCI score of 0 for comorbidities, and among those with comorbidities, hypertension was the most common, accounting for 15.82%. In terms of treatment methods, the highest number of patients had undergone surgical treatment, accounting for 93.16%.
The factors significantly associated with whether NSCLC patients receive adjunctive TCHM therapy (as shown in Table 2) include cancer stage, age, gender, marital status, education level, monthly salary, degree of urbanization of residential area, severity of comorbidities, comorbid diseases, hospital ownership, experience with Chinese medicine, receipt of chemotherapy, and year of diagnosis (p < 0.05). Compared to patients in stage I, those in stages II and III have a higher probability of receiving adjunctive TCHM therapy (OR = 1.35, 95% CI: 1.11-1.65; OR = 1.23, 95% CI: 1.06-1.41). Elderly patients aged 65–74 years and those aged 75 years and above are less likely to receive adjunctive TCHM therapy compared to the 20-54 age group (OR = 0.80, 95% CI: 0.70-0.92; OR = 0.46, 95% CI: 0.39-0.55). Females are significantly more likely than males to seek adjunctive TCHM therapy (OR = 1.37, 95% CI: 1.25-1.50). Married patients are more likely to receive adjunctive TCHM therapy compared to unmarried, divorced/separated, or widowed patients. Regarding education level, patients with higher levels of education are more inclined to use adjunctive TCHM therapy, with those having a college degree or above being more likely to use it compared to those with elementary school education or below (OR = 2.17, 95% CI: 1.89-2.48). Patients with higher monthly salaries (≥57,801 NT$) are more likely to use adjunctive TCHM therapy compared to those with the lowest monthly salary (≤17,280 NT$) (OR = 1.22, 95% CI: 1.04-1.44). Patients with a CCI score ≥2 are more likely to receive adjunctive TCHM therapy compared to those with a CCI score of 0 (OR = 1.36, 95% CI: 1.02-1.82). However, patients with certain comorbidities are less likely to use adjunctive TCHM therapy, such as those with hypertension (OR = 0.83, 95% CI: 0.72-0.96), diabetes (OR = 0.67, 95% CI: 0.54-0.83), renal failure (OR = 0.36, 95% CI: 0.15-0.88), or chronic obstructive pulmonary disease (OR = 0.72, 95% CI: 0.55-0.96) compared to those without these comorbidities. Patients in public hospitals are less likely to receive adjunctive TCHM therapy compared to those in non-public hospitals (OR = 0.90, 95% CI: 0.82-0.99). Patients with prior experience with Chinese medicine are significantly more likely to receive adjunctive TCHM therapy compared to those without such experience (OR = 1.94, 95% CI: 1.78-2.11). Patients who have undergone chemotherapy are significantly more likely to seek adjunctive TCHM therapy compared to those who have not (OR = 1.13, 95% CI: 1.03-1.25). Patients diagnosed in later years are more likely to seek adjunctive TCHM therapy (ORs: 1.28–2.18). This analysis reveals that only hospital level does not significantly affect patients' receipt of adjunctive TCHM therapy (p > 0.05).
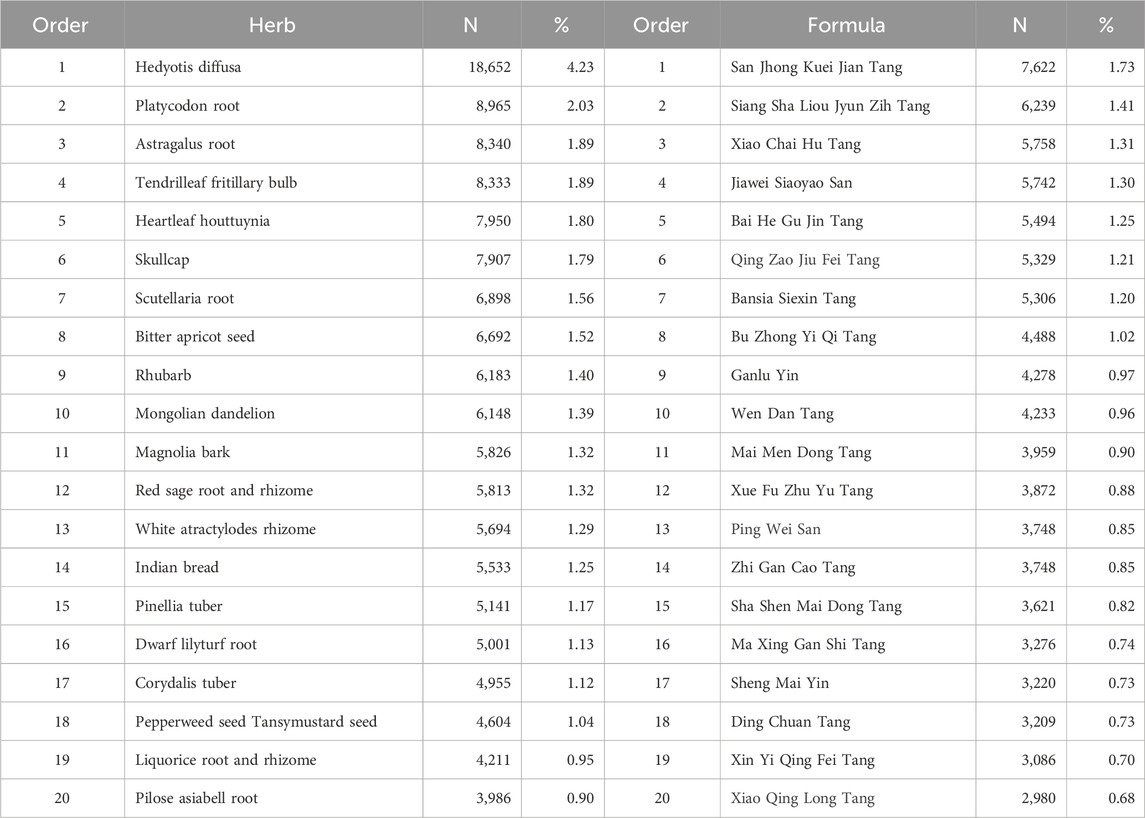
In this study, adjunctive TCM therapy primarily focuses on exploring herbal medicine. Table 3 presents the 20 most commonly used single herb and formula among NSCLC patients. There are 439 single herb medicine items, totaling 440,971 prescription records, and 456 formula items, totaling 251,750 prescription records. The top 10 most commonly used single herb medicines are Hedyotis diffusa, Platycodon root, Astragalus root, Tendrilleaf fritillary bulb, Heartleaf houttuynia, Skullcap, Scutellaria root, Bitter apricot seed, Rhubarb, and Mongolian dandelion. The top 10 most commonly used formulas are San Jhong Kuei Jian Tang, Siang Sha Liou Jyun Zih Tang, Xiao Chai Hu Tang, Jiawei Siaoyao San, Bai He Gu Jin Tang, Qing Zao Jiu Fei Tang, Bansia Siexin Tang, Bu Zhong Yi Qi Tang, Ganlu Yin, and Wen Dan Tang. Hedyotis diffusa accounts for 4.23% of all prescriptions, making it significantly higher than other single herb medicines, while San Jhong Kuei Jian Tang accounts for 1.73% of all prescriptions, making it the most prescribed formula, slightly higher than the second most prescribed Siang Sha Liou Jyun Zih Tang (1.41%).
In total, 43,122 patients with NSCLC were enrolled in the study. Among them, 40,638 patients (94.24%) did not receive adjunctive TCHM therapy, while 2,484 patients did. To mitigate data bias and confounding variables, we employed Propensity Score Matching (PSM) at a 1:5 ratio to precisely match cancer stage, age, gender, and severity of comorbidities. After matching, there were 2,308 patients who received adjunctive TCHM therapy and 11,540 patients who did not. The matched variables included cancer stage, age, gender, monthly salary, education level, marital status, severity of comorbidities, diabetes, cirrhosis, renal failure, cerebrovascular disease, chronic obstructive pulmonary disease, and whether surgery was received within 90 days of diagnosis. The differences between patients receiving and not receiving adjunctive TCHM therapy were not significant (p > 0.05) after matching (see Figure 1; Table 1).
Table 4 presents the emergency department visits within 1 year of diagnosis for patients with NSCLC and its relevant factors. 57.06% of NSCLC patients had emergency department visits within 1 year of diagnosis. Patients who received adjunctive TCM therapy for 181–365 days had significantly lower emergency department visits (45.45%) compared to those who did not receive adjunctive TCHM therapy (57.31%) (OR = 0.84, 95% CI: 0.74-0.95).
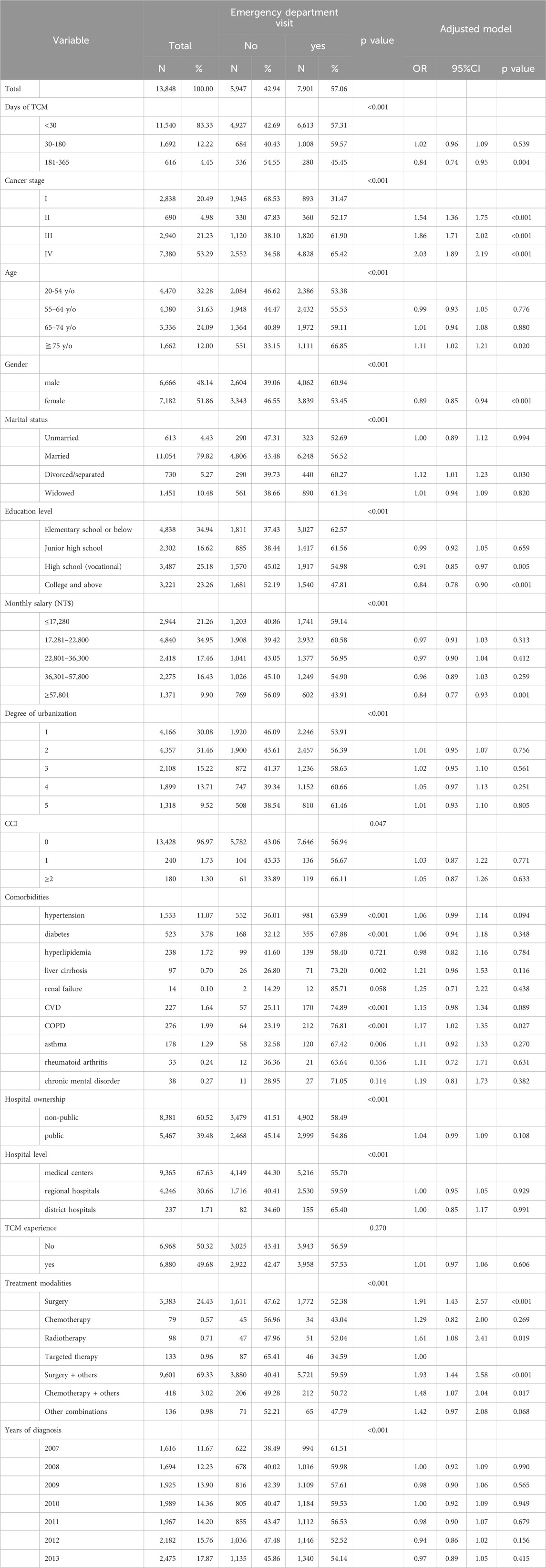
Table 4. Emergency department visit and related factors among NSCLC patients within 1 year of diagnosis.
In terms of other relevant factors, the cancer stage of NSCLC patients is directly proportional to emergency department visits (ORs: 1.54–2.03). Patients aged 75 years and above have more emergency department visits compared to those aged 20–54 years (OR = 1.11, 95% CI: 1.02-1.21). Female patients have fewer emergency department visits compared to male patients (OR = 0.89, 95% CI: 0.85-0.94). Regarding education level, patients with a high school (vocational) education and those with a college degree or above significantly utilize emergency department services fewer than those with elementary school education or below (OR = 0.91, 95% CI: 0.85-0.97; OR = 0.84, 95% CI: 0.78-0.90). Patients with a monthly salary of ≥57,801 NT$ have significantly fewer emergency department visits compared to those with a monthly salary of ≤17,280 NT$ (OR = 0.84, 95% CI: 0.77-0.93). Regarding the impact of treatment modalities for NSCLC, only surgical treatment (OR = 1.91, 95% CI: 1.43-2.57), only radiation therapy (OR = 1.61, 95% CI: 1.08-2.41), surgery + other treatments (OR = 1.93, 95% CI: 1.44-2.58), and chemotherapy + other treatments (OR = 1.48, 95% CI: 1.07-2.04) significantly increase emergency department visits compared to only targeted therapy. However, urbanization level of patients’ residential areas, severity of comorbidities (CCI), comorbid diseases, hospital ownership and level, patients’ experience with Chinese medicine, and year of diagnosis show no significant association with patients’ emergency department visits (p > 0.05), except for patients with comorbid chronic obstructive pulmonary disease, who significantly increase their use of emergency department visits (OR = 1.17, 95% CI: 1.02-1.35).
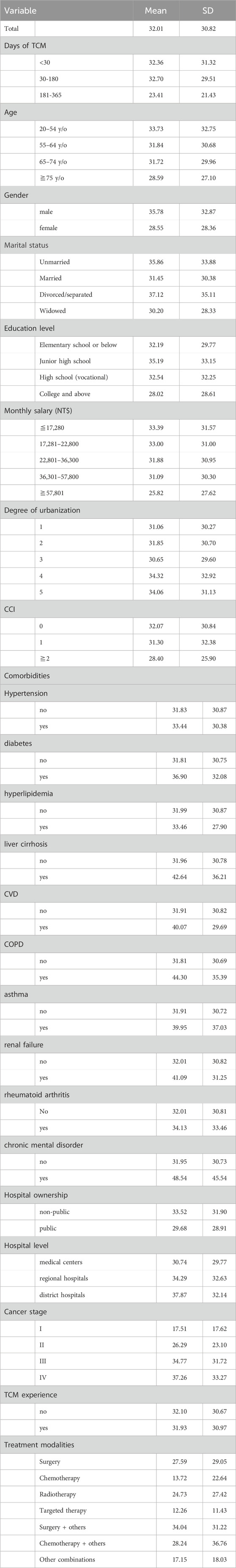
Using GEE multiple regression analysis to examine the association between the influence factors and the hospitalization days within 1 year of diagnosis for patients with NSCLC (Tables 5, 6), it was found that the average hospitalization days for NSCLC patients within 1 year was 32.01 ± 30.82. For patients using adjunctive TCHM therapy for 181–365 days, the average hospitalization days within 1 year decreased to 23.41 ± 21.43. Patients with NSCLC who used adjunctive TCHM therapy for 181–365 days had significantly shorter hospitalization days compared to those who did not receive adjunctive TCHM therapy (Ratio = 0.83, 95% CI: 0.75-0.91).
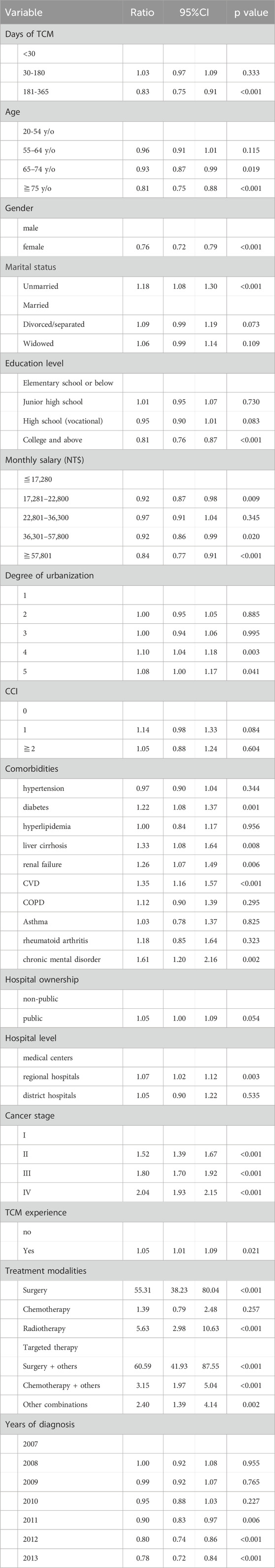
Table 6. GEE multiple regression analysis of hospitalization days in NSCLC patients within 1 year of diagnosis.
Regarding other relevant factors, the longer the age of the patient, the shorter the hospitalization days. Compared to patients aged 20–54 years, patients aged 65–74 years have shorter hospitalization days (Ratio = 0.93, 95% CI: 0.87-0.99), and patients aged 75 years and above have even shorter hospitalization days (Ratio = 0.81, 95% CI: 0.75-0.88). Female patients have shorter hospitalization days within 1 year compared to male patients (Ratio = 0.76, 95% CI: 0.72-0.79), while unmarried patients have longer hospitalization days compared to married patients (Ratio = 1.18, 95% CI: 1.08-1.30). Patients with higher education levels have shorter hospitalization days; those with a college degree or above have significantly different hospitalization days compared to those with elementary school education or below (Ratio = 0.81, 95% CI: 0.76-0.87). Similarly, patients with higher monthly salaries also have shorter hospitalization days; for example, patients with a monthly salary of ≥57,801 NT$ have shorter hospitalization days compared to those with a monthly salary of ≤17,280 NT$ (Ratio = 0.84, 95% CI: 0.77-0.91). Patients living in less urbanized areas have longer hospitalization days; for example, patients in level 5 urbanization areas have longer hospitalization days compared to those in level 1 urbanization areas (Ratio = 1.08, 95% CI: 1.00-1.17). The CCI does not affect the hospitalization days, but patients with comorbidities such as diabetes (Ratio = 1.22, 95% CI: 1.08-1.37), cirrhosis (Ratio = 1.33, 95% CI: 1.08-1.64), cerebrovascular disease (Ratio = 1.26, 95% CI: 1.07-1.49), chronic obstructive pulmonary disease (Ratio = 1.35, 95% CI: 1.16-1.57), and chronic mental illness (Ratio = 1.61, 95% CI: 1.20-2.16) have significantly longer hospitalization days. The ownership of hospitals (public, non-public) does not affect the hospitalization days for NSCLC patients, but the hospital level does. Patients treated at regional hospitals have longer hospitalization days compared to those treated at medical centers (Ratio = 1.07, 95% CI: 1.02-1.12). The higher the cancer stage of NSCLC patients, the longer the hospitalization days. Compared to stage I patients, stage II patients have a ratio of 1.52 (95% CI: 1.39-1.67), stage III patients have a ratio of 1.80 (95% CI: 1.70-1.92), and stage IV patients have a ratio of 2.04 (95% CI: 1.93-2.15) of hospitalization days. Patients with experience using Chinese medicine have longer hospitalization days compared to those without experience (ratio = 1.05, 95% CI: 1.01-1.09). In terms of treatment combinations, patients receiving pure targeted therapy have the shortest hospitalization days. Patients undergoing surgical treatment have longer hospitalization days, with pure surgical patients having a ratio of 55.31 (95% CI: 38.23-80.04) and patients receiving surgery + other treatments having a ratio of 60.59 (95% CI: 41.93-87.55). Patients receiving pure radiation therapy also have longer hospitalization days (ratio = 5.63, 95% CI: 2.98-10.63), as do patients receiving chemotherapy + other treatments (ratio = 3.15, 95% CI: 1.97-5.04) and other treatment combinations (ratio = 2.40, 95% CI: 1.39-4.14). As for the year of cancer diagnosis, the later the diagnosis, the shorter the hospitalization days; for example, compared to patients diagnosed in 2007, patients diagnosed in 2013 have a ratio of 0.78 (95% CI: 0.72-0.84).
Discussion
The results of this study indicate that many factors are associated with the use of TCHM as adjunctive therapy, including cancer stage, age, gender, marital status, education level, monthly income, urbanization level of residence area, CCI, comorbid diseases, hospital ownership, experience with TCM, receipt of chemotherapy, and year of diagnosis. Several factors are consistent with previous research findings (Lai et al., 2017; Lin et al., 2008; Lin et al., 2016; Lu et al., 2019; Weng et al., 2016), such as patients undergoing chemotherapy, female patients compared to male patients, younger age groups, higher severity of comorbidities, presence of multiple comorbidities, higher income levels, and residence in urban areas having a higher probability of using TCM treatment. However, some results differ from previous studies (Sun et al., 2018). For example, this study found that patients in the early stages of cancer are not more likely to seek TCM treatment, possibly because early-stage NSCLC can be treated with surgery and cured, which may explain why patients in Taiwan with early-stage NSCLC may not necessarily use TCM. The level of hospital and the receipt of TCM treatment are not associated, but NSCLC patients in non-public hospitals are more likely to receive TCM treatment than those in public hospitals. It is speculated that patients in hospitals with TCM departments can conveniently receive TCM treatment nearby, and Western medicine departments are more likely to consult TCM. Hospitals with TCM departments are more common in non-public hospitals than in public hospitals (Ministry of Health, 2023). This study’s data is linked to the household registration database from the Ministry of the Interior, and compared to previous studies, it includes marital status and education level as variables. Married individuals and those with higher education levels have a higher probability of receiving TCM treatment, highlighting this study’s significance, particularly as it is a nationwide cohort study.
This study examines the commonly used TCHM single herbs and formulas among NSCLC patients, with results differing slightly from previous research. A study from Taiwan in 2017 reported that the most commonly used formula was Qing Zao Jiu Fei Tang (Liao et al., 2017), which differs from the findings of this study, where San Jhong Kuei Jian Tang was most common. The reason for this difference may be attributed to the disparity in study periods. The previous study analyzed data from the NHIRD from 2000 to 2009, whereas this study covers the years 2007–2013, resulting in significant overlapping differences in time. San Jhong Kuei Jian Tang is known for its efficacy in clearing heat, detoxification, and resolving masses and swelling; it is often used to treat complications of NSCLC, lymphadenitis, acute folliculitis, thyroiditis, and thyroid nodules (Chinese Medicine formulae, 2024a). On the other hand, Qing Zao Jiu Fei Tang is known for clearing dryness and nourishing the lungs, suitable for conditions such as pneumonia, pulmonary tuberculosis, bronchial asthma, acute and chronic bronchitis, emphysema, lung cancer, urticaria, and laryngitis (Chinese Medicine formulae, 2024b). Based on the aforementioned, it can be inferred that San Jhong Kuei Jian Tang is mainly used for complications associated with NSCLC, while Qing Zao Jiu Fei Tang is employed as an anticancer formula. Moreover, a Taiwanese study from 2020 reported results consistent with this study (Yeh et al., 2020), where Hedyotis diffusa was the most commonly used single herb. Hedyotis diffusa is known for its efficacy in clearing heat, detoxification, promoting urination, and having antibacterial and anti-inflammatory properties. It also exhibits anti-tumor effects, inhibits spermatogenesis, and has hepatoprotective and choleretic effects (Ministry of Agriculture, 2024).
Among the top ten commonly used single herbs and formulas in this study for NSCLC patients receiving adjunctive TCHM therapy, herbs such as Hedyotis diffusa, Platycodon root, Astragalus root, Tendrilleaf fritillary bulb, Heartleaf houttuynia, Skullcap, Scutellaria root, Bitter apricot seed, Rhubarb, and Mongolian dandelion are all associated with lung cancer treatment. Among the formulas, Siang Sha Liou Jyun Zih Tang, Bai He Gu Jin Tang, Qing Zao Jiu Fei Tang, Bu Zhong Yi Qi Tang, and Ganlu Yin are related to anticancer effects. Additionally, formulas like San Jhong Kuei Jian Tang, Xiao Chai Hu Tang, Jiawei Siaoyao San, Bansia Siexin Tang, and Wen Dan Tang exhibit anti-inflammatory, immune-enhancing, and digestive system-strengthening effects, which can alleviate complications of NSCLC and side effects of Western medication (Zhang et al., 2021; Su et al., 2020; Lo and Hung, 2021).
The adjunctive TCHM therapy for 181–365 days in patients with NSCLC can significantly reduce emergency department visits by 16% and hospitalization days by 17%. The adjunctive TCHM therapy can improve medical utilization in NSCLC patients, provided that the duration of TCHM use reaches 181–365 days. Previous literature has not studied the emergency department visits and hospitalization days in the NSCLC patients treated with adjunctive TCHM therapy. Therefore, our study has reached a new conclusion and cannot be compared with other similar studies. This crucial finding can provide evidence-based recommendations for clinicians, indicating that TCHM must be used for at least 6 months to significantly reduce emergency department visits and hospitalization days. In other words, the adjunctive TCHM therapy of NSCLC should focus on the “course of treatment” rather than just the dosage effect. Even though the life expectancy of patients with advanced stage NSCLC may be shorter, this study showed that the benefits of adjunctive TCHM therapy were more significant in patients with advanced stage NSCLC, and patients with advanced stage NSCLC should be encouraged to receive the adjunctive TCHM therapy.
In addition to other relevant factors affecting emergency department visits, patients with more advanced cancer stages, those aged 75 and above, males, individuals with lower education levels, those with comorbid chronic obstructive pulmonary disease (COPD), and patients undergoing surgery or chemotherapy tend to have higher rates of emergency department visits. The findings of this study regarding gender, age, and income align with a study from mainland China in 2021 (Zhu et al., 2021), but differ from a study conducted by American scholars in 2008 regarding gender (Shugarman et al., 2008). However, the medical utilization patterns of lung cancer patients with comorbidities in mainland China, as observed in a 2020 study, differ from those in this study. In Taiwan, only comorbid COPD increases emergency department visits among NSCLC patients, while the mainland Chinese study found that several comorbid conditions were associated with medical utilization (Ding et al., 2020).
In terms of other relevant factors affecting hospitalization days, patients with more advanced cancer stages, males, those with lower education levels, individuals with comorbid chronic obstructive pulmonary disease (COPD), and patients undergoing surgery tend to have longer hospitalization days, in addition to higher rates of emergency department visits. However, some factors show different patterns compared to emergency department visits. For instance, patients aged 75 and above tend to have shorter hospitalization days compared to other age groups. Previous literature often focused on the frequency of hospitalizations among NSCLC patients rather than the duration, making direct comparisons difficult (Zhu et al., 2021). This could be attributed to the higher mortality rate among patients aged 75 and above, leading to shorter average hospitalization days. Patients with multiple comorbidities, including diabetes, liver cirrhosis, cerebrovascular diseases, and chronic mental disorders, significantly increase hospitalization days. While these four comorbidities do not increase the emergency department visit, they do prolong hospitalization days, providing crucial indicators for clinical caregivers. Regarding treatment combinations, only pure targeted therapy and pure chemotherapy do not significantly increase hospitalization days, while other treatments may require hospitalization or pose an increased risk of hospitalization.
Strengths
This study has several strengths. Firstly, it utilizes nationwide statistical data, encompassing 7 years of lung cancer patients (2007-2013). Secondly, the study employs Propensity Score Matching (PSM) with a 1:5 ratio to control for variables such as cancer stage, gender, age, monthly income, education level, marital status, disease severity, medical history (diabetes, liver cirrhosis, renal failure, cerebrovascular diseases, chronic obstructive pulmonary disease), and whether surgery was performed within 90 days. This meticulous matching ensures precise comparison between patients receiving and not receiving adjunctive TCHM therapy for lung cancer, effectively addressing potential confounders.
Limitations
This study’s sample was obtained from the NHIRD, and when analyzing based on diagnosis codes and medical order codes, the real-world compliance of patients with TCHM and Western medicine was overlooked. Retrospective studies may encounter unmeasured confounders (such as BMI, smoking status, or alcohol drinking) that might potentially impact the analysis results. The administration data used in retrospective studies may have incomplete data, data quality issues, temporal bias, or a lack of some relevant variables, making it impossible to completely reflect the current clinical situation. Additionally, data on certain TCHM treatments that are paid out-of-pocket (such as a few herbal decoctions) are not available in the NHIRD. If these out-of-pocket TCM treatments contribute to reduced medical utilization, the study also included their effects in the analysis for comparison. The out-of-pocket herbal decoctions will not affect the results because they were part of the TCM group. Each country’s medical system and economic environment were different; the results of this study might not be applicable outside of Taiwan. Finally, this study explored association between main outcomes and relevant variables and did not focus on examining causal inference.
Conclusion
Patients with NSCLC who receive adjunctive TCHM therapy for 181–365 days could significantly reduce emergency department visits and shorten hospitalization days. Clinical treatment teams may recommend and encourage patients with late-stage cancer, older age, male gender, low education level, and low income to undergo adjunctive TCHM therapy for at least 6 months. We strongly suggest the need for more research to confirm the findings.
Data availability statement
This study used databases including the National Health Insurance Research Database and the Cause of Death File. Data are available from the National Health Insurance Research Database published and managed by the Ministry of Health and Welfare, Taiwan. Due to legal restrictions imposed by the Taiwan government related to the Personal Information Protection Act, these databases cannot be made publicly available. All researchers can apply to access the databases for the purpose of conducting their studies. Requests for using the data can be sent as a formal proposal to the Science Center of the Ministry of Health and Welfare (https://www.mohw.gov.tw/mp-2.html). Any raw data are not allowed to be brought out from the Science Center. Only the analytic outputs in the format of a table or figure can be printed out. These restrictions prohibit the authors from making the minimal datasets publicly available. All remaining data are available in the article. Further inquiries can be directed to the corresponding author(s).
Author contributions
M-BT: Conceptualization, Funding acquisition, Methodology, Resources, Validation, Visualization, Writing – original draft, Writing – review and editing. W-YK: Formal analysis, Software, Project administration, Writing – original draft, Writing – review and editing. P-TK: Methodology, Software, Supervision, Writing – original draft, Writing – review and editing. W-CT: Conceptualization, Methodology, Resources, Supervision, Writing – original draft, Writing – review and editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by China Medical University Hospital (DMR-111-093). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Acknowledgments
We are grateful for using the National Health Insurance Research Databases provided by the Ministry of Health and Welfare, Taiwan. We also thank Health Data Science Center, China Medical University Hospital, for providing administrative, technical, and funding support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
NSCLC, Non-Small Cell Lung Cancer; NHIRD, National Health Insurance Research Database; ICD, International Classification of Diseases; CCI, Charlson Comorbidity Index; CI, confidence interval; TCM, Traditional Chinese Medicine; TCHM, Traditional Chinese Herbal Medication; OR, odds ratio.
References
Au, D. H., Udris, E. M., Fihn, S. D., McDonell, M. B., and Curtis, J. R. (2006). Differences in health care utilization at the end of life among patients with chronic obstructive pulmonary disease and patients with lung cancer. Arch. Intern Med. 166, 326–331. doi:10.1001/archinte.166.3.326
Cancer Organization (2021). Cancer organization, W.H. 3 march 2021. Available online at: https://www.who.int/news-room/fact-sheets/detail/cancer.
Chen, F. P., Chen, T. J., Kung, Y. Y., Chen, Y. C., Chou, L. F., Chen, F. J., et al. (2007). Use frequency of traditional Chinese medicine in Taiwan. BMC health Serv. Res. 7, 26–11. doi:10.1186/1472-6963-7-26
Chinese Medicine formulae (2024a). Department of Chinese Medicine and Pharmacy in the Ministry of Health and Welfare of Taiwan. Available online at: https://dep.mohw.gov.tw/DOCMAP/cp-866-7100-108.html.
Chinese Medicine formulae (2024b). Department of Chinese Medicine and Pharmacy in the Ministry of Health and Welfare of Taiwan. Available online at: https://dep.mohw.gov.tw/DOCMAP/cp-866-7078-108.html.
Deyo, R. A., Cherkin, D. C., and Ciol, M. A. (1992). Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J. Clin. Epidemiol. 45, 613–619. doi:10.1016/0895-4356(92)90133-8
Ding, R., Zhu, D., He, P., Ma, Y., Chen, Z., and Shi, X. (2020). Comorbidity in lung cancer patients and its association with medical service cost and treatment choice in China. BMC Cancer 20, 250. doi:10.1186/s12885-020-06759-8
Duggan, K. J., Wiltshire, J., Strutt, R., Boxer, M. M., Berthelsen, A., Descallar, J., et al. (2019). Palliative care and psychosocial care in metastatic non-small cell lung cancer: factors affecting utilisation of services and impact on patient survival. Support Care Cancer 27, 911–919. doi:10.1007/s00520-018-4379-7
Hirsch, F. R., Scagliotti, G. V., Mulshine, J. L., Kwon, R., Curran, W. J., Wu, Y. L., et al. (2017). Lung cancer: current therapies and new targeted treatments. Lancet 389, 299–311. doi:10.1016/S0140-6736(16)30958-8
Huang, H. L., Kung, P. T., Chiu, C. F., Wang, Y. H., and Tsai, W. C. (2014). Factors associated with lung cancer patients refusing treatment and their survival: a national cohort study under a universal health insurance in Taiwan. PloS One 9, e101731. doi:10.1371/journal.pone.0101731
Kay, F. U., Kandathil, A., Batra, K., Saboo, S. S., Abbara, S., and Rajiah, P. (2017). Revisions to the Tumor, Node, Metastasis staging of lung cancer (8th edition): rationale, radiologic findings and clinical implications. World J. radiology 9, 269–279. doi:10.4329/wjr.v9.i6.269
Kuo, Y. H., Tsay, S. L., Chang, C. C., Liao, Y. C., and Tung, H. H. (2018). Cancer impact, complementary/alternative medicine beliefs, and quality of life in cancer patients. J. Altern. Complementary Med. 24, 276–281. doi:10.1089/acm.2016.0396
Lai, C. Y., Wu, M. Y., Chiang, J. H., Sun, M. F., Chen, Y. H., Chang, C. T., et al. (2017). Utilization of Western medicine and traditional Chinese medicine among patients with Alzheimer’s disease in Taiwan: a nationwide population-based study. Eur. J. Neurology 24, 1166–1172. doi:10.1111/ene.13361
Lam, Y. C., Cheng, C. W., Peng, H., Law, C. K., Huang, X., and Bian, Z. (2009). Cancer patients’ attitudes towards Chinese medicine: a Hong Kong survey. Chin. Med. 4, 25–28. doi:10.1186/1749-8546-4-25
Li, T. M., Yu, Y. H., Tsai, F. J., Cheng, C. F., Wu, Y. C., Ho, T. J., et al. (2018). Characteristics of Chinese herbal medicine usage and its effect on survival of lung cancer patients in Taiwan. J. Ethnopharmacol. 213, 92–100. doi:10.1016/j.jep.2017.10.031
Liao, Y. H., Li, C. I., Lin, C. C., Lin, J. G., Chiang, J. H., and Li, T. C. (2017). Traditional Chinese medicine as adjunctive therapy improves the long-term survival of lung cancer patients. J. cancer Res. Clin. Oncol. 143, 2425–2435. doi:10.1007/s00432-017-2491-6
Lin, H. C., Lin, C. L., Huang, W. Y., Shangkuan, W. C., Kang, B. H., Chu, Y. H., et al. (2015). The use of adjunctive traditional Chinese medicine therapy and survival outcome in patients with head and neck cancer: a nationwide population-based cohort study. QJM An Int. J. Med. 108, 959–965. doi:10.1093/qjmed/hcv079
Lin, H. C., Yang, W. C. V., and Lee, H. C. (2008). Traditional Chinese medicine usage among schizophrenia patients. Complementary Ther. Med. 16, 336–342. doi:10.1016/j.ctim.2007.11.001
Lin, S. K., Yan, S. H., Lai, J. N., and Tsai, T. H. (2016). Patterns of Chinese medicine use in prescriptions for treating Alzheimer’s disease in Taiwan. Chin. Med. 11, 12–19. doi:10.1186/s13020-016-0086-9
Liu, C. Y., Hung, Y. T., Chuang, Y. L., Chen, Y. J., Weng, W. S., Liu, J. S., et al. (2006). Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J. Health Manag. 4, 1–22.
Lo, Y. T., and Hung, Y. C. (2021). Modern literature review of lung cancer with traditional Chinese medicine. J. Traditional Chin. Intern. Med. 19, 1–14.
Lu, M. C., Livneh, H., Chiu, L. M., Lai, N. S., Yeh, C. C., and Tsai, T. Y. (2019). A survey of traditional Chinese medicine use among rheumatoid arthritis patients: a claims data–based cohort study. Clin. Rheumatol. 38, 1393–1400. doi:10.1007/s10067-018-04425-w
Medscape (2021). Non-small cell lung cancer (NSCLC). Available online at: https://emedicine.medscape.com/article/279960-overview.
Ministry of Agriculture (2024). Illustrated directory of medicinal plants of the Ministry of Agriculture. Available online at: https://kmweb.moa.gov.tw/subject/subject.php?id=42506.
Ministry of Health (2023). List of hospitals with Chinese medicine departments from the department of Chinese medicine and pharmacy in the. Ministry of Health and Welfare. Available online at: https://dep.mohw.gov.tw/DOCMAP/cp-763-5517-108.html.
Ministry of Health and Welfare (2023). Statistics on causes of death in 2022 from the department of statistics in. the Ministry of Health and Welfare. Available online at: https://www.mohw.gov.tw/cp-16-74869-1.html.
Shugarman, L. R., Bird, C. E., Schuster, C. R., and Lynn, J. (2008). Age and gender differences in medicare expenditures and service utilization at the end of life for lung cancer decedents. Womens Health Issues 18, 199–209. doi:10.1016/j.whi.2008.02.008
Su, X. L., Wang, J. W., Che, H., Wang, C. F., Jiang, H., Lei, X., et al. (2020). Clinical application and mechanism of traditional Chinese medicine in treatment of lung cancer. Chin. Med. J. 133, 2987–2997. doi:10.1097/CM9.0000000000001141
Sun, L., Mao, J. J., Vertosick, E., Seluzicki, C., and Yang, Y. (2018). Evaluating cancer patients’ expectations and barriers toward traditional Chinese medicine utilization in China: a patient-support group–based cross-sectional survey. Integr. Cancer Ther. 17, 885–893. doi:10.1177/1534735418777117
Tang, W. R., Yang, S. H., Yu, C. T., Wang, C. C., Huang, S. T., Huang, T. H., et al. (2016). Long-Term effectiveness of combined treatment with traditional Chinese medicine and western medicine on the prognosis of patients with lung cancer. J. Altern. Complement. Med. 22, 212–222. doi:10.1089/acm.2015.0214
Weng, S. W., Chen, B. C., Wang, Y. C., Liu, C. K., Sun, M. F., Chang, C. M., et al. (2016). Traditional Chinese medicine use among patients with psoriasis in Taiwan: a nationwide population-based study. Evidence-Based Complementary Altern. Med. 2016, 3164105. doi:10.1155/2016/3164105
Xiong, S. Q., Chen, Y., Wang, L. J., Lyu, P. P., Liao, W., Wang, C., et al. (2020). Usage of Chinese herbs in cancer patients in southern China: a survey. Chin. J. Integr. Med. 27, 502–508. doi:10.1007/s11655-019-3184-6
Yeh, M. H., Wu, H. C., Lin, N. W., Hsieh, J. J., Yeh, J. W., Chiu, H. P., et al. (2020). Long-term use of combined conventional medicine and Chinese herbal medicine decreases the mortality risk of patients with lung cancer. Complementary Ther. Med. 52, 102427. doi:10.1016/j.ctim.2020.102427
Zhang, L., Zhang, F. Y., and Li, G. F. (2021). Traditional Chinese medicine and lung cancer – from theory to practice. Biomed. and Pharmacother. 137, 111381. doi:10.1016/j.biopha.2021.111381
Keywords: non-small cell lung cancer, adjunctive Chinese medicine therapy, national health insurance research database, medical utilization, Chinese herbal medicine
Citation: Tang M-B, Kuo W-Y, Kung P-T and Tsai W-C (2025) Associated factors, emergency department visits, and hospitalization days of receiving adjunctive Chinese herbal medicine therapy for patients with non-small cell lung cancer: a nationwide cohort study in Taiwan. Front. Pharmacol. 16:1435541. doi: 10.3389/fphar.2025.1435541
Received: 20 May 2024; Accepted: 28 April 2025;
Published: 20 May 2025.
Edited by:
Yi Guo, Tianjin University of Traditional Chinese Medicine, ChinaCopyright © 2025 Tang, Kuo, Kung and Tsai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wen-Chen Tsai, d2N0c2FpMjAxMUBnbWFpbC5jb20=
 Meng-Bin Tang
Meng-Bin Tang Wei-Yin Kuo
Wei-Yin Kuo Pei-Tseng Kung
Pei-Tseng Kung Wen-Chen Tsai
Wen-Chen Tsai