- 1Department of Pharmacy, Clinical Pharmacy Unit, Wachemo University, Hossana, Ethiopia
- 2Department of Pharmacology, School of Pharmacy, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 3Department of Clinical Pharmacy, School of Pharmacy, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 4Discipline of Pharmacy, University of Canberra, Canberra, ACT, Australia
Background: Drug therapy problems are common in hospitalized patients and may lead to increased hospital stays, healthcare costs, and increased risk of morbidity and mortality. Despite these facts, limited data exist on the magnitude of DTPs and associated factors among adult surgical patients in resource-limited settings, particularly in a current study setting. Therefore, this study aimed to assess the magnitude of DTPs and associated factors among adult surgical patients at study setting in Ethiopia.
Methods: A hospital-based cross-sectional study was conducted at Wachemo University Comprehensive Specialized Hospital from January 1 to 30 March 2024. Data were collected through patients’ interviews and chart reviews using pre-tested questionnaires and data abstraction formats. Data were analyzed using Statistical Package for Social Science version 20. Factors associated with drug therapy problems were determined by binary logistic regression analysis. A p-value of less than or equal to 0.05 was considered statistically significant in the final analysis, and an adjusted odds ratio with a 95% confidence interval was used to determine the strength of the association.
Results: The total number of recruited patients was 330. Of them, 304 participants who fulfilled the inclusion criteria. Of those participants, 216 (71.1%) were males. The mean age of the study participants was 44 (±17) years. Nearly half of the patients encountered at least one drug therapy problem, and 464 drug therapy problems were identified with a magnitude of 73.68% (95% CI: 0.684–0.785). Non-compliance (27.0%) was the most frequently identified drug therapy problem, followed by a need for additional drug therapy (21.1%). Length of hospital stay ≥7 days [adjusted odds ratio (AOR) = 2.47 [95% confidence interval (CI) 1.243–4.909, p = 0.01]), ≥5 drugs taken per day (AOR = 2.874 [95%CI: 1.411–5.851, p = 0.004]), and postoperative antibiotic use (AOR = 0.057 [95%CI: [0.028–0.115, p = 0.001]) significantly affect drug therapy problems.
Conclusion: This study identified a high prevalence of DTPs that was independently predicted by the presence of polypharmacy, prolonged hospital stay (≥7 days), and postoperative antibiotic use. Non-compliance were the most frequent identified drug therapy problems. Therefore, early identification of drug therapy problems and the associated factors may enhance the prevention and management of drug therapy problems.
Introduction
Drugs are vital tools in healthcare services that contribute to the improvement in the quality and expectancy of patients’ lives by preventing, and curing diseases (Muche et al., 2022). However, when drugs are used improperly, they can lead to drug-related problems (Patil et al., 2019). Drug therapy problems (DTPs) refer to a situation concerning pharmaceutical care practice that either directly or indirectly hinders the desired treatment outcomes (Abate et al., 2020; Tegegn et al., 2018; Cipolle et al., 2012a). The World Health Organization (WHO) launched “The Global Patient Safety Challenge: Medication without Harm” to stop preventable pharmaceutical damage. A recognized technique for classifying DTPs in a variety of contexts is the Pharmaceutical Care Network Europe (PCNE) categorization system, which may be incorporated into routine pharmaceutical care operations (Organization, 2024). DTPs are a significant contributor to morbidity and mortality and create considerable pressure on the healthcare systems (Alayed et al., 2019). It is estimated that approximately 5%–10% of all hospital admissions are drug-related, and about 22% of patients are discharged with DTPs. As many as 28% of all emergency department visits are drug-related issues (Belayneh et al., 2018).
Around 50% of patients undergoing surgery regularly take a significant number of medications both for surgery and for reasons unrelated to surgery, putting them at risk for drug problems and postoperative complications (Mohammed et al., 2022). As a result, it is important to identify and address DTPs as soon as possible (Tefera et al., 2020). Globally, fewer studies directly assessed DTP among surgical patients, and the majority of the studies focused on the issue of antibiotic misuse and their costs, adverse drug events, and medication errors (Krähenbühl-Melcher et al., 2007; Mejía et al., 2020; Niriayo et al., 2023). However, patients in the surgical ward also utilize different drug classes for various illness conditions in addition to antimicrobials, which require judicious administration for better results (Mattana et al., 2024).
The prevalence and factors associated with DTPs vary in diverse studies. For example, DTPs were generally documented by several studies in various nations, regardless of the wards, medications, or disease of concern, with an incidence of 33.3%–99.4% (Tefera et al., 2020). A study performed in the surgical department of a major city in southwest China reported that a total of 19.6% had at least one DTP (Qu et al., 2019). Age category, sex, presence of multiple comorbidities, rural residency, lower educational and economic status, functional dependence, impaired cognition, lower patient awareness, prolonged hospital stay, and polypharmacy were mentioned as determinants for DTPs in several studies (Ayalew et al., 2019; Short et al., 2023; Dammalapati et al., 2018). In Ethiopia, a study conducted at Jimma Medical Center among surgical patients revealed that 76% of the 300 study participants had a total of 449 DTPs identified, equating to an average of 1.97 per patient. The most prevalent types of DTPs were dose-too-low (27.6%) and dose-too-high (18.0%). The only independent predictors of DTPs were polypharmacy and hospital stays greater than 20 days (Tefera et al., 2020).
Limited data exist on the magnitude of DTPs and associated factors among adult surgical patients in Ethiopia, particularly in the current study setting. The prior study conducted at Jimma Medical Center did not consider variables such as preoperative complications like perforated appendicitis, peritonitis, gangrene, and types of anesthesia (local or general) used, which might have an impact on DTPs among surgical patients. Therefore, this study aimed to assess the magnitude of drug therapy problems and their associated factors among surgical patients admitted to the surgical ward of WUCSH, Hossana, Ethiopia.
This study will provide important information to tertiary hospitals, including study settings and healthcare providers about the magnitude of the drug therapy problem and its associated factors among adult surgical patients. The findings can be used to develop interventions and strategies to improve patient care by establishing protocols and guidelines for monitoring and managing DTPs in surgical patients. The findings may also be used as a baseline for researchers as well as for other stakeholders to reduce the burden of DTPs and their complications.
Methods and materials
Study area and study period
The study was conducted at the surgical ward of WUCSH in Hossana, central Ethiopia, from January 1 to 30 March 2024. Hosanna town is located at a distance of 232 km southwest of the capital city of Ethiopia, Addis Ababa, and 194 km northwest of Hawassa City. WUCSH was established in 1984 E.C.; and currently, the hospital is under the administration of Wachemo University. It provides healthcare services to more than 3.2 million people around Hosanna and nearby towns. It delivers different healthcare services to the community like internal medicine, surgery, gynecology and obstetrics, pediatrics, maternal and child health (MCH), tuberculosis (TB) and HIV (TB/HIV), intensive medical care, mental healthcare, dermatology and venereal disease services, pharmacy, and different laboratory services.
Study design
A hospital-based cross-sectional study was conducted.
Population
The source population was all adult patients admitted to the WUCSH surgical ward. The study population consisted of all adult patients admitted to the surgical ward of WUCSH from January 1 to 30 March 2024, and who fulfilled the inclusion criteria.
Eligibility criteria
Adult patients admitted to the surgical ward, patients who were aged ≥18 years admitted for surgical procedures, and those who were hospitalized for >24 h were included in our study. However, those who have been readmitted within the data collection period, self-discharged, and severely ill patients were excluded from this study.
Sample size determination and sampling technique
The sample size was calculated based on a single population proportion formula by taking the estimated prevalence of DTPs (76%) from the Jimma Medical Centre among adult surgical patients in a tertiary hospital (Tefera et al., 2020) as follows:
Where n is the sample size required; p is the estimated prevalence of DTPs; Zα/2 is the standard normal deviation at a 95% confidence interval corresponding to 1.96; and d is the absolute error between the estimated and true population prevalence of DTPs of 5%. The sample sizes for associated factors were determined by considering different associated factors. By using EPI Info version 7 statistical software with the assumptions of confidence level 95%, power 80%, and the ratio of exposed to unexposed 1:1, the sample size was 110 surgical patients for polypharmacy and 111 for prolonged length of hospital stay. Therefore, the larger final sample size was 310 admitted surgical patients after adding a 10% non-response rate. A convenient sampling technique was used for this study.
Data collection methods
A structured questionnaire was developed from reviewing different literature (English version) (Mohammed et al., 2022) and (Tefera et al., 2020). The questionnaire contains four sections: part I (patient-related factors), part II (disease-related factors), part III (medication-related factors), and part IV (drug therapy problems). Two trained pharmacists and one nurse professional participated as data collectors in data collection. Two days of training were given to the data collectors and one senior clinical pharmacist to familiarize them with the data collection instrument as well as how to collect the necessary data from charts and how to conduct patient interviews. Daily supervision and routine follow-up were done by the principal investigator, and drug therapy problems were identified by a multidisciplinary team which includes senior clinical pharmacists.
Relevant information about each patient, like patient characteristics, laboratory results, current medications, co-morbidities, length of hospitalization, and relevant previous medical and medication histories, was recorded using data abstraction format by reviewing patients’ medical charts. Additional information and clarifications on some patient’s medical information were obtained through interviewing the patients. Micromedex® and Lexicomp drug interaction checker were used to identify drug-drug interactions. Identified DTPs were recorded and classified using the DTP registration format taken from Cipolle’s model, which has details of DTP measurement and classifications (Cipolle et al., 2012b).
Study variables
Dependent variable: Drug therapy problems
Independent variables
Patient-related factors: Age, sex, religion, occupation, education status, monthly income, place of residency, marital status, alcohol consumption, khat chewing, and smoking status.
Disease-related (clinical) factors: Presence of comorbid conditions, number of comorbid conditions, presence of complications, surgical procedure done, types of procedure, hospitalization since the last year and length of hospitalization for current conditions.
Drug-related factors: types of medications, number of medications, preadmission medication, types of anesthesia used, postoperative drugs, postoperative pain management, patient drug compliance, prescribing preference based on guidelines, and number of drugs used at a time.
Operational definition
Drug therapy problem: an event or circumstance involving drug therapy that actually or potentially interferes with desired health outcomes in this study patient is considered to have DTP if the patient has one or more of the following DTP: dosage too low, dosage too high, need for additional drug therapy, ineffective drug, unnecessary drug, adverse drug reaction, and noncompliance (Cipolle et al., 2012b).
Adverse drug reaction: any noxious, unintended, and undesired effect of a drug, which occurs at doses used in humans for prophylaxis, diagnosis or therapy (Bekele et al., 2021).
Unnecessary drug therapy: The drug therapy is unnecessary because the patient does not have a clinical indication at this time.
Needs additional drug therapy: Additional drug therapy is required to treat or prevent a medical condition or illness from developing (Cipolle et al., 2012b).
Dosage too high: is a DTP where the dose is too high the dosing frequency is too short or the duration of therapy is too long for the patient (Cipolle et al., 2012b).
Dosage too low: is a DTP that occurs when the dose is too low to produce the desired outcome, the dosage interval is too long or the duration of therapy is too short (Cipolle et al., 2012b).
Ineffective drug therapy: The drug product is not effective at producing the desired response or outcome (Cipolle et al., 2012b).
Noncompliance: is a DTP that occurs when the patient does not understand the instructions or the patient prefers not to take or forgets to take the medication the cost of the drug product is not affordable for the patient, or the patient cannot swallow or self-administer the medication properly, or the drug product is not available for the patients (Cipolle et al., 2012b).
Polypharmacy: polypharmacy is the use of at least five drugs concurrently. Different strengths of the same drug were counted as one item. However, formulations of one drug requiring different routes of administration were regarded as separate items (Pazan and Wehling, 2021).
Data quality control
A pre-test study was conducted among 5% of the calculated sample size (16 patients) before the days of the data collection period at Gembichu Primary Hospital to check for the uniformity and understandability of the questionnaire. Two days of training were given for data collectors with continuous supervision and follow-up during the data collection process. Every day, the principal investigator cross-checks the accuracy and consistency of the data. Data were stored in a safe and secure place, and all materials utilized for data gathering were organized sequentially.
Methods of data analysis
The collected data was checked for its completeness, coded, and entered into Epi data version 3.1 and it was analyzed by using SPSS version 20 software. Descriptive statistics were performed to describe the demographic profile of the study participants. Cleaning was performed to check for frequencies, accuracy, consistencies, and missed values and variables. Binary and multivariable logistic regression was used to assess the association between independent variables and a dependent variable. A variable with a p-value less than 0.25 in the bivariable analysis was entered into the multivariable model. In multivariable logistic regression, model goodness of fit was checked by the Hosmer and Lemeshow test, and Multicollinearity was detected by variance inflation factor (VIF). Then, the adjusted odds ratio (AOR) along with a 95% CI was used to determine the strength of association with the level of statistical significance at a p-value less than 0.05. Finally, statistically significant factors were reported as factors associated with drug therapy problems for admitted surgical patients in this study.
Results
Sociodemographic and clinical data of study participants
During the 3-month study period, a total of 330 patients were admitted to the surgical ward. After excluding 26 patients, 304 patients fulfilled the eligibility criteria, and they were enrolled in our study. Among the study participants, 216 surgical patients were males, and more than one-third of study participants were in the age range of 31–50 years with a mean age of 44.41 (±17.39) years. More than half of the study participants were married, 161 (53.0%). About 106 (34.9%) had not attended formal education, and 141 (46.4%) of the study participants were farmers with a monthly income of less than 1000 ETB. Of the total patients, 119 (39.1%) had been hospitalized once since last year and the majority of them, 179 (58.9%), stayed at the hospital longer than 7 days. More than half of the study participants, 215 (70.7%), took more than five drugs (Table 1).
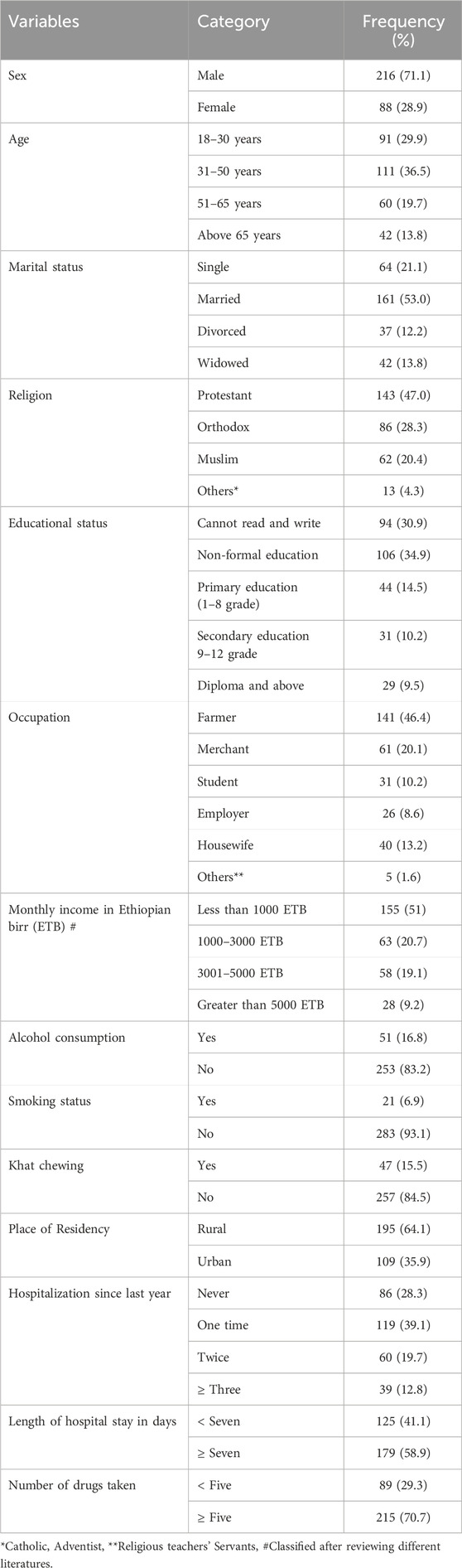
Table 1. Sociodemographic and clinical characteristics of hospitalized adult patients in surgical of WUCSH from January 1 to 30 March 2024 (n = 304).
Types of procedures performed
As demonstrated in Figure 2, the most common type of surgery done during the study period was abdominal surgery, 107 (35.2%). The remaining surgical procedures were urologic surgery 78 (25.7%), thyroid surgery 31 (10.2%), skin and subcutaneous 46 (15.1%), breast surgery 24 (7.9%), and others (5.9%) such as hernias, vascular, and esophageal surgery (Figure 1).
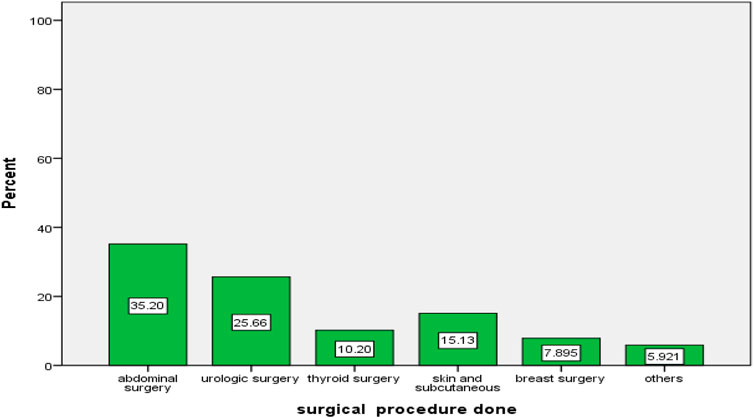
Figure 1. Types of surgery done during the study period in the surgical ward of WUCSH from January 1 to 30 March 2024 (n = 304).
Prescribed preadmission and surgical-related medications
Around 279 (91.7%) study participants had at least one preadmission medication prescribed for medical and surgical comorbidities. The most prescribed drug classes during the study period were anti-infective 90 (32.26%); cardiovascular drugs 42 (15.1%); anti-diabetic drugs 25 (9%); anti-thyroid drugs 40 (14.3%); alpha-1 antagonist drugs 27 (9.7%); respiratory drugs 18 (6.5%; and other drugs [tamoxifen, antiretroviral treatment, phenytoin, pyridoxine, amitriptyline, phenobarbital, and sodium valproate], 37 (13.3%) (Table 2).
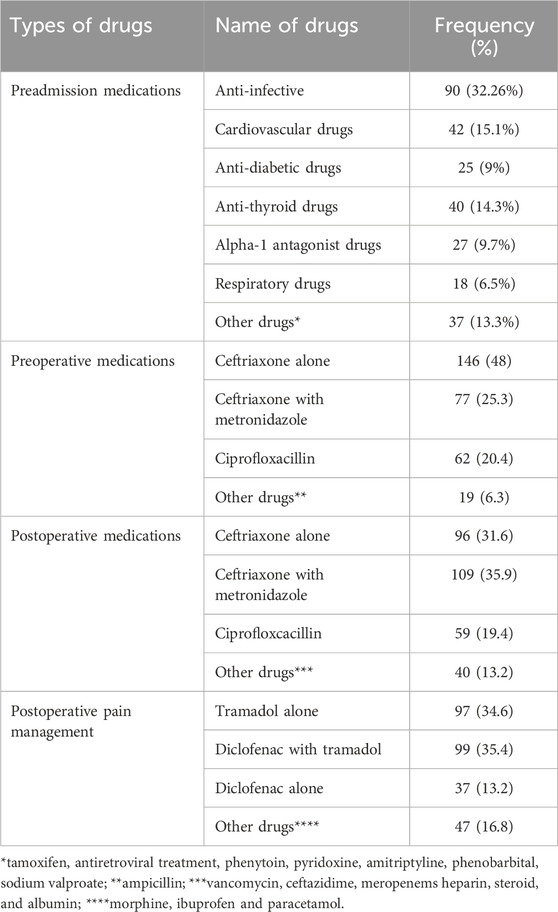
Table 2. Description of used medications among adult surgical patients admitted at WUCSH from January 1 to 30 March 2024 (n = 304).
During the study period, ceftriaxone 146 (48%) and metronidazole with ceftriaxone 109 (35.9%) were the most frequently prescribed medications for the treatment of preoperative and postoperative surgical conditions, respectively. More than ninety percent of patients, 280 (92.1%), were provided postoperative pain management, diclofenac with tramadol 99 (35.4%) frequently prescribed (Table 2).
The magnitude of DTPs and percentage of DTPs per patient
The magnitude of DTPs among study participants was found to be 73.68% (95% CI: 0.684–0.785) (Figure 2).

Figure 2. Magnitude of DTPs among study participants in the surgical ward of WUCSH from January 1 to 30 March 2024 (n = 304).
Among those study participants, 107 (47.77%) had one DTP, 66 (29.46%) had two DTPs, 24 (10.71%) had three DTPs, 18 (8.03%) had four DTPs and 9 (4.01%) of patients had greater than four DTPs in this study (Figure 3).
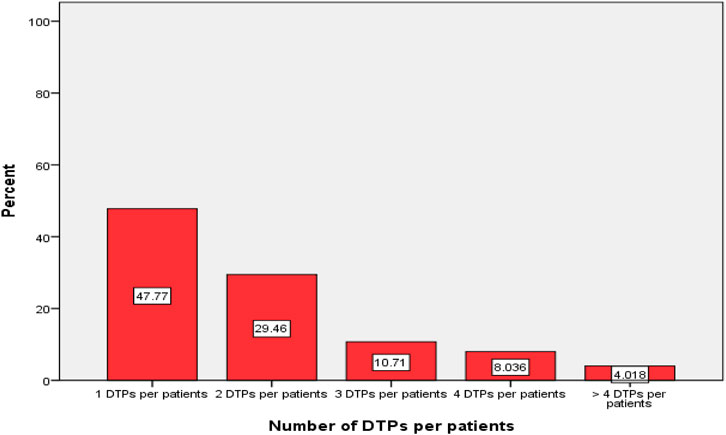
Figure 3. Percentage DTPs per-patients during the study period in the surgical ward of WUCSH from January 1 to 30 March 2024 (n = 304).
Drug therapy problem types and their causes
Out of 304 study participants, a total of 464 DTPs were identified. Non-compliance was the most common (27%), followed by the need for additional drug therapy (21.1%). Other types included ineffective drug therapy, dosage too low, unnecessary drug therapy dosage too high, and adverse drug reactions (Table 3).
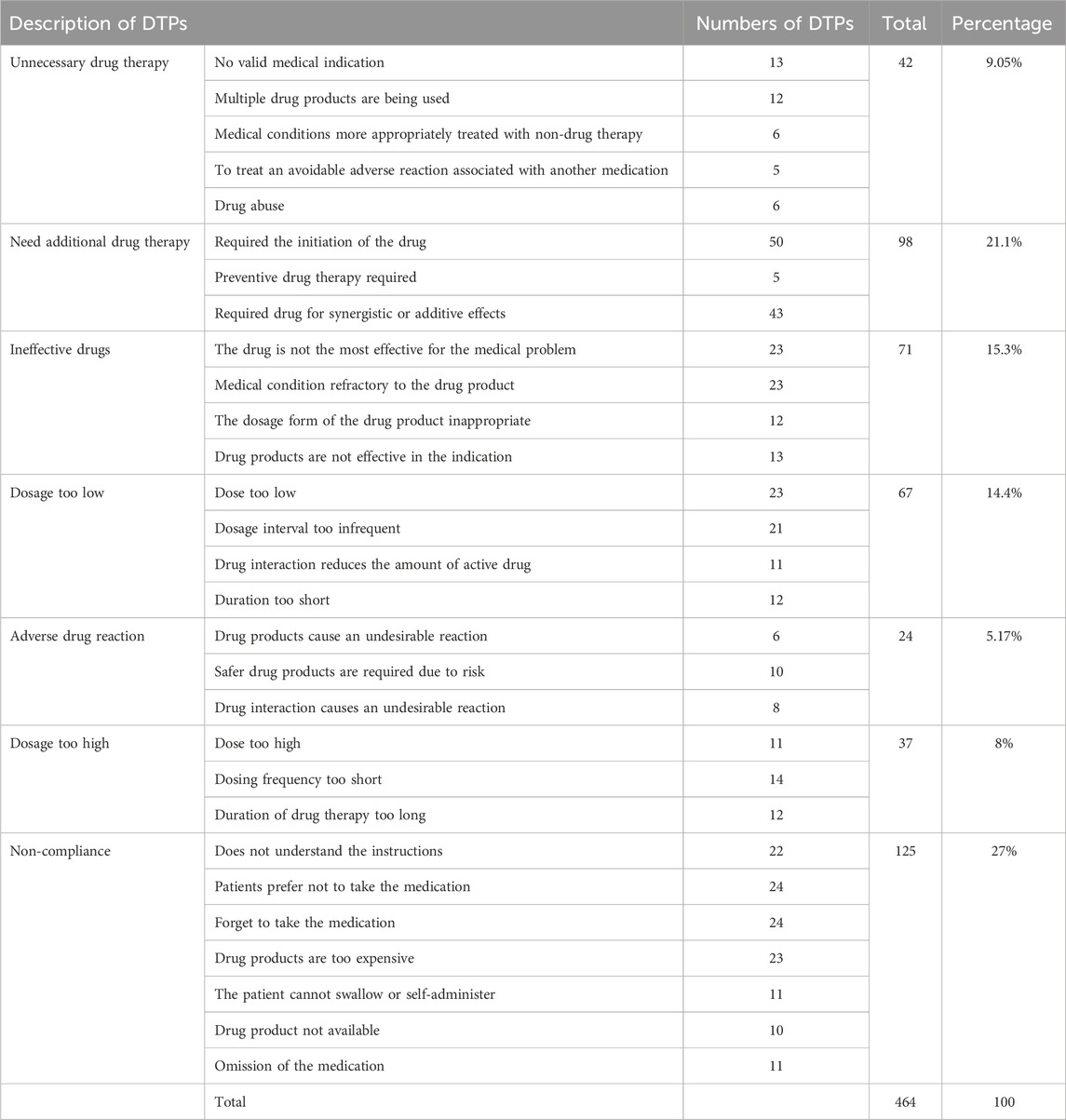
Table 3. Details of each identified DTP during the study period at the surgical ward of WUCSH from January 1 to 30 March 2024 (n = 304).
Factors associated with drug therapy problems
Bivariate analysis
Variables such as educational status, types of surgery done, length of hospital stay, number of drugs prescribed, and postoperative use of antibiotics had a p-value of less than 0.25. These variables are taken in multivariable analysis. To identify factors associated with the occurrence of DTPs among study participants, the variables with a p-value of less than 0.25 in binary logistic regression were entered into multivariable logistic regression (Table 4).
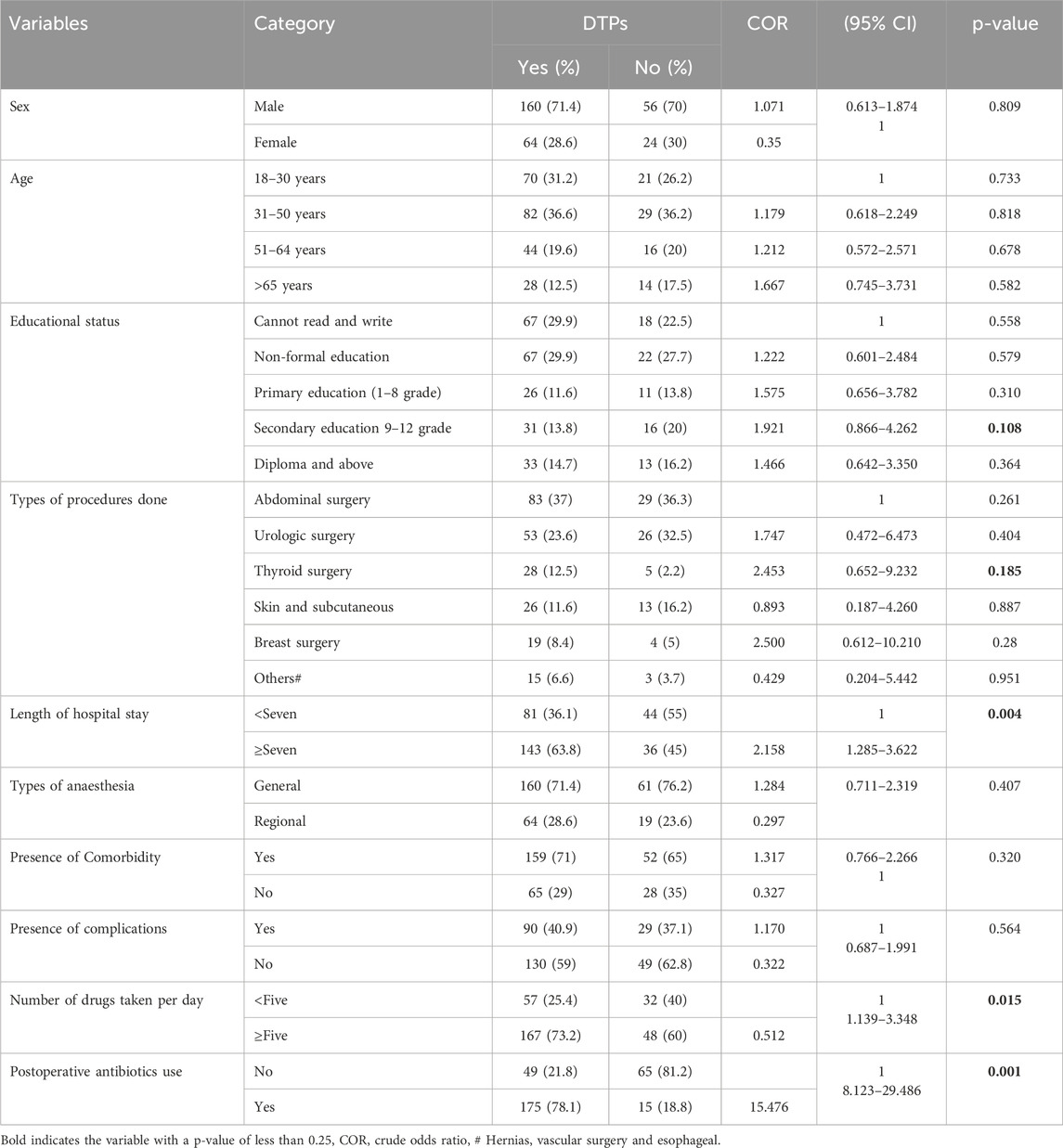
Table 4. Univariate binary logistic regression analysis between explanatory and dependent variables among surgical patients at WUCSH from January 1 to 30 March 2024 (n = 304).
Multivariable analysis
The multivariable logistic regression analysis showed that length of hospital stay, number of drugs taken per day, and administration of postoperative antibiotics had a significant association with the occurrence of DTPs. Accordingly, study participants who had stayed more than 7 days in the hospital were nearly 2.5 times to experience DTPs (AOR = 2.470, 95% CI: 1.243–4.909, p = 0.01) as compared to study participants who stayed less than 7 days in the hospital. The study participants who took more than five drugs per day were 2.87 times to experience DTPs (AOR = 2.874, 95% CI: 1.411–5.851, p = 0.004) as compared to study subjects who took less than five drugs per day. Whereas patients who took postoperative antibiotics were less likely to experience DTPs (AOR = 0.057, 95% CI: 0.028–0.115, p = 0.001) compared to those who did not take post-op antibiotics (Table 5).
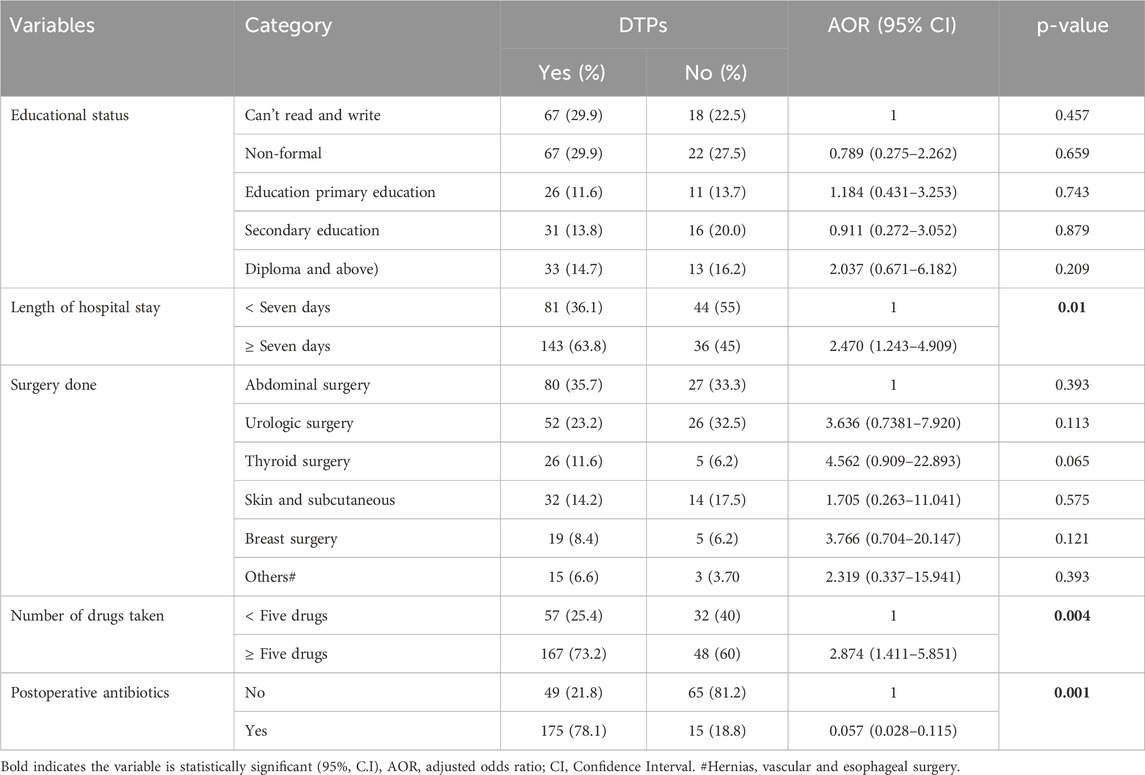
Table 5. Multivariable binary logistic regression analysis for factors associated with DTPs during the study period at the surgical ward of WUCSH, 2024 (n = 304).
Discussion
The use of medication therapy is expanding, which makes it more difficult to prescribe medicines appropriately, and suboptimal use of medication is preventable (Levy, 2023). It has been demonstrated that handling DTPs using pharmaceutical care services can result in financial savings, a decrease in adverse drug events, a decrease in mortality, and an improvement in overall quality of life (Kjeldsen et al.). Assessing the extent of DTPs and factors associated with this problem among hospitalized patients is very crucial for the prevention and control of DTPs to achieve positive therapeutic outcomes in hospitals (Oki et al., 2021). In this study, the magnitude of DTPs was high, and factors associated with DTPs among adult admitted surgical patients in the study setting were prolonged length of hospital stay, number of drugs taken per day, and administration of postoperative antibiotics.
The current study showed that nearly three-fourths of study participants (73.68%) admitted to the surgical ward of WUCSH during the study period were experienced DTPs. This result is higher than a study conducted in Canadian tertiary care hospitals (66.4%) (Neville et al., 2014). However, the prevalence of DTPs is lower than the current finding in tertiary hospitals of South India (Alagiriswami et al., 2009), and Southwest China (Qu et al., 2019), which reported 7.9% and 42.8%, respectively. These differences might be due to study settings, study design, sampling technique, and healthcare professionals’ skill variation. This result is consistent with a study conducted in southwest Ethiopia, which showed a prevalence of 69.5% (Mohammed et al., 2022). The present study also showed a similar prevalence of DTPs with another study conducted in Malaysia (76.1%) (Zaman Huri et al., 2014).
In this study, a total of 464 DTPs were identified, with approximately 47.77% (95% CI: 0.41–0.55) of participants having at least one DTP. This finding is similar to a study conducted at tertiary and academic medical centers (48%) in Northwestern Chicago (Phatak et al., 2016) and tertiary hospitals in Chongqing (55.4%), Southwest China (Qu et al., 2019); and lower prevalence (60%) in New Zealand (Wood and Lightfoot, 2018). These discrepancies highlight how different healthcare practices, resources, and patient management approaches across various countries and facilities can impact the prevalence of DTPs in tertiary hospitals.
Non-compliance was the most frequently identified DTP, accounting for 27% (95% CI: 0.23–0.31) in the current study. This finding is slightly lower than the non-compliance rate of (37.8%), reported studies involving surgical patients in New Zealand (Wood and Lightfoot, 2018). This discrepancy might result from differences in how non-compliance was identified, the resources available in the clinical settings, the sample size used, or the characteristics of the study population and differences in post-surgical care practices in different hospitals.
The current finding showed that need for the additional drug therapy was the second most commonly identified DTP with a prevalence of 21.1% (95% CI:0.176–0.25). This result is similar to the study conducted in Canada at adult tertiary care hospitals (25.5%) (Haley et al., 2009). However, the need for additional drug therapy was the major category of drug-related problems in referral hospitals in Kenya (Degu et al., 2023). The variation could be due to the level of pharmaceutical care experience and clinical practice which can help to easily identify and classify DTPs.
In the present study, approximately 15.3% (95% CI: 0.12–0.19) of DTPs were attributed to the prescribing of ineffective drugs. This finding was lower than the study conducted in Malaysian (45.9%) (Zaman Huri et al., 2014) and in China (25.1%) (Meng et al., 2021); and the higher than finding was reported from a teaching hospital in Amman, Jordan which showed that the ineffective drugs (6.5%) were the most frequent observed DTPs (AbuRuz et al., 2021). The discrepancy might be the factors such as different patient populations, sample size, and differences in healthcare practices between settings could have contributed to the higher detection of ineffective prescriptions.
In this study, the dosage too low was 14.4% (95% CI: 0.11–0.18). This finding is higher than a study accompanied in Canada (9%) and Saudi Arabian (11%) (Aljadhey et al., 2014). However, it is lower than the study done in Ethiopia which showed dosage too low was 27.6% (Tefera et al., 2020). This difference might be due to the study setting, study design, sample size, involvement of clinical pharmacist, and difference in patient understanding use of medications through different ways.
According to the present study, 13.17% of safety-related problems were observed among surgical patients, of which 8% were dosages too high and 5.17% were adverse drug reactions. This finding was lower than the study conducted in Jordan (20.2%) (AbuRuz et al., 2021); and higher than the study revealed in Canada (10.5%) (Meng et al., 2021). The difference might be due to the categorization and classification of DTPs, experience practice in detecting, and reporting of ADR, and study design.
The least prevalent DTP was unnecessary drug therapy, which accounts for 9.05%, often due to prescribing medication without a valid medical indication in this study. This finding is lower than the study conducted in China (16.8%) (Qu et al., 2019), and Jordan (18.9%) (AbuRuz et al., 2021). The variation could be due to the study design, study setting, study populations, and differences in healthcare practice. However, it is higher than the reported in a study conducted by Jimma Medical Center in Ethiopia that indicated 1.97% (Mohammed et al., 2022).
In the current study, the number of drugs taken per day, length of hospital stay, and post-operative antibiotics were shown to be associated factors for the occurrence of DTPs. Patients who took greater than or equal to five drugs per day were 2.874 times have DTPs compared to patients who took less than five drugs per day. This finding is in line with a study conducted at Jimma Medical Center (Tefera et al., 2020). This study indicates that polypharmacy predictor for the occurrence of DTPs and it is a generalizable risk factor in healthcare settings, which means that patients’ drug regimens need to be reviewed frequently, especially if they are prescribed five or more prescriptions (Al Hamid et al., 2014). Consequently, the use of clinical pharmacists in hospitalized patient care might help lower the risk of DTPs and minimize the hazards related to polypharmacy (Bhatty et al., 2018).
The patients who received antibiotics postoperatively decreased the occurrence of DTPs by 0.057 (AOR = 0.057, 95%CI: 0.028–0.115, p = 0.001) than those who didn’t take antibiotics postoperatively in this study. This finding is similar to a study done at Jimma Medical Center (Mohammed et al., 2022). This finding showed that postoperative antibiotics use is associated with a lower incidence of DTPs suggesting that antibiotics play a crucial role in preventing complications like surgical site infections that could lead to DTPs when appropriately prescribed. Therefore, reducing the likelihood of complications and subsequent need for additional medications which in turn lowers the risk of DTPs among surgical patients.
The present study showed that patients whose hospital stay was greater than 7 days were 2.5 times more likely to have DTPs than patients whose hospital stay was less than 7 days. This result was consistent with those studies done by Jimma Medical Center (Tefera et al., 2020). This could be due to prolonged hospitalization may increase the number of drugs, drug-drug interactions, reasons for changing medications, a chance to acquire new infections, and non-adherence which increases the possibility of the development of DTPs.
Limitations of the study
The study’s strength was demonstrated through interviewing the participants who had accurate and updated information, which enabled easy identification of various DTP categories. Additionally, by including all adult surgical patients, both elective and emergency, the study was able to obtain an adequate study sample size. This study also had some limitations: first, since this study is a cross-sectional study, it cannot establish causal relationships. Second, the study was conducted at a single institution with convenience sampling, and this may affect the generalizability of the findings. Finally, this study did not consider severity and types of surgery performed, physician variability, impacts of each DTP on the patient’s outcomes, and DTPs were considered based on patients’ responses and/or from medical records without the establishment of a causal relationship. Therefore, the results of this study should be interpreted with caution, and we recommend further multicenter studies with follow-up to establish a causal relationship between the occurrence of DTPs and associated factors by addressing other limitations of this study.
Conclusion
The present finding showed a high magnitude of DTPs among patients in the surgical ward at WUCSH, and this finding highlights the need for significant attention and intervention in this area. The most frequently identified DTP was noncompliance, indicating a critical area for improvement in patient adherence to prescribed therapies. Additionally, the study identified several factors associated with an increased likelihood of DTPs, including polypharmacy, prolonged hospital stay in days, and the use of postoperative antibiotics. Generally, this study emphasizes the importance of targeted strategies to minimize DTPs through clinical pharmacist integration, developing protocols for DTP screening, and patient counselling strategies to improve the treatment outcomes of surgical patients. Nationalwide interventional studies with multicenter settings will be needed to establish the impacts of DTPs on treatment outcomes of surgical patients in Ethiopia.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Haramaya University College of Health and Medical Sciences Institutional Health Research Ethics Review Committee, with reference number of IHRERC/248/2023. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Participants’ confidentiality was assured by excluding names and identifiers in the questionnaire.
Author contributions
TS: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Resources, Software, Validation, Writing – original draft, Writing – review and editing. JA: Conceptualization, Data curation, Formal Analysis, Methodology, Supervision, Validation, Writing – original draft, Writing – review and editing. MD: Conceptualization, Formal Analysis, Methodology, Supervision, Writing – original draft, Writing – review and editing, Investigation, Validation. SN: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Writing – original draft, Writing – review and editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
First, we want to express our gratitude to the Almighty God for his unending assistance in our day-to-day activities. Then, we would like to express our gratitude to Haramaya University’s Institutional Health Research Ethics Review Committees for their review and constructive comments before approval of our research proposal. Finally, we also like to thank the study participants and staff of WUCSH for their contributions directly or indirectly to the accomplishment of this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ADEs, Adverse Drug Events; ADR, Adverse Drug Reaction; CVS, Cardiovascular System; DRHs, Drug-related hospitalizations; DTPs, Drug Therapy Problems; PCNE, Pharmaceutical Care Network Europe; US, United States; WHO, World Health Organization; and WUCSH, Wachamo University Comprehensive Specialized Hospital.
References
Abate, W., Berhan, B., and Birhanetensay, M. (2020). Assessment of drug related problems among ambulatory heart failure patients on follows up at debre berhan comprehensive specialized hospital, debre berhan, Ethiopia, 2020.
AbuRuz, S., Jaber, D., Basheti, I., Sadeq, A., Arafat, M., AlAhmad, M., et al. (2021). Impact of pharmacist interventions on drug-related problems in general surgery patients: a randomised controlled trial. Eur. J. Hosp. Pharm. 28 (e1), e72–e78. doi:10.1136/ejhpharm-2020-002206
Alagiriswami, B., Ramesh, M., Parthasarathi, G., and Basavanagowdappa, H. (2009). A study of clinical pharmacist initiated changes in drug therapy in a teaching hospital. Indian J. Pharm. Pract. 2 (1).
Alayed, N., Alkhalifah, B., Alharbi, M., Alwohaibi, N., and Farooqui, M. (2019). Adverse drug reaction (ADR) as a cause of hospitalization at a government hospital in Saudi Arabia: a prospective observational study. Curr. drug Saf. 14 (3), 192–198. doi:10.2174/1574886314666190520105330
Al Hamid, A., Ghaleb, M., Aljadhey, H., and Aslanpour, Z. (2014). A systematic review of hospitalization resulting from medicine-related problems in adult patients. Br. J. Clin. Pharmacol. 78 (2), 202–217. doi:10.1111/bcp.12293
Aljadhey, H., Mahmoud, M. A., Hassali, M. A., Alrasheedy, A., Alahmad, A., Saleem, F., et al. (2014). Challenges to and the future of medication safety in Saudi Arabia: a qualitative study. Saudi Pharm. J. 22 (4), 326–332. doi:10.1016/j.jsps.2013.08.001
Ayalew, M. B., Tegegn, H. G., and Abdela, O. A. (2019). Drug related hospital admissions; a systematic review of the recent literature. Bull. Emerg. and Trauma. 7 (4), 339–346. doi:10.29252/beat-070401
Bekele, F., Tsegaye, T., Negash, E., and Fekadu, G. (2021). Magnitude and determinants of drug-related problems among patients admitted to medical wards of Southwestern Ethiopian hospitals: a multicenter prospective observational study. PLoS One 16 (3), e0248575. doi:10.1371/journal.pone.0248575
Belayneh, Y. M., Amberbir, G., and Agalu, A. (2018). A prospective observational study of drug therapy problems in medical ward of a referral hospital in northeast Ethiopia. BMC health Serv. Res. 18, 808–7. doi:10.1186/s12913-018-3612-x
Bhatty, E. T., Meraj, A., Malik, M., Imtiaz, M., Nasir, A., Saleem, N., et al. (2018). Drug related problems associated with polypharmacy: a literature review. Pak. J. Pharm. 30 (1).
Cipolle, R. J., Strand, L. M., and Morley, P. C. (2012a). Pharmaceutical care practice: the patient-centered approach to medication management. New York, NY, USA: McGraw-Hill Medical.
Cipolle, R. J., Strand, L. M., and Morley, P. C. (2021b). Pharmaceutical care practice: the patient-centered approach to medication management services.
Dammalapati, S. G., Challa, S. R., Challa, P., Irfan, M., Chanumolu, K., Pingili, R., et al. (2018). Incidence and factors associated with drug related hospital admissions in a south Indian tertiary care hospital. Indian J. Pharm. Pract. 11 (1), 37–43. doi:10.5530/ijopp.11.1.7
Degu, A., Karimi, P. N., Opanga, S. A., and Nyamu, D. G. (2023). Drug-related problems among esophageal, gastric and colorectal cancer patients at the national and referral hospital in Kenya. J. Oncol. Pharm. Pract. 30 (3), 493–506. doi:10.1177/10781552231178297
Haley, M., Raymond, C., Nishi, C., and Bohm, E. (2009). Drug-related problems in patients undergoing elective total joint arthroplasty of the hip or knee. Can. J. Hosp. Pharm. 62 (5), 360–366. doi:10.4212/cjhp.v62i5.822
Kjeldsen, L. J., Birkholm, T., Fischer, H., Graabæk, T., Kibsdal, K. P., Ravn-Nielsen, L. V., et al. (2014). Characterization of drug-related problems identified by clinical pharmacy staff at Danish hospitals. Int. J. Clin. Pharm. 36, 734–741. doi:10.1007/s11096-014-9939-4
Krähenbühl-Melcher, A., Schlienger, R., Lampert, M., Haschke, M., Drewe, J., and Krähenbühl, S. (2007). Drug-related problems in hospitals: a review of the recent literature. Drug Saf. 30, 379–407. doi:10.2165/00002018-200730050-00003
Levy, H. B. (2023). Maybe it's your medications: how to avoid unnecessary drug therapy and adverse drug reactions. Simon & Schuster.
Mattana, F., Muraglia, L., Barone, A., Colandrea, M., Saker Diffalah, Y., Provera, S., et al. (2024). Prostate-specific membrane antigen-targeted therapy in prostate cancer: history, combination therapies, trials, and future perspective. Cancers 16 (9), 1643. doi:10.3390/cancers16091643
Mejía, G., Saiz-Rodríguez, M., Gómez de Olea, B., Ochoa, D., and Abad-Santos, F. (2020). Urgent hospital admissions caused by adverse drug reactions and medication Errors—A population-based study in Spain. Front. Pharmacol. 11, 734. doi:10.3389/fphar.2020.00734
Meng, L., Qu, C., Qin, X., Huang, H., Hu, Y., Qiu, F., et al. (2021). Drug-related problems among hospitalized surgical elderly patients in China. BioMed Res. Int. 2021, 8830606. doi:10.1155/2021/8830606
Mohammed, M., Bayissa, B., Getachew, M., and Adem, F. (2022). Drug-related problems and determinants among elective surgical patients: a prospective observational study, SAGE Open Med. 10. doi:10.1177/20503121221122438
Muche, E. A., Amsalu, A., and Baraki, A. G. (2022). Drug-related problems and associated factors among hospitalized pediatric patients at the university of gondar comprehensive and specialized hospital. medRxiv.
Neville, H. L., Chevalier, B., Daley, C., Nodwell, L., Harding, C., Hiltz, A., et al. (2014). Clinical benefits and economic impact of post-surgical care provided by pharmacists in a Canadian hospital. Int. J. Pharm. Pract. 22 (3), 216–222. doi:10.1111/ijpp.12058
Niriayo, Y. L., Ayalneh, M., Demoz, G. T., Tesfay, N., and Gidey, K. (2023). Antimicrobial use related problems and determinants in surgical ward of Ethiopian tertiary hospital. Plos one 18 (12), e0296284. doi:10.1371/journal.pone.0296284
Oki, T., Ishii, S., Furukawa, K., Shono, A., and Akazawa, M. (2021). Assessment of the potential impact of resolving drug-related problems by clinical pharmacists in Japan: a retrospective observational study. J. Pharm. health care Sci. 7, 47–49. doi:10.1186/s40780-021-00232-9
Organization, W. H. (2024). Medication without harm: policy brief. Geneva, Switzerland: World Health Organization.
Patil, S. B., Jain, B. U., and Kondawar, M. (2019). A review on drug therapy problems. Asian J. Res. Pharm. Sci. 9 (2), 137–140. doi:10.5958/2231-5659.2019.00020.1
Pazan, F., and Wehling, M. (2021). Polypharmacy in older adults: a narrative review of definitions, epidemiology and consequences. Eur. Geriatr. Med. 12, 443–452. doi:10.1007/s41999-021-00479-3
Phatak, A., Prusi, R., Ward, B., Hansen, L. O., Williams, M. V., Vetter, E., et al. (2016). Impact of pharmacist involvement in the transitional care of high-risk patients through medication reconciliation, medication education, and postdischarge call-backs (IPITCH study). J. Hosp. Med. 11 (1), 39–44. doi:10.1002/jhm.2493
Qu, C., Meng, L., Wang, N., Chen, Y., Yang, X., Wang, J., et al. (2019). Identify and categorize drug-related problems in hospitalized surgical patients in China. Int. J. Clin. Pharm. 41, 13–17. doi:10.1007/s11096-018-0777-7
Short, A., McPeake, J., Andonovic, M., McFee, S., Quasim, T., Leyland, A., et al. (2023). Medication-related problems in critical care survivors: a systematic review. Eur. J. Hosp. Pharm. 30 (5), 250–256. doi:10.1136/ejhpharm-2023-003715
Tefera, G. M., Zeleke, A. Z., Jima, Y. M., and Kebede, T. M. (2020). Drug therapy problems and the role of clinical pharmacist in surgery ward: prospective observational and interventional study. Healthc. Patient Saf. 12, 71–83. doi:10.2147/DHPS.S251200
Tegegn, H. G., Abdela, O. A., Mekuria, A. B., Bhagavathula, A. S., and Ayele, A. A. (2018). Challenges and opportunities of clinical pharmacy services in Ethiopia: a qualitative study from healthcare practitioners' perspective. Pharm. Pract. (Granada) 16 (1), 1121. doi:10.18549/pharmpract.2018.01.1121
Wood, D., and Lightfoot, N. (2018). An audit of regular medication compliance prior to presentation for elective surgery. N. Z. Med. J. (Online) 131 (1480), 75–80.
Keywords: drug therapy problems, magnitude, prevalence, surgical patients, central Ethiopia
Citation: Seid T, Abdela J, Dechasa M and Nigussie S (2025) Drug therapy problems and associated factors among adult patients admitted to the surgical ward in a resource-limited setting. Front. Pharmacol. 16:1548105. doi: 10.3389/fphar.2025.1548105
Received: 19 December 2024; Accepted: 18 June 2025;
Published: 04 July 2025.
Edited by:
Catherine M. T. Sherwin, University of Western Australia, AustraliaReviewed by:
Yaman Walid Kassab, National University of Science and Technology, OmanAbdul Wahid, Quaid-i-Azam University, Pakistan
Yirga Legesse Niriayo, Mekelle University, Ethiopia
Copyright © 2025 Seid, Abdela, Dechasa and Nigussie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mesay Dechasa, bWVzYXlnYzIwMDhAZ21haWwuY29t
 Taju Seid1
Taju Seid1 Jemal Abdela
Jemal Abdela Mesay Dechasa
Mesay Dechasa Shambel Nigussie
Shambel Nigussie