Abstract
Introduction:
Pregnant women use medicinal plants for the treatment of illnesses associated with pregnancy. Women might resort to using medicinal plants because they are easily accessible and inexpensive. This study aims to determine the prevalence, to document and to analyse the traditional use of medicinal plants during pregnancy.
Methods:
A cross-sectional study was conducted among pregnant and postpartum women attending the Obstetrics and Gynecology Service at the regional hospital center, Hassan II of Souss Massa region. An Ethnopharmacological survey was used for data collection. After collection, data were coded, entered, and analyzed by Jamovi Software.
Results:
A total of 420 women participated in this study. The mean age was 28.7 ± 6.35. The prevalence of herbal medicine consumption among pregnant and postpartum women is 48% with CI 95% (43.2%–52.7%). 35 varieties of medicinal plants from 22 families were used during pregnancy. Each of the other families had one species. Plant extracts were primarily prepared through decoction, infusion, maceration, Fumigation, extraction, and powder. The oral route was the most common route of administration used, about the number of plates used by pregnant and postpartum women (90.9%).
Conclusion:
The utilization of herbal medicine among pregnant mothers in this study was high in the region of Souss Massa. This research expands our understanding of the role that different plant species have in the management of disorders that affect women during pregnancy.
Introduction
Herbal medicine is known as the practice of using plant-derived substances or preparations for the treatment, diagnosis, prevention, and maintenance of health (World Health Organization, 2001). Based on the World Health Organization’s data, up to 80% of Africans still depend on traditional medicine to manage their healthcare requirements, while in China, traditional medicines make up an estimated 40% of all healthcare services (World Health Organization, 2002). Throughout the world, herbal medicines use is frequently used during pregnancy (Adams et al., 2009; Hall et al., 2011; Pallivalappila et al., 2013). Based on a study reported that approximately of 50% of pregnant women from various non-American nations utilized at least one herbal medicine (Strouss et al., 2014). In the Arabian countries, a systematic review investigated the prevalence of using herbal medicine in pregnancy in the Middle East and North Africa showed a high prevalence varied from 22.3% to 82.3% (John and Shantakumari, 2015). In southern Morocco, a cross-sectional study conducted by Kamel et al. (Kamel et al., 2022) found that 375 pregnant women out of 560 (70%) used herbal products during pregnancy and these were used for a variety of things, including pain relief, easing childbirth, preventing flu syndrome, treating anemia, and inducing delivery (Kamel et al., 2022).
Throughout pregnancy, the female’s body experiences physical and physiological changes which can cause a variety of disorders related to pregnancy, such as heartburn, nausea, vomiting, and constipation (Bruno et al., 2018). Pregnancy is mostly accompanied by minor complaints. However, these complaints can rarely cause serious problems that could affect the health of the mother and newborn and eventually result in their mortality. The World Health Organization and the United Nations International Children’s Emergency Fund reported that each year, health problems related to pregnancy or childbirth cause the deaths of more than 500,000 women and four million newborns who are less than 1 month old (La Situation Des Enfants Dans Le Monde, 2009; World Health Organization, 2007). Poverty and risky pregnancies (refer to pregnancies in which the health of the mother, the baby, or both is at an increased risk of complications before, during, or after childbirth) are closely related to 99% of all deaths worldwide as represented in Asia and Sub-Saharan Africa (World Health Organization, 2008). Furthermore, the use of conventional medication during pregnancy has been greatly limited due to the first-term pregnancy’s teratogenic sensitivity and the adverse effects caused by synthetic medicines, for example Aristolochia spp. (Birthwort) contains aristolochic acids, which are known to cause severe kidney damage, increase the risk of urothelial cancer, and lead to DNA mutations. Despite its historical use in traditional medicine, Aristolochia has been banned in many countries due to its carcinogenic properties. Another highly toxic herb is Aconitum spp. (Aconite, Monkshood, Wolf’s Bane), which contains aconitine, a potent neurotoxin and cardiotoxin. Even in small doses, aconite can cause severe cardiac arrhythmias, paralysis, and respiratory failure, often leading to death. Due to their concerns for the fetus’ safety, pregnant women frequently turn to natural medicin rather than prescribed medications to deal with these changes. To resolve some of these problems pregnant women favor the return to phytotherapy (Pinn and Pallett, 2002). Previous studies have reported the use of herbal medicine among pregnant women according to the geographical location, socio-cultural character, and ethnicity of the pregnant women, the prevalence of herbal medicine used to treat maternal problems ranged widely from 33% to 77.1% (Abd El-Mawla, 2020; Aljofan and Alkhamaiseh, 2020; Eid et al., 2020; Sadeghia and Mahmood, 2014).
The limited clinical data on the safety and effectiveness of herbal medicines makes the benefit-risk assessments very difficult but some herbs have been identified as being harmful and contain toxic elements (Ahmed et al., 2017). Furthermore, nothing is known about the interactions between different herbs, drugs, and foods. Due to additives or contamination with poisonous metals or even hidden conventional medicines, herbal treatments have been associated with undesirable side effects (Saper et al., 2004). The risk of undesired effects is increased by a limited understanding of the potential risks of some herbs during pregnancy as well as the fact that natural herbs and vitamin supplements are not subject to the Food Drugs Administration assessment procedure necessary for prescribed drugs (Skerrett and Harvard Health, 2012).
Morocco is a Mediterranean nation that has a rich heritage of phytotherapy (Jouad et al., 2001). Many authors have investigated traditional pharmacopeia in various regions of Morocco. There is a lack of available information on the usage of herbs in pregnancy, especially in the Souss Massa region. However, some studies reported the use of herbal medicines among Moroccan Southern populations (El-Ghazouani et al., 2021). The Agadir Ida Outanane province is particularly notable for its rich diversity of medicinal plants. (Thymus vulgaris L., Lavandula angustifolia Mill., Argania Spinosa (L). However, this region is characterized by unregulated and excessive use of botanical species, surpassing the natural regeneration capacity and posing a threat to certain species (Ouhaddou et al., 2014).
This study aims to determine the prevalence, and focus on documenting and analyzing the traditional use of medicinal plants consumption during pregnancy, labor, and after delivery in the Hospital Center Hassan II at Souss Massa region.
Material and methods
Study area
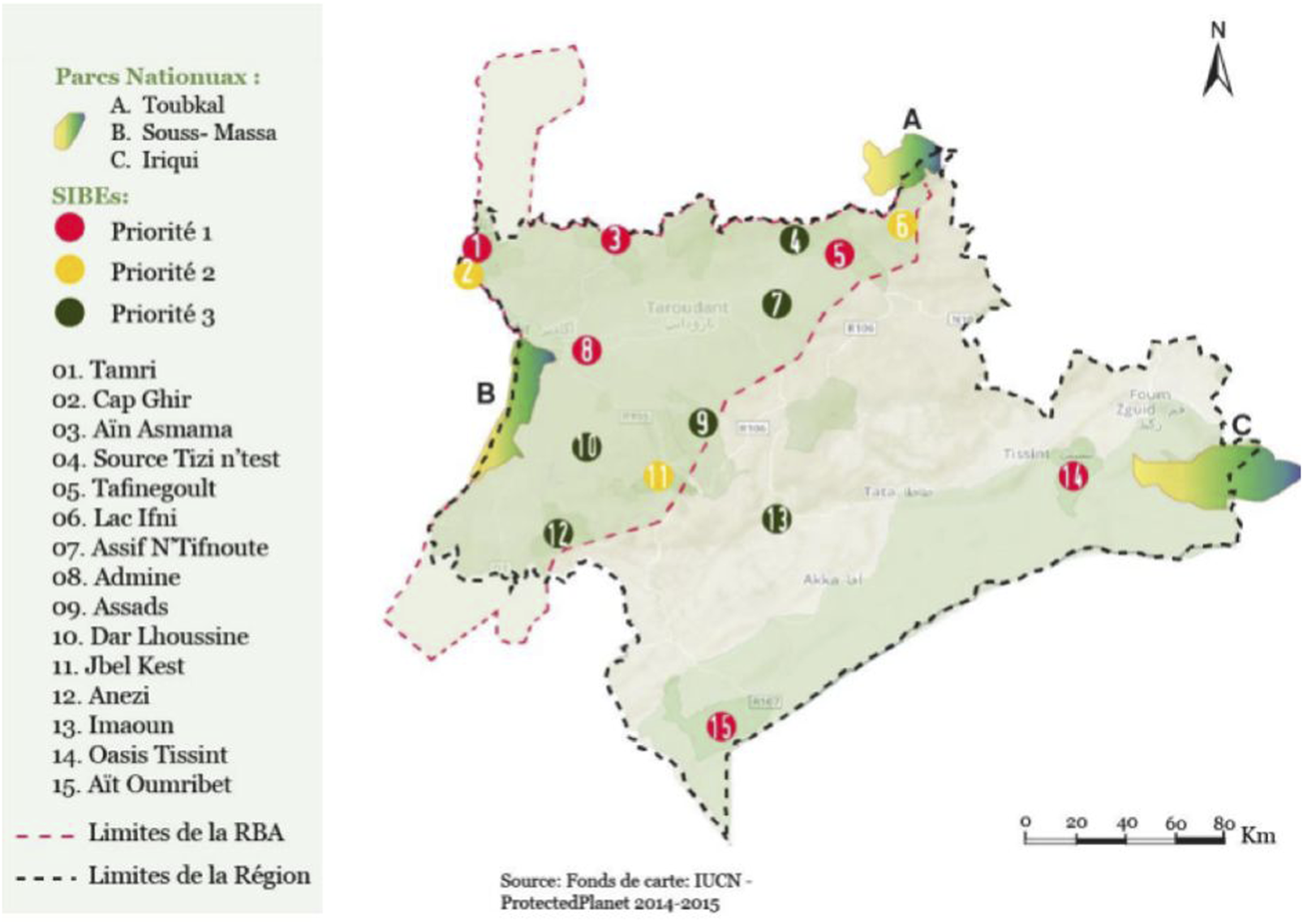
Souss Massa region Covering an area of 53,789 km2, i.e., 8% of the national territory, the Souss Massa region is made up of 2 prefectures: Agadir Ida Outanane and Inezgane Ait Melloul and 4 provinces: Chtouka Ait Baha, Tiznit, Taroudannt, and Tata. The total population reached 2 million 677 thousand inhabitants in 2014, which is 8% of the national population. The rate of urbanization of the regional population reached nearly 56% (compared to 60.3% at the national level). The population density of 50 inhabitants per km2 is slightly higher than the national average (Monographie régionale souss massa, 2020) (Figure 1).
FIGURE 1

Map of the Sous Massa Region and boundaries of the study area; High Commission for Planning–Souss Massa regional directorate.
Flora biodiversity of Souss Massa region
The Souss Massa region is a vast fertile plain punctuated on the edge of two river valleys. This bioclimatic zone is of botanical and environmental interest. The coexistence of both Mediterranean and Saharan regions in this area allows it to have species originating from both climates. Some of these species are rare or even threatened, and they do not extend beyond this natural border (Author anonymous, 2025a). Due to specific environmental conditions, the flora has had to adapt, evolve, and over time, differentiate from the rest. The region is home to around fifty endemic plant species (Author anonymous, 2025b). On a territorial scale, the total forest area is estimated at over 1.5 million hectares, including Argan trees, Junipers, Pine, and Evergreen Oak. Approximately 801,810 ha are prominently occupied by the Argan tree in a more or less pure state, with various combinations with other forest species or on cultivated lands as the main species (SIREDD, 2025) (Figure 2).
FIGURE 2
Map of the Sous Massa Region and flora diversity of the region; Ministry Of Energy Transition And Sustainable Development, Morocco (SIREDD, 2025).
Study design and period
This is a cross-sectional, descriptive, and analytical study of women attending the Obstetrics and Gynecology Service at the regional hospital center Hassan II conducted in the region of Souss Massa. This study was conducted from April 2022 to December 2022 to assess the consumption of herbal medicines among pregnant and postpartum women.
Sample size determination and sampling method
Using the prevalence of a previous study (Ekrasarian et al., 2017). The sample size was determined by using the single-proportion formula.
Based on the assumption that 10% of participants would not reply and the prevalence is 48% a conservative choice (p = 0.05) has been employed. To ensure that the estimation error would be at most alpha 0.05 with 95% confidence. The calculated optimal sample size was 383. Three hundred eighty-three pregnant women formed the initial calculated sample size, but the sample size was expanded to 420 to account for any missed data or non-response rate to ensure reliability. A convenient sampling technique was used in this study (Bartlett et al., 2025; Cochran, 1977). In this survey, we employed random sampling. Each day, we visit the gynecology and obstetrics department to record new patient cases. We then compile a database of all pregnant and postpartum women who have visited the department in the past 24 h. This list is entered into Excel, and using the random function, we randomly select participants from the list.
Study population
The study chose to include all of the expecting pregnant women who came forward to the Obstetrics and Gynecology Service at the regional hospital center Hassan II either for the prenatal consultation (PNC) or for giving birth. To collect as much as possible data on the use of herbal medicines during pregnancy and childbirth, the research systematically enrolled all women who were admitted to the hospital’s maternity department during the study period.
Inclusion criteria: all voluntary and consenting pregnant or post-partum women presenting themselves for prenatal consultation at all of the primary healthcare institutions in the network, and women who were admitted to give birth at the maternity at the regional hospital center Hassan II.
Questionnaire
The questionnaire was prepared and reviewed by a panel of specialists in the fields of clinical pharmacology and biostatistics for content validity. A primary survey was used to conduct a pilot study. The pilot study aimed to measure the respondents’ comprehension of the questions. There were five sections in the questionnaire. The first component of the survey asked questions about the respondents’ socioeconomic status and demographic details, including their age, place of residence, level of education., income, occupation, and social security. The second section is related to pregnancy such as exercise, diet, smoking, and alcohol intake. It includes also the reason for consultation and the time of pregnancy. The third part of the questionnaire covered information on the use of herbal medicine, including the common names for each species, the methods of preparation and administration, the period of use and reasons for use, and their sources of information. The last part includes some questions about the safety of medicinal herbs used by the participants. Women who were pregnant in their first trimester provided information on self-medication during this period, those who were pregnant in their second and third trimesters released details on the first and second trimesters, and those who were pregnant in their third and final trimesters or were in term of childbirth provided information on the whole period of their pregnancy. The questionnaire is attached to the manuscript as an appendix for your reference.
Data collection procedure
Women who met the study’s eligibility requirements and consented were asked to complete the questionnaires on their own. However, the researchers conducted oral interviews with a small number of illiterate women to complete their questionnaires. The researchers avoided lead questions to prevent any biases and just read the questions for those women. When necessary, the women received explanations to make sure they comprehended the questions.
The research administrators addressed the subjects and explained the purpose of the study to them. All participants were then given an informed consent form to sign before receiving a printed copy of the surveys and were given time to complete them. The completed questionnaires were securely stored in a locked cabinet to ensure confidentiality. Access was restricted to authorized personnel only, and electronic copies were stored on a password-protected computer system to further safeguard the data. The ethnobotanical data was collected, as well as the botanical name of the plant, family name, vernacular name, plant part(s) used in herbal preparation, mode of application to treat women’s diseases, and the method(s) by which it is prepared (i.e. decoction, maceration, power, or infusion …). Data was uploaded and saved into a well-structured and organized file that ensures data accuracy, consistency, and ease of analysis.
Ethical approval
The biomedical research ethics committee of the Faculty of Medicine and Pharmacy in Rabat, Morocco approved the study protocol. Before starting, the study was approved by the biomedical research ethics committee at Mohamed V University (68-21). All procedures were performed by the revised Declaration of Helsinki published in October 2013 (WMA, 2025). Additionally, a signed informed consent form was provided from each participant. These were worded and indicated the purpose of the study. Confidentiality was ensured by giving each participant a code number for analysis. There was no financial assistance, no rewards, and no conflict of interest. Each responder had the option of not taking part in the survey. It was also emphasized that their access to medical treatment will not be impacted.
Statistical analysis
For the study subjects, descriptive statistical analyses were conducted. The mean and standard deviation (SD) were used to describe continuous variables, while proportions were used to summarize categorical variables. Demographic and pregnancy-related factors were evaluated and compared with regard to herbal medicine usage. The chi-square test was used to compare data. Statistical significance was considered at P < 0.05 (Author anonymous, 2025b; Jamovi, 2025).
Relative frequency of citation (RFC)
Ethnobotanical data were analyzed using the frequency of citation (FC) and relative frequency citation (RFC) to determine which species were well-known and most used by the participants in this study. The frequency of citation (FC), or the number of informants who reported using a species, was divided by the total number of informants who took part in the survey (N), to get the relative frequency of citation (RFC). RFC index varies from zero (no one mentions the plants as valuable) to one (every informant would consider it as useful) (Tardío and Pardo-de-Santayana, 2025).
Results
General characteristics of the population surveyed
The characteristics of the study participants are shown in Table 1. A total of 420 pregnant women and postpartum women were consecutively interviewed. The mean age was 28.7 ± 6.35. Almost all (95.7%) of the respondents were married, 51.4% were living in rural areas, 87.9% were housewives, 42.1% had at least a middle school education and only those with a university level represented 4%. More than half of the participants (72.1%) belonged to low-income households. Women with health insurance made up 23.1% of the population, while those insured by the Medical Assistance Scheme for Economically Underprivileged Persons (RAMED),Medical Assistance Scheme, represented 24%. In terms of gestation, 67.4% were postpartum, and 22.9% third-trimester.
TABLE 1
| Variable | Overall n (%) | Non Herbal Medicine users n (%) | Herbal Medicine users n (%) | P-value |
|---|---|---|---|---|
| Age | ||||
| 28.7 ± 6.35 | 28.8 ± 6.15 | 28.6 ± 6.57 | 0.700 | |
| Family situation | ||||
| Not Married | 18 (4.3) | 7 (3.2) | 11 (5.4) | 0.259 |
| Married | 402 (95.7) | 211 (96.8) | 191 (94.6) | |
| Origin | ||||
| Rural | 216 (51.4) | 118 (54.1) | 98 (48.5) | 0.250 |
| Urbain | 204 (48.6) | 100 (45.9) | 104 (51.5) | |
| Nationality | ||||
| Not Moroccan | 3 (0.7) | 2 (0.9) | 1 (0.5) | 1.000 |
| Moroccan | 417 (99.3) | 216 (99.1) | 201 (99.5) | |
| Education | ||||
| Illiterate | 133 (31.7) | 62 (28.4) | 71 (35.1) | 0.140 |
| Educated | 287 (68.3) | 156 (71.6) | 131 (64.9) | |
| Employement | ||||
| Unemployed | 369 (87.9) | 191 (87.6) | 178 (88.1) | 0.874 |
| Employed | 51 (12.1) | 27 (12.4) | 24 (11.9) | |
| Income level | ||||
| Low | 303 (72.1) | 161 (73.9) | 142 (70.3) | 0.417 |
| Middle | 117 (27.9) | 57 (26.1) | 60 (29.7) | |
| Medical insurance | ||||
| None | 222 (52.9) | 117 (53.7) | 105 (52) | 0.729 |
| Insured | 198 (47.1) | 101 (46.3) | 97 (48) | |
| Parity | ||||
| Nulliparity | 44 (10.5) | 25 (11.5) | 19 (9.4) | 0.491 |
| Parity | 376 (89.5) | 193 (88.5) | 183 (90.6) | |
| Nutrition | ||||
| Healthy | 312 (74.3) | 168 (77.1) | 144 (71.3) | 0.176 |
| Mixed | 108 (25.7) | 50 (22.9) | 58 (28.7) | |
| Sport | ||||
| No | 229 (54.5) | 112 (51.4) | 117 (57.9) | 0.178 |
| Yes | 191 (45.5) | 106 (48.6) | 85 (42.1) | |
| Yes | 1 (0.2) | 0 (0) | 1 (0.5) | |
| Pregnancy Age | ||||
| Pregnant | 125 (29.8) | 61 (28) | 64 (31.7) | 0.407 |
| Postpartum | 295 (70.2) | 157 (72) | 138 (68.3) | |
| Malformation | ||||
| No | 416 (99) | 218 (100) | 198 (98) | 0.053* |
| Yes | 4 (1) | 0 (0) | 4 (2) | |
| Premature | ||||
| None | 416 (99) | 216 (99.1) | 200 (99) | 1.000 |
| Yes | 4 (1) | 2 (0.9) | 2 (1) | |
| Miscarriage | ||||
| None | 405 (96.4) | 213 (97.7) | 192 (95) | 0.143 |
| Yes | 15 (3.6) | 5 (2.3) | 10 (5) | |
| Gestational diabetes | ||||
| None | 346 (82.4) | 178 (81.7) | 168 (83.2) | 0.683 |
| Yes | 74 (17.6) | 40 (18.3) | 34 (16.8) | |
| Hypertension | ||||
| None | 383 (91.2) | 201 (92.2) | 182 (90.1) | 0.447 |
| Yes | 37 (8.8) | 17 (7.8) | 20 (9.9) | |
| Pregnancy at Risk | ||||
| None | 127 (30.7) | 61 (28) | 68 (33.7) | 0.207 |
| Yes | 291 (69.3) | 157 (72) | 134 (66.3) | |
| Pregnancy Follow up | ||||
| Not followed | 125 (29.8) | 61 (28) | 64 (31.4) | |
| Followed | 295 (70.2) | 157 (72) | 138 (68.3) | |
| What type of treatment do you prefer to take during pregnancy | ||||
| None | 40 (10.7) | 27 (13.4) | 13 (7.6) | 0.020* |
| Herbal Medicine | 82 (22) | 37 (18.4) | 45 (26.2) | |
| Drugs | 217 (58.2) | 124 (61.7) | 93 (54.1) | |
| Both | 34 (9.1) | 13 (6.5) | 21 (12.2) | |
Socio-demographic and obstetric characteristics of participants (n = 420) and their association with Herbal medicine use during pregnancy.
∗ Values in bold represent statistically significant differences (p < 0.05)
Designing the habits during pregnancy, the majority of the respondents 74.3% have a healthy diet, generally, they have a Mediterranean diet. 45.5% of women are physically active.
Prevalence of herbal medicine consumption among pregnant and postpartum women
The prevalence of herbal medicine consumption among pregnant and postpartum women is 48% with Confidence interval CI 95% (43.2%–52.7%). A total of 202 women who participated in the survey reported using an herbal medicine during pregnancy. A comparison of the Socio-demographic and obstetric characteristics of herbal and non-herbal medicine users during pregnancy. The results indicated that no significant difference (p-value >0.05) resulted in all sociodemographic and obstetric characteristics, with the exception in terms of malformation and the type of treatment that the participants prefer to take during pregnancy which showed a significant difference p-value <0.05 (Table 1). As revealed in Table 1, pregnant and postpartum women who reported a malformation used herbal medicine (p-value = 0.053) and 26.2% of women who preferred to be treated by herbal medicine used it during pregnancy and 61.7% of women who preferred to use drugs reported that they did not use the herbal medicine during pregnancy (p-value = 0.020).
Diversity of plant species used
According to the survey, 35 varieties of medicinal plants from 22 families were used during pregnancy to treat gynecologic and obstetrics diseases. A list of the scientific and common names, the family, illness treated, plant part(s), method of preparation, and mode of administration are presented in Table 2. The Lamiaceae and Apiaceae families contributed the most species with (Pallivalappila et al., 2013), followed by Compositae (Adams et al., 2009), and Alliaceae (World Health Organization, 2002). Each of the other families had one species. However, the current study results reported that mugwort (Artemisia herba-alba Asso), lavender (Lavandula angustifolia Mill.), thyme (Thymus maroccanus Ball), fennel (Foeniculum vulgare Mill.)), fenugreek (Trigonella foenum-graecum L), verbena (Aloysia citriodora Palau) and cinnamon (Cinnamomum verum J. Presl.) are the most plants that are cited by the pregnant women with FC of 43, 33, 28,25, 19, and 11respectively as presented in Table 2.
TABLE 2
| Plant family | Plant species | Vernacular name | Preparation method | Solvant used | Used parts | Administration route | Reason of use | Frequency of citation Fc | Relative frequency of citation RFC |
|---|---|---|---|---|---|---|---|---|---|
| Alliaceae | Allium cepa L. | Onion | Decoction | Milk | Fruit, Seeds | Oral | Cold/Flu/Cough Allergy | 2 | 0.005 |
| Allium sativum L. | Garlic | Decoction | Olive Oil | Fruit | Oral | Respiratory diseases | 1 | 0.002 | |
| Apiaceae | Cuminum cyminum L. | Cumin | Infusion | Water | Seeds | Oral | Abdominal Pain Intestinal Gas. | 1 | 0.002 |
| Pimpinella anisum L. | Green anise | Powder, maceration, infusion | Water | Seeds | Oral | Gastric pain Abdominal Pain Intestinal Gas. Cough | 5 | 0.012 | |
| Foeniculum vulgare Mill. | Fennel | infusion, decoction, Powder | Water | Seeds | Oral | Abdominal Pain Intestinal Gas. Nausea and Vomissement Gastric pain | 28 | 0.067 | |
| Ammodaucus leucotrichus Coss. Durieu | Woolly cumin | Infusion | Water | Seeds | Oral | Abdominal Pain Intestinal Gas. | 1 | 0.002 | |
| Carum carvi L. | Caraway | Infusion | Water | Seeds | Oral | Intestinal Gas | 1 | 0.002 | |
| Brassicaceae | Lepidium sativum L. | Cress Garden | Infusion, decoction | Milk, Eggs Yolk | Seeds | Oral | Amenorrhea. Accelerate labor (Childbirth) | 6 | 0.014 |
| Compositae | Artemisia herba-alba Asso | Mugwort | Infusion | Water,Tea | Whole Plant | Oral/Vaginal | Induces an abortion Abdominal pain. pruritus, vaginal itching. Urinary infections Gastric Pain | 43 | 0.102 |
| Dolomiaea baltalensis Dar & Naqshi | Costus Indien | Infusion | Water | Roots | Oral | Diabetes | 1 | 0.002 | |
| Matricaria chamomilla L. | Chamomile | Infusion | Water | Flowers | Oral | to relieve and reduce stress. Abdominal and uterine pain | 4 | 0.010 | |
| Fabaceae | Trigonella foenum-graecum L. | Feneugrec | Maceration, powder | Water, Honey | seeds | Oral | Epigastralgie, Pyrosis To induces an Abortion Appetite, To increase weight |
25 | 0.060 |
| Fagaceae | Quercus lusitanica Lam. | Gall Oak | Decoction | Water | fruit | Vaginal | Vaginal itching Pruritus | 1 | 0.002 |
| Iridaceae | Crocus sativus L. | Saffron | Infusion | Water,Tea | Flower stigma | Oral | Acceleration of Labor Cold/Flu/Cough | 6 | 0.014 |
| Lamiaceae | Lavandula angustifolia Mill. | Lavender | Infusion,fumigation | Water | Leaf | Oral/Vaginal | Vaginal itching induces an abortion. Infection urinary Flu/cold. Diabetes | 33 | 0.079 |
| Rosmarinus officinalis L. | Rosemary | Infusion, decoction | Water | Oral | Intestinal Gas | 5 | 0.012 | ||
| Thymus maroccanus Ball | Thyme | Infusion,decoction, fumigation | Water, Milk, Tea | Leaf | Oral/Vaginal/Nasal | Cold/Flu/Cough, Urinary burns, Abdominal pain, Asthma Diabetes, Facilte Labor (Childbirth), Epigastralgie, Pyrosis. Amenorrhea Intestinal Gas pruritus, vaginal itching | 33 | 0.079 | |
| Marrubium vulgare L. | Marrube blanc | Infusion, decoction | Water | Whole Plant | Vaginal | Vaginal itching | 2 | 0.005 | |
| Salvia officinalis L. | Sage | Infusion | Water,Tea | Leaf | Oral | Diabetes, Fertility | 5 | 0.012 | |
| Lauraceae | Cinnamomum verum J. Presl | Cinnamon | Powder | Milk, Cola, Eggs Yolk, Orange Juice | Internal bark of the tree | Oral | induces an abortion Gastric Pain, Amenorrhea, Anemia, Accelerate labor | 11 | 0.026 |
| Leguminosae | Glycyrrhiza glabra L. | Licorice | Infusion, decoction | Water | Roots | Oral | Allergy, To Induce an Abortion | 2 | 0.005 |
| Lythraceae | Punica granatum L. | Grenade | Infusion | Water | Fruit peels | Oral | Nausea, Vomissement | 1 | 0.002 |
| Myrtaceae | Syzygium aromaticum (L.) Merr. and Perry | Clove | Infusion,fumigation | Water | Seeds | Oral, Nasal | Cold/Flu/Cough | 1 | 0.002 |
| Oleaceae | Olea europaea L. | Olive | Extraction | - | Oil | Dermal, Oral | Vaginal itching Flu/cold/Cough | 3 | 0.007 |
| Pedaliaceae | Sesamum indicum L. | Sesame | Maceration | Water | Seeds | Oral | Gastric pain | 1 | 0.002 |
| Ranunculaceae | Nigella sativa L. | Nigella | infusion, powder | Water, Honey, Olive Oil | Seeds | Oral | Abdominal and uterine COVID-19. To Induce Labor | 7 | 0.017 |
| Rosaceae | Prunus dulcis (Mill.) D.A.Webb |
Almond |
Extraction | - | Oil | Dermal | Stretch marks | 1 | 0.002 |
| Rubiaceae | Rubia tinctorum L. | Rubia | Powder | Honey | Whole Plant | Oral | Anemia | 1 | 0.002 |
| Schisandraceae | Illicium verum Hook.f. | Star anise | Infusion | Water | seeds | Oral | Cold/Flu/Cough Allergy Respiratory diseases | 2 | 0.005 |
| Verbenaceae | Aloysia citriodora Palau | Verbena | Infusion, decoction | Water,Tea | Leaf | Oral | Abdominal and uterine pain Intestin gas Hight blood pressure to relieve and reduce stress | 19 | 0.045 |
| Xanthorrhoeaceae | Aloe vera (L.) Burm.f. | Aloe | Infusion | Water | Leaf | Oral | to relieve | 1 | 0.002 |
| Zingiberaceae | Zingiber officinale Roscoe | Ginger | Infusion, decoction | Water, Milk | Roots | Oral | Cold/Flu/Cough to induces an Abortion | 3 | 0.007 |
| Zygophyllaceae | Peganum harmala L. | Harmel | Fumigation | Water | Seeds | Oral/Nasal | To induce Abortion Cold/flu/Cough | 3 | 0.007 |
List of herbal medicine used among pregnant and postpartum women.
Aliments treated using medicinal plant species
Medicinal plant species were used to treat a total of 22 diseases. The diseases related to the period of pregnancy and delivery like digestive disorders, infections, anemia, and finally skin complications, sleep disorders, and weight loss are the final three less common causes we have noticed among some users. Several illnesses were treated with a single plant species, while others were treated with a combination of plant parts from various species. In contrast to herbal mixes, monotherapy preparations were more common. Table 2.
Method of preparation and administration
The current findings revealed that herbal preparations are administered through a variety of routes. The methods of preparation are shown in Table 2. Plant extracts were primarily prepared through decoction, infusion, maceration, Fumigation, extraction, and powder. The main solvent used in the preparation of herbal remedies was water and milk. Some of the preparation was prepared using specific ingredients such as orange juice, egg yolk, and a tea infusion. Infusions (69.69%) were frequently employed, which involves soaking plant material in hot or warm water and letting the combination cool. Decoctions (33.3%) were prepared by boiling plant materials in a specific amount of water for 15–20 min and allowing the mixture to cool before administration. In 9.9% of the plant species, maceration was employed to extract a liquid for patient administration by crushing plant components from a single species or a mixture of plant parts from several species. Minor preparation methods such as pounding (18.18%) like usage of the powder of the plants and fumigation were used with a low frequency in the range of 12.12% % of the medicinal plant species. Fumigation of the plant was used by dropping a mixture of plants in a bowl filled with boiling water, the mode of use is to inhale the steam while holding a towel over the nose. There is another Moroccan traditional method of fumigation consisting to use hot charcoal to burn the plant so that the smoker is sprayed by the user. Extraction (6.06%) is defined as the separation of triglyceride (TAG) using a variety of mechanical or chemical manipulation techniques.
The oral route was the most common route of administration used about the number of plates used by pregnant and postpartum women (90.9%), followed by vaginal (15.15%), nasal (9.9%), and dermal (6.6%). The oral route was administered by swallowing dry powdered plant materials, particularly plant seeds, drinking decoctions, infusions, and maceration extracts (Table 2).
Reasons and source of information for herbal medicine usage during pregnancy
As shown in Table 3, 92.9% of participants agreed that herbal medicine uses are not harmful to pregnant women and for the fetus and it can be used freely during pregnancy. Although 22% of the participants use herbal medicine because they are available and more accessible compared to medical therapy. Only 3 (2.4%) of the participants reported that herbal medicine costs are cheaper than medical therapy. Seventy (52.6%) of the respondents reported using herbal medicine based on their previous experiences and 44.4% of the participants were recommended by their family, and 3.8% by friends and physicians, respectively. Only 2.3% of the participants get information from the internet about the use of herbal medicine.
TABLE 3
| Reasons of herbal medicine uses | n (%)a |
|---|---|
| They are available and more accessible compared to medical therapy | 28 (22) |
| Their cost is cheaper than medical therapy | 3 (2.4) |
| They are not harmful for you and your baby during pregnancy. | 118 (92.9) |
| Sources of information | n (%)a |
|---|---|
| Family | 59 (44.4) |
| Friends | 5 (3.8) |
| Internet | 3 (2.3) |
| Myself | 70 (52.6) |
| Physician | 5 (3.8) |
Reasons and sources of information about herbal medicine uses by the participants during pregnancy.
Total percentages exceed 100% due to the selection of more than one source.
Disclosure, satisfaction, and side effects of herbal medicine use in pregnancy
Only 11.2% of the participants were asked if they disclosed herbal medicine used to a medical doctor. The majority of the participants (78.1%) reported that they remark on the benefits of taking herbal medicine during pregnancy. In contrast, some of the participants (5.9%, 4.4%), respectively, observed special side effects and suspected a miscarriage from taking herbal medicine during pregnancy (Supplementary Table S1).
Discussion
This is the first ethnopharmacology study conducted among pregnant and postpartum women. This study aims to determine the prevalence, and motives behind herbal medicine consumption during pregnancy, during labor, and after delivery in the Hospital Center Hassan II at Souss Massa region. The findings of this study showed that the prevalence of herbal medicine consumption among pregnant and postpartum women at Hospital Center Hassan II of Souss Massa region was 48% with CI 95% (43.2%–52.7%). This is identical to the prevalence found in a similar study. 48.6% reported in a study conducted at the University of Gondar teaching hospital (northwest Ethiopia) (Mekuria et al., 2017), 40% in Palestine (Al-Ramahi et al., 2013) and 48.4% (Abdollahi et al., 2018), 48% (Ekrasarian et al., 2017) each in Iran. In Morocco, a study showed that pregnant women in the province of Guelmim also use MPs during pregnancy with a prevalence of 66.96% (Kamel et al., 2023). Similar findings are reported in other studies with the prevalence of medicinal plants being very high (Eid et al., 2020; Ali-Shtayeh et al., 2015; Yazdi et al., 2019; Dabirifard et al., 2017). This rate is significantly high compared to our findings. These variations in prevalence could be associated with the existence and implementation of regulations governing the sales of medicinal plants, the affordability and availability of herbal products, as well as cultural variations among study participants which differ from one country to another.
This study showed that the participants reported that the main reason for medicinal plant use are easy accessibility, effectiveness, lower cost and there are not harmful for the pregnant woman and for her baby. This finding is consistent with other studies conducted at Hossana town health facilities (Bayisa et al., 2014), and a review of published literature from Middle Eastern countries all of which indicate similar reasoning for herbal medicine use (John and Shantakumari, 2015).
The present study showed that the most common use of herbal medicine among pregnant women was mugwort (Artemisia herba-alba Asso), lavender (Lavandula angustifolia Mill.), thyme (Thymus maroccanus Ball), fennel (Foeniculum vulgare Mill.)), fenugreek (Trigonella foenum-graecum L), verbena (Aloysia citriodora Palau) and cinnamon (Cinnamomum verum J. Presl.). In a study conducted in a region located in the south of Morocco, they found that the herbs used were (mugwsort) A. herba-alba Asso, (thyme) T. maroccanus Ball., (verbena) A. citriodora Palau, and, (fenugreek) T. foenum-graecum L. This similarity can be explained by the identical geographic culture between the two regions: Sous Massa and Guelmim wish both are located in the south of Morocco. In this region, there is a large number of species which have been traditionally used by local communities for generations. The knowledge about these natural products is deeply rooted in the local culture and is largely based on empirical practices and oral transmission (Saadi et al., 2013). Many of these plants have documented uses in ethnopharmacology, demonstrating a strong link between traditional knowledge and scientific findings. Therefore, the natural products identified in this study align with previous ethnopharmacological knowledge, highlighting the importance of preserving and further exploring these traditional practices (Barkaoui et al., 2022; Barkaoui et al., 2017).
In the other country, there is a large number of species used by pregnant women. To manage diseases related to pregnancy. For example, Asteraceae, Lamiaceae, and Solanaceae were dominant families in a study conducted in Uganda (Tugume et al., 2016; Tugume and Nyakoojo, 2019). This large use is due to the vast amount of bioactive compounds found in them (Thomas et al., 2009). Other results at Dessie Referral Hospital, Northeast Ethiopia showed that the medicinal herbs used during pregnancy were Zingiber officinale Roscoe, Allium sativum, Ocimum lamiifolium Hochst and Ruta chalepensis (Belayneh et al., 2022). Those examples are from two countries in Africa but they are different. In a systematic review conducted in sub-Saharan Africa, the top herbal medicines cited in the studies were Zingiber officinale Roscoe, Allium sativum L, Cucurbita pepo L., Ricinus communis L., Vernonia amygdalina debile and Garcinia kola heckel was the most common species for the treatment of pregnancy-induced nausea and vomiting and reported in 15 studies (El Hajj and Holst, 2020). While the frequently used herbs in most studies from the Euro-Mediterranean region are peppermint, (ginger) Zingiber officinale Roscoe, (thyme) Thymus maroccanus Ball, (chamomile) Matricaria chamomilla L., (sage) Salvia officinalis L., (anise) Pimpinella anisum L., (fenugreek) Trigonella foenum-graecum L., and (green tea) Camellia sinensis (John and Shantakumari, 2015).
The current findings revealed that herbal preparations are administered through a variety of routes. The oral route was the most common route of administration, followed by vaginal, nasal, and dermal routes. Similar findings are reported in other studies (Kamel et al., 2022; Al-Ramahi et al., 2013; Ali-Shtayeh et al., 2015; Raoufinejad et al., 2020). Oral administration often leads to the systemic absorption of active compounds, which can pose greater risks to the pregnancy due to the potential for higher bioavailability and systemic circulation, especially when the compounds cross the placenta. On the other hand, dermal administration typically results in local absorption, potentially limiting the systemic exposure and thus reducing the risk to the fetus. The absorption of active compounds through the skin is often lower, which may lead to a decreased likelihood of adverse effects compared to oral administration. However, the dermal route is not without risks, as certain compounds could still be absorbed into the bloodstream through the skin, albeit at lower levels (Sarecka-Hujar and Szulc-Musioł, 2025). Previous ethnopharmacological knowledge suggests that many traditional practices favor topical applications of herbal products, believing them to be safer for pregnant women. However, more research is required to further explore these differences in terms of both clinical safety and efficacy, particularly with regard to the specific herbs used during pregnancy. Therefore, a careful distinction must be made between the risks associated with oral and dermal herbal remedies, and their potential effects on maternal and fetal health should be considered accordingly (Ahmed et al., 2022).
Plant extracts were primarily prepared through decoction, infusion, maceration, Fumigation, extraction, and powder. The main solvent used in the preparation of herbal therapies was water and milk. This is consistent with other studies conducted in Morocco and elsewhere in the world (Kamel et al., 2022; Eid et al., 2020; Sadeghia and Mahmood, 2014; Ali-Shtayeh et al., 2015; Nergard et al., 2015).
Herbal medicine was used to treat diseases that are related to the period of pregnancy and delivery like digestive disorders, infections, anemia, and skin problems. Several illnesses were treated with a single plant species, while others were treated with a combination of plant parts from various species. Whereas other studies reported this use for stimulating labor or facilitating labor and delivery (Raoufinejad et al., 2020; Tabatabaee, 2011; Soleymani and Makvandi, 2018). Other uses were specifically to enhance neonates’ intelligence and to promote fetal health (Ekrasarian et al., 2017).
The quality and source of information received on herbal medicine influence automatically in the choice of treatment for maternal illnesses. In the research, the most frequent sources of referrals and information were family and friends. This finding is identical to other studies (Abdollahi and Yazdani Chareti, 2019; Al Essa et al., 2019; Kamel, 2013; and Quzmar et al., 2021). Other participants reported physicians as a source of information. Healthcare professionals were also mentioned as a source of information in the studies reviewed. In a Russia, physician recommendations were most often cited (Kennedy et al., 2016). In other places such as a Norwegian study, 80.7% of doctors rated their awareness of herbal medicine as poor (Thomas and Coleman, 2004). As a result, in order to effectively manage herbs during pregnancy, healthcare providers should update their knowledge of the effectiveness, potential hazards, side effects, herb-drug interactions, and fundamental ideas. They should also check their patients for the use of herbal medicine (Duraz and Khan, 2011). Only 11.2% of the participants were asked if they disclosed herbal medicine used to a medical doctor. The majority of the participants (78.1%) reported that they remark on the benefits of taking herbal medicine during pregnancy. In contrast, some of the participants (5.9%, 4.4%), respectively, observed special side effects and suspected a miscarriage from taking herbal medicine during pregnancy. The teratogenicity of herbal medications in animal models has to be studied further. Pregnant women should receive health education from prenatal care professionals who are knowledgeable about the data surrounding the possible advantages and hazards of herbal products.
Conclusion
The high utilization of herbal medicine among pregnant women in the Souss Massa region, as demonstrated in this study, underscores the importance of understanding its widespread use. The majority of participants considered herbal remedies safe during pregnancy, with nearly half perceiving them as more beneficial than conventional medical treatments. This finding highlights a significant area for further research, as it calls for a deeper investigation into both the potential benefits and risks of herbal medicines. This study contributes to expanding our knowledge of the role various plant species play in managing pregnancy-related health issues. However, to fully understand their therapeutic potential, further phytochemical and pharmacological studies are needed to identify their bioactive components. Additionally, to ensure the safe and effective use of these medicines, more research is required to establish standardized dosages and formulations. These efforts will provide clearer guidelines for the use of herbal medicines during pregnancy and help guide future medical research in this field.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by The biomedical research ethics committee of the Faculty of Medicine and Pharmacy in Rabat, Morocco. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AB: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review and editing. LL: Formal Analysis, Funding acquisition, Methodology, Software, Validation, Visualization, Writing – review and editing. FA: Investigation, Methodology, Software, Validation, Visualization, Writing – review and editing. SB: Methodology, Software, Validation, Writing – review and editing. MA: Formal Analysis, Investigation, Methodology, Validation, Visualization, Writing – review and editing. YK: Conceptualization, Project administration, Supervision, Validation, Visualization, Writing – review and editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We would like to sincerely thank Professor Abellah EL FAROUQI, Head of the Gynecology and Obstetrics Department, University hosiptal of Sous Massa for granting us the opportunity to conduct this study within his unit. We are also deeply grateful to the entire medical staff for their invaluable support, which greatly facilitated the data collection process. Our thanks go to all the pregnant women who agreed to participate and contributed to this study. We are especially thankful to the postpartum women for their enthusiastic involvement, despite the delicate period following childbirth. Their willingness to take part in the study is highly appreciated.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2025.1567930/full#supplementary-material
Abbreviations
CI, Confidence Interval; FC, Frequence of citation; RAMED, Medical Assistance Scheme (Régime d’Assistance Médicale); RFC, Relative frequency of citation; SD Standard of deviation; TAG, Triglyceride; WHO, World Health Organization.
References
1
Abd El-Mawla A. M. A. (2020). Prevalence and use of medicinal plants among pregnant women in assiut governorate. Bull. Pharm. Sci.43 (1), 73–78. 10.21608/BFSA.2020.93590
2
Abdollahi F. Khani S. Charati J. Abdollahi F. Khani S. Charati J. Y. (2018). Prevalence and related factors to herbal medicines use among pregnant females. Jundishapur J. Nat. Pharm. Prod.13 (3). 10.5812/jjnpp.13785
3
Abdollahi F. Yazdani Chareti J. (2019). The relationship between women’s characteristics and herbal medicines use during pregnancy. Women Health59 (6), 579–590. 10.1080/03630242.2017.1421285
4
Adams J. Lui C. W. Sibbritt D. Broom A. Wardle J. Homer C. et al (2009). Women's use of complementary and alternative medicine during pregnancy: a critical review of the literature. sept36 (3), 237–245. 10.1111/j.1523-536X.2009.00328.x
5
Ahmed M. Hwang J. H. Ali M. N. Al-Ahnoumy S. Han D. (2022). Irrational use of selected herbal medicines during pregnancy: a pharmacoepidemiological evidence from Yemen. Front. Pharmacol.13, 926449. 10.3389/fphar.2022.926449
6
Ahmed M. Hwang J. H. Choi S. Han D. (2017). Safety classification of herbal medicines used among pregnant women in Asian countries: a systematic review. BMC Complementary Altern. Med.17 (1), 489. 10.1186/s12906-017-1995-6
7
Al Essa M. Alissa A. Alanizi A. Bustami R. Almogbel F. Alzuwayed O. et al (2019). Pregnant women’s use and attitude toward herbal, vitamin, and mineral supplements in an academic tertiary care center, Riyadh, Saudi Arabia. Saudi Pharm. J.27 (1), 138–144. 10.1016/j.jsps.2018.09.007
8
Ali-Shtayeh M. S. Jamous R. M. Jamous R. M. (2015). Plants used during pregnancy, childbirth, postpartum and infant healthcare in Palestine. Complement. Ther. Clin. Pract.21 (2), 84–93. 10.1016/j.ctcp.2015.03.004
9
Aljofan M. Alkhamaiseh S. (2020). Prevalence and factors influencing use of herbal medicines during pregnancy in hail, Saudi Arabia a cross-sectional study. Sultan Qaboos Univ. Med. J.20 (1), e71–e76. 10.18295/squmj.2020.20.01.010
10
Al-Ramahi R. Jaradat N. Adawi D. (2013). Use of herbal medicines during pregnancy in a group of Palestinian women. J. Ethnopharmacol.150 (1), 79–84. 10.1016/j.jep.2013.07.041
11
Author Anonymous (2025a). The comprehensive R archive network. Available online at: https://cran.r-project.org/ (Accessed March 05, 2023).
12
Author anonymous (2025b). Faune and Flore. Available online at: https://siredd.environnement.gov.ma/Souss-Massa/BIODIVERSITEV2/index.html (Accessed March 25, 2022).
13
Barkaoui M. Katiri A. Boubaker H. Msanda F. (2017). Ethnobotanical survey of medicinal plants used in the traditional treatment of diabetes in Chtouka Ait Baha and Tiznit (Western Anti-Atlas), Morocco. J. Ethnopharmacol.198, 338–350. 10.1016/j.jep.2017.01.023
14
Barkaoui M. Msanda F. Boubaker H. Elasri O. El Boullani R. Benchelha H. et al (2022). Ethnobotany and diversity of medicinal and food plants used in the region Chtouka Ait Baha and Tiznit (western anti-atlas), Morocco. IOP Conf. Ser. Earth Environ. Sci.1090, 012021. 10.1088/1755-1315/1090/1/012021
15
Bartlett J. E. Kotrlik J. W. Higgins C. C. (2025). Organizational research: determining appropriate sample size in survey research.
16
Bayisa B. Tatiparthi R. Mulisa E. (2014). Use of herbal medicine among pregnant women on antenatal care at nekemte hospital, Western Ethiopia. Jundishapur J. Nat. Pharm. Prod.9 (4), e17368. 10.17795/jjnpp-17368
17
Belayneh Y. M. Yoseph T. Ahmed S. (2022). A cross-sectional study of herbal medicine use and contributing factors among pregnant women on antenatal care follow-up at Dessie Referral Hospital, Northeast Ethiopia. BMC Complementary Med. Ther.22 (1), 146. 10.1186/s12906-022-03628-8
18
Bruno L. O. Simoes R. S. de Jesus S. M. Girão MJBC Grundmann O. (2018). Pregnancy and herbal medicines: an unnecessary risk for women’s health—a narrative review. Phytotherapy Res.32 (5), 796–810. 10.1002/ptr.6020
19
Cochran (1977). Sampling techniques. Available online at: https://ia801409.us.archive.org/35/items/Cochran1977SamplingTechniques_201703/Cochran_1977_Sampling%20Techniques.pdf (Accessed March 05, 2023).
20
Dabirifard M. Maghsoudi Z. Dabirifard S. Salmani N. (2017). Frequency, causes and how to use medicinal herbs during pregnancy. Iran. J. Obstetrics, Gynecol. Infertil.20 (4), 66–75. 10.22038/IJOGI.2017.8984
21
Duraz A. Y. Khan S. A. (2011). Knowledge, attitudes and awareness of community pharmacists towards the use of herbal medicines in muscat region. Oman Med. J.26 (6), 451–453. 10.5001/omj.2011.115
22
Eid A. Jaradat N. Eid A. M. Jaradat N. (2020). Public knowledge, attitude, and practice on herbal remedies used during pregnancy and lactation in west bank Palestine. Front. Pharmacol.11, 46. 10.3389/fphar.2020.00046
23
Ekrasarian S. Rostami F. Charati J. Y. Abdollahi F. (2017). Use of medicinal plants during pregnancy in pregnant women in Sari, Iran. J. Mazandaran Univ. Med. Sci.26 (144), 341–345.
24
El-Ghazouani F. El-Ouahmani N. Teixidor-Toneu I. Yacoubi B. Zekhnini A. (2021). A survey of medicinal plants used in traditional medicine by women and herbalists from the city of Agadir, southwest of Morocco. Eur. J. Integr. Med.1 (42), 101284. 10.1016/j.eujim.2021.101284
25
El Hajj M. Holst L. (2020). Herbal medicine use during pregnancy: a review of the literature with a special focus on sub-saharan Africa. Front. Pharmacol.11, 866. 10.3389/fphar.2020.00866
26
Hall H. G. Griffiths D. L. McKenna L. G. (2011). The use of complementary and alternative medicine by pregnant women: a literature review. Midwifery. déc. 27 (6), 817–824. 10.1016/j.midw.2010.08.007
27
Jamovi (2025). Open statistical software for the desktop and cloud. Available online at: https://www.jamovi.org/.(Accessed March 05, 2023).
28
John L. J. Shantakumari N. (2015). Herbal medicines use during pregnancy: a review from the Middle East. Oman Med. J.30 (4), 229–236. 10.5001/omj.2015.48
29
Jouad H. Haloui M. Rhiouani H. El Hilaly J. Eddouks M. (2001). Ethnobotanical survey of medicinal plants used for the treatment of diabetes, cardiac and renal diseases in the North centre region of Morocco (Fez-Boulemane). J. Ethnopharmacol.77 (2-3), 175–182. 10.1016/s0378-8741(01)00289-6
30
Kamel H. H. (2013). Role of phyto-oestrogens in ovulation induction in women with polycystic ovarian syndrome. Eur. J. Obstetrics Gynecol. Reproductive Biol.168 (1), 60–63. 10.1016/j.ejogrb.2012.12.025
31
Kamel N. El Boullani R. Cherrah Y. (2022). Use of medicinal plants during pregnancy, childbirth and postpartum in southern Morocco. Healthcare10 (11), 2327. 10.3390/healthcare10112327
32
Kennedy D. A. Lupattelli A. Koren G. Nordeng H. (2016). Safety classification of herbal medicines used in pregnancy in a multinational study. BMC Complement. Altern. Med.16, 102. 10.1186/s12906-016-1079-z
33
La Situation Des Enfants Dans Le Monde (2009). Available online at: https://www.unicef.fr/sites/default/files/userfiles/ (Accessed November 30, 2022).
34
Mekuria A. B. Erku D. A. Gebresillassie B. M. Birru E. M. Tizazu B. Ahmedin A. (2017). Prevalence and associated factors of herbal medicine use among pregnant women on antenatal care follow-up at University of Gondar referral and teaching hospital, Ethiopia: a cross-sectional study. BMC Complementary Altern. Med.17 (1), 86. 10.1186/s12906-017-1608-4
35
Monographie régionale souss massa (2020). Haut-commissariat au Plan. Available online at: https://www.hcp.ma/region-agadir/docs/monographie%202020.pdf (Accessed December 26, 2022).
36
Nergard C. S. Ho T. P. T. Diallo D. Ballo N. Paulsen B. S. Nordeng H. (2015). Attitudes and use of medicinal plants during pregnancy among women at health care centers in three regions of Mali, West-Africa. J. Ethnobiol. Ethnomed11, 73. 10.1186/s13002-015-0057-8
37
Ouhaddou H. Boubaker H. Msanda F. Mousadik A. E. (2014). An ethnobotanical study of medicinal plants of the Agadir Ida Ou Tanane province (southwest Morocco). J. Appl. Biosci.84, 7707–7722. 10.4314/jab.v84i1.5
38
Pallivalappila A. R. Stewart D. Shetty A. Pande B. McLay J. S. (2013). Complementary and alternative medicines use during pregnancy: a systematic review of pregnant women and healthcare professional views and experiences. Evid. Based Complement. Altern. Med.2013, 205639. 10.1155/2013/205639
39
Pinn G. Pallett L. (2002). Herbal medicine in pregnancy. Complementary Ther. Nurs. Midwifery8 (2), 77–80. 10.1054/ctnm.2001.0620
40
Quzmar Y. Istiatieh Z. Nabulsi H. Zyoud S. H. Al-Jabi S. W. (2021). The use of complementary and alternative medicine during pregnancy: a cross-sectional study from Palestine. BMC Complementary Med. Ther.21 (1), 108. 10.1186/s12906-021-03280-8
41
Raoufinejad K. Gholami K. Javadi M. Rajabi M. Torkamandi H. Moeini A. et al (2020). A retrospective cohort study of herbal medicines use during pregnancy: prevalence, adverse reactions, and newborn outcomes. Traditional Integr. Med.5 (2), 70–85. 10.18502/tim.v5i2.3627
42
Saadi B. Msanda B. Boubaker H. (2013). Contributions of folk medicine knowledge in South-western Morocco: the case of rural communities of Immouzer Ida Outanane region. Int. J. Med. Plant Res.2, 135–145.
43
Sadeghia Z. Mahmood A. (2014). Ethno-gynecological knowledge of medicinal plants used by Baluch tribes, southeast of Baluchistan, Iran. Rev. Bras. Farmacogn.24 (6), 706–715. 10.1016/j.bjp.2014.11.006
44
Saper R. B. Kales S. N. Paquin J. Burns M. J. Eisenberg D. M. Davis R. B. et al (2004). Heavy metal content of ayurvedic herbal medicine products. JAMA.292 (23), 2868–2873. 10.1001/jama.292.23.2868
45
Sarecka-Hujar B. Szulc-Musioł B. (2025). Herbal medicines—are they effective and safe during pregnancy?Pharmaceutics14 (1), 171. 10.3390/pharmaceutics14010171
46
SIREDD (2025). SOUSS-MASSA. Available online at: https://siredd.environnement.gov.ma/Souss-Massa/Biodiversite (Accessed December 29, 2022).
47
Skerrett P. J. Harvard Health (2012). FDA needs stronger rules to ensure the safety of dietary supplements. Available online at: https://www.health.harvard.edu/blog/fda-needs-stronger-rules-to-ensure-the-safety-of-dietary-supplements-201202024182 (Accessed November 30, 2022).
48
Soleymani S. Makvandi S. (2018). Rate of herbal medicines use during pregnancy and some related factors in women of Ahvaz, Iran: 2017. Iran. J. Obstetrics, Gynecol. Infertil.21 (5), 80–86. 10.22038/IJOGI.2018.11388
49
Strouss L. Mackley A. Guillen U. Paul D. A. Locke R. (2014). Complementary and Alternative Medicine use in women during pregnancy: do their healthcare providers know?BMC Complement. Altern. Med.414, 85. 10.1186/1472-6882-14-85
50
Tabatabaee M. (2011). Use of herbal medicine among pregnant women referring to Valiasr Hospital in Kazeroon, Fars, South of Iran. J. Med. Plants10 (37), 96–108.
51
Tardío J. Pardo-de-Santayana M. (2025). Cultural importance indices: a comparative analysis based on the useful wild plants of southern cantabria (northern Spain)1. Econ bot. 62(1):24–39. 10.1007/s12231-007-9004-5
52
Thomas E. Vandebroek I. Sanca S. Van Damme P. (2009). Cultural significance of medicinal plant families and species among Quechua farmers in Apillapampa, Bolivia. J. Ethnopharmacol.122 (1), 60–67. 10.1016/j.jep.2008.11.021
53
Thomas K. Coleman P. (2004). Use of complementary or alternative medicine in a general population in Great Britain. Results from the National Omnibus survey. J. Public Health (Oxf). juin26 (2), 152–157. 10.1093/pubmed/fdh139
54
Tugume P. Kakudidi E. K. Buyinza M. Namaalwa J. Kamatenesi M. Mucunguzi P. et al (2016). Ethnobotanical survey of medicinal plant species used by communities around Mabira Central Forest Reserve, Uganda. J. Ethnobiol. Ethnomed12, 5. 10.1186/s13002-015-0077-4
55
Tugume P. Nyakoojo C. (2019). Ethno-pharmacological survey of herbal remedies used in the treatment of paediatric diseases in Buhunga parish, Rukungiri District, Uganda. BMC Complementary Altern. Med.19 (1), 353. 10.1186/s12906-019-2763-6
56
WMA (2025). The world medical association-WMA declaration of Helsinki – ethical principles for medical research involving human participants. Available online at: https://www.wma.net/policies-post/wma-declaration-of-helsinki/(Accessed March 25, 2025).
57
World Health Organization (2001). WHO_EDM_TRM_2001.2_eng.pdf. Dispon.Available online at: https://apps.who.int/iris/bitstream/handle/10665/42452/WHO_EDM_TRM_2001.2_eng.pdf?sequence=1&isAllowed=y (Accessed November 30, 2022).
58
World Health Organization (2002). Programme on Traditional Medicine. WHO traditional medicine strategy 2002-2005. World Health Organization. Available online at: https://iris.who.int/handle/10665/67163 (Accessed November 30, 2022).
59
World Health Organization (2007). Validation of neonatal tetanus elimination in Mali.pdf. Available online at: https://apps.who.int/iris/bitstream/handle/10665/43132/9242562904.pdf?sequence=1&isAllowed=y (Accessed November 30, 2022).
60
World Health Organization (2008). Mortalité maternelle en 2005 estimations de lαOM. Available online at: http://apps.who.int/iris/bitstream/handle/10665/43808/9789242596212_fre.pdf?sequence=1. (Accessed 30, November, 2022)
61
Yazdi N. Salehi A. Vojoud M. Sharifi M. H. Hoseinkhani A. (2019). Use of complementary and alternative medicine in pregnant women: a cross-sectional survey in the south of Iran. J. Integr. Med.17 (6), 392–395. 10.1016/j.joim.2019.09.003
Summary
Keywords
traditional medicine, herbal medicine, childbirth, pregnancy, ethnopharmacology, survey
Citation
Bouqoufi A, Lahlou L, Ait El Hadj F, Boujraf S, Abdessadek M and Khabbal Y (2025) An ethnopharmacological survey of herbal medicines use among pregnant and postpartum women in Souss Massa (Morocco). Front. Pharmacol. 16:1567930. doi: 10.3389/fphar.2025.1567930
Received
28 January 2025
Accepted
16 April 2025
Published
09 May 2025
Volume
16 - 2025
Edited by
Zhe Wang, China Pharmaceutical University, China
Reviewed by
Abad Khan, University of Swabi, Pakistan
Francesca Scotti, University College London, United Kingdom
Updates
Copyright
© 2025 Bouqoufi, Lahlou, Ait El Hadj, Boujraf, Abdessadek and Khabbal.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Youssef Khabbal, youssef.khabbal@uiz.ac.ma; Afaf Bouqoufi, a.bouqoufi@uiz.ac.ma
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.