- 1Department of Clinical Practice, Faculty of Pharmacy, Northern Border University, Rafha, Saudi Arabia
- 2Department of Pharmaceutical Care, King Fahad University Hospital, Imam Abdulrahman bin Faisal University, Al Khobar, Saudi Arabia
- 3Department of Pharmaceutical Care, Mouwasat Hospital, Qatif, Saudi Arabia
- 4Department of Pharmacy, Mohammed Al-Mana College for Medical Sciences, Dammam, Saudi Arabia
- 5Department of Pharmaceutical Care, RAM Clinics, Al Khobar, Saudi Arabia
- 6Department of Pharmaceutical Care, Mouwasat Hospital, Al Khobar, Saudi Arabia
- 7School of Medicine, Dar Al Uloom University, Riyadh, Saudi Arabia
- 8Department of Respiratory Therapy, Mohammed Al-Mana College for Medical Sciences, Dammam, Saudi Arabia
- 9Pharmacy Services Department, Johns Hopkins Aramco Healthcare (JHAH), Dhahran, Saudi Arabia
- 10Foundation Year Department, Mohammed Al-Mana College for Medical Sciences, Dammam, Saudi Arabia
- 11Department of Pharmacy Practice, College of Pharmacy, Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia
- 12Department of Pharmacology, College of Pharmacy, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia
Background: Calcium channel blockers, such as amlodipine, are commonly prescribed for hypertension but can cause peripheral edema, often requiring adjunctive frusemide. Concerns exist regarding the potential increase in fall risk, particularly in older populations. However, few studies have assessed the prevalence of amlodipine and frusemide combination (AFC) prescriptions and their association with fall risk factors.
Objectives: The aims of this study are to determine the prevalence of AFC prescriptions and evaluate their association with fall risk factors in an outpatient cardiology clinic population.
Methods: This retrospective, cross-sectional study included patients aged ≥40 years from Al-Qatif Central Hospital’s outpatient cardiology clinic (January 2021 -December 2022) prescribed amlodipine. Fall risk factors were identified from literature. The Charlson Comorbidity Index (CCI) was used to estimate 1-year mortality risk. The number of prescribed orthostatic hypotension-inducing drugs (OHDs) and fall-risk increasing drugs (FRIDs) was recorded. Binary logistic regression was performed to determine the association between AFC prescriptions and fall risk factors, adjusting for significant covariates. Results are expressed as adjusted odds ratios (OR) with 95% confidence intervals (CI).
Results: Of 3,681 patients, 18%. Were prescribed AFC. AFC patients were older (70 vs. 64 years, P < 0.001), had a higher prevalence of diabetes mellitus (64% vs. 44%, P < 0.001), anemia (55% vs. 32%, P < 0.001), and osteoporosis (51% vs. 28%, P < 0.001), and received more OHDs prescriptions (2.8 vs. 1.3, P < 0.001) compared to non-AFC patients. Higher CCI scores (OR = 1.51, 95% CI 1.41–1.62) and more OHDs prescriptions (OR = 2.5, 95% CI 2.3–2.7) were significantly associated with AFC prescriptions.
Conclusion: AFC prescriptions are prevalent, and patients prescribed AFC have higher prevalence of fall risk factors. Comprehensive patients assessment is essential to minimize fall risk and related complications.
1 Introduction
The phenomenon of prescribing cascades, where additional medications are prescribed to manage adverse drug effects, is a growing concern, particularly in poly-medicated older population (Kalisch et al., 2011; Rochon and Gurwitz, 2017). One such cascade involves the concurrent prescription of amlodipine, a calcium channel blocker for hypertension and angina, and frusemide, a loop diuretic for fluid retention and edema (Savage et al., 2020; Woodford, 2020; Shahid et al., 2024). While this combination is common, concerns about its safety have been raised, particularly regarding increased fall risk due to its effects on blood pressure regulation and orthostatic hypotension (Savage et al., 2020; Ndai et al., 2024).
Amlodipine is linked to dose-dependent peripheral edema, a common adverse effect that often prompts the addition of frusemide (Shahid et al., 2024). However, studies suggest that diuretics may not effectively mitigate calcium channel blockers-induced edema, leading to unnecessary medication use and exposing patients to additional adverse drug reactions, such as dehydration, electrolyte imbalance, and hypotension (van Hamersvelt et al., 1996).
Therefore, amlodipine and frusemide combination (AFC) serves as a key example of a prescribing cascade that may inadvertently increase the risk of falls, particularly among older patients. Fall risk is multifactorial, influenced by factors such as advanced age, polypharmacy, chronic comorbidities, and medications that affect hemodynamic stability (Liu et al., 1995; Gale et al., 2016; Juraschek et al., 2017; Rashedi et al., 2019; Amano et al., 2024). Falls among older populations represent a major public health concern, as they are a leading cause of morbidity, disability, and mortality (Liu et al., 1995; Milos et al., 2014). Orthostatic hypotension-inducing drugs (OHDs) and fall-risk increasing drugs (FRIDs) are frequently implicated in fall-related hospitalizations (Milos et al., 2014; Al-Qurain et al., 2020). Given that both amlodipine and frusemide have hypotensive effects, their concurrent use requires careful assessment of fall risk, particularly in patients with additional predisposing factors.
Despite concerns regarding the safety of AFC prescriptions, limited research has explored the prevalence of this combination and its association with known fall risk factors. Understanding these associations is crucial for optimizing prescribing practices and minimizing unnecessary medication exposure, especially among poly-medicated older patients (Alqurain et al., 2024a). This study aims to determine the prevalence of AFC prescriptions in an outpatient cardiology clinic, identify the prevalence of key fall risk factors, including polypharmacy, comorbidities, and medication-related risks, among AFC users, and evaluate the association between AFC prescriptions and the presence of fall risk factors. By addressing these objectives, this study provides essential data that may inform safer prescribing practices and enhance fall prevention strategies for patients receiving AFC prescriptions.
2 Materials and methods
2.1 Study design, study population, and ethical considerations
This study is a secondary analysis of data collected retrospectively from patients medical records. The cross-sectional design was selected because both the exposure and the associated risk factors were assessed concurrently at the time of the patient’s initial recorded visit during the study period. No follow-up or longitudinal data were collected to assess outcomes over time. Data for this study were collected as per the approval from the Institutional Review Board (IRB) at Mohammed Al-Mana College for Medical Sciences (SR/RP/79, Approval Date 17 February 2022) and the IRB at the Qatif Central Hospital (QCH-SRECO 19-2022, Approval Date 8 June 2022). Data were collected between 1st August 2022 and 20th February 2023 from the hospital information technology department. All participants were deidentified, and a waiver of consent collection was approved by the IRB as data were collected retrospectively.
The study included patients aged 40 years or older who attended an outpatient cardiology clinic and were prescribed amlodipine between the period of January 2021 and December 2022. The age of 40 years was chosen as the inclusion criteria, as aging influences the epidemiology of multiple morbidities, often requiring the prescription of multiple drugs to manage these comorbidities, thereby increasing the risk of drug-drug interactions and adverse drug reactions (Divo et al., 2014). Patients younger than 40 years old, those attending other medical care or surgical care clinics, an emergency department, admitted to the hospital wards or intensive care units, and those not prescribed amlodipine or who visited the hospital outside the study period, were excluded. For patients with multiple visits during the study period, only data from their first reported visit were included.
2.2 Data collection, measures and definitions
Patients’ demographic data, comorbidities and recent laboratory findings were retrieved from the electronic medical record, while the prescribed medications were verified from the pharmacy electronic records. Comorbidities were identified and coded as per the International Classification of Diseases, 10th revision, 2016 (ICD-10) (World Health Organisation, 2016). Fall risk factors were identified based on literature and included selected comorbidities and medication profiles. Due to incomplete documentation, prior falls were not included in the analysis. Comorbidities associated with an increased risk of falls, such as anemia, diabetes mellitus, and osteoporosis were identified and documented based on established literature (Rashedi et al., 2019; Amano et al., 2024). The Charlson Comorbidities Index (CCI) was calculated to predict 1-year mortality risk, and the creatinine clearance (CrCl) was estimated using the Cockcroft-Gault Equation (Cockcroft and Gault, 1976; Charlson et al., 1987). Due to the inability to fully discriminate specific morbidities, osteoarthritis and rheumatoid arthritis were grouped under “arthritis-related diseases”, whereas different types of pain in the lower and upper back, muscles, bones, joints, ligaments, and tendons were grouped under “musculoskeletal pain” (Alqurain et al., 2024b).
The medications data, including long-term regular prescriptions, short-term, as-needed prescriptions, and supplements were collected and coded as per the Anatomical Therapeutic Chemical (ATC) classification system. The total number of prescribed medications (NPM), the total number of OHDs and FRIDs were counted and documented (Milos et al., 2014; Al-Qurain et al., 2020). Notably, for statistical analysis, “OHDs” was adjusted by excluding amlodipine and frusemide from the final count to avoid repeating variables in the binary regression.
Several situations were identified where the AFC prescription may not be considered a prescriber cascade, such as congestive heart failure, chronic kidney disease, or end-stage renal disease (Yancy et al., 2017). Frusemide is prescribed in these clinical situations to maintain euvolemia in patients at risk of hypervolemia (Vouri et al., 2018). Therefore, in the current study, AFC was defined as the initiation or continuation of frusemide in the absence of congestive heart failure, chronic kidney disease, or end-stage renal disease.
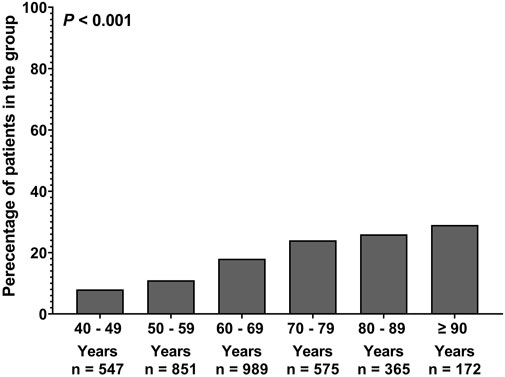
In the current study, two types of classification were used. In the first, patients were classified based on their age into two groups: middle-aged patients (<65 years) and older patients (≥65 years), to assess differences in prevalence pattern between these two cohorts. In the second, more detailed classification, patients were divided into six different groups (40–49, 50–59, 60–69, 70–79, 80–89, 90 years or older) to better examine trends in AFC prevalence across different age groups.
2.3 Statistical analysis
Demographic variables, comorbidities, and medication were summarized as follows: mean ± standard deviation (SD) for parametric continuous variables, median with interquartile range (IQR) for non-parametric continuous variables, and number with frequency (%) for binary variables. For comparisons of continuous variables, the Student’s T-test, and the Mann-Whitney U test were used for parametric and non-parametric data, respectively. The Chi-square test was used to compare the frequency of categorical variables between groups. Trends in AFC across different age groups were assessed using analysis of variance (ANOVA) test. Binary logistic regression was performed to compute unadjusted and adjusted odds ratios (OR) with 95% confidence interval (95% CI) to examine the association between the factors contributing to increased fall risk and AFC prescription within the cohort. The binary logistic regression was adjusted for covariates that either reached statistical significance at (P < 0.05) in univariate analysis or had clinically relevant to fall risk, as recommended by previous studies (Ranganathan et al., 2017). Multicollinearity was assessed using the variance inflation factor. Statistical analysis was performed using the SPSS statistical software package, version 23, and a P ≤ 0.05 was considered statistically significant.
3 Results
This study included 3,681 patients, with a prevalence of AFC prescription of 18%. Female patients were more frequent prescribed AFC compared to male patients (54% vs. 46%, p = 0.02) (Table 1). Patients prescribed AFC were older (70 vs. 64 years, p < 0.001), had a higher body weight (79 kg vs. 77 kg, p = 0.01), a lower average CrCl value (87 mL/min vs. 92 mL/min, p = 0.009) and a higher median CCI score (7 vs. 5, p < 0.001) compared to those not prescribed AFC. Interestingly, patients prescribed AFC were also more frequently prescribed OHDs and FRIDs compared to those not prescribed AFC (2.8 vs. 1.3, p < 0.001 and 0.7 vs. 0.5, p < 0.001 respectively) (Table 1). As shown in Table 1, patients prescribed AFC had a significantly higher prevalence of diabetes mellitus (65% vs. 44%, p < 0.001), anemia (55% vs. 32%, p < 0.001), musculoskeletal pain (65% vs. 57%, p = 0.001) and osteoporosis (51% vs. 38%, p < 0.001) compared to those not prescribed AFC. Table 1 shows that patients with AFC prescription had higher prevalence of hypertension (91% vs. 64%, p < 0.001), ischemic heart diseases (100% vs. 61%, p < 0.001) and arrhythmia (8% vs. 1%, p < 0.001) compared to those not prescribed AFC.
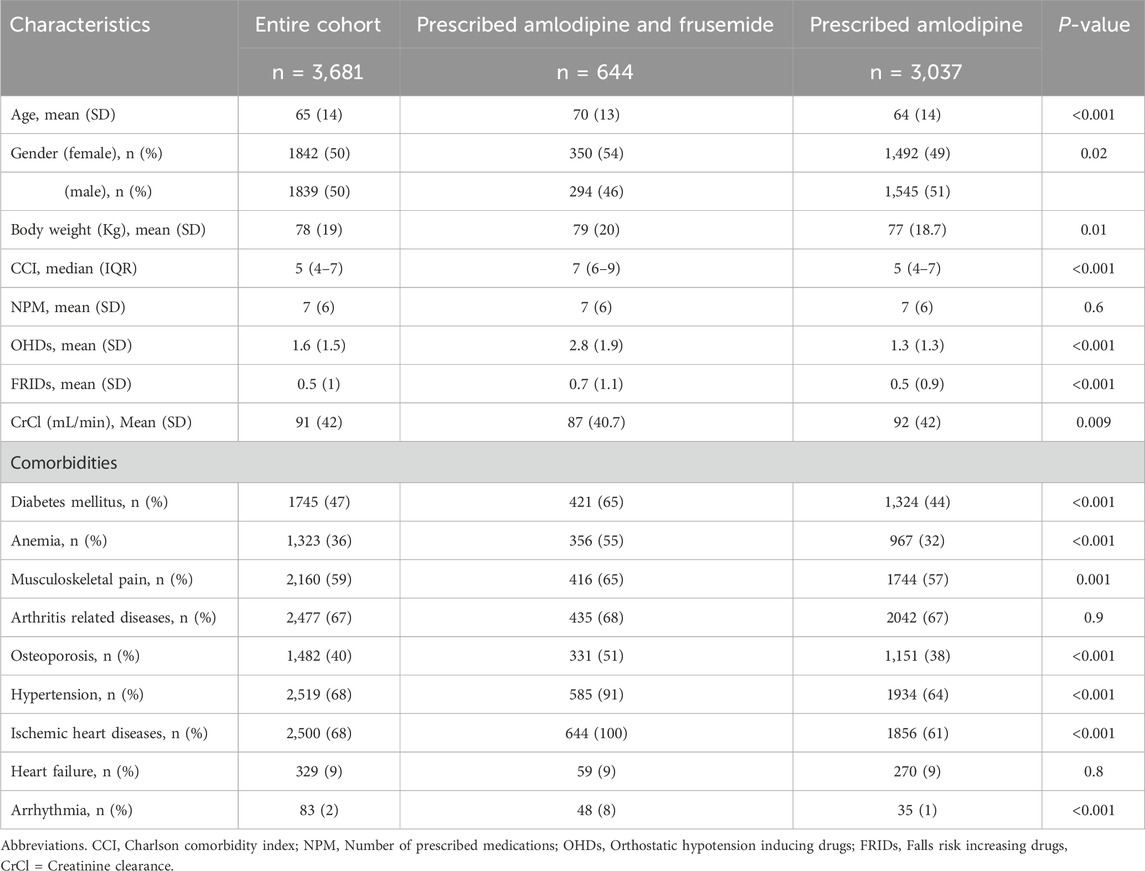
Table 1. Characteristics of the patients included in the study classified based on amlodipine and frusemide combination prescription.
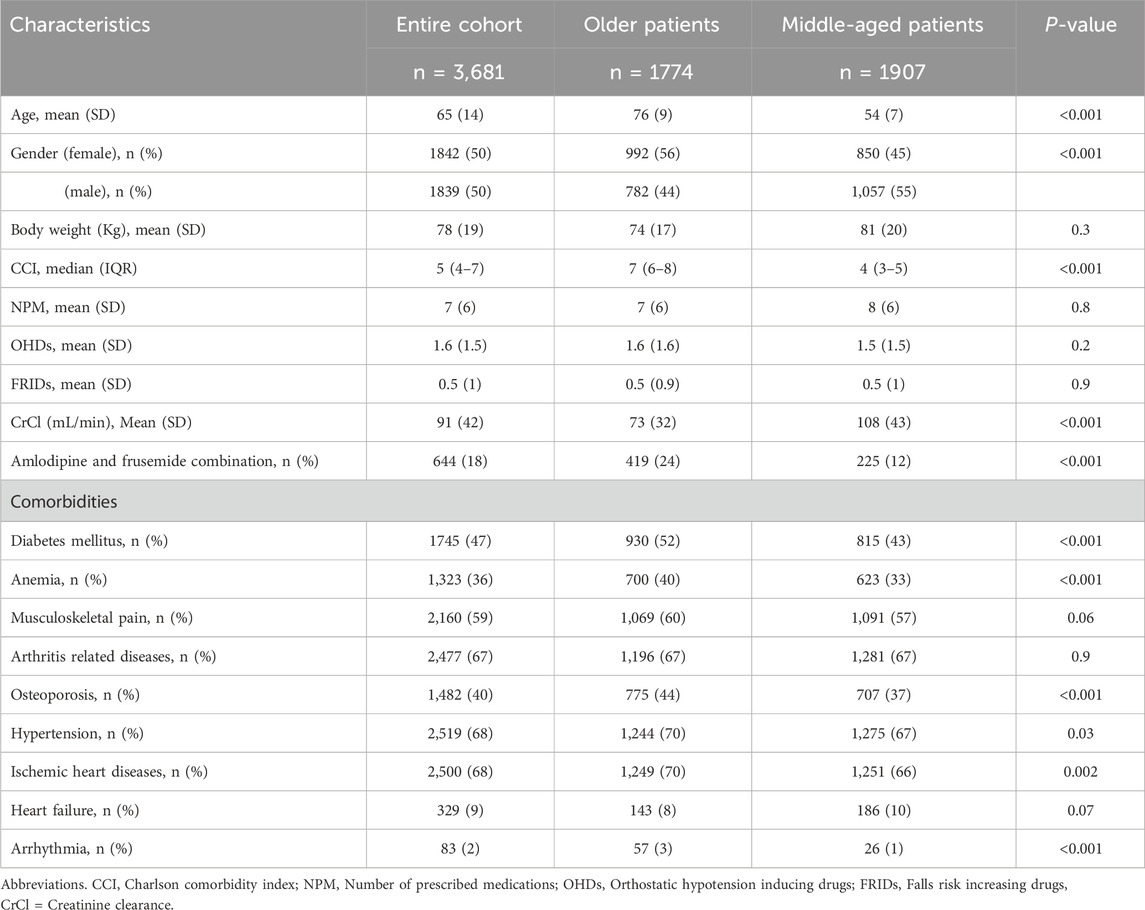
Another analysis was conducted to determine the pattern of AFC occurrence across different age groups. Figure 1 illustrates a progressive increase in AFC occurrence with advancing age. Further analysis was conducted to assess the different characteristics between older vs. middle-aged patients. The analysis revealed that older patients were more likely to be female individuals (56% vs. 45%, p < 0.001), had a higher CCI score (7 vs. 4, p < 0.001) and had a lower CrCl value (73 vs. 108, p < 0.001) (Table 2). In addition, older patients presented with a higher prevalence of diabetes mellitus (52% vs. 43%, p < 0.001), anaemia (40% vs. 33%, p < 0.001), osteoporosis (44% vs. 37%, p < 0.001), hypertension (70% vs. 67%, p = 0.03), ischemic heart diseases (70% vs. 76%, p = 0.002), and arrhythmia (3% vs. 1%, p < 0.001) (Table 2). Interestingly, Table 2 shows that older patients were prescribed AFC more often compared to middle-aged patients (24% vs. 12%, p < 0.001).
After adjusting for confounding covariates including age, body weight, sex, CCI, CrCl, OHDs and FRIDs, logistic regression analysis demonstrated that AFC prescription was positively associated with increasing body weight (OR = 1.02, 95% CI 1.01–1.024), higher CCI score (OR = 1.5, 95% CI 1.4–1.6), and greater OHDs prescription (OR = 2.5, 95% 2.3–2.7), while it was negatively associated with increasing FRIDs prescription (OR = 0.8, 95% CI 0.7–0.9) (Table 3).
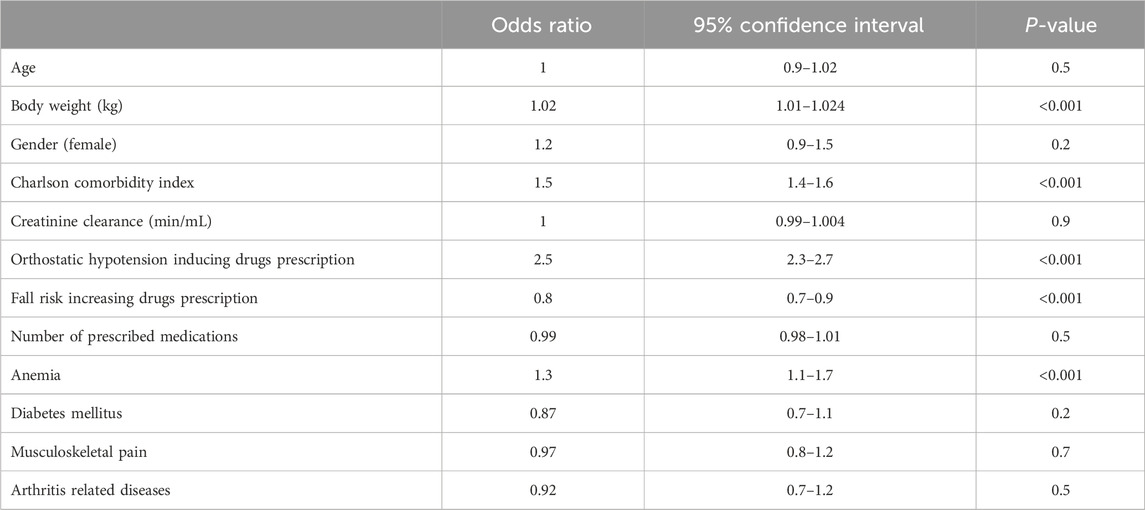
Table 3. Association between patients’ characteristics and the occurrence of amlodipine and frusemide combination among the cohort.
4 Discussion
This study highlights significant associations between the prescription of AFC and factors contributing to an increased risk of falls. The findings demonstrate that AFC prescriptions were prevalent among older adults and were strongly associated with higher CCI score, the use of OHDs prescriptions, and the presence of anaemia. Considering these associations, healthcare providers must carefully evaluate the appropriateness of AFC use in older patients, ensuring that the therapeutic benefits outweigh the potential risks while minimizing adverse drug reactions.
A key finding from this study is that 18% of the included cohort were prescribed AFC, a notably higher proportion compared to previously reported values. A study from the United States reported that 5%–12% of the cohort were exposed to and continued using AFC, whereas another study reported that about 3.5% of older patients with hypertension were prescribed AFC during their first year of therapy (Vouri et al., 2018; Ndai et al., 2024). The high prevalence reported in the current study highlights the importance of early detection of this combination to mitigate the risk of falls associated with orthostatic hypotension.
Another key finding is the significant association between increasing CCI scores and AFC occurrence. A higher CCI score reflects a greater burden of chronic illness, which inherently increases the risk of falls (Charlson et al., 1987; Milos et al., 2014; Rashedi et al., 2019). Additionally, due to the retrospective design of the current study, the CCI index was used as an alternative measure of frailty (Al-Qurain et al., 2021). Frail older patients exhibit a higher rate of falls, including recurrent falls compared to non-frail (Wong et al., 2015; Cheng and Chang, 2017). Recent studies have further demonstrated that frailty is associated with an increased risk of orthostatic hypotension and falls in older patients (Kocyigit et al., 2019; Shaw et al., 2019).
Another significant observation is the association between the prescription of OHDs and the occurrence of AFC. This finding is particularly relevant given that a recent study highlighted that OHDs prescriptions, including antihypertensives, increase the likelihood of polypharmacy by 20% among older patients (Alqurain et al., 2024a). Polypharmacy is a well-established risk factor for falls due to the increased potential for drug-drug interactions and adverse drug reactions (Alqurain et al., 2024a). Considering this association, routine medication reviews should prioritize minimizing unnecessary OHDs use, while maintaining optimal cardiovascular management (Scott et al., 2015; Zhou et al., 2017). Collaboration between pharmacists and healthcare providers is essential to evaluate whether alternative treatment strategies can be employed to reduce fall risk while achieving therapeutic goals.
Another important finding from the current study is the inverse association observed between FRIDs prescriptions and AFC use (OR = 0.8, 95% CI 0.7–0.9). This may reflect clinician-driven deprescribing behaviours, as prescribers intentionally avoid or reduce FRIDs use in patients already exposed to falls risk increasing drugs. This explanation is supported by previous study finding as prescribers often reduce or deprescribe medications potentiating risk of falls among vulnerable patients presented with polypharmacy and frailty (Reeve et al., 2014). Similarly, a clinical review reported that similar interventions are linked to reduced fall risk via medication review and deprescribing strategies (Van Poelgeest et al., 2021).
Furthermore, the study identified a high prevalence of diabetes mellitus, anaemia, and osteoporosis among AFC users, conditions that collectively increase the risk of falls. Diabetes mellitus contributes to fall risk through peripheral neuropathy and hypoglycaemia-related dizziness, while anaemia exacerbates fatigue and muscle weakness due to impaired oxygen delivery. (Stauder and Thein, 2014; Zhou et al., 2017; Rashedi et al., 2019; Amano et al., 2024). Osteoporosis further increases susceptibility to severe injuries following a fall, increasing morbidity and mortality risk (Avdic et al., 2004; Wang et al., 2021). The combination of AFC prescriptions and these comorbid conditions emphasizes the need for targeted fall prevention strategies, including regular screening for anaemia, careful monitoring of glucose levels, and interventions aimed at enhancing bone health in high-risk individuals.
Older patients are at an increased risk of lower extremity edema and prescribing amlodipine may further exacerbate this risk, potentially leading to the concurrent use of frusemide (Vouri et al., 2018; Ndai et al., 2024). Notably, this study identified a higher prevalence of AFC prescription among older patients. Advanced age is also associated with the presence of multiple morbidities, which often necessitate the use of multiple drugs, leading to polypharmacy (Al-Qurain et al., 2020). Therefore, healthcare providers should consider conducting comprehensive medication reviews to assess the risk of adverse drug reactions associated with AFC prescription among older patients, ensuring the effective management of hypertension while minimizing adverse drug reactions and drug-drug interactions (Al-Qurain et al., 2021).
Another finding from the current study is that age, gender, and body weight were significantly higher in the AFC group. This finding aligns with previously published studies where these characteristics were linked to increased risk of falls and falls related injuries among older population (Wei and Hester, 2014; Waters et al., 2019; Minhee et al., 2023). However, the regression model did not identify significant association between these characteristics and AFC prescribing. Instead, these variables were included in the multivariable regression model to control for their confounding effect. The associations observed between AFC prescribing and high CCI scores and OHD use suggest an independent link, supporting the need for caution in AFC prescribing irrespective of baseline demographic differences.
In the current study, patients with CHF, CKD, and ESRD were excluded from the definition of AFC to reduce misclassification because the retrospective design precludes confirmation of prescribing intent. Therefore, we cannot definitively confirm whether frusemide was added to manage amlodipine-induced oedema. To address this, a sensitivity analysis excluding patients with liver cirrhosis, a potential alternative indication for diuretics, was conducted and the results were consistent with the early findings. However, prospective studies are needed to accurately establish causality and sequence of prescribing decisions.
This study has several notable strengths. The current study is the first of its kind to report on the prevalence of AFC prescriptions and evaluate factors contributing to increased fall risk among patients attending a cardiology clinic in the Eastern Region of Saudi Arabia. Specifically, amlodipine and frusemide are common medications prescribed for older populations and their use can be defined as prescriber cascade in some cases which is an important medication related problem especially in the geriatric medicine. Additionally, the study benefits from a large sample size, providing robust statistical power to detect associations between AFC prescription and the identified risk factors. The comprehensive analysis, incorporating binary linear regression, allows for a more thorough assessment of the factors contributing to increased fall risk associated with AFC prescription. Furthermore, the study explores differences in AFC prescription patterns between middle-aged and older patients, which could help develop strategies for detecting the phenomenon and mitigating fall risk in different patient groups.
However, several limitations should be acknowledged. As retrospective cross-sectional study, it was difficult to accurately identify the phenomenon of prescribing cascade owing to the inability to determine the exact initiation date of the prescribed medications. To address this, the study investigated the concurrent prescription of amlodipine and frusemide as an indicator for the occurrence of this phenomenon (Vouri et al., 2018; Savage et al., 2020). Another limitation is the lack of information regarding the duration of AFC prescription. Due to the retrospective design and the nature of electronic health records used in this study, we were unable to determine whether the prescriptions were chronic or short-term. As such, the AFC exposure was assessed only as a binary variable, and the impact of duration on fall risk could not be evaluated. In addition, the cross-sectional design limited the ability to assess the appropriateness of medications and to interpret adverse drug reactions more broadly. Another limitation is the absence of body mass index data due to incomplete height documentation in the medical records, which precluded the assessment of obesity status. While body weight was included in the analysis, it may not fully capture obesity-related risk. Frailty was not directly measured in this study due to the retrospective nature of data collection. While CCI was used as a proxy indicator of frailty-related burden (Charlson et al., 1987), we recognize that it is primarily a mortality risk tool and not a validated frailty assessment instrument, but was used to estimate frailty status based on the patients’ current disease states. Future prospective studies should incorporate structured frailty tools for more accurate risk stratification. The Lack of follow-up data further limited the understanding of longer-term treatment outcomes, including efficacy, adverse drug reactions, and readmission rates. Lastly, due to its cross-sectional in nature, this study did not allow for an examination of the trajectory of AFC prescription over time or their associations with changes in hypertension and fall incidence trajectories.
Based on our results, interventions should be implemented to increase healthcare providers’ awareness of the potential fall risk associated with AFC prescriptions. Such interventions could include educational programs, clinical guidelines, or decision-support tools to equip healthcare professionals with the necessary knowledge to identify and prevent unnecessary prescribing cascades in these patients.
The phenomenon of prescribing cascade has gained attention within geriatric medicine as a significant contributor to the global challenge of polypharmacy (Brath et al., 2018). Therefore, early detection and assessment of AFC prescription are a crucial component of comprehensive care for these patients (Scott et al., 2015). It is recommended that patients at risk of falls associated with AFC prescription be closely monitored to ensure appropriate management of blood pressure and prevention of adverse drug reactions.
5 Conclusion
AFC prescriptions remain an ongoing concern, with 18% of the cohort being prescribed this combination. Older age, diabetes mellitus and anemia were more common among patients prescribed AFC. AFC prescriptions were associated with OHDs prescriptions and increasing CCI score. This study highlights the importance of comprehensive patient assessment to minimize fall risk and related complications among patients prescribed AFC.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The Institutional Review Board (IRB) at Mohammed Al-Mana College for Medical Sciences (SR/RP/79, Approval Date 17 February 2022) and the Qatif Central Hospital’s IRB (QCH-SRECO 19-2022, Approval Date 8 June 2022). The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because retrospective nature of the study.
Author contributions
AyA: Writing – original draft, Data curation, Conceptualization, Writing – review and editing, Methodology, Formal Analysis, Project administration, Supervision, Validation, Visualization. MrA: Methodology, Writing – original draft, Conceptualization, Data curation, Writing – review and editing, Formal Analysis, Investigation. SA: Software, Writing – review and editing, Writing – original draft, Data curation, Conceptualization, Methodology, Resources. MhA: Formal Analysis, Data curation, Validation, Writing – review and editing, Writing – original draft, Software. RzA: Writing – review and editing, Data curation, Validation, Formal Analysis, Investigation, Writing – original draft. RwA: Writing – review and editing, Data curation, Methodology, Validation. RnA: Writing – review and editing, Validation, Data curation, Methodology, Visualization. AlA: Writing – review and editing, Data curation, Validation. MsA: Data curation, Validation, Writing – review and editing. SA-S: Writing – review and editing, Data curation, Validation. LA: Writing – review and editing, Data curation, Validation. SG: Writing – review and editing. MwA: Writing – review and editing, Validation, Data curation. NA: Validation, Writing – review and editing, Data curation. AfA: Data curation, Writing – review and editing, Validation. FA: Writing – review and editing, Validation, Data curation.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The authors sincerely thank the Research Development and Innovation Authority (RDIA) for their ongoing support, as this work received partial funding from RDIA, grant (ID: 12990-iau-2023-iau-R-3-1-HW).
Acknowledgments
The authors also extend their gratitude to the medical records and information technology staff at QCH for their invaluable support in reviewing and collecting patient data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2025.1598161/full#supplementary-material
References
Alqurain, A., Alomar, F. A., Albaharnah, M. H., Alzayer, S. H., Ameer, L., Ghosn, S. A., et al. (2024a). The prevalence of polypharmacy and hyper-polypharmacy among middle-aged vs older patients in Saudi Arabia: a cross-sectional study. Front. Pharmacol. 15, 1357171. doi:10.3389/fphar.2024.1357171
Alqurain, A. A., Alomar, M. F., Fakhreddin, S., Julayh, Z., Korikeesh, Z., Al-Shaibi, S., et al. (2024b). Pattern of prescribing proton pump inhibitors: evaluating appropriateness and factors contributing to their adverse effect reaction risk. J. Clin. Med. 13, 6187. doi:10.3390/jcm13206187
Al-Qurain, A. A., Gebremichael, L. G., Khan, M. S., Williams, D. B., Mackenzie, L., Phillips, C., et al. (2020). Prevalence and factors associated with analgesic prescribing in poly-medicated elderly patients. Drugs Aging 37, 291–300. doi:10.1007/s40266-019-00742-0
Al-Qurain, A. A., Gebremichael, L. G., Khan, M. S., Williams, D. B., Mackenzie, L., Phillips, C., et al. (2021). Opioid prescribing and risk of drug-opioid interactions in older discharged patients with polypharmacy in Australia. Int. J. Clin. Pharm. 43, 365–374. doi:10.1007/s11096-020-01191-1
Amano, S., Ohta, R., and Sano, C. (2024). Relationship between anemia and readmission among older patients in rural community hospitals: a retrospective cohort study. J. Clin. Med. 13, 539. doi:10.3390/jcm13020539
Avdic, D., Pecar, D., and Mujic-Skikic, E. (2004). Risk factors of fall in elderly people. Bosn. J. Basic Med. Sci. 4, 71–78. doi:10.17305/bjbms.2004.3366
Brath, H., Mehta, N., Savage, R. D., Gill, S. S., Wu, W., Bronskill, S. E., et al. (2018). What is known about preventing, detecting, and reversing prescribing cascades: a scoping review. J. Am. geriatrics Soc. 66, 2079–2085. doi:10.1111/jgs.15543
Charlson, M. E., Pompei, P., Ales, K. L., and Mackenzie, C. R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chronic Dis. 40, 373–383. doi:10.1016/0021-9681(87)90171-8
Cheng, M. H., and Chang, S. F. (2017). Frailty as a risk factor for falls among community dwelling people: evidence from a meta-analysis. J. Nurs. Scholarsh. 49, 529–536. doi:10.1111/jnu.12322
Cockcroft, D. W., and Gault, M. H. (1976). Prediction of creatinine clearance from serum creatinine. Nephron 16, 31–41. doi:10.1159/000180580
Divo, M. J., Martinez, C. H., and Mannino, D. M. (2014). Ageing and the epidemiology of multimorbidity. Eur. Respir. J. 44, 1055–1068. doi:10.1183/09031936.00059814
Gale, C. R., Cooper, C., and Aihie Sayer, A. (2016). Prevalence and risk factors for falls in older men and women: the English longitudinal study of ageing. Age Ageing 45, 789–794. doi:10.1093/ageing/afw129
Juraschek, S. P., Daya, N., Appel, L. J., Miller Iii, E. R., Windham, B. G., Pompeii, L., et al. (2017). Orthostatic hypotension in middle-age and risk of falls. Am. J. Hypertens. 30, 188–195. doi:10.1093/ajh/hpw108
Kalisch, L. M., Caughey, G. E., Roughead, E. E., and Gilbert, A. L. (2011). The prescribing Cascade. Aust. Prescr. 34, 162–166. doi:10.18773/austprescr.2011.084
Kocyigit, S. E., Soysal, P., Bulut, E. A., Aydin, A. E., Dokuzlar, O., and Isik, A. T. (2019). What is the relationship between frailty and orthostatic hypotension in older adults? J. geriatric Cardiol. JGC 16, 272–279. doi:10.11909/j.issn.1671-5411.2019.03.005
Liu, B. A., Topper, A. K., Reeves, R. A., Gryfe, C., and Maki, B. E. (1995). Falls among older people: relationship to medication use and orthostatic hypotension. J. Am. Geriatrics Soc. 43, 1141–1145. doi:10.1111/j.1532-5415.1995.tb07016.x
Milos, V., Bondesson, A., Magnusson, M., Jakobsson, U., Westerlund, T., and Midlov, P. (2014). Fall risk-increasing drugs and falls: a cross-sectional study among elderly patients in primary care. BMC Geriatr. 14, 40. doi:10.1186/1471-2318-14-40
Minhee, S., Kim, D. H., Insook, C., and Ham, O. K. (2023). Age and gender differences in fall-related factors affecting community-dwelling older adults. J. Nurs. Res. 31, e270. doi:10.1097/jnr.0000000000000545
Ndai, A. M., Morris, E. J., Winterstein, A. G., and Vouri, S. M. (2024). Evaluating provider and pharmacy discordance in potential calcium channel blocker-loop diuretic prescribing Cascade. Drugs Aging 41, 177–186. doi:10.1007/s40266-023-01091-9
Ranganathan, P., Pramesh, C., and Aggarwal, R. (2017). Common pitfalls in statistical analysis: logistic regression. Perspect. Clin. Res. 8, 148–151. doi:10.4103/picr.PICR_87_17
Rashedi, V., Iranpour, A., Mohseni, M., and Borhaninejad, V. (2019). Risk factors for fall in elderly with diabetes mellitus type 2. Diabetes Metab. Syndr. 13, 2347–2351. doi:10.1016/j.dsx.2019.06.001
Reeve, E., Shakib, S., Hendrix, I., Roberts, M. S., and Wiese, M. D. (2014). The benefits and harms of deprescribing. Med. J. Aust. 201, 386–389. doi:10.5694/mja13.00200
Rochon, P. A., and Gurwitz, J. H. (2017). The prescribing Cascade revisited. Lancet 389, 1778–1780. doi:10.1016/S0140-6736(17)31188-1
Savage, R. D., Visentin, J. D., Bronskill, S. E., Wang, X., Gruneir, A., Giannakeas, V., et al. (2020). Evaluation of a common prescribing Cascade of calcium channel blockers and diuretics in older adults with hypertension. JAMA Intern. Med. 180, 643–651. doi:10.1001/jamainternmed.2019.7087
Scott, I. A., Hilmer, S. N., Reeve, E., Potter, K., Le Couteur, D., Rigby, D., et al. (2015). Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern. Med. 175, 827–834. doi:10.1001/jamainternmed.2015.0324
Shahid, F., Doherty, A., Wallace, E., Schmiedl, S., Alexander, G. C., and Dreischulte, T. (2024). Prescribing cascades in ambulatory care: a structured synthesis of evidence. Pharmacotherapy 44, 87–96. doi:10.1002/phar.2880
Shaw, B. H., Borrel, D., Sabbaghan, K., Kum, C., Yang, Y., Robinovitch, S. N., et al. (2019). Relationships between orthostatic hypotension, frailty, falling and mortality in elderly care home residents. BMC Geriatr. 19, 80–14. doi:10.1186/s12877-019-1082-6
Stauder, R., and Thein, S. L. J. (2014). Anemia in the elderly: clinical implications and new therapeutic concepts. Haematologica 99, 1127–1130. doi:10.3324/haematol.2014.109967
Van Hamersvelt, H. W., Kloke, H. J., De Jong, D. J., Koene, R. A., and Huysmans, F. T. M. (1996). Oedema formation with the vasodilators nifedipine and diazoxide: direct local effect or sodium retention? J. Hypertens. 14, 1041–1046. doi:10.1097/00004872-199608000-00016
Van Poelgeest, E., Pronk, A., Rhebergen, D., and Van Der Velde, N. (2021). Depression, antidepressants and fall risk: therapeutic Dilemmas—A clinical review. Eur. Geriatr. Med. 12, 585–596. doi:10.1007/s41999-021-00475-7
Vouri, S. M., Van Tuyl, J. S., Olsen, M. A., Xian, H., and Schootman, M. (2018). An evaluation of a potential calcium channel blocker-lower-extremity edema-loop diuretic prescribing Cascade. J. Am. Pharm. Assoc. (2003) 58, 534–539. doi:10.1016/j.japh.2018.06.014
Wang, L., Yu, W., Yin, X., Cui, L., Tang, S., Jiang, N., et al. (2021). Prevalence of osteoporosis and fracture in China: the China osteoporosis prevalence study. JAMA Netw. Open 4, e2121106. doi:10.1001/jamanetworkopen.2021.21106
Waters, D. L., Qualls, C., Cesari, M., Rolland, Y., Vlietstra, L., and Vellas, B. (2019). Relationship of incident falls with balance deficits and body composition in Male and female community-dwelling elders. J. Nutr. health and aging 23, 9–13. doi:10.1007/s12603-018-1087-4
Wei, F., and Hester, A. L. (2014). Gender difference in falls among adults treated in emergency departments and outpatient clinics. J. gerontology and geriatric Res. 3, 152. doi:10.4172/2167-7182.1000152
Wong, T. H., Nguyen, H. V., Chiu, M. T., Chow, K. Y., Ong, M. E. H., Lim, G. H., et al. (2015). The low fall as a surrogate marker of frailty predicts long-term mortality in older trauma patients. PLoS One 10, e0137127. doi:10.1371/journal.pone.0137127
Woodford, H. J. J. (2020). Calcium channel blockers co-prescribed with loop diuretics: a potential marker of poor prescribing? Drugs Aging 37, 77–81. doi:10.1007/s40266-019-00730-4
World health organisation (2016). International statistical classification of disease and related health problems 10th revision (ICD-10)-WHO version for 2016. Geneva: World Health Organization.
Yancy, C. W., Jessup, M., Bozkurt, B., Butler, J., Casey, J. , D. E., Colvin, M. M., et al. (2017). 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American college of cardiology/american heart association task force on clinical practice guidelines and the heart failure society of America. Circulation 136, e137–e161. doi:10.1161/CIR.0000000000000509
Keywords: amlodipine, frusemide, prescribing cascade, fall risk, orthostatic hypotension
Citation: Alqurain A, Albaharnah M, Al Zayer S, Alanzi M, Alblushi R, Aleid R, Ashoor R, Albahrani A, Almahdi M, Al-Shaibi S, Ameer L, Ghosn S, Algoraini M, Alsubaie N, Alshnbari A and Alomar FA (2025) Amlodipine and frusemide: pharmacological factors contributing to increased fall risk in concurrently treated patients – a retrospective cross-sectional study. Front. Pharmacol. 16:1598161. doi: 10.3389/fphar.2025.1598161
Received: 22 March 2025; Accepted: 07 July 2025;
Published: 28 July 2025.
Edited by:
Mohammed Salahudeen, University of Tasmania, AustraliaReviewed by:
Santenna Chenchula, All India Institute of Medical Sciences, IndiaNoha Ahmed, Damanhour University, Egypt
Copyright © 2025 Alqurain, Albaharnah, Al Zayer, Alanzi, Alblushi, Aleid, Ashoor, Albahrani, Almahdi, Al-Shaibi, Ameer, Ghosn, Algoraini, Alsubaie, Alshnbari and Alomar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aymen Alqurain, YXltZW4uYWxxdXJhaW5AbmJ1LmVkdS5zYQ==; Fadhel A. Alomar, ZmFsbW9hckBpYXUuZWR1LnNh
†ORCID: Fadhel A. Alomar, orcid.org/0000-0003-0788-6919; Aymen Alqurain, orcid.org/0000-0002-4284-0265
 Aymen Alqurain
Aymen Alqurain Murtada Albaharnah
Murtada Albaharnah Samanah Al Zayer3
Samanah Al Zayer3 Sherihan Ghosn
Sherihan Ghosn Nawal Alsubaie
Nawal Alsubaie Fadhel A. Alomar
Fadhel A. Alomar