- 1Jaseng Spine and Joint Research Institute, Jaseng Medical Foundation, Seoul, Republic of Korea
- 2Department of Preventive Medicine, College of Korean Medicine, Kyung Hee University, Seoul, Republic of Korea
- 3Department of Neurosurgery, Hallym University College of Medicine, Chuncheon, Republic of Korea
- 4Kyung Hee University Medical Center, Department of Cardiology and Neurology, College of Korean Medicine, Kyung Hee University, Seoul, Republic of Korea
Background: Stroke survivors often take multiple medications (polypharmacy), raising concerns about falls and mortality in older adults. This study investigated whether Korean Medicine (KM)—primarily acupuncture—is associated with fall risk and mortality among older adults with stroke and polypharmacy.
Methods: A population-based retrospective cohort study using South Korea’s National Health Insurance Service (NHIS) claims database. Adults aged 65 or older with a first stroke in 2015 were included if they had five or more prescribed medications (polypharmacy) or ten or more (hyper-polypharmacy) for at least 270 days. KM users received acupuncture or electroacupuncture (≥3 outpatient visits or ≥1 inpatient stay) within a year of stroke onset. The primary outcome was falls resulting in fracture; the secondary outcome was all-cause mortality—both assessed over 3 years. Propensity score matching balanced demographics, comorbidities, and medication use. Cox proportional hazards and subgroup analyses were conducted. Subgroup and sensitivity analyses explored effect modification.
Results: Among 25,034 older stroke patients, 10,011 had polypharmacy; of those, 6,809 used KM. After matching, 3,127 KM users were compared with 3,127 non-users. KM users with polypharmacy had a higher rate of falls but lower all-cause mortality than non-users. In hyper-polypharmacy, KM use did not significantly affect falls but was associated with lower mortality. Sensitivity analyses of the unmatched cohort, alternative outcome definitions, and interactions yielded consistent patterns.
Conclusion: In older adults with stroke and polypharmacy, KM may improve functional recovery and mobility, potentially increasing falls if balance training is inadequate, yet simultaneously confer survival advantages—perhaps through neuro-immune or systemic effects—irrespective of medication load. Among the more frail hyper-polypharmacy group, KM reduced mortality without altering falls, suggesting that functional gains and competing-risk dynamics differ by medication intensity. Prospective studies with granular functional measures, drug–drug interaction data, and formal competing-risk models are needed to optimize the safe integration of KM into comprehensive stroke care.
1 Introduction
Polypharmacy—taking more medications than clinically necessary—usually refers to the use of five or more drugs (Kim et al., 2014; Masnoon et al., 2017). With population aging and the rising prevalence of multiple chronic conditions, polypharmacy has become a growing global concern, with about half of those aged 65 and older taking five or more medications (Wastesson et al., 2018). In South Korea, 86.4% of older adults take six or more medications, and 44.9% are in a state of excessive polypharmacy by taking 21 or more medications (Kim et al., 2014). Older adults with polypharmacy face a heightened risk of adverse events, including cognitive impairment, falls, and mortality (Gnjidic et al., 2012; Kojima et al., 2012b). Potentially inappropriate medications often contribute to this problem by negatively affecting cognitive function and elevating the likelihood of neurodegenerative diseases (Park et al., 2017a; Park et al., 2017b).
Stroke survivors are particularly vulnerable to polypharmacy. As stroke commonly co-occurs with hypertension, diabetes, dyslipidemia, and heart disease, many patients take multiple drugs to address both risk factors and symptoms (Kose et al., 2017). A Scottish study reported that patients with stroke were more than twice as likely to have multimorbidity than those without stroke, with 12.6% taking 11 or more medications, compared with only 1.5% of the general population (Gallacher et al., 2014). Indeed, patients with stroke on more than five or six medications face an elevated risk of adverse events and falls (Kojima et al., 2012a; Kojima et al., 2012b). Given the physical disabilities and reduced quality of life often associated with stroke, polypharmacy can further complicate recovery and create additional barriers to rehabilitation.
Korean Medicine (KM), a branch of Traditional East Asian Medicine (TEAM), has a long history alongside Chinese and Kampo medicine (Lee et al., 2014). In recent years, TEAM approaches have been investigated for their potential to reduce polypharmacy. One retrospective study of 159 patients reported a significant drop in the total number of medications used after treatment with TEAM in those who showed symptomatic improvement (Takano et al., 2018). Another case report documented a reduction from 13 to two medications alongside clinical improvement (Nogami et al., 2019). These findings suggest that by addressing the symptoms that originally led to multiple prescriptions, TEAM—including KM—may lessen the medication burden. However, prior investigations have focused mainly on drug count reduction rather than exploring the broader impact on falls and mortality.
We utilize data from the National Health Insurance Service (NHIS) to examine whether insurance-covered KM treatments, namely acupuncture, can influence polypharmacy-related outcomes in older patients with stroke. Specifically, we compare fall and mortality rates among those with and without polypharmacy and KM usage. By clarifying KM’s potential role in mitigating the risks associated with multiple medications, we aim to inform more integrative approaches to managing the complex care needs of older stroke survivors.
2 Methods
2.1 Data source
We utilized the health claims database maintained by the NHIS in South Korea, which includes data for 97.0% of the population (Sun-Min Kim, 2020). The remaining 3.0% of the population is covered by Medical Aid (Kim et al., 2020). Mortality data were obtained from Statistics Korea. The database, along with related materials and metadata, is publicly accessible on the National Health Insurance Data Sharing Service website (Cheol Seong et al., 2017). Access to the database is granted following a review by the NHIS inquiry committee for research purposes. The Institutional Review Board of Kyung Hee University provided a formal waiver for consent [KHSIRB-20-361(EA)].
2.2 Study cohort
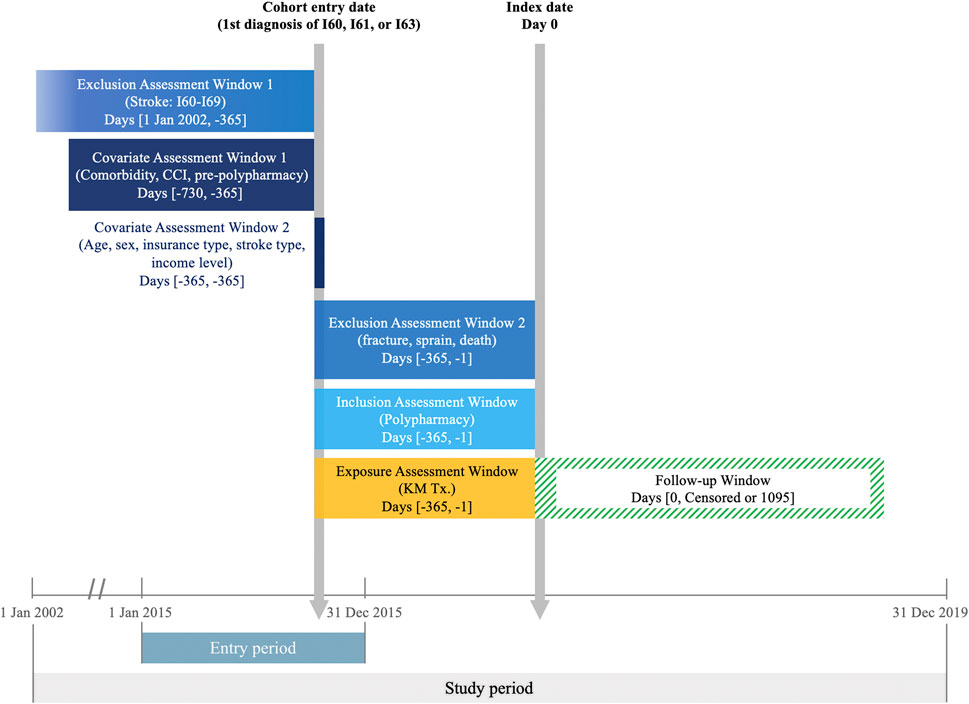
Using NHIS claims data, we identified patients diagnosed with cerebral hemorrhage (I60, subarachnoid hemorrhage; I61, intracerebral hemorrhage) or cerebral infarction (I63, cerebral infarction) between January 1 and 31 December 2015, according to the International Classification of Diseases 10th revision. The cohort was restricted to individuals aged 65 and above. Exclusion criteria included patients without a record of hospitalization for at least 1 day and those with a history of any type of stroke (I60–I69) since 2002, the earliest data available from the NHIS. The cohort entry date was determined by the first recorded stroke diagnosis in 2015 (Figure 1).
2.3 Polypharmacy
Polypharmacy was defined as the use of five or more medications from a predefined list (Supplementary Table S1) for 270 days or more within the 1-year period following stroke onset (Masnoon et al., 2017; Onoue et al., 2018; Sirois et al., 2019; Chang et al., 2020; Beezer et al., 2021). This particular study was referenced because it utilized the same database (Chang et al., 2020). The use of 10 or more medications from the list of medications for 270 days or more during the same exposure window was defined as hyper-polypharmacy. The list of medications was developed through expert consultations and included 227 drugs commonly prescribed to patients with stroke. These drugs fall into various categories, including cardiovascular agents, anti-Parkinson and anti-dementia agents, psycholeptics and hypnotics (Supplementary Table S1).
2.4 Intervention
The intervention of interest was acupuncture and/or electroacupuncture, as documented in NHIS reimbursement records. Patients were considered to have received acupuncture if they had at least three reimbursement records for treatment sessions at a KM outpatient clinic or at least one hospitalization record for treatment at KM hospitals within 1 year of the initial stroke diagnosis.
2.5 Outcome and covariates
The primary outcome was the occurrence of various types of fractures within 3 years from the index date. Falls were identified using specific International Classification of Diseases 10th revision (ICD-10) codes: M483–M485, M80, M843, S020–S021, S22–S23, S32–S33, and S72–S73 (Supplementary Table S2). The secondary outcome was all-cause mortality within 3 years from the index date. Patients who experienced falls or died before the index date were excluded from the analysis, as only outcome events occurring after the index date were considered. All patients were followed for 3 years post-index date.
Covariates included baseline demographic factors such as age, sex, and economic status, with economic status determined by annual premiums paid for National Health Insurance in 2015. Predefined comorbid conditions recorded within 1 year prior to the cohort entry date included diabetes mellitus, cancers, chronic back pain, osteoarthritis, rheumatoid arthritis, osteoporosis, chronic obstructive pulmonary disease, dementia, schizophrenia, depressive and anxiety disorders, hyperlipidemia, hypertension, cardiovascular diseases, renal failure, and chronic liver diseases. The Charlson Comorbidity Index (CCI) was also calculated during this period (Supplementary Table S3).
2.6 Statistical analysis
Descriptive statistics were utilized to examine the baseline characteristics. Standardized mean differences were calculated for each variable, with an absolute value of ≥0.2 indicating significant imbalances (McCaffrey et al., 2013). Incidence rate ratio (IRR) was calculated for the cohort prior to propensity score matching. A propensity score (PS) representing the probability of receiving KM treatment was calculated using sex, age group, income, types of stroke, pre-stroke polypharmacy, and CCI as classification variables. One-to-one matching was conducted using the greedy nearest neighbor method, with a caliper of 0.1, ensuring exact matches for the abovementioned variables.
Primary analysis focused on assessing the relationship between post-stroke KM treatment and the risk of falls and all-cause mortality among patients with stroke and polypharmacy, using Cox proportional hazards models. A subgroup analysis was conducted for patients with hyper-polypharmacy (10 or more medications). Four prespecified sensitivity analyses were conducted. First, prespecified comorbid conditions were included as a covariate. Second, the number of medications was included as a covariate. Third, the risk of falls and all-cause mortality was estimated for patients with stroke without polypharmacy, or non-polypharmacy (fewer than 5 medications). Fourth, the interaction between KM utilization and medication counts was analyzed. A two-sided p-value of <0.05 was considered statistically significant. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC).
3 Results
3.1 Patient characteristics of polypharmacy cohort
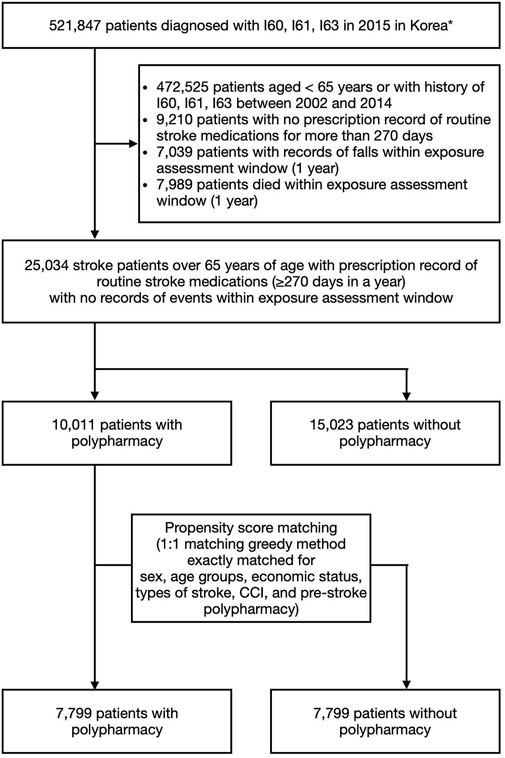
The study cohort included 25,034 patients (Figure 2), with 10,011 in the polypharmacy group and 15,023 in the non-polypharmacy group. Within the polypharmacy and non-polypharmacy groups, 6,809 patients (68%) and 10,506 patients (70%), respectively, utilized KM within 1 year following stroke onset. Baseline characteristics revealed that the majority of KM users, regardless of polypharmacy status, were aged 70–79. Additionally, a greater proportion of patients with higher CCI scores, indicative of more severe cases, were among KM users. The distribution of KM use was consistent across various stroke subtypes, including hemorrhagic and ischemic strokes. Patients with pre-existing conditions such as chronic back pain and osteoarthritis also exhibited higher KM use (Table 1).
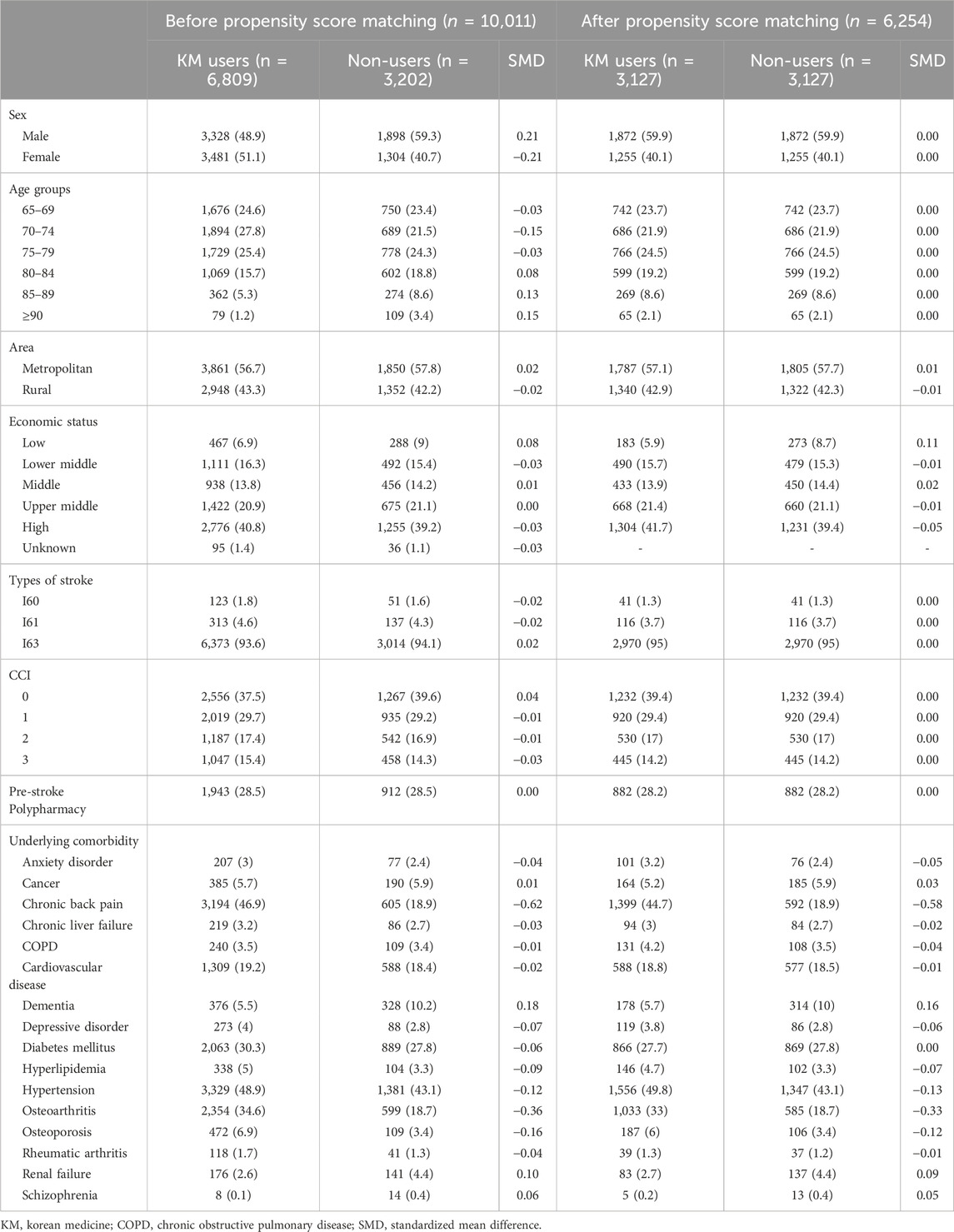
Table 1. Baseline characteristics of Korean medicine treatment users and non-users among patients with stroke and polypharmacy.
The PS matching process within the polypharmacy group successfully balanced the covariates, with no significant differences between KM users (n = 3,127) and non-users (n = 3,127). However, disparities in the prevalence of chronic back pain and osteoarthritis persisted. Similarly, in the hyper-polypharmacy group, PS matching resulted in balanced covariates between KM users (n = 160) and non-users (n = 160), although differences in the incidence of chronic back pain remained.
3.2 Relationship of all-cause falls and mortality with KM use among patients with polypharmacy
Among patients in the polypharmacy group, those utilizing KM exhibited a higher risk of falls from all causes, with an adjusted hazard ratio (aHR) of 1.52 (95% confidence interval [CI] 1.325–1.751). Conversely, the all-cause mortality rate was lower in KM users compared with non-users, with an aHR of 0.66 (95% CI 0.59–0.74). These trends of increased falls and decreased mortality remained consistent across all univariate and multivariate models (Table 2).
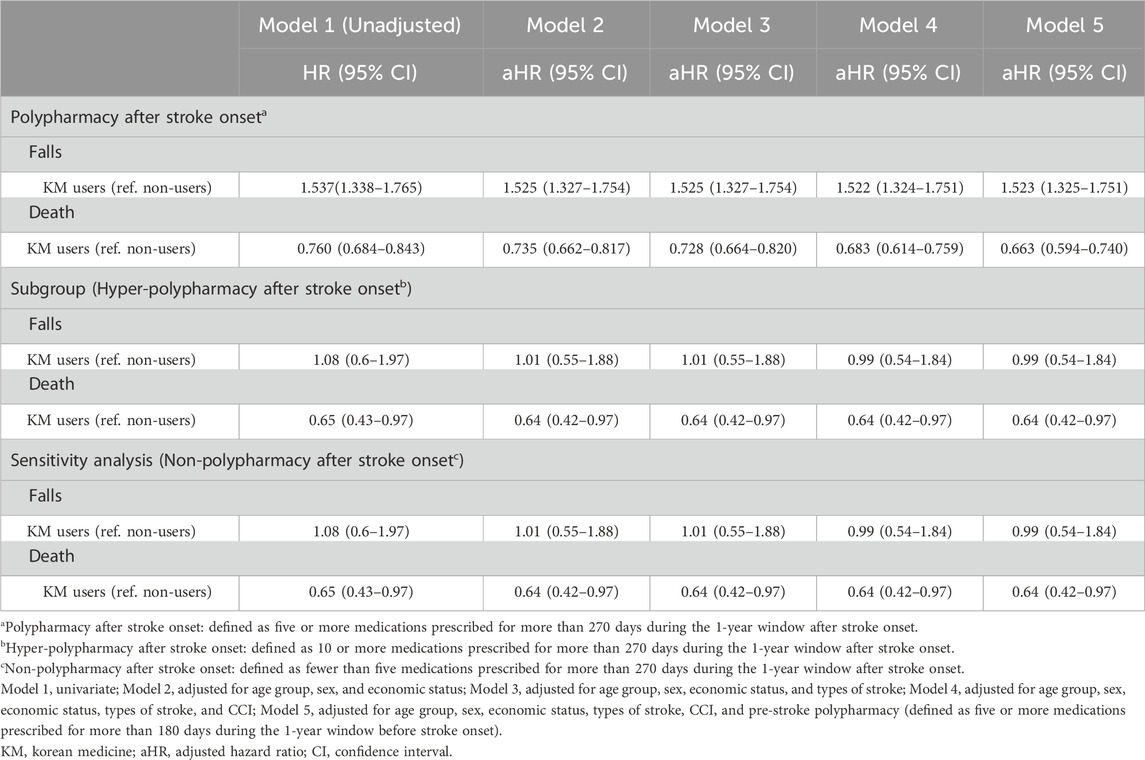
Table 2. Risk of falls and deaths from all causes in polypharmacy, hyper-polypharmacy, and non-polypharmacy groups.
3.3 Patient characteristics of the hyper-polypharmacy cohort
Compared with the PS-matched polypharmacy cohort, which showed an even distribution across age groups, the hyper-polypharmacy group had a higher concentration of patients aged 70–79 and an underrepresentation of those above 85. The hyper-polypharmacy group also had higher CCI scores, with 67.5% reporting pre-stroke polypharmacy, compared with only 28.2% in the general polypharmacy group. This group exhibited an overall increase in most prespecified comorbidities, including anxiety disorder, cancer, chronic liver failure, chronic obstructive pulmonary disease, cardiovascular disease, dementia, depressive disorder, diabetes mellitus, hyperlipidemia, rheumatoid arthritis, renal failure, and schizophrenia. In contrast, KM users in the hyper-polypharmacy group showed a decreased prevalence of chronic back pain, hypertension, osteoarthritis, and osteoporosis (Supplementary Table S4).
3.4 Relationship of all-cause falls and mortality with KM use among patients with hyper-polypharmacy
In the hyper-polypharmacy group, the risk of falls from all causes was not significantly different between KM users and non-users (aHR 0.99, 95% CI 0.54–1.84). However, KM users had a lower all-cause mortality rate (aHR 0.64, 95% CI 0.42–0.97). These findings of no significant difference in falls and a decreased mortality risk were consistent across all univariate and multivariate models (Table 2).
3.5 Sensitivity analyses
No notable differences in the risk of falls and deaths from all causes were observed in the subgroup and sensitivity analyses. For the PS-matched non-polypharmacy group (Supplementary Table S5), the risk of falls was not statistically different between KM users and non-users (aHR 0.99, 95% CI 0.54–1.84). On the contrary, the decreased mortality with KM use remained significant (aHR 0.64, 95% CI 0.42–0.97, Table 2).
When prespecified comorbidities were included as covariates (Supplementary Table S6), the trends of increased falls (aHR 1.45, 95% CI 1.25–1.69) and decreased mortality (aHR 0.72, 95% CI 0.65–0.81) in the polypharmacy group due to KM use were robust. In the PS-matched hyper-polypharmacy subgroup, fall risk remained unaffected by the inclusion of prespecified comorbidities as covariates (aHR 1.11, 95% CI 0.56–2.19). Similarly, the reduced all-cause mortality in KM users remained insignificant when prespecified comorbidities were considered (aHR 0.73, 95% CI 0.47–1.14). In the PS-matched non-polypharmacy group, fall risk increased by the inclusion of prespecified comorbidities (aHR 1.22, 95% CI 0.74–1.39). The reduced all-cause mortality remained insignificant (aHR 0.79, 95% CI 0.72–0.88).
When medication counts were included as covariates (Supplementary Table S7), the trends of increased falls (aHR 1.45, 95% CI 1.25–1.69) and decreased mortality (aHR 0.72, 95% CI 0.67–0.77) in the polypharmacy group owing to KM use were consistent. In the PS-matched hyper-polypharmacy subgroup, fall risk remained unaffected by the inclusion of medication counts as covariates (aHR 1.12, 95% CI 0.56–2.24). Similarly, the reduced all-cause mortality in KM users remained insignificant when medication counts were considered (aHR 0.72, 95% CI 0.46–1.14). In the PS-matched non-polypharmacy group, fall risk increased by the inclusion of medication counts (aHR 1.23, 95% CI 1.08–1.40). The reduced all-cause mortality remained insignificant (aHR 0.77, 95% CI 0.70–0.85).
The potential interaction between KM use and medication counts (Supplementary Table S8) for fall risk was not statistically significant (p = 0.844), indicating that the effect of KM on the hazard of falls does not significantly vary with the number of medications. The hazard ratios for KM use showed consistent results for falls up to 10 medications, with a nonsignificant trend for 10 or more medications. Similarly, the interaction between KM use and medication counts for all-cause mortality was not significant (p = 0.526). This suggests that the effect of KM on the risk of death does not significantly differ based on medication counts, with a consistent decrease in mortality risk for KM users compared with non-users across various levels of medication counts.
Lastly, incidence-rate ratios derived from the unmatched cohort paralleled those observed after propensity matching (Supplementary Table S9), supporting the robustness of the primary findings. We then used the same crude event counts to bound the influence of mortality as a competing risk for falls. Under a maximal-overlap scenario—every patient who fractured eventually died within the follow-up window—deaths still represented 16% of all first events. Under a no-overlap scenario—no faller died during follow-up—deaths rose to 54% of first events. Because even the most conservative bound exceeds the commonly cited 15% threshold at which cause-specific and Fine–Gray estimates begin to diverge, competing mortality is likely to meaningfully affect fracture estimates. A person-time–based calculation yielded a concordant result: assuming constant hazards, the probability that death occurs before a first fracture was approximately 52%. These figures confirm that mortality is a substantial competing event and may partly underlie the higher observed fall rates in KM users.
4 Discussion
We investigated how KM usage—primarily acupuncture—affects falls and mortality among older stroke survivors with varying degrees of polypharmacy. Using the NHIS database, we analyzed 25,034 patients who experienced a stroke, categorized them into polypharmacy (≥5 medications) or hyper-polypharmacy (≥10 medications) groups, and examined two outcomes over 3 years: all-cause mortality and falls resulting in fractures. PS matching was used to minimize baseline differences between KM users and non-users, balancing factors such as demographics, comorbidities, and stroke severity. We then applied Cox proportional hazards models to assess how KM influenced our outcomes, performing sensitivity checks to confirm the robustness of the results.
In the polypharmacy group, KM use was associated with a heightened risk of falls (aHR 1.52) but a reduced risk of all-cause mortality (aHR 0.66) compared with non-use. This seemingly paradoxical pattern of higher fall incidence yet lower all-cause mortality among KM users can be reconciled by mechanisms well documented in stroke-rehabilitation research, even though functional status could not be measured directly in the NHIS data. Multiple studies including randomized controlled trials show that post-stroke acupuncture, combined with targeted physical training and herbal prescriptions, accelerate gains in motor strength, gait speed, and activities of daily living, and shorten the modified Rankin Scale recovery (Liu et al., 2009; Yan and Hui-Chan, 2009; Zhao et al., 2009; Hong et al., 2024; Hu et al., 2024). Improved mobility enlarges patients’ “activity envelope”; because most post-stroke falls occur during routine ambulation rather than high-risk tasks (Wang et al., 2025; Morone et al., 2014), increased activity envelope predictably yields into more opportunities to fall. At the same time, enhanced locomotion curtails secondary complications such as pneumonia, pressure ulcers, sarcopenia and facilitates cardiovascular conditioning, which together have been linked to better long-term survival (Lui and Nguyen, 2018), which inadvertently raises fall risk if patients do not receive adequate balance training (Morone et al., 2014; Wei et al., 2019).
In contrast, among those with hyper-polypharmacy, KM did not significantly change fall risk (aHR 0.99) but still lowered all-cause mortality (aHR 0.64). As patients with severe polypharmacy often have more advanced multimorbidity and frailty, KM’s positive impact on mobility might be less pronounced in that group, explaining the nonsignificant difference in falls. These findings were consistent across various models and sensitivity analyses, indicating a robust protective effect of KM on mortality regardless of medication burden. The absence of significant interaction effects between KM use and medication counts for both falls and mortality suggests that the benefits of KM, particularly in reducing mortality, are broadly applicable across medication complexity levels.
Although the primary KM intervention was acupuncture, another major therapy is herbal medicine. Owing to gaps in insurance coverage, herbal medicine use is not fully captured in the NHIS claims data. However, nationwide survey data indicate that a substantial portion of KM users also utilize herbal remedies: 94.3% use acupuncture, 28.5% use herbal extracts, and 26.7% use herbal decoctions (Development, 2024). This widespread use likely means most herbal medicine users were included in our KM cohort. By analyzing how an insured medical services provided within the scope of KM interacts with extensive Western polypharmacy, our study tackles a genuinely ethnopharmacological question: can a traditional, system-based medical paradigm mitigate drug-burden complications in real-world stroke care? Herbal medicine has been reported to alleviate neurologic deficits (Yang et al., 2016; Yu et al., 2015; Han et al., 2018) and improve independence (Goto et al., 2011). By enhancing motor function and mobility, herbal therapies could further increase the risk of falls—walking is the most common activity preceding falls in stroke survivors (Weerdesteyn et al., 2008)—but also contribute to better overall recovery. Although the NHIS database does not allow itemization of separate herbs and herbal decoctions, their silent presence implies the integrated KM practice provided to the treatment group actually seen in clinics in real-world settings.
Well-documented herbal effects that we could not model quantitatively nevertheless remain clinically relevant for post-stroke patients. The reduction in mortality may be attributed to KM’s ability to improve various factors that can worsen prognosis in the post-stroke recovery period in addition to functional recovery, such as acupuncture improving post-stroke dysphagia (Long and Wu, 2012; Cohen et al., 2016), herbal medicines inhibiting the progression of acute cerebral infarction (Jung et al., 2003), preventing aspiration pneumonia (Iwasaki et al., 2007), promoting negative conversion of resistant bacteria (Kohno et al., 2021), reducing early neurological deterioration (Tian et al., 2021), and preventing recurrence (Lee et al., 2023; Jung et al., 2018). Collectively these mechanisms—neuroprotection, infection control, and secondary prevention—could explain the lower all-cause mortality we observed among KM users. In patients with severe multimorbidity, however, KM’s impact on mobility could be blunted (Yao et al., 2020) owing to increased medications (Muth and Glasziou, 2015), potentially explaining why fall risk was unchanged in the hyper-polypharmacy group. Even though individual herbal prescriptions were unmeasurable, the aforementioned literature shows that they plausibly augment the neuromuscular and systemic benefits of acupuncture while also carrying their own risk-benefit trade-offs. Recognizing those unseen contributions strengthens the biological coherence of our findings and highlights why future linked-dataset or prospective studies that capture uninsured herbal dispensing are essential for a full pharmacological accounting of KM in stroke rehabilitation.
While the neuromotor benefits of acupuncture and other KM modalities are well documented, the higher fall rate observed in KM recipients is more plausibly driven by survivor bias than by treatment-related harm. Our competing-risk sensitivity analysis showed that deaths accounted for 16%–54% of all first events and that, assuming constant hazards, the probability of death preceding a first fracture was ≈52%. Because KM users experienced lower early mortality, they contributed more person-time at risk and therefore had more opportunity to incur a fall. When this prolonged exposure is combined with the greater mobility that KM appears to foster, the crude fall incidence is inevitably inflated without implying an intrinsic increase in fall propensity. Accordingly, the excess falls should be viewed not as an adverse effect of KM itself but as the by-product of improved survival and functional recovery. Future studies with patient-level event ordering and richer clinical detail are needed to apply formal competing-risk methods—such as Fine–Gray sub-distribution models—and to verify this interpretation.
In the matched cohort, KM users had a higher prevalence of chronic pain conditions such as low back pain and osteoarthritis, suggesting that individuals with persistent pain may be more inclined to seek KM owing to its perceived or actual effectiveness. Acupuncture can alleviate chronic pain and encourage greater activity (Vickers et al., 2018), potentially improving quality of life (Manyanga et al., 2014; Seca et al., 2019). The resulting improvement in pain control and quality of life may encourage increased activity, contributing to fall risk but also enhancing overall health. This increased activity, however, can raise fall risk if patients resume normal routines without proper balance training or physical conditioning (Skelton, 2023). Nonetheless, better pain management may also slow the progression of other chronic conditions, potentially contributing to improved survival (Nielsen et al., 2022). While these benefits do not inherently lower fall risk, they highlight acupuncture’s broader role in chronic disease management, which can enhance patients’ overall longevity despite an accompanying increase in activity-related hazards.
Our study offers a fresh perspective on managing polypharmacy in older stroke survivors. Established criteria (Beers (Panel, 2015), STOPP/START (O'Mahony et al., 2023)) aim to reduce inappropriate prescribing but have shown mixed results in preventing adverse events (Frankenthal et al., 2014; Cole et al., 2023). In South Korea, where prescribing practices differ from Western settings (Lee et al., 2022), KM could serve as an integrative approach, potentially mitigating some negative outcomes of polypharmacy without reducing medication counts directly. We could not confirm whether KM helps discontinue medications, as we focused only on whether participants were in a polypharmacy state. Nevertheless, our findings strongly suggest that KM use is associated with improved survival regardless of medication load.
This study has limitations. First, we did not assess whether the number of medications changed over time or whether fewer drugs, in conjunction with KM, led to improved outcomes. Second, while acupuncture (including electroacupuncture) formed the main exposure, other integrative therapies such as herbal medicine might also have contributed to the outcomes (Lee et al., 2024). Third, the findings are specific to older stroke survivors and may not translate to other populations. We also did not examine prognostic factors such as cognitive impairment or frailty, which could influence falls and mortality.
This study has several strengths and limitations that must be weighed when interpreting the findings. On the strength side, we applied rigorous propensity-score methods and a large, nationally representative cohort of older stroke survivors, enabling precise estimates for outcomes such as post-stroke mortality. Nevertheless, limitations remain. First, we could not assess the relationship between the changes of the number of medications and the outcomes, precluding evaluation of whether subsequent de-prescribing—or the synergy between fewer drugs and Korean Medicine (KM)—mediated the observed associations. Second, although acupuncture (including electroacupuncture) constituted the primary exposure, ancillary KM modalities such as herbal prescriptions and manual therapies were not covered by NHIS and therefore were incompletely recorded in the database. It is important to note that these modalities may have contributed to both fall risk and survival. Third, several prognostic factors unavailable in NHIS database—including neurological severity (e.g., NIHSS), rehabilitation dose, family support, cognitive impairment, and frailty—could confound the results; if KM users were functionally milder or enjoyed greater social resources, the mortality benefit could be over-estimated and the excess falls under-estimated, whereas preferential KM use by more disabled patients would bias effects toward the null. Fourth, we could not evaluate pharmacodynamic interactions involving high-risk combinations—e.g., anticoagulants taken concurrently with selective-serotonin reuptake inhibitors or benzodiazepines—even though these pairings are well known to increase bleeding, sedation, and fall propensity. Reliable identification of such interactions would require granular data on dose, formulation, and administration timing, none of which are available in the NHIS claims files; thus a clinically meaningful co-exposure definition could not be constructed for the present analysis. Finally, because the cohort comprised elderly stroke survivors, generalizability to younger patients or to non-stroke populations is uncertain. Prospective studies that track dynamic medication exposure and incorporate detailed functional, cognitive, and social metrics are warranted to validate and extend these findings.
5 Conclusion
Among older stroke survivors, initiation of Korean Medicine (KM) within the first post-stroke year was linked to a higher incidence of falls yet a lower 3-year all-cause mortality, and these associations persisted regardless of baseline polypharmacy status. In the hyper-polypharmacy subgroup, KM left fall risk unchanged but still conferred a survival advantage. The absence of significant interaction terms indicates that KM neither amplifies nor attenuates the effect of polypharmacy on either outcome; rather, its mortality benefit appears broadly applicable, whereas the excess falls likely reflect enhanced mobility and survivor bias. Prospective studies with granular medication data and detailed KM exposure—including uninsured herbal prescriptions—are warranted to determine whether specific KM components can simultaneously reduce drug burden and adverse clinical events in diverse geriatric populations.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board of Kyung Hee University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
Y-SL: Conceptualization, Writing – original draft, Investigation, Visualization, Data curation. B-HJ: Validation, Resources, Writing – review and editing. JJ: Writing – review and editing, Project administration, Methodology. H-GL: Formal Analysis, Writing – original draft, Validation, Project administration. SK: Project administration, Funding acquisition, Supervision, Methodology, Writing – review and editing. W-SJ: Writing – review and editing, Resources.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (No. HF20C0147 & No. RS-2022-KH127675). The authors alone are responsible for the content and writing of the paper.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2025.1621819/full#supplementary-material
References
Beezer, J., Al Hatrushi, M., Husband, A., Kurdi, A., and Forsyth, P. (2021). Polypharmacy definition and prevalence in heart failure: a systematic review. Heart Fail Rev. 27, 465–492. doi:10.1007/s10741-021-10135-4
Chang, T. I., Park, H., Kim, D. W., Jeon, E. K., Rhee, C. M., Kalantar-Zadeh, K., et al. (2020). Polypharmacy, hospitalization, and mortality risk: a nationwide cohort study. Sci. Rep. 10 (1), 18964. doi:10.1038/s41598-020-75888-8
Cheol Seong, S., Kim, Y. Y., Khang, Y. H., Heon Park, J., Kang, H. J., Lee, H., et al. (2017). Data resource profile: the national health information database of the national health insurance service in South Korea. Int. J. Epidemiol. 46 (3), 799–800. doi:10.1093/ije/dyw253
Cohen, D. L., Roffe, C., Beavan, J., Blackett, B., Fairfield, C. A., Hamdy, S., et al. (2016). Post-stroke dysphagia: a review and design considerations for future trials. Int. J. Stroke 11 (4), 399–411. doi:10.1177/1747493016639057
Cole, J. A., Gonçalves-Bradley, D. C., Alqahtani, M., Barry, H. E., Cadogan, C., Rankin, A., et al. (2023). Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst. Rev. 10 (10), Cd008165. doi:10.1002/14651858.CD008165.pub5
Development, N. I. f.K. M. (2024). “Ministry of health and Welfare,” in MoHa Welfare: Korean medicine utilization and herbal medicine consumption survey 2023. (Gyeongsan, South Korea: National Institute for Korean Medicine Development).
Frankenthal, D., Lerman, Y., Kalendaryev, E., and Lerman, Y. (2014). Intervention with the screening tool of older persons potentially inappropriate prescriptions/screening tool to alert doctors to right treatment criteria in elderly residents of a chronic geriatric facility: a randomized clinical trial. J. Am. Geriatr. Soc. 62 (9), 1658–1665. doi:10.1111/jgs.12993
Gallacher, K. I., Batty, G. D., McLean, G., Mercer, S. W., Guthrie, B., May, C. R., et al. (2014). Stroke, multimorbidity and polypharmacy in a nationally representative sample of 1,424,378 patients in Scotland: implications for treatment burden. BMC Med. 12, 151. doi:10.1186/s12916-014-0151-0
Gnjidic, D., Hilmer, S. N., Blyth, F. M., Naganathan, V., Waite, L., Seibel, M. J., et al. (2012). Polypharmacy cutoff and outcomes: five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J. Clin. Epidemiol. 65 (9), 989–995. doi:10.1016/j.jclinepi.2012.02.018
Goto, H., Satoh, N., Hayashi, Y., Hikiami, H., Nagata, Y., Obi, R., et al. (2011). A Chinese herbal medicine, tokishakuyakusan, reduces the worsening of impairments and independence after stroke: a 1-year randomized, controlled trial. Evid. Based Complement. Altern. Med. 2011, 194046. doi:10.1093/ecam/nep026
Han, C. H., Kim, M., Cho, S. Y., Jung, W. S., Moon, S. K., Park, J. M., et al. (2018). Adjunctive herbal medicine treatment for patients with acute ischemic stroke: a systematic review and meta-analysis. Complement. Ther. Clin. Pract. 33, 124–137. doi:10.1016/j.ctcp.2018.09.007
Hong, X., Li, S., Zhong, Z., Lin, Y., and Zhang, K. (2024). Effects of acupuncture combined with trunk strengthening training on balance and gait abilities in stroke hemiplegic patients. Medicine 103 (29), e37784. doi:10.1097/MD.0000000000037784
Hu, C., Wang, X., and Pan, T. (2024). Effect of acupuncture combined with lower limb gait rehabilitation robot on improving walking function in stroke patients with hemiplegia. NeuroRehabilitation 54 (2), 309–317. doi:10.3233/NRE-230258
Iwasaki, K., Kato, S., Monma, Y., Niu, K., Ohrui, T., Okitsu, R., et al. (2007). A pilot study of banxia houpu tang, a traditional Chinese medicine, for reducing pneumonia risk in older adults with dementia. J. Am. Geriatr. Soc. 55 (12), 2035–2040. doi:10.1111/j.1532-5415.2007.01448.x
Jung, W. S., Choi, D. J., Cho, K. H., Lee, K. S., Moon, S. K., Kim, Y. S., et al. (2003). Safety and efficacy assessment of chungpyesagan-tang for acute ischemic stroke. Am. J. Chin. Med. 31 (2), 181–190. doi:10.1142/s0192415x03000898
Jung, W. S., Min, I. K., Jin, C., Park, J. Y., Kim, H. G., Kwak, Y., et al. (2018). Inhibitory effect of Chunghyul-dan on stroke recurrence in small vessel disease patients: a 5-year observational study. J. evidence-based Integr. Med. 23, 2515690X18789374. doi:10.1177/2515690X18789374
Kim, H. A., Shin, J. Y., Kim, M. H., and Park, B. J. (2014). Prevalence and predictors of polypharmacy among Korean elderly. PLoS One 9 (6), e98043. doi:10.1371/journal.pone.0098043
Kim, S., Kim, M. S., You, S. H., and Jung, S. Y. (2020). Conducting and reporting a clinical research using Korean healthcare claims database. Korean J. Fam. Med. 41 (3), 146–152. doi:10.4082/kjfm.20.0062
Kohno, J., Kawamura, T., Kikuchi, A., Akaishi, T., Takayama, S., and Ishii, T. (2021). A Japanese traditional medicine Hochuekkito promotes negative conversion of vancomycin-resistant Enterococci. Sci. Rep. 11 (1), 11300. doi:10.1038/s41598-021-90890-4
Kojima, T., Akishita, M., Kameyama, Y., Yamaguchi, K., Yamamoto, H., Eto, M., et al. (2012a). High risk of adverse drug reactions in elderly patients taking six or more drugs: analysis of inpatient database. Geriatr. Gerontol. Int. 12 (4), 761–762. doi:10.1111/j.1447-0594.2012.00868.x
Kojima, T., Akishita, M., Nakamura, T., Nomura, K., Ogawa, S., Iijima, K., et al. (2012b). Polypharmacy as a risk for fall occurrence in geriatric outpatients. Geriatr. Gerontol. Int. 12 (3), 425–430. doi:10.1111/j.1447-0594.2011.00783.x
Kose, E., Toyoshima, M., Okazoe, S., Oka, R., Shiratsuchi, Y., and Hayashi, H. (2017). The relationship between polypharmacy and recovery of activities of daily living among convalescent stroke patients: a propensity score-matched analysis. Eur. Geriatr. Med. 8 (3), 250–255. doi:10.1016/j.eurger.2017.04.009
Lee, B., Kim, S. N., Park, H. J., and Lee, H. (2014). Research advances in treatment of neurological and psychological diseases by acupuncture at the Acupuncture Meridian Science Research Center. Integr. Med. Res. 3 (2), 41–48. doi:10.1016/j.imr.2014.03.003
Lee, H. G., Arai, I., and Kwon, S. (2024). A herbal prescription of insamyangyeongtang as a therapeutic agent for frailty in elderly: a narrative review. Nutrients 16 (5), 721. doi:10.3390/nu16050721
Lee, H. G., Kwon, S., Cho, S. Y., Park, S. U., Jung, W. S., Moon, S. K., et al. (2023). Effect of an herbal medicine, Chunghyul-dan, on prevention of recurrence in patients with ischemic stroke: a retrospective cohort study. Med. Baltim. 102 (45), e35840. doi:10.1097/md.0000000000035840
Lee, H. G., Kwon, S., Jang, B. H., Jeon, J. P., Lee, Y. S., Jung, W. S., et al. (2022). A study on the perceptions of Korean older adult patients and caregivers about polypharmacy and deprescribing. Int. J. Environ. Res. Public Health 19 (18), 11446. doi:10.3390/ijerph191811446
Liu, S. Y., Hsieh, C. L., Wei, T. S., Liu, P. T., Chang, Y. J., and Li, T. C. (2009). Acupuncture stimulation improves balance function in stroke patients: a single-blinded controlled, randomized study. Am. J. Chin. Med. 37 (3), 483–494. doi:10.1142/s0192415x09006990
Long, Y. B., and Wu, X. P. (2012). A meta-analysis of the efficacy of acupuncture in treating dysphagia in patients with a stroke. Acupunct. Med. 30 (4), 291–297. doi:10.1136/acupmed-2012-010155
Lui, S. K., and Nguyen, M. H. (2018). Elderly stroke rehabilitation: overcoming the complications and its associated challenges. Curr. Gerontol. Geriatr. Res., 9853837. doi:10.1155/2018/9853837
Manyanga, T., Froese, M., Zarychanski, R., Abou-Setta, A., Friesen, C., Tennenhouse, M., et al. (2014). Pain management with acupuncture in osteoarthritis: a systematic review and meta-analysis. BMC Complement. Altern. Med. 14, 312. doi:10.1186/1472-6882-14-312
Masnoon, N., Shakib, S., Kalisch-Ellett, L., and Caughey, G. E. (2017). What is polypharmacy? A systematic review of definitions. BMC Geriatr. 17 (1), 230. doi:10.1186/s12877-017-0621-2
McCaffrey, D. F., Griffin, B. A., Almirall, D., Slaughter, M. E., Ramchand, R., and Burgette, L. F. (2013). A tutorial on propensity score estimation for multiple treatments using generalized boosted models. Stat. Med. 32 (19), 3388–3414. doi:10.1002/sim.5753
Morone, G., Iosa, M., Pratesi, L., and Paolucci, S. (2014). Can overestimation of walking ability increase the risk of falls in people in the subacute stage after stroke on their return home? Gait Posture 39 (3), 965–970. doi:10.1016/j.gaitpost.2013.12.022
Muth, C., and Glasziou, P. P. (2015). Guideline recommended treatments in complex patients with multimorbidity. BMJ 351, h5145. doi:10.1136/bmj.h5145
Nielsen, A., Dusek, J. A., Taylor-Swanson, L., and Tick, H. (2022). Acupuncture therapy as an evidence-based nonpharmacologic strategy for comprehensive acute pain care: the academic consortium pain task force white paper update. Pain Med. 23 (9), 1582–1612. doi:10.1093/pm/pnac056
Nogami, T., Fujimoto, M., Watari, H., Kimbara, Y., Shibahara, N., and Shimada, Y. (2019). Kampo medicine resolves a case of polypharmacy with improvement sustained for 10 years. Traditional Kampo Med. 6 (2), 109–112. doi:10.1002/tkm2.1217
O’Mahony, D., Cherubini, A., Guiteras, A. R., Denkinger, M., Beuscart, J. B., Onder, G., et al. (2023). STOPP/START criteria for potentially inappropriate prescribing in older people: version 3. Eur. Geriatr. Med. 14 (4), 625–632. doi:10.1007/s41999-023-00777-y
Onoue, H., Koyama, T., Zamami, Y., Hagiya, H., Tatebe, Y., Mikami, N., et al. (2018). Trends in polypharmacy in Japan: a nationwide retrospective study. J. Am. Geriatr. Soc. 66 (12), 2267–2273. doi:10.1111/jgs.15569
Panel, A. G. S. B. C. U. E. (2015). American geriatrics society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J. Am. Geriatr. Soc. 63 (11), 2227–2246. doi:10.1111/jgs.13702
Park, H. Y., Park, J. W., Sohn, H. S., and Kwon, J. W. (2017a). Association of Parkinsonism or Parkinson disease with polypharmacy in the year preceding diagnosis: a nested case-control study in South Korea. Drug Saf. 40 (11), 1109–1118. doi:10.1007/s40264-017-0559-5
Park, H. Y., Park, J. W., Song, H. J., Sohn, H. S., and Kwon, J. W. (2017b). The association between polypharmacy and dementia: a nested case-control study based on a 12-year longitudinal cohort database in South Korea. PLoS One 12 (1), e0169463. doi:10.1371/journal.pone.0169463
Seca, S., Miranda, D., Cardoso, D., Nogueira, B., Greten, H. J., Cabrita, A., et al. (2019). Effectiveness of acupuncture on pain, physical function and health-related quality of life in patients with rheumatoid arthritis: a systematic review of quantitative evidence. Chin. J. Integr. Med. 25, 704–709. doi:10.1007/s11655-018-2914-x
Sirois, C., Domingues, N. S., Laroche, M. L., Zongo, A., Lunghi, C., Guenette, L., et al. (2019). Polypharmacy definitions for multimorbid older adults need stronger foundations to guide research, clinical practice and public health. Pharm. (Basel) 7 (3), 126. doi:10.3390/pharmacy7030126
Skelton, D. A. (2023). When physical activity increases risk of injurious falls: right activity, right person, right time. Age Ageing 52 (11), afad209. doi:10.1093/ageing/afad209
Takano, S., Nakamura, M., Morita, A., Ryuu, K., Izumi, Y., Nagai, C., et al. (2018). Usefulness of Kampo medicine for avoiding polypharmacy among hospitalized patients. Kampo Med. 69, 328–335. doi:10.3937/kampomed.69.328
Tian, Z. Y., Feng, L. D., Xie, Y., Xu, D. H., Zhang, C. Y., Kong, L. B., et al. (2021). Chinese herbal medicine Xingnaojing injection for acute ischemic stroke: an overview of systematic reviews and meta-analyses. Front. Pharmacol. 12, 659408. doi:10.3389/fphar.2021.659408
Vickers, A. J., Vertosick, E. A., Lewith, G., MacPherson, H., Foster, N. E., Sherman, K. J., et al. (2018). Acupuncture for chronic pain: update of an individual patient data meta-analysis. J. Pain 19 (5), 455–474. doi:10.1016/j.jpain.2017.11.005
Wang, J., Bernhardt, J., Johns, H., Churilov, L., Said, C., Fini, N. A., et al. (2025). An exploration of serious falls after stroke using a large international stroke rehabilitation database. Int. J. Stroke. 20 (5), 550–558. doi:10.1177/17474930251314330
Wastesson, J. W., Morin, L., Tan, E. C. K., and Johnell, K. (2018). An update on the clinical consequences of polypharmacy in older adults: a narrative review. Expert Opin. Drug Saf. 17 (12), 1185–1196. doi:10.1080/14740338.2018.1546841
Weerdesteyn, V. P. P. T., de Niet, M. M., van Duijnhoven, H. J. R. M., and Geurts, A. C. H. M. D. P. (2008). Falls in individuals with stroke. J. Rehabil. Res. Dev. 45 (8), 1195–1213. doi:10.1682/jrrd.2007.09.0145
Wei, W. E., De Silva, D. A., Chang, H. M., Yao, J., Matchar, D. B., Young, S. H. Y., et al. (2019). Post-stroke patients with moderate function have the greatest risk of falls: a National Cohort Study. BMC Geriatr. 19 (1), 373. doi:10.1186/s12877-019-1377-7
Yan, T., and Hui-Chan, C. W. (2009). Transcutaneous electrical stimulation on acupuncture points improves muscle function in subjects after acute stroke: a randomized controlled trial. J. Rehabil. Med. 41 (5), 312–316. doi:10.2340/16501977-0325
Yang, A., Wu, H. M., Tang, J. L., Xu, L., Yang, M., and Liu, G. J. (2016). Acupuncture for stroke rehabilitation. Cochrane Database Syst. Rev. 2016 (8), Cd004131. doi:10.1002/14651858.CD004131.pub3
Yao, S. S., Meng, X., Cao, G. Y., Huang, Z. T., Chen, Z. S., Han, L., et al. (2020). Associations between multimorbidity and physical performance in older Chinese adults. Int. J. Environ. Res. Public Health 17 (12), 4546. doi:10.3390/ijerph17124546
Yu, M., Sun, Z. J., Li, L. T., Ge, H. Y., Song, C. Q., and Wang, A. J. (2015). The beneficial effects of the herbal medicine Di-huang-yin-zi (DHYZ) on patients with ischemic stroke: a Randomized, Placebo controlled clinical study. Complement. Ther. Med. 23 (4), 591–597. doi:10.1016/j.ctim.2015.06.003
Keywords: polypharmacy, Korean medicine, stroke, falls, mortality
Citation: Lee Y-S, Jang B-H, Jeon JP, Lee H-G, Kwon S and Jung W-S (2025) Association of Korean Medicine and polypharmacy with fall risk and mortality in older adults with stroke. Front. Pharmacol. 16:1621819. doi: 10.3389/fphar.2025.1621819
Received: 02 May 2025; Accepted: 09 June 2025;
Published: 19 June 2025.
Edited by:
Elaine Wat, The Chinese University of Hong Kong, ChinaReviewed by:
Liuding Wang, China Academy of Chinese Medical Sciences, ChinaYufeng Peng, Ningbo Zhenhai Hospital of Traditional Chinese Medicine, China
Copyright © 2025 Lee, Jang, Jeon, Lee, Kwon and Jung. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Han-Gyul Lee, Z3l1bGVlMDYxNEBoYW5tYWlsLm5ldA==; Seungwon Kwon, a2tva2tvdHR1bmdAaGFubWFpbC5uZXQ=
 Ye-Seul Lee
Ye-Seul Lee Bo-Hyoung Jang
Bo-Hyoung Jang Jin Pyeong Jeon3
Jin Pyeong Jeon3 Han-Gyul Lee
Han-Gyul Lee Seungwon Kwon
Seungwon Kwon