- Department of Thoracic Surgery, The Second Hospital of Tianjin Medical University, Tianjin, China
Background: Effective analgesia is crucial for patients with blunt thoracic trauma, yet the optimal analgesic approach remains controversial. This study aimed to evaluate the efficacy of opioids combined with Sodium Aescinate in blunt thoracic trauma management.
Methods: Fifty patients with blunt thoracic trauma were randomly assigned to receive either opioids alone (morphine hydrochloride sustained-release tablets (MHST), Group A) or opioids combined with Sodium Aescinate (Group B). Pain scores, respiratory parameters, complications, and hospitalization metrics were assessed.
Results: When pain number rating scale (NRS) scores reached ≤4, Group B required significantly lower opioid doses throughout therapy. Group B demonstrated significantly higher FEV1, FVC, and arterial PO2, and lower PCO2 compared to Group A, while respiratory rates remained similar between groups. Opioid-related complications (nausea, constipation) were significantly reduced in Group B, which also experienced shorter hospital stays and lower costs.
Conclusion: This study demonstrated synergism between opioids and Sodium Aescinate in providing effective analgesia. The combination therapy offers an efficient and economical approach for pain management in blunt thoracic trauma, with improved respiratory function and reduced opioid-related complications.
Introduction
Thoracic trauma represents one of the most significant causes of mortality and morbidity in trauma patients worldwide, with substantial clinical and socioeconomic implications. Blunt thoracic trauma carries an alarming mortality rate ranging from 10% to 25% (Hoogma et al., 2024). The management of blunt thoracic trauma has been subject to ongoing clinical debate and evolution over decades. Traditionally, treatment protocols have centered around two fundamental principles: immobilization and analgesia. However, research focus has been disproportionately directed toward various immobilization techniques, including mechanical stabilization methods and ventilatory support strategies (Gamberini et al., 2025; Gola et al., 2020). This research imbalance has resulted in relatively fewer evidence-based innovations in pain management protocols despite its critical importance. Current literature increasingly recognizes that pain control and immobilization should be considered equally essential components in the comprehensive management of thoracic trauma patients.
Effective pain control represents a crucial determinant of patient outcomes following thoracic trauma. The successful management of pain has been demonstrated to significantly reduce morbidity and enhance overall patient satisfaction during the recovery process (Feray et al., 2023). Pain associated with blunt thoracic trauma, particularly in cases involving rib fractures, can severely impair respiratory mechanics, leading to reduced lung volumes, inadequate clearance of secretions, and potentially progressive atelectasis (Cha et al., 2021; Chin et al., 2021). These complications can subsequently result in pneumonia, respiratory failure, and prolonged hospitalization if pain remains inadequately controlled. Despite this clinical significance, comprehensive research specifically examining pain control strategies in thoracic trauma remains relatively limited compared to other aspects of management (Koushik et al., 2023; Lazar et al., 2024; Lodhia et al., 2023; Mohamed et al., 2024; Mukherjee et al., 2023; Niazi et al., 2025). Sodium aescinate (SA), a triterpene saponin extract from horse chestnut seeds, demonstrates multiple therapeutic properties and finds extensive application in clinical practice for treating edema and inflammatory conditions (Xi et al., 2025). Studies have investigated sodium aescinate in acute lung injury. It can mitigate oleic acid-induced acute lung injury by modulating the levels of SOD, MDA, and MMP-9 in plasma and lung tissue (Wei et al., 2011). However, research on sodium aescinate in blunt thoracic trauma remains limited.
To explore novel approaches for pain management after trauma, we retrospectively analyzed patient data comparing the effects of a combination therapy of opioids and glycyrrhetinic acid (saponin) with monotherapy using opioids alone. Our analysis focused on three primary outcomes: assessing the differences in analgesic effects between the two groups, evaluating the impact of each treatment on respiratory parameters, and determining the effectiveness of the combined therapy in mitigating adverse effects associated with opioid use alone.
Methods
Study design and ethical considerations
This retrospective study consecutively screened inpatients diagnosed with blunt thoracic trauma at the Second Hospital of Tianjin Medical University between January 2017 and January 2023. We confirm that the parent trial has not been published, and all the data originates from the hospital medical record database. The protocol received ethical approval from the institutional review board of Tianjin Medical University (Approval No.KY 2025K294) and adhered to the Declaration of Helsinki principles. Written informed consent was obtained from all participants prior to data collection.
Participant selection criteria
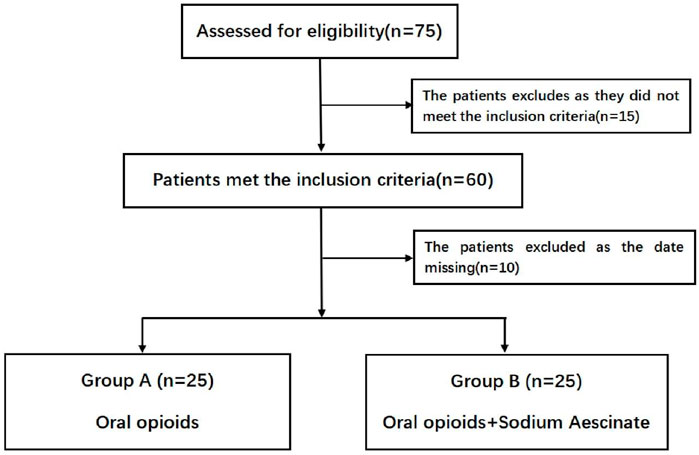
Inclusion required radiologically confirmed blunt thoracic trauma involving soft tissue injuries or bony fractures (rib fractures/flail chest). Exclusion criteria comprised: 1) polytrauma with Injury Severity Score (ISS) > 25; 2) chronic pain disorders or cancer-related pain syndromes; 3) severe cardiopulmonary/renal/hepatic insufficiency (Child-Pugh C or eGFR <30 mL/min/1.73 m2); 4) active malignancies; 5) body mass index (BMI) > 30 kg/m2; 6) tobacco use (>10 cigarettes/day) or alcohol abuse (>3 standard drinks/day); 7) incomplete clinical records. A total of 75 patients met eligibility criteria and completed follow-up (Figure 1).
Clinical data collection
Demographic parameters (age, sex, BMI) and injury characteristics (ISS, fracture patterns) were systematically recorded (Table 1). Respiratory function was assessed through serial measurements of respiratory rate (RR), arterial blood gases (PaO2/PaCO2), and spirometry (FVC/FEV1). Pain intensity was quantified using the 11-point Numerical Rating Scale (NRS: 0 = no pain, 10 = worst imaginable pain) under standardized resting conditions.
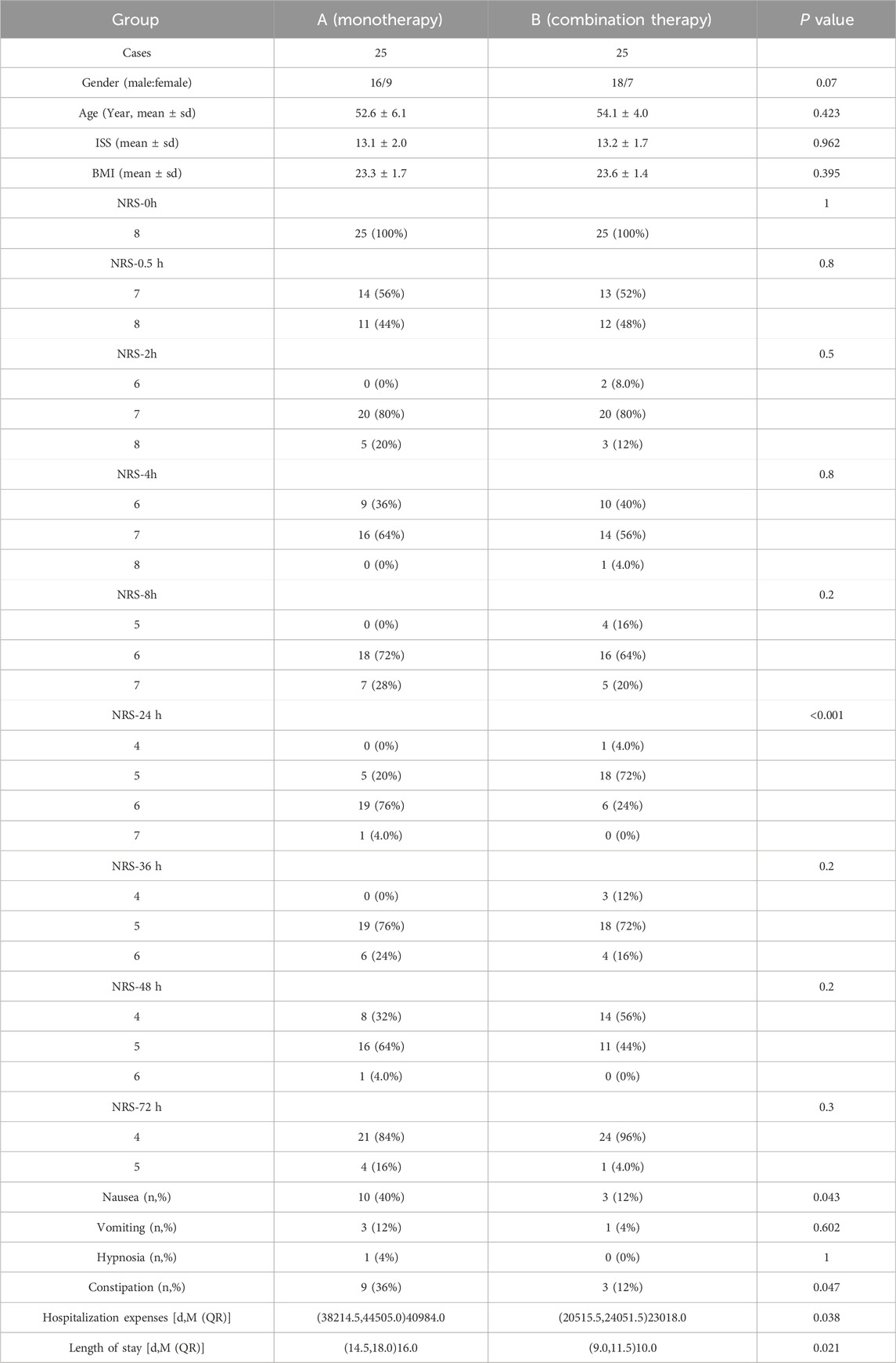
Table 1. Comparison of baseline characteristics, complications, and hospitalization parameters between groups A and B.
Pain scores (NRS), respiratory function parameters (FVC, FEV1, PaO2, PaCO2), and cumulative opioid consumption were measured at baseline (pre-admission or pre-treatment) and at nine post-treatment timepoints (6, 12, 24, 36, 48, 60, 72, 84, and 96 h).
Pharmacological intervention and outcome measures
Patients were randomly allocated to either the control group (A) receiving MHST (10 mg PO BID) or the experimental group (B) receiving combined therapy of MHST (10 mg PO BID) plus sodium aescinate tablets (30 mg PO BID). Rescue analgesia with 10 mg MHST was administered when NRS scores exceeded 4 points post-intervention, and medication adherence was monitored through pill counts and pharmacy records (the NRS ≥4 threshold aligns with International Association for the Study of Pain guidelines for moderate pain requiring intervention). Primary endpoints included pain control efficacy (defined as NRS ≤4) and opioid consumption (the unit is milligrams). Secondary outcomes encompassed hospitalization duration and costs, pulmonary function recovery (measured by FVC/FEV1 change from baseline), and analgesia-related complications (including nausea/vomiting incidence, somnolence duration, and constipation severity). Adverse events were documented using CTCAE v5.0 criteria through daily clinician assessments and patient self-reports.
Average daily opioid consumption (mg/day) was defined as the total cumulative opioid dose (mg) administered during the hospitalization divided by the length of hospital stay (days).
Statistical analysis
Data analysis utilized SPSS 24.0 (IBM Corp.) with two-tailed α = 0.05. Normality was verified using Shapiro-Wilk tests (W > 0.90). Continuous variables were expressed as mean ± SD (parametric) or median [IQR] (non-parametric), analyzed via independent t-tests or Mann-Whitney U tests respectively. Categorical variables underwent χ2 or Fisher’s exact testing with effect sizes reported as odds ratios [95%CI]. Multivariable regression adjusted for age, ISS, and baseline NRS scores.
For the longitudinal data on respiratory function parameters and cumulative opioid consumption, a linear mixed-effects model was employed. Fixed effects included time (in hours), treatment group, and their interaction, while subjects were entered as random effects to account for individual variability. If the overall model was significant, post hoc comparisons at each time point were performed with Bonferroni correction.
Results
Participant enrollment and group allocation
A total of 75 patients with blunt thoracic trauma were initially identified and assessed for eligibility. Following the application of exclusion criteria, 25 patients were excluded from the study: 15 due to history of chronic pain and long-term analgesic use, and 10 due to incomplete data documentation. The remaining 50 patients were equally allocated into two treatment groups: Group A (n = 25) received standard (morphine hydrochloride sustained-release tablets) MHST alone, while Group B (n = 25) received MHST combined with Sodium Aescinate Tablets. Both groups demonstrated comparable baseline characteristics, allowing for meaningful between-group comparisons. All enrolled participants completed the study protocol with no dropouts recorded during the follow-up period.
Analgesic requirements and opioid consumption patterns
Opioid consumption was systematically monitored over a 72-h period following trauma onset while maintaining pain scores at or below NRS ≤4 across both groups. Group B demonstrated significantly reduced MHST dosage requirements compared to Group A at multiple time points: at 24 h (30.8 ± 2.76 vs 37.2 ± 4.58), 36 h (33.6 ± 4.89 vs 55.2 ± 5.85), 48 h (42.8 ± 4.58 vs 82.4 ± 7.78), and 72 h (53.6 ± 4.89 vs 105.2 ± 10.84). This pattern resulted in a markedly lower cumulative opioid consumption in Group B compared to Group A (233.6 ± 28.71 vs 363.2 ± 27.04, p < 0.001). The temporal progression of opioid requirements exhibited distinct trajectories between groups, with Group A showing a steeper increase over time as illustrated in Figure 2.
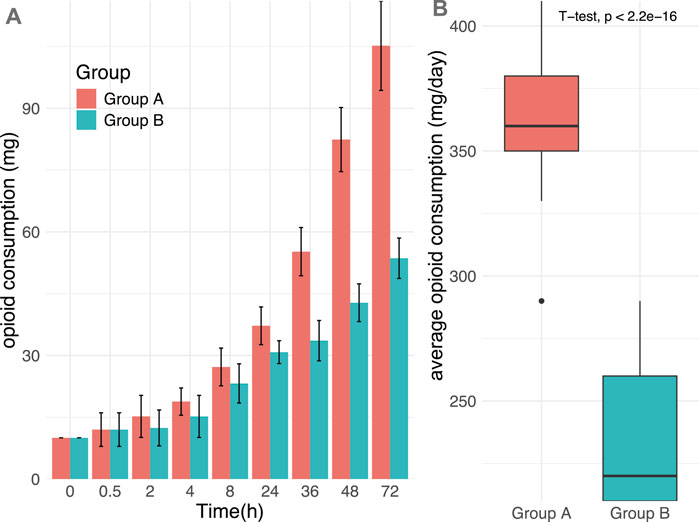
Figure 2. The time progression of opioid demand in two groups over time trajectories. (A) The trajectory of the change of opioid needs over time; (B) The trajectory of the change of opioid needs during the entire process. Group A = monotherapy. Group B = combination therapy.
Respiratory function and physiological parameter improvements
Comprehensive assessment of physiological parameters revealed comparable baseline values between groups prior to intervention. Following treatment, both groups demonstrated significant improvements in pain scores, PO2, PCO2, respiratory rate (RR), forced vital capacity (FVC), and forced expiratory volume in one second (FEV1) compared to their respective baseline values (p < 0.001). Notably, Group B exhibited superior outcomes in several key parameters compared to Group A, including higher PO2 levels, greater improvements in FVC and FEV1, and lower PaCO2 values (p < 0.001 for all comparisons). Interestingly, no statistically significant difference was observed in respiratory rate between the two treatment groups (p > 0.05). The comparative improvements in pulmonary function parameters are graphically presented in Figure 3, demonstrating the enhanced respiratory recovery profile of patients receiving combination therapy.
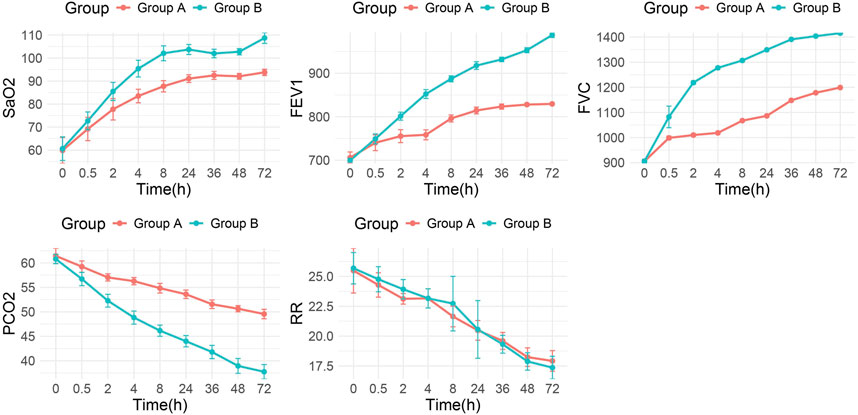
Figure 3. Trends of lung function parameters over time between the two groups. Group A = monotherapy. Group B = combination therapy.
Healthcare utilization, safety profile, and economic outcomes
The safety assessment revealed no instances of severe respiratory depression or hypotension in either treatment group. However, significant differences emerged in healthcare utilization metrics and adverse event profiles. Patients in Group B exhibited a significantly shorter hospital length of stay and consequently lower hospitalization expenses compared to Group A (P < 0.05 for both measures). The incidence of opioid-associated complications, particularly nausea and constipation, was significantly reduced in Group B (P < 0.05), suggesting enhanced tolerability of the combination therapy. The rates of vomiting and somnolence were comparable between groups with no statistically significant differences observed. A comprehensive comparison of clinical outcomes, adverse events, and economic parameters is presented in Table 1, highlighting the multidimensional benefits of the combination therapy approach.
Discussion
Our primary finding reveals that the combination of opioids and Sodium Aescinate effectively alleviates pain in blunt thoracic trauma patients while significantly reducing required opioid dosages. This reduction directly translated to a marked decrease in opioid-related adverse effects, including nausea and constipation. The combination therapy significantly improved respiratory parameters, with Group B (combination therapy) demonstrating higher FEV1 and FVC values and lower PCO2 levels compared to Group A (opioid monotherapy). These improved respiratory mechanics subsequently contributed to shorter hospital stays and reduced hospitalization costs for patients receiving the combined regimen. These findings are particularly relevant given that blunt thoracic trauma represents the majority of thoracic trauma cases and encompasses both soft tissue and bone injuries, including rib fractures that affect approximately two-thirds of chest trauma patients. The prevalence of complications in blunt thoracic trauma patients underscores the need for optimized treatments that minimize respiratory complications while providing adequate pain control. Future studies should validate whether age-specific benefits exist.
The efficacy of the combined therapy can be explained through complementary mechanisms of action. Pain in blunt chest trauma patients arises from multiple pathways, including inflammatory responses that lead to hyperemia, increased peripheral capillary permeability, and tissue exudation (Polycarpou and Kim, 2021; Schnadthorst et al., 2023). These processes result in tissue swelling and increased tension, exacerbating pain sensation. Sodium Aescinate appears to inhibit serum lysosomal activity, stabilize lysosomal membranes, prevent protease metabolism, and reduce capillary permeability—all contributing to decreased exudation and subsequent pain (Sharma et al., 2022; Stopenski et al., 2022). Additionally, it affects vascular endothelial cell receptors, causing constriction of capacitance vessels and enhancing venous return, which reduces venous congestion and tissue swelling. By addressing these underlying inflammatory mechanisms, Sodium Aescinate provides a pathway for pain relief that is complementary to the direct analgesic effects of opioids, thereby allowing for dose reduction of the latter while maintaining effective analgesia (Szamborski et al., 2022; van Zyl et al., 2024).
The management of blunt thoracic trauma has consistently posed significant challenges to thoracic surgeons. Despite extensive research, a universally recognized optimal treatment modality remains elusive. Current management strategies have centered on immobilization, chest physiotherapy, and effective pain control. Adequate analgesia remains the cornerstone of successful management as it enhances respiratory mechanics, whereas uncontrolled pain causes splinting and guarding, leading to reduced tidal volumes, decreased mobility, and impaired ability to cough and clear secretions (Sharma et al., 2022; Simon and Wickham, 2019). Various pain control strategies have been employed clinically, including intravenous narcotics, local rib blocks, pleural infusion catheters, paravertebral blocks, and epidural analgesia (Polycarpou and Kim, 2021). Each method presents distinct advantages and limitations. Epidural analgesia has gained advocacy in numerous studies due to its minimal effects on respiratory depression, somnolence, and gastrointestinal symptoms. However, it is not universally applicable due to several drawbacks. The procedure requires specialized technical expertise and carries potential complications including hypotension, epidural infections, hematoma, and spinal cord trauma (Almeida, 2021). It is contraindicated in patients with fever, coagulation abnormalities, or altered mental status, and some patients resist invasive procedures regardless of efficacy. Oral analgesics remain widely accepted due to their non-invasive nature, effectiveness, and ease of administration. While non-steroidal anti-inflammatory drugs can contribute to pain management in blunt thoracic trauma, they often provide insufficient relief, necessitating opioid supplementation (Cha et al., 2021; Chin et al., 2021; Ja et al., 2020; Kourouche et al., 2018).
However, the dose-dependent side effects of opioids (nausea, vomiting, drowsiness, and constipation) limit their widespread use. The study shows that traumatic injury significantly predisposes patients to chronic opioid use, and those who develop long-term consumption face a higher subsequent mortality risk (von Oelreich et al., 2020). Prolonged opioid exposure initiates regulatory adaptations of opioid receptors—such as desensitization and internalization—that culminate in receptor tolerance. These adaptations recruit several intracellular pathways, most prominently the upregulation of the cyclic AMP/PKA cascade and activation of cAMP response element–binding signaling (Wang et al., 2019). In a randomized study of outpatient laparoscopic cholecystectomy and appendectomy patients, a 3-day multimodal regimen of acetaminophen, ibuprofen, and up to five 5 mg rescue oxycodone tablets provided effective analgesia—patients used an average of only 1.8 oxycodone tablets, and 50% required no opioids at all (Sim et al., 2019). A meta-analysis showed that postoperative bleeding rates were comparable between ketorolac (33/1304, 2.5%) and control groups (21/1010, 2.1%; OR = 1.1, 95% CI 0.61–2.06, P = 0.72) (Wick et al., 2017). These studies demonstrate the need to reduce opioid use in clinical settings to lower patient mortality and addiction risks, making multimodal treatment strategies essential.
Our findings suggest several important clinical implications. First, by reducing opioid requirements, the combination therapy significantly diminishes respiratory inhibition that could otherwise impede expectoration and potentially lead to atelectasis and pulmonary infection. The absence of RR changes in Group B, despite improved PO2and FEV1, suggests enhanced alveolar ventilation efficiency and reduced dead space ventilation rather than altered respiratory drive. This may result from reduced Splinting Respiration due to better analgesia, permitting deeper tidal volumes without increasing respiratory frequency. This respiratory advantage may partially explain the improved clinical outcomes observed in the combination therapy group, including enhanced ventilation function, prevention of pulmonary complications, shortened hospital stays, and reduced hospitalization costs. Second, the combination therapy represents a non-invasive, safe, and easily administered alternative. This characteristic makes it particularly valuable for patients with contraindications to invasive procedures or those with preferences for non-invasive treatment options.
Despite these promising results, several limitations warrant consideration. Although no renal adverse events occurred in our cohort, sodium aescinate carries theoretical nephrotoxicity risks in vulnerable populations (e.g., pre-existing renal impairment). We recommend cautious use in patients with eGFR <60 mL/min/1.73 m2 and routine renal function monitoring during therapy. Our study did not stratify outcomes by age groups or injury severity, which could provide more nuanced insights into which patient populations might benefit most from this combination therapy. Additionally, long-term follow-up data would be valuable to assess any potential differences in chronic pain development or functional outcomes between treatment approaches. Future research should explore optimal dosing regimens, potential interactions with other commonly prescribed medications in trauma patients, and direct comparison with regional anesthetic techniques like paravertebral blocks or serratus plane blocks. Prospective multicenter trials with larger patient cohorts would strengthen the evidence base for this promising treatment approach.
Conclusion
Effective analgesia remains crucial in the treatment of blunt thoracic trauma. The combination of opioids with Sodium Aescinate represents a promising approach that reduces opioid dosage requirements while enhancing patient ventilation function, preventing pulmonary complications, shortening hospital stays, and lowering treatment costs. Compared to other analgesic approaches, this oral medication regimen offers advantages of being non-invasive, safe, effective, and easily administered. These findings suggest that the combined use of opioids and Sodium Aescinate could significantly improve recovery outcomes following blunt thoracic trauma and merits consideration as a standard treatment option in appropriate clinical scenarios.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the institutional review board of Tianjin Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JZ: Visualization, Writing – original draft, Validation, Conceptualization, Methodology, Investigation. YY: Validation, Investigation, Methodology, Supervision, Writing – original draft, Visualization. ZG: Visualization, Resources, Conceptualization, Methodology, Funding acquisition, Writing – review and editing, Supervision.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the: 1. Youth Foundation of The Second Hospital of Tianjin Medical University (2017ydey09). 2. State Key Laboratory of Molecular Vaccinology and Molecular Diagnostics (SKLVD2019KF002).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2025.1623916/full#supplementary-material
References
Almeida, C. R. (2021). Parascapular sub-Iliocostalis plane block: comparative Description of a novel technique for Posterior rib fractures. Pain Pract. 21 (6), 708–714. doi:10.1111/papr.13003
Cha, P. I., Min, J. G., Patil, A., Choi, J., Kothary, N. N., and Forrester, J. D. (2021). Efficacy of intercostal cryoneurolysis as an analgesic adjunct for chest wall pain after surgery or trauma: systematic review. Trauma Surg. Acute Care Open 6 (1), e000690. doi:10.1136/tsaco-2021-000690
Chin, K. J., Versyck, B., and Pawa, A. (2021). Ultrasound-guided fascial plane blocks of the chest wall: a state-of-the-art review. Anaesthesia 76 (Suppl. 1), 110–126. doi:10.1111/anae.15276
Feray, S., Lemoine, A., Aveline, C., and Quesnel, C. (2023). Pain management after thoracic surgery or chest trauma. Minerva Anestesiol. 89 (11), 1022–1033. doi:10.23736/S0375-9393.23.17291-9
Gamberini, L., Moro, F., Dallari, C., Tartaglione, M., Mazzoli, C. A., Allegri, D., et al. (2025). Regional anesthesia modalities in blunt thoracic trauma: a systematic review and Bayesian network meta-analysis. Am. J. Emerg. Med. 89, 199–208. doi:10.1016/j.ajem.2024.12.029
Gola, W., Zajac, M., and Cugowski, A. (2020). Adjuvants in peripheral nerve blocks - the current state of knowledge. Anaesthesiol. Intensive Ther. 52 (4), 323–329. doi:10.5114/ait.2020.98213
Hoogma, D. F., Brullot, L., and Coppens, S. (2024). Get your 7-point golden medal for pain management in video-assisted thoracoscopic surgery. Curr. Opin. Anaesthesiol. 37 (1), 64–68. doi:10.1097/ACO.0000000000001325
Jack, J. M., McLellan, E., Versyck, B., Englesakis, M. F., and Chin, K. J. (2020). The role of serratus anterior plane and pectoral nerves blocks in cardiac surgery, thoracic surgery and trauma: a qualitative systematic review. Anaesthesia 75 (10), 1372–1385. doi:10.1111/anae.15000
Kourouche, S., Buckley, T., Munroe, B., and Curtis, K. (2018). Development of a blunt chest injury care bundle: an integrative review. Injury 49 (6), 1008–1023. doi:10.1016/j.injury.2018.03.037
Koushik, S. S., Bui, A., Slinchenkova, K., Badwal, A., Lee, C., Noss, B. O., et al. (2023). Analgesic techniques for rib fractures-A comprehensive review article. Curr. Pain Headache Rep. 27 (11), 747–755. doi:10.1007/s11916-023-01172-9
Lazar, A. E., Butiulca, M., and Farczadi, L. (2024). Challenges of the regional anesthetic techniques in intensive care Units - a narrative review. J. Crit. Care Med. Targu Mures. 10 (3), 198–208. doi:10.2478/jccm-2024-0023
Lodhia, J. V., Eyre, L., Smith, M., Toth, L., Troxler, M., and Milton, R. S. (2023). Management of thoracic trauma. Anaesthesia 78 (2), 225–235. doi:10.1111/anae.15934
Mohamed, E. H., Elmoheen, A., Bashir, K., Fayed, M., Abdurabu, M., Abdelrahim, M. G., et al. (2024). Comparative analysis of intravenous opioids versus thoracic epidural anesthesia in fractured rib pain management: a systematic review and meta-analysis. Cureus 16 (1), e51740. doi:10.7759/cureus.51740
Mukherjee, K., Schubl, S. D., Tominaga, G., Cantrell, S., Kim, B., Haines, K. L., et al. (2023). Non-surgical management and analgesia strategies for older adults with multiple rib fractures: a systematic review, meta-analysis, and joint practice management guideline from the Eastern Association for the Surgery of Trauma and the Chest Wall Injury Society. J. Trauma Acute Care Surg. 94 (3), 398–407. doi:10.1097/TA.0000000000003830
Niazi, A. U., Solish, M., Moorthy, A., Niazi, F., Abate, A. H., Devion, C., et al. (2025). Use of fascial plane blocks for traumatic rib fractures: a scoping review. Reg. Anesth. Pain Med.–2024-106366. doi:10.1136/rapm-2024-106366
Polycarpou, A., and Kim, B. D. (2021). Pediatric surgical rib fixation: a collected case series of a rare entity. J. Trauma Acute Care Surg. 91 (6), 947–950. doi:10.1097/TA.0000000000003376
Schnadthorst, P. G., Lankes, C., and Schulze, C. (2023). Treatment of trauma-related vertebral body fractures of the thoracic and lumbar spine with orthotic devices: a review. Unfallchirurgie (Heidelb) 126 (8), 632–642. doi:10.1007/s00113-022-01195-8
Sharma, R., Louie, A., Thai, C. P., and Dizdarevic, A. (2022). Chest wall nerve blocks for Cardiothoracic, breast surgery, and rib-related pain. Curr. Pain Headache Rep. 26 (1), 43–56. doi:10.1007/s11916-022-01001-5
Sim, V., Hawkins, S., Gave, A. A., Bulanov, A., Elabbasy, F., Khoury, L., et al. (2019). How low can you go: achieving postoperative outpatient pain control without opioids. J. Trauma Acute Care Surg. 87 (1), 100–103. doi:10.1097/TA.0000000000002295
Simon, J. B., and Wickham, A. J. (2019). Blunt chest wall trauma: an overview. Br. J. Hosp. Med. (Lond). 80 (12), 711–715. doi:10.12968/hmed.2019.80.12.711
Stopenski, S., Binkley, J., Schubl, S. D., and Bauman, Z. M. (2022). Rib fracture management: a review of surgical stabilization, regional analgesia, and intercostal nerve cryoablation. Surg. Pract. Sci. 10, 100089. doi:10.1016/j.sipas.2022.100089
Szamborski, M., Janc, J., Rosinczuk, J., Janc, J. J., Lesnik, P., and Lysenko, L. (2022). Use of ultrasound-guided interfascial plane blocks in anterior and lateral thoracic wall region as safe method for patient anesthesia and analgesia: review of techniques and approaches during COVID-19 pandemic. Int. J. Environ. Res. Public Health 19 (14), 8696. doi:10.3390/ijerph19148696
van Zyl, T., Ho, A. M., Klar, G., Haley, C., Ho, A. K., Vasily, S., et al. (2024). Analgesia for rib fractures: a narrative review. Can. J. Anaesth. 71 (4), 535–547. doi:10.1007/s12630-024-02725-1
von Oelreich, E., Eriksson, M., Brattstrom, O., Sjolund, K. F., Discacciati, A., Larsson, E., et al. (2020). Risk factors and outcomes of chronic opioid use following trauma. Br. J. Surg. 107 (4), 413–421. doi:10.1002/bjs.11507
Wang, S. C., Chen, Y. C., Lee, C. H., and Cheng, C. M. (2019). Opioid addiction, genetic susceptibility, and medical treatments: a review. Int. J. Mol. Sci. 20 (17), 4294. doi:10.3390/ijms20174294
Wei, T., Tong, W., Wen-ping, S., Xiao-hui, D., Qiang, X., Tian-shui, L., et al. (2011). The impact of sodium aescinate on acute lung injury induced by oleic acid in rats. Exp. Lung Res. 37 (10), 585–599. doi:10.3109/01902148.2011.622426
Wick, E. C., Grant, M. C., and Wu, C. L. (2017). Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg. 152 (7), 691–697. doi:10.1001/jamasurg.2017.0898
Keywords: blunt thoracic trauma, opioids, sodium aescinate, analgesic effect, combined therapy
Citation: Zhang J, Yan Y and Guan Z (2025) Combined opioid-sodium aescinate therapy in blunt thoracic trauma: retrospective evaluation. Front. Pharmacol. 16:1623916. doi: 10.3389/fphar.2025.1623916
Received: 07 May 2025; Accepted: 27 August 2025;
Published: 19 September 2025.
Edited by:
Shangke Huang, Southwest Medical University, ChinaReviewed by:
Constanza de Dios, University of Texas Health Science Center at Houston, United StatesHao Li, China Medical University, China
Copyright © 2025 Zhang, Yan and Guan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhiyu Guan, Y25zMjAyMEAxNjMuY29t
 Jun Zhang
Jun Zhang Zhiyu Guan
Zhiyu Guan