- 1Department of Psychiatry, University of Ottawa, Ottawa, ON, Canada
- 2Department of Mental Health, The Ottawa Hospital, Ottawa, ON, Canada
- 3Early Psychosis: Interventions and Clinical-Detection (EPIC) Lab, Department of Psychosis Studies, Institute of Psychiatry, Psychology, London, United Kingdom
- 4Faculty of Environmental and Life Sciences, Center for Innovation in Mental Health, School of Psychology, University of Southampton, Southampton, United Kingdom
- 5Clinical Epidemiology Program, Ottawa Hospital Research Institute, Ottawa, ON, Canada
- 6Pain and Rehabilitation Centre, and Department of Health, Medicine and Caring Sciences, Linköping University, Linköping, Sweden
- 7Neurosciences Department, University of Padua, Padua, Italy
- 8Imaging of Mood- and Anxiety-Related Disorders (IMARD) Group, Institut d'Investigacions Biomèdiques August Pi i Sunyer (IDIBAPS), CIBERSAM, Barcelona, Spain
- 9Department of Clinical Neuroscience, Centre for Psychiatric Research and Education, Karolinska Institutet, Solna, Sweden
- 10Department of Psychiatry, Medical Faculty, University of Basel, Basel, Switzerland
- 11Department of Psychiatry, Psychosomatics and Psychotherapy, University of Lübeck, Lübeck, Germany
- 12Department of Psychiatry, Faculty of Medicine, University of Toronto, Toronto, ON, Canada
- 13Centre for Addiction and Mental Health, Toronto, ON, Canada
- 14Clinical and Experimental Medicine PhD Program, University of Modena and Reggio Emilia, Modena, Italy
- 15Clienia AG, Wetzikon Psychiatric Centre, Wetzikon, Switzerland
- 16Department of General Practice, University Medical Center Würzburg, Würzburg, Germany
- 17Faculty of Education and Health, University of Greenwich, London, United Kingdom
- 18Clinical and Experimental Sciences (CNS and Psychiatry), Faculty of Medicine, University of Southampton, Southampton, United Kingdom
- 19Solent NHS Trust, Southampton, United Kingdom
- 20Hassenfeld Children's Hospital at NYU Langone, New York University Child Study Center, New York, NY, United States
- 21Division of Psychiatry and Applied Psychology, School of Medicine, University of Nottingham, Nottingham, United Kingdom
- 22Department of Pediatrics, Yonsei University College of Medicine, Seoul, South Korea
- 23Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy
- 24Department of Psychosis Studies, Institute of Psychiatry, Psychology & Neuroscience, King's College London, London, United Kingdom
- 25Outreach and Support in South London (OASIS) Service, South London and Maudsley NHS Foundation Trust, London, United Kingdom
The putative risk/protective factors for several personality disorders remain unclear. The vast majority of published studies has assessed personality characteristics/traits rather than disorders. Thus, the current umbrella review of meta-analyses (MAs) aims to systematically assess risk or protective factors associated with personality disorders. We searched PubMed–MEDLINE/PsycInfo databases, up to August 31, 2020. Quality of MAs was assessed with AMSTAR-2, while the credibility of evidence for each association was assessed through standard quantitative criteria. Out of 571 initial references, five meta-analyses met inclusion criteria, encompassing 56 associations of 26 potential environmental factors for antisocial, dependent, borderline personality disorder, with a median of five studies per association, and median 214 cases per association. Overall, 35 (62.5%) of the associations were nominally significant. Six associations met class II (i.e., highly suggestive) evidence for borderline personality disorder, with large effect sizes involving childhood emotional abuse (OR = 28.15, 95% CI 14.76–53.68), childhood emotional neglect (OR = 22.86, 95% CI 11.55–45.22), childhood any adversities (OR = 14.32, 95% CI 10.80–18.98), childhood physical abuse (OR = 9.30, 95% CI 6.57–13.17), childhood sexual abuse (OR = 7.95, 95% CI 6.21–10.17), and childhood physical neglect (OR = 5.73, 95% CI 3.21–10.21), plus 16 further associations supported by class IV evidence. No risk factor for antisocial or dependent personality disorder was supported by class I, II, and III, but six and seven met class IV evidence, respectively. Quality of included meta-analyses was rated as moderate in two, critically low in three. The large effect sizes found for a broad range of childhood adversities suggest that prevention of personality disorders should target childhood-related risk factors. However, larger cohort studies assessing multidimensional risk factors are needed in the field.
Introduction
Personality disorders are defined as “an enduring pattern of inner experience and behavior that deviates markedly from the expectations of the individual's culture, is pervasive and inflexible, has an onset in adolescence or early adulthood, is stable over time, and leads to distress or impairment.”
It has been reported that globally, personality disorders have a prevalence around 3 to 10% in the global population (1), and much higher in people affected by other mental disorders (2), and so it is considered a global mental health priority (3). Their peak age at onset is at age 20.5 years (4).
In the last 50 years, a lot of interest went into personality disorders, promoting their status from an unreliable and not so valid diagnosis before the 1960s, to a condition with clear diagnostic criteria in particular after introduction of DSM-III (5). Then, DSM-based criteria have raised criticism, and alternative diagnostic frameworks have been proposed (1). They are now classified differently in Diagnostic and Statistical Manual (DSM), 5th version (6) and in International Classification Diseases (ICD)-11 (7). DSM-V classifies personality disorders in three clusters (A, B, and C) and “other personality disorders.” Cluster A includes paranoid personality disorder, schizoid personality disorder, and schizotypal personality disorder; cluster B includes antisocial personality disorder, borderline personality disorder, histrionic personality disorder, and narcissistic personality disorder; cluster C includes avoidant personality disorder, dependent personality disorder, and obsessive-compulsive personality disorder (6). ICD-11 applies a different approach, with the aim to identify fewer categories, which overlap less and ultimately have greater clinical utility (1). Specifically, ICD-11 categorizes personality disorders (6D10) into mild personality disorder, moderate personality disorder, and severe personality disorder, in addition to which Prominent personality traits or patterns (6D11), namely, Negative affectivity, Detachment, Dissociality, Disinhibition, Anankastic, or Borderline pattern in personality disorder or difficulty, must be further specified (7).
Structural brain alterations, namely, bilateral gray matter reductions in concentrations in ventral cingulate gyrus, medial temporal lobe, and fronto-limbic structures, are associated with different personality disorders defined according to several versions of DSM (8–11). Beyond cross-sectional associations with phenotypes and biomarkers, several risk factors for personality disorders have also been described. An overview of systematic reviews (12) focused on systematic reviews on risk factors for personality disorders. However, it only focused on parenting style, and it also focused on qualitative reviews rather than quantitative meta-analyses (12). Also, evidence from meta-analyses is frequently biased, and the credibility of the claimed associations between putative risk or protective factors for personality disorders remains unknown. To fill this gap in the literature, we conducted an umbrella review focused on environmental risk and protective factors for personality disorders, to identify and measure possible methodological limitations and sources of bias in the published and unpublished evidence, which might have underestimated or inflated claimed associations, as previously shown in several previous umbrella reviews on risk factors for mental disorders or obesity (13–17). Therefore, the aim of this umbrella review was to grade the evidence from meta-analyses of cohort and case–control studies on protective and risk factors for personality disorders accounting for several sources of bias and applying established quantitative criteria.
Methods
This umbrella review adhered to state-of-the-art methods of previously published or planned umbrella reviews (15, 18–23), and according to the Meta-analysis of Observational Studies in Epidemiology (MOOSE) and the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) were followed in conducting and reporting this umbrella review (Supplementary Tables 1, 2) (24, 25). The study followed an a priori protocol, available on request. MS, AFC, PF-P designed the study, prepared the search key, and drafted the protocol. ED run the statistical analyses. Four investigators (MS, ED, AM, and PK, all MDs) divided into two couples independently performed literature screening and data extraction, including quality assessment of included meta-analyses.
Literature Search Strategy
We conducted a systematic search in PubMed and PsycINFO from inception to August 31, 2020. We included meta-analyses of case–control and cohort studies that assessed risk or protective factors for personality disorders, defined according to ICD or DSM, any version (6, 7, 26). The search strategy was “(personality disorder) AND meta-analysis.” No restrictions regarding year of publication, language, country, ethnicity, or any other characteristic were applied during the search process. We also hand searched references of included meta-analyses and other relevant articles. When authors did not agree regarding screening or data extraction, a third author (MS) resolved any conflict, reaching a consensus with the two authors.
Eligibility Criteria
We only included systematic reviews that also conducted a quantitative meta-analysis pooling data from case–control or cohort (either retrospective or prospective) studies reporting on environmental factors that may affect the risk of the disorders of interest, as per the ICD or DSM criteria. Specifically, we included disorders that corresponded to ICD-10 “F60 Specific personality disorders” (26) and “Personality disorder” in DSM-5 (6). Risk or protective factors of interest were deemed eligible, regardless of the direction of the association (protective or risk factor). No language restriction was applied.
Meta-analyses of studies that included other-than-human population, having a cross-sectional design, as well as focusing on genome-wide associations or on single nucleotide polymorphism were excluded. Also, systematic reviews without a quantitative meta-analytic data synthesis, narrative reviews, and commentaries/letters to the editor were not included in the present umbrella review.
Finally, if multiple meta-analyses investigated the same risk or protective factor and the same outcome, only the meta-analysis with the largest number of studies pooled to measure the association was retained.
Data Extraction
We extracted information into a standardized pre-defined template. The list of variables of interest included PMID/DOI of the included study, first author, year of publication, design of included studies (cohort, case–control), number of included studies in the meta-analysis, specific population cohort (i.e., general population, primary school, secondary school, university students, hospital sample, or a sample with a specific somatic, mental, or somatic/mental comorbid condition, etc.) as well as the reference/comparison population (i.e., no risk factor in cohort studies, no disorder in case–control studies), tools for the definition of both population and risk/protective factor (DSM, ICD, clinical records, rating scales), specific protective or risk factor, outcome (ICD or DSM code if available, or definition of specific disorders as reported by authors given inclusion criteria were met), and its risk estimate. We assessed the methodological quality of included meta-analyses as independent couples of two investigators (JD, PK, AM, and MS, all MDs) by means of the AMSTAR (A Measurement Tool to Assess Systematic Reviews) version 2 (27). If needed, we contacted authors to ask for data.
Data Analysis
For each association (i.e., between each specific risk or protective factor and personality disorder), we pooled effect sizes of individual studies reported in each meta-analysis, as well as cases developing personality disorder and total sample size, and recalculated the pooled effect sizes with its 95% CIs, using random-effects models (28). We transformed the effect sizes or modified the direction of associations reported in original publications only for the associations with continuous or correlational data (e.g., Hedges g, beta coefficients) to present comparable estimates (i.e., equivalent odds ratio—eOR) (22). Heterogeneity was measured with the I2 statistic (29). In addition, 95% prediction intervals for the effect sizes were computed to estimate the possible range in which the effect sizes of future studies were anticipated to fall (30). We also examined small-study effect bias, testing whether smaller studies generated larger effect sizes compared with larger studies (15, 18–22, 31). Specifically, as indicators of small-study effect, we used both the Egger regression asymmetry test (p ≤ 0.10) and whether the random-effects summary effect size were larger than the effect size of the largest study contributing to that association (18, 20, 21, 31). We finally measured the presence of excess significance bias by assessing whether the observed number of studies with nominally statistically significant results was different from the expected number of studies with statistically significant results (32, 33). The expected number of statistically significant studies per association was calculated by summing the statistical power estimates for each component study. The power estimates of each component study depend on the plausible effect size for the examined association, which we assumed to be the effect size of the largest study (i.e., the smallest SE) per association (33). For excess significance bias, a p ≤ 0.10 was considered statistically significant (32). All analyses were conducted in Stata/MP, version 10.0 (StataCorp LLC).
Assessment of the Credibility of Evidence, and Sensitivity Analyses
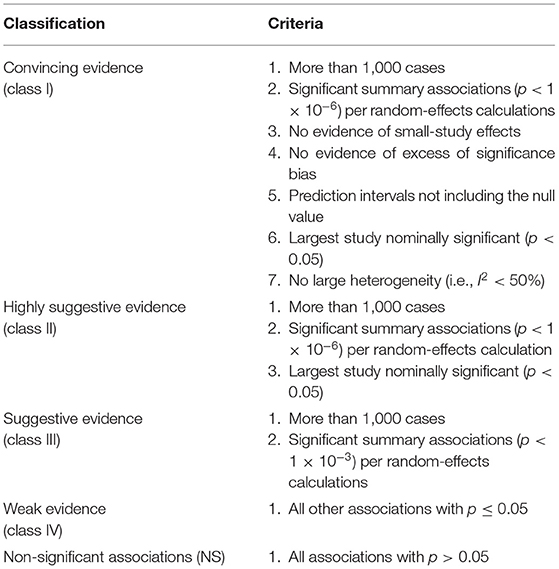
In line with former umbrella reviews (14, 16, 17, 34). eligible associations for personality disorders were classified into five levels according to the strength of the evidence of potential environmental risk/protective factors: convincing (class I), highly suggestive (class II), suggestive (class III), weak (class IV), and not significant (NS) (Table 1).
Sensitivity analyses were conducted removing the >1,000 cases criterion.
Results
Search Results
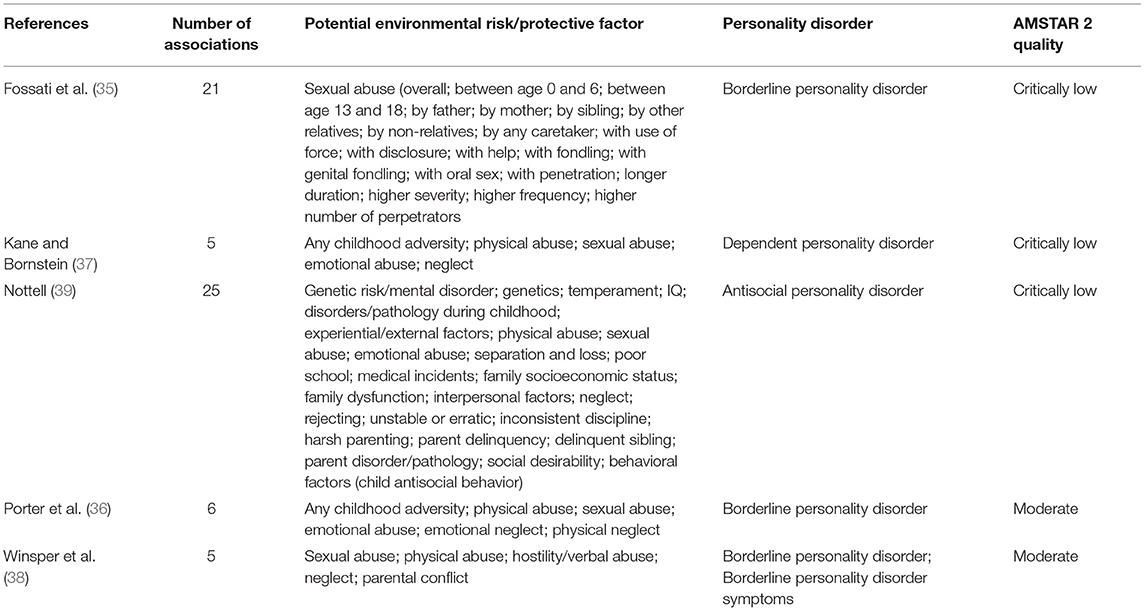
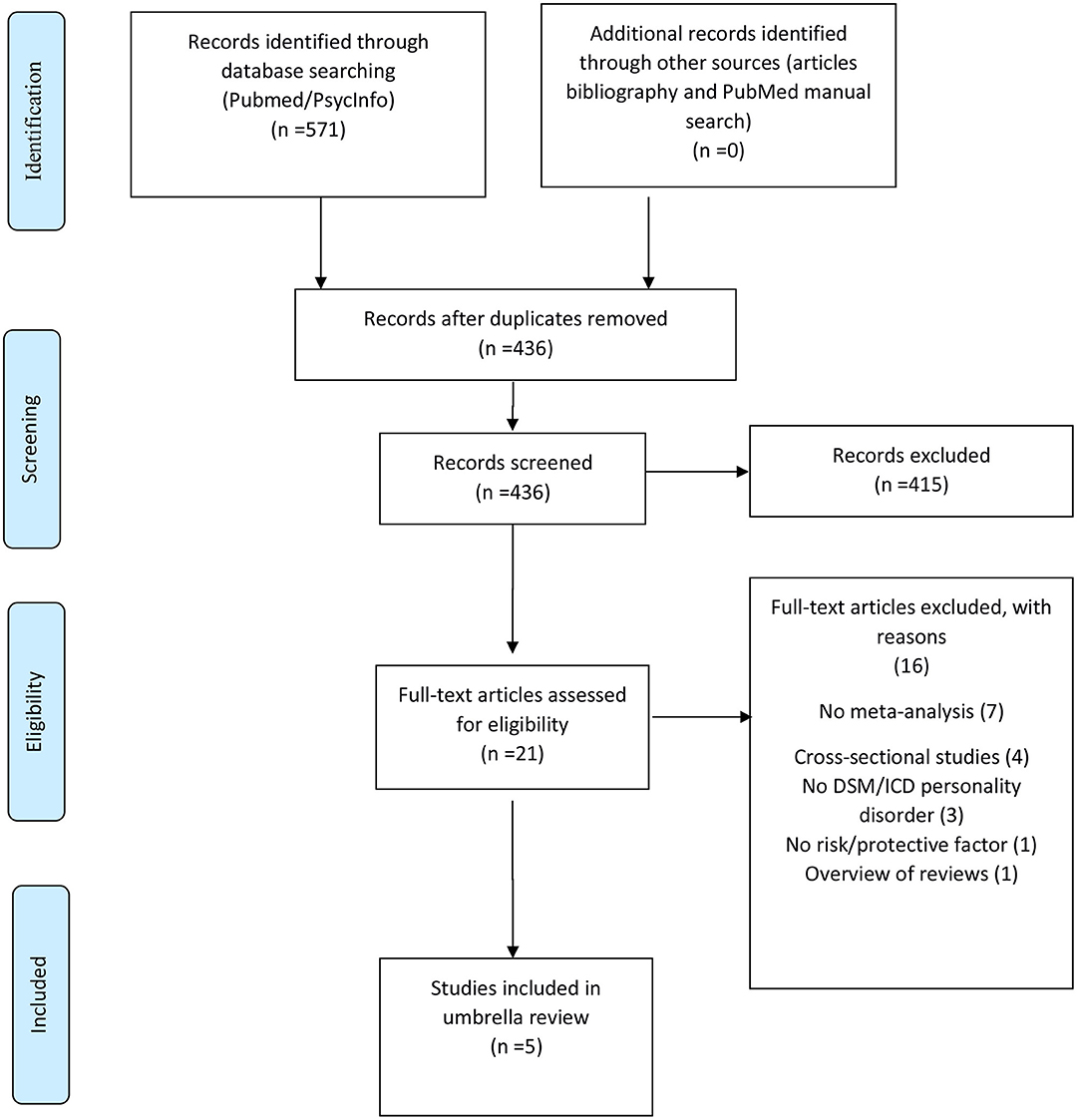
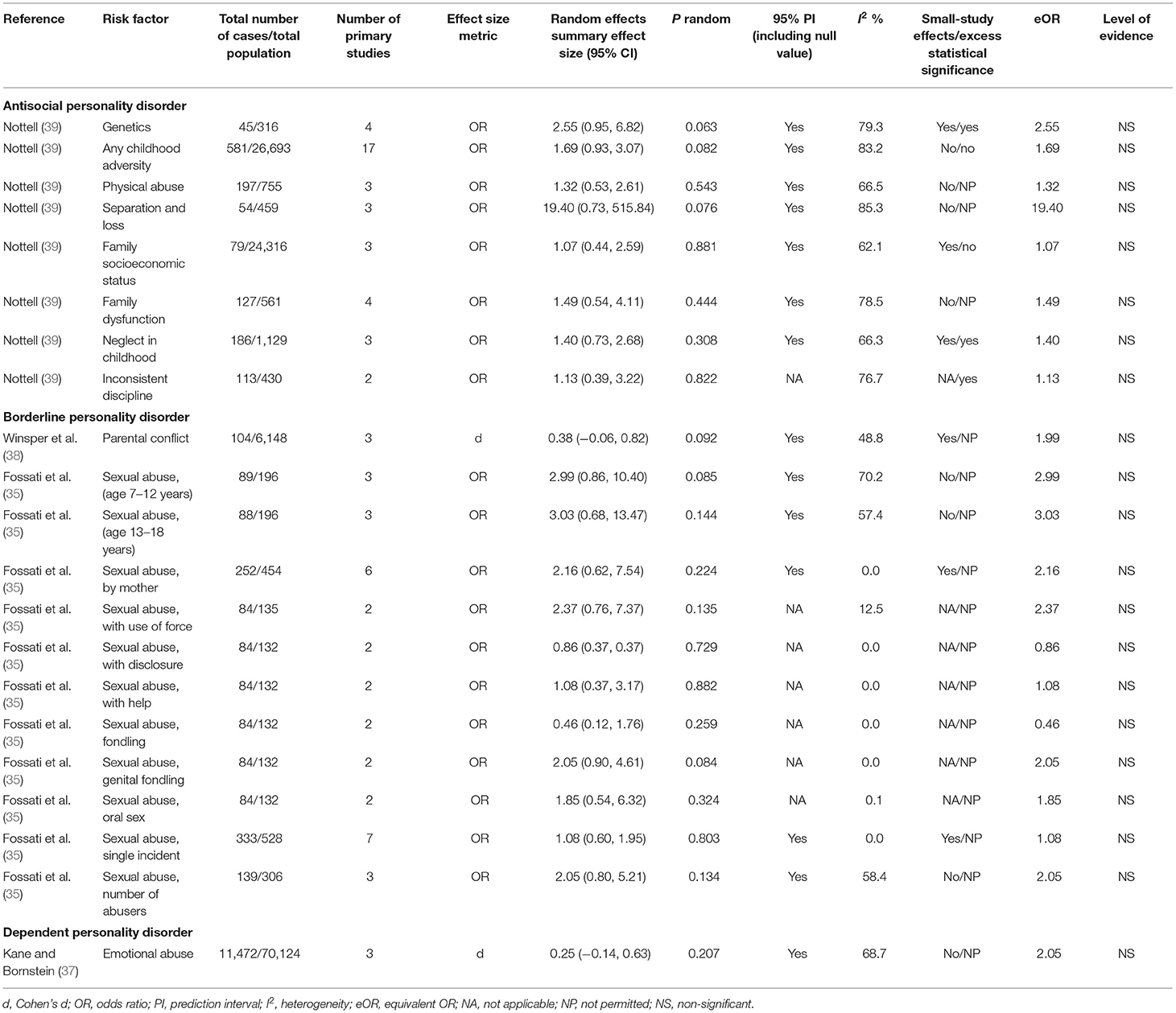
Out of 571 initial hits, 436 were assessed at title and abstract level, and 415 were excluded. The remaining 21 were assessed at full-text level, and 16 were excluded, ultimately including 5 meta-analyses. The list of excluded meta-analyses after full-text assessment, with specific reason for exclusion, is reported in online Supplementary Material. Finally, five meta-analyses were included in this umbrella review (35–39) (Table 2). The study selection flow is reported in Figure 1. The whole dataset with results from individual studies is available on reasonable request.
Descriptive Results of the Included Associations
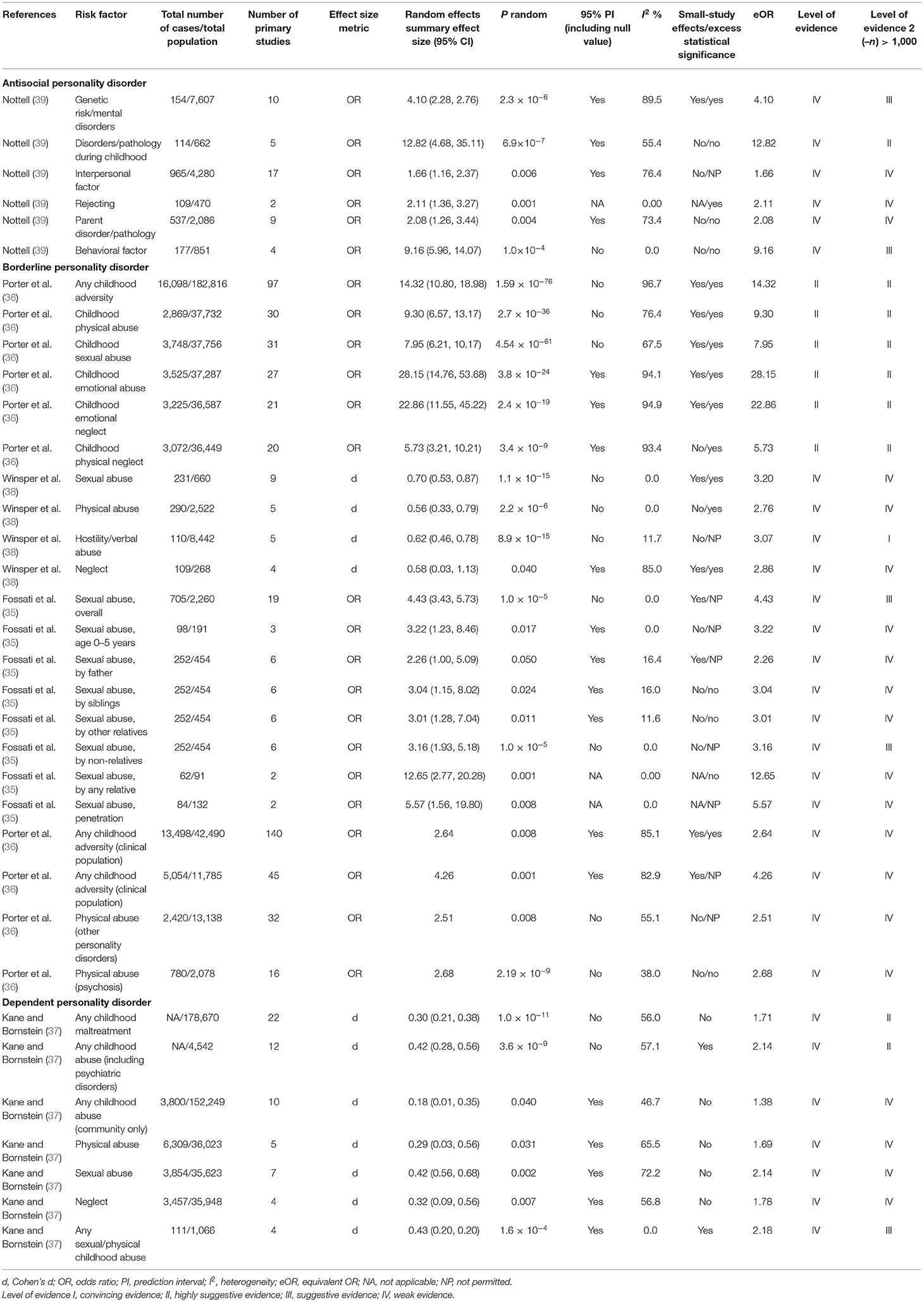
The characteristics of included studies are described in Table 2. The five eligible meta-analyses corresponded to 56 with available data for synthesis, between 26 potential putative risk/protective factors and 3 personality disorders (antisocial, borderline, and dependent personality disorder) (Tables 2, 3). The eligible meta-analyses were published between 1999 and 2020. The median number of studies per association was 5 [interquartile range (IQR) = 3–14]. The median number of cases per association was 214 (IQR = 98–2,420) and the number of cases was >1,000 in 14 associations, while in 2 associations the number of cases was not reported (Tables 3, 4). All eligible meta-analyses used summary-level data from published literature. No protective factors were identified.
Quality Assessment of Included Articles
Based on the AMSTAR2 assessment, two meta-analyses (40%) met the moderate quality level and three (60%) were of low quality (Table 2).
Summary of Associations
Thirty-five of the 56 analyzed associations (62.5%) presented a statistically significant effect (p < 0.05) under the random-effects model, but only 12 (21.4%) reached p < 10−6. Twenty-five associations (44.6%) presented a large heterogeneity (I2 > 50%), while only for 13 associations (23.2%) the 95% prediction interval did not include the null. In addition, the evidence for small-study effects and excess significance bias was noted for 20 (35.7%) and 16 (28.5%) associations, respectively.
Associations for Antisocial Personality Disorder
A total of 14 of the 56 associations examined associations for antisocial personality disorder. Six of those presented a nominally statistically significant effect (p ≤ 0.05) and met the class IV evidence criteria while only 1 association reached p < 10−6. None of those associations were supported by class I, II, and III evidence. After excluding the criterion of 1,000 cases, one factor, namely, disorders/pathology during childhood, was upgraded to the class II evidence while two others, namely, psychobiological factor and behavioral factor, were upgraded to the class III evidence (Tables 3, 4).
Associations for Borderline Personality Disorder
A total of 22 of the 56 associations examined associations for borderline personality disorder. Twenty-two of those presented a nominally statistically significant effect (p ≤ 0.05), while nine of those associations reached p < 10−6. None of those associations were supported by class I or III evidence (Table 3). Six associations were supported by class II evidence (Table 3) involving childhood emotional abuse, childhood emotional neglect, childhood any adversities, childhood physical abuse, childhood sexual abuse, and childhood physical neglect. Sixteen other associations were supported by class IV evidence (Table 3) and 12 were non-significant (Table 4). After excluding the criterion of 1,000 cases, all factors with class II evidence remained at the same level while two others, namely, sexual abuse overall and sexual abuse by non-relatives, were upgraded to the class III evidence.
Associations for Dependent Personality Disorder
A total of 8 of the 56 associations examined associations for dependent personality disorder. Seven of those presented a nominally statistically significant effect (p ≤ 0.05) and met the class IV evidence criteria while only two associations reached p < 10−6. None of those associations were supported by class I, II, and III evidence. After excluding the criterion of 1,000 cases, two factors, namely, any childhood maltreatment and any childhood abuse in other clinical populations, were upgraded to the class II evidence, while another one, namely, any childhood abuse vs. no childhood abuse, was upgraded to the class III evidence (Tables 3, 4).
Discussion
This is the first umbrella review pooling data from five meta-analyses on risk factors for personality disorders. Findings show that out of 56 associations between 26 potential environmental factors and antisocial, dependent, borderline personality disorder, despite 35 (62.5%) of the associations were nominally significant, only 6 (8.92%) associations met class II evidence for borderline personality disorder, involving childhood emotional abuse, childhood emotional neglect, childhood any adversities, childhood physical abuse, childhood sexual abuse, and childhood physical neglect. All other significant associations were classified as weak (class IV evidence).
These results likely reflect the epidemiological distribution of borderline personality disorders, which represents the most common personality disorders both in clinical populations (36) and in the young general population, with a lifetime prevalence cumulating to about 10% in university students (40). The relatively high prevalence of this condition is likely to have facilitated etiopathological research in this field and, consequently, accumulation of established evidence, reviewed in the current study. At the same time, it is also the most reliable diagnosis within personality disorders, with superior diagnostic reliability (Kappa 0.54) compared with other personality disorders, and similar diagnostic reliability to that observed in bipolar I disorders (0.56) or schizophrenia (0.46) (41). Given the severe individual and societal burden and impact of borderline personality disorder and the limited effect of psychological interventions (42), knowledge into risk factors associated with this condition may advance clinical care. The findings that childhood emotional abuse, emotional/physical neglect, physical/sexual abuse, and adversities in general emerge as robust risk factor for this condition align with multiple salient clinical features such as affect instability, emotion regulation difficulties, and maladaptive coping strategies including substance misuse and frequent self-harm (43, 44). Indeed, it has been suggested that several core experiences of borderline personality disorders may be understood as complex post-traumatic stress disorders (45). The current finding that individuals with a diagnosis of borderline personality disorders are consistently more likely to report childhood adversity than non-clinical controls is consistent with this strong clinical narrative linking childhood adversity and this condition, and show that evidence survives several stringent additional criteria making it into class II. Furthermore, the magnitude of these associations appeared as very large, with ORs superior to 5 in all cases: emotional abuse, 28.15; emotional neglect, OR 22.86; adversities, OR 14.32; physical abuse, OR 9.30; sexual abuse, OR 7.95; physical neglect, OR 5.73. Although it is important to note that these ORs relate to case–control studies not surviving prospective analyses, their large magnitude holds clinical relevance. For example, these findings indicate that childhood trauma should be systematically ascertained during the diagnostic assessment of suspected cases or during their initial clinical management. Notably, these ORs were not controlled against each other, albeit being likely correlated. The next generation of research should then develop a multivariable assessment interview to collect these multiple exposures in the same individuals assessed for a potential borderline personality disorder, thus allowing multivariable association analyses, yet accounting for multicollinearity of different risk factors. Another future development of research may involve exploring the transdiagnosticity of childhood trauma as potential risk factor for other mental disorders such as eating disorders, depressive disorders, anxiety disorders, and even psychotic disorders. These considerations are particularly relevant in the context of potential screening (46) and preventive interventions (47, 48) and mental health promotion initiatives (49, 50), because it could potentially be possible to target multiple outcomes/mental disorders by reducing childhood trauma.
Interestingly, childhood trauma exposure has been linked with neurobiological modifications in personality disorders, particularly borderline personality disorder. For example, variations in volumes of the main brain regions involved in BPD (especially amygdala and hippocampus) have been associated to adverse childhood experiences and trauma exposure (51–54). Also, there is evidence of an association between childhood trauma and alterations of the cortisol circadian rhythm and levels, indicating a deregulation of the HPA axis responsiveness, which could also affect hippocampal volumes (51, 55, 56). Yet, such alterations are not exclusively present in BPD, as well as childhood traumatic events are risk factors for other mental disorders (57), including dependent personality disorder. Hence, the specific component justifying such a high association between BPD and childhood adversities remains unknown.
The present work also has several limitations. First, none of the findings met class I evidence. However, this is due to the available evidence. Indeed, findings inform the field that more cohort studies assessing multidimensional risk factors for personality disorders are needed. Similarly, the lack of evidence on protective factors is also due to lack of eligible meta-analyses reporting on protective factors. Second, compared with umbrella reviews assessing credibility of evidence on risk factors for other mental or physical disorders (14–17, 58, 59), we included a limited number of meta-analyses. Again, this indicates that more research efforts should focus on this clinically relevant field. Third, despite the large ORs, carefully designed longitudinal research, including examination of dose–response relationships, is required before definitive conclusions can be drawn regarding any causal role played by childhood adversity in the development of borderline personality disorders.
In conclusion, this umbrella review shows that risk factors for borderline personality disorder occur during childhood, and primary prevention strategies should encompass a multidisciplinary mental health promotion activity going beyond health professionals, to protect children from any maltreatment, neglect, or abuse. Risk factors for other personality disorders have been poorly identified so far, and more longitudinal studies should be conducted to inform prevention strategies.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, upon request.
Author Contributions
AFC, MS, PF-P, and ED designed the study. GC, PK, ED, and MS, extracted the data. ED run the analyses. MS and ED drafted the first version of the manuscript. All authors contributed to the manuscript, revised it, and approved the final version and protocol.
Conflict of Interest
MS received fee/honoraria from Angelini, Lundbeck. SC declares honoraria and reimbursement for travel and accommodation expenses for lectures from the following non-profit associations: Association for Child and Adolescent Central Health (ACAMH), Canadian ADHD Alliance Resource (CADDRA), British Association of Pharmacology (BAP), and from Healthcare Convention for educational activity on ADHD. PF-P has received research fees from Lundbeck and honoraria from Lundbeck, Angelini, Menarini, and Boehringer Ingelheim outside the current study.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.679379/full#supplementary-material
References
1. Tyrer P, Mulder R, Crawford M, Newton-Howes G, Simonsen E, Ndetei D, et al. Personality disorder: a new global perspective. World Psychiatry. (2010) 9:56–60. doi: 10.1002/j.2051-5545.2010.tb00270.x
2. Newton-Howes G, Tyrer P, Anagnostakis K, Cooper S, Bowden-Jones O, Weaver T. The prevalence of personality disorder, its comorbidity with mental state disorders, and its clinical significance in community mental health teams. Soc Psychiatry Psychiatr Epidemiol. (2010) 45:453–60. doi: 10.1007/s00127-009-0084-7
3. Grenyer BFS, Ng FYY, Townsend ML, Rao S. Personality disorder: a mental health priority area. Aust New Zeal J Psychiatry. (2017) 51:872–5. doi: 10.1177/0004867417717798
4. Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. (2021). doi: 10.1038/s41380-021-01161-7 [Epub ahead of print].
5. KENDELL RE. Diagnostic and statistical manual of mental disorders, 3rd ed., revised (DSM-III-R). Am J Psychiatry. (1988) 145:1301–2. doi: 10.1176/ajp.145.10.1301
6. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-V). Washington, DC: American Psychiatric Association (2013). doi: 10.1176/appi.books.9780890425596
7. WHO. International Classification of Diseases−11 (ICD-11), Version: 2020. (2019) Available online at: https://icd.who.int/browse11/l-m/en
8. Soloff P, Nutche J, Goradia D, Diwadkar V. Structural brain abnormalities in borderline personality disorder: a voxel-based morphometry study. Psychiatry Res. (2008) 164:223–36. doi: 10.1016/j.pscychresns.2008.02.003
9. Tebartz van Elst L, Hesslinger B, Thiel T, Geiger E, Haegele K, Lemieux L, et al. Frontolimbic brain abnormalities in patients with borderline personality disorder: a volumetric magnetic resonance imaging study. Biol Psychiatry. (2003) 54:163–71. doi: 10.1016/S0006-3223(02)01743-2
10. Dickey CC, McCarley RW, Voglmaier MM, Niznikiewicz MA, Seidman LJ, Hirayasu Y, et al. Schizotypal personality disorder and MRI abnormalities of temporal lobe gray matter. Biol Psychiatry. (1999) 45:1393–402. doi: 10.1016/S0006-3223(99)00030-X
11. Nunes PM, Wenzel A, Borges KT, Porto CR, Caminha RM, De Oliveira IR. Volumes of the hippocampus and amygdala in patients with borderline personality disorder: a meta-analysis. J Pers Disord. (2009) 23:333–45. doi: 10.1521/pedi.2009.23.4.333
12. Steele KR, Townsend ML, Grenyer BFS. Parenting and personality disorder: an overview and meta-synthesis of systematic reviews. PLoS ONE. (2019) 14:e0223038. doi: 10.1371/journal.pone.0223038
13. Solmi M, Radua J, Stubbs B, Ricca V, Moretti D, Busatta D, et al. Risk factors for eating disorders: an umbrella review of published meta-analyses. Braz J Psychiatry. (2020) 314–23. doi: 10.1590/1516-4446-2020-1099
14. Köhler CA, Evangelou E, St B, Solmi M, Veronese N, Belbasis L, et al. Mapping risk factors for depression across the lifespan: an umbrella review of evidence from meta-analyses and mendelian randomization studies. J Psychiatr Res. (2018) 103:189–207. doi: 10.1016/j.jpsychires.2018.05.020
15. Kim JY, Son MJ, Son CY, Radua J, Eisenhut M, Gressier F, et al. Environmental risk factors and biomarkers for autism spectrum disorder: an umbrella review of the evidence. Lancet Psychiatry. (2019) 6:590–600. doi: 10.1016/S2215-0366(19)30181-6
16. Bortolato B, Köhler CA, Evangelou E, León-Caballero J, Solmi M, Stubbs B, et al. Systematic assessment of environmental risk factors for bipolar disorder: an umbrella review of systematic reviews and meta-analyses. Bipolar Disord. (2017) 19:84–96. doi: 10.1111/bdi.12490
17. Solmi M, Köhler CA, Stubbs B, Koyanagi A, Bortolato B, Monaco F, et al. Environmental risk factors and nonpharmacological and nonsurgical interventions for obesity: an umbrella review of meta-analyses of cohort studies and randomized controlled trials. Eur J Clin Invest. (2018) 48:e12982. doi: 10.1111/eci.12982
18. Dragioti E, Solmi M, Favaro A, Fusar-Poli P, Dazzan P, Thompson T, et al. Association of antidepressant use with adverse health outcomes: a systematic umbrella review. JAMA Psychiatry. (2019) 76:1241–55. doi: 10.1001/jamapsychiatry.2019.2859
19. Dragioti E, Karathanos V, Gerdle B, Evangelou E. Does psychotherapy work? An umbrella review of meta-analyses of randomized controlled trials. Acta Psychiatr Scand. (2017) 136:236–46. doi: 10.1111/acps.12713
20. Bellou V, Belbasis L, Tzoulaki I, Middleton LT, Ioannidis JPA, Evangelou E. Systematic evaluation of the associations between environmental risk factors and dementia: an umbrella review of systematic reviews and meta-analyses. Alzheimers Dement. (2017) 13:406–18. doi: 10.1016/j.jalz.2016.07.152
21. Belbasis L, Bellou V, Evangelou E, Ioannidis JPA, Tzoulaki I. Environmental risk factors and multiple sclerosis: an umbrella review of systematic reviews and meta-analyses. Lancet Neurol. (2015) 14:263–73. doi: 10.1016/S1474-4422(14)70267-4
22. Radua J, Ramella-Cravaro V, Ioannidis JPA, Reichenberg A, Phiphopthatsanee N, Amir T, et al. What causes psychosis? An umbrella review of risk and protective factors. World Psychiatry. (2018) 17:49–66. doi: 10.1002/wps.20490
23. Cortese S, Solmi M, Arrondo G, Cipriani A, Fusar-Poli P, Larsson H, et al. Association between mental disorders and somatic conditions: protocol for an umbrella review. Evid Based Ment Health. (2020) 23:135–39. doi: 10.1136/ebmental-2020-300158
24. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. J Am Med Assoc. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
25. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. (2009) 62:1006–12. doi: 10.1016/j.jclinepi.2009.06.005
26. WHO. International Classification of Diseases - 10 (ICD-10). Version: 2019. Available online at: https://icd.who.int/browse10/2019/en
27. Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. (2017) 358:j4008. doi: 10.1136/bmj.j4008
28. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. (1986) 7:177–88. doi: 10.1016/0197-2456(86)90046-2
29. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
30. Riley RD, Higgins JPT, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. (2011) 342:964–7. doi: 10.1136/bmj.d549
31. Dragioti E, Evangelou E, Larsson B, Gerdle B. Effectiveness of multidisciplinary programmes for clinical pain conditions: an umbrella review. J Rehabil Med. (2018) 50:779–91. doi: 10.2340/16501977-2377
32. Ioannidis JPA, Trikalinos TA. An exploratory test for an excess of significant findings. Clin Trials. (2007) 4:245–53. doi: 10.1177/1740774507079441
33. Ioannidis JPA. Clarifications on the application and interpretation of the test for excess significance and its extensions. J Math Psychol. (2013) 57:184–7. doi: 10.1016/j.jmp.2013.03.002
34. Papola D, Ostuzzi G, Gastaldon C, Morgano GP, Dragioti E, Carvalho AF, et al. Antipsychotic use and risk of life-threatening medical events: umbrella review of observational studies. Acta Psychiatr Scand. (2019) 140:227–43. doi: 10.1111/acps.13066
35. Fossati A, Madeddu F, Maffei C. Borderline personality disorder and childhood sexual abuse: a meta-analytic study. J Pers Disord. (1999) 13 3:268–80. doi: 10.1521/pedi.1999.13.3.268
36. Porter C, Palmier-Claus J, Branitsky A, Mansell W, Warwick H, Varese F. Childhood adversity and borderline personality disorder: a meta-analysis. Acta Psychiatr Scand. (2020) 141:6–20. doi: 10.1111/acps.13118
37. Kane FA, Bornstein RF. Unhealthy dependency in victims and perpetrators of child maltreatment: a meta-analytic review. J Clin Psychol. (2018) 74:867–82. doi: 10.1002/jclp.22550
38. Winsper C, Lereya ST, Marwaha S, Thompson A, Eyden J, Singh SP. The aetiological and psychopathological validity of borderline personality disorder in youth: a systematic review and meta-analysis. Clin Psychol Rev. (2016) 44:13–24. doi: 10.1016/j.cpr.2015.12.001
39. Nottell AN. Childhood indicators of developing anti-social personality disorder: a meta-analysis of published research (Unpublished doctoral thesis). Calgary, AB: University of Calgary (2001). doi: 10.11575/PRISM/15336
40. Meaney R, Hasking P, Reupert A. Prevalence of borderline personality disorder in university samples: systematic review, meta-analysis and meta-regression. PLoS ONE. (2016) 11:e0155439. doi: 10.1371/journal.pone.0155439
41. Freedman R, Lewis DA, Michels R, Pine DS, Schultz SK, Tamminga CA, et al. The initial field trials of DSM-5: new blooms and old thorns. Am J Psychiatry. (2013) 170:1–5. doi: 10.1176/appi.ajp.2012.12091189
42. Cristea IA, Gentili C, Cotet CD, Palomba D, Barbui C, Cuijpers P. Efficacy of psychotherapies for borderline personality disorder: a systematic review and meta-analysis. JAMA Psychiatry. (2017) 74:319–28. doi: 10.1001/jamapsychiatry.2016.4287
43. Herzog JI, Schmahl C. Adverse childhood experiences and the consequences on neurobiological, psychosocial, and somatic conditions across the lifespan. Front Psychiatry. (2018) 9:420. doi: 10.3389/fpsyt.2018.00420
44. Liu RT, Scopelliti KM, Pittman SK, Zamora AS. Childhood maltreatment and non-suicidal self-injury: a systematic review and meta-analysis. Lancet Psychiatry. (2018) 5:51–64. doi: 10.1016/S2215-0366(17)30469-8
45. Ford JD, Courtois CA. Complex PTSD, affect dysregulation, and borderline personality disorder. Borderline Personal Disord Emot Dysregul. (2014) 1:9. doi: 10.1186/2051-6673-1-9
46. Gordon JB, Nemeroff CB, Felitti V. Screening for adverse childhood experiences. JAMA. (2020) 324:1789. doi: 10.1001/jama.2020.16449
47. Ghastine L, Kerlek AJ, Kopechek JA. Childhood sexual abuse: a call to action in pediatric primary care. Pediatrics. (2020) 146:e20193327. doi: 10.1542/peds.2019-3327
48. Ashraf IJ, Pekarsky AR, Race JE, Botash AS. Making the most of clinical encounters: prevention of child abuse and maltreatment. Pediatr Clin North Am. (2020) 67:481–98. doi: 10.1016/j.pcl.2020.02.004
49. Salazar de Pablo G, De Micheli A, Nieman DH, Correll CU, Kessing LV, Pfennig A, et al. Universal and selective interventions to promote good mental health in young people: systematic review and meta-analysis. Eur Neuropsychopharmacol J Eur Coll Neuropsychopharmacol. (2020) 41:28–39. doi: 10.1016/j.euroneuro.2020.10.007
50. Fusar-Poli P, Salazar de Pablo G, De Micheli A, Nieman DH, Correll CU, Kessing LV, et al. What is good mental health? A scoping review. Eur Neuropsychopharmacol. (2019) 31:33–46. doi: 10.1016/j.euroneuro.2019.12.105
51. Cattane N, Rossi R, Lanfredi M, Cattaneo A. Borderline personality disorder and childhood trauma: exploring the affected biological systems and mechanisms. BMC Psychiatry. (2017) 17:221. doi: 10.1186/s12888-017-1383-2
52. Bilek E, Itz ML, Stößel G, Ma R, Berhe O, Clement L, et al. Deficient amygdala habituation to threatening stimuli in borderline personality disorder relates to adverse childhood experiences. Biol Psychiatry. (2019) 86:930–8. doi: 10.1016/j.biopsych.2019.06.008
53. Weniger G, Lange C, Sachsse U, Irle E. Reduced amygdala and hippocampus size in trauma-exposed women with borderline personality disorder and without posttraumatic stress disorder. J Psychiatry Neurosci. (2009) 34:383–8.
54. Bounoua N, Miglin R, Spielberg JM, Johnson CL, Sadeh N. Childhood trauma moderates morphometric associations between orbitofrontal cortex and amygdala: implications for pathological personality traits. Psychol Med. (2020). doi: 10.1017/S0033291720004468.[Epub ahead of print].
55. Bourvis N, Aouidad A, Cabelguen C, Cohen D, Xavier J. How do stress exposure and stress regulation relate to borderline personality disorder? Front Psychol. (2017) 8:2054. doi: 10.3389/fpsyg.2017.02054
56. Ruocco AC, Carcone D. A neurobiological model of borderline personality disorder: systematic and integrative review. Harv Rev Psychiatry. (2016) 24:311–29. doi: 10.1097/HRP.0000000000000123
57. Arango C, Dragioti E, Solmi M, Cortese S, Domschke K, Murray R, et al. Evidence-based atlas of risk and protective factors of mental disorders: meta-umbrella review. World Psychiatry. (2021). [Epub ahead of print].
58. Fullana M, Tortella-Feliu M, Fernández de la Cruz L, Chamorro J, Pérez-Vigil A, Ioannidis J, et al. Risk and protective factors for anxiety and obsessive-compulsive disorders: An umbrella review of systematic reviews and meta-analyses. Psychol Med. (2020) 50:1300–15. doi: 10.1017/S0033291719001247
Keywords: umbrella review, personality disorder, prevention, meta-analysis, risk factor, systematic review, psychiatry, mental health
Citation: Solmi M, Dragioti E, Croatto G, Radua J, Borgwardt S, Carvalho AF, Demurtas J, Mosina A, Kurotschka P, Thompson T, Cortese S, Shin JI and Fusar-Poli P (2021) Risk and Protective Factors for Personality Disorders: An Umbrella Review of Published Meta-Analyses of Case–Control and Cohort Studies. Front. Psychiatry 12:679379. doi: 10.3389/fpsyt.2021.679379
Received: 11 March 2021; Accepted: 06 July 2021;
Published: 06 September 2021.
Edited by:
Sara Calderoni, Fondazione Stella Maris (IRCCS), ItalyReviewed by:
Michael Gordon, Monash Health, AustraliaMichele Fornaro, New York State Psychiatric Institute (NYSPI), United States
Copyright © 2021 Solmi, Dragioti, Croatto, Radua, Borgwardt, Carvalho, Demurtas, Mosina, Kurotschka, Thompson, Cortese, Shin and Fusar-Poli. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marco Solmi, TWFyY28uc29sbWk4M0BnbWFpbC5jb20=; Jae Il Shin, U0hJTkpJQHl1aHMuYWM=
†These authors share first authorship
‡ORCID: Peter Kurotschka, orcid.org/0000-0003-3750-6147
 Marco Solmi
Marco Solmi Elena Dragioti
Elena Dragioti Giovanni Croatto7
Giovanni Croatto7 Joaquim Radua
Joaquim Radua Stefan Borgwardt
Stefan Borgwardt Andre F. Carvalho
Andre F. Carvalho Jacopo Demurtas
Jacopo Demurtas Anna Mosina
Anna Mosina Peter Kurotschka
Peter Kurotschka Samuele Cortese
Samuele Cortese Jae Il Shin
Jae Il Shin Paolo Fusar-Poli
Paolo Fusar-Poli