- Department of Primary Care & Mental Health, Institute of Population Health, University of Liverpool, Liverpool, United Kingdom
Background: Current diagnostic systems of mental disorders are criticized for their poor validity and reliability, owing to the within disorder heterogeneity and between disorder homogeneity. The issue is important if treatments for mental disorders are to be tailored to individual needs. There is little information in this area on perinatal depression (PND), a highly prevalent condition globally.
Aims: i) Quantify heterogeneity attributable to the polythetic diagnostic framework for PND and, ii) present evidence for the effectiveness of a multicomponent and low-intensity cognitive behavioral Thinking Healthy Programme (THP) across the heterogeneous presentations of PND.
Methods: This investigation presents secondary analyses of a cluster randomized controlled trial, conducted in Kallar Syedan, Pakistan. A total of 903 pregnant women were randomized to an intervention group receiving the THP intervention or control group receiving enhanced usual care. Principal component analyses and clustering algorithm were utilized to identify heterogenous subtypes of PND. Linear mixed effects models were used to assess effectiveness of the intervention across the identified subtypes of PND.
Results: Four different clusters of PND were identified: mixed anxiety-depression, somatic depression, mild depression, and atypical depression. All clinical phenotypes responded well to the THP intervention. Compared to their counterparts in the control group, mothers with mild depression in the treatment group yielded lowest risk ratios 0.24 (95% CI: 0.15 to 0.37), followed by mothers with anxiety-depression 0.50 (95% CI: 0.37 to 0.68), atypical depression 0.51 (95% CI: 0.27 to 0.99) and somatic depression 0.59 (95% CI: 0.42 to 0.83).
Conclusion: The Thinking Healthy Programme was found to be effective in reducing severity of depressive symptoms and disability across the four subtypes of PND.
Background
Perinatal Depression
While research trends in quantifying heterogeneity in mental disorders have gained momentum, knowledge gaps exist in perinatal psychiatry. The present investigation thus, aims to explore heterogeneity in perinatal depression (PND). PND is a prevalent and debilitating common mental disorder associated with pregnancy and child-birth. Although common worldwide, women living in low- and middle-income countries such as Pakistan report a higher preponderance toward the condition (1, 2). The high prevalence of PND is associated with deleterious effects on psychosocial functioning of the mothers and child development (1, 3). Previous PND literature has shown that the PND is a complex disorder with a biopsychosocial etiology, compounded by social risk factors including stressful birthing experiences and role transition to motherhood (2). Limited research on biological underpinning of PND shows dysregulation of Hypothalamic Pituitary Adrenal (HPA) axis, oxytocin system, inflammatory response, neuronal differentiation and circadian rhythms (4, 5).
Heterogeneity in Perinatal Depression
Symptom-wise, PND presentation is idiosyncratic with a complex and yet poorly understood gene-environment interaction (6). This complex nature of PND is likely to result in a highly heterogeneous disorder, with varying onset, longitudinal trajectory, and symptom configuration (6). This variability in PND among women may hamper the assessment and diagnosis of this condition, and result in variable response to prevention and treatment strategies. Therefore, an understanding of the heterogeneity for PND ought to be emphasized for development of personalized prevention and treatment. Despite this recognition, there has been little research on this aspect of PND, with previous literature targeted on major depressive disorder.
With the recent advent of powerful statistical and machine learning procedures, it has become possible to study the heterogeneous nature of PND (6–8). Traditionally, the categorical conceptualization of mental disorders was done clinically, as evident in the Diagnostic & Statistical Manual and the International Classification of Diseases. This approach was also evident in the field of psychometrics, where a mental disorder was assessed as a latent construct based on a constellation of symptoms (9). This was usually done using a variety of rating scales that classify depression as a categorical diagnosis (yes/no) or symptom severity levels (mild/moderate/severe) (10–12). Although these approaches have improved our understanding of mental disorders especially depression, these problematic assumptions have limited it as an essentially homogenous disorder, hampering our understanding of causation and mechanistic mediational pathways (13). The limited understanding of the condition might also translate to a lack of efficacious and tailored interventions that work across specific contexts. Epidemiological, genetic and intervention studies rely on psychiatric diagnoses, which, if inadequate, might lead to erroneous conclusions (9, 14, 15).
Objectives of the Study
Unfortunately, while the evidence for the differences in MDD subtypes is available, it is virtually non-existent for PND, a subtype of depression associated with pregnancy. This subtype of depression has been identified by the DSM and ICD as an individual identity and PND is a distinct condition with a different pathophysiology when compared with MDD among other study populations (12). Therefore, this study explores two research objectives:
a) Present evidence pertaining to heterogeneous combination/constellation of PND symptoms among perinatal women in Pakistan and explore subtypes of PND, driven from exploratory analyses and unsupervised machine learning techniques.
b) Present evidence pertaining to effectiveness of the multicomponent Thinking Healthy Programme across the newly identified subtypes of PND.
Methods
Study Design
The present investigation uses data from the baseline assessments of a large-scale cluster randomized controlled trial (cRCT) assessing the effectiveness of a cognitive behavior therapy-based intervention by community health workers for perinatal depression (16). Briefly, this cRCT was conducted in two rural subdistricts of rural Punjab: Gujar Khan and Kallar Syedan, with a combined population of about 750,000 people, and comprising of 40 union councils (administrative units). The union councils also served as the cluster unit of randomization. These rural areas are geographically, ethnically, and socioeconomically homogenous and comprise primarily of low to lower middle class rural households.
Both subdistricts are served by basic health units (BHU) that deliver primary healthcare to the residents. In addition to doctor and a midwife, each BHU is also staffed by 15 to 20 lady health workers. These women are community health workers that provide preventive maternal and child health services in the area. For data collection and delivery of intervention, LHWs in each union council were trained in conduct of baseline and follow up assessments as well as delivery agents. Further details on the study design of the cRCT have been reported in the primary publication (16). Ethical approval for the original randomized controlled trial was granted by the University of Manchester, UK and the Institute of Psychiatry, Rawalpindi, Pakistan. The present secondary analyses, however, were exempt from ethical review. Informed verbal and written consent were taken the participants, who were assured anonymity and that only group level findings will be reported.
For recruitment, LHWs in their union councils invited eligible participants identified using a central official register maintained at each BHU. Study participants were pregnant women in their third trimester, aged 16 to 45 years and married. Exclusion criteria included diagnosis of a serious medical condition, physical or learning disability or severe psychiatric illnesses. The baseline assessments were conducted by two experienced psychiatrists, from April 2005 to March 2006. Using the structured clinical interview for Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV diagnosis of perinatal depression, all eligible women fulfilling the criteria of PND were recruited in the trial. Post-intervention and follow up assessments were conducted at 6 months and 12 months, respectively (17). Thereafter, long term follow-up was conducted for the mother-child dyads when the index child was 7 years old.
Intervention
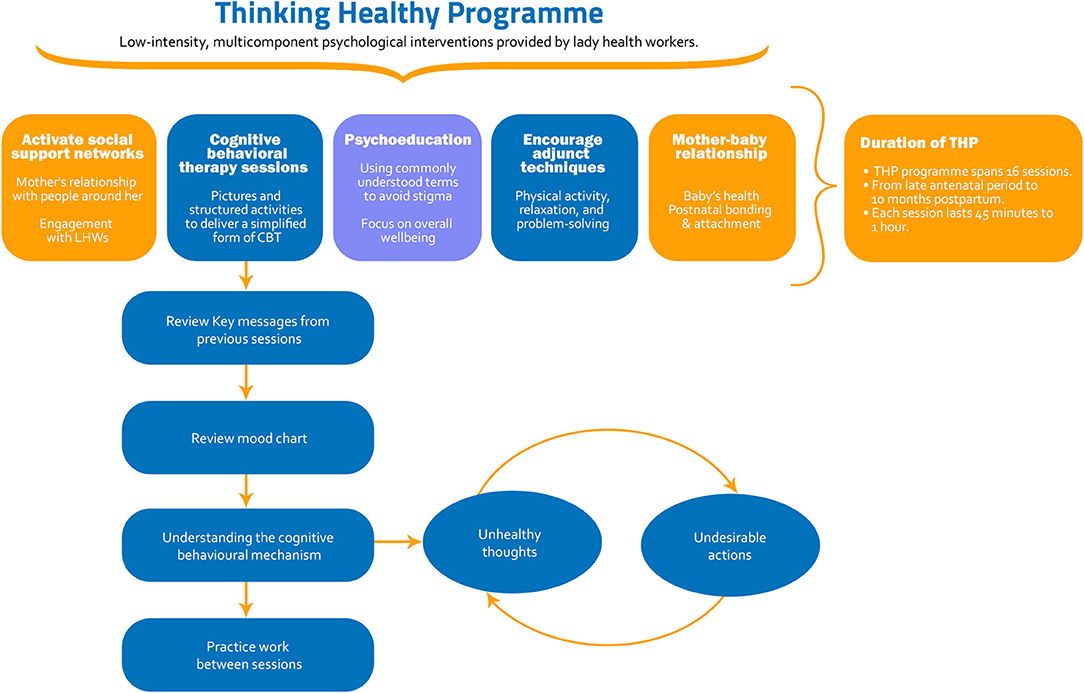
Thinking Healthy Programme (THP) is a multicomponent cognitive behavioral therapy based intervention that was designed primarily as a task shifted intervention (18). The standard THP is an evidence-based manualised intervention targeting women with perinatal depression in low socioeconomic settings (18). It aims to improve health outcomes among mothers and their children through the adaptation and integration of Cognitive Behavior Therapy (CBT) techniques into the routine work of LHWs (18). Non-specific techniques include active listening, psychoeducation and fostering social support from key family members to support the mother in negotiating the challenges she faces. Owing to its effectiveness and ease of delivery, it was recommended by the World Health Organization as a model intervention and included in the Mental Health GAP Action Programme (mhGAP) (19) for scaling up of mental health services around the world. THP trains non-specialist delivery agents in several evidence-based strategies to improve symptoms of perinatal depression.
The CBT techniques include challenging unhelpful thoughts, behavioral activation, and problem solving. It includes cognitive behavioral therapy sessions delivered in a simplified form through pictures, illustrations, and activities. The THP illustrates the use of CBT strategies in three simplified steps. By employing guided discovery technique, LHWs use culturally appropriate figures and illustrations to educate the intervention recipients about maladaptive thinking styles and ways to identify them. Intervention recipients are educated about strategies to replace maladaptive thoughts and use alternative healthy strategies. Thereafter, they are educated about the link between thoughts and actions. They are further taught the use of health calendar to monitor their thoughts and behaviors to practice healthy thinking.
All modules further provide psychoeducation to mothers using commonly used terms for mental health to avoid stigma. It also aims to improve mothers' social support networks by teaching them strategies to identify and acquire social support from people around her and encourages engagement with delivery agents. Finally, advice on mother-baby relationship and practical activities aim to improve postnatal bonding and physical health and nutrition of the baby. It also encourages adjunct techniques such as physical activity, relaxation and problem solving (20). The intervention thus aims to improve maternal well-being, mother-infant interaction and relationship with key family members including spouses. The intervention identifies resources within the family and community to address potential risks to her mental health (20).
The intervention programme comprised of a total of sixteen session. After one or two introductory sessions with the LHW, one session of the THP was delivered weekly for four weeks in the last month of pregnancy. These sessions comprise the module 1 of the THP, called the “preparing for the baby”. This was followed by three sessions in the first month postpartum, collectively termed as module 2, “The baby's arrival”. And then monthly sessions for nine months thereafter, comprising three modules preparing mother for early (2nd to 4th month postnatal), middle (5th to 7th month postnatal) and late (8th to 10th month postnatal) infancy. The timing of the sessions could be adapted according to the convenience of the intervention recipient. Each session lasted between 45 to 60 minutes. Details on the THP are provided in Figure 1 and the Thinking Healthy Manual distributed by the World Health Organizations (20).
Baseline and Outcome Assessments
For this investigation, baseline assessments comprising of three classes of variables were used from the data set of the original trial: (a) demographic and socioeconomic variables (b) all items of the Hamilton Depression Rating Scale and (c) all items of the Brief Disability Questionnaire. All the tools were translated, adapted, and validated for the population, prior to their use in this trial.
The demographic and socioeconomic characteristics included age, education levels, income levels, parity, family structure, and empowerment. The Hamilton Depression Rating Scale (HDRS) comprised of 19 items assessing different symptoms of major depressive disorder (16, 21, 22). In addition to items mapped on the DSM-IV criteria of diagnoses, this scale also inquires about the participants' insight toward their illness, details on symptoms of physical and psychic anxiety, somatic complaints, and hypochondriasis. It also provides more information on compound symptoms in the DSM-IV diagnostic criteria. For instance, it rates symptoms of insomnia as per different stages (early, middle, and late) as well as hypersomnia. Items on problems with appetite are classified into loss of appetite and hyperphagia, as opposed to the DSM-IV. It has shown excellent validity and reliability in the screening for depression and measuring treatment response (22). All items on this scale are measured on a 4-point Likert scale. The third section comprised of the Brief Disability Questionnaire (BDQ) which measures disability among psychiatric populations. It measures dysfunction in daily physical and psychosocial functioning (16). It comprises of 8 items, recording responses on a 3-point Likert scale, ranging from '0' (not at all impaired) to '2' (moderately or definitively impaired). It has previously been found to be valid and reliable for use in the Pakistani population.
Statistical Analysis
All data were analyzed in SPSS (v. 27). Quantitative variables were described as mean (SD) and categorical as frequencies (%). Frequencies and percentages were presented for all the symptoms records on the HDRS. Frequencies (%) were calculated for different symptom profile after breaking them into two classes: (a) similar profiles of depressive symptom (b) Disjointed symptom profiles presenting a unique symptom combination by one individual only and (c) range of symptoms endorsed in different symptom combinations.
Thereafter, we conducted exploratory factor analyses (EFA) using alpha factoring and oblique rotation (direct oblimin), to delineate the factor structure of the HDRS. Kaiser-Meyer-Olkin measure of sampling adequacy and Bartlett's test of sphericity was conducted to assess the adequacy of sample size prior to running the EFA. Suitability of items to retain in the resulting pattern matrix were decided based on communalities ≥0.20 and factor loadings ≥0.40. Number of factors to retain were judged based on Eigen value ≥1 and Cattell's Scree plot and interpretability criterion. The resulting factors were subjectively named based on predominant symptomatology captured by each factor. The resulting factors were then fed into a two-step clustering model, to cluster study participants based on their depressive symptomatology. Study participants were clustered based on Akaike's Information Criterion based on log-likelihood distance measure. Cluster quality was parsimonious at Silhouette measure of cohesion and separation >0.20.
Thereafter, to investigate the relationship between symptom clusters and treatment effectiveness in reducing depressive symptom severity and disability scores, we performed two linear mixed models analyses separately with HDRS scores and BDQ scores as dependent variables. These models were run with maximum likelihood method, and random effects for union councils of participants, to account for clustering. In both models, treatment condition and symptoms clusters of perinatal depression were added as fixed effects, with two-way interactions between both. Further decision for adding suitable covariates and choice between adding a fixed or a random intercept was based on significant improvements in 2 log-likelihood criteria.
The results of linear mixed effects models were difficult to interpret in a clinical context. Therefore, we also presented improvements in rates of perinatal depressive disorder across the four subtypes of PND. These results were presented as risk ratios for easier interpretation, and Chi-square test of association to assess statistical significance.
Results
Baseline Characteristics
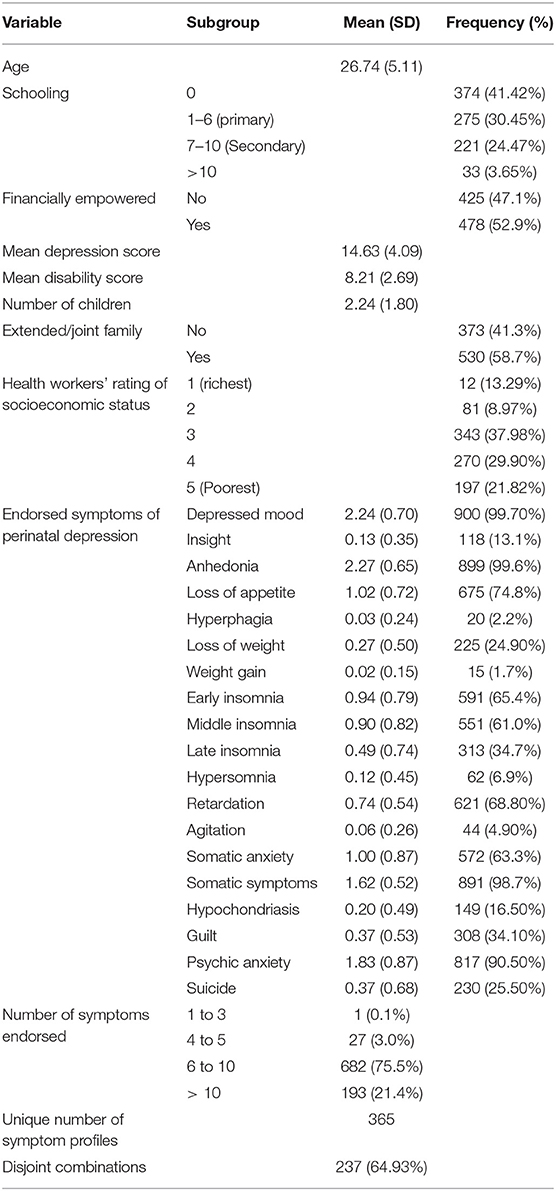
A total of 903 pregnant women in their third trimester participated in baseline interviews. The respondents had a mean age of 26.74 (5.11), with a higher proportion being non-educated or educated till primary class. A total of 478 (52.9%) were financially empowered, with 530 (58.7%) living in extended household systems. Majority of the study participants were rated by LHWs from the poorest to lower middle-income households. Mean disability scores were 8.21 (2.69) and depression scores were 14.63 (4.09) (Table 1).
Heterogeneous Symptom Profiles
Almost all participants reported experiencing core symptoms of depression: depressed mood (900, 99.70%) and anhedonia (899, 99.60%). In addition to core symptoms of depression, comorbid symptoms of somatic anxiety (572, 63.30%), psychic anxiety (817, 90.50%) and somatic symptoms (891, 98.70%) were highly prevalent. Psychomotor retardation was reported by a higher proportion of respondents (621, 68.80%) than agitation (4.90%). Physical manifestations such as loss of appetite were reported by 675 (74.8%), loss of weight (225, 24.90%). Symptoms of insomnia were reported as early (591, 65.4%), middle 551 (61.0%) and late (313, 34.7%). Atypical symptoms of hyperphagia were reported by 20 (2.2%), weight gain (15, 1.7%), and hypersomnia (62, 6.9%). Suicidal ideation was reported by a quarter (25.50%) of the participants (Table 1).
Out of 19 symptoms recorded on the HDRS, most of the participants reported having 6 to 10 symptoms of depression. Less than a quarter (21.4%) reported having over ten symptoms while the rest reported between 1 to 9 symptoms. These symptoms clustered together into 365 different combinations, where 237 (64.93%) of the combinations were disjointed; reported by only one individual in the study sample. Almost all the symptom clusters had depressed mood and anhedonia as the overlapping symptom (Table 1).
Clinical Phenotypic Clusters of PND
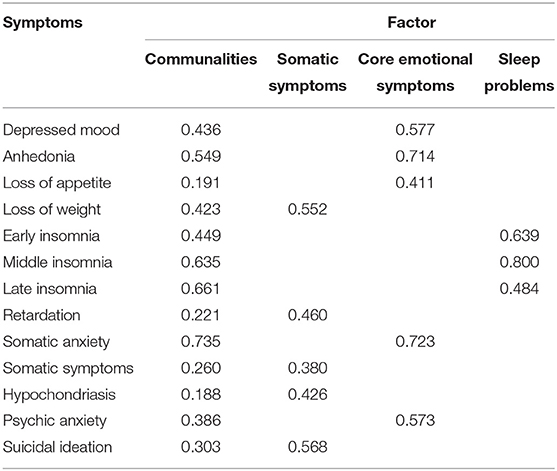
Two successive EFA were run before reaching an interpretable factor structure. In the first model, symptoms pertaining to agitation, hypersomnia, hyperphagia, weight gain, and guilt and insight were removed due to poor inter-item correlation and weak communalities. In the second EFA, a total of thirteen symptoms were retained in the factor analytic model, yielding adequate KMO measures of sampling adequacy (0.782) and significant Bartlett's test of sphericity. All communalities were adequate (≥0.20) except for loss of appetite (0.19), and hypochondriasis (0.19). Assessment of Eigen values and visualization of Scree plot suggested a three-factor solution for the HDRS, explaining 54.68% of the variance in HDRS (Supplementary Figure 1).
The three factors were named as: (a) core emotional symptoms representing symptoms of depressed mood, anhedonia, loss of appetite, somatic anxiety, and psychic anxiety. (b) somatic problems comprising of loss of weight, retardation, somatic symptoms, hypochondriasis, and suicidal ideation. And (c) sleep problems: insomnia during early, middle, and late night (Table 2). All these factors yielded Cronbach's Alpha > 0.60.
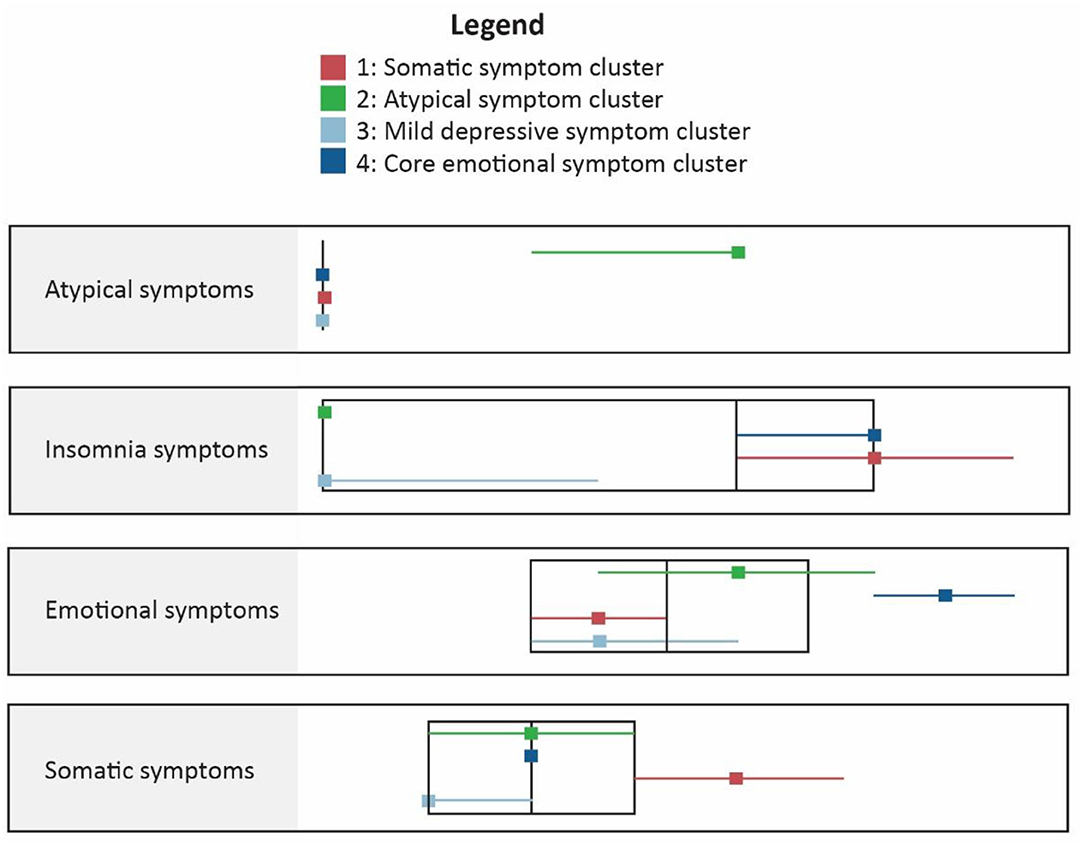
A two-step clustering algorithm clustered the study participants into four clusters based on above symptoms. In addition to the factors, we also introduced an additional variable for presence of any of the atypical symptoms (hypersomnia, hyperphagia and weight gain) which were endorsed by 88 (9.7%) of the participants. These did not load previously on the EFA, primarily due to their heterogeneous nature when compared with other symptoms. The two-step cluster model revealed a fair quality four cluster solution, with a silhouette measure of cohesion and separation at 0.5. Ratio of the largest to smallest cluster was 4.28.
Cluster 1 (atypical depression) comprised of participants with highest proportion of atypical symptoms and mild core emotional and somatic symptoms. Cluster 2 (Somatic symptoms) reported higher scores on somatic symptoms and insomnia symptoms. Cluster 3 (mild depression) reported mild symptoms overall while the fourth cluster (mixed anxiety and depression) reported severe core emotional symptoms (Figure 2 and Supplementary Figure 2).
Effectiveness of the Thinking Healthy Programme
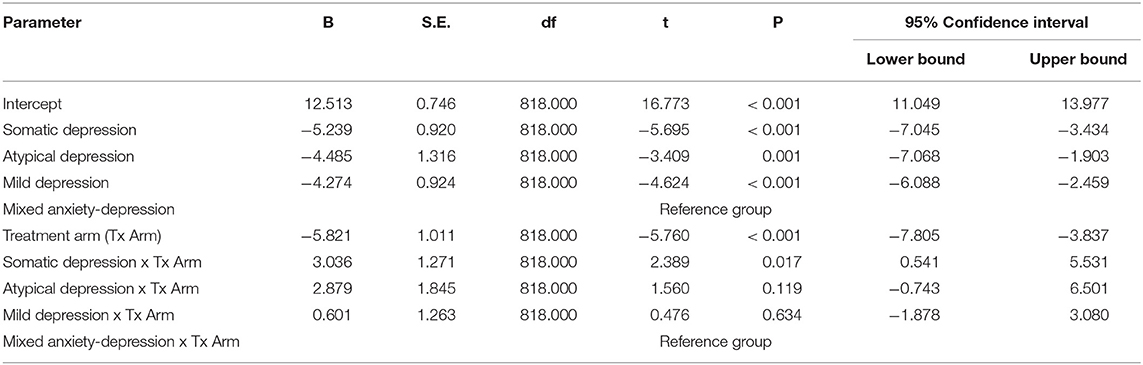
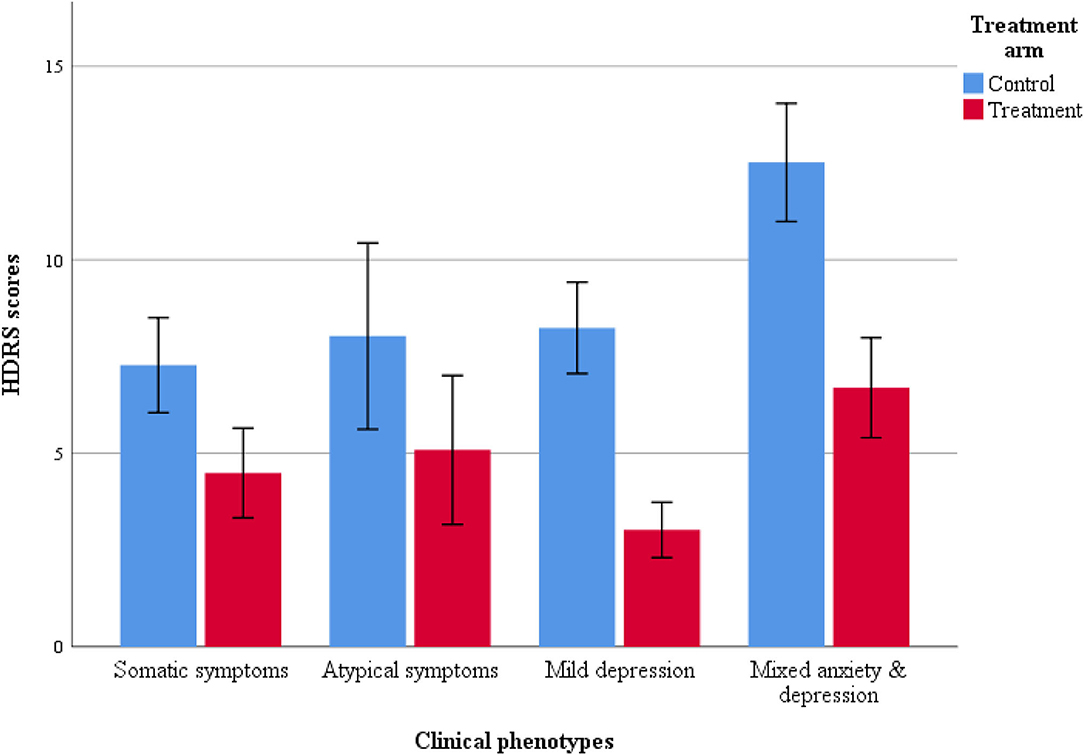
Linear mixed effects models revealed significant differences in depression severity among participants with different symptom profiles (Table 3, Figure 3). Pairwise comparisons using Bonferroni correction revealed that mixed anxiety and depression symptom cluster reported higher HDRS scores than their counterparts. The rest of the subtypes did not differ significantly on HDRS scores (Supplementary Table 1). Treatment condition x subtype interaction was also statistically significant (Supplementary Figure 3). However, fixed effects were only significant for the somatic subtype of PND. Addition of additional covariates did not lead to any significant changes in the BIC and 2-LL, however, these are presented as Supplementary Tables 2, 3.
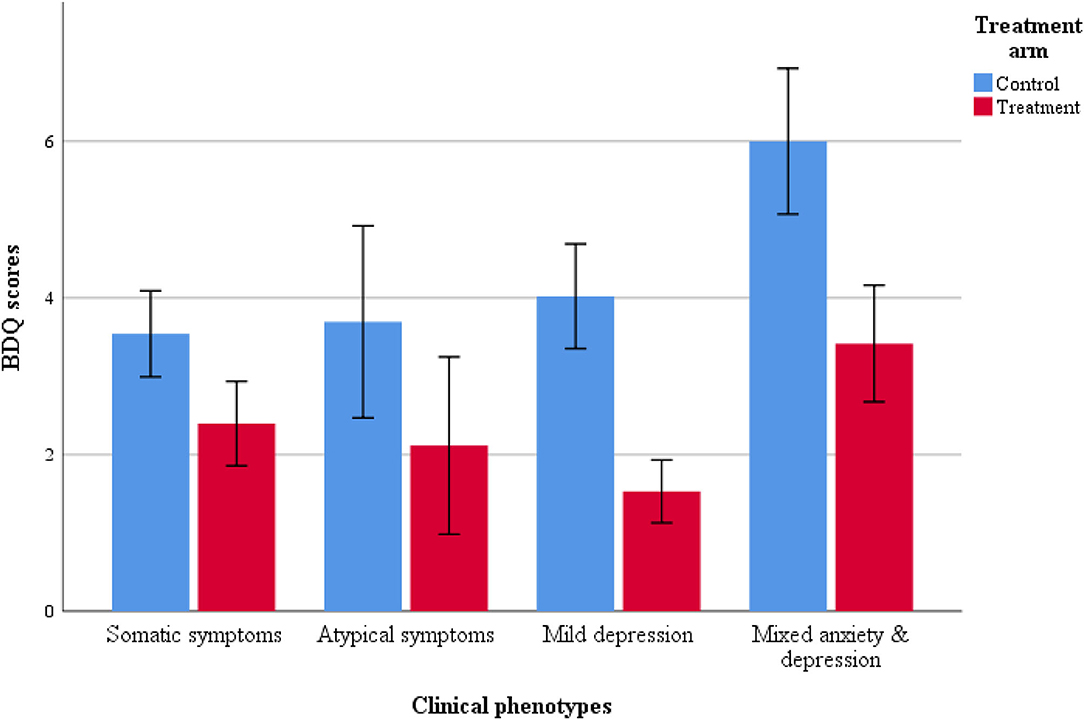
Similar trends were noted for the disability (BDQ) scores, participants reporting mixed anxiety and depression reported least improvement in disability when compared with other symptom clusters (Table 4 and Figure 4). However, the treatment x subtype interaction was non-significant.
As per clinical assessments, all clinical phenotypes responded well to the THP programme. Compared to their counterparts in the control group, mothers with mild depression in the treatment group yielded lowest risk ratios 0.24 (95% CI: 0.15 to 0.37), followed by mothers with anxiety-depression 0.50 (95% CI: 0.37 to 0.68), atypical depression 0.51 (95% CI: 0.27 to 0.99) and somatic depression 0.59 (95% CI: 0.42 to 0.83).
Discussion
This study presents evidence pertaining to the extent of heterogeneity in perinatal depressive symptoms in a sample of women in rural Pakistan. We found 365 different combination of symptom fulfilling DSM criteria of perinatal depression among 903 Pakistani women. Four distinct phenotypes of PND were revealed, with different clinical characteristics. The THP intervention was found to be effective in improving severity of symptoms and disability across the identified subtypes of PND.
This investigation reports a high extent of heterogeneity in perinatal depressive symptoms among diagnosed cases. Previous literature on heterogeneity of depression has focused solely on major depressive disorder in the general population (15, 23–27). Therefore, this investigation substantiates previous work by providing relevant data pertaining to PND. It highlights the shortcomings associated with the polythetic nature of psychiatric diagnoses where individuals diagnosed with similar disorder may have completely non-overlapping symptoms. This assumption is problematic because variable symptom profiles point to a single diagnosis as a latent entity, as posited in psychometrics (13). This position and underappreciation of within disorder heterogeneity, although seemingly plausible, has impeded progress in etiological and biological understanding of psychiatric diagnoses including perinatal depression (28–30). Our findings are corroborated by previous literature on major depressive disorder, which has shown this condition to be highly heterogeneous, yielding as many as 1,030 unique symptom profiles in secondary analyses of large scale datasets (27, 31).
Our analyses reveal three important insights pertaining to the polythetic nature of perinatal depression diagnosed as a set of few symptoms (including compound symptoms). Firstly, it challenges the assumption that each symptom is equally distressful to the patient. Secondly, it scrutinizes the DSM/ICD approach of presenting problems with sleep, appetite, and weight changes as compound symptoms. And lastly, that the symptoms qualifying the DSM criteria of perinatal depression warrant further scrutiny. Our model shows that even non-DSM symptoms such as physical and psychic anxiety and hypochondriasis were highly prevalent in our sample. And that these symptoms may sometimes be more distressful to the patient than the classical DSM symptoms. Therefore, a clinical staging approach rooted in a transdiagnostic framework should take precedence over traditional categorical diagnoses, at least in epidemiological studies. These findings have previously been corroborated by several studies, albeit focused on major depressive disorders, which emphasize that the consideration should be given toward study of individual symptoms rather than depending on sum-scores (15, 23), including the symptoms not covered by the DSM criteria (32) such as anxiety, aggression and irritability (33, 34).
More recently, with the advent of network psychometrics and mixture and cluster modeling approaches, empirical evidence has come into light, regarding the shortcomings associated with the covert within disorder heterogeneity and homogeneity and symptom overlap across different mental disorders (6, 7, 35). Most of the literature studying heterogeneity in perinatal depression have focused on either studying longitudinal trajectories of depression or classification based on severity of symptoms (6, 7). The study of longitudinal trajectories of PND have led to our understanding of variation in severity of depression according to onset during peripartum period, or nature of trajectory as subclinical, stable, chronic or remitting and relapsing (7).
However, only a few studies have considered individual symptoms leading to variation in clinical phenotypes of PND. Two studies of note explored PND using network analyses to emphasize the study of symptoms of depression because different clinical profiles of women with PND may point out to varying biological etiology. And treating all women with a similar paint brush of a categorical diagnosis may mask the underlying biological processes, and hamper treatment. In this context, Santos Jr. et al. (36) reported that cortisol levels among women with perinatal depression yield an association with positive mood and social support and negative with sadness and crying. Another study by Phua et al. emphasized the consideration of perinatal anxiety symptoms which emerged as a bridging symptom while studying depressive-anxiety network structures among Singaporean women. They also indicated that anxiety symptoms may precede development of maternal depression (8).
Similar to our study, the study of symptom clusters was taken up by an international perinatal psychiatry consortium Postpartum Depression: Action Toward Causes and Treatment (PACT) (37, 38). Using the Edinburgh Postnatal Depression Scale, three symptom dimensions were identified including depressed mood, anxiety and anhedonia, leading to five distinct clusters of women with PND. These clusters included “severe anxious depression, moderate anxious depression, anxious anhedonia, pure anhedonia, and resolved depression”. These subtypes differed in symptom quality, time of onset, with dimensions of anxiety and anhedonia associated with high severity and postpartum onset. Latent class analyses using the same dataset revealed three subclasses based on severity scores, with varying risk factors, resulting complications and prognosis (37, 38).
Considering the above, it is necessary to tailor interventions according to heterogeneous symptom profiles, to achieve optimum effectiveness. The Postpartum Depression: Action Toward Causes and Treatment (PACT) Consortium also emphasizes this need for development of personalized interventions, especially considering lower remission rates to currently available pharmacological therapies for PND (39). Cognitive behavioral therapy (CBT) as compared to other high intensity psychotherapies is evidence based and has shown good effectiveness in PND (40). Although previous research has studied effectiveness of psychological interventions and to some extent pharmacological interventions, none has acknowledged heterogeneity in this condition. Thus, there is an increasing evidence for heterogeneity in PND, and the need for tailoring of treatment for individuals. However, for most of the mental health systems in the low- and middle-income countries, this would translate to higher costs and human resource utilization. This is a considerable barrier in uptake of treatments in these regions, which are already under resourced and struggle with provision of mental health care to masses.
To bridge this evidence gap, we provide evidence for a multicomponent CBT based intervention the Thinking Healthy Programme (THP, for heterogeneous presentations of the PND. We hypothesized that the THP due to its multicomponent nature (20) would prove to be effective in achieving remission for different clinical phenotypes of PND. Indeed, THP was found to be effective in all the clinical phenotypes of PND in this study. The present investigation thus, strengthens evidence base for THP, proving its utility in achieving clinical and cost effective mental healthcare, especially in resource constrained areas (41). The inclusion of the THP in mhGAP programme by the WHO, provides an impetus for scale up of this programme in LMICs.
Strengths and Limitations
This study has several strengths. It is based on a large randomly selected study sample which improves its generalizability to rural Pakistan. The participants in this study were diagnosed clinically for PND, therefore, it overcomes limitations pertaining to recall bias associated with use of psychometric scales. However, the results of this study should be generalized with caution because the symptom profiles reported in this study may differ cross-culturally.
An important limitation of this study was the lack of information pertaining to prior diagnoses of major depressive disorder. This information is immensely helpful in categorizing postpartum depression as recurrent or continuation of a previous episode of major depression. This was primarily because this intervention was conducted in a rural subdistrict, which at the time had poor awareness regarding mental illnesses and little to no access to either primary or specialized mental health care. Therefore, it is likely most of the study sample may not have been aware of their diagnoses of major depressive disorder. Inquiring about covert depressive mood symptoms prior to the study may have introduced significant recall bias. Moreover, the findings may have been questionable due to validity and reliability issues when labeling a participant with major depressive disorder retrospectively.
Another concern pertains to the factorial invariance of the HDRS, which has often been raised in depression research. This issue was highlighted by Bagby et al. who reviewed evidence pertaining to psychometric properties of the HDRS (42). They noted that HDRS yielded inconsistent factor structures across different populations and studies. Authors reported as few as 2 and as many as 8 subscales of HDRS, with inconsistent item level factor structures and loading values. They concluded that HDRS was thus, conceptually flawed, and newer tools were needed based on the DSM and contemporary definitions of depression. Unfortunately, all the reviewed studies were performed among populations other than the perinatal ones. However, we opine that this factorial invariance of HDRS across different populations merely points to the covert heterogeneity of major depressive disorder and the need for studying different subtypes of depression rather than treating it as a single syndromic construct (13).
Implication for Future Research and Implementation
This study, comprising of a largely descriptive evidence of heterogeneity in PND, should inspire further empirical work in this domain. Based on our results, we emphasize the adoption of a transdiagnostic framework in etiological and intervention research pertaining to PND. PND when visualized in a transdiagnostic framework should overcome limits related to study of a subset of symptoms of PND (43). We recommend that interventions should be designed in a transdiagnostic framework to account for comorbid symptoms of anxiety, hypochondriasis, and somatic complaints. We also recommend that future research should study clustering of symptoms of PND to inform The Hierarchical Taxonomy of Psychopathology (HiTOP) and Research Domain Criteria (rDOC) frameworks (44, 45). It is also important to study PND from a network perspective to delineate important symptoms as targets for interventions and overlap with other DSM disorders (29). From the perspective of psychometrics, it is important to consider development and deployment of scales that account for prevalent symptoms comorbid with PND for screening as well as measurement of response to intervention (46).
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethical approval for the original randomized controlled trial was granted by the University of Manchester, UK and the Institute of Psychiatry, Rawalpindi, Pakistan. The present secondary analyses, however, were exempt from ethical review. The patients/participants provided their written informed consent to participate in this study.
Disclosure
The preliminary findings from this study were presented at the Annual Congress of the European Psychiatric Association. This manuscript is to be submitted as partial fulfilment for a Ph.D. degree in Psychiatry at the University of Liverpool, Liverpool, UK.
Author Contributions
AW conceived the idea, conducted the secondary analyses, and wrote the first draft of the manuscript. AR led the original project, supervised the current analyses, and extensively edited the first draft of the manuscript. All authors approved the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.736790/full#supplementary-material
References
1. Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ. (2012) 90:139G–49G. doi: 10.2471/BLT.11.091850
2. Waqas A, Raza N, Lodhi HW, Jamal M, Muhammad Z, Rehman A. Psychosocial factors of antenatal anxiety and depression in Pakistan: is social support a mediator? PLoS ONE. (2015) 10:e0116510. doi: 10.1371/journal.pone.0116510
3. Gelaye B, Rondon MB, Araya R, Williams MA. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. The Lancet Psychiatry. (2016) 3:973–82. doi: 10.1016/S2215-0366(16)30284-X
4. Sha Q, Achtyes E, Nagalla M, Keaton S, Smart LA, Leach R, et al. Associations between estrogen and progesterone, the kynurenine pathway, and inflammation in the post-partum. J Affect Disord. (2021) 281:9–12. doi: 10.1016/j.jad.2020.10.052
5. Carnevali GS, Buoli M. The role of epigenetics in perinatal depression: Aee there any candidate biomarkers? J Affect Disord. (2021) 280:57–67. doi: 10.1016/j.jad.2020.11.056
6. Santos Jr. H, Tan X, Salomon R. Heterogeneity in perinatal depression: how far have we come? A systematic review. Arch Womens Ment Heal. (2017) 20:11–23. doi: 10.1007/s00737-016-0691-8
7. Baron E, Bass J, Murray SM, Schneider M, Lund C. A systematic review of growth curve mixture modelling literature investigating trajectories of perinatal depressive symptoms and associated risk factors. J Affect Disord. (2017) 223:194–208. doi: 10.1016/j.jad.2017.07.046
8. Phua DY, Chen H, Chong YS, Gluckman PD, Broekman BFP, Meaney MJ. Network analyses of maternal pre- and post-partum symptoms of depression and anxiety. Front Psychiatry. (2020) 11:1–13. doi: 10.3389/fpsyt.2020.00785
9. Flake JK, Fried EI. Measurement schmeasurement: questionable measurement practices and how to avoid them. Adv Method Pract Psychol Sci. (2020) 3:456–65. doi: 10.1177/2515245920952393
10. Gibson J, McKenzie-McHarg K, Shakespeare J, Price J, Gray R. A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand. (2009) 119:350–64. doi: 10.1111/j.1600-0447.2009.01363.x
11. Naveed S, Waqas A, Memon AR, Jabeen M, Sheikh MH. Cross-cultural validation of the Urdu translation of the Patient Health Questionnaire for Adolescents among children and adolescents at a Pakistani school. Public Health. (2019) 168:59–66. doi: 10.1016/j.puhe.2018.11.022
12. Waqas A, Aedma KK, Tariq M, Meraj H, Naveed S. Validity and reliability of the Urdu version of the Hospital Anxiety & Depression Scale for assessing antenatal anxiety and depression in Pakistan. Asian J Psychiatr. (2019) 45:20–5. doi: 10.1016/j.ajp.2019.08.008
13. Fried EI. Problematic assumptions have slowed down depression research: why symptoms, not syndromes are the way forward. Front Psychol. (2015) 6:1–11. doi: 10.3389/fpsyg.2015.00309
14. Fried EI, van Borkulo CD, Cramer AOJ, Boschloo L, Schoevers RA, Borsboom D. Mental disorders as networks of problems: a review of recent insights. Soc Psychiatry Psychiatr Epidemiol. (2017) 52:1–10. doi: 10.1007/s00127-016-1319-z
15. Fried EI, Nesse RM. Depression sum-scores don't add up: Why analyzing specific depression symptoms is essential. BMC Med. (2015) 13:1–11. doi: 10.1186/s12916-015-0325-4
16. Rahman A, Malik A, Sikander S, Roberts C, Creed F. Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. Lancet. (2008) 372:902–9. doi: 10.1016/S0140-6736(08)61400-2
17. Maselko J, Sikander S, Bhalotra S, Bangash O, Ganga N, Mukherjee S, et al. Effect of an early perinatal depression intervention on long-term child development outcomes: follow-up of the Thinking Healthy Programme randomised controlled trial. Lancet Psychiatry. (2015) 2:609–17. doi: 10.1016/S2215-0366(15)00109-1
18. Rahman A, Iqbal Z, Roberts C, Husain N. Cluster randomized trial of a parent-based intervention to support early development of children in a low-income country. Child Care Health Dev. (2009) 35:56–62. doi: 10.1111/j.1365-2214.2008.00897.x
19. Keynejad RC, Dua T, Barbui C, Thornicroft G, WHO. Mental Health Gap Action Programme (mhGAP) Intervention Guide: a systematic review of evidence from low and middle-income countries. Evid Based Ment Health. (2018) 21:30–4. doi: 10.1136/eb-2017-102750
20. World Health Organization. Thinking Healthy: A manual for psychological management of perinatal depression. (2015).
21. Williams JB. Standardizing the Hamilton Depression Rating Scale: past, present, and future. Eur Arch Psychiatry Clin Neurosci. (2001) 251:II6–12. doi: 10.1007/BF03035120
22. Hashmi AM, Naz S, Asif A, Khawaja IS. Urdu translation of the Hamilton Rating Scale for Depression: results of a validation study. Pak J Med Sci. (2016) 32:1479–83. doi: 10.12669/pjms.326.11399
23. Fried EI, Nesse RM. The impact of individual depressive symptoms on impairment of psychosocial functioning. PLoS One. (2014) 9:e90311. doi: 10.1371/journal.pone.0090311
24. Fried EI. The 52 symptoms of major depression: lack of content overlap among seven common depression scales. J Affect Disord. (2017) 208:191–7. doi: 10.1016/j.jad.2016.10.019
25. Arnow BA, Blasey C, Williams LM, Palmer DM, Rekshan W, Schatzberg AF, et al. Depression subtypes in predicting antidepressant response: a report from the iSPOT-D trial. Am J Psychiatry. (2015) 172:743–50. doi: 10.1176/appi.ajp.2015.14020181
26. Zimmerman M, Ellison W, Young D, Chelminski I, Dalrymple K. How many different ways do patients meet the diagnostic criteria for major depressive disorder? Compr Psychiatry. (2015) 56:29–34. doi: 10.1016/j.comppsych.2014.09.007
27. Fried EI, Nesse RM. Depression is not a consistent syndrome: an investigation of unique symptom patterns in the STAR*D study. J Affect Disord. (2015) 172:96–102. doi: 10.1016/j.jad.2014.10.010
28. Robinaugh DJ, Hoekstra RHA, Toner ER, Borsboom D. The network approach to psychopathology: a review of the literature 2008-2018 and an agenda for future research. Psychol Med. (2020) 50:353–66. doi: 10.1017/S0033291719003404
29. Borsboom D. A network theory of mental disorders. World Psychiatry. (2017) 16:5–13. doi: 10.1002/wps.20375
30. Kapur S, Phillips AG, Insel TR. Why has it taken so long for biological psychiatry to develop clinical tests and what to do about it? Mol Psychiatry. (2012) 17:1174–9. doi: 10.1038/mp.2012.105
31. Fried EI, Coomans F, Lorenzo-Luaces L. The 341 737 ways of qualifying for the melancholic specifier. The Lancet Psychiatry. (2020) 7:479–80. doi: 10.1016/S2215-0366(20)30169-3
32. Zimmerman M, McGlinchey JB, Young D, Chelminski I. Diagnosing major depressive disorder III: can some symptoms be eliminated from the diagnostic criteria? J Nerv Ment Dis. (2006) 194:313–7. doi: 10.1097/01.nmd.0000217806.16329.ff
33. Judd LL, Schettler PJ, Coryell W, Akiskal HS, Fiedorowicz JG. Overt irritability/anger in unipolar major depressive episodes: past and current characteristics and implications for long-term course. JAMA Psychiatry. (2013) 70:1171–80. doi: 10.1001/jamapsychiatry.2013.1957
34. Fava M, Rush AJ, Alpert JE, Balasubramani GK, Wisniewski SR, Carmin CN, et al. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiatry. (2008) 165:342–51. doi: 10.1176/appi.ajp.2007.06111868
35. Jones PJ, Ma R, McNally RJ. Bridge centrality: a network approach to understanding comorbidity. Multivariate Behav Res. (2019) 56:353–67. doi: 10.1080/00273171.2019.1614898
36. Santos H Jr, Fried E, Afasu-Adjei J, Ruiz R. Network structure of perinatal depressive symptoms in latinas: relationship to stress and reproductive biomarkers hudson. Physiol Behav. (2017) 176:139–48. doi: 10.1002/nur.21784
37. Guintivano J, Putnam KT, Sullivan PF, Meltzer-Brody S. Clinical phenotypes of peripartum depression and time of onset : the PACT Consortium. In: Biomarkers of Postpartum Psychiatric Disorders. (2019). doi: 10.1016/B978-0-12-815508-0.00001-1
38. Postpartum Depression: Action Towards C, Consortium T. Heterogeneity of postpartum depression: a latent class analysis. Lancet Psychiatry. (2015) 2:59–67. doi: 10.1016/S2215-0366(14)00055-8
39. Brown JVE, Wilson CA, Ayre K, Robertson L, South E, Molyneaux E, et al. Antidepressant treatment for postnatal depression. Cochrane Database Syst Rev. (2021) 2:CD013560. doi: 10.1002/14651858.CD013560.pub2
40. National Collaborating Center for Mental Health. National Clinical Guideline Number 192: Antenatal and postnatal mental health Clinical management and service guidance Updated edition. (2020). Available online at http://www.nice.org.uk/guidance/cg192
41. Sikander S, Lazarus A, Bangash O, Fuhr DC, Weobong B, Krishna RN, et al. The effectiveness and cost-effectiveness of the peer-delivered Thinking Healthy Programme for perinatal depression in Pakistan and India: the SHARE study protocol for randomised controlled trials. Trials. (2015) 16:534. doi: 10.1186/s13063-015-1063-9
42. Bagby RM, Ryder AG, Schuller DR, Marshall MB. The Hamilton Depression Rating Scale: has the gold standard become a lead weight? Am J Psychiatry. (2004) 161:2163–77. doi: 10.1176/appi.ajp.161.12.2163
43. Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, et al. The Lancet Commission on global mental health and sustainable development. Lancet. (2018) 392:1553–98. doi: 10.1016/S0140-6736(18)31612-X
44. Conway CC, Forbes MK, Forbush KT, Fried EI, Hallquist MN, Kotov R, et al. A hierarchical taxonomy of psychopathology can transform mental health research. Perspect Psychol Sci. (2019) 14:419–36. doi: 10.31234/osf.io/wsygp
45. Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Med. (2013) 11:126. doi: 10.1186/1741-7015-11-126
Keywords: perinatal depression, heterogeneity, disability, subtypes, machine learning, cluster analysis, postpartum depression, clinical phenotypes
Citation: Waqas A and Rahman A (2021) Does One Treatment Fit All? Effectiveness of a Multicomponent Cognitive Behavioral Therapy Program in Data-Driven Subtypes of Perinatal Depression. Front. Psychiatry 12:736790. doi: 10.3389/fpsyt.2021.736790
Received: 05 July 2021; Accepted: 13 October 2021;
Published: 17 November 2021.
Edited by:
Yuan-Pang Wang, University of São Paulo, BrazilReviewed by:
Chutima Roomruangwong, Chulalongkorn University, ThailandAmritha Bhat, University of Washington, United States
Copyright © 2021 Waqas and Rahman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ahmed Waqas, YWhtZWQud2FxYXNAbGl2ZXJwb29sLmFjLnVr
 Ahmed Waqas
Ahmed Waqas Atif Rahman
Atif Rahman