- 1Department of Clinical Child and Adolescent Psychology, Philipps University Marburg, Marburg, Germany
- 2Mental Health Research Program, The Village, Ludwig Boltzmann Gesellschaft, Innsbruck, Austria
- 3Department of Psychiatry, Psychotherapy and Psychosomatics, Division of Psychiatry I, Medical University Innsbruck, Innsbruck, Austria
- 4Care Policy and Evaluation Centre (CPEC), London School of Economics and Political Science, London, United Kingdom
Stigma can have devastating health and wellbeing impacts, not just on people with mental health problems, but on people associated with the stigmatized person. This is called stigma-by-association. Children whose parents have mental health problems are a particularly vulnerable group, and stigma acts as a mechanism, contributing to the transgenerational transmission of mental disorders. The current study is a systematic mixed studies review, synthesizing knowledge about how this group of children experience stigma-by-association. Overall, 32 studies were included, after a systematic search including quantitative, qualitatative, and mixed methods studies. The methodological quality was assessed and qualitative content analysis undertaken. We grouped children's stigma experiences into four dimensions, i.e., experienced stigma, anticipated stigma, internalized stigma, and structural discrimination. Results show that stigma is an important factor in those children's lives, and needs further investigation in qualitative and quantitative research. The current study emphasizes the importance of anti-stigma interventions and campaigns.
Introduction
Children of parents with a mental illness1 have received increasing attention over recent years, especially as it is estimated that one in five children world-wide has a parent with a mental illness (1–3). Those children often face specific challenges that are associated with reduced mental health, poorer academic achievement, and impaired social well-being and quality of life (1, 4, 5). Social adversities associated with mental illness, including poverty, as well as genetic predisposition and family dysfunction, act as mechanisms contributing to these risks (6). Those mechanisms have been integrated into a comprehensive model: the transgenerational transmission of mental disorders (TTMD) model identifies four major domains (1. parent, 2. family, 3. child, 4. social environment) that interact with their respective systems, and are influenced by five transmission mechanisms1 (1. genetics, 2. prenatal factors, 3. parent-child-interaction, 4. family, and 5. social factors) (1, 7). According to this model, stigma can be seen as a component of social factors, acting as a mechanism for the transmission of mental disorders that leads to multiple challenges and negative outcomes.
As captured in the concepts of stigma-by-association (SBA) (8), family stigma [e.g., (9)], or courtesy stigma (10, 11), stigma can affect not only the person with a mental health problem, but also people connected to the person, such as family or friends (12). The conceptual thinking of SBA by Pryor et al. (8) focuses on the general public and potential mechanisms that might contribute to the emergence of SBA, but lacks the perspective and experiences of those affected. Current research mostly describes SBA as guilt, blame, and contamination, ascribed to and experienced by family members (13, 14). Children are most frequently described as experiencing such “contamination” stigma, i.e., the general public tends to see them as being contaminated by the parental mental illness [e.g., (13, 14)]. The theoretical model of SBA by Philipps and Gates (15) focuses on various stigma dimensions and facets that could affect children, but for the very special group with incarcerated parents. On an experiential level, perceived stigma, internalized stigma, discrimination, and differences in social, cultural, economic, and political power are identified for this group. Another qualitative study classified stigma dimensions described by family members of people with schiziophrenia, finding structural elements of discrimination, and interpersonal interaction elements, such as social exclusion (16, 17).
Goffman has defined experiencing “courtesy stigma” as ‘an individual who is related through the social structure to the stigmatized (…) leads the wider society to treat both individuals in some respect as one' (11), and research so far has not conceived of the stigma dimensions for relatives, but rather solely named the stigma facets to be important for relatives of people with a stigmatized condition. Given this, we assume that SBA for children can potentially contain all of the stigma facets described for the primary recipients: Experienced SBA describes personally experienced prejudice and discrimination (18, 19); perceived SBA explains the “belief that most people will devalue, discriminate the stigmatized” (19); anticipated SBA includes expectations that others will devalue and discriminate against them (18); affiliate stigma describes the self-stigma of associates of people with a mental illness, i.e., the “internalization of stigma among associates of targeted individuals” on the affective, cognitive and behavioral level (20); and structural discrimination targets societal and policy structures that reproduce existing social inequalities (21).
The experience of SBA and discrimination, the anticipation of what others may think about them, and accommpaning self-stigmatization, can have a deep impact on individuals. There is evidence that 8–22 % of family members of people with a mental illness experienced stigma's negative impacts on themselves, e.g., ruined self-esteem (21%), disrupted family relationships with other family members (22%), and with their ill family members (20%) (16). It has also been reported that family members of someone with a mental illness may avoid social situations and events, reduce or break contact with family and friends, spend energy on hiding the secret, and experience discrimination within employment and/or housing situations (14, 22). Although a growing body of research focuses on SBA, very few studies investigated how these stigma experiences affect individual family members (23); systematic studies, especially those targeting children, are missing that would shed light on their SBA experiences while classifying their experiences into the various stigma dimensions. The same is true for the concept of affiliate stigma (20): while children of parents with a mental illness often do care for their parents [parentification, e.g., (24)], they have not been the focus in studies on affiliate stigma so far.
A recent systematic review on the evidence of stigma concepts for children of parents with a mental illness aimed to identify stigma-related experiences and outcomes as reported by parents and children (25). Their findings summarize stigma concepts from the primary literature, all of which describe different individual facets of children's and their parents' experiences of stigma. This review highlights the lack of uniform definitions for such stigma experiences, as well as the lack of an all-encompassing concept that includes the various dimensions of stigma experiences of children whose parents have a mental illness. The main finding of this review is that affected children report feelings of embarrassment, shame, and the need to hide their parental mental illness, though those findings are not integrated into an overall framework of different stigma dimensions.
The aim of the present study is therefore (1) to gain knowledge about how the children of parents with a mental illness experience stigma, (2) to synthesize this knowledge into a primary model of SBA on an experienced level for this population. In so doing, we (3) hope to contribute to SBA's theoretical model, that is currently insubstantial and not focused on children.
To achieve this, evidence from qualitative, quantitative, and mixed-method studies regarding children's stigma experiences related to their parents' mental illness is synthesized and collated.
Methods
Protocol and Registration
The review is registered and approved by PROSPERO, registration number CRD42019112838 (www.crd.york.ac.uk/PROSPERO).
Design
This review follows the PRISMA statement for conducting systematic reviews (26). Considering stigmatization of mental illness and its impact upon children is a complex and multifaceted problem. We thus included qualitative, quantitative, and mixed-methods studies to synthesize knowledge from different methodological perspectives, and diverse evidence.
Search Strategy
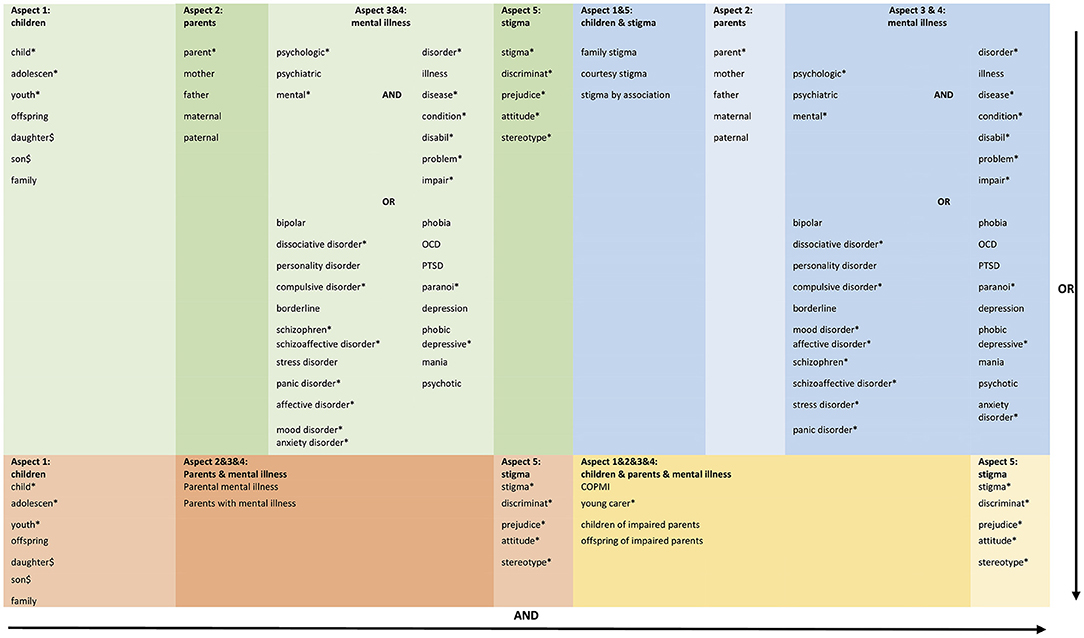
Five electronic databases (PubMed, Cochrane Library, PsycINFO, PSYNDEX, Web of Sciences) were searched (updated April 2020), using a detailed search strategy developed for PubMed and adapted for other databases, see Figure 1. The four different search term combinations (illustrated in the figure by the colors blue, green, orange and yellow) were combined with the OR function. Additional references from current reviews and theoretical articles were also reviewed to identify additional citations. Our search strategy consisted of five aspects and was developed with the Village research team (https://village.lbg.ac.at/about), an expert librarian, and an expert in stigma theories.
Eligibility Criteria
Studies were eligible for inclusion if they met the following criteria: (a) original primary peer-reviewed research; (b) published in English or German, (c) investigation of stigma experiences, or stigma as a relevant issue for children, and (d) children of parents with a mental illness were a (sub-)sample in the study. We did not use a filter for publication dates.
Exclusion Criteria
Studies were excluded if they: (a) focused on the general public as study population, i.e., we were not interested in the stigma that public stigma carries against children, but on the experience-level of the affected individuals, or (b) their stigma measures did not allow for a clear distinction between the different stigma dimensions, or if their only informative value for children was whether they experienced more or less stigma than other family members, or (c) did not differentiate enough between children and other family members regarding their stigma experiences, i.e., if the original paper did not state clearly if their results reflect the experiences of all family members, including children, we excluded them as we could not ensure whether those findings applied to this population. In qualitative studies with different subsamples, we used only those statements made by the children. In quantitative studies, we only used the analysis results of the subgroup of children.
Study Selection
After conducting the standard search as outlined above, all titles and abstracts were screened by independent reviewers (L-MD, FS). They were eligible for full text screening if children of parents with mental illness were participants in the study, and if the abstract either directly highlighted stigma or stigma-related concepts (see search strategy, aspect 5) or included children's specific experiences that may include stigma experiences. Full texts of potentially eligible studies were retrieved and independently assessed for eligibility by two review authors (L-MD, JF). Any disagreement was resolved through discussion with a third review author (HC).
Quality Appraisal
Three review authors (L-MD, AB, JLP) independently assessed the risk of bias in the included studies. Two authors independently appraised the quality and looked for convergence. Due to heterogeneity in methodological approaches in the included studies, i.e., qualitative, quantitative as well as mixed methods methodology, the “Mixed Methods Appraisal Tool” [MMAT; (27)] was used. The quality of each study was assessed applying two general criteria for all the studies, and five criteria adapted to each specific methodology requirement. As recommended by the authors of the MMAT tool, we did not exclude any studies due to low methodological quality, but used their information to estimate potential biases. Nevertheless, to provide an overview of study quality, we calculated an overall score for each study in terms of study quality, ranging from 0 to 100%, in which we allocated one star for each 20% of the criteria met.
Data Extraction
Various information was extracted from the original studies addressing our research question. In addition to general information on data collection, analysis methods, and study population, all text passages related to stigma experiences were extracted. This means that the results and discussion sections of the included studies were systematically searched for stigma-related terms and content. Once the data analysis was completed, we determined which stigma dimensions could be allocated to which studies. All the extracted data are summarized in Supplementary Table S1. Two authors (L-MD, DP) extracted data independently, discrepancies were identified and resolved through discussion with a third author (HC).
Analysis
Qualitative content analysis was conducted for comprehensive description and interpretation. A qualitative data-based convergent synthesis design was adopted (28). We used Kuckartz' (29) guidance for conducting qualitative content analyses, using the same synthesis method for both qualitative and quantitative studies. Thus, quantitative data were transformed into qualitative categories in order to explore similarities and/or differences between studies. The quantitative data were also examined in terms of their stigma results, and narratively described results were coded. Any evidence found was summarized correspondingly. We used the software MAXQDA (Version 2018) to manage the storage of analysis. Extracted results were read several times, and memos were made to become immersed in the meaning. Sub-categories were compiled inductively and material-driven. Out of the formulated sub-categories, generic categories were abstracted, describing themes that emerged. Those generic categories were grouped into main categories with the help of comprehensive stigma frameworks (18, 19). The complete data (i.e., extracted results of interest) was coded with those main categories.2 Coding was done independently by two researchers (L-MD, FS) to ensure the reliability of data analysis. Discrepancies were resolved through discussion with HC.
Results
Search Outcome
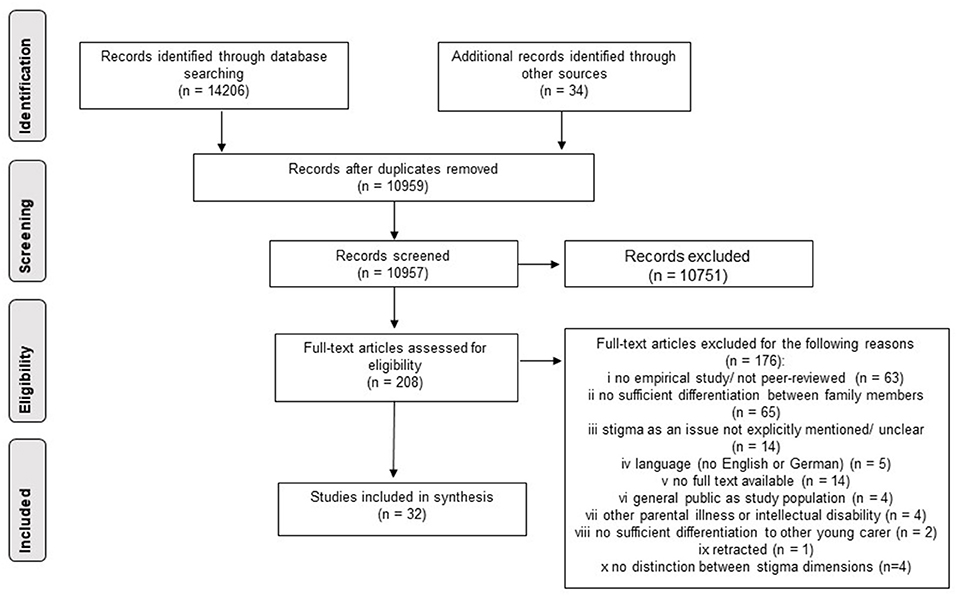
Most studies were excluded at the title/abstract screening stage (see Figure 2), leaving 208 for full-text screening. Most of the studies were excluded at this stage because we could not differentiate their findings to other family members well enough, or because studies were not empirical or not peer-reviewed. A few quantitative studies also had to be excluded in the last stage because they measured unclear and mixed-up stigma dimensions, making it impossible to assign them to individual dimensions (see Figure 1). We were ultimately able to include a total of 32 articles from 30 studies3.
Study and Population Characteristics
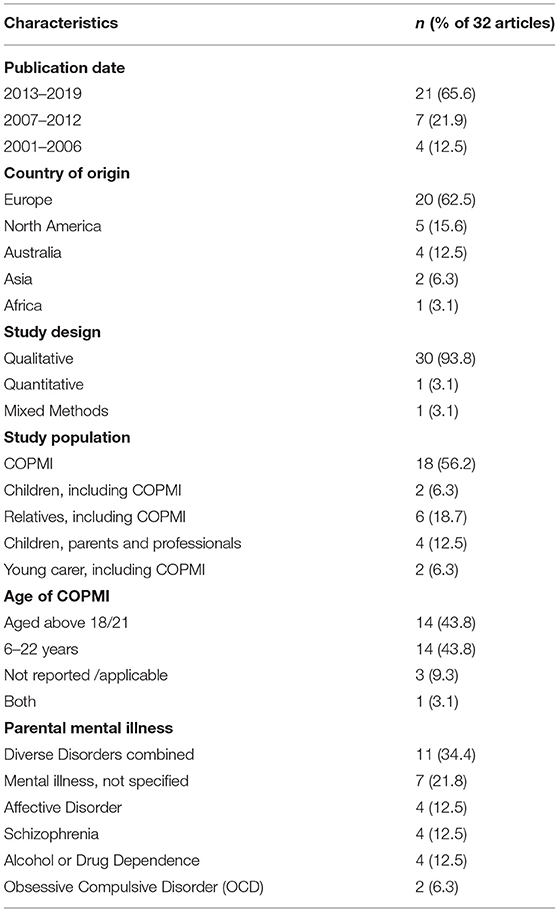
The majority of studies (30 ≜ 93.8 %) were qualitative; only one quantitative and one mixed method study were included, Table 1. Most of the studies were conducted in Europe (20 ≜ 62.5 %). Half of them had minor children as participants, the other half had adult children; one study combined the two. We ended up including more than half of the studies that had not aimed to explore stigma in this population, but aimed to capture their (everyday) experiences and burden. Stigma then emerged as one of the central themes in these studies. However, this also meant that most of the studies lacked a clear definition of stigma. Supplementary Table S1 provides a detailed description of the included studies.
Quality Appraisal
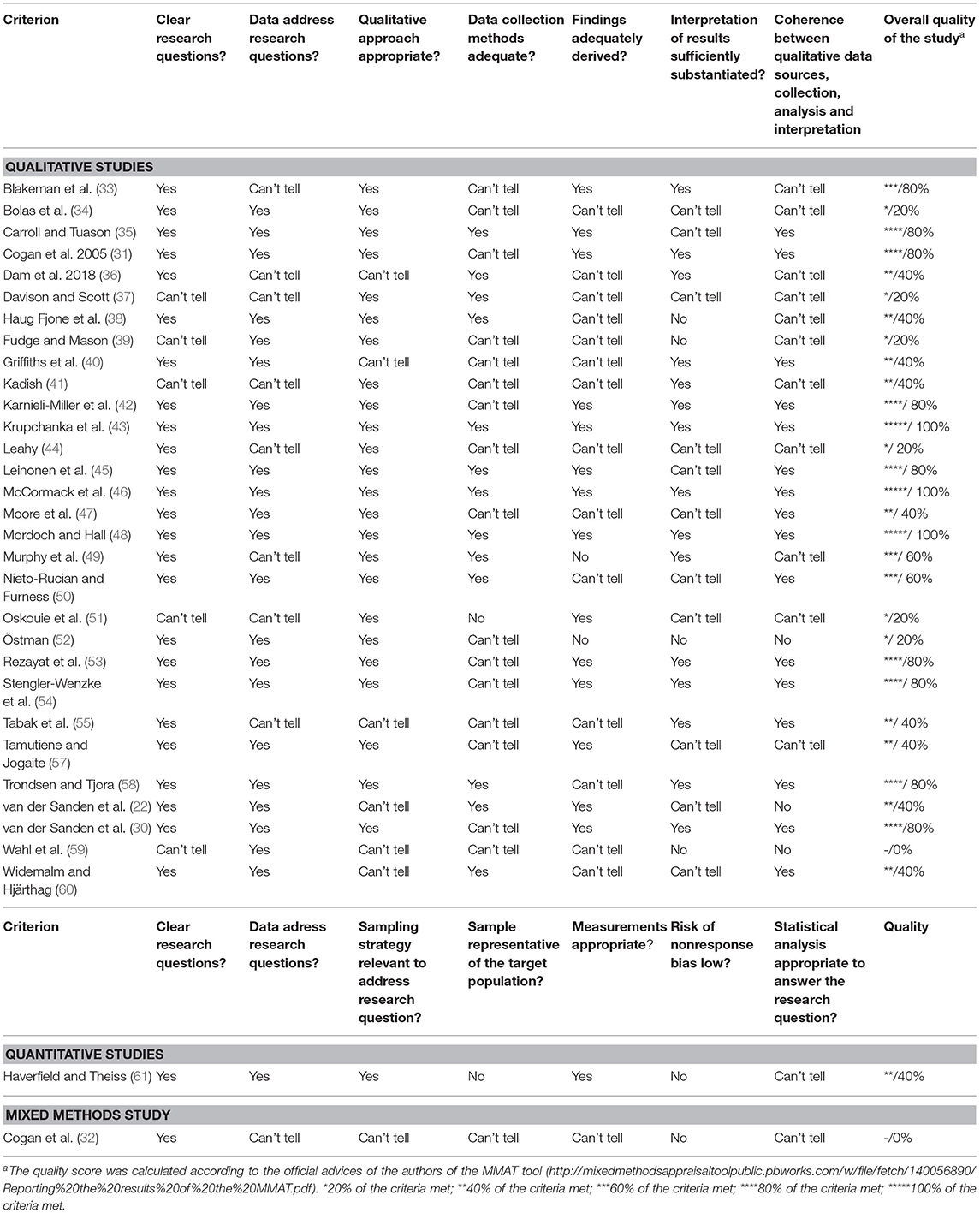
The quality of the studies was very heterogeneous and overall, 13 of the included studies met 60% or more criteria (for details see Table 2). They ranged from zero to five in their score, meaning that they ranged from 0 to 100 % of the criteria met. In qualitative studies, that were assessed as being of lower quality, often a clear rationale regarding the data collection method, the method of analysis or interview guidelines was missing, or the study population was not sufficiently defined. Quantitative studies of lower quality did not include a representative sample for their target population and had a low risk of non-response bias. The mixed-method study especially lacked in contrasting the results from the two study approaches and bringing the results together.
Identified Aspects of Stigma Related to Parental Mental Illness
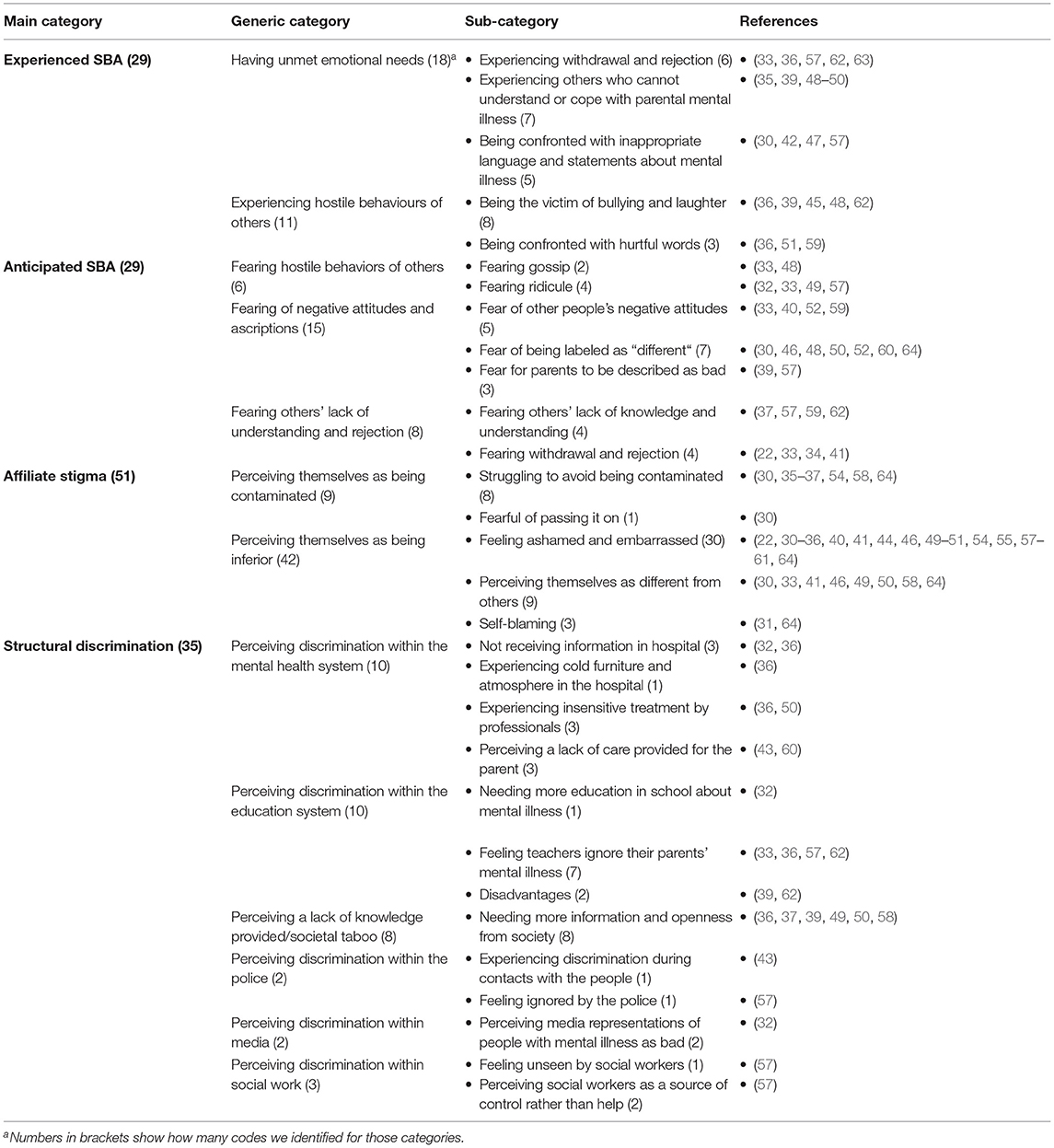
Following our analysis, we identified four different stigma dimensions described by or regarding children that are well-known from the stigma experiences of people who have a stigmatized condition themselves: experienced SBA, anticipated SBA, affiliate (internalized) stigma, as well as structural discrimination. Within these main categories, we identified various subcategories that are described in the following sections. Table 3 reports the category system for stigma dimensions, their frequencies, and associated studies.
Experienced SBA—Having Experienced Unpleasant (Re)Actions of Others
We identified two generic categories of SBA in this section: (1) having unmet emotional needs, and (2) experiencing the hostile behaviors of others. Both revealed various subcategories and are now described in more detail.
Having Unmet Emotional Needs
Being Confronted With Inappropriate Language and Contents About Mental Illness.
Some children reported that they were unhappy about being classified in a way that they would not describe themselves, e.g., being called a “young carer”, and were unhappy about not being asked whether they identified with that designation (47). Some participants reported that others gave them unwanted advice, such as recommending them to use birth control to avoid passing on mental illness to their children (42). One child remembers that her boyfriend's family reacted to her parent's mental illness saying “What if you two got married and you have children and they have a mental illness?” (42).
Experiencing Others Who Cannot Understand Them or Cope With Their Situation.
Often, children reported that people did not know how to act and cope with the information of parental illness [e.g., (48)]. One participant stated that they wished there was greater community awareness so “that they know there's nothing wrong—anyone could get it if they get stressed out—they could get it” (39). Some also reported that others failed to intervene, could make things worse (35), or that friends did not understand their experiences and they were disappointed in how friends responded (48). Some children emphasized that they wanted to talk to family members, but their parents and grandparents refused, and they felt unable to talk openly about such family issues (49, 50). A few children described having nobody to talk to and ask for help. They believed that this was due to taboos and others' ignorant behaviors [e.g., (35, 36)], having direct influences on their social interactions.
Experiencing Withdrawal and Rejection.
In addition, children perceived that others actively avoided them: for example, an adult child in Dam's study described, respectively (36) “When I met someone, they ignored me; they went over to the other side of the road”, as a result of having lived in a small community with a mentally-ill parent. Moreover, participants reported family members breaking off their relationship with them after finding out about their parent's illness (65), or experiencing the loss of friendships: “...my friend's mother called me over and told me that I couldn't be friends with her, because I'll be the same as my mother” (57).
Experiences of Hostile Behaviors of Others
Being the Victim of Bullying and Laughter.
Bullying (e.g., “I was bullied, the others laughed at me.”) (36) as one form of overt hostile behavior, was frequently mentioned: Children reported being: teased, laughed at, drawn into fights, and treated like a “leper” (36). A participant in Mordoch and Hall's (48) study stated that they “Sometimes [I] get in fights by accident” because other people labeled them as different. In another study, one participant wished that others would “stop teasing” (39).
Being Confronted With Hurtful Words.
Furthermore, children reported that their peers used stigmatizing words when talking about their ill parents, like ‘crazy' (36), ‘mad' (51), or their living situation as a ‘crazy house' (59).
Anticipated SBA—Fearing Reactions of Others in the Future
Regarding anticipated stigma in the future, similar topics that we identified in the experienced SBA emerged for anticipated SBA: Children feared overt hostile behaviors from others, as well as negative attitudes and ascriptions. They were also worried that others would not be able to understand and would reject them. Those generic categories are now presented together with their sub-categories.
Fearing Hostile Behaviors of Others
Fearing Ridicule.
When children were asked why they hesitate to tell others about their parent's mental illness, they described being afraid others would laugh at them (32, 57), and being afraid of being teased or bullied (33, 49).
Fearing Gossip.
Furthermore they feared that other people would share this information and gossip about them (33, 48). One participant describes her tendency to isolate herself due to fearing gossip and accompanying discrimination: “I was not able to develop close friendships at school because I had this fear of them coming home with me and seeing what it was like and then telling everybody at school and I would be a laughing stock” (33).
Fear of Negative Attitudes and Ascriptions
Fear of Being Labeled as “Different”.
Children frequently feared being labeled as “different from others” if people discovered their parent's mental illness. They thought people might believe their mothers, for example, might not act like other mothers [e.g., (60, 64)], or that they are “berserk” (33).
Fear of Other People's Negative Attitudes.
They also feared that others might be scared or have negative attitudes toward them or their family (52). One participant stated that they do not invite friends home because they are scared that others might think something bad about their family (33). Another child reported being scared of being judged or criticized for having a “whacko” father (46).
Fear for Parents to be Described as Bad.
Some children worried others might think their parents could not take care of them because of their mental illness and that they might be taken away (39, 57). One participant stated: “(…) It's just that I'm scared they'll put it down to her being a bad mum... she's not a bad mum, she loves us” (32).
Fearing Others' Lack of Understanding and Rejection
Fearing Others' Lack of Knowledge About Mental Illness and Lack of Understanding.
Moreover, children worried that others have little knowledge of mental illness (59) and that their situation and experiences will not be understood (57, 62). In some instances, they anticipated others' misconceptions and did not get any help, or tell anybody about it “because some children just do not know what this [mental illness] is and then just tell people that it is something really bad, that is stupid for you” (59). On the other hand, two participants in the study from Davison and Scott (37) anticipated that personal support interventions could even make things worse for children, in case other people try too hard to help them, leading to more worries and fear: “People sort of trying to help them too much when they don't have a problem could make people overthink things… It might increase the fear factor…”.
Fearing Withdrawal and Rejection.
They also feared others might withdraw from, reject (34, 41), or exclude them (33). Some children also feared losing contacts, such as relationships when their partner discovers their parent's mental illness: “I've got a girlfriend, should I tell her… I've been going out with her for 3 or 4 months…but she's never met my mother. And I do have a particular reason, for, like, putting it off as long as possible. And that, oh I don't know, feeling embarrassed, it's just the idea, I don't know actually. Let her get to know me first and if she likes me enough, then it won't make any difference any more” (22).
Affiliate Stigma—Internalizing the Stigma
The self-stigmatization of children manifested in two different ways, namely the two generic categories we identified: (1) perceiving themselves as being contaminated, and (2) perceiving themselves as being inferior. Both are now presented in more detail together with their subcategories.
Perceiving Themselves as Being Contaminated
Struggling to Avoid Being Contaminated.
van der Sanden et al. (30) found that adult children feared contamination. The fear of being contaminated relied on one of two components: Either (1) children knew about their status of being a member of an at-risk group for developing a mental illness, which could result in fear and self-reflexive sensitivity related to possible symptoms (58); or (2) they feared being seen as connected to their ill parent so closely that they would also be considered “crazy” (35): “My Mom is crazy, so they are going to think I am crazy”. One child reported that parental mental illness is something that cannot be discussed because it is like a “an infected tumor never to heal” (P9) (36). An online self-help group for adolescents with a mentally ill parent reduced these fears, as one participant described: “They seemed quite normal; after all, it was just that they had a terrible situation. Then I thought, “Oh my God, they are never going to be mentally ill like that.”... I felt it was less likely that I would also become like my mom.... Because [one of the participants] had a boyfriend, I felt that I too had a chance to get a boyfriend, friends, and live a completely normal life […]” (58).
Fearful of Passing It on.
One child reported fearing stigmatization being passed on to the next generation when they have children themselves (30), and thus characterize themselves as a possible source for transmitting mental illness.
Perceiving Themselves as Being Inferior
Feeling Ashamed and Embarrassed.
Beliefs of being inferior were mainly characterized by statements related to shame and embarrassment: Children often viewed their parents' mental illness as a “secret” (35, 44) that must be kept “behind closed doors” (31). One child described doing this to protect their parent from other people's stigmatizing behaviors (44). Often, children mentioned that they did not want anybody to know about their parent's mental health issues, but sometimes were unsure why they were ashamed, or did not want anybody to know: “And I do have a particular reason, for, like, putting it off as long as possible. And that, oh I don't know, feeling embarrassed, it's just the idea, I don't know actually” (22). Sometimes participants even reflected that this secrecy would keep them from establishing deep relationships, for example one participant said: “I avoid entering deep relations with others due to fear of explaining my situation” (51). One son of a father with a mental illness stated: “I wish my father had another disease and didn't suffer from mental illness. Father's illness is very bad for me. I am ashamed to speak about it and to communicate with others” (51). In the quantitative study by Haverfield and Theiss (61), intrafamilial topic avoidance regarding parental illness was also associated with magnified avoidance of disclosing the topic to others—this was evident in the male participants at least.
Perceiving Themselves as Different to Others.
Frequently, this shame, embarrassment, and disclosure was described as a result of being seen as “different”, “abnormal”, or “wrong”. A commonly mentioned experience for children was that they felt different from their peers (41, 49, 50), and the feeling of being different led them to think dichotomously, i.e., believing other families were “right”, while their own family was “wrong”: “Our family was wrong…we were just a dysfunctional, broken family, we just weren't normal like other families” (46).
Self-Blaming.
Self-blame was also identified in children: They were more likely to blame themselves for their parents' difficult situation than were children whose parents have no mental illness (31). One child explained: “I sometimes think it's my fault, I blame myself for the way my dad is feeling, even though he tells me it's not” (31).
Structural Discrimination—Perceiving Inequalities in Institutions and Within the Society
We identified three generic categories within the structural discrimination facet now discussed in more detail, namely perceived discrimination within (1) the mental health system; (2) the education system, and (3) other sources of discrimination
Perceiving Discrimination Within the Mental Health System.
Most of the references for structural discrimination related to interactions with the healthcare system: Children described interactions at the interpersonal level within the health care system, such as being treated insensitively, and perceived that doctors were afraid of them and maintained an emotional distance (50): “To visit mum in the hospital was like coming to an office. It was a nonexistent relationship, you know. Hello, Goodbye, You must go in that direction (P4)” (36). Furthermore, they felt ignored by staff (36). Due to feeling fear and insecure when visiting their parents in hospital, they wished that someone would stay with them and talk to them about their situation (36). On a broader institutional level, children strongly requested more general information about mental illness from mental health workers (32). Children remarked that the cold furniture in the hospitals made them feel uncomfortable (36). They also mention a general lack of care for their parents. They had the impression that their parents were getting inadequate healthcare, and were discharged due to inadequate bed capacity, leaving the children in charge of their parents: “After 2 weeks she was sent home, even though she didn't feel ready. I and my sister had to move home and take care of her ourselves. I will never forgive the psychiatric institution for what they did to me and my sister. We literally had to act like ‘extra mothers' to our own mother” (60).
Perceiving Discrimination Within the Education System
The education system was also identified as a source of structural discrimination: children complained of a lack of education about mental illness at school (32). They criticized a lack of understanding about students who have to look after their parents (39), with teachers ignoring their situation instead of talking with them “Well it's a very stereotypical town where you would never want to admit that anything is wrong... so a lot of it was hush hush. So, like, we'll give you a little extension on your homework. If you need someone to talk to you can go and talk to somebody. But we're not going to like, raise any ags” (33); see also (36, 62).
Other Sources of Structural Discrimination
Other sources of structural discrimination were the police (43, 57), media (31), and social work (57). Events experienced there or unclarified mandates from the institutions led to a mistrust in the children, who felt abandoned or did not seek help for fear of losing their parents (57). Above all, the general taboo around this topic was identified, which is not inherent in a specific organization, but rather within society in general, with people not talking to children about these problems, which might hinder children obtaining appropriate and useful information (49, 50, 58). Not getting any information about parental mental illness and its heritability or about their risks in general left children to overestimate their risk of developing a bipolar disorder themselves (37). One participant said: “I think knowing about the risk would be really helpful—I've always worried that I would get it (BD)” (37).
Discussion
We identified 32 studies for this review that investigated or addressed the stigma experiences of children with parents with a mental illness. The studies are heterogeneous in their design and methodological quality. Low-quality papers failed to state a comprehensible rationale for their data collection or analysis, or failed to sufficiently describe (or even recruit) a representative sample. More than half of the studies did not investigate stigma primarily, rather, they only identified stigma as an important problem for this population. Due to a mixed-up and vague measurement of stigma dimensions, we were only able to include one quantitative study and one mixed-method study. Qualitative content analysis was done inductively, and we were able to cluster our results in four stigma dimensions that match those absorbed in stigma theories (18, 19, 66): experienced SBA, anticipated SBA, affiliate stigma, and structural discrimination. We were able to fill those dimensions with content that is specific for the stigma experiences that the children of parents with a mental illness suffer, and we have thus closed the gap in showing that these theoretical categories were confirmed with qualitative content analyses, and that the stigma experiences that the children expressed align with theory. The affiliate stigma dimensions we identified highlight the close connections between stigma and feelings of guilt, isolation, and secrecy in affected children, supporting results of the review by Reupert et al. (25).
While this review does not enable causal conclusions about the health risks after stigmatizing experiences, our results demonstrate that such experiences are indeed stressful and likely to affect the health and well-being of those stigmatized, as conceptualized in the TTMD model (1, 7). Stigma is therefore no mere isolated mechanism that impairs a child's well-being—it is a mechanism interwoven and manifold on different levels in families with mental illness.
Dimensions of Stigma
Experienced SBA
Our findings regarding experienced SBA reveal that children do have experiences that are very specific to their role as the offspring of a parent with a mental illness. At school and in other areas of social life, they are bullied and teased. They often feel incapable of making strong connections with other people in a satisfying way, as they often sense the need to keep their parent's mental illness a secret. In their early years, children can experience—depending on the severity and symptoms of their parent's mental illness and the existence of reliable other family members—a lack of emotional support within their family (55, 56). For them therefore, relationships functioning as a secure base outside the family might be even more important than for other children. In adolescence, this can be problematic, as it is a life phase characterized by various developmental steps that include the establishment of new and meaningful relationships outside the primary family, and developing a strong sense of identity (70).
Anticipated SBA
As far as we know, anticipated stigma has not been described in the literature to characterize family members of people with a mental illness. This SBA dimension was identified in this review and was closely connected to feelings of fear and worry. This could be an important aspect of hiding the parent's mental illness and failing to seek help, and it supports the evidence from studies on the primary recipients of mental illness stigma, which showed that anticipated stigma and discrimination are key reasons for not seeking help [e.g.,(67)].
Affiliate Stigma
This review sheds light on how children might internalize the stigma. While some quantitative studies claimed that children are more apt to experience contamination, and that blame and shame play more important roles for the parents and spouses of people with a mental illness (13, 68), our review's results show that blame and shame are also important for children. This is especially true regarding the negative perception of themselves as being different from others—thereby perceiving themselves as inferior. This review reveals this as a specific and frequently mentioned self-stigma for children. This finding is in line with general stigma theories for primary recipients, which posit that a core component of stigma is the mark of otherness, which is then followed by negative evaluation (69). Children seem to internalize this otherness by feeling a sense of being “abnormal” or “wrong”. Park and Park's (71) family-stigma concepts could explain the frequent mention of feeling “different” identified in this review. According to their theory, general family stigma arises for two reasons: (1) it might be due to negative events (like the parental illness) or (2) to exceptional family structures. As structures in families with a parental illness differ in many ways [e.g., (53)] from those of other families, we can assume that such children are perceived and perceive themselves differently because of both labels. This may provide an explanation for the perceived family otherness so frequently cited in this review. Often, this otherness was associated with inferiority, which was considered a reason that this must be kept a secret and possibly keeping children and their families from seeking help. As previous research has shown for relatives of people with a mental illness, internalized stigmatization is especially associated with psychological problems such as reduced self-esteem—causing both psychological distress and lower quality of life (72, 73).
Structural Discrimination
Furthermore, our review demonstrates that structural discrimination is a key stigma dimension not only for those suffering from mental illness, but also for their children. A recently published systematic review (25) described structural discrimination being detected within law, medicine and education: in legal terms, for example, the greater likelihood of parents losing custody of their child, as well as being accused of having an “unsound mind” in all matters for people with mental illness. These are undoubtedly important findings for families and especially parents with a mental illness that probably affect the entire family system including children. Nevertheless, our review suggests that there is structural discrimination surpassing those descriptions that is described by the children themselves and which we clustered as an element of structural discrimination, as it occurs within institutions or characterizes a societal attitude that differs from individual attitudes. The results of the current review show that there is an inherent stigmatizing structure in different areas of society, e.g., schools and hospitals. For children, structural discrimination includes their parents' experiences, which in turn have consequences for themselves. This form of stigma also entails disadvantages personally experienced through various institutions. There is evidence that healthcare systems are a main source of children's structural discrimination. Children are affected by the lack of care offered or provided to their parents: They are often put in charge of taking care of their parents when hospitals/adult mental health professionals turn them away. Generally, the most significant themes within structural discrimination is the lack of education and information about mental illness, and society's tendency to ignore the subject. This prevents children from getting the necessary information and support to establish a healthy way of coping with their situation, like talking to others. Mental health literacy and positive family communication about the disorder are both known to be major protective factors for children (74, 75). However, the results of this review reveal a societal structure in which they do not get enough information at all.
Strengths and Limitations
This is the first systematic mixed-method review to explore and collate different facets of stigma for children of parents with a mental illness, focusing on the experience level of children themselves and grouping those facets into dimensions to inform how we conceive of affiliate stigma on the experience level. Having included both qualitative and quantitative study designs is a strength of this review—the topic is thus covered from different perspectives and with various measures. Furthermore, including both under-age and adult children deepens our knowledge of their stigma experiences: Views from children still living with their parent (as in about half of the included studies) provide information on how they are assessing their current situation. Retrospective views from adult children add important information, especially as some thoughts cannot be expressed and understood by children of younger ages, as they might not be aware of stigmatizing structures. For instance, children cannot anticipate that some stigmatizing experiences might influence their future in a specific way.
However, retrospective views can also lead to bias. Memories can change, and ascriptions made more easily [recall-bias (76)]. Secondly, we only included studies written in English or German, as well as peer-reviewed publications, and no gray literature. Thus, it is possible some important literature is missing. In addition, the studies mostly came from Western countries, restricting our results and conclusions to those cultures. As stigma is the result of the social context and therefore differs over time and cultures, the present review provides an overview of possible topics relevant for children, but to ensure generalizability, a wider range of cultures would need to be addressed. As most of the studies came from Europe, this review mainly contributes to understanding how stigma affects children of parents with a mental illness in European countries, which might well differ in other countries. Third, the quality of studies we included ranged from very low to very high quality. In many qualitative studies, data collection methods, analyses methods, as well as interview guidelines were not specified, which made it difficult to assess their quality and adequacy. In addition, we mainly included qualitative studies as we could only include one quantitative and one mixed-method study. The other quantitative studies of potential relevance had to be excluded because of their low relevance for this specific population, i.e., they only assessed which kinship status experienced more or less stigma by association, or they mixed up different stigma measures which made it impossible to classify the stigma.
Implications for Policy, Practice, and Future Research Directions
We propose several policy, practice, and research implications as a result of our review. Our findings highlight that much more education about mental illnesses for the general public, and especially children, is essential. Enhanced education about the risks and potential support networks that can lower those risks could lead to addressing some of these misconceptions and fears children may have: It could pave the way for a realistic evaluation of their own risks, but also various means of dealing with these risks. According to the literature on the manifold effects of stigma on relatives of people with mental illness [e.g., (14, 16, 22)] and our study results, we can assume that stigma is a major factor contributing to the transgenerational transmission of mental disorders. Thus, at the level of social factors contributing to mental illness, stigma represents a target for prevention and intervention programs for the children of parents with a mental illness. This should be highlighted when considering stigma for this population, and could make an important difference in developing strategies to reduce stigma. Overall, stigma-reducing interventions, in terms of minimizing the public stigma of people with a mental illness, as well as encouraging more openness and acceptance by “normalizing” mental health problems, and empowering people to talk openly about mental illness, would be a further promising step to escape the vicious circle of mental illness stigma that contributes to the transgenerational transmission of mental illness.
The review has shown that adult health care services seem to be an important source of discrimination: It is not just the fact that children feel so ignored and insensitively treated by healthcare staff, but also the atmospheres that keep kids from feeling comfortable that should be addressed. Hospital and psychiatric staff for adult health care should undergo training in engaging with the children of parents with a mental illness [see also (77)]. Other support structures need to be established to lessen the pressure children feel that it is up to them to look after their parents.
Our findings emphasize the need for individual investigations to determine whether different aspects are important for specific family members. They might indeed differ more than previous research suggests, considering the homogeneity of the questionnaires used for all family members. As very few studies have provided evidence about which aspects influence how strongly children experience stigma, there is a need for researchers to investigate additional factors in more detail and across more types of parental mental illnesses. Future research should focus on a deeper differentiation of stigma dimensions and how they interact, and on their impact on the health and well-being of this specific population, which is worldwide, large, and carries such a high risk.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
L-MD designed and completed the study, wrote the protocol, was involved as the main person in charge in all analyses steps, and wrote the manuscript. JF did the independent full text screening as the second rater and was involved in the studies' inclusion process. DP did the data extraction as second rater and was involved in the studies' inclusion process. JLP did the quality assessment for qualitative studies as a second rater, supported the intersubjective validity by discussing the categories, and supported the writing of the manuscript by reviewing and editing. AB did the quality assessment for quantitative studies and the mixed method study as a second rater, supported the intersubjective validity by discussing the categories, and supported the writing of the manuscript by reviewing and editing. HC functions as PhD advisor and supervised the study and preparation of manuscript and supported finding agreement between two independent raters by discussing ambiguous study inclusions. All authors contributed to the article and approved the submitted version.
Funding
The paper was written as part of a 4-year research project the Village funded by the Austrian Federal Ministry of Health—Science and Research through the Open Innovation in Science Center at the Ludwig Boltzmann Gesellschaft GmbH, hosted at the Medical University of Innsbruck, with collaboration of Co-Investigator institutions. The funders did not influence the collection, analysis, or interpretation of data, and played no role in writing the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
Authors would like to thank the whole Village team for their support during the entire process of creating and conducting this systematic review. Furthermore, authors would like to acknowledge the support of the librarian Susanne Waldmann of the Philipps University of Marburg in the systematic literature search. We would also like to acknowledge the contribution of Sara Evans-Lacko from the London School of Economics and Political Science in the compilation of the search strategy, as well as Feline Schelhammer, who supported the data management of the review within her student assistant job at the Philipps University of Marburg.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.813519/full#supplementary-material
Footnotes
1. ^Throughout our paper we mainly use the term “children” when referring to the children of people with a mental illness as this is the population of interest. This can also mean that we are talking about the adult children of parents with a mental illness—depending on the study population in the original papers—by using the term ‘children', referring to children of parents with a mental illness.
2. ^The coding guideline is available upon request.
3. ^Van der Sanden (22) and van der Sanden (30) stem from one study with different research questions but the same data; Cogan et al. (31) and Cogan et al. (32) also stem from one study.
References
1. Hosman CMH, van Doesum KTM, van Santvoort F. Prevention of emotional problems and psychiatric risks in children of parents with a mental illness in the Netherlands. I The scientific basis to a comprehensive approach. Aust e-J Adv Mental Health. (2009) 8:250–63. doi: 10.5172/jamh.8.3.250
2. Maybery D, Reupert AE. The number of parents who are patients attending adult psychiatric services. Curr Opin Psychiatry. (2018) 31:358–62. doi: 10.1097/YCO.0000000000000427
3. Maybery DJ, Reupert AE, Patrick K, Goodyear M, Crase L. Prevalence of parental mental illness in Australian families. Psychiatr bull. (2009) 33:22–6. doi: 10.1192/pb.bp.107.018861
4. Radicke A, Barkmann C, Adema B, Daubmann A, Wegscheider K, Wiegand-Grefe S. Children of parents with a mental illness. Predictors of health-related quality of life and determinants of child-parent agreement. Int J Environ Res Public Health. (2021) 18:379. doi: 10.3390/ijerph18020379
5. Rasic D, Hajek T, Alda M, Uher R. Risk of mental illness in offspring of parents with schizophrenia, bipolar disorder, and major depressive disorder. A meta-analysis of family high-risk studies. Schizophrenia Bull. (2014) 40:28–38. doi: 10.1093/schbul/sbt114
6. Reupert A, Maybery D. What do we know about families where parents have a mental illness? A systematic review. Child Youth Serv. (2016) 37:98–111. doi: 10.1080/0145935X.2016.1104037
7. Christiansen H, Reck C, Zietlow A-L, Otto K, Steinmayr R, Wirthwein L, et al. Children of Mentally III Parents at Risk Evaluation (COMPARE): Design and Methods of a Randomized Controlled Multicenter Study-Part I. Front Psychiatry. (2019) 10:128. doi: 10.3389/fpsyt.2019.00128
8. Pryor JB, Reeder GD, Monroe AE. The infection of bad company. Stigma by association. J Pers Social Psychol. (2012) 102:224–41. doi: 10.1037/a0026270
9. Phelan JC, Bromet EJ, Link BG. Psychiatric illness and family stigma. Schizophrenia Bull. (1998) 24:115–26. doi: 10.1093/oxfordjournals.schbul.a033304
10. DeFleur ML. Stigma: notes on the management of spoiled identity. In: Erving Goffman, Englewood Cliffs. New Jersey: Prentice-Hall (1963). 147 pp. Cloth, $4.50; paper, $1.95. In: Social Forces 43:127–128. doi: 10.1093/sf/43.1.127
11. Goffman E. Stigma. Notes on the management of spoiled identity. 26th pr. New York: Simon and Schuster (A Touchstone Book) (1986).
12. Goffman E. Stigma. Über Techniken der Bewältigung beschädigter Identität. 1. Aufl. Frankfurt/M.: Suhrkamp (Suhrkamp Taschenbuch, 235) (1967).
13. Corrigan P, Watson AC, Miller FE. Blame, shame, and contamination. The impact of mental illness and drug dependence stigma on family members. J Family Psychol. (2006) 20:239–46. doi: 10.1037/0893-3200.20.2.239
14. Larson JE, Corrigan P. The Stigma of Families with Mental Illness (2008). doi: 10.1176/appi.ap.32.2.87
15. Phillips SD, Gates T. A conceptual framework for anderstanding the stigmatization of children of incarcerated parents. J Child Fam Stud. (2011) 20:286–94. doi: 10.1007/s10826-010-9391-6
16. Angermeyer MC, Schulze B, Dietrich S. Courtesy stigma—a focus group study of relatives of schizophrenia patients. Soc Psychiatry Psychiatr Epidemiol. (2003) 38:593–602. doi: 10.1007/s00127-003-0680-x
17. Wahl OF, Harman CR. Family views of stigma. Schizophr Bull. (1989) 15:131–9. doi: 10.1093/schbul/15.1.131
18. Fox AB, Earnshaw VA, Taverna EC, Vogt D. Conceptualizing and Measuring Mental Illness Stigma. The mental illness stigma framework and critical review of measures. Stigma Health. (2018) 3:348–76. doi: 10.1037/sah0000104
19. Pescosolido BA, Martin JK. The stigma complex. Annu Rev Sociol. (2015). 41:87–116. doi: 10.1146/annurev-soc-071312-145702
20. Mak WWS, Cheung RYM. Affiliate stigma among caregivers of people with intellectual disability or mental illness. J Appl Res Intell Disabilities. (2008) 21:532–45. doi: 10.1111/j.1468-3148.2008.00426.x
21. Bos AER, Pryor JB, Reeder GD, Stutterheim SE. Stigma. Adv Theor Res Basic Appl Social Psychol. (2013) 35:1–9. doi: 10.1080/01973533.2012.746147
22. van der Sanden RLM, Stutterheim SE, Pryor JB, Kok G, Bos AER. Coping with stigma by association and family burden among family members of people with mental illness. J Nerv Ment Dis. (2014) 202:710–7. doi: 10.1097/NMD.0000000000000189
23. Corrigan P, Kerr A, Knudsen L. The stigma of mental illness. Explanatory models and methods for change. Appl Prevent Psychol. (2005) 11:179–90. doi: 10.1016/j.appsy.2005.07.001
24. van Loon LMA, van de Ven MOM, van Doesum KTM, Hosman CMH, Witteman CLM. Parentification, stress, and problem behavior of adolescents who have a parent with mental health problems. Fam Process. (2017) 56:141–53. doi: 10.1111/famp.12165
25. Reupert A, Gladstone B, Helena Hine R, Yates S, McGaw V, Charles G, et al. Stigma in relation to families living with parental mental illness. An integrative review. Int J Mental Health Nurs. (2021) 30:6–26. doi: 10.1111/inm.12820
26. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferring reporting items for systematic reviews and meta analyses: the PRISMA statement. J Clin Epidemiol. (2009) 62:1006–12. doi: 10.1371/journal.pmed.1000097
27. Hong QN, Pluye P, Fabregues S, Bartlett G, Boardman F, Cargo M, et al. Microsoft Word—MMAT_2018_criteria-manual_2018-08-08.docx (2018).
28. Hong QN, Pluye P, Bujold M, Wassef M. Convergent and sequential synthesis designs. Implications for conducting and reporting systematic reviews of qualitative and quantitative evidence. Syst Rev. (2017) 6:61. doi: 10.1186/s13643-017-0454-2
29. Kuckartz U, Rädiker S. Datenaufbereitung and Datenbereinigung in der qualitativen Sozialforschung. Nina Baur and Jörg Blasius (Hg) Handbuch Methoden der empirischen Sozialforschung Wiesbaden. Springer Fachmedien Wiesbaden:(2019) 441–56. doi: 10.1007/978-3-658-21308-4_31
30. van der Sanden RLM, Bos AER, Stutterheim SE, Pryor JB, Kok G. Stigma by association among family members of people with a mental illness. A qualitative analysis. J Community Appl Soc Psychol. (2015) 25:400–17. doi: 10.1002/casp.2221
31. Cogan N, Riddell S, Mayes G. Children living with an affectively ill parent. How do they cope? Educ Child Psychol. (2005) 22:16–28.
32. Cogan N, Riddell S, Mayes G. The anderstanding and experiences of children affected by parental mental health problems. A qualitative study. Qual Res Psychol. (2005) 2:47–66. doi: 10.1191/1478088705qp024oa
33. Blakeman M, Martin C, Gupta A. Making sense of growing up with a parent with psychosis. An interpretative phenomenological analysis study. Psychosis. (2019) 11:54–62. doi: 10.1080/17522439.2019.1573916
34. Bolas H, van Wersch A, Flynn D. The well-being of young people who care for a dependent relative. An interpretative phenomenological analysis. Psychol Health. (2007) 22:829–50. doi: 10.1080/14768320601020154
35. Carroll L, Tuason MTG. Perpetually self-reflective. Couns Psychol. (2015) 43:1059–83. doi: 10.1177/0011000015602316
36. Dam K, Joensen DG, Hall EOC. Experiences of adults who as children lived with a parent experiencing mental illness in a small-scale society. A qualitative study. J Psychiatric Mental Health Nurs. (2018) 25:78–87. doi: 10.1111/jpm.12446
37. Davison J, Scott J. Should we intervene at stage 0? A qualitative study of attitudes of asymptomatic youth at increased risk of developing bipolar disorders and parents with established disease. Early Interven Psychiatry. (2018) 12:1112–9. doi: 10.1111/eip.12421
38. Haug Fjone H, Ytterhus B, Almvik A. How children with parents suffering from mental health distress search for ‘Normality' and avoid stigma. J Glob child Res. (2009) 16:17.
39. Fudge E, Mason P. Consulting with young people about service guidelines relating to parental mental illness. Aus e-J Adv Mental Health. (2004) 3:50–8. doi: 10.5172/jamh.3.2.50
40. Griffiths J, Norris E, Stallard P, Matthews S. Living with parents with obsessive-compulsive disorder. Children's lives and experiences. Psychol Psychother. (2012) 85:68–82. doi: 10.1111/j.2044-8341.2011.02016.x
41. Kadish Y. Five women's recollections and reflections on being raised by a mother with psychosis. S Afr J Psychol. (2015) 45:480–94. doi: 10.1177/0081246315581565
42. Karnieli-Miller O, Perlick DA, Nelson A, Mattias K, Corrigan P, Roe D. Family members' of persons living with a serious mental illness. Experiences and efforts to cope with stigma. J Mental Health. (2013) 22:254–62. doi: 10.3109/09638237.2013.779368
43. Krupchanka D, Kruk N, Murray J, Davey S, Bezborodovs N, Winkler P, et al. Experience of stigma in private life of relatives of people diagnosed with schizophrenia in the Republic of Belarus. Soc Psychiatry Psychiatr Epidemiol. (2016) 51:757–65. doi: 10.1007/s00127-016-1190-y
44. Leahy MA. Children of mentally ill parents. Anderstanding the effects of childhood trauma as it pertains to the school setting. Int J Educ Res. (2015) 71:100–107. doi: 10.1016/j.ijer.2015.04.005
45. Leinonen A, Seikkula J, Alasuutari M. Can I tell just by myself? Discussing a parental mental disorder with a child in a research interview. Int J Child, Youth Family Stud. (2016) 7. doi: 10.18357/ijcyfs.71201615675
46. McCormack L, White S, Cuenca J. A fractured journey of growth. Making meaning of a ‘Broken' childhood and parental mental ill-health. Community, Work Family. (2016) 20:327–45. doi: 10.1080/13668803.2015.1117418
47. Moore T, McArthur M, Noble-Carr D. Different but the same? Exploring the experiences of young people caring for a parent with an alcohol or other drug issue. J Youth Stud. (2010) 14:161–77. doi: 10.1080/13676261.2010.522561
48. Mordoch E, Hall WA. Children's perceptions of living with a parent with a mental illness. Finding the rhythm and maintaining the frame. Qual Health Res. (2008) 18:1127–44. doi: 10.1177/1049732308320775
49. Murphy G, Peters K, Wilkes L, Jackson D. Adult children of parents with mental illness. Navigating stigma. Child Family Social Work. (2015) 22:330–8. doi: 10.1111/cfs.12246
50. Nieto-Rucian V, Furness PJ. The experience of growing up with a parent with schizophrenia—A qualitative study. In: Qualitative Psychology (2017).
51. Oskouie F, Zeighami R, Joolaee S. Outcomes of parental mental illness on children. A qualitative study from Iran. J Psychosocial Nurs Mental Health Serv. (2011) 49:32–40. doi: 10.3928/02793695-20110802-06
52. Ostman M. Interviews with children of persons with a severe mental illness. Investigating their everyday situation. Nordic J Psychiatry. (2008) 62:354–9. doi: 10.1080/08039480801960065
53. Reedtz C, Lauritzen C, Stover YV, Freili JL, Rognmo K. Identification of Children of Parents With Mental Illness. A Necessity to Provide Relevant Support. Front Psychiatry. (2019) 9:358. doi: 10.3389/fpsyt.2018.00728
54. Stengler-Wenzke K, Trosbach J, Dietrich S, Angermeyer MC. Experience of stigmatization by relatives of patients with obsessive compulsive disorder. Arch Psychiatr Nurs. (2004) 18:88–96. doi: 10.1016/j.apnu.2004.03.004
55. Tabak I, Zabłocka-Zytka L, Ryan P, Poma SZ, Joronen K, Viganò G, et al. Needs, expectations and consequences for children growing up in a family where the parent has a mental illness. Int J Ment Health Nurs. (2016) 25:319–29. doi: 10.1111/inm.12194
56. Trondsen MV. Living with a mentally ill parent: exploring adolescents' experiences and perspectives. Qual Health Res. (2012) 22::174–88. doi: 10.1177/1049732311420736
57. Tamutiene I, Jogaite B. Disclosure of alcohol-related harm: children's experiences. Nordisk Alkohol Narkotikatidskrift. (2019) 36:209–22. doi: 10.1177/1455072518807789
58. Trondsen MV, Tjora A. Communal normalization in an online self-help group for adolescents with a mentally ill parent. Qual Health Res. (2014) 24:1407–17. doi: 10.1177/1049732314547708
59. Wahl P, Otto C, Lenz A. dann würde ich traurig werden, weil alle über meinen Papa reden“—Die Rolle des Stigmas in Familien mit psychisch erkranktem Elternteil. Gesandheitswesen (Bandesverband der Arzte des Offentlichen Gesandheitsdienstes (Germany)). (2017) 79:987–92. doi: 10.1055/s-0043-122234
60. Widemalm M, Hjärthag F. The forum as a friend. Parental mental illness and communication on open Internet forums. Social Psychiatry Psychiatric Epidemiol. (2015) 50:1601–7. doi: 10.1007/s00127-015-1036-z
61. Haverfield MC, Theiss JA. Parent's alcoholism severity and family topic avoidance about alcohol as predictors of perceived stigma among adult children of alcoholics: Implications for emotional and psychological resilience. Health Commun. (2016) 31:606–16. doi: 10.1080/10410236.2014.981665
62. Gray B, Robinson C, Seddon D. Invisible children. Young Carers of Parents with Mental Health Problems—The Perspectives of Professionals. Child Adolesc Mental Health. (2008) 13:169–72. doi: 10.1111/j.1475-3588.2007.00477.x
63. Rezayat F, Mohammadi E, Fallahi-Khoshknab M, Sharifi V. Experience and the meaning of stigma in patients with schizophrenia spectrum disorders and their families. A qualitative study .Jpn J Nurs Sci. (2019) 16:62–70. doi: 10.1111/jjns.12212
64. Haug Fjone H, Ytterhus B, Almvik A. How children with parents suffering from mental health distress search for ‘normality' and avoid stigma. Childhood. (2009) 16:461–77. doi: 10.1177/0907568209343743
65. Rezayat F, Mohammadi E, Fallahi-Khoshknab M. The process of responding to stigma in people with schizophrenia spectrum disorders and families. A groanded theory study. Perspect Psychiatric Care. (2019) 56:564–73. doi: 10.1111/ppc.12468
66. CORRIGAN PW, Markowitz FE, Watson AC. Structural levels of mental illness stigma and discrimination. Schizophr Bull. (2004) 30:481–91. doi: 10.1093/oxfordjournals.schbul.a007096
67. Schomerus G, Angermeyer MC. Stigma and its impact on help-seeking for mental disorders. What do we know? Epidemiologia e psichiatria sociale. (2008) 17:31–7. doi: 10.1017/S1121189X00002669
68. van der Sanden RLM, Bos AER, Stutterheim SE, Pryor JB, Kok G. Experiences of stigma by association among family members of people with mental illness. Rehabil Psychol. (2013) 58:73–80. doi: 10.1037/a0031752
69. Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. (2001) 27:363–85. doi: 10.1146/annurev.soc.27.1.363
70. Havighurst RJ. Developmental Tasks and Education. 3rd ed. New York, NY: McKay and Company (1972).
71. Park S, Park KS. Family Stigma. A Concept Analysis. Asian Nurs Res. (2014) 8:165–71. doi: 10.1016/j.anr.2014.02.006
72. van der Sanden RLM, Pryor JB, Stutterheim SE, Kok G, Bos AER. Stigma by association and family burden among family members of people with mental illness. The mediating role of coping. Soc Psychiatry Psychiatr Epidemiol. (2016) 51:1233–45. doi: 10.1007/s00127-016-1256-x
73. Ostman M, Kjellin L. Stigma by association. Psychological factors in relatives of people with mental illness. Br J Psychiatry. (2002) 181:494–8. doi: 10.1192/bjp.181.6.494
74. Riebschleger J, Tableman B, Rudder D, Onaga E, Whalen P. Early outcomes of a pilot psychoeducation group intervention for children of a parent with a psychiatric illness. Psychiatr Rehabil J. (2009) 33:133–41. doi: 10.2975/33.2.2009.133.141
75. Reupert AE, Maybery J, Darryl K, Kowalenko NM. Children whose parents have a mental illness. Prevalence, need and treatment. MJA Open. (2012) 1:7–9. doi: 10.5694/mjao11.11200
76. Coughlin SS. Recall bias in epidemiologic studies. J Clin Epidemiol. (1990) 43:87–91. doi: 10.1016/0895-4356(90)90060-3
Keywords: children of parents with mental illness, stigma, child mental health, systematic review, qualitative content analysis
Citation: Dobener L-M, Fahrer J, Purtscheller D, Bauer A, Paul JL and Christiansen H (2022) How Do Children of Parents With Mental Illness Experience Stigma? A Systematic Mixed Studies Review. Front. Psychiatry 13:813519. doi: 10.3389/fpsyt.2022.813519
Received: 11 November 2021; Accepted: 10 January 2022;
Published: 18 February 2022.
Edited by:
Francisco José Eiroa-Orosa, University of Barcelona, SpainReviewed by:
Joanna Fox, Anglia Ruskin University, United KingdomSami Richa, Saint Joseph University, Lebanon
Copyright © 2022 Dobener, Fahrer, Purtscheller, Bauer, Paul and Christiansen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lisa-Marie Dobener, bGlzYS1tYXJpZS5kb2JlbmVyQHVuaS1tYXJidXJnLmRl
†ORCID: Lisa-Marie Dobener orcid.org/0000-0001-8901-2312
Julia Fahrer orcid.org/0000-0002-1661-9313
Daniel Purtscheller orcid.org/0000-0002-9993-262X
Annette Bauer orcid.org/0000-0001-5156-1631
Jean Lillian Paul orcid.org/0000-0003-0891-7035
Hanna Christiansen orcid.org/0000-0002-8104-0711
 Lisa-Marie Dobener
Lisa-Marie Dobener Julia Fahrer
Julia Fahrer Daniel Purtscheller2,3†
Daniel Purtscheller2,3† Annette Bauer
Annette Bauer Jean Lillian Paul
Jean Lillian Paul Hanna Christiansen
Hanna Christiansen