- 1Department of Neurobiology, Faculty of Natural Sciences, University of Haifa, Haifa, Israel
- 2Faculty of Social Welfare and Health Sciences, University of Haifa, Haifa, Israel
- 3Division of Health Systems Policy and Administration, Faculty of Social Welfare and Health Sciences, University of Haifa, Haifa, Israel
Background: Although telemedicine care has grown in recent years, telepsychiatry is growing at a slower pace than expected, because service providers often hamper the assimilation and expansion of telepsychiatry due their attitudes and perceptions. The unified theory of acceptance and use of technology (UTAUT) is a model that was developed to assess the factors influencing the assimilation of a new technology. We used the UTAUT model to examine the associations between the attitudes and perceptions of psychiatrists in Israel toward telepsychiatry and their intention to use it.
Methods: An online, close-ended questionnaire based on a modified UTAUT model was distributed among psychiatrists in Israel. Seventy-six questionnaires were completed and statistically analyzed.
Results: The behavioral intention of Israeli psychiatrists to use telepsychiatry was relatively low, despite their perceptions of themselves as capable of high performance with low effort. Nonetheless, they were interested in using telepsychiatry voluntarily. Experience in telepsychiatry, and to a lesser extent, facilitating conditions, were found to be positively correlated with the intention to use telepsychiatry. Psychiatrists have a positive attitude toward treating patients by telepsychiatry and perceive its risk as moderate.
Discussion: Despite high performance expectancy, low effort expectancy, low perceived risk, largely positive attitudes, high voluntariness, and the expectancy for facilitating conditions, the intention to use telepsychiatry was rather low. This result is explained by the low level of experience, which plays a pivotal role. We recommend promoting the facilitating conditions that affect the continued use of telepsychiatry when initiating its implementation, and conclude that it is critical to create a sense of success during the initial stages of experience.
Introduction
In the Western world, increases in both life expectancy and chronic morbidity have greatly enhanced the demand for medical services, resulting in an overburdened health system. One of the main difficulties that public mental health services are facing is the discrepancy between supply and demand, as mental disorders are among the most prevalent illnesses in Western civilization (1), while there is a global shortage of mental health professionals in general, and of psychiatrists, in particular. The global median number of psychiatrists is ~1:100,000 people, making them a rare resource in mental health systems around the world (2). In an attempt to mitigate the shortage in human medical resources, to increase access to mental health services, and to reduce psychiatrists' burnout without compromising quality and satisfaction, there is a recommendation to use telemedicine in mental health (3, 4). Telemedicine is defined as “the delivery of health care and the exchange of health-care information across distances” (5). Previous research supports the claim that telehealth interventions can effectively shorten waiting lists and improve the coordination of specialist services (6).
Within telemedicine, telepsychiatry is defined as the use of communication technology to provide or support psychiatric services across distances. It usually refers to video-calls, which enable interactive, live, and colorful two-way communication (7). Randomized controlled trials comparing video-based interventions with face-to-face (FTF) interventions have shown that in most of the disorders examined—depression (8) anxiety (9), post-trauma (10), eating disorders (11), substance abuse (12), and suicide prevention (13)—the outcomes are comparable. Moreover, other studies have suggested that mental health care provided via video calls is equivalent to FTF interventions for creating and maintaining a solid rapport, and a satisfying therapeutic relationship between physicians and patients (14, 15). In general, both providers and patients were satisfied with telepsychiatry and found it acceptable, but patients reported higher satisfaction than did service providers. In addition, telepsychiatry has some economic benefits, as it reduces the direct and indirect costs of health care and increases the quality of life of patients in adjusted years when compared to FTF (16).
Although telemedicine care has increased significantly in recent years, telepsychiatry assimilation has been slower than expected, because the service providers, not the patients, have hampered its assimilation and expansion (17). The most frequently identified barriers for its acceptance were the licensing regulations, risks to patient confidentiality, concerns regarding reimbursement of expenses, patient safety, and interoperability (16, 18, 19). Clinicians' perspectives served as gatekeepers for the implementation and sustainability of telepsychiatry services (17), and despite the multiple benefits of telepsychiatry, studies have shown that various barriers prevent its assimilation and optimal use, and it is critical that psychiatrists support telepsychiatry (20). If psychiatrists are not prepared to use it at the clinical level, it will not be accessible for the patient to use (21).
In Israel, the therapeutic mental health care system is based in the community and supplied by the health maintenance organizations (HMOs). Accessibility to health services varies between regions, being usually lower in the periphery (22), and there is a severe shortage of psychiatrists (23). Hence, telepsychiatry has the potential to alleviate this shortage by enhancing the efficiency of mental health services. Therefore, the need to assess barriers and incentives for the use of telepsychiatry in Israel has emerged.
One of the most widely used models for investigating the acceptance of new technologies is the unified theory of acceptance and use of technology (UTAUT) model, aimed at understanding the concept of “actual use” and its estimation. The term “behavioral intention to use” was formulated to predict the behavior of using a technology (24).
The present study seeks to examine various aspects related to psychiatrists attitudes toward telepsychiatry. In particular, we aim to examine the extent to which psychiatrists in Israel show a behavioral intention to use telepsychiatry, and to identify the factors that may constitute an obstacle, or alternatively, encourage psychiatrists to use telepsychiatry. Assessment of the intent to use telepsychiatry was based upon variables derived from the UTAUT model using a validated questionnaire. This study, which was executed before the use of telemedicine services became more frequent in Israel during COVID-19, may provide a baseline for further studying the use of telepsychiatry. In addition, it can enable a better understanding of the barriers and incentives toward telepsychiatry assimilation amongst psychiatrists. This comprehension can assist in designing an effective policy to make psychiatric services more accessible.
Based on the UTAUT model (Figure 1) (24), we hypothesize that:
H1: The effect of performance expectancy on behavioral intention will be correlated with gender and age. We predict that the correlation will be stronger for men, particularly younger men.
H2: The effect of effort expectancy on behavioral intention will be correlated with gender, age, and experience. We predict that the correlation will be stronger for women, particularly younger women, and particularly in the early stages of experience.
H3: The effect of social influence on behavioral intention will be correlated with gender, age, voluntariness, and experience. We predict that the correlation will be stronger for women, particularly older women, particularly in mandatory settings in the early stages of experience.
H4: Facilitating conditions will not be significantly correlated with behavioral intention.
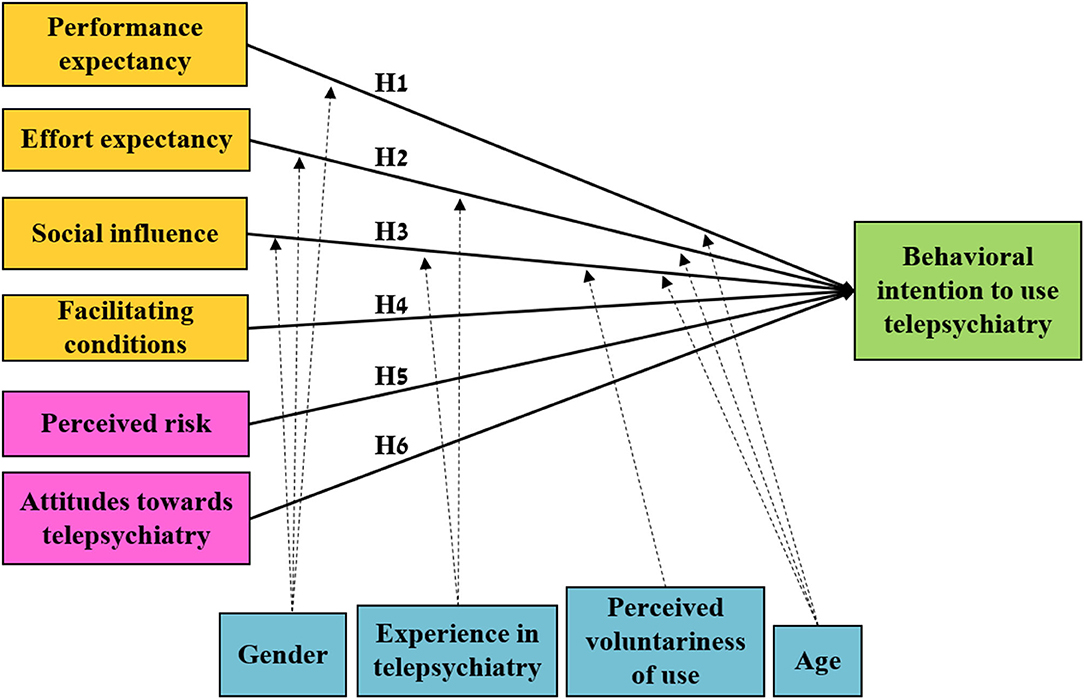
Figure 1. An illustration of the modified UTAUT model used in the study. The model is similar to the UTAUT model, except for the addition of the perceived risk and attitudes toward telepsychiatry variables. Orange and pink—independent variables, blue—confounding variables (covariables), green—dependent variable.
In addition, based on previous findings that attitudes toward technology (25) and perceived risk of practicing electronic health (26) are correlated to behavioral intention to practice health technology (Figure 1), we hypothesis that:
H5: Perceived risk will be negatively correlated to behavioral intention.
H6: Attitudes toward telepsychiatry will be positively correlated with behavioral intention.
Materials and Methods
We used a modified version of the UTAUT model (Figure 1) (24). Since telepsychiatry is not yet commonly used in Israel, we defined “behavioral intention to use telepsychiatry” as the dependent variable in our study, and tested its association with four independent variables. Three of these variables have been found to be associated with the intention to use: Performance expectancy, Effort expectancy, and Social influence. The fourth variable, Facilitating conditions, is associated with actual use (24). All variables are defined in Supplementary Table 1. In addition, the UTAUT model contains four confounding variables (i.e., covariables): gender, age, experience, and perceived voluntariness of use. Perceived voluntariness of use reflects the interest in using telepsychiatry voluntarily, and not only when mandatory. The framework of this model frequently requires modification for its application in complex health care settings (19).
To examine the attitudes of psychiatrists toward confidentiality and privacy when using telepsychiatry, we defined the variable, perceived risk, as the potential for loss in the pursuit of a desired outcome of using an e-service (27). The UTAUT model also incorporates attitudes toward telemedicine and the use of technology in general, but to estimate these two elements, we used two additional questionnaires; the attitude toward telemedicine in psychiatry and psychotherapy (ATIPP) questionnaire, and the attitude toward using technology questionnaire. The ATIPP questionnaire examines the attitudes of psychiatrists toward specific aspects of telemedicine in mental health (25), while the attitude toward using technology questionnaire estimates an individual's overall affective reaction to using a system (24). Altogether, according to the UTAUT model, all of the aforementioned variables should be associated with the outcome of behavioral intention, which refers to the individual's motivation regarding the performance of a given behavior (28).
The questionnaire used in this study was based on previous UTAUT model studies and was distributed online using Qualtrics software. The study used a convenience sampling of psychiatrists who practice psychiatry in Israel. The questionnaire was distributed via lists of email addresses of all registered psychiatrists in the Israeli Medical Association (IMA). The survey data were collected from November 2019 to April 2020, mostly before the COVID-19 pandemic. The study was ethically approved by the University of Haifa Ethics Committee.
Participants
The participants were Israeli board-certified psychiatrists who work in Israel's public and private health systems, and psychiatry residents who work in Israel's public health system. The survey was based on responses to an online questionnaire. The questionnaire was anonymous and participants stated that they were psychiatrists and agreed to participate in the survey.
The survey link was sent by email via the Israeli Psychiatric Association (IPA), which is the official union of psychiatrists within the IMA. The link was sent to all member psychiatrists including managers of psychiatric hospitals, psychiatric departments in general hospitals, mental health centers and psychiatric clinics. Subsequently, the managers of these facilities were asked several times to encourage and distribute the survey among the psychiatrists in their facilities.
Out of 100 respondents who agreed to participate in the online survey, 76 completed the survey. The remaining 24 respondents began the survey but did not complete it and their responses were excluded.
Measures and Questionnaires
The survey comprised demographic variables (age, gender, religion, native language, years of experience in psychiatry, geographical area of work, job title, and place of work). Each of the independent variables of UTAUT—Performance expectancy, Effort expectancy, Social influence, and Facilitating conditions—were tested using four questions, and the dependent variable, behavioral intention, was tested using three questions. The variables, experience, and perceived voluntariness of use were tested using one question each (24). Attitude toward using technology, was tested using the ATIPP questionnaire, comprising eight questions; Cronbach's alpha for the physicians' version of the questionnaire used in this study was 0.827 (25). Perceived risk—a question taken from a study about physicians' perceptions of trust in the system and risk-related factors, was divided into two questions in the present study (26). In the demographic questionnaire, psychiatrists could choose more than one option when answering the question about job title and place of work.
All variables were measured on a 5-point Likert scale ranging from strongly disagree to strongly agree, except for experience, which was measured on a scale of 1–3 (not at all, little and much experience). For statistical calculations, the scores for this variable were divided into two groups: without experience (1) and with experience (2-3). For variables with more than one question, the mean value was used for statistical analyses.
Since telemedicine has not been used often in Israel, some of the questions in the UTAUT model were adjusted to future tense. The questionnaire was delivered in Hebrew. To confirm the quality of translation, the questions were translated into Hebrew and then back-translated to English by independent qualified personnel. Following the back translation, the two English versions were compared.
The English versions of the UTAUT and ATIPP questionnaires are in the Supplementary Materials.
Data Analysis
The Qualtrics online survey responses were exported to SPSS. Descriptive statistics were calculated for the demographic variables (mean, standard deviation, frequency, and percentages). Three hypotheses, H1, H2, and H3, were analyzed using linear regressions (unstandardized coefficients B, unstandardized coefficients standard error, and adjusted R2). The other hypotheses, H4, H5, and H6, were tested using Pearson correlations. Significance was determined at P < 0.05. The rationale for presenting the separate regressions for each hypothesis is the small N.
Results
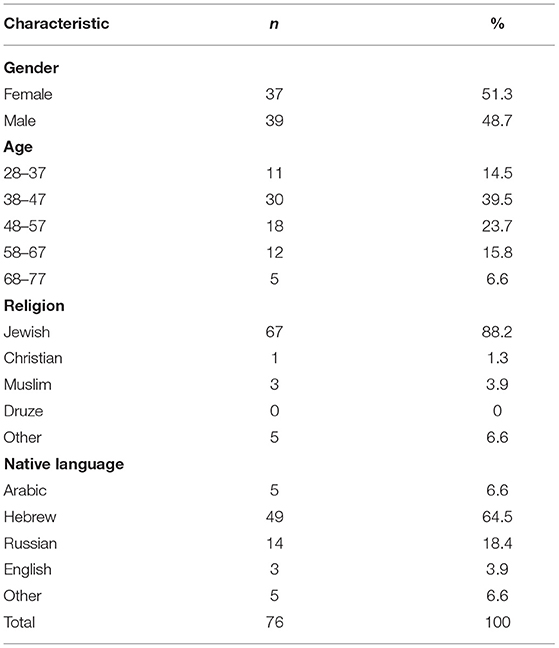
One hundred psychiatrists initially responded to the survey, of whom 76 psychiatrists completed the survey and participated in the study. This represents ~10% of the practicing psychiatrists in Israel. The data collected included demographic data (Table 1) and data related to their professional occupation as psychiatrists (Table 2). The study sample had similar participation of men and women (male = 39, female = 37) (Table 1). The age of the participants ranged from 28 to 77. Most participants were of Jewish origin (88%) and most participants worked in Tel Aviv and the central region of Israel (31.6%), a fair representation of the population distribution in the country which is 40% in Tel Aviv and the Central District, 13% in the Jerusalem District, 29% in Haifa and the Northern District, and 15% in the South and Shfela (29) (Table 2).
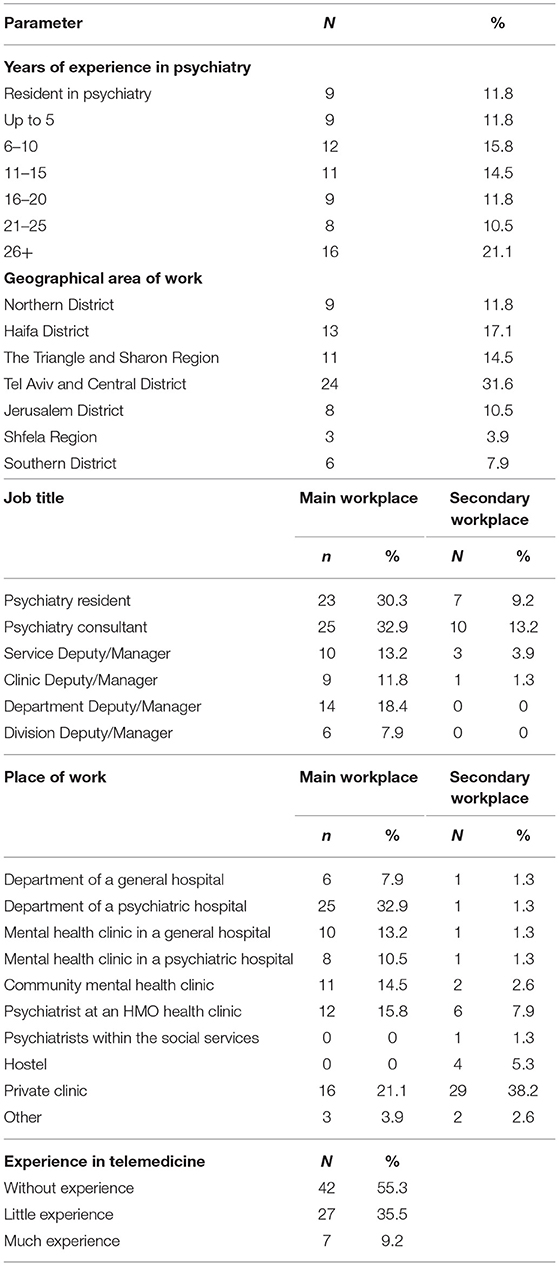
Table 2. Profession-related data of the survey participants (n = 74, as two participants did not provide demographic data).
The distribution of years of experience was quite homogenous, with 21% of participants having over 26 years of experience (Table 2). The position levels—resident, consultant, or managerial position—were also distributed almost equally between these three levels. Psychiatrists could choose more than one option if they worked as both consultants and managers. Nearly one third of the participants worked in a department within a mental health institute as their primary workplace, while the others were distributed among other workplaces. Approximately 59% of psychiatrists also worked in a private clinic, either as their primary workplace (main position and time dedication) or their secondary workplace (Table 2).
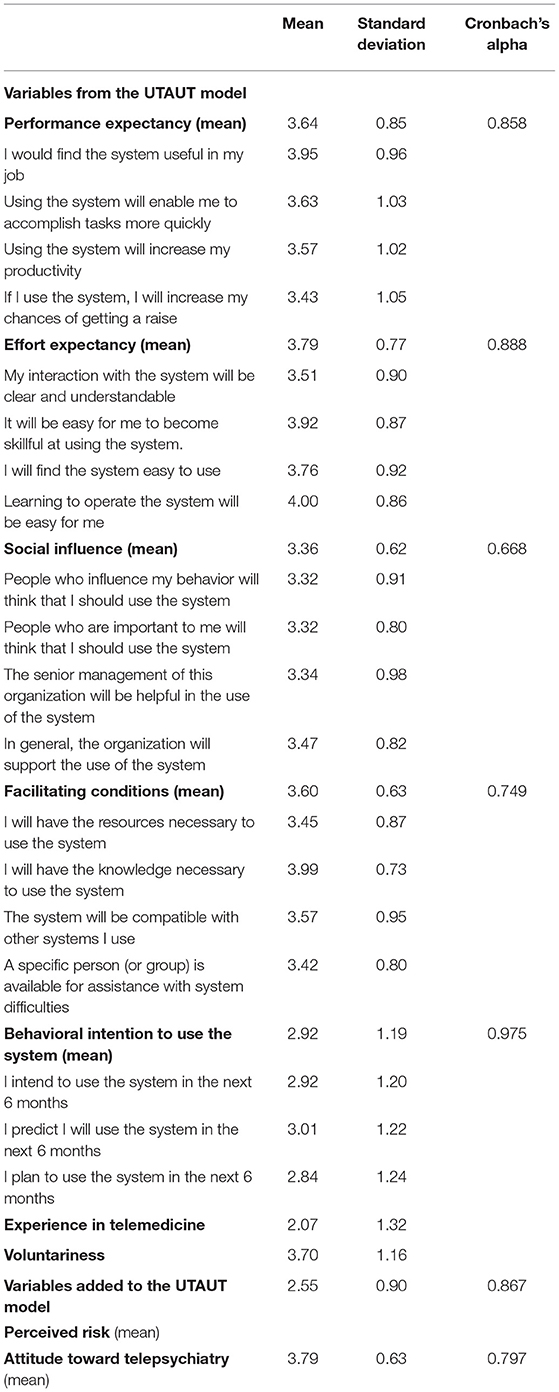
Since our primary reference framework was the UTAUT model, data are presented in accordance with the UTAUT variables. Cronbach's alpha mostly ranged from acceptable to good (0.668–0.975), confirming a reasonable to high internal consistency within our questionnaire, with the exception of the social influence, which had a value of 0.67 (Table 3). Experience using the technology and voluntariness to use the technology were each based on a single question (Table 3).
Overall, the data show that although the values of the independent variables (Effort expectancy, Performance expectancy, Social influence and Facilitating conditions) were rather high (3.4–3.8), including Perceived voluntariness of use (3.70), the dependent variable of the model (Behavioral intention) was quite low (2.9) (Table 3). The only independent variable that was also low was personal experience in telepsychiatry (Experience = 2.07) (Table 3). This variable comprised 55.3% psychiatrists without experience, 35.5% with little experience, and only 9.2% with much experience. Despite the average low experience, Israeli psychiatrists perceive themselves as capable of high performance (3.64) and believe that using telepsychiatry will require a low effort (3.70) (Table 3). Furthermore, they perceive the facilitating conditions as being quite good (3.60) (Table 3).
We note that the variables added to the UTAUT model in the present study, perceived risk and attitudes, indicated a largely positive attitude toward telepsychiatry (3.79) with a low perceived risk (2.55) (Table 3).
Behavioral Intention to Use Telepsychiatry Is Correlated With Performance Expectancy, Age, and Gender (H1)
The linear regression between the dependent variable, behavioral intention to use telepsychiatry, and the independent variables, performance expectancy, age, and gender, showed that behavioral intention to use telepsychiatry was strongly correlated with performance expectancy and gender [F(3,72) = 9.933, P <0.01, adjusted R2 = 0.263] (Table 4). The correlation was stronger for men. Interestingly, there was no correlation with age.
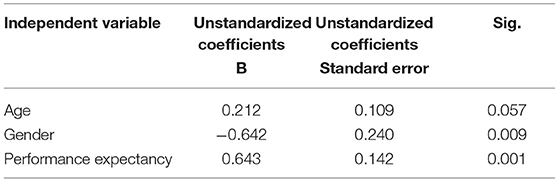
Table 4. Linear regression of behavioral intention to use telepsychiatry on performance expectancy, age, and gender.
Behavioral Intention to Use Telepsychiatry Is Correlated With Effort Expectancy and Experience (H2)
Similarly, linear regression analysis show that behavioral intention to use telepsychiatry, and the independent variables, effort expectancy, experience, age, and gender, showed that behavioral intention to use telepsychiatry was strongly correlated with effort expectancy and experience [F(4,71) = 10.83, P < 0.01, and adjusted R2 = 0.344] (Table 5); however, there was no correlation with age or gender.
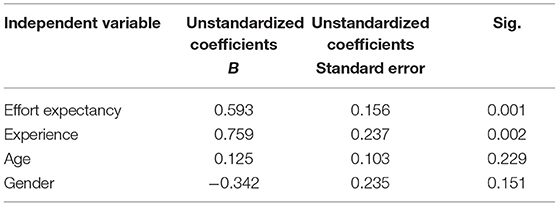
Table 5. Linear regression of behavioral intention to use telepsychiatry on effort expectancy, experience, age, and gender.
Behavioral Intention to Use Telepsychiatry Is Correlated With Experience and Voluntariness (H3)
The linear regression analysis of the dependent variable, behavioral intention to use telepsychiatry, on the independent variables, social influence, experience, age, gender, and voluntariness, showed that behavioral intention to use telepsychiatry was strongly correlated with experience in using telepsychiatry and voluntariness [F(5,70) = 8.108, P < 0.01, and adjusted R2 = 0.322] (Table 6). However, there was no correlation with age, gender, or social influence.
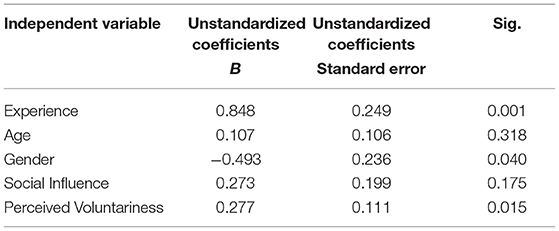
Table 6. Linear regression of behavioral intention to use telepsychiatry on experience, age, gender, social influence, and perceived voluntariness of use.
The Relationship Between Behavioral Intention to Use Telepsychiatry and Facilitating Conditions (H4)
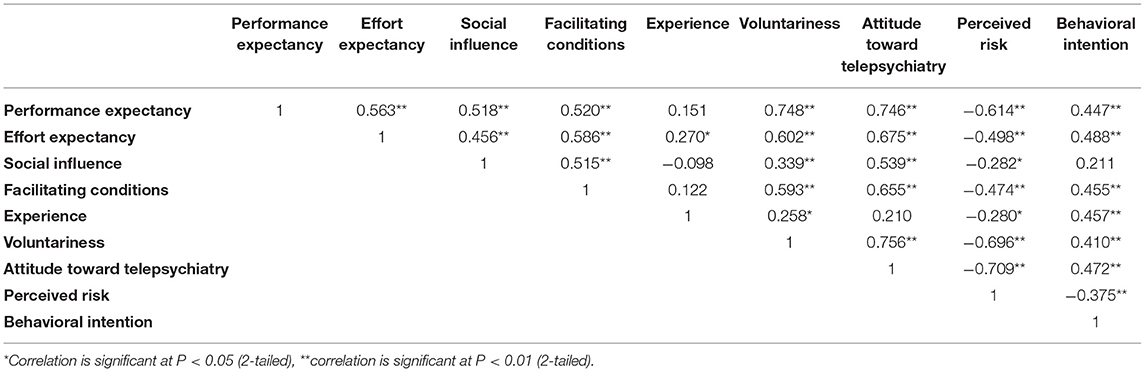
The Pearson correlation analysis between behavioral intention to use telepsychiatry and facilitating conditions showed a strong to moderate positive relationship [r(76) = 0.45, p < 0.01] (Table 7). This finding was in contrast to our hypothesis that facilitating conditions will not have a significant effect on behavioral intention.
The Relationship Between Behavioral Intention to Use Telepsychiatry and Perceived Risk (H5)
The Pearson correlation between behavioral intention to use telepsychiatry and perceived risk showed a moderate, negative relationship [r(76) = −0.37, p < 0.01] (Table 7). This finding is consistent with our hypothesis that perceived risk will be negatively correlated with behavioral intention.
The Relationship Between Behavioral Intention to Use Telepsychiatry and Psychiatrists' Attitudes Toward Telepsychiatry (H6)
The Pearson correlation analysis between behavioral intention to use telepsychiatry and psychiatrists' attitudes toward telepsychiatry showed a strong to moderate positive relationship [r(76) = 0.47, p < 0.01] (Table 7). This finding is consistent with our hypothesis that attitudes toward telepsychiatry will have a significant effect on behavioral intention to use telepsychiatry.
The Relationships Between Behavioral Intention to Use Telepsychiatry and the Independent Variables
The Pearson correlation analyses between the dependent variable, behavioral intention to use telepsychiatry, and the independent variables showed strong to moderate positive relationships with some of them, such as facilitating conditions [r(76) = 0.45, P < 0.01], attitudes toward telepsychiatry [r(76) = 0.47, P < 0.01], and a moderate negative relationship with perceived risk [r(76) = −0.37, P < 0.01].
In each of the models where the independent variable, psychiatrists' experience in using telepsychiatry, was tested it was statistically significant even if there were additional variables in the model. That is, experience is strongly correlated with the behavioral intention to use telepsychiatry.
Altogether, the data suggest that although the behavioral intention of psychiatrists in Israel to use telepsychiatry is relatively low, they perceive themselves as being capable of high performance and that using telepsychiatry will require a low effort. They are interested in using telepsychiatry voluntarily even when it is not mandatory. Experience in using telepsychiatry had the most significant correlation with their behavioral intention to use it. Additionally, facilitating conditions were perceived as being able to make it easier for them to use telepsychiatry and correlated with their intention to use it. Furthermore, they have a positive attitude toward treating patients by telepsychiatry and perceive the risk in using it to be average. There was a gender difference in the correlation with performance expectancy and social influence, where women's behavioral intention to use telepsychiatry was lower than that of men. The age of the psychiatrists and social influence were not found to be influential variables.
Discussion
The present study aimed to identify barriers or facilitators associated with the assimilation of telepsychiatry use by psychiatrists in Israel. To this end, we used the UTAUT model to examine the behavioral intention to use telepsychiatry in daily practice, and tested various variables that determine this intention to use telepsychiatry. The study showed that variables such as performance expectancy, effort expectancy, voluntariness and attitude toward telepsychiatry, were positively associated with the intention to use telepsychiatry, whereas a lack of experience and facilitating conditions that assist in the use of telepsychiatry were significant barriers to telepsychiatry assimilation.
In the UTAUT framework, performance expectancy was reported to be a determinant of intention to use a new technology (24). In line with the UTAUT model, we found that both effort expectancy and performance expectancy were correlated with behavioral intention. Nonetheless, while the UTAUT model determined that experience was merely a moderator of performance expectancy and social influence, we found that experience alone was strongly associated with the intention to use telepsychiatry. Moreover, the UTAUT model found that social influence is correlated with the intention to use, while in our study we observed that social influence was not significantly correlated with intention to use. We note that the UTAUT model determined that intention to use is a good predictor of actual use. It is possible that these differences stem from the fact that 44.7% of our study participants had some amount of experience with telepsychiatry, correlated with intention to use. This resonates with previous findings that with increasing experience, perceived behavioral control becomes a significant direct determinant of use over and above intention (24).
As found in previous studies, psychiatrists generally supported the idea of conducting consultations by videoconferencing, but raised concerns that video consultations may be less effective than FTF treatment (30). Nonetheless, we found that these expressed attitudes were correlated with prior experience, thus acceptance may increase with use. This finding corresponds with previous reports claiming that those who received training and found it easy and useful to use, were more likely to use telepsychiatry, and that it became easier with use (21, 31, 32). Coinciding with a study by Interian et al. (33), we also found that there were three distinct levels of experience that posed different challenges to the service providers. Those with no direct experience were more likely to be concerned about the fit between videoconferencing modality and mental health practice. Those with limited experience faced initial adoption of services and exposure to logistical barriers, and the most experienced providers reported more instances of patient satisfaction and being able to provide care to patients who otherwise had difficulty accessing care. Inexperience with telepsychiatry can be found in other developed countries, such as the USA, where a study that reviewed 183 residency programs found that only 21 offered any training or experience in telepsychiatry (34).
In the UTAUT model, facilitating conditions were significant predictors of the actual use of technology, but not a significant determinant of the intention to use the system (24). Nonetheless, in our study there was a strong correlation between the degree to which psychiatrists believed that the organization and technical infrastructure support their use of telepsychiatry and their intention to use it. We found that facilitating conditions generate a stronger sense of positivity and success during the initial use of telepsychiatry, associated with higher intention to use telepsychiatry. Unfortunately, most of the public mental health facilities in Israel do not have a strong support system or well-developed infrastructure for the use of telepsychiatry, and it is probable that the responsibility for learning the system will lie largely with the users.
Unlike the UTAUT model, where social influence was found to be a significant predictor for the intention to use technology (24), our study showed that social influence was not associated with the intention to use telepsychiatry. This discrepancy can be explained by the fact that in the two decades that passed since the original UTAUT study, the use of technology has become very widespread and therefore may no longer be a significant barrier to the assimilation of tools such as telepsychiatry. Another possible explanation is that our sample constituted a highly educated population that is used to working with technology and computer systems in everyday work.
The UTAUT model reported a significant correlation of age and gender with the intention to use (24), but we did not observe any of these correlations in our study. However, a more detailed examination of age and gender showed that gender was significantly correlated with performance expectancy and social influence, but not with the other variables, while age was not significantly correlated with any variable. It is plausible that in Israel, even older providers are proficient in implementing communication technology.
Our study encompassed additional variables that were not included in the UTAUT model, such as perceived risk. Unlike studies that reported perceived risk as a considerable factor associated with the intention to use health information technology (26), we did not find perceived risk to be significantly correlated with the intention to use telepsychiatry. In addition, the attitude toward telepsychiatry, which is not addressed in the UTAUT model, was found to be largely positive among Israeli psychiatrists.
To conclude, the present study revealed an intriguing result. Despite multiple factors that favor the use of telepsychiatry (high performance expectancy, low effort expectancy, low perceived risk, a largely positive attitude, high voluntariness, and high expectancy for facilitating conditions) the intention to use was rather low. This awkward result might be explained by the low experience element, which probably plays a pivotal role. Experience can mitigate some of the providers' negative aspects, and contribute to more positive overall attitudes toward an innovation (21). Therefore, we recommend creation of a positive experience for psychiatrists who are beginning to use telepsychiatry, so that the chance of using it in the future will increase. This can be addressed by education and training, which should begin at medical school, and continue with guidance during subsequent use together with continuous, up-to-date support for new developments in the field (21, 33). The opportunity to learn and practice telepsychiatry can encourage providers to be more inclined to use it when appropriate (31). Furthermore, for the provider to experience success in experimenting with a new system, a broader organizational culture is required to provide policy support, including training and administration (35). Hence, the connection between the facilitating conditions and their effects on the continued use of telepsychiatry should be acknowledged, and a training program that provides knowledge about the various aspects of telepsychiatry should be developed.
Beyond learning, training and practice, facilitating conditions can also be directed in various ways to facilitate the daily use of telepsychiatry. For example, support staff could handle ordering and scheduling consultations at both ends for assisting the patient remotely when needed, as well as assisting the service providers [Rolf (36)]. Facilitating conditions can also be a platform that enables easy scheduling and tracking of patients and providers, exchange of clinical data, and data collection and analysis. An example of such is the successful establishment of a web portal, the North Carolina Statewide Telepsychiatry Program (NC-STeP), which facilitates the use of telepsychiatry by patients and providers. It enables navigating and sharing the electronic health records system, and providers can use this platform for scheduling, billing, tracking and reporting encounters, and providing information to health care systems (37).
Limitations and Future Research
This study has a number of limitations: first, although the sample size is small, it comprises 10% of the active psychiatrists in Israel. Moreover, the demographic and profession-related data indicate an inclusive sample that reflects the full spectrum of Israeli psychiatrists. According to the Ministry of Health (38), female psychiatrists comprised 49% of all psychiatrists in Israel in 2019, similar to the current sample (48.7%). However, only 15% of all psychiatrists were 44 years old or younger, in contrast to the current study, in which 54% of the psychiatrists were 47 years old or younger. It seems that the sample of psychiatrists who participated in the study is slightly younger than the general population of psychiatrists in Israel. Second, there is a possibility that the participants who answered the questionnaire were already interested in telepsychiatry, and therefore their attitude was more positive. Third, self-reporting data are subjective and any given answer may be influenced by self-interest, a lack of knowledge about telepsychiatry or a lack of experience in using telepsychiatry (55.3% psychiatrists without experience). Fourth, the sample used in the study is a convenience sample; therefore, it does not represent all psychiatrists in Israel. Fifth, due to the small N we could not test the full UTAUT model and we recommend a future study with a larger number of participants. Finally, the study took place just before the outbreak of the COVID-19 pandemic in Israel and the questionnaires were completed before or at the very beginning of the COVID-19 era. The pandemic resulted in rapid assimilation of telemedicine and telepsychiatry in the world including in Israel (39–41), with higher odds of attending and completing treatment than FTF during this period (42, 43). Mental health providers reported satisfaction with electronic health services (44), patients received telepsychiatry well as a solution for emergency situations when FTF meetings were not possible (45), and in a US study most patients said they would consider it in the future (46). In light of the COVID-19 crisis, the attitudes of the study participants may have changed. While this study reflects the pre-COVID era, when use of telemedicine was less frequent in Israel, it provides an excellent baseline for further studying telepsychiatry. Further research on the post COVID-19 era can, for example, teach us about the actual use of telepsychiatry with respect to the intention to use it, and about the ways in which an emergency is associated with overcoming barriers to the assimilation of new technologies in mental health.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors upon request, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by University of Haifa Faculty of Health and Social Welfare Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
HK and MN conceived the study, designed the experimental approach, supervised the work, and obtained the funding. HK, MN, and MS designed, edited the questionnaires, and wrote the manuscript. HK and MS performed the statistical analyses, disseminated the questionnaires, and approached the psychiatrists. MS collected the completed questionnaires, registered, and gathered the data. All authors contributed to the article and approved the submitted version.
Funding
This work was funded by the Israel National Institute for Health Policy Research (Grant No. 2018/11/r).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.829965/full#supplementary-material
References
1. Charlson F, van Ommeren M, Flaxman A, Cornett J, Whiteford H, Saxena S. New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. Lancet. (2019) 394:240–8. doi: 10.1016/S0140-6736(19)30934-1
3. Al Achkar M, Bennett IM, Chwastiak L, Hoeft T, Normoyle T, Vredevoogd M, et al. Telepsychiatric consultation as a training and workforce development strategy for rural primary care. Ann Fam Med. (2020) 18:438–45. doi: 10.1370/afm.2561
4. Gardner JS, Plaven BE, Yellowlees P, Shore JH. Remote telepsychiatry workforce: a solution to psychiatry's workforce issues. Curr Psychiatry Rep. (2020) 22:8. doi: 10.1007/s11920-020-1128-7
5. Wootton R. Realtime telemedicine. J Telemed Telecare. (2006) 12:328–36. doi: 10.1258/135763306778682387
6. Caffery LJ, Farjian M, Smith AC. Telehealth interventions for reducing waiting lists and waiting times for specialist outpatient services: a scoping review. J Telemed Telecare. (2016) 22:504–12. doi: 10.1177/1357633X16670495
7. Malhotra S, Chakrabarti S, Shah R. Telepsychiatry: promise, potential, and challenges. Indian J Psychiatry. (2013) 55:3–11. doi: 10.4103/0019-5545.105499
8. Ruskin PE, Silver-Aylaian M, Kling MA, Reed SA, Douglas Bradham CD, Richard Hebel DJ, et al. Treatment outcomes in depression: comparison of remote treatment through telepsychiatry to in-person treatment. Am J Psychiatry. (2004) 161:1471–6. doi: 10.1176/appi.ajp.161.8.1471
9. Stubbings DR, Rees CS, Roberts LD, Kane RT. Comparing in-person to videoconference-based cognitive behavioral therapy for mood and anxiety disorders: randomized controlled trial. J Med Internet Res. (2013) 15:e258. doi: 10.2196/jmir.2564
10. Morland LA, Greene CJ, Rosen CS, Foy D, Reilly P, Shore J, et al. Telemedicine for anger management therapy in a rural population of combat veterans with posttraumatic stress disorder: a randomized noninferiority trial. J Clin Psychiatry. (2010) 71:855–63. doi: 10.4088/JCP.09m05604blu
11. Mitchell JE, Crosby RD, Wonderlich SA, Crow S, Lancaster K, Simonich H, et al. A randomized trial comparing the efficacy of cognitive-behavioral therapy for bulimia nervosa delivered via telemedicine versus face-to-face. Behav Res Ther. (2008) 46:581–92. doi: 10.1016/j.brat.2008.02.004
12. Kinley A, Zibrik L, Cordeiro J, Lauscher HN, Ho K. TeleHealth for Mental Health and Substance Use: Literature Review. BC Ministry of Health, Mental Health and Substance Use (MHSU) Branch (2012).
13. Seidel RW, Kilgus MD. Agreement between telepsychiatry assessment and face-to-face assessment for Emergency Department psychiatry patients. J Telemed Telecare. (2014) 20:59–62. doi: 10.1177/1357633X13519902
14. Glueck D. Establishing therapeutic rapport in telemental health. In: Myers K, Turvey LC, editors. Telemental Health. Oxford: Elsevier (2013). p. 29–46.
15. Modai I, Jabarin M, Kurs R, Barak P, Hanan I, Kitain L. Cost effectiveness, safety, and satisfaction with video telepsychiatry versus face-to-face care in ambulatory settings. Telemed J E Health. (2006) 12:515–20. doi: 10.1089/tmj.2006.12.515
16. Hubley S, Lynch SB, Schneck C, Thomas M, Shore J. Review of key telepsychiatry outcomes. World J Psychiatry. (2016) 6:269. doi: 10.5498/wjp.v6.i2.269
17. Cowan KE, McKean AJ, Gentry MT, Hilty DM. Barriers to use of telepsychiatry: clinicians as gatekeepers. Mayo Clin Proc. (2019) 94:2510–23. doi: 10.1016/j.mayocp.2019.04.018
18. Deslich S, Stec B, Tomblin S, Coustasse A. Telepsychiatry in the 21(st) century: transforming healthcare with technology. Perspect Health Inf Manag. (2013) 10:1f.
19. Jacob C, Sanchez-Vazquez A, Ivory C. Understanding clinicians' adoption of mobile health tools: a qualitative review of the most used frameworks. JMIR Ment Health. (2020) 8:1–20. doi: 10.2196/preprints.18072
20. Brooks E, Turvey C, Augusterfer EF. Provider barriers to telemental health: obstacles overcome, obstacles remaining. Telemed E-Health. (2013) 19:433–7. doi: 10.1089/tmj.2013.0068
21. Connolly SL, Miller CJ, Lindsay JA, Bauer MS. A systematic review of providers' attitudes toward telemental health via videoconferencing. Clin Psychol. (2020) 27:e12311. doi: 10.1111/cpsp.12311
23. State Comptroller. Annual Report 70B: Ministry of Health - Aspects of the Reform for the Transfer of Insurance Responsibility in Mental Health. (2020). p. 771–844.
24. Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. Innov Manag Policy Pract. (2003) 27:425–78. doi: 10.2307/30036540
25. Tonn P, Reuter SC, Kuchler I, Reinke B, Hinkelmann L, Stöckigt S, et al. Development of a questionnaire to measure the attitudes of laypeople, physicians, and psychotherapists toward telemedicine in mental health. JMIR Ment Health. (2017) 4:e39. doi: 10.2196/mental.6802
26. Egea OJM, González MVR. Explaining physicians' acceptance of EHCR systems: an extension of TAM with trust and risk factors. Comput Hum Behav. (2011) 27:319–32. doi: 10.1016/j.chb.2010.08.010
27. Featherman MS, Pavlou PA. Predicting e-services adoption: a perceived risk facets perspective. Int J Hum Comput Stud. (2003) 59:451–74. doi: 10.1016/S1071-5819(03)00111-3
28. Gagnon MP, Godin G, Gagné C, Fortin JP, Lamothe L, Reinharz D, et al. An adaptation of the theory of interpersonal behaviour to the study of telemedicine adoption by physicians. Int J Med Inform. (2003) 71:103–15. doi: 10.1016/S1386-5056(03)00094-7
29. Central Bureau of Statistics. Population by Districts. (2020). Available online at: www.cbs.gov.il (accessed February 7, 2022).
30. Wynn R, Bergvik S. P02-306 Clinicians' attitudes to the use of videoconferencing for psychiatric consultations. Eur Psychiatry. (2009) 24:S996. doi: 10.1016/S0924-9338(09)71229-5
31. Gibson K, O'Donnell S, Coulson H, Kakepetum-Schultz T. Mental health professionals' perspectives of telemental health with remote and rural first nations communities. J Telemed Telecare. (2011) 17:263–7. doi: 10.1258/jtt.2011.101011
32. Gilmore AK, Ward-Ciesielski EF. Perceived risks and use of psychotherapy via telemedicine for patients at risk for suicide. J Telemed Telecare. (2019) 25:59–63. doi: 10.1177/1357633X17735559
33. Interian A, King AR St. Hill LM, Robinson CH, Damschroder LJ. Evaluating the implementation of home-based videoconferencing for providing mental health services. Psychiatr Serv. (2018) 69:69–75. doi: 10.1176/appi.ps.201700004
34. Hoffman P, Kane JM. Telepsychiatry education and curriculum development in residency training. Acad Psychiatry. (2014) 39:108–9. doi: 10.1007/s40596-013-0006-6
35. Newman L, Bidargaddi N, Schrader G. Service providers' experiences of using a telehealth network 12 months after digitisation of a large Australian rural mental health service. Int J Med Inform. (2016) 94:8–20. doi: 10.1016/j.ijmedinf.2016.05.006
36. Wynn R, Bergvik S, Pettersen G, Fossum S. Clinicians' experiences with videoconferencing in psychiatry. Stud Health Technol Inform. (2012) 180:1218–20. doi: 10.3233/978-1-61499-101-4-1218
37. Saeed SA. Successfully navigating multiple electronic health records when using telepsychiatry: the NC-STeP experience. Psychiatr Serv. (2018) 69:948–51. doi: 10.1176/appi.ps.201700406
38. Ministry of Health. Healthcare Professions Manpower 2019. (2020). Retrieved from: https://www.health.gov.il/English/News_and_Events/Spokespersons_Messages/Pages/18082020_01.aspx (accessed February 7, 2022).
39. Looi JC, Allison S, Bastiampillai T, Pring W, Kisely SR. Telepsychiatry and face-to-face psychiatric consultations during the first year of the COVID-19 pandemic in Australia: patients being heard and seen. Australas Psychiatry. (2021) 23:10398562211046301. doi: 10.1177/10398562211046301
40. Schinasi DA, Foster CC, Bohling MK, Barrera L, Macy ML. Attitudes and perceptions of telemedicine in response to the COVID-19 pandemic: a survey of naïve healthcare providers. Front Pediatrics. (2021) 9:647937. doi: 10.3389/fped.2021.647937
41. Zeltzer D, Einav L, Rashba J, Balicer RD. The Impact of Increased Access to Telemedicine (No. w28978). National Bureau of Economic Research (2021).
42. Avalone L, Barron C, King C, Linn-Walton R, Lau J, McQuistion HL, et al. Rapid telepsychiatry implementation during COVID-19: Increased attendance at the largest health system in the United States. Psychiatr Serv. (2021) 72:708–11. doi: 10.1176/appi.ps.202000574
43. Hong JS, Sheriff R, Smith K, Tomlinson A, Saad F, Smith T, et al. Impact of COVID-19 on telepsychiatry at the service and individual patient level across two UK NHS mental health Trusts. Evid Based Ment Health. (2021) 24:161–16. doi: 10.1136/ebmental-2021-300287
44. Guinart D, Marcy P, Hauser M, Dwyer M, Kane JM. Mental health care providers' attitudes toward telepsychiatry: a systemwide, multisite survey during the COVID-19 pandemic. Psychiatr Serv. (2021) 72:704–7. doi: 10.1176/appi.ps.202000441
45. Malka M, Gropp C, Jaworowski S, Oberbaum M, Katz DE. Telepsychiatry for patients with post-traumatic stress disorder during the COVID-19 outbreak. Curr Treat Options Psychiatry. (2021) 8:158–65. doi: 10.1007/s40501-021-00245-z
Keywords: telepsychiatry, telemedicine, unified theory of acceptance and the use of technology, mental health services, barriers and facilitative factors
Citation: Kaphzan H, Sarfati Noiman M and Negev M (2022) The Attitudes and Perceptions of Israeli Psychiatrists Toward Telepsychiatry and Their Behavioral Intention to Use Telepsychiatry. Front. Psychiatry 13:829965. doi: 10.3389/fpsyt.2022.829965
Received: 06 December 2021; Accepted: 24 February 2022;
Published: 21 March 2022.
Edited by:
Larisa Ivascu, Politehnica University of Timisoara, RomaniaReviewed by:
Efrat Neter, Ruppin Academic Center, IsraelAldina Venerosi, National Institute of Health (ISS), Italy
Copyright © 2022 Kaphzan, Sarfati Noiman and Negev. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hanoch Kaphzan, aGthcGh6YW5AdW5pdi5oYWlmYS5hYy5pbA==
 Hanoch Kaphzan
Hanoch Kaphzan Margaret Sarfati Noiman2
Margaret Sarfati Noiman2