- 1Department of Psychiatry and Behavioral Sciences, University of California, San Francisco, San Francisco, CA, United States
- 2Department of Anthropology, Emory University, Atlanta, GA, United States
- 3College of Nursing, The University of Tennessee Health Science Center, Memphis, TN, United States
- 4Center on Developmental Disabilities, The University of Tennessee Health Science Center, Memphis, TN, United States
- 5Department of Preventative Medicine, The University of Tennessee Health Science Center, Memphis, TN, United States
- 6Department of Pediatrics, University of Washington, Seattle, WA, United States
- 7Department of Environmental and Occupational Health Sciences, University of Washington, Seattle, WA, United States
- 8Center for Child Health, Behavior and Development, Seattle Children's Research Institute, Seattle, WA, United States
- 9Department of Pediatrics, University of California, San Francisco, San Francisco, CA, United States
Objective: Experiences of stress and adversity, such as intimate partner violence, confer risk for psychiatric problems across the life span. The effects of these risks are disproportionately borne by women and their offspring—particularly those from communities of color. The prenatal period is an especially vulnerable period of fetal development, during which time women's experiences of stress can have long-lasting implications for offspring mental health. Importantly, there is a lack of focus on women's capacity for resilience and potential postnatal protective factors that might mitigate these intergenerational risks and inform intervention efforts. The present study examined intergenerational associations between women's prenatal stressors and child executive functioning and externalizing problems, testing maternal parenting quality and child sex as moderators, using a large, prospective, sociodemographically diverse cohort.
Methods: We used data from 1,034 mother-child dyads (64% Black, 30% White) from the Conditions Affecting Neurocognitive Development and Learning in Early Childhood (CANDLE) pregnancy cohort within the ECHO PATHWAYS consortium. Women's prenatal stressors included stressful life events (pSLE) and intimate partner violence (pIPV). Measures of child psychopathology at age 4–6 included executive functioning and externalizing problems. Parenting behaviors were assessed by trained observers, averaged across two sessions of mother-child interactions. Linear regression models were used to estimate associations between women's prenatal stressors and child psychopathology, adjusting for confounders and assessing moderation effects by maternal parenting quality and child sex.
Results: Women's exposures to pSLE and pIPV were independently associated with child executive functioning problems and externalizing problems in fully-adjusted models. Maternal parenting quality moderated associations between pSLE and both outcomes, such that higher parenting quality was protective for the associations between women's pSLE and child executive functioning and externalizing problems. No moderation by child sex was found.
Discussion: Findings from this large, sociodemographically diverse cohort suggest women's exposures to interpersonal violence and major stressful events—common for women during pregnancy—may prenatally program her child's executive functioning and externalizing problems. Women's capacity to provide high quality parenting can buffer this intergenerational risk. Implications for universal and targeted prevention and early intervention efforts to support women's and children's wellbeing are discussed.
Intergenerational Transmission of Effects of Women's Stressors During Pregnancy: Child Psychopathology and the Protective Role of Parenting
Exposure to various forms of stressors, including economic precarity, housing insecurity, loss of a loved one, and interpersonal violence, are well-established predictors of psychiatric problems across the life span (1–5). The impact of these experiences is disproportionately borne by women—especially women in underserved communities of color (6–9) and with lower incomes (10)—which also places their offspring at increased risk for later psychiatric problems. Indeed, the World Health Organization considers intimate partner violence against women a “major public health problem and a violation of women's human rights,” estimating that roughly one in three women are subjected to intimate partner violence during their lifetime, with up to 13% of women experiencing intimate partner violence during pregnancy (pIPV) (11). Further, the most common form of violence committed against women is intimate partner violence, and women who experience partner violence are at increased risk for a range of mental health problems, such as depression, posttraumatic stress, anxiety, and suicidality (11). In addition, according to the Centers for Disease Control and Prevention's Pregnancy Risk Assessment Monitoring System, in 2010 about 70% of pregnant women experienced at least one stressful life event (pSLE) in the year before their infant's birth (12). These include: emotional stressors (e.g., a family member being hospitalized or dying), financial stressors (e.g., moving, losing a job, being unable to pay rent/bills), partner-related stressors (e.g., separation/divorce), and traumatic stressors (e.g., becoming homeless) (12). Despite these alarming rates of exposure to stressors during pregnancy—a time when women's social and biological wellbeing is in flux and particularly vulnerable to stress (13, 14)— there has been limited focus on the intergenerational transmission of the effects of stressors, such as pSLE and pIPV, on offspring psychopathology and related developmental processes. The perinatal period is a critical time for offspring development, wherein such intergenerational risks pose a threat to offspring mental health across the lifespan. Crucially, there is also a lack of focus on women's capacity for resilience and associated research on potential postnatal resilience-promoting factors that might mitigate these intergenerational risks for child mental health problems and shed light on opportunities to support maternal and child wellbeing after exposure to prenatal adversity in affected communities.
A large body of research has documented the association of both pSLE and pIPV with deleterious outcomes for women, including maternal mortality, labor and delivery complications, poor perinatal mental health (such as depression, post-traumatic stress disorder, and substance use disorder), and enduring alterations to women's immune function (13, 15, 16). The intergenerational impact of pIPV and pSLE is seen in neonatal outcomes of higher rates of preterm birth and low birth weight, but also in longer-term neurodevelopmental problems that extend into childhood and beyond (17–20). Investigations of maternal IPV exposure are especially crucial considering the established continuity of IPV within families and across generations. For example, women who witness IPV as children have greater odds of experiencing IPV as adults, and their own children are more likely to witness IPV (21, 22). Children exposed to IPV also have increased risk for both externalizing and internalizing problems, as well as higher levels of symptoms of trauma, compared to non-exposed children (15, 23). Women's exposure to stressors in pregnancy might affect offspring development through both pre- and post-natal pathways, with potentially cumulative effects, making it important to expand empirical understanding of these risks.
Prenatal programming of offspring neurodevelopment and psychopathology in the context of maternal prenatal stress is a complex biopsychosocial phenomenon that requires attention to the social dynamics and biology that is unique to women. Women's experiences of stress during pregnancy result in altered fetal exposure to maternal glucocorticoids, immune tolerance, and nutrient supply that can shift trajectories of offspring growth and stress reactivity in the postnatal environment (24–27). Despite the fact that prenatal stressors such as pIPV and pSLE for women can co-occur, their dual contributions to child psychopathology are rarely studied—especially in communities of color (17, 28, 29). This is a particularly important population within which to examine such stressors given that women of color have higher prevalence rates of intimate partner violence compared to non-Hispanic White women (6–9).
Studies examining the intergenerational associations between maternal prenatal stress and risk for offspring psychopathology during infancy and early childhood have found that maternal prenatal stress is generally linked to her child's subsequent inability to self-regulate, manifesting as more difficult temperaments and increased stress reactivity (17, 30). These problems with self-regulation during early school-ages (i.e., preschool and kindergarten) can manifest as executive functioning (EF) deficits, which are also closely related to externalizing psychopathology, such as ADHD (31, 32). Given the high prevalence rates of EF problems and externalizing behavior in young children (33, 34) and how they set the stage for later, more severe psychopathology and health risk (35, 36), examining their etiology and development in early childhood is critical. Although some studies have found associations between prenatal maternal stress and offspring externalizing psychopathology, including risk for ADHD (28), fewer studies have examined this potential link between prenatal stress and child EF problems (37, 38), and to our knowledge, none have examined both executive functioning and externalizing problems within the same conceptual model. Importantly, very few studies have prospectively examined these associations in large, sociodemographically diverse samples, which is particularly salient given that lower SES places both women and their offspring at increased risk for psychopathology, in part due to greater exposure to stressors across generations (17, 18, 39).
There is evidence regarding differential sex effects of maternal stress on offspring psychopathology; however, to date these findings have been quite mixed—necessitating additional inquiry (17, 33, 40–43). This is particularly important to examine in outcomes with well-established sex differences, such as externalizing behavior problems during childhood. Sex-dependent differences in offspring responses to prenatal stress are complex biopsychosocial phenomena, wherein socially patterned norms for gendered child behavior interact with developmental psychobiology. Female and male fetuses exhibit sexually dimorphic responses to the maternal stress-related hormonal and cytokine milieu, investing differentially in placental and somatic growth in ways that may confer sex-dependent trajectories of buffering and risk in the wake of prenatal adversity (41, 44). While female fetal buffering from maternal inflammation or nutritional stress may confer increased resilience in terms of viability relative to males, trade-offs in increased sensitivity to HPA axis programming and risk for psychopathology may also occur (45, 46). For example, Graham and colleagues (47) found that elevated cortisol levels during pregnancy predicted increased amygdala and default mode network connectivity and mediated increased internalizing symptoms in 24-month-old girls but not boys. There is some evidence that boys might be more likely to develop externalizing problems during childhood within the context of maternal prenatal stress (40, 48, 49). Yet, findings here are still mixed, and fewer studies have examined these potential sex differences in early childhood, when externalizing problems are less sex differentiated (43, 47, 50).
Although research on integrational transmission of stress effects has burgeoned recently, there remains a dearth of research identifying opportunities for intervention or prevention regarding prenatal stress and risk for offspring psychopathology (17, 51–53). Identifying malleable, postnatal environmental factors that capitalize on women's strengths is also critical to reducing potential intergenerational risk (19). Parenting is certainly a key factor, with a wealth of research indicating that it can serve as both a risk and a protective factor for child mental health. For example, negative aspects of parenting, such as harsh discipline, neglect, and punishment, are associated with increased risk for offspring psychopathology—especially externalizing behavior problems (54, 55). In addition, multiple studies have found that prior exposure to IPV has a negative impact on parenting behaviors (56), and that such parenting behaviors are also associated with child behavior problems (57–59). However, the increased focus on the negative aspects of parenting has perhaps overshadowed the benefits that the positive aspects of parenting (such as warmth, responsiveness, and scaffolding) can have on offspring mental health. Indeed, positive parent-child interactions have been shown to confer beneficial effects on executive functioning and externalizing psychopathology in both observational and intervention studies (39, 60–62), and positive parenting has been identified as an important resilience-promoting factor for children at increased risk for psychopathology (63). Sensitive caregiving in the context of ongoing stressors is contingent on a caregiver's ability to harness emotional, cognitive, and material resources, especially when caregiving demands are high, such as when children are young (64). Notably, research findings emphasize the ability of caregivers to buffer children from adversity and support healthy child development through supportive parenting, even when facing socioeconomic barriers and other high-adversity contexts (65). For example, Narayan and colleagues found that women with high levels of childhood trauma and positive memories of nurturing care were able to buffer their children from future intergenerational trauma exposure (66). In another example, effective parenting and parental use of positive coregulation skills were associated with higher child executive functioning skills and had positive benefits at school among families who were experiencing homelessness (67). Most studies examining the associations between women's parenting behaviors and child psychopathology, however, rely on parent self-report of their own parenting behaviors, which can produce biased results (68, 69). Fewer studies use more objective, observer ratings of mother-child interactions and parenting behaviors which are less influenced by such biases.
The present study examined the intergenerational association between maternal prenatal stress and risk for executive functioning and externalizing behavior problems during early childhood (ages 4–6) in a large, prospective, pregnancy cohort study of mother-child dyads. We had three main aims to address gaps in extant literature. First, we tested whether women's stressors during pregnancy, including exposure to multiple types of pSLE and pIPV, were predictive of two key aspects of self-regulation and psychopathology in their children: EF and externalizing behavior problems. Importantly, we utilized a large, racially diverse (64% Black, 30% White) sample with a broad representation of lower-income families, characteristic of an urban Southern metropolitan area in the United States—a population that is largely understudied in extant literature and, due to structural inequalities, are likely to be exposed to higher levels of stressors during pregnancy (10, 70, 71). Second, we tested whether observer-rated parenting behaviors might serve as a postnatal environmental factor that moderates the association between prenatal stressors and risk for child psychopathology. Finally, given the potential for differential effects of prenatal stress on male vs. female offspring, we examined whether child sex moderated the effects of women's pregnancy stressors on both child outcomes.
Materials and Methods
Participants and Procedure
The present study utilized data from the Conditions Affecting Neurocognitive Development and Learning in Early Childhood (CANDLE) study, which is part of the ECHO PATHWAYS consortium (72, 73). CANDLE is a longitudinal pregnancy cohort study that enrolled 1,503 women from Memphis/Shelby County, Tennessee, between 2006 and 2011 during their second trimester of pregnancy. Women were between ages 16–40, did not have pre-existing chronic conditions that required medication, and had low-risk pregnancies. Overall, the sample was racially diverse (64% Black, 30% White) and, although the sample had a broad range of socioeconomic status, it was predominantly low-income (59% having federal or state-supplemented health insurance)—representative of the urban area from which it was drawn. All women provided informed consent and the study was approved by the University of Tennessee Health Science Center Institutional Review Board.
Baseline data were collected at study enrollment during the women's second trimester of pregnancy. Subsequent perinatal data were collected during a third trimester visit and at childbirth. Families were then prospectively followed, with data collected at a home visit 4-weeks postpartum, a 6-month phone follow-up, and subsequently at multiple clinic visits occurring at approximately child ages 1-, 2-, 3-, 4–6-, and 8-years. The final analytic sample comprised 1,034 women for whom child data were available on at least one outcome measure. Compared to the total enrolled sample of 1,503, women in the analytic sample tended to be older at study enrollment (t = 3.94, p < 0.001), but did not otherwise significantly differ on study variables.
Measures
Prenatal Predictors
Stressful Life Events
Women reported retrospectively on whether they experienced 14 different types of major pSLE during pregnancy, using a measure adapted from the widely used Centers for Disease Control and Prevention Pregnancy Risk Assessment Monitoring System survey (74), within the age eight visit maternal questionnaire. This scale included the following 14 items: a family member was hospitalized; death of a close friend/family member; moving to a new address; loss of job/employment; partner lost their job; participant/partner had a reduction in work hours or pay; problems paying the rent/mortgage or other bills; separation/divorce from partner; was apart from partner due to military deployment or extended work-related travel; argued with partner more than usual; partner did not want participant to be pregnant; close friend/family member had a problem with drinking/drugs; participant/partner was incarcerated; participant was homeless. Women responded yes or no to each item; all responses were summed into a total count of different types of pSLE experienced (range 0–14). Given the magnitude and significance of these stressful life events, such measures are thought to have limited recall bias and be accurate over a span of years (75, 76).
Intimate Partner Violence
Women reported on their experiences of pIPV via the short-form version of the revised Conflict Tactics Scale (77), which assesses multiple forms of partner violence. Information was collected during the third trimester of pregnancy, wherein women indicated if they experienced any of four different forms of partner violence (including physical, sexual, or emotional abuse, and/or injury) during the past year. Each item (answered yes or no) was summed to create a total pIPV score (range 0–4).
Moderators
Parenting Quality
Parenting behaviors were assessed at both the age 2 and age 3 clinic visits using the Nursing Child Assessment Satellite Training (NCAST) Parent-Child Interaction Teaching Scale (78, 79). The NCAST comprises 73 items, each endorsed yes or no. This form was completed by study staff members who received rigorous training in the NCAST coding system, and was filled out by a staff member immediately after observing interactions between the mother and child as the mother teaches her child a developmentally challenging task (80). This measure has been utilized with diverse populations and has shown good internal consistency and test-retest reliability. Cronbach's alphas for the present sample were also good (α = 0.83 for Total Caregiver score and α = 0.81 for Total Caregiver-Child score) (81). We use the term “parenting quality” to describe the overall measure of parenting behavior captured by the Total Caregiver score. This comprises a range of parenting behaviors, including social, nurturant, and didactic caregiving (81). The Total Caregiver score consists of four subscales, including: parental sensitivity to cues, response to distress, social-emotional growth-fostering, and cognitive growth-fostering. Higher scores indicate more sensitivity, supportiveness, and scaffolding by mothers during observed interactions with their child. We created a composite parenting quality score across both the age 2 and age 3 clinic visits by averaging the Total Caregiver score across both visits. Data from one visit was used if both visit data were not available.
Child Sex
We tested the potential moderating effects of child biological sex, ascertained from birth records, on both outcome variables, given the mixed evidence regarding potential differences from previous research (17, 40).
Child Outcomes
Child psychopathology was assessed using two measures at the age 4–6 clinic visit.
Executive Functioning Problems
Women reported on their children's EF using the Behavior Rating Inventory of Executive Functioning–Preschool version (BRIEF-P) (82) at the age 4–6 clinic visit. The BRIEF is a widely used measure that assesses a broad range of executive functioning problems in everyday life and is used in clinical and research settings. The BRIEF-P comprises 3 indexes—inhibitory self-control, flexibility, and emergent metacognition, which make up the overall global executive composite. Cronbach's alpha for the present sample was excellent (α = 0.96). The present study utilized t-scores of the overall composite to assess problems with executive functioning.
Externalizing Problems
Women reported on their children's externalizing problems via the well-validated and widely-used Child Behavior Checklist for ages 1.5–5 (CBCL) (83) at the age 4–6 clinic visit. Consistent with prior research, we used t-scores from the broadband Externalizing Problems scale, which has been widely used to assess overall problems of externalizing psychopathology, including hyperactivity/impulsivity, self-regulation, oppositionality, conduct, and aggression in children. Internal consistency for the Externalizing Problems scale was excellent (Cronbach's α = 0.91).
Covariates
Several pre- and postnatal covariates were included to address potential confounding. We included several socioeconomic factors, given they have demonstrated associations with child psychopathology. The following were obtained from women during study enrollment: age, annual household income (adjusted for number of dependents), education, marital status, and self-reported race [the authors acknowledge that race is not a biological variable and is a political and social construct that often serves as a proxy for the impact of racist practices and structural inequality (84); thus, it is examined in the current paper with this premise in mind]. We also included women's full-scale IQ from the Wechsler Abbreviated Scale of Intelligence, Second Edition (85) assessed at the postnatal 1-year clinic visit, or thereafter if that visit was missed. Given that parent psychopathology, in particular depression, is also associated with later child psychopathology, we included both postpartum and concurrent maternal depression as covariates. Women's postpartum depression across the 1st year of the child's life was measured with the 10-item, self-reported Edinburgh Postnatal Depression Scale (86), which was assessed at 4-, 6-, and 12-months post-birth; the total depression score across all three time points was averaged into a single composite. Concurrent maternal depression was measured at the age 4–6 clinic visit with the Center for Epidemiologic Studies Depression Scale, a 20-item self-report (87). Finally, child biological sex and age at the outcome timepoint were included as covariates in all models.
Statistical Analyses
All linear regression models were conducted using R (RStudio version 1.2.5033) and fitted using the lm function. Data were first examined for normality and for the presence of outliers in study variables. The missForest package (88) was used to impute missing data using the random forest multiple imputation method. In comparison with other multiple imputation methods (e.g., MICE), this machine learning technique can accommodate non-linearities and interactions and does not need a specific regression model to be specified, which makes this approach more useful for imputing larger data sets where some participants have missing data (89). All variables had missing data of 5% or less except for maternal pSLE, which was missing for 22%. Linear regressions were conducted to test hypotheses using the imputed data set. All predictor variables and covariates were standardized before being entered into the models. The following analyses were conducted in two separate models, one for each outcome variable (EF and externalizing problems).
In Step 1, we estimated main effects by performing multiple linear regressions to examine the relation between both prenatal predictors (pSLE, pIPV) and each outcome variable without including covariates in the model. In Step 2, we added all covariates to the models in Step 1 to obtain our fully-adjusted models. In Step 3, we examined potential interactions with parenting quality by additionally incorporating the two interaction terms between each prenatal predictor and the parenting quality moderator (pSLE x parenting quality; pIPV x parenting quality) into both of the fully-adjusted models for our two outcome variables. Significant interaction terms were then probed to test for simple slopes at three different values of the moderator (+1 SD, mean, −1 SD) (90). Finally, we repeated the same procedures to examine potential interaction effects of child sex by prenatal predictors on both outcome variables by including interaction terms between each prenatal predictor and child biological sex.
Results
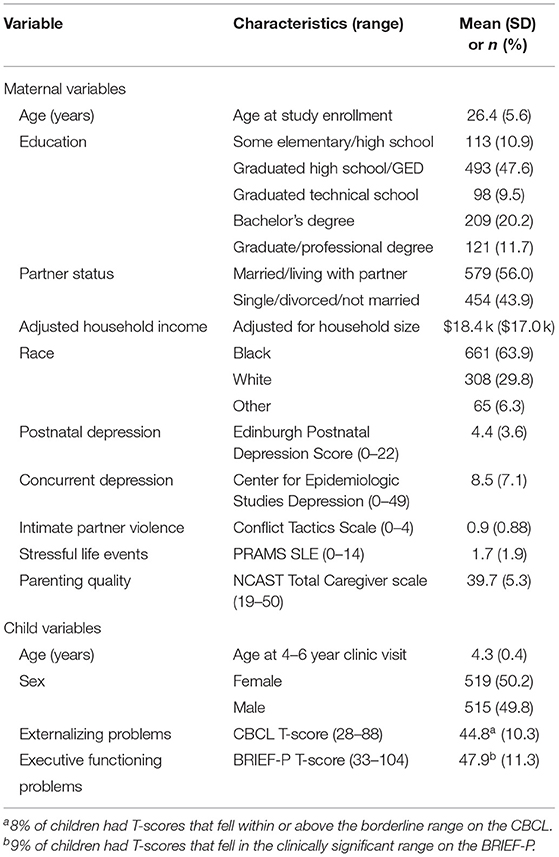
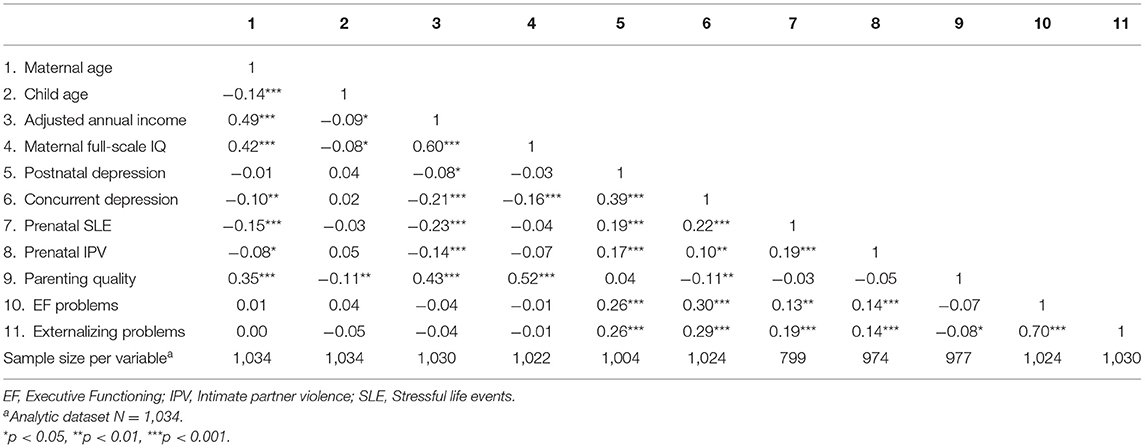
Descriptive statistics of the primary study variables are presented in Table 1. Median education level was completion of high school; mean household-adjusted income was $18.4 k. Regarding pSLE, 28% of women reported experiencing no pSLE; 50% reported experiencing at least 1 type of pSLE; 32% reported experiencing at least 2; and 21% reported experiencing 3 or more. For pIPV, 28% of women reported experiencing no forms of pIPV; 66% reported experiencing at least 1 form; 18% reported experiencing at least 2; and 7% reported experiencing 3 or more forms of pIPV. Thirty four percent of women reported experiencing both pIPV and pSLE. Children's EF problems were strongly correlated with externalizing problems (r = 0.7, p < 0.001). Bivariate correlations are provided in Table 2. Of note, maternal pSLE and pIPV were weakly correlated (r = 0.19, p < 0.001), suggesting they captured largely unique domains of stress exposure. Also of note, observed parenting quality was neither correlated with pSLE (r = −0.03, p = 0.49) nor pIPV (r = −0.05, p = 0.16), suggesting the consideration of parenting as a potential moderator, rather than a mediator, was appropriate.
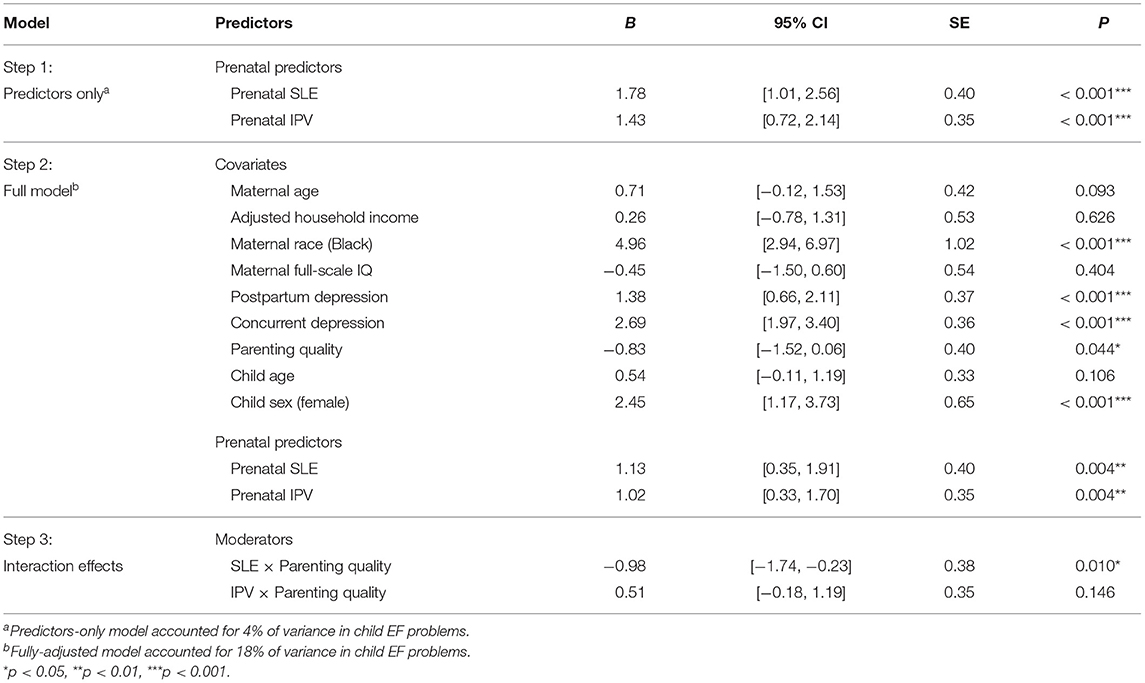
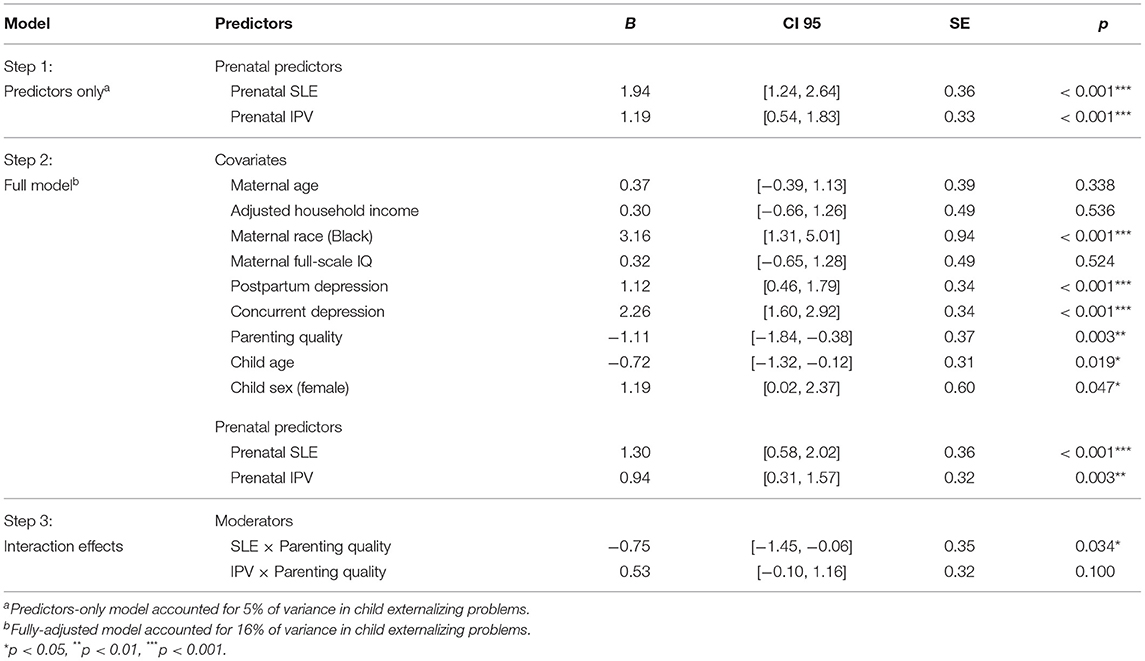
Tables 3, 4 present results from the regression analyses, examining both main and moderated effects, for child EF problems and externalizing problems, respectively. Results for the fully-adjusted model for child EF problems (Table 3) showed maternal pSLE (b = 1.13, p = 0.004) and pIPV (b = 1.02, p = 0.004) independently predicted child EF problems, such that higher levels of pSLE and pIPV were uniquely, positively associated with levels of child EF problems. There was a marginally significant main effect of observed parenting quality on child EF problems, wherein higher levels of parenting quality were associated with lower levels of EF problems in childhood (b = −0.81, p = 0.044). Regression results for the fully-adjusted model for child externalizing problems (Table 4) similarly showed women's pSLE (b = 1.30, p < 0.001) and pIPV (b = 0.94, p = 0.003) independently predicted child externalizing problems, such that higher levels of pSLE and pIPV were uniquely, positively associated with levels of child externalizing problems. In addition, higher levels of parenting quality were significantly associated with fewer child externalizing problems (b = −1.11, p = 0.003). Of note, women's postpartum depression and concurrent depression independently predicted both child outcomes.
Next, we examined whether parenting quality moderated the aforementioned associations. Two significant interactions emerged, qualifying the main effects found. Regarding child EF problems (Table 3, Step 3), there was a significant pSLE x parenting interaction (b = −0.98, p = 0.010). Figure 1 provides illustration of the continuous interaction term plotted, with tests of the simple slopes, at the mean and +/– 1 SD, showing a significant positive association between women's pSLE and children's EF problems at average (b = 1.00, SE = 0.40, p = 0.012) and at low levels (−1 SD; b = 1.99, SE = 0.53, p < 0.001) of observed parenting quality. However, at higher levels of observed parenting quality (+1 SD), there was a buffering effect such that pSLE was not significantly associated with child EF problems (b = 0.01, SE = 0.57, p = 0.985). Parenting quality did not significantly interact with pIPV to predict child EF problems (b = 0.51, p = 0.146).
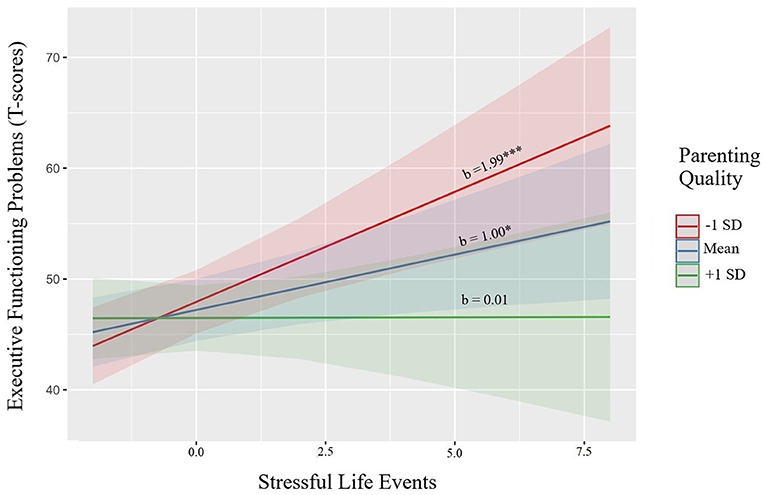
Figure 1. Parenting quality moderates the association between maternal prenatal stressful life events and child executive functioning problems.
A similar pattern was found for child externalizing problems (Table 4, Step 3), revealing a significant pSLE × parenting interaction (b = −0.75, p = 0.034). Figure 2 provides illustration of the continuous interaction term plotted, with tests of the simple slopes, showing a significant positive association between women's pSLE and children's externalizing problems at average (b = 1.22, SE = 0.36, p < 0.001) and low levels (−1 SD; b = 1.96, SE = 0.49, p < 0.001) of parenting quality. At higher levels of observed parenting quality, there was again a buffering effect, such that pSLE was not significantly associated with child externalizing problems (b = 0.46, SE = 0.52, p = 0.373). There was no significant interaction between pIPV and parenting quality for child externalizing problems (b = 0.53, p = 0.100). Finally, we examined associations between child sex and both measures of women's pregnancy stress exposure, predicting both outcomes. Although girls displayed lower problems in adjusted models for both outcomes, there was no evidence for moderation by child sex for either stress exposure (results not shown).
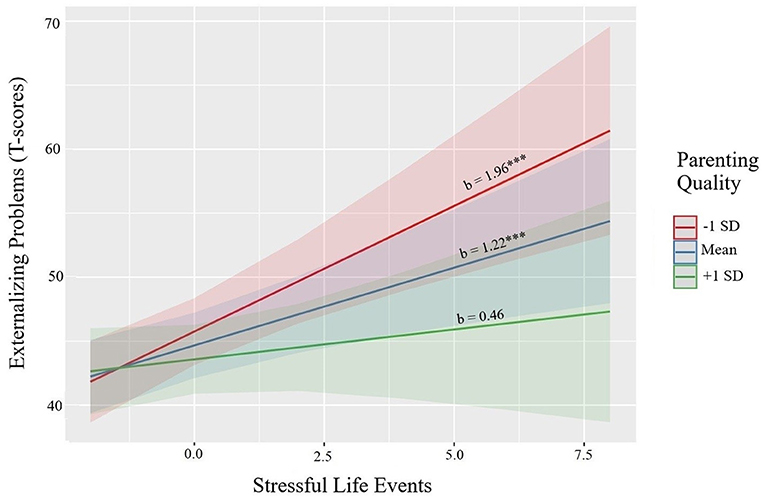
Figure 2. Parenting quality moderates the association between maternal prenatal stressful life events and child externalizing problems.
Discussion
Understanding the complex biopsychosocial phenomenon of relations between women's exposure to stressors in pregnancy and child psychopathology is important for the prevention of mental illness and the promotion of women and children's wellbeing. The aim of the present study was to examine the intergenerational associations between women's stress exposures during pregnancy and young childhood executive functioning and externalizing problems in a large, sociodemographically diverse sample. Crucially, we also examined women's observed parenting quality as a potential postnatal protective factor that might buffer children from the risks of later psychopathology. To our knowledge, this is one of the largest U.S. pregnancy cohorts examining intergenerational associations of maternal prenatal stress exposures and child psychopathology that includes a large percentage of Black women as well as a broad representation of families with lower household income—a sample with particular generalizability to Southern metropolitan U.S. populations. We found that women's exposure to intimate partner violence and stressful life events during pregnancy independently predicted higher levels of EF and externalizing problems in their 4–6-year-old children, even after controlling for a variety of pre- and post-natal factors. Notably, these two prenatal stress exposures were very weakly correlated, suggesting that different domains of women's risk exposure during pregnancy have unique relevance to child development and psychopathology. In addition, we found that higher levels of sensitivity, supportiveness, and scaffolding provided by women to their children during observed parent-child interaction tasks served as a postnatal protective factor, buffering their children from the association between pSLE and both child outcomes—providing insights into heterogeneity of main effects and potential targets for intervention.
Our findings for the associations between women's prenatal stressors and child externalizing problems are largely consistent with extant literature (17, 28), yet they expand the evidence base to EF outcomes within a large, sociodemographically diverse sample. Although the operationalization of child EF across the few existing studies has varied (37, 38), our findings—which utilized a behaviorally-based measure of EF—are generally consistent with the few prenatal programming studies that have used lab-based measures of EF, indicating that women who experienced more forms of stress during pregnancy reported that their children demonstrated poorer overall inhibition, flexibility, planning and/or working memory in everyday settings. Given the strong association between child EF and externalizing problems, the fact that we see a similar pattern in prediction by both prenatal stressors is not necessarily surprising and further suggests shared etiology or developmental mechanisms (91). In addition, our finding regarding the negative associations between maternal parenting quality and child EF and externalizing problems is also consistent with a large body of extant research on parenting and child behaviors. Women who have the social/emotional/economic resources, structural supports, and ability to provide more scaffolding, warmth, and nurturing to their children are more likely to help mitigate and reduce potential externalizing behavior problems. Interventions that support a caregiver's ability to harness resources for supportive parenting may thus play a crucial role in mitigating the impact of early adversity in children most at risk. Importantly, although parenting behaviors can certainly be shaped by prior experiences of stress and adversity, we found that neither stress exposure was associated with observer-rated postnatal parenting behaviors in the present study, suggesting that these parenting behaviors were not influenced by women's experiences of stressful life events or intimate partner violence during pregnancy.
A robust literature documents the effects of the postnatal environment on child mental health, including stressors within the home, parental psychopathology, and parenting behaviors (70, 92–96). Accordingly, the present study accounted for many of these in our models—including several socioeconomic, psychosocial, and environmental factors—though this was not an exhaustive list. Although a growing body of work also documents the intergenerational associations between the prenatal environment and offspring psychopathology, such prenatal stressors likely operate through multiple pre- and postnatal pathways (both psychobiological and psychosocial). Findings presented herein should be interpreted within this context. Indeed, our findings suggest that these main effects of prenatal stressors should be considered within the context of the postnatal caregiving environment. Our study makes a particularly novel contribution in demonstrating that multi-year assessments of observer-rated maternal parenting behaviors moderated the association between women's pSLE and both child EF and externalizing problems. Specifically, for women who were able to provide higher levels of scaffolding, support, and encouragement to their children across several parent-child interaction tasks spanning two assessment time points, there was no increased risk of later child psychopathology associated with higher levels pSLE. This is contrasted with women who might not have had the necessary resources, structural supports, and ability to provide the same levels of scaffolding and encouragement to their children, wherein there was an increased risk of both later child EF and externalizing problems associated with higher levels of pSLE. These findings also suggest that many individuals are capable of providing high quality parenting despite prior exposure to adversity and violence (14, 66, 97). Interestingly, this moderating pattern was not found for prenatal intimate partner violence and either measure of child functioning. Methodology may be a possible explanation, given the difference in the range of possible values for each measure of maternal prenatal stress. Whereas, the pSLE measure had a range of 0–14, the measure for pIPV only had a range of 0–4, which might have reduced the ability to detect variations in scores between study participants based on differences in parenting quality. It is also possible that women's violence exposure, specifically, has less heterogeneous effects on offspring.
The present study highlights the importance of supporting and fostering women's capacity to optimize the caregiver-child relationship—often ignored in the prenatal programming literature—which served as a potential resilience-promoting factor in the prediction of child mental health problems. Women's capacity to provide sensitive, supportive parenting is not simply the product of—or responsibility of—a single caregiver, but rather a reflection of the larger community and societal context within which that parenting occurs (98). Many social determinants that affect maternal or child health and wellbeing also affect children's rearing environments, and therefore the resources that parents and caregivers have available to them within a given environment. Viewed in that framework, it is not surprising that community-based parenting programs that promote caregiver self-care, connection to resources, and knowledge of child attachment have proven efficacious in communities affected by violence (99, 100). Beyond community-based interventions that focus on providing more supports to parents and caregivers in higher-risk settings, national policies that increase resources for pregnant women and other caregivers—such as expansion of perinatal Medicaid coverage, increased parental leave, and perinatal cash transfer programs—can uplift our capacity to break intergenerational cycles of risk for child psychopathology and poor health (101–103). A growing body of literature highlights the importance and benefits of offering universal access to evidence-based parenting support and training programs—especially early in child development (104). In addition to improving child functioning, such intervention programs have also been shown to improve women's mental health (105). Indeed, multiple studies have shown that interventions focused on either parents or the parent-child relationship among families exposed to IPV, for example, have positive effects for both mothers and children (106, 107). Further, providing such universal access at a population level would not only allow all families to benefit from such programs but would also help in destigmatizing them.
Finally, regarding our test of moderation by child sex, we did not find that child sex significantly moderated the association between women's prenatal stressors and child psychopathology—although our sample was likely sufficiently powered to do so. This is not necessarily surprising, given the mixed findings regarding sex differences in previous examinations (17, 40). Indeed, although there was a main effect of child sex, wherein, on average, girls displayed marginally lower levels of EF problems, and significantly lower levels of externalizing problems, compared to boys—consistent with prior literature—these associations were not moderated by maternal stressful life events or intimate partner violence during pregnancy.
Also of note, fully one half of our sample experienced at least one type of pSLE (with almost one-third experiencing at least two), two-thirds reported experiencing at least one form of pIPV, and fully one third experienced at least one form of both pSLE and pIPV. These rates are in the higher range of estimates for pIPV prevalence, and may reflect unmet need for violence prevention and perinatal adversity support for women in this population (6, 8). Social inequity in the greater Memphis/Shelby County, Tennessee area—from which the present study cohort was recruited—has been associated with poor child health and educational outcomes, yet our findings also indicate the need for attention to upstream perinatal prevention and intervention efforts for families in this and similar populations (108–110). Further, we found that the associations between both pIPV and pSLE and child outcomes were independent of each other and, considered cumulatively, may have a greater impact on child mental health. Indeed, the stress exposures amounted to roughly 20–30% of the overall variance in psychopathology risk accounted for by each model.
The present study has a number of strengths: the use of a large, sociodemographically diverse sample including understudied Black urban Southern women, broad socioeconomic distribution across the sample, multiple indicators of prenatal stress exposure, and observer-rated parenting quality. However, there are several limitations. First, child outcome measures were reported by mothers. Recent work suggests limited bias from maternal report of child psychopathology (111), though we included important maternal covariates in our models to minimize potential reporter biases. Future studies would benefit from utilizing other informants and objective measures of child behavior. Second, although the inclusion of multiple domains of stressors, using two fairly distinct measures of exposures, is a strength—and adverse exposure counts are increasingly found to be strong predictors of health (112)—our measures did not consider the frequency or severity of the events, or the perceived experiences of distress from these stress exposures—all of which can contribute to the intergenerational effects of toxic stress on child functioning. Third, women retrospectively reported on pSLE when their children were ~8 years old. Although this approach is commonly used and recent evidence further supports validity of its use (especially for more significant and memorable life events) (75, 76, 113), there is still a potential for event recall bias. In addition, women's pIPV was assessed in the third trimester of pregnancy, wherein women reported their experiences over the past year, leaving the possibility that some pIPV was experienced in the few months prior to pregnancy. Finally, other sources of stress and adversity—both during pregnancy and postnatally—are relevant to offspring psychopathology (such as maternal experiences of daily stressors, racism, discrimination, as well as offspring exposure to traumatic events during childhood) but were not assessed with the present sample. Future intergenerational research would benefit from their inclusion.
Our findings add support to a growing body of research indicating the importance of preventing women's experiences of traumatic and stressful events during pregnancy—not just to protect women, but also for the potential intergenerational benefits with respect to offspring mental health. Moreover, our novel findings show that prenatal risks for child psychopathology are not uniform across families and may be buffered by strengthening and supporting the caregiving environment in the home. Interventions that provide additional support to families—both during the prenatal and postnatal period—and that include strategies and resources to strengthen caregiver-child relationships can play a key role in promoting caregiver and child resilience—even in the context of adversity (114). Indeed, caregiver wellbeing and behavior is key to promoting the development of child self-regulation skills, and could help prevent the development of later psychopathology (32, 54, 63). Further, given the transactional and cascading nature of the parent-child relationship—especially with regard to child externalizing psychopathology—ameliorating or preventing child mental health problems can also have downstream benefits of improving or preventing mental health problems for women who are mothers (115–117). Future research and intervention work, as well as health policy efforts, should focus on providing standard screening and universal preventative care to women during pregnancy (118) as a means of preemptively eliminating or reducing stressors for pregnant women and expecting families. Finally, additional research is certainly needed to identify more modifiable, postnatal resilience-promoting factors (19, 119, 120) in order to promote wellbeing across two generations and ameliorate risks for child psychopathology.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author.
Ethics Statement
This study was reviewed and approved by the University of Tennessee Health Science Center Institutional Review Board. Written informed consent to participate in this study was provided by the participants and/or their legal guardian/next of kin.
Author Contributions
NB, KL, CK, SS, and FT played a role in funding acquisition for the project supporting this manuscript. FT, JG, NB, and KL contributed to conception and design of the cohort study from which the data were drawn. FT was primarily responsible for project administration and supervision of data acquisition and curation, with support for data curation from NB and KL. SA and NB devised the manuscript study question. SA and ES designed the analytic approach for the study, with oversight by NB and wrote the first draft of the manuscript. ES performed the statistical analyses. LR and NB wrote sections of the manuscript. NB supervised the writing. All authors contributed to the interpretation of results, manuscript revision, and read and approved the submitted version.
Funding
The ECHO PATHWAYS consortium was funded by the NIH (grants 1UG3OD023271-01 and 4UH3OD023271-03). The CANDLE study was also funded by the Urban Child Institute and the NIH (R01 HL109977). The present study was also affiliated with support from the CANDLE Developmental Origins of Health and Disease study (CIHR award number MWG-146331). NB is the Lisa and John Pritzker Distinguished Professor of Developmental and Behavioral Health and receives support from the Lisa Stone Pritzker Family Foundation and the Tauber Family Foundation.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We are grateful for the participation of families enrolled in the CANDLE cohort, as well as the dedication of CANDLE research staff and investigators.
Abbreviations
EF, executive functioning; pIPV, prenatal intimate partner violence; pSLE, prental stressful life events.
References
1. Turner HA, Finkelhor D, Ormrod R. The effect of lifetime victimization on the mental health of children and adolescents. Soc Sci Med. (2006) 62:13–27. doi: 10.1016/j.socscimed.2005.05.030
2. Finkelhor D, Turner HA, Shattuck A, Hamby SL. Prevalence of childhood exposure to violence, crime, and abuse: results from the National Survey of Children's Exposure to Violence. J Am Med Assoc Pediatr. (2015) 169:746–54. doi: 10.1001/jamapediatrics.2015.0676
3. Barrero-Castillero A, Morton SU, Nelson CA, Smith VC. Psychosocial stress and adversity: effects from the perinatal period to adulthood. Neoreviews. (2019) 20:e686–96. doi: 10.1542/neo.20-12-e686
4. Sheffler JL, Stanley I, Sachs-Ericsson N. ACEs and mental health outcomes. Adv Res Pract Policy Prev. (2020) 5:47–69. doi: 10.1016/B978-0-12-816065-7.00004-5
5. Schilling EA, Aseltine RH, Gore S. Adverse childhood experiences and mental health in young adults: a longitudinal survey. BMC Public Health. (2007) 7:1–10. doi: 10.1186/1471-2458-7-30
6. Hayashi KS, Hitomi CC. Intimate partner violence and its health impact on ethnic minority women. J Womens Health. (2014) 24:62–79. doi: 10.1089/jwh.2014.4879
7. Graham LM, Ranapurwala SI, Zimmer C, Macy RJ, Rizo CF, Lanier P, et al. Disparities in potential years of life lost due to intimate partner violence: data from 16 states for 2006–2015. PLoS ONE. (2021) 16:e0246477. doi: 10.1371/journal.pone.0246477
8. Devries KM, Kishor S, Johnson H, Stöckl H, Bacchus LJ, Garcia-Moreno C, et al. Intimate partner violence during pregnancy: analysis of prevalence data from 19 countries. Reprod Health Matters. (2010) 18:158–70. doi: 10.1016/S0968-8080(10)36533-5
9. Ahmad SI, Rudd KL, LeWinn KZ, Mason WA, Murphy L, Juarez PD, et al. Maternal childhood trauma and prenatal stressors are associated with child behavioral health. J Dev Orig Health Dis. (2021) 2021:1–11. doi: 10.1017/S2040174421000581
10. Braveman P, Marchi K, Egerter S, Kim S, Metzler M, Stancil T, et al. Poverty, near-poverty, and hardship around the time of pregnancy. Matern Child Health J. (2010) 14:20–35. doi: 10.1007/s10995-008-0427-0
11. World Health Organization. Violence Against Women. (2021). Available online at: https://www.who.int/news-room/fact-sheets/detail/violence-against-women (accessed December 9, 2021).
12. Burns ER, Farr SL, Howards PP. Stressful life events experienced by women in the year before their infants' births — United States, 2000–2010. MMWR Morb Mortal Wkly Rep. (2015) 64:247–51.
13. Aschbacher K, Hagan M, Steine IM, Rivera L, Cole S, Baccarella A, et al. Adversity in early life and pregnancy are immunologically distinct from total life adversity: macrophage-associated phenotypes in women exposed to interpersonal violence. Transl Psychiatry. (2021) 11:1–9. doi: 10.1038/s41398-021-01498-1
14. Davis EP, Narayan AJ. Pregnancy as a period of risk, adaptation, and resilience for mothers and infants. Dev Psychopathol. (2020) 32:1625–39. doi: 10.1017/S0954579420001121
15. Ehrensaft MK, Cohen P. Contribution of family violence to the intergenerational transmission of externalizing behavior. Prev Sci. (2012) 13:370–83. doi: 10.1007/s11121-011-0223-8
16. Campbell JC. Health consequences of intimate partner violence. Lancet. (2002) 359:1331–6. doi: 10.1016/S0140-6736(02)08336-8
17. Van den Bergh BRH, van den Heuvel MI, Lahti M, Braeken M, de Rooij SR, Entringer S, et al. Prenatal developmental origins of behavior and mental health: the influence of maternal stress in pregnancy. Neurosci Biobehav Rev. (2020) 117:26–64. doi: 10.1016/j.neubiorev.2017.07.003
18. Monk C, Lugo-Candelas C, Trumpff C. Prenatal developmental origins of future psychopathology: mechanisms and pathways. Annu Rev Clin Psychol. (2019) 15:317–44. doi: 10.1146/annurev-clinpsy-050718-095539
19. Hartman S, Belsky J. Prenatal programming of postnatal plasticity revisited - and extended. Dev Psychopathol. (2018) 30:825–42. doi: 10.1017/S0954579418000548
20. Alhusen JL, Bullock L, Sharps P, Schminkey D, Comstock E, Campbell J. Intimate partner violence during pregnancy and adverse neonatal outcomes in low-income women. J Womens Health. (2014) 23:920–6. doi: 10.1089/jwh.2014.4862
21. Cannon EA, Bonomi AE, Anderson ML, Rivara FP. The intergenerational transmission of witnessing intimate partner violence. Arch Pediatr Adolesc Med. (2009) 163:706–8. doi: 10.1001/archpediatrics.2009.91
22. Smith CA, Ireland TO, Park A, Elwyn L, Thornberry TP. Intergenerational continuities and discontinuities in intimate partner violence: a two-generational prospective study. J Interpers Violence. (2011) 26:3720–52. doi: 10.1177/0886260511403751
23. Evans SE, Davies C, DiLillo D. Exposure to domestic violence: a meta-analysis of child and adolescent outcomes. Aggress Violent Behav. (2008) 13:131–40. doi: 10.1016/j.avb.2008.02.005
24. Steine IM, LeWinn KZ, Lisha N, Tylavsky F, Smith R, Bowman M, et al. Maternal exposure to childhood traumatic events, but not multi-domain psychosocial stressors, predict placental corticotrophin releasing hormone across pregnancy. Soc Sci Med. (2020) 266:113461. doi: 10.1016/j.socscimed.2020.113461
25. Cottrell EC, Seckl JR. Prenatal stress, glucocorticoids and the programming of adult disease. Front Behav Neurosci. (2009) 3:19. doi: 10.3389/neuro.08.019.2009
26. Krontira AC, Cruceanu C, Binder EB. Glucocorticoids as mediators of adverse outcomes of prenatal stress. Trends Neurosci. (2020) 43:394–405. doi: 10.1016/j.tins.2020.03.008
27. Osborne S, Biaggi A, Chua TE, Du Preez A, Hazelgrove K, Nikkheslat N, et al. Antenatal depression programs cortisol stress reactivity in offspring through increased maternal inflammation and cortisol in pregnancy: the Psychiatry Research and Motherhood – Depression (PRAM-D) Study. Psychoneuroendocrinology. (2018) 98:211–21. doi: 10.1016/j.psyneuen.2018.06.017
28. MacKinnon N, Kingsbury M, Mahedy L, Evans J, Colman I. The association between prenatal stress and externalizing symptoms in childhood: evidence from the avon longitudinal study of parents and children. Biol Psychiatry. (2018) 83:100–8. doi: 10.1016/j.biopsych.2017.07.010
29. Waltermaurer E, Watson CA, McNutt LA. Black women's health: the effect of perceived racism and intimate partner violence. Violence Against Women. (2006) 12:1214–22. doi: 10.1177/1077801206293545
30. Bush NR, Jones-Mason K, Coccia M, Caron Z, Alkon A, Thomas M, et al. Effects of pre- and postnatal maternal stress on infant temperament and autonomic nervous system reactivity and regulation in a diverse, low-income population. Dev Psychopathol. (2017) 29:1553–71. doi: 10.1017/S0954579417001237
31. Schoemaker K, Mulder H, Deković M, Matthys W. Executive functions in preschool children with externalizing behavior problems: a meta-analysis. J Abnorm Child Psychol. (2013) 41:457–71. doi: 10.1007/s10802-012-9684-x
32. Bridgett DJ, Burt NM, Edwards ES, Deater-Deckard K. Intergenerational transmission of self-regulation: a multidisciplinary review and integrative conceptual framework. Psychol Bull. (2015) 141:602–54. doi: 10.1037/a0038662
33. Hodes GE, Epperson CN. Sex differences in vulnerability and resilience to stress across the life span. Biol Psychiatry. 86:421–32. doi: 10.1016/j.biopsych.2019.04.028
34. Young SE, Friedman NP, Willcutt EG, Corley RP, Hewitt JK. Behavioral disinhibition: Liability for externalizing spectrum disorders and its genetic and environmental relation to response inhibition across adolescence. J Abnorm Psychol. (2009) 118:117–30. doi: 10.1037/a0014657
35. Beauchaine TP, Shader TM, Hinshaw SP. An ontogenic processes model of externalizing psychopathology. In: Beauchaine TP, Hinshaw SP, editors, The Oxford Handbook of Externalizing Spectrum Disorders. New York, NY: Oxford University Press (2016). p. 485–501, Chapter 27, 521 Pages. (Oxford library of psychology BT - The Oxford handbook of externalizing spectrum disorders).
36. Reef J, Diamantopoulou S, Van Meurs I, Verhulst FC, Van Der Ende J. Developmental trajectories of child to adolescent externalizing behavior and adult DSM-IV disorder: results of a 24-year longitudinal study. Soc Psychiatry Psychiatr Epidemiol. (2011) 46:1233–41. doi: 10.1007/s00127-010-0297-9
37. Neuenschwander R, Hookenson K, Brain U, Grunau RE, Devlin AM, Weinberg J, et al. Children's stress regulation mediates the association between prenatal maternal mood and child executive functions for boys, but not girls. Dev Psychopathol. (2018) 30:953–69. doi: 10.1017/S095457941800041X
38. Buss C, Davis EP, Hobel CJ, Sandman CA. Maternal pregnancy-specific anxiety is associated with child executive function at 6–9 years age. Stress. (2011) 14:665–76. doi: 10.3109/10253890.2011.623250
39. Obradović J, Portilla XA, Ballard PJ. Biological sensitivity to family income: differential effects on early executive functioning. Child Dev. (2016) 87:374–84. doi: 10.1111/cdev.12475
40. Glover V, Hill J. Sex differences in the programming effects of prenatal stress on psychopathology and stress responses: an evolutionary perspective. Physiol Behav. (2012) 106:736–40. doi: 10.1016/j.physbeh.2012.02.011
41. Sutherland S, Brunwasser SM. Sex differences in vulnerability to prenatal stress: a review of the recent literature. Curr Psychiatry Rep. (2018) 20:4. doi: 10.1007/s11920-018-0961-4
42. Seiffge-Krenke I, Persike M, Besevegis E, Chau C, Karaman NG, Lannegrand-Willems L, et al. Culture beats gender? The importance of controlling for identity- and parenting-related risk factors in adolescent psychopathology. J Adolesc. (2018) 63:194–208. doi: 10.1016/j.adolescence.2017.12.011
43. Rudd KL, Cheng S, Cordeiro A, Coccia M, Karr CJ, LeWinn KZ, et al. Associations between maternal stressful life events and perceived distress during pregnancy and child mental health at age 4. Res Child Adolesc Psychopathol. (2022). doi: 10.1007/s10802-022-00911-7
44. DiPietro JA, Voegtline KM. The gestational foundation of sex differences in development and vulnerability. Neuroscience. (2017) 342:4–20. doi: 10.1016/j.neuroscience.2015.07.068
45. Carpenter T, Grecian SM, Reynolds RM. Sex differences in early-life programming of the hypothalamic–pituitary–adrenal axis in humans suggest increased vulnerability in females: a systematic review. J Dev Orig Health Dis. (2017) 8:244–55. doi: 10.1017/S204017441600074X
46. Braithwaite EC, Pickles A, Sharp H, Glover V, O'Donnell KJ, Tibu F, et al. Maternal prenatal cortisol predicts infant negative emotionality in a sex-dependent manner. Physiol Behav. (2017) 175:31–6. doi: 10.1016/j.physbeh.2017.03.017
47. Graham AM, Rasmussen JM, Entringer S, Ben Ward E, Rudolph MD, Gilmore JH, et al. Maternal cortisol concentrations during pregnancy and sex-specific associations with neonatal amygdala connectivity and emerging internalizing behaviors. Biol Psychiatry. (2019) 85:172–81. doi: 10.1016/j.biopsych.2018.06.023
48. Hicks LM, Swales DA, Garcia SE, Driver C, Davis EP. Does prenatal maternal distress contribute to sex differences in child psychopathology? Curr Psychiatry Rep. (2019) 21:7. doi: 10.1007/s11920-019-0992-5
49. Rodriguez A, Bohlin G. Are maternal smoking and stress during pregnancy related to ADHD symptoms in children? J Child Psychol Psychiatry Allied Discip. (2005) 46:246–54. doi: 10.1111/j.1469-7610.2004.00359.x
50. Ronald A, Pennell CE, Whitehouse AJO. Prenatal maternal stress associated with ADHD and autistic traits in early childhood. Front Psychol. (2011) 1:1–8. doi: 10.3389/fpsyg.2010.00223
51. Doyle C, Cicchetti D. Future directions in prenatal stress research: challenges and opportunities related to advancing our understanding of prenatal developmental origins of risk for psychopathology. Dev Psychopathol. (2018) 30:721–4. doi: 10.1017/S095457941800069X
52. Hartman S, Freeman SM, Bales KL, Belsky J. Prenatal stress as a risk—and an opportunity—factor. Psychol Sci. (2018) 29:572–80. doi: 10.1177/0956797617739983
53. Hartman S, Eilertsen EM, Ystrom E, Belsky J, Gjerde LC. Does prenatal stress amplify effects of postnatal maternal depressive and anxiety symptoms on child problem behavior? Dev Psychol. (2020) 56:128–37. doi: 10.1037/dev0000850
54. Fay-Stammbach T, Hawes DJ, Meredith P. Parenting influences on executive function in early childhood: a review. Child Dev Perspect. (2014) 8:258–64. doi: 10.1111/cdep.12095
55. Pinquart M. Associations of parenting dimensions and styles with externalizing problems of children and adolescents: an updated meta-analysis. Dev Psychol. (2017) 53:873–932. doi: 10.1037/dev0000295
56. Chiesa AE, Kallechey L, Harlaar N, Rashaan Ford C, Garrido EF, Betts WR, et al. Intimate partner violence victimization and parenting: a systematic review. Child Abuse Negl. (2018) 80:285–300. doi: 10.1016/j.chiabu.2018.03.028
57. Holmes MR. Aggressive behavior of children exposed to intimate partner violence: an examination of maternal mental health, maternal warmth and child maltreatment. Child Abuse Negl. (2013) 37:520–30. doi: 10.1016/j.chiabu.2012.12.006
58. Gustafsson HC, Cox MJ, Blair C. Maternal parenting as a mediator of the relationship between intimate partner violence and effortful control. J Fam Psychol. (2012) 26:115. doi: 10.1037/a0026283
59. Chung G, Jensen TM, Parisi A, Macy RJ, Lanier P. Impact of intimate partner violence on parenting and children's externalizing behaviors: transactional processes over time. Violence Against Women. (2021) 27:2576. doi: 10.1177/1077801220985125
60. Johnson AM, Hawes DJ, Eisenberg N, Kohlhoff J, Dudeney J. Emotion socialization and child conduct problems: a comprehensive review and meta-analysis. Clin Psychol Rev. (2017) 54:65–80. doi: 10.1016/j.cpr.2017.04.001
61. Mingebach T, Kamp-Becker I, Christiansen H, Weber L. Meta-meta-analysis on the effectiveness of parent-based interventions for the treatment of child externalizing behavior problems. PLoS ONE. (2018) 13:e0202855. doi: 10.1371/journal.pone.0202855
62. Zelazo PD. Executive function and psychopathology: a neurodevelopmental perspective. Annu Rev Clin Psychol. (2020) 16:431–54. doi: 10.1146/annurev-clinpsy-072319-024242
63. Traub F, Boynton-Jarrett R. Modifiable resilience factors to childhood adversity for clinical pediatric practice. Pediatrics. (2017) 139:2569. doi: 10.1542/peds.2016-2569
64. Sturge-Apple ML, Jones HR, Suor JH. When stress gets into your head: socioeconomic risk, executive functions, and maternal sensitivity across childrearing contexts. J Fam Psychol. (2017) 31:160–9. doi: 10.1037/fam0000265
65. Pettit GS, Bates JE, Dodge KA. Supportive parenting, ecological context, and children's adjustment: a seven-year longitudianl study. Child Dev. (1997) 68:908–23. doi: 10.1111/j.1467-8624.1997.tb01970.x
66. Narayan AJ, Ippen CG, Harris WW, Lieberman AF. Protective factors that buffer against the intergenerational transmission of trauma from mothers to young children: a replication study of angels in the nursery. Dev Psychopathol. (2019) 31:173–87. doi: 10.1017/S0954579418001530
67. Herbers JE, Cutuli JJ, Supkoff LM, Narayan AJ, Masten AS. Parenting and coregulation: adaptive systems for competence in children experiencing homelessness. Am J Orthopsychiatry. (2014) 84:420. doi: 10.1037/h0099843
68. Korelitz KE, Garber J. Congruence of parents' and children's perceptions of parenting: a meta-analysis. J Youth Adolesc. (2016) 45:1973. doi: 10.1007/s10964-016-0524-0
69. Morsbach SK, Prinz RJ. Understanding and improving the validity of self-report of parenting. Clin Child Fam Psychol Rev. (2006) 9:1–21. doi: 10.1007/s10567-006-0001-5
70. Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. (2011) 32:381–98. doi: 10.1146/annurev-publhealth-031210-101218
71. Slopen N, Shonkoff JP, Albert MA, Yoshikawa H, Jacobs A, Stoltz R, et al. Racial disparities in child adversity in the US: interactions with family immigration history and income. Am J Prev Med. (2016) 50:47–56. doi: 10.1016/j.amepre.2015.06.013
72. Sontag-Padilla L, Burns R, Shih R, Griffin B, Martin L, Chandra A. The Urban Child Institute CANDLE Study: Methodological Overview Baseline Sample Description. RAND Corporation (2015). Available online at: http://www.rand.org/pubs/research_reports/RR1336.html (accessed April 1, 2022).
73. LeWinn KZ, Bush NR, Batra A, Tylavsky F, Rehkopf D. Identification of modifiable social and behavioral factors associated with childhood cognitive performance. J Am Med Assoc Pediatr. (2020) 94143:1–10. doi: 10.1001/jamapediatrics.2020.2904
74. Whitehead NS, Brogan DJ, Blackmore-Prince C, Hill HA. Correlates of experiencing life events just before or during pregnancy. J Psychosom Obstet Gynecol. (2003) 24:77–86. doi: 10.3109/01674820309042805
75. Ramos AM, Marceau K, Neiderhiser JM, De Araujo-Greecher M, Natsuaki MN, Leve LD. Maternal consistency in recalling prenatal experiences at 6 months and 8 years postnatal. J Dev Behav Pediatr. (2020) 41:698–705. doi: 10.1097/DBP.0000000000000841
76. Reuben A, Moffitt TE, Caspi A, Belsky DW, Harrington H, Schroeder F, et al. Lest we forget: comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. J Child Psychol Psychiatry Allied Discip. (2016) 57:1103–12. doi: 10.1111/jcpp.12621
77. Straus MA, Douglas EM. A short form of the revised conflict tactics scales, and typologies for severity and mutuality. Violence Vict. (2004) 19:507–20. doi: 10.1891/vivi.19.5.507.63686
78. Huber CJ. Documenting quality of parent-child interaction: use of the NCAST scales. Infants Young Children. (1991) 4:63–75. doi: 10.1097/00001163-199110000-00012
79. Oxford ML, Findlay DM. NCAST Caregiver/Parent-Child Interaction Teaching Manual. Seattle, WA: NCAST Programs, University of Washington, School of Nursing (2013).
80. Ransone SH, Graff JC, Bush AJ, Oxford M, Wicks MN. Psychometric evaluation of the nursing child assessment teaching (NCAT) scale in a community-based sample. Res Nurs Health. (2018) 41:301–11. doi: 10.1002/nur.21867
81. Graff JC, Bush AJ, Palmer FB, Murphy LE, Whitaker TM, Tylavsky FA. Maternal and child characteristics associated with mother–child interaction in one-year-olds. Res Nurs Heal. (2017) 40:323–40. doi: 10.1002/nur.21798
82. Gioia GA, Espy KA, Isquith PK. Behavior Rating Inventory of Executive Function-Preschool Version. Lutz, FL: Psychological Assessment Resources (2003).
83. Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms and Profiles. Burlington, VT: Research Center for Children, Youth, and Families, University of Vermont (2000).
84. Bryant BE, Jordan A, Clark US. Race as a social construct in psychiatry research and practice. J Am Med Assoc Psychiatry. (2022) 79:93. doi: 10.1001/jamapsychiatry.2021.2877
85. Wechsler D. Wechsler Abbreviated Scale of Intelligence–Second Edition Manual. Bloomington, MN: Pearson (2011). doi: 10.1037/t15171-000
86. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item edinburgh postnatal depression scale. Br J Psychiatry. (1987) 150:782–6. doi: 10.1192/bjp.150.6.782
87. Radloff LS. The CES-D scale. Appl Psychol Meas. (1977) 1:385–401. doi: 10.1177/014662167700100306
88. Stekhoven DJ, Buhlmann P. MissForest–non-parametric missing value imputation for mixed-type data. Bioinformatics. (2012) 28:112–8. doi: 10.1093/bioinformatics/btr597
89. Shah AD, Bartlett JW, Carpenter J, Nicholas O, Hemingway H. Comparison of random forest and parametric imputation models for imputing missing data using MICE: a CALIBER study. Am J Epidemiol. (2014) 179:764–74. doi: 10.1093/aje/kwt312
90. Aiken LS, West SG. Testing and Interpreting Interactions in Multiple Regression. Thousand Oaks, CA: Sage Publications (1991).
91. Sulik MJ. Introduction to the special section on executive functions and externalizing symptoms. J Abnormal Child Psychol. (2017) 45:1473–5. doi: 10.1371/journal.pone.0112393
92. Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. J Am Med Assoc. (2009) 301:2252–9. doi: 10.1001/jama.2009.754
93. Herba CM, Glover V, Ramchandani PG, Rondon MB. Maternal depression and mental health in early childhood: an examination of underlying mechanisms in low-income and middle-income countries. Lancet Psychiatry. (2016) 3:983–92. doi: 10.1016/S2215-0366(16)30148-1
94. Allen J, Balfour R, Bell R, Marmot M. Social determinants of mental health. Int Rev Psychiatry. (2014) 26:392–407. doi: 10.3109/09540261.2014.928270
95. Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, et al. Child and adolescent mental health worldwide: evidence for action. Lancet. (2011) 378:1515–25. doi: 10.1016/S0140-6736(11)60827-1
96. Peverill M, Dirks MA, Narvaja T, Herts KL, Comer JS, McLaughlin KA. Socioeconomic status and child psychopathology in the United States: a meta-analysis of population-based studies. Clin Psychol Rev. (2021) 83:101933. doi: 10.1016/j.cpr.2020.101933
97. Narayan AJ, Lieberman AF, Masten AS. Intergenerational transmission and prevention of adverse childhood experiences (ACEs). Clin Psychol Rev. (2021) 85:101997. doi: 10.1016/j.cpr.2021.101997
98. Winett LB, Wulf AB, Wallack L. Framing strategies to avoid mother-blame in communicating the origins of chronic disease. Am J Public Health. (2016) 106:1369–73. doi: 10.2105/AJPH.2016.303239
99. Rosenblum KL, Muzik M, Morelen DM, Alfafara EA, Miller NM, Waddell RM, et al. A community-based randomized controlled trial of Mom Power parenting intervention for mothers with interpersonal trauma histories and their young children. Arch Womens Ment Health. (2017) 20:673–86. doi: 10.1007/s00737-017-0734-9
100. Waters SF, Hulette A, Davis M, Bernstein R, Lieberman A. Evidence for attachment vitamins: a trauma-informed universal prevention programme for parents of young children. Early Child Dev Care. (2018) 190:1109–14. doi: 10.1080/03004430.2018.1516650
101. Ginja R, Jans J, Karimi A. Parental leave benefits, household labor supply, and children's long-run outcomes. J Labor Econ. (2019) 38:261–320. doi: 10.1086/704615
102. Margerison CE, Hettinger K, Kaestner R, Goldman-Mellor S, Gartner D. Medicaid expansion associated with some improvements in perinatal mental health. Health Aff. (2021) 40:1605–11. doi: 10.1377/hlthaff.2021.00776
103. Struck S, Enns JE, Sanguins J, Chartier M, Nickel NC, Chateau D, et al. An unconditional prenatal cash benefit is associated with improved birth and early childhood outcomes for Metis families in Manitoba, Canada. Child Youth Serv Rev. (2021) 121:105853. doi: 10.1016/j.childyouth.2020.105853
104. Sanders MR, Divan G, Singhal M, Turner KMT, Velleman R, Michelson D, et al. Scaling up parenting interventions is critical for attaining the sustainable development goals. Child Psychiatry Hum Dev. (2021) 2021:1–12. doi: 10.1007/s10578-021-01171-0
105. Everett Y, Martin CG, Zalewski M. A systematic review focusing on psychotherapeutic interventions that impact parental psychopathology, child psychopathology and parenting behavior. Clin Child Fam Psychol Rev. (2021) 24:579–98. doi: 10.1007/s10567-021-00355-3
106. Katz LF, Gurtovenko K, Maliken A, Stettler N, Kawamura J, Fladeboe K. An emotion coaching parenting intervention for families exposed to intimate partner violence. Dev Psychol. (2020) 56:638–51. doi: 10.1037/dev0000800
107. Austin AE, Shanahan ME, Barrios Y V, Macy RJ. A systematic review of interventions for women parenting in the context of intimate partner violence. Trauma Violence Abus. (2019) 20:498–519. doi: 10.1177/1524838017719233
108. Nelson SL. Special Education Reform Policies and the Permanence of Oppression: A Critical Race Case Study of Special Education Reform in Shelby County, Tennessee. Washington, DC: Howard Law J. (2016). p. 60.
109. Shin EK, Shaban-Nejad A. Urban decay and pediatric asthma prevalence in Memphis, Tennessee: urban data integration for efficient population health surveillance. IEEE Access. (2018) 6:46281–9. doi: 10.1109/ACCESS.2018.2866069
110. Turner D, Simpson P, Li SH, Scanlon M, Quasney MW. Racial disparities in pediatric intensive care unit admissions. South Med J. (2011) 104:640–6. doi: 10.1097/SMJ.0b013e3182296e52
111. Olino TM, Michelini G, Mennies RJ, Kotov R, Klein DN. Does maternal psychopathology bias reports of offspring symptoms? A study using moderated non-linear factor analysis. J Child Psychol Psychiatry. (2021) 2021:13394. doi: 10.1111/jcpp.13394
112. Grummitt LR, Kreski NT, Kim SG, Platt J, Keyes KM, McLaughlin KA. Association of childhood adversity with morbidity and mortality in US adults: a systematic review. J Am Med Assoc Pediatr. (2021) 2021:2320. doi: 10.1001/jamapediatrics.2021.2320
113. Felder JN, Epel E, Coccia M, Cordeiro A, Laraia B, Adler N, et al. Prenatal maternal objective and subjective stress exposures and rapid infant weight gain. J Pediatr. (2020) 222:45–51. doi: 10.1016/j.jpeds.2020.03.017
114. Wakschlag LS, Tandon D, Krogh-Jespersen S, Petitclerc A, Nielsen A, Ghaffari R, et al. Moving the dial on prenatal stress mechanisms of neurodevelopmental vulnerability to mental health problems: a personalized prevention proof of concept. Dev Psychobiol. (2020) 2020:dev.22057. doi: 10.1002/dev.22057
115. Patterson GR, Forgatch MS, Degarmo DS. Cascading effects following intervention. Dev Psychopathol. (2010) 22:949. doi: 10.1017/S0954579410000568
116. Masten AS, Lucke CM, Nelson KM, Stallworthy IC. Resilience in development and psychopathology: multisystem perspectives. Annu Rev Clin Psychol. (2021) 17:521–49. doi: 10.1146/annurev-clinpsy-081219-120307
117. Yan N, Ansari A, Peng P. Reconsidering the relation between parental functioning and child externalizing behaviors: a meta-analysis on child-driven effects. J Fam Psychol. (2021) 35:225–35. doi: 10.1037/fam0000805
118. Bush NR, Savitz J, Coccia M, Jones-Mason K, Adler N, Boyce WT, et al. Maternal stress during pregnancy predicts infant infectious and noninfectious illness. J Pediatr. (2020) 228:41. doi: 10.1016/j.jpeds.2020.08.041
119. Kentner AC, Cryan JF, Brummelte S. Resilience priming: translational models for understanding resiliency and adaptation to early life adversity. In: Developmental Psychobiology. John Wiley and Sons Inc. (2019). p. 350–75. Available online at: https://onlinelibrary.wiley.com/doi/full/10.1002/dev.21775 (accessed December 2, 2020).
Keywords: prenatal stress, executive functioning, externalizing behavior, parenting, child psychopathology
Citation: Ahmad SI, Shih EW, LeWinn KZ, Rivera L, Graff JC, Mason WA, Karr CJ, Sathyanarayana S, Tylavsky FA and Bush NR (2022) Intergenerational Transmission of Effects of Women's Stressors During Pregnancy: Child Psychopathology and the Protective Role of Parenting. Front. Psychiatry 13:838535. doi: 10.3389/fpsyt.2022.838535
Received: 17 December 2021; Accepted: 23 March 2022;
Published: 25 April 2022.
Edited by:
Liat Helpman, University of Haifa, IsraelReviewed by:
Roser Granero, Universitat Autònoma de Barcelona, SpainDominik A. Moser, Centre Hospitalier Universitaire Vaudois (CHUV), Switzerland
Copyright © 2022 Ahmad, Shih, LeWinn, Rivera, Graff, Mason, Karr, Sathyanarayana, Tylavsky and Bush. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nicole R. Bush, bmljb2xlLmJ1c2hAdWNzZi5lZHU=
 Shaikh I. Ahmad
Shaikh I. Ahmad Emily W. Shih
Emily W. Shih Kaja Z. LeWinn
Kaja Z. LeWinn Luisa Rivera
Luisa Rivera J. Carolyn Graff3,4
J. Carolyn Graff3,4 Nicole R. Bush
Nicole R. Bush