- 1Department of Psychiatry and Behavioral Medicine, School of Medicine, Louisiana State University Health Sciences Center—Shreveport, Shreveport, LA, United States
- 2Louisiana Addiction Research Center, Shreveport, LA, United States
- 3Caddo Parish Magnet High School, Shreveport, LA, United States
- 4Yale University, New Haven, CT, United States
- 5Child Study Center, Yale School of Medicine, New Haven, CT, United States
- 6School of Communication and Media Studies, Louisiana Tech University, Ruston, LA, United States
- 7Department of Pharmacology, Toxicology and Neuroscience, School of Graduate Studies, Louisiana State University Health Sciences Center—Shreveport, Shreveport, LA, United States
Background: The evaluation of teens with self-harming thoughts (SHT) is a high-stakes task for physicians in community and emergency department (ED) settings. The lived experience of adolescents with stress and SHT provides an important source of insight for mental health professionals who evaluate and treat teens A snapshot of the lived experience of teens in northwest Louisiana was captured by the Step Forward Teen Advisory Council (TAC) in 2019. The TAC surveyed peers with the goal of identifying common stressors experienced by local teens in order to inform policy and practices in the local school system. The identification of stressors is a critical step in addressing SHT as adolescents who experience life stressors are at increased risk for self-harming thoughts (SHT), a known precursor to self-harm and suicide. Assessing youth for life stressors is a critical element of suicide prevention.
Methods: Local teens queried 5,070 peers attending Caddo Parish schools to better understand the stressors faced by high school students in Northwest Louisiana using a student developed survey. Results were presented to peers at a virtual summit where teens developed action items to reduce stress and presented findings to local leaders. Their efforts ultimately lead to increased supports for students in local schools.
Results: Over half of the teens surveyed reported stressors that negatively impacted their physical or emotional well-being. Students endorsing self-harming thoughts reported an average of 7.82 stressors as compared to 3.47 in peers without SHT. Teens with stressors at both home and school were more likely to experience SHT than teens with stressors in a single location.
Conclusion: The Gen Z students who developed the TAC Survey identified stress as a major concern for teens in Northwest Louisiana. The TAC Survey data aligns local experience with established data regarding the association between stress, depression and SHT. Second, the results highlight the importance of diving deep to identify all stressors when assessing the risk of self-harm. Finally, the lived experience of local teens with SHT provides critical information for professionals to better understand risk for SHT and suicide in our region and beyond.
Introduction
The evaluation of teens with self-harming thoughts (SHT) is a high-stakes task for physicians in community and emergency department (ED) settings. ED visits related to SHT doubled nationally between 2007 and 2015 (1, 2). Rates of suicidal ideation (SI) increased in March through July 2020 as compared with 2019; however, rates were significant only in March and July (3). During the pandemic, emergency departments have experienced a marked increase in visits by teens related to suspected suicide attempts, with a 50.6% increase for girls and a 3.7% for boys in 2021 compared to 2019 (4).
Self-harming thoughts (SHT), including but not limited to suicide ideation (SI), are a precursor to self-harm and suicide, the second leading cause of death for youth between the ages of 12–18 years (5). Reports of the lifetime prevalence of SI among adolescents range from 9.6 to 39.4% with increased prevalence noted among specific subgroups, including LGBTQ youth and females (6–9). The rate of SI among LGBTQ adolescents exceeds that of peers, with 42% endorsing SI compared to 14% for those non-identifying youth in a study of nearly 5,000 teens (10). Furthermore, the rate of SI for females is twice that of males (11, 12). Despite a slight overall decrease in self-reported suicidal ideation (SI) between 2015 and 2017, SI remains common with a weighted overall prevalence rate of 18.8% among high school students between 1991 and 2017 (13). Alarmingly, Caddo Parish data does not reflect this trend. According to the Caring Communities Youth Survey, SI increased by 19% among 10th graders and a 27% among 12th graders between 2016 and 2020 (14).
The United States Surgeon General's 2021 Call to Action to Implement the National Strategy for Suicide Prevention (15) highlights the importance of screening for SHT. While the presence of a mental disorder is up to 90% in persons who die by suicide, adolescence is a time when mental disorders often emerge. This fact supports the importance of screening for symptoms and identifying emerging mental illness in youth with SHT in order to prevent suicide (16). Psychosocial factors contributing to suicide risk include being bullied, child abuse, stressful life events, and suicide contagion (17–20). Teens lived experience with bullying, abuse, and stress were factors that were also included in the Teen Advisory Council's survey.
Assessing SHT requires query into many factors including symptoms of mental illness, risk and protective factors, and psychosocial stressors. Symptoms of mental illness that are correlated with SHT include depressed mood, anxiety, hopelessness, social isolation, eating disorders, and substance use (9, 21–24). Support from family and friends is protective against SHT, especially for girls (25). Lower parent-family connectedness has been reported among sexual minority youth, a population at increased risk for SHT (26). School connectedness has also been identified as a protective factor in reducing suicide risk (27, 28). Beliefs surrounding help-seeking may moderate the progression of SHT to a suicide attempt (10). The assessment of suicide risk balances symptoms of mental disorders, risk factors, and psychosocial stressors against protective factors to design individualized safety and treatment plans. Knowledge of local trends in SI, youth stress, and youth supports is critical if clinicians are to protect youth.
Methods
Step Forward is a community organization in Northwest Louisiana working to intentionally address complex problems in the local community. Specifically, they aim to ensure success for every child from cradle to career. To further this goal, the Step Forward Teen Advisory Committee (TAC) was established in the spring of 2019 to allow local teens to share their knowledge and perspectives regarding the needs of local youth. The TAC served as expert advisors to Step Forward community leaders in to identify key focus areas and to develop action plans aimed at improving outcomes for all teens in Northwest Louisiana. These young leaders identified three key objectives: improve teen mental health, increase diverse career training opportunities, and increase youth civic involvement. Improving teen mental health became the primary focus of the TAC.
With the goal of formulating a strategic plan to improve teen mental health, the TAC first sought to establish a baseline for Teen Mental Wellness in the region through a survey. The TAC survey consisted of 15 questions concerning students' age, gender, parish of residence, and stressors that they may have faced or were facing at the time. Additional questions focused on feelings of belonging, engagement with their school and community, and social media usage. The survey questions were reviewed by a professional mental health evaluator for scope and language use, specifically to focus on wellness rather than mental illness.
The local school superintendent approved survey before it was distributed through an online platform, SurveyMonkey. All students in attending public high schools in Northwest Louisiana were invited to participate individually and during their English classes from mid-December 2019 to mid-January 2020. The survey received 5,070 student responses with student ages ranging from 14 to 19 years. While all high school students were invited to participate, most respondents (4,989) were from the Caddo Parish School District due to the robust support from the superintendent. The data received was first analyzed through SurveyMonkey and then transferred to Microsoft Excel for further analysis by the TAC for presentation to area leaders. Analysis for this article was performed using STATA/BE v17 (StataCorp, LLC). Continuous variables are presented as mean (SD). Categorical variables are presented as the number (proportion or %) of participants. P-values for continuous variables correspond to Two-sample T-test (for comparison of means between groups). P-values for categorical variables correspond to Pearson's χ2 tests. Univariate logistic regression models were used to identify predictors to estimate the odds of the outcome of student variables in relation to SHT.
During the 2019–20 school year, there were 11,248 students enrolled in ten public high schools in Caddo Parish. The demographics of Caddo Parish at this time were characterized by 71% minority populations with 29% being White. 49.52% were female and 50.48% were male with 69.9% considered economically disadvantaged. Population per grade was 9th−3,156; 10th−2,802; 11th−2,666; 12th−2,624.
Results
Participants
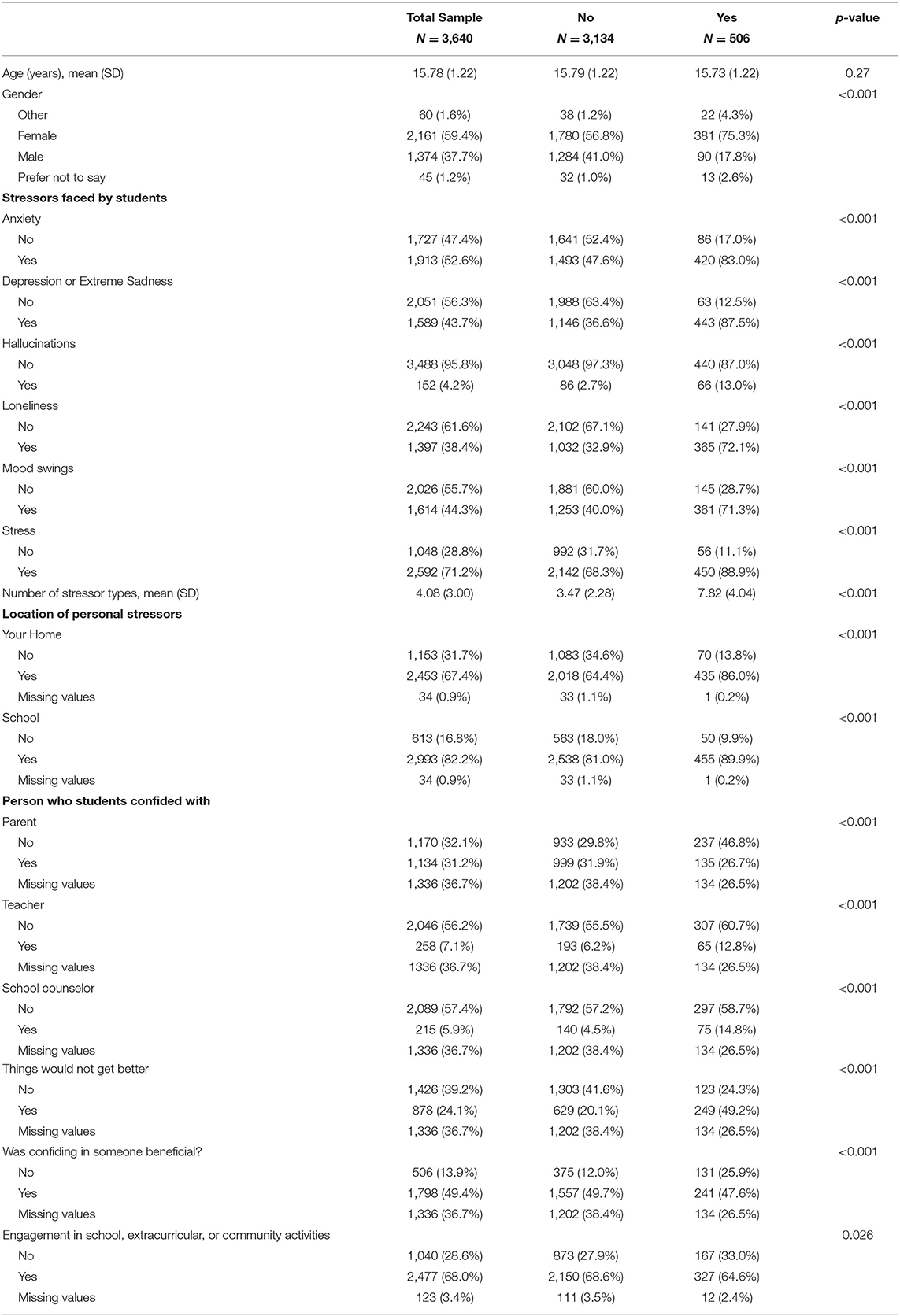
Respondents to the Teen Mental Wellness Survey included 5,070 Louisiana public high school students in Bossier, Caddo, and Red River parishes, with 98.4 percent of respondents residing in Caddo Parish. The average age for respondents was 15.79 years. Female students were more prevalent in this sample (54.3%) followed by males (43.5%), “Other gender” (1.3%), and “Prefer Not to Say” (1%) (Table 1).
Self-Harm by Gender
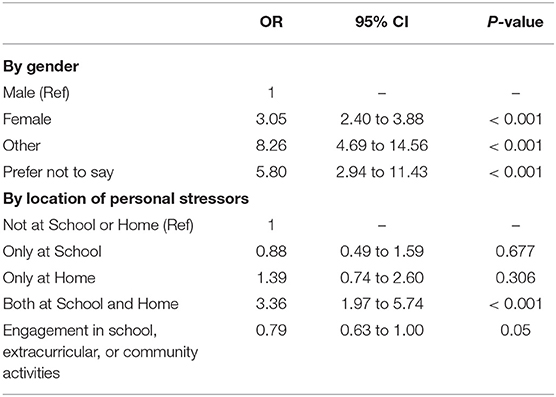
Some genders were more likely to endorse SHT as a stressor. Female (OR = 3.05; 95% CI = 2.40–3.88), Other Gender (OR 8.26; CI 4.69 to 14.56), and Prefer Not to Say Gender (OR = 5.80; 95% CI = 2.94–11.43) students had a substantially increased risk of endorsing SH as a stressor (Table 2).
Stressors Faced by Students With SHT
Students who endorsed SHT as a stressor also were at much greater risk for other stressors, including Stress (OR = 3.72; 95% CI = 2.79–4.96), Mood Swings (OR = 3.74; 95% CI = 3.04–4.59), Loneliness (OR = 5.27; 95% CI = 4.28–6.49), Hallucinations (OR = 5.32; 95% CI = 3.80 to 7.44), and Anxiety (OR = 5.37; 95% CI = 4.21–6.84). The stressor with the greatest co-occurring risk for SHT was Depression or Extreme Sadness (OR = 12.20; 95% CI = 9.28–16.04). The average number of stressors was also significantly different revealing that SH was included in an average total of 7.82 stressors as compared to 3.47 (OR = 1.58; 95% CI 1.52–1.65) total stressors for students who did not endorse SHT. Students endorsing SHT were also significantly more likely to believe that things would not get better (OR = 4.19; 95% CI = 3.31–5.31) (Figure 1).
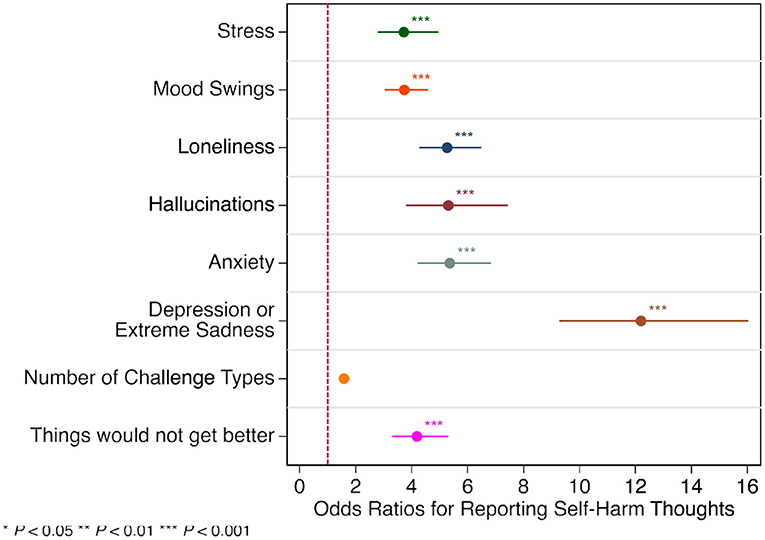
Figure 1. Odds ratios for students reporting self-harm thoughts by stressor type. *P < 0.05, **P < 0.01, ***P < 0.001.
Location of Personal Stressors
Location of personal stressors, whether home or school, did not reveal a significant difference for students with the stressor of SHT. However, when stressors occurred in both places simultaneously, the risk for SHT was substantially greater (OR = 3.36; 95% CI = 1.97–5.74) (Table 2).
Other Factors
Students with the stressor of SHT had an associated risk for loneliness. Engagement in school, extracurricular, or community activities was significantly associated with a decreased likelihood of SHT (OR = 0.79; 95% CI= 0.62 to 1; p = 0.05) (Table 2). There were also no significant differences in the groups for the perceived benefits of confiding in a teacher or school counselor; however, those who endorsed SHT were more likely consider confiding in a parent to be beneficial (OR = 1.40; 95% CI = 0.89–2.20) (Table 3).
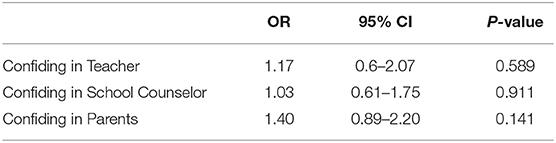
Table 3. Odds ratios for finding confiding in someone beneficial among students who reported self-harm thoughts.
Discussion
During patient care, the assessment of suicide risk is one of the most complex and challenging tasks faced by clinicians. Even the most experienced psychiatrists may long for a definitive assessment scale or additional patient information. In examining the lived experience of local high school students, this study provides a valuable additional data source. Namely, the importance of an exhaustive exploration of all stressors faced by the patient. During evaluations clinicians typically identify the most pressing stressor but it is the total stressor load that contributes to self-harm risk, particularly if stress is significant at both home and school.
The high school students who developed the TAC Survey identified stress as a major concern for teens in Northwest Louisiana. This was an astute choice. The TAC are members of Generation Z, persons born between 1997 and 2010. GenZers report a higher level of stress than other groups, and during the pandemic, GenZers have struggled the most. Fortunately, they are more likely to seek mental health services than others. As digital natives, they are at ease with online research, surveys, virtual meetings, and therapy. Many GenZers, like the TAC, are comfortable engaging leaders and leveraging data to promote change. The TAC embraced the concept that all health is local (29) and became influencers for change in our region, documenting their lived experiences and increasing awareness and access to mental health services in our schools.
While the TAC had systems change as a goal, their research yields important lessons for mental health professionals in three major ways. First, the TAC data confirms that our local experience aligns with established data indicating that depression and anxiety are associated with self-harm. Second, the importance of diving deep to identify stressors when assessing youth for suicide prevention is highlighted as ameliorating stressors is critical to minimizing the risk of self-harm. And finally, the experience of local teens with SHT provides critical information for professionals to understand risk in our area and beyond. This is critical knowledge given that SHT and suicide by peers can promote contagion. While this study represents the lived experience of urban and rural teens in the southern United States, similar stresses are widely reported for adolescents, suggesting that the results found here would generalize to other locales (29).
The TAC data shows that symptoms of depression, anxiety, mood swings, and eating disorders are associated with SHT. The TAC study found young women to be at three times the risk for SHT compared young men, in contrast to the findings of Howarth et al. (19) that males were at greater risk than females. This highlights the fact that the assessment of suicide risk is informed by research but ultimately treatment decisions must be based on the presentation and needs of the individual patient. The self-report of symptoms of mental disorders by teens highlights the need for accessible and comprehensive mental health services. In fact, the TAC requested such from local governing bodies, including Bossier Parish Public Schools and Caddo Parish Public Schools. TAC provided the school districts with a list of policy recommendations, including increased interaction with school counselors, incorporating mental health content into health education classes, and education for teachers on the signs and symptoms of mental health disorders in youth. In addition to stress due to symptoms of mental illness, the TAC survey revealed that where stressors occur, the number of stressors is a significant predictor of SHT. A 2020 systematic review and meta-analysis found suicidal ideations were increased by 45% among persons reporting life stressors (19). The TAC data shows over three times the risk for SHT when stress is high at home and school compared to stress in a single setting. This highlights the importance of exploring life circumstances at home and school when assessing youth for SHT. Youth with SHT reported a higher number of stressors than those without SHT, with ranges of 5–11 and 3–5, respectively. This serves as a lesson to mental health professionals to seek to identify as many stressors as possible in order to construct the most beneficial safety plan possible by addressing each stressor specifically and identifying where the teen feels safe. If stressors are present in both school and home, the lack of a safe respite from one or the other may result in unrelenting distress during all waking hours. Life events scales can assist in identifying stressors, but a follow-up interview is necessary to understand the meaning of the stressful event to the adolescent in order to intervene appropriately (30).
Potential Limitations
This study is limited due to the use of a non-validated, self-report survey instrument. A standardized instrument would have resulted in greater generalizability and would have allowed more robust comparison to existing data on stress in teens. The TAC Survey was created by the TAC to promote system change rather than measure variables associated with SHT. It was not designed to be a scientific research instrument. By design, the instrument did not capture race, sexual orientation, or gender identity—all critical factors for understanding SHT and preventing suicide. Finally, this study examines the lived experience of American teens in northwest Louisiana, the generalizability to broader populations, while likely, is uncertain and bears further study.
Future Directions
The TAC Survey data identified the importance of comprehensive exploration of stressors as part of the overall assessment of SHT and Safety Planning. Each stressor represents a critical intervention point for suicide prevention. This finding has important implications for safety planning and the design of safety planning forms. The Warning Signs section of most Safety Plan templates captures stressors but does not encourage listing more than a few warning signs and does not explicitly indicate that location where the stressor is experienced should be documented (31). Constructing a Safety Plan in collaboration with the patient and family is the current standard of care. This study suggests that the failure to explore all stressors contributing to distress and hopelessness represents a missed opportunity for preventing death by suicide. Future research might explore the feasibility and benefits of expanding the Warnings Signs section when completing a collaborative Safety Plan with adolescents to capture 5–7 stressors that are warning signs. In this study, students with SHT experienced an average of 7.8 stressors. While understanding the most significant stressor is important, reducing the number of stressors could be just as beneficial and remains an area for future study.
The TAC Survey found that stressors in multiple locations can increase risk for SHT, highlighting the importance of a safe harbor as part of overall suicide prevention efforts. Providing parents, teachers, coaches, and others working with teens information on how to support teens and reduce stress in order to create a safe place is critical. Student advocacy has led some states and school districts to recognize mental health days as excused absences, creating a brief space free of academic stress (32). The impact of such efforts to reduce SHT is promising but bears further study. In addition to reducing the number of stressors, a therapeutic goal should be to establish a safe haven from distress. Safety planning should include discussion of places where the teen feels safe. Cyberspace, a locus without physical boundaries, as a source of both distress and a safe haven must also be considered. The influences of social media and gaming and teens strategies for recognizing and managing these influences must be understood for a given individual as part of safety planning to manage SHT.
Finally, the use of a teen-developed survey to leverage change across an entire school district with the subsequent presentation of the data at a regional suicide prevention summit and scientific publication of the data in multiple articles illustrates the power of teens to use their lived experience to change the world. The TAC experience has provided a source of hope and inspiration for those involved as mentors as we observed the student's ingenuity and progress with awe. We would challenge other communities to empower adolescents to identify needs and capture their own experience to inform medical care and broader community solutions for complex stressors.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by LSU Heath Sciences Center—Shreveport. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
RL, JT, LA, PM, and JM contributed to the conception and design of the study. VA-Q performed the statistical analysis. PM, JT, and LA wrote sections of the article. KM, JP, and CS contributed to manuscript revision. All authors contributed to the article and approved the submitted version.
Funding
This work was completed with the support of the Department of Psychiatry and Behavioral Medicine, the Institute for Childhood Resilience, the Louisiana Addiction Research Center, and the Department of Pharmacology, Toxicology, and Neuroscience at the Louisiana State University Health Sciences Center -Shreveport. It was also supported by the Community Foundation of Northwest Louisiana and Caddo Parish Schools.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to acknowledge the 2019–20 Step Forward Teen Advisory Council for their significant contributions to improve the support for teens in local schools.
References
1. Burstein B, Agostino H. Suicidal attempts and ideation among children and adolescents in US emergency departments, 2007-2015. JAMA Pediatr. (2019) 173:598–600. doi: 10.1001/jamapediatrics.2019.0464
2. Gentil L, Huỳnh C, Grenier G. Predictors of emergency department visits for suicidal ideation and suicide attempt. Psychiatry Res. (2020) 285:112805. doi: 10.1016/j.psychres.2020.112805
3. Hill RM, Rufino K, Kurian S, Saxena J, Saxena K. Suicide ideation and attempts in a pediatric emergency department before and during COVID-19. Pediatrics. (2021) 147:e2020029280. doi: 10.1542/peds.2020-029280
4. Yard E, Radhakrishnan L, Ballesteros MF, Sheppard M, Gates A, Stein Z. Emergency department visits for suspected suicide attempts among persons aged 12–25 years before and during the COVID-19 pandemic—United States, January 2019–May 2021. MMWR Morb Mortal Wkly Rep. (2021) 70:888–94. doi: 10.15585/mmwr.mm7024e1
5. Leading Causes of Death Reports. (2009–2019). Centers for Disease Control. Available online at: https://webappa.cdc.gov/sasweb/ncipc/leadcause.html (retrieved March 28).
6. Donath C, Bergmann MC, Kliem S, Hillemacher T. Epidemiology of suicidal ideation, suicide attempts, and direct self-injurious behavior in adolescents with a migration background: a representative study. BMC Pediatr. (2019) 19:1–15. doi: 10.1186/s12887-019-1404-z
7. Donath C, Graessel E, Baier D, Bleich S. Is parenting style a predictor of suicide attempts in a representative sample of adolescents? BMC Pediatr. (2014) 14:113. doi: 10.1186/1471-2431-14-113
8. Mars B, Heron J, Klonsky ED, Moran P, O'Connor RC, Tilling K. What distinguishes adolescents with suicidal thoughts from those who have attempted suicide? A population-based birth cohort study. J Child Psychol Psychiatry. (2019) 60:91–9. doi: 10.1111/jcpp.12878
9. Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, Kessler RC. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA psychiatry. (2013) 70, 300–10. doi: 10.1001/2013.jamapsychiatry.55
10. Hatchel T, Ingram KM, Mintz S, Hartley C, Valido A, Espelage DL. Predictors of suicidal ideation and attempts among lgbtq adolescents: the roles of help-seeking beliefs, peer victimization, depressive symptoms, and drug use. J Child Fam Stud. (2019) 28:2443–55. doi: 10.1007/s10826-019-01339-2
11. Ivey-Stephenson AZ, Demissie Z, Crosby AE, Stone DM, Gaylor E, Wilkins N, et al. Suicidal ideation and behaviors among high school students—Youth Risk Behavior Survey, United States, 2019. MMWR supplements. (2020) 69:47. doi: 10.15585/mmwr.su6901a6
12. Orri M, Scardera S, Perret LC, Bolanis D, Temcheff C, Séguin JR, et al. Mental health problems and risk of suicidal ideation and attempts in adolescents. Pediatrics. (2020) 146:e20193823. doi: 10.1542/peds.2019-3823
13. Lindsey MA, Sheftall AH, Xiao Y. Trends of suicidal behaviors among high school students in the United States: 1991–2017. Pediatrics. (2019) 144:e20191187. doi: 10.1542/peds.2019-1187
14. Cecil J. Picard Center for Child Development and Lifelong Learning. Louisiana Caring Communities Youth Survey (2021). Available at: https://picardcenter.louisiana.edu/sites/picardcenter/files/2020%20Parish%20Reports_Caddo%20Parish%20Profile%20Report.pdf (accessed September 11, 2021).
15. U.S. Surgeon General. (2021). The Surgical General Call U. S. to Action to Implement the National Strategy for Suicide Prevention. Office of the Surgeon General. https://www.hhs.gov/sites/default/files/sprc-call-to-action.pdf
16. Isometsä E. Suicidal behaviour in mood disorders—who, when, and why? Can J Psychiatry. (2014) 59:120–30. doi: 10.1177/070674371405900303
17. Bilsen J. Suicide and youth: risk factors. Front Psychiatry. (2018) 9:540. doi: 10.3389/fpsyt.2018.00540
18. Holt MK, Vivolo-Kantor AM, Polanin JR, Holland KM, DeGue S, Matjasko JL, et al. Bullying and suicidal ideation and behaviors: a meta-analysis. Pediatrics. (2015) 135:e496–509. doi: 10.1542/peds.2014-1864
19. Howarth EJ, O'Connor DB, Panagioti M, Hodkinson A, Wilding S. Are stressful life events prospectively associated with increased suicidal ideation and behaviour? A systematic review and meta-analysis. J Affect Disord. (2020) 266:731–42. doi: 10.1016/j.jad.2020.01.171
20. Miller AB, Esposito-Smythers C, Weismoore JT. The relation between child maltreatment and adolescent suicidal behavior: a systematic review and critical examination of the literature. Clin Child Fam Psychol Rev. (2013) 16:146–72. doi: 10.1007/s10567-013-0131-5
21. Calati R, Ferrari C, Brittner M, Oasi O, Olié E, Carvalho AF. Suicidal thoughts and behaviors and social isolation: A narrative review of the literature. J Affect Disord. (2019) 245:653–67. doi: 10.1016/j.jad.2018.11.022
22. Miranda R, Ortin A, Scott M. Characteristics of suicidal ideation that predict the transition to future suicide attempts in adolescents. J Child Psychol Psychiatry. (2014) 55:1288–96. doi: 10.1111/jcpp.12245
23. Orsolini L, Latini R, Pompili M, Serafini G, Volpe U, Vellante F. Understanding the complex of suicide in depression: from research to clinics. Psychiatry Investig. (2020) 17:207–21. doi: 10.30773/pi.2019.0171
24. Smith AR, Velkoff EA, Ribeiro JD. Are eating disorders and related symptoms risk factors for suicidal thoughts and behaviors? A meta-analysis. Suicide Life Threat Behav. (2019) 49:221–39. doi: 10.1111/sltb.12427
25. Tseng F-Y. Internet Use and Web Communication Networks, Sources of Social Support, and Forms of Suicidal and Nonsuicidal Self-Injury Among Adolescents: Different Patterns Between Genders. Suicide Life Threat Behav. (2015) 45, 178–191. doi: 10.1111/sltb.12124
26. Horwitz AG, Grupp-Phelan J, Brent D, Barney BJ, Casper TC, Berona J, et al. Risk and protective factors for suicide among sexual minority youth seeking emergency medical services. J Affect Disord. (2021) 279:274–81. doi: 10.1016/j.jad.2020.10.015
27. Janiri D, Doucet GE, Pompili M, Sani G, Luna B, Brent DA. Risk and protective factors for childhood suicidality: a US population-based study. Lancet Psychiatry. (2020)7:317–26. doi: 10.1016/S2215-0366(20)30049-3
28. Marraccini ME. School connectedness and suicidal thoughts and behaviors: A systematic meta-analysis. School Psychol Q. (2017) 32:5. doi: 10.1037/spq0000192
29. Kohl HW, Satinsky III, Whitfield SBGP, Evenson KR. All health is local: state and local planning for physical activity promotion. J Public Health Manage Pract. (2013) 19:S17–22. doi: 10.1097/PHH.0b013e3182848081
30. Coddington RD. The significance of life events as etiologic factors in the diseases of children: II. A study of a normal population. J Psychosom Res. (1972) 16:205–13. doi: 10.1016/0022-3999(72)90045-1
31. Stanley B, Brown GK. Safety planning intervention: a brief intervention to mitigate suicide risk. Cogn Behav Pract. (2012) 19:256–64. doi: 10.1016/j.cbpra.2011.01.001
Keywords: self-harming thoughts, suicide, lived experience, stress, Gen Z, Caddo Parish
Citation: McPherson P, Alderman LL, Temple J, Lawrence R, Avila-Quintero VJ, Magner J, Sagrera CE, Patterson JC and Murnane KS (2022) Teen Advisory Council Survey's Factors Associated With Self-Harming Thoughts. Front. Psychiatry 13:851477. doi: 10.3389/fpsyt.2022.851477
Received: 09 January 2022; Accepted: 19 April 2022;
Published: 23 June 2022.
Edited by:
Alberto Forte, Sapienza University of Rome, ItalyReviewed by:
Gianluca Serafini, San Martino Hospital (IRCCS), ItalyMartina Brandizzi, ASL Roma, Italy
Copyright © 2022 McPherson, Alderman, Temple, Lawrence, Avila-Quintero, Magner, Sagrera, Patterson and Murnane. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Laura Lane Alderman, bGF1cmEuYWxkZXJtYW5AbHN1aHMuZWR1
 Pamela McPherson
Pamela McPherson Laura Lane Alderman
Laura Lane Alderman Jazzlynn Temple3
Jazzlynn Temple3 Robert Lawrence
Robert Lawrence Victor J. Avila-Quintero
Victor J. Avila-Quintero