- 1Department of Psychology, School of Public Health, Guangxi Medical University, Nanning, China
- 2Department of Guangxi Zhuang Autonomous Region Center for Disease Control and Prevention, Nanning, China
- 3Department of Graduate Management, Guangxi Medical University Cancer Hospital, Nanning, China
- 4Department of Psychology, School of Medicine, Guangxi Medical College, Nanning, China
Background: Adolescents who have experienced childhood trauma are more likely to have insomnia and psychotic-like experiences (PLEs) than adolescents from other ethnic groups. However, little is known about the youth of ethnic minorities. This study aimed to investigate the epidemiology of childhood trauma and its relationship with insomnia and PLEs in Chinese Zhuang adolescents, focusing on the role of a specific type of trauma and accumulation.
Methods: A questionnaire of Childhood Trauma Questionnaire-Short Form (CTQ-SF), Athens Insomnia Scale (AIS), and Chinese Version Community assessment psychic experiences-8 (CCAPE- 8) were all completed by 1,493 Chinese Zhuang adolescents. Chi-square and multivariate logistic regression analyses examined the association between childhood trauma and insomnia/PLEs.
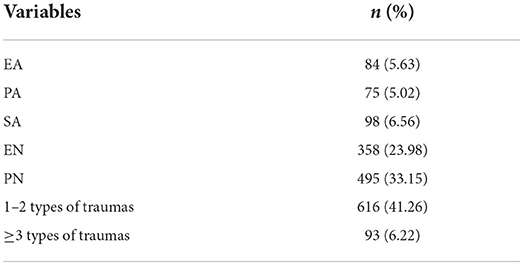
Results: The incidences of emotional abuse (EA), physical abuse (PA), sexual abuse (SA), emotional neglect (EN), and physical neglect (PN) occurred at rates of 5.63, 5.02, 6.56, 23.98, and 33.15%, respectively. EA, SA, EN, and PN were all positively related to insomnia (OR: 1.314–7.720, all p < 0.05). EA and SA were positively associated with PLEs (OR: 2.131–3.202, all p < 0.001). Adolescents who had experienced three or more types of traumas were more likely to have insomnia (OR = 6.961, p < 0.001) and PLEs (OR = 3.558, p < 0.001).
Conclusion: The most common type of childhood trauma is PN. Childhood trauma has the primary effect on insomnia/PLE. A significant dose-response relationship was found between Childhood trauma and insomnia/ PLEs. This association varied depending on the type and accumulation of exposure.
Introduction
Childhood trauma refers to various types of neglect and abuse that a person may experience as a child (1), including emotional abuse (EA), physical abuse (PA), sexual abuse (SA), emotional neglect (EN), and physical neglect (PN) (2). According to the World Health Organization (WHO) (3), more than one-third of the population has experienced childhood trauma, with a much higher prevalence among ethnic minority children (4). Further studies suggest that childhood trauma has a significant negative impact on a child's physical and psychological health throughout adolescence and even the entire life course (5) and may be responsible for mental disorders (3). It is worth noting that a single type of trauma can be misleading (6), as clients experience only this type of trauma in their lifetime, which may be a rare condition. However, the classification of trauma is an essential tool for a good assessment, as different types of trauma produce different symptoms. Researchers found a dose-response relationship (7, 8), between physical and mental conditions, with those exposed to a higher number of traumas having a greater risk of physical and mental illness. Thus, in this article, we explored not only the contribution of individual trauma types to determine whether specific trauma types were driving the association between trauma and health outcomes but also the cumulative effect of childhood trauma on health outcomes to evaluate the dose-response relationship.
According to a recent WHO report, 23, 36, and 16 % worldwide have experienced PA, EA, or PN (9). Previous research on childhood trauma has mostly focused on adults, with only a few studies focusing on adolescents. Adolescence is a critical period of behavioral, cognitive, mental, and physical development and a period of potential vulnerability (10). Furthermore, one of the especially neglected aspects of trauma assessment is ethnicity (6). Significant disparities in childhood neglect and abuse have been observed due to racial and ethnic differences (11, 12). Zhuang, is the largest one of Chinese minorities, with the majority growing up in a remote village far from the school grounds. Besides, they may face incorrect parenting styles due to their unique culture, spoken language, and lower parental education (13, 14). As a result, they have much higher rates of physical, mental (15, 16) and neglect than those in Han areas (17). However, few existing studies focused on ethnic minority adolescents, and it remains unclear if the prevalence of childhood trauma is higher or different due to ethnic minorities. The current study aims to fill this gap.
Insomnia is common in adolescents; it is one of the top health concerns for parents (18) and global public health concerns (19). Researchers found that insomnia is associated with increased mental and physical health consequences in adolescents, including depression (20), anxiety (21), obesity (22), alcohol abuse (23), and suicidal behavior (24). The causes of insomnia are complex (25). Current evidence indicates that adolescents who have experienced childhood trauma are more likely to experience insomnia (26), with a clear dose-response relationship throughout the life cycle (27). Although these studies suggest a link between childhood trauma and insomnia, there is a lack of research on the potential associations between each specific type of trauma and insomnia in adolescents.
Psychotic-like experiences (PLEs) resemble the positive symptoms of psychosis and are relatively common in adolescents (28). While PLEs have been considered as the mildest manifestation of psychosis tendencies, evidence exists that they are also associated with a wide range of mental health problems (29). For example, PLEs, including unusual beliefs, perceptual abnormalities, and persecutory ideation during childhood, are positively associated with psychotic disorders, depression, and anxiety in adulthood (30). A number of studies have found that childhood trauma is associated with an increased risk of psychotic disorders (31). As suggested by previous research, specific types of traumas, such as witnessing violence (32) or emotional abuse (33), may be strongly associated with PLEs.
Currently, the co-occurrence of insomnia and PLEs has been strongly supported in a large number of articles, including community and clinical populations (34, 35). Furthermore, insomnia is a common prodrome feature of psychosis or PLEs (36). On the other hand, specific sleep structures associated with insomnia, may be hallmarks of PLEs, such as reduced slow-wave sleep (37). Moreover, neurotransmitter changes in psychotic symptoms may also induce insomnia through excessive dopamine activity (38). Although the relationship between insomnia and PLEs has been explained no matter epidemiological investigation or physiological mechanism research, some environmental risk factors, such as childhood trauma, still need to be identified simultaneously. Further, evaluating such symptoms in adolescents is essential as adolescence is a particularly crucial period for both insomnia and PLEs (29).
In summary, we designed this study to investigate: (1) the prevalence of specific types of childhood trauma in Zhuang adolescents; and (2) the relationship between multi-types of trauma and insomnia and PLEs. We also hypothesized a dose-response relationship between childhood trauma with insomnia and PLEs.
Methods
Participants
A cross-sectional study was conducted in September 2019 at three schools (two junior highs and a senior high school) in Guangxi, China. We selected freshman students to reduce the recall bias of traumatic childhood events. The inclusion criteria were the age of 12 to 18 years and must be of Zhuang nationality. Exclusion criteria were a history of psychological disease, and the use of psychoactive drugs. Finally, 1,493 questionnaires were included after excluding those who refused to participate in the study or failed to submit their completed questionnaires. Among them, 712 (47.7%) were boys, while 781 (52.3%) were girls. The average age of participants was 14.9 ± 1.5 years old. The studies involving human participants were reviewed and approved by the Institutional Ethical Committee of Guangxi Medical University (approval number: 20160302-13). The participants and their parents or legal guardians provided written informed consent to participate in this study.
Measurements
Childhood trauma questionnaire-short form
The CTQ-SF created by Bernstein is a 28-item retrospective self-reporting screening measure for a history of neglect and abuse in childhood, with five categories for children 12 years and older (39). The five subscales included were emotional abuse (EA), physical abuse (PA), sexual abuse (SA), emotional neglect (EN), and physical neglect (PN). Each subscale contains five items rated on a 5-point Likert scale (1 = “never true” to 5 = “very often true”). To estimate the incidence of each type of childhood trauma, we used the cut-off values EA ≥ 13, PA ≥ 10, SA ≥ 8, EN ≥ 15, or PN ≥ 10, suggested by Bernstein (40). These cut-off scores showed a good validity in Zhuang people (41, 42) and Chinese adolescents (43, 44). The current sample for the CTQ-SF was calculated using Cronbach's alpha with a value of α = 0.816. In this article, the summing of trauma exposure referred to the sum of five indicators of childhood trauma: EA, PA, SA, EN, and PN.
Chinese version community assessment psychic experiences-8
The 42-item CAPE scale was proposed by Stefanis et al. (45) which was used to assess the positive, negative and depressive dimensions of psychotic symptoms in the past 12 months. Wang et al. (46) chose eight common items from Arseneault et al. (47) study to investigate the occurrence frequency of adolescents' PLEs, owing to a large number of positive items in the questionnaire and the lack of representativeness in the adolescent population. The simplified CAPE-8 has better reliability and validity with the Cronbach α = 0.768. Participants were asked if they had ever experienced each PLE (e.g., “Have you ever seen something that was not there that other people could not see?”; “Have you ever heard any voices that other people said did not exist?” etc.). Each frequency question is answered on the 4-point Likert scale (0 = “never” to 3 = “almost always”), and any items that reach the top of the scale are considered positive. The present sample for the CCAPE- 8 was calculated using Cronbach's alpha with a value of α = 0.715.
Athens insomnia scale
The AIS is a self-report questionnaire consisting of 8 items designed to assess participants' insomnia symptoms. Each item is scored on a 4-point Likert scale (0 = “no problem” to 3 = “very severe problem”). The total score ranges from 0 to 24, and the cut-off score for insomnia is 6 (48). According to reports, AIS has good reliability and validity in Chinese adolescent groups (49, 50). The current sample for the AIS was calculated using Cronbach's alpha with a value of α = 0.790.
Statistical analysis
Statistical analyses were performed using the SPSS Statistics, version 23 (IBM, Armonk, NY, USA). The significant level was set at p < 0.05. Before proceeding with the analysis, statistical assumptions were performed on each variable, including demographic and psychological characteristics. All assumptions were met for the chi-square and multivariate logistic regression tests.
Chi-square analyses were used to test demographic differences in different types of childhood trauma. Multivariate logistic regressions analyses examined the association between childhood trauma and insomnia/PLEs. The strength of the association was calculated by odds ratio (OR) and 95% confidence interval (CI).
Given the small sample size, a priori analysis was performed using G* Power software (version 3.1) (51) with a target power of β = 0.80 and an alpha level of 0.05 to determine a large effect size (0.15) (52). A post hoc power analysis was also performed, which indicated that statistical power (power = 0.92) was adequate.
Results
The prevalence and demographics of childhood trauma
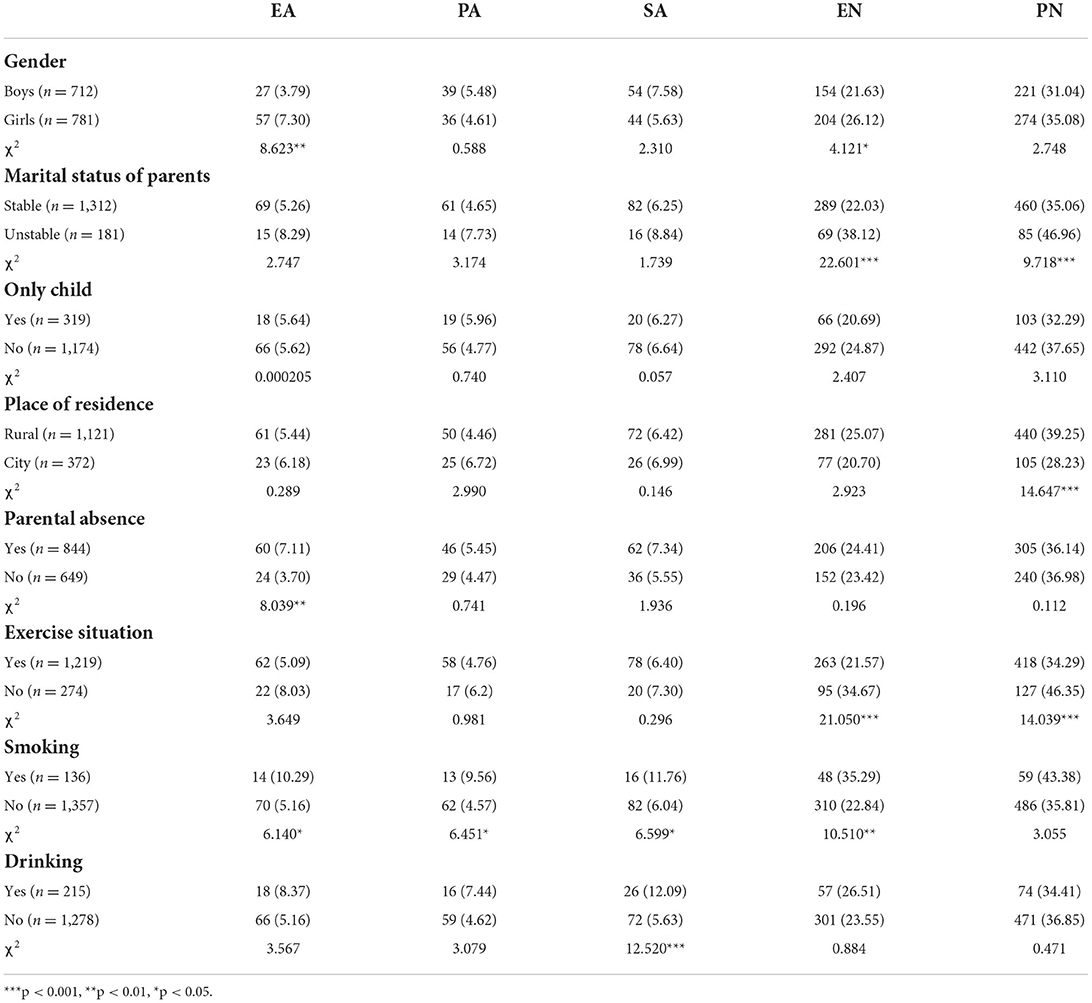
The final analyses included 1,493 participants. The incidences of EA, PA, SA, EN, PN, 1-2 types of traumas, and ≥3 types of traumas were 5.63, 5.02, 6.56, 23.98, 33.15, 41.26, and 6.22%, respectively (Table 1). The proportion of boys was slightly higher than girls (52.31 vs. 47.67%). Their age ranged from 12 to 16 years. Table 2 presents the comparison of different types of childhood trauma in demographics.
Multivariate logistic regression analysis of insomnia/ PLEs
Associations between childhood trauma and insomnia
In addition to controlling for demographic factors, such as gender, parental marital status, having an only child, place of residence, parental absences, smoking, and drinking, we also controlled for exposure to other types of trauma (for example, the relation of PA on insomnia while accounting for EN, EA, SA and PN), as the high co-occurrence of different traumas makes it difficult to tell whether these effects are attributable to the specific type of trauma. Multivariate logistic regression analysis showed that gender, smoking, EN, EA, SA, and PN were all positively related to insomnia (OR: 1.314–7.720, all p < 0.05). Those who experienced three or more types of traumas (OR = 6.961, p < 0.001) or 1–2 types of traumas (OR = 1.690, p < 0.001) had a significantly higher risk of insomnia than those who had no traumas (Tables 3, 4).
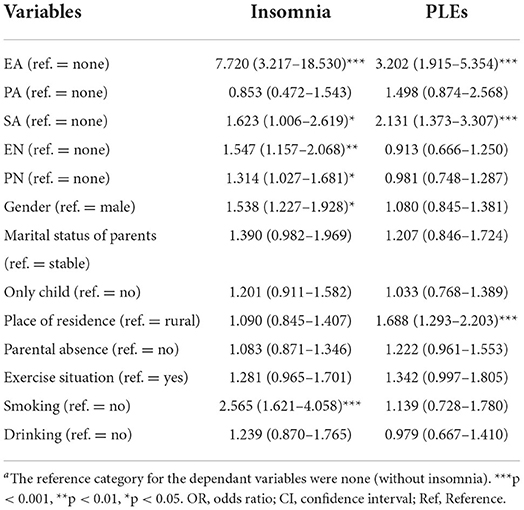
Table 3. Multivariate logistic regression of different types of childhood trauma on insomnia / PLEs [OR (95% CI)]a.
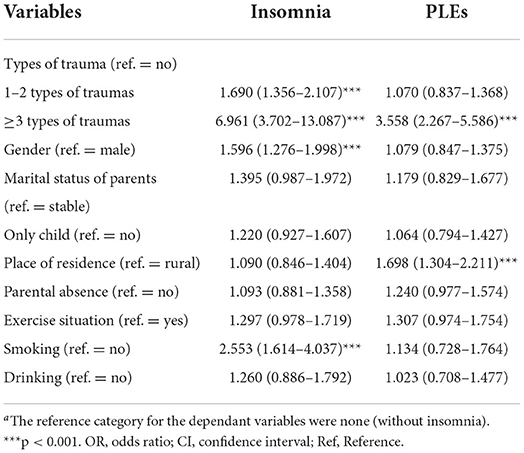
Table 4. Multivariate logistic regression of the number of types of childhood trauma on insomnia/ PLEs [OR (95% CI)]a.
Associations between childhood trauma and PLEs
In addition to controlling for demographic factors, we also controlled for exposure to other types of trauma (for example, the relation of PA to insomnia while accounting for EN, EA, SA, and PN). Multivariate logistic regression analysis revealed that place of residence, EA, and SA were all positively related with PLEs (OR: 2.131–3.202, all p < 0.001). Those who reported three or more types of traumas (OR = 3.558, p < 0.001) were significantly more likely to develop PLEs than those who did not report any traumas (Tables 3, 4).
In Summary, EA, SA, and having experienced three or more types of traumas are all predominant correlated with insomnia and PLEs.
Discussion
The prevalence and demographics of childhood trauma
There are several main findings on the prevalence of childhood trauma in the present study. Firstly, we found that the highest rate of trauma was PN, followed by EN, SA, EA, and PA. This ranking order was consistent with the previous research reported in China (31, 43) while inconsistent with western research (53). This analysis indicates that many Chinese parents still widely consider physical neglect as a legitimate means of inculcating child discipline (54). Furthermore, girls had significantly higher rates in EN and EA than boys, consistent with previous research (55, 56). In contrast, Xiao et al. (27) found that the prevalence of EN and EA (also assessed by the CTQ-SF) was higher in boys than in girls. However, there is disagreement about the gender characteristics of childhood trauma in the current study. Thus, future studies should be further divided into subgroups to understand the gender characteristic of childhood trauma (57). Thirdly, those who reported that unstable parental relations had a high incidence of EN and PN. One explanation for this finding is that emotional turmoil of a high-conflict marriage frequently overlooks concern for children when parents are constantly fighting (58), resulting in the problem that a child is so neglected by parents. Moreover, we found that adolescents living in rural areas were more vulnerable to PN than those in cities. Generally, this group's parents likely face lower socioeconomic status, schooling, and mental health education (57). According to the family stress model (FSM) (59), stressors such as socioeconomic strains cause psychological distress (e.g., depression and family dysfunction), which results in non-optimal parenting (e.g., lack of warmth and support). Furthermore, adolescents with parental absence are more likely to suffer from EA. For this group, parents tended to leave their children to go to the cities in search of better jobs because of limited local jobs (60, 61), which means children are separated from their parents, which can be emotionally damaging (62). And children who grow up without parental involvement, protection, or emotional support are more likely to experience emotional abuse (63). Those who reported smoking, drinking, and not exercising had a higher rate of various types of childhood trauma, reminding us to pay more attention to the impact of bad living habits on mental health (64).
Association between the different types of childhood trauma and insomnia/ PLEs
In the current study, we found that all four types of trauma except PA significantly increased the risk of insomnia, indicating that dimensional models are not important, particularly with childhood trauma where co-exposure is highly prevalent (65). On the other hand, this result is consistent with most recent studies, which support that childhood neglect and abuse may confer risk for insomnia (66, 67). Combined analyses of trauma, stress, sleep neurobiology, and psychophysiology offer possible insights (68). Some evidence suggests that exposure to trauma triggers a strong stress/fear response that causes hyperarousal in specific brain regions (e.g., amygdala, prefrontal cortex, reticular activating system) (69). As a result, during sensitive developmental periods, overactivation of the hypothalamic-pituitary-adrenal (HPA) axis persists, preventing it from maintaining normal sleep patterns during stressful times and increasing the risk of insomnia (70). Adolescents who had experienced emotional abuse were nearly eight times more likely to report insomnia than those who had not experienced emotional abuse. This suggests that specific types of trauma were driving the association between trauma and health outcomes (8). We can also speculate that EA is a chronic stressor that perpetuates a pattern of chronic stress in subsequent sleep throughout a child's life, possibly for a decade or more.
Besides, we found that EA and SA were risk factors for PLEs. These findings are consistent with previous research suggesting that childhood trauma (33), particularly those characterized by abuse, can cause negative cognition about oneself and the world, resulting in psychological and/or physical vulnerability and positive psychotic symptoms such as psychotic experiences (71). Neurodevelopmental changes related to the HPA axis may be the underlying mechanism of psychotic symptoms in children who have experienced childhood trauma (72).
Emotional abuse, the most harmful form of childhood trauma, was also the strongest predictor of PLEs (3), which may lead to a decreased cortisol response in the HPA axis and thus induce childhood psychotic symptoms (73). Another explanation was that self-esteem and fearful attachment were mediators between emotional abuse and PLEs (74, 75). Notably, no single mechanism explains the observed relationship between childhood trauma and insomnia. More likely, these mechanisms interact with one another, involving biological and social pathways (76). Furthermore, the emergence of an SA-PLEs co-occurrence class was not unexpected. In this context, several studies have corroborated the association that PLE may be associated with SA in some people. Biological, attachment, dissociative, and cognitive perspectives have been used to explain the relationship between SA and PLEs (77).
Association between the number of types of childhood trauma and insomnia/ PLEs
Our results indicated that the greater childhood trauma, the higher is his/her risk for insomnia during puberty, with the aOR increasing from 1.690 to 6.961 as the number of cumulative childhood trauma increased from one or two to three or more, respectively. This finding is similar to previous studies, which also found that the risk of insomnia in adolescence increases with additional exposure to a traumatic event (78). Simultaneously, this result confirms the cumulative perspective of trauma, indicating that any preventive measures aimed at detecting and reducing it should target a broad range of childhood trauma rather than a single type (79).
Experiencing one or two traumas did not increase the risk of PLEs, indicating that most people can self-regulate the mental state related to low levels of traumas (80). Furthermore, suffering three or more types of traumas increases the risk of PLEs, which parallels previous research that showed a clear dose-response association between childhood trauma and psychotic experiences (81). However, the single-factor analysis showed that only EA and SA are associated with PLEs. We can speculate the difference between “1-2 types of traumas” and “≥3 types of traumas” just caused by EA or SA, which is an interesting founding. Although it is unclear why there is such interesting results at this stage, it can emphasize the importance of considering separately the different forms of trauma to PLEs (82). Meanwhile, it is necessary to further discuss the dose-response relationship. The mechanism of this association could involve multiple emotions of childhood trauma, the cognitive models of psychosis and biological models of stress (82), including improved emotional response and poor emotion regulation abilities (83), and deficits in cognitive control (84), as well as dysregulation of dopaminergic and glutamatergic systems (85).
We also found EA, SA and suffering three or more types of traumas are all predominant correlated with insomnia and PLEs. According to previous research, the relationship between these variables and insomnia / PLEs may mediated by lack of resilience or negative emotions, such as anxiety, worry and depression (70, 86, 87). Consequently, this suggested that insomnia / PLEs could be prevented if exposure to traumas were removed or interventions were developed to mitigate the risk pathways linking childhood trauma to insomnia / PLEs.
Generalize in summary, the type and number of childhood trauma increase the risk of insomnia and PLEs. Different childhood trauma has different impacts on insomnia and PLEs, showing a dose-response association. This could imply that childhood trauma was distal risk factor that harmed adolescents' physical and mental development. PN has the highest rate of trauma, indicating that physical neglect should be prioritized during the vulnerable age period. Childhood traumas affect insomnia and PLE in adolescents negatively and thus should be considered when screening for adolescents' mental health.
Limitation
This study has several limitations. Above all, these findings are based on a cross-sectional survey, which cannot reveal its causal association with insomnia/PLEs. Since the assessments of childhood trauma, insomnia, and PLEs were based on the self-reported, participants may also have recall bias, with insomnia not corroborated by actigraphy, polysomnography, or medical records. Such reports may lead to over-/under- reporting. Besides, the dichotomous approach (i.e., exposed versus unexposed) we used to estimate childhood trauma may obscure the impact of its intensity or chronicity. Furthermore, determining the precise timeline of childhood trauma, collecting more information on sociodemographic characteristics and structural environment will make our studies more interesting and aid reproducibility and transparency in describing the sample composition. Finally, our research has not yet revealed enough the ethnic differences due to lack of ethnic comparisons.
Conclusion
For Chinese Zhuang adolescents, PN is the most common type of childhood trauma. Childhood traumas of various types have different effects on insomnia and PLE. As the number of childhood trauma increases, the risk ratio for insomnia and PLE also increases. Consequently, in order to reduce the burden of insomnia and mental disorders, Chinese parents should be educated about childhood neglect and abuse, and educators and mental health professionals should provide targeted interventions for adolescents who have experienced childhood trauma.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Ethical Committee of Guangxi Medical University (approval number: 20160302-13). The participants and their parents or legal guardians provided written informed consent to participate in this study.
Author contributions
QW, YP, and SZ designed the study and supervised the data collection. WY, QL, SP, CD, and LZ undertook data collection. QW conducted the statistical analyses and drafted the manuscript. JW participated in coaching as a leader. All authors contributed to and have approved the final manuscript.
Funding
This work was funded by the National Nature Science Foundation of China (No. 81660569). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. McCoy ML, Keen SM. Child Abuse and Neglect. Psychology Press (2013). (2013). doi: 10.4324/9780203120699
2. Stoltenborgh M, Bakermans-Kranenburg MJ, Alink LR, van IJzendoorn MH. The prevalence of child maltreatment across the globe: Review of a series of meta-analyses. Child Abuse Rev. (2015) 24:37–50. 24:37–50. doi: 10.1002/car.2353
3. Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, et al. Childhood adversities and adult psychopathology in the WHO world mental health surveys. Br J Psychiatry. (2010) 197:378–85. doi: 10.1192/bjp.bp.110.080499
4. Dakil SR, Cox M, Lin H, Flores G. Racial and ethnic disparities in physical abuse reporting and child protective services interventions in the United States. J Natl Med Assoc. (2011) 103:926–31. 103:926–31. doi: 10.1016/S0027-9684(15)30449-1
5. Brennenstuhl S, Fuller-Thomson E. The painful legacy of childhood violence: migraine headaches among adult survivors of adverse childhood experiences. Headache J Head Face Pain. (2015) 55:973–83. doi: 10.1111/head.12614
6. Kira IA, Fawzi MH, Fawzi MM. The dynamics of cumulative trauma and trauma types in adults patients with psychiatric disorders: Two cross-cultural studies. Traumatology. (2013) 19:179–95. 19:179–95. doi: 10.1177/1534765612459892
7. Kira IA, Lewandowski L, Templin T, Ramaswamy V, Ozkan B, Mohanesh J. Measuring cumulative trauma dose, types, and profiles using a development-based taxonomy of traumas. Traumatology. (2008) 14:62–87. doi: 10.1177/1534765608319324
8. Hashemi L, Fanslow J, Gulliver P, McIntosh T. Exploring the health burden of cumulative and specific adverse childhood experiences in New Zealand: results from a population-based study. Child Abuse Negl. (2021) 122:105372. doi: 10.1016/j.chiabu.2021.105372
10. Kaplan SJ, Pelcovitz D, Salzinger S, Weiner M, Mandel FS, Lesser ML, et al. Adolescent physical abuse: Risk for adolescent psychiatric disorders. Am J Psychiatry. (1998) 155:954–9. 155:954–9. doi: 10.1176/ajp.155.7.954
11. Grey A. A polity study of minority language management in China focusing on Zhuang. Curr Issues Lang Plan. (2019) 20:443–502. doi: 10.1080/14664208.2018.1502513
12. Li L, Chen X, Wu D, Li H. Effects of attending preschool on adolescents' reading literacy: evidence from the ethnic minority children in China. Child Youth Serv Rev. (2020) 116:105211. 116:105211. doi: 10.1016/j.childyouth.2020.105211
13. Ma Y, Goto A, Yasumura S, Wu Q, Xu J. Mental health and its relationship to life events and family socio-economic status among Chinese medical students in Guangxi Zhuang autonomous region. Stress Health. (2009) 25:71–9. doi: 10.1002/smi.1220
14. Li L, Liu Y, Peng Z, Liao M, Lu L, Liao H, et al. Peer relationships, motivation, self-efficacy, and science literacy in ethnic minority adolescents in China: a moderated mediation model. Child Youth Serv Rev. (2020) 119:105524. doi: 10.1016/j.childyouth.2020.105524
15. Yan-ling L, Hong C, Hong-bing XU, Ping L, Jing-ling X. Mental health traits of children of Zhuang nationality in Guangxi. Chin J Clin Psychol. (2005) 13:183–6. (In Chinese).
16. Wei L. Mental health status of primary and middle-school students in the Zhuang nationality region. China J Health Psychol. (2013) 21:1549–52. (In Chinese).
17. Wan G, Wang M, Chen S. Child abuse in ethnic regions: evidence from 2899 girls in Southwest China. Child Youth Serv Rev. (2019) 105:104457. 105:104457. doi: 10.1016/j.childyouth.2019.104457
18. Donskoy I, Loghmanee D. Insomnia in adolescence. Med Sci. (2018) 6:72. 6:72. doi: 10.3390/medsci6030072
19. Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep Med. (2011) 12:110–8. doi: 10.1016/j.sleep.2010.11.008
20. Roberts RE, Duong HT. Depression and insomnia among adolescents: a prospective perspective. J Affect Disord. (2013) 148:66–71. doi: 10.1016/j.jad.2012.11.049
21. Blake MJ, Trinder JA, Allen NB. Mechanisms underlying the association between insomnia, anxiety, and depression in adolescence: implications for behavioral sleep interventions. Clin Psychol Rev. (2018) 63:25–40. doi: 10.1016/j.cpr.2018.05.006
22. Duraccio KM, Simmons DM, Beebe DW, Byars KC. Relationship of overweight and obesity to insomnia severity, sleep quality, and insomnia improvement in a clinically referred pediatric sample. J Clin Sleep Med. (2022) 18:1083–91. doi: 10.5664/jcsm.9806
23. Miller MB, Janssen T, Jackson KM. The prospective association between sleep and initiation of substance use in young adolescents. J Adolesc Health. (2017) 60:154–60. 60:154–60. doi: 10.1016/j.jadohealth.2016.08.019
24. Liu B-P, Wang X-T, Liu Z-Z, Wang Z-Y, Liu X, Jia C-X. Stressful life events, insomnia and suicidality in a large sample of Chinese adolescents. J Affect Disord. (2019) 249:404–9. 249:404–9. doi: 10.1016/j.jad.2019.02.047
25. Taylor D, Gehrman P, Dautovich ND, Lichstein KL, McCrae CS. Causes of Insomnia. Handbook of Insomnia. Springer (2014). p. 11–27. doi: 10.1007/978-1-907673-73-3_2
26. Geng F, Zou J, Liang Y, Zhan N, Li S, Wang J. Associations of positive and adverse childhood experiences and adulthood insomnia in a community sample of Chinese adults. Sleep Med. (2021) 80:46–51. doi: 10.1016/j.sleep.2021.01.022
27. Xiao D, Wang T, Huang Y, Wang W, Zhao M, Zhang W-H, et al. Gender differences in the associations between types of childhood maltreatment and sleep disturbance among Chinese adolescents. J Affect Disord. (2020) 265:595–602. doi: 10.1016/j.jad.2019.11.099
28. Kelleher I, Connor D, Clarke MC, Devlin N, Harley M, Cannon M. Prevalence of psychotic symptoms in childhood and adolescence: a systematic review and meta-analysis of population-based studies. Psychol Med. (2012) 42:1857–63. doi: 10.1017/S0033291711002960
29. Kalman JL, Bresnahan M, Schulze TG, Susser E. Predictors of persisting psychotic like experiences in children and adolescents: a scoping review. Schizophr Res. (2019) 209:32–9. 209:32–9. doi: 10.1016/j.schres.2019.05.012
30. Fisher HL, Schreier A, Zammit S, Maughan B, Munafó MR, Lewis G, et al. Pathways between childhood victimization and psychosis-like symptoms in the ALSPAC birth cohort. Schizophrenia Bull. (2013) 39:1045–55. doi: 10.1093/schbul/sbs088
31. Lu D, Wang W, Qiu X, Qing Z, Lin X, Liu F, et al. The prevalence of confirmed childhood trauma and its' impact on psychotic-like experiences in a sample of chinese adolescents. Psychiatry Res. (2020) 287:112897. doi: 10.1016/j.psychres.2020.112897
32. Mojtabai R. Psychotic-like experiences and interpersonal violence in the general population. Soc Psychiatry Psychiatr Epidemiol. (2006) 41:183–90. 41:183–90. doi: 10.1007/s00127-005-0020-4
33. Alemany S, Arias B, Aguilera M, Villa H, Moya J, Ibanez MI, et al. Childhood abuse, the BDNF-Val66Met polymorphism and adult psychotic-like experiences. Br J Psychiatry. (2011) 199:38–42. 199:38–42. doi: 10.1192/bjp.bp.110.083808
34. Barton J, Kyle SD, Varese F, Jones SH, Haddock G. Are sleep disturbances causally linked to the presence and severity of psychotic-like, dissociative and hypomanic experiences in non-clinical populations? a systematic review. Neurosci Biobehav Rev. (2018) 89:119–31. 89:119–31. doi: 10.1016/j.neubiorev.2018.02.008
35. Reeve S, Sheaves B, Freeman D. The role of sleep dysfunction in the occurrence of delusions and hallucinations: a systematic review. Clin Psychol Rev. (2015) 42:96–115. 42:96–115. doi: 10.1016/j.cpr.2015.09.001
36. Lee YJ, Cho S-J, Cho IH, Jang JH, Kim SJ. The relationship between psychotic-like experiences and sleep disturbances in adolescents. Sleep Med. (2012) 13:1021–7. 13:1021–7. doi: 10.1016/j.sleep.2012.06.002
37. Göder R, Bares S, Vogel C, Böttcher H, Drews HJ, Lechinger J, et al. Psychotic-like experiences in patients with insomnia or sleep apnea: associations with sleep parameters. Sleep Med. (2021) 77:367–73. doi: 10.1016/j.sleep.2020.04.015
38. Kamath J, Virdi S, Winokur A. Sleep disturbances in schizophrenia. Psychiatric clinics. (2015) 38:777–92. doi: 10.1016/j.psc.2015.07.007
39. Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse Negl. (2003) 27:169–90. doi: 10.1016/S0145-2134(02)00541-0
40. Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the childhood trauma questionnaire in an adolescent psychiatric population. J Am Acad Child Adolesc Psychiatry. (1997) 36:340–8. 36:340–8. doi: 10.1097/00004583-199703000-00012
41. Yuli P, Xuan Z, Xiujin L, Miuyu Y, Shengjie Z, Fenglan C, et al. Relationship of the risk of adulthood depression with serum CRP, IP-10, TGF-β1 and childhood trauma: a case-control study. Chin Gen Pract. (2021) 24:1349. (In Chinese).
42. Zhou Y-h. Childhood trauma and subjective well-being in postgraduates: the mediating of coping style. Chin J Clin Psychol. (2016) 24:509–13. (In Chinese).
43. Tong J, Zhang T, Chen F, Wang Q, Zhao X, Hu M. Prevalence and contributing factors of childhood trauma, anxiety, and depression among adolescents from two-child families in china. Front Psychiatry. (2022) 13:782087. doi: 10.3389/fpsyt.2022.782087
44. Wang J, He X, Chen Y, Lin C. Association between childhood trauma and depression: a moderated mediation analysis among normative Chinese college students. J Affect Disord. (2020) 276:519–24. 276:519–24. doi: 10.1016/j.jad.2020.07.051
45. Stefanis N, Hanssen M, Smirnis N, Avramopoulos D, Evdokimidis I, Stefanis C, et al. Evidence that three dimensions of psychosis have a distribution in the general population. Psychol Med. (2002) 32:347–58. doi: 10.1017/S0033291701005141
46. Dong-fang W, Wen Z, Si-si W, Meng S, Chang P, Wei-dan P, et al. Psychotic-like experiences and associated socio-demographic factors among adolescents:comparison between urban and rural areas. Chin J Clin Psychol. (2019) 27:302–5+55. (In Chinese).
47. Arseneault L, Cannon M, Fisher HL, Polanczyk G, Moffitt TE, Caspi A. Childhood trauma and children's emerging psychotic symptoms: a genetically sensitive longitudinal cohort study. Am J Psychiatry. (2011) 168:65–72. doi: 10.1176/appi.ajp.2010.10040567
48. Sun J-L, Chiou J-F, Lin C-C. Validation of the Taiwanese version of the athens insomnia scale and assessment of insomnia in Taiwanese cancer patients. J Pain Symptom Manage. (2011) 41:904–14. 41:904–14. doi: 10.1016/j.jpainsymman.2010.07.021
49. Chung K-F, Kan KK-K, Yeung W-F. Assessing insomnia in adolescents: comparison of insomnia severity index, athens insomnia scale and sleep quality index. Sleep Med. (2011) 12:463–70. 12:463–70. doi: 10.1016/j.sleep.2010.09.019
50. Wei Q, Zhang S, Pan Y, Hu H, Chen F, Yin W, et al. Epidemiology of gaming disorder and its effect on anxiety and insomnia in Chinese ethnic minority adolescents. BMC Psychiatry. (2022) 22:1–9. 22:1–9. doi: 10.1186/s12888-022-03894-3
51. Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analysis. Behav Res Methods. (2009) 41:1149–60. doi: 10.3758/BRM.41.4.1149
52. Cohen J. A power primer. Psychol Bull. (1992) 112:155–9. 112:155–9. doi: 10.1037/0033-2909.112.1.155
53. Forde DR, Baron SW, Scher CD, Stein MB. Factor structure and reliability of the childhood trauma questionnaire and prevalence estimates of trauma for male and female street youth. J Interpers Violence. (2012) 27:364–79. doi: 10.1177/0886260511416461
54. Chan Y-c, Lam GL, Shae W-C. Children's views on child abuse and neglect: Findings from an exploratory study with Chinese children in Hong Kong. Child Abuse Neglect. (2011) 35:162–72. 35:162–72. doi: 10.1016/j.chiabu.2010.12.001
55. Moody G, Cannings-John R, Hood K, Kemp A, Robling M. Establishing the international prevalence of self-reported child maltreatment: a systematic review by maltreatment type and gender. BMC Public Health. (2018) 18:1–15. doi: 10.1186/s12889-018-6044-y
56. Witt A, Brown RC, Plener PL, Brähler E, Fegert JM. Child maltreatment in Germany: prevalence rates in the general population. Child Adolesc Psychiatry Ment Health. (2017) 11:1–9. 11:1–9. doi: 10.1186/s13034-017-0185-0
57. Liu J, Lin X, Shen Y, Zhou Y, He Y, Meng T, et al. Epidemiology of childhood trauma and analysis of influencing factors in psychiatric disorders among Chinese adolescents: a cross-sectional study. J Interpers Violence. (2021) 1–19. doi: 10.1177/08862605211039244
58. Joyce AN. High-conflict divorce: a form of child neglect. Fam Court Rev. (2016) 54:642–56. 54:642–56. doi: 10.1111/fcre.12249
59. Emmen RA, Malda M, Mesman J, van IJzendoorn MH, Prevoo MJ, Yeniad N. Socioeconomic status and parenting in ethnic minority families: testing a minority family stress model. J Fam Psychol. (2013) 27:896. doi: 10.1037/a0034693
60. Jia Z, Tian W. Loneliness of left-behind children: a cross-sectional survey in a sample of rural China. Child Care Health Dev. (2010) 36:812–7. 36:812–7. doi: 10.1111/j.1365-2214.2010.01110.x
61. Asis MM. Living with migration: experiences of left-behind children in the Philippines. Asian Popul Stud. (2006) 2:45–67. doi: 10.1080/17441730600700556
62. Kruk E. Parental alienation as a form of emotional child abuse: current state of knowledge and future directions for research. Fam Sci Rev. (2018) 22:141–64. 22:141–64. doi: 10.26536/EVMS9266
63. Zhao J, Liu X, Wang M. Parent–child cohesion, friend companionship and left-behind children's emotional adaptation in rural China. Child Abuse Negl. (2015) 48:190–9. 48:190–9. doi: 10.1016/j.chiabu.2015.07.005
64. Blanner Kristiansen C, Juel A, Vinther Hansen M, Hansen A, Kilian R, Hjorth P. Promoting physical health in severe mental illness: patient and staff perspective. Acta Psychiatr Scand. (2015) 132:470–8. doi: 10.1111/acps.12520
65. McLaughlin KA, Sheridan MA, Humphreys KL, Belsky J, Ellis BJ. The value of dimensional models of early experience: thinking clearly about concepts and categories. Perspect Psychol Sci. (2021) 16:1463–72. doi: 10.1177/1745691621992346
66. Gelaye B, Kajeepeta S, Zhong Q-Y, Borba CP, Rondon MB, Sánchez SE, et al. Childhood abuse is associated with stress-related sleep disturbance and poor sleep quality in pregnancy. Sleep Med. (2015) 16:1274–80. doi: 10.1016/j.sleep.2015.07.004
67. Becker SP, Gregory AM. Editorial perspective: perils and promise for child and adolescent sleep and associated psychopathology during the COVID-19 pandemic. J Child Psychol Psychiatry. (2020) 61:757–9. 61:757–9. doi: 10.1111/jcpp.13278
68. Sinha SS. Trauma-induced insomnia: a novel model for trauma and sleep research. Sleep Med Rev. (2016) 25:74–83. doi: 10.1016/j.smrv.2015.01.008
69. Williams LM, Kemp AH, Felmingham K, Barton M, Olivieri G, Peduto A, et al. Trauma modulates amygdala and medial prefrontal responses to consciously attended fear. Neuroimage. (2006) 29:347–57. 29:347–57. doi: 10.1016/j.neuroimage.2005.03.047
70. Reffi AN, Kalmbach DA, Cheng P, Jovanovic T, Norrholm SD, Sexton MB, et al. Sleep reactivity as a potential pathway from childhood abuse to adult insomnia. Sleep Med. (2022) 94:70–5. 94:70–5. doi: 10.1016/j.sleep.2022.03.026
71. Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington P. A cognitive model of the positive symptoms of psychosis. Psychol Med. (2001) 31:189–95. 31:189–95. doi: 10.1017/S0033291701003312
72. Cotter D, Pariante CM. Stress and the progression of the developmental hypothesis of schizophrenia. Br J Psychiatry. (2002) 181:363–5. doi: 10.1192/bjp.181.5.363
73. Carpenter LL, Tyrka AR, Ross NS, Khoury L, Anderson GM, Price LH. Effect of childhood emotional abuse and age on cortisol responsivity in adulthood. Biol Psychiatry. (2009) 66:69–75. 66:69–75. doi: 10.1016/j.biopsych.2009.02.030
74. Sheinbaum T, Kwapil TR, Barrantes-Vidal N. Fearful attachment mediates the association of childhood trauma with schizotypy and psychotic-like experiences. Psychiatry Res. (2014) 220:691–3. 220:691–3. doi: 10.1016/j.psychres.2014.07.030
75. Finzi-Dottan R, Karu T. From emotional abuse in childhood to psychopathology in adulthood: a path mediated by immature defense mechanisms and self-esteem. J Nerv Ment Dis. (2006) 194:616–21. 194:616–21. doi: 10.1097/01.nmd.0000230654.49933.23
76. Hall Brown TS, Akeeb A, Mellman TA. The role of trauma type in the risk for insomnia. J Clin Sleep Med. (2015) 11:735–9. doi: 10.5664/jcsm.4846
77. Murphy J, Shevlin M, Houston JE, Adamson G. Modelling the co-occurrence of psychosis-like experiences and childhood sexual abuse. Soc Psychiatry Psychiatr Epidemiol. (2014) 49:1037–44. 49:1037–44. doi: 10.1007/s00127-014-0845-9
78. Wang Y, Raffeld MR, Slopen N, Hale L, Dunn EC. Childhood adversity and insomnia in adolescence. Sleep Med. (2016) 21:12–8. doi: 10.1016/j.sleep.2016.01.011
79. Steine IM, Winje D, Krystal JH, Bjorvatn B, Milde AM, Grønli J, et al. Cumulative childhood maltreatment and its dose-response relation with adult symptomatology: findings in a sample of adult survivors of sexual abuse. Child Abuse Negl. (2017) 65:99–111. 65:99–111. doi: 10.1016/j.chiabu.2017.01.008
80. He Y, Zhang Y, Cui X, Zhong Y, He W, Liu J, et al. Epidemiology of major childhood adversities and its effect on depression and suicide attempts in Chinese college students. J Affect Disord. (2021) 281:331–7. doi: 10.1016/j.jad.2020.12.031
81. Janssen I, Krabbendam L, Bak M, Hanssen M, Vollebergh W, de Graaf R, et al. Childhood abuse as a risk factor for psychotic experiences. Acta Psychiatr Scand. (2004) 109:38–45. 109:38–45. doi: 10.1046/j.0001-690X.2003.00217.x
82. McGrath JJ, McLaughlin K, Saha S, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, et al. The association between childhood adversities and subsequent first onset of psychotic experiences: a cross-national analysis of 23 998 respondents from 17 countries. Psychol Med. (2017) 47:1230–45. 47:1230–45. doi: 10.1017/S0033291716003263
83. McLaughlin KA, Conron KJ, Koenen KC, Gilman SE. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychol Med. (2010) 40:1647–58. 40:1647–58. doi: 10.1017/S0033291709992121
84. Bentall RP, Corcoran R, Howard R, Blackwood N, Kinderman P. Persecutory delusions: a review and theoretical integration. Clin Psychol Rev. (2001) 21:1143–92. 21:1143–92. doi: 10.1016/S0272-7358(01)00106-4
85. Grace AA. Dysregulation of the dopamine system in the pathophysiology of schizophrenia and depression. Nat Rev Neurosci. (2016) 17:524–32. doi: 10.1038/nrn.2016.57
86. Alameda L, Conus P, Ramain J, Solida A, Golay P. Evidence of mediation of severity of anxiety and depressive symptoms between abuse and positive symptoms of psychosis. J Psychiatr Res. (2022) 150:353–9. doi: 10.1016/j.jpsychires.2021.11.027
Keywords: childhood trauma, insomnia, psychotic-like experiences, epidemiology, association, adolescents, ethnic minorities
Citation: Wei Q, Pan Y, Zhang S, Yin W, Lin Q, Pan S, Dai C, Zhou L and Wu J (2022) Epidemiology of childhood trauma and its association with insomnia and psychotic-like experiences in Chinese Zhuang adolescents. Front. Psychiatry 13:974674. doi: 10.3389/fpsyt.2022.974674
Received: 21 June 2022; Accepted: 03 August 2022;
Published: 22 August 2022.
Edited by:
Yuan Yuan Wang, De Montfort University, United KingdomReviewed by:
Teresa Vargas, Northwestern University, United StatesFeiwen Wang, Second Xiangya Hospital, Central South University, China
Copyright © 2022 Wei, Pan, Zhang, Yin, Lin, Pan, Dai, Zhou and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Junduan Wu, d3VqdW5kdWFuQGd4bXUuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
 Qiaoyue Wei
Qiaoyue Wei Yuli Pan2†
Yuli Pan2† Junduan Wu
Junduan Wu