- 1Section of Child and Adolescent Neuropsychiatry, Department of Public Health and Pediatric Sciences, University of Turin, Turin, Italy
- 2Service of Child and Adolescent Psychiatry, Department of Psychiatry, Lausanne University Hospital and the University of Lausanne, Lausanne, Switzerland
- 3Psychiatric Liaison Service, Department of Psychiatry, Lausanne University Hospital, Lausanne, Switzerland
- 4Center for Psychiatric Neuroscience, Department of Psychiatry, Lausanne University Hospital and the University of Lausanne, Lausanne, Switzerland
High rates of co-occurring depression are commonly reported in youth with Autism Spectrum Disorder (ASD), especially in individuals without intellectual disability (ID). Depression in ASD undermines adaptive behavior and is associated with a higher risk of suicidality. Females with ASD may be particularly vulnerable due to their greater use of camouflaging strategies. Indeed, in comparison to males, ASD is underdiagnosed in females, despite higher rates of internalizing symptoms and suicidality. Trauma exposure may also play a role in the development of depressive symptoms in this population. Moreover, evidence for effective treatments of depression in autistic youth are lacking, with ASD individuals frequently experiencing low efficacy and side effects. We present the case of an adolescent female with previously undiagnosed ASD without ID, admitted for active suicidal plans and a treatment-resistant depression (TRD), occurred after a COVID-19 lockdown in the context of cumulative exposure to stressful life events. Comprehensive clinical assessments performed at intake confirmed severe depression with suicidality. Intensive psychotherapy and different changes in medications were carried out (SSRI, SNRI, SNRI + NaSSA, SNRI + aripiprazole), all of which were ineffective, with persistent suicidal thoughts, often requiring intensive individual monitoring. The patient was finally successfully treated with lithium augmentation of fluoxetine, with no side effects. During hospitalization she was also evaluated by an ASD specialized center, where a diagnosis of ASD was made according to the Autism Diagnostic Observation Schedule (ADOS) and the Autism Diagnostic Interview-Revised (ADI-R) scores, as well as to clinical judgment of a senior psychiatrist. The present case report shows that clinicians should not overlook undiagnosed autism as a possible cause of TRD, especially in females without ID, where higher rates of under diagnosis may be in part related to their greater use of camouflage. It also suggests that ASD underdiagnosis and resulting unmet needs may be involved in vulnerability to stressful experiences, depression, and suicidality. Furthermore, it shows the complexity of providing care to TRD in youth with autism, suggesting that an augmentation therapy with lithium, a commonly recommended therapeutic strategy for refractory depression in typically developing samples, may also be effective in this population.
Introduction
Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder characterized by deficits in social communication and interaction, and by restricted, repetitive patterns of behaviors and /or interests (1). High rates of co-occurring depression are commonly reported in youth with ASD (2, 3), with a lifetime prevalence rate estimated at 20.2% (4). ASD individuals are up to 4 times more likely to develop depressive symptoms than neurotypical subjects, with an increasing trend from adolescence to middle adulthood (5). Depression in ASD undermines adaptive behavior and is associated with a higher risk of suicidality and an increased healthcare burden (3).
A recent body of literature on adolescent and adult samples suggests that females with ASD may experience higher rates of depression and other internalizing symptoms compared to males, including anxiety, suicidality and eating disorders (5–7), although others studies found no sex differences (8, 9). Females with ASD also show higher rates of completed suicide than their male counterpart, in contrast to what is reported in non-ASD samples (i.e., completed suicide more frequent in males) (10). Moreover, evidence suggests that ASD is potentially underdiagnosed in females (11), who are also later diagnosed than their male counterpart and frequently misdiagnosed with other mental disorders, especially personality disorders (12–15). In line with this, some authors suggest that there's a female autism phenotype, including female specific manifestations of autism less likely to be captured by current diagnostic tools (16, 17). Also, females seem to mask more their autistic traits than males, a phenomenon known as camouflage (18), which has been associated to higher rates of distress, depression and suicidality in both adolescents and adults with ASD (19–21). Conversely, an earlier ASD diagnosis has shown a protective effect on depression and self-harm behaviors (22, 23), potentially enabling timely interventions and social support, and reducing the risk of traumatic experiences (24), that have been linked to mood symptoms and suicidality in ASD (25, 26).
Since current evidence is heavily based on male samples, providing information on the female autism phenotype could reduce mis- and missed-diagnosis rates and prevent secondary comorbidities in this population.
Moreover, evidence for efficacious pharmacological interventions is lacking and therapeutic strategies used for neurotypical patients may not be effective in ASD population (27, 28). Some authors suggest considering ASD in case of treatment-resistant depression (TRD) (29), which is defined by the presence of persistent depressive symptoms despite at least two trials of antidepressants at an appropriate dosage and duration. Lithium augmentation is a first-line treatment strategy for TRD in neurotypical samples (30). Moreover, lithium has demonstrated an anti-suicidal effect (31). Despite its potential use, to date, no randomized controlled trials have studied lithium's use in ASD, however, evidence from previous studies suggested a potential efficacy in this population. A preclinical study by Wu et al. (32) found an improvement in anxiety and depressive symptoms in rats with isolation-induced autistic behaviors. Previous chart reviews of youth and adults with ASD suggested a potential efficacy on mood dysregulation and maladaptive behaviors (33, 34). A previous case report showed a completed remission of catatonia and regression in two people with ASD with SHANK3 mutation treated with lithium (35). Epperson et al. (36) reported significant improvements in social relatedness and aggressivity with lithium augmentation of fluvoxamine in a man with ASD. Another case report documented a marked reduction in self-injury and aggressive behavior with lithium augmentation in a depressed adolescent male with intellectual disability (ID) (37). However, to our knowledge, this is the first case report of lithium augmentation efficacy in TRD with suicidality in an adolescent female with ASD, without ID. She was admitted multiple times for chronic suicidal plans and a TRD occurring after COVID-19 lockdown and exposure to traumatic events. Despite different changes in antidepressant treatments, all were ineffective. Eventually, she was diagnosed with ASD during her 4th hospital stay and successfully treated with lithium augmentation, without side effects.
Case description
Patient information
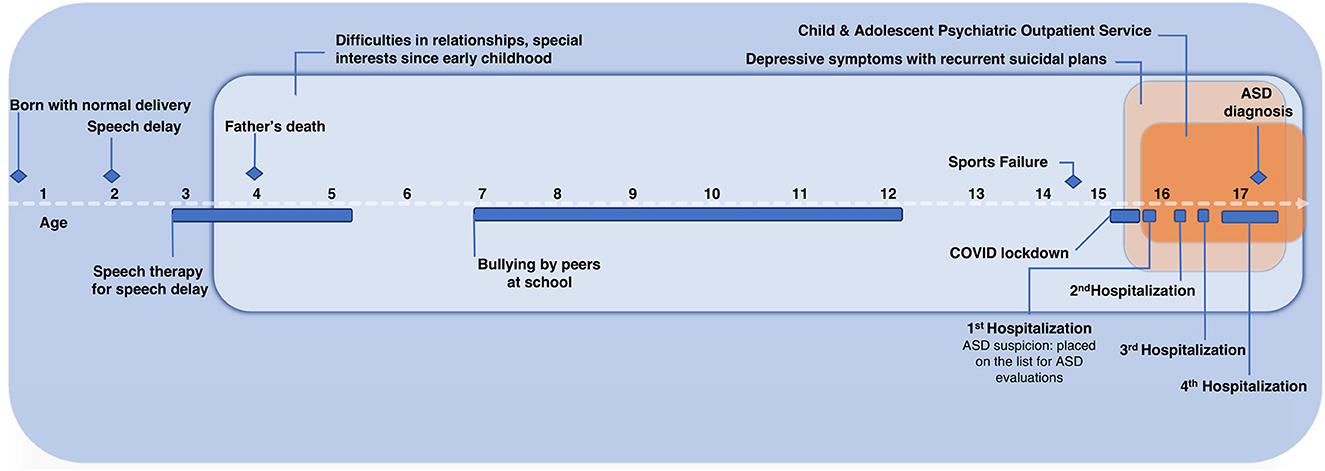
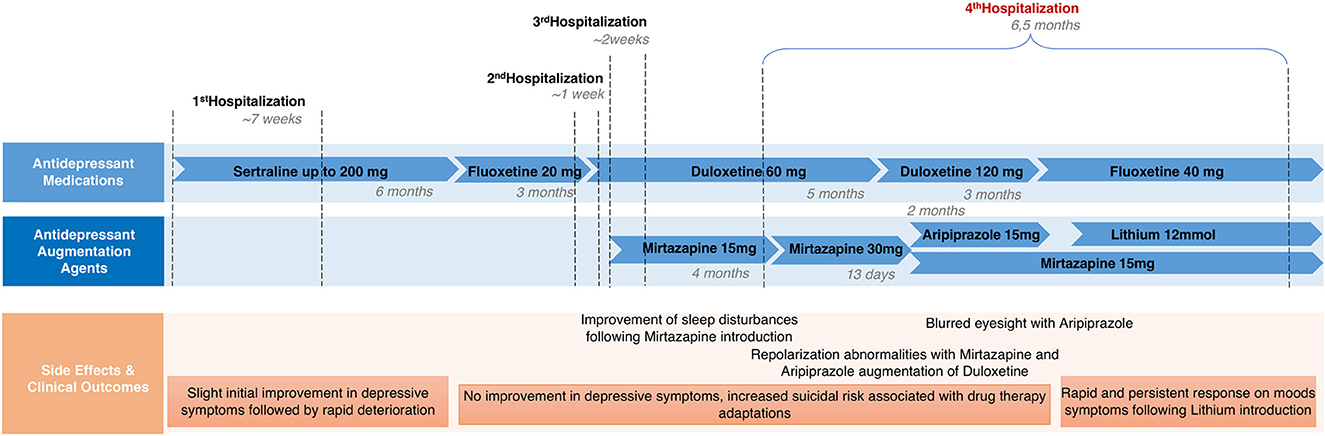
A. is a 16-year-old girl who was admitted four times in our adolescent psychiatric inpatient unit for depressive symptoms and active suicidal plans. The early development was normal, except for a mild language delay (i.e., she did not speak single words until 2.5 years and had poor speech until 4 years), that benefited from speech therapy. Since early childhood she showed difficulties in interacting with peers, isolation, peculiar interests (i.e., drawing letters and numbers), and was described by teachers as “being in her world,” which was interpreted as a reaction to the sudden death of her father when she was 5 years old. Moreover, she presented poor cognitive flexibility and a marked sense of justice, especially concerning school rules. Her peers frequently bullied her due to this. Also, the school context required her great effort due to her noise sensitivity. During adolescence, she reported a sense of being inadequate in social situations, so that she had to constantly monitor and adjust her reactions to fit into peer contexts. All her activities were organized with a rigid timetable, with a large amount of time dedicated to study and sport training, achieving brilliant sport and school results. Interactions with peers were mostly around these specific interests. Depressive symptoms started during the COVID-19 pandemic lockdown and the interruption of her high-performance sport training due to a sports failure. She presented low mood, fatigue, anhedonia, increased social withdrawal and ruminations about her father's death and the sports failure. She was first referred to an outpatient psychiatric unit, where she was treated with psychotherapy. Despite an initial mild improvement, she was later hospitalized four times for recurrent suicidal plans and diagnosed with major depressive disorder (MDD) according to DSM-5 criteria. During the first three admissions, several changes in medications were carried out: she was first treated with sertraline, up to 200 mg daily, that was then switched to fluoxetine, up to 20 mg daily, that was finally switched to duloxetine, up to 60 mg daily. She was also treated with mirtazapine up to 15 mg daily for her sleep disturbances, with a positive effect. The antidepressant treatments showed only a partial and temporary improvement, with a rapid recrudescence of suicidal plans after each hospitalization. A suspicion of ASD was also hypothesized during her first hospitalization, and the patient was put on a waiting list for outpatient specialized evaluations.
Family history
There was no family history of psychiatric disorders, except a suspicion of autism in her small brother, who had never been investigated.
Clinical findings
At the present hospitalization (i.e., the 4th one), a clinical interview was conducted at intake by a senior psychiatrist, confirming the diagnosis of MDD with active suicidal plans. She was also evaluated by the Prodromal Questionnaire-16 (38), with a score of 6 (cut-off 7) and by the Health of the Nation Outcome Scales for Children and Adolescents, self-rated version (HoNOSCA-SR) (39), suggesting severe depressive symptoms with suicidality (HoNOSCA-SR: “Have you done anything to injure or harm your-self on purpose”- 4/5; “Have you been feeling in a low or anxious mood, or troubled by fears, obsessions or rituals”- 5/5). During interviews, she reported depressed mood, guilt, anhedonia, apathy, sleep and appetite disturbances. She struggled to express emotions and her affect was blunted with limited eye contact, neutral facial expressions, and monotone speech. The intelligence quotient was not evaluated due to symptoms severity, however, she demonstrated good cognitive and linguistic competence, as evidenced by her school results and sophisticated vocabulary.
Therapeutic intervention, follow-up, and outcomes
The current hospitalization was complicated by recurrent non-suicidal self-injuries (NSSI) (e.g., self-cutting) and suicidal threats, including an interrupted suicide attempt, requiring intensive individual monitoring during high-risk periods. A. also developed severe food restriction, initially describing it as her only way to die. She subsequently lost significant weight, reaching a body mass index of 16, and ultimately met all diagnostic criteria for anorexia nervosa (DSM-5), necessitating a nasogastric feeding tube.
Concerning pharmacological treatment, duloxetine was initially raised up to 120 mg daily, with no clinical response. Thus, an augmentation treatment, first with mirtazapine (up to 30 mg daily), and then with aripiprazole (up to 15 mg daily), was tried in combination with duloxetine, showing no clinical improvements. Duloxetine was then switched to fluoxetine, augmented up to 40 mg daily (since it had only been previously tried at a low dose), showing no clinical improvements. Lithium was finally added to fluoxetine as an augmentation treatment. Blood tests were conducted periodically to monitor thyroid, parathyroid, and renal function, as well as lithium plasma concentration, to determine the optimal dose and detect possible side effects. The therapeutic dose was 12 mmol daily (corresponding to a lithium plasma level of 0.5 mmol/L), split into two administrations, resulting in a rapid and satisfactory improvement in mood and suicidality, without side effects. A. also showed a parallel improvement in food intake restriction that allowed the removal of the nasogastric tube. During hospitalization, she was evaluated by an ASD specialized center (Centre Cantonal de l'Autisme) and diagnosed with ASD based on ADOS-2 and ADI-R scores (40, 41) (Table 1), as well as the clinical judgment of a senior psychiatrist. A brief psychoeducational intervention followed to help her elaborate the diagnosis. A. also had several ergotherapy sessions focused on recognizing and managing emotions. At hospital discharge, we observed a clinical improvement that was confirmed by the HoNOSCA-SR (with a score of 3/5 as regards to mood and anxiety symptoms, and a score of 3/5 as regards to suicidal thoughts). The patient was addressed to an outpatient clinic for psychological and psychiatric follow-up, as well as to a social skills training group for ASD. Clinically relevant data and medication history are shown in Figures 1, 2.
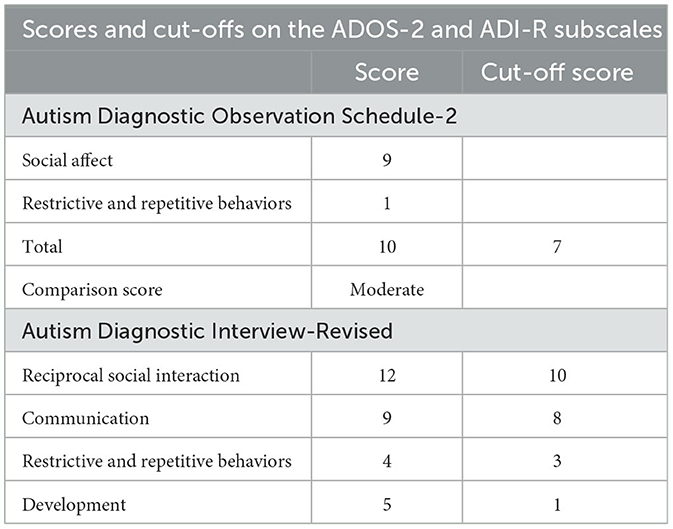
Table 1. Scores on the Autism Diagnostic Observation Schedule-2 (ADOS-2) and Autism Diagnostic Interview-Revised (ADI-R), with cut-off values.
Discussion
We present the case of a TRD with NSSI, suicidal behaviors and anorexia nervosa in a 16-year-old-girl with comorbid previously undiagnosed ASD, without ID. The strength of our case report is that it highlights the clinical challenges of females with ASD, describing the factors possibly involved in both autism misdiagnosis and in the development of TRD with suicidality. To our knowledge, this is the first case report specifically exploring lithium augmentation's efficacy for TRD with suicidality in an adolescent female with ASD, without ID, suggesting a potential effectiveness. The limitation of our case report is that the evaluations for ASD were performed during hospitalization (albeit together with the improvement of depressive symptoms), therefore, the possible influence of depression on the scores may not be completely excluded. However, ASD suspicions preceded the current patient's hospitalization and the patient's history was thoroughly explored by clinicians with the aid of the ADI-R, a standardized tool providing a developmental perspective.
Our case is in line with the evidence suggesting a greater incidence of depressive symptoms, suicidality and eating disorders in ASD population, especially in females without ID (5, 42). Also, A. showed many typical characteristics of the female autism presentation, including a late ASD diagnosis, being initially referred for depression and using camouflage to fit in with peers (12, 16, 17). Additionally, she displayed “socially acceptable” repetitive interests (e.g., sport and school performance), consistent with studies indicating that females with ASD exhibit less bizarre interests and externalizing behaviors than their male counterpart, contributing to fewer mental health concerns and missed diagnosis (43, 44). Camouflaging strategies adopted by the patient, described as “constantly monitoring and adjusting her reactions to fit in social contexts,” may both have contributed to ASD misrecognition, and represented a risk factor for depression and suicidality, as evidence highlighted that camouflage is a risk factor for a wide range of mental health problems (16, 45). Despite being “exhausting and distressing,” qualitative studies in adolescent girls with ASD highlighted that camouflage was aimed at “fitting into” neurotypical contexts and avoiding bullying experiences (46). Traumatic experiences also seem to play a major role in the development of secondary comorbidities in ASD, including depression and suicidality (26, 47). Indeed, evidence show that individuals with ASD reported higher rates of trauma, such as bullying victimization and marginalization, compared to neurotypical peers, especially in females with ASD (48). Furthermore, typical autistic traits, including ruminative thinking, unusual sensory processing and need for predictability, may alter the appraisal of stressful events and hinder coping with changes. This may lead to a wider range of traumatic experiences and a greater impact on mental health (47, 49).
Multiple traumatic events in our patient's history, including sports failure and COVID-19 school closures, preceded the onset of depressive symptoms, and disrupted her routine, highlighting the impact of trauma and COVID-19 pandemic in depression development in ASD samples, as evidenced in previous studies and reports (26, 50–52). Also, COVID-19 lockdown may have exacerbated maladaptive coping strategies, such as ruminations on past traumatic experiences.
In sum, we hypothesize that the delayed diagnosis due to the female-typical ASD presentation, combined with exposure to multiple traumatic events, may have increased the risk of depression and suicidality in our patient. Furthermore, in line with literature findings (22), an earlier ASD diagnosis may have been a protective factor in reducing the patient's exposure to social stressors and in providing appropriate interventions and support. Indeed, evidence-based psychological treatments adapted for autism have shown efficacy for depression (53, 54).
Regarding pharmacological interventions, current evidence for effective treatments for depression in ASD is limited (27, 28). Studies exploring SSRI efficacy in reducing ASD core symptoms suggest that ASD youth may experience more adverse side effects than typically developing peers, especially behavioral activation (55, 56). In general population samples, current treatment guidelines recommend augmentation strategies after the failure of two antidepressants or a partial response with a primary antidepressant (57), with atypical antipsychotics and lithium commonly used as augmentation agents in both adults and adolescents (58, 59). Despite our patient's lack of response to various medications, including SSRI and SNRI monotherapy, as well as aripiprazole or mirtazapine augmentation, she showed improvement in depressive symptoms and suicidality with lithium augmentation. Limited evidence supports lithium's use in ASD, but previous clinical and pre-clinical studies documented its potential efficacy for mood symptoms, catatonia, social relatedness, and maladaptive behaviors in this population (32, 34, 36, 37). Our case also suggests lithium as a potential effective strategy for treating TRD and reducing suicide risk in youth with ASD.
Conclusions
This case report has several clinical implications. First, it provides evidence on the female-typical ASD presentation, which could help recognize ASD in females and prevent secondary comorbidities. Second, it suggests that clinicians should not overlook undiagnosed autism as a possible cause of TRD with suicidality, especially in females without ID. Third, it suggests that an augmentation therapy with lithium, an agent commonly recommended for TRD in neurotypical samples, may also be considered for refractory depression in youth with ASD. Given the high rates of depression and suicidality in ASD and limited evidence for effective interventions, further research is needed to evaluate the efficacy of lithium augmentation strategy for TRD in this population. To address this gap in knowledge, prospective controlled trials with larger samples seem necessary.
Patient perspective
The patient identified with the ASD diagnosis, describing difficulties in understanding other people's feelings or intentions since childhood, expressing relief when we discussed the increased prevalence of bullying among youth with autism. Also, she recognized the benefits of the augmentation therapy with lithium and was satisfied with the psychoeducational intervention that provided her with practical techniques to improve emotions recognition and expression.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
IS contributed to the conceptualization and writing of the manuscript. LP worked with the patient and her family and contributed to the writing. AC, LP, PK, and AN worked with the patient and her family, contributed to the conceptualization, and supervised the work. CK and MA contributed to the conceptualization and supervised the work. All authors have approved the submitted version.
Funding
Open access funding was provided by the University of Lausanne.
Acknowledgments
The authors express thanks to the patient and her family for their cooperation and the permission to publish their experience.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ASD, Autism Spectrum Disorder; MDD, major depressive disorder; TRD, treatment-resistant depression; NSSI, non-suicidal self-injuries; SSRI, selective serotonin re-uptake inhibitors; SNRI, selective noradrenaline re-uptake inhibitors; NaSSA, noradrenergic and specific serotonergic antidepressants; DSM-5, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition; ID, intellectual disability; ADOS-2, Autism Diagnostic Observation Schedule; ADI-R, Autism Diagnostic Interview-Revised; HoNOSCA-SR, Health of the Nation Outcome Scale for Children and Adolescents—Self rated.
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Washington, DC: American Psychiatric Pub (2013). doi: 10.1176/appi.books.9780890425596
2. Bougeard C, Picarel-Blanchot F, Schmid R, Campbell R, Buitelaar J. Prevalence of Autism spectrum disorder and co-morbidities in children and adolescents: a systematic literature review. Front Psychiatry. (2021) 12:744709. doi: 10.3389/fpsyt.2021.744709
3. Pezzimenti F, Han GT, Vasa RA, Gotham K. Depression in youth with autism spectrum disorder. Child Adolesc Psychiatr Clin N Am. (2019) 28:397–409. doi: 10.1016/j.chc.2019.02.009
4. Greenlee JL, Mosley AS, Shui AM, Veenstra-VanderWeele J, Gotham KO. Medical and behavioral correlates of depression history in children and adolescents with autism spectrum disorder. Pediatrics. (2016) 137(Suppl. 2):S105–14. doi: 10.1542/peds.2015-2851I
5. Uljarević M, Hedley D, Rose-Foley K, Magiati I, Cai RY, Dissanayake C, et al. Anxiety and depression from adolescence to old age in autism spectrum disorder. J Autism Dev Disord. (2020) 50:3155–65. doi: 10.1007/s10803-019-04084-z
6. Schwartzman JM, Williams ZJ, Corbett BA. Diagnostic- and sex-based differences in depression symptoms in autistic and neurotypical early adolescents. Autism. (2022) 26:256–69. doi: 10.1177/13623613211025895
7. Westwood H, Tchanturia K. Autism spectrum disorder in anorexia nervosa: an updated literature review. Curr Psychiatry Rep. (2017) 19:41. doi: 10.1007/s11920-017-0791-9
8. Gotham K, Brunwasser SM, Lord C. Depressive and anxiety symptom trajectories from school age through young adulthood in samples with autism spectrum disorder and developmental delay. J Am Acad Child Adolesc Psychiatry. (2015) 54:369–76.e3. doi: 10.1016/j.jaac.2015.02.005
9. Nasca BC, Lopata C, Donnelly JP, Rodgers JD, Thomeer ML. Sex differences in externalizing and internalizing symptoms of children with ASD. J Autism Dev Disord. (2020) 50:3245–52. doi: 10.1007/s10803-019-04132-8
10. Hirvikoski T, Mittendorfer-Rutz E, Boman M, Larsson H, Lichtenstein P, Bölte S. Premature mortality in autism spectrum disorder. Br J Psychiatry. (2016) 208:232–8. doi: 10.1192/bjp.bp.114.160192
11. Dworzynski K, Ronald A, Bolton P, Happé F. How different are girls and boys above and below the diagnostic threshold for autism spectrum disorders? J Am Acad Child Adolesc Psychiatry. (2012) 51:788–97. doi: 10.1016/j.jaac.2012.05.018
12. Gesi C, Migliarese G, Torriero S, Capellazzi M, Omboni AC, Cerveri G, et al. Gender differences in misdiagnosis and delayed diagnosis among adults with autism spectrum disorder with no language or intellectual disability. Brain Sci. (2021) 11:912. doi: 10.3390/brainsci11070912
13. Huang Y, Arnold SRC, Foley K, Lawson LP, Richdale AL, Trollor JN. Factors associated with age at autism diagnosis in a community sample of Australian adults. Autism Research. (2021) 14:2677–87. doi: 10.1002/aur.2610
14. Kirby AV, Bakian AV, Zhang Y, Bilder DA, Keeshin BR, Coon H. A 20-year study of suicide death in a statewide autism population. Autism Res. (2019) 12:658–66. doi: 10.1002/aur.2076
15. South M, Beck JS, Lundwall R, Christensen M, Cutrer EA, Gabrielsen TP, et al. unrelenting depression and suicidality in women with autistic traits. J Autism Dev Disord. (2020) 50:3606–19. doi: 10.1007/s10803-019-04324-2
16. Bargiela S, Steward R, Mandy W. The experiences of late-diagnosed women with autism spectrum conditions: an investigation of the female autism phenotype. J Autism Dev Disord. (2016) 46:3281–94. doi: 10.1007/s10803-016-2872-8
17. Hull L, Petrides KV, Mandy W. The female autism phenotype and camouflaging: a narrative review. Rev J Autism Dev Disord. (2020) 7:306–17. doi: 10.1007/s40489-020-00197-9
18. Attwood T. The Complete Guide to Asperger's Syndrome, 1st ed. London, Philadelphia: Jessica Kingsley Publishers (2006).
19. Bernardin CJ, Mason E, Lewis T, Kanne S. “You must become a chameleon to survive”: adolescent experiences of camouflaging. J Autism Dev Disord. (2021) 51:4422–35. doi: 10.1007/s10803-021-04912-1
20. Cage E, Troxell-Whitman Z. Understanding the reasons, contexts and costs of camouflaging for autistic adults. J Autism Dev Disord. (2019) 49:1899–911. doi: 10.1007/s10803-018-03878-x
21. Cassidy S, Bradley L, Shaw R, Baron-Cohen S. Risk markers for suicidality in autistic adults. Mol Autism. (2018) 9:42. doi: 10.1186/s13229-018-0226-4
22. Hosozawa M, Sacker A, Cable N. Timing of diagnosis, depression and self-harm in adolescents with autism spectrum disorder. Autism. (2021) 25:70–8. doi: 10.1177/1362361320945540
23. Jadav N, Bal VH. Associations between co-occurring conditions and age of autism diagnosis: implications for mental health training and adult autism research. Autism Res. (2022) 15:2112–25. doi: 10.1002/aur.2808
24. Zuckerman K, Lindly OJ, Chavez AE. Timeliness of autism spectrum disorder diagnosis and use of services among U.S. Element Schl Aged Child Psychiatr Serv. (2017) 68, 33–40. doi: 10.1176/appi.ps.201500549
25. Holden R, Mueller J, McGowan J, Sanyal J, Kikoler M, Simonoff E, et al. Investigating bullying as a predictor of suicidality in a clinical sample of adolescents with autism spectrum disorder. Autism Res. (2020) 13:988–97. doi: 10.1002/aur.2292
26. Taylor JL, Gotham KO. Cumulative life events, traumatic experiences, and psychiatric symptomatology in transition-aged youth with autism spectrum disorder. J Neurodev Disord. (2016) 8:28. doi: 10.1186/s11689-016-9160-y
27. Deb S, Roy M, Lee R, Majid M, Limbu B, Santambrogio J, et al. Randomised controlled trials of antidepressant and anti-anxiety medications for people with autism spectrum disorder: systematic review and meta-analysis. BJPsych Open. (2021) 7:e179. doi: 10.1192/bjo.2021.1003
28. Menezes M, Harkins C, Robinson MF, Mazurek MO. Treatment of depression in individuals with autism spectrum disorder: a systematic review. Res Autism Spectr Disord. (2020) 78:101639. doi: 10.1016/j.rasd.2020.101639
29. White MJ. Treatment-resistant depression: consider autism. Br J Gen Pract. (2019) 69:14. doi: 10.3399/bjgp19X700373
30. Bauer M, Adli M, Baethge C, Berghöfer A, Sasse J, Heinz A, et al. (2003). Lithium augmentation therapy in refractory depression: clinical evidence and neurobiological mechanisms. Can J Psychiatr. 48:440–8. doi: 10.1177/070674370304800703
31. Smith KA, Cipriani A. Lithium and suicide in mood disorders: updated meta-review of the scientific literature. Bipolar Disord. (2017) 19:575–86. doi: 10.1111/bdi.12543
32. Wu X, Bai Y, Tan T, Li H, Xia S, Chang X, et al. Lithium ameliorates autistic-like behaviors induced by neonatal isolation in rats. Front Behav Neurosci. (2014) 8:234. doi: 10.3389/fnbeh.2014.00234
33. Siegel M, Beresford CA, Bunker M, Verdi M, Vishnevetsky D, Karlsson C, et al. Preliminary investigation of lithium for mood disorder symptoms in children and adolescents with autism spectrum disorder. J Child Adolesc Psychopharmacol. (2014) 24:399–402. doi: 10.1089/cap.2014.0019
34. Mintz M, Hollenberg E. Revisiting lithium: utility for behavioral stabilization in adolescents and adults with autism spectrum disorder. Psychopharmacol Bull. (2019)49:28.
35. Serret S, Thümmler S, Dor E, Vesperini S, Santos A, Askenazy F. Lithium as a rescue therapy for regression and catatonia features in two SHANK3 patients with autism spectrum disorder: case reports. BMC Psychiatry. (2015) 15:107. doi: 10.1186/s12888-015-0490-1
36. Epperson CN, McDougle CJ, Anand A, Marek GJ, Naylor ST, Volkmar FR, et al. Lithium augmentation of fluvoxamine in autistic disorder: a case report. J Child Adolesc Psychopharmacol. (1994) 4:201–7. doi: 10.1089/cap.1994.4.201
37. Clarke D, Baxter M, Perry D, Prasher V. The diagnosis of affective and psychotic disorders in adults with autism: seven case reports. Autism. (1999) 3:149–64. doi: 10.1177/1362361399003002005
38. Ising HK, Veling W, Loewy RL, Rietveld MW, Rietdijk J, Dragt S, et al. The validity of the 16-item version of the prodromal questionnaire (PQ-16) to screen for ultra high risk of developing psychosis in the general help-seeking population. Schizophr Bull. (2012) 38:1288–96. doi: 10.1093/schbul/sbs068
39. Gowers S, Levine W, Bailey-Rogers S, Shore A, Burhouse E. Use of a routine, self-report outcome measure (HoNOSCA–SR) in two adolescent mental health services. Br J Psychiatry. (2002) 180:266–9. doi: 10.1192/bjp.180.3.266
40. Lord C, Rutter M, Goode S, Heemsbergen J, Jordan H, Mawhood L, et al. Austism diagnostic observation schedule: a standardized observation of communicative and social behavior. J Autism Dev Disord. (1989) 19:185–212. doi: 10.1007/BF02211841
41. Lord C, Rutter M, Le Couteur A. Autism diagnostic interview-revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord. (1994) 24:659–85. doi: 10.1007/BF02172145
42. Oswald TM, Winter-Messiers MA, Gibson B, Schmidt AM, Herr CM, Solomon M. Sex differences in internalizing problems during adolescence in autism spectrum disorder. J Autism Dev Disord. (2016) 46:624–36. doi: 10.1007/s10803-015-2608-1
43. Lai M-C, Szatmari P. Sex and gender impacts on the behavioural presentation and recognition of autism. Curr Opin Psychiatry. (2020) 33:117–23. doi: 10.1097/YCO.0000000000000575
44. Stephenson KG, Norris M, Butter EM. Sex-based differences in autism symptoms in a large, clinically-referred sample of preschool-aged children with ASD. J Autism Dev Disord. (2021) 53:624–32. doi: 10.1007/s10803-020-04836-2
45. Leedham A, Thompson AR, Smith R, Freeth M. ‘I was exhausted trying to figure it out': the experiences of females receiving an autism diagnosis in middle to late adulthood. Autism. (2020) 24:135–46. doi: 10.1177/1362361319853442
46. Halsall J, Clarke C, Crane L. “Camouflaging” by adolescent autistic girls who attend both mainstream and specialist resource classes: perspectives of girls, their mothers and their educators. Autism. (2021) 25:2074–86. doi: 10.1177/13623613211012819
47. Dell'Osso L, Carpita B, Cremone IM, Muti D, Diadema E, Barberi FM, et al. The mediating effect of trauma and stressor related symptoms and ruminations on the relationship between autistic traits and mood spectrum. Psychiatry Res. (2019) 279:123–9. doi: 10.1016/j.psychres.2018.10.040
48. Haruvi-Lamdan N, Horesh D, Zohar S, Kraus M, Golan O. Autism spectrum disorder and post-traumatic stress disorder: an unexplored co-occurrence of conditions. Autism. (2020) 24:884–98. doi: 10.1177/1362361320912143
49. Kerns CM, Lankenau S, Shattuck PT, Robins DL, Newschaffer CJ, Berkowitz SJ. Exploring potential sources of childhood trauma: a qualitative study with autistic adults and caregivers. Autism. (2022) 26:1987–98. doi: 10.1177/13623613211070637
50. Carmassi C, Bertelloni CA, Salarpi G, Diadema E, Avella MT, Dell'Oste V, et al. Is there a major role for undetected autism spectrum disorder with childhood trauma in a patient with a diagnosis of bipolar disorder, self-injuring, and multiple comorbidities? Case Rep Psychiatry. (2019) 2019:1–6. doi: 10.1155/2019/4703795
51. Lew-Koralewicz A. Psychosocial Functioning and the Educational Experiences of Students with ASD during the COVID-19 Pandemic in Poland. Int J Environ Res Public Health. (2022) 19:9468. doi: 10.3390/ijerph19159468
52. Oomen D, Nijhof AD, Wiersema JR. The psychological impact of the COVID-19 pandemic on adults with autism: a survey study across three countries. Mol Autism. (2021) 12:21. doi: 10.1186/s13229-021-00424-y
53. Cooper K, Loades ME, Russell A. Adapting psychological therapies for autism. Res Autism Spectr Disord. (2018) 45:43–50. doi: 10.1016/j.rasd.2017.11.002
54. Linden A, Best L, Elise F, Roberts D, Branagan A, Tay YBE, et al. Benefits and harms of interventions to improve anxiety, depression, and other mental health outcomes for autistic people: a systematic review and network meta-analysis of randomised controlled trials. Autism. (2022) 2022:136236132211179. doi: 10.1177/13623613221117931
55. Persico AM, Ricciardello A, Lamberti M, Turriziani L, Cucinotta F, Brogna C, et al. The pediatric psychopharmacology of autism spectrum disorder: a systematic review - part I: the past and the present. Progress Neuro Psychopharmacol Biol Psychiatry. (2021) 110:110326. doi: 10.1016/j.pnpbp.2021.110326
56. Williams K, Brignell A, Randall M, Silove N, Hazell P. Selective serotonin reuptake inhibitors (SSRIs) for autism spectrum disorders (ASD). Cochrane Database Syst Rev. (2013) 8. doi: 10.1002/14651858.CD004677.pub3
57. Kennedy SH, Lam RW, McIntyre RS, Tourjman SV, Bhat V, Blier P, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 3. Pharmacological Treat Can J Psychiatry. (2016) 61:540–60. doi: 10.1177/0706743716659417
58. Grunze H, Vieta E, Goodwin GM, Bowden C, Licht RW, Azorin J-M, et al. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders: acute and long-term treatment of mixed states in bipolar disorder. World J Biol Psychiatry. (2018) 19:2–58. doi: 10.1080/15622975.2017.1384850
Keywords: Autism Spectrum Disorder, depression, adolescent, case report, female, lithium, COVID-19, suicidality
Citation: Secci I, Petigas L, Cuenod A, Klauser P, Kapp C, Novatti A and Armando M (2023) Case report: Treatment-resistant depression, multiple trauma exposure and suicidality in an adolescent female with previously undiagnosed Autism Spectrum Disorder. Front. Psychiatry 14:1151293. doi: 10.3389/fpsyt.2023.1151293
Received: 25 January 2023; Accepted: 03 April 2023;
Published: 26 April 2023.
Edited by:
Fengyu Zhang, Global Clinical and Translational Research Institute, United StatesReviewed by:
Ramalingam Senthil, SRM Institute of Science and Technology, IndiaCamilla Gesi, ASST Fatebenefratelli Sacco, Italy
Copyright © 2023 Secci, Petigas, Cuenod, Klauser, Kapp, Novatti and Armando. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ilaria Secci, aWxhcmlhLnNlY2NpQHVuaXRvLml0
 Ilaria Secci
Ilaria Secci Lucie Petigas
Lucie Petigas Alexandra Cuenod2,3
Alexandra Cuenod2,3 Carole Kapp
Carole Kapp Audrey Novatti
Audrey Novatti Marco Armando
Marco Armando