- 1Department of Psychiatry, University of Melbourne, Melbourne, VIC, Australia
- 2North West Area Mental Health, Division of Mental Health, Northern Health, Melbourne, VIC, Australia
- 3Social Work and Social Policy, Department of Community and Clinical Health, La Trobe University, Bundoora, VIC, Australia
- 4Neami National, Preston, VIC, Australia
- 5Centre for Mental Health, Melbourne School of Population and Global Health, University of Melbourne, Melbourne, VIC, Australia
- 6Centre for Mental Health Nursing, Department of Nursing, The University of Melbourne, Melbourne, VIC, Australia
- 7Department of Epidemiology and Applied Clinical Research, Division of Psychiatry, University College London, London, United Kingdom
- 8Camden and Islington NHS Foundation Trust, London, United Kingdom
- 9The Bouverie Centre, School of Psychology and Public Health, La Trobe University, Brunswick, VIC, Australia
Objective: This study aims to assess the effectiveness of community-based models of care (MoCs) supporting the recovery of individuals who experience persistent and complex mental health needs.
Method: We conducted a systematic review and narrative synthesis of MoC studies reporting clinical, functional, or personal recovery from October 2016 to October 2021. Sources were Medline, EMBASE, PsycInfo, CINAHL, and Cochrane databases. Studies were grouped according to MoC features. The narrative synthesis was led by our researchers with lived experience.
Results: Beneficial MoCs ranged from well-established to novel and updated models and those explicitly addressing recovery goals and incorporating peer support: goal-focused; integrated community treatment; intensive case management; partners in recovery care coordination; rehabilitation and recovery-focused; social and community connection-focused; supported accommodation; and vocational support. None of our diverse group of MoCs supporting recovery warranted a rating of best practice. Established MoCs, such as intensive case management, are promising practices regarding clinical and functional recovery, with potential for enhancements to support personal recovery. Emerging practice models that support personal and functional recovery are those where consumer goals and priorities are central.
Conclusion: Evidence for established models of care shows that there is a need for inevitable evolution and adaptation. Considering the high importance of effective MoCs for people experiencing persistent and complex mental health needs, further attention to service innovation and research is required. Greater emphasis on the inclusion of lived and living experience in the design, delivery, implementation, and research of MoCs is needed, to enhance MOCs' relevance for achieving individual consumer recovery outcomes.
Background
Many people living with severe or persistent mental health conditions experience psychosocial disability and have complex support needs. Although common, the use of diagnosis alone as a proxy for disability is contested (1). Longitudinal evidence suggests that ~25% of people newly diagnosed with a severe mental illness such as schizophrenia, schizoaffective disorder, or bipolar affective disorder develop particularly complex problems and psychosocial disability that may require rehabilitation and/or a multi-sector response (2). The term psychosocial disability (rather than psychiatric disability) recognizes the social determinants and social consequences of disability (3). People living with persistent and complex mental health needs are one of the most excluded groups in society (4).
Thus, a person living with persistent and complex mental health needs may experience difficulties in day-to-day social and occupational functioning and have related needs due to some or all of the following: the impacts of their symptoms or cognitive difficulties; social factors such as homelessness, poverty, unemployment, stigma, and discrimination; and concurrent challenges such as substance use disorders and long-term physical health conditions (5, 6). They are often excluded from participation in education, employment, recreation, and relationships, and from securing stable, safe accommodation (3, 7). Experiences of exclusion may include poor access to health services and for some be compounded by previous negative experiences of the mental health system (including coercion, trauma, and discrimination) which may lead to reluctance to engage with treatment and support (8, 9). Dissatisfaction with treatment and poor recovery outcomes may also be due to limited treatment options, including a lack of access to needed evidence-based psychosocial models of care (10). These may all present significant impediments to both their clinical and personal recovery (11).
Despite considerable needs, this group of people has been missing from recent mental health policy which tends to focus on mental health promotion and the much larger group of people who experience more common mental health issues, such as anxiety and depression (12). For these reasons, we chose to focus this review on people with persistent and complex mental health needs, while noting that most research literature considers a wider group of people, using common but contested descriptors of serious mental illness or severe mental illness.
The needs and preferences of people living with psychosocial disabilities are diverse, along with their potential for different recovery trajectories. For many people, care and support are required to optimize the potential for a full life in the community (3, 13, 14), so mental health service provision should focus on personal as well as clinical recovery (15). Personal recovery looks different for every person, thwarting simplistic or singular descriptions. It “is ultimately about creating and living a meaningful life in a community of choice, with or without the presence of mental illness” (15, 16). However, the conditions for recovery are increasingly recognized, including empowerment, choice, and meaningful social engagement free of stigma and discrimination. These conditions may, in turn, foster enhanced participation in treatment and support (17).
Mental health services for people living with psychosocial disabilities are configured differently in each country but are typically delivered through clinical and non-government (NGO) sectors. To varying extents, these services focus on enhancing clinical, functional, and/or personal recovery. The potential inter-relationships between these types of recovery are increasingly recognized, especially when treatment and support are linked with personal goals (2, 15). With few exceptions (18), most research concerning this consumer subgroup has evaluated individual service components, rather than the whole mental health system. Furthermore, there is a need for systematic reviews of the evidence for improving individuals' clinical, functional, and personal recovery through specific models of care. Using a whole system perspective, such a review should encompass models of care across both clinical and NGO sectors, as well as blended models of care [e.g., (19, 20)].
The term “model of care” (MoC), while not universally defined, broadly, describes the multi-dimensional way (21) health services are delivered (22). Ideally, a model of care should have a delivery component, defining how care is provided (including structural components of the model: hours of operation and staffing profile), and a content component, defining the treatment, care, and support that are delivered (23). Furthermore, an MoC should have a reasonable prospect of being able to offer much of the treatment, care, and support consumers might need, though it might be supplemented by other MoCs or interventions at times. Both inpatient and community-based MoCs have a role in achieving clinical, functional, and personal recovery outcomes. However, this review focuses on community-based models of care because of the increased emphasis on community-based care, with greater potential to support clinical, functional, and personal recovery, whereas inpatient units generally focus on the former.
This systematic review aimed to generate a narrative synthesis of recent evidence, regarding community-based models of care that support the clinical, functional, and personal recovery outcomes of people living with persistent and complex mental health needs. It contains varied language to describe the experience of severe and/or persistent mental illness or mental distress, including, for example, “patient,” “consumer,” “recovery,” and “rehabilitation.” The use of any term does not imply author endorsement but reflects the context of the studies and the extent of the review. This language and construction of the research issue may rightly be contested by consumers and their families; indeed, a limitation of a systematic review is only drawing from peer-reviewed literature which is, until now, almost entirely dominated by clinical and research constructions. We aimed to identify these challenges and alternative perspectives in this article.
Methods
We conducted a systematic review of recent literature on models of care and interventions for individuals with severe and persistent mental illness and complex needs, for the Royal Commission into Victoria's Mental Health System in Australia (RCVMHS) (24). Elsewhere, we have provided a systematic review of a subset of identified studies reporting on the effectiveness of community-based models of care and interventions in supporting social inclusion for people living with severe mental illness (10), including supported accommodation, supported education, and supported employment. The present review reports on the effectiveness of community-based models of care, for individuals who experience persistent and complex mental health needs in supporting personal, functional, and clinical recovery outcomes. We did not preregister this review.
Review team
The review team is deliberately interdisciplinary and includes researchers who bring their lived and living experiences of mental health issues and psychological distress. We learned from each other and evolved our understandings of different perspectives on important foundational concepts, in undertaking literature reviews. This includes what we consider to be evidence, its critical appraisal, and choice of language.
Search strategy, and inclusion and exclusion criteria
Our search was conducted in October 2021 using Medline, EMBASE, PsycInfo, CINAHL, and Cochrane databases and included peer-reviewed articles published between October 2016 and October 2021. Our search terms (key words and MeSH terms) reflected three central concepts: “severe mental illness,” “models of care and/or interventions,” and “outcome and experience measurement” (full search string available upon request). These terms encompassed difficulties in day-to-day social and occupational functioning, co-existing conditions such as substance use and poor physical health, and other social experiences, such as unemployment and homelessness, which are likely to reflect persistent and complex mental health needs. We limited the search to publications in English and available in full text. Authors were contacted for relevant articles if the full text could not be accessed.
Inclusion criteria for the original RCVMHS search were (a) models of care (MoC) for adults aged 18–65 years with severe and persistent mental illness; and (b) group or individual interventions delivered alone or through an identified MoC. For example, Assertive Community Treatment (ACT) is a MoC (a form of intensive case management), whereas family psychoeducation is an intervention. Additional inclusion criteria for the present review were (c) community-based models of care with a delivery component that defines how care is provided and a content component that defines what treatment and care are delivered, in line with our previous definition (23); and (d) studies that evaluated MoCs for people with severe mental illness (SMI), defined as a primary diagnosis of schizophrenia, schizoaffective disorder, bipolar disorder, or other severe and enduring psychotic disorder.
Given the inconsistent terms to describe models of care, we adopted a broad definition for MoC. We used terms such as delivery of healthcare, continuity of patient care, quality of healthcare, model of care, and service delivery model. Since we aimed to identify MoCs in community settings, we included examples of integrated/coordinated care and transition pathways between hospital and community. Community-based residential services focused on clinical, functional, and/or personal recovery were also in scope. This included transitional residential rehabilitation MoCs if they were not registered as an inpatient ward. We also included studies of interventions (e.g., peer support or physical health interventions) but only when the intervention was described as augmenting or enhancing a recognized and well-described MoC (e.g., case management).
The individual-level outcomes of interest were clinical recovery (improvements in symptoms, insight, etc.); personal recovery [improvements related to illness self-management, discrimination, wellbeing, quality of life, and relational recovery (25)]; and functional recovery. We excluded service-level outcomes such as inpatient admissions and bed days as these were not capturing personal, functional, and clinical recovery outcomes per se. Similarly, we excluded days in stable housing and the number of days employed, respectively, for supported accommodation and vocational support MoCs. For MoCs other than supported employment or supported accommodation, we included employment or housing outcomes where they were used to assess functional recovery outcomes.
Study selection
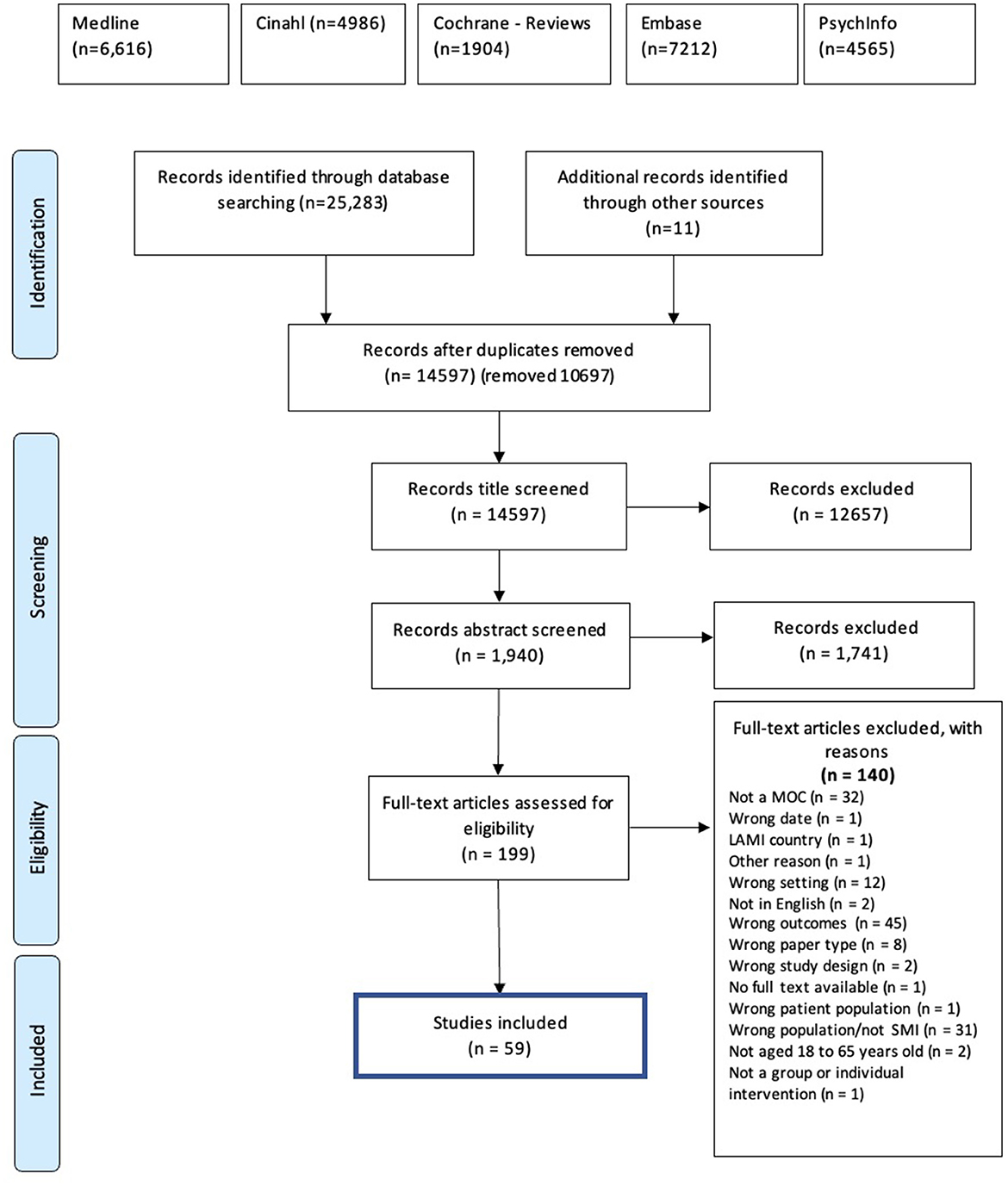
The results of the original search undertaken for the RCVMHS, updated in October 2021 to extend the study period to 5 years, were screened using the Covidence online software (https://www.covidence.org). After duplicates were removed, reviewers screened by title, abstract, and full text, with each study requiring two “yes” votes at the abstract and full-text screening stage to be included. Conflicting votes were resolved through consulting with the project leads (CH and LB).
Quality of evidence
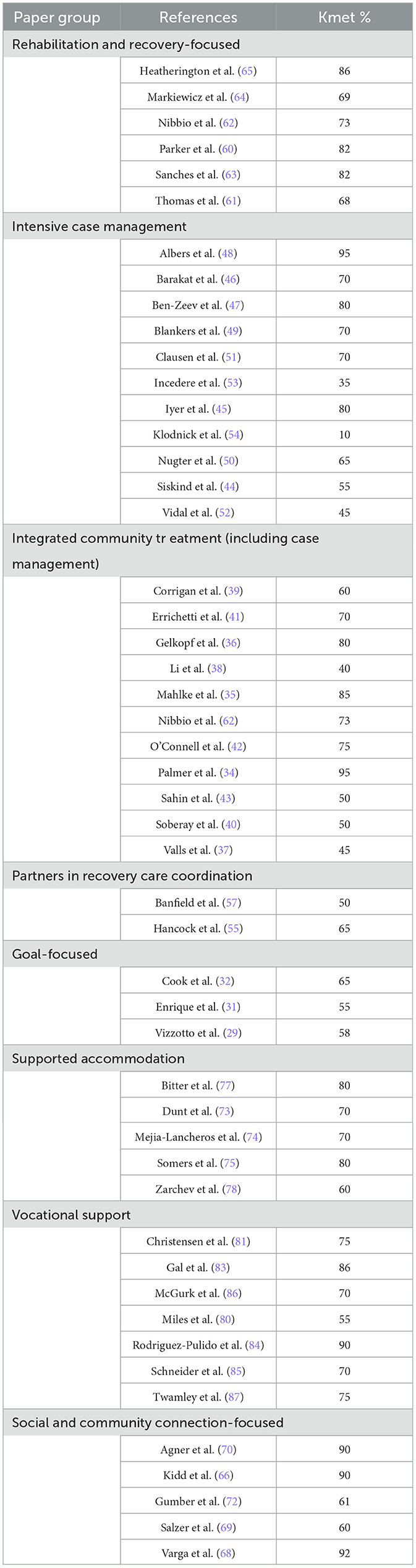
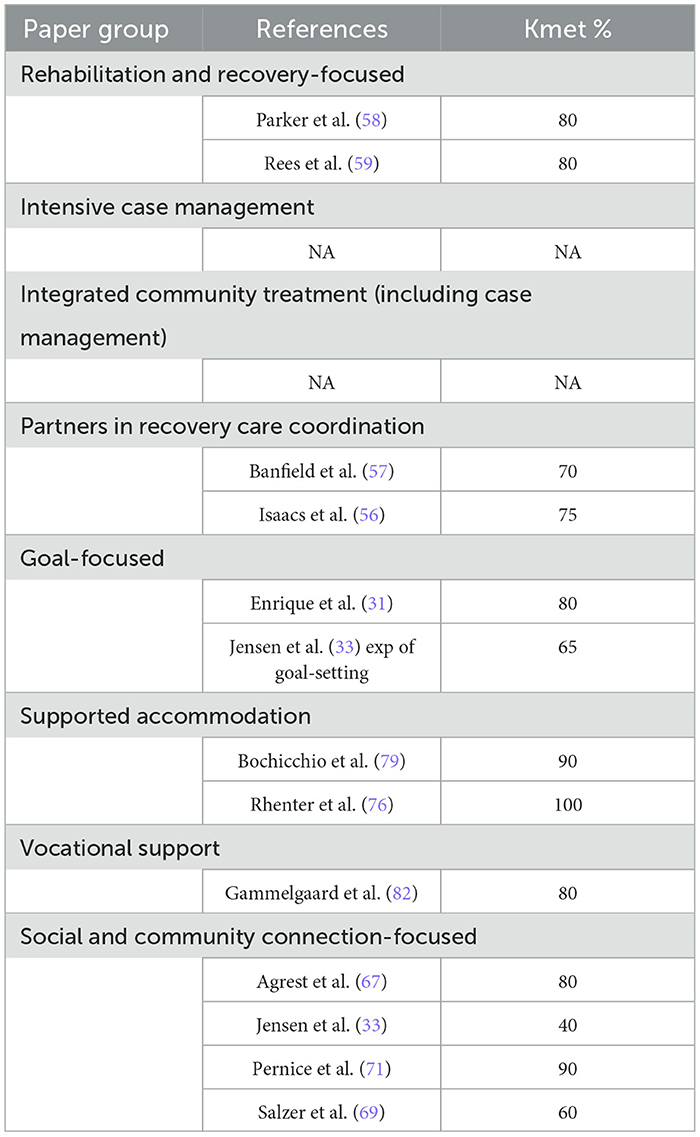
The included articles were evaluated by the Kmet standard criteria to assess the methodological quality of both quantitative and qualitative research (26). Quantitative papers were rated on 14 items and qualitative papers on 10 items, related to the study design; participant selection; data analysis methods; and the clarity and interpretation of results. Each article was rated by one reviewer and validated through discussion between reviewers at regular meetings, to ensure consistency in rating. Total scores were reported out of 100 (i.e., as percentage equivalents), to take account of non-applicable items.
We developed a data extraction table and guidance notes, to enhance consistency in the description and synthesis of findings from studies. Studies were grouped according to MoCs derived from our original RCVMHS review and collective knowledge of this area of service delivery, and each co-author produced a textual summary for one model. To ensure consistency, the textual summaries were refined and finalized through consensus discussion across the author group. A descriptive overview of the features and findings for each MoC was then generated. This allowed for further scrutiny and reorganization of study groupings and their optimum placement within the final set of MoCs.
Narrative synthesis
Given the range of MoCs included, we chose a narrative synthesis as the most suitable approach to summarize our findings. Narrative synthesis includes a preliminary synthesis to identify patterns of findings across studies; exploration of whether effects of an intervention vary according to study population; identification of factors influencing the results within individual studies and explaining differences between studies; development of a theoretical framework underpinning specific intervention effects; assessment of the robustness of the synthesis based on the strength of evidence; and discussion of the generalizability of conclusions to wider populations and contexts (27). Each model was rated and categorized as either best practice, promising practice, or emerging practice, according to an overall rating of the level of evidence (28). Since our review included multiple MoCs, we did not aim to develop a theoretical framework underpinning the effects of each model. Our four researchers with lived experience led the narrative synthesis.
Results
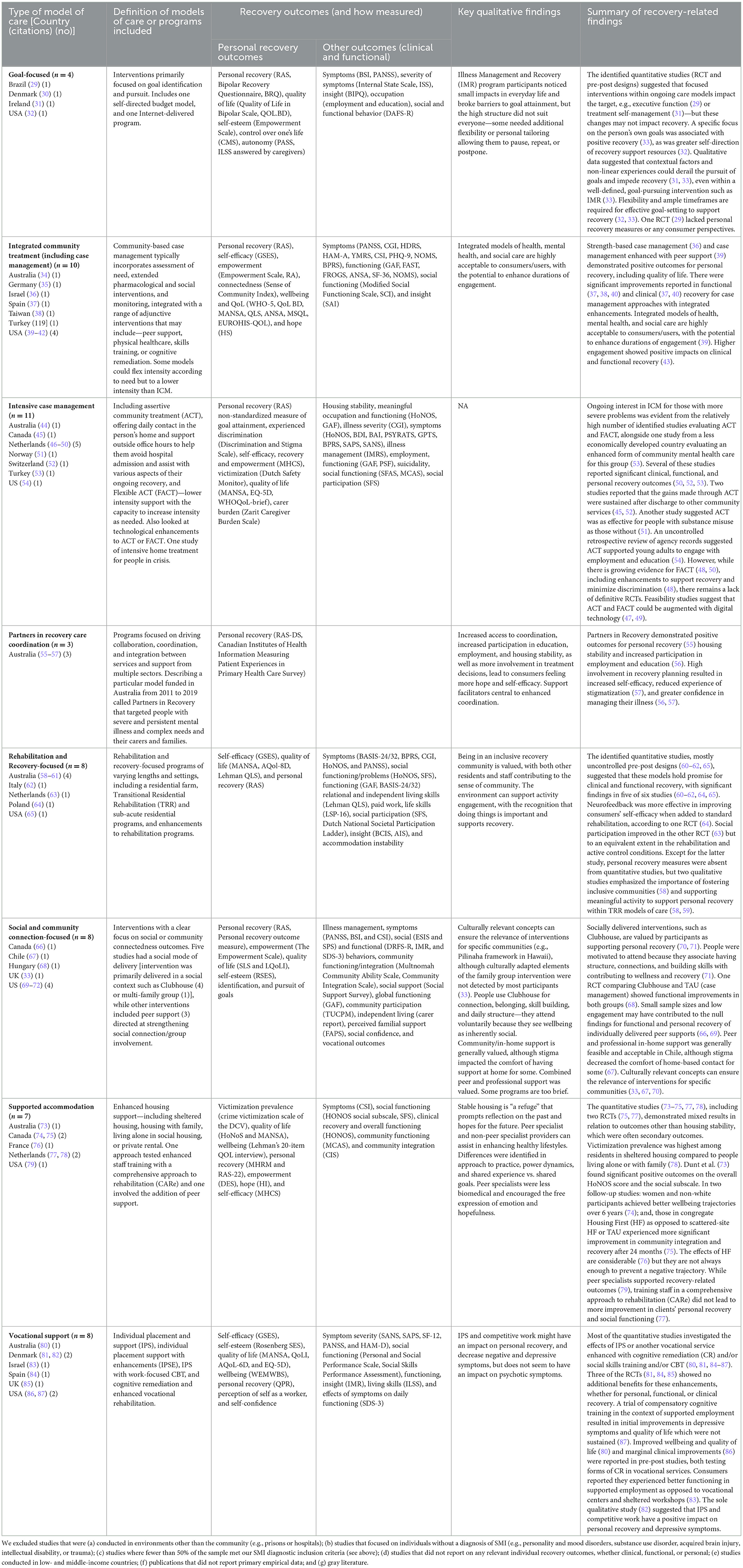
Fifty-nine studies that met our inclusion criteria (46 quantitative,10 qualitative, three mixed methods; PRISMA flowchart in Figure 1; summary of study characteristics in Table 1) across 20 high-income countries are Australia (11), Brazil (1), Canada (4), Chile (1), Denmark (3), France (1), Germany (1), Hungary (1), Ireland (1), Israel (2), Italy (1), Netherlands (8), Norway (1), Poland (1), Spain (2), Switzerland (1), Taiwan (1), Turkey (2), UK (2), and US (14). Sample sizes ranged from 15 to 4,216 participants. The average Kmet score for quantitative papers was 68 (range = 10–95) and for qualitative papers was 76 (range = 40–100) (Tables 2A, B).
The studies considered a range of clinical, functional, and personal recovery outcomes. More measurement efforts focused on clinical recovery—symptoms, psychological distress, and illness severity—and functional recovery—general functioning, employment, housing stability, and social functioning. Personal recovery was assessed by a range of measures, some of which had clear evidence of co-design with people with lived and living experience, whereas others, such as the General Self-Efficacy Scale (88), did not. Qualitative studies noted factors relevant to personal recovery including hope, empowerment, connectedness, and inclusion. Where social outcomes were measured, this was more typically through social skills/functioning (functional recovery) than through the establishment of meaningful social connections (personal recovery).
Methods of assessing outcomes varied considerably (see Table 1) and included both standardized measures, subscales or individual items from standardized measures, or uniquely developed measures for individual studies. The specificity or generality of outcomes varied considerably across studies, making comparison and integration of findings challenging. For example, measurement of functioning varied from global (e.g., Global Assessment of Functioning, GAF) (89) to fine-grained (e.g., social functioning using the Social Functioning Assessment Scale, SFAS, the External Social Integration Scale, ESIS, and the Social Provisions Scale, SPS) (90–92).
Model of care characteristics and study findings
Papers evaluating different MoCs were grouped as follows: goal-focused; integrated community treatment (including case management); intensive case management; partners in recovery care coordination; rehabilitation and recovery-focused; social and community connection-focused; supported accommodation; and vocational support. Each of these is defined in Table 1, along with a high-level summary of the findings per group. Details of each study's findings and corresponding details of the delivery and content characteristics of the researched MoC are presented in Tables 3, 4, respectively. Most MoCs either had some examples of team delivery (e.g., integrated community treatment) or were explicitly a team-based approach (e.g., partners in recovery care coordination; see Table 4). Where studies included a comparison to treatment as usual (TAU), this was often poorly described [e.g., (37, 45, 46)].
Narrative synthesis
Overall pattern of findings
This systematic review identified a diverse array of MoCs that seek to improve clinical, functional, and personal recovery outcomes in people who experience SMI. Almost half of the included studies reflected MoCs with a well-established evidence base such as intensive case management, supported accommodation, and vocational support (10, 95–97). We also identified novel or less established MoCs, which either updated community treatment models, including case management and care coordination (e.g., integrated community treatment), or more explicitly addressed participants' personal (and functional) recovery goals [e.g., (32, 67, 68)].
Few of the studies reported on our outcomes of interest (i.e., clinical, functional, or personal recovery) as primary outcomes. Personal recovery was reported as a primary outcome in only four studies (31, 32, 34, 77). The rehabilitation and recovery-focused MoC and the intensive case management MoC both had the strongest emphasis on clinical outcomes. This may be because they are older MoCs (98, 99). Personal recovery was reported more frequently in newer MoCs (e.g., goal-focused and social and community connection-focused) and in nearly all models involving peer workers. The findings suggest participants' clinical and functional improvement can be supported by some intensive case management and rehabilitation and recovery-focused models, adding to the existing evidence of their association with reduced service use (18, 95). We also identified potential for personal recovery to be supported by both these types of MoC, as shown by qualitative studies concerning the rehabilitation and recovery-focused MoC, for example (58, 59).
This review identified less intensive case management models, often with novel enhancements or better integration of care (see Table 1 for details). These articles reported promising evidence for all three of this review's outcomes of interest (i.e., clinical, functional, and personal recovery) [e.g., (36, 37, 39)]. Our previous systematic review of social interventions for people with SMI (10) suggested that the supported accommodation MoC can support consumers' social inclusion. This review also provided some evidence that it could improve personal recovery outcomes such as hope and subjective wellbeing (74, 79). The studies in the goal-focused and the social and community connection-focused MoCs reported encouraging improvement in some functional and personal recovery outcomes, but we found only limited evidence for the vocational support MoC in improving clinical, personal, or functional recovery (80, 83, 86, 87).
Overall, 10 studies reported incorporating peer work. Four belonged to the integrated community treatment MoC (35, 39, 40, 42), three to the social and community connection-focused MoC (66, 67, 69), and one each to rehabilitation and recovery-focused (58), intensive case management (45), and supported accommodation (79) MoCs.
Factors influencing the findings
The findings of this review should be interpreted with consideration of the potential impact of clinician and researcher bias on the formulation of the research problem, the chosen measurement tools, the interpretation of the results, and the impact of study quality [see Tables 2A, B (Kmet scores)]. Some studies were constructed in a way that lacked a depth of understanding of the complexities of recovery and the needs of participants. Studies often did not report a deeper contextual understanding of the participants' lives, and, particularly in uncontrolled studies, the impact of key mediators, moderators, or confounders such as family support, loneliness, or the impact of stigma.
Overall, the studies typically included clinical, functional, and personal recovery outcomes as secondary outcomes after primary outcomes such as service use. We used a broad interpretation of personal recovery and thus included wellbeing and quality of life outcomes, resulting in all the included MoCs having at least one quantitative or qualitative study that assessed personal recovery outcomes. However, we found that the use of measures specifically focused on personal recovery outcomes was limited, in contrast to other areas of recovery. A small number of measures featured the domains that have emerged from the recovery movement, such as hope and empowerment. These were the Recovery Assessment Scale and associated modified versions (RAS) (100), the Personal Recovery Outcome Measure (PROM) (101), Canadian Institutes of Health Information Measuring Patient Experiences in Primary Health Care Survey (CIHI) (102), the Mental Health Recovery Measure (MHRM) (103), Questionnaire about the Process of Recovery (QPR) (104), and the Bipolar Recovery Questionnaire (BRQ) (105). Only the RAS and modified versions (RAS-R, RAS-D, RAS-DS, and RAS-22) were used in more than one study (32, 34, 39, 47, 52, 55, 63, 69, 75). Thus, when compared to commonly used clinical or functional recovery outcome measures such as the PANSS or GAF, routine focus on personal recovery using established, standardized tools is apparently still in its infancy.
Context
The involvement of Lived Experience in the design of the MoCs or the research efforts was not always clear. Few publications reported consumer co-design (34, 70) or consumer involvement in the development or conduct of the study (36, 58, 59, 63), and none were consumer-led. Only Kidd et al. (66) had consumer co-authors, of which there were three. A few studies reported consumer input into the research interview questions (59), the analysis coding framework (58), and consultation to inform the study methodology (63). Peer support was reported in some models across multiple study designs showing beneficial results (35, 79). The clubhouse model was particularly successful in enabling a recovery-oriented environment (70–72).
In addition, few articles took account of relational and family factors, despite these having been shown to be important in the outcome of psychosocial interventions (106). Some of the evidence suggested families and carers were better equipped to provide care when supported. One small uncontrolled study showed significantly reduced “carer burden” (which we took to mean pressure on carers), within an intensive case management model incorporating family psychoeducation and supported employment (53). Positive or rewarding impacts of caring were not assessed by any studies, despite evidence that relationships within families may be mutually supportive (107) and culturally significant (70). Furthermore, caring relationships can benefit consumers. An MoC incorporating family involvement (33) showed both personal and interpersonal benefits for consumers. Family support was also associated with better social integration within a Clubhouse (72), echoing the findings of Fossey and Harvey (108).
Problems with terminology
Variations in terminology presented problems in understanding and defining the population, the MoC, and the outcomes. Furthermore, to limit the heterogeneity of the target population, we only included consumers experiencing SMI, which posed several challenges, due to the lack of a standardized definition for SMI. Previous conceptions have most often defined SMI in terms of (i) diagnosis; (ii) intensity and chronicity of symptoms; and (iii) complexity of service use needs. Our review defined SMI based on diagnosis, with consideration of the complexity of service needs. Therefore, in articles where our population was comprised of numerous diagnoses, we required that over 50% of the study population experienced schizophrenia, schizoaffective disorder, bipolar disorder, or other severe and enduring psychotic disorders. Articles with participants with unclear diagnoses were excluded. Some articles did not define individuals based on diagnosis, making it challenging to understand who received the intervention [e.g., (72)]. While we understood the potential value of being cautious in not describing people using diagnostic labels, this contributed to challenges regarding who was receiving the intervention and how generalizable the findings may be.
Delivery and content of the interventions
We attempted to define MoCs in terms of delivery and content components for this systematic review (23), but the identified studies were still challenging to assess. As an illustration, 32 articles were excluded at the full-text review stage because we could not determine that an MoC was described. The delivery of care in terms of its intensity and availability throughout the week differed between and within the MoC groups, despite our efforts to create meaningful groupings (Table 4). Delivery was typically face-to-face, team-based, and sometimes embedded in existing services [e.g., (48, 53, 66)]. This latter was particularly the case for peer-led or self-directed interventions. There was a typically higher intensity of contact in the intensive case management MoC compared with the goal-focused MoC. Within the social and community connection-focused MoC, the frequency of delivery varied from a mean of 1 h per month (69) to opportunities to participate in a Clubhouse every weekday (71). These variations might help explain differences in outcomes between models, as well as negative outcomes.
The content of interventions within each MoC grouping was also diverse, although generally well-described. Poor descriptions of the content of interventions in some publications may have led to them being excluded from our final sample. Control or comparison groups were also poorly described at times [e.g., (36, 68)]. This was particularly problematic in studies where the intervention was offered as an enhancement to usual care (59, 81, 86).
Generalizability
Whether findings are generalizable requires consideration of the study environments, interventions, and participants. All the studies were conducted in high-income countries, and findings may not be generalizable to low- and middle-income countries. Most studies had more male than female participants (see Tables 2A, B). Other factors that could impact generalizability, such as language spoken at home, other service use, and family support, were rarely reported.
Strength of the evidence
Only two of the MoC subgroups included a majority of articles reporting on RCTs or cohort studies, i.e., stronger evidence (https://www.cebm.ox.ac.uk, Intensive Case Management MoC-−8 of 11; Integrated Community Treatment MoC-−6 of 10; see Table 3). The absence of good-quality study designs was evident in MoCs that were both longstanding (e.g., rehabilitation and recovery-focused, supported accommodation) and newer (social and community connection-focused, and goal-focused). Well-established models such as intensive case management, vocational support, and supported accommodation may be difficult to evaluate through RCTs as 'TAU' is not considered an ethical comparison (10). Perhaps this explains why a substantial minority of included studies examined subtypes of the model [e.g., (75)], newer modes of delivery [e.g., (49)], the relevance of the model to specific consumer subgroups [e.g., (51)], or enhancements to the model [e.g., (84)]. This methodological range made it difficult to conclude the overall benefits of each model, in relation to our outcomes. We also noted a lack of qualitative (n = 10) and mixed-method (n = 3) study designs. Qualitative research could provide a greater understanding of each model's benefits and how to maximize their value to consumers, while also soliciting their perspectives.
Some high-quality studies failed to show benefits to consumers in relation to our outcomes of interest. For example, three studies of intensive case management failed to show improved consumer self-efficacy (46, 48, 49). Two trials of staff training in comprehensive approaches to rehabilitation (63, 77) were negative. Three trials of enhancements for vocational services were negative (81, 84, 85). In the social and community connection-focused model, there were null findings for functional and personal recovery of individually delivered peer supports (66, 69). Various explanations are reported, beyond the conclusion that the model is not effective, concerning the outcomes in question. The impact of comparing the model with an active control (63), difficulties in implementing rehabilitation-supporting practice (77), and low engagement in the model (66, 69, 81) may all be relevant and have been reported elsewhere (109).
There were further subtle differences in the quality of the evidence within sub-groupings of articles. For example, integrated community treatment models of care research activity generally scored quite high against the Kmet criteria, suggesting that recent trials have led to more consistent and robust evidence of the value of this model of care. Intensive case management had wider variation in the quality of the studies, with scores ranging from 10 to 95, suggesting that the research base for this MoC has developed less consistently, resulting in a more mixed picture concerning study quality.
Bearing these issues in mind, our findings provided promising evidence for clinical and functional outcomes associated with intensive case management, rehabilitation and recovery-focused, and integrated community treatment models, with the latter also showing some promise for supporting personal recovery. Nonetheless, these findings are consistent with previous calls for more high-quality research concerning such models (18, 110), especially studies of outcomes valued by consumers (and their families) themselves (111). Supported accommodation and models focused on goals or social and community connections are all emerging practices with respect to supporting personal recovery. Models focused on specific outcomes consistent with consumers' priorities also appear helpful in supporting functional recovery. Although the potential for vocational support to support personal recovery is well-recognized (112), we found limited evidence for improved personal and functional recovery. A specific care coordination service model for people living with severe and persistent mental illness showed emerging evidence of benefits for personal recovery (Partners in recovery care coordination). This is noteworthy, since such approaches offer the potential to overcome recognized service access difficulties experienced by this group of consumers (113).
Limitations of the included studies
The included studies had some limitations. There were far more quantitative studies than qualitative, but the quality of these studies was not consistently strong. Across all included studies where there was capacity for blinding, this was not typically used. The studies were often small-scale, lacked a comparison group, had high drop-out rates, and did not report on the sustainability of changes longitudinally, or on between-group differences. Studies had potential response bias, and some had difficulties in sustaining the engagement of participants (40, 66). Another limitation is the time frame we chose. There are potentially relevant studies that predated our review period.
Discussion
Our review considered the recovery outcomes achieved by both long-standing and emerging models of care in mental health service delivery. Our purpose was to consider the attention being given to recovery outcomes, considering the overarching imperative to ensure models of care are addressing what people want and need. In previous research, consumers have been asked what they consider to be the most important issues in their lives. Most of these priorities are related to clinical, functional, and personal recovery, including social connection and managing distressing symptoms (5).
There are significant expectations that mental health services can demonstrate the implementation of MoCs, especially for people with persistent and complex mental health needs. This review originated in efforts to identify optimal MoCs in the context of a potentially transformative process being undertaken by the Royal Commission into Victoria Mental Health Services (RCVMHS) (10). Model of care is a term frequently used and perhaps relied on for system development and reform, but this review confirmed there is minimal consistency regarding its meaning.
We concluded that community-based MoCs include a delivery component that defines how care is provided and a content component which comprises a set of interventions. In our previous study, we demonstrated that MoCs are usually delivered within a multidisciplinary team that increasingly includes peer support workers or experts through Lived Experience (10). While we established a definition related to providing a holistic approach to treatment, care, and support, it was difficult to apply our definition in practice. We found that defining and grouping MoCs required careful thought and agreement among our team. We noticed some MoCs were well-established, such as intensive case management, supported accommodation, and vocational support, while others were emerging. The evolution of the models impacted the quality of evidence, the outcomes that tended to focus on, and the degree to which they were incorporating more contemporary paradigms and practices. For example, there was variation in the degree to which personal recovery and peer support were incorporated into service provision and research. Some MoCs, particularly the more well-established, had good detail about structure, consumer group, and content, whereas newer MoCs tended to be less well-defined and consistent.
The diversity of content and delivery components within related MoCs may represent innovation and local adaptation on the one hand [e.g., (114)] and model drift and poor implementation on the other. Alternatively, it may represent a tailoring to the needs of a cohort that becomes better understood over time. This is the crux of the challenge in implementing any complex intervention, of which any MoC is a prime example (115). Indeed, a focus on fidelity may unintentionally restrict how an MoC might adapt in relation to local contexts and fluctuating consumer needs, emergent knowledge, or in relation to the way outcomes are measured. For example, in this review, many vocational support MoCs were excluded because the predominant primary outcome measure in these studies remains the number of days or hours a participant was in paid employment—not an individual recovery outcome measure. Although we cannot conclude this from our review, it is feasible that MoCs that do not evolve to become more person-centered and adopt contemporary ideas about what represents a “good” outcome for consumers, may be at risk of reinforcing more “institutional” practices, especially when services are under pressure. However, we noted that even MoCs achieving positive recovery outcomes (55–57) are not guaranteed ongoing support to enable them to consolidate, as is evident in the partners in recovery care coordination model, which has been gradually defunded in Australia, despite the promising evidence (116).
One sign of the evolution of a model is the incorporation of Lived Experience perspectives and peer support workers. This is gaining traction, but it requires evaluation of why and how it works, how it adds value, and when and how it is appropriately included. Overall, consumer input could have been used more widely to increase understanding of the research problem, co-develop and co-conduct the research, and improve data collection and dissemination (117). People with persistent and complex mental health needs commonly experience marginalization and exclusion, including opportunities to participate in research and service improvement. Ensuring their voices are heard is an opportunity to address this gap (118).
The lack of attention to recovery outcomes may be related to the timeframes studies are conducted within—it may take many years to see genuine recovery outcomes, and recovery tends not to be linear. So, even studies with a 1- or 2-year follow-up (and rarely it is longer) may find measuring recovery unrealistic—especially personal recovery (119). There are also issues in relation to whether the “dose” participants received in the timeframe of a study is sufficient to measure its impact (80). The individual meaning of personal recovery may create measurement challenges, but similar complexity is dealt with elsewhere, e.g., in cognitive neuroscience where no one person has the same pattern of individual strengths and weaknesses (120)—so it ought to be possible to incorporate recovery measures that respond to this challenge, especially if the goal of MoCs is be person-centered, holistic, and recovery-oriented (121).
Evaluation of models of care can be challenging when uptake and engagement are low [e.g., (42, 85, 87)]. This again suggests the importance of appreciating the context of intervention and the factors explaining poor engagement, or high levels of attrition (34). The impact of COVID-19 on attrition and completion rates needs to also be considered as this potentially had an important impact on studies [e.g., (37)]. Funding uncertainty also appears to impact outcomes (57).
Conclusion and recommendations
Our findings provided promising and emerging evidence for recovery outcomes associated with a range of existing models of care. However, MoCs should evolve to meet the varied needs of people with persistent and complex mental health problems. Our review suggests the need for a sophisticated response that likely requires a multidisciplinary team approach, to respond and adapt to the context within which a MoC operates. While MoCs need specific design parameters for successful implementation, they also need to be able to incorporate consumer perspectives, ideally through co-design, to enhance recovery outcomes (122). Therefore, we recommend that (1) further research be conducted into outcomes associated with the MoCs we identified, ensuring that all three types of outcomes are assessed; (2) future research into these models should prioritize a consistent set of reliable and valid outcome measures such as the RAS and MANSA and attend to other identified methodological limitations so that meta-analyses can be conducted; (3) practice guidelines should recommend team-based models of care in line with this evidence, such as ICM and ICT, while enhancements to team-based MoCs should particularly focus on supporting personal recovery; (4) when developing new service models and improving existing service models for this consumer group, consumer goals and priorities should be a specific focus, to help clinicians challenge unhelpful ways of relating to consumers, and (5) further research should attend more closely to timeframes, including extended follow-up phases, to understand recovery impacts over time.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
CH: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing—original draft, Writing—review and editing. T-MZ: Data curation, Formal analysis, Investigation, Project administration, Writing—original draft, Writing—review and editing. CB: Data curation, Formal analysis, Investigation, Methodology, Writing—original draft, Writing—review and editing. PE: Data curation, Formal analysis, Investigation, Methodology, Writing—original draft, Writing—review and editing. JF: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing—original draft, Writing—review and editing. BH: Data curation, Formal analysis, Investigation, Methodology, Supervision, Writing—original draft, Writing—review and editing. HKi: Data curation, Formal analysis, Investigation, Methodology, Writing—original draft, Writing—review and editing. PM: Formal analysis, Investigation, Writing—review and editing. HKe: Data curation, Formal analysis, Writing—review and editing. LB: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing—original draft, Writing—review and editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The previous iteration of this review was funded by the Royal Commission into Victorian Mental Health services. This update of the initial review did not receive funding.
Conflict of interest
PE was employed by Neami National.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hayes L, Brophy L, Harvey C, Herrman H, Killackey E, Tellez JJ. Effective, Evidence-Based Psychosocial Interventions Suitable for Early Intervention in the National Disability Insurance Scheme (NDIS): Promoting Psychosocial Functioning and Recovery. Melbourne, VIC (2016).
2. National Institute For Health And Care Excellence. Rehabilitation for Adults With Complex Psychosis. London (2020).
3. Killackey E, Harvey C, Amering M, Herrman H. Partnerships for meaningful community living: rehabilitation and recovery-informed practices. In: A Tasman, J Kay, JA Lieberman, MB First, and MB Riba, editors, Psychiatry. 5th ed. London: Wiley-Blackwell (2024).
4. Boardman J, Killaspy H, Mezey G. Social Inclusion and Mental Health: Understanding Poverty, Inequality and Social Exclusion. Cambridge: Cambridge University Press (2022).
5. Morgan VA, Waterreus A, Carr V, Castle D, Cohen M, Harvey C, et al. Responding to challenges for people with psychotic illness: updated evidence from the Survey of High Impact Psychosis. Austr N Zeal J Psychiatry. (2017) 51:124–40. doi: 10.1177/0004867416679738
6. Harvey C, Brophy L, Parsons S, Moeller-Saxone K, Grigg M, Siskind D. People living with psychosocial disability: Rehabilitation and recovery-informed service provision within the second Australian national survey of psychosis. Austr N Zeal J Psychiatry. (2016) 50:534–47. doi: 10.1177/0004867415610437
7. Craig T. What is psychiatric rehabilitation? In: G Roberts, S Davenport, F Holloway, and T Tattan, editors, Enabling Recovery: The Principles and Practice of Rehabilitation Psychiatry. London: Royal College of Psychiatrists (2006) 3–17.
8. Dawson S, Muir-Cochrane E, Simpson A, Lawn S. Community treatment orders and care planning: how is engagement and decision-making enacted? Health Expect. (2021) 24:1859–67. doi: 10.1111/hex.13329
9. Mcmillan J, Lawn S, Delany-Crowe T. Trust and community treatment orders. Front Psychiatry. (2019) 10:349. doi: 10.3389/fpsyt.2019.00349
10. Killaspy H, Harvey C, Brasier C, Brophy L, Ennals P, Fletcher J, et al. Community-based social interventions for people with severe mental illness: a systematic review and narrative synthesis of recent evidence. World Psychiatry. (2022) 21:96–123. doi: 10.1002/wps.20940
11. Holloway F. The Forgotten Need for Rehabilitation in Contemporary Mental Health Services: A Position Statement From the Executive Committee of the Faculty of Rehabilitation and Social Psychiatry. London: Royal College of Psychiatrists (2005).
12. Vistorte AOR, Ribeiro WS, Jaen D, Jorge MR, Evans-Lacko S, Mari JJ. Stigmatizing attitudes of primary care professionals towards people with mental disorders: a systematic review. Int J Psychiatry Med. (2018) 53:317–38. doi: 10.1177/0091217418778620
13. Davidson L, O'connell M, Tondora J, Styron T, Kangas K. The top ten concerns about recovery encountered in mental health system transformation. Psychiatr Serv. (2006) 57:640–5. doi: 10.1176/ps.2006.57.5.640
14. Mueser K. Evidence-based practices and recovery-oriented services: is there a relationship? Should there be one? Psychiatr. Rehabil. J. (2012) 35:287–8. doi: 10.2975/35.4.2012.287.288
15. Davidson L. The recovery movement: implications for mental health care and enabling people to participate fully in life. Health Affect. (2016) 35:1091–7. doi: 10.1377/hlthaff.2016.0153
16. State of Victoria. Royal Commission into Victoria's Mental Health System, Interim Report, Parliament Paper No. 87. State of Victoria: Melbourne (2018).
17. Dixon LB, Holoshitz Y, Nossel I. Treatment engagement of individuals experiencing mental illness: review and update. World Psychiatry. (2016) 15:13–20. doi: 10.1002/wps.20306
18. Dalton-Locke C, Marston L, Mcpherson P, Killaspy H. The effectiveness of mental health rehabilitation services: a systematic review and narrative synthesis. Front Psychiatry. (2021) 11:607933. doi: 10.3389/fpsyt.2020.607933
19. Parker S, Arnautovska U, Korman N, Harris M, Dark F. comparative effectiveness of integrated peer support and clinical staffing models for community-based residential mental health rehabilitation: a prospective observational study. Community Ment Health J. (2023) 59:459–70. doi: 10.1007/s10597-022-01023-8
20. Harvey C, Brophy L, Tibble H, Killaspy H, Spittal MJ, Hamilton B, et al. Prevention and recovery care services in Australia: developing a state-wide typology of a subacute residential mental health service model. Front Psychiatry. (2019) 10:383. doi: 10.3389/fpsyt.2019.00383
21. Nancarrow S, Roots A, Moran A, Grace S, Lyons K, Hulcombe J, et al. Queensland Health Practioners' Models of Care Project: Evaluation, Learning and Upscaling of Results for a National Audience. Final Report. Southern Cross University, Lismore and Coffs Harbour, NSW, Australia (2013).
22. NSW Agency For Clinical Innovation. Evaluation and Monitoring Tool Rehabilitation Model of Care. Sydney, NSW: NSW Agency For Clinical Innovation (2013).
23. Kakuma R, Hamilton B, Brophy L, Minas H, Harvey C. Models of Care for People With Severe and Enduring Mental Illness: An Evidence Check Rapid Review Brokered by the Sax Institute for the NSW Ministry of Health. Sydney, NSW: Sax Institute; University of British Colombia Centre for Health Services and Policy Research (2017).
24. Royal Commission Into Victoria's Mental Health System. A New Approach to Mental Health and Wellbeing in Victoria. Melbourne: Royal Commission Into Victoria's Mental Health System (2021).
25. Price-Robertson R, Obradovic A, Morgan B. Relational recovery: beyond individualism in the recovery approach. Adv Mental Health. (2017) 15:108–20. doi: 10.1080/18387357.2016.1243014
26. Kmet L, Lee R, Cook L. Standard Quality Assessment Criteria for Evaluating Primary Research Papers From a Variety of Fields. Alberta Heritage Foundation for Medical Research (2004).
27. Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews: A Product From the ESRC Methods Programme. (2006).
28. Canadian Homelessness Research Network. What Works and for Whom? A Framework for Promising Practices. York, ON (2013).
29. Vizzotto A, Celestino D, Buchain P, Oliveira A, Oliveira G, Di Sarno E, et al. Occupational goal intervention method for the management of executive dysfunction in people with treatment-resistant schizophrenia: a randomized controlled trial. Am J Occup Therapy. (2021) 75:43257. doi: 10.5014/ajot.2021.043257
30. Jensen SB, Eplov LF, Mueser KT, Petersen KS. Participants' lived experience of pursuing personal goals in the Illness Management and Recovery program. Int J Soc Psychiatry. (2021) 67:360–8. doi: 10.1177/0020764020954471
31. Enrique A, Duffy D, Lawler K, Richards D, Jones S. An internet-delivered self-management programme for bipolar disorder in mental health services in Ireland: results and learnings from a feasibility trial. Clin Psychol Psychother. (2020) 27:925–39. doi: 10.1002/cpp.2480
32. Cook JA, Shore S, Burke-Miller JK, Jonikas JA, Hamilton M, Ruckdeschel B, et al. Mental health self-directed care financing: efficacy in improving outcomes and controlling costs for adults with serious mental illness. Psychiatric Services. (2019) 70:191–201. doi: 10.1176/appi.ps.201800337
33. Jensen E, Carr R, Degnan A, Berry K, Edge D. Exploring service user and family perspectives of a Culturally adapted Family Intervention (CaFI) for African-Caribbean people with psychosis: a qualitative study. Br J Clin Psychol. (2021) 60:270–89. doi: 10.1111/bjc.12273
34. Palmer VJ, Chondros P, Furler J, Herrman H, Pierce D, Godbee K, et al. The CORE study—an adapted mental health experience codesign intervention to improve psychosocial recovery for people with severe mental illness: a stepped wedge cluster randomized-controlled trial. Health Expectationsat. (2021) 24:1948–61. doi: 10.1111/hex.13334
35. Mahlke CI, Priebe S, Heumann K, Daubmann A, Wegscheider K, Bock T. Effectiveness of one-to-one peer support for patients with severe mental illness - a randomised controlled trial. Eur Psychiatry. (2017) 42:103–10. doi: 10.1016/j.eurpsy.2016.12.007
36. Gelkopf M, Lapid L, Werbeloff N, Levine SZ, Telem A, Zisman-Ilani Y, et al. A strengths-based case management service for people with serious mental illness in Israel: a randomized controlled trial. Psychiatry Res. (2016) 241:182–9. doi: 10.1016/j.psychres.2016.04.106
37. Valls È, Bonnín CM, Torres I, Brat M, Prime-Tous M, Morilla I, et al. Efficacy of an integrative approach for bipolar disorder: preliminary results from a randomized controlled trial. Psychol Med. (2022) 52:4094–105. doi: 10.1017/S0033291721001057
38. Li JB, Liu WI, Huang MW. Integrating evidence-based community-care services to improve schizophrenia outcomes: a preliminary trial. Arch Psychiatr Nurs. (2016) 30:102–8. doi: 10.1016/j.apnu.2015.08.018
39. Corrigan P, Sheehan L, Morris S, Larson JE, Torres A, Lara JL, et al. The impact of a peer navigator program in addressing the health needs of latinos with serious mental illness. Psychiatric Services. (2018) 69:456–61. doi: 10.1176/appi.ps.201700241
40. Soberay A, Tolle LW, Kienitz E, Olson A. The hope health and wellness clinic: outcomes of individuals with serious mental illness in a bidirectional integrated care clinic. Community Ment Health J. (2021) 57:675–83. doi: 10.1007/s10597-020-00730-4
41. Errichetti KS, Flynn A, Gaitan E, Ramirez MM, Baker M, Xuan Z. Randomized trial of reverse colocated integrated care on persons with severe, persistent mental illness in Southern Texas. J Gen Intern Med. (2020) 35:2035–42. doi: 10.1007/s11606-020-05778-2
42. O'Connell MJ, Sledge WH, Staeheli M, Sells D, Costa M, Wieland M, et al. Outcomes of a peer mentor intervention for persons with recurrent psychiatric hospitalization. Psychiatric Serv. (2018) 69:760–7. doi: 10.1176/appi.ps.201600478
43. Sahin SK, Elboga G, Altindag A. The effects of the frequency of participation to the community mental health center on insight, treatment adherence and functionality. Klinik Psikiyatri Dergisi. (2020) 23:64–71. doi: 10.5505/kpd.2020.49369
44. Siskind D, Dark F, Carney K, Gore-Jones V, Kar Ray M, Steginga A, et al. Placing rehabilitation at the core of assertive community treatment. Australasian Psychiatry. (2021) 29:47–51. doi: 10.1177/1039856220928876
45. Iyer SN, Mustafa SS, Moro L, Jarvis GE, Joober R, Abadi S, et al. Suicidality over the first 5 years of psychosis: does extending early intervention have benefits? Can J Psychiatry. (2021) 66:468–76. doi: 10.1177/0706743720961714
46. Barakat A, Blankers M, Cornelis JE, Lommerse NM, Beekman ATF, Dekker JJM. The effects of intensive home treatment on self-efficacy in patients recovering from a psychiatric crisis. Int J Ment Health Syst. (2021) 15:1. doi: 10.1186/s13033-020-00426-y
47. Ben-Zeev D, Buck B, Meller S, Hudenko WJ, Hallgren KA. Augmenting evidence-based care with a texting mobile interventionist: a pilot randomized controlled trial. Psychiatric Services. (2020) 71:1218–24. doi: 10.1176/appi.ps.202000239
48. Albers WMM, Roeg DPK, Nijssen YAM, Deen ML, Bongers IMB, Van Weeghel J. Intervention to prevent and manage the effects of victimization related to social participation for people with severe mental illness: results from a cluster randomized controlled trial. Psychiatr Rehabil J. (2021) 44:254–65. doi: 10.1037/prj0000449
49. Blankers M, Van Emmerik A, Richters B, Dekker J. Blended internet care for patients with severe mental illnesses: an open label prospective controlled cohort pilot study. Internet Interventions. (2016) 5:51–5. doi: 10.1016/j.invent.2016.07.004
50. Nugter MA, Engelsbel F, Bähler M, Keet R, Van Veldhuizen R. Outcomes of FLEXIBLE assertive community treatment (FACT) implementation: a prospective real life study. Community Ment Health J. (2016) 52:898–907. doi: 10.1007/s10597-015-9831-2
51. Clausen H, Ruud T, Odden S, Benth J, Heiervang KS, Stuen HK, et al. Improved rehabilitation outcomes for persons with and without problematic substance use after 2 years with assertive community treatment-a prospective study of patients with severe mental illness in 12 Norwegian ACT Teams. Front Psychiatry. (2020) 11:607071. doi: 10.3389/fpsyt.2020.607071
52. Vidal S, Perroud N, Correa L, Huguelet P. Assertive community programs for patients with severe mental disorders: are benefits sustained after discharge? Community Ment Health J. (2020) 56:559–67. doi: 10.1007/s10597-019-00513-6
53. Incedere A, Yildiz M. Case management for individuals with severe mental illness: outcomes of a 24-month practice. Turk Psikiyatri Derg. (2019) 30:245–52. doi: 10.5080/u23532
54. Klodnick VV, Malina C, Fagan MA, Johnson RP, Brenits A, Zeidner E, et al. Meeting the developmental needs of young adults diagnosed with serious mental health challenges: the emerge model. J Behav Health Serv Res. (2021) 48:77–92. doi: 10.1007/s11414-020-09699-0
55. Hancock N, Scanlan JN, Gillespie JA, Smith-Merry J, Yen I. Partners in Recovery program evaluation: changes in unmet needs and recovery. Austral Health Rev. (2018) 42:445–52. doi: 10.1071/AH17004
56. Isaacs AN, Sutton K, Dalziel K, Maybery D. Outcomes of a care coordinated service model for persons with severe and persistent mental illness: a qualitative study. Int J Soc Psychiatry. (2017) 63:40–7. doi: 10.1177/0020764016678014
57. Banfield M, Forbes O. Health and social care coordination for severe and persistent mental illness in Australia: a mixed methods evaluation of experiences with the Partners in Recovery Program. Int J Ment Health Syst. (2018) 12:13. doi: 10.1186/s13033-018-0194-2
58. Parker S, Wyder M, Pommeranz M, Newman E, Meurk C, Dark F. Consumer experiences of community-based residential mental health rehabilitation for severe and persistent mental illness: a pragmatic grounded theory analysis. Int J Ment Health Nurs. (2021) 30:733–46. doi: 10.1111/inm.12842
59. Rees EF, Ennals P, Fossey E. Implementing an action over inertia group program in community residential rehabilitation services: group participant and facilitator perspectives. Front Psychiatry. (2021) 12:624803. doi: 10.3389/fpsyt.2021.624803
60. Parker S, Arnautovska U, Siskind D, Dark F, Mckeon G, Korman N, et al. Community-care unit model of residential mental health rehabilitation services in Queensland, Australia: predicting outcomes of consumers 1-year post discharge. Epidemiol Psychiatr Sci. (2020) 29:e109. doi: 10.1017/S2045796020000207
61. Thomas KA, Rickwood DJ, Brown PM. Symptoms, functioning and quality of life after treatment in a residential sub-acute mental health service in Australia. Health Soc Care Community. (2017) 25:243–54. doi: 10.1111/hsc.12301
62. Nibbio G, Barlati S, Cacciani P, Corsini P, Mosca A, Ceraso A, et al. Evidence-based integrated intervention in patients with schizophrenia: a pilot study of feasibility and effectiveness in a real-world rehabilitation setting. Int J Environ Res Public Health. (2020) 17:103352. doi: 10.3390/ijerph,17103352
63. Sanches SA, Swildens WE, Schaefer B, Moerbeek M, Feenstra TL, Van Asselt ADI, et al. Effectiveness of the Boston University approach to psychiatric rehabilitation in improving social participation in people with severe mental illnesses: a randomized controlled trial. Front Psychiatry. (2020) 11:571640. doi: 10.3389/fpsyt.2020.571640
64. Markiewicz R, Markiewicz-Gospodarek A, Dobrowolska B, Łoza B. Improving clinical, cognitive, and psychosocial dysfunctions in patients with schizophrenia: a neurofeedback randomized control trial. Neural Plasticity. (2021) 2021:4488664. doi: 10.1155/2021/4488664
65. Heatherington L, Bonner BL, Rosenberg D, Patterson RD, Linsley J. Sustaining outcomes research in residential treatment: a 15-year study of the Gould Farm program. Psychol Serv. (2019) 16:675–86. doi: 10.1037/ser0000253
66. Kidd SA, Mutschler C, Lichtenstein S, Yan S, Virdee G, Blair F, et al. Randomized trial of a brief peer support intervention for individuals with schizophrenia transitioning from hospital to community. Schizophr Res. (2021) 231:214–20. doi: 10.1016/j.schres.2021.03.019
67. Agrest M, Le PD, Yang LH, Mascayano F, Alves-Nishioka S, Dev S, et al. Implementing a community-based task-shifting psychosocial intervention for individuals with psychosis in Chile: perspectives from users. Int J Soc Psychiatry. (2019) 65:38–45. doi: 10.1177/0020764018815204
68. Varga E, Endre S, Bugya T, Tényi T, Herold R. A community-based psychosocial treatment has an impact on social processing and functional outcome in schizophrenia. Front Psychiatry. (2018) 9:247. doi: 10.3389/fpsyt.2018.00247
69. Salzer MS, Rogers J, Salandra N, O'callaghan C, Fulton F, Balletta AA, et al. Effectiveness of peer-delivered Center for Independent Living supports for individuals with psychiatric disabilities: a randomized, controlled trial. Psychiatric Rehabil J. (2016) 39:239–47. doi: 10.1037/prj0000220
70. Agner J, Barile JP, Botero A, Cha T, Herrera N, Kakau TM, et al. Understanding the role of mental health clubhouses in promoting wellness and health equity using Pilinahā-an Indigenous framework for health. Am J Community Psychol. (2020) 66:290–301. doi: 10.1002/ajcp.12457
71. Pernice FM, Price MH, Rice K. Why we come: clubhouse members seek connection, purpose and meaning. Community Ment Health J. (2021) 57:446–56. doi: 10.1007/s10597-020-00685-6
72. Gumber S, Stein CH. Beyond these walls: Can psychosocial clubhouses promote the social integration of adults with serious mental illness in the community? Psychiatr Rehabil J. (2018) 41:29–38. doi: 10.1037/prj0000262
73. Dunt DR, Day SE, Collister L, Fogerty B, Frankish R, Castle DJ, et al. Evaluation of a Housing First programme for people from the public mental health sector with severe and persistent mental illnesses and precarious housing: Housing, health and service use outcomes. Austr N Zeal J Psychiatry. (2022) 56:281–91. doi: 10.1177/00048674211011702
74. Mejia-Lancheros C, Lachaud J, Aubry T, Wiens K, O'campo P, Stergiopoulos V, et al. Multi-trajectory group profiles of well-being and associated predictors among adults experiencing homelessness and mental illness: findings from the At Home/Chez Soi study, Toronto site. Soc Psychiatry Psychiatric Epidemiol. (2022) 57:67–81. doi: 10.1007/s00127-021-02093-x
75. Somers JM, Moniruzzaman A, Patterson M, Currie L, Rezansoff SN, Palepu A, et al. A randomized trial examining housing first in congregate and scattered site formats. PLoS ONE. (2017) 12:e0168745. doi: 10.1371/journal.pone.0168745
76. Rhenter P, Moreau D, Laval C, Mantovani J, Albisson A, Suderie G, et al. Bread and shoulders: reversing the downward spiral, a qualitative analyses of the effects of a housing first-type program in France. Int J Environ Res Public Health. (2018) 15:30520. doi: 10.3390/ijerph15030520
77. Bitter N, Roeg D, Van Assen M, Van Nieuwenhuizen C, Van Weeghel J. How effective is the comprehensive approach to rehabilitation (CARe) methodology? A cluster randomized controlled trial. BMC Psychiatry. (2017) 17:396. doi: 10.1186/s12888-017-1565-y
78. Zarchev M, Mulder CL, Henrichs J, Roeg DPK, Bogaerts S, Van Weeghel J, et al. Victimisation of individuals with serious mental illness living in sheltered housing: differential impact of risk factors related to clinical and demographic characteristics. BJPsych Open. (2021) 7:e97. doi: 10.1192/bjo.2021.57
79. Bochicchio L, Stefancic A, McTavish C, Tuda D, Cabassa LJ. “Being there” vs “being direct:” perspectives of persons with serious mental illness on receiving support with physical health from peer and non-peer providers. Adm Policy Ment Health. (2021) 48:539–50. doi: 10.1007/s10488-020-01098-z
80. Miles A, Crosse C, Jenkins Z, Morgan P, Fossey E, Harvey C, et al. Improving cognitive skills for people with mental illness to increase vocational and psychosocial outcomes: the employ your mind program. J Psychosoc Rehabil Mental Health. (2021) 8:287–97. doi: 10.1007/s40737-021-00225-9
81. Christensen TN, Wallstrøm IG, Stenager E, Bojesen AB, Gluud C, Nordentoft M, et al. Effects of individual placement and support supplemented with cognitive remediation and work-focused social skills training for people with severe mental illness: a randomized clinical trial. J Am Med Assoc Psychiatry. (2019) 76:1232–40. doi: 10.1001/jamapsychiatry.2019.2291
82. Gammelgaard I, Christensen TN, Eplov LF, Jensen SB, Stenager E, Petersen KS. 'I have potential': Experiences of recovery in the individual placement and support intervention. Int J Soc Psychiatry. (2017) 63:400–6. doi: 10.1177/0020764017708801
83. Gal G, Shadmi E, Hoter-Ishay G, Gelkopf M, Roe D. Comparing outcome measures of persons with severe mental illness in vocational rehabilitation programs: a dual perspective of consumers and providers. Int J Qual Health Care. (2022) 34:ii105–11. doi: 10.1093/intqhc/mzaa030
84. Rodríguez Pulido F, Caballero Estebaranz N, González Dávila E, Melián Cartaya MJ. Cognitive remediation to improve the vocational outcomes of people with severe mental illness. Neuropsychol Rehabil. (2019) 31:293–315. doi: 10.1080/09602011.2019.1692671
85. Schneider J, Akhtar A, Boycott N, Guo B, Latimer E, Cao Z, et al. Individual placement and support versus individual placement and support enhanced with work-focused cognitive behaviour therapy: feasibility study for a randomised controlled trial. Br J Occup Therapy. (2016) 79:257–69. doi: 10.1177/0308022615619184
86. McGurk SR, Mueser KT, Xie H, Feldman K, Shaya Y, Klein L, et al. Cognitive remediation for vocational rehabilitation nonresponders. Schizophr Res. (2016) 175:48–56. doi: 10.1016/j.schres.2016.04.045
87. Twamley EW, Thomas KR, Burton CZ, Vella L, Jeste DV, Heaton RK, et al. Compensatory cognitive training for people with severe mental illnesses in supported employment: a randomized controlled trial. Schizophr Res. (2019) 203:41–8. doi: 10.1016/j.schres.2017.08.005
88. Schwarzer R, Jerusalem M, Weinman J, Wright S, Johnston M. Generalized self-efficacy scale. Measur Health Psychol. (1995) 1995:t00393. doi: 10.1037/t00393-000
89. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. Washington, DC: American Psychiatric Association (1994).
90. Cutrona C, Russell D. The Provisions of Social Relationships and Adaptation to Stress. In: Jones WH, Perlman D, editors. Advances in Personal Relationships. JAI Press (1983).
91. Segal S, Aviram U. The Mentally Ill in Community Based Sheltered-Care: A Study of Community Care and Social Integration (Preface+ Chapter Sixteen). New York, NY: John Wiley & Sons (1978).
92. Yildiz M, Kiras F, Incedere A, Esen D, Gürcan M, Abut B, et al. Development of social functioning assessment scale for people with schizophrenia: validity and reliability study. Anatolian J Psychiatry. (2018) 1:2374. doi: 10.5455/apd.2374
93. Mueser KT, Meyer PS, Penn DL, Clancy R, Clancy DM, Salyers MP. The Illness Management and Recovery program: rationale, development, and preliminary findings. Schizophr Bull. (2006) 32(Suppl. 1):S3243. doi: 10.1093/schbul/sbl022
94. Maples NJ, Velligan DI. Cognitive adaptation training: establishing environmental supports to bypass cognitive deficits and improve functional outcomes. Am J Psychiatr Rehabil. (2008) 11:164–80. doi: 10.1080/15487760801963686
95. Dieterich M, Irving CB, Bergman H, Khokhar MA, Park B, Marshall M. Intensive case management for severe mental illness. Cochr Datab Systemat Rev. (2017) 1:CD007906. doi: 10.1002/14651858.CD007906.pub3
96. Modini M, Joyce S, Mykletun A, Christensen H, Bryant RA, Mitchell PB, et al. The mental health benefits of employment: results of a systematic meta-review. Australasian Psychiatry. (2016) 24:331–6. doi: 10.1177/1039856215618523
97. Rog DJ, Marshall T, Dougherty RH, George P, Daniels AS, Ghose SS, et al. Permanent supportive housing: assessing the evidence. Psychiatr Serv. (2014) 65:287–94. doi: 10.1176/appi.ps.201300261
98. Stein LI, Test MA. Alternative to mental hospital treatment. I. Conceptual model, treatment program, and clinical evaluation. Archiv General Psychiatry. (1980) 37:392–7. doi: 10.1001/archpsyc.1980.01780170034003
99. Mueser KT, Bond GR, Drake RE, Resnick SG. Models of community care for severe mental illness: a review of research on case management. Schizophr Bull. (1998) 24:37–74. doi: 10.1093/oxfordjournals.schbul.a033314
100. Hancock N, Scanlan JN, Honey A, Bundy AC, O'Shea K. Recovery Assessment Scale – Domains and Stages (RAS-DS): its feasibility and outcome measurement capacity. Austral N Zeal J Psychiatry. (2015) 49:624–33. doi: 10.1177/0004867414564084
101. Barbic SP, Kidd SA, Durisko ZT, Yachouh R, Rathitharan G, McKenzie K. What are the personal recovery needs of community-dwelling individuals with mental illness? Preliminary findings from the canadian personal recovery outcome measurement (C-PROM) study. Can J Commun Mental Health. (2018) 37:29–47. doi: 10.7870/cjcmh-2018-005
102. Wong S, Haggerty J. Measuring Patient Experiences in Primary Health Care a Review and Classification of Items and Scales Used in Publicly-Available Questionnaires. Vancouver (2013).
103. Bullock W. The mental health recovery measure. In: T Campbell-Orde, JCJ Chamberlin, and HS Leff, editors, Measuring the Promise of Recovery: A Compendium of Recovery Measures. Volume II. Cambridge: The Evaluation Center@HSRI (2005).
104. Neil S, Kilbride M, Pitt L, Nothard S, Welford M, Sellwood W, et al. The questionnaire about the process of recovery (QPR): a measurement tool developed in collaboration with service users. Psychosis. (2009) 1:145–55. doi: 10.1080/17522430902913450
105. Jones S, Mulligan LD, Higginson S, Dunn G, Morrison AP. The bipolar recovery questionnaire: psychometric properties of a quantitative measure of recovery experiences in bipolar disorder. J Affect Disord. (2013) 147:34–43. doi: 10.1016/j.jad.2012.10.003
106. Morgan VA, Waterreus A, Jablensky A, MacKinnon A, Mcgrath JJ, Carr V, et al. People living with psychotic illness in 2010: the second Australian national survey of psychosis. Austr N Zeal J Psychiatry. (2012) 46:735–52. doi: 10.1177/0004867412449877
107. Poon A, Hayes L, Harvey C. Caregiving by people with psychotic disorders in the second Australian prevalence study of psychosis. Health Soc Care Commun. (2019) 27:1042–52. doi: 10.1111/hsc.12721
108. Fossey EM, Harvey CA. Finding and sustaining employment: a qualitative meta-synthesis of mental health consumer views. Can J Occup Therapy. (2010) 77:303–14. doi: 10.1177/000841741007700501
109. Barratt H, Rojas-García A, Clarke K, Moore A, Whittington C, Stockton S, et al. epidemiology of mental health attendances at emergency departments: systematic review and meta-analysis. PLoS ONE. (2016) 11:e0154449. doi: 10.1371/journal.pone.0154449
110. Rosen A, Rosen T, McGorry P. The human rights of people with severe and persistent mental illness: can conflicts between dominant and non-dominant paradigms be reconciled? In: M Dudley, F Gale, and D Silove, editors, Mental Health and Human Rights: Vision, Praxis, and Courage. Oxford: Oxford University Press (2012). p. 19.
111. Faulkner A. Survivor research and Mad Studies: the role and value of experiential knowledge in mental health research. Disabil Soc. (2017) 32:500–20. doi: 10.1080/09687599.2017.1302320
112. Slade M, Amering M, Farkas M, Hamilton B, O'Hagan M, Panther G, et al. Uses and abuses of recovery: implementing recovery-oriented practices in mental health systems. World Psychiatry. (2014) 13:12–20. doi: 10.1002/wps.20084
113. Brophy L, Hodges C, Halloran K, Grigg M, Swift M. Impact of care coordination on Australia's mental health service delivery system. Austr Health Rev. (2014) 38:396–400. doi: 10.1071/AH13181
114. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. (2009) 4:50. doi: 10.1186/1748-5908-4-50
115. Starling A. Implementing new models of care: lessons from the new care models programme in England. Int J Care Coordinat. (2018) 21:50–4. doi: 10.1177/2053434518770613
116. McKenzie K, Smith-Merry J. Responding to complexity in the context of the national disability insurance scheme. Soc Pol Soc. (2023) 22:139–54. doi: 10.1017/S1474746422000562
117. Lemaster JW. PPIE in intervention studies: randomized trials and clinical quality improvement. Health Expectationsat. (2020) 23:1–2. doi: 10.1111/hex.13009
118. Allen D, Cree L, Dawson P, El Naggar S, Gibbons B, Gibson J, et al. Exploring patient and public involvement (PPI) and co-production approaches in mental health research: learning from the PARTNERS2 research programme. Res Involv Engagem. (2020) 6:56. doi: 10.1186/s40900-020-00224-3
119. Castelein S, Timmerman ME, Van Der Gaag M, Visser E. Clinical, societal and personal recovery in schizophrenia spectrum disorders across time: states and annual transitions. Br J Psychiatry. (2021) 219:401–8. doi: 10.1192/bjp.2021.48
120. Allott K, Steele P, Boyer F, De Winter A, Bryce S, Alvarez-Jimenez M, et al. Cognitive strengths-based assessment and intervention in first-episode psychosis: a complementary approach to addressing functional recovery? Clin Psychol Rev. (2020) 79:101871. doi: 10.1016/j.cpr.2020.101871
121. World Health Organization. Human Rights: WHO QualityRights Core Training—for All Services and All People: Course Slides. Geneva: World Health Organization (2019).
Keywords: recovery, complex, mental illness, models of care, community
Citation: Harvey C, Zirnsak T-M, Brasier C, Ennals P, Fletcher J, Hamilton B, Killaspy H, McKenzie P, Kennedy H and Brophy L (2023) Community-based models of care facilitating the recovery of people living with persistent and complex mental health needs: a systematic review and narrative synthesis. Front. Psychiatry 14:1259944. doi: 10.3389/fpsyt.2023.1259944
Received: 17 July 2023; Accepted: 23 August 2023;
Published: 14 September 2023.
Edited by:
Antonio Vita, University of Brescia, ItalyReviewed by:
Armida Mucci, University of Campania Luigi Vanvitelli, ItalyPasquale Scognamiglio, ASL Napoli 3 Sud, Italy
Copyright © 2023 Harvey, Zirnsak, Brasier, Ennals, Fletcher, Hamilton, Killaspy, McKenzie, Kennedy and Brophy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tessa-May Zirnsak, dC56aXJuc2FrQGxhdHJvYmUuZWR1LmF1
 Carol Harvey
Carol Harvey Tessa-May Zirnsak
Tessa-May Zirnsak Catherine Brasier
Catherine Brasier Priscilla Ennals
Priscilla Ennals Justine Fletcher
Justine Fletcher Bridget Hamilton
Bridget Hamilton Helen Killaspy
Helen Killaspy Peter McKenzie9
Peter McKenzie9 Hamilton Kennedy
Hamilton Kennedy Lisa Brophy
Lisa Brophy