- 13rd Department of Psychiatry, School of Medicine, Aristotle University of Thessaloniki Greece, Thessaloniki, Greece
- 2WHO Collaboration Center for Quality in Mental Health, Aristotle University of Thessaloniki, Thessaloniki, Greece
- 3Academic Affairs Division, Faculty of Education, Universiti Teknologi MARA, Sungai Buloh, Selangor, Malaysia
- 4Department of Psychiatry and Psychological Medicine, University Hospital Centre Zagreb, Zagreb, Croatia
- 5Faculty of Medicine, Medical University of Sofia, Sofia, Bulgaria
- 6Department of Psychiatry and Psychotherapy, Semmelweis University, Budapest, Hungary
- 7Clinic of Psychiatry, Medical Faculty, Institute of Clinical Medicine, Vilnius University, Vilnius, Lithuania
- 8School of Medicine, University of Zagreb, Zagreb, Croatia
- 9Department of Clinical Psychology, Semmelweis University, Budapest, Hungary
- 10Symbiosis Centre for Emotional Wellbeing, Symbiosis International (Deemed) University, Pune, India
- 11Faculty of Medicine, School of Health Sciences, Aristotle University of Thessaloniki, Thessaloniki, Greece
- 12Department of Mental Health, University of Abuja Teaching Hospital, Abuja, Nigeria
- 13David Tvildiani Medical University, Tbilisi, Georgia
- 14School of Social Sciences, Hellenic Open University, Patras, Greece
- 15Department of Internal Medicine, Nicosia General Hospital, Nicosia, Cyprus
- 16Education Center, Mental-Health Clinic No. 1 n.a. N.A. Alexeev of Moscow Healthcare Department, Moscow, Russia
- 17Faculty of Medicine, Riga Stradins University, Riga, Latvia
- 18Department of Psychiatry, Faculty of Medicine, Universiti Teknologi MARA, Sungai Buloh, Selangor, Malaysia
- 19Department of Psychiatry, Samara State Medical University, Samara, Russia
- 20Second Psychiatric Clinic, University Hospital for Active Treatment in Neurology and Psychiatry “Saint Naum”, Sofia, Bulgaria
- 21Department of Psychiatry, Bayero University, Kano, Nigeria
- 22Aminu Kano Teaching Hospital, Kano, Nigeria
- 23Georgian Medical Students' Association, Tbilisi, Georgia
- 24Department of Psychiatry and Narcology, Riga Stradins University, Riga, Latvia
- 25Institute of Public Health, Riga Stradins University, Riga, Latvia
- 26Riga Centre of Psychiatry and Narcology, Riga, Latvia
- 27Institute of Applied Health Research, University of Birmingham, Birmingham, United Kingdom
- 28Warwick Medical School, University of Warwick, Coventry, United Kingdom
- 29Pakistan Psychiatric Research Centre, Fountain House, Lahore, Pakistan
- 30Health Policy, WHO Regional Office for Europe, Copenhagen, Denmark
- 31WHO Athens Quality of Care Office, WHO Regional Office for Europe, Copenhagen, Denmark
- 32International Centre for Education and Research in Neuropsychiatry, Samara State Medical University, Samara, Russia
Introduction: The aim of the study was to search rates of depression and mental health in university students, during the COVID-19 pandemic.
Materials and methods: This is an observational cross-sectional study. A protocol gathering sociodemographic variables as well as depression, anxiety and suicidality and conspiracism was assembled, and data were collected anonymously and online from April 2020 through March 2021. The sample included 12,488 subjects from 11 countries, of whom 9,026 were females (72.2%; aged 21.11 ± 2.53), 3,329 males (26.65%; aged 21.61 ± 2.81) and 133 “non-binary gender” (1.06%; aged 21.02 ± 2.98). The analysis included chi-square tests, correlation analysis, ANCOVA, multiple forward stepwise linear regression analysis and Relative Risk ratios.
Results: Dysphoria was present in 15.66% and probable depression in 25.81% of the total study sample. More than half reported increase in anxiety and depression and 6.34% in suicidality, while lifestyle changes were significant. The model developed explained 18.4% of the development of depression. Believing in conspiracy theories manifested a complex effect. Close to 25% was believing that the vaccines include a chip and almost 40% suggested that facemask wearing could be a method of socio-political control. Conspiracism was related to current depression but not to history of mental disorders.
Discussion: The current study reports that students are at high risk for depression during the COVID-19 pandemic and identified specific risk factors. It also suggested a role of believing in conspiracy theories. Further research is important, as it is targeted intervention in students' groups that are vulnerable both concerning mental health and conspiracism.
Introduction
University students' mental health constitutes an area of special interest. This group is considered to belong to vulnerable groups and one reason is young age (1) but also the fact that any disruption during of the studies has deep long-term effects, plus that their personality is not mature enough to deal with additional stress (2, 3).
On top of these, the COVID-19 outbreak caused significant disruption in university studies, resulting in an enduring change in the academic environment, which is expected to lead to the emergence of feelings of fear and worry in the students population. The above should be considered in the frame of an extreme threat to the community as well as the individual. Additionally, expecting an economic crisis resulting in future unemployment, in combination with changes at present in social behavior, routine and daily habits, impose further stress.
Even during the pre-pandemic period, reports were suggesting that the rate of probable depression among university students is >20% while suicidal thoughts are also unexpectedly high and above 10% (1, 4). Concerning the mental health of students during the pandemic, a lot of published empirical data exist (5–11), but the literature is also overwhelmed with papers reflecting opinions or viewpoints and perspectives, including narrations as well as guidelines of how to cope with the pandemic. All utilize previous experience from pandemics of the past and also utilize common sense. The result is that they often obscure rather than clarify matters. Within the scope of precision and personalized psychiatry, an important goal is to identify specific variables and their exact contribution, including the belief in conspiracy theories which has been shown to exert a complex effect on mental health during the pandemic (7, 12, 13).
A recent meta-analysis of ~1.5 million students altogether (6) reported that the prevalence of anxiety was 32%, of depressive symptoms was 34%, and of sleep disturbances was 33%. These authors concluded that their results are indicative of an increase in these symptoms during the pandemic, despite of the similar findings by meta-analysis of data from before the pandemic (14). Deng et al. (6) argued that their findings should be considered as reflecting an increase because they were based mainly on studies on Chinese students, who are expected to manifest lower baseline rates of these symptoms. A second smaller meta-analysis reported similar results (5, 7).
The aim of current study was to calculate the rate of probable depression and its determinants in the population of university students in eleven countries Bulgaria, Croatia, Georgia, Greece, Hungary, India, Latvia, Lithuania, Malaysia, Nigeria and Russia during the COVID-19 outbreak. Secondary aims were to investigate the changes in distress, anxiety, and suicidal ideation as well as the role of conspiracism. The paper conforms with the STROBE statement for the reporting of observational studies and the respected checklist is included in the Webappendix (15).
Material and methods
Method
To assess the primary objective and rate depression, the self-report CES-D scale was used. According to a previously developed method (7, 16, 17) the cut-off score of 23/24 for the CES-D and a derived algorithm were used to identify cases of probable depression. This algorithm utilized the weighted scores of selected CES-D items to arrive at the diagnosis of depression, and has already been validated. Cases identified by only either method were considered cases of distress (false positive cases in terms of depression), while cases identified by both the cut-off and the algorithm were considered as probable depression. The STAI-S (18) and the RASS (17) were used to assess anxiety and suicidality respectively.
The protocol also included the collection of sociodemographic data and previous mental and somatic health history. A long questionnaire concerning beliefs in conspiracy theories was also utilized.
The data were collected online and anonymously from April 2020 through March 2021, covering periods of full implementation of lockdowns as well as of relaxations of measures in countries around the world. Announcements and advertisements were made on social media and through news sites, but no other organized effort had been undertaken. The first page included a declaration of consent which everybody accepted by continuing with the participation. Filling of all fields was obligatory to avoid the problem of missing data.
The complete protocol used is available in the Webappendix; each question was given an ID code; these ID codes were used throughout the results for increased accuracy.
Approval was initially given by the Ethics Committee of the Faculty of Medicine, Aristotle University of Thessaloniki, Greece, and locally concerning each participating country.
Material
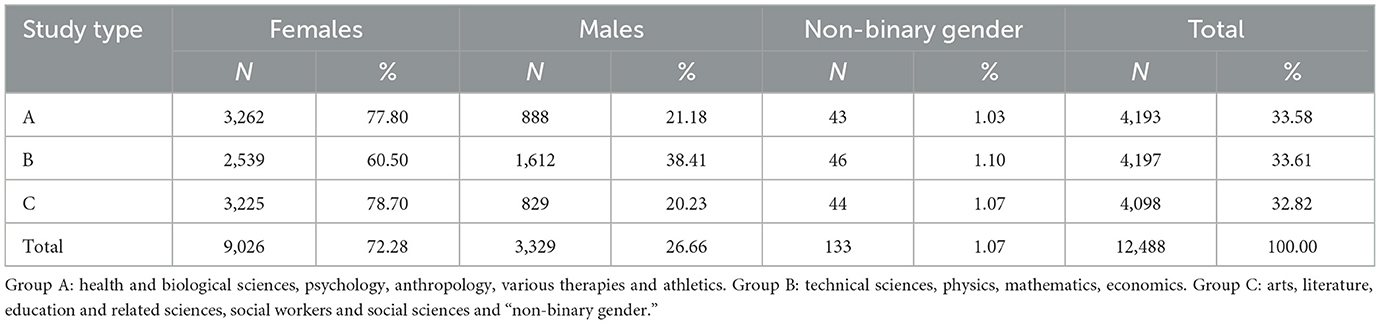
Eleven countries (Bulgaria, Croatia, Georgia, Greece, Hungary, India, Latvia, Lithuania, Malaysia, Nigeria, and Russia) participated in the study, and data from 13,354 persons were initially gathered. Only data from those aged between 17 and 30 years were kept and thus, the sample included 12,488 subjects, of whom 9,026 were females (72.27 %; aged 21.11 ± 2.53), 3,329 males (26.65%; aged 21.61 ± 2.81) and 133 “non-binary gender” (1.06%; aged 21.02 ± 2.98). The sample composition in terms of country of origin (A1) by sex (A2) and of the field of studies (A8) is shown in WebTables 1, 2. Subjects were classified, depending on their studies, into three groups: group A (health and biological sciences), group B (technical sciences), and group C (arts, literature, education and related sciences). Psychology, anthropology, various therapies, and athletics were included in group A, Economics in group B, social workers, and social sciences in group C. The size and composition of each group are shown in Table 1 and WebTable 2. Each of the three groups accounted for roughly one-third of the study sample with the percentage of males being double in group B in comparison to groups A and C.
The fact that the majority were females reflects a common phenomenon in this kind of studies with online gathering of data and self-selection of participation. This means that results should be calculated separately for males and females.
The study population was self-selected. It was not possible to apply post-stratification on the sample as it was done in a previous study (7), because this would mean that we would utilize a similar methodology across much different countries and the population data needed were not available for all. There was no a-priori calculation of the sample size.
Statistical analysis
The analysis of data included the following:
• Descriptive tables were created for the variables under investigation.
• Chi-square tests were used for the comparison of frequencies when categorical variables were present and for the post-hoc analysis of the results a Bonferroni-corrected method of pair-wise comparisons was utilized (19).
• Pearson Product Moment Correlation Coefficient (R) to investigate the relationship between variables
• Analysis of Covariance (ANCOVA) was used to test for the main effect as well as the interaction among categorical variables, with Schefee as post hoc test to investigate which variables could contribute to the development of others.
• Multiple forward stepwise linear regression analysis (MFSLRA) was performed to investigate which variables could function as predictors and contribute to the development of others (e.g., depression).
• Relative Risk (RR) was calculated as the ratio of the incidence in two groups under comparison.
The way each of the above methods was utilized is described specifically in the Results Section.
There were no missing data since the filling of all questionnaire fields was obligatory.
Results
Description of the study sample
Demographics
The composition of the study sample is described in the “Material” Section and Table 1 and WebTables 1, 2. Additionally, 10.05% of the study sample were suffering from a chronic medical condition (B2) and 54.58% of them had a person belonging to a vulnerable group in the family (B4).
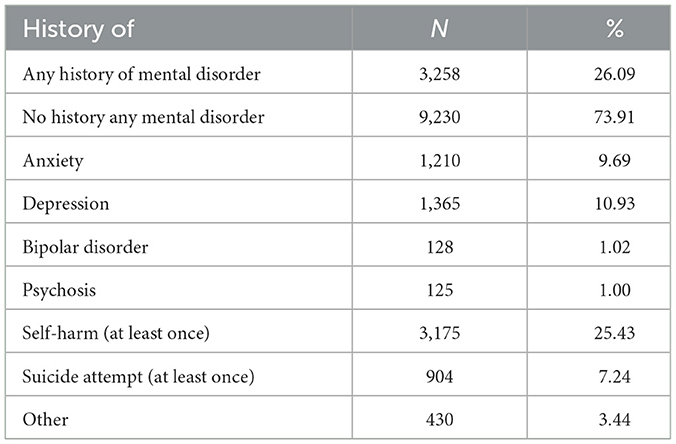
History of mental health (B5, O12, O13)
The detailed mental health history is shown in Table 2 and Webtables 4–6. Any such history was reported by 3,258 subjects (26.09%; B5). The lowest rate was observed in males of study type C and the highest in “non-binary gender” of study type A. Anxiety ranged from 4.95% (in males of type C studies) to 13.95% (in “non-binary gender” of study type A) and 13.27% (in females of study type C). Depression ranged from 7.96% (in males of type C studies) to 22.73% (in “non-binary gender” of study type C).
History of self-injury (at least once; O12) was present in 25.43% with the highest rate in “non-binary gender” in type C studies (47.73%) and the lowest in males in type B studies (17.87%). Suicidal attempt (at least once; O13) was reported by 7.24%, with the highest rate reported by “non-binary gender” in study type A (25.58%) and the lowest in males of type C studies (5.55%).
The rate of females to males for a history of any mental disorders was 1.5:1 and the rate of “non-binary gender” was 1.48 vs. females and 2.22 vs. males.
Chi-square tests suggested that females had higher rates of self-injury and suicidal attempts (both p < 0.01), while the interaction of sex and type of studies produced more complex results. In females, subjects in type C had more self-injuries and in males, this was true for males of type A. The above suggests that the ranking of types of studies in terms of the history of self-injury (C > A > B) is driven by females in group C and males in group A. Concerning suicidal attempts, in females there were lower rates in type B while there were no differences among types of studies for males. The above suggest that the ranking of types of studies in terms of history of suicidal attempt (B < A = C) is driven by females in group B (see Appendix for details, section 3.2).
Current probable depression
Probable depression was found in 29.19% of females and 16.10% of males (25.81% of the total sample) and dysphoria was present in an additional 16.10% of females and 14.29% of males (15.66% of the total sample). The detailed results are shown in Webtables 7–11.
There was a large difference among countries in terms of current probable depression with the lowest rate observed in Nigeria (4.94%) and the highest in Lithuania (43.88%).
The RR for depression was 1.81 for females in comparison to males. Rates of depression were higher for “non-binary gender” in type of study B (46.67%) and lowest for males in A and C (15.99% and 15.92%).
Chi-square test revealed an effect of type of studies by gender concerning probable depression. There was a difference among females in the three types (chi-square = 21.623, df = 2, p < 0.001), which was due to A vs. B (chi-square = 16.947, df = 1, p < 0.001), A vs. C (chi-square = 15.241, df = 1, p < 0.001), but not B vs. C (chi-square = 0.194, df = 1, p = 0.659). Concerning males, there was no difference among males in the three types (chi-square = 0.055, df = 2, p = 0.972). Similarly, there were no differences concerning “non-binary gender” in the three types of studies (chi-square = 1.027, df = 2, p = 0.598). These results suggest a lower depression rate in females in the A type of studies.
There was a difference among sexes (chi-square = 233.240, df = 2, p < 0.001), with males having lower rates of probable depression in comparison both to females (chi-square = 218.274, df = 1, p < 0.001), and “non-binary gender” (chi-square = 55.258, df = 1, p < 0.001), and “non-binary gender” having higher rates both to females (chi-square = 8.622, df = 1, p = 0.003) and males.
Four MSLRA were performed. The dependent variables were the change in anxiety, change in depressive feelings, change in suicidal thoughts and probable depression separately, while in all analyses the same set of independent predictors was used and it included sex (A2) split into dummy variables, age (A3), type of studies (split into dummy variables), people living with (A6), health status (B1-2), vulnerable relative (B4), history of specific mental disorders (B5 split in dummy variables), thoughts pertaining to COVID-19 fears (C1-4), the degree of lockdown (D2), satisfaction by information (D4), family issues (E1-7), conspiracy theories (J1-26) and spirituality/religiosity (P1).
The detailed results are shown in Table 3 and confirm the effect of sex, history of mental disorder, fears because of the pandemic, and believing in conspiracy theories on the mental health of students during the pandemic. The complete model which can be derived based on these MSLRA is shown in Figure 1.
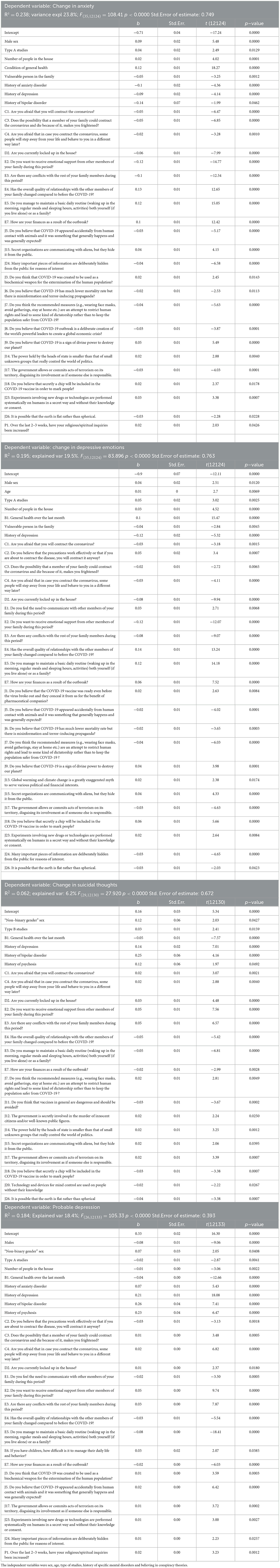
Table 3. Multiple linear stepwise regression analysis with changes in anxiety, depression, or suicidality and the presence of probable depression as dependent variables separately.
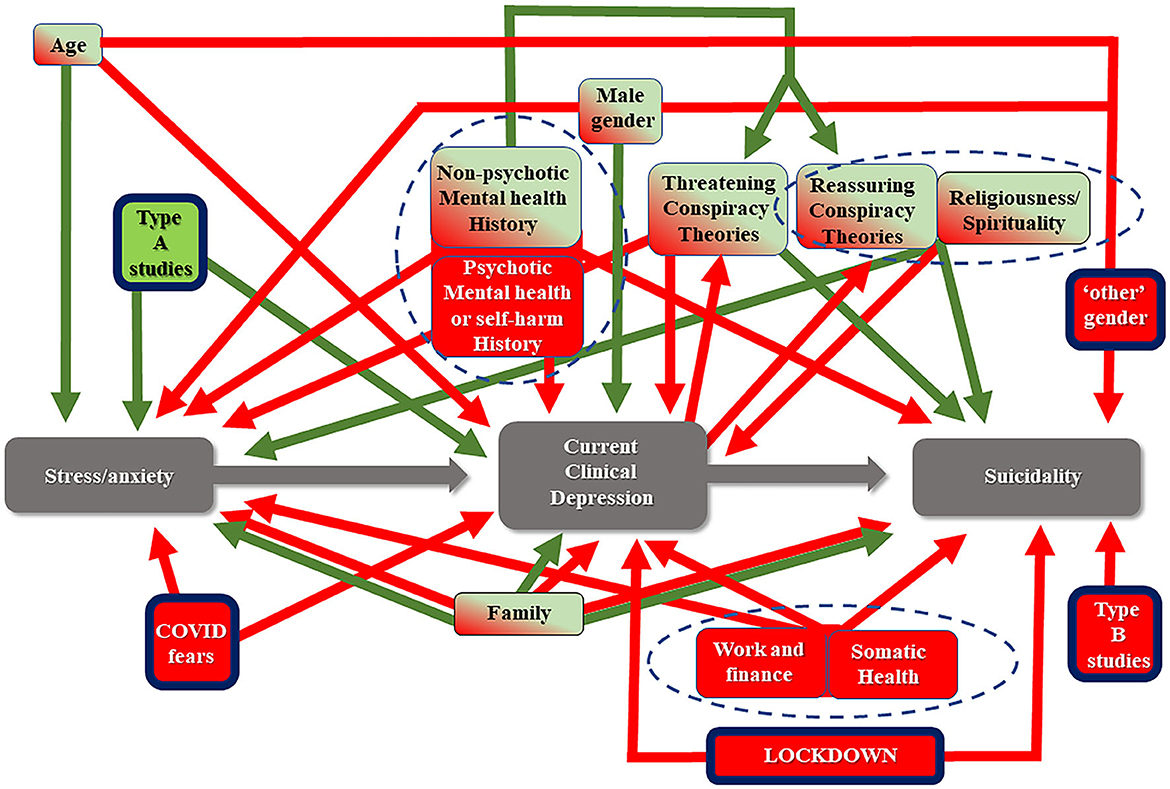
Figure 1. The developed multiple vulnerabilities model representing the mechanism through which the COVID-19 outbreak in combination a great number of factors could lead to depression through stress, and eventually to suicidality in university students. A number of variables act as risk factors (red) or as protective factors (green), while some of them change direction of action depending on the phase (green/red). Three core clusters emerge (delineated with the doted lines). The model differs from a more general model concerning the general population in that the type of studies, “non-binary gender” sex, COVID-related fears and strict lockdown specifically play an additional role (rectangles with thick black frame).
Secondary aims of the study
Current mental health
In the total study sample, increased anxiety (at least “a little”) was present in ~60% (F21), more depressive feelings (at least “a little”) in > 55% (G21); suicidal thoughts were increased (at least “a bit”) in 6.34% (O11). The detailed results are shown in Webtables 7–11.
The presence of history of any mental disorder had a RR of 2.04 for the development of depression which was highest for “non-binary gender” in the type of studies B (RR = 2.76) and lowest for females in the same type of studies (RR = 1.66). In detail the effect of history in the development of depression by sex and type of study is shown in Webtable 12. The highest rate of current probable depression was observed in females and type of studies B or C with a history of bipolar disorder (63.33% and 72.73%) or psychosis (60.71% and 61.29%). “Non-binary gender” had very high rates with any history or type of studies. The lowest rates were observed in type A studies with “other history” in females (21.67%) and males (18.18%), and also in males with a history of anxiety and type B studies (16.16%) and type C studies and “other history” (8.70%).
ANCOVA with the presence of probable depression and history of each mental disorder separately as grouping variables, and changes in anxiety, depressive feelings, and suicidal thoughts as independent variables and sex and age as covariates returned a main effect for probable depression (wilks = 0.851; F = 725.9; effect df:3; error df:12475; p < 0.001), history of anxiety (wilks = 0.995; F = 19.1; effect df:3; error df:12475; p < 0.001), depression (wilks = 0.996; F = 17.9; effect df:3; error df:12475; p < 0.001) and bipolar disorder (wilks = 0.999; F = 4.5 effect df:3; error df:12475; p = 0.004). All scheffe post-hoc tests were significant at p < 0.01. All group means pointed toward a negative change in all three independent variables reflecting a change in mental health.
In terms of suicidality, 17.63% reported that they were thinking of committing suicide (O5) with 5.97% reporting “much” or “very much.”
Family, lifestyle changes, and the pandemic
At the time of the interview, 17.11%, were under strict lockdown (D2), 41.90%, to a high degree 24.95% partially, and 16.03% were under no lockdown at all. Chi-square test in pairs among the four lockdown groups and the presence of probable depression returned no differences except for the complete lockdown which manifested significantly higher depression rates in comparison to all the other states of lockdown (31.63% 24.62%; RR = 1.28; p < 0.01). All correlations were significant (p < 0.05) but minimal among the degree of lockdown and changes in anxiety (R = −0.13), changes in depressive feelings (R = −0.14), changes in suicidal thoughts (R = 0.07), STAI (R = 0.02), CES-D (0.06), RASS-Intention (R = 0.03), RASS life (R = 0.02).
More than 50% of the total sample reported that the time spent outside the house was less than humanly necessary or worse, without any differences among types of studies. More than 90% were suggesting that they were following the precaution measures suggested by the WHO at least moderately, with 2/3 saying that they were much or very much following them. One-third felt that the information was not adequate.
Family dynamics changed toward increased emotional bonding and on average conflicts did not change. Only close to 20% did not manage to keep a basic daily routine and almost half were expecting their financial status to worsen.
More than 90% considered exercise to be of high importance during the pandemic but more persons experienced a decrease in physical activity. Eating increased in 40% and ~20% was eating in an unhealthier way. More than 30% put weight.
Half of the study sample increased the time spent on the internet and almost 2/3 increased the use of social media. Close to 25% acquired new internet habits.
Sleep worsened in ~45% with more than 50% going to sleep rather late and 20% having nightmares. Smoking increased in 25%, alcohol use in close to 40%, and illegal substance use in 25%. Sexual life was poor in ~45% with a decrease in desire in ~20%.
These findings were comparable across types of studies (WebTable 13).
Beliefs in conspiracy theories
The rates of the beliefs in conspiracy theories depended on the nature of the belief, with more bizarre theories enjoying lower acceptance. Differences among countries were significant, but there were no overall differences among the sexes. Interestingly, the type A studies had surprisingly high acceptance rates of COVID-19 conspiracy theories with close to 25% believing that the vaccines include a chip and almost 40% suggesting that facemask wearing could be a method of socio-political control. One-third of persons of type A studies were reserved toward vaccines in general, 20% were accepting the chemtrail conspiracy, 20% disputed climate change, 40% were not precluding that mind control devices are used upon the population, 45% were believing that experiments of new drugs and technologies are systematically performed secretly on the population and 8% were accepting the flat earth theory. The rate of the flat earth theory adds validity to our study sample as it is comparable, although lower to that reported by other studies.
Rates of believing were lower in persons without dysphoria or depression, intermediate in those with dysphoria, and higher in those with current probable depression. There was no relationship between history of any mental disorders and conspiracism.
The results concerning conspiracy theories are shown in detail in WebTables 14–19.
Discussion
The results of the current international study on a large convenient sample, across 11 countries, probable depression was present in 25.81% with an additional 15.66% experiencing severe distress. Prior history doubled the risk of developing depression. A significant number of variables contributed to the developed model and acted either as risk or as protective factors. Altogether they explained 18.4% of the development of depression. An unfortunate finding was that the individual contribution of individual variables was very small. A quarter of these 12,488 university students manifested a history of mental disorder and ~7% had attempted at least once. The fact that the majority were females reflects a common phenomenon in this kind of studies with online gathering of data and self-selection of participation (11, 20–22). During the COVID-19 pandemic, over half of these university students reported an increase in anxiety and depressive feelings and 6.34% in suicidal thoughts. A worsening of quality of life and deterioration of lifestyle issues were also found. Conspiracy theories manifested a complex effect, and the belief in them seemed widely prevalent with acceptance rates depending on the nature of the belief, with more bizarre theories enjoying lower acceptance. Differences among countries were significant, but there were no overall differences among the sexes. Interestingly, health-related university studies had surprisingly high acceptance rates of COVID-19 conspiracy theories with close to 25% believing that the vaccines include a chip and almost 40%, suggesting that facemask wearing could be a method of socio-political control. One-third of them were reserved toward vaccines in general, 20% were accepting the chemtrail conspiracy, 20% disputed climate change, 40% were not precluding that mind control devices are used upon the population, 45% believed that experiments of new drugs and technologies are systematically performed secretly on the population and 8% were accepting the flat earth theory. Rates of believing were lower in persons without dysphoria or depression, intermediate in those with dysphoria, and higher in those with current probable depression. There was no relationship between history of any mental disorders and conspiracism.
The first question that arises from this kind of study samples (online study with self-selection) is the extent to which the conclusions are valid, and the study sample does not manifest some kind of systematic bias. The features that support the validity of the study sample are the high depression levels, even in the subgroup which was not under any kind of lockdown, the large discrepancy (which makes sense) among rates of beliefs in individual conspiracy theories, with the rate of believing in flat earth being a cardinal finding, which is more or less in accord with the reports of yougov.com (23).
The female:male ratio in terms of probable depression is another feature that supports the validity of our study sample.
The basic results of the current study are in accord with the literature, which however includes many studies that report on depressive symptoms (24), but only a few on rates of probable depression. Most of them are on medical students and so far support that during the COVID-19 outbreak, the depression rates were around 20-30% while also similar rates of anxiety were present (8–11, 21, 25–32). The overall rates probable depression reported by the current study were lower than the rates reported in the literature, and this was likely a consequence of the algorithm used and of the stringent criteria it applied. Self-injuring acts were reported in up to 40% (33). Others report that up to half of students were suffering from a mental disorder (22, 34, 35). Interestingly, some report no differences between sexes (32) but this is not the rule. There are studies in the general population concerning the role of self-determined sex (36–41). Lockdown was recognized as a strong risk factor (42), along with prior history (43). The finding that rates of depression increase significantly with strict lockdown (RR = 1.28) is in accord with other reports (26) and also point to the possibility this increase is only temporary and questions whether these rates reflect true depression or an intense adjustment reaction with depressive affect. This lockdown effect has been well documented on the general population (20, 44–48), but most results seem to suggest an enduring effect (49) which might not be in accord with our findings.
However one critical element is that the rates of probable depression in university students were reported to be high even before the pandemic (1, 4, 14, 50–71). It is therefore questionable whether the findings of the current study reflect elevated rates of depression. One finding that supports this is the relationship between these rates with the intensity of lockdown.
The multivariate analysis in the current study proposed a model for the development of depression and suicidality during the pandemic. Similar but less specific or detailed models have been proposed (72), with some authors suggesting that the increase in suicidality is limited to sexual minorities (73). The developed model (Figure 1) includes a significant number of variables. They seem to act either as risk or as protective factors. Altogethere they explain 18.4% of the phenomenon of depression development. Interestingly, the individual contribution of each variable was very small. Another finding was that conspiracism manifested a complex effect. Current probable depression acted as a risk factor for the development of such beliefs. This model starts with the assumption that stress and anxiety develop first. Depression then follows, while suicidality emerges as the end result. These are distinct stages, and the basic assumption is that there is progress from earlier to later stages, which however, is not mandatory.
In line with the proposed model, as the pandemic appeared, it exerted a severe psychological impact that resulted in severe anxiety and distress. Both were determined by several sociodemographic and interpersonal variables that included sex, age, thoughts, beliefs and fears that were specific to the outbreak and to the intensity of lockdowns, as well as to relationships among family members, the ability to keep a basic daily routine, the economic situation and its changes, the presence of mental disorder history and, most important, the fear that the person or a family member will get COVID-19 and die. The role of the type of studies was important also, with studies pertaining to health sciences being protective during the early stages while studies related to polytechnic, physics, mathematics, and related sciences being risk factors for the development of suicidality. In the literature there are reports with similar findings but the contribution of the current study is that it identified their specific contribution and developed a comprehensive model.
Conspiracism is currently widely accepted as being an important contributing factor since the literature strongly supports its relationship with anxiety and depression (74, 75), but most important is their role in the resistance against vaccination of the entire population. The high rates of believing in conspiracy theories are in accord with findings from various countries (76–79). Conspiracism and especially those beliefs regarding medicine, and health-related issues are not uncommon (80), they are widely discussed in social media (76, 81) and they challenge the capacity of the average person to distill and assess the content (82, 83). Their adverse effect on health behaviors is well-documented, and this concerns especially vaccination (78, 84–97). Some relationship might be present between believing in bizarre conspiracy theories and the presence of psychotic tendencies or of a history of psychosis (98). Our current findings did not support previous reports that particular type of studies are preferentially related to conspiracism (8, 9).
What is extremely interesting is the finding of the current study concerning the rates of believing in conspiracy theories (WebTables 14–19). For example, ~20% of medical students were believing that maybe the vaccine was ready before the COVID-19 outbreak (J1) with 5% believing it strongly. The respected rates for the 5G theory (J4) were 7% and 1.5%, while concerning the possibility of the deliberately inflated mortality rates (J6) were >20% and 6% respectively. In the same group of students, the acceptance of the chemtrails conspiracy (J10) was 7% and close to 2% and that a chip will be included in the vaccines (J18) was 9% and >2% respectively. The vaccines in general were considered as dangerous (J11) by >11% and 1.77% while astonishingly, the flat earth theory (J26) was embraced by close to 5.5% and 1.5% of medical students respectively with an additional 2.8% not precluding it! Reserved toward vaccination in general were ~25% of medical students. Measures including facemask wearing were considered to be rather an attempt of socio-political control (J7) by 15% and >3% respectively, while only 72% precluded this idea. All these rates were much higher in students of nursing. These results are generally in accord with the yougov.com reports (23) and explain the resistance to measures and especially to vaccination by a minority of doctors and other health professionals.
Current probable depression is a critical factor related to conspiracism. As correlation does not imply causation, conspiracism could be any of the following: the cause of depression, a copying mechanism, or a marker of maladaptive psychological patterns of cognitive appraisal. The authors suggest that the most likely explanation is that conspiracism is probably a coping mechanism against stress and concerns the entire general population (75, 99, 100).
A question that is difficult-to-answer is the real rates of major depression since the use of questionnaires and sophisticated algorithms is not as reliable and valid as direct interview and the underlying neurobiology is unknown (101).
Conclusion
The current study reports high rates of depression, dysphoria, and suicidal thoughts in university students during the pandemic and especially during the periods of strict lockdown. The prevalence of conspiracism was high, including medical conspiracy theories in medical students. A complex model is proposed for the development of depression, which includes female sex, strict lockdown, family and economic factors, type of studies, and prior history, while believing in conspiracy theories probably acts as a protective factor. These findings, support previous suggestions by other authors, and although they should be closely monitored longitudinally, they clearly point to the need for a proactive intervention that would aim to protect the mental health of the general population but more specifically of vulnerable groups (102, 103).
Strengths and limitations
The strengths of the current paper include the large number of persons who filled out the questionnaire and the large bulk of in-depth information obtained. A number of anchor points e.g., rates of believing in the flat earth theory and differences in rates among conspiracy theories support the validity of the sample.
The major limitation was that the data were obtained anonymously online through the self-selection of the responders. Additionally, the assessment included only the cross-sectional application of self-report scales, although the advanced algorithm used for the diagnosis of probable depression corrected the problem to a certain degree. However, what is included under the umbrella of “probable depression” in the stressful times of the pandemic remains a matter of debate. Also, the lack of baseline data concerning the mental health of a similar study sample before the pandemic is also a problem.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Aristotle University of Thessaloniki. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
KF: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. NA: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. SB: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. NF: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. XG: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. JH: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. MJ: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. BK: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. GM: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. AM: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. MM: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. IN: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. AN: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. MP: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. AP: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. SP: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. SR: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. DR: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. IR: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. ASS: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. AS: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. MS: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. KT: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. JVo: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. ER: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. JVr: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. AJ: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. PT: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. JB: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. DS: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The study was under the auspice of the Faculty of Medicine, School of Health Sciences, and the Rector of the Aristotle University of Thessaloniki, Greece and constituted an initiative of the Faculty and the Rector in the frame of actions concerning students' mental health.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1320156/full#supplementary-material
References
1. Puthran R, Zhang MW, Tam WW, Ho RC. Prevalence of depression amongst medical students: a meta-analysis. Med Educ. (2016) 50:456–68. doi: 10.1111/medu.12962
2. Fountoulakis KN, Gonda X. Modeling human temperament and character on the basis of combined theoretical approaches. Ann Gen Psychiatry. (2019) 18:21. doi: 10.1186/s12991-019-0247-1
3. Fountoulakis KN, Gonda X. Sex differences in maturation and aging of human personality on the basis of a recently developed complex hierarchical model of temperament and character. Int J Psychiatr Clin Prac. (2022) 26:58–71. doi: 10.1080/13651501.2020.1804941
4. Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. (2016) 316:2214–36. doi: 10.1001/jama.2016.17324
5. Chang JJ, Ji Y, Li YH, Pan HF, Su PY. Prevalence of anxiety symptom and depressive symptom among college students during COVID-19 pandemic: a meta-analysis. J Affect Disord. (2021) 292:242–54. doi: 10.1016/j.jad.2021.05.109
6. Deng J, Zhou F, Hou W, Silver Z, Wong CY, Chang O, et al. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. (2021) 301:113863. doi: 10.1016/j.psychres.2021.113863
7. Fountoulakis KN, Apostolidou MK, Atsiova MB, Filippidou AK, Florou AK, Gousiou DS, et al. Self-reported changes in anxiety, depression and suicidality during the COVID-19 lockdown in Greece. J Affect Disord. (2021) 279:624–9. doi: 10.1016/j.jad.2020.10.061
8. Kaparounaki CK, Patsali ME, Mousa DV, Papadopoulou EVK, Papadopoulou KKK, Fountoulakis KN, et al. University students' mental health amidst the COVID-19 quarantine in Greece. Psychiatry Res. (2020) 290:113111. doi: 10.1016/j.psychres.2020.113111
9. Patsali ME, Mousa DV, Papadopoulou EVK, Papadopoulou KKK, Kaparounaki CK, Diakogiannis I, et al. University students' changes in mental health status and determinants of behavior during the COVID-19 lockdown in Greece. Psychiatry Res. (2020) 292:113298. doi: 10.1016/j.psychres.2020.113298
10. Wathelet M, Duhem S, Vaiva G, Baubet T, Habran E, Veerapa E, et al. Factors associated with mental health disorders among university students in france confined during the COVID-19 pandemic. JAMA Network Open. (2020) 3:e2025591–e2025591. doi: 10.1001/jamanetworkopen.2020.25591
11. Wathelet M, Fovet T, Jousset A, Duhem S, Habran E, Horn M, et al. Prevalence of and factors associated with post-traumatic stress disorder among French university students 1 month after the COVID-19 lockdown. Transl Psychiatry. (2021) 11:327. doi: 10.1038/s41398-021-01438-z
12. Fountoulakis KN, Karakatsoulis G, Abraham S, Adorjan K, Ahmed HU, Alarcon RD, et al. Results of the COVID-19 mental health international for the general population (COMET-G) study. Eur Neuropsychopharmacol. (2021) 54:21–40. doi: 10.1016/j.euroneuro.2021.10.004
13. Surina S, Martinsone K, Perepjolkina V, Kolesnikova J, Vainik U, Ruza A, et al. Factors related to COVID-19 preventive behaviors: a structural equation model. Front Psychol. (2021) 12:676521. doi: 10.3389/fpsyg.2021.676521
14. Ibrahim AK, Kelly SJ, Adams CE, Glazebrook C. A systematic review of studies of depression prevalence in university students. J Psychiatr Res. (2013) 47:391–400. doi: 10.1016/j.jpsychires.2012.11.015
15. von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. (2014) 12:1495–9. doi: 10.1016/j.ijsu.2014.07.013
16. Fountoulakis K, Iacovides A, Kleanthous S, Samolis S, Kaprinis SG, Sitzoglou K, et al. Reliability, validity and psychometric properties of the Greek translation of the center for epidemiological studies-depression (CES-D) scale. BMC Psychiatry. (2001) 1:3. doi: 10.1186/1471-244X-1-3
17. Fountoulakis KN, Pantoula E, Siamouli M, Moutou K, Gonda X, Rihmer Z, et al. Development of the risk assessment suicidality scale (RASS): a population-based study. J Affect Disord. (2012) 138:449–57. doi: 10.1016/j.jad.2011.12.045
18. Spielberger CD. State-Trait Anxiety Inventory for Adults. Mind Garden, Redwood City California (2005).
19. MacDonald PL, Gardner RC. Type i error rate comparisons of post hoc procedures FOR I j chi-square tables. Educ Psychol Meas. (2016) 60:735–54. doi: 10.1177/00131640021970871
20. Rossi R, Jannini TB, Socci V, Pacitti F, Lorenzo GD. Stressful life events and resilience during the COVID-19 lockdown measures in italy: association with mental health outcomes and age. Front Psychiatry. (2021) 12:635832. doi: 10.3389/fpsyt.2021.635832
21. Xiong P, Ming WK, Zhang C, Bai J, Luo C, Cao W, et al. Factors Influencing mental health among chinese medical and non-medical students in the early stage of the COVID-19 pandemic. Front Public Health. (2021) 9:603331. doi: 10.3389/fpubh.2021.603331
22. Zheng X, Guo Y, Yang H, Luo L, Ya B, Xu H, et al. A cross-sectional study on mental health problems of medical and nonmedical students in shandong during the COVID-19 epidemic recovery period. Front Psychiatry. (2021) 12:680202. doi: 10.3389/fpsyt.2021.680202
23. Foster C. Do People Really Think Earth Might Be Flat? Scientific American. (2020). Available online at: https://blogs.scientificamerican.com/observations/do-people-really-think-earth-might-be-flat/
24. Luo W, Zhong BL, Chiu HF. Prevalence of depressive symptoms among Chinese university students amid the COVID-19 pandemic: a systematic review and meta-analysis. Epidemiol Psychiatr Sci. (2021) 30:e31. doi: 10.1017/S2045796021000202
25. Alkhamees AA, Alrashed SA, Alzunaydi AA, Almohimeed AS, Aljohani MS. The psychological impact of COVID-19 pandemic on the general population of Saudi Arabia. Compr Psychiatry. (2020) 102:152192. doi: 10.1016/j.comppsych.2020.152192
26. Evans S, Alkan E, Bhangoo JK, Tenenbaum H, Ng-Knight T. Effects of the COVID-19 lockdown on mental health, wellbeing, sleep, and alcohol use in a UK student sample. Psychiatry Res. (2021) 298:113819. doi: 10.1016/j.psychres.2021.113819
27. Gao J, Wang F, Guo S, Hu F. Mental health of nursing students amid coronavirus disease 2019 pandemic. Front Psychol. (2021) 12:699558. doi: 10.3389/fpsyg.2021.699558
28. Gupta P, Anupama BK, Ramakrishna K. Prevalence of depression and anxiety among medical students and house staff during the COVID-19 health-care crisis. Acad Psychiatry. (2021) 45:575–80. doi: 10.1007/s40596-021-01454-7
29. Li Y, Wang A, Wu Y, Han N, Huang H. Impact of the COVID-19 pandemic on the mental health of college students: a systematic review and meta-analysis. Front Psychol. (2021) 12:669119. doi: 10.3389/fpsyg.2021.669119
30. Li Y, Zhao J, Ma Z, McReynolds LS, Lin D, Chen Z, et al. Mental health among college students during the COVID-19 pandemic in China: a 2-wave longitudinal survey. J Affect Disord. (2021) 281:597–604. doi: 10.1016/j.jad.2020.11.109
31. Liu J, Zhu Q, Fan W, Makamure J, Zheng C, Wang J, et al. Online mental health survey in a medical college in china during the COVID-19 outbreak. Front Psychiatry. (2020) 11:459. doi: 10.3389/fpsyt.2020.00459
32. Ominde B, Jaiyeoba-Ojigho JE, Igbigbi PS. Impact of COVID-19 on the mental health of delta state university students, Nigeria. Acta Biomed. (2021) 92:e2021316. doi: 10.23750/abm.v92i4.10600
33. Tang WC, Lin MP, You J, Wu JYW, Chen KC. Prevalence and psychosocial risk factors of nonsuicidal self-injury among adolescents during the COVID-19 outbreak. Curr Psychol. (2023) 42:17270–9. doi: 10.1007/s12144-021-01931-0
34. Ghafari R, Mirghafourvand M, Rouhi M, Osouli Tabrizi S. Mental health and its relationship with social support in Iranian students during the COVID-19 pandemic. BMC Psychol. (2021) 9:81. doi: 10.1186/s40359-021-00589-4
35. Ma Z, Zhao J, Li Y, Chen D, Wang T, Zhang Z, et al. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol Psychiatr Sci. (2020) 29:e181. doi: 10.1017/S2045796020000931
36. Duarte M, Pereira H. The impact of COVID-19 on depressive symptoms through the lens of sexual orientation. Brain Sci. (2021) 11:523. doi: 10.3390/brainsci11040523
37. Fu W, Wang C, Zou L, Guo Y, Lu Z, Yan S, et al. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Transl Psychiatry. (2020) 10:225. doi: 10.1038/s41398-020-00913-3
38. Garcia-Fernandez L, Romero-Ferreiro V, Padilla S, David Lopez-Roldan P, Monzo-Garcia M, Rodriguez-Jimenez R, et al. Gender differences in emotional response to the COVID-19 outbreak in Spain. Brain Behav. (2021) 11:e01934. doi: 10.1002/brb3.1934
39. Gualano MR, Lo Moro G, Voglino G, Bert F, Siliquini R. Effects of COVID-19 lockdown on mental health and sleep disturbances in Italy. Int J Environ Res Public Health. (2020) 17:4779. doi: 10.3390/ijerph17134779
40. Shi L, Lu ZA, Que JY, Huang XL, Liu L, Ran MS, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open. (2020) 3:e2014053. doi: 10.1001/jamanetworkopen.2020.14053
41. Solomou I, Constantinidou F. Prevalence and predictors of anxiety and depression symptoms during the COVID-19 pandemic and compliance with precautionary measures: age and sex matter. Int J Environ Res Public Health. (2020) 17:4924. doi: 10.3390/ijerph17144924
42. Xin M, Luo S, She R, Yu Y, Li L, Wang S, et al. Negative cognitive and psychological correlates of mandatory quarantine during the initial COVID-19 outbreak in China. Am Psychol. (2020) 75:607–17. doi: 10.1037/amp0000692
43. Husky MM, Kovess-Masfety V, Gobin-Bourdet C, Swendsen J. Prior depression predicts greater stress during COVID-19 mandatory lockdown among college students in France. Compr Psychiatry. (2021) 107:152234. doi: 10.1016/j.comppsych.2021.152234
44. Di Blasi D, Gullo M, Mancinelli S, Freda E, Esposito MF, Gelo G, et al. Psychological distress associated with the COVID-19 lockdown: a two-wave network analysis. J Affect Disord. (2021) 284:18–26. doi: 10.1016/j.jad.2021.02.016
45. Lei L, Huang X, Zhang S, Yang J, Yang L, Xu M, et al. Comparison of Prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in Southwestern China. Med Sci Monit. (2020) 26:e924609. doi: 10.12659/MSM.924609
46. Li J, Yang Z, Qiu H, Wang Y, Jian L, Ji J, et al. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatry. (2020) 19:249–50. doi: 10.1002/wps.20758
47. Ozdin S, Bayrak Ozdin S. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int J Soc Psychiatry. (2020) 66:504–11. doi: 10.1177/0020764020927051
48. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
49. Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. (2020) 87:40–8. doi: 10.1016/j.bbi.2020.04.028
50. Akvardar Y, Demiral Y, Ergor G, Ergor A. Substance use among medical students and physicians in a medical school in Turkey. Soc Psychiatry Psychiatr Epidemiol. (2004) 39:502–6. doi: 10.1007/s00127-004-0765-1
51. Amiri L, Voracek M, Yousef S, Galadari A, Yammahi S, Sadeghi MR, et al. Suicidal behavior and attitudes among medical students in the United Arab Emirates. Crisis. (2013) 34:116–23. doi: 10.1027/0227-5910/a000170
52. Baldassin S, Alves TC, de Andrade LA, Nogueira Martins AG. The characteristics of depressive symptoms in medical students during medical education and training: a cross-sectional study. BMC Med Educ. (2008) 8:60. doi: 10.1186/1472-6920-8-60
53. Bunevicius A, Katkute A, Bunevicius R. Symptoms of anxiety and depression in medical students and in humanities students: relationship with big-five personality dimensions and vulnerability to stress. Int J Soc Psychiatry. (2008) 54:494–501. doi: 10.1177/0020764008090843
54. Chan DW. Depressive symptoms and depressed mood among Chinese medical students in Hong Kong. Compr Psychiatry. (1991) 32:170–80. doi: 10.1016/0010-440X(91)90010-A
55. Chan DW. Coping with depressed mood among Chinese medical students in Hong Kong. J Affect Disord. (1992) 24:109–16. doi: 10.1016/0165-0327(92)90025-2
56. Chandavarkar U, Azzam A, Mathews CA. Anxiety symptoms and perceived performance in medical students. Depress Anxiety. (2007) 24:103–11. doi: 10.1002/da.20185
57. Eskin M, Voracek M, Stieger S, Altinyazar V. A cross-cultural investigation of suicidal behavior and attitudes in Austrian and Turkish medical students. Soc Psychiatry Psychiatr Epidemiol. (2011) 46:813–23. doi: 10.1007/s00127-010-0254-7
58. Jeong Y, Kim JY, Ryu JS, Lee KE, Ha EH, Park H, et al. The associations between social support, health-related behaviors, socioeconomic status and depression in medical students. Epidemiol Health. (2010) 32:e2010009. doi: 10.4178/epih/e2010009
59. Khokher S, Khan MM. Suicidal ideation in Pakistani college students. Crisis. (2005) 26:125–7. doi: 10.1027/0227-5910.26.3.125
60. Ludwig AB, Burton W, Weingarten J, Milan F, Myers DC, Kligler B, et al. Depression and stress amongst undergraduate medical students. BMC Med Educ. (2015) 15:141. doi: 10.1186/s12909-015-0425-z
61. Marzec J, Seweryn M, Kolarczyk A, Bonk M, Krupka-Matuszczyk I. EPA-0883 - Analysis of depression among medical students from different parts of the world. European Psychiatry. (2014) 29:1. doi: 10.1016/S0924-9338(14)78213-6
62. Miletic V, Lukovic JA, Ratkovic N, Aleksic D, Grgurevic A. Demographic risk factors for suicide and depression among Serbian medical school students. Soc Psychiatry Psychiatr Epidemiol. (2015) 50:633–8. doi: 10.1007/s00127-014-0950-9
63. Quince TA, Wood DF, Parker RA, Benson J. Prevalence and persistence of depression among undergraduate medical students: a longitudinal study at one UK medical school. BMJ Open. (2012) 2:e001519. doi: 10.1136/bmjopen-2012-001519
64. Ristic-Ignjatovic D, Hinic D, Jakovljevic M, Fountoulakis K, Siepera M, Rancic N, et al. A ten-year study of depressive symptoms in Serbian medical students. Acta Clin Croat. (2013) 52:157–63.
65. Serra RD, Dinato SLM, Caseiro MM. Prevalence of depressive and anxiety symptoms in medical students in the city of Santos. J Bras Psiquiatr. (2015) 64:213–20. doi: 10.1590/0047-2085000000081
66. Shi M, Liu L, Wang ZY, Wang L. Prevalence of depressive symptoms and its correlations with positive psychological variables among Chinese medical students: an exploratory cross-sectional study. BMC Psychiatry. (2016) 16:3. doi: 10.1186/s12888-016-0710-3
67. Sidana S, Kishore J, Ghosh V, Gulati D, Jiloha R, Anand T, et al. Prevalence of depression in students of a medical college in New Delhi: a cross-sectional study. Australas Med J. (2012) 5:247–50. doi: 10.4066/AMJ.2012.750
68. Sreeramareddy CT, Shankar PR, Binu VS, Mukhopadhyay C, Ray B, Menezes RG, et al. Psychological morbidity, sources of stress and coping strategies among undergraduate medical students of Nepal. BMC Med Educ. (2007) 7:26. doi: 10.1186/1472-6920-7-26
69. Sun L, Sun LN, Sun YH, Yang LS, Wu HY, Zhang DD, et al. Correlations between psychological symptoms and social relationships among medical undergraduates in Anhui Province of China. Int J Psychiatry Med. (2011) 42:29–47. doi: 10.2190/PM.42.1.c
70. Vasegh S, Mohammadi MR. Religiosity, anxiety, and depression among a sample of Iranian medical students. Int J Psychiatry Med. (2007) 37:213–27. doi: 10.2190/J3V5-L316-0U13-7000
71. Zoccolillo M, Murphy GE, Wetzel RD. Depression among medical students. J Affect Disord. (1986) 11:91–6. doi: 10.1016/0165-0327(86)90065-0
72. Yalcin I, Can N, Mance Calisir O, Yalcin S, Colak B. Latent profile analysis of COVID-19 fear, depression, anxiety, stress, mindfulness, and resilience. Curr Psychol. (2021) 22:1–11. doi: 10.1007/s12144-021-01667-x
73. Gratz KL, Mann AJD, Tull MT. Suicidal ideation among university students during the COVID-19 pandemic: identifying at-risk subgroups. Psychiatry Res. (2021) 302:114034. doi: 10.1016/j.psychres.2021.114034
74. Chen X, Zhang SX, Jahanshahi AA, Alvarez-Risco A, Dai H, Li J, et al. Belief in a COVID-19 conspiracy theory as a predictor of mental health and well-being of health care workers in ecuador: cross-sectional survey study. JMIR Public Health Surveill. (2020) 6:e20737. doi: 10.2196/20737
75. De Coninck D, Frissen D, Matthijs TK, Lits G, Champagne-Poirier O, Carignan ME, et al. Beliefs in conspiracy theories and misinformation about COVID-19: comparative perspectives on the role of anxiety, depression and exposure to and trust in information sources. Front Psychol. (2021) 12:646394. doi: 10.3389/fpsyg.2021.646394
76. Ahmed W, Vidal-Alaball J, Downing J, Lopez Segui F. COVID-19 and the 5G conspiracy theory: social network analysis of Twitter data. J Med Internet Res. (2020) 22:e19458. doi: 10.2196/19458
77. Leibovitz T, Shamblaw AL, Rumas R, Best MW. COVID-19 conspiracy beliefs: relations with anxiety, quality of life, and schemas. Pers Individ Dif. (2021) 175:110704. doi: 10.1016/j.paid.2021.110704
78. Salali GD, Uysal MS. COVID-19 vaccine hesitancy is associated with beliefs on the origin of the novel coronavirus in the UK and Turkey. Psychol Med. (2022) 52:3750–2. doi: 10.1017/S0033291720004067
79. Uscinski J, Enders A, Klofstad C, Seelig M, Funchion J, Everett C, et al. Why do people believe COVID-19 conspiracy theories? The Harvard Kennedy School Misinform Rev. (2020) 1:15. doi: 10.37016/mr-2020-015
80. Oliver JE, Wood T. Medical conspiracy theories and health behaviors in the United States. JAMA Intern Med. (2014) 174:817–8. doi: 10.1001/jamainternmed.2014.190
81. Banerjee D, Meena KS. COVID-19 as an “infodemic” in public health: critical role of the social media. Front Pu Health. (2021) 9:610623. doi: 10.3389/fpubh.2021.610623
82. Desta TT, Mulugeta T. Living with COVID-19-triggered pseudoscience and conspiracies. Int J Pub Health. (2020) 65:713–4. doi: 10.1007/s00038-020-01412-4
83. Duplaga M. The determinants of conspiracy beliefs related to the COVID-19 pandemic in a nationally representative sample of internet users. Int J Environ Res Pub Health. (2020) 17:7818. doi: 10.3390/ijerph17217818
84. Allington D, Duffy B, Wessely S, Dhavan N, Rubin J. Health-protective behaviour, social media usage and conspiracy belief during the COVID-19 public health emergency. Psychol Med. (2021) 51:1763–9. doi: 10.1017/S003329172000224X
85. Allington D, McAndrew S, Moxham-Hall V, Duffy B. Coronavirus conspiracy suspicions, general vaccine attitudes, trust and coronavirus information source as predictors of vaccine hesitancy among UK residents during the COVID-19 pandemic. Psychol Med. (2021) 12:1–12. doi: 10.1017/S0033291721001434
86. Bertin P, Nera K, Delouvee S. conspiracy beliefs, rejection of vaccination, and support for hydroxychloroquine: a conceptual replication-extension in the COVID-19 pandemic context. Front Psychol. (2020) 11:565128. doi: 10.3389/fpsyg.2020.565128
87. Biddlestone M, Green R, Douglas KM. Cultural orientation, power, belief in conspiracy theories, and intentions to reduce the spread of COVID-19. Br J Soc Psychol. (2020) 59:663–73. doi: 10.1111/bjso.12397
88. Bogart LM, Wagner G, Galvan FH, Banks D. Conspiracy beliefs about HIV are related to antiretroviral treatment nonadherence among african american men with HIV. J Acquir Immune Defic Syndr. (2010) 53:648–55. doi: 10.1097/QAI.0b013e3181c57dbc
89. Freeman D, Loe BS, Chadwick A, Vaccari C, Waite F, Rosebrock L, Jenner L, Petit A, Lewandowsky S, Vanderslott S, Innocenti S. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol Med. (2022) 52:3127–41. doi: 10.1017/S0033291720005188
90. Gu F, Wu Y, Hu X, Guo J, Yang X, Zhao X, et al. The role of conspiracy theories in the spread of COVID-19 across the United States. Int J Environ Res Public Health. (2021) 18:843. doi: 10.3390/ijerph18073843
91. Jolley D, Douglas KM. The effects of anti-vaccine conspiracy theories on vaccination intentions. PLoS ONE. (2014) 9:e89177. doi: 10.1371/journal.pone.0089177
92. Lazarevic LB, Puric D, Teovanovic P, Lukic P, Zupan Z, Knezevic G, et al. What drives us to be (ir)responsible for our health during the COVID-19 pandemic? The role of personality, thinking styles, and conspiracy mentality. Pers Individ Dif. (2021) 176:110771. doi: 10.1016/j.paid.2021.110771
93. Marinthe G, Brown G, Delouvee S, Jolley D. Looking out for myself: Exploring the relationship between conspiracy mentality, perceived personal risk, and COVID-19 prevention measures. Br J Health Psychol. (2020) 25:957–80. doi: 10.1111/bjhp.12449
94. Romer D, Jamieson KH. Conspiracy theories as barriers to controlling the spread of COVID-19 in the US. Soc Sci Med. (2020) 263:113356. doi: 10.1016/j.socscimed.2020.113356
95. Sallam M, Dababseh D, Yaseen A, Al-Haidar A, Taim D, Eid H, et al. COVID-19 misinformation: mere harmless delusions or much more? A knowledge and attitude cross-sectional study among the general public residing in Jordan. PLoS ONE. (2020) 15:e0243264. doi: 10.1371/journal.pone.0243264
96. Soveri A, Karlsson LC, Antfolk J, Lindfelt M, Lewandowsky S. Unwillingness to engage in behaviors that protect against COVID-19: the role of conspiracy beliefs, trust, and endorsement of complementary and alternative medicine. BMC Pub Health. (2021) 21:684. doi: 10.1186/s12889-021-10643-w
97. Teovanović P, Lukić P, Zupan Z, Lazić A, Ninković M, Žeželj I. Irrational beliefs differentially predict adherence to guidelines and pseudoscientific practices during the COVID-19 pandemic. Appl Cognit Psychol. (2021) 35:486–96. doi: 10.1002/acp.3770
98. Jolley D, Paterson JL. Pylons ablaze: examining the role of 5G COVID-19 conspiracy beliefs and support for violence. Br J Soc Psychol. (2020) 59:628–40. doi: 10.1111/bjso.12394
99. Freyler A, Simor P, Szemerszky R, Szabolcs Z, Koteles F. Modern health worries in patients with affective disorders. A pilot study. Ideggyogy Sz. (2019) 72:337–41. doi: 10.18071/isz.72.0337
100. Tomljenovic H, Bubic A, Erceg N. It just doesn't feel right - the relevance of emotions and intuition for parental vaccine conspiracy beliefs and vaccination uptake. Psychol Health. (2020) 35:538–54. doi: 10.1080/08870446.2019.1673894
101. He L, Wei D, Yang F, Zhang J, Cheng W, Feng J, et al. Functional connectome prediction of anxiety related to the COVID-19 pandemic. Am J Psychiatry. (2021) 178:530–40. doi: 10.1176/appi.ajp.2020.20070979
102. Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. (2020) 63:e32. doi: 10.1192/j.eurpsy.2020.35
Keywords: depression, university students, mental health, COVID-19, suicidality, conspiracy theories
Citation: Fountoulakis KN, Alias NA, Bjedov S, Fountoulakis NK, Gonda X, Hilbig J, Jakovljević M, Kulig B, Mahale G, Manafis A, Mohammed M, Nadareishvili I, Navickas A, Patsali ME, Pavlichenko A, Pilaga SM, Razali S, Romanov D, Rossitza I, Salihu AS, Sinauridze A, Stoyanova M, Thosar K, Vorobjova J, Vrublevska J, Rancans E, Javed A, Theodorakis PN, Breda J and Smirnova D (2024) Students' mental health during the pandemic: results of the observational cross-sectional COVID-19 MEntal health inTernational for university Students (COMET-S) study. Front. Psychiatry 14:1320156. doi: 10.3389/fpsyt.2023.1320156
Received: 11 October 2023; Accepted: 28 December 2023;
Published: 11 January 2024.
Edited by:
Gonzalo Haro, Universidad CEU Cardenal Herrera, SpainReviewed by:
Hongyu Xu, Virginia Commonwealth University, United StatesRossetos Gournellis, National and Kapodistrian University of Athens, Greece
Copyright © 2024 Fountoulakis, Alias, Bjedov, Fountoulakis, Gonda, Hilbig, Jakovljević, Kulig, Mahale, Manafis, Mohammed, Nadareishvili, Navickas, Patsali, Pavlichenko, Pilaga, Razali, Romanov, Rossitza, Salihu, Sinauridze, Stoyanova, Thosar, Vorobjova, Vrublevska, Rancans, Javed, Theodorakis, Breda and Smirnova. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nikolaos K. Fountoulakis, bmlrb2xhc2ZvdW50b3VsYWtpc0BnbWFpbC5jb20=
†ORCID: Konstantinos N. Fountoulakis orcid.org/0000-0001-5503-0811
Nikolaos K. Fountoulakis orcid.org/0000-0002-5965-707X
 Konstantinos N. Fountoulakis
Konstantinos N. Fountoulakis Nor Aziah Alias3
Nor Aziah Alias3 Sarah Bjedov
Sarah Bjedov Nikolaos K. Fountoulakis
Nikolaos K. Fountoulakis Xenia Gonda
Xenia Gonda Miro Jakovljević
Miro Jakovljević Alexandros Manafis
Alexandros Manafis Muftau Mohammed
Muftau Mohammed Ilia Nadareishvili
Ilia Nadareishvili Alvydas Navickas
Alvydas Navickas Alexey Pavlichenko
Alexey Pavlichenko Sindija Mairita Pilaga
Sindija Mairita Pilaga Salmi Razali
Salmi Razali Maria Stoyanova
Maria Stoyanova Ketaki Thosar
Ketaki Thosar Jelena Vrublevska
Jelena Vrublevska Elmars Rancans
Elmars Rancans Afzal Javed
Afzal Javed Pavlos N. Theodorakis
Pavlos N. Theodorakis Joao Breda
Joao Breda Daria Smirnova
Daria Smirnova