Abstract
Introduction:
Stress and anxiety are emotional states that often accompany patients who have to receive dental treatments, leading them to postpone or avoid treatments with the consequent deterioration of their oral health and, hence, their general condition. Music therapy has been shown to be an alternative to other treatments that are invasive and not without danger, such as anxiolytics or sedation. This systematic review and meta-analysis evaluated the effect of music therapy on anxiety and stress prior to dental treatments.
Methods:
Studies published in PubMed (through Medline), Web of Science (WOS), Embase, and Cochrane Library databases were consulted up to October 2023. The inclusion criteria were established for intervention studies (randomized controlled trials, RCTs) according to the PICOS (population, intervention, comparison, outcomes, and study) strategy in subjects with dental stress and anxiety (participants) treated with music therapy (intervention) in comparison with patients without music therapy (control) and evaluating the response to treatment (outcomes).
Results:
A total of 154 results were obtained, with 14 studies finally selected. The risk of bias and the methodological quality were assessed using the Cochrane Risk of Bias Tool and the Jadad scale, respectively. A random-effects meta-analysis was used to quantify the results of the pooled studies, while a fixed-effects meta-analysis was used for studies in the pediatric population. The meta-analysis of pooled studies found statistical significance in the subgroups of anxiety and anxiety–stress (p = 0.03 and p = 0.05, respectively), with an overall effect in favor of the intervention group (p = 0.005). Meta-analysis of the studies in the pediatric population showed considerable statistical significance for the experimental group (p < 0.00001).
Conclusion:
Music therapy as a treatment for stress and anxiety, prior to dental treatment, proved to be effective in both children and adults although more well-designed randomized clinical studies are needed to validate its efficacy.
Systematic review registration:
INPLASY, identifier 202312000.
1 Introduction
Anxiety is considered an emotional state that precedes confrontation with a stimulus and is distinguished from fear in that fear is the emotional response to a perceived threat (1). Both fear and dental anxiety are used interchangeably in the scientific literature although they represent progressive degrees of the same psychological state (2).
Dental treatments often cause, in patients who have to receive them, states of fear and anxiety, inducing them to avoid dental treatment, which results in a poorer quality of life in relation to oral health (3, 4).
There is some agreement that fear of dental treatment affects approximately one in five individuals although some studies place the prevalence at one in three (5–7). It has been known by clinicians that patients in this state, in addition to prolonging or even interrupting treatments, increase their economic costs and, in general, hinder dental practice, resulting in great frustration among dental health professionals (8, 9).
Dental anxiety has been shown to be a stress factor and is associated with personal traits, such as fear of pain, generally induced by unpleasant experiences of dental treatment in childhood or incited by others who have undergone such unpleasant experiences, as well as fear of blood or dental instruments (9, 10). These situations produce in the patient, in addition to psychological alterations, physiological ones, such as tachycardia, arterial hypertension, hyperthermia, mydriasis, hyperglycemia, and elevated cortisol levels, among others, which are caused by the activation of the hypothalamic–pituitary–adrenal axis that can lead to the development of certain systemic pathologies (11, 12).
Music is an auditory stimulus that includes, in addition to the melody itself, harmony, form, rhythm, timbre, and style, and music therapy (MT) is the clinical and evidence-based use of music interventions to achieve individualized goals within a therapeutic relationship by a credentialed professional who has completed an approved MT program (13).
The use of MT dates back to antiquity: the Greek philosopher Pythagoras stated that music exerted a positive influence on both the body and the soul, harmonizing both structures. In fact, philosophers of the Western world, from Pythagoras himself, Plato, and Aristotle to contemporaries including Schopenhauer and Nietzsche, have emphasized the healing power of music both for mental and bodily ailments (14). After the Second World War, MT began to be used conventionally, with the aim of accelerating the recovery of injured combatants, although previously, at the end of the 19th century, the psychology of music began to be studied, especially in the laboratories created in Germany and the USA (15). A good part of the current scientific literature has proposed MT as a positive modulator of patients’ physiological responses to anxiety (16).
In general, in patients with high anxiety in the dental room, anxiolytic drugs and conscious sedation have been used; however, studies have indicated that patients prefer non-pharmacological interventions, mainly due to the low risks involved (17). Therefore, listening to music to control fear and anxiety during dental procedures is widely accepted by adult patients, parents of pediatric patients, and professionals.
For all these reasons, this meta-analytical and systematic quantitative study aimed to examine and assess in the scientific literature the usefulness of MT in the management of stress/anxiety suffered by certain patients before undergoing dental treatments.
2 Methods
2.1 Study design and registration
This study was performed in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement (18) and the guidelines of the Clinical Practice Guidelines (19) (Supplementary Table S1, PRISMA checklist) and was registered in INPLASY no. 202312000 (DOI: 10.37766/inplasy2023.12.0008).
2.2 Question of interest: PICOS format
The question of interest was posed according to the PICOS (population, intervention, comparison, outcomes, and study) format: Is MT a tool that reduces or suppresses stress and anxiety in patients who are going to receive dental treatments? Intervention studies in humans who suffer anxiety before dental treatment (P) and that compared conventional dental treatment together with MT (I), versus subjects who only received conventional treatment (C), were considered with the aim of examining the results obtained for dental stress and anxiety (O) in randomized clinical studies (S) (Table 1).
Table 1
| Population | Patients with stress and anxiety |
| Intervention | Conventional dental treatment + MT |
| Comparisons | Conventional dental treatment |
| Outcomes | To observe the effects of MT on the stress levels (salivary cortisol) (ΔSL) and/or values of anxiety levels (Corah’s Dental Anxiety Scale and Corah’s Modified Anxiety Scale) (ΔAL) |
| Study design | Randomized controlled trials (RCTs) |
PICOS (population, intervention, comparison, outcomes, and study) format.
MT, music therapy; SL, stress level; AL, anxiety level; Δ, values obtained with experimental treatment.
2.3 Study selection and inclusion criteria
Table 2 shows the inclusion and exclusion criteria. We searched for English-language studies that included musical interventions along with conventional oral treatments, rather than only traditional oral treatments, to manage dental stress and anxiety. All included research studies were categorized as randomized controlled clinical trials. Studies in which the full text could not be accessed, retrospective studies, case reports, reviews, and preclinical studies were not included. In addition, overlapping data from two or more studies or samples were excluded. The criteria and methodological operations were evaluated and performed separately by several people.
Table 2
| Inclusion criteria |
|---|
| 1. English language |
| 2. Conventional dental treatment + music therapy (experimental) and conventional dental treatment (control) |
| 3. Outcome indicators: stress levels (cortisol in saliva) and anxiety levels (ΔSL and ΔAL) |
| 4. Randomized clinical trials (RCTs) |
| Exclusion criteria |
| 1. Studies in which full text cannot be accessed |
| 2. Studies on non-conventional treatments (treatment of oral mucosal lesions, oral cancer, and resective surgery, among others) |
| 3. Non-relevant articles (clinical cases, reviews, conference abstracts, meta-analyses, and preclinical studies, among others) |
| 4. Small sample size (less than 5 subjects) |
| 5. Duplicate studies in the databases consulted |
Inclusion and exclusion criteria.
2.4 Literature search
A computerized search of the electronic databases PubMed (via Medline), Web of Science (WOS), Embase, and the Cochrane Library was carried out up to October 2023. The following terms were used to formulate the search strategies: Anxiety Disorders* OR Stress Disorders* OR Dental Anxiety*/therapy OR Dental Fear* OR Phobic Disorders OR Dental Phobic/therapy* OR Dental Fear* AND Music Therapy* AND Humans* AND Randomized Controlled Trial*. The electronic search was supplemented with a manual search; moreover, the gray literature and the bibliographic references of the included studies were examined in order to obtain as much bibliographic information as possible and to minimize publication bias.
2.5 Data extraction and management
Two reviewers (NL-V and AL-V) independently performed a systematic screening of the titles and abstracts of the previously selected English-language registries. From the studies that met the inclusion criteria, the full text was read. Data extraction and disagreements between reviewers were resolved by discussion or consultation with a third reviewer (BMS); however, inter-reviewer agreement was assessed using Cohen’s kappa index (κ) (20). Although Cohen’s kappa (κ) suffers from a number of inconsistencies long debated by clinicians, it is considered the standard technique for diagnostic agreement and is used in the vast majority of analyses, having had its efficacy proven over the past 60 years.
2.6 Evaluation of study quality
To assess the methodological quality of the RCTs included in the meta-analysis, the Oxford Quality Scoring System or the Jadad Scale (21) was used, which takes into account biases related to randomization, masking, and loss to follow-up. The score assigned to each study ranged from 1 to 6 points, with those that obtained 5 and 6 points being considered studies of rigorous methodology, those that obtained 3 and 4 points of medium quality, and those that obtained scores lower than 3 points of low quality.
2.7 Risk of bias
The risk of bias was independently assessed using the Cochrane Risk of Bias Tool (RoB2) from the Cochrane Handbook for Systematic Reviews of Interventions (22) by two assessors (NL-V and AL-V). Five domains of bias were assessed: randomization process, deviations from intended interventions, missing outcome data, outcome measurement, and selection of reported outcomes. Studies with a high risk of bias were given a rating of “high,” those considered at low risk were rated “low,” while those with uncertainty bias or lack of information about possible bias were considered “borderline.” The studies included in the meta-analysis were classified as having a low, high, or borderline risk of bias. Discrepancies in the evaluation of RoB2 were discussed by NL-V and AL-V to reach a consensus.
2.8 Analysis
Data to evaluate the efficacy of MT on dental stress and anxiety were analyzed using Review Manager software (RevMan software, version 5.4.1; The Cochrane Collaboration, Copenhagen, Denmark, 2020).
Different meta-analyses were performed for anxiety and stress in children and adults. All were based on the mean difference (MD) and standard deviation (SD) to estimate the effect size, with 95% confidence intervals (CIs) to assess adverse outcomes. A random effects model was selected taking into account the uncertainty in I2, considering the scarcity of studies in some situations (children) and the methodological heterogeneity found in the included studies. Heterogeneity was considered unimportant with I2 = 0%–30%, moderate with I2 = 40%–50%, substantial with I2 = 60%–75%, and considerable with I2 ≥ 75%. The threshold for statistical significance was set at p < 0.05. Meta-analysis of adverse outcomes was not performed due to lack of data reporting.
A sensitivity analysis was performed excluding studies that could lead to heterogeneity of the results and successive meta-analyses, each time excluding one of the selected trials. If any of the results were strongly discordant with the rest, the study that contributed the greatest degree of heterogeneity was identified.
3 Results
3.1 Study selection
The four databases consulted yielded a total of 154 records. After eliminating 117 duplicates and 15 more as ineligible for automation tools and other reasons, 29 records were considered suitable. The full texts of these studies were obtained for further evaluation, after which 14 were excluded for cause. A total of 15 studies were included in the final analysis (Figure 1).
Figure 1

Flowchart of the study selection.
The discrepancy between the two reviewers (NL-V and AL-V) was 18%, resulting in high concordance (κ = 82%).
3.2 Study characteristics
The 15 studies included in the meta-analysis analyzed a sample of 1,402 subjects, of whom 308 were patients under 18 years of age. The largest samples were presented by the studies of Dixit and Jasani (23) (120 children), Sorribes de Ramón et al. (24) (275 adults), Kim et al. (25) (219 adults), and Janthasila and Keeratisiroj (26) (128 children).
Three studies evaluated a child population (26–28), while all the others included an adult population. The age range of the adult subjects included in the studies was between 18 and 57 years, while that of the child subjects was between 4 and 12 years.
Anxiety levels were assessed in all included studies. The study by Thoma et al. (29) assessed anxiety and stress, while those by Yamashita et al. (27) and Janthasila and Keeratisiroj (26) assessed anxiety and fear. The measurement scales used were Corah’s Dental Anxiety Scale (CDAS), Modified Dental Anxiety Scale (MDAS), North Carolina Behavior Rating Scale (NCBRS), The Dental Subscale of Children’s Fear Survey Schedule (CFSS-DS), State-Trait Anxiety Inventory (STAI), Hierarchical Anxiety Questionnaire (HAQ), Children’s Fear Survey Schedule (CFSS-DS), and Facial Image Scale (FIS). Salivary cortisol was measured by ELISA (30) and DRG (31). The music styles used varied between pop–folk and classical music.
The characteristics of the studies are presented in Table 3.
Table 3
| Study detail | Participant characteristics | Dental procedure | Music specification | Measurement tools | Outcomes | Funding |
|---|---|---|---|---|---|---|
| Lahmann et al. (32) Germany PRCS |
Sample size: 90 Sex: 48 women Age: >18 years Diagnosis: Dental anxiety Demographic: NR Others: Subjects married or living with someone: 20 ± 71.4 MT, 26 ± 86.7 C Blue collar workers: 14 ± 50 MT, 11 ± 36.7 C Homemakers: 7 ± 25 MT, 9 ± 30 C |
Restorative treatment of simple caries that were not in the advanced stage | NR | HAQ; STAI | MT significantly reduced dental anxiety; however, in very anxious subjects, it had no clinically relevant effect. | NR |
| Kim et al. (25) South Korea RCT |
Sample size: 219 Sex: 99 women Age: >18 years Diagnosis: Dental anxiety Demographic: <40 years MT, <53 years C University education: 65 ± 61.3 MT, 73 ± 64.6 C Employed: 55 ± 51.9 MT, 51 ± 45.1 C Others: Reason for curative surgery: 51 ± 48.1 MT, 46 ± 40.7 C Reason for preventive surgery: 55 ± 51.9 MT, 67 ± 59.3 C |
Mandibular third molar extraction | The patient selected his or her favorite songs from a list that included classical music, pop songs, folk songs, hymns, and Korean-style country songs. | CDAS | The music-treated group reported significantly less intraoperative anxiety than the control group (no music treatment) | NR |
| Mejía-Rubalcava et al. (33) Mexico REPS |
Sample size: 34 Sex: 23 women Age: >18 years Diagnosis: Dental anxiety and stress Demographic: Housewife: 9 ± 52.9% Student: 3 ± 17.7% MT, 1 ± 5.8% C Employee: 5 ± 29.4% MT, 3 ± 17.7% C Education: Elementary, 2 ± 11.8%; high school, 9 ± 52.9% MT, 13 ± 76.4% C Others: Marital status: Single, 8 ± 47.0% MT, 2 ± 11.8% C Married/union: 7 ± 41.2% MT, 14 ± 82.3% C |
Endodontic treatment Extraction |
Music instrumentals soothing, calming, positive, relaxing daily “Essence No. 1” (iTunes) | MDAS; Concentration of cortisol in the saliva (Salimetrics, State College, PA, USA) |
Significant differences were registered in the salivary cortisol concentration for the MT-treated group. | NR |
| Thoma et al. (29) Switzerland RCCT |
Sample size: 92 Sex: 49 women Age: mean, 57 years Diagnosis: Dental anxiety and stress Demographic: Years of education: 13.56 ± 3.0 MT, 13.93 ± 3.01 C No. of appointments per year: 2.46 ± 1.07 MT, 2.33 ± 1.35 C Others: Trait dental anxiety: 34.6 ± 9.85 MT, 31.76 ± 9.34 C |
Dental hygiene treatment | Relaxing music (“Miserere” by Allegri) | STAI; HAQ | The state anxiety levels in the music group decreased significantly after the intervention compared to the control group. | University of Zurich. Grant no. 56233208 (MVT) |
| Yamashita et al. (27) Thailand RCT |
Sample size: 128 Sex: Women: 20 ± 60.6 MT, 13 ± 40.6 C Age: 20–40 years Diagnosis: Dental anxiety Demographic: Education: Grade 4, 13 ± 39.4 MT, 12 ± 37.5 C; Grade 5, 10 ± 30.3 MT, 8 ± 25.0 C; Grade 6, 10 ± 30.3 MT, 12 ± 37.5 C Others: Religion: Buddhism, 100% |
Filling; extraction; scaling; application of fluoride sealant | NR | FIS; CFSS | Evaluation of the between-subjects effects revealed a significant effect of MT on dental anxiety and fear. | NF |
| Dixit and Jasani (23) India PGRCT |
Sample size: 120 Sex: Women: 18 ± 45 MT, 14 ± 35 C Age: 4–6 years Diagnosis: Dental anxiety Demographic: NR Others: NR |
Oral prophylaxis and fluoride treatment | Indian classical instrumental music (Raag Sohni played by Pandit Shiv Kumar Sharma on santoor) | FIS; NCBRS | Significant effects of exposure to MT on the reduction of dental anxiety in young children | NF |
| Aravena et al. (34) Chile PGRCT |
Sample size: 42 Sex: 64.2% women Age: 15–40 years Diagnosis: Moderate level of dental anxiety and stress Demographic: NR Others: NI |
Simple dental extraction | Two songs by Giorgio Costantini 2012 from the album “Universound” | Corah-MDAS; salivary cortisol levels (salivary cortisol: ELISA kit, Salimetrics Assays™, Pennsylvania, USA) | Significantly lower values of anxiety and salivary cortisol levels were observed in the music group compared to the control group. | NF |
| Kupeli and Gülnahar (35) Turkey ORCT |
Sample size: 80 Sex: 44 women Age: 18–30 years Diagnosis: Moderate dental anxiety; high-level dental anxiety; extreme dental anxiety Demographic: NR Others: NR |
Third molar extraction | Turkish music Classical music Rock music |
CDAS | Anxiety levels decreased in all groups with different types of music; the postoperative CDAS values of the classical music group were significantly lower than those of the other groups. | NF |
| Gülnahar and Kupeli (36) Turkey PRCT |
Sample size: 80 Sex: 47 women Age: 40–70 years Diagnosis: Extreme anxiety Demographic: NR Others: NR |
Dental implant surgery | Classic Turkish music (Saba or Rast Tune Classical music (Vivaldi) Soft rock music |
CDAS | All groups with music treatment presented a significant decrease in anxiety levels. It was observed that listening to music had a positive effect on dental anxiety regardless of the type of music. Postoperatively, Turkish music and classical music were much more effective in decreasing dental anxiety compared to soft rock music. | NF |
| Wazzan et al. (30) United Arab Emirates RCCT |
Sample size: 46 Sex: Women 8 ± 17.4 Age: >18 years Diagnosis: Dental anxiety and stress Demographic: Education: Primary–high school, 25 ± 54.3; University, 18 ± 39.1 Visits to the dentists: First time, 21 ± 45.7; Previous visits, 25 ± 54.3 Others: Nationality: Arab, 20 ± 43.5; Non-Arab, 26 ± 56.5 Consumption of caffeine, alcohol, or nicotine: Yes, 16 ± 34.8; No, 30 ± 65.8 |
Dental treatment | Regular soft music | CDAS; cortisol in the saliva (salivary cortisol ELISA kit; Salimetrics Assays™, Pennsylvania, USA) | MT may help reduce salivary cortisol among patients in the intervention group who were exposed to slow-paced music compared to the control group treated without exposure to music; however, this reduction was not statistically significant. | NF |
| Kayaaltı-Yüksek and Yildirim (28) Turkey ORCT |
Sample size: 60 Sex: 28 girls Age: 8–12 years Diagnosis: Dental anxiety Demographic: Plaque index: 0.82 ± 0.07 MT, 1.98 ± 0.08 C Gingival index: 0.77 ± 0.08 MT, 1 ± 0.07 C Others: NR |
Oral hygiene training | First movement of Mozart’s Sonata for two pianos in D major, K. 448, during oral hygiene training (approximately 3 min) | CFSS | Listening to Mozart’s music before toothbrushing training had a significant effect on plaque removal in children with high dental anxiety. | NF |
| Esteban Pellicer et al. (37) Spain RCT |
Sample size: 26 Sex: 13 women Age: 24–69 years Diagnosis: Dental anxiety Demographic: Anxiety level: 4.25 ± 3.92 MT, 2.63 ± 3.62 C Others: Pain level: 1.25 ± 1.75 MT, 0.75 ± 1.75 C |
Dental implant surgery | Four Seasons (Vivaldi), Overture No. 3 (Bach), Adagio for Strings and Organ (T. Albinoni); Symphony N. 40, Sonata for 2 Pianos (Mozart) and Symphony N. 41 (Mozart) | Corah-MDAS; VAS | The incorporation of a musical flow in an individualized way into each patient in dental clinics is a useful non-pharmacological therapy to reduce anxiety in patients. | NF |
| Karapicak et al. (31) Turkey RCCT |
Sample size: 70 Sex: 56 women Age: >18 years Diagnosis: Moderate dental anxiety and stress Demographic: Single: 27 ± 77.1 MT, 25 ± 71.4 C; Married: 8 ± 22.9 MT, 10 ± 28.6 C Others: High school: 10 ± 28.6 MT, 12 ± 34.3 C University: 25 ± 71.4 MT, 23 ± 65.7 C Duration of dental treatment (in minutes): 49.3 ± 9.2 MT, 46.0 ± 9.4 C |
Restorative dental treatments | Each patient’s favorite music | MDAS; salivary cortisol levels (enzyme-linked immunosorbent assay kit; DRG, Germany) | The study was performed in a dental hospital during the COVID-19 pandemic, which could have impacted the anxiety levels during treatment. Moreover, since it is a cross-sectional study, it may not be reliable in determining the cause–effect relationship. | Karadeniz Technical University Scientific Research Project Coordination Unit |
| Sorribes De Ramón et al. (24) Spain RCCT |
Sample size: 275 Sex: 56.4% women Age: 18–50 years Diagnosis: Anxiety Demographic: Laterality of third molar (%): Right, 43 ± 47.3 MT, 42 ± 46.2 C; Left, 485 ± 2.7 MT, 4953 ±.8 C Others: Winter classification (%): Vertical, 313 ± 4.1 MT, 384 ± 1.8 C; Mesioangular, 192 ± 0.9 MT, 171 ± 8.7 C; Horizontal, 323 ± 5.2 MT, 272 ± 9.7 C |
Extraction of the third molar | “Introduction and Allegro for harp, flute, clarinet, and string quartet” by Ravel and “Aria” by J.S. Bach | STAI; VAS | In the patients in the MT group, a significant decrease in the scores for the levels of anxiety was observed. | NF |
| Janthasila and Keeratisiroj (26) Thailand RCCT |
Sample size: 128 Sex: women: 206 ± 0.6 MT, 134 ± 0.6 C Age: 10–12 years Diagnosis: Dental anxiety Demographic: Education: Grade 4, 13 ± 39.4 MT, 12 ± 37.5) C; Grade 5, 10 ± 30.3 MT, 8 ± 25.0 C; Grade 6, 10 ± 30.3 MT, 12 ± 37.5 C Others: Religion: Buddhism, 32% |
Filling Extraction Scaling Application of fluoride sealant |
Thai pop instrumental folk songs | CFSS | The use of an MT program reduced anxiety and fear of dental services in school-aged children. | NF |
Characteristics of the studies.
PGRCT, parallel-group randomized clinical trial; PRCT, prospective randomized controlled trial; NR, none reported; NI, no interest; NF, not funded; MT, music treatment; C, control; HAQ, Hierarchical Anxiety Questionnaire; STAI, State-Trait Anxiety Inventory; CDAS, Corah’s Dental Anxiety Scale; Corah’s-MDAS, Modified Dental Anxiety Scale; RCT, randomized clinical trial; REPS, randomized experimental prospective study; RCCT, randomized controlled clinical trial; FIS, Facial Image Scale; CFSS, Children’s Fear Survey Schedule; NCBRS, North Carolina Behavior Rating Scale; ORCT, observational randomized controlled trial.
3.3 Methodological quality of the studies
Only one of the studies included in the meta-analysis (34) achieved a score on the Jadad scale compatible with a rigorous study (≥5 points). Medium quality (3 and 4 points) was achieved by 5 studies (24, 26, 28, 31, 37), while the rest of the studies were of poor quality (≤2 points) (Table 4).
Table 4
| Study | Randomization | Adequate randomization method | Blinding | Double blinding | Appropriate blinding method | Dropouts | Total score |
|---|---|---|---|---|---|---|---|
| Lahmann et al. (32) | 1 | 1 | 0 | 0 | 0 | DNR | 2a |
| Kim et al. (25) | 1 | 1 | 0 | 0 | 0 | DNR | 2a |
| Mejía-Rubalcava et al. (33) | 1 | 1 | 0 | 0 | 0 | DNR | 2a |
| Thoma et al. (29) | 1 | 1 | 0 | 0 | 0 | DNR | 2a |
| Yamashita et al. (27) | 1 | 1 | 0 | 0 | 0 | DNR | 2a |
| Dixit and Jasani (23) | 1 | 1 | 0 | 0 | 0 | DNR | 2a |
| Aravena et al. (34) | 1 | 1 | 1 | 1 | 1 | DNR | 5b |
| Kupeli and Gülnahar (35) | 1 | 1 | 0 | 0 | 0 | DNR | 2a |
| Gülnahar and Kupeli (36) | 1 | 1 | 0 | 0 | 0 | DNR | 2a |
| Wazzan et al. (30) | 1 | 1 | 0 | 0 | 0 | DNR | 2a |
| Kayaaltı-Yüksek and Yildirim (28) | 1 | 1 | 1 | 0 | 1 | DNR | 4c |
| Esteban Pellicer et al. (37) | 1 | 1 | 1 | 0 | 1 | DNR | 4c |
| Karapicak et al. (31) | 1 | 1 | 1 | 0 | 1 | DNR | 4c |
| Sorribes De Ramón et al. (24) | 1 | 1 | 1 | 0 | 0 | DNR | 3a |
| Janthasila and Keeratisiroj (26) | 1 | 1 | 0 | 0 | 0 | 1 | 3a |
Scores of the included studies on the Jadad scale.
Each study was assigned a score of 0–6.
DNR, does not report.
Poor quality (≤2 points).
Rigorous study (≥5 points).
Medium quality (3 and 4 points).
3.4 Risk of bias
Two reviewers (NL-V and AL-V) independently assessed the quality of the included studies, according to RoB2 (Cochrane Risk of Bias Tool) (22), based on 5 domains (i.e., randomization process, deviations from intended interventions, missing outcome data, outcome measurement, and selection of reported outcomes) and according to the Cochrane Handbook for Systematic Reviews of Interventions, outcome measurement, and selection of reported outcomes). According to the Cochrane Handbook for Systematic Reviews of Interventions, a “high” rating was given to studies considered with high risk of bias, “low” to those with low risk of bias, and “borderline” to those with uncertainty bias or lack of information on potential bias. Discrepancies between evaluators were settled by discussion and consensus. All included studies (23–37) addressed the domains “random sequence generation” (selection bias) and “allocation concealment” (selection bias), while the domain “blinding of participants and personnel” (performance bias) was met by only 4 studies (24, 25, 34, 37). The studies by Aravena et al. (34) and. Pellicer et al. (37) were the best rated. The study by Wazzan et al. (30) was the worst rated, together with the studies by Mejía Rubalcava et al. (33), Dixit and Jasani (23), and Kupeli and Gülnahar (35), which showed the greatest uncertainty (Figure 2). The risk of bias of the different subgroups is presented on the left of Figure 2.
Figure 2
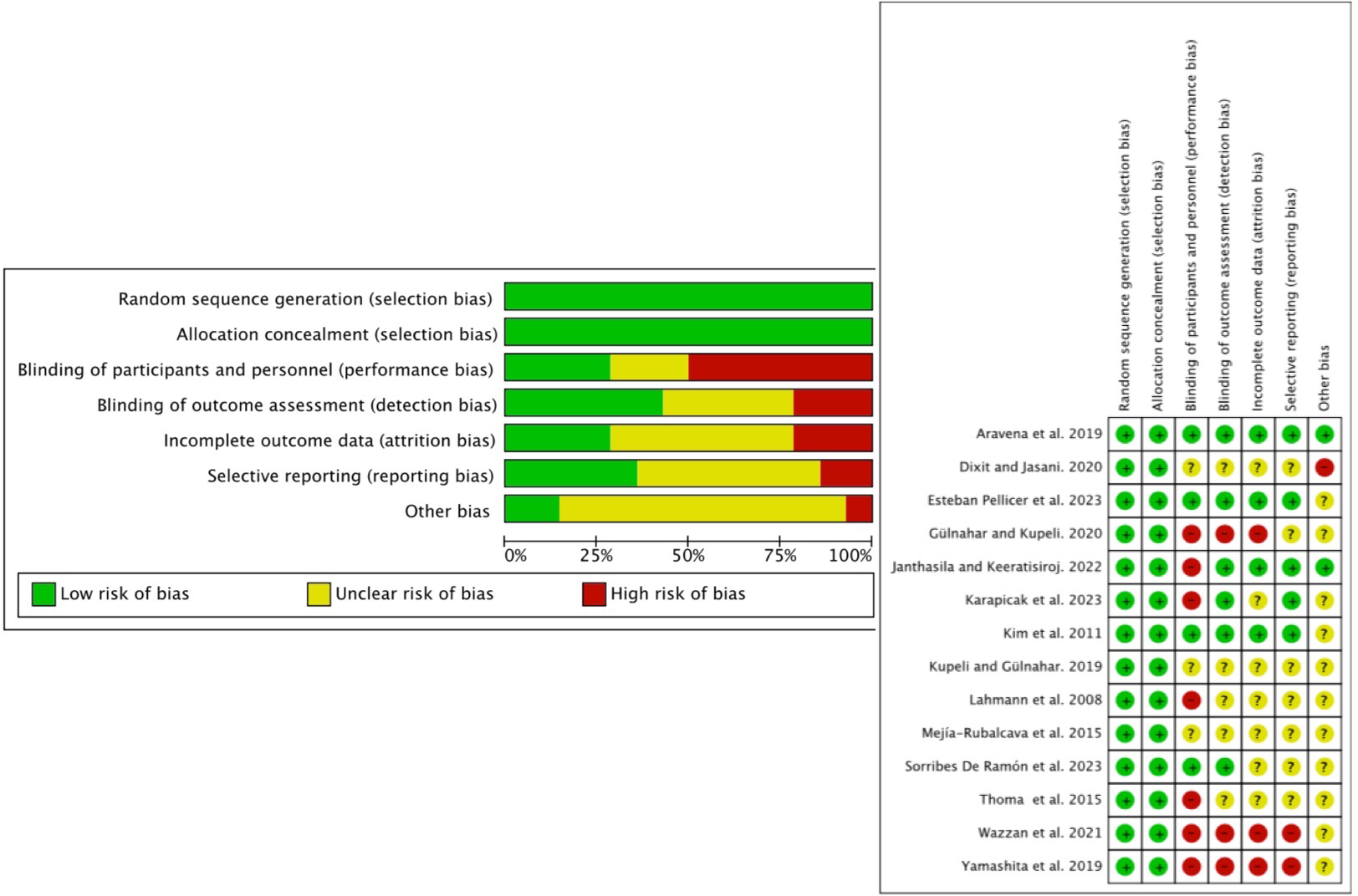
Risk of bias of the included studies.
3.5 Meta-analysis
For the meta-analysis, only 14 studies were included since the study by Kayaalti-Yüksek and Yildirim (28) evaluated the effectiveness of music in learning toothbrushing behavior in children with high and low levels of anxiety.
All of the studies in the adult population assessed dental anxiety. Stress was assessed in five studies (29–31, 33, 34), and only two studies (23, 26) assessed dental anxiety in the pediatric population.
A meta-analysis by subgroups (anxiety, stress, and anxiety–stress) was performed. All subgroups presented considerable heterogeneity (I2 > 75%); however, statistical significance was only found in the anxiety and anxiety–stress subgroups (p = 0.03 and p = 0.05, respectively), with an overall effect in favor of the experimental group (p = 0.005) (Figure 3).
Figure 3
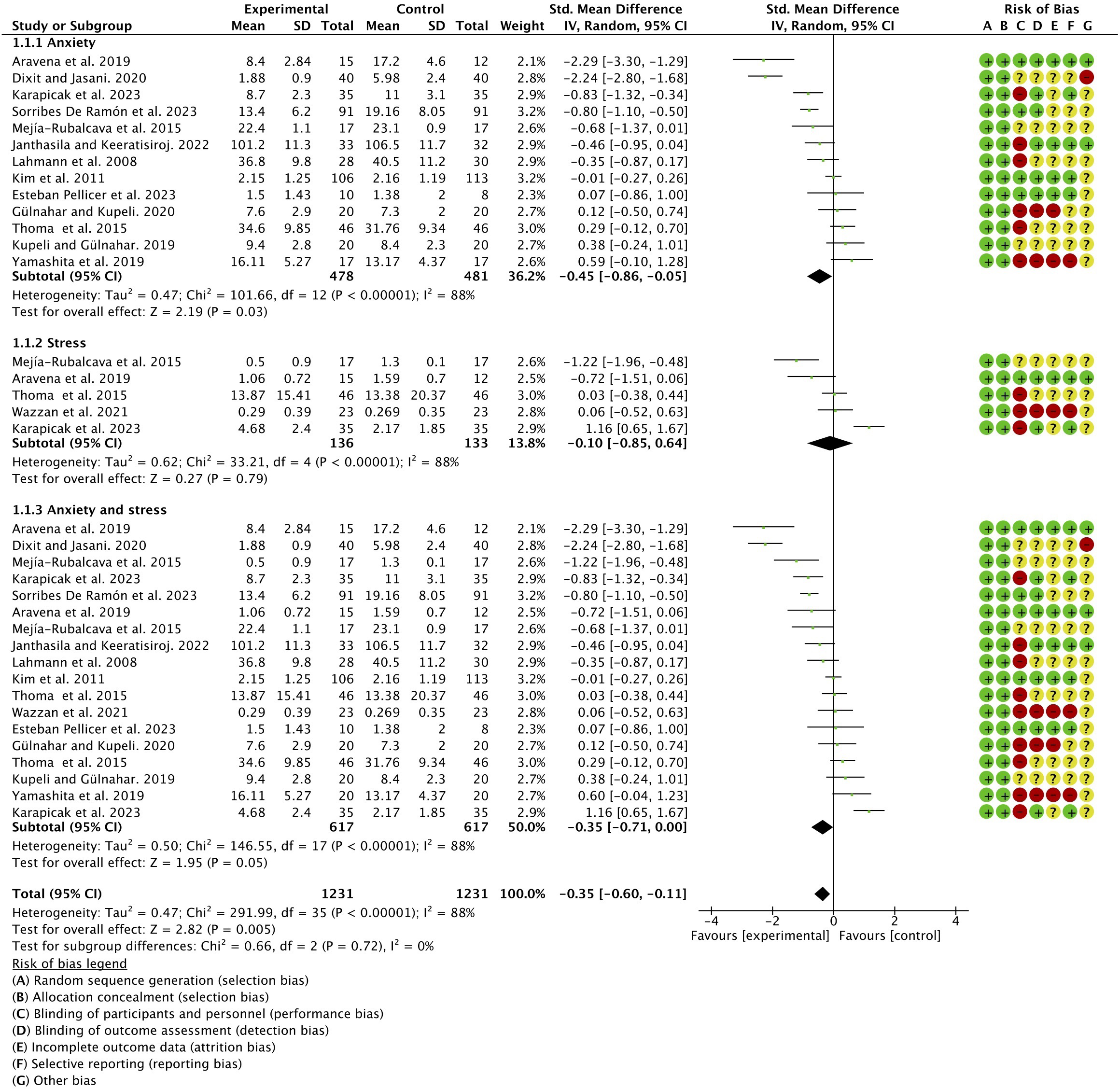
Meta-analysis (forest plot) by subgroups.
A sensitivity test was carried out in adults, discarding studies suspected of bias until a heterogeneity I2 = 0% was achieved (Figure 4).
Figure 4
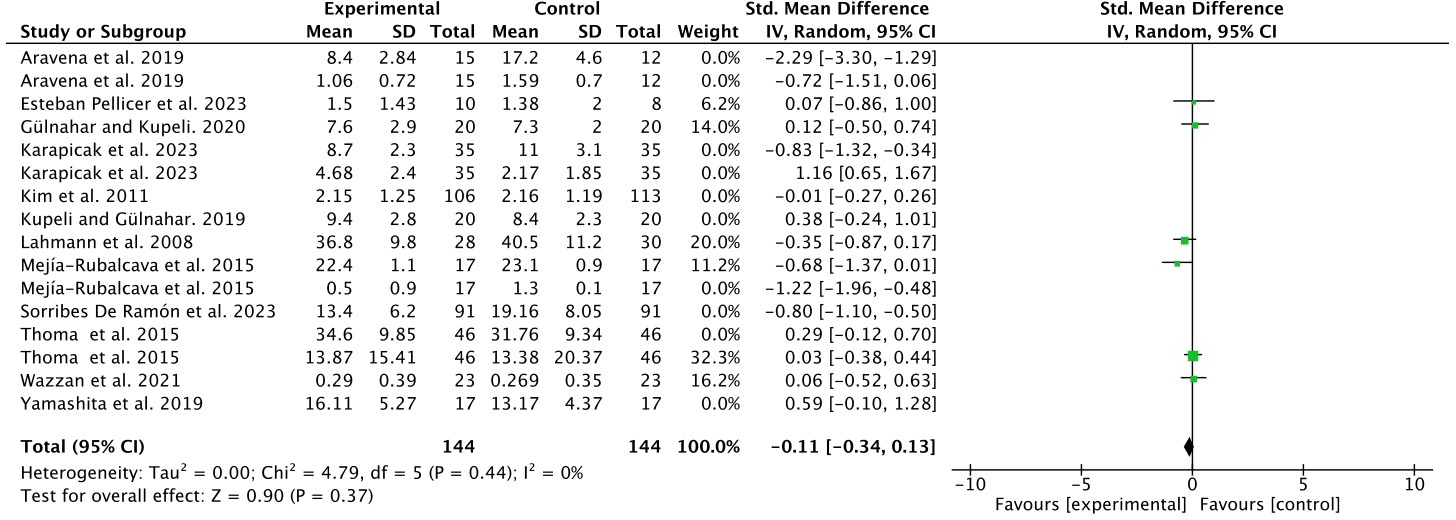
Sensitivity test in adults.
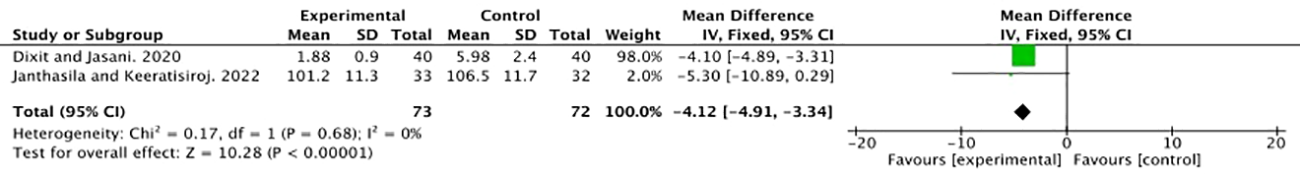
Despite the paucity of studies on the effect of MT in the pediatric population (23, 26) and due to the considerable sample size (248 subjects), a meta-analysis was performed for this subgroup, resulting in zero heterogeneity (I2 = 0%) and considerable statistical significance in favor of the experimental group (p < 0.00001) (Figure 5).
Figure 5
Forest plot in the child population.
A meta-analysis of adverse effects was also not performed due to the lack of data in the included studies.
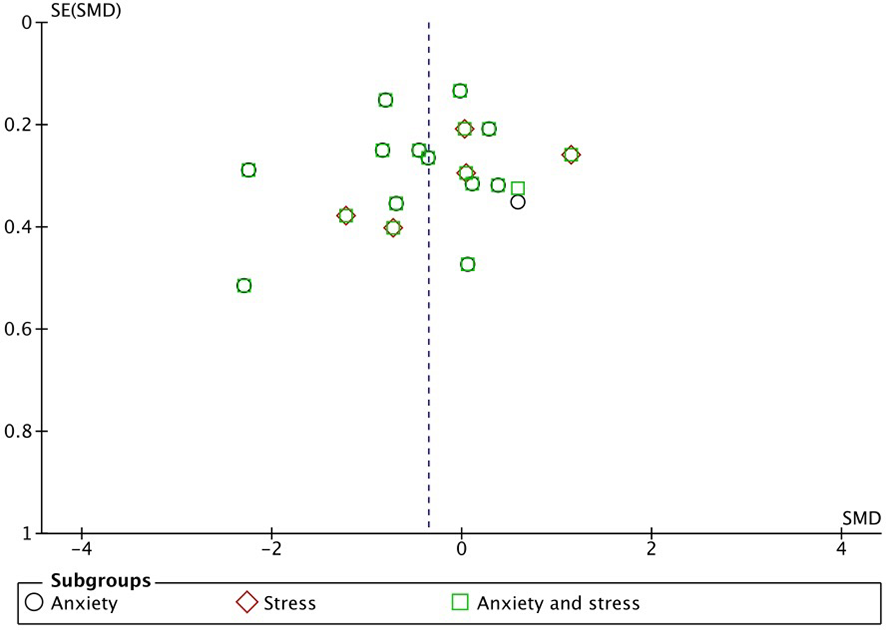
3.6 Publication bias
The graph in Figure 6, in which the abscissa axis (X) represents the observed results and the ordinate axis (Y) the standard error, shows low asymmetry and, therefore, low publication bias.
Figure 6
Funnel plot.
4 Discussion
Our meta-analysis found a positive association between the use of MT and the reduction of stress and anxiety in patients undergoing dental treatments.
Both routine visits to the dentist and the different dental treatments generally provoke different states of stress and anxiety in patients who have to receive them, depending, in general, on the complexity of the treatments. This leads to avoidance of dental treatments, with the consequent deterioration of health. Many of the patients who suffer from this type of alteration, especially high levels of dental anxiety, are treated with sedation, a technique that is costly and not without danger (38). For this reason, attempts have been made to develop effective and noninvasive psychological interventions to deal with this issue, with the aim of preventing patients from reducing dental care, which has important implications for public health (39).
Music has been used as a tool to improve well-being, reduce stress, and provide distraction to patients, which has been shown to be effective in reducing anxiety and improving mood in patients undergoing dental procedures and which is an affordable intervention (13).
The systematic review and meta-analysis presented here evaluated the effect of MT on stress and anxiety in patients undergoing dental treatments.
Several studies have investigated the effect of MT on stress and anxiety before and after the intervention (40–42). A Cochrane review of 20 studies suggested that listening to music may have a beneficial effect on anxiety in people awaiting surgery, in addition to highlighting that preoperative sedatives and anxiolytics often have negative side effects that lengthen patients’ recovery. Thus, offering musical interventions to patients was suggested as an alternative to these types of drugs (43). Another large-scale study indicated that listening to music produced greater benefits than midazolam in reducing preoperative anxiety (44). All these led to the increasing use of MT as a stress-reducing intervention in both medical and mental health settings (45).
The stress and anxiety that a good number of patients present before and during dental treatments justify the search for alternative, noninvasive, and inexpensive treatments without side effects that prevent the resistance of patients to receive dental treatments or diminish their quality, precisely because of this rejection. Based on these aspects, we conducted the present systematic review and meta-analysis, which had positive results and evaluated the effects of MT on stress and anxiety in patients undergoing dental treatments. Subjects in the experimental group with moderate, high, or extreme stress/anxiety states received MT and were compared to a control group that did not receive MT. Miyata et al. (46), in an RCT, estimated the effect of MT on preoperative anxiety by analyzing the heart rates in patients undergoing dental surgery under intravenous sedation and local anesthesia. The authors concluded that MT can alleviate anxiety by reducing sympathetic nervous activity; furthermore, they reported that MT would allow the treatment of stress on a continuous basis, i.e., from the patient’s arrival at the dental clinic for intravenous sedation until the completion of dental surgery, and concluded that taking into account the cost-effectiveness, the absence of adverse effects, the immediate effect, the safety in terms of no drug use, and the absence of concerns about recovery, MT would be instrumental in treating anxiety in dentistry. Other studies have also evaluated the role of MT in anxiety in patients undergoing dental extraction. A study conducted on a sample of 50 patients undergoing this intervention evaluated the anxiety levels in the experimental group treated with MT compared to the control group and found significant changes in both the hemodynamic levels and Corah’s-MDAS (47). Studies including large samples have evaluated the usefulness of different types of MT on anxiety levels, through the plasma noradrenaline level, in patients undergoing dental extraction, reporting benefits on anxiety in the experimental group treated with Islamic religious music (48).
In our meta-analysis, the anxiety scales and salivary cortisol values for dental anxiety and stress were evaluated as we considered these to be sufficient determinants for the diagnosis of these conditions. Cortisol is known as the stress hormone that is released in response to anxiety, while salivary cortisol is frequently used as a biomarker of psychological stress (49). We found statistical significance in the subgroups assessing anxiety and anxiety and stress combined (p = 0.03 and p = 0.05, respectively), with an overall effect in favor of the MT group. The meta-analysis of studies in the pediatric population, despite there being only two (23, 26) but with a large sample of patients, was particularly significant in favor of the experimental group (p < 0.00001).
Despite the results found on the effect of MT on stress and anxiety, we are aware of a series of limitations in this study. On the one hand, with respect to stress, only the salivary cortisol levels were considered, which we estimated to be more reliable than certain hemodynamic values, but which could be influenced by concomitant pathological situations (e.g., hypertension and paroxysmal tachycardia, among others). This was not clearly contemplated in many of the studies included in this meta-analysis, which could alter the results. Another aspect to consider would be the different types of scales used in the studies and their impact on the reported anxiety values, as well as the methods used to determine salivary cortisol. The differences between adults and children when assessing anxiety should also be mentioned.
A final aspect to take into consideration, which many patients report when receiving dental care, is the special odor that usually exists in dental clinics, generally due to the products used for the disinfection of surfaces and reusable instruments and the phenolic derivatives used as antiseptics in endodontic treatments, especially in teeth with necrotic pulp (50, 51). This aspect was covered by only one of the studies included in our meta-analysis (26).
Considering all these, our results should be taken with some caution.
5 Conclusions
The present systematic review and meta-analysis found that MT produced a beneficial effect on stress and anxiety control in patients receiving dental treatments; however, we believe that well-designed RCTs according to CONSORT standards are necessary and justifiable to corroborate this efficacy.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
NL-V: Conceptualization, Data curation, Investigation, Writing – original draft, Writing – review & editing. AL-V: Writing – original draft, Writing – review & editing. BM: Data curation, Methodology, Writing – original draft, Writing – review & editing. JB: Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This article has been partially funded by the research group “Advances in Oral Health” of the University of Salamanca, directed by Javier Montero.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1352817/full#supplementary-material
Supplementary Table S1Checklist.
References
1
Crocq MA . A history of anxiety: from Hippocrates to DSM. Dialogues Clin Neurosci. (2015) 17:319–225. doi: 10.31887/DCNS.2015.17.3/macrocq
2
Klingberg G Broberg AG . Dental fear/anxiety and dental behaviour management problems in children and adolescents: a review of prevalence and concomitant psychological factors. Int J Paediatr Dent. (2007) 17:391–406. doi: 10.1111/j.1365-263X.2007.00872.x
3
Qiao F Zhang M Zhang T Zhu D . Dental anxiety is related to postoperative symptoms in third molar surgery. Front Psychiatry. (2022) 13:956566. doi: 10.3389/fpsyt.2022.956566
4
Buldur B Güvendi ON . Conceptual modelling of the factors affecting oral health-related quality of life in children: A path analysis. Int J Paediatr Dent. (2020) 30:181–92. doi: 10.1111/ipd.12583
5
Enkling N Marwinski G Jöhren P . Dental anxiety in a representative sample of residents of a large German city. Clin Oral Investig. (2006) 10:84–91. doi: 10.1007/s00784-006-0035-6
6
Lahti S Vehkalahti MM Nordblad A Hausen H . Dental fear among population aged 30 years and older in Finland. Acta Odontol Scand. (2007) 65:97–102. doi: 10.1080/00016350601058085
7
Armfield JM Spencer AJ Stewart JF . Dental fear in Australia: who's afraid of the dentist? Aust Dent J. (2006) 51:78–85. doi: 10.1111/j.1834-7819.2006.tb00405.x
8
Buldur B . Pathways between parental and individual determinants of dental caries and dental visit behaviours among children: Validation of a new conceptual model. Community Dent Oral Epidemiol. (2020) 48:280–7. doi: 10.1111/cdoe.12530
9
Buldur B Armfield JM . Development of the Turkish version of the Index of Dental Anxiety and Fear (IDAF-4C+): Dental anxiety and concomitant factors in pediatric dental patients. J Clin Pediatr Dent. (2018) 42:279–86. doi: 10.17796/1053-4628-42.4.7
10
Vanhee T Mourali S Bottenberg P Jacquet W Vanden Abbeele A . Stimuli involved in dental anxiety: What are patients afraid of?: A descriptive study. Int J Paediatr Dent. (2020) 30:276–85. doi: 10.1111/ipd.12595
11
Bellingrath S Kudielka BM . Effort-reward-imbalance and overcommitment are associated with hypothalamus-pituitary-adrenal (HPA) axis responses to acute psychosocial stress in healthy working schoolteachers. Psychoneuroendocrinology. (2008) 33:1335–43. doi: 10.1016/j.psyneuen.2008.07.008
12
Pani L Porcella A Gessa GL . The role of stress in the pathophysiology of the dopaminergic system. Mol Psychiatry. (2000) 5:14–21. doi: 10.1038/sj.mp.4000589
13
The American Music Therapy Association (AMTA) . (2021). Available online at: www.musictherapy.org (Accessed 12 January 2024).
14
Kemper KJ Danhauer SC . Music as therapy. South Med J. (2005) 98:282–8. doi: 10.1097/01.SMJ.0000154773.11986.39
15
Wigram T Pedersen IN Bonde LO . A Comprehensive Guide to Music Therapy: Theory, Clinical Practice, Research and Training. London and Philadelphia: Jessica Kingsley Publishers (2002).
16
Ainscough SL Windsor L Tahmassebi JF . A review of the effect of music on dental anxiety in children. Eur Arch Paediatr Dent. (2019) 20:23–6. doi: 10.1007/s40368-018-0380-6
17
Aartman IH de Jongh A Makkes PC Hoogstraten J . Dental anxiety reduction and dental attendance after treatment in a dental fear clinic: a follow-up study. Community Dent Oral Epidemiol. (2000) 28:435–42. doi: 10.1034/j.1600-0528.2000.028006435.x
18
Page MJ McKenzie JE Bossuyt PM Boutron I Hoffmann TC Mulrow CD et al . The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
19
Institute of Medicine (US) Committee on Standards for Developing Trustworthy Clinical Practice Guidelines . Clinical Practice Guidelines We Can Trust. GrahamRMancherMMiller WolmanDGreenfieldSSteinbergE, editors. Washington (DC: National Academies Press (US (2011). doi: 10.17226/13058
20
Casagrande A Fabris F Girometti R . Beyond kappa: an informational index for diagnostic agreement in dichotomous and multivalue ordered-categorical ratings. Med Biol Eng Comput. (2020) 58:3089–99. doi: 10.1007/s11517-020-02261-2
21
Jadad AR Moore RA Carroll D Jenkinson C Reynolds DJ Gavaghan DJ et al . Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. (1996) 17:1–12. doi: 10.1016/0197-2456(95)00134-4
22
Minozzi S Dwan K Borrelli F Filippini G . Reliability of the revised Cochrane risk-of-bias tool for randomised trials (RoB2) improved with the use of implementation instruction. J Clin Epidemiol. (2022) 141:99–105. doi: 10.1016/j.jclinepi.2021.09.021
23
Dixit UB Jasani RR . Comparison of the effectiveness of Bach flower therapy and music therapy on dental anxiety in pediatric patients: A randomized controlled study. J Indian Soc Pedod Prev Dent. (2020) 38:71–8. doi: 10.4103/JISPPD.JISPPD_229_19
24
Sorribes De Ramón LA Ferrández Martínez AF García Carricondo AR Espín Gálvez F Alarcón Rodríguez R . Effect of virtual reality and music therapy on anxiety and perioperative pain in surgical extraction of impacted third molars. J Am Dent Assoc. (2023) 154:206–14. doi: 10.1016/j.adaj.2022.11.008
25
Kim YK Kim SM Myoung H . Musical intervention reduces patients' anxiety in surgical extraction of an impacted mandibular third molar. J Oral Maxillofac Surg. (2011) 69:1036–45. doi: 10.1016/j.joms.2010.02.045
26
Janthasila N Keeratisiroj O . Music therapy and aromatherapy on dental anxiety and fear: A randomized controlled trial. J Dent Sci. (2023) 18:203–10. doi: 10.1016/j.jds.2022.06.008
27
Yamashita K Kibe T Ohno S Kohjitani A Sugimura M . The effects of music listening during extraction of the impacted mandibular third molar on the autonomic nervous system and psychological state. J Oral Maxillofac Surg. (2019) 77:1153.e1–1153.e8. doi: 10.1016/j.joms.2019.02.028
28
Kayaaltı-Yüksek S Yıldırım S . Effect of Mozart's music on the learning of toothbrushing behavior in children with high and low dental anxiety levels. Clin Oral Investig. (2022) 26:5979–88. doi: 10.1007/s00784-022-04614-7
29
Thoma MV Zemp M Kreienbühl L Hofer D Schmidlin PR Attin T et al . Effects of music listening on pre-treatment anxiety and stress levels in a dental hygiene recall population. Int J Behav Med. (2015) 22:498–505. doi: 10.1007/s12529-014-9439-x
30
Wazzan M Estaitia M Habrawi S Mansour D Jalal Z Ahmed H et al . The effect of music therapy in reducing dental anxiety and lowering physiological stressors. Acta Biomed. (2022) 92:e2021393. doi: 10.23750/abm.v92i6.11668
31
Karapicak E Dulger K Sahin E Alver A . Investigation of the effect of music listened to by patients with moderate dental anxiety during restoration of posterior occlusal dental caries. Clin Oral Investig. (2023) 27:3521–30. doi: 10.1007/s00784-023-04966-8
32
Lahmann C Schoen R Henningsen P Ronel J Muehlbacher M Loew T et al . Brief relaxation versus music distraction in the treatment of dental anxiety: a randomized controlled clinical trial. J Am Dent Assoc. (2008) 139:317–24. doi: 10.14219/jada.archive.2008.0161
33
Mejía-Rubalcava C Alanís-Tavira J Mendieta-Zerón H Sánchez-Pérez L . Changes induced by music therapy to physiologic parameters in patients with dental anxiety. Complement Ther Clin Pract. (2015) 21:282–6. doi: 10.1016/j.ctcp.2015.10.005
34
Aravena PC Almonacid C Mancilla MI . Effect of music at 432 Hz and 440 Hz on dental anxiety and salivary cortisol levels in patients undergoing tooth extraction: a randomized clinical trial. J Appl Oral Sci. (2020) 28:e20190601. doi: 10.1590/1678-7757-2019-0601
35
Kupeli I Gülnahar Y . Comparing different music genres in decreasing dental anxiety in young adults who underwent third molar surgery in Turkey: randomized controlled trial. J Oral Maxillofac Surg. (2020) 78:546.e1–7. doi: 10.1016/j.joms.2019.11.029
36
Gulnahar Y Kupeli I . Effect of different kinds of music on anxiety during implant surgery in Turkey: randomized controlled study. Int J Oral Maxillofac Implants. (2020) 35:762–6. doi: 10.11607/jomi.8329
37
Esteban Pellicer LÁ Conde Villar AJ Martínez Rubio JL Casañas E Estévez Luaña R . Can music decrease anxiety and pain during dental implant surgery? A Randomized Clin TrialJ Oral Maxillofac Surg. (2023) 81:194–200. doi: 10.1016/j.joms.2022.10.004
38
Boyle CA Newton T Milgrom P . Who is referred for sedation for dentistry and why? Br Dent J. (2009)206:E12. doi: 10.1038/sj.bdj.2009.251
39
Sheikh H . CAEP dental care statement. CJEM. (2020) 22:36–9. doi: 10.1017/cem.2019.437
40
Casarin J Cromi A Sgobbi B Di Siena A Serati M Bolis ME et al . Music therapy for preoperative anxiety reduction in women undergoing total laparoscopic hysterectomy: A randomized controlled trial. J Minim Invasive Gynecol. (2021) 28:1618–1624.e1. doi: 10.1016/j.jmig.2021.02.002
41
Jiménez-Jiménez M García-Escalona A Martín-López A De Vera-Vera R De Haro J . Intraoperative stress and anxiety reduction with music therapy: a controlled randomized clinical trial of efficacy and safety. J Vasc Nurs. (2013) 31:101–6. doi: 10.1016/j.jvn.2012.10.002
42
Nilsson U . The effect of music intervention in stress response to cardiac surgery in a randomized clinical trial. Heart Lung. (2009) 38:201–7. doi: 10.1016/j.hrtlng.2008.07.008
43
Bradt J Dileo C Shim M . Music interventions for preoperative anxiety. Cochrane Database Syst Rev. (2013) 2013:CD006908. doi: 10.1002/14651858.CD006908.pub2
44
Bringman H Giesecke K Thorne A Bringman S . Relaxing music as pre-medication before surgery: A randomised controlled trial. Acta Anaesthesiologica Scandinavica. (2009) 53:759–64. doi: 10.1111/j.1399-6576.2009.01969.x.
45
de Witte M Pinho ADS Stams GJ Moonen X Bos AER van Hooren S . Music therapy for stress reduction: a systematic review and meta-analysis. Health Psychol Rev. (2022) 16:134–59. doi: 10.1080/17437199.2020.1846580
46
Miyata K Odanaka H Nitta Y Shimoji S Kanehira T Kawanami M et al . Music before dental surgery suppresses sympathetic activity derived from preoperative anxiety: A randomized controlled trial. JDR Clin Trans Res. (2016) 1:153–62. doi: 10.1177/2380084416650613
47
Packyanathan JS Lakshmanan R Jayashri P . Effect of music therapy on anxiety levels on patient undergoing dental extractions. J Family Med Prim Care. (2019) 8:3854–60. doi: 10.4103/jfmpc.jfmpc_789_19
48
Maulina T Djustiana N Shahib MN . The effect of music intervention on dental anxiety during dental extraction procedure. Open Dent J. (2017) 11:565–72. doi: 10.2174/1874210601711010565
49
Glienke K Piefke M . Stress-related cortisol responsivity modulates prospective memory. J Neuroendocrinol. (2017) 29(12). doi: 10.1111/jne.12544
50
Shurrab MY . Antimicrobial efficiency of some antiseptic products on endodontic microflora isolated from gangrenous pulp tissue. J Contemp Dent Pract. (2006) 7:53–62. doi: 10.5005/jcdp-7-4-53.
51
Paños-Crespo A Traboulsi-Garet B Sánchez-Garcés MÁ Gay-Escoda C . Disinfection of the air and surfaces in the dental clinic using hydroxyl radical (OH-) based technology: a systematic review. J Clin Exp Dent. (2023) 15:e494–504. doi: 10.4317/jced.60461
Summary
Keywords
dental anxiety, dental fear, dental phobia, stress, music therapy, randomized clinical trial, meta-analysis
Citation
López-Valverde N, López-Valverde A, Macedo de Sousa B and Blanco Rueda JA (2024) Efficacy of music therapy on stress and anxiety prior to dental treatment: a systematic review and meta-analysis of randomized clinical trials. Front. Psychiatry 15:1352817. doi: 10.3389/fpsyt.2024.1352817
Received
08 December 2023
Accepted
30 January 2024
Published
23 February 2024
Volume
15 - 2024
Edited by
Mahire Olcay Çam, Ege University, Türkiye
Reviewed by
Burak Buldur, Cumhuriyet University, Türkiye
Badii Amamou, University of Monastir, Tunisia
Updates
Copyright
© 2024 López-Valverde, López-Valverde, Macedo de Sousa and Blanco Rueda.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Antonio López-Valverde, alopezvalverde@usal.es
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.