- 1Department of Clinical Psychology, Jiangsu Province Hospital and The First Affiliated Hospital with Nanjing Medical University, Nanjing, China
- 2Department of Psychiatry, Nanjing Meishan Hospital, Nanjing, China
- 3Chinese Academy of Sciences (CAS) Key Laboratory of Mental Health, Institute of Psychology, Chinese Academy of Sciences, Beijing, China
Background: This study aimed to identify socio-demographic, physiologic, and psychologic related factors of the first-time suicide attempt (FSA) in the past 14 days in Chinese adult patients with first-episode drug-naïve (FEDN) major depressive disorder (MDD).
Methods: A total of 1718 adult patients with FEDN MDD were enrolled in this cross-sectional survey. Depression, anxiety symptoms, and suicide attempts were assessed. Additionally, biological samples were collected and measured, while Logistic regression analysis was employed to explore the risk factors for FSA in the past 14 days among FEDN MDD patients.
Results: Among suicide attempters, 12.11% (208 out of 1718) reported experiencing FSA in the past 14 days. Logistic regression analysis showed that the risk factors for FSA included more severe anxiety symptoms (OR=1.37, 95%CI: 1.28-1.48, p<0.001), higher levels of total cholesterol (TC) (OR=1.42, 95%CI: 1.13-1.77, p=0.003), and elevated thyroid-stimulating hormone (TSH) (OR=1.13, 95%CI: 1.03-1.25, p=0.01). The regression model exhibited good discriminatory power for FSA with an area under the curve (AUC) of 0.82.
Conclusion: FEDN MDD patients with more severe anxiety and higher levels of TSH and TC are more likely to develop FSA in the past 14 days. These factors are risk factors for short-term (in the past 14 days) FSA and may serve as indicators for early intervention.
1 Introduction
Major depressive disorder (MDD) is a mental disorder in which low mood and anhedonia persist for at least two weeks to a distressing or disabling degree (1). According to the World Health Organization (WHO) reports, MDD was one of the top 10 leading causes of disability-adjusted life years (DALYs) among people aged 10-49 in 2019 (2). Suicidal behaviors, an intentional self-inflicted act that ends in death, are one of the recognized diagnostic criteria for MDD in the DSM-5 (3). Suicide is the most severe symptom of MDD patients and may or may not be fatal (4, 5). Up to 50% of people with MDD report suicidal thoughts or suicide attempts (3, 6). People with MDD have a 20-fold higher risk of suicide attempts (7), and they are three times more likely to suicide (8).
A number of factors have been recognized as possible risk factors for suicide. According to a meta-analysis, various confounding factors such as low age, female, underweight or obesity, a longer duration of illness, and comorbid psychiatric or somatic symptoms were identified as risk factors for suicide attempts (9–11). Studies have also shown that a history of suicide attempts increases the risk of suicide, and serves as one of the strongest factors of impending suicide attempts (12–15). Therefore, it is critical to explore the first-time suicide attempt (FSA).
It is estimated that up to 13% of people with MDD who have made a non-fatal suicide attempt later die by suicide (3). 1.6% of suicide attempters die by suicide within 12 months, and 3.9% of them die by suicide within five years (16). In the first month following an emergency department visit for a psychiatric problem, 12.9% of people with MDD have attempted suicide (17). Approximately 40% of those who die by suicide have visited a physician one month before death. Of these, 20% have visited a physician one week before death (18, 19). According to a recent meta-analysis of suicide risk studies over the past 50 years, they mostly focused on predicting suicide attempts in the next 12-24 months, with less than 1% on predicting suicide attempts in the next 30 days (20). Risk factors for suicide attempts have been explored over a long term (i.e., over a lifetime or the past year), but clinicians are still frequently asked to assess the suicide risk in the near term (17).
In recent decades, researchers have attempted to identify biomarkers associated with suicide attempts, such as cholesterol levels, thyroid hormones, and impaired fasting glucose (21–23). The median time from the last psychiatric outpatient visit to the death is 18 days (24). Therefore, identifying possible biomarkers of FSA within 14 days of MDD onset is critical to prevention and treatment. In this study, different from previous studies, FSA was focused on the past 14 days.
To the best of our knowledge, this study was the first to explore FSA in the past 14 days in patients with first-episode drug-naïve (FEDN) MDD. Notably, investigating FEDN MDD patients offers distinct advantages of minimizing confounding factors such as antidepressant effects, long-term medication use, and associated medical and psychiatric complications. The objectives of this study were to (1) comprehensively analyze the occurrence and clinical characteristics of FSA in FEDN MDD patients over 14 days, and (2) identify key factors significantly associated with FSA in the past 14 days in patients with FEDN MDD.
2 Methods
2.1 Participants and settings
The protocol of this cross-sectional study was approved by the Institutional Review Board (IRB) of the First Hospital of Shanxi Medical University (ID No. 2016-Y27). All 1718 patients were consecutively recruited from the psychiatric outpatient clinic between September 2016 and December 2018, and they were all informed about this study and voluntarily signed an informed consent form.
Inclusion criteria included: (1) patients aged 18-60 years old and of Han people; (2) those who were assessed and diagnosed at enrollment by two trained and experienced clinical psychiatrists based on the diagnostic interview of the Structured Clinical Interview for DSM-IV (SCID); (3) those with first-episode depressive symptoms and a HAMD-17 score of ≥24; (4) those who never received psychotropic medication; (5) those who provided written informed consent prior to participation and were able to participate in the clinical assessment.
Exclusion criteria included: (1) patients comorbid with a serious condition, such as organic brain disease, cancer, epilepsy, brain injury, stroke, or persistent infections that required immediate medical attention (n = 9); (2) those with Axis I psychiatric disorders other than MDD, such as bipolar disorder and schizophrenia (n = 15); (3) those with substance dependence other than tobacco use (n = 9); (4) pregnant or breastfeeding women (n = 10); (5) those who refused to provide written informed consent (n = 21); and other unspecified factors (n = 14). Finally, 78 patients were excluded from the research.
2.2 Socio-demographic and general information
Detailed socio-demographic information including age, gender, time of onset, duration of illness, educational level and marital status was collected by questionnaire. In addition, we assessed patients’ body mass index (BMI), diastolic blood pressure (DBP) and systolic blood pressure (SBP). After at least 15 minutes of rest in a sitting posture, the right arm’s SBP and DBP were calculated by averaging two measurements with a conventional mercury sphygmometer. Each patient provided standard anthropometric measurements of their weight (kg) and height (m) to calculate their BMI using the formula: BMI = weight/(height)2.
2.3 Clinical measures
The 17-item Hamilton Rating Scale (HAMD-17) was used in the study to assess the severity of depression, with a higher score indicating more severe depressive symptoms (25). The Hamilton Anxiety Rating Scale (HAMA) was used to evaluate anxiety symptoms, with a higher score indicating more severe anxiety symptoms (26). The positive subscale of the Positive and Negative Syndrome Scale (PANSS) was used to measure psychotic symptoms. Subjects who scored more than 15 points were considered to have psychotic symptoms (27, 28). Two psychiatrists participated in pre-survey training about the HAMD, HAMA, and PANSS to ensure the reliability and consistency of scores on these scales throughout the study. Repeated assessments after the training showed interrater correlation coefficients for the total scores of the HAMD, HAMA, and PANSS > 0.8.
2.4 Suicide attempts
Suicide attempt is a potentially self-injurious behavior (29), which should also incorporate a high likelihood of death as well as a true intent to kill oneself (30). Information on suicide attempts was collected through face-to-face interviews, in which all participants were asked the same question: “Have you ever attempted suicide in your life?” In case of an affirmative response, they were further asked about their prior suicidal behavior, including the following questions: “When, in what way, and how many times did you attempt suicide?”. If the answers were ambiguous, the researchers would conduct additional interviews with the patient’s family members or clinicians for confirmation. Based on whether or not they had tried suicide attempts in the time frame prior to the last 14 days, we divided patients into those with and without a history of suicide. We focused on patients who had not previously attempted suicide but had their first-time suicide attempt (FSA) in the past 14 days.
2.5 Blood samples
Blood samples were collected from each patient between 6:00 a.m. and 8:00 a.m. following an overnight fast, and immediately sent to the Laboratory Center of the First Hospital of Shanxi Medical University before 11:00 a.m. on the same day. Then the biomarkers including total cholesterol (TC), high-density lipoproteins (HDL), triglycerides (TG), low-density lipoproteins (LDL), free tri-iodothyronine (FT3), free thyroxine (FT4), thyroid-stimulating hormone (TSH), thyroid peroxidase antibody (TPOAb), anti-thyroglobulin antibody (TgAb) and fasting blood glucose (FBG) were measured by a BECKMAN AU5800 system (Beckman Coulter, Brea, California, USA).
2.6 Statistical analysis
SPSS25.0 was used for statistical analysis. p < 0.05 was considered a statistically significant difference.
The prevalence of suicide attempts in patients with MDD was expressed as a percentage. To compare demographic and clinical factors, analysis of variance (ANOVA) and χ2 test were performed. Non-normally distributed rank-ordered variables were compared by the Mann-Whitney U test. On this basis, binary Logistic regression analysis was used to identify variables that had a significant effect on FSA. Bonferroni correction was used to adjust for multiple tests. A variance inflation factor (VIF) was used to measure multicollinearity among independent variables. A VIF > 5 showed multicollinearity, which was not accounted for in the final model. The multivariate model included variables in Table 1 with P < 0.1. The discriminatory power of the regression model for FSA was determined by receiver operating characteristic (ROC) analysis. The area under the curve (AUC) was interpreted according to the classification of Hosmer et al. (0.5 = no differentiation; 0.51-0.69 = poor; 0.7-0.79 = acceptable; 0.8-0.89 = excellent; ≥0.9 = superior) (31).
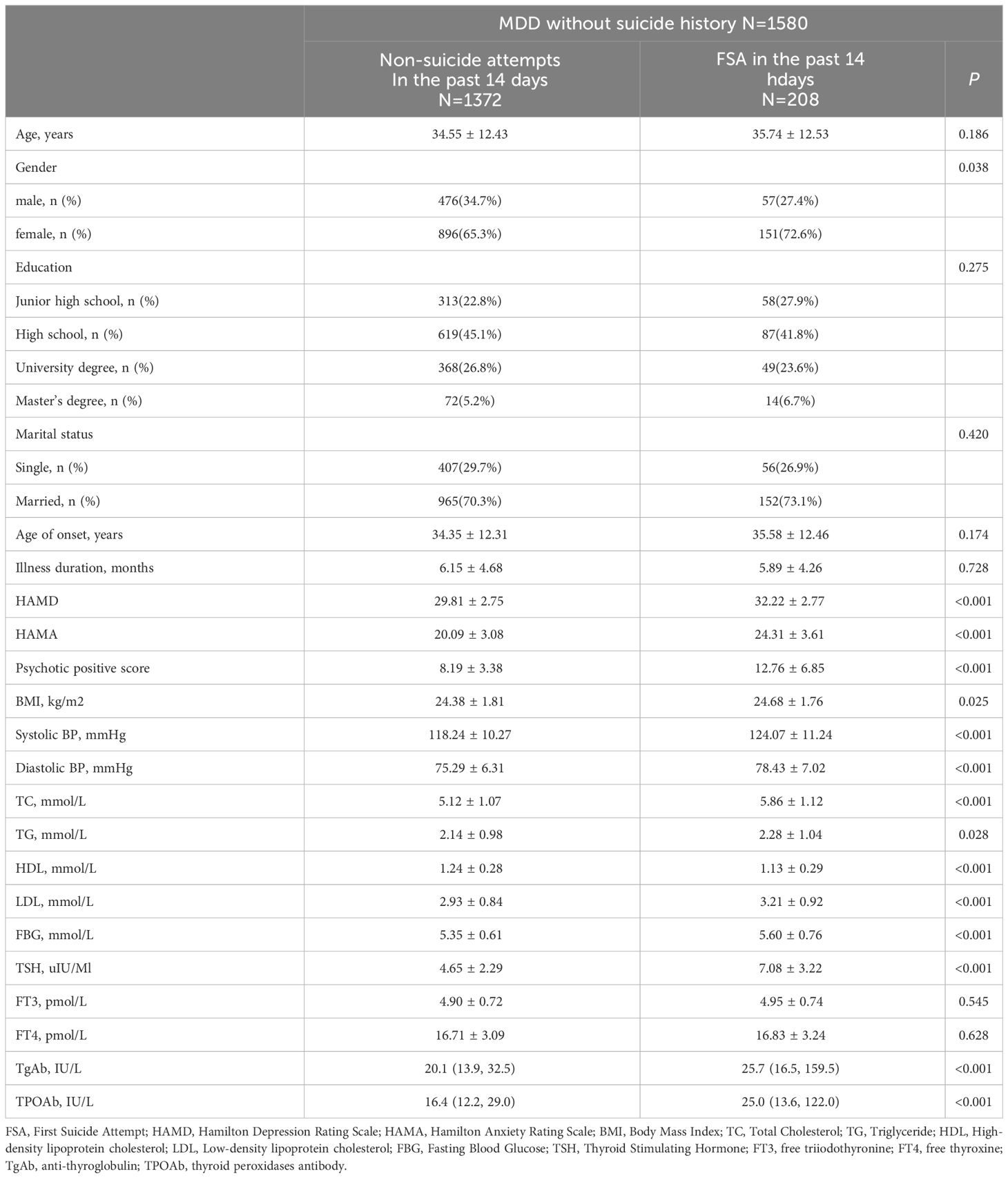
Table 1 Socio-demographic and clinical characteristics among FEDN MDD without suicide history before the past 14 days.
3 Results
A total of 1718 patients with FEDN MDD were recruited, with a mean age of (34.9 ± 12.4) years and a mean duration of illness of (6.4 ± 4.7) months, of whom 588 were males and 1130 were females. Of these, 138 had a history of suicide, and 1,580 had no history of suicide in the time frame prior to the past 14 days. The most recent suicide attempt occurred the day before the interview, while the most distant suicide attempt occurred more than a year ago. The largest number of suicide attempts was four.
3.1 Prevalence of suicide attempts among FEDN MDD patients with and without a history of suicide attempts
We observed that 20.1% (346/1718) of patients with FEDN MDD attempted suicide, with 13.68% (235/1718) occurring in the past 14 days, and 12.11% (208/1718) being FSA. Patients with a history of suicide attempts had higher HAMA and HAMD scores than those without a history of suicide attempts (p < 0.0001).
The prevalence of suicide attempts in the past 14 days was higher in patients with a history of suicide attempts (n = 27, 19.6%) than in those without a history of suicide attempts (n = 208, 13.2%) (χ2 = 4.40, p < 0.05, OR = 1.60, 95% CI: 1.03-2.50). After controlling for HAMA and HAMD scores, FEDN MDD patients with a history of suicide attempts had an 11-fold higher risk of suicide attempts in the past 14 days than those without a history of suicide attempts (β = 2.43, Wald = 58.91, p < 0.0001, OR = 11.3, 95% CI: 6.09-21.00).
Compared to patients without suicide attempts, those with FSA in the past 14 days had significantly greater symptoms of depression, anxiety, and positive psychotic symptoms, as well as higher levels of blood pressure (SBP, DBP), BMI, lipids (TC, TG, HDL, LDL), thyroid hormones (TSH, TgAb, TPOAb), and FBG (p < 0.05). After Bonferroni correction, no significant differences were found between the groups in terms of gender, educational level, and marital status (p > 0.05).
3.2 Clinical characteristics and biochemical parameters of patients who attempted suicide in the past 14 days versus those who did not attempt suicide among those without a history of suicide attempts
Descriptive statistics of socio-demographic data and clinical variables of those who attempted suicide in the past 14 days versus those who did not attempt suicide among FEDN MDD patients without a history of suicide attempts are presented in Table 1. Depression, anxiety and positive symptoms were significantly greater, and blood pressure (SBP, DBP), BMI, lipids (TC, TG, HDL, LDL), thyroid hormones (TSH, TgAb, TPOAb), and FBG were all higher in patients with FSA in the past 14 days than those who did not attempt suicide (p < 0.05). After Bonferroni correction, there were no significant differences between the groups in terms of gender, educational level and marital status.
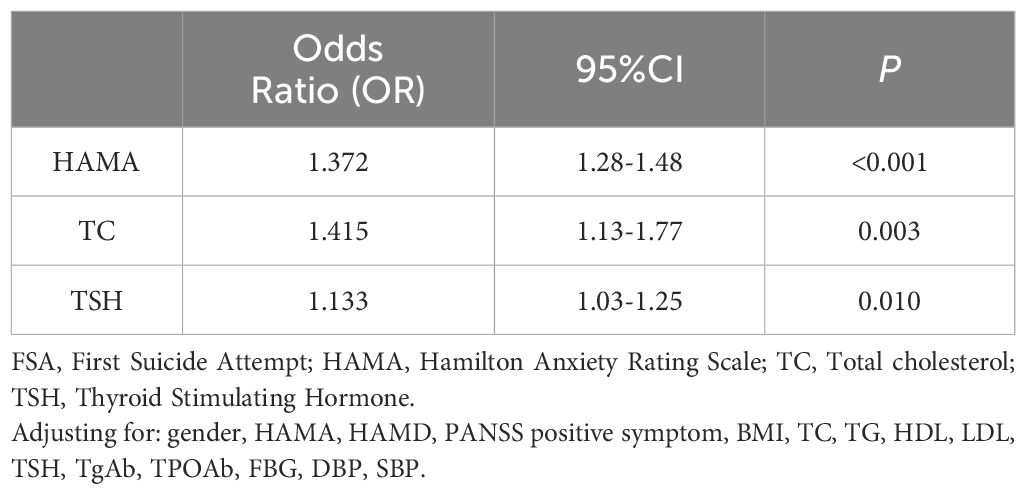
3.3 Risk factors for FSA in the past 14 days in patients with FEDN MDD
The results of binary Logistic regression analysis showed that more severe anxiety symptoms (OR = 1.37, 95% CI: 1.28-1.48, p < 0.001), higher levels of TC (OR = 1.42, 95% CI: 1.13-1.77, p = 0.003), and elevated TSH (OR = 1.13, 95% CI: 1.03-1.25, p = 0.010) were significant independent risk factors for FSA in the past 14 days in patients with FEDN MDD (Table 2).
Additionally, the AUC revealed the optimal threshold values for HAMA score, TSH, and TC to differentiate FSA in the past 14 days. The optimal threshold value of the HAMA score was 22.5 (AUC: 0.81; 95% CI: 0.78-0.84), with a sensitivity of 67.3% and a specificity of 79.6%. The optimal threshold value of TSH was 6.60 (AUC: 0.72; 95% CI: 0.68-0.77), with a sensitivity and specificity of 62% and 81.1%, respectively. The optimal threshold value of TC was 5.68 (AUC: 0.69; 95% CI: 0.65-0.73), with a sensitivity and specificity of 55.8% and 71.9%, respectively. Finally, it was found that the combination of HAMA score, TC, and TSH level was the most effective in differentiating FSA in the past 14 days, with an AUC of 0.82 (95% CI: 0.79-0.85) (Figure 1).
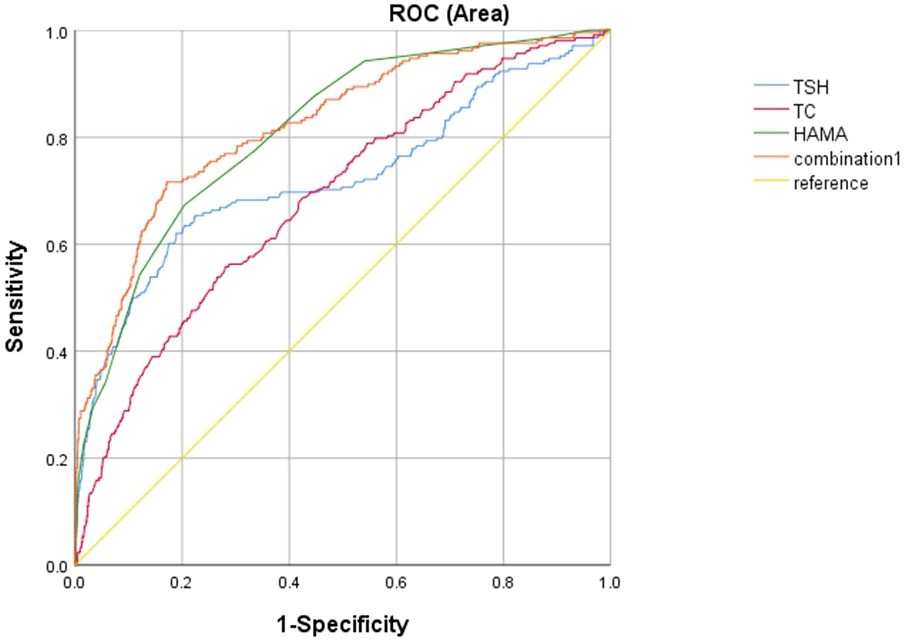
Figure 1 The discriminatory power of related factors for distinguishing patients with FSA in MDD in the past 14 days. The area under the curve of HAMA score, TSH, TC and the combination of these factors were 0.81, 0.72, 0.69, and 0.82, respectively. FSA, First Suicide Attempt; TSH, Thyroid Stimulating Hormone; TC, Total Cholesterol; HAMA, Hamilton Anxiety Rating Scale.
4 Discussion
This study is the first to investigate the prevalence of FSA in the past 14 days and its associated factors in patients with FEDN MDD. Identifying individuals at risk of short-term suicide poses a significant challenge for clinical professionals and is of paramount importance. This study aimed to identify variables that differentiate between FEDN MDD patients with FSA in the past 14 days and those who did not attempt suicide. It was found that (1) 20.1% (346/1718) of FEDN MDD patients attempted suicide, of which 13.68% (235/1718) occurred in the past 14 days and 12.11% (208/1718) were FSA; (2) MDD patients with a history of suicide attempts were approximately 11 times more likely to attempt suicide in the past 14 days than those without a history of suicide attempts; (3) more severe anxiety symptoms, higher levels of TC, and TSH in patients with FEDN MDD were associated with a higher risk of FSA in the past 14 days. The combination of HAMA score, TC, and TSH level was the most effective in differentiating FSA in the past 14 days (AUC = 0.82).
The above results suggest that a 14-day window is critical. To date, only a few cross-sectional studies have reported the prevalence of short-term suicide attempts in patients with MDD. For example, Mash et al. reported that 2.6% of soldiers with MDD attempted suicide without suicidal thoughts, 16.2% of which occurred within 30 days. Among soldiers with documented suicidal thoughts, 7.4% attempted suicide, with 46.3% occurring within 30 days (32, 33). In Brazil, Brunon et al. found that 0.67% of participants had suicidal thoughts in the week prior to the interview (34). A China-based meta-analysis revealed that 20.3% of participants had attempted suicide one month before the interview (35). The prevalence of suicide attempts in previous studies varied for several reasons. First, little data are available on specific time windows related to suicidal behaviors (36). Many studies focused on suicide attempts over a long term (i.e., over a lifetime or the past year) (12). Second, there is no universally agreed upon definition of acute or chronic suicide (i.e., subsequent hours, days, weeks, or months) (12). Third, cultural and sample differences may exist. It was found that MDD patients with a history of suicide attempts were approximately 11 times more likely to attempt suicide in the last 14 days than those without a history of suicide attempts. A history of suicide attempts strongly predicts future suicide attempts or suicide deaths (37–43). According to systematic reviews and meta-analyses, adults with a history of suicide attempts have a ten-fold higher risk of suicide compared to normal people (44). MDD patients with a history of suicide attempts have a 4.84-fold higher risk of suicide than those without a history of suicide attempts (19). Sohn et al. predicted the 6-month suicide attempt rates and found that patients with a history of suicide attempts have a higher risk of suicide (OR = 2.99) (45). A history of suicide attempts was also incorporated in the final multivariate model predicting the risk of suicide in adolescents within three months (46). These studies suggest that individuals with a history of suicide attempts are more likely to attempt suicide in the long or short term. Therefore, it is critical to analyze the risk of FSA in patients with MDD.
Among MDD patients without a history of suicide attempts, the risk factors for FSA in the past 14 days were explored. It was found that more severe anxiety symptoms and higher levels of TC and TSH might contribute to short-term suicide (14 days). MDD patients with anxiety symptoms were more prone to suicide attempts, consistent with the results of several previous studies (19, 47–49). Mood disorders strongly predict future suicide attempts (50). MDD and anxiety disorders are common co-occurring psychiatric disorders (48). Patients with mild, moderate, or severe anxiety symptoms are at greater risk of suicide (49), and anxiety symptoms are more prevalent in patients with MDD who attempt suicide (3). Some researchers have suggested that the presence of depressive symptoms influences suicide attempts among patients with anxiety disorders (51). In a population-based survey, Sareen et al. conducted two follow-up assessments one year after baseline and three years after baseline, respectively. They found that a history of anxiety disorders is a unique risk factor for future suicide attempts, and MDD patients with anxiety disorders have a 4.15-fold increased risk of suicide attempts compared to those without anxiety disorders (47). In this study, anxiety remained an independent risk factor for FSA in the past 14 days in patients with MDD.
MDD patients with higher TC levels were more likely to undergo FSA in the past 14 days. In recent years, there have been an increasing number of studies on biomarkers associated with suicidal behavior, and lipid levels have emerged as a potential factor in this regard (52–55). Metabolic syndrome is common in patients with MDD, and it is associated with suicide attempts (56). One theory suggests that serum lipid levels play a crucial role in the pathogenesis of suicide; high levels of serum TC increase the risk of violent suicide (52). Higher levels of TC are associated with a higher risk of suicide in adult women (57, 58), irrespective of menopause status (59). Zhou et al. revealed that TC levels may be discovered as a potential and valuable biomarker for first-episode MDD suicide risk within two weeks (60). A recent study showed that patients with suicide attempts had higher LDL and TC but lower HDL in FEDN MDD patients (10). The underlying association mechanisms between serum cholesterol and suicide are still unclear. Surace et al. reported that higher total cholesterol blood levels may be linked to an increased risk of self-harm through the pro-inflammatory state that directly affects the brain (61). Comings et al. found that higher levels of blood cholesterol were connected to polymorphisms in the serotonin transporter gene (HTT, SLC6A4) (62), which were associated with suicidal behavior (63). Penttinen et al. hypothesized that elevated cytokine production, particularly interleukin-2 (IL-2), contributes to higher total blood cholesterol and reduced HDL cholesterol, subsequently influencing melatonin release and elevating impulsivity and suicide risk (64). Brunner et al. speculated that patients with higher cholesterol may exhibit maladaptive nutritional behaviors (such as binge eating), which was associated with suicide attempts (65).
However, different findings have been reported in other studies. For example, an association has been observed between depressive symptoms and low plasma TC levels, and low levels of TC are associated with suicide and violent death (66). Additionally, low levels of TC lead to an increased risk of suicide in patients with mental illness (67). A meta-analysis revealed that individuals with lower serum TC levels are more prone to suicidal behavior (53). A follow-up study showed that lower total cholesterol levels were significant predictors of suicide re-attempts (68). Some studies reported no association between serum cholesterol and recent suicide attempts (occurring within 72 hours before hospital admission), either violent or nonviolent (69, 70). Research including 11,653 Korean participants found that men’s depression was associated with higher triglycerides. However, there was no obvious effect of the blood lipid variables on suicidal thoughts (71). It’s important to note that drugs were used in these studies, which may have impacted the results. We recruited first-episode and drug-naïve young MDD patients to avoid the influence of many confounding factors, and this may partially explain the differences between our findings and other studies. Several other factors may account for these differences. First, different populations, genders, and ages in each study may lead to differences in findings. Cho et al. suggested that the relationship between lipids and suicide varies by age (72). Second, lipid levels fluctuate across different stages of illness. Lipid levels are lower during acute episodes of depression but increase during periods of remission (73). Some previous studies on suicide did not consider the time window, so the relationship between lipid levels and suicide appeared to vary greatly depending on the stage of MDD. Third, serum TC levels are not a reliable marker of lipid content in the brain (74). Finally, further study is needed to determine the association between TC and suicide attempts.
This study showed that elevated TSH levels in patients with MDD were associated with an increased prevalence of FSA in the past 14 days, consistent with many previous studies (75–78). A China-based study involving FEDN MDD patients found that the levels of serum TSH and TC are statistically higher in suicide attempters than in non-suicide attempters (76). Another study reported that 179 adolescents with MDD who attempted suicide had higher TSH levels, consistent with our findings, and that TSH levels are a significant predictor of suicide attempts, with an adjusted OR of 5.14 (77). Among participants with suicide attempts, there was a substantial correlation between suicide attempts and higher TSH levels (79). Furthermore, a systematic review and meta-analysis confirmed the association between higher TSH levels and suicidal behavior (75). However, some studies reported no difference in TSH levels between individuals with and without suicidal behavior (80, 81). There are several possible explanations for the inconsistency among previous studies. First, the sample sizes varied widely, ranging from 179 to 1279 subjects. Second, the sampling time was different. Some studies collected blood samples within 24 hours after suicide attempts (80), whereas some did not mention the specific time of blood collection. Therefore, future investigations are needed.
This study exhibits several strengths. First, this study used a relatively large sample size to minimize the impact of extreme data on trial results. Second, this study recruited drug-naïve MDD patients who were first-episode. Compared to previous studies, our study can relatively reduce the interference of confounding variables on FSA, such as drugs, course of disease, and comorbidities. Third, we focused on first-time suicide attempts, which made the correlation results more accurate and avoided the impact of the duration from suicide attempt to blood sampling.
However, it’s essential to acknowledge the limits of this research. First, the patients in this study were all Han people recruited from outpatient clinics; hence, it is imperative to validate our findings across diverse populations, encompassing distinct ethnicities and clinical profiles. Second, this case-control study could not determine the causal relationship between associated factors and suicide attempts in patients with MDD. Prospective cohort studies are needed to confirm our results. Third, suicide attempts were determined by interview, rather than a structured assessment tool. In addition, the data collected focused solely on suicide attempts without capturing information regarding suicidal thoughts or ideation. Despite these limitations, this study is the first to evaluate suicide attempts over a brief period of time (in the past 14 days), thereby providing valuable insights into the precise association.
5 Conclusion
In summary, the results of this study are essential for identifying at-risk populations for suicide attempts and making timely and appropriate clinical decisions and interventions. More severe anxiety and higher levels of TC and TSH may be risk factors for FSA in the past 14 days in patients with MDD. Future studies should focus on the changes in variables involved in the transition from no suicide risk to suicide attempts and create predictive algorithms as clinical aids to better identify patients with MDD who are at high risk of suicide. By analyzing data from a variety of sources, we hoped to provide clinicians with more valuable information for decision-making and improve prognosis. Understanding the factors contributing to FSA is critical to developing effective interventions for patients with MDD.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The protocol of this cross-sectional study was approved by the Institutional Review Board (IRB) of the First Hospital of Shanxi Medical University (ID No. 2016-Y27). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
XC: Conceptualization, Data curation, Formal Analysis, Investigation, Writing – original draft, Writing – review & editing, Methodology. XZ: Resources, Supervision, Writing – review & editing. TZ: Data curation, Investigation, Writing – review & editing. RB: Data curation, Investigation, Writing – review & editing. YL: Investigation, Writing – review & editing. JL: Funding acquisition, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Medical Science and Technology Development Foundation, Nanjing Department of Health (Nos. YKK21216, YKK20184, YKK22264). The funding sources of this study had no role in study design, data collection and analysis, decision to publish, or preparation of the article.
Acknowledgments
The authors thank the First Clinical Medical College, Shanxi Medical University for the supports. We would like to clarify that the research project is a collaborative effort between the Institute of Psychology, Chinese Academy of Sciences, and the Department of Psychiatry at the First Hospital of Shanxi Medical University. It was agreed upon by both parties that the data collected could be shared and utilized for publications by either institution independently.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Drevets WC, Wittenberg GM, Bullmore ET, Manji HK. Immune targets for therapeutic development in depression: towards precision medicine. Nat Rev Drug Discovery. (2022) 21:224–44. doi: 10.1038/s41573-021-00368-1
2. Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
3. Lundberg J, Cars T, Lampa E, Ekholm Selling K, Leval A, Gannedahl A, et al. Determinants and outcomes of suicidal behavior among patients with major depressive disorder. JAMA Psychiatry. (2023) 340:732–42. doi: 10.1001/jamapsychiatry.2023.2833
4. Wang J, Sumner SA, Simon TR, Crosby AE, Annor FB, Gaylor E, et al. Trends in the incidence and lethality of suicidal acts in the United States 2006 to 2015. JAMA Psychiatry. (2020) 77:684–93. doi: 10.1001/jamapsychiatry.2020.0596
5. Ye G, Li Z, Yue Y, Wu Y, Yang R, Wang H, et al. Suicide attempt rate and the risk factors in young, first-episode and drug-naive Chinese Han patients with major depressive disorder. BMC Psychiatry. (2022) 22:612. doi: 10.1186/s12888-022-04254-x
6. Sokero TP, Melartin TK, Rytsala HJ, Leskela US, Lestela-Mielonen PS, Isometsa ET. Suicidal ideation and attempts among psychiatric patients with major depressive disorder. J Clin Psychiatry. (2003) 64:1094–100. doi: 10.4088/jcp.v64n0916
7. Osby U, Brandt L, Correia N, Ekbom A, Sparen P. Excess mortality in bipolar and unipolar disorder in Sweden. Arch Gen Psychiatry. (2001) 58:844–50. doi: 10.1001/archpsyc.58.9.844
9. Liu Z, Sun L, Zhang Y, Wang J, Sun F, Zhang Z, et al. The prevalence of underweight and obesity in Chinese children and adolescents with major depressive disorder and relationship with suicidal ideation and attempted suicide. Front Psychiatry. (2023) 14:1130437. doi: 10.3389/fpsyt.2023.1130437
10. Song X, Liu X, Zhou Y, Zhang X. Prevalence and correlates of suicide attempts in young patients with first-episode and drug-naive major depressive disorder: A large cross-sectional study. J Affect Disord. (2023) 340:340–6. doi: 10.1016/j.jad.2023.08.006
11. Su Y, Ye C, Xin Q, Si T. Major depressive disorder with suicidal ideation or behavior in Chinese population: A scoping review of current evidence on disease assessment, burden, treatment and risk factors. J Affect Disord. (2023) 340:732–42. doi: 10.1016/j.jad.2023.08.106
12. Glenn CR, Nock MK. Improving the short-term prediction of suicidal behavior. Am J Prev Med. (2014) 47:S176–180. doi: 10.1016/j.amepre.2014.06.004
13. Klonsky ED, Dixon-Luinenburg T, May AM. The critical distinction between suicidal ideation and suicide attempts. World Psychiatry. (2021) 20:439–41. doi: 10.1002/wps.20909
14. Force U. S. P. S. T., Mangione CM, Barry MJ, Nicholson WK, Cabana M, Chelmow D, et al. Screening for depression and suicide risk in children and adolescents: US preventive services task force recommendation statement. JAMA. (2022) 328:1534–42. doi: 10.1001/jama.2022.16946
15. Toll A, Pechuan E, Berge D, Legido T, Martinez-Sadurni L, El-Abidi K, et al. Factors associated with suicide attempts in first-episode psychosis during the first two years after onset. Psychiatry Res. (2023) 325:115232. doi: 10.1016/j.psychres.2023.115232
16. Olfson M, Wall M, Wang S, Crystal S, Gerhard T, Blanco C. Suicide following deliberate self-harm. Am J Psychiatry. (2017) 174:765–74. doi: 10.1176/appi.ajp.2017.16111288
17. Nock MK, Millner AJ, Ross EL, Kennedy CJ, Al-Suwaidi M, Barak-Corren Y, et al. Prediction of suicide attempts using clinician assessment, patient self-report, and electronic health records. JAMA Netw Open. (2022) 5:e2144373. doi: 10.1001/jamanetworkopen.2021.44373
18. Pirkis J, Burgess P. Suicide and recency of health care contacts. A systematic review. Br J Psychiatry. (1998) 173:462–74. doi: 10.1192/bjp.173.6.462
19. Hawton K, Casanas ICC, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. (2013) 147:17–28. doi: 10.1016/j.jad.2013.01.004
20. Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, et al. Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychol Bull. (2017) 143:187–232. doi: 10.1037/bul0000084
21. Chen SW, Li X, Lang X, Li J, Zhang XY. Metabolic parameters and thyroid hormones in relation to suicide attempts in patients with first-episode and drug-naive major depressive disorder with comorbid glucose disturbances: a large cross-sectional study. Eur Arch Psychiatry Clin Neurosci. (2023) 273:199–207. doi: 10.1007/s00406-022-01490-w
22. Kang HJ, Kim JW, Kim SW, Han JS, Lyoo IK, Kim JM. Peripheral markers of suicidal behavior: current findings and clinical implications. Clin Psychopharmacol Neurosci. (2023) 21:650–64. doi: 10.9758/cpn.22.1046
23. Yang W, Wang X, Kang C, Yang L, Liu D, Zhao N, et al. Establishment of a risk prediction model for suicide attempts in first-episode and drug naive patients with major depressive disorder. Asian J Psychiatr. (2023) 88:103732. doi: 10.1016/j.ajp.2023.103732
24. Schaffer A, Sinyor M, Kurdyak P, Vigod S, Sareen J, Reis C, et al. Population-based analysis of health care contacts among suicide decedents: identifying opportunities for more targeted suicide prevention strategies. World Psychiatry. (2016) 15:135–45. doi: 10.1002/wps.20321
25. Hamilton M. (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry. 23(1):52–62. doi: 10.1136/jnnp.23.1.56
26. Hamilton M. (1959) The assessment of anxiety states by rating. Br J Med Psychol. 32(1):50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x
27. Kay S. R., Fiszbein A., Opler L. A.. (1987) The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 13(2):261–276. doi: 10.1093/schbul/13.2.261
28. Zhou Y., Li Z., Wang Y., Huang H., Chen W., Dong L., Zhang X.. (2020) Prevalence and clinical correlates of psychotic depression in first-episode and drug-naive outpatients with major depressive disorder in a Chinese Han population. J Affect Disord. 263:500–506. doi: 10.1016/j.jad.2019.10.051
29. Posner K., Oquendo M. A., Gould M., Stanley B., Davies M.. (2007) Columbia Classification Algorithm of Suicide Assessment (C-CASA): classification of suicidal events in the FDA's pediatric suicidal risk analysis of antidepressants. Am J Psychiatry. 164(7):1035–1043. doi: 10.1176/ajp.2007.164.7.1035
30. Silverman M. M., Berman A. L., Sanddal N. D., O'Carroll P. W., Joiner T. E.. (2007) Rebuilding the tower of Babel: a revised nomenclature for the study of suicide and suicidal behaviors. Part 1: Background, rationale, and methodology. Suicide Life Threat Behav. 37(3):248–263. doi: 10.1521/suli.2007.37.3.248
32. Mash HBH, Ursano RJ, Kessler RC, Naifeh JA, Fullerton CS, Aliaga PA, et al. Predictors of suicide attempt within 30 days after first medically documented suicidal ideation in U.S. Army soldiers. Am J Psychiatry. (2021) 178:1050–9. doi: 10.1176/appi.ajp.2021.20111570
33. Mash HBH, Ursano RJ, Kessler RC, Naifeh JA, Fullerton CS, Aliaga PA, et al. Predictors of suicide attempt within 30 days of first medically documented major depression diagnosis in U.S. army soldiers with no prior suicidal ideation. BMC Psychiatry. (2023) 23:392. doi: 10.1186/s12888-023-04872-z
34. Brunoni AR, Nunes MA, Lotufo PA, Bensenor IM. Acute suicidal ideation in middle-aged adults from Brazil. Results from the baseline data of the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Psychiatry Res. (2015) 225:556–62. doi: 10.1016/j.psychres.2014.11.047
35. Dong M, Wang SB, Li Y, Xu DD, Ungvari GS, Ng CH, et al. Prevalence of suicidal behaviors in patients with major depressive disorder in China: A comprehensive meta-analysis. J Affect Disord. (2018) 225:32–9. doi: 10.1016/j.jad.2017.07.043
36. Ballard ED, Vande Voort JL, Luckenbaugh DA, MaChado-Vieira R, Tohen M, Zarate CA. Acute risk factors for suicide attempts and death: prospective findings from the STEP-BD study. Bipolar Disord. (2016) 18:363–72. doi: 10.1111/bdi.12397
37. Hawton K, van Heeringen K. Suicide. Lancet. (2009) 373:1372–81. doi: 10.1016/S0140-6736(09)60372-X
38. Nock MK, Park JM, Finn CT, Deliberto TL, Dour HJ, Banaji MR. Measuring the suicidal mind: implicit cognition predicts suicidal behavior. Psychol Sci. (2010) 21:511–7. doi: 10.1177/0956797610364762
39. Ten Have M, van Dorsselaer S, de Graaf R. Prevalence and risk factors for first onset of suicidal behaviors in the Netherlands Mental Health Survey and Incidence Study-2. J Affect Disord. (2013) 147:205–11. doi: 10.1016/j.jad.2012.11.005
40. Barnes SM, Bahraini NH, Forster JE, Stearns-Yoder KA, Hostetter TA, Smith G, et al. Moving Beyond Self-Report: Implicit Associations about Death/Life Prospectively Predict Suicidal Behavior among Veterans. Suicide Life Threat Behav. (2017) 47:67–77. doi: 10.1111/sltb.12265
41. Eikelenboom M, Beekman ATF, Penninx B, Smit JH. A 6-year longitudinal study of predictors for suicide attempts in major depressive disorder. Psychol Med. (2019) 49:911–21. doi: 10.1017/S0033291718001423
42. Garcia de la Garza A, Blanco C, Olfson M, Wall MM. Identification of suicide attempt risk factors in a national US survey using machine learning. JAMA Psychiatry. (2021) 78:398–406. doi: 10.1001/jamapsychiatry.2020.4165
43. Sobanski T, Josfeld S, Peikert G, Wagner G. Psychotherapeutic interventions for the prevention of suicide re-attempts: a systematic review. Psychol Med. (2021) 51:2525–40. doi: 10.1017/S0033291721003081
44. Favril L, Yu R, Uyar A, Sharpe M, Fazel S. Risk factors for suicide in adults: systematic review and meta-analysis of psychological autopsy studies. Evid Based Ment Health. (2022) 25:148–55. doi: 10.1136/ebmental-2022-300549
45. Sohn MN, McMorris CA, Bray S, McGirr A. The death-implicit association test and suicide attempts: a systematic review and meta-analysis of discriminative and prospective utility. Psychol Med. (2021) 51:1789–98. doi: 10.1017/S0033291721002117
46. King CA, Grupp-Phelan J, Brent D, Dean JM, Webb M, Bridge JA, et al. Predicting 3-month risk for adolescent suicide attempts among pediatric emergency department patients. J Child Psychol Psychiatry. (2019) 60:1055–64. doi: 10.1111/jcpp.13087
47. Sareen J, Cox BJ, Afifi TO, de Graaf R, Asmundson GJ, ten Have M, et al. Anxiety disorders and risk for suicidal ideation and suicide attempts: a population-based longitudinal study of adults. Arch Gen Psychiatry. (2005) 62:1249–57. doi: 10.1001/archpsyc.62.11.1249
48. Moffitt TE, Harrington H, Caspi A, Kim-Cohen J, Goldberg D, Gregory AM, et al. Depression and generalized anxiety disorder: cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Arch Gen Psychiatry. (2007) 64:651–60. doi: 10.1001/archpsyc.64.6.651
49. Sanches M, Nguyen LK, Chung TH, Nestadt P, Wilcox HC, Coryell WH, et al. Anxiety symptoms and suicidal thoughts and behaviors among patients with mood disorders. J Affect Disord. (2022) 307:171–7. doi: 10.1016/j.jad.2022.03.046
50. Uebelacker LA, Weisberg R, Millman M, Yen S, Keller M. Prospective study of risk factors for suicidal behavior in individuals with anxiety disorders. Psychol Med. (2013) 43:1465–74. doi: 10.1017/S0033291712002504
51. Cox BJ, Direnfeld DM, Swinson RP, Norton GR. Suicidal ideation and suicide attempts in panic disorder and social phob\ia. Am J Psychiatry. (1994) 151:882–7. doi: 10.1176/ajp.151.6.882
52. Tanskanen A, Vartiainen E, Tuomilehto J, Viinamaki H, Lehtonen J, Puska P. High serum cholesterol and risk of suicide. Am J Psychiatry. (2000) 157:648–50. doi: 10.1176/appi.ajp.157.4.648
53. Wu S, Ding Y, Wu F, Xie G, Hou J, Mao P. Serum lipid levels and suicidality: a meta-analysis of 65 epidemiological studies. J Psychiatry Neurosci. (2016) 41:56–69. doi: 10.1503/jpn.150079
54. Kim JM, Kang HJ, Kim JW, Choi W, Lee JY, Kim SW, et al. Multiple serum biomarkers for predicting suicidal behaviours in depressive patients receiving pharmacotherapy. Psychol Med. (2022) 53:1–10. doi: 10.1017/S0033291722001180
55. Qing G, Deng W, Zhou Y, Zheng L, Wang Y, Wei B. The association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and suicidal ideation in adults: a population-based study in the United States. Lipids Health Dis. (2024) 23:17. doi: 10.1186/s12944-024-02012-4
56. Zheng S, Wang Z, Yang L, Zhang X. Clinical correlates and thyroid hormones of metabolic syndrome in first-episode and drug-naive major depressive disorder outpatients with and without hyperglycemia: a comprehensive cross-sectional study. BMC Psychiatry. (2023) 23:649. doi: 10.1186/s12888-023-05150-8
57. Svensson T, Inoue M, Sawada N, Charvat H, Mimura M, Tsugane S, et al. High serum total cholesterol is associated with suicide mortality in Japanese women. Acta Psychiatr Scand. (2017) 136:259–68. doi: 10.1111/acps.12758
58. Cho Y, Choi S, Kim K, Park SM. Sociodemographic factors, health behaviors, and biological indicators associated with suicide mortality among young adults in South Korea: A nationwide cohort study among 15 million men and women. J Clin Psychiatry. (2020) 82. doi: 10.4088/JCP.19m13037
59. Svensson T, Inoue M, Sawada N, Mimura M, Tsugane S. High serum total cholesterol is associated with suicide mortality in Japanese women independently of menopause. Acta Psychiatr Scand. (2018) 137:80–1. doi: 10.1111/acps.12841
60. Zhou S, Zhao K, Shi X, Sun H, Du S, Miao X, et al. Serum lipid levels and suicide attempts within 2 weeks in patients with major depressive disorder: is there a relationship? Front Psychiatry. (2021) 12:676040. doi: 10.3389/fpsyt.2021.676040
61. Surace T, Capuzzi E, Caldiroli A, Ceresa A, Esposito CM, Auxilia AM, et al. Which clinical and biochemical parameters are associated with lifetime suicide attempts in bipolar disorder? Diagnostics (Basel). (2022) 12. doi: 10.3390/diagnostics12092215
62. Comings DE, MacMurray JP, Gonzalez N, Ferry L, Peters WR. Association of the serotonin transporter gene with serum cholesterol levels and heart disease. Mol Genet Metab. (1999) 67:248–53. doi: 10.1006/mgme.1999.2870
63. Lindholm Carlstrom E, Saetre P, Rosengren A, Thygesen JH, Djurovic S, Melle I, et al. Association between a genetic variant in the serotonin transporter gene (SLC6A4) and suicidal behavior in patients with schizophrenia. Behav Brain Funct. (2012) 8:24. doi: 10.1186/1744-9081-8-24
64. Penttinen J. Hypothesis: low serum cholesterol, suicide, and interleukin-2. Am J Epidemiol. (1995) 141:716–8. doi: 10.1093/oxfordjournals.aje.a117492
65. Brunner J, Bronisch T, Pfister H, Jacobi F, Hofler M, Wittchen HU. High cholesterol, triglycerides, and body-mass index in suicide attempters. Arch Suicide Res. (2006) 10:1–9. doi: 10.1080/13811110500318083
66. Morgan RE, Palinkas LA, Barrett-Connor EL, Wingard DL. Plasma cholesterol and depressive symptoms in older men. Lancet. (1993) 341:75–9. doi: 10.1016/0140-6736(93)92556-9
67. Kulak-Bejda A, Bejda G, Lech M, Waszkiewicz N. Are lipids possible markers of suicide behaviors? J Clin Med. (2021) 10. doi: 10.3390/jcm10020333
68. Aguglia A, Solano P, Parisi VM, Asaro P, Caprino M, Trabucco A, et al. Predictors of relapse in high lethality suicide attempters: a six-month prospective study. J Affect Disord. (2020) 271:328–35. doi: 10.1016/j.jad.2020.04.006
69. Bartoli F, Crocamo C, Dakanalis A, Riboldi I, Miotto A, Brosio E, et al. Association between total serum cholesterol and suicide attempts in subjects with major depressive disorder: Exploring the role of clinical and biochemical confounding factors. Clin Biochem. (2017) 50:274–8. doi: 10.1016/j.clinbiochem.2016.11.035
70. Capuzzi E, Bartoli F, Crocamo C, Malerba MR, Clerici M, Carra G. Recent suicide attempts and serum lipid profile in subjects with mental disorders: A cross-sectional study. Psychiatry Res. (2018) 270:611–5. doi: 10.1016/j.psychres.2018.10.050
71. Lee K, Kim S, Jo JK. The relationships between abnormal serum lipid levels, depression, and suicidal ideation according to sex. J Clin Med. (2022) 11. doi: 10.3390/jcm11082119
72. Choi W, Kang HJ, Kim JW, Kim HK, Kang HC, Lee JY, et al. Age-specific associations between serum cholesterol levels and suicidal behaviors in patients with depressive disorders: A naturalistic prospective observational cohort study. Front Psychiatry. (2023) 14:1095579. doi: 10.3389/fpsyt.2023.1095579
73. Rabe-Jablonska J, Poprawska I. Levels of serum total cholesterol and LDL-cholesterol in patients with major depression in acute period and remission. Med Sci Monit. (2000) 6:539–47.
74. Capuzzi E, Caldiroli A, Capellazzi M, Tagliabue I, Buoli M, Clerici M. Biomarkers of suicidal behaviors: A comprehensive critical review. Adv Clin Chem. (2020) 96:179–216. doi: 10.1016/bs.acc.2019.11.005
75. Fu XL, Li X, Ji JM, Wu H, Chen HL. Blood hormones and suicidal behaviour: A systematic review and meta-analysis. Neurosci Biobehav Rev. (2022) 139:104725. doi: 10.1016/j.neubiorev.2022.104725
76. Liu W, Wu Z, Sun M, Zhang S, Yuan J, Zhu D, et al. Association between fasting blood glucose and thyroid stimulating hormones and suicidal tendency and disease severity in patients with major depressive disorder. Bosn J Basic Med Sci. (2022) 22:635–42. doi: 10.17305/bjbms.2021.6754
77. Zhang Q, Zhao S, Liu Z, Luo B, Yang Y, Shi Y, et al. Association of thyroid-stimulating hormone and lipid levels with suicide attempts among adolescents with major depressive disorder in China. Front Psychiatry. (2022) 13:1031945. doi: 10.3389/fpsyt.2022.1031945
78. Peng P, Wang Q, Lang X, Liu T, Zhang XY. Clinical symptoms, thyroid dysfunction, and metabolic disturbances in first-episode drug-naive major depressive disorder patients with suicide attempts: A network perspective. Front Endocrinol (Lausanne). (2023) 14:1136806. doi: 10.3389/fendo.2023.1136806
79. Zhu Q, Lang X, Zhang XY. Gender differences in prevalence and clinical risk factors of suicide attempts in young adults with first-episode drug-naive major depressive disorder. BJPsych Open. (2024) 10:e19. doi: 10.1192/bjo.2023.635
80. Peng R, Dai W, Li Y. Low serum free thyroxine level is correlated with lipid profile in depressive patients with suicide attempt. Psychiatry Res. (2018) 266:111–5. doi: 10.1016/j.psychres.2018.05.059
Keywords: first-time suicide attempt, first-episode, drug-naïve, major depressive disorder, prevalence
Citation: Cong X, Zhang T, Bian R, Li Y, Liu J and Zhang X (2024) Prevalence and related factors of first-time suicide attempts in the past 14 days in Chinese adult patients with first-episode drug-naïve major depressive disorder. Front. Psychiatry 15:1366475. doi: 10.3389/fpsyt.2024.1366475
Received: 06 January 2024; Accepted: 13 March 2024;
Published: 22 March 2024.
Edited by:
Gábor Gazdag, Jahn Ferenc Dél-Pesti Kórház és Rendelőintézet, HungaryCopyright © 2024 Cong, Zhang, Bian, Li, Liu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Junjun Liu, MzI1NzIzNDhAcXEuY29t; Xiangyang Zhang, emhhbmd4eUBwc3ljaC5hYy5jbg==
 Xiaoyin Cong1
Xiaoyin Cong1 Junjun Liu
Junjun Liu Xiangyang Zhang
Xiangyang Zhang