- 1Faculty of Humanities and Arts, Macau University of Science and Technology, Macao, Macao SAR, China
- 2State Key Laboratory of Quality Research in Chinese Medicines, Macau University of Science and Technology, Macao, Macao SAR, China
- 3Faculty of Chinese Medicine, Macau University of Science and Technology, Macao, Macao SAR, China
- 4College of Computer Science and Technology Zhejiang University, Hangzhou, Zhejiang, China
- 5Operation Management Centre, Guangzhou Wanqu Cooperative Institute of Design, Guangzhou, Guangdong, China
- 6Qinghai Province Cardiovascular and Cerebrovascdular Disease Specialist Hospital, Xining, Qinghai, China
- 7Centre for Epidemiology and Evidence-Based Practice, Department of Social and Preventive Medicine, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia
Introduction: Arts therapies offer effective non-pharmacological intervention for Sleep Initiation and Maintenance Disorders (SIMDs), encompassing both passive and active modalities. This review assesses their effectiveness and ethical considerations, focusing on music therapy, meditation, and Tai Chi.
Methods: Following PRISMA guidelines, a detailed search across PubMed, the Cochrane Library, Web of Science, and CNKI identified 17 relevant RCTs. Utilizing the Joanna Briggs Institute (JBI) quality criteria and the PICO(S) framework for data extraction ensured methodological integrity.
Results: Analysis shows arts therapies significantly improve sleep quality. Music therapy and meditation yield immediate benefits, while Tai Chi and Qigong require longer commitment for significant outcomes.
Discussion: The link between SIMDs and mental health issues like anxiety, stress, and depression suggests arts therapies not only enhance sleep quality but also address underlying mental health conditions. The evidence supports a wider adoption of arts therapies in treating SIMDs due to their dual benefits.
Systematic review registration: PROSPERO, ID: CRD42024506393.
1 Introduction
In the rapid pace of modern life, Sleep initiation and maintenance disorders (SIMDs) have emerged as a global health challenge, exacerbated by the aftereffects experienced by many in the wake of the pandemic, severely impacting physical health and daily routines (1). A study by the World Health Organization (WHO) estimates that approximately 1.7 billion people globally suffer from sleep disturbances, accounting for 27% of the world’s population (2). The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) characterizes insomnia as a prevalent clinical condition, with approximately one-third of adults reporting symptoms of insomnia, and 6 to 10% meeting the diagnostic criteria for an insomnia disorder (3). SIMDs encompass a variety of abnormalities during sleep, including excessive daytime sleepiness, insomnia, abnormal movements or behaviors during sleep, and difficulty initiating sleep when desired (4, 5), often accompanied by other physical conditions or mental health issues, including insomnia, obstructive sleep apnea, somnambulism, narcolepsy, and restless legs syndrome among different types (6, 7). More than 50% of adults globally have experienced a sleep disorder at least once in their lives (8). The distribution of sleep problems across certain age groups and populations is even broader, becoming a significant and growing public health issue (9). Sleep, as a fundamental human need, plays a crucial role in maintaining overall health, cognitive function, and quality of life (10). Research indicates that most SIMDs are preventable or treatable (11), yet the majority of sufferers do not seek professional help. The consequences of SIMDs are wide-ranging, adversely affecting individual health and socioeconomic well-being. Conditions such as insomnia, obstructive sleep apnea (OSA), and restless legs syndrome (RLS) continue to have high prevalence rates and exert profound effects on physical and mental health (12–14). Studies have shown a close correlation between sleep and an increased risk of obesity, diabetes, cardiovascular diseases, and mental health disorders, including depression and anxiety (15–17). Sleep issues not only have a strong bidirectional relationship with mood disorders such as depression and anxiety but are also associated with cognitive decline, physical health problems, and decreased work efficiency (18–21). Particularly among the elderly, over 50% suffer from sleep issues, impacting their physical and mental well-being (22). Furthermore, approximately 80% of individuals with clinical depression experience sleep disturbances (23). Research also reveals that sleep problems are prevalent in high-stress groups, such as college students (24). Traditional sleep interventions have relied on pharmacological treatments, which may come with side effects that limit their long-term application (25), such as residual drowsiness, tolerance, dependence, altered sleep architecture, and rebound insomnia (26–29). Common medications used in traditional treatments include sleep aids like zopiclone, zolpidem, and eszopiclone, as well as medications used to alleviate anxiety or depression associated with sleep issues, such as alprazolam, quetiapine, and fluoxetine (30, 31). These medications often result in side effects during the medication-induced sleep process, such as nasal congestion, convulsions, nightmares or hallucinations, and breathing difficulties, and are accompanied by side effects such as dizziness, nausea, dry mouth, muscle weakness, and headache upon waking. Moreover, these drugs carry the risk of dependency and resistance, often leading to withdrawal reactions upon cessation, and place significant financial stress on many patients over the long term (32, 33). This has paved the way for non-pharmacological interventions (34), given the burdens of pharmacotherapy, exploring benign non-pharmacological interventions for sleep issues becomes the focus of this article.
Among the numerous methods for sleep healing, various forms of arts therapies as non-pharmacological treatments have shown unique advantages and potential. To refine and expand our definition of arts within arts therapies, it’s crucial to adopt a nuanced and comprehensive perspective that acknowledges the wide array of non-pharmacological therapeutic arts as defined by the five senses: visual, auditory, olfactory, gustatory, and tactile. For example, visual art and color therapy utilize form, color, and imagery to engage the visual sense, potentially evoking feelings of calmness and relaxation that can improve sleep quality (35). Similarly, music therapy leverages auditory stimuli to influence emotional states and stress levels, indirectly promoting healthier sleep patterns (36). Aromatherapy, targeting the olfactory sense, uses essential oils and fragrant extracts to harmonize the mind and body, with certain scents known for their sedative properties that aid sleep. While gustatory arts, such as culinary arts therapy, may indirectly influence sleep through mood and wellbeing improvements, tactile forms of therapy like body movement and dance therapy emphasize physical expression and the tactile experience to relieve stress and enhance sleep quality (37, 38). This inclusive approach not only broadens the review’s scope but also underscores the multifaceted nature of arts therapies in mitigating sleep initiation and maintenance disorders by alleviating mental stress and emotional tension. Moreover, arts therapies promote and encourage individuals to actively manage their own health, placing a greater emphasis on intrinsic motivation and personal involvement. By engaging with art, individuals improve their mood and mental health, releasing inner stress and uneasy emotions, which in turn reduces levels of anxiety and depression (39). This engagement in creative activities provides an outlet for emotional release and self-exploration, not only offering immediate relief from sleep issues but also increasing individual life satisfaction and happiness over the long term. As a non-pharmacological treatment, arts therapies not only highlights its uniqueness in addressing sleep problems but also robustly supports the improvement of sleep quality, promising to become an important tool for enhancing individual and community health (40).
Therefore, this review explores a gentler approach to improving sleep health through non-pharmacological interventions. Focusing on various art forms, this review examines diversified alternative therapies including mindfulness-based stress reduction (MBSR) (41), yoga (42), music therapy (43), virtual reality (VR) (44), and meditation (45) that offer sensory engagement. Studies indicate that these therapies assist in regulating both physiological and psychological states, thus improving sleep quality. These arts therapies not only eliminate the need for injections or oral medications but also provide multidimensional benefits unreachable by traditional treatment methods (46). For instance, group yoga not only promotes relaxation and improves sleep quality but also enhances social interaction, boosts self-esteem, and positively affects posture (47). Beyond sleep, these interventions also include stress reduction, enhanced emotional regulation, and improved cognitive function (48, 49). These intervention methods offer assistance not just to the elderly but have also shown potential in ICU patients, college students, and other populations affected by high stress levels.
This review aims to comprehensively examine and compare evidence supporting various non-pharmacological interventions for SIMDs, delving into how these measures can improve sleep issues across different populations and assessing their benefits and potential limitations in clinical practice. Specifically, this review will focus on the following research questions:
1) Which arts therapies have been effective in addressing SIMDs?
2) How do different art forms and practices leverage their unique advantages in the intervention of SIMDs?
3) What are the mechanisms of effect when these arts therapies are used as alternative treatments, and what hypotheses can be explored?
This review intends to provide healthcare professionals with practical guidelines to make more informed decisions in treating SIMDs and offer value to patients seeking alternative and complementary treatments. By considering the multidimensional benefits of arts therapies, this article aims to present a new perspective and direction for the management of SIMDs within the healthcare system.
2 Methods
This systematic review adheres to the PRISMA statement for systematic reviews and meta-analyses (PRISMA) (50, 51) and is registered with PROSPERO (52) under the registration number CRD42024506393. We developed the research question using the PICOS acronym, as follows:
PICOS
• P: Any patient associated with SIMDS.
• I: Interventional arts therapies.
• C: Conventional therapy.
• O: Improved clinical and/or mental health outcomes.
• S: randomized controlled trials, quasi experimental studies (non-randomized controlled trials), and single-arm, pre-test/post-test studies.
2.1 Study inclusion and exclusion criteria
In the systematic review, we rigorously defined the inclusion and exclusion criteria to ensure a thorough examination of the impact of arts therapies on Sleep Initiation and Maintenance Disorders (SIMDs). Studies eligible for inclusion are those that adhere to the Joanna Briggs Institute (JBI) research design guidelines, involve participants diagnosed with SIMDs, and implement arts therapies, including but not limited to music, visual arts, dance/movement, drama therapy, and bibliotherapy as a primary intervention. The interventions could be carried out across various settings and delivered by arts therapy professionals. These studies should compare the outcomes against any type of control group and report on sleep quality indicators such as sleep latency and efficiency. Our focus is on gathering empirical evidence from randomized controlled trials, quasi-experimental studies, and analytical cross-sectional studies that meet ethical and methodological standards.
Conversely, the review excludes non-peer-reviewed documents, studies not employing art-based interventions, and those concerning individuals without SIMDs diagnoses. Additionally, research designs such as non-experimental studies, narrative reviews, animal studies, and publications not in English are omitted to maintain the review’s integrity and manageability. This selectivity ensures the inclusion of studies with robust methodologies and relevant outcomes, thereby providing reliable evidence on the effectiveness of arts therapies in treating sleep disorders. The exclusion of non-English articles and grey literature is acknowledged as a limitation but is necessary for ensuring thorough analysis and interpretation within the language proficiency of the review team.
2.2 Electronic databases
This systematic search was conducted across five electronic databases: PubMed, Cochrane Library, Web of Science, Embase, and the Chinese database CNKI, for publications spanning from 2004 to 2024.
2.3 Search strategy
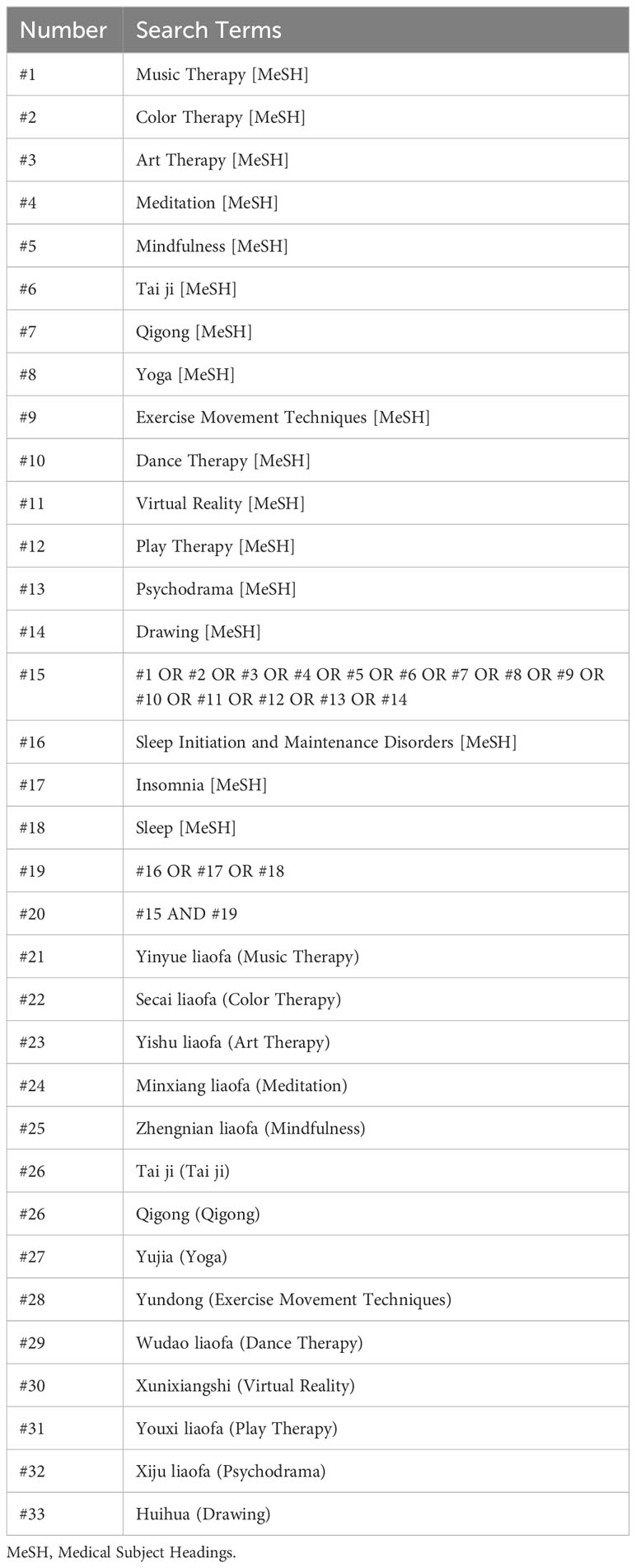
A meticulously structured search strategy was implemented by a team of three independent researchers. This strategy aimed to capture a wide array of studies that investigate the intersection of arts therapies and sleep disorders. Table 1 of the original article delineates the search strategy, highlighting the employment of specific keywords and Medical Subject Headings (MeSH) to guide the literature search. The primary keywords included ‘Arts Therapies’ and ‘Sleep Disorders,’ which were chosen for their broad applicability to studies exploring the therapeutic use of art in the context of sleep-related issues.
To ensure a comprehensive gathering of relevant literature, various forms of art therapy were considered, encompassing visual arts and color-related therapies, auditory music-related therapies, and tactile movement-related therapies. This approach acknowledges the multifaceted nature of arts therapies and their potential impact on sleep disorders across different sensory modalities. Furthermore, to mitigate the risk of overlooking pertinent studies, a manual search was conducted through the reference lists of key reviews and articles identified during the initial search phase. This dual-faceted search strategy, combining both electronic database searches with manual reference checking, was aimed at creating a thorough and all-encompassing review of the literature available on the subject matter, enhancing the reliability and depth of the systematic review.
2.4 Study selection
Three independent reviewers, LXX, HL, and AJZ, engaged in the screening, eligibility, and selection review processes. LXX was tasked with downloading and reviewing the filtered articles, excluding those deemed irrelevant. Subsequently, pertinent literature was forwarded to HL for an eligibility review. Upon determining the eligibility of 17 documents, AJZ conducted a meticulous evaluation and scoring based on JBI’s critical appraisal tools (53, 54). These instruments are designed to assess the methodological quality of the studies and ascertain the extent to which the studies address the potential for bias in their design, execution, and analysis. Moreover, literature meeting the eligibility criteria was subjected to a dual examination by LXX and HL. Every one of the 17 included studies, particularly those identified as randomized controlled trials, underwent a thorough data extraction process using the PICO(S) framework (55). This approach allowed for the systematic organization and assessment of pertinent information extracted from the documents, enhancing the clarity and conciseness of the analysis.
2.5 Data extraction
In the systematic review process, the task of data extraction was meticulously planned and executed by three independent researchers, ensuring a thorough and unbiased collection of data from the selected studies. This critical phase was structured around the creation of four distinct tables, each designed with a specific function to aid in the systematic organization and analysis of the collected data.
The first table was developed to provide a clear visualization of the core content extracted from each piece of literature, organized into categories such as Study Aims, Participants, Methods, Results, and Discussion. This table aimed to facilitate an immediate understanding of each study’s key components, allowing for a quick yet comprehensive overview of the collected data. The second table was tailored to display subgroups of different arts therapies, enabling the researchers to categorize and compare the results and author names within specific therapeutic groups, thereby highlighting the diversity and specific outcomes associated with each art therapy type.
To ensure the quality and reliability of the included studies, a third table was utilized for conducting a quality review of the literature. This table employed checklists derived from the Joanna Briggs Institute (JBI) guidelines, which are renowned for their robustness in assessing the methodological quality of research. The fourth table was dedicated to extracting detailed data about patient samples, intervention and control group methodologies, and outcomes, specifically from randomized controlled trials (RCTs). For this purpose, the researchers adopted the PICOS (Population, Intervention, Comparator, Outcomes, and Study Design) model, which facilitated a structured and comprehensive analysis of the RCTs. This strategic approach to data extraction not only enhanced the clarity and organization of the data but also laid a solid foundation for the systematic review’s subsequent analysis and discussions.
2.6 Quality appraisal of the included studies
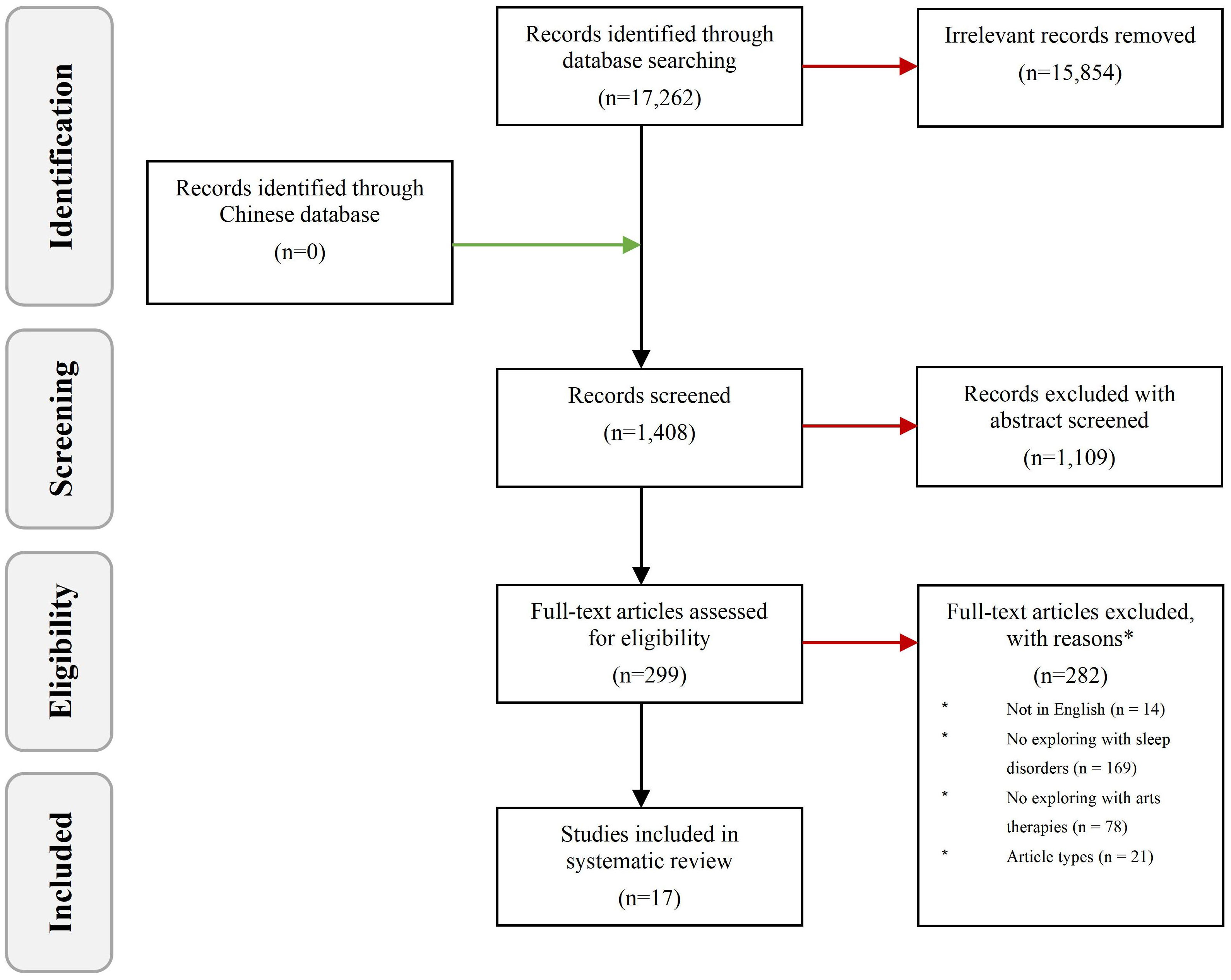
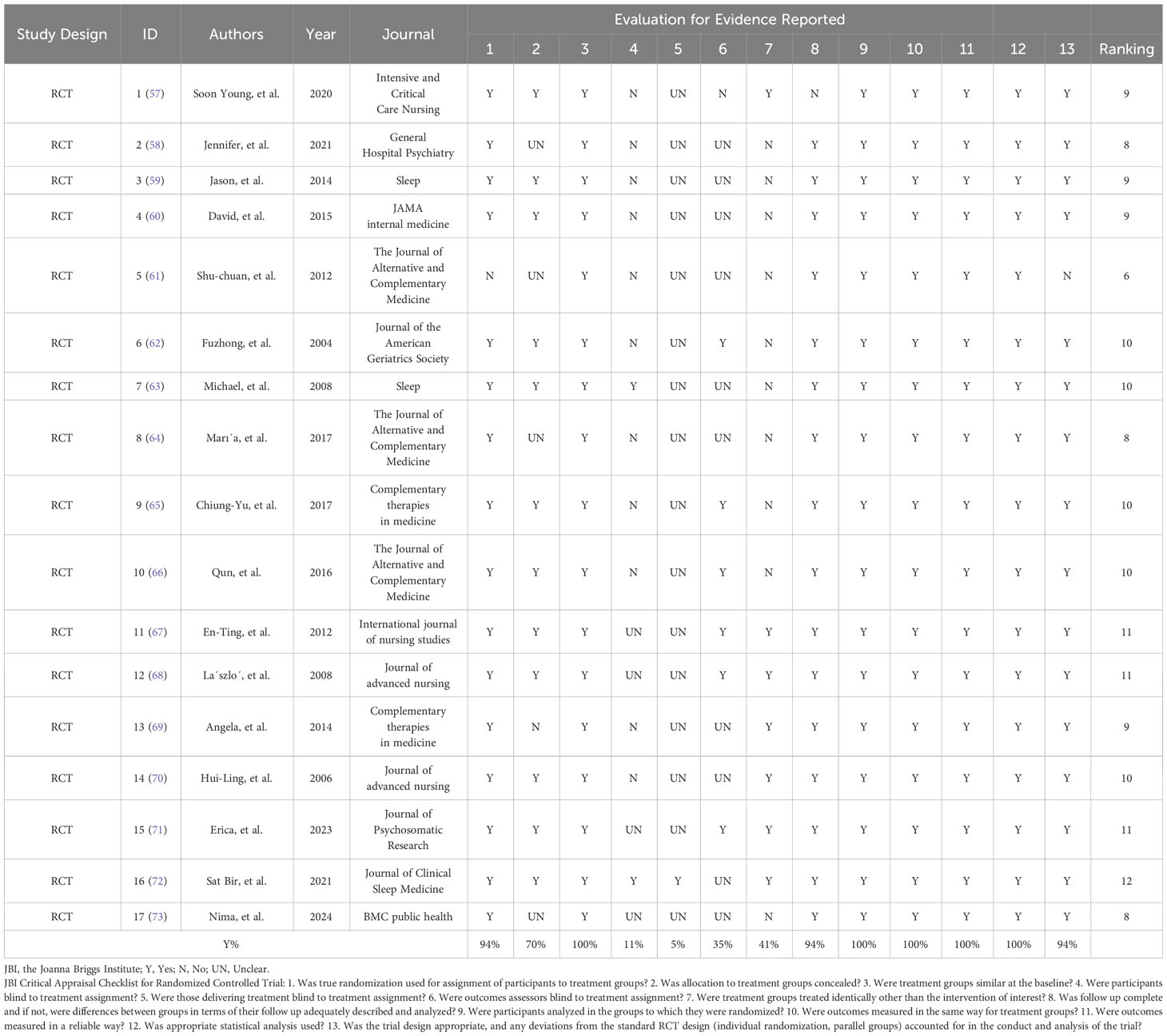
The initial comprehensive search yielded 17,262 publications, from which irrelevant studies were excluded through a meticulous screening of titles and abstracts, followed by a detailed full-text review as required. This rigorous selection process leveraged the PICO(S) framework (Population, Intervention, Comparison, Outcome, and Study design) to systematically define inclusion and exclusion criteria, ensuring focus and relevance in the selection of studies, to uphold the methodological integrity of the review, the Joanna Briggs Institute (JBI) critical appraisal tools were employed, facilitating the evaluation of the studies’ quality. This approach underlined our commitment to incorporating only the most methodologically sound literature into our analysis (53–56).
The quality appraisal of randomized controlled trials (RCTs) within our dataset was conducted using a scoring system informed by JBI guidelines. This involved assigning a score of one point for each criterion adequately met ‘yes’, zero points for unmet criteria ‘no’ and ‘unclear’. This scoring facilitated a horizontal comparison of study quality, ranking them based on their aggregate scores. A score of ≤6 was considered as low quality, from 7 to 9 as moderate and ≥ 10 as high quality. No studies were excluded based on methodological quality. Vertically, this method allowed for the assessment of commonalities across the reviewed literature, evaluating the proportion of studies that successfully met each quality criterion.
Furthermore, the application of the PICO(S) framework extended beyond initial study selection, informing the structured tabulation of the research data. This included organizing studies and ranking them by the number of participants, recognizing that larger sample sizes typically contribute to a stronger evidence base.
3 Results
3.1 Study characteristics
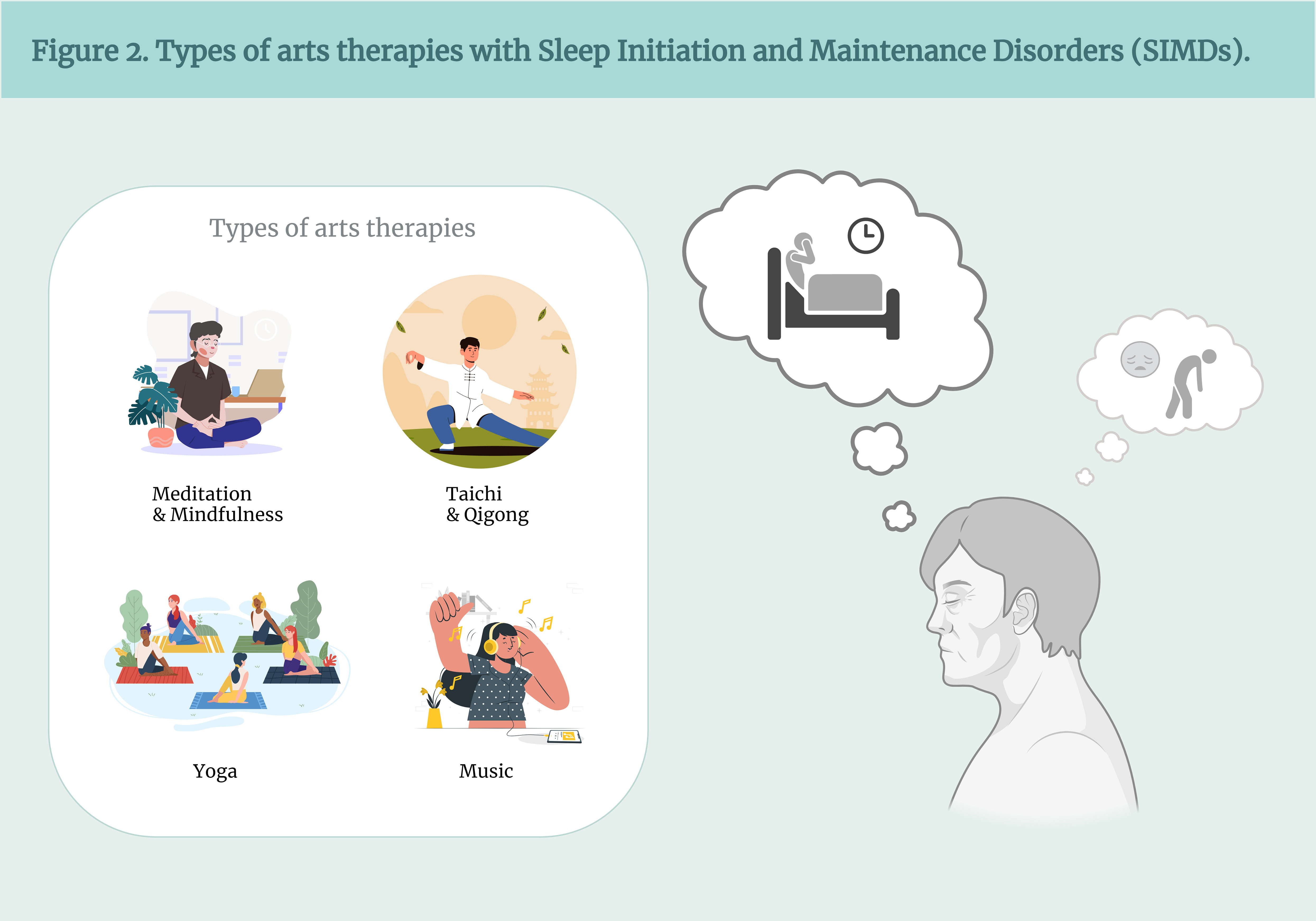
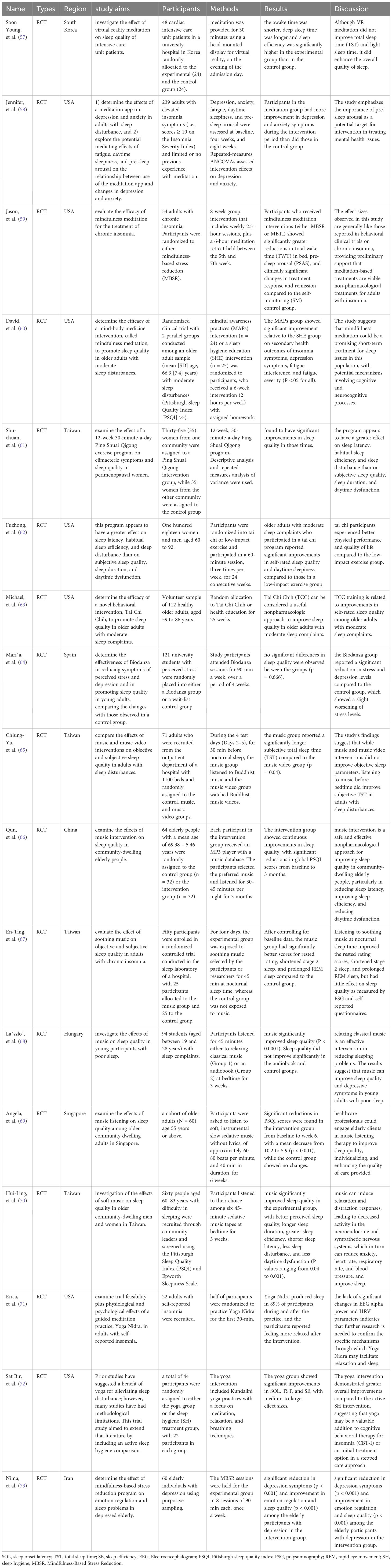
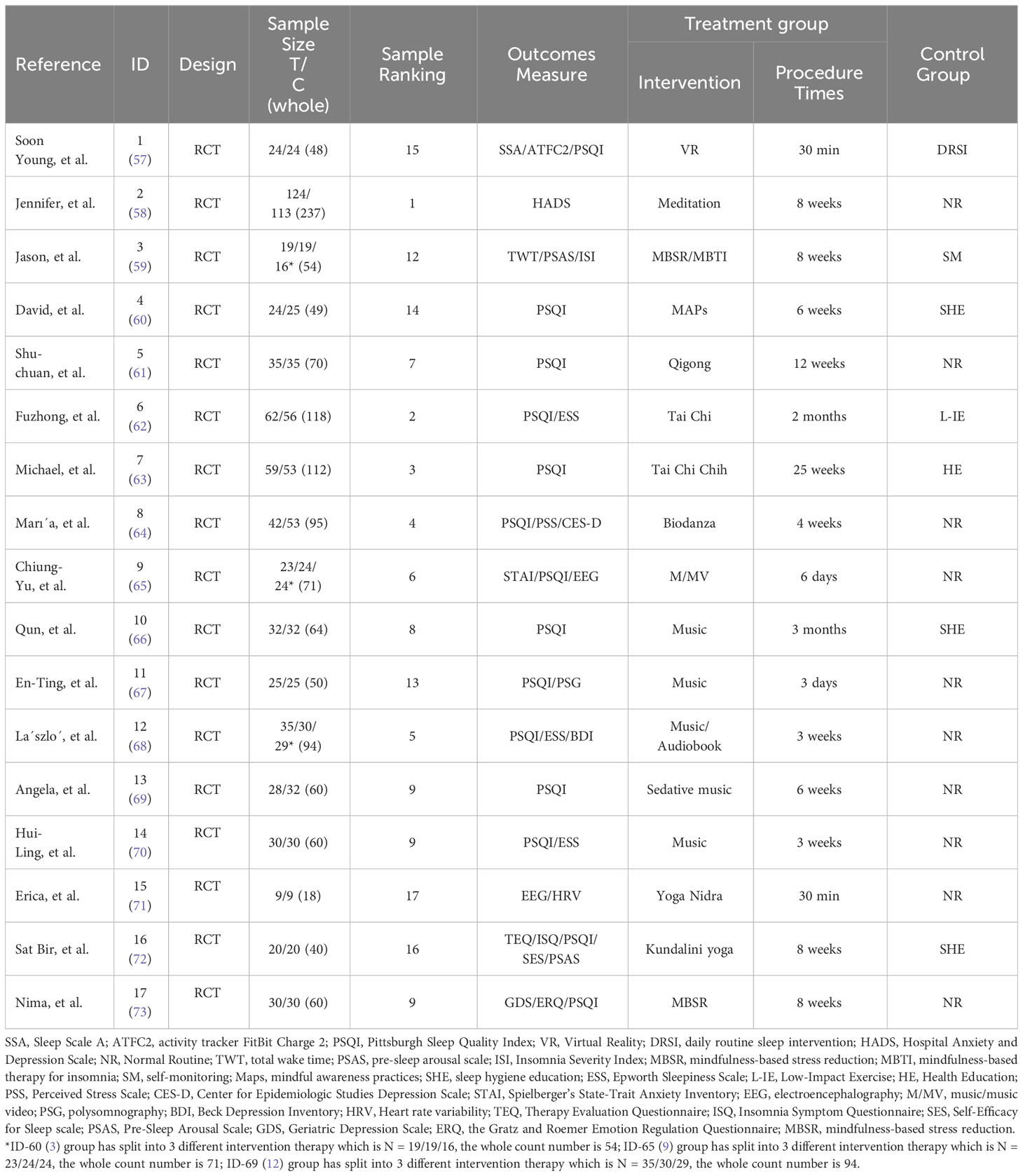
This manuscript incorporates 17 studies focusing on experimental design, wherein 10 studies juxtapose art therapy with a standard routine, and three compare art therapy to sleep hygiene education, see in Figure 1. The control groups in other investigations employed a variety of methods including daily routine sleep intervention, self-monitoring, low-impact exercise, and health education, see in Figure 2, primarily encompassing Virtual Reality (VR) (57), meditation (58–60), qigong (61), tai chi (62, 63), Biodanza (64), music therapy (65–70), yoga (71, 72), and Mindfulness-Based Stress Reduction (MBSR)/Mindfulness-Based Cognitive Therapy (MBCT) (73).
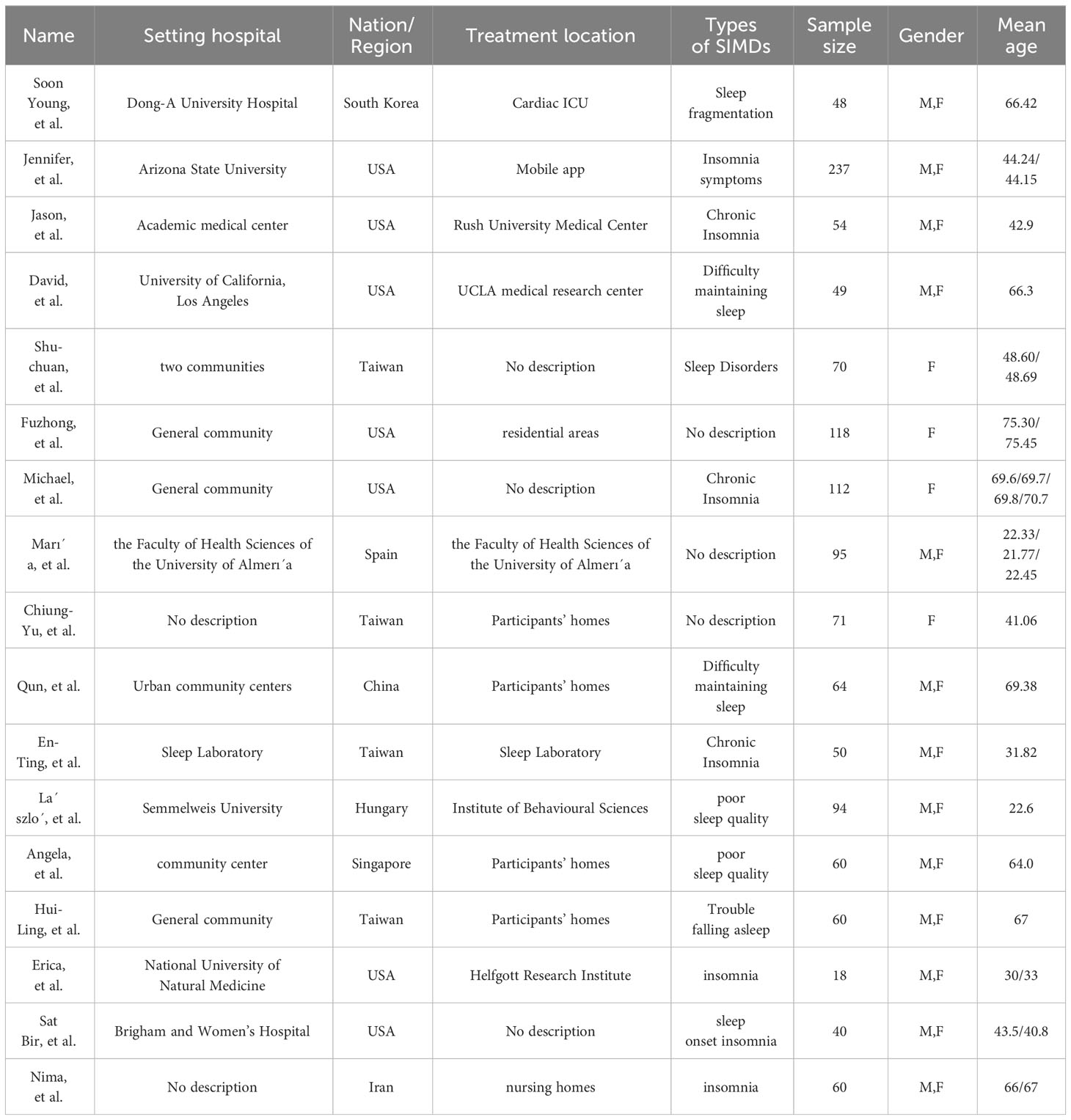
Tables 2, 3 synthesize the principal characteristics of the qualifying studies. The 17 included studies comprise 1,300 participants (treatment conditions= 694, control conditions= 606) hailing from South Korea (57), the USA (58–60, 62, 63, 71, 72), China (61, 65–67, 70), Spain (64), Hungary (68), Singapore (69), and Iran (73), with the largest sample consisting of 237 individuals (58) and the smallest of 18 (71). The age range of participants was broad, from teenagers aged 19 to senior citizens aged 92, encompassing healthy individuals (61–63, 66, 69, 72), cardiac patients (57), those with chronic insomnia and moderate SIMDs (58–60, 65–68, 70, 71), stressed university students (64), and individuals with depression (73).
Regarding the evaluation of study outcomes, the research included varied in their focus on therapeutic outcomes, hence employing diverse testing methodologies. The studies measured characteristics related to sleep quality (57, 59–73), or outcomes in other categories such as anxiety (58, 65), depression (58, 64, 68), stress (64), heart rate (71), electroencephalography (65, 71), or mood (73). The Pittsburgh Sleep Quality Index and scales were the most frequently utilized measures for assessing sleep quality. Additionally, the activity tracker FitBit Charge 2 (57), electroencephalography (65, 71), and heart rate variability (71) represented the latest measurement techniques.
An analysis using the JBI Critical Appraisal Checklist indicates that the quality of evidence from the included studies is relatively high. However, nearly all studies did not rigorously implement a double-blind experimental methodology (Table 4).
3.2 Description of the population
The comprehensive review of literature on the application of arts therapies in addressing Sleep Initiation and Maintenance Disorders (SIMDs) culminated in the selection of 17 pivotal papers. These studies are meticulously tabulated in Tables 3, 5, adhering to the PICOs methodological framework, thereby illustrating the core experimental data extracted from each randomized controlled trial (RCT) article. Collectively, these papers encapsulate a population of 1,300 patients, underscoring the substantial empirical effort directed toward exploring the efficacy of diverse art therapy interventions in mitigating SIMDs.
Among this aggregation of research, the RCTs conducted by Jason, Chiung-Yu, and László are particularly notable for their methodological rigor. By segregating patients into three distinct groups, these studies not only facilitated a nuanced examination of the therapeutic outcomes attributable to various arts interventions and settings but also implemented strategic measures to curtail potential data bias (references 59, 65, 68). Contrasting with these, the remainder of the corpus, comprising 14 papers, predominantly adopted a dual-group treatment versus control design, which is a conventional approach within clinical trial methodologies.
Within this diverse array of studies, Jennifer’s research stands out due to its scale, encompassing a total of 237 patients divided into two groups (124:113), marking it as the study with the highest number of trials among the 17 papers reviewed (reference 58). Following closely, the works of Fuzhong and Michael also contribute significantly to the dataset with totals of 118 and 112 patients, respectively (references 62, 63). Conversely, the study led by Erica, involving a comparatively modest cohort of 18 patients, commands attention not for its volume but rather for its profound implications. Despite its smaller scale, the depth of insights and the meticulous attention to minimizing data bias within Erica’s study necessitate a detailed examination of its experimental outcomes and methodological strengths (reference 71).
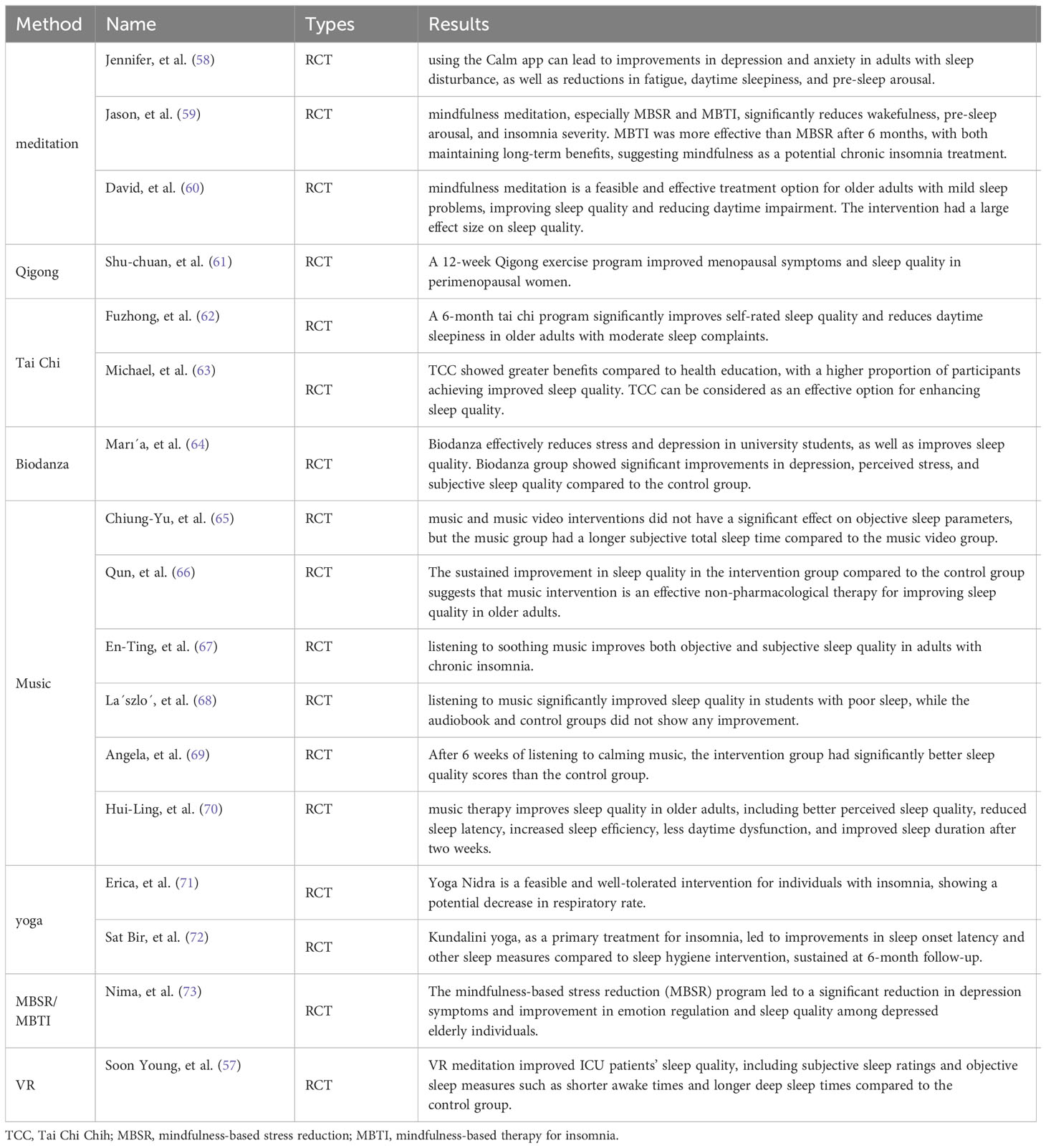
3.3 Analysis the function with arts therapies
The main effects of each art therapy on sleep quality are shown in Table 6. In modern society, sleep issues have become a common health concern, not only affecting the quality of individual lives but also leading to a range of physical and mental health problems (74). As research into non-pharmacological treatments for SIMDs deepens, art therapy has gained attention as an alternative method. This review aims to explore the effectiveness and mechanisms of various arts therapies in improving sleep quality through a systematic analysis of 17 research articles.
With technological advancements, meditation practices using virtual reality (VR) technology have become feasible (75). By simulating natural environments and combining deep breathing and guided meditation, VR meditation has shown significant effects in shortening the time to fall asleep, reducing the number of awakenings during the night, and increasing deep sleep duration, offering a new perspective and method for sleep therapy (57, 76).
Meditation, especially mindfulness meditation, has proven to be an effective self-regulation method for chronic insomnia sufferers by reducing anxiety and stress before sleep, shortening the time to fall asleep, and improving sleep quality (77). Research indicates that meditation not only alleviates SIMDs but also reduces negative emotions such as anxiety and depression, thereby enhancing daytime function and quality of life. These multiple benefits make meditation a powerful tool for treating SIMDs (59).
Qigong and Tai Chi, ancient Chinese mind-body practices (78), improve sleep quality through a series of slow, orderly movements and breathing techniques. These practices not only promote physical relaxation and reduce psychological stress but also regulate the endocrine system, effectively improving SIMDs (79). For example, a 12-week Qigong training for premenopausal women successfully improved their sleep quality and daytime drowsiness (61). Similarly, Tai Chi practice has been shown to enhance self-reported sleep quality and physical function in the elderly, indicating its positive effect on sleep improvement (62).
Biodanza therapy, a dance movement therapy that integrates music, movement, and emotional expression (64), did not show significant differences in directly improving sleep quality but effectively alleviated stress and depression, indirectly promoting a better rest state. Its significant effect in relieving stress, anxiety, and depression indirectly helps attain better sleep (80). Music therapy, including listening to soothing music and music videos, has also shown potential in improving sleep quality in adults and the elderly (65). Music can extend subjective sleep duration, shorten stage two sleep duration, prolong rapid eye movement sleep, and overall improve participants’ sleep experience (67, 81). These studies emphasize music as a non-pharmacological intervention that improves sleep quality by reducing stress responses, relaxing the body and mind, and diverting attention (82).
Yoga therapy, particularly Kundalini yoga and Yoga Nidra, has been proven to have a positive impact on improving sleep quality (71, 72). By improving physical flexibility, enhancing muscle strength, deep breathing, and meditation practices, it not only improves sleep quality but also has a significant therapeutic effect on emotional disorders such as depression and anxiety (83). These improvements suggest that yoga can be an effective treatment method for SIMDs. This effectiveness is not only immediate at the end of yoga practice but can last up to six months after the practice has ended (84), implying that the improvement in sleep quality through yoga is not temporary but has a certain durability. This underscores yoga practice as a long-term effective non-pharmacological treatment method, not just a short-term intervention.
Mindfulness-Based Stress Reduction (MBSR)/Mindfulness-Based Cognitive Therapy (MBCT) courses have had a positive effect on improving emotional regulation and sleep problems (73), significantly reducing depressive symptoms and improving sleep quality in the elderly population with depression.
Overall, these arts therapies provide a diverse range of non-pharmacological treatment options for SIMDs. They significantly improve sleep issues through various mechanisms such as emotional regulation, stress reduction, improving the wakefulness state before sleep, and enhancing sleep quality. Future research should further explore the specific mechanisms of action, sustained effects, and how these arts therapies can be effectively integrated into existing sleep disorder treatment frameworks.
3.4 Literature quality assessment
Leveraging Table 4, our analysis meticulously appraised the comprehensive quality of each study through the Joanna Briggs Institute (JBI) methodology, assigning a one-point increment for every “Yes” response, culminating in an aggregate score out of 13. Within this cohort of 17 randomized controlled trials (RCTs), the paper authored by Sat Bir distinguished itself with a high-quality score of 12 (reference 72), closely trailed by the contributions from En-Ting, László, and Erica, each securing a commendable score of 11 (references 67, 68, 72). This echelon of papers stands apart for their rigorous alignment with quality parameters, whereas the corpus of remaining studies predominantly manifested moderate quality, with the exception of Shu-chuan’s work, which uniquely aligns with the aforementioned group by also securing a score of 11 (references 67, 68, 72). One RCT article notably diverged from this trend, recording a modest score of 6 (reference 61) upon JBI evaluation.
A deeper dive into the JBI quality assessment criteria across these 17 RCT articles revealed that questions 3, 9, 10, 11, and 12 witnessed unanimous affirmative responses. This uniformity underscores a foundational concordance among the studies with regards to the critical aspects of including treatment groups based on clear baseline characteristics, ensuring randomness in subgroup allocations, maintaining uniformity and authenticity in measurement techniques, and employing appropriate statistical analyses. Such consistency is pivotal for establishing the foundational integrity of trial methodologies.
Conversely, a nuanced examination reveals that questions 4 and 5, which probe the implementation of double-blind or single-blind protocols in RCTs, presented a spectrum of “No” and “Unclear” responses across all examined literature. This variance highlights a prevalent methodological vulnerability within the domain, signifying a crucial area for future methodological refinement and adherence to ensure the elimination of bias and elevation of research quality standards.
3.5 Description of the control intervention
According to Table 3, within the ambit of the 17 randomized controlled trials (RCTs) scrutinized in the presented literature, a discernible allocation of control group methodologies is observed. Notably, a majority, specifically 10 RCTs, embraced a ‘Normal Routine’ strategy for their control groups, an approach characterized by the absence of any specialized methodological intervention for participants afflicted with sleep disorders (58, 61, 64, 65, 67–71, 73). This strategy ostensibly serves to mirror the unaltered daily routines of individuals, thereby establishing a baseline for comparative analysis. An integrative approach was adopted in three RCTs, employing ‘Sleep Hygiene Education’ as the control group intervention. This methodological choice is predicated on the dissemination of essential medical knowledge, aiming to cultivate an awareness among patients regarding the principles conducive to healthy sleep patterns (60, 66, 72).
Complementing these, the remainder of the dataset, comprising four RCTs, instituted a varied spectrum of control conditions, specifically ‘Daily Routine Sleep Intervention,’ ‘Self-Monitoring,’ ‘Low-Impact Exercise,’ and ‘Health Education.’ These interventions (57, 59, 62, 63) were distinctively implemented.
3.6 Main results on the primary outcomes
Under PICO(S) design in Table 3, In the analytical examination of 17 randomized controlled trials (RCTs) delineated in our systematic review, the utilization of the Pittsburgh Sleep Quality Index (PSQI) emerged as the predominant tool for outcome measurement, with an overwhelming 14 studies (57, 60–70, 72, 73) electing the PSQI as their principal evaluative instrument. This universal adoption underscores the PSQI’s acknowledged efficacy in gauging the multifaceted aspects of sleep quality within clinical research paradigms. The Pre-Sleep Arousal Scale (PSAS) was employed as the measurement methodology in two distinct RCTs (59, 72), signifying its specialized application in assessing pre-sleep cognitive and somatic arousal levels. Of note, one study (57) innovatively combined the PSQI with both the Sleep Scale A (SSA) and an activity tracker (FitBit Charge 2, ATFC2), thus broadening the spectrum of sleep-related data acquisition. Similarly, an additional study (59) integrated Total Wake Time (TWT) alongside the PSQI, thereby enriching the dimensional coverage of sleep disturbances being investigated.
The Epworth Sleepiness Scale (ESS), a tool designed to measure daytime sleepiness, was cohesively utilized across three studies (62, 68, 70). Notably, the sophisticated technology of electroencephalography (EEG) was harnessed for data collection in two studies (65, 71).
3.7 Therapeutic with SIMDs
Music therapy, featured prominently as the most frequently cited intervention method among the 17 studies reviewed, distinguishes itself from other modalities by its passive nature, as opposed to the active engagement required by the others (65–70). This form of therapy, characterized by the passive auditory reception of music, serves to alleviate emotional tension and soothe neural stress without necessitating physical movement, making it particularly well-suited for improving sleep disturbances among the elderly with limited mobility. According to Table 4 of the PICO(S) framework, in the elderly population, two randomized controlled trials (RCTs), each involving around 60 participants split into two groups, conducted interventions over periods of 3 and 6 weeks. The pre and post-intervention data, gauged by the Pittsburgh Sleep Quality Index (PSQI), demonstrated a comprehensive amelioration of SIMDs in the elderly (69, 70). In studies targeting younger demographics, such as college students, La´szlo´ divided participants into three groups of 35, 30, and 29. After a 3-week intervention, data from the PSQI and Beck Depression Inventory (BDI) indicated that music therapy could concurrently suppress depressive symptoms and sleep disorder manifestations (68). A 3-day experiment focusing on adults with chronic insomnia revealed that listening to soothing music for 45 minutes before sleep significantly prolonged the rapid eye movement (REM) sleep phase (67). As a form of passive intervention, music therapy, a non-pharmacological measure, has been shown to effectively enhance sleep initiation and maintenance in patients with sleep quality issues (85), particularly benefiting those who prefer natural remedies or are concerned about the side effects of sleep medications, without requiring physical movement (86). Allowing participants to select their preferred music enhances the effectiveness of the intervention, as personal preference plays a critical role in the therapeutic impact of music. However, choices in music can vary greatly, and there is no standardized method for selecting the type or duration of music to be used for sleep therapy. Nevertheless, according to Table 4 of the PICO(S) framework, most studies on music therapy interventions had short durations, lacking data on the long-term efficacy and sustainability of music therapy for treating SIMDs (65, 67, 68, 70).
Besides music therapy’s passive interventions, all other methods included in the 17 studies fall under active interventions, with meditation and mindfulness being primary modalities (57–60, 73), followed by physical movement-based interventions like Qigong, Tai Chi, dance, and yoga (61–64, 71, 72). Tai Chi and Qigong therapies, among these active interventions, had the longest durations of engagement, spanning 2 months, 3 months, and 6 months, utilizing slow, rhythmic movements and deep breathing to achieve relaxation and equilibrium of body and mind. Studies have shown that Qigong improved menopausal symptoms and sleep quality in the intervention group after 6 and 12 weeks compared to the control group, while Tai Chi required long-term intervention, such as more than 24 weeks, to exhibit a significant improvement in sleep, with the Pittsburgh Sleep Quality Index (PSQI) and Epworth Sleepiness Scale (ESS) serving as primary measurement tools (61–63). Meditation is a commonly employed method in the treatment of SIMDs, typically involving 6–8 week interventions focused primarily on elderly individuals, especially those experiencing sleep disturbances. Research suggests that mindfulness meditation may correlate with reduced concentrations of NF-κB (a transcription factor associated with inflammatory responses), indicating a potential anti-inflammatory effect beneficial to seniors. Furthermore, meditation therapy has been found to improve mental health issues in the elderly, alleviating depression, anxiety, and feelings of loneliness. Meditation, often linked to Buddhism or yoga, typically incorporates techniques such as silence, breath counting, and visualization during training, aimed at reducing stress and intrusive thoughts, thereby psychologically remedying non-organic insomnia (58–60, 73). Yoga and dance, requiring some degree of physical effort, have shown varying impacts. Despite no significant intergroup differences in EEG alpha-wave power, heart rate variability (HRV), or sleep latency observed with Yoga Nidra (a form of guided meditation practice), a statistically significant difference in respiratory rate between the Yoga Nidra group and the control group suggests that Yoga Nidra may aid in relaxation, though further research is necessary to confirm (71). The effects of Kundalini yoga and Sleep Hygiene Education (SH) on chronic primary insomnia showed the yoga group had greater improvements in sleep onset latency (SOL), total sleep time (TST), and sleep efficiency (SE), with these improvements persisting at a 6-month follow-up. Over 50% of participants in the yoga group reported a decrease of at least 8 points in the Insomnia Severity Index (ISI) at the end of treatment and during the follow-up period (72). The dance therapy Biodanza, after a 4-week intervention among university students, significantly reduced stress, tension, and depressive moods, indirectly ameliorating sleep issues to some extent (64).
Virtual reality (VR) devices, with their immersive capabilities, offer a promising complement to meditation or mindfulness therapies. However, caution is warranted when applying this emerging technology to older populations, as it may induce fear, stress, and anxiety, potentially exacerbating sleep disorder issues (57).
In conclusion, music therapy emerges as the most extensively documented passive intervention within the study, utilizing auditory reception to mitigate emotional and stress-related issues. It has proven effective in improving sleep disturbances among both the elderly and younger populations, requiring no physical exertion and allowing for personalized music selection to enhance intervention outcomes. Despite the absence of data on long-term effectiveness, music therapy remains a beneficial non-pharmacological intervention (87). Concurrently, the study also explores active interventions such as meditation, Qigong, Tai Chi, yoga, and dance, which are also effective in improving sleep quality among specific groups. The nascent combination of VR technology with meditation shows potential therapeutic effects but should be approached cautiously when applied to older individuals to avoid eliciting adverse emotional responses.
4 Discussion
Given the comprehensive analysis of the results surrounding different arts therapies for mitigating SIMDs, our discussion will explore the optimal combination of these therapies to achieve maximum effectiveness for various demographics. The results highlight the varying benefits of passive and active interventions, including music therapy, meditation, Tai Chi, Qigong, Yoga, and Biodanza, as well as emerging technologies like virtual reality (VR) meditation. By understanding the unique advantages of each method, we can propose tailored, multimodal therapy regimens that cater to specific needs.
The evidence strongly suggests that a combination of passive and active therapies might offer a synergistic effect on improving sleep quality and duration (88–90). Music therapy, the most extensively studied passive intervention in the included literature, demonstrated significant potential in improving sleep quality for both elderly and younger populations without the necessity of physical movement (91, 92). This points to the utility of integrating music therapy into the bedtime routine of individuals across different age groups, particularly those with limited physical mobility or preference for less physically demanding interventions (93, 94).
On the other hand, active therapies like Meditation, Tai Chi, Qigong, and Yoga, have shown promise in not only improving sleep quality but also enhancing psychological well-being and reducing stress, anxiety, and depressive symptoms. These findings suggest that active interventions, which often incorporate elements of mindfulness, physical movement, and breathwork, can address both the physiological and psychological contributors to SIMDs.
The diversity in demographics across the studies, including varying age groups, health statuses, and cultural backgrounds, underscores the necessity of personalized therapy plans. For instance, older adults may benefit more from a combination of music therapy with gentle Qigong exercises, which mitigate the risk of falls while promoting relaxation and improving sleep (95). Conversely, younger individuals, particularly those experiencing stress and anxiety (e.g., college students), might find a combination of high-intensity Biodanza and meditation more effective, leveraging the physical exertion of dance to alleviate stress and the mindfulness aspect of meditation to prepare the mind for rest (96, 97).
Additionally, for those experiencing more profound psychological issues, such as depression, integrating therapies that specifically target emotional well-being—like meditation with music therapy (98)—can be particularly beneficial. This combination can leverage the stress-reducing and mood-enhancing benefits of music alongside the mindfulness and self-awareness cultivated through meditation, offering a holistic approach to treating SIMDs.
The integration of VR technology into meditation practices presents an innovative approach to enhancing the immersion and effectiveness of mindfulness exercises for SIMDs. However, given the potential for VR to induce anxiety or discomfort in certain populations, its application should be carefully considered. Tailoring VR experiences to match individual preferences and introducing these technologies gradually can mitigate potential adverse reactions. Furthermore, combining VR-enhanced meditation with more traditional, familiar therapeutic practices like music therapy could offer a balanced approach, providing the novel benefits of VR while ensuring comfort and accessibility (99).
For the integration of arts therapies to be most effective, ongoing assessment and adaptation of therapy plans are crucial. This includes regular monitoring of individual responses to therapy, readiness to modify or switch therapies based on efficacy and preference, and continually updating the therapy plan as new evidence emerges. Future research should focus on longitudinal studies to better understand the long-term effectiveness of combined therapies and to refine these recommendations further.
SIMDs frequently coexist with, or are exacerbated by, psychological conditions such as anxiety, depression, and stress, suggesting a bidirectional relationship between sleep disturbances and mental health issues (100). The complex interplay between these factors highlights the importance of emotional regulation in the effective management of SIMDs. As sleep problems often serve as both a symptom and a contributor to mental health issues, addressing the psychological underpinnings is paramount (101). This underscores the necessity for therapeutic approaches that not only target the physiological aspects of SIMDs but also focus on psychological de-escalation. Arts therapies, with their inherent capacity for emotional expression and regulation, offer a unique conduit for this purpose (102). In the forward trajectory of research, it is imperative that experimental designs embody stringent rigor, with the incorporation of single-blind and double-blind methodologies in randomized controlled trials (RCTs) being non-negotiable to mitigate the potential for data skewness. Furthermore, the endeavor to extend art therapy over protracted durations for the amelioration of sleep disorders poses a formidable challenge in the context of healthcare personnel ratios. The paucity of healthcare professionals in numerous developing nations presents a tangible barrier to the scalable application of art therapy to a broad demographic afflicted with sleep disturbances. This scenario necessitates a considerable investment of resources and dedication, thereby underscoring the exploration of artificial intelligence (AI) as a plausible adjunct or enhancer of art therapy practices. The potential for AI to bridge the gap in patient care and augment the efficacy of arts therapies represents a nascent yet promising paradigm, meriting earnest scholarly attention.
5 Limitations
The systematic review of randomized controlled trials (RCTs) evaluating the efficacy of arts therapies in addressing SIMDs provides strong evidence supporting the potential advantages of these interventions. Nonetheless, the presence of several methodological limitations within the analyzed studies necessitates thorough scrutiny, as it could affect the interpretation of results and guide the trajectory of subsequent research in this domain.
The systematic review highlights a prevalent issue in the included randomized controlled trials (RCTs) regarding participant blinding and the blinding of individuals administering treatments. As identified using the Joanna Briggs Institute (JBI) critical appraisal tool, a majority of the studies (11 out of 17) lacked participant blinding, raising serious concerns about bias in self-reporting of symptoms and treatment response. This lack of blinding could lead participants to have heightened expectations or placebo effects, which are well-documented phenomena in clinical research. These biases can significantly skew the reported efficacy of the arts therapies, leading to potentially inflated outcomes.
The absence of blinding among treatment administrators in 16 out of the 17 reviewed studies poses a critical threat to the validity of the study findings. Unblinded facilitators might unconsciously convey their expectations to participants, affecting the latter’s responses and engagement. This methodological oversight complicates the interpretation of the efficacy of arts therapies, as the observed benefits could be attributed to non-specific effects rather than the therapeutic intervention itself. Restricting the systematic review to English-language studies introduces another significant limitation by potentially overlooking valuable research conducted in other languages. This limitation not only restricts the diversity of the data but also introduces a cultural bias, limiting the generalizability of the findings to English-speaking populations. Art therapy practices, being deeply influenced by cultural contexts, might show different levels of efficacy and engagement in diverse cultural settings. Therefore, extending future systematic reviews to include multiple languages and cultural contexts could uncover more nuanced insights about the applicability and effectiveness of arts therapies across different global populations.
The short duration of interventions reported in four of the RCTs presents another limitation regarding the sustainability of the therapy benefits. While immediate improvements in sleep quality were noted, the long-term efficacy of these interventions remains uncertain. This limitation is significant as the chronic nature of SIMDs requires sustained management strategies. Future research should focus on longitudinal studies that assess the effects of arts therapies over extended periods to better understand and validate the longevity of the therapeutic benefits.
6 Conclusion
This comprehensive review, through an extensive analysis of 17 studies, examines the efficacy and mechanisms of arts therapies—including music therapy, meditation, Tai Chi, Qigong, yoga, Biodanza, and VR meditation—in improving Sleep Initiation and Maintenance Disorders (SIMDs). The findings reveal that these arts therapies, whether employed singularly or in conjunction, serve as effective non-pharmacological interventions to enhance sleep quality. Notably, music therapy, as a passive modality, significantly improves sleep quality in both elderly and younger populations, indicating its suitability as a pre-sleep routine across various age groups. Active therapies such as meditation, Tai Chi, Qigong, and yoga not only aid in augmenting sleep quality but also demonstrate positive effects on mental health, offering relief from stress, anxiety, and symptoms of depression. These active interventions, integrating mindfulness, physical movements, and breathing techniques, provide a holistic approach to addressing both physiological and psychological factors associated with SIMDs. The research underscores the importance of tailoring personalized arts therapy programs based on age, health status, and cultural backgrounds—for instance, combining music therapy and Qigong to improve sleep in the elderly, while Biodanza and meditation are more effective in stress relief among the younger demographic. Integrating new technologies like VR with traditional therapies offers innovative experiences in treating sleep disorders. Specific to practical applications in existing medical protocols, integration strategies such as professional training on arts therapies and infrastructural enhancements in healthcare settings can facilitate their adoption. Challenges such as cultural and institutional resistance, alongside hurdles in cost and resource allocation, may impede implementation, yet growing patient preference for non-drug treatments and supportive research outcomes provide favorable conditions for their integration. Future research should focus on the long-term effects of these interventions, integration of technological innovations like artificial intelligence, and the execution of cross-cultural studies to better understand global applicability and cultural influences on therapy effectiveness. Although this review confirms the effectiveness of arts therapies in treating SIMDs, future research should focus on the longevity of therapeutic outcomes, refinement of personalized treatment plans, and innovation through new technology integration, emphasizing longitudinal study designs to understand the long-term effects of combined therapies more comprehensively and further refine treatment recommendations.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
XL: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AZ: Writing – original draft, Writing – review & editing. HL: Writing – original draft, Writing – review & editing. YL: Conceptualization, Data curation, Formal analysis, Writing – review & editing. FY: Funding acquisition, Writing – review & editing. XW: Data curation, Software, Writing – review & editing. QY: Data curation, Software, Writing – review & editing. ZZ: Investigation, Writing – review & editing. GH: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Macau University of Science and Technology’s Faculty Research Grant (No.: FRG-24–049-FA) and the Science and Technology Planning Project of Guangdong Province (2020B1212030008).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Jahrami H, BaHammam AS, Bragazzi NL, Saif Z, Faris M, Vitiello MV. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. (2021) 17:299–313. doi: 10.5664/jcsm.8930
2. Yu J, Xiang T, Pan J. The relationship between dysfunctional beliefs and attitudes about sleep and sleep structure in patients with insomnia: A controlled study. Psychology. (2020) 11:541. doi: 10.4236/psych.2020.113035
3. American Psychiatric Association D, Association AP. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American psychiatric association (2013). doi: 10.1176/appi.books.9780890425596
5. Thorpy MJ. Classification of sleep disorders. Neurotherapeutics. (2012) 9:687–701. doi: 10.1007/s13311-012-0145-6
6. Slater G, Steier J. Excessive daytime sleepiness in sleep disorders. J Thorac disease. (2012) 4:608. doi: 10.3978/j.issn.2072-1439.2012.10.07
7. Johnson DA, Billings ME, Hale L. Environmental determinants of insufficient sleep and sleep disorders: implications for population health. Curr Epidemiol Rep. (2018) 5:61–9. doi: 10.1007/s40471-018-0139-y
8. Gradisar M, Gardner G, Dohnt H. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep Med. (2011) 12:110–8. doi: 10.1016/j.sleep.2010.11.008
9. Altevogt BM, Colten HR. Institute of Medicine (US) Committee on sleep medicine and research. Sleep disorders and sleep deprivation: an Unmet public health problem [Internet]. Colten HR, Altevogt BM, editors. Washington (DC): National Academies Press (US). (2006) (The National Academies Collection: Reports funded by National Institutes of Health). Available from: http://www.ncbi.nlm.nih.gov/books/NBK19960/.
10. Khan-Hudson A, Alessi CA. Sleep and quality of life in older people. Sleep Qual Life Clin Med. (2008), 131–8. doi: 10.1007/978-1-60327-343-5_15
11. Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders: an opportunity for prevention? JAMA. (1989) 262:1479–84. doi: 10.1001/jama.262.11.1479
12. Theorell-Haglöw J, Miller CB, Bartlett DJ, Yee BJ, Openshaw HD, Grunstein RR. Gender differences in obstructive sleep apnoea, insomnia and restless legs syndrome in adults–What do we know? A clinical update. Sleep Med Rev. (2018) 38:28–38. doi: 10.1016/j.smrv.2017.03.003
13. Lee T-H, Yen T-T, Chiu N-Y, Chang C-C, Hsu W-Y, Chang Y-J, et al. Depression is differently associated with sleep measurement in obstructive sleep apnea, restless leg syndrome and periodic limb movement disorder. Psychiatry Res. (2019) 273:37–41. doi: 10.1016/j.psychres.2018.12.166
14. Diaz S, Abad K, Patel SR, Unruh ML eds. Emerging treatments for insomnia, sleep apnea, and restless leg syndrome among dialysis patients. In: Seminars in Nephrology. Elsevier. doi: 10.1016/j.semnephrol.2021.10.005
15. Liu Y, Croft JB, Wheaton AG, Perry GS, Chapman DP, Strine TW, et al. Association between perceived insufficient sleep, frequent mental distress, obesity and chronic diseases among US adults, 2009 behavioral risk factor surveillance system. BMC Public Health. (2013) 13:1–8. doi: 10.1186/1471-2458-13-84
16. Araghi MH, Jagielski A, Neira I, Brown A, Higgs S, Thomas GN, et al. The complex associations among sleep quality, anxiety-depression, and quality of life in patients with extreme obesity. Sleep. (2013) 36:1859–65. doi: 10.5665/sleep.3216
17. Riera-Sampol A, Bennasar-Veny M, Tauler P, Nafría M, Colom M, Aguilo A. Association between depression, lifestyles, sleep quality, and sense of coherence in a population with cardiovascular risk. Nutrients. (2021) 13:585. doi: 10.3390/nu13020585
18. Alvaro PK, Roberts RM, Harris JK. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep. (2013) 36:1059–68. doi: 10.5665/sleep.2810
19. Guarnieri B, Sorbi S. Sleep and cognitive decline: a strong bidirectional relationship. It is time for specific recommendations on routine assessment and the management of sleep disorders in patients with mild cognitive impairment and dementia. Eur Neurol. (2015) 74:43–8. doi: 10.1159/000434629
20. Wennberg AM, Wu MN, Rosenberg PB, Spira AP eds. Sleep disturbance, cognitive decline, and dementia: a review. In: Seminars in neurology. NIH Public Access. doi: 10.1055/s-0037-1604351
21. Medic G, Wille M, Hemels ME. Short-and long-term health consequences of sleep disruption. Nat Sci sleep. (2017) 9:151–61. doi: 10.2147/NSS
22. Rodriguez JC, Dzierzewski JM, Alessi CA. Sleep problems in the elderly. Med Clinics. (2015) 99:431–9. doi: 10.1016/j.mcna.2014.11.013
23. Nutt D, Wilson S, Paterson L. Sleep disorders as core symptoms of depression. Dialogues Clin Neurosci. (2008) 10:329–36. doi: 10.31887/DCNS.2008.10.3/dnutt
24. Amaral AP, Soares MJ, Pinto AM, Pereira AT, Madeira N, Bos SC, et al. Sleep difficulties in college students: The role of stress, affect and cognitive processes. Psychiatry Res. (2018) 260:331–7. doi: 10.1016/j.psychres.2017.11.072
25. Sateia MJ, Buysse DJ, Krystal AD, Neubauer DN, Heald JL. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin sleep Med. (2017) 13:307–49. doi: 10.5664/jcsm.6470
26. Morin AK, Jarvis CI, Lynch AM. Therapeutic options for sleepnsuticicnsyo and sleepnsutic insomnia. Pharmacotherapy: J Hum Pharmacol Drug Ther. (2007) 27:89–110. doi: 10.1592/phco.27.1.89
27. Estivill E, Bové A, García-Borreguero D, Gibert J, Paniagua J, Pin G, et al. Consensus on drug treatment, definition and diagnosis for insomnia. Clin Drug Invest. (2003) 23:351–86. doi: 10.2165/00044011-200323060-00001
28. Morin CM, Drake CL, Harvey AG, Krystal AD, Manber R, Riemann D, et al. Insomnia disorder. Nat Rev Dis primers. (2015) 1:1–18. doi: 10.1038/nrdp.2015.26
29. Monti J, Attali P, Monti D, Zipfel A, de la Giclais B, Morselli P. Zolpidem and rebound insomnia-a double-blind, controlled polysomnographic study in chronic insomniac patients. Pharmacopsychiatry. (1994) 27:166–75. doi: 10.1055/s-2007-1014298
30. Zisapel N. Drugs for insomnia. Expert Opin emerging Drugs. (2012) 17:299–317. doi: 10.1517/14728214.2012.690735
31. Pagel J, Pandi-Perumal SR, Monti JM. Treating insomnia with medications. Sleep Sci Practice. (2018) 2:5. doi: 10.1186/s41606-018-0025-z
32. Pepe M, Lanzotti P, Mazza M. Hypnotics: course and duration of therapy, side effects, contraindications, interactions, withdrawal syndromes, and resistance to therapy. In: NeuroPsychopharmacotherapy. Springer (2021). p. 1–28. doi: 10.1007/978-3-030-62059-2_455
33. Babiloni AH, Beetz G, Bruneau A, Martel MO, Cistulli PA, Nixdorf DR, et al. Multitargeting the sleep-pain interaction with pharmacological approaches: A narrative review with suggestions on new avenues of investigation. Sleep Med Rev. (2021) 59:101459. doi: 10.1016/j.smrv.2021.101459
34. Kayumov L, Hawa R, Shapiro CM, Kurland HD, Oster M, Bornstein J, et al. Alternative therapies in sleep medicine. Sleep Psychiatry. (2004) 434:19.
35. Sembian N, Aathi MK. Chromo therapy: healing power of colors. i-Manager's J Nursing. (2015) 5:6. doi: 10.26634/jnur.5.4.4811
36. Kavurmacı M, Dayapoğlu N, Tan M. Effect of music therapy on sleep quality. Altern therapies Health Med. (2020) 26:4.
37. Halder D, Barik B, Dasgupta R, Saumendu D. Aroma therapy: An art of healing. Indian Res J Pharm Science. (2018) 17:1540–58. doi: 10.21276/irjps
38. Dieterich-Hartwell R. Dance/movement therapy in the treatment of post traumatic stress: A reference model. arts psychother. (2017) 54:38–46. doi: 10.1016/j.aip.2017.02.010
39. Stuckey HL, Nobel J. The connection between art, healing, and public health: A review of current literature. Am J Public Health. (2010) 100:254–63. doi: 10.2105/AJPH.2008.156497
40. Gräsel E, Wiltfang J, Kornhuber J. Non-drug therapies for dementia: an overview of the current situation with regard to proof of effectiveness. Dementia geriatric Cogn Disord. (2003) 15:115–25. doi: 10.1159/000068477
41. Chen T-L, Chang S-C, Hsieh H-F, Huang C-Y, Chuang J-H, Wang H-H. Effects of mindfulness-based stress reduction on sleep quality and mental health for insomnia patients: a meta-analysis. J psychosomatic Res. (2020) 135:110144. doi: 10.1016/j.jpsychores.2020.110144
42. Chen K-M, Chen M-H, Lin M-H, Fan J-T, Lin H-S, Li C-H. Effects of yoga on sleep quality and depression in elders in assisted living facilities. J Nurs Res. (2010) 18:53–61. doi: 10.1097/JNR.0b013e3181ce5189
43. Wang C-F, Sun Y-L, Zang H-X. Music therapy improves sleep quality in acute and chronic sleep disorders: A meta-analysis of 10 randomized studies. Int J Nurs Stud. (2014) 51:51–62. doi: 10.1016/j.ijnurstu.2013.03.008
44. Lee S, Kang J. Meditation through virtual reality has a positive effect on the sleep of intensive care unit patients. Aust Crit Care. (2020) 33:S23–S4. doi: 10.1016/j.aucc.2020.04.073
45. He B, Zhang L, Zhuang J-h, Xu J, Li P, Peng H. The effects of different meditation exercises on sleep quality in older people: a network meta-analysis. Eur Geriatric Med. (2019) 10:543–52. doi: 10.1007/s41999-019-00212-1
46. Liu C. Examining the effectiveness of Solution-Focused Art Therapy (SF-AT) for sleep problems of children with traumatic experience. The Ohio State University (2017).
47. Atkinson NL, Permuth-Levine R. Benefits, barriers, and cues to action of yoga practice: A focus group approach. Am J Health behavior. (2009) 33:3–14. doi: 10.5993/AJHB.33.1.1
48. Menezes CB, Dalpiaz NR, Kiesow LG, Sperb W, Hertzberg J, Oliveira AA. Yoga and emotion regulation: A review of primary psychological outcomes and their physiological correlates. Psychol Neurosci. (2015) 8:82. doi: 10.1037/h0100353
49. Gard T, Noggle JJ, Park CL, Vago DR, Wilson A. Potential self-regulatory mechanisms of yoga for psychological health. Front Hum Neurosci. (2014) 770. doi: 10.3389/fnhum.2014.00770
50. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J surg. (2021) 88:105906. doi: 10.1016/j.ijsu.2021.105906
51. Moher D, Liberati A, Tetzlaff J, Altman DG, Group* P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Internal Med. (2009) 151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135
52. Page MJ, Shamseer L, Tricco AC. Registration of systematic reviews in PROSPERO: 30,000 records and counting. Systematic Rev. (2018) 7:1–9. doi: 10.1186/s13643-018-0699-4
53. Munn Z, Peters MD, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res methodology. (2018) 18:1–7. doi: 10.1186/s12874-018-0611-x
54. Singh C, Cross W, Munro I, Jackson D. Occupational stress facing nurse academicsna mixedmicsnals systematic review. J Clin Nurs. (2020) 29:720–35. doi: 10.1111/jocn.15150
55. Amir-Behghadami M, Janati A. Population, Intervention, Comparison, Outcomes and Study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emergency Med J. (2020) 37(6):387. doi: 10.1136/emermed-2020-209567
56. Treadwell JR, Singh S, Talati R, McPheeters ML, Reston JT. A framework for best evidence approaches can improve the transparency of systematic reviews. J Clin Epidemiol. (2012) 65:1159–62. doi: 10.1016/j.jclinepi.2012.06.001
57. Lee SY, Kang J. Effect of virtual reality meditation on sleep quality of intensive care unit patients: a randomised controlled trial. Intensive Crit Care Nursing. (2020) 59:102849. doi: 10.1016/j.iccn.2020.102849
58. Huberty J, Puzia ME, Green J, Vlisides-Henry RD, Larkey L, Irwin MR, et al. A mindfulness meditation mobile app improves depression and anxiety in adults with sleep disturbance: Analysis from a randomized controlled trial. Gen Hosp Psychiatry. (2021) 73:30–7. doi: 10.1016/j.genhosppsych.2021.09.004
59. Ong JC, Manber R, Segal Z, Xia Y, Shapiro S, Wyatt JK. A randomized controlled trial of mindfulness meditation for chronic insomnia. Sleep. (2014) 37:1553–63. doi: 10.5665/sleep.4010
60. Black DS, O’Reilly GA, Olmstead R, Breen EC, Irwin MR. Mindfulness meditation and improvement in sleep quality and daytime impairment among older adults with sleep disturbances: a randomized clinical trial. JAMA Internal Med. (2015) 175:494–501. doi: 10.1001/jamainternmed.2014.8081
61. Yeh S-CJ, Chang M-Y. The effect of Qigong on menopausal symptoms and quality of sleep for perimenopausal women: a preliminary observational study. J Altern Complementary Med. (2012) 18:567–75. doi: 10.1089/acm.2011.0133
62. Li F, Fisher KJ, Harmer P, Irbe D, Tearse RG, Weimer C. Tai Chi and selfer8(6) quality of sleep and daytime sleepiness in older adults: a randomized controlled trial. J Am Geriatrics Society. (2004) 52:892–900. doi: 10.1111/j.1532-5415.2004.52255.x
63. Irwin MR, Olmstead R, Motivala SJ. Improving sleep quality in older adults with moderate sleep complaints: a randomized controlled trial of Tai Chi Chih. Sleep. (2008) 31:1001–8. doi: 10.5665/sleep/31.7.1001
64. López-Rodríguez MM, Baldrich-Rodríguez I, Ruiz-Muelle A, Cortés-Rodríguez AE, Lopezosa-Estepa T, Roman P. Effects of Biodanza on stress, depression, and sleep quality in university students. J Altern Complementary Med. (2017) 23:558–65. doi: 10.1089/acm.2016.0365
65. Huang C-Y, Chang E-T, Hsieh Y-M, Lai H-L. Effects of music and music video interventions on sleep quality: A randomized controlled trial in adults with sleep disturbances. Complementary therapies Med. (2017) 34:116–22. doi: 10.1016/j.ctim.2017.08.015
66. Wang Q, Chair SY, Wong EML, Li X. The effects of music intervention on sleep quality in community-dwelling elderly. J Altern Complementary Med. (2016) 22:576–84. doi: 10.1089/acm.2015.0304
67. Chang E-T, Lai H-L, Chen P-W, Hsieh Y-M, Lee L-H. The effects of music on the sleep quality of adults with chronic insomnia using evidence from polysomnographic and self-reported analysis: a randomized control trial. Int J Nurs Stud. (2012) 49:921–30. doi: 10.1016/j.ijnurstu.2012.02.019
68. Harmat L, Takács J, Bódizs R. Music improves sleep quality in students. J advanced nursing. (2008) 62:327–35. doi: 10.1111/j.1365-2648.2008.04602.x
69. Shum A, Taylor BJ, Thayala J, Chan MF. The effects of sedative music on sleep quality of older community-dwelling adults in Singapore. Complementary therapies Med. (2014) 22:49–56. doi: 10.1016/j.ctim.2013.11.003
70. Lai HL, Good M. Music improves sleep quality in older adults. J advanced nursing. (2006) 53:134–44. doi: 10.1111/j.1365-2648.2006.03693.x
71. Sharpe E, Butler MP, Clark-Stone J, Soltanzadeh R, Jindal R, Hanes D, et al. A closer look at yoga nidra-early randomized sleep lab investigations. J Psychosomatic Res. (2023) 166:111169. doi: 10.1016/j.jpsychores.2023.111169
72. Khalsa SBS, Goldstein MR. Treatment of chronic primary sleep onset insomnia with Kundalini yoga: a randomized controlled trial with active sleep hygiene comparison. J Clin Sleep Med. (2021) 17:1841–52. doi: 10.5664/jcsm.9320
73. Winbush NY, Gross CR, Kreitzer MJ. The effects of mindfulness-based stress reduction on sleep disturbance: a systematic review. Explore. (2007) 3:585–91. doi: 10.1016/j.explore.2007.08.003
74. Reimer MA, Flemons WW. Quality of life in sleep disorders. Sleep Med Rev. (2003) 7:335–49. doi: 10.1053/smrv.2001.0220
75. Navarro-Haro MV, López-del-Hoyo Y, Campos D, Linehan MM, Hoffman HG, García-Palacios A, et al. Meditation experts try Virtual Reality Mindfulness: A pilot study evaluation of the feasibility and acceptability of Virtual Reality to facilitate mindfulness practice in people attending a Mindfulness conference. PloS One. (2017) 12:e0187777. doi: 10.1371/journal.pone.0187777
76. Ma J, Zhao D, Xu N, Yang J. The effectiveness of immersive virtual reality (VR) based mindfulness training on improvement mental-health in adults: A narrative systematic review. Explore. (2023) 19:310–8. doi: 10.1016/j.explore.2022.08.001
77. Victorson D, Kentor M, Maletich C, Lawton RC, Kaufman VH, Borrero M, et al. Mindfulness meditation to promote wellness and manage chronic disease: a systematic review and meta-analysis of mindfulness-based randomized controlled trials relevant to lifestyle medicine. Am J Lifestyle Med. (2015) 9:185–211. doi: 10.1177/1559827614537789
78. Klich W, Milert A. Tai chi and Qigong as a form of physical activity of people of all ages in the context of modern physiotherapy. Phys Activity Review. (2018) 6:22–8. doi: 10.16926/par.
79. Abbott R, Chang DD, Eyre H, Lavretsky H. Mind-body practices tai chi and qigong in the treatment and prevention of psychiatric disorders. Complementary Integr Treatments Psychiatr Pract. (2017) 261:261–79.
80. Moratelli JA, Veras G, Lyra VB, Silveira Jd, Colombo R, de Azevedo Guimarães AC. Evidence of the effects of dance interventions on adults mental health: A systematic review. J Dance Med Sci. (2023) 27(4):1089313X231178095. doi: 10.1177/1089313X231178095
81. Trahan T, Durrant SJ, Müllensiefen D, Williamson VJ. The music that helps people sleep and the reasons they believe it works: A mixed methods analysis of online survey reports. PloS One. (2018) 13:e0206531. doi: 10.1371/journal.pone.0206531
82. Dickson GT, Schubert E. How does music aid sleep? Literature review. Sleep Med. (2019) 63:142–50. doi: 10.1016/j.sleep.2019.05.016
83. Cabral P, Meyer HB, Ames D. Effectiveness of yoga therapy as a complementary treatment for major psychiatric disorders: a meta-analysis. primary Care companion CNS Disord. (2011) 13:26290. doi: 10.4088/PCC.10r01068
84. Khalsa S. Yoga as a therapeutic intervention. Principles Pract Stress management. (2007) 3:449–62.
85. Pavlov A, Kameg K, Cline TW, Chiapetta L, Stark S, Mitchell AM. Music therapy as a nonpharmacological intervention for anxiety in patients with a thought disorder. Issues Ment Health Nursing. (2017) 38:285–8. doi: 10.1080/01612840.2016.1264516
86. Mofredj A, Alaya S, Tassaioust K, Bahloul H, Mrabet A. Music therapy, a review of the potential therapeutic benefits for the critically ill. J Crit Care. (2016) 35:195–9. doi: 10.1016/j.jcrc.2016.05.021
87. Firdaus FA, Khaerunnisa RN, Ariyanto H. The effect music therapy on quality of sleep. Genius J. (2020) 1:23–31. doi: 10.56359/gj.v1i1
88. Neuendorf R, Wahbeh H, Chamine I, Yu J, Hutchison K, Oken BS. The effects of mind-body interventions on sleep quality: a systematic review. Evidence-Based Complementary Altern Med. (2015) 2015:7–8. doi: 10.1155/2015/902708
89. Kim J, Choi D, Yeo MS, Yoo GE, Kim SJ, Na S. Effects of patient-directed interactive music therapy on sleep quality in postoperative elderly patients: a randomized-controlled trial. Nat Sci sleep. (2020) 12:791–800. doi: 10.2147/NSS.S286375
90. Montgomery P, Dennis J. A systematic review of non-pharmacological therapies for sleep problems in later life. Sleep Med Rev. (2004) 8:47–62. doi: 10.1016/S1087-0792(03)00026-1
91. Chan MF, Wong ZY, Thayala N. The effectiveness of music listening in reducing depressive symptoms in adults: a systematic review. Complementary therapies Med. (2011) 19:332–48. doi: 10.1016/j.ctim.2011.08.003
92. Wang C, Li G, Zheng L, Meng X, Meng Q, Wang S, et al. Effects of music intervention on sleep quality of older adults: A systematic review and meta-analysis. Complementary therapies Med. (2021) 59:102719. doi: 10.1016/j.ctim.2021.102719
93. Mindell JA, Williamson AA. Benefits of a bedtime routine in young children: Sleep, development, and beyond. Sleep Med Rev. (2018) 40:93–108. doi: 10.1016/j.smrv.2017.10.007
94. Schmid W, Ostermann T. Home-based music therapy-a systematic overview of settings and conditions for an innovative service in healthcare. BMC Health Serv Res. (2010) 10:1–10. doi: 10.1186/1472-6963-10-291
95. Gaylord S, Crotty N. Enhancing function with complementary therapies in geriatric rehabilitation. Topics Geriatric Rehabilitation. (2002) 18:63–80. doi: 10.1097/00013614-200212000-00007
96. Berger BG. Coping with stress: The effectiveness of exercise and other techniques. Quest. (1994) 46:100–19. doi: 10.1080/00336297.1994.10484112
97. Baghurst T, Kelley BC. An examination of stress in college students over the course of a semester. Health promotion practice. (2014) 15:438–47. doi: 10.1177/1524839913510316
98. Innes KE, Selfe TK, Khalsa DS, Kandati S. Effects of meditation versus music listening on perceived stress, mood, sleep, and quality of life in adults with early memory loss: A pilot randomized controlled trial. J Alzheimer's Disease. (2016) 52:1277–98. doi: 10.3233/JAD-151106
99. Ong TL, Ruppert MM, Akbar M, Rashidi P, Ozrazgat-Baslanti T, Bihorac A, et al. Improving the intensive care patient experience with virtual reality—A feasibility study. Crit Care Explor. (2020) 2:6. doi: 10.1097/CCE.0000000000000122
100. Farzaneh F, Momayyezi M, Lotfi MH. Relationship between quality of sleep and mental health in female students of Shahid Sadoughi University of Medical Sciences (2015). J Fundamentals Ment Health. (2018) 20:2.
101. Gupta R, Das S, Gujar K, Mishra K, Gaur N, Majid A. Clinical practice guidelines for sleep disorders. Indian J Psychiatry. (2017) 59:S116. doi: 10.4103/0019-5545.196978
102. Haeyen S, van Hooren S, van der Veld WM, Hutschemaekers G. Measuring the contribution of art therapy in multidisciplinary treatment of personality disorders: The construction of the Selftructionina and Emotion Regulation in Art Therapy Scale (SERATS). Pers Ment Health. (2018) 12:3–14. doi: 10.1002/pmh.1379
Keywords: Arts Therapies, sleep disorders, psychotherapy, complementary interventions, mental health
Citation: Luo X, Zhang A, Li H, Li Y, Ying F, Wang X, Yang Q, Zhang Z and Huang G (2024) The role of arts therapies in mitigating Sleep Initiation and Maintenance Disorders: a systematic review. Front. Psychiatry 15:1386529. doi: 10.3389/fpsyt.2024.1386529
Received: 15 February 2024; Accepted: 01 May 2024;
Published: 16 May 2024.
Edited by:
Guanhu Yang, Ohio University, United StatesReviewed by:
Hao Chi, Southwest Medical University, ChinaYinghua He, FR Acupuncture & Chinese Medicine Clinic, United States
Copyright © 2024 Luo, Zhang, Li, Li, Ying, Wang, Yang, Zhang and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guanghui Huang, Z2hodWFuZzFAbXVzdC5lZHUubW8=
†These authors have contributed equally to this work
 Xuexing Luo
Xuexing Luo Aijia Zhang
Aijia Zhang Hong Li1†
Hong Li1†