- 1IFT Institut für Therapieforschung, Centre for Mental Health and Addiction Research, Munich, Germany
- 2Department of Child and Adolescent Psychiatry, Psychosomatics, and Psychotherapy, University of Cologne, Faculty of Medicine and University Hospital Cologne, Cologne, Germany
- 3Department of Public Health Sciences, Centre for Social Research on Alcohol and Drugs, Stockholm University, Stockholm, Sweden
- 4Centre of Interdisciplinary Addiction Research (ZIS), Department of Psychiatry and Psychotherapy, University Medical Centre Hamburg-Eppendorf, Hamburg, Germany
- 5Institute of Psychology, ELTE, Eötvös Loránd University, Budapest, Hungary
- 6German Youth Institute (Deutsches Jugendinstitut e.V. (DJI)), Munich, Germany
- 7Department of Psychiatry and Psychotherapy, University Hospital of Munich, Munich, Germany
- 8Charlotte Fresenius University, Munich, Germany
- 9Pettenkofer School of Public Health, Munich, Germany
Introduction: Individuals with gambling disorder (GD) harbor cognitive distortions and dysfunctional beliefs about gambling that may foster problematic gambling behaviour. Evidence on particularly detrimental attitudes and beliefs is however lacking. To close this knowledge gap, we analysed associations between gambling attitudes and beliefs (Gambling Attitudes and Beliefs Survey (GABS-15)) and severity of gambling disorder (DSM-5 criteria met) in a German cohort of 123 individuals receiving outpatient gambling treatment.
Methods: Data from the "Katamnese-Study" covering a 36-months timeframe with 5 assessment points was pooled. The multidimensional structure of the GABS-15 was examined using explorative and confirmatory factor analyses, followed by mixed-effect regression models using different operationalizations of the GABS-15.
Results: A three-factorial structure comprising “attitudes while gambling”, “sensation-seeking / excitement”, and "gambling fallacies” demonstrated better fit indices than the GABS-15 sum score. Only the "gambling fallacies " factor (1.00, p<0.05; 15.36, p < 0.01) was significantly associated with increased severity of GD.
Discussion: As a one-dimensional conceptualization of gambling-related attitudes and beliefs might not sufficiently guide staff of outpatient treatment facilities regarding priority setting in gambling care, evidence on attitudes with particularly detrimental associations is highly warranted. Here, focussing on mitigating "gambling' fallacies" by tailored treatment strategies appears promising.
Introduction
Gambling disorder (GD), a behavioral addiction characterized by uncontrollable gambling (1) causes societal harm as well as substantial psychological, social, and financial strain (2). Individuals with GD experience lower quality of life, work, and health, and often face high rates of psychiatric comorbidity compared to non-gamblers (2, 3).
Gambling behavior is triggered by gambling-related attitudes (4, 5), emotions [e. g., arousal, emotional excitement, see (6, 7)], as well as cognitive biases and irrational beliefs (4, 8, 9), which are crucial factors in the development and maintenance of problem gambling and GD (9, 10). Cognitive biases and irrational beliefs stem from an erroneous attribution of random game outcomes to a presumed but not existing cause-and-effect relationship. For instance, players may attribute favorable outcomes to personal skills and unfavorable ones to bad luck. The concept of “gambler’s fallacy”, meaning that players expect deviations from chance (such as prolonged losses) to eventually balance out and correct themselves in subsequent sequences, relies on similar assumptions (11, 12).
These misconceptions also support the development of specific beliefs, gambling strategies, and behaviors aiming at exerting control over game outcomes (13). Gamblers often adopt specific attitudes that they assume to influence the game’s outcome and to increase the chance of winning. These include being cautious and composed regardless of the situation (whether winning or losing), exuding confidence during the game, and, for some, even gambling with passion (4, 14, 15). Additionally, in some cases, superstitious beliefs come into play. These are understood as a strong conviction that arises from the mistaken perception of a cause-and-effect relationship between two unrelated events, leading to the belief that certain rituals or the presence of “lucky charms” can influence the outcome of a game and contribute to success (16).
Individuals with gambling problems are more likely to endorse irrational beliefs about gambling (17) and to experience increased illusions of control (18, 19). Furthermore, findings indicate a correlation between positively valued attitudes to gambling and GD, perpetuating a misguided sense of control (20, 21).
A widely used tool to assess cognitive distortions in gamblers is the Gambling Attitudes and Beliefs Survey (GABS) (5), which assesses “gambling affinity” via a one-dimensional sum score created from 35 items on cognitive biases, irrational beliefs, and positively valued attitudes to gambling. GABS and its 15-items short version (GABS 15) (22), have been demonstrated to be associated with gambling behavior (23), to discriminate between problem and non-problem gamblers, to capture behavioral and cognitive changes during inpatient treatment (24), and to predict relapse (25, 26) as well as recovery (27).
However, concerns have been raised about the one-dimensionality claim. Factor analyses revealed a multidimensional structure for both the original GABS (5 factors: strategies, chasing, attitudes, luck, and emotions) (15) and the GABS-15 (3 factors: sensation seeking/illusion of control, luck/gambler’s fallacy, and attitude/emotions) (28). Our study aims to 1) broaden the pre-existing body of evidence on the GABS-15’s factorial structure and 2) investigate how the factorial structure interacts with problem gambling.
Methods
Design and setting
Data were collected as part of the “Katamnese-Study”, a prospective, naturalistic cohort study conducted in 28 Bavarian outpatient addiction care facilities (OACF) between 2014 and 2019. Participants completed a composite diagnostic interview at admission and written questionnaires at admission and at 6-, 12-, 24-, and 36-month follow-ups. These data were linked to individual routine documentation from the German Addiction Care Statistical Service. Further details on study design, instruments used, and methodology have been published elsewhere (29).
Study sample
Adults receiving treatment for GD, possessing proficient German language skills, and engaging in a minimum of three interactions with their corresponding OACF were eligible for inclusion in the study. Recruitment took place between December 2014 and August 2016. 145 clients provided informed consent and participated in the baseline assessment. From this initial pool, 22 individuals were excluded from the final analysis due to missing baseline information on the GABS-15 (n = 6), gambling-related problems (n = 2) and/or treatment termination at follow-up 3 (n = 7). Additionally, participants still undergoing treatment at follow-up 3 (n = 7) were excluded, resulting in a final sample size of 123 participants. Detailed information on the study’s sampling procedure has been published elsewhere (30, 31).
Measures of interest
Gambling-related problems during the 12 months prior to baseline and the period between the distinct follow-up assessments were assessed using a German translation of the DSM-IV-oriented “Stinchfield criteria” (hereafter: GD criteria questionnaire), a validated tool to measure the severity of GD (32). The more recent DSM-5 classification categorizes GD as mild (4 – 5 criteria met), moderate (6 – 7 criteria met), and severe (8 – 9 criteria met). To align the GD criteria questionnaire with DSM-5 guidelines, those items about the eighth criterion concerning illegal activities were excluded. Thus, the adapted GD criteria questionnaire assesses eight of the nine DSM-5 criteria for GD by two dummy-coded items and the remaining ninth criterion (“withdrawal”) by one dummy-coded item. Each DSM-5 criterion was considered fulfilled if at least one of the associated items was affirmed. The total number of endorsed DSM-5 criteria was summed up at each assessment point (baseline, follow-up 1, follow-up 2, follow-up 3, follow-up 4), resulting in a GD score ranging from 0 to 9 which reflects severity of GD according to DSM-5.
Gambling-related attitudes and beliefs were measured by the German version of the GABS-15 (33) (Supplementary Table 1). The GABS-15 is a 15 item, forced-choice instrument capturing cognitive biases, irrational beliefs, degree of subjective arousal, and excitement experienced through gambling, as well as positively valued attitudes towards gambling. Each item is measured on a 4-point Likert scale (1 = “strongly disagree” to 4 = “strongly agree”). Item-specific scores are summed up resulting in a total score of 15 to 60 points, with higher scores indicating more substantial cognitive distortions.
Covariables
Comorbid mental disorders were assessed at baseline via the Composite International Diagnostic Interview (CIDI) (34). We considered affective disorders (yes/no), an umbrella term for major depression, dysthymic disorder, and bipolar disorders (35), and anxiety disorders (yes/no), an umbrella term for panic disorder, agoraphobia, specific phobia, social phobia, generalized anxiety disorder, unspecified anxiety disorder, obsessive-compulsive disorder, and post-traumatic stress disorder (35).
Electronic gambling machines (EGMs) represent one of the detrimental forms of gambling and were reported to be extensively used by individuals seeking help (36, 37). Thus, participation in EGM plays was incorporated as a dichotomized covariable (yes/no).
Migration background has been identified as a risk factor for the less favorable development of GD (30, 38). Thus, self-reported migration background (yes/no) according to the definition provided by the Federal Statistical Office of the Federal Republic of Germany was accounted for. This means that a migration background exists if individuals had migrated to Germany themselves or if one of their (grand)parents had immigrated prior to their birth (39).
Furthermore, we collected self-reported information if GD-related help had already been sought prior to the current help-seeking episode (yes/no). Self-reported age (in years) and sex (male/female) were used as standard demographic covariates.
Ethical statement
All ethical protocols, including those related to data protection and participant well-being, were strictly adhered to in the conduct of this research. The research project received ethical clearance from the German Association for Psychology (Deutsche Gesellschaft für Psychologie - DGPs) under the reference LK 092014 on November 3, 2014, indicating its compliance with ethical standards.
Statistical analysis
Using our longitudinal data, we pooled all individual observations over the distinct assessment points and conducted exploratory factor analyses (EFA) on the GABS-15 items using varimax rotation. Kaiser-Meyer-Olkin index, Bartlett test of sphericity, Kaiser-Guttmann criterion, and scree plot inspection were used for interpreting the factor structure. Additionally, Cronbach’s Alpha was computed to evaluate internal consistency. Factor scores were saved for further analyses.
To evaluate the compatibility of our empirically derived factor solution with the one-dimensional factor structure suggested by Breen and Zuckerman (5) and the three-factor structure proposed by Gehlenborg and colleagues (28), we conducted confirmatory factor analyses (CFA) using the Chi-square test, comparative fit index (CFI), Tucker–Lewis index (TLI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR) for comparison and interpretation.
To investigate the association between the identified dimensions and severity of GD, we applied three mixed-effects regression models that compared a) the GABS-15 sum score [model 1; Breen and Zuckermann (5)], b) the three-factor solution suggested by Gehlenborg et al. (28) (model 2), and c) our empirically derived solution (model 3).
To address individual variation in changes over time and to account for intra-subject correlation in the context of repeated measurements, all models incorporated time and participant ID as random effects. Furthermore, all analyses were adjusted for the presence of affective (reference: no) or anxiety disorders (reference: no), migration background (reference: no), EGM-play at baseline (reference: no), GD-related help sought prior to the current help-seeking episode (reference: no), age, and sex (reference: male). Considering the small sample size, we performed 1,000 non-parametric bootstrap replications to obtain more accurate parameter estimates and measures of uncertainty [i. e., 95%-confidence intervals (CI) (40)].
To assess the robustness of our findings, we repeated our models in a sensitivity analysis using gambling behavior as an alternative outcome. Here gambling behavior was represented as weekly gambling hours. This parameter was derived as a multiplicative index using information on gambling frequency (average number of gambling days per week) and gambling intensity (average number of hours spent per gambling day) in the previous 12 months (for baseline) and the time since the last assessment point for each follow-up.
All statistical analyses were conducted using Stata/SE 15 (Stata Corp LP; College Station, TX, USA).
Results
Study participation and participants’ baseline characteristics
Of the 123 individuals included, 73.2% (n = 90) participated at follow-up 1, 62.6% (n = 77) at follow-up 2, 55.3% (n = 68) at follow-up 3, and 49.6% (n = 61) at follow-up 4. 43.9% (n = 54) responded at all four follow-ups.
As summarized in Table 1, at baseline, study participants were on average 35.5 (SD = 10.8) years old, 86.2% (n = 106) were male, and 30.9% (n = 38) had a migration background. 55.1% (n = 59) were diagnosed with an affective disorder and 33.6% (n = 36) with an anxiety disorder. 88.4% (n = 107) had previously sought GD-related help and 76.0% (n = 92) reported gambling on EGMs. The average GABS-15 score was 35.7 (SD = 8.0). Agreement to the distinct GABS-15 Items is visualized in Supplementary Figure 1.
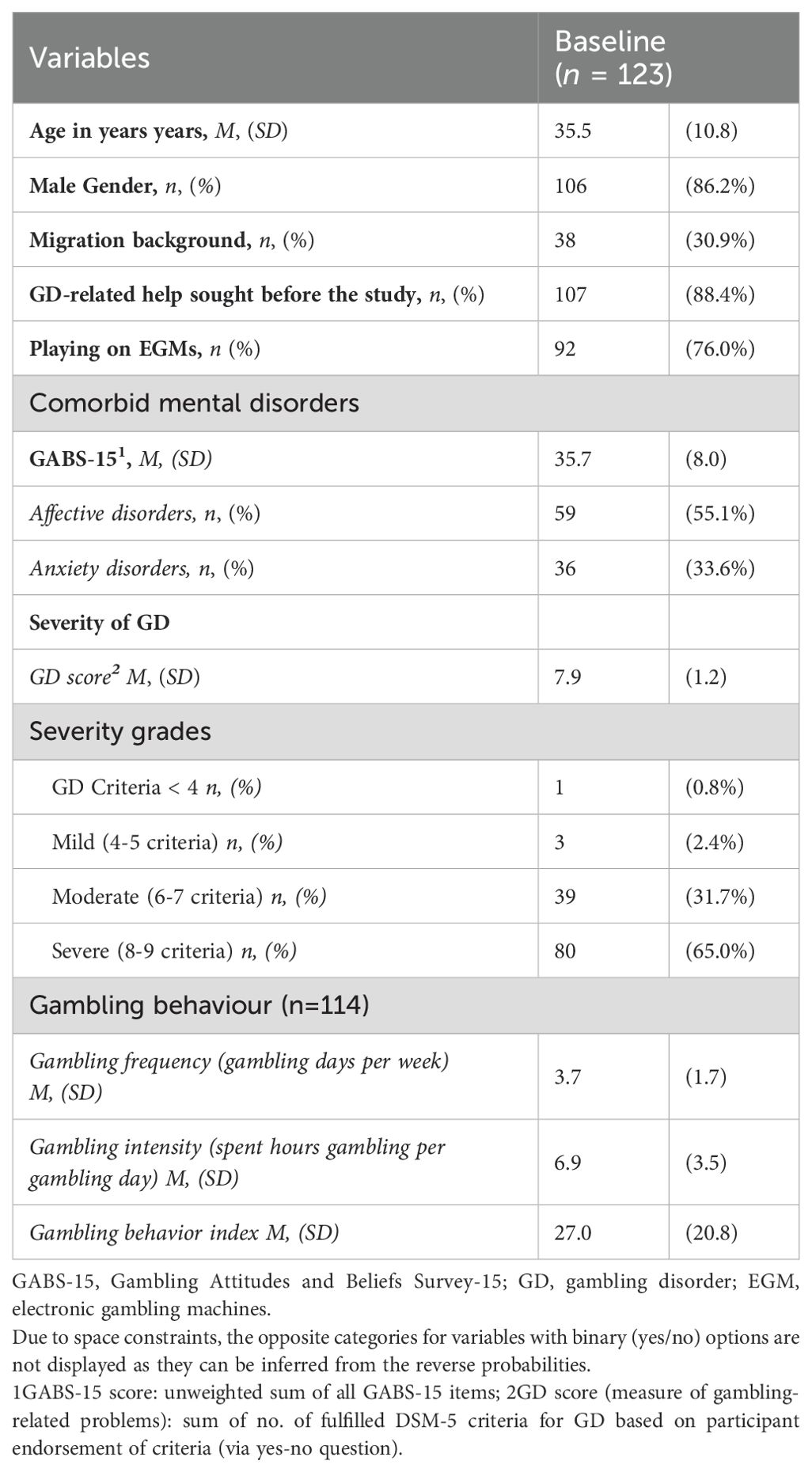
Table 1. Participant demographics, comorbid mental disorders, GABS-15, and gambling characteristics.
The average GD score was 7.9 (SD = 1.2), with 2.4% (n = 3) of participants meeting the criteria for mild GD, 31.7% (n = 39) for moderate GD, and 65.0% (n = 80) for severe GD. The participants gambled on average 3.7 days (SD = 1.7) per week and 6.9 hours (SD = 3.5) per gambling day corresponding to 27.0 weekly gambling hours (SD = 20.8).
Factor analysis
Supplementary Table 2 presents the item-total correlations among GABS items and Cronbach’s alpha coefficients of the GABS-15 scale. The criteria for conducting an EFA were met, as indicated by a Kaiser-Meyer-Olkin index of 0.94. Additionally, a significant Bartlett test (χ2(105) = 3440.54, p < 0.001) supported the assumption of sphericity. Applying the Kaiser-Guttmann criterion (eigenvalue > 1), three factors were extracted, collectively explaining 92.2% of the total variance. We labelled the first dimension “gambling fallacies” (explaining 40.0% of the variance after rotation), the second dimension “attitudes while gambling” (explaining 30.1% of the variance after rotation), and the third dimension “sensation seeking/excitement” (explaining 22.1% of the variance after rotation). Table 2 provides the factor loadings for all 15 items.
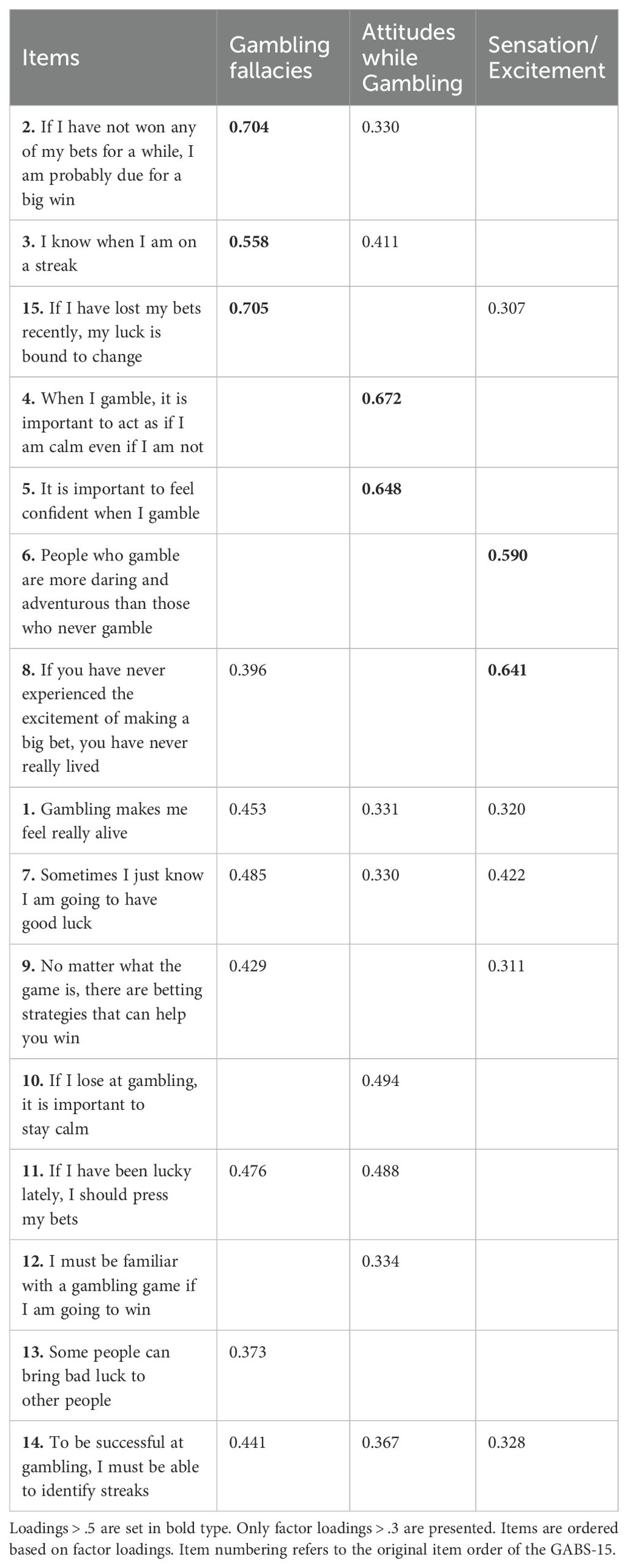
Table 2. Loadings of GABS-15 items on the three dimensions from the varimax-rotated factor analysis.
Three items loaded on the first dimension (all loadings > 0.5), two items on the second dimension (all loadings > 0.6), and two items on the third dimension (all loadings > 0.5).
Within the CFA, our three-factor model (χ2(11) = 43.53, p < 0.001, CFI = 0.98, TLI = 0.96, RMSEA = 0.08, SRMR = 0.03) demonstrated superior fit compared to both the conventional GABS-15 sum score (χ2(90) = 455.88, p < 0.001, CFI = 0.89, TLI = 0.87, RMSEA = 0.10, SRMR = 0.05) and the three-factor model proposed by Gehlenborg and colleagues (χ2(74) = 280.01, p < 0.001, CFI = 0.93, TLI = 0.92, RMSEA = 0.08, SRMR = 0.04).
Comparison of the longitudinal associations of GABS-15 and GD
As depicted in Table 3, we found a significant association between the GABS-15 sum score (model 1) and severity of GD (0.14, p < 0.01). For Gehlenborg’s three-factor structure (model 2), we observed a significant association only for the ‘luck/gambler’s fallacy’ factor (1.94, p < 0.01). Also, in our empirically derived three-factor model (model 3), only the ‘gambling fallacies’ factor (1.00, p < 0.05) presented a statistically significant association.
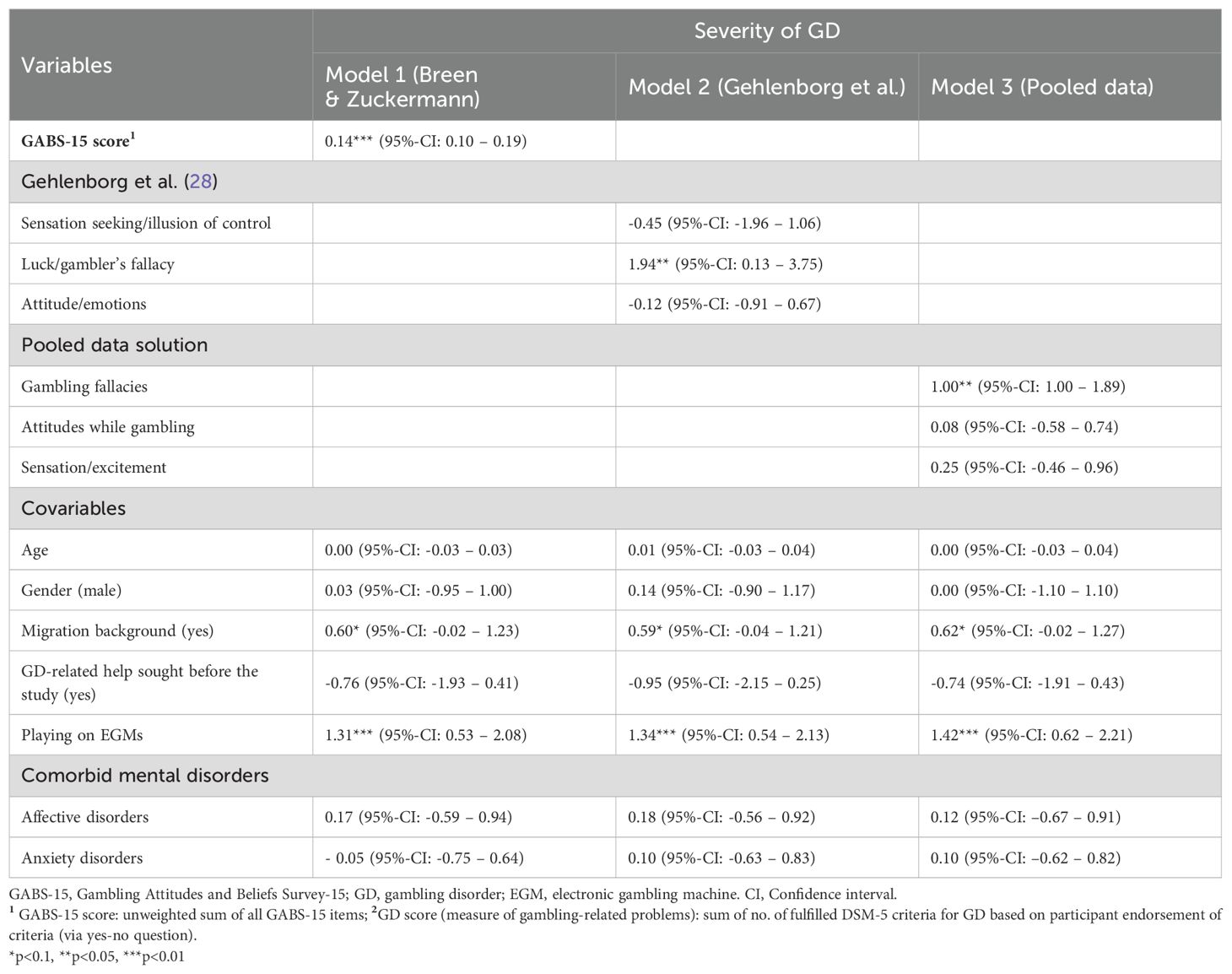
Table 3. Comparison of mixed-effects regression estimates for associations between GABS-15 score, factor scores based on Gehlenborg et al. (28) and factor scores based on pooled data with covariables on GD-score.
Sensitivity analysis
The sensitivity analysis included 114 participants who provided information on gambling frequency and intensity. Generally, the GABS-15 sum score (model 1) and the factors derived from model 2 and model 3 were more pronouncedly associated with weekly gambling hours than with severity of GD (Supplementary Table 3). We observed notable increases in effect sizes regarding GABS-15 sum score (model 1; 0.76, p < 0.01), the ‘luck/gambler’s fallacy’ factor (2; 24.75, p < 0.01) in model 2, and the ‘gambling fallacies’ factor (15.36, p < 0.01) in model 3. Additionally, both the sensation seeking/illusion of control factor (-11.54, p < 0.10) and the attitude/emotions factor (-6.72, p < 0.10) of model 2 displayed negative associations with weekly gambling hours.
Discussion
Using longitudinal data collected over a 3-year timeframe, the primary objective of this paper was to analyze the dimensional framework of the GABS-15 within an outpatient cohort of individuals with GD. Additionally, we sought to investigate to which extent personal attitudes and beliefs contribute to individual differences course GD over time. Contravening the previously stated one-dimensional structure of GABS-15, our analysis suggests a three-dimensional structure comprising “gambling fallacies”, “attitudes while gambling”, and “sensation-seeking/excitement”. Focusing on presumed associations of gambling-related attitudes and beliefs with the severity of GD, our empirically derived three-factor structure outperformed the (one-factorial) GABS-15 sum score, with “gambling fallacies” being the most indicative factor.
Considering that the GABS and the GABS-15 are less frequently used in gambling research than other measurement tools and that they had been mainly applied in samples largely consisting of undergraduates (41), evidence on “archetypic” sum scores across diverse populations is sparse. The baseline GABS-15 sum score of our sample closely mirrors the sum scores observed among individuals engaging in self-guided interventions or metacognitive training for gambling problems (e. g., 42, 43). Hence, our sample apparently resembles other populations of help-seeking individuals with gambling-related problems in an outpatient setting.
Like us, a previous study examining the dimensional structure of the GABS-15 revealed three distinct factors, namely “sensation seeking/illusion of control”, “luck/gambler’s fallacy”, and “attitude/emotions” (28). These factors apparently capture similar aspects as those derived from our sample, albeit with slightly different factor compositions. Despite differences in the factor composition both three-factorial concepts (Gehlenborg structure, our empirically derived structure) presented slightly better fit indices than the (one-factorial) GABS-15 sum score. This supports the rising body of evidence questioning the initially claimed one-dimensional structure of the GABS and the GABS 15 (15, 23, 28).
Out of the three identified factors only the factor “gambling fallacies” demonstrated a significant association with the severity of GD. This was also the case when the factors of the Gehlenborg model were included in the regression analysis. Consistent with these results, a meta-analytical investigation of the connection between problem gambling and various cognitive bias assessment instruments revealed that subscales explicitly addressing ‘gambler’s fallacy’ consistently exhibited stronger and more robust associations with problem gambling than other biases (41). One potential rationale for this observation could be that the predominant use of EGMs was popular in our sample. EGMs have been demonstrated to foster the development of gambling fallacies and excitement (44, 45), as they present past gambling events in an immediate and sequential manner. This format supports elements (i.e., sequential observation and recency effects) that contribute to the emergence of gambling fallacies (46). Hence, the role of the ‘gambling fallacies’ factor might be less prominent in samples of non-EGM players.
The large share of EGM players might also explain that only items unrelated to gambling strategies or illusions of control exerted a significant impact on the factors linked to cognitive distortions or excitement within our sample. Evidence suggests that among EGM players, illusions of control are less influential compared to superstitious beliefs and the elicitation of positive emotions (16). Building on Trivedi & Reichert’s (47) study of online gamblers, which identified a negative correlation between the use of gambling strategies and the severity of gambling problems, our negative findings may reflect a similar pattern in our predominantly EGM player sample. It is likely that these players are primarily focused on smaller, immediate rewards, and that more individual gambling strategies may be perceived negatively when subjected to personal reflection. Moreover, strategic aspects in gambling seem to have a lesser role, particularly when compared to skill-based forms of gambling such as poker or sports-betting (28, 48).
Within our analyses, the associations with gambling fallacies became even more accentuated when gambling behavior instead of the severity of GD was looked at. Contrary to our expectations our sensitivity analysis also revealed mitigating associations for the factors “sensation seeking/illusion of control” and “attitude/emotions” of the Gehlenborg structure. Although we do not have a definitive explanation for this counterintuitive result, it is possible that delay discounting—referring to the tendency to devalue future, larger rewards in favor of smaller, immediate ones—played a role in the observed gambling behavior (47).
Limitations and strengths
When interpreting the results of our study the following caveats must be kept in mind: First, even though we exceeded the suggested minimum sample size of n >=50 for modelling psychometric properties of socio-psychological constructs (49), the small sample size employed for the EFA stage of our analysis may have favored an inaccurate factor structure and factor solution. Through pooling individual-level data from distinct assessment points, we increased the number of observations which supposedly mitigated issues of a small sample size. However, further validation of the factors derived based on larger and more diverse samples is needed to enhance generalizability and reliability of the findings. Second, the comparative fit indices of the three models contrasted within our CFA must be interpreted with caution. As we identified and validated our factors within the same data set it is not surprising that our model structure outperformed Gehlenborg’s structure and the GABS-15 sum score. Nevertheless, it is quite common to perform CFA and EFA within the same sample (28, 50, 51). Furthermore, our prior interest was to investigate associations of factors with indicators for problem gambling (severity of GD, weekly gambling hours) and not to best possibly explain pre-existing gambling-related attitudes and beliefs within the observed sample. Hence, we consider the chosen approach – which is not unimpeachable from a methodological point of view – justified. Third, the observational one-armed design of our study does not allow drawing strictly causal relationships. Indeed, a bidirectional relationship between gambling fallacies and GD was suggested: Thus, gambling fallacies can exacerbate problematic gambling behavior, but conversely, they can also develop and strengthen as sequelae of intensified gambling (8, 52).
The strength of our study on the other hand lies in our comprehensive approach that not only explored the connections of gambling-related attitudes and beliefs with problem severity but also delved into actual gambling behavior. This was achieved by employing multilevel mixed models on two outcomes, enabling an assessment based on an intersubjective perspective. Moreover, the naturalistic approach in our study facilitated a degree of generalizability among individuals seeking outpatient care for GD. This contrasts with other studies that exclusively focused on isolated clinical samples and supports external validity by encompassing a diverse group of individuals. Finally, by contrasting our factor model with two alternative models, we indirectly performed a kind of cross-validation of previous work, improving our knowledge of the factor structure of the GABS-15.
Conclusions and further research
While the creators of the GABS emphasize its one-dimensional nature, intended to measure a general affinity for gambling, our findings – in alliance with previous studies – suggest that the GABS reveals greater potential when approached from a multidimensional perspective. This enables researchers, counsellors, and therapists to focus on distinct cognitive distortions that are strongly correlated with severity and course of GD which in turn might support effective treatment. In this regard, adequate addressing of gambling fallacies appears to be of high therapeutic relevance.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by German Association for Psychology (DGPs). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AB: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. JL: Conceptualization, Data curation, Project administration, Writing – review & editing. LK: Conceptualization, Funding acquisition, Project administration, Supervision, Validation, Writing – review & editing. BG: Conceptualization, Data curation, Project administration, Writing – review & editing. EH: Funding acquisition, Project administration, Supervision, Writing – review & editing. LS: Conceptualization, Formal analysis, Methodology, Project administration, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was conducted in the context of the Bavarian Coordination Centre for Gambling Issues (Bayerische Landesstelle Gluecksspielsucht (LSG)). The LSG is funded by the Bavarian State Ministry of Public Health and Care Services. The State of Bavaria provides gambling services (lotteries, sports betting and casino games) within the State gambling monopoly via the State Lottery Administration and provided funding for the Bavarian Coordination Centre for Gambling Issues as an unrestricted grant. Support for LK came from the Swedish program grant ‘Responding to and Reducing Gambling Problems -Studies in Help-seeking, Measurement, Comorbidity and Policy Impacts’ financed by the Swedish Research Council for Health, Working Life and Welfare (Forte), grant number 2016-07091.
Acknowledgments
The authors thank the participating outpatient care facilities of the Bavarian Competence Network of Gambling Issues for smooth cooperation in the context of conducting the study. We especially acknowledge the study participants’ willingness to take part in the ‘Katamnese-Studie’ from enrolment to end of follow-up. We furthermore express our heartfelt thanks to our colleagues Joana Daniel, Pia Wullinger, Nina Stefan, Carla Faßbender and Marieke Neyer, who provided advice and support in conducting the study or drafting this paper.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer KS declared a shared affiliation with the author LK to the handling editor at the time of review.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1481733/full#supplementary-material.
References
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5. Washington, DC: American Psychiatric Publishing (2013). doi: 10.1176/appi.books.9780890425596
2. Abbott MW. The changing epidemiology of gambling disorder and gambling-related harm public health implications. Public Health. (2020) 184:41–5. doi: 10.1016/j.puhe.2020.04.003
3. Sulkunen P, Babor TF, Cisneros Örnberg J, Egerer M, Hellman M, Livingstone C, et al. Setting limits: gambling, science and public policy—summary of results. Addiction. (2021) 116:32–40. doi: 10.1111/add.15241
4. Toneatto T. Cognitive psychopathology of problem gambling. Subst Use Misuse. (1999) 34:1593–604. doi: 10.3109/10826089909039417
5. Breen RB, Zuckerman M. Chasing” in gambling behavior: Personality and cognitive determinants. Pers Individ Dif. (1999) 27:1097–111. doi: 10.1016/S0191-8869(99)00052-5
6. Hammelstein P. Faites vos jeux! Another look at sensation seeking and pathological gambling. Pers Individ Dif. (2004) 37:917–31. doi: 10.1016/j.paid.2003.10.014
7. Müller KW, Dreier M, Beutel ME, Wölfling K. Is Sensation Seeking a correlate of excessive behaviors and behavioral addictions? A detailed examination of patients with Gambling Disorder and Internet. Addiction. Psychiatry Res. (2016) 242:319–25. doi: 10.1016/j.psychres.2016.06.004
8. Leonard CA, Williams RJ. The relationship between gambling fallacies and problem gambling. Psychol Addictive Behav. (2016) 30:694. doi: 10.1037/adb0000189
9. Ciccarelli M, Griffiths MD, Nigro G, Cosenza M. Decision making, cognitive distortions and emotional distress: A comparison between pathological gamblers and healthy controls. J Behav Ther Exp Psychiatry. (2017) 54:204–10. doi: 10.1016/j.jbtep.2016.08.012
10. Fortune EE, Goodie AS. Cognitive distortions as a component and treatment focus of pathological gambling: A review. Psychol Addictive Behav. (2012) 26:298–310. doi: 10.1037/a0026422
11. Sundali J, Croson R. Biases in casino betting: the hot hand and the gambler’s fallacy. Judgment Decision Making. (2006) 1:1–12. doi: 10.1017/S1930297500000309
12. Leonard CA, Williams RJ, Vokey J. Gambling fallacies: what are they and how are they best measured? J Res Ther Addict. (2015) 6(4):256. doi: 10.4172/2155-6015.1000256
13. Delfabbro P. The stubborn logic of regular gamblers: obstacles and dilemmas in cognitive gambling research. J Gambling Stud. (2004) 20:1–21. doi: 10.1023/b:jogs.0000016701.17146.d0
14. Toneatto T, Blitz-Miller T, Calderwood K, Dragonetti R, Tsanos A. Cognitive distortions in heavy gambling. J gambling Stud. (1997) 13:253–66. doi: 10.1023/a:1024983300428
15. Bouju G, Hardouin JB, Boutin C, Gorwood P, Le Bourvellec JD, Feuillet F, et al. A shorter and multidimensional version of the Gambling Attitudes and Beliefs Survey (GABS-23). J Gambling Stud. (2014) 30:349–67. doi: 10.1007/s10899-012-9356-3
16. Joukhador J, Blaszczynski A, Maccallum F. Superstitious beliefs in gambling among problem and non-problem gamblers: preliminary data. J Gambling Stud. (2004) 20:171–80. doi: 10.1023/b:jogs.0000022308.27774.2b
17. Ladouceur R. Perceptions among pathological and nonpathological gamblers. Addictive Behav. (2004) 29:555–65. doi: 10.1016/j.addbeh.2003.08.025
18. Moore SM, Ohtsuka K. Beliefs about control over gambling among young people, and their relation to problem gambling. Psychol Addictive Behav. (1999) 13:339. doi: 10.1037/0893-164X.13.4.339
19. Källmén H, Andersson P, Andren A. Are irrational beliefs and depressive mood more common among problem gamblers than non-gamblers? A survey study of Swedish problem gamblers and controls. J Gambling Stud. (2008) 24:441–50. doi: 10.1007/s10899-008-9101-0
20. Chiu J, Storm L. Personality, perceived luck and gambling attitudes as predictors of gambling involvement. J Gambling Stud. (2010) 26:205–27. doi: 10.1007/s10899-009-9160-x
21. Derevensky J, Sklar A, Gupta R, Messerlian C. An empirical study examining the impact of gambling advertisements on adolescent gambling attitudes and behaviors. Int J Ment Health Addict. (2010) 8:21–34. doi: 10.1007/s11469-009-9211-7
22. Strong DR, Breen RB, Lejuez CW. Using item response theory to examine gambling attitudes and beliefs. Pers Individ Dif. (2004) 36:1515–29. doi: 10.1016/j.paid.2003.06.001
23. Strong DR, Daughters SB, Lejuez CW, Breen RB. Using the Rasch model to develop a revised Gambling Attitudes and Beliefs Scale (GABS) for use with male college student gamblers. Subst Use Misuse. (2004) 39:1013–24. doi: 10.1081/JA-120030897
24. Breen RB, Kruedelbach N, Walker H. Cognitive changes in pathological gamblers following a 28-day inpatient program. Psychol Addictive Behav. (2001) 3:246–8. doi: 10.1037/0893-164X.15.3.246
25. Oei TPS, Gordon LM. Psychological factors related to gambling abstinence and relapse in members of gamblers anonymous. J Gambling Stud. (2008) 24:91–105. doi: 10.1007/s10899-007-9071-7
26. Smith DP, Battersby MW, Pols RG, Harvey PW, Oakes JE, Baigent MF. Predictors of relapse in problem gambling: A prospective cohort study. J Gambling Stud. (2015) 31:299–313. doi: 10.1007/s10899-013-9408-3
27. Rossini-Dib D, Fuentes D, Tavares H. A naturalistic study of recovering gamblers: What gets better and when they get better. Psychiatry Res. (2015) 227:17–26. doi: 10.1016/j.psychres.2015.03.003
28. Gehlenborg J, Moritz S, Bücker L. The dimensional structure of the gambling attitudes and beliefs survey: challenging the assumption of the unidimensionality of gambling-specific cognitive distortions. J Gambling Stud. (2023) 39:75–86. doi: 10.1007/s10899-022-10133-7
29. Schwarzkopf L, Loy JK, Braun-Michl B, Grüne B, Sleczka P, Kraus L. Gambling disorder in the context of outpatient counselling and treatment: Background and design of a prospective German cohort study. Int J Methods Psychiatr Res. (2021) 30:e1867. doi: 10.1002/mpr.1867
30. Bickl AM, Schwarzkopf L, Loy JK, Grüne B, Braun-Michl B, Sleczka P, et al. Changes in gambling behaviour and related problems in clients seeking help in outpatient addiction care: Results from a 36-month follow-up study in Bavaria. J Behav Addict. (2021) 10:690–700. doi: 10.1556/2006.2021.00043
31. Wullinger PM, Bickl AM, Loy JK, Kraus L, Schwarzkopf L. Longitudinal associations between psychiatric comorbidity and the severity of gambling disorder: Results from a 36-month follow-up study of clients in Bavarian outpatient addiction care. J Behav Addict. (2023) 12:535–46. doi: 10.1556/2006.2023.00026
32. Stinchfield R. Reliability, validity, and classification accuracy of a measure of DSM-IV diagnostic criteria for pathological gambling. Am J Psychiatry. (2003) 160:180–2. doi: 10.1176/appi.ajp.160.1.180
33. Banz M, Lang P. Glückspielverhalten und Glückspielsucht in Deutschland. Ergebnisse des Surveys 2017 und Trends. BZgAForschungsbericht, [Gambling behavior and gambling addiction in Germany. Results of the Survey 2017 and Trends. BZgA Research Report. (2017). doi: 10.17623/BZGA:225-GS-SY17-1.0
34. Wittchen H-U, Pfister H. DIA-X-Interviews: Manual für Screening-Verfahren und Interview; Interviewheft. In: Manual for screening procedure and interview; Interview booklet. Swets & Zeitlinger, Frankfurt, Germany (1997).
35. World Health Organization. ICD-10: International statistical classification of diseases and related health problems. Geneva: World Health Organization (2004).
36. Binde P. What are the most harmful forms of gambling? Analyzing problem gambling prevalence surveys. Rapport nr.: CEFOS Working Papers. (2011) 12.
37. Braun B, Ludwig M, Kraus L, Kroher M, Bühringer G. Ambulante Suchthilfe für pathologische Glücksspieler in Bayern: Passung zwischen Behandlungsbedarf und -angebot. Suchttherapie. (2013) 14:37–45. doi: 10.1055/s-0032-1323802
38. Schulte L, Orlowski S, Brandt D, Bischof A, Besser B, Bischof G, et al. The role of migration background and cognitive distortions in the trajectories of gambling problems-a longitudinal study. Int Gambling Stud. (2021) 21:17–37. doi: 10.1080/14459795.2020.1791220
39. Statistisches Bundesamt. Demographische Standards Ausgabe 2010: Eine gemeinsame Empfehlung des ADM Arbeitskreis Deutscher Markt- und Sozialforschungsinstitute e.V., der Arbeitsgemeinschaft Sozialwissenschaftlicher Institute e.V. In: (ASI) und des Statistischen Bundesamtes, 2010, vol. 17. Statistik und Wissenschaft, Wiesbaden: Statistisches Bundesamt (2010).
40. Thai HT, Mentré F, Holford NH, Veyrat-Follet C, Comets E. A comparison of bootstrap approaches for estimating uncertainty of parameters in linear mixed-effects models. Pharm Stat. (2013) 12:129–40. doi: 10.1002/pst.1561
41. Goodie AS, Fortune EE. Measuring cognitive distortions in pathological gambling: Review and meta-analyses. Psychol Addictive Behav. (2013) 27(3):730–43. doi: 10.1037/a0031892
42. Bücker L, Gehlenborg J, Moritz S, Westermann S. A randomized controlled trial on a self-guided Internet-based intervention for gambling problems. Sci Rep. (2021) 11:13033. doi: 10.1038/s41598-021-92242-8
43. Gehlenborg J, Bücker L, Berthold M, Miegel F, Moritz S, et al. Feasibility, acceptance, and safety of metacognitive training for problem and pathological gamblers (Gambling-MCT): A pilot study. J Gambl Stud. (2021) 37(2):663–87. doi: 10.1007/s10899-020-09975-w
44. Rockloff MJ, Hing N. The impact of jackpots on EGM gambling behavior: A review. J Gambling Stud. (2013) 29:775–90. doi: 10.1007/s10899-012-9336-7
45. Schüll ND. Addiction by design. In: Addiction by design. United States: Princeton University Press (2012).
46. Barron G, Leider S. The role of experience in the Gambler's Fallacy. J Behav Decision Making. (2010) 23:117–29. doi: 10.1002/bdm.676
47. Trivedi RH, Teichert T. Attitudes, beliefs and impulsivity in online gambling addiction. Int Gambling Stud. (2018) 18:327 342. doi: 10.1080/14459795.2018.1466188
48. Moritz S, Gehlenborg J, Bierbrodt J, Wittekind CE, Bücker L. A ghost in the machine? The predictive role of metacognitive beliefs, cognitive biases, and machine-related features in the severity of problematic slot machine gambling. Pers Individ Dif. (2021) 171:110539. doi: 10.1016/j.paid.2020.110539
49. de Winter JC, Dodou D, Wieringa PA. Exploratory factor analysis with small sample sizes. Multivariate Behav Res. (2009) 44:147–81. doi: 10.1080/00273170902794206
50. Kim H, Ku B, Kim JY, Park YJ, Park YB. Confirmatory and exploratory factor analysis for validating the phlegm pattern questionnaire for healthy subjects. Evidence-Based Complementary Altern Med. (2016) 2016(1):2696019. doi: 10.1155/2016/2696019
51. Van Prooijen JW, Van Der Kloot WA. Confirmatory analysis of exploratively obtained factor structures. Educ psychol Measurement. (2001) 61:777–92. doi: 10.1177/00131640121971518
Keywords: addictive behavior, addiction, gambling, pathological gambling, gambling related beliefs and attitudes, longitudinal
Citation: Bickl AM, Loy JK, Kraus L, Grüne B, Hoch E and Schwarzkopf L (2024) Gambling-related attitudes and dimensional structure of the GABS-15 in outpatient addiction care patients: associations with gambling disorder. Front. Psychiatry 15:1481733. doi: 10.3389/fpsyt.2024.1481733
Received: 16 August 2024; Accepted: 24 September 2024;
Published: 21 October 2024.
Edited by:
Liana Fattore, CNR Neuroscience Institute (IN), ItalyReviewed by:
Doris Malischnig, Office of Addiction and Drug Policy of Vienna, AustriaKristina Sundqvist, Department of Psychology, Stockholm University, Sweden
Copyright © 2024 Bickl, Loy, Kraus, Grüne, Hoch and Schwarzkopf. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andreas M. Bickl, Ymlja2xAaWZ0LmRl
 Andreas M. Bickl
Andreas M. Bickl Johanna K. Loy
Johanna K. Loy Ludwig Kraus3,4,5
Ludwig Kraus3,4,5 Larissa Schwarzkopf
Larissa Schwarzkopf