- 1Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong, Hong Kong SAR, China
- 2Department of Psychological Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
Introduction: This meta-analysis aimed to quantitatively evaluate the association between homosexual and bisexual orientation and borderline personality disorder (BPD), including factors contributing to the association and clinical outcomes of homosexual and bisexual patients with BPD.
Methods: We systematically searched PUBMED, PsycINFO, Cochrane Library, MEDLINE, EMBASE and Web of Science for cross-sectional or cohort studies comparing the prevalence of homosexual and bisexual orientation amongst patients with BPD and controls.
Results: Our search identified 7 eligible studies, with a total sample case of 636 subjects with BPD and 535 subjects without BPD. Patients with BPD had a significantly higher likelihood of homosexual and bisexual orientation (Risk ratio [RR] 3.39, 95%CI 1.88-6.12) with a pooled prevalence of 28% (95% CI 0.24-0.31; I2 73%; 7 studies, 1171 participants). Subgroup analyses validated that BPD was independently associated with higher prevalence of both homosexual (RR 8.51, 95% CI 3.36-21.54) and bisexual orientation (RR 3.82, 95% CI 1.81-8.04), but no gender difference was yielded. Childhood sexual abuse (CSA) was associated with the development of homosexual and bisexual orientation in patients with BPD.
Discussion: Poorer clinical outcomes, including physical and mental health, were associated with BPD status. Further studies are necessary to evaluate the feasibility and efficacy of sexual minority-specific treatment for these patients.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=538356, identifier CRD42024538356.
Introduction
Borderline personality disorder (BPD) is characterised by pervasive emotional instability, impulsivity and difficult interpersonal relationships. These features predispose to repeated self-injury or suicidal attempts, requiring more frequent hospital admissions than other major psychiatric disorders (1). The prevalence of BPD in the community setting was estimated to be 1% according to previous studies (2). In psychiatric inpatient and outpatient clinics, the prevalence was 22% and 12% respectively (2). Patients with BPD not only more readily suffer from comorbid psychiatric disorders, including affective disorders, sleep disorders and substance use disorder, but physical comorbidities are also more common amongst patients with BPD (3). The aetiology of BPD is multifactorial, with childhood adversity, especially emotional abuse or neglect, being a significant risk factor (4).
Identity disturbance is one of the diagnostic criteria of BPD and refers to a markedly and persistently unstable self-image. Identity disturbance in BPD is likely a multifaceted psychological construct rather than a single entity. Wilkinson-Ryan et al. elicited four major identity disturbance factors: role absorption, painful incoherence, objective incoherence and lack of commitment (5). Painful incoherence, defined as a subjective sense of incoherence, was the most critical factor distinguishing BPD from other personality disorders.
On the other hand, identity disturbance is also a salient feature in the psychosexual development of the homosexual and bisexual population. Cass’s model of homosexual identity development highlighted a 6-stage process beginning with identity confusion as an individual questions his/her sexual orientation (6). Another proposed model for lesbian identity development shared a resemblance with Cass’s model, describing a sense of incongruence that lesbians might experience as they navigate their sexual orientation through interactions with the community (7). Whilst the sequentiality of these multi-stage models limited their applicability in contemporary settings, they underscored the importance of identity formation in homosexual and bisexual individuals and the likelihood of identity disturbance amidst the process.
Identity disturbance may, therefore, be a shared experience between patients with BPD and the homosexual and bisexual population. This raises suspicion for an increased prevalence of homosexual and bisexual orientation amongst patients with BPD and vice versa. This notion was supported by a previous study revealing an association between sexual minority and BPD features in a community sample of adolescents (8). Another study examining the prevalence of BPD in sexual minorities yielded similar findings, and their results derived from a national database dismissed the possibility of provider bias leading to the observed disparity (9). Instead, their findings alluded to the possibility of transdiagnostic psychopathologies unique to sexual minorities.
Homosexual and bisexual patients with BPD describe a subgroup of patients with specific therapeutic challenges. Firstly, homosexual and bisexual patients with BPD may encounter more discrimination and relationship difficulties than their heterosexual counterparts. This, combined with heightened identity disturbance intrinsic to this population, might exacerbate manifestations of BPD traits, such as increased suicidal attempts or impulsive behaviours (9). In addition, both BPD and homosexual and bisexual orientation are independently associated with more frequent risky sexual behaviours (10). Therefore, it is clinically relevant to understand the prevalence of homosexual and bisexual orientation amongst patients with BPD to provide adequate support for this subgroup. This review aims to bridge the gap in the current literature and examine the prevalence of homosexual and bisexual orientation amongst patients with BPD compared to subjects without BPD. In addition, associated factors predisposing to the development of homosexual and bisexual orientation and subsequent clinical implications, including psychiatric comorbidities, sexual and overall health status, would be evaluated.
The primary objective of this review was to assess the prevalence of homosexual and bisexual orientation amongst patients with BPD compared with subjects without BPD. Secondary objectives included evaluation of gender differences in the prevalence of homosexual and bisexual patients with BPD, factors contributing to homosexual and bisexual orientation amongst patients with BPD and the differences in clinical outcomes between heterosexual and homosexual and bisexual patients with BPD.
Methods
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and was registered with PROSPERO, CRD42024538356 (11). Institutional review board review and approval was not required for this study.
Eligibility criteria
We included any published cross-sectional or longitudinal studies investigating the prevalence of homosexual and bisexual orientation amongst BPD. Sexual orientation was defined as any self-reported or measured patterns of romantic or sexual attraction, including any relevant sexual experience. Subjects with gender dysphoria or paraphilia were not included in this review. For study outcomes, studies were only included if any validated battery was utilised to diagnose BPD. This included the Revised Diagnostic Interview for Borderlines (12), the Diagnostic and Statistical Manual of Mental Disorders Studies or other validated batteries of choice (13). Studies must meet all of the above criteria to be considered. For the study population, studies recruiting patients with BPD with comorbid psychiatric diagnoses were not excluded, given the inherently high prevalence of concomitant psychiatric conditions in this patient population (14).
Studies meeting any one of the below criteria were excluded: (i) case controls, case studies or case reports, (ii) paediatric populations, (iii) study population not fulfilling diagnostic criteria of BPD or only demonstrating certain personality traits, and (iv) inclusion of transgender population.
Information sources and search strategy
We identified eligible cross-sectional or cohort studies by searching PUBMED, PsycINFO, Cochrane Library, MEDLINE, EMBASE and Web of Science from inception to 8th April 2024 (Supplementary Table S1). No publication language limitations were implemented. We used the following text words “borderline/impulsive pattern/personality/disorder/trait”, “BPD”, “emotionally unstable personality disorder”, “EUPD”, “emotional intensity disorder”, “EID”, “sex/bisexual/homosexual/pansexual/polysexual/asexual/gender orientation/attraction/behaviours/preference/leaning/identity” and relevant MESH or subject headings.
Outcome definition
The primary outcome was the prevalence of homosexual and bisexual orientation amongst patients with BPD compared to subjects without BPD. We accepted the study authors’ definition of homosexual and bisexual orientations and/or sexual relationships with the same or both genders using validated and reliable measurement tools, such as the Barratt Impulsiveness Scale (BIS-11) (15), items within the Revised Diagnostic Interview for Borderlines (12), the ASHR Health and Relationships Questionnaire and the Abuse History Interview (AHI) (16, 17). Structured research questionnaires with questions exploring sexual orientation specifically designed for the studies were also accepted.
The secondary outcomes were the associated factors linked to homosexual and bisexual orientation in patients with BPD and the clinical implications, including psychiatric comorbidities, sexual and overall health status in homosexual and bisexual patients with BPD.
Study selection and data extraction
Two independent review authors screened titles, abstracts and full texts to identify eligible studies using Covidence software (Veritas Health Innovation Ltd, Australia). The decision-making process for including studies in this systematic review was documented and shown in a PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram (11).
Data from each included study were independently extracted using a standardised form by the two review authors using Covidence software. For each study, we extracted data on the title, authors, publication name, year of publication, language of publication, study design, setting, eligibility criteria, number of eligible participants, age and sex of the study participants, status of borderline personality disorder, sexual orientation, possible factors associated with homosexual and bisexual orientation and any reported clinical outcomes including sexual health and overall health status. Any disagreements were resolved by consultation with a third senior reviewer. Data were entered into Review Manager 5.4 (Copenhagen; The Nordic Cochrane Collaboration) by one author, and another author verified the data entry before meta-analyses.
Risk of bias and certainty in evidence
Two review authors independently assessed the risk of bias and methodological quality for all included studies, utilising the Joanna Briggs Institute (JBI) critical appraisal checklist (18). An 8-item and 11-item checklist were used for appraising cross-sectional and cohort studies, respectively. Any “yes” was given 1 score, whilst “no” or “unclear” was given 0 score. The total score would be converted into a percentage of the maximum attainable score, where 70% was considered good quality and 50% was acceptable (19). Any disagreements were resolved by consulting a third senior reviewer. Studies were included regardless of the appraisal score.
Statistical analysis and data synthesis
MetaXL was used for data analysis. Risk ratio (RR) and mean difference (MD) values with 95% confidence intervals (95% CI) were reported for dichotomous and continuous outcomes, respectively. The DerSimonian and Laird random-effects model was applied as clinical and methodological heterogeneity were anticipated among studies. The statistical heterogeneity was reported with the I2 statistic: an I2 of 25% was considered low heterogeneity, 50% moderate heterogeneity and 75% high heterogeneity. Double arcsine transformation was applied to raw data on prevalence. Pooled prevalence was derived using an inverse variance model.
Results
A systematic search identified 894 records after removing duplicates (Figure 1). Upon screening, 7 studies, including 6 cross-sectional studies and 1 longitudinal prospective cohort study (20–26), were included in this review. Four studies were conducted in the United States, with the remaining conducted in Australia, Canada, and Spain. A total of 1171 patients were involved in the included studies.
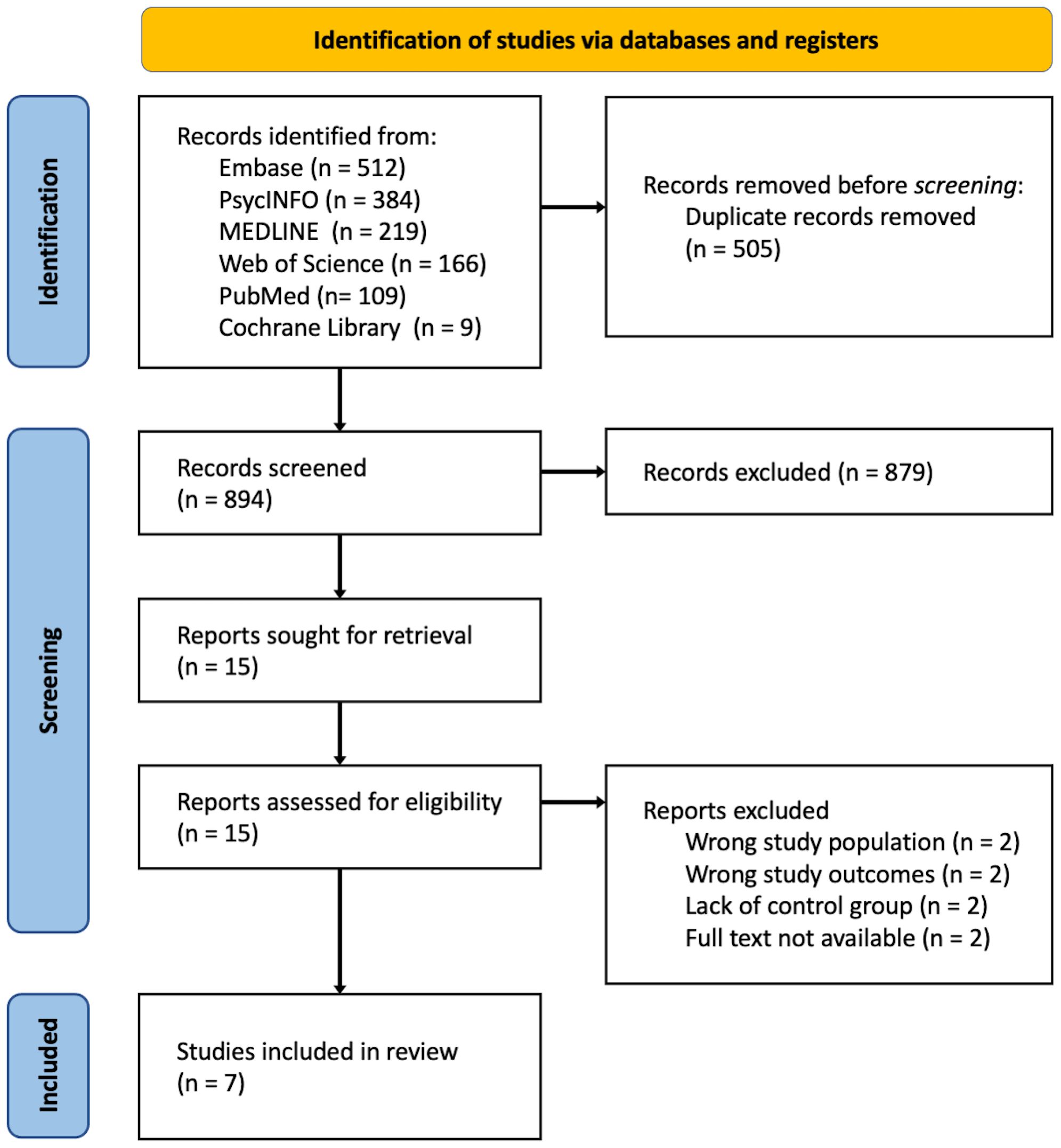
Figure 1. Preferred reporting items for systematic reviews and meta-analyses flow chart showing results of systematic literature search.
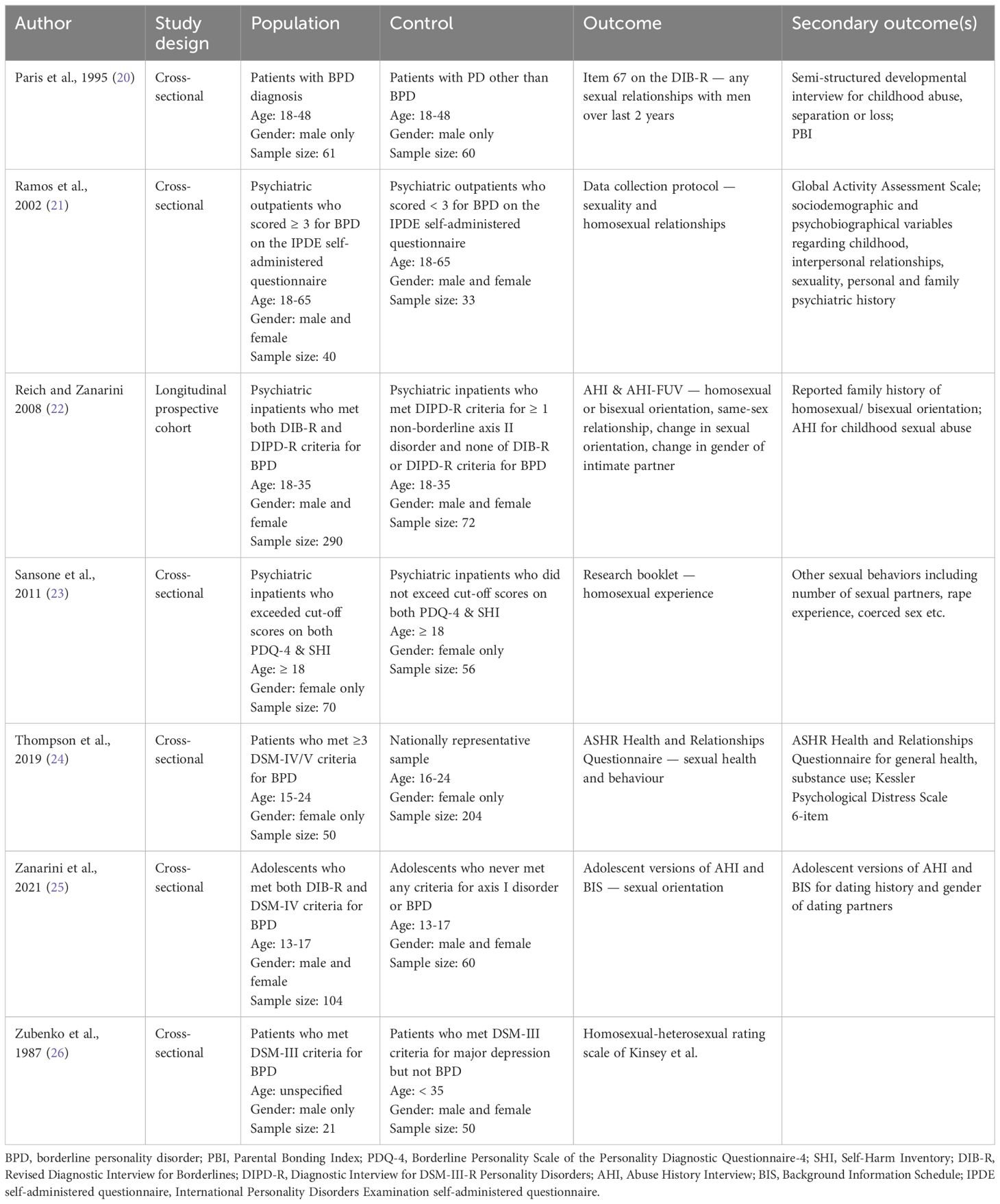
All the included studies recruited patients diagnosed with BPD by validated measures (Table 1). Most studies limited the scope to adults above 18 years old except for the studies by Thompson et al. and Zanarini et al. (24, 25). The study by Zubenko et al. did not specify any age limit for the BPD group, but the reported mean age was 24.3 ± 3.7 years (26). Three studies recruited subjects of both genders; two recruited males only, and two recruited females only. The study by Zubenko et al. limited BPD subjects to males but included both genders in the control group (26). For outcomes, five studies employed questions from validated questionnaires to assess sexual orientation, while two adopted questions from proprietary questionnaires. The studies by Paris et al. and Zubenko et al. only reported homosexuality (20, 26), whilst other studies reported both homosexuality and bisexuality.
Risk of bias
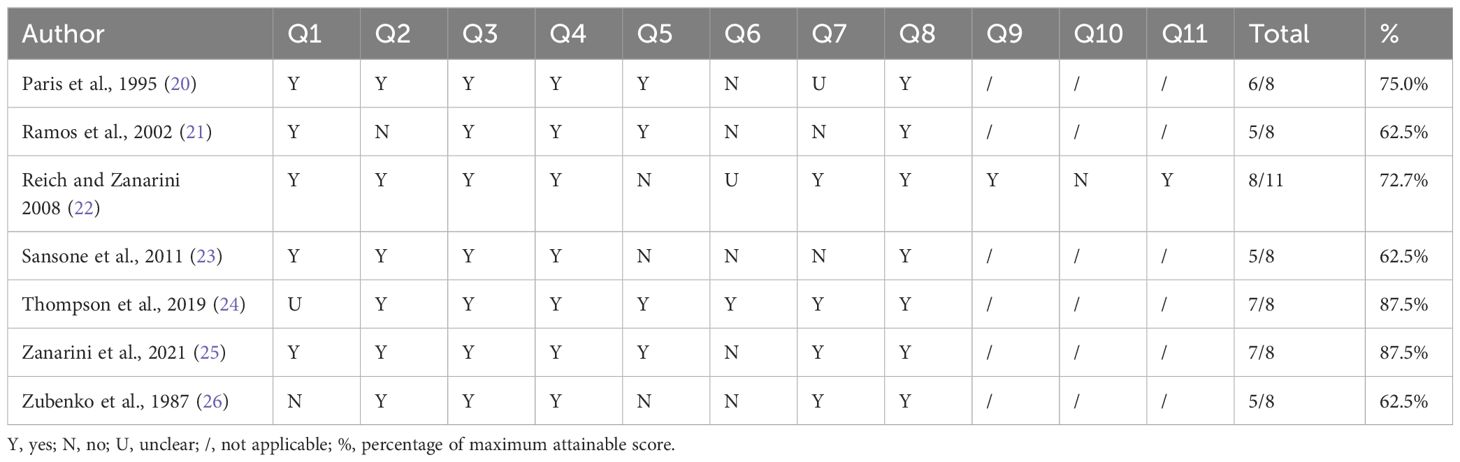
The risk of bias assessment using the Joanna Briggs Institute critical appraisal tools revealed that all studies had an acceptable level of bias (Table 2). 4 out of 7 studies were considered good quality with a percentage JBI score above 70%. Most studies identified confounding factors, including demographic factors such as age, race and sex, but some studies did not report such baseline characteristics. Regarding strategies to deal with the confounders, some studies utilised matching within the study design, but none performed multivariate regression analysis. An issue with outcome measurement was also noted. As the outcome of sexual orientation is intrinsically difficult to assess objectively, most studies relied on self-reported scales, most of which were validated questionnaires or semi-structured interview questions.
Homosexual and bisexual orientation in BPD
Six cross-sectional studies reported the prevalence and one prospective cohort study reported the incidence of homosexual and bisexual orientation amongst patients with BPD and control groups without BPD (Figure 2). All studies demonstrated a higher percentage of homosexual and bisexual orientation in patients with BPD when compared to control groups. The results were statistically significant except in the studies by Ramos et al. (p=0.2) and Sansone et al. (p=0.06) (21, 23). Overall, there was a significantly higher percentage of homosexual and bisexual patients amongst patients with BPD compared to subjects without BPD. (Risk ratio [RR] 3.39, 95% confidence interval [CI] 1.88-6.12; p<0.0001; I2 59%; 7 studies, 1171 participants).
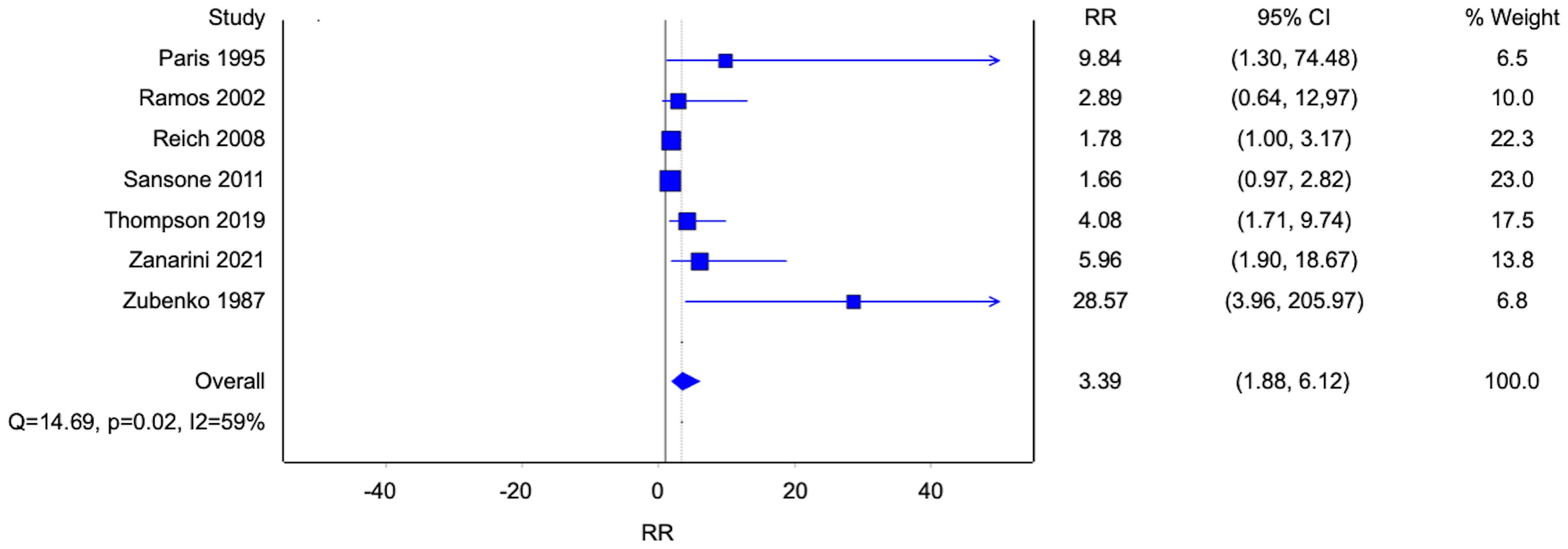
Figure 2. Forest plot of the risk ratio of homosexual and bisexual orientation in patients with borderline personality disorder.
Five studies reported data on homosexuality, and three studies reported data on bisexuality (Figures 3, 4). There were statistically significant associations between BPD and homosexuality (Risk ratio [RR] 8.51, 95% confidence interval [CI] 3.36-21.54; p<0.0001; I2 0%; 5 studies, 683 participants) and bisexuality (Risk ratio [RR] 3.82, 95% confidence interval [CI] 1.81-8.04; p=0.0004; I2 0%; 5 studies, 491 participants) respectively. In addition, patients with BPD were also more likely to have developed homosexual relationships (Figure 5) (Risk ratio [RR] 2.56, 95% confidence interval [CI] 1.36-4.82; p=0.004; I2 13%; 3 studies, 689 participants).
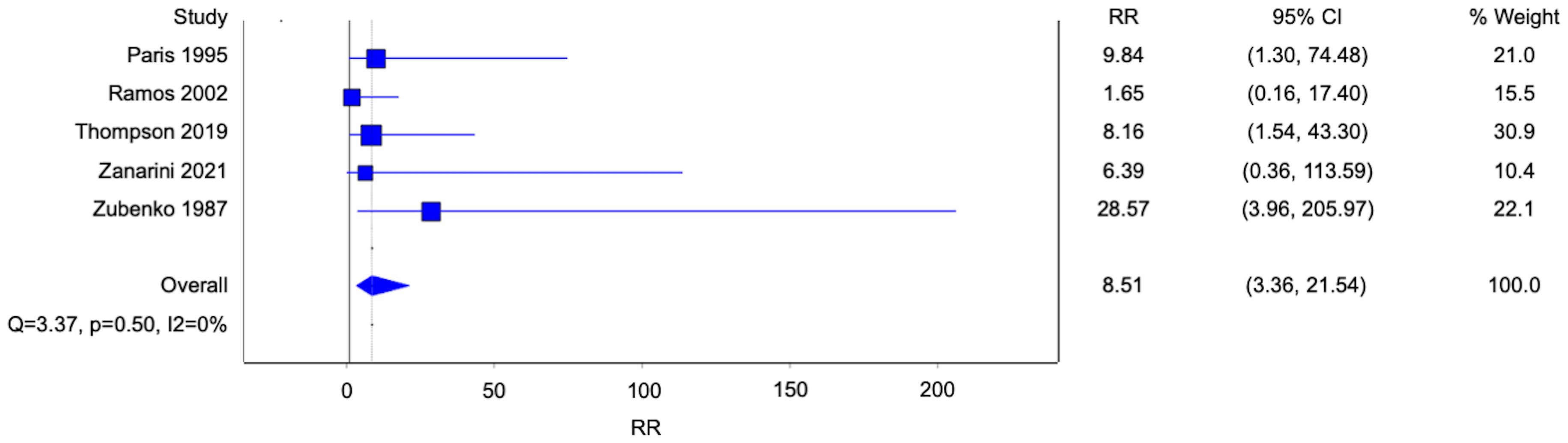
Figure 3. Forest plot of the risk ratio of homosexual orientation in patients with borderline personality disorder.
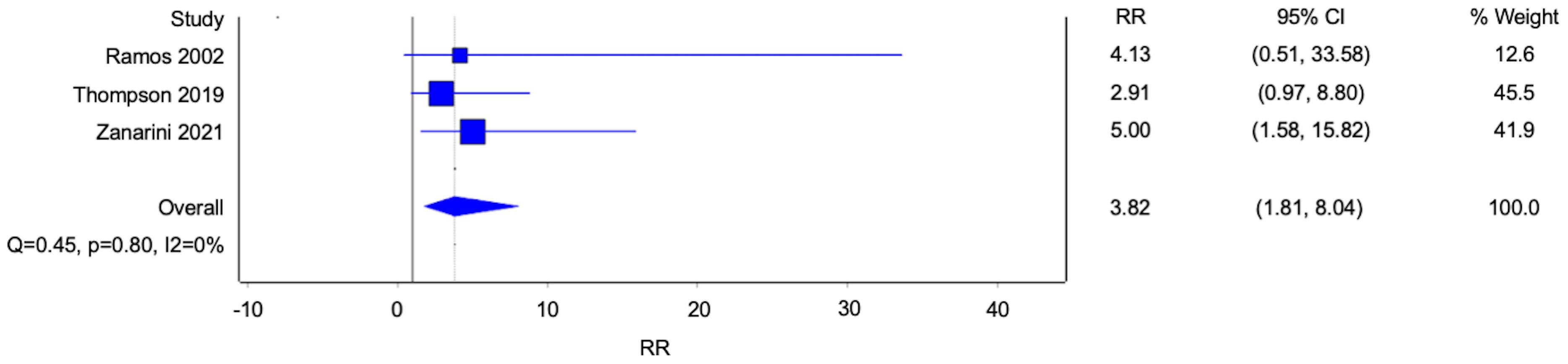
Figure 4. Forest plot of the risk ratio of bisexual orientation in patients with borderline personality disorder.
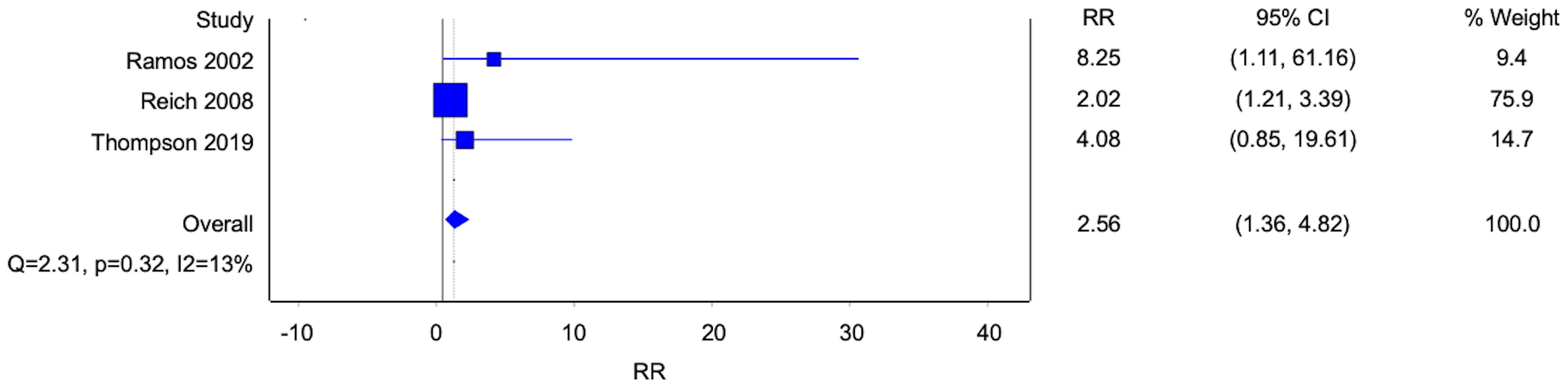
Figure 5. Forest plot of the risk ratio of homosexual relationships in patients with borderline personality disorder.
Prevalence of homosexual and bisexual orientation in BPD
The prevalence of homosexual and bisexual orientation amongst patients with BPD was derived from the data of each study. Reported prevalence ranged from 16-57% with moderate-high heterogeneity (Figure 6). The overall pooled prevalence was 28% (95% confidence interval [CI] 0.24-0.31; I2 73%; 7 studies, 1171 participants). The study by Reich et al. had the most subjects and contributed to nearly half of the pooled average under the inverse variance model.
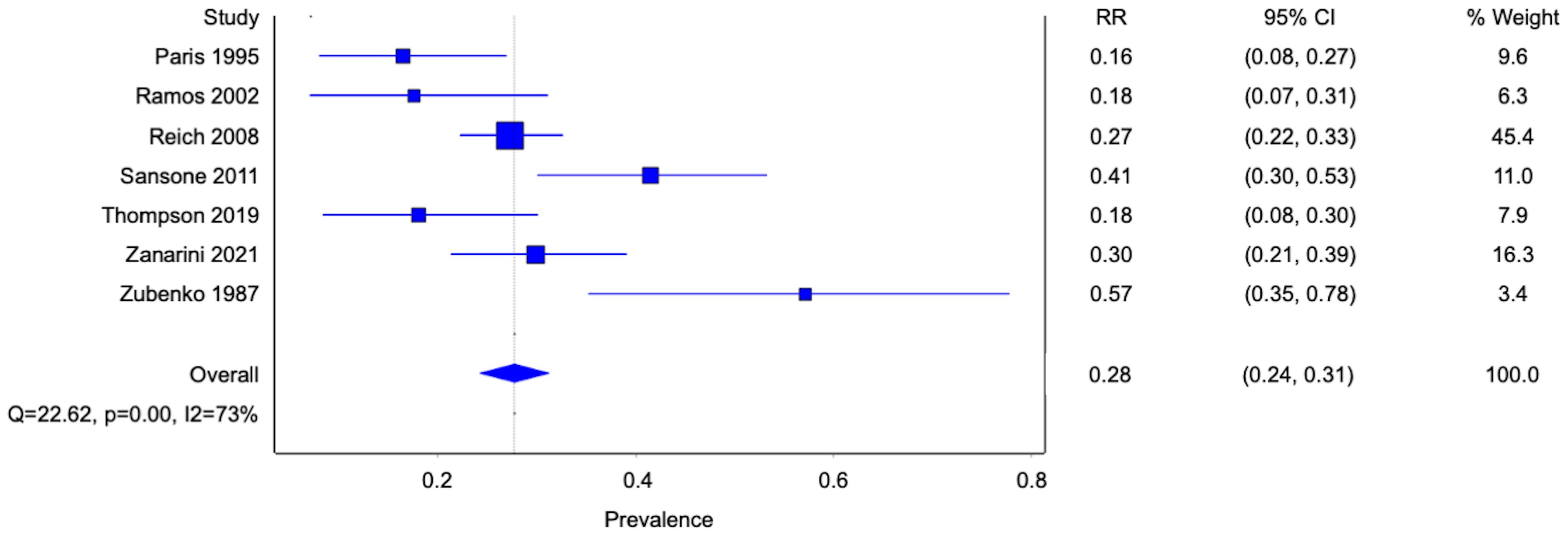
Figure 6. Forest plot of the pooled prevalence of homosexual and bisexual orientation in patients with borderline personality disorder.
Factor associated with homosexual and bisexual orientation: gender differences
Two studies reported the prevalence of homosexual and bisexual orientation for both genders with BPD and were used to examine for any gender differences. The two studies had contradicting results. The study by Zanarini et al. reported a much higher prevalence of homosexual and bisexual orientation in female patients with BPD than in male counterparts (25), though the statistical significance of this finding was not discussed in the original publication. The study by Reich et al. reported a slightly lower incidence amongst females (22). Overall, no statistically significant gender differences were seen. (Risk ratio [RR] 1.13, 95% confidence interval [CI] 0.37-3.45; p=0.83; I2 25%; 2 studies, 394 participants) The remaining studies included only one gender or did not report gender-specific prevalence and were thus not included in the pooled effect analysis.
Factor associated with homosexual and bisexual orientation: childhood sexual abuse
Two studies reported a history of childhood sexual abuse (CSA) as an associated factor of homosexual and bisexual orientation in patients with BPD (Figure 7). Both studies reported a higher likelihood of developing homosexual and bisexual orientation given a background of CSA with an overall statistically significant finding. (Risk ratio [RR] 1.85, 95% confidence interval [CI] 1.00-3.42; p=0.05; I2 83%; 2 studies, 351 participants). Other studies discussing CSA as a general association with BPD without alluding to the development of homosexual and bisexual orientation were not included in this analysis.
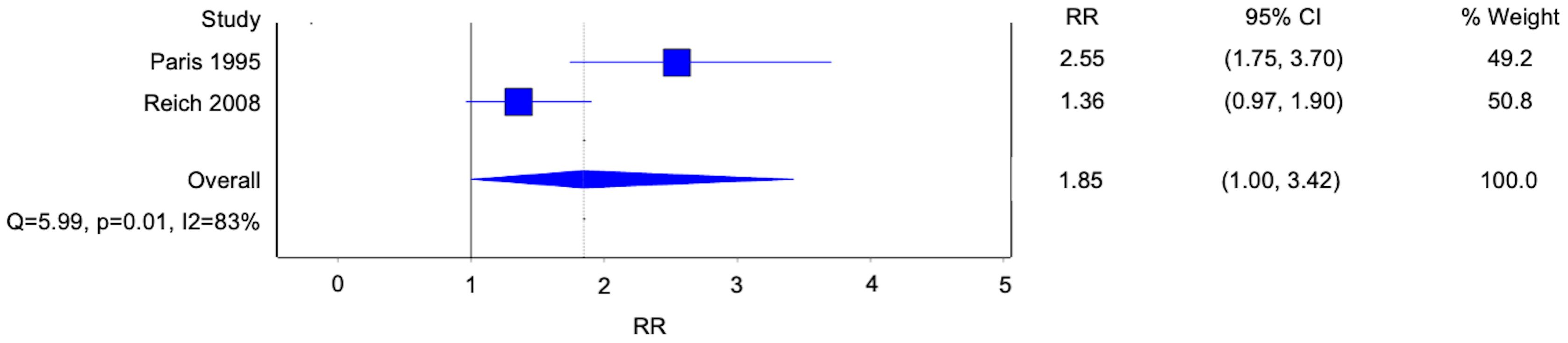
Figure 7. Forest plot of the risk ratio of childhood sexual abuse in patients with borderline personality disorder.
Factor associated with BPD: age of first sexual intercourse
Two studies reported the age of first sex as an associated factor of patients with BPD. Compared with the control group, the age of first sexual intercourse was about 1 year younger. However, this finding was not statistically significant (Weighted mean difference -0.99, 95% confidence interval [CI] -2.03-0.05; p=0.06; I2 69%, 2 studies, 313 patients).
Factor associated with BPD: number of sexual partners
Two studies compared the number of sexual partners between subjects with and without BPD. Overall, there were no statistically significant differences in the number of sexual partners between the two groups (Weighted mean difference 3.19, 95% confidence interval [CI] -1.30-7.68; p=0.16; I2 69%, 2 studies, 313 patients).
Factor associated with BPD: sexual coercion
Two studies reported a history of being coerced into sex as an associated factor of BPD (Figure 8). Patients with BPD were 2.65 times more likely to have been coerced into sex compared to subjects without BPD. (Risk ratio [RR] 2.65, 95% confidence interval [CI] 1.83-3.85; p<0.001; I2 0%; 2 studies, 313 participants).
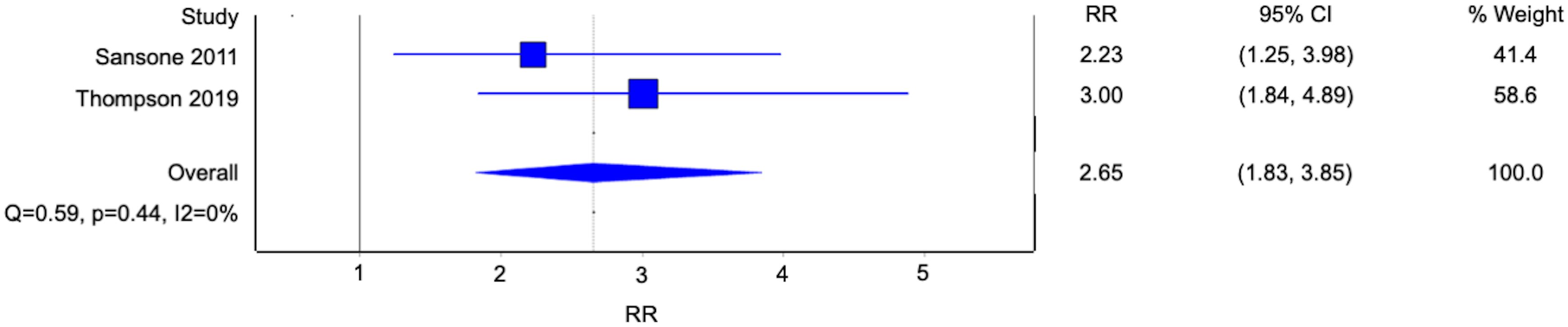
Figure 8. Forest plot of the risk ratio of sexual coercion in patients with borderline personality disorder.
Clinical outcomes
Patients with BPD had less optimal psychological health than their counterparts without BPD. Thompson et al. found that the BPD group encountered significantly greater psychological distress compared to the control group evaluated by the 6-item Kessler Psychological Distress Scale (K6) (24). This was echoed by Ramos et al., who reported that patients with BPD were 2.58 times more likely to have a history of committing suicide compared to those without (21). The hospitalisation rate of patients with BPD was reported to be 4.68 times that of subjects without BPD in the same study.
In addition to psychological well-being, overall health status was also compromised in the BPD group. Ramos et al. reported the BPD group to have poorer global functioning, reflected by a lower mean score of 70 ± 6.25 in the Global Assessment of Functioning (GAF) scale compared to subjects without BPD who scored a mean of 75 ± 9.92 (20). Thompson et al. also reported a worsening mean general health score in the BPD group compared to the control group (24). Although specific medical conditions were not explored in this study, patients with BPD were significantly more likely to smoke, consume alcohol in greater amounts and suffer concomitant substance use disorders (24). These factors combined might have contributed in part to the undermined physical health.
Concerning sexual health, studies did not reveal a higher risk of sexually transmitted diseases (STD) in patients with BPD. Sansone et al. reported an insignificant difference in the total number of times treated for STD between the BPD group and the control group (23). The study by Thompson et al. also reported similar rates of contracting most STD including HPV, genital herpes, syphilis and gonorrhoea (24). However, there was a statistically significantly higher rate of Candida/Thrush in the BPD group compared to the control group.
Discussion
Our findings demonstrated a strong and consistent association between BPD and homosexual and bisexual orientation. Homosexuality and bisexuality were both independently associated with BPD. The phenomenon did not exhibit any gender difference. It might have arisen from a history of childhood sexual abuse, positive family history of homosexual and bisexual orientation and certain parental bonding patterns, including higher maternal or paternal control and low maternal affection (20). For secondary outcomes, BPD was associated with having more sexual partners and sexual coercion. These factors, coupled with a high prevalence of homosexual and bisexual orientation, might heighten the risks to the physical and mental well-being of patients with BPD. Previous studies reported the prevalence of homosexual and bisexual orientation in the general population to be 9.7-11.3% (27, 28). This was congruent with our findings that patients with BPD were two times more likely than subjects without BPD to be homosexual and bisexual, and a pooled prevalence of 28% among patients with BPD.
Previous evidence from a single-centre study alluded to a potential diagnostic bias leading to elevated BPD diagnosis amongst sexual minorities (29). However, our review findings pooled from multiple studies suggested a genuine association between BPD and homosexual and bisexual orientation, with CSA being a direct contributing factor. This echoed with empirical evidence that a potential causal relationship existed between CSA and homosexual orientation. In female CSA victims, the development of homosexual attraction was postulated to arise from the propensity to avoid repeating sex with males, though this model failed to account for a similar phenomenon amongst male victims (30). Nonetheless, given the higher prevalence of CSA in both BPD and homosexual and bisexual populations, it could be inferred that BPD and sexual minorities might share certain psychosocial determinants that contribute to their experiences, and leading to some overlapping areas of concern.
Homosexual and bisexual orientation in the background of BPD might thus exacerbate clinical concerns regarding BPD. Both non-suicidal self-harm (NSSH) and suicidal attempts were pervasive in patients with BPD as manifestations of their emotional dysfunction, impulsivity and hypersensitivity to interpersonal rejection (31). A population-based study further reported increased suicidal attempts in homosexual and bisexual males. It was shown that lifetime bullying and homophobic discrimination could have contributed to the increased risk of NSSH and suicidal thoughts (32, 33). These together might confer poorer prognostic outcomes for homosexual and bisexual patients with BPD. Regarding neuropsychiatric illnesses, including depression and anxiety, a previous meta-analysis with pooled data from 12 health surveys presented a doubled likelihood for homosexual and bisexual adults to report mental health complaints, especially in the bisexual group who struggled more with identity development, concealment of sexual orientation and connecting with the lesbian, gay, bisexual and transgender (LGBT) community (34). Coupling with the salient features of affective dysregulation and, thus, mood swings in BPD, homosexual and bisexual patients with BPD might have a heightened risk of suffering from an Axis I disorder.
Physical health outcomes were also compromised in homosexual and bisexual patients with BPD. For sexual health, both BPD and homosexual and bisexual orientation have been shown to significantly increase self-reported STD rates (35), rendering patients with BPD vulnerable to poor sexual health. Whilst our review did not demonstrate a significant association between BPD status and most STDs, it could be explained by the exposure to early intervention programs in the specific study sample (24). This highlighted the importance of sexual education and contraception services in holistically treating homosexual and bisexual patients with BPD. In addition, the homosexual and bisexual group exhibited a higher incidence of common chronic conditions such as hypertension, obesity and alcoholism compared to their heterosexual counterparts (36). This finding, coupled with our findings of inferior overall health in patients with BPD, underscored the importance of screening for general medical conditions among homosexual and bisexual patients with BPD.
Furthermore, treatment for BPD appeared to be less effective in the homosexual and bisexual BPD group. Dialectical behavioural therapy (DBT) is the first-line psychotherapy for patients with BPD. While both heterosexual and homosexual or bisexual patients with BPD benefited from DBT, the magnitude of improvement differed between the two groups. The homosexual and bisexual subgroup showed less change in depressive symptoms, functional impairment and other psychiatric domains (37). It was postulated that microaggressions arising from clinicians’ bias or knowledge deficit might render homosexual and bisexual patients reluctant to engage in therapy. This represented the potential challenges in treating this subset of patients with BPD and the need for specific therapeutic approaches.
Our findings highlighted the need for clinicians to recognise a high prevalence of homosexual and bisexual orientation amongst patients with BPD. Providing an accepting and non-judgmental environment with adequate safety signals would be crucial to establishing therapeutic alliance in this subgroup of patients with BPD (38). Furthermore, standard DBT models for BPD with a hierarchy of targets prioritising risky behaviours might compromise the attention to minority-related issues. Instead, specific themes like resolving identity confusion and managing cis-heterosexism should be given prominence in DBT for maximising efficacy (38). Preliminary evidence has demonstrated that psychotherapy incorporating minority stress, such as Affirmative DBT, could improve emotional regulation and depression (39). Further studies are necessary to evaluate the role of sexual minority-specific therapy in treating homosexual and bisexual patients with BPD.
Our findings paved way for future research into the interplay between sexual and gender minorities and BPD. Gender diversity is increasingly recognised in clinical settings, which may complicate the management of mental health disorders. Previous studies have shown that gender-diverse individuals often experience higher levels of borderline symptoms and suicidality (40, 41). This underscored the necessity for further investigation into how gender identities intersect with BPD across epidemiological, etiological, and clinical dimensions. Clinicians should be prepared to navigate the complexities of these associations and may benefit from adopting a more individualised, minority-specific management approach.
Strength and limitations
Our meta-analysis was the first to systematically and quantitatively evaluate the association between BPD and homosexual and bisexual orientation. Expanding on the existing evidence, we demonstrated that BPD was independently associated with both homosexuality and bisexuality with no significant gender difference. We were also the first to demonstrate a statistical association between CSA and the development of homosexual and bisexual orientation in BPD.
Our review was limited by the inclusion of older studies of insufficient quality. Most studies were also cross-sectional and could not demonstrate a definitive causal relationship between BPD and homosexual and bisexual orientation. Moreover, patients with BPD recruited by most studies were not free of other psychiatric comorbidities. This potentially introduced confounding factors in establishing the association between BPD and homosexual and bisexual orientation.
Conclusions
Homosexual and bisexual orientation was more prevalent amongst patients with BPD, with CSA being a contributory factor. The concurrence of BPD and homosexual and bisexual orientation elevated risks of poor physical, psychiatric and sexual health outcomes. Our review findings serve to guide the management principles targeting these specific risks and suggest the need for sexual minority-specific psychotherapy to improve clinical outcomes. Further studies should be conducted to explore the longitudinal relationship between BPD and homosexual and bisexual orientation and evaluate the specific needs of this patient subgroup.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
YS: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. KL: Formal analysis, Methodology, Writing – original draft, Writing – review & editing. CH: Conceptualization, Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1490157/full#supplementary-material
References
1. Peritogiannis V, Stefanou E, Damigos D, Mavreas V. Admission rates of patients with borderline personality disorder in a psychiatric unit in a General Hospital. Int J Psychiatry Clin Pract. (2008) 12:78–80. doi: 10.1080/13651500701531455
2. Ellison WD, Rosenstein LK, Morgan TA, Zimmerman M. Community and clinical epidemiology of borderline personality disorder. Psychiatr Clin North Am. (2018) 41:561–73. doi: 10.1016/j.psc.2018.07.008
3. Shen C-C, Hu L-Y, Hu Y-H. Comorbidity study of borderline personality disorder: applying association rule mining to the Taiwan national health insurance research database. BMC Med Inform Decis Mak. (2017) 17:8. doi: 10.1186/s12911-016-0405-1
4. Porter C, Palmier-Claus J, Branitsky A, Mansell W, Warwick H, Varese F. Childhood adversity and borderline personality disorder: a meta-analysis. Acta Psychiatr Scand. (2020) 141:6–20. doi: 10.1111/acps.13118
5. Wilkinson-Ryan T, Westen D. Identity disturbance in borderline personality disorder: an empirical investigation. Am J Psychiatry. (2000) 157:528–41. doi: 10.1176/appi.ajp.157.4.528
6. Cass VC. Homosexual identity formation: a theoretical model. J Homosex. (1979) 4:219–35. doi: 10.1300/J082v04n03_01
7. Chapman BE, Brannock JC. Proposed model of lesbian identity development: an empirical examination. J Homosex. (1987) 14:69–80. doi: 10.1300/J082v14n03_05
8. Reuter TR, Sharp C, Kalpakci AH, Choi HJ, Temple JR. Sexual orientation and borderline personality disorder features in a community sample of adolescents. J Pers Disord. (2016) 30:694–707. doi: 10.1521/pedi_2015_29_224
9. Rodriguez-Seijas C, Morgan TA, Zimmerman M. A population-based examination of criterion-level disparities in the diagnosis of borderline personality disorder among sexual minority adults. Assessment. (2021) 28:1097–109. doi: 10.1177/1073191121991922
10. Lavan H, Johnson JG. The association between axis I and II psychiatric symptoms and high-risk sexual behavior during adolescence. J Pers Disord. (2002) 16:73–94. doi: 10.1521/pedi.16.1.73.22559
11. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
12. Zanarini MC, Gunderson JG, Frankenburg FR, Chauncey DL. The revised diagnostic interview for borderlines: discriminating BPD from other axis II disorders. J Pers Disord. (1989) 3:10–8. doi: 10.1521/pedi.1989.3.1.10
13. Regier DA, Kuhl EA, Kupfer DJ. The DSM-5: Classification and criteria changes. World Psychiatry. (2013) 12:92–8. doi: 10.1002/wps.20050
14. Zimmerman M, Mattia JI. Axis I diagnostic comorbidity and borderline personality disorder. Compr Psychiatry. (1999) 40:245–52. doi: 10.1016/S0010-440X(99)90123-2
15. Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. (1995) 51:768–74. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1
16. Smith AMA, Pitts MK, Shelley JM, Richters J, Ferris J. The Australian longitudinal study of health and relationships. BMC Public Health. (2007) 7:139. doi: 10.1186/1471-2458-7-139
17. Zanarini MC, Frankenburg FR, Reich DB, Hennen J, Silk KR. Adult experiences of abuse reported by borderline patients and Axis II comparison subjects over six years of prospective follow-up. J Nerv Ment Dis. (2005) 193:412–6. doi: 10.1097/01.nmd.0000165295.65844.52
18. Aromataris E, Lockwood C, Porritt K, Pilla B, Jordan Z eds. JBI Manual for Evidence Synthesis. JBI (2024). doi: 10.46658/JBIMES-24-01
19. George P, DeCastro Molina J, Heng B. The methodological quality of systematic reviews comparing intravitreal bevacizumab and alternates for neovascular age related macular degeneration: A systematic review of reviews. Indian J Ophthalmol. (2014) 62:761. doi: 10.4103/0301-4738.138615
20. Paris J, Zweig-Frank H, Guzder J. Psychological factors associated with homosexuality in males with borderline personality disorder. J Pers Disord. (1995) 9:56–61. doi: 10.1521/pedi.1995.9.1.56
21. Molina Ramos R, Carrasco Perera JL, Pérez Urdaniz A, Sánchez Iglesias S. Factors associated to the diagnoses of borderline personality disorder in psychiatric out-patients. Actas Esp Psiquiatr. (2002) 30:153–9.
22. Reich DB, Zanarini MC. Sexual orientation and relationship choice in borderline personality disorder over ten years of prospective follow-up. J Pers Disord. (2008) 22:564–72. doi: 10.1521/pedi.2008.22.6.564
23. Sansone RA, Chu JW, Wiederman MW. Sexual behaviour and borderline personality disorder among female psychiatric inpatients. Int J Psychiatry Clin Pract. (2011) 15:69–73. doi: 10.3109/13651501.2010.507871
24. Thompson KN, Betts J, Jovev M, Nyathi Y, McDougall E, Chanen AM. Sexuality and sexual health among female youth with borderline personality disorder pathology. Early Interv Psychiatry. (2019) 13:502–8. doi: 10.1111/eip.12510
25. Zanarini MC, Magni LR, Temes CM, Hein KE, Aguirre BA, Goodman M. Sexual orientation and gender of intimate relationship partners among adolescents with BPD and psychiatrically healthy adolescents. J Pers Disord. (2021) 35:1–7. doi: 10.1521/pedi_2020_34_470
26. Zubenko GS, George AW, Soloff PH, Schulz P. Sexual practices among patients with borderline personality disorder. Am J Psychiatry. (1987) 144:748–52. doi: 10.1176/ajp.144.6.748
27. Rahman Q, Xu Y, Lippa RA, Vasey PL. Prevalence of sexual orientation across 28 nations and its association with gender equality, economic development, and individualism. Arch Sex Behav. (2020) 49:595–606. doi: 10.1007/s10508-019-01590-0
28. Rapoport E, Athanasian CE, Adesman A. Prevalence of nonheterosexual identity and same-sex sexual contact among high school students in the US from 2015 to 2019. JAMA Pediatr. (2021) 175:970–2. doi: 10.1001/jamapediatrics.2021.1109
29. Becker LG, Asadi S, Zimmerman M, Morgan TA, Rodriguez-Seijas C. Is there a bias in the diagnosis of borderline personality disorder among racially minoritized patients? Pers Disord. (2023) 14:339–46. doi: 10.1037/per0000579
30. Haugaard JJ, Reppucci ND. The sexual abuse of children: a comprehensive guide to current knowledge and intervention strategies. 1st ed. San Francisco: Jossey-Bass Publishers (1988). 432 p.
31. Colle L, Hilviu D, Rossi R, Garbarini F, Fossataro C. Self-harming and sense of agency in patients with borderline personality disorder. Front Psychiatry. (2020) 11:449. doi: 10.3389/fpsyt.2020.00449
32. Kidd G, Marston L, Nazareth I, Osborn D, Pitman A. Suicidal thoughts, suicide attempt and non-suicidal self-harm amongst lesbian, gay and bisexual adults compared with heterosexual adults: analysis of data from two nationally representative English household surveys. Soc Psychiatry Psychiatr Epidemiol. (2024) 59:273–83. doi: 10.1007/s00127-023-02490-4
33. Remafedi G, French S, Story M, Resnick MD, Blum R. The relationship between suicide risk and sexual orientation: results of a population-based study. Am J Public Health. (1998) 88:57–60. doi: 10.2105/ajph.88.1.57
34. Semlyen J, King M, Varney J, Hagger-Johnson G. Sexual orientation and symptoms of common mental disorder or low wellbeing: combined meta-analysis of 12 UK population health surveys. BMC Psychiatry. (2016) 16:67. doi: 10.1186/s12888-016-0767-z
35. Everett BG. Sexual orientation disparities in sexually transmitted infections: examining the intersection between sexual identity and sexual behavior. Arch Sex Behav. (2013) 42:225–36. doi: 10.1007/s10508-012-9902-1
36. Jackson CL, Agénor M, Johnson DA, Austin SB, Kawachi I. Sexual orientation identity disparities in health behaviors, outcomes, and services use among men and women in the United States: a cross-sectional study. BMC Public Health. (2016) 16:807. doi: 10.1186/s12889-016-3467-1
37. Oshin LA, Silamongkol T, Pucker H, Finkelstein J, King AM, Rizvi SL. [amp]]hellip; And we could do better: Comparing the efficacy of dialectical behavior therapy between LGBQ and heterosexual adults with borderline personality disorder. Prof Psychol: Res Pract. (2024) 55:58–67. doi: 10.1037/pro0000529
38. Camp J, Morris A, Wilde H, Smith P, Rimes KA. Gender- and sexuality-minoritised adolescents in DBT: A reflexive thematic analysis of minority-specific treatment targets and experience. Cognit Behav Therap. (2023) 16:s1754470x23000326. doi: 10.1017/S1754470X23000326
39. Cohen JM, Norona JC, Yadavia JE, Borsari B. Affirmative dialectical behavior therapy skills training with sexual minority veterans. Cogn Behav Pract. (2021) 28:77–91. doi: 10.1016/j.cbpra.2020.05.008
40. Ceccolini CJ, Green JB, Friedman-Yakoobian MS. Gender-affirming care in the assessment and treatment of psychosis risk: Considering minority stress in current practice and future research. Early Intervent Psych. (2024) 18(3):207–16. doi: 10.1111/eip.13456
Keywords: meta-analysis, borderline personality disorder, sexual orientation, homosexuality, bisexuality
Citation: Shu YCC, Lau KT and Ho CSH (2024) Prevalence of homosexual and bisexual orientation in patients with borderline personality disorder and associated factors – a systematic review and meta-analysis. Front. Psychiatry 15:1490157. doi: 10.3389/fpsyt.2024.1490157
Received: 02 September 2024; Accepted: 28 October 2024;
Published: 21 November 2024.
Edited by:
Lionel Cailhol, University Institute in Mental Health of Montreal, CanadaReviewed by:
Lanlan Wang, Shanghai Jiao Tong University, ChinaPierre David, University Institute in Mental Health of Montreal, Canada
Copyright © 2024 Shu, Lau and Ho. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cyrus Su Hui Ho, cGNtaHNoQG51cy5lZHUuc2c=
 Ying Chi Camille Shu
Ying Chi Camille Shu Ka To Lau
Ka To Lau Cyrus Su Hui Ho
Cyrus Su Hui Ho