- 1Department of Education Sciences, Faculty of Psychology and Education Sciences, Alexandru Ioan Cuza University, Iaşi, Romania
- 2Department of Surgery II, Faculty of Medicine, Grigore T. Popa University of Medicine and Pharmacy, Iaşi, Romania
Introduction: Mothers caring for children with autism or chronic illnesses may experience heightened psychological distress due to the ongoing demands associated with caregiving. This study aimed to examine levels of psychological distress among Romanian mothers of children with autism, chronic illness, or typical development, and to explore the role of health-related quality of life and emotion regulation strategies.
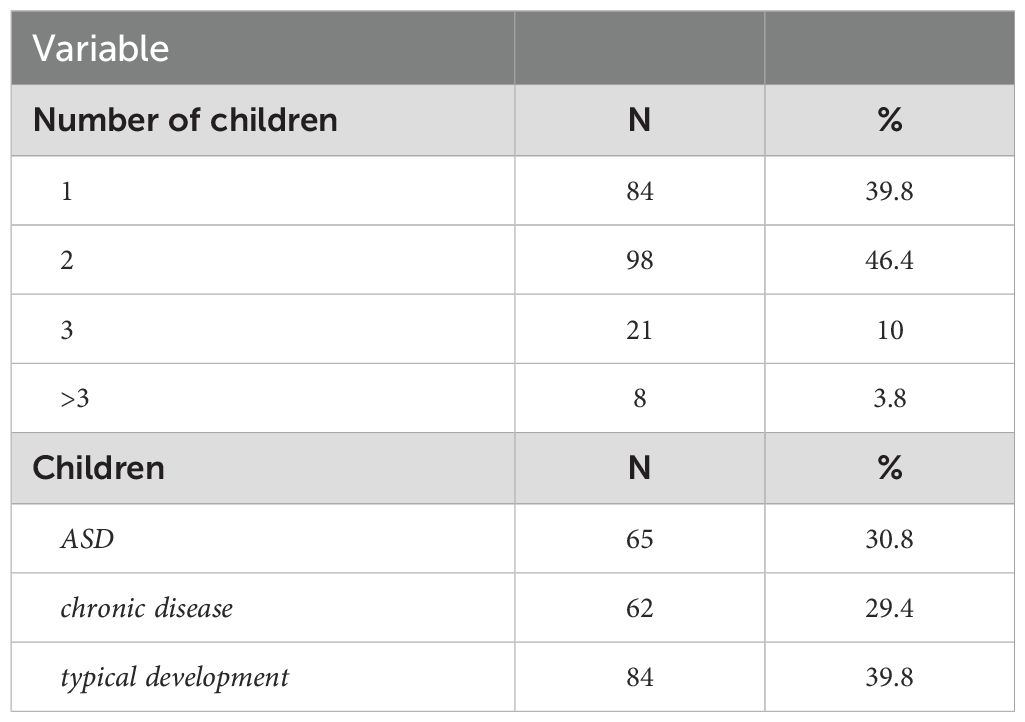
Methods: A total of 211 Romanian mothers aged 20 to 67 years (M = 38, SD = 8.07) participated in this study. The sample included mothers of children with autism (30.8%), chronic illness (29.4%), and typical development (39.8%). Participants completed self-report questionnaires assessing psychological distress, emotion regulation strategies (cognitive reappraisal and expressive suppression), and health-related quality of life.
Results: Health-related quality of life was found to be a significant predictor of psychological distress across all participant groups. Additionally, mothers of children with autism reported significantly higher levels of psychological distress compared to mothers of typically developing children.
Discussion: The findings underscore the psychological burden experienced by mothers of children with autism and highlight the importance of targeted support interventions. Addressing psychological distress and its contributing factors may improve the well-being of these caregivers. The results carry important implications for mental health practitioners, researchers, and policymakers aiming to support families managing childhood disability or chronic illness.
Introduction
Parenting stress represents a universal phenomenon, experienced by all parents, in varying degrees, although its prevalence is often accentuated by several factors such as challenging life situations, poverty, divorce, or single parenthood (1). In this context, parents of children with physical or mental conditions experience a significant amount of stress, often dealing with more parenting stress than parents of typically developed children (2). Previous research also suggests that parents of children with autism spectrum disorder (ASD) might be particularly vulnerable to experiencing higher levels of parental stress, even when compared to parents of children with other neurodevelopmental disorders or chronic conditions (3).
Previous research suggested that mothers of children with special needs might present higher levels of psychological distress when compared to the fathers (4). Moreover, the current research literature suggests that mothers’ parental stress might have a stronger impact on children’s behavior problems when compared to the parental stress of fathers (5). These differences might be explained by several factors, including (but not limited to) pregnancy, giving birth, and spending more time with the infants (6). However, it is important to note that this pattern might be consistent even several years after the birth of the child, with mothers presenting higher levels of distress. Moreover, while mothers’ stress might be more influenced by social isolation, spouse relationship problems, and perceived incompetence, fathers’ stress might be better explained by social isolation and health problems (7). While both mothers and fathers might have a strong impact on the cognitive and social development of their children, mothers’ parenting might have a stronger impact on curbing the development of behavior problems among children (5). The between maternal well-being and the challenges posed by raising children with specific needs, raised by diagnoses such as ASD or chronic conditions, has become a subject of increasing importance within the realm of psychological research (8). The need to explore maternal psychological distress in the context of raising children with ASD and chronic conditions stems from the significant impact that this may have on both mothers and the overall family dynamics (9–11), as highlighted by previous studies (12, 13).
In the current study, we aimed to investigate psychological distress among Romanian mothers, and the focus on this specific population was motivated by several factors. First, Romania offers a unique cultural framework to examine the proposed variables, given its ongoing transition from communism – a culture of segregation, to an inclusive society (14). Second, while there is a growing body of research addressing maternal psychological distress in the context of raising children with an autism spectrum disorder (ASD) and chronic diseases, studies that focus on specific Eastern European cultural contexts, such as Romania, are relatively scarce (15). Further, Romanian parents of children with special needs might be more likely to report a lower quality of life and less likely to expect the state to provide help when compared to their counterparts from other nations, both in Europe and in other regions (16).
The Double ABCX framework (17) describes how individuals cope and adapt to stressful conditions throughout time. In the context of parental experiences related to having a child with ASD, this model offers a conceptual framework for understanding the factors underlying parental distress and how families react to such stressors (15). The factors described by the model refer to (aA) child characteristics (e.g., the diagnosis and the associated behaviors, service needs, financial issues), (bB) internal and external resources (e.g., self-esteem, emotion regulation, perceived social support), (cC) appraisal of stressors – i.e., perceptions (e.g., psychological well-being, quality of life), and (BC) coping strategies and the way (xX) families adapt. According to the available literature exploring this model, the xX factor can be understood as either an “end result” or a “sequence of events”, which can be a favorable outcome (when families successfully modify their roles, routines, and other interactions to meet the new demands associated with the child’s diagnosis), or an unfavorable response (maladaptation) to the aA factor, resulting in a crisis (18).
In the present study, we focused on ASD and chronic conditions as reflecting the aA factor in the Double ABCX framework, two emotion regulation strategies (i.e., cognitive reappraisal and expressive suppression) as an expression of the bB factor (internal resources), health-related quality of life as the cC factor (appraisal of stressors), and maternal psychological distress as the xX factor – which was the primary focus of this study (see Figure 1).

Figure 1. The proposed research framework, based on an adopted version of the modified Double ABCX model (17).
Maternal psychological distress
The current research literature suggests that parents of children with ASD generally report higher levels of psychological distress and a lower quality of life compared to the parents of typically developed (TD) children (19). Also, mothers of children with special needs might present higher levels of psychological distress when compared to the fathers (4), and maternal distress might have a stronger impact on children’s behaviors compared to the parental stress of fathers (5). A recent review suggested that single young mothers of children with ASD who employ maladaptive coping strategies, exhibiting problem behaviors and sensory issues, are more susceptible to experiencing elevated levels of parental stress and poorer mental health (20).
Further, mothers of children diagnosed with a chronic condition (e.g., inflammatory bowel diseases, asthma, diabetes, cystic fibrosis, celiac disease) often report elevated levels of psychological distress due to the complexity of medical regimes (21), financial demands, and the complex management of unpredictable situations related to their medical condition (22). They also often experience guilt and worries, not only related to their child’s medical condition but also related to their other siblings, with a negative impact on the family system as a whole (23). The significantly higher psychological distress is generally higher than that of caregivers of healthy children, as systematic reviews previously highlighted (24). However, to date, no studies explored the specific roles of cognitive reappraisal, expressive suppression), and health-related quality of life among Romanian mothers of children with ASD, chronic conditions, and TD children, as in the present study.
Emotion regulation strategies
Emotion regulation represents a set of cognitive skills aimed at managing emotions, in order to minimize the harmful impact of strong emotions. (25). The process of emotion regulation occurs in a concurrent manner with the emotions that the individual is feeling, individuals being determined to present strong emotional reactions toward significant events, then, through emotion regulation, they return to a state without strong emotions (26). Developing appropriate emotion regulation skills is important both for the mother’s well-being and for the proper development of the emotional skills of their children (27). Parents with better emotion-regulation skills often exhibit more positive parenting behavior and generally have children with better emotion regulation skills (28). The adoption of maladaptive emotion regulation strategies might increase parental stress (29), which further predict lower levels of parents’ bonding with their children.
In this study, we focused on two emotion regulation strategies, i.e., cognitive reappraisal and expressive suppression, as conceptualized by Gross and John (30). Cognitive reappraisal refers to regulating emotions by altering an individual’s interpretation or perception of a circumstance to adjust its emotional effect. For instance, when confronted with a difficult scenario, one may attempt to reframe the event in a more optimistic manner, emphasizing potential benefits or different viewpoints (31). Cognitive reappraisal was previously suggested as a more effective strategy for managing parental stress, parents that adopt this strategy are less likely to report parental burnout and more likely to manage negative emotions even when receiving insufficient social support (32). While the previous study focused on parents of typical children, similar effects were reported for parents of children with mental conditions, cognitive reappraisal being suggested as the most beneficial emotion regulation strategy (33). Moreover, the endorsement of cognitive reappraisal is also associated with better parental caregiving for children diagnosed with ASD (34). Furthermore, in the case of parents of children with a chronic condition or ASD, instead of solely viewing the diagnosis as a source of distress, parents employing cognitive reappraisal might think that this experience may strengthen family bonds as they support each other through this journey, may connect with other parents sharing this experience, or may gain a deeper understanding of their child’s needs. Thus, cognitive reappraisal can entail a deliberate alteration of their interpretation of this situation, fostering a more optimistic (and less stressful) perspective (35).
On the other hand, expressive suppression involves inhibiting the outward expression of one’s emotions, essentially masking or hiding one’s true feelings. For instance, a parent of a child with a chronic condition might inhibit the outward expression of their emotions to maintain composure and support their child. They might suppress their sadness, avoid showing tears, and maintaining a neutral or positive facial expression (36). Though this strategy may lead to short-term emotional regulation, it can negatively affect interpersonal relationships and long-term well-being due to the inhibition of genuine emotional expression (37).
As the available literature suggests, generally, cognitive reappraisal – compared to expressive suppression, contributes to a better psychological adjustment in various challenging situations among parents of children with ASD and chronic conditions (38). Effective emotion regulation strategies such as cognitive reappraisal may enhance the quality of parent-child interactions while decreasing parental psychological distress (34, 35). However, less effective strategies such as expressive suppression seem to have the opposite effect, contributing to increased levels of parental psychological distress (37, 39).
Health-related quality of life
Health-Related Quality of Life (HRQoL) is a multidimensional concept referring to an individual’s perception of their health and the numerous ways in which it affects them in their daily lives. In addition to conventional indicators of health, such as the absence of disease or illness, it encompasses subjective assessments of one’s mental, physical, and social welfare (40).
Parents of children with disabilities or chronic illnesses are particularly susceptible in terms of the impact on their quality of life about health (41). The available literature suggests that parents of children with ASD or chronic conditions often report lower HRQoL, higher psychological distress, and lower overall quality of life compared to parents of TD children (42–44) and that mothers’ HRQoL in these cases seems to be lower than fathers’ (45, 46). Moreover, mothers of children with ASD are more likely to report lower HRQoL and present a higher likelihood of dealing with mental disorders (47). Generally, parents of children with ASD report a lower HRQoL, which is also associated with higher levels of parental stress (48). More recent meta-analytical reports also suggest that parents of children with mental disorders are experiencing a clinically relevant reduction in their quality of life, compared to the parents of typical children (49). Some scholars also reported that parents of children with ASD also reported lower HRQoL compared to caregivers of children with chronic conditions (50).
Nevertheless, there seems to be a bidirectional relation between parental psychological distress and HRQoL, which is highlighted by several studies. For instance, many scholars suggested that lower well-being and higher parental stress among parents of children with ASD seem to significantly predict lower HRQoL (51). At the same time, low HRQoL was suggested as a significant associated factor (52) and a significant predictor of psychological distress (53), though this direction is less investigated; thus, we aimed to add to the related literature by focusing on the predictive role of HRQoL on maternal psychological distress.
The present study
The current study was built on the Double ABCX framework, focusing on two emotion regulation strategies (i.e., cognitive reappraisal and expressive suppression) and HRQoL as potential predictors of psychological distress among mothers of children with ASD, a chronic condition, or TD children.
Based on previous studies, the primary hypotheses of this study were the following:
H1. Cognitive reappraisal would be negatively associated with maternal psychological distress, regardless of the child’s status (with ASD, a chronic condition, or TD).
H2. Expressive suppression would be negatively associated with maternal psychological distress, regardless of the child’s status (with ASD, a chronic condition, or TD).
H3. HRQoL would be positively associated with maternal psychological distress, regardless of the child’s status (with ASD, a chronic condition, or TD).
H4. Cognitive reappraisal would negatively predict maternal psychological distress, regardless of the child’s status (with ASD, a chronic condition, or TD).
H5. Expressive suppression would positively predict maternal psychological distress, regardless of the child’s status (with ASD, a chronic condition, or TD).
H6. HRQoL would positively predict maternal psychological distress, regardless of the child’s status (with ASD, a chronic condition, or TD).
H7. Maternal psychological distress would be significantly higher among mothers of children with ASD and chronic conditions, compared to mothers of TD children, with the highest rates among mothers of children with ASD.
Materials and methods
Participants and procedure
The sample comprised 211 Romanian mothers aged 20 to 67 (M = 38, SD = 8.07). Most had two children (46.4%) and were married (85.3%). Among the participants, 30.8% (N = 65) reported having a child with ASD, 29.4% (N = 62) reported having a child with a chronic disease, and 39.8% (N = 84) reported they had TD children (see Table 1 for a detailed description). The chronic diseases reported by the participants included epilepsy, ADHD, Rett syndrome, KBG syndrome, and tetraparesis.
A web-based questionnaire was distributed using social media groups (i.e., Facebook and Whatsapp); also, personal e-mail invitations were distributed at the end of 2022 and the beginning of 2023 (12.11.2022- 19.03.2023). Participants were briefed about the participation prerequisites, incentives, and their prerogative to exit the study at will. Furthermore, we assured all participants that their input would remain confidential and unidentified, solely intended for this research. The research protocol was designed following the ethical guidelines from the university where the authors are affiliated and the 2013 Helsinki Declaration. Following their informed consent, participants needed around 10 minutes to answer all the questions.
Measures
Psychological distress
We measured participants’ psychological distress using the DASS-21 scale developed by Lovibond and Lovibond (54). In the present study, we used the Romanian version of the scale (14). The 21 items measured participants’ depression, anxiety, and stress symptoms, which were self-reported considering the preceding week. Participants gave their answers on a Likert scale ranging from 0 (did not apply at all) to 3 (very applicable). Example items included “I couldn’t seem to experience any positive feeling at all” (depression); “I was aware of dryness of my mouth” (anxiety); and “I found it hard to wind down” (stress). Higher scores indicated higher psychological distress. Cronbach’s alpha in the present study was.95.
Emotion regulation
We used the 10-item Emotional Regulation Questionnaire developed by Gross and John (30) to measure two emotion regulation strategies, i.e., cognitive reappraisal (6 items) and expressive suppression (4 items). The Romanian version that we used was previously used in studies among Romanian samples (55) and showed good psychometric properties. Example items include “I keep my emotions to myself” (expressive suppression), and “When I want to feel more positive emotion (such as joy or amusement), I change what I’m thinking about” (cognitive reappraisal). Items were measured on a 7-point Likert scale, where 1 = strong disagreement, and 7 = strong agreement. The internal consistency (Cronbach’s alpha-s) was α=.86 for the cognitive reappraisal subscale, and α=.80 and for expressive suppression. Higher scores indicated a higher tendency to use one of the two strategies.
Health-related quality of life
We used the Health-Related Quality of Life (WB-HRQoL) scale developed by Janković et al. (40), which is a 19-item instrument measuring physical (5 items), mental health (8 items), social (three items), and environmental (three items) quality of life. Example items included “I do not feel any pain” (physical aspects of quality of life), “I am always in a good mood” (mental health aspects), “My family relations are excellent”, and “I regularly meet my friends and enjoy their company” (social aspects). Participants responded using a 5-point Likert scale ranging from 1 (I do not agree completely”) to 5 (I agree completely). Cronbach’s alpha-s for each dimension were the following: 0.70 for the physical dimension, 0.81 for mental health, 0.71 for the social dimension, and 0.77 for the environmental dimension. The instrument was translated from the English language into the Romanian language using the forward-backward translation design (56), and the few discrepancies between the original and the back-translated version were identified and solved, resulting in the final versions of the scale. Cronbach’s alpha for the overall scale (measuring global health-related quality of life) was 0.89. Higher scores indicated higher health-related quality of life.
A demographic scale assessed participants’ age, number of children, and child’s status (i.e., with ASD, a chronic disease, or no diagnosis – which will further be referred to as TD children).
Results
Overview of data analysis
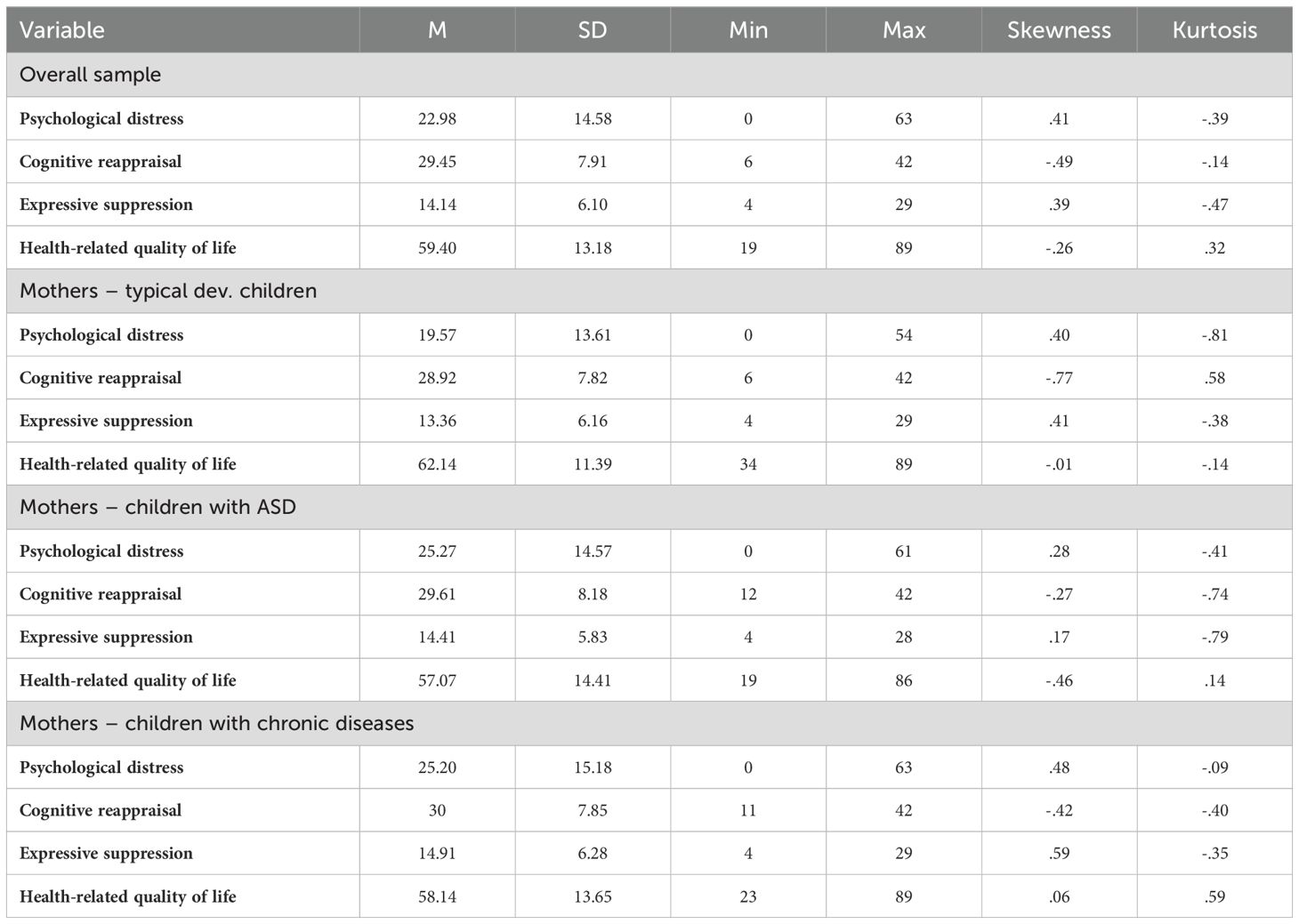
We used the 26v. of the SPSS program to analyze our data. There were no missing data, as the items were set as required (i.e., mandatory) to complete the study. The assumptions were first evaluated using descriptive univariate analysis (see Table 2). Skewness and Kurtosis indicators were calculated to determine the distributions’ normality (57).
Associations between the main variables
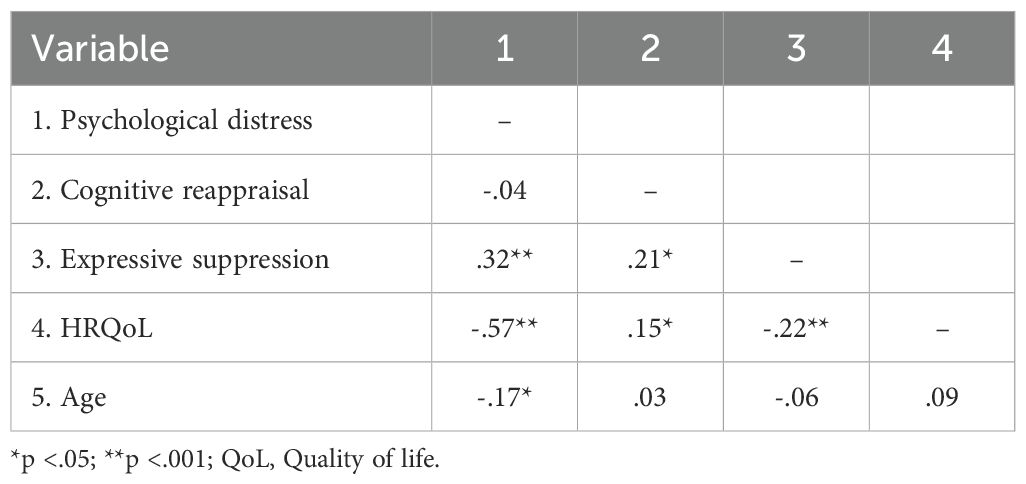
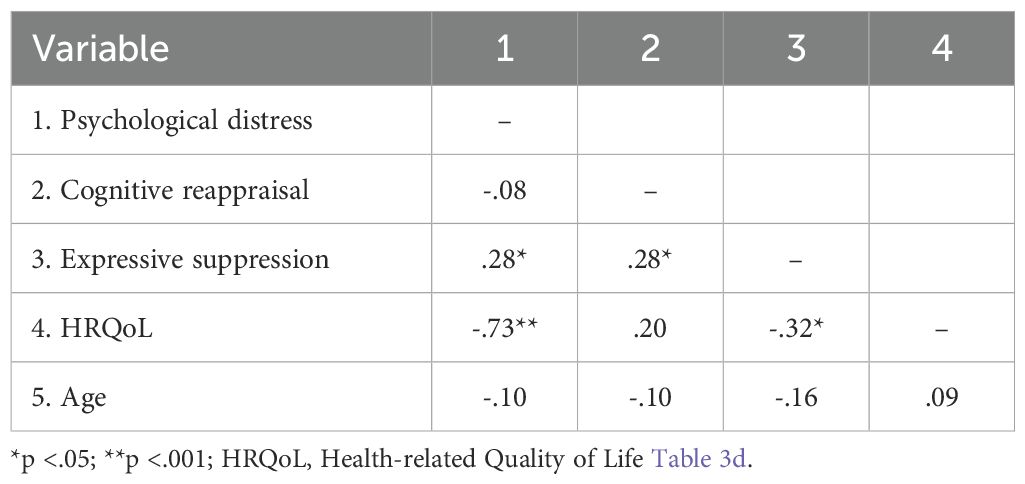
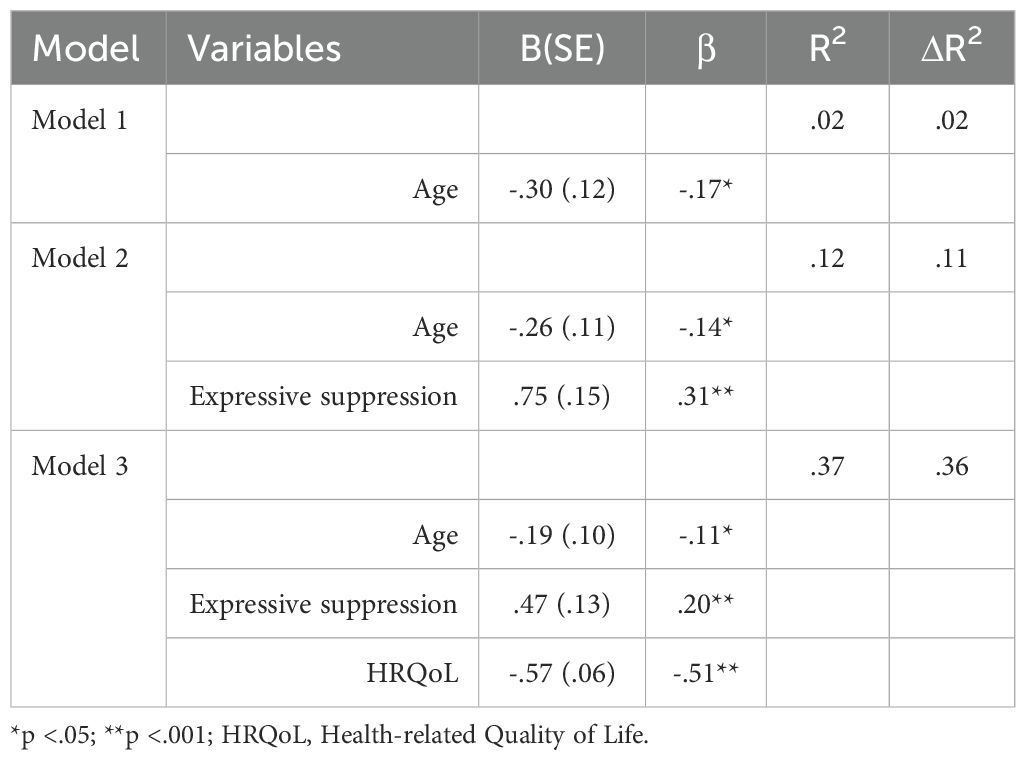
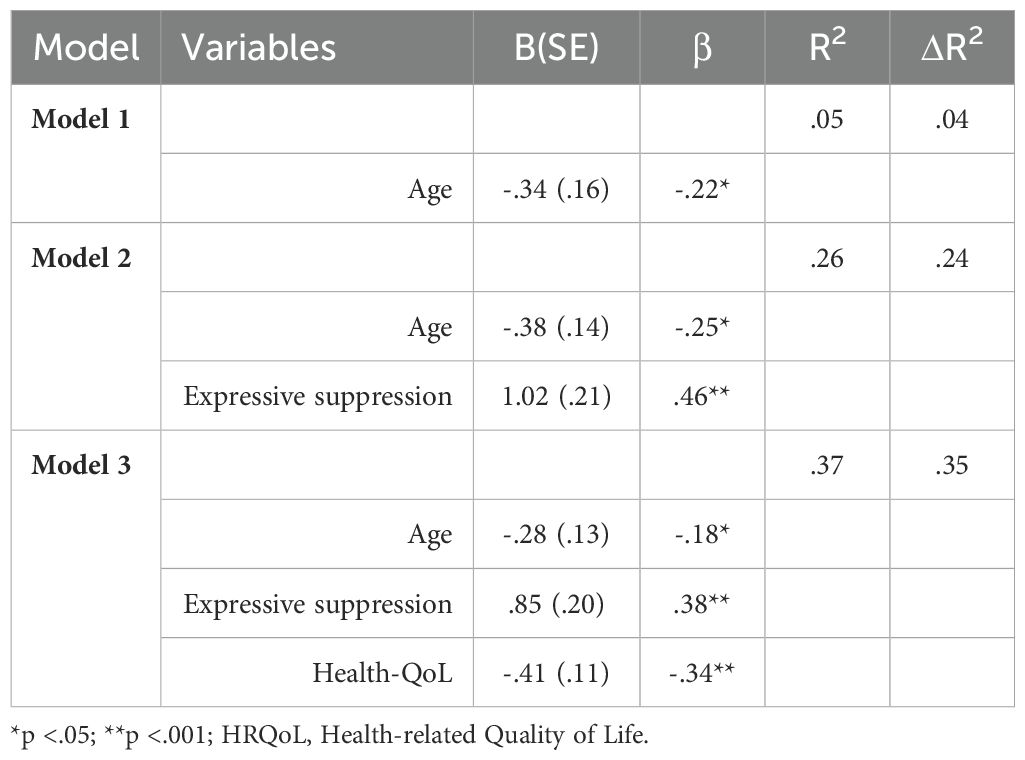
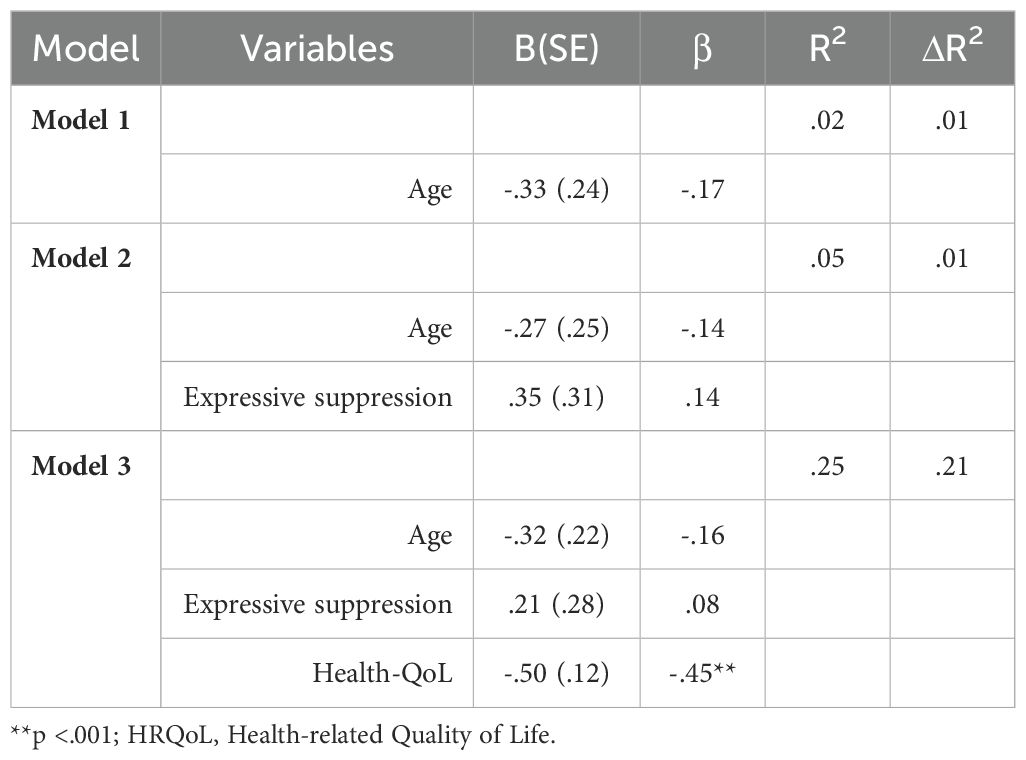
Next, we examined the associations between the primary variables in the overall sample, as well as separately – depending on the targeted groups (i.e., mothers of TD children/children with ASD/children with a chronic disease diagnosis - CD). Results are presented in Tables 3A-D.
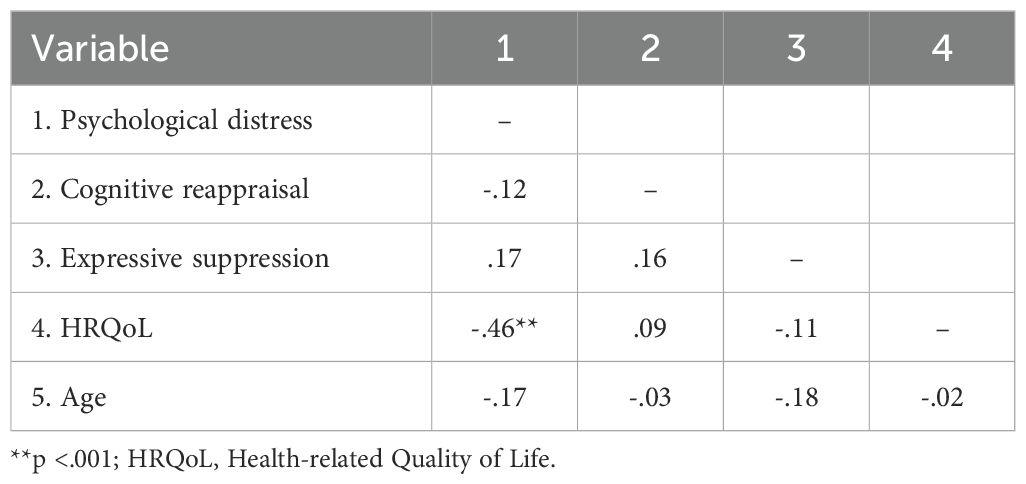
Table 3d. Correlations between the main variables – mothers of children diagnosed with a chronic condition, N = 62.
Overall sample
Results suggested that psychological distress was negatively associated with HRQoL, r = -.57, p <.001 and age, r = -.17, p = .01. Also, psychological distress was positively associated with expressive suppression, r = .32, p <.001 (Table 3A).
Parents of TD children
Results suggested that psychological distress was negatively associated with HRQoL, r = -.46, p <.001 and age, r = -.22, p = .03. Also, psychological distress was positively associated with expressive suppression, r = .45, p <.001 (Table 3B).
Parents of children with ASD
Results suggested that psychological distress was negatively associated with HRQoL, r = -.73, p <.001 and positively associated with expressive suppression, r = .28, p = .02 (Table 3C).
Parents of children with a chronic condition
Results suggested that psychological distress was negatively associated with HRQoL, r = -.46, p <.001. No other significant associations emerged (Table 3D).
Hierarchical regression analysis predicting maternal psychological distress (depending on child’s status)
Next, we conducted a hierarchical regression analysis to predict maternal psychological distress. We performed the analyses in the overall sample and separately (depending on the child’s diagnosis). In all cases, we introduced age in Step 1, expressive suppression in Step 2, and health-related quality of life in Step 3 (see Tables 4A–D).
Overall sample
The first model (Table 4A), which only included age, was significant, F(1, 210) = 6,19, p = .01, explaining 2.4% in the variance of psychological distress. The second model, which added expressive suppression, was significant, F(2, 210) = 15.17, p <.001, and explained 11.90% of the variance in psychological distress. The change brought by the addition of this variable was also significant, Fch = 23.48, p <.001. Model 3, which added HRQoL, was also significant, F(3, 210) = 41,85, p <.001; the change brought by the addition of this variable was also significant, Fch = 83.20, p <.001. The final model explained 36.9% of the variance in mothers’ psychological distress. In the final model, all predictors were significant, but the strongest was HRQoL, β = -.51, p <.001, followed by expressive suppression, β = .20, p <.001, and age, β = -.11, p = .04.
Parents of TD children
The first model (Table 4B), which only included age, was significant, F(1, 83) = 4.42, p = .03 explaining 4% in the variance of psychological distress. The second model, which added expressive suppression, was significant, F(2, 83) = 14.71, p <.001, and explained 24.80% of the variance in psychological distress. The change brought by the addition of this variable was also significant, Fch = 23.77, p <.001. Model 3, which added HRQoL, was also significant, F(3, 83) = 16.23, p <.001; the change brought by the addition of this variable was also significant, Fch = 14.41, p <.001. The final model explained 35.5% of the variance in mothers’ psychological distress. In the final model, all predictors were significant, but the strongest was expressive suppression, β = .38, p <.001, followed by HRQoL, β = -.34, p <.001, and age, β = -.18, p = .04.
Parents – children with ASD
The first model (Table 4C), which only included age, was not significant, F(1, 64) = .72, p = .39. The second model, which added expressive suppression, was not significant, F(2, 64) = 2.90, p =.06; the change brought by the addition of this variable was, however, significant, Fch = 5.04, p =.02. Model 3, which added HRQoL, was the only significant model, F(3, 64) = 24.56, p<.001; the change brought by the addition of this variable was significant, Fch = 62.14, p<.001. The final model explained 52.5% of the variance in mothers’ psychological distress. In the final model, the only significant predictor was HRQoL, β = -.71, p<.001.
Parents – children with a chronic disease
The first model (Table 4D), which only included age, was not significant, F(1, 61) = 1.78, p = .18. The second model, which added expressive suppression, was also not significant, F(2, 61) = 1.54, p=.22. Model 3, which added HRQoL, was the only significant model, F(3, 61) = 6.63, p<.001; the change brought by the addition of this variable was significant, Fch = 62.14, p=.001. The final model explained 52.5% of the variance in maternal psychological distress. In the final model, the only significant predictor was HRQoL, β = -.71, p<.001.
Finally, to better understand the potential differences in mothers’ psychological distress (depending on their child’s status/condition), we performed One-way ANOVA analyses. Results suggested significant differences between the groups, F (2, 210) = 3.93, p=.02. More specifically, the mothers of children diagnosed with ASD (M=25.27) reported marginally significantly higher psychological distress (Mdif=-5.70, p=.052) than those with TD (M=25.20). No other significant differences emerged.
Discussions
Through the current study, we aimed to investigate psychological distress experienced by mothers of TD children, children with ASD, and children with chronic illnesses, through the lens of the Double ABCX framework (17). For the aA factor of the framework, child characteristics, we focused on investigating children with TD, ASD, and chronic illnesses. We operationalized the bB factor (i.e., internal and external resources) through two emotion regulation strategies, cognitive reappraisal, and expressive suppression, respectively. The cC factor (i.e., appraisal of stressors) was operationalized through HRQoL, and, finally, the xX factor was operationalized through maternal psychological distress. Moreover, we included the age of our participants as a potential predictor of maternal psychological distress.
In the overall sample, HRQoL was the strongest predictor of maternal psychological distress, with higher levels of HRQoL being associated with lower levels of distress. The second strongest predictor was expressive suppression, having a positive effect on maternal psychological distress, followed by age, which had a negative effect. Therefore, the cC factor (i.e., appraisal of stressors) represented the most important predictor of psychological distress among our participants. These results are in line with previous research, with parents of children with disabilities or physical or psychological disorders presenting lower levels of HRQoL, compared to parents of TD children (41).
In the group of mothers of TD children, expressive suppression was the strongest predictor of psychological distress, having a positive effect, followed by HRQoL and age, both having a negative impact. For this group, the bB factor represented the most important predictor of maternal psychological distress. The current results suggest that expressive suppression might be a more relevant predictor of parental psychological distress for mothers of TD children when compared to cognitive reappraisal. The endorsement of maladaptive emotion regulation strategies might be more impactful toward psychological distress, compared to the adoption of adaptive strategies.
When investigating the group of mothers of children with ASD, HRQoL was the only significant predictor of maternal psychological distress, with higher levels of HRQoL being associated with lower levels of distress. The current results are in line with the previous literature, which suggests that parents of children with ASD usually report lower levels of HRQoL when compared to other parental groups (48). Furthermore, our results suggest that Romanian parents of children with ASD are particularly vulnerable to reduced levels of HRQoL, this factor being more important for predicting their levels of psychological distress.
Finally, in the group of mothers of children with chronic diseases, HRQoL was the only significant predictor, having a negative effect on maternal psychological distress. The final model for the group in this case followed a similar pattern to the model for the group of mothers of children with ASD. The current results suggest that parents of children with special needs might follow a similar pattern in developing psychological distress, with HRQoL playing a particularly relevant role in the Romanian context. Nevertheless, further research is needed to test the validity of these claims.
An important finding that diverged from our expectations was represented by the absence of a significant effect of cognitive reappraisal toward maternal psychological distress in all the investigated groups. These results seem counterintuitive, considering previous research that suggests that cognitive reappraisal might be a more efficient mechanism for reducing psychological distress, compared to expressive suppression (32). However, the current results might suggest that HRQoL might be particularly relevant in predicting psychological distress for Romanian mothers of children with special needs, to the point where emotion regulation strategies might no longer make a significant difference. Finally, when comparing the three groups, mothers of children with ASD presented higher levels of psychological distress. These results are convergent with previous research (3), which suggests that parents of children diagnosed with ASD are experiencing higher levels of psychological distress compared to other parents.
Limitations and future directions
Several limitations of the current study need to be addressed. First, we collected our data through an online survey, which limited our ability to control potential confounding variables that might have influenced the responses offered by our participants. To counter this limitation, future studies should consider using a more controlled environment (i.e., a laboratory) for data collection. Second, we operationalized our research variables through questionnaires, which relied on subjective evaluations reported by our participants. Furthermore, using questionnaires increased the risk of desirability bias in the responses offered by our participants. To counter this limitation, future studies should employ experimental designs allowing more objective measurements of the research variables. Third, we used a convenience sample, which does not reflect the characteristics of the investigated demographic group. To counter this limitation, future studies might benefit from using representative samples that better reflect the characteristics of the investigated population.
Fourth, through the current study, we focused on a limited number of variables related to maternal psychological distress. However, we did not consider several variables that might be relevant in predicting maternal psychological distress. For example, social support was previously suggested to play a crucial role in predicting psychological distress among parents (58). Moreover, parental psychological distress might further be accentuated by poverty, divorce, and single parenthood (1). Therefore, future studies might benefit from introducing various variables that contribute to explaining psychological distress.
Finally, in the current study, we focused on investigating mothers of TD children, children with ASD, and children with chronic diseases. Various disorders and medical conditions experienced by children might have varying effects on the mental well-being of their parents. Moreover, we did not compare the parents whose children presented different chronic illnesses. Furthermore, future research might benefit from investigating parents of children with other diagnoses (e.g., Down syndrome) (59).
Implications
The current study provides relevant data on the Romanian cultural context of mothers of children with special needs. Our findings provide various practical implications for practitioners, researchers, and policymakers. First, for the groups of mothers of children with ASD and mothers of children with chronic diseases, HRQoL was the only significant predictor of psychological distress. The cultural context might play an important role in the observed results, with Romanian parents of children with special needs being particularly vulnerable to presenting a lower HRQoL, while also being less likely to expect support from the authorities (16). Therefore, policymakers should consider interventions that aim to address this problem by providing more social, material, and emotional support for parents of children with special needs. Addressing these needs might prove more beneficial than investing in interventions aimed toward the development of emotion regulation skills because neither expressive suppression nor cognitive reappraisal was a significant predictor of maternal psychological distress in the two groups of parents of children with special needs. However, further research is needed to test the validity of these claims.
Second, cognitive reappraisal had no significant effect on psychological distress in any of the models. In contrast, expressive suppression had a negative effect on psychological distress in the overall sample and the group of mothers of children with TD. These results seem unexpected, considering previous research suggested that cognitive reappraisal might be one of the most adaptive emotion regulation strategies (33). However, these findings suggest that interventions aimed at developing emotion regulation skills for Romanian parents might benefit from diminishing the negative impact of maladaptive coping strategies rather than enhancing cognitive reappraisal. Nevertheless, more research is needed, to explore the relevance of various emotion regulation strategies.
Third, age had a negative impact on psychological distress for mothers of children with TD. However, age was no longer a significant predictor of psychological distress for mothers of children with special needs. These results suggest that for mothers of TD children, psychological distress might become easier to manage with age. However, it is important to note that, generally speaking, mothers of higher ages might also have children of higher ages, which might also explain the decrease in psychological distress. Nevertheless, for mothers of children with special needs, age no longer played a significant role. This might suggest that raising children with ASD or chronic disorders might represent a significant source of psychological distress, regardless of their age. Therefore, interventions aimed at diminishing parental psychological distress might be efficient for various age groups.
Conclusion
The current study contributed to the current research literature by investigating the predictive factors of parental psychological distress in Romania. HRQoL was the most relevant predictor, followed by expressive suppression and age. Expressive suppression was a stronger predictor for psychological distress among mothers of TD children. In comparison, HRQoL was a stronger predictor for psychological distress among mothers of children with ASD or chronic diseases. The current study brought valuable insights into the Romanian context of parental psychological distress, highlighting a potentially stronger impact of HRQoL on parental distress, compared to emotion regulation strategies, and age. In the Double ABCX framework, appraisal of stressors represented the most important factor in predicting maternal psychological distress, followed by internal resources. Moreover, in our study, we observed a similar pattern to the one previously reported in the current research literature, suggesting that mothers of children with ASD experience higher levels of psychological distress, compared to mothers of TD children and children with other conditions.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Faculty of Psychology and Education Sciences, UAIC Iasi. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AC: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. I-AM: Formal analysis, Visualization, Writing – original draft, Writing – review & editing. DI: Data curation, Writing – original draft, Writing – review & editing. IR: Data curation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The financial support of the project (EXCELENT-UAIC), code CNFIS-FDI-2025-F-0318, is acknowledged by the authors.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Louie AD, Cromer LD, and Berry JO. Assessing parenting stress: review of the use and interpretation of the parental stress scale. Family J. (2017) 25:359–67. doi: 10.1177/1066480717731347
2. Feizi A, Najmi B, Salesi A, Chorami M, and Hoveidafar R. Parenting stress among mothers of children with different physical, mental, and psychological problems. J Res Med Sci. (2014) 19:145–52.
3. Hayes SA and Watson SL. The impact of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. J Autism Dev Disord. (2013) 43:629–42. doi: 10.1007/s10803-012-1604-y
4. Grebe SC, Mire SS, Kim H, and Keller-Margulis MA. Comparing fathers’ and mothers’ Perspectives about their child’s autism spectrum disorder. J Autism Dev Disord. (2022) 52:1841–54. doi: 10.1007/s10803-021-05077-7
5. Ward KP and Lee SJ. Mothers’ and fathers’ parenting stress, responsiveness, and child wellbeing among low-income families. Children Youth Serv Rev. (2020) 116:105218. doi: 10.1016/j.childyouth.2020.105218
6. Hildingsson I and Thomas J. Parental stress in mothers and fathers one year after birth. J Reprod Infant Psychol. (2014) 32:41–56. doi: 10.1080/02646838.2013.840882
7. Johansson M, Nordström T, and Svensson I. Depressive symptoms, parental stress, and attachment style in mothers and fathers two and a half years after childbirth: Are fathers as affected as mothers? J Child Health Care. (2021) 25:368–78. doi: 10.1177/1367493520942050
8. Nomaguchi K and Milkie MA. Parenthood and well-being: A decade in review. J Marriage Family. (2020) 82:198–223. doi: 10.1111/jomf.12646
9. Burton L. The family life of sick children: A study of families coping with chronic childhood disease Vol. 8. Routledge (2022).
10. Halstead E, Ekas N, Hastings RP, and Griffith GM. Associations between resilience and the well-being of mothers of children with autism spectrum disorder and other developmental disabilities. J Autism Dev Disord. (2018) 48:1108–21. doi: 10.1007/s10803-017-3447-z
11. Totsika V, Hastings RP, Emerson E, Berridge DM, and Lancaster GA. Prosocial skills in young children with autism, and their mothers’ psychological well-being: Longitudinal relationships. Res Autism Spectr Disord. (2015) 13:25–31. doi: 10.1016/j.rasd.2015.01.001
12. Pruitt MM, Willis K, Timmons L, and Ekas NV. The impact of maternal, child, and family characteristics on the daily well-being and parenting experiences of mothers of children with autism spectrum disorder. Autism. (2016) 20:973–85. doi: 10.1177/1362361315620409
13. Sav A, King MA, Whitty JA, Kendall E, McMillan SS, Kelly F, et al. Burden of treatment for chronic illness: A concept analysis and review of the literature. Health Expectations. (2015) 18:312–24. doi: 10.1111/hex.12046
14. Maftei A, Gherguț A, Roca D, and Danila O. Transitioning from decades of segregation: Religiosity and the attitudes towards intellectual disability in Romania. Journal of Beliefs & Values. (2023) 44(3):334–48. doi: 10.1080/13617672.2022.2125674
15. Čolić M, Dababnah S, Garbarino N, and Betz G. Parental experiences raising children with autism spectrum disorder in Eastern Europe: A scoping review. Int J Dev Disabil. (2022) 68:1–13. doi: 10.1080/20473869.2019.1688931
16. Eapen V, Karlov L, John JR, Beneytez C, Grimes PZ, Kang YQ, et al. Quality of life in parents of autistic children: A transcultural perspective. Front Psychol. (2023) 14:1022094. doi: 10.3389/fpsyg.2023.1022094
17. Lavee Y, McCubbin HI, and Patterson JM. The double ABCX model of family stress and adaptation: An empirical test by analysis of structural equations with latent variables. J Marriage Family. (1985), 811–25. doi: 10.2307/352326
18. Pozo P, Sarriá E, and Brioso A. Family quality of life and psychological well-being in parents of children with autism spectrum disorders: A double ABCX model. J Intellectual Disability Res. (2014) 58:442–58. doi: 10.1111/jir.2014.58.issue-5
19. Pisula E and Porębowicz-Dörsmann A. Family functioning, parenting stress and quality of life in mothers and fathers of Polish children with high functioning autism or Asperger syndrome. PloS One. (2017) 12:e0186536. doi: 10.1371/journal.pone.0186536
20. Enea V and Rusu DM. Raising a child with autism spectrum disorder: A systematic review of the literature investigating parenting stress. J Ment Health Res Intellectual Disabil. (2020) 13:283–321. doi: 10.1080/19315864.2020.1822962
21. Javalkar K, Rak E, Phillips A, Haberman C, Ferris M, and Van Tilburg M. Predictors of caregiver burden among mothers of children with chronic conditions. Children. (2017) 4:39. doi: 10.3390/children4050039
22. Baker K and Claridge AM. I have a Ph.D. @ in my daughter”: Mother and Child Experiences of Living with Childhood Chronic Illness. J Child Family Stud. (2023) 32:2625–36. doi: 10.1007/s10826-022-02506-8
23. Nabors L, Liddle M, Graves ML, Kamphaus A, and Elkins J. A family affair: Supporting children with chronic illnesses. Child: Care Health Dev. (2019) 45:227–33. doi: 10.1111/cch.12635
24. Cousino MK and Hazen RA. Parenting stress among caregivers of children with chronic illness: A systematic review. J Pediatr Psychol. (2013) 38:809–28. doi: 10.1093/jpepsy/jst049
25. Gross JJ. Emotion regulation: current status and future prospects. psychol Inq. (2015) 26:1–26. doi: 10.1080/1047840X.2014.940781
26. Campos JJ, Frankel CB, and Camras L. On the nature of emotion regulation. Child Dev. (2004) 75:377–94. doi: 10.1111/j.1467-8624.2004.00681.x
27. Morelen D, Shaffer A, and Suveg C. Maternal emotion regulation: links to emotion parenting and child emotion regulation. J Family Issues. (2016) 37:1891–916. doi: 10.1177/0192513X14546720
28. Zimmer-Gembeck MJ, Rudolph J, Kerin J, and Bohadana-Brown G. Parent emotional regulation: A meta-analytic review of its association with parenting and child adjustment. Int J Behav Dev. (2022) 46:63–82. doi: 10.1177/01650254211051086
29. Hu X, Han ZR, Bai L, and Gao MM. The mediating role of parenting stress in the relations between parental emotion regulation and parenting behaviors in chinese families of children with autism spectrum disorders: A dyadic analysis. J Autism Dev Disord. (2019) 49:3983–98. doi: 10.1007/s10803-019-04103-z
30. Gross JJ and John OP. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. J Pers Soc Psychol. (2003) 85:348–62. doi: 10.1037/0022-3514.85.2.348
31. Clark DA. Cognitive reappraisal. Cogn Behav Pract. (2022) 29:564–6. doi: 10.1016/j.cbpra.2022.02.018
32. Lin G-X, Goldenberg A, Arikan G, Brytek-Matera A, Czepczor-Bernat K, Manrique-Millones D, et al. Reappraisal, social support, and parental burnout. Br J Clin Psychol. (2022) 61:1089–102. doi: 10.1111/bjc.12380
33. van der Veek SMC, Kraaij V, and Garnefski N. Cognitive coping strategies and stress in parents of children with down syndrome: A prospective study. Intellectual Dev Disabil. (2009) 47:295–306. doi: 10.1352/1934-9556-47.4.295
34. Enav Y, Hardan AY, and Gross JJ. Cognitive reappraisal training for parents of children with autism spectrum disorder. Front Psychiatry. (2022) 13:995669. doi: 10.3389/fpsyt.2022.995669
35. Garnefski N and Kraaij V. Cognitive coping and psychological adjustment in different types of stressful life events. Individ Dif Res. (2009) 7.
36. Juszko K and Szczepańska-Gieracha J. Expressive suppression in parents of children with disabilities. Int J Special Educ (IJSE). (2021) 35. doi: 10.52291/ijse.2020.35.5
37. Del Giudice E, Lubrano R, Bramanti SM, Babore A, Trumello C, De Maria SG, et al. Facing pediatric rheumatic diseases: the role of disease activity and parental emotion regulation strategy in parents’ and children’s psychological adjustment. Children. (2023) 10:1863. doi: 10.3390/children10121863
38. Le BM and Impett EA. The costs of suppressing negative emotions and amplifying positive emotions during parental caregiving. Pers Soc Psychol Bull. (2016) 42:323–36. doi: 10.1177/0146167216629122
39. Van Ness CR. Relationship Between the Broad Autism Phenotype, Social Support, Emotion Regulation, and Depression in Parents of Children with Autism. (2022). Available at: https://red.library.usd.edu/diss-thesis/41.
40. Janković SM, Bogavac-Stanojević N, Mikulić I, Izetbegović S, Iličković I, Krajnović D, et al. A questionnaire for rating health-related quality of life. Slovenian J Public Health. (2021) 60:260–8. doi: 10.2478/sjph-2021-0035
41. Vonneilich N, Lüdecke D, and Kofahl C. The impact of care on family and health-related quality of life of parents with chronically ill and disabled children. Disability Rehabil. (2016) 38:761–7. doi: 10.3109/09638288.2015.1060267
42. Eslami Shahrbabaki M, Mazhari S, Haghdoost A-A, and Zamani Z. Anxiety, depression, quality of life and general health of parents of children with autism spectrum disorder. Health Dev J. (2018) 6. doi: 10.22062/jhad.2018.91268
43. Hunfeld JA, Perquin CW, Duivenvoorden HJ, Hazebroek-Kampschreur AA, Passchier J, van Suijlekom-Smit LW, et al. Chronic pain and its impact on quality of life in adolescents and their families. J Pediatr Psychol. (2001) 26:145–53. doi: 10.1093/jpepsy/26.3.145
44. Kuhlthau K, Payakachat N, Delahaye J, Hurson J, Pyne JM, Kovacs E, et al. Quality of life for parents of children with autism spectrum disorders. Res Autism Spectr Disord. (2014) 8:1339–50. doi: 10.1016/j.rasd.2014.07.002
45. Johnson N, Frenn M, Feetham S, and Simpson P. Autism spectrum disorder: Parenting stress, family functioning and health-related quality of life. Families Syst Health. (2011) 29:232–52. doi: 10.1037/a0025341
46. Wiedebusch S, Konrad M, Foppe H, Reichwald-Klugger E, Schaefer F, Schreiber V, et al. Health-related quality of life, psychosocial strains, and coping in parents of children with chronic renal failure. Pediatr Nephrol. (2010) 25:1477–85. doi: 10.1007/s00467-010-1540-z
47. Guðmundsson ÓÓ and Tómasson K. Quality of life and mental health of parents of children with mental health problems. Nordic J Psychiatry. (2002) 56:413–7. doi: 10.1080/08039480260389325
48. Hsiao Y-J. Autism spectrum disorders: family demographics, parental stress, and family quality of life. J Policy Pract Intellectual Disabil. (2018) 15:70–9. doi: 10.1111/jppi.12232
49. Dey M, Castro RP, Haug S, and Schaub MP. Quality of life of parents of mentally-ill children: A systematic review and meta-analysis. Epidemiol Psychiatr Sci. (2019) 28:563–77. doi: 10.1017/S2045796018000409
50. Kheir N, Ghoneim O, Sandridge AL, Al-Ismail M, Hayder S, and Al-Rawi F. Quality of life of caregivers of children with autism in Qatar. Autism. (2012) 16:293–8. doi: 10.1177/1362361311433648
51. Lee GK, Lopata C, Volker MA, Thomeer ML, Nida RE, Toomey JA, et al. Health-related quality of life of parents of children with high-functioning autism spectrum disorders. Focus Autism Other Dev Disabil. (2009) 24:227–39. doi: 10.1177/1088357609347371
52. Haverman L, Van Oers HA, Maurice-Stam H, Kuijpers TW, Grootenhuis MA, and Van Rossum MA. Health related quality of life and parental perceptions of child vulnerability among parents of a child with juvenile idiopathic arthritis: Results from a web-based survey. Pediatr Rheumatol. (2014) 12:34. doi: 10.1186/1546-0096-12-34
53. Mourad G, Alwin J, Jaarsma T, Strömberg A, and Johansson P. The associations between psychological distress and health-related quality of life in patients with non-cardiac chest pain. Health Qual Life Outcomes. (2020) 18:68. doi: 10.1186/s12955-020-01297-0
54. Lovibond PF and Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. (1995) 33:335–43. doi: 10.1016/0005-7967(94)00075-U
55. Maftei A, Bostan C-M, and Zaharia D-V. Hostility and civic moral disengagement: Cognitive reappraisal and expressive suppression as moderators. Journal of Moral Education. (2021) 50(2):202–18. doi: 10.1080/03057240.2019.1691512
56. Hambleton RK and Li S. Translation and Adaptation Issues and Methods for Educational and Psychological Tests. In Hambleton R. K., Merenda P. F., and Spielberger C. D. (Eds.), Adapting educational and psychological tests for cross-cultural assessment (pp. 3–38). Mahwah, NJ: Lawrence Erlbaum Associates (2005).
57. Kim D, Kim BJ, Lee SO, and Cho YS. Best-fit distribution and log-normality for tsunami heights along coastal lines. Stochastic Environmental Research and Risk Assessment. (2014) 28:881–93. doi: 10.1007/s00477-013-0778-y
58. Jones L, Rowe J, and Becker T. Appraisal, coping, and social support as predictors of psychological distress and parenting efficacy in parents of premature infants. Children’s Health Care. (2009) 38:245–62. doi: 10.1080/02739610903235976
Keywords: mothers, distress, children, autism, chronic disease
Citation: Cobzeanu A, Merlici I-A, Ionescu DE and Roca IC (2025) A closer look into maternal psychological distress and the associated factors: the case of autism and chronic conditions. Front. Psychiatry 16:1461040. doi: 10.3389/fpsyt.2025.1461040
Received: 17 August 2024; Accepted: 30 April 2025;
Published: 23 May 2025.
Edited by:
Jonna Bobzien, Old Dominion University, United StatesReviewed by:
Antonio Narzisi, Stella Maris Foundation (IRCCS), ItalyAmelia Díaz, University of Valencia, Spain
Copyright © 2025 Cobzeanu, Merlici, Ionescu and Roca. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alexandra Cobzeanu, YWxleGFuZHJhLm1hZnRlaUB1YWljLnJv
 Alexandra Cobzeanu
Alexandra Cobzeanu Ioan-Alex Merlici
Ioan-Alex Merlici Daria Elena Ionescu
Daria Elena Ionescu Iulia Cristina Roca
Iulia Cristina Roca