- 1Department of Urology, Renmin Hospital, Hubei University of Medicine, Shiyan, Hubei, China
- 2School of Public Health, Ningxia Medical University, Yinchuan, Ningxia, China
Background: Suicidal ideation, a critical public health issue, is notably associated with mental health disorders. Overactive bladder (OAB), a prevalent urological disorder, significantly impacts patients’ quality of life and is associated with mental health problems such as anxiety and depression. This study investigates the association between OAB and suicidal ideation in US adults.
Methods: This population-based cross-sectional study utilized data from six consecutive NHANES datasets (2007-2018). Suicidal ideation was assessed using the ninth item of the Patient Health Questionnaire-9 (PHQ-9), and OAB was identified through a simplified Overactive Bladder Symptom Score (OABSS). Multivariate logistic regression models, Restricted Cubic Splines, and subgroup analyses were used to analyze. The association between OAB and suicidal ideation, adjusting for potential confounders.
Results: Among the 28,085 participants, 3.30% reported suicidal ideation, and 20.39% were identified with OAB. Individuals with suicidal ideation had a significantly higher prevalence of OAB compared to those without suicidal ideation. After adjusting for covariates, each point increase in OABSS was associated with a 15% higher likelihood of suicidal ideation (OR=1.15, 95% CI: 1.10-1.20). Participants with OAB had a 47% increased likelihood of suicidal ideation compared to those without OAB (OR=1.47, 95% CI: 1.26-1.72). Subgroup analysis proved the robustness of the results of this study.
Conclusion: The findings indicate a significant positive association between OAB and suicidal ideation in US adults. These findings underscore the necessity of integrating urological and mental health care to enhance suicide prevention strategies.
1 Background
Suicide is death due to purposeful self-injury, and its incidence varies by factors such as gender and age (1). Globally, more than 700,000 people die by suicide each year. In the United States, more than 16 out of every 100,000 people die by suicide annually (2, 3). These numbers may be underestimated due to incomplete registration of deaths and inaccurate statistics (4). Suicide is not only a personal and family tragedy but also places a heavy burden on community and public health resources (5).
Suicidal ideation, the generation of thoughts about ending one’s life or committing suicide, is a precursor to suicide (6). Studies have shown that there is a strong correlation between suicide and suicidal ideation and that individuals with suicidal ideation face a significantly higher risk of suicide (6, 7). Of those with suicidal ideation, 60% will attempt suicide within a year (7). Suicidal ideation among young Americans increased significantly during the COVID-19 epidemic (8). Therefore, it is critical to explore risk factors for suicidal ideation clinically. One of the primary goals of suicide prevention is to identify at-risk populations (9). Suicidal thoughts are substantially common in individuals in general when mental health issues are present (10). Notably, feelings of sadness and anxiety are among the mental health conditions that overactive bladder illness sufferers are more prone to experience (11, 12). However, it is unclear whether overactive bladder disorder is associated with suicidal ideation. Understanding this relationship is important for effective suicide prevention and intervention.
Overactive bladder (OAB) is a urological disorder characterized by urinary urgency, accompanied by urinary frequency, nocturia, and sometimes urge incontinence, but without pathologic changes such as urinary tract infections (13). The prevalence of OAB is closely related to aging, with a rate exceeding 16% among adults in the United States (14). This disease seriously affects the quality of life of patients and adversely impacts mental health and sleep (15, 16). In addition, OAB imposes a financial burden on patients. As the population ages, this disease also puts increasing pressure on public health (17).
Research has indicated a strong correlation between OAB and interpersonal and psychological aspects. Various causes may trigger OAB and lead to psychological problems, which in turn exacerbate the symptoms of OAB, creating a vicious cycle (18, 19). In the general population, mental health problems are significantly associated with suicidal ideation (10). Therefore, people with OAB may be at risk for mental health risks including suicide (20). However, current studies tend to be limited to women or certain specific populations, which may lead to gender and population bias in the findings, thus reducing their reliability. This is due to gender differences in the urinary system and the different pathophysiologic mechanisms of OAB (21, 22). Therefore, there is a need for a larger population-based study to validate the correlation between OAB and suicidal ideation and to fully detail the interactions between the two. This study was a population-based cross-sectional analysis of U.S. adults aged 20 years and older, based on data from the National Health and Nutrition Examination Survey (NHANES). The investigation of the relationship between OAB and suicidal thoughts was the aim of the study.
2 Materials and methods
2.1 Study population
The National Health and Nutrition Examination Survey (NHANES) is an ongoing project of the National Center for Health Statistics (NCHS) that provides a comprehensive assessment of the health and nutritional status of the U.S. population. NHANES employs a complex stratified sampling methodology to enhance the accuracy and reliability of its representative sample. NHANES collects extensive data on socioeconomic status, demographic characteristics, dietary habits, and health-related information. Trained personnel conduct the data collection to ensure consistency and precision. All NHANES participants sign a written informed consent form, and the survey protocol receives approval from the NCHS Research Ethics Review Board.
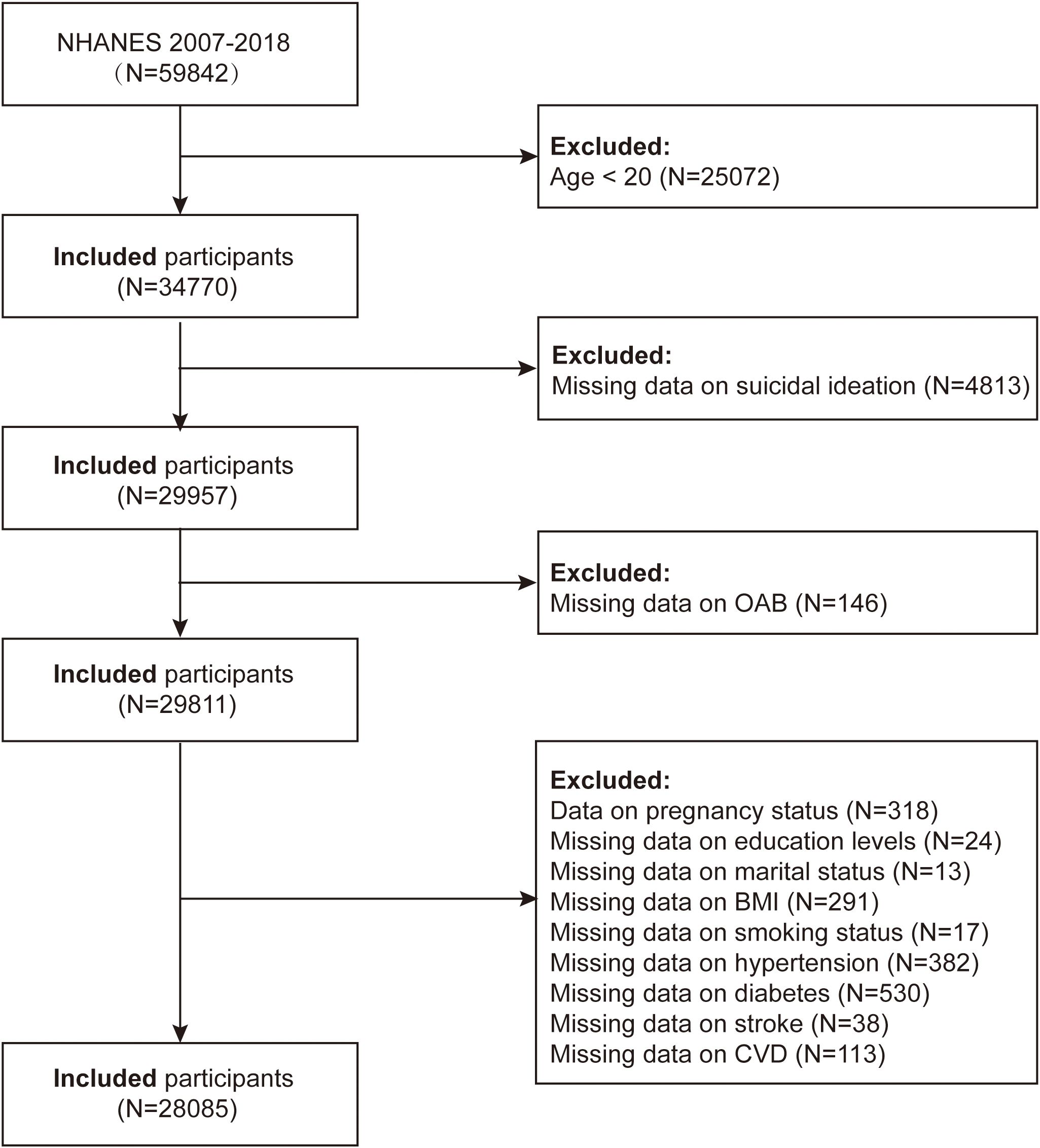
In the present study, we downloaded six consecutive datasets (2007-2008, 2009-2010, 2011-2012, 2013-2014, 2015-2016, and 2017-2018) for an accurate evaluation of the connection between OAB and suicidal ideation, consult the NHANES website. We pooled 12 years of data from NHANES. Of the total sample of 59,842 participants, a total of 31,757 were excluded, including data on age <20 years (n=25,072), missing data on OAB (n=146) and suicidal ideation (n=4,813), pregnancy status (n=318), missing data on education (n=24), marital status (n=13), BMI (n=291), smoking (n=17), hypertension (n=382), diabetes (n=530), stroke (n=38), and cardiovascular disease (n=113). The analysis comprised the remaining 28,085 adult US individuals (Figure 1).
2.2 Definition of suicidal ideation
The ninth item of the Patient Health Questionnaire-9 (PHQ-9) assesses suicidal ideation in the Mental Health Depression Screening section of the survey (23). The PHQ-9 comprises nine items evaluating depressive symptoms experienced over the past two weeks. The ninth item specifically asks, “In the past two weeks, how often have you had thoughts of self-harm or thought it would be better to end your life?” Response options include “Not at all,” “A few days,” “More than half the days,” and “Almost every day.” For this analysis, responses of “Not at all” indicate no suicidal ideation, while all other responses indicate suicidal ideation (24, 25).
2.3 Definition of OAB
The International Continence Society (ICS) defines OAB as a syndrome characterized by urinary urgency in the absence of urinary tract infection or other pathology, often accompanied by urinary frequency, nocturia, and urge urinary incontinence (UUI). OAB diagnosis should be considered in patients presenting with UUI or nocturia, and assessed through specific questions regarding the frequency and urgency of urinary leakage. Nocturia burden was evaluated by asking participants how many times they typically got up to urinate at night over the past 30 days. The simplified OABSS was used to measure the severity of OAB, with a score of ≥3 indicating the presence of the disorder, as detailed in Supplementary Table S1 (26, 27).
2.4 Covariates
In this study, covariates included gender, age, race, education level, marital status, household poverty-to-income ratio (PIR), BMI, smoking status, alcohol use, diabetes, hypertension, cardiovascular disease (CVD), and stroke. Individuals in the survey who had smoked at least 100 cigarettes in their lifetime and were smoking at the time of the questionnaire were designated as smokers. Participants who drank at least 12 alcoholic beverages in any year were designated as alcohol drinkers (28, 29). Participants were considered to have diabetes if their physician told them they had diabetes or if their fasting blood glucose was ≥126 mg/dL.
2.5 Statistical analysis
All statistical analyses followed the data analysis guidelines provided by NHANES, using appropriate NHANES weights for complex multi-stage cluster sampling designs. The Kolmogorov-Smirnov test was used to check the assumption of normal distribution for each variable. Normally distributed continuous variables were expressed as mean and standard deviation (SD), while non-normally distributed variables were expressed as median and interquartile range (IQR). Categorical variables were expressed as frequency and percentage (%). The study population was categorized into two groups based on the presence or absence of suicidal ideation. The chi-square test, t-test, and Mann–Whitney U test were used to compare the distribution of baseline characteristics between groups.
We used weighted logistic regression to explore the correlation between OAB scores and suicidal ideation. We constructed three logistic regression models. Three statistical models were employed: Model 1 remained unadjusted, Model 2 was adjusted for age, gender, and race, and Model 3 incorporated additional adjustments for education level, marital status, BMI, PIR, smoking, alcohol consumption, diabetes, hypertension, cardiovascular disease, and stroke, along with the covariates in Model 2. We then tested for nonlinear associations between Overactive Bladder Symptom Score (OABSS) and suicidal ideation using restricted cubic spline (RCS) after adjusting for covariates. Finally, subgroup analyses and interaction tests were conducted on the potential confounders listed in the baseline table to explore potential changes in associations between subgroups. Statistical analyses were conducted using R (version 4.3.2), with the significance level set at P < 0.05.
3 Results
3.1 Basic characteristics of the study population
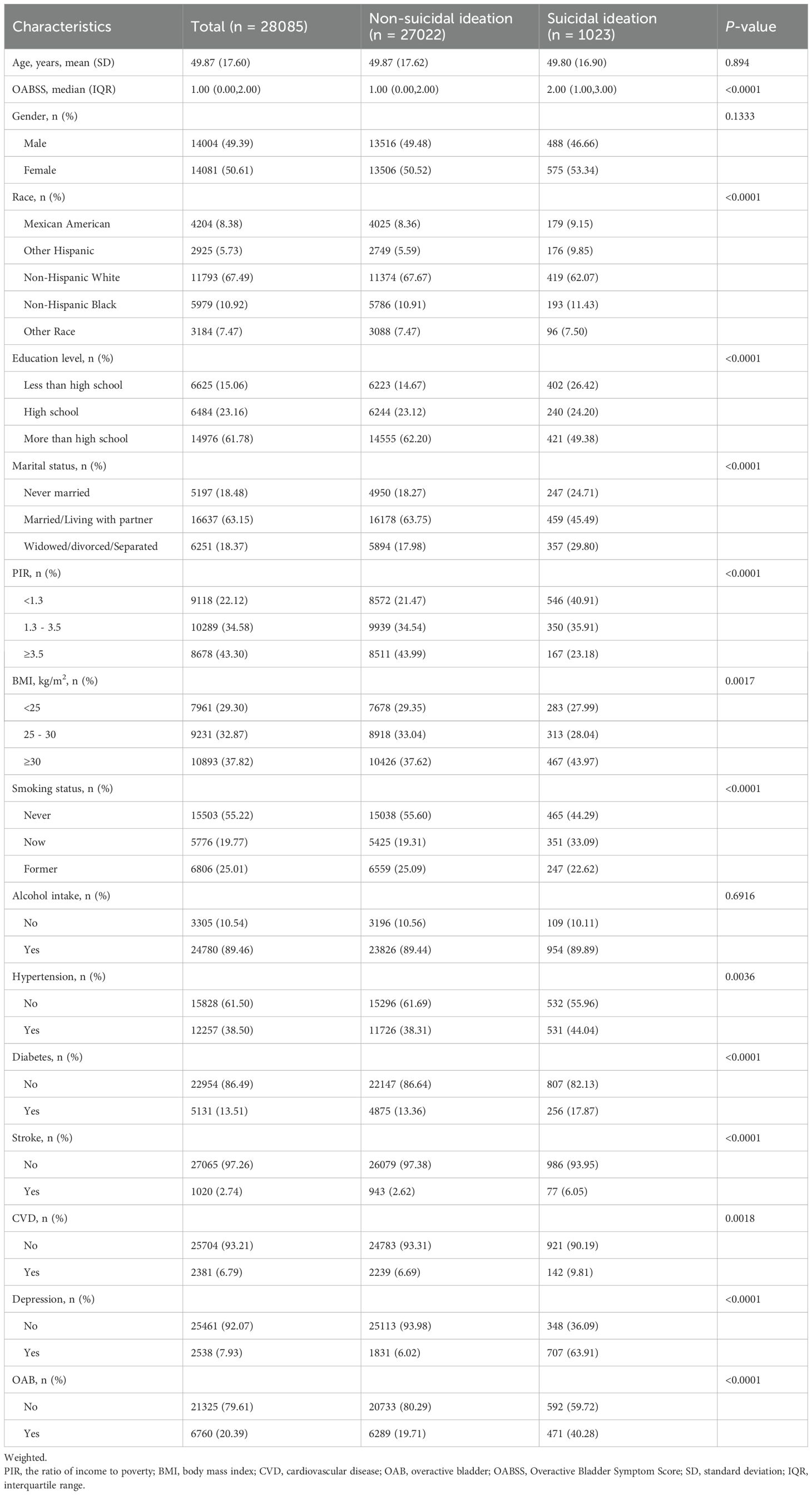
This research comprised 28,085 individuals in total. with 3.30% reporting suicidal ideation. Participants with suicidal ideation were more likely to have OAB (40.28%) and higher OABSS scores compared to those without suicidal ideation (19.71%). The suicidal ideation group was characterized by a higher prevalence of cohabitation with a spouse, high education level, lower PIR level, BMI ≥ 30, hypertension, diabetes, coronary heart disease, stroke, and depression, with significant differences between the groups (P < 0.01) (Table 1).
3.2 Association between overactive bladder and suicidal ideation.
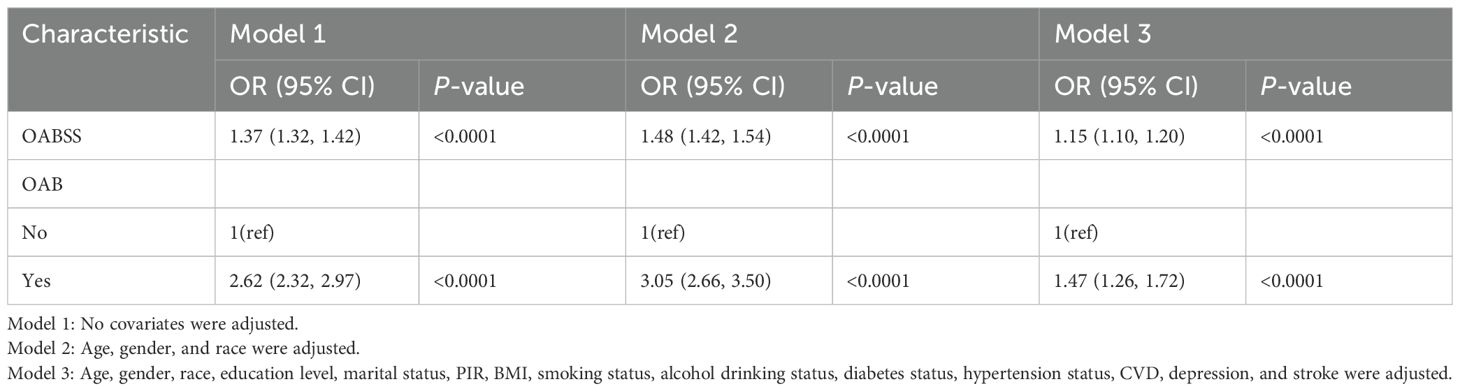
Table 2 shows the multivariate logistic regression analysis between overactive bladder syndrome and suicidal ideation, which revealed a positive association between OABSS and suicidal ideation. In Model 3, each point increase in OABSS increased the likelihood of participants’ suicidal ideation by 15% (OR = 1.15, 95% CI: 1.10, 1.20). We defined OABSS ≥ 3 points as OAB. Participants with OAB had a 47% increased likelihood of suicidal ideation compared to non-OAB participants (OR = 1.47, 95% CI: 1.26, 1.27) (Table 2). Additionally, restricted cubic spline analysis showed no nonlinear association between the Overactive Bladder Symptom Score and suicidal ideation (P for nonlinear = 0.588) (Figure 2).
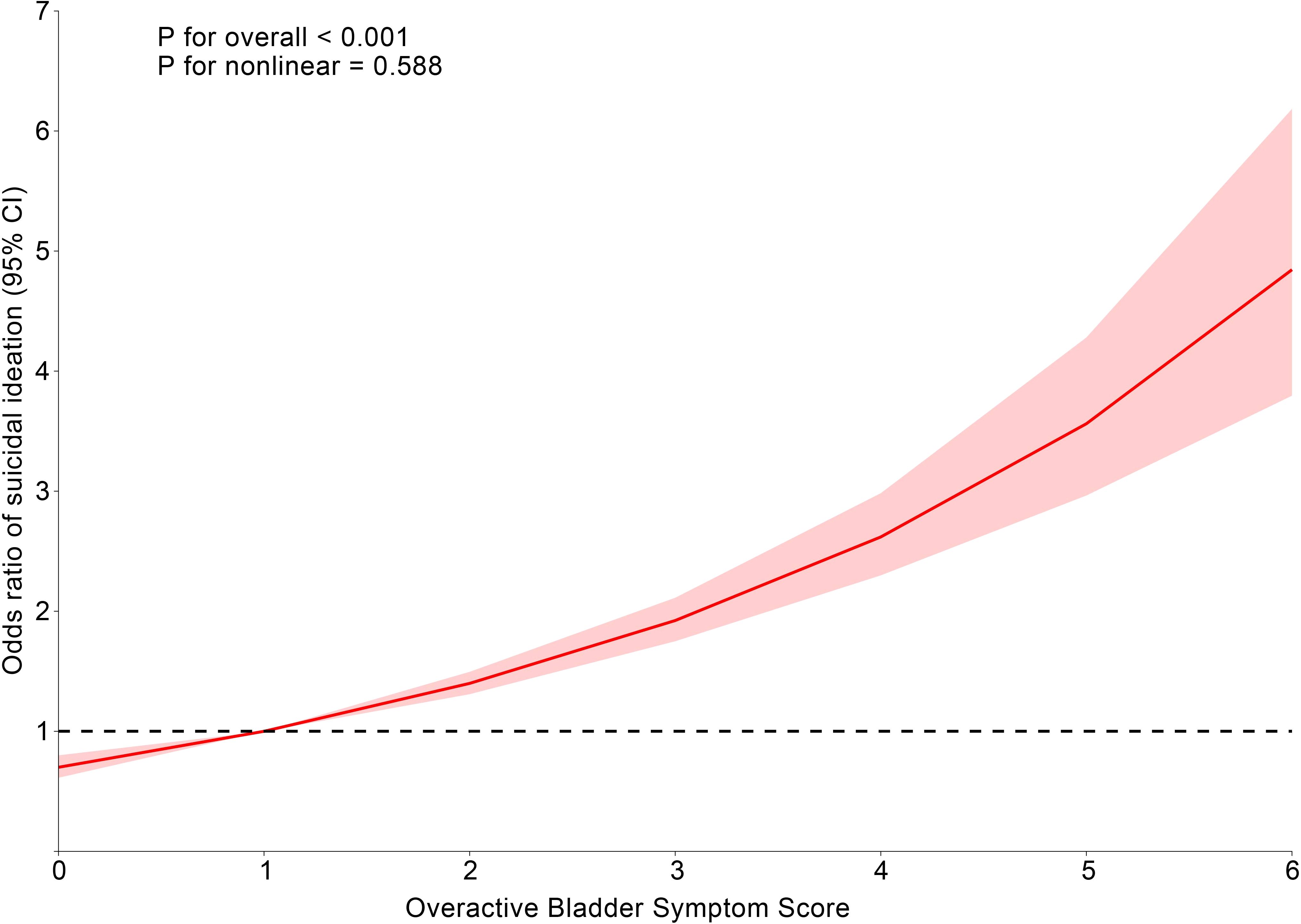
Figure 2. Dose-effect relationship between overactive bladder symptom score and suicidal ideation. Age, gender, race, education level, marital status, PIR, BMI, smoking status, alcohol drinking status, diabetes status, hypertension status, CVD, depression, and stroke were adjusted.
3.3 Subgroup analysis
As shown in Figure 3, there was a positive correlation between OAB and suicidal ideation in all subgroups, and this positive correlation was not significantly different across subgroups (p for interaction > 0.05). In the gender subgroup, there was a trend of increasing suicidal ideation in both males [OR = 2.94 (95% CI: 2.13, 4.05), p < 0.001] and females [OR = 2.39 (95% CI: 1.92, 2.98), p < 0.001]. There was a trend of increasing suicidal ideation in both the 20–50 age group [OR = 2.86 (95% CI: 2.17, 3.75), p < 0.001] and the >50 age group [OR = 2.24 (95% CI: 1.75, 2.88), p < 0.001] (Figure 3).
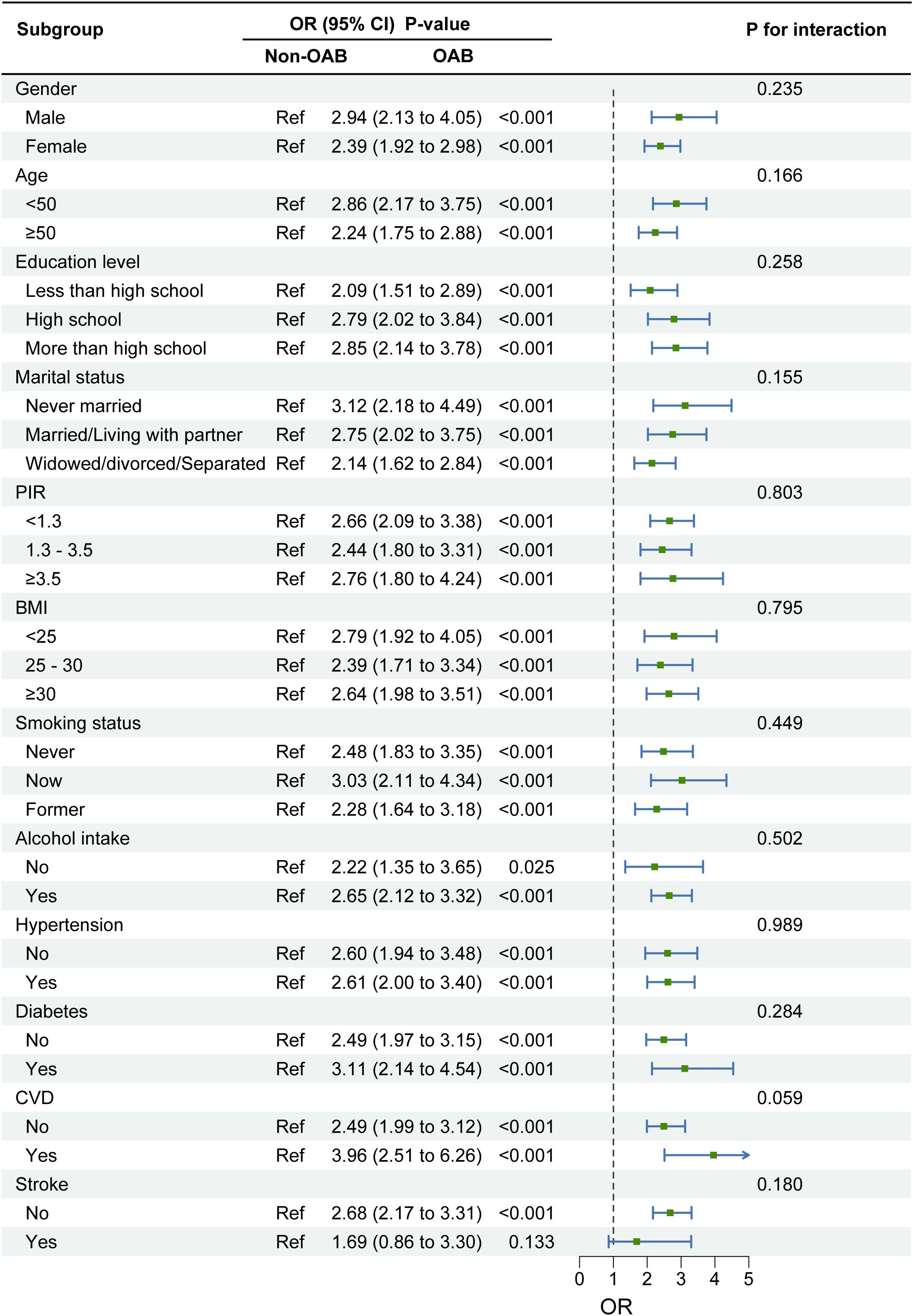
Figure 3. Subgroup analysis of the association between overactive bladder syndrome and suicidal ideation. Note 1: The above model adjusted for gender, age, race, education level, marital status, PIR, BMI, smoking status, alcohol drinking status, diabetes status, hypertension status, CVD, depression, and stroke. Note 2: In each case, the model is not adjusted for the stratification variable.
4 Discussion
Using NHANES data, the present research investigated the link between suicidal thoughts and overactive bladder (OAB), offering fresh perspectives on the connection between urologic conditions and psychological conditions. The findings indicated that in contrast to people without OAB, those with OAB had a greater incidence of suicidal thoughts, demonstrating the potential impact of OAB on mental health. The robustness of these findings highlights several key points. First, psychiatrists should focus on the impact of urinary symptoms on suicide risk to improve treatment adherence and effectiveness. A comprehensive approach that integrates both urological symptom management and psychological evaluation is essential when treating patients with OAB. Addressing mental health issues such as anxiety, depression, and suicidal ideation may improve treatment adherence, quality of life, and overall prognosis. Therefore, while routine psychological evaluation may not be necessary for all patients with OAB, it is advisable to consider mental health screening in individuals presenting with severe urinary symptoms, low treatment compliance, or signs of psychological distress.
Previous research has concentrated on the relationship between OAB and depression, frequently using samples from hospitals or particular groups of women (30, 31). These studies compared psychological conditions between two groups by dividing the population into case and control groups but were slightly less persuasive due to the limitations of the research methodology. Nonetheless, studies agree that OAB has a strong correlation with the development of depression (32). First, according to a study of a community-based population assessed using a depression scale, a significant correlation was found between depressive symptoms and OAB, suggesting that an elevated risk factor for incontinence in the urine was depressed symptoms (33). Second, Debra et al. demonstrated in their study that there is a significant association between OAB and the development of depressive symptoms (34). Third, one large population-based study found that the risk of developing depression increased as the severity of OAB increased (35). However, this study was conducted via a web-based survey and disregarded the significance of in-person interviews with doctors, and did not control for covariates. In contrast, the present study analyzed data for U.S. adults, effectively controlled for covariates, and improved the credibility and feasibility of the findings.
The relationship between overactive bladder (OAB) and mental health is likely bidirectional. On one hand, psychological distress may contribute to altered bladder function, and on the other, the burden of OAB symptoms may lead to mental health deterioration. Preclinical studies have shown that psychological stress may affect bladder contractility through pathways such as the Rho-kinase (ROCK) signaling cascade, leading to increased voiding frequency and detrusor overactivity. Stress-induced alterations in gut microbiota have also been hypothesized to influence bladder function. Additionally, anxiety and depression may contribute to heightened somatic sensitivity and lower perception thresholds, possibly exacerbating OAB symptoms (20, 36). Conversely, the social and emotional impact of OAB—such as embarrassment, sleep disturbances, reduced work productivity, and social withdrawal—may predispose individuals to depressive symptoms and suicidal ideation (19, 37, 38).
However, it is important to clarify that we do not advocate for psychology as the primary treatment for OAB or as a replacement for conventional urological interventions. OAB is primarily a bladder dysfunction, and treatment should remain focused on behavioral therapies, pharmacological interventions, and, when necessary, surgical options. However, mental health issues, particularly anxiety and depression, may exacerbate OAB symptoms and negatively impact treatment adherence and quality of life. Therefore, while the primary focus of OAB treatment should remain within the urological domain, we suggest that for individuals with significant emotional distress, poor treatment compliance, or reduced quality of life, considering integrated psychological support may improve overall health outcomes and treatment effectiveness.
5 Strengths and limitations
This study has several noteworthy strengths. First, it evaluated a large sample of 28,085 participants, each of whom provided comprehensive clinically informative data. The data collection underwent a rigorous quality assurance process to ensure its reliability. Second, the study conducted subgroup analyses based on common co-morbidities. Subgroup and sensitivity analyses were also carried out to strengthen the reliability of the findings. This thorough examination emphasizes how crucial it is for psychiatrists to concentrate on patients’ symptoms connected to the urinary system.
Although NHANES provides a large, nationally representative sample with standardized data collection procedures, it has several limitations that must be acknowledged. First, it is a cross-sectional survey, which limits the ability to infer temporal or causal relationships between OAB and suicidal ideation. Second, the assessment of both OAB and suicidal ideation is based on self-report questionnaires rather than clinical diagnosis, which may lead to misclassification or underreporting. Third, the data lack granularity on the duration, severity, or context of symptoms, which could influence interpretation. Fourth, although we defined OAB as an OABSS ≥3 in accordance with prior NHANES-based literature, this threshold may inadvertently include individuals whose urinary symptoms stem from other causes, such as nocturnal polyuria, sleep apnea, metabolic or behavioral factors, or anatomical abnormalities. Fifth, relying solely on an OABSS ≥3 cutoff to define OAB may lead to misclassification. Future studies should consider incorporating more nuanced symptom-based subtyping and physiological markers to improve the accuracy and clinical utility of OAB phenotyping. Sixth, while NHANES utilizes a multi-stage, stratified probability sampling method to ensure national representativeness, certain subpopulations (e.g., individuals with severe OAB or hospitalized patients) may not be adequately represented. This could limit the generalizability of findings to these specific groups. Additionally, the reliance on self-reported OAB symptoms may not fully capture the clinical complexity or underlying physiology of OAB, thus affecting the precision of the data in elucidating OAB’s impact. These limitations warrant caution when extrapolating our findings to clinical settings or guiding intervention strategies.
6 Conclusion
This study reveals a positive association between OAB and suicidal ideation in U.S. adults, emphasizing the need for an integrated clinical approach to address both urinary and mental health symptoms to enhance suicide prevention efforts.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by The portions of this study involving human participants, human materials, or human data were conducted in accordance with the Declaration of Helsinki and were approved by the National Center for Health Statistics (NCHS) Ethics Review Board. The patients/participants provided their written informed consent to participate in this study. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
HL: Conceptualization, Resources, Validation, Writing – original draft, Writing – review & editing. DH: Data curation, Visualization, Writing – original draft, Writing – review & editing. MJ: Formal Analysis, Writing – review & editing, Funding acquisition, Investigation. YZ: Methodology, Writing – review & editing. HH: Writing – review & editing, Project administration, Resources. YY: Software, Writing – original draft. HJ: Supervision, Writing – original draft, Writing – review & editing. JL: Formal Analysis, Funding acquisition, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We would like to thank all participants in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1483684/full#supplementary-material
Abbreviations
NHANES, National Health and Nutrition Examination Survey; NCHS, National Center for Health Statistics; PIR, income to poverty ratio; CVD, cardiovascular disease; BMI, body mass index; PHQ-9, Patient Health Questionnaire-9; OAB, Overactive bladder; OABSS, Overactive Bladder Symptom Score; UUI, urinary incontinence; SD, standard deviation; IQR, interquartile range; RCS, restricted cubic spline.
References
1. Qing G, Deng W, Zhou Y, Zheng L, Wang Y, and Wei B. The association between non-high-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio (NHHR) and suicidal ideation in adults: a population-based study in the United States. Lipids Health Dis. (2024) 23:17. doi: 10.1186/s12944-024-02012-4
2. Huang D, Zhong S, Yan H, Lai S, Lam M, and Jia Y. Association between serum zinc levels and suicidal ideation in US adults: A population-based cross-sectional study. J Affect Disord. (2023) 329:359–68. doi: 10.1016/j.jad.2023.02.039
3. Liang JH, Ge WX, Jin ZG, Wang C, Liu ML, Pu YQ, et al. Zhang YS et al: Sexual orientation disparities in the prevalence of suicidal ideation among U.S adults aged 20 to 59 years: Results from NHANES 2005-2016. Psychiatry Res. (2024) 331:115639. doi: 10.1016/j.psychres.2023.115639
4. Wang P, Wang Y, and Jia X. Association between fecal incontinence and suicidal ideation in adult Americans: Evidence from NHANES 2005-2010. J psychosomatic Res. (2023) 170:111377. doi: 10.1016/j.jpsychores.2023.111377
5. Daurio AM, Ennis CR, Duffy ME, and Taylor J. A comparative study of suicidal and nonsuicidal self-injury characteristics in heterosexual versus sexual minority females. Psychiatry Res. (2022) 309:114421. doi: 10.1016/j.psychres.2022.114421
6. Hubers AAM, Moaddine S, Peersmann SHM, Stijnen T, van Duijn E, van der Mast RC, et al. Suicidal ideation and subsequent completed suicide in both psychiatric and non-psychiatric populations: a meta-analysis. Epidemiol Psychiatr Sci. (2018) 27:186–98. doi: 10.1017/s2045796016001049
7. Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, et al. Gluzman S et al: Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J psychiatry: J Ment Sci. (2008) 192:98–105. doi: 10.1192/bjp.bp.107.040113
8. Bersia M, Koumantakis E, Berchialla P, Charrier L, Ricotti A, Grimaldi P, et al. Suicide spectrum among young people during the COVID-19 pandemic: A systematic review and meta-analysis. EClinicalMedicine. (2022) 54:101705. doi: 10.1016/j.eclinm.2022.101705
9. Hawton K and van Heeringen K. Suicide. Lancet (London England). (2009) 373:1372–81. doi: 10.1016/s0140-6736(09)60372-x
10. Lawrence HR, Balkind EG, Ji JL, Burke TA, and Liu RT. Mental imagery of suicide and non-suicidal self-injury: A meta-analysis and systematic review. Clin Psychol Rev. (2023) 103:102302. doi: 10.1016/j.cpr.2023.102302
11. Zhang Y, Wu X, Liu G, Feng X, Jiang H, and Zhang X. Association between overactive bladder and depression in American adults: A cross-sectional study from NHANES 2005-2018. J Affect Disord. (2024) 356:545–53. doi: 10.1016/j.jad.2024.04.030
12. Vrijens D, Drossaerts J, van Koeveringe G, Van Kerrebroeck P, van Os J, and Leue C. Affective symptoms and the overactive bladder - a systematic review. J psychosomatic Res. (2015) 78:95–108. doi: 10.1016/j.jpsychores.2014.11.019
13. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. (2003) 61:37–49. doi: 10.1016/s0090-4295(02)02243-4
14. Wei B, Zhao Y, Lin P, Qiu W, Wang S, Gu C, et al. The association between overactive bladder and systemic immunity-inflammation index: a cross-sectional study of NHANES 2005 to 2018. Sci Rep. (2024) 14:12579. doi: 10.1038/s41598-024-63448-3
15. Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. (2003) 20:327–36. doi: 10.1007/s00345-002-0301-4
16. Kinsey D, Pretorius S, Glover L, and Alexander T. The psychological impact of overactive bladder: A systematic review. J Health Psychol. (2016) 21:69–81. doi: 10.1177/1359105314522084
17. Reynolds WS, Fowke J, and Dmochowski R. The burden of overactive bladder on US public health. Curr bladder dysfunction Rep. (2016) 11:8–13. doi: 10.1007/s11884-016-0344-9
18. Jin Z, Zhang Q, Yu Y, Zhang R, Ding G, Li T, et al. Progress in overactive bladder: novel avenues from psychology to clinical opinions. PeerJ. (2023) 11:e16112. doi: 10.7717/peerj.16112
19. Sexton CC, Coyne KS, Thompson C, Bavendam T, Chen CI, and Markland A. Prevalence and effect on health-related quality of life of overactive bladder in older americans: results from the epidemiology of lower urinary tract symptoms study. J Am Geriatrics Soc. (2011) 59:1465–70. doi: 10.1111/j.1532-5415.2011.03492.x
20. Zhang X, Ma L, Li J, Zhang W, Xie Y, and Wang Y. Mental health and lower urinary tract symptoms: Results from the NHANES and Mendelian randomization study. J psychosomatic Res. (2024) 178:111599. doi: 10.1016/j.jpsychores.2024.111599
21. Bradley CS, Nygaard IE, Hillis SL, Torner JC, and Sadler AG. Longitudinal associations between mental health conditions and overactive bladder in women veterans. Am J obstetrics gynecology. (2017) 217:430. doi: 10.1016/j.ajog.2017.06.016
22. Buford K, Jivanji D, and Polland A. Microhematuria in women presenting for overactive bladder. Curr Urol Rep. (2023) 24:25–32. doi: 10.1007/s11934-022-01128-3
23. Kroenke K, Spitzer RL, and Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Internal Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
24. Han KM, Ko YH, Shin C, Lee JH, Choi J, Kwon DY, et al. Tinnitus, depression, and suicidal ideation in adults: A nationally representative general population sample. J Psychiatr Res. (2018) 98:124–32. doi: 10.1016/j.jpsychires.2018.01.003
25. Tan MY, Wu S, Zhu SX, and Jiang LH. Association between exposure to organophosphorus pesticide and suicidal ideation among U.S. adults: A population-based study. Ecotoxicology Environ Saf. (2024) 281:116572. doi: 10.1016/j.ecoenv.2024.116572
26. Zhu S, Wang Z, Tao Z, Wang S, and Wang Z. Relationship between marijuana use and overactive bladder (OAB): A cross-sectional research of NHANES 2005 to 2018. Am J Med. (2023) 136:72–8. doi: 10.1016/j.amjmed.2022.08.031
27. Tang F, Zhang J, Huang R, Zhou H, Yan T, Tang Z, et al. The association between wet overactive bladder and consumption of tea, coffee, and caffeine: Results from 2005–2018 National Health and Nutrition Examination Survey. Clin Nutr (Edinburgh Scotland). (2024) 43:1261–9. doi: 10.1016/j.clnu.2024.03.027
28. Lv J, Xu T, Lou S, Zhan Z, Cheng Z, and Fu F. Association between serum β-carotene and suicidal ideation in adults: a cross-sectional study. Front Nutr. (2024) 11:1500107. doi: 10.3389/fnut.2024.1500107
29. Huang H, Fu J, Lu K, Fu Y, Zhuge P, and Yao Y. Association between dietary fiber intake and suicidal ideation: a cross-sectional survey. Front Nutr. (2024) 11:1465736. doi: 10.3389/fnut.2024.1465736
30. Bradley CS, Nygaard IE, Torner JC, Hillis SL, Johnson S, and Sadler AG. Overactive bladder and mental health symptoms in recently deployed female veterans. J Urol. (2014) 191:1327–32. doi: 10.1016/j.juro.2013.11.100
31. Lai HH, Rawal A, Shen B, and Vetter J. The relationship between anxiety and overactive bladder or urinary incontinence symptoms in the clinical population. Urology. (2016) 98:50–7. doi: 10.1016/j.urology.2016.07.013
32. Lai H, Gardner V, Vetter J, and Andriole GL. Correlation between psychological stress levels and the severity of overactive bladder symptoms. BMC Urol. (2015) 15:14. doi: 10.1186/s12894-015-0009-6
33. Ikeda Y, Nakagawa H, Ohmori-Matsuda K, Hozawa A, Masamune Y, Nishino Y, et al. Risk factors for overactive bladder in the elderly population: a community-based study with face-to-face interview. Int J urology: Off J Japanese Urological Assoc. (2011) 18:212–8. doi: 10.1111/j.1442-2042.2010.02696.x
34. Irwin DE, Milsom I, Kopp Z, Abrams P, Artibani W, and Herschorn S. Prevalence, severity, and symptom bother of lower urinary tract symptoms among men in the EPIC study: impact of overactive bladder. Eur Urol. (2009) 56:14–20. doi: 10.1016/j.eururo.2009.02.026
35. Lee KS, Yoo TK, Liao L, Wang J, Chuang YC, Liu SP, et al. Association of lower urinary tract symptoms and OAB severity with quality of life and mental health in China, Taiwan and South Korea: results from a cross-sectional, population-based study. BMC Urol. (2017) 17:108. doi: 10.1186/s12894-017-0294-3
36. Mills KA, West EG, Sellers DJ, Chess-Williams R, and McDermott C. Psychological stress induced bladder overactivity in female mice is associated with enhanced afferent nerve activity. Sci Rep. (2021) 11:17508. doi: 10.1038/s41598-021-97053-5
37. Coyne KS, Sexton CC, Irwin DE, Kopp ZS, Kelleher CJ, and Milsom I. The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: results from the EPIC study. BJU Int. (2008) 101:1388–95. doi: 10.1111/j.1464-410X.2008.07601.x
Keywords: overactive bladder, suicidal ideation, NHANES, OAB, population-based study
Citation: Liu H, Dong H, Jin M, Zhou Y, Hao H, Yuan Y, Jia H and Li J (2025) Association between overactive bladder and suicidal ideation in US adults: a population-based study. Front. Psychiatry 16:1483684. doi: 10.3389/fpsyt.2025.1483684
Received: 20 August 2024; Accepted: 19 May 2025;
Published: 09 June 2025.
Edited by:
Yicheng Long, Central South University, ChinaReviewed by:
Jens Djurhuus, Aarhus University, DenmarkSteve Fisher, University of Texas Medical Branch at Galveston, United States
Copyright © 2025 Liu, Dong, Jin, Zhou, Hao, Yuan, Jia and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongtao Jia, NTM5OTcyODkwQHFxLmNvbQ==; Junyong Li, MTg3NzI5NDYwMTJAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Heng Liu
Heng Liu Huqiang Dong2†
Huqiang Dong2† Mingchu Jin
Mingchu Jin