- 1Department of Psychiatry, University of Alberta, Edmonton, AB, Canada
- 2Department of Psychiatry, Dalhousie University, Halifax, NS, Canada
- 3School of Nursing, University of British Columbia, Okanagan, BC, Canada
- 4Alberta Health Services, Addiction and Mental Health Services, Edmonton, AB, Canada
- 5School of Public Health, University of Alberta, Edmonton, AB, Canada
- 6Department of Psychiatry, Cumming School of Medicine, University of Calgary, Calgary, AB, Canada
Introduction: Patients with mental health challenges often see the transition from hospital to community as a test of resilience and a potential threat to recovery. Many question their ability to cope with everyday challenges. This paper examines how demographic and clinical factors predict resilience, personal recovery, and quality of life.
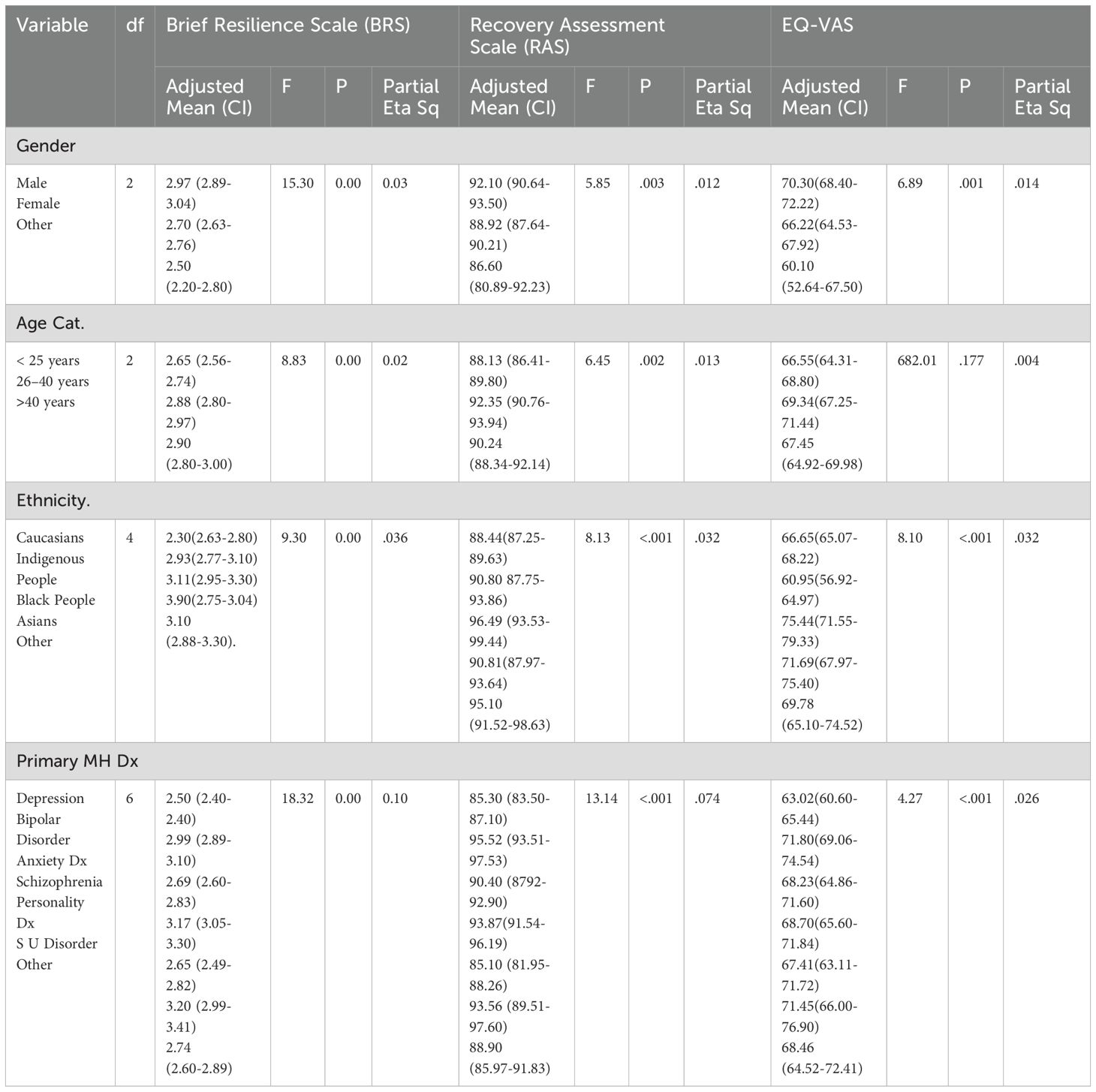
Methods: Data were collected from psychiatric inpatients before discharge using REDCap, an online survey platform. Resilience, recovery, and quality of life were assessed with the Brief Resilience Scale (BRS), Recovery Assessment Scale (RAS), and EQ-Visual Analogue Scale (EQ-VAS). ANCOVA was used to compare group relationships. Demographic and clinical variables such as age, gender, ethnicity, and mental health diagnosis were independent variables.
Results: Males had significantly higher resilience scores than females (Mdiff = 0.270, p<.001) and others (Mdiff = 0.470, p<.001). Self-identified Black individuals had higher quality of life scores than Caucasians (Mdiff = 8.79, p<.001) and Indigenous individuals (Mdiff = 14.50, p<.001). Participants with depression had significantly lower recovery scores compared to those with bipolar disorder (Mdiff = -10.25, p<.001), schizophrenia (Mdiff = -8.60, p<.001), and substance use disorder (Mdiff = -8.30, p<.005).
Conclusion: Results suggest that women, younger adults, Indigenous peoples, and individuals with depression struggle more with adapting to post-discharge life. Policymakers should implement programs that focus on supporting resilience in these vulnerable groups.
1 Introduction
Transitions from inpatient mental healthcare to community care can be especially challenging for individuals with mental health issues, with these challenges typically categorized into personal and systemic factors (1, 2). These transitions can be perceived as tests of resilience, threatening recovery and causing anxiety about daily life challenges (3). As a result, some inpatients may relapse even before discharge (4). Addressing these concerns, such as housing, job security, and income, is essential for a successful transition (5). Systemic challenges include the risk of readmission, availability of continuity of care, suicide risks, medication management, and poor communication with community structures (6, 7). Additionally, discharge processes may be delayed due to issues such as securing community support, funding, and family factors (4). Building resilience during discharge planning can mitigate these challenges, improving post-discharge recovery outcomes (8), thereby enhancing quality of lives of patients in the community.
The theoretical framework of this paper as illustrated in (Figure 1) emphasizes the connection between resilience, personal recovery, and quality of life, all influenced by demographic and clinical factors (9, 10). Understanding these factors allows healthcare professionals to tailor interventions to improve recovery outcomes. This framework acknowledges how both individual and systemic factors affect resilience and overall recovery (11, 12). Resilience, defined as the ability to adapt to adversity, is critical in mental health recovery. Research suggests resilience is a protective factor against depression and other mental disorders, fostering the ability to cope with stress (8, 13). Personal recovery, in contrast to symptom remission, emphasizes social inclusion, self-determination, and hope (14). It is a process of finding meaning in life beyond mental illness and trauma, focusing on personal goals and aspirations (14–16). Personal recovery differs from clinical recovery, as it centers on empowerment, hope, and self-directed goals (16, 17). Quality of life is perceived satisfaction in mental, physical, and social domains, which is shaped by individual goals and societal values (18).
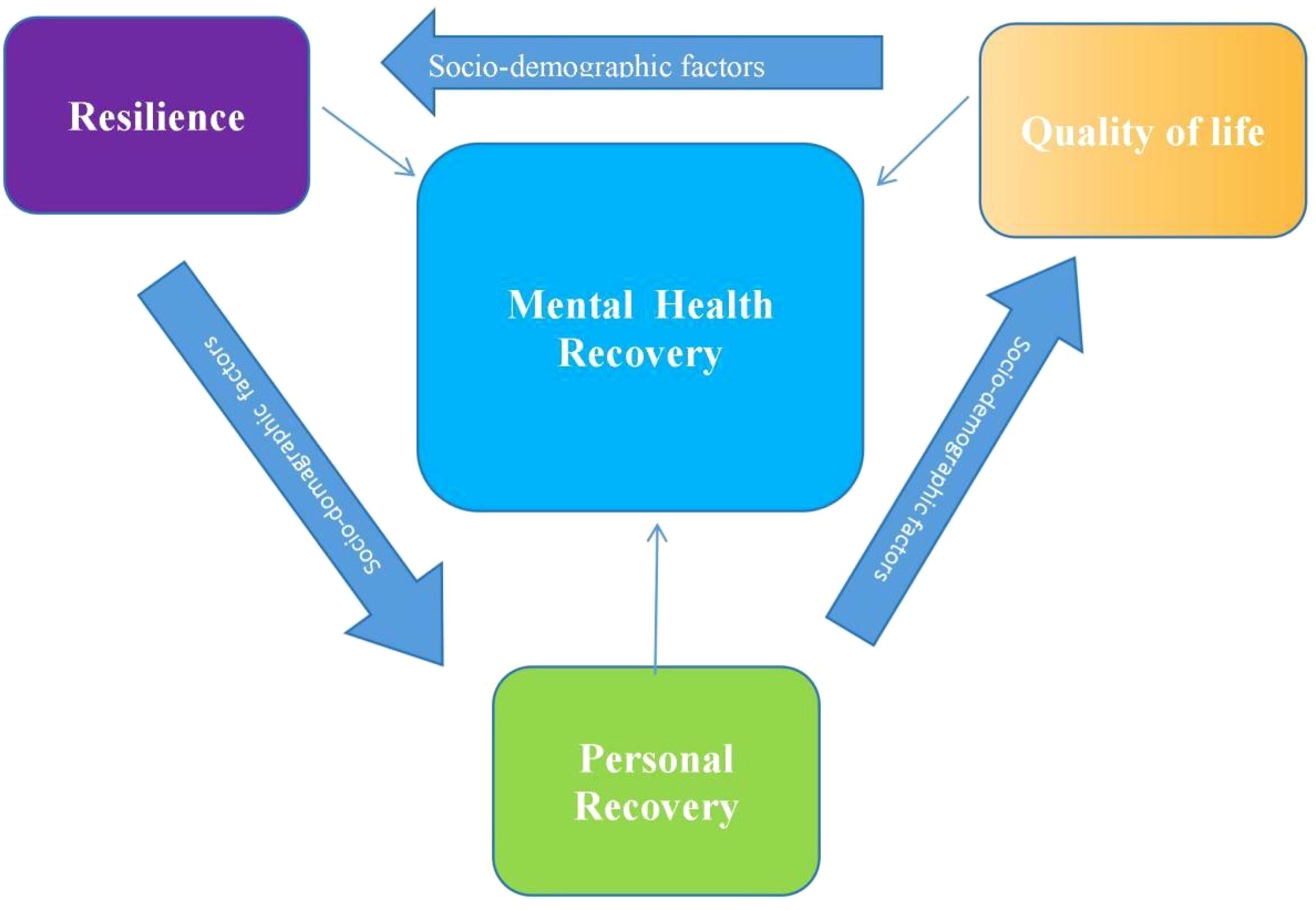
Figure 1. Illustration of the main conceptual framework for resilience, personal recovery, and quality of life as core contructs of mental health recovery.
Research has shown resilience positively impacts recovery outcomes (19, 20), with resilient individuals managing mental health challenges better, adapting to stress, and having a higher perceived quality of life (21, 22). Personal recovery, focusing on self-empowerment, also enhances resilience and quality of life (23, 24). Positive psychiatry, which integrates resilience, coping skills, and social engagement, supports the idea that resilience helps individuals find meaning and adapt after mental illness (25, 26).
In Alberta, Canada, Alberta Health Services (AHS) emphasizes the importance of stable living conditions for recovery, with housing insecurity potentially hindering recovery progress (26). Programs like “My Recovery Plan” (MRP) focus on resilience-building and meaning in life, which can improve quality of life and reduce readmissions (26, 27). Research indicates that uncoordinated discharge planning leads to higher readmission rates, as individuals may feel unsupported (28, 29). For example, Alberta’s long wait times for mental health services contribute to feelings of neglect and may lead to relapse and readmission (30).
Sociodemographic factors, such as gender, age, and ethnicity, influence resilience, recovery, and quality of life (31, 32) Gender roles impact how individuals cope with mental health challenges, with studies suggesting that women are more likely to seek social support, potentially giving them a resilience advantage (33, 34). Age also plays a role in resilience, with younger individuals facing challenges related to emerging adulthood, while older individuals may contend with physical health issues, which can affect recovery (35, 36). Mental health diagnosis significantly impacts recovery trajectories, with conditions like depression, anxiety, schizophrenia, and bipolar disorder presenting unique challenges (30, 37). Research suggests that males may have higher resilience and recovery scores than females, and that individuals over 65 tend to be more resilient than younger individuals (38, 39). Ethnic disparities also influence recovery, with Caucasians generally experiencing higher resilience and recovery compared to Black, Asian, and Indigenous individuals due to systemic barriers and discrimination (40, 41).
Research on resilience factors in mental health disorders has highlighted that conditions such as anxiety, depression, and schizophrenia are affected by individual resilience levels (42, 43). Resilience factors, like perceived ability to cope with life stressors, help individuals thrive and find meaning in their experiences (44, 45). Healthcare workers’ understanding of vulnerability and resilience factors can improve interventions and support for individuals transitioning to community care (8, 29). Ongoing research into these factors is vital for developing evidence-based practices that foster recovery.
In mental health diagnoses, depression often correlates with lower resilience and poorer recovery outcomes compared to conditions like schizophrenia or bipolar disorder (46, 47). Patients with depression may face more challenges in recovery due to the nature of their condition, which affects their ability to adapt and recover post-discharge (48, 49).
There remain gaps in the literature about how gender, age, ethnicity, and clinical diagnosis impact resilience, recovery, and quality of life after discharge. Understanding the complex factors that influence resilience, personal recovery, and quality of life is crucial for improving outcomes for individuals transitioning from inpatient psychiatric care to community care.
To address gaps in the literature, this study seeks to assess resilience, personal recovery, and quality of life levels using the Brief Resilience Scale (BRS), Recovery Assessment Scale (RAS), and EQ-VAS respectively (13, 50, 51). The study seeks to explore the relationship between sociodemographic and clinical characteristics and how they impact resilience, personal recovery, and quality of life of patients who are ready to be discharged from inpatient psychiatric units in Alberta.
2 Methodology
2.1 Study setting and design
This study was conducted in Alberta, Canada, with a population of 4.7 million (52). In 2018, there were 28,571 adult discharges from psychiatric inpatient units across Alberta (4, 28). Participants were recruited from ten acute mental health units across Edmonton, Calgary, and Grand Prairie using a pragmatic stepped-wedge cluster-randomized design. The study aimed to evaluate the impact of supportive text messages (Text4Support) and peer support services (PSS) on readmission rates for patients with mental illness discharged from acute psychiatric hospitals. The main study protocol is available online (4, 28).
2.2 Sample size calculation
Using a projected margin of error of 3 for the mean EQ-VAS, a 95% confidence level, a population of 28,571, and a population variance of 2000, an online script (53) estimated a required sample size of 829. This estimation ensures an adequate number of participants to minimize errors while avoiding an excessively large sample size (54). For the ANCOVA, the observed power for the BRS, RAS and EQ-VAS were 0.99 (99%), 1.00 (100%), 1.00 (100%) respectively at alpha 0.05.
2.3 Ethics statement
The study was approved by the University of Alberta Health Ethics Research Board (Ref Pro00111459) and received additional approval from the regional health authority. Ethical approval was obtained for verbal consent to interviews and implied consent for electronic surveys. Written informed consent was obtained from all participants to access their health records.
2.4 Data collection
Data were collected through REDCap (55), an online platform, as part of an ongoing clinical trial examining the utility of Text4Support and Peer Support in reducing inpatient readmission rates in Alberta (28). Eligible participants were adults (18+), diagnosed with any mental health condition, ready for discharge, had a mobile device, could read English, and could provide informed consent. Sociodemographic data (age, gender, ethnicity, education, relationship status, employment) and clinical data (diagnosis, admission duration) were collected. The study data were gathered from March 8, 2022, to November 5, 2023. Baseline surveys were administered with the assistance of research team members after written consent. Phone and healthcare numbers served as primary identifiers.
2.5 Outcome measures
Primary outcomes included scores on the BRS, RAS, and EQ-VAS, and the association between these scores and demographic/clinical factors like gender, age, ethnicity, and mental health diagnosis.
The BRS evaluates resilience, defined as the ability to recover from stress (13). It comprises six statements, with responses ranging from 1–5 on a Likert scale, yielding a score between 6–30. Resilience levels are categorized as low (1.00–2.99), normal (3.00–4.30), and high (4.31–5.00) (4). For this analysis, normal and high resilience were grouped into one category (3.00–5.0). The BRS demonstrated good internal consistency (Cronbach α = 0.84) and reliability (r = 0.67) (56, 57). In a related study, the BRS showed good reliability (α = 0.84) and validity (r = 0.80, p <.001) (58).
The RAS is a 24-item scale that assesses recovery perceptions on a 5-point Likert scale (42). It includes five factors: (1) personal confidence and hope, (2) willingness to ask for help, (3) goal orientation, (4) reliance on others, and (5) no domination by symptoms (59). The RAS shows excellent psychometric properties (α = 0.94) and test-retest reliability (r = 0.88) (50, 60). The total score ranges from 24–120, with higher scores correlating with better quality of life and empowerment, while lower scores reflect more severe symptoms.
The EQ-VAS measures quality of life by assessing perceived health status on a scale from 0 (worst) to 100 (best) (51). It has proven to be a reliable and valid tool with test-retest reliability ranging from 0.65 to 0.91 (61–63).
2.6 Statistical analysis
Statistical analysis was conducted using SPSS for Mac, version 25 (IBM) (64). Baseline characteristics (sociodemographic, clinical) were summarized by age groups (<=25, 26–40, >40 years) as numbers, percentages, or means with standard deviations. Multiple ANCOVAs compared the relationship between groups, with self-rated BRS, RAS, and EQ-VAS scores as dependent variables investigated separately. The independent variables included demographic/clinical factors like age, gender, ethnicity, and diagnosis. Covariates included other demographic or clinical factors not designated as independent variables. Assumptions of ANCOVA were checked (linearity, normality, homogeneity). A post-hoc Tukey’s HSD test assessed group differences. Missing data were not imputed, and significance was set at p < 0.05.
Skewness and kurtosis were calculated to assess the normality of the data distribution. The results were as follows
● BRS: skewness = -0.33, kurtosis = 0.00 (standard error of skewness = 0.08, standard error of kurtosis = 0.15),
● RAS: skewness = -0.33, kurtosis = 0.74 (standard error of skewness = 0.08, standard error of kurtosis = 0.15),
● EQ-VAS: skewness = 0.48, kurtosis = 0.31 (standard error of skewness = 0.08, standard error of kurtosis = 0.16).
Based on the skewness values falling between -2 and 2 and kurtosis values falling between -7 and 7, the data were deemed to follow a normal distribution.
3 Results
Table 1 outlines the sociodemographic distribution of participants. Among the 1,004 participants, 35.8% were 25 years or younger, 34.7% were between 26 and 40 years, and 29.5% were over 40 years. Most participants identified as female (54.8%), with 42.4% identifying as male. Ethnically, 62.4% were Caucasian, and 51.4% had completed high school. The majority were single (58.9%), unemployed (53.4%), and rented their homes (32.3%). Over 26% had a clinical diagnosis of depression. The mean scores were: BRS 2.81 (SD=0.83), RAS 90.21 (SD=15.42), and EQ-VAS 67.79 (SD=20.12). For the ANCOVA, the observed power for the BRS, RAS and EQ-VAS were 0.99 (99%), 1.00 (100%), 1.00 (100%) respectively at alpha 0.05.
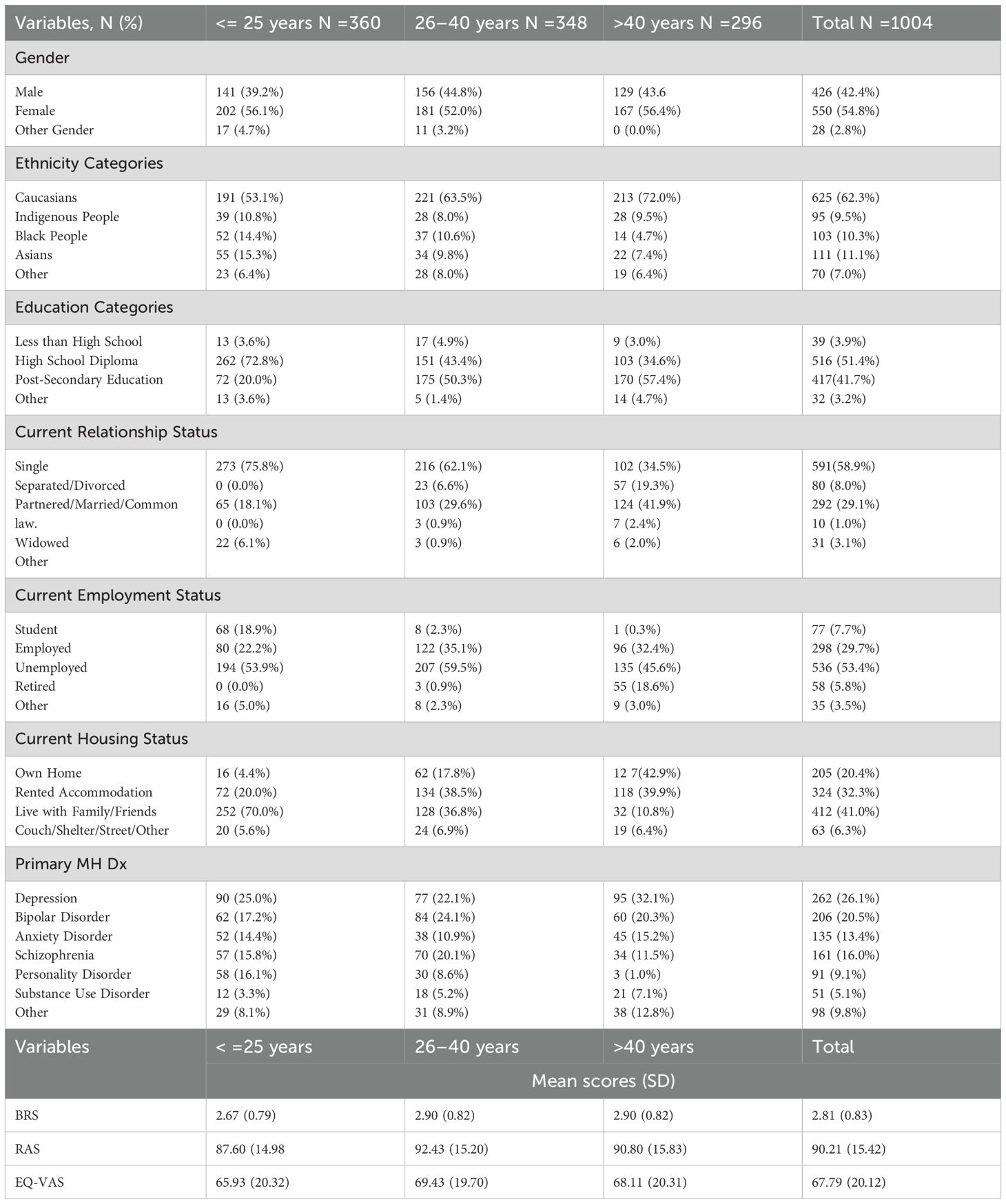
Table 1. Distribution of participants’ sociodemographic and clinical characteristics across age categories, entries are means ± (SD).
Table 2 presents the ANCOVA results for four covariates (gender, age, ethnicity, and mental health diagnosis). Statistically significant differences in BRS, RAS, and EQ-VAS scores were observed across different age, gender, ethnicity, and mental health diagnosis groups, after adjusting for other demographic and clinical factors. Gender was significantly associated with all three scores: RAS (F(2,992)=5.85, p=0.003), BRS (F(2,994)=15.30, p<0.001), and EQ-VAS (F(2,981)=6.89, p=0.001). Age was linked to both RAS (F(2,992)=6.45, p=0.002) and BRS (F(2,994)=8.83, p<0.001), but not EQ-VAS (F(2,981)=0.682, p=0.177). Ethnicity significantly influenced all three scores: RAS (F(4,990)=8.13, p<0.001), BRS (F(4,992)=9.30, p<0.001), and EQ-VAS (F(4,979)=8.10, p<0.001). Mental health diagnosis also significantly impacted all scores: RAS (F(6,998)=13.14, p<0.001), BRS (F(6,990)=18.23, p<0.001), and EQ-VAS (F(6,977)=4.27, p<0.001).
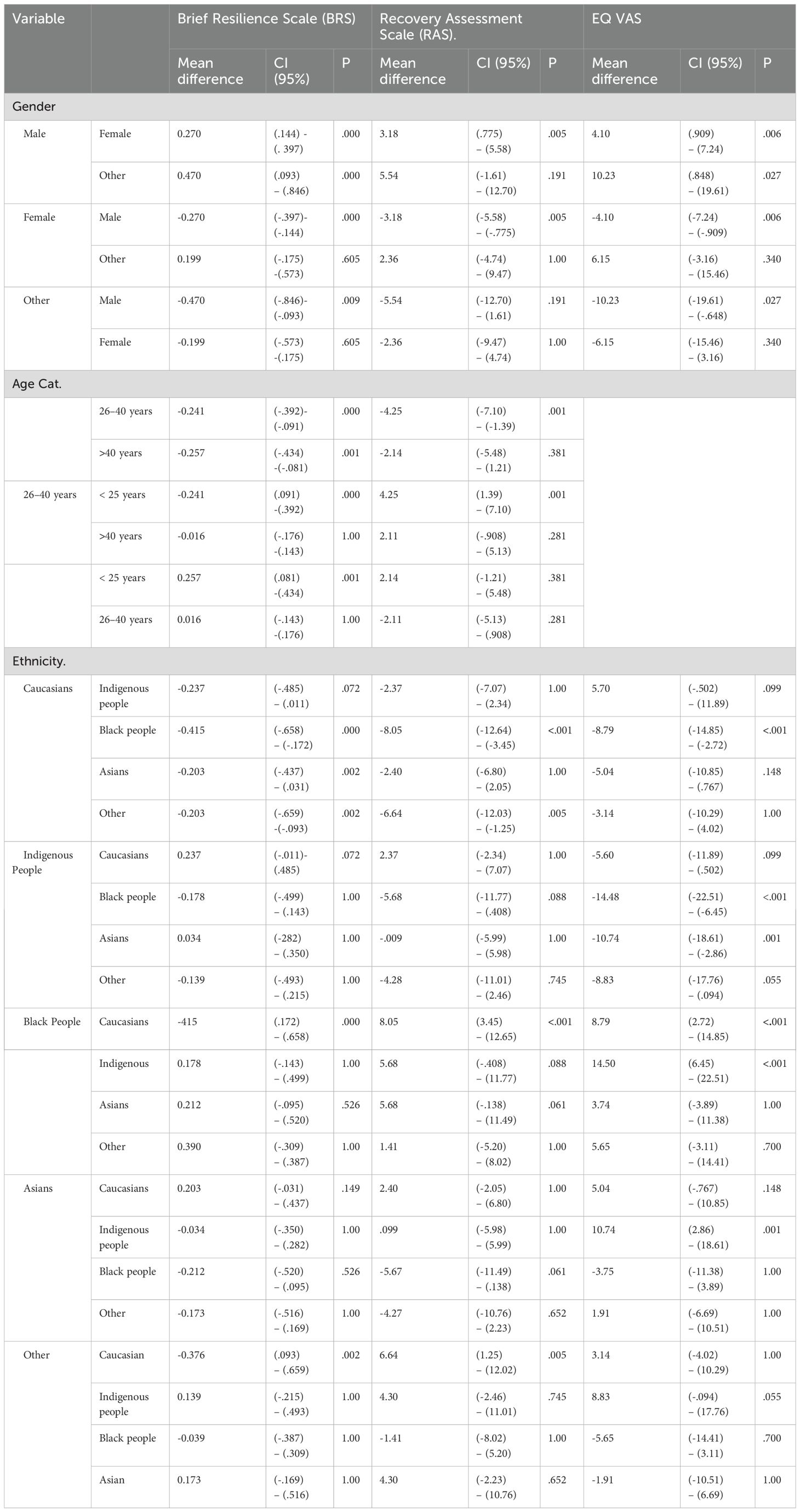
Given these significant differences, pairwise comparisons of BRS, RAS, and EQ-VAS scores were performed using Tukey’s HSD. Table 3 summarizes these findings. Regarding gender, males scored higher in BRS, EQ-VAS, and RAS than females. In terms of age, participants under 26 had lower resilience scores compared to those between 26-40 (Mdiff = -0.241) and over 40 years (Mdiff = -0.257). Participants aged 26–40 also had significantly higher recovery scores than those under 26 (Mdiff = 4.25).
Ethnicity comparisons revealed that Caucasians had lower resilience than Black participants (Mdiff = -0.415), Asians (Mdiff = -0.203), and others (Mdiff = -0.203). Black participants had higher quality-of-life scores compared to Caucasians (Mdiff = 8.79), and Asians scored better than Indigenous participants (Mdiff = 10.74). In terms of recovery, Black participants scored higher than Caucasians (Mdiff = 8.05).
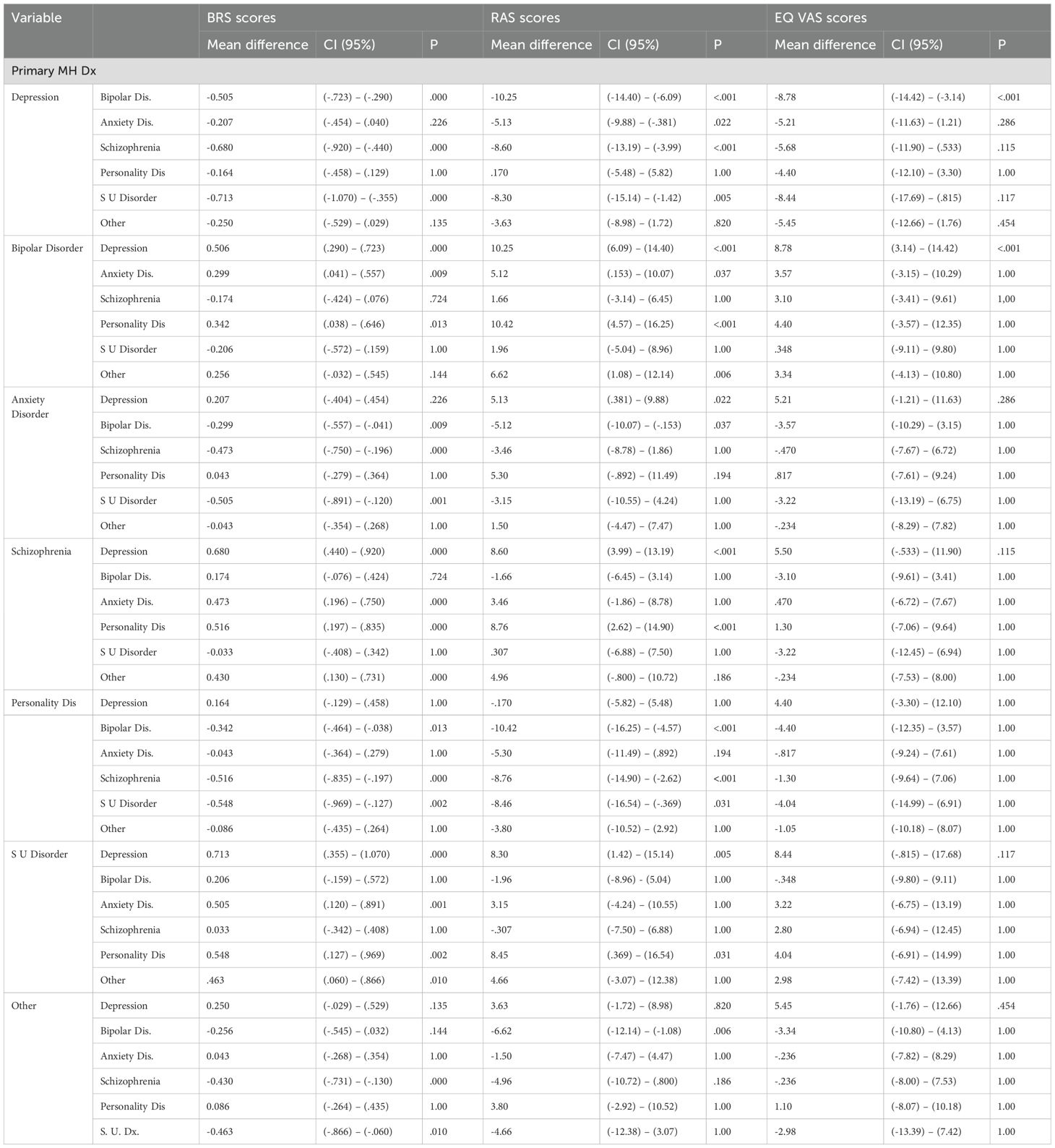
Table 4 shows the pairwise comparison for mental health diagnoses. Participants with depression had significantly lower resilience compared to those with bipolar disorder (Mdiff = -0.505), schizophrenia (Mdiff = -0.680), and substance use disorder (Mdiff = -0.713). Depression also correlated with lower quality of life and recovery compared to bipolar disorder, schizophrenia, and substance use disorder. Participants with bipolar disorder had better resilience and recovery than those with anxiety, personality disorder, and others. Additionally, individuals with schizophrenia had higher resilience and recovery compared to those with personality disorders. Participants with substance use disorder had lower resilience than those with schizophrenia (Mdiff = 0.463).
4 Discussion
The primary objective of this paper was to explore the relationship between sociodemographic and clinical characteristics and how they impact resilience, personal recovery, and quality of life of patients who are ready to be discharged from inpatient psychiatric units in Alberta. The study’s results reveal notable variations in resilience, personal recovery, and quality of life across different sociodemographic groups.
First, males scored significantly higher than females on resilience, recovery, and quality of life. Previous studies, including those by Bahadır (2015) (65) and Sürücü & Bacanlı (2010) (66), also report higher resilience in males, especially in personal power, initiative, and leadership. Research suggests that women may be more susceptible to the effects of childhood trauma than men (67), with resilience serving as a protective factor. Gender-sensitive approaches to resilience must consider the biological and social factors that influence men’s and women’s vulnerability to trauma and their mental health responses (68, 69). This study aligns with a study on university students that found higher resilience in male students (70). Societal gender expectations such as competitiveness for men and nurturing roles for women (71, 72) may shape resilience levels (45). Gender influences mental health responses, with men less likely to seek help due to social stigma, which can affect their recovery (73, 74).
Second, younger participants, particularly those under 26, showed lower resilience levels than older groups (26–40 and 40+), suggesting that age influences resilience. Older individuals often demonstrate greater adaptability and recovery, though resilience in younger people may be linked to emerging adulthood traits such as individualism and financial independence (75). Studies comparing resilience in young and older adults consistently find greater resilience in those over 65 (38, 75). Similarly, a UK study found that older adults were more resilient than younger adults under 26 (75).
Third, racial and ethnic differences were also evident in this study, with Black participants displaying higher resilience and recovery than their Caucasian counterparts. This suggests cultural, social, and community factors shape resilience. Research indicates that Black Canadians experience higher rates of depression, often linked to experiences of racism and discrimination (76, 77). Despite this, resilience is a key factor in improving treatment outcomes for depression (13), and Black individuals may have stronger resilience due to cultural identity and community support (78). A study on African American and Caucasian breast cancer patients found that perceived discrimination affected recovery and quality of life, with African Americans reporting lower quality of life (79). Similarly, Black participants with schizophrenia reported higher life quality than their White counterparts (80). This highlights the role of cultural identity and community engagement in resilience and recovery.
Fourth, individuals with depression had significantly lower resilience and personal recovery than those with other diagnoses, indicating the influence of mental health on these factors. Depressive disorder was associated with lower resilience and recovery compared to other mental health diagnoses, reinforcing the idea that some conditions may impede recovery and adaptation. This aligns with studies indicating lower resilience in those with depression (81, 82). Depression is often marked by hopelessness and low self-esteem, factors that contribute to lower resilience (81). Depression also correlates with higher relapse rates and poorer quality of life (48, 83, 84).
These findings underscore the complex relationships between gender, age, race, and mental health in determining resilience and recovery outcomes. Interventions may need to be designed and tailored to address the unique challenges faced by different sociodemographic groups, particularly younger individuals and those with mental health diagnoses such as depression.
5 Limitations
The study has several limitations. First, due to the self-report nature of the scales, patients’ responses could not be clinically validated. However, the scales used were validated, and self-reporting is practical for this type of study. Second, the study sample was drawn from a subset of a larger stepped-wedge cluster-randomized study, with an inclusion criterion of owning a mobile phone (28). This selection bias may have skewed the sample, as those without cell phones were excluded. Future studies could reduce this bias by offering alternative communication methods, such as email. Third, the lack of a control group limits the ability to draw conclusions about how the scores compare to the general population. Fourth, the study did not gather data on participants’ biological sex, preventing an analysis of its impact on resilience, recovery, and quality of life. Again, this paper did not include interaction analysis to provide the joint interaction effects for the sociodemographic and clinical characteristics to identify individuals at greatest risk of poorer outcome of resilience, personal recovery and quality of life. Future studies may examine these interaction effects. Also, while the study achieved a statistical power of 100%, which indicates a very low risk of Type II errors, this can also be considered a limitation. A power of 100% is often regarded as unrealistic or unnecessary in real-world settings, as it might suggest that the sample size was too large. Additionally, measurement invariance of the outcome measures used in this study is not well-known (56, 85, 86). Therefore, any comparisons of indicator means and covariances across demographics should be interpreted cautiously, which we acknowledge as a limitation of our study. Despite these limitations, the study provides valuable insights into how demographic and clinical factors influence resilience, recovery, and quality of life in patients discharged from inpatient psychiatric units.
6 Conclusions
In summary, the study outcome suggests that while there are some strengths, such as perceived recovery, there may also be areas for improvement, such as enhancing resilience and addressing the variability in health perceptions. The findings indicate that males tend to report higher resilience and quality of life compared to females, younger participants (under 26) appear to have lower resilience than older individuals, and Black participants seem to experience better resilience and recovery outcomes than Caucasians. These results may inform the development of policies and interventions aimed at improving mental health and well-being for individuals discharged from psychiatric hospitals. Programs designed to build resilience and improve recovery, such as daily supportive text messaging (87–89) and peer support services (90–92), might be helpful. The ongoing randomized trial related to this research seeks to explore the impact of these interventions on health outcomes for patients discharged from acute psychiatric hospitals. Tailoring interventions that consider sociodemographic characteristics and mental health diagnoses might enhance recovery and reduce readmission risk. Further research clarifies the long-term trajectories and factors influencing resilience, recovery, and quality of life for patients post-discharge and supports the refinement of practices that aid individuals with mental health challenges throughout their recovery. Also, future research will examine the measurement properties and invariance of these outcome measures most especially the BRS to ensure more robust and valid comparisons across diverse populations.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Health Research Ethics Board of the University of Alberta (Ref Pro00111459). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
EO: Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. WM: Data curation, Formal analysis, Methodology, Writing – review & editing. RS: Data curation, Formal analysis, Methodology, Writing – review & editing. HE: Data curation, Formal analysis, Methodology, Writing – review & editing. BA: Data curation, Formal analysis, Methodology, Writing – review & editing. EE: Data curation, Formal analysis, Methodology, Writing – review & editing. ML: Data curation, Formal analysis, Methodology, Writing – review & editing. NN: Data curation, Formal analysis, Methodology, Writing – review & editing. CH: Data curation, Formal analysis, Methodology, Writing – review & editing. YW: Data curation, Formal analysis, Methodology, Writing – review & editing. PS: Data curation, Formal analysis, Methodology, Writing – review & editing. PC: Data curation, Formal analysis, Methodology, Writing – review & editing. XL: Data curation, Formal analysis, Methodology, Writing – review & editing. WV: Data curation, Formal analysis, Methodology, Writing – review & editing. AO: Data curation, Formal analysis, Methodology, Writing – review & editing. VT: Data curation, Formal analysis, Methodology, Writing – review & editing. AG: Data curation, Formal analysis, Funding acquisition, Methodology, Supervision, Writing – review & editing. VA: Data curation, Formal analysis, Methodology, Writing – review & editing, Conceptualization, Funding acquisition, Project administration, Supervision.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Funding for this project was provided by Alberta Innovates.
Acknowledgments
The staff of Alberta Health Services provided varied support in conducting this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Farnham FR and James DV. Patients’ attitudes to psychiatric hospital admission. Lancet. (2000) 355:594. doi: 10.1016/S0140-6736(00)00077-5
2. Mongelli F, Georgakopoulos P, and Pato MT. Challenges and opportunities to meet the mental health needs of underserved and disenfranchised populations in the United States. Focus. (2020) 18:16–24. doi: 10.1176/appi.focus.20190028
3. Owusu E, Oluwasina F, Nkire N, Lawal MA, and Agyapong VI eds. Readmission of Patients to Acute Psychiatric Hospitals: Influential Factors and Interventions to Reduce Psychiatric Readmission Rates. Healthcare. Basel, Switzerland: MDPI (2022).
4. Owusu E, Shalaby R, Elgendy H, Mao W, Shalaby N, Agyapong B, et al eds. Comparison of Resilience, Personal Recovery, and Quality of Life Measures Pre-and Post-Discharge from Inpatient Mental Health Units in Alberta: Analysis of Control Group Data from a Randomized Trial. Healthcare. Basel, Switzerland: MDPI (2023).
5. Nurjannah I, Mills J, Usher K, and Park T. Discharge planning in mental health care: an integrative review of the literature. J Clin Nurs. (2014) 23:1175–85. doi: 10.1111/jocn.2014.23.issue-9pt10
6. Chung DT, Ryan CJ, Hadzi-Pavlovic D, Singh SP, Stanton C, and Large MM. Suicide rates after discharge from psychiatric facilities: a systematic review and meta-analysis. JAMA Psychiatry. (2017) 74:694–702. doi: 10.1001/jamapsychiatry.2017.1044
7. Niimura J, Tanoue M, and Nakanishi M. Challenges following discharge from acute psychiatric inpatient care in Japan: patients’ perspectives. J Psychiatr Ment Health Nurs. (2016) 23:576–84. doi: 10.1111/jpm.2016.23.issue-9pt10
8. Popham CM, McEwen FS, and Pluess M. Psychological resilience in response to adverse experiences. Multisyst Resilience. (2021), 395–416. doi: 10.1093/oso/9780190095888.001.0001
9. Gerino E, Rollè L, Sechi C, and Brustia P. Loneliness, resilience, mental health, and quality of life in old age: A structural equation model. Front Psychol. (2017) 8:2003. doi: 10.3389/fpsyg.2017.02003
10. Iwasaki Y, Coyle CP, and Shank JW. Leisure as a context for active living, recovery, health and life quality for persons with mental illness in a global context. Health Promotion Int. (2010) 25:483–94. doi: 10.1093/heapro/daq037
11. Harvey MR. An ecological view of psychological trauma and trauma recovery. J Traumatic Stress. (1996) 9:3–23. doi: 10.1002/jts.2490090103
12. Zimmerman EB, Woolf SH, and Haley A. Understanding the relationship between education and health: a review of the evidence and an examination of community perspectives. Population Health: Behav Soc Sci Insights Rockville (MD): Agency Health-care Res Quality. (2015) 22:347–84.
13. Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, and Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. (2008) 15:194–200. doi: 10.1080/10705500802222972
14. Marshall SL, Oades LG, and Crowe TP. Mental health consumers’ perceptions of receiving recovery-focused services. J Eval Clin Practice. (2009) 15:654–9. doi: 10.1111/j.1365-2753.2008.01070.x
15. Tew J, Ramon S, Slade M, Bird V, Melton J, and Le Boutillier C. Social factors and recovery from mental health difficulties: A review of the evidence. Br J Soc Work. (2012) 42:443–60. doi: 10.1093/bjsw/bcr076
16. Slade M. Personal recovery and mental illness: A guide for mental health professionals. Cambridge: Cambridge University Press (2009).
17. Slade M, Amering M, Farkas M, Hamilton B, O’Hagan M, Panther G, et al. Uses and abuses of recovery: implementing recovery-oriented practices in mental health systems. World Psychiatry. (2014) 13:12–20. doi: 10.1002/wps.20084
18. Billington DR, Landon J, Krägeloh CU, and Shepherd D. The New Zealand World Health organization quality of life (WHOQOL) group. NZ Med J. (2010) 123:65–70.
19. Werner EE. Protective factors and individual resilience. Handb Early Childhood Intervention. (2000) 2:115–32. doi: 10.1017/CBO9780511529320.008
20. Aburn G, Gott M, and Hoare K. What is resilience? An integrative review of the empirical literature. J Advanced Nurs. (2016) 72:980–1000. doi: 10.1111/jan.2016.72.issue-5
21. Lawford J and Eiser C. Exploring links between the concepts of quality of life and resilience. Pediatr Rehabilitation. (2001) 4:209–16. doi: 10.1080/13638490210124024
22. Simón-Saiz MJ, Fuentes-Chacón RM, Garrido-Abejar M, Serrano-Parra MD, Larrañaga-Rubio E, and Yubero-Jiménez S. Influence of resilience on health-related quality of life in adolescents. Enfermería Clínica (English Edition). (2018) 28:283–91. doi: 10.1016/j.enfcle.2018.06.004
23. Provencher HL, Gregg R, Mead S, and Mueser KT. The role of work in the recovery of persons with psychiatric disabilities. Psychiatr Rehabil J. (2002) 26:132. doi: 10.2975/26.2002.132.144
24. Polacsek M, Boardman GH, and McCann TV. Self-identity and meaning in life as enablers for older adults to self-manage depression. Issues Ment Health Nurs. (2022) 43:409–17. doi: 10.1080/01612840.2021.1998263
25. Leamy M, Bird V, Le Boutillier C, Williams J, and Slade M. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry. (2011) 199:445–52. doi: 10.1192/bjp.bp.110.083733
26. Fukui S, Starnino VR, Susana M, Davidson LJ, Cook K, Rapp CA, et al. Effect of Wellness Recovery Action Plan (WRAP) participation on psychiatric symptoms, sense of hope, and recovery. Psychiatr Rehabil J. (2011) 34:214. doi: 10.2975/34.3.2011.214.222
27. Klevan T, Sommer M, Borg M, Karlsson B, Sundet R, and Kim HS. Part III: Recovery-oriented practices in community mental health and substance abuse services: A meta-synthesis. Int J Environ Res Public Health. (2021) 18:13180. doi: 10.3390/ijerph182413180
28. Eboreime E, Shalaby R, Mao W, Owusu E, Vuong W, Surood S, et al. Reducing readmission rates for individuals discharged from acute psychiatric care in Alberta using peer and text message support: Protocol for an innovative supportive program. BMC Health Serv Res. (2022) 22:1–11. doi: 10.1186/s12913-022-07510-8
29. Ritchie A, Sautner B, Omege J, Denga E, Nwaka B, Akinjise I, et al. Long-term mental health effects of a devastating wildfire are amplified by sociodemographic and clinical antecedents in college students. Disaster Med Public Health Preparedness. (2020), 1–11. doi: 10.1017/dmp.2020.87
30. Llewellyn-Beardsley J, Rennick-Egglestone S, Callard F, Crawford P, Farkas M, Hui A, et al. Characteristics of mental health recovery narratives: systematic review and narrative synthesis. PloS One. (2019) 14:e0214678. doi: 10.1371/journal.pone.0214678
31. Górska S, Singh Roy A, Whitehall L, Irvine Fitzpatrick L, Duffy N, and Forsyth K. A systematic review and correlational meta-analysis of factors associated with resilience of normally aging, community-living older adults. Gerontol. (2022) 62:e520–e33. doi: 10.1093/geront/gnab110
32. Stewart DE and Yuen T. A systematic review of resilience in the physically ill. Psychosomatics. (2011) 52:199–209. doi: 10.1016/j.psym.2011.01.036
33. Valentine SE and Shipherd JC. A systematic review of social stress and mental health among transgender and gender non-conforming people in the United States. Clin Psychol Review. (2018) 66:24–38. doi: 10.1016/j.cpr.2018.03.003
34. Tamres LK, Janicki D, and Helgeson VS. Sex differences in coping behavior: A meta-analytic review and an examination of relative coping. Pers Soc Psychol Review. (2002) 6:2–30. doi: 10.1207/S15327957PSPR0601_1
35. Rybarczyk B, Emery EE, Guequierre LL, Shamaskin A, and Behel J. The role of resilience in chronic illness and disability in older adults. Annu Rev Gerontol Geriatr. (2012) 32. doi: 10.1891/0198-8794.32.173
36. Agli O, Bailly N, and Ferrand C. Spirituality and religion in older adults with dementia: a systematic review. Int Psychogeriatrics. (2015) 27:715–25. doi: 10.1017/S1041610214001665
37. Nandi A, Beard JR, and Galea S. Epidemiologic heterogeneity of common mood and anxiety disorders over the lifecourse in the general population: a systematic review. BMC Psychiatry. (2009) 9:1–11. doi: 10.1186/1471-244X-9-31
38. Hayman KJ, Kerse N, and Consedine NS. Resilience in context: the special case of advanced age. Aging Ment Health. (2017) 21:577–85. doi: 10.1080/13607863.2016.1196336
39. Yalcin-Siedentopf N, Pichler T, Welte A-S, Hoertnagl CM, Klasen CC, Kemmler G, et al. Sex matters: stress perception and the relevance of resilience and perceived social support in emerging adults. Arch Women’s Ment Health. (2021) 24:403–11. doi: 10.1007/s00737-020-01076-2
40. Keyes CL. The Black–White paradox in health: Flourishing in the face of social inequality and discrimination. J Personality. (2009) 77:1677–706. doi: 10.1111/j.1467-6494.2009.00597.x
41. Marrast L, Himmelstein DU, and Woolhandler S. Racial and ethnic disparities in mental health care for children and young adults: A national study. Int J Health Services. (2016) 46:810–24. doi: 10.1177/0020731416662736
42. Calvete E, Las Hayas C, and Del Barrio AG. Longitudinal associations between resilience and quality of life in eating disorders. Psychiatry Res. (2018) 259:470–5. doi: 10.1016/j.psychres.2017.11.031
43. Echezarraga A, Calvete E, González-Pinto A, and Las Hayas C. Resilience dimensions and mental health outcomes in bipolar disorder in a follow-up study. Stress Health. (2018) 34:115–26. doi: 10.1002/smi.v34.1
45. Vella S-LC and Pai NB. A theoretical review of psychological resilience: Defining resilience and resilience research over the decades. Arch Med Health Sci. (2019) 7:233–9. doi: 10.4103/amhs.amhs_119_19
46. Toukhsati SR, Jovanovic A, Dehghani S, Tran T, Tran A, and Hare D. Low psychological resilience is associated with depression in patients with cardiovascular disease. Eur J Cardiovasc Nurs. (2017) 16:64–9. doi: 10.1177/1474515116640412
47. Mulder RT, Joyce PR, Frampton CM, Luty SE, and Sullivan PF. Six months of treatment for depression: outcome and predictors of the course of illness. Am J Psychiatry. (2006) 163:95–100. doi: 10.1176/appi.ajp.163.1.95
48. Shayan NA, Azizi AT, Razaqi N, Afzali H, Neyazi A, Waez H, et al. Phase wise assessment of COVID-19 related depression, anxiety, and stress level among patients in Herat city, Afghanistan-A descriptive study. Razi Int Med J. (2021) 1. doi: 10.56101/rimj.v1i1.14
49. Stein LK, Dhamoon MS, Kornspun A, and Erdman J. Readmissions for depression and suicide attempt following stroke and myocardial infarction. Cerebrovascular Dis Extra. (2020) 10:94–104. doi: 10.1159/000509454
50. Salzer MS and Brusilovskiy E. Advancing recovery science: Reliability and validity properties of the Recovery Assessment Scale. Psychiatr Services. (2014) 65:442–53. doi: 10.1176/appi.ps.201300089
51. Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. (2011) 20:1727–36. doi: 10.1007/s11136-011-9903-x
52. Population statistics. Government of alberta (2023). Available online at: https://www.alberta.ca/population-statistics:~:text=As%20of%20July%201%2C%202023%2C%20Alberta's%20population%20was%204%2C695%2C290 (Accessed July 27, 2024).
53. Campbell M. Sample size: methods of calculation and reporting. Afr J Midwifery Women’s Health. (2019) 13:1–9. doi: 10.12968/ajmw.2019.0008
54. Sihoe AD. Rationales for an accurate sample size evaluation. J Thorac Dis. (2015) 7:E531. doi: 10.3978/j.issn.2072-1439.2015.10.33
55. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, and Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42:377–81. doi: 10.1016/j.jbi.2008.08.010
56. Kyriazos TA, Stalikas A, Prassa K, Galanakis M, Yotsidi V, and Lakioti A. Psychometric evidence of the Brief Resilience Scale (BRS) and modeling distinctiveness of resilience from depression and stress. Psychology. (2018) 9:1828–57. doi: 10.4236/psych.2018.97107
57. Margetts JL, Hazelton M, Santangelo P, Yorke J, and Wilson RL. Measurement of psychological resilience to support therapy interventions for clients in the clinical mental healthcare setting: A scoping review. Int J Ment Health Nurs. (2024) 33:1921–40. doi: 10.1111/inm.13404
58. Cantero-García M and Alonso-Tapia J. Brief resilience scale in front children’s behavior problems (BRS-BP). Anales Psicol. (2018) 34:531. doi: 10.6018/analesps.34.3.312601
59. Shalaby R, Hrabok M, Spurvey P, Abou El-Magd RM, Knox M, Rude R, et al. Recovery following peer and text messaging support after discharge from acute psychiatric care in Edmonton, Alberta: controlled observational study. JMIR Formative Res. (2021) 5:e27137. doi: 10.2196/27137
60. Felix S, Valery K-M, Caiada M, Guionnet S, Bonilla-Guerrero J, Destaillats J-M, et al. Personal recovery self-report outcome measures in serious mental illness: A systematic review of measurement properties. Clin Psychol Rev. (2024) 112, 102459. doi: 10.1016/j.cpr.2024.102459
61. Feng Y-S, Kohlmann T, Janssen MF, and Buchholz I. Psychometric properties of the EQ-5D-5L: a systematic review of the literature. Qual Life Res. (2021) 30:647–73. doi: 10.1007/s11136-020-02688-y
62. Dams J, Rimane E, Steil R, Renneberg B, Rosner R, and König H-H. Reliability, validity and responsiveness of the EQ-5D-5L in assessing and valuing health status in adolescents and young adults with posttraumatic stress disorder: a randomized controlled trail. Psychiatr Quarterly. (2021) 92:459–71. doi: 10.1007/s11126-020-09814-6
63. Van Krugten F, Feskens K, Busschbach J, Hakkaart-van Roijen L, and Brouwer W. Instruments to assess quality of life in people with mental health problems: a systematic review and dimension analysis of generic, domain-and disease-specific instruments. Health Qual Life Outcomes. (2021) 19:1–13. doi: 10.1186/s12955-021-01883-w
64. IBM. IBM support. Release notes - IBM® SPSS® Statistics 25.0 . Available online at: https://www.ibm.com/support/pages/release-notes-ibm%C2%AE-spss%C2%AE-statistics-250 (Accessed December 8, 2020).
65. Bahadir-Yilmaz E and Fatma Oz R. The resilience levels of first-year medical, dentistry, pharmacy and health sciences students. Int J Caring Sci. (2015) 8:385.
66. SÜRÜCÜ M, BACANLI F. An examination of university adjustment according to psychological hardiness and demographic variables. Ankara Turkey: Gazi Üniversitesi Gazi Eğitim Fakültesi Dergisi; Cilt: 30 Sayı: 2 (2010).
67. Wei J, Gong Y, Wang X, Shi J, Ding H, Zhang M, et al. Gender differences in the relationships between different types of childhood trauma and resilience on depressive symptoms among Chinese adolescents. Prev Med. (2021) 148:106523. doi: 10.1016/j.ypmed.2021.106523
68. Smith SG and Sinkford JC. Gender equality in the 21st century: Overcoming barriers to women’s leadership in global health. J Dental Education. (2022) 86:1144–73. doi: 10.1002/jdd.13059
69. Corps M. Priming resilience with intra-household change, addressing gender norms. Portland, OR: Mercy Corps (2018).
70. Erdogan E, Ozdogan O, and Erdogan M. University students’ resilience level: The effect of gender and faculty. Procedia-social Behav Sci. (2015) 186:1262–7. doi: 10.1016/j.sbspro.2015.04.047
71. Kline BE and Short EB. Changes in emotional resilience: Gifted adolescent females. Roeper Review. (1991) 13:118–21. doi: 10.1080/02783199109553333
73. Liddon L, Kingerlee R, and Barry JA. Gender differences in preferences for psychological treatment, coping strategies, and triggers to help-seeking. Br J Clin Psychol. (2018) 57:42–58. doi: 10.1111/bjc.2018.57.issue-1
74. Coyne JC and Downey G. Social factors and psychopathology: Stress, social support, and coping processes. Annu Rev Psychol. (1991) 42:401–25. doi: 10.1146/annurev.ps.42.020191.002153
75. Masten AS, Obradović J, and Burt KB. Resilience in emerging adulthood: developmental perspectives on continuity and transformation. American Psychological Association. (2006), 173–90. doi: 10.1037/11381-007
76. Cénat JM, Kogan C, Noorishad PG, Hajizadeh S, Dalexis RD, Ndengeyingoma A, et al. Prevalence and correlates of depression among Black individuals in Canada: The major role of everyday racial discrimination. Depression Anxiety. (2021) 38:886–95. doi: 10.1002/da.23158
77. Fava GA and Tomba E. Increasing psychological well-being and resilience by psychotherapeutic methods. J Personality. (2009) 77:1903–34. doi: 10.1111/j.1467-6494.2009.00604.x
79. Merluzzi TV, Philip EJ, Zhang Z, and Sullivan C. Perceived discrimination, coping, and quality of life for African-American and Caucasian persons with cancer. Cultural Diversity Ethnic Minority Psychol. (2015) 21:337. doi: 10.1037/a0037543
80. Prince JD. Ethnicity and life quality of recently discharged inpatients with schizophrenia. Am J Orthopsychiatry. (2006) 76:202–5. doi: 10.1037/0002-9432.76.2.202
81. Wang C. Depression and suicide behavior among college students: Understanding the moderator effects of self-esteem and suicide resilience. Ann Arbor, Michigan: University of Denver (2013).
82. Nunes KG and da Rocha NS. Resilience in severe mental disorders: correlations to clinical measures and quality of life in hospitalized patients with major depression, bipolar disorder, and schizophrenia. Qual Life Res. (2022) 31:507–16. doi: 10.1007/s11136-021-02920-3
83. Verhoeven FE, Wardenaar KJ, Ruhe HG, Conradi HJ, and de Jonge P. Seeing the signs: Using the course of residual depressive symptomatology to predict patterns of relapse and recurrence of major depressive disorder. Depression Anxiety. (2018) 35:148–59. doi: 10.1002/da.2018.35.issue-2
84. Neyazi A, Mohammadi AQ, Neyazi M, Timilsina S, Padhi BK, and Griffiths MD. Hypertension, depression, and health-related quality of life among hospitalized patients in Afghanistan. J Hum Hypertension. (2024), 1–9. doi: 10.1038/s41371-024-00914-5
85. Rodríguez-Rey R, Alonso-Tapia J, and Hernansaiz-Garrido H. Reliability and validity of the brief resilience scale (BRS) Spanish version. psychol Assessment. (2016) 28:e101. doi: 10.1037/pas0000191
86. de Holanda Coelho GL, Hanel PH, Medeiros Cavalcanti T, Teixeira Rezende A, and Veloso Gouveia V. Brief Resilience Scale: Testing its factorial structure and invariance in Brazil. Universitas Psychol. (2016) 15:397–408. doi: 10.11144/Javeriana.upsy15-2.brst
87. Agyapong V, Mrklas K, Juhas M, Omeje J, Ohinmaa A, Dursun S, et al. Mobile health program to reduce psychological treatment gap in mental healthcare in Alberta through daily supportive text messages–Cross-sectional survey evaluating Text4Mood. Eur Psychiatry. (2017) 41:S139–S. doi: 10.1016/j.eurpsy.2017.01.1970
88. Agyapong VI, Juhás M, Ohinmaa A, Omeje J, Mrklas K, Suen VY, et al. Randomized controlled pilot trial of supportive text messages for patients with depression. BMC Psychiatry. (2017) 17:1–10. doi: 10.1186/s12888-017-1448-2
89. Agyapong VIO, Mrklas K, Suen VYM, Rose MS, Jahn M, Gladue I, et al. Supportive text messages to reduce mood symptoms and problem drinking in patients with primary depression or alcohol use disorder: protocol for an implementation research study. JMIR Res Protoc. (2015) 4:e4371. doi: 10.2196/resprot.4371
90. Chinman M, George P, Dougherty RH, Daniels AS, Ghose SS, Swift A, et al. Peer support services for individuals with serious mental illnesses: assessing the evidence. Psychiatr Services. (2014) 65:429–41. doi: 10.1176/appi.ps.201300244
91. O’Connell MJ, Sledge WH, Staeheli M, Sells D, Costa M, Wieland M, et al. Outcomes of a peer mentor intervention for persons with recurrent psychiatric hospitalization. Psychiatr Serv (Washington DC). (2018) 69:760–7. doi: 10.1176/appi.ps.201600478
Keywords: personal recovery, resilience, mood disorders, substance use disorder, schizophrenia
Citation: Owusu E, Mao W, Shalaby R, Elgendy HE, Agyapong B, Eboreime E, Lawal MA, Nkire N, Hilario CT, Wei Y, Silverstone P, Chue P, Li X-M, Vuong W, Ohinmaa A, Taylor V, Greenshaw AJ and Agyapong VIO (2025) Resilience, personal recovery, and quality of life for psychiatric in-patients prior to hospital discharge: demographic and clinical determinants. Front. Psychiatry 16:1494493. doi: 10.3389/fpsyt.2025.1494493
Received: 10 September 2024; Accepted: 24 April 2025;
Published: 23 May 2025.
Edited by:
Juan Diego Ramos-Pichardo, University of Huelva, SpainReviewed by:
Natasha Seaton, King’s College London, United KingdomSimon Felix, Université de Bordeaux, France
Kavita Gupta, Maharaja Sayajirao University of Baroda, India
Copyright © 2025 Owusu, Mao, Shalaby, Elgendy, Agyapong, Eboreime, Lawal, Nkire, Hilario, Wei, Silverstone, Chue, Li, Vuong, Ohinmaa, Taylor, Greenshaw and Agyapong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vincent I. O. Agyapong, dm42MDIzNjdAZGFsLmNh
 Ernest Owusu
Ernest Owusu Wanying Mao
Wanying Mao Reham Shalaby
Reham Shalaby Hossam Eldin Elgendy
Hossam Eldin Elgendy Belinda Agyapong1
Belinda Agyapong1 Yifeng Wei
Yifeng Wei Peter Silverstone
Peter Silverstone Pierre Chue
Pierre Chue Xin-Min Li
Xin-Min Li Wesley Vuong
Wesley Vuong Andrew J. Greenshaw
Andrew J. Greenshaw Vincent I. O. Agyapong
Vincent I. O. Agyapong