- 1Laboratory of Alcohology, Department of Pathology, Medical School of Crete, University of Crete, Herakleion, Greece
- 2Department of Psychiatry, General Hospital of Agios Nikolaos, Agios Nikolaos, Greece
- 3Department of Psychiatry, Agioi Anargyroi Hospital, National and Kapodistrian University of Athens, Athens, Greece
- 4Department of Social Psychiatry, Medical University of Vienna, Vienna, Austria
Importance: Aripiprazole, a partial D2 receptor agonist, is proposed to enhance prefrontal cortex (PFC) dopamine function, improving working memory and GABA transmission, which supports social functioning. Long-acting injectable (LAI) antipsychotics are known to improve patient adherence, leading to enhanced long-term effects on behavioral outcomes.
Objective: To evaluate whether aripiprazole LAI treatment improves general functioning, quality of life, and reduces hospitalizations in psychotic patients, both in community settings and within incarcerated populations.
Design, settings, and participants: The study included 55 patients, with 34 from the community and 21 incarcerated at a prison in Southeastern Greece (Neapolis). The World Health Organization Quality of Life Brief Version (WHOQOL-BREF) and the Clinical Global Impression-Severity (CGI-S) scale were used to assess outcomes. Comparisons were made between pre-treatment and post-treatment periods, with a minimum follow-up of six months.
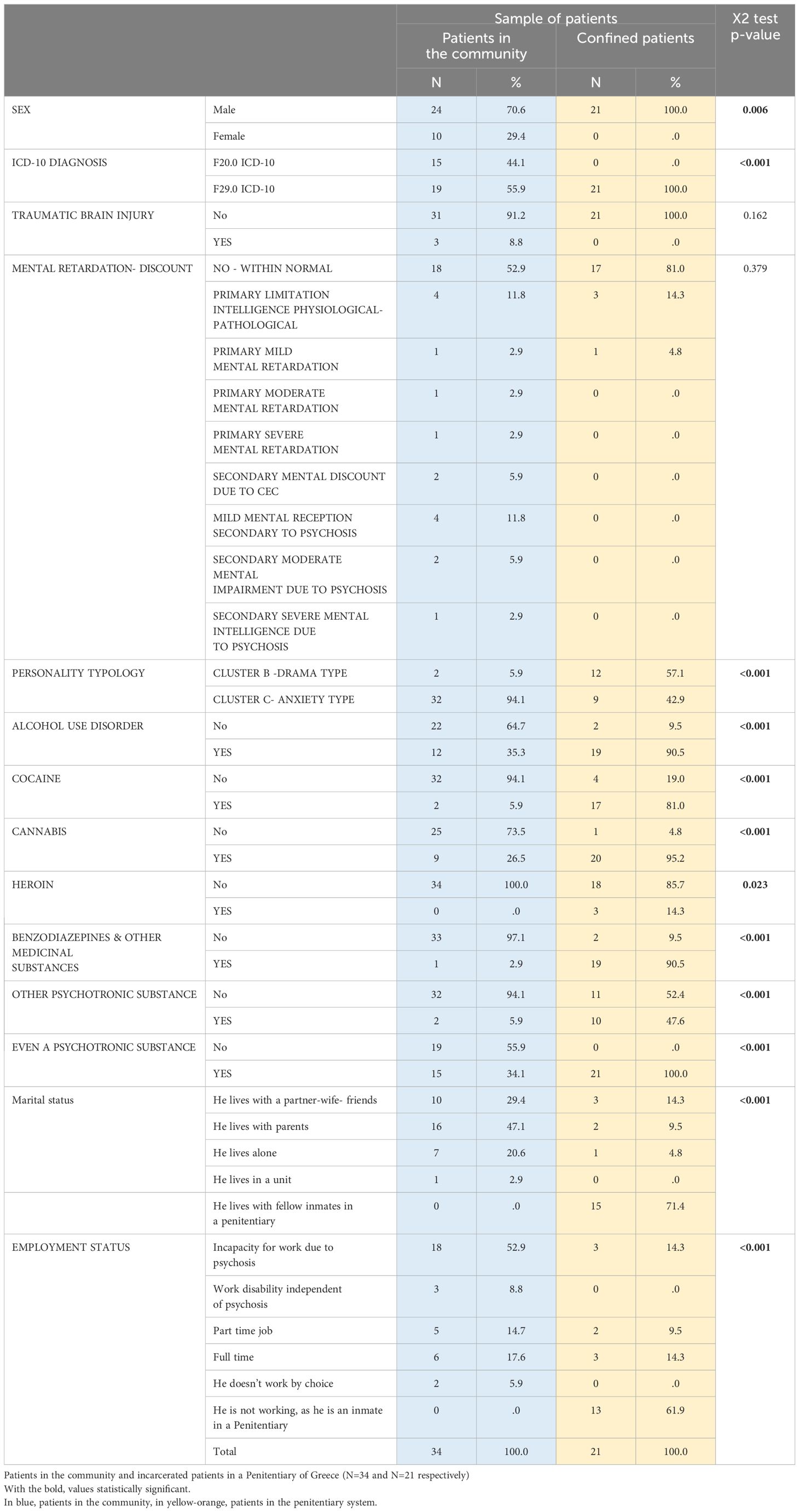
Results: • Demographics: Community patients (70.6% male) included 44.1% with paranoid schizophrenia. Incarcerated patients (all male) had an F29.0 diagnosis, with 57.1% exhibiting Cluster B personality disorder and all reporting psychoactive substance use.
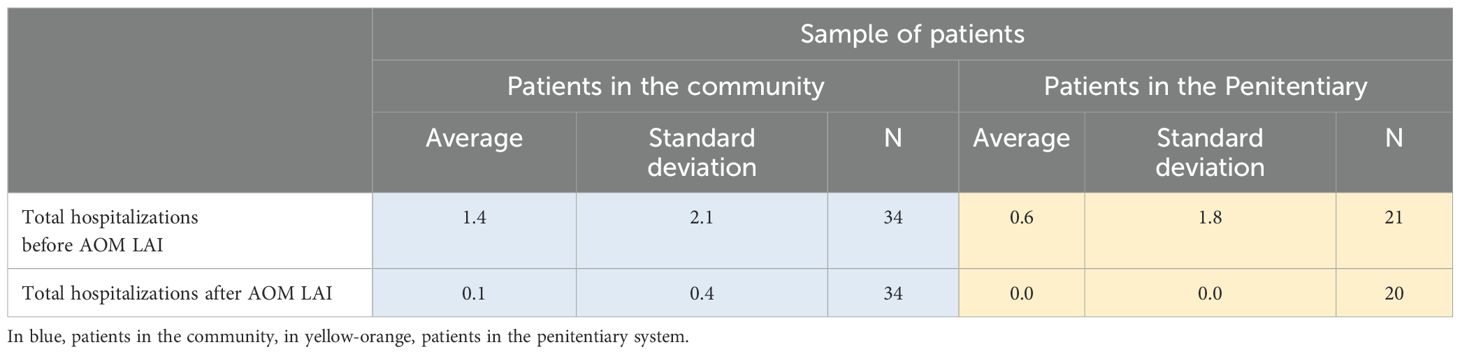
• Hospitalizations: Community patients’ hospitalizations decreased from 1.4 to 0.1 over six months (p=0.001). Incarcerated patients’ hospitalizations dropped from 0.6 to 0.0 (p=0.066), with no significant intergroup difference (p=0.150).
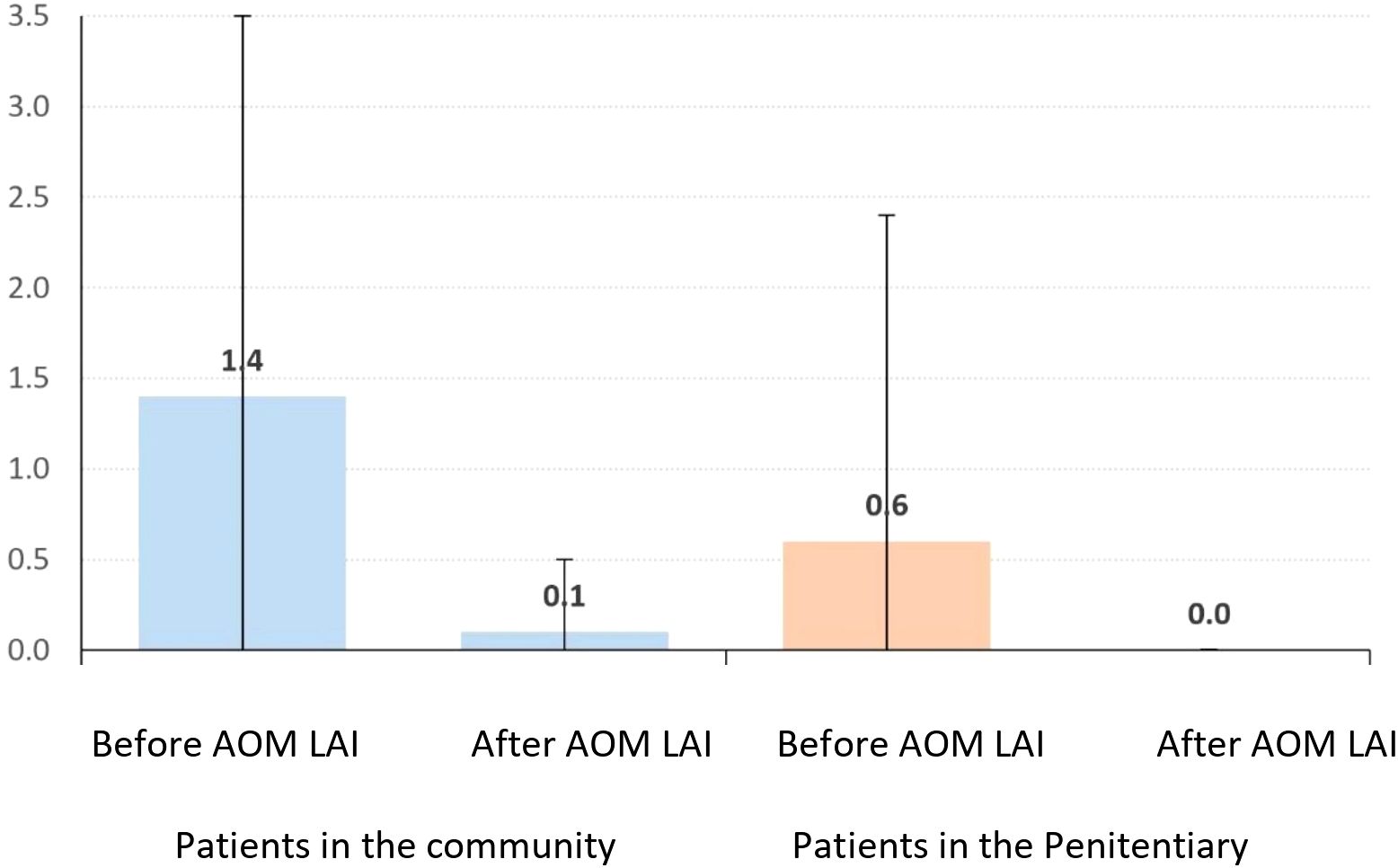
• CGI-S: Community patients’ scores improved from 6.0 to 3.9 (p<0.001). Incarcerated patients’ scores improved from 5.3 to 3.2 (p<0.001), with no significant difference between groups (p=0.814).
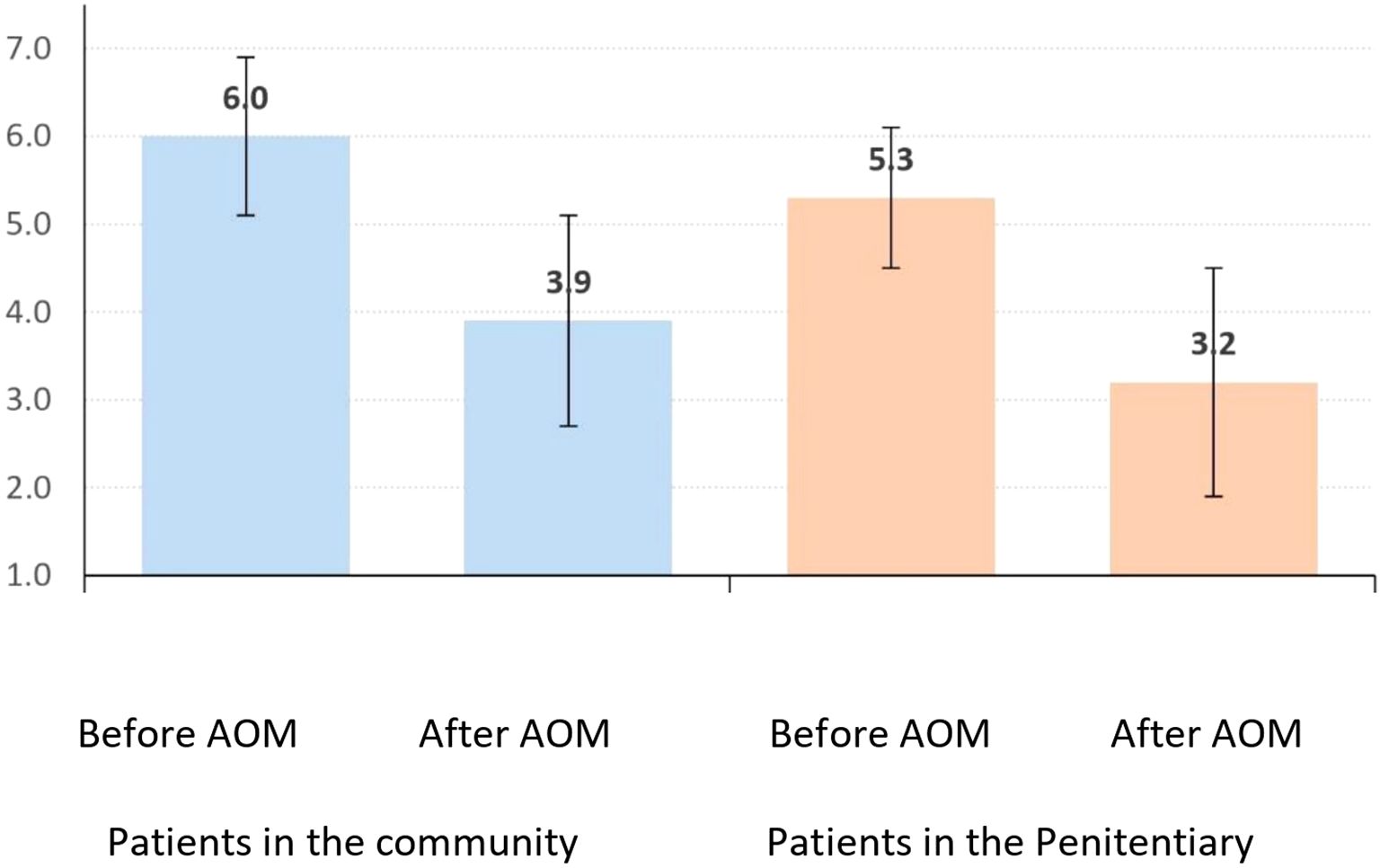
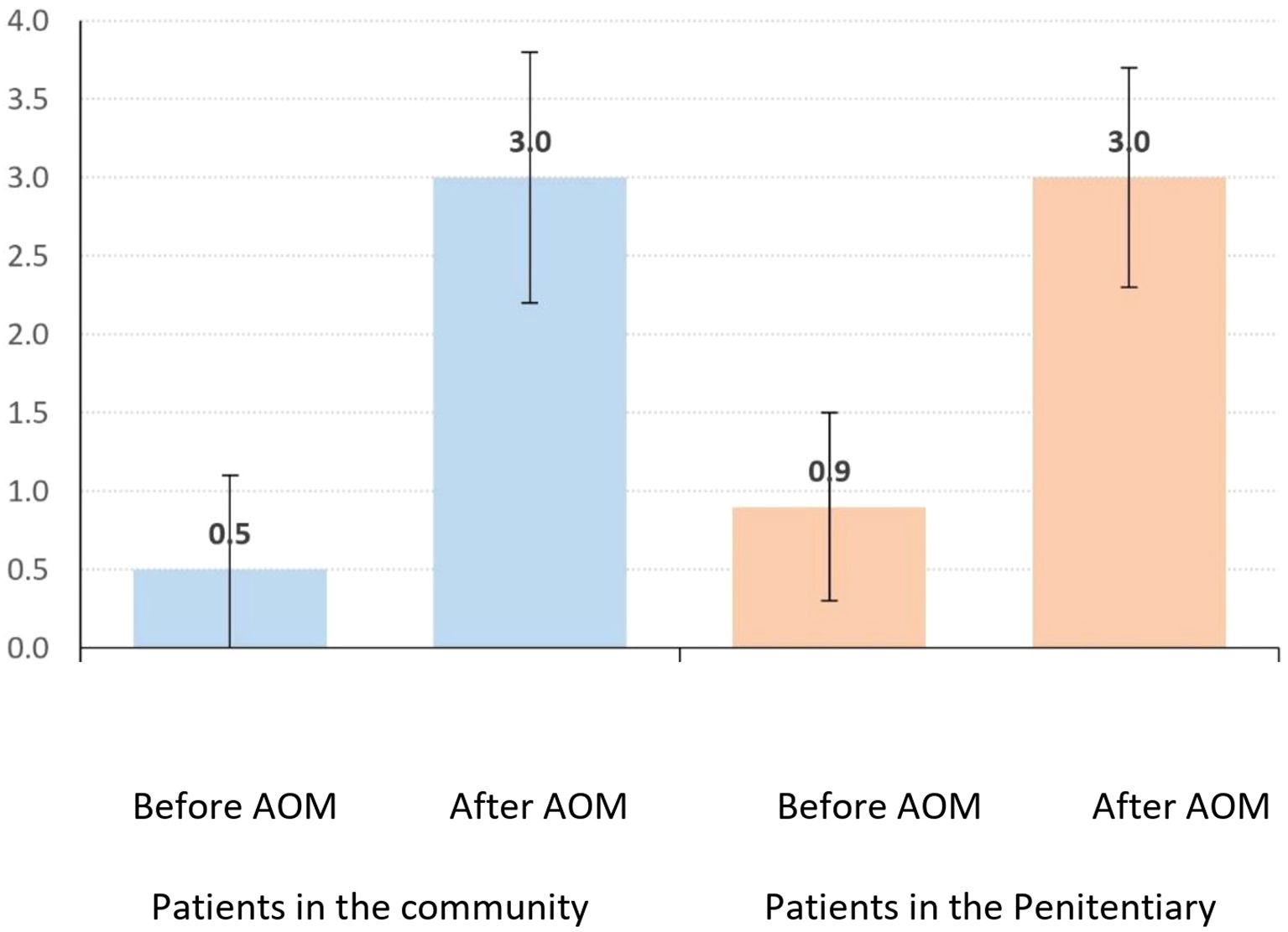
• Quality of Life: Community patients’ scores rose from 0.5 to 3.0 (p<0.001), while incarcerated patients’ scores also increased significantly (p<0.001).
Conclusions: This study of 34 community and 21 incarcerated patients revealed significant demographic and medical history differences. Both groups experienced reduced hospitalizations and improvements in CGI-S scores and quality of life following aripiprazole LAI administration. Community patients showed a greater reduction in hospitalizations, while clinical and quality-of-life improvements were comparable across groups.
Introduction
Non-adherence to antipsychotic medication is a primary reason for treatment inefficacy in psychotic patients, particularly those with co-occurring substance use disorders (SUD) or alcohol use disorders (AUD). Poor adherence increases relapse risk, hospitalization rates, treatment costs, and the likelihood of legal issues, perpetuating a “revolving door” cycle of hospitalization and incarceration. In Greece, the impending implementation of Law 5129/2024, effective February 1, 2025, will integrate psychiatric services with the penitentiary system, prompting this study to assess aripiprazole LAI benefits for community and incarcerated patients in Eastern Crete. The findings aim to inform health policy, optimize resource allocation, and support psychiatric reform. Long-acting injectable (LAI) antipsychotics, such as aripiprazole once-monthly monohydrate (AOM) and aripiprazole lauroxil, address non-adherence by reducing daily dosing needs. AOM, approved for schizophrenia since 2012 and bipolar disorder since 2017, and aripiprazole lauroxil, approved for schizophrenia, offer sustained treatment options (1). A new formulation, Ari 2MRTU 960, administered bimonthly, is under investigation for schizophrenia and bipolar I disorder (2). As a third-generation antipsychotic, aripiprazole acts as a partial D2 and 5-HT1A agonist and 5-HT2A antagonist, approved by the FDA in 2002 (1). Its unique mechanism (3) may reduce hyperdopaminergic activity in the mesolimbic system (antipsychotic effect) while enhancing hypodopaminergic activity in the prefrontal cortex, potentially alleviating negative symptoms and cognitive deficits (4–6). Partial 5-HT1A agonism may also provide anxiolytic benefits (7). Studies, including a 2015 trial in the UK and Canada, demonstrated aripiprazole’s ability to enhance dorsolateral prefrontal cortex (DLPFC) activation during working memory tasks, suggesting improved processing speed (8).
Methods
The study enrolled 55 patients: 34 from the community (15 with schizophrenia [F20.0, ICD-10], 19 with unspecified psychosis [F29.0, ICD-10]; 35.3% with AUD, 26.5% with cannabis use disorder) and 21 incarcerated males (all with F29.0; 90.5% with AUD, 95.2% with cannabis use disorder) (Table 1). Ethical approval was granted by the General Hospital of Agios Nikolaos (decision 514/19-07-2023) and the Ministry of Public Order (Prot. No. 10456/10-04-2023). Participants were assessed using the WHOQOL-BREF and CGI-S scales, with outcomes compared pre- and post-aripiprazole LAI treatment over a minimum six-month period.
Statistical analysis
Categorical data (e.g., gender) were analyzed with frequency tables, while continuous (e.g., age) and ordinal data (e.g., CGI-S) were reported as means and standard deviations. The χ² test compared sociodemographic and medical history differences (except age), and the Mann-Whitney U test assessed age, hospitalizations, CGI-S, and quality-of-life differences between groups. The Wilcoxon signed-rank test evaluated pre- and post-treatment changes within groups, with a significance level of α=0.05.
Results
● Community Patients (n=34): 70.6% male, mean age 42.3 ± 11.9 years, 44.1% with F20.0, 94% with Cluster C personality, 34.1% with psychoactive substance use, mean treatment duration 23.2 ± 18.3 months.
● Incarcerated Patients (n=21): All male, mean age 37.6 ± 7.7 years, all with F29.0, 57.1% with Cluster B personality, 100% with psychoactive substance use, mean treatment duration 14.5 ± 11.3 months.
● Significant differences were noted between groups in most demographic and medical history parameters, except for traumatic brain injury, mental retardation, age, and treatment duration.
Number of Hospitalizations
Community patients’ hospitalizations decreased from 1.4 ± 2.1 to 0.1 ± 0.4 (p=0.001), a mean reduction of 1.3 ± 2.1. Incarcerated patients’ hospitalizations fell from 0.6 ± 1.8 to 0.0 ± 0.0 (p=0.066), a mean reduction of 0.6 ± 1.8, with no significant intergroup difference (p=0.150) (Tables 2, 3; Figure 1).
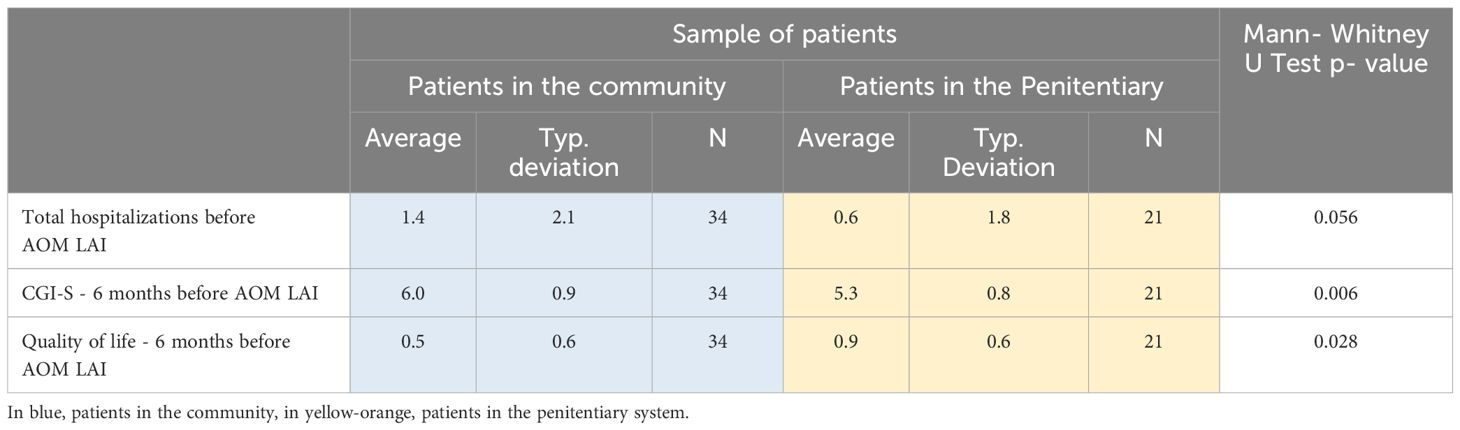
Table 2. Total hospitalizations, CGI-S scale (1=Normal, 2=Borderly ill, 3=Mildly ill, 4=Moderately ill, 5=Significantly ill, 6=Severely ill, 7=Among the most severe cases), Quality of Life scale (0=very bad, 1=bad, 2=neither good-nor bad, 3=good, 4=very good) before AOM LAI.
CGI-S
Community patients’ CGI-S scores improved from 6.0 ± 0.9 to 3.9 ± 1.2 (p<0.001), a mean reduction of 2.2 ± 1.4. Incarcerated patients’ scores improved from 5.3 ± 0.8 to 3.2 ± 1.3 (p<0.001), a mean reduction of 2.1 ± 1.2, with no significant intergroup difference (p=0.814) (Table 4; Figure 2).
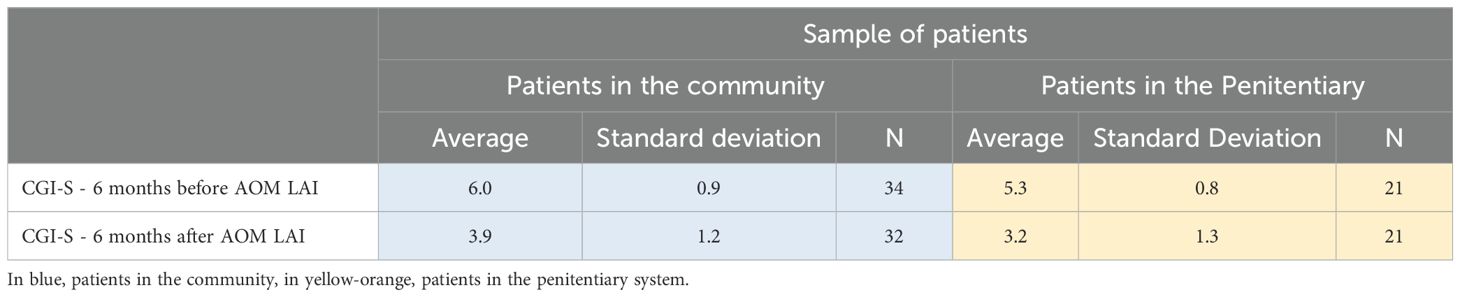
Table 4. CGI-S scale before and after AOM LAI (1=Normal, 2=Borderly ill, 3=Mildly ill, 4=Moderately ill, 5=Significantly ill, 6=Severely ill, 7=Among the most severe cases).
Quality of life
Community patients’ quality-of-life scores increased from 0.5 ± 0.6 to 3.0 ± 0.8 (p<0.001), a mean gain of 2.5 ± 1.0. Incarcerated patients’ scores rose from 0.9 ± 0.6 to 3.0 ± 0.7 (p<0.001), a mean gain of 2.1 ± 0.9, with no significant intergroup difference (p=0.147) (Table 5; Figure 3).
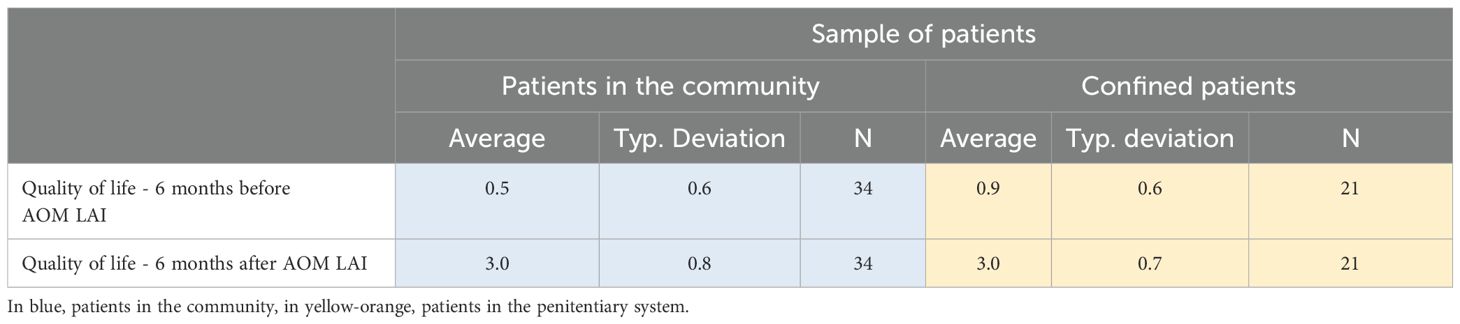
Table 5. Quality of life scale before and after AOM LAI (0=very bad, 1=bad, 2=neither good-nor bad, 3=good, 4=very good).
Discussion
This study is the first in Greece to evaluate aripiprazole LAI for community patients with psychosis and SUD, and the first in Europe for incarcerated patients with unspecified psychosis and SUD. Observed outcomes may reflect temperamental traits, as noted by Favaretto et al. (2024) (9), which influence psychopathology severity and treatment engagement, especially in dual-diagnosis or Cluster B populations (10). Aripiprazole’s D2 partial agonism enhances prefrontal dopamine and GABA transmission, improving working memory (6) and social skills (7). It is indicated for schizophrenia relapse prevention, bipolar I manic episodes, and autism-related irritability and may benefit conduct disorders linked to AUD or cannabis use (11). A Madrid study (2020) reported a >30% CGI-S reduction and reduced substance use in 40 schizophrenia patients with SUD after six months of aripiprazole LAI (12). A German study (2018) highlighted cost savings, with hospitalization rates dropping from 55.1% to 14% post-switch to aripiprazole LAI (13).
Our findings confirm significant improvements in quality of life, functionality, and hospitalization rates, aligning with Sampogna et al. (2023) on LAI benefits (14). For incarcerated patients, 19 of 21 maintained stability, though two relapsed post-release, underscoring adherence challenges. The study supports expanded community mental health services, including crisis intervention and early psychosis programs, to reduce incarceration cycles.
Aripiprazole LAI also shows promise for AUD, with four community patients achieving abstinence and others reducing consumption. Animal studies support its efficacy in reducing ethanol-related behaviors (15, 16). Further research is needed to quantify cost savings and explore off-label use in AUD.
Limitations
The study focused solely on aripiprazole LAI, limiting generalizability to other LAIs. The small sample size and potential self-report bias are additional constraints. In Greece, inadequate emergency psychiatric assessment may underestimate hospitalization needs, particularly for incarcerated patients with Cluster B traits and SUD.
Data availability statement
The datasets presented in this article are not readily available because The data is controlled exclusively by the main research team. Requests to access the datasets should be directed to ZXBhc3BhcmFraXNAYWduaG9zcC5ncg==.
Ethics statement
The studies involving humans were approved by the General Hospital of Agios Nikolaos (decision 514/19-07-2023), Scientific Council of the General Hospital of Agios Nikolaos Lasithi of Crete – National Health System of Greece (Prot. No. 10/15-02-2023), 7th Sanitary Region of Crete (Prot. No. 28386/30-06-2023), and Ministry of Public Order (Prot. No. 10456/10-04-2023) under Law 4812/2021, Article 87. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
EK: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Supervision, Writing – original draft. IM: Supervision, Writing – review & editing. GA: Supervision, Writing – review & editing, Conceptualization, Methodology, Validation, Visualization. OL: Visualization, Writing – review & editing. HW: Visualization, Writing – review & editing. EP: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Supervision, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Acknowledgments
Corresponding authors Erasmia I. Koiliari and Emmanouil L. Pasparakis extend their deepest gratitude to Dr. Emmanouil Andreadakis, Surgeon and Hospital Administrator of the General Hospital of Agios Nikolaos (Lassithi, Crete), upon acceptance and initiation of the research protocol (“DNAng”), to Georgios Mavrikakis, Nephrologist, President of the Scientific Council of the General Hospital of Agios Nikolaos, upon acceptance and initiation of the research protocol (“DNAng”) and to Dr. Nikolaos Moudatsakis, Surgeon, Hospital Administrator and President of the Scientific Council of the General Hospital of Agios Nikolaos, during the development of the Medical Research entitled “DNAng”.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Di Sciascio G and Riva MA. Aripiprazole: from pharmacological profile to clinical use. Neuropsychiatr Dis Treat. (2015) 11:2635. doi: 10.2147/NDT.S88117
2. ABILIFY (aripiprazole) tablets, ABILIFY DISCMELT (aripiprazole) orally disintegrating tablets, ABILIFY (aripiprazole) oral solution, ABILIFY (aripiprazole) injection for intramuscular use only. Otsuka Pharmaceutical Company (2014).
3. Abilify 7.5 mg/ml solution for injection (intramuscular) – summary of product characteristics (SmPC). Available online at: https://www.medicines.org.uk/emc/product/6239/pil (Accessed January 20, 2023).
4. DeLeon A, Patel NC, and Crismon ML. Aripiprazole: a comprehensive review of its pharmacology, clinical efficacy, and tolerability. Clin Ther. (2004) 26:649–66. doi: 10.1016/S0149-2918(04)90066-5
5. Millan MJ. The neurobiology and control of anxious states. Prog Neurobiol. (2003) 70:83–244. doi: 10.1016/S0301-0082(03)00087-X
6. Murphy A, Dursun S, McKie S, Elliott R, and Deakin JF. An investigation into aripiprazole’s partial D2 agonist effects within the dorsolateral prefrontal cortex during working memory in healthy volunteers. Psychopharmacol (Berl). (2016) 233:1415–26. doi: 10.1007/s00213-016-4234-9
7. Lee JS, Lee JD, Park H-J, Oh M-K, Chun JW, Kim S-J, et al. Is the GABA system related to the social competence improvement effect of aripiprazole? An (18)F-fluoroflumazenil PET study. Psychiatry Investig. (2013) 10:75–80. doi: 10.4306/pi.2013.10.1.75
8. Hahn M and Roll SC. Dosing recommendations of aripiprazole depot with strong cytochrome P450 3A4 inhibitors: A relapse risk. Drug Saf Case Rep. (2016) 3:5. doi: 10.1007/s40800-016-0027-7
9. Favaretto E, Bedani F, Brancati GE, De Berardis D, Giovannini S, Scarcella L, et al. Synthesising 30 years of clinical experience and scientific insight on affective temperaments in psychiatric disorders: State of the art. J Affect Disord. (2024) 362:406–415. doi: 10.1016/j.jad.2024.07.011
10. Burnette EM, Nieto SJ, Grodin EN, Meredith LR, Hurley B, Miotto K, et al. Novel agents for the pharmacological treatment of alcohol use disorder. Drugs. (2022) 82:251–74. doi: 10.1007/s40265-021-01670-3
11. Coles AS, Knezevic D, George TP, Correll CU, Kane JM, and Castle D. Long-acting injectable antipsychotic treatment in schizophrenia and co- occurring substance use disorders: A systematic review. Front Psychiatry. (2021) 12:808002. doi: 10.3389/fpsyt.2021.808002
12. Szerman N, Basurte-Villamor I, Vega P, Martinez-Raga J, Parro-Torres C, Cambra Almerge J, et al. Once-monthly long-acting injectable aripiprazole for the treatment of patients with schizophrenia and co-occurring substance use disorders: A multicentre, observational study. Drugs Real World Outcomes. (2020) 7:75–83. doi: 10.1007/s40801-020-00178-8
13. Potempa C and Rychlik R. Hospitalization rates and resource utilization of schizophrenic patients switched from oral antipsychotics to aripiprazole-depot in Germany. Health Econ Rev. (2018) 8:30. doi: 10.1186/s13561-018-0215-5
14. Sampogna G, Di Vincenzo M, Giuliani L, Menculini G, Mancuso E, Arsenio E, et al. A systematic review on the effectiveness of antipsychotic drugs on the quality of life of patients with schizophrenia. Brain Sci. (2023) 13:1577. doi: 10.3390/brainsci13111577
15. Ingman K, Kupila J, Hyytia P, et al. Effects of aripiprazole on alcohol intake in an animal model of high-alcohol drinking. Alcohol. (2006) 41:391–8. doi: 10.1093/alcalc/agl037
Keywords: aripiprazole, long -acting treatment, serious mental illness (SMI), psychosis, quality of life, hospitalizations, functionality, substance use disorder (SUD)
Citation: Koiliari EI, Mouzas I, Alevizopoulos G, Lesch O, Walter H and Pasparakis EL (2025) Better treatment outcomes with aripiprazole long-acting injection in community and incarcerated patients with serious mental illness. Front. Psychiatry 16:1499400. doi: 10.3389/fpsyt.2025.1499400
Received: 20 September 2024; Accepted: 21 July 2025;
Published: 08 August 2025.
Edited by:
Roberto Ciccocioppo, University of Camerino, ItalyReviewed by:
Vassilis Martiadis, Department of Mental Health, ItalyNazzareno Cannella, University of Camerino, Italy
Copyright © 2025 Koiliari, Mouzas, Alevizopoulos, Lesch, Walter and Pasparakis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Erasmia I. Koiliari, ZWlrb2lsaWFyaUBnbWFpbC5jb20=; Emmanouil L. Pasparakis, ZW1tYW5vdWlscGFzcGFyYWtpc0BnbWFpbC5jb20=
 Erasmia I. Koiliari
Erasmia I. Koiliari Ioannis Mouzas
Ioannis Mouzas Georgios Alevizopoulos
Georgios Alevizopoulos Otto Lesch
Otto Lesch Henriette Walter
Henriette Walter Emmanouil L. Pasparakis
Emmanouil L. Pasparakis