- 1School of Public Administration (School of Philanthropy), Shandong Technology and Business University, Yantai, China
- 2Department of Social Welfare, Jeonbuk National University, Jeonju, Republic of Korea
Introduction: Depressive symptoms among older adults are a growing public health concern, particularly in rapidly aging populations like China. Functional limitations, commonly experienced with advancing age, have been shown to exacerbate depressive symptoms.
Methods: This study investigates the moderating effects of sociodemographic factors (including individual, familial, and society) on the association between functional limitations and depressive symptoms among Chinese older adults, using data from the 2018 Chinese Longitudinal Healthy Longevity Survey (CLHLS). The sample included 9,354 adults aged 65 and above.
Results: Results indicate that age group, living arrangement, and region significantly moderate the relationship between functional limitations and depressive symptoms. Specifically, functional limitations have a greater impact on depressive symptoms among the "young-old" compared to the "oldest-old," are more pronounced among those living alone versus with family, and affect rural residents more than urban ones.
Discussion: These findings underscore the need for targeted interventions that address these moderating factors to improve mental health outcomes among older Chinese adults.
1 Introduction
Depressive symptoms are a pervasive mental health concern that disproportionately affects the older adult population, significantly diminishing their overall well-being and quality of life (1, 2). This heightened vulnerability to depressive symptoms in older adults is frequently associated with the increasing prevalence of functional limitations within this demographic (3). Functional limitations refer to difficulties in performing everyday activities due to physical, cognitive, or sensory impairments, which tend to accumulate with age (4). These limitations often encompass both basic activities of daily living (ADLs)—such as eating, dressing, and bathing—and more complex instrumental activities of daily living (IADLs), including tasks like managing finances, preparing meals, or shopping (5). As these limitations worsen, they not only impede an individual’s ability to live independently but also contribute to a heightened risk of mental health issues, particularly depressive symptoms (6). Given the significant impact that depressive symptoms have on both mental and physical health, understanding how functional limitations contribute to depressive symptoms is vital for informing interventions and public health policies aimed at improving the lives of older adults.
A large body of research consistently demonstrates a robust association between functional limitations and depressive symptoms in older adults, underlining the substantial influence of physical health on mental well-being in later life (4, 7, 8). Functional limitations often stem from chronic illnesses or age-related conditions, including arthritis, cardiovascular disease, sensory impairments, and neurological disorders, which reduce the ability of older individuals to engage independently in routine activities, fostering a sense of dependency and loss of autonomy (9). The psychological burden associated with losing independence frequently leads to a decline in self-esteem, feelings of helplessness, and increased anxiety, ultimately resulting in depressive symptoms (10). This loss of autonomy significantly heightens emotional distress among older adults, as it often leads to increased social isolation and reduced participation in community activities, exacerbating depressive symptoms (11, 12). Functional impairments further contribute to emotional and psychological burdens for older adults, particularly as these limitations become cumulative over time and lead to increased reliance on others for daily activities (13). As these challenges accumulate, they underscore the importance of addressing social and mental health interventions tailored to mitigate the adverse effects of functional decline on emotional well-being in older populations.
The relationship between functional limitations and depressive symptoms, however, is not uniform and can vary significantly depending on several sociodemographic factors, including age, gender, residence, and socioeconomic status (14). These factors can either exacerbate or mitigate the impact of functional impairments on mental health, creating a complex and multifaceted association. For example, studies indicate that women often experience a stronger association between functional limitations and depressive symptoms compared to men, potentially due to differences in social roles, caregiving responsibilities, and coping mechanisms (15). Women, particularly those who have traditionally served as caregivers, may experience a more pronounced sense of loss when their independence is compromised, leading to heightened psychological distress and vulnerability to depressive symptoms. Similarly, older adults with lower socioeconomic status face greater psychological challenges related to functional limitations, as restricted financial resources often limit their access to healthcare, social support services, and resources that could alleviate their physical and mental health burdens (16).
In China, urban-rural disparities introduce an additional layer of complexity to this relationship (17, 18). Older adults in rural areas frequently encounter barriers to accessing healthcare and social services, which can amplify the mental health impacts of physical impairments, while their urban counterparts may benefit from better healthcare infrastructure and more available support networks (19). Rural older adults may rely heavily on family support due to limited public health resources, which places an additional burden on families and may increase the psychological stress associated with physical limitations (20). In contrast, urban residents may have greater access to medical facilities, mental health professionals, and social programs designed to support older adults, allowing for more effective management of both functional limitations and mental health needs (20). Thus, the urban-rural divide in healthcare access plays a critical role in shaping the experience of functional impairments and their mental health implications in the aging population (21).
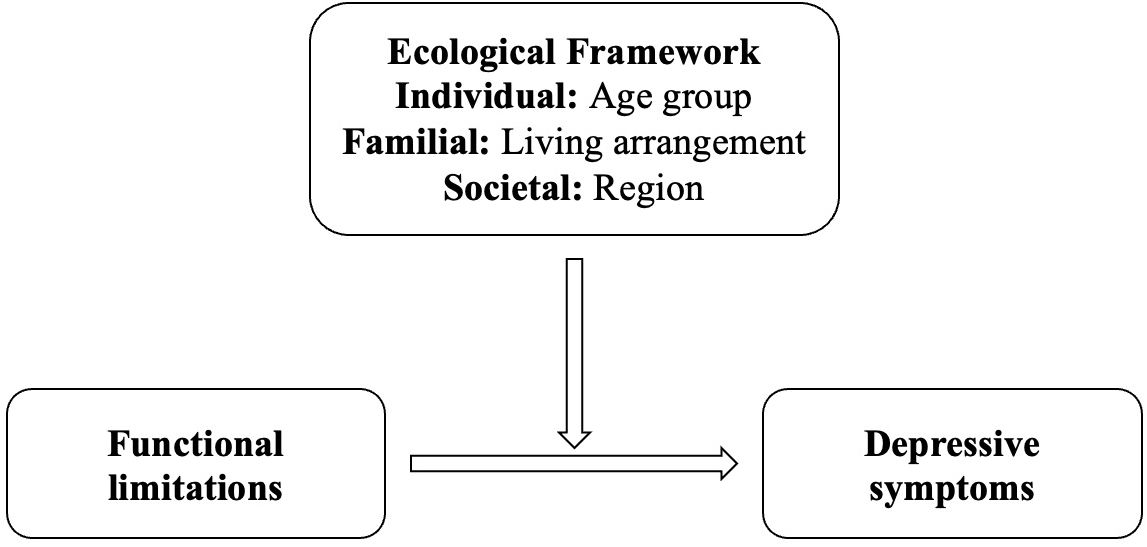
The Ecological Model of Health Behavior, as originally proposed by Bronfenbrenner (22), delineates five hierarchical levels of influence on health: individual, interpersonal, organizational, community, and policy (societal). However, in empirical research and applied intervention studies, this model is frequently conceptually condensed into three primary levels to facilitate analytical clarity and practical application. These commonly adopted tiers include: the individual level (e.g., biological and personal factors), the interpersonal or familial level (e.g., social relationships and household dynamics), and the societal or structural level (e.g., institutional resources, community context, and policy environment). This tripartite framework is especially useful in public health research for identifying multilevel intervention targets and understanding how health outcomes are shaped by nested environmental systems.
This study adopts a tripartite ecological framework grounded in Bronfenbrenner’s ecological systems theory (1979), and further informed by McLeroy et al.’s (23) ecological model of health promotion. While the original ecological theory includes multiple nested systems, contemporary health behavior research often categorizes them into three analytically tractable layers—individual, familial, and societal (24, 25). These levels allow for a nuanced analysis of how personal characteristics (e.g., age), family context (e.g., living arrangement), and social-structural environment (e.g., urban-rural region) interact to influence mental health outcomes among older adults. Building on this theoretical framework, the present study examines how specific sociodemographic characteristics—categorized across individual, familial, and societal domains—moderate the relationship between functional limitations and depressive symptoms in later life.
The role of sociodemographic factors such as age, residence, and living arrangements in the relationship between functional limitations and depressive symptoms highlights the need for a nuanced understanding of how these factors intersect with health outcomes in the aging population (26, 27). Age itself is a critical factor, as functional limitations and the severity of depressive symptoms tend to increase with age, compounding the impact on overall well-being, with older adults often experiencing multiple chronic conditions that exacerbate functional limitations and contribute to higher levels of depressive symptoms (3, 16). Additionally, social isolation frequently accompanies aging, further increasing the risk of depressive symptoms, particularly in rural areas where limited social support and healthcare resources are common (28). Urban-rural differences also shape this association, as urban older adults generally have better access to healthcare and social services, whereas rural older adults often experience restricted access, intensifying the psychological effects of functional impairments (29). Living arrangements—whether living alone, with a spouse, or with extended family—impact both social and instrumental support levels, which can mediate the extent to which functional limitations contribute to depressive symptoms (30, 31). Socioeconomic status plays an equally crucial role, as higher income levels generally enable broader access to health services, assistive devices, and social engagement, all of which help mitigate the psychological impact of functional limitations (20).
Understanding the intricate relationship between functional limitations and depressive symptoms, as well as the moderating effects of sociodemographic factors, is essential for developing effective support systems and targeted interventions (32). By recognizing the impact of functional limitations on mental health outcomes, healthcare providers and policymakers can create interventions tailored to the unique needs of older adults facing these impairments, which can be particularly effective given the increasing prevalence of functional limitations in aging populations (33). For instance, enhancing access to assistive technologies, mental health support services, and programs encouraging social engagement has been shown to reduce the psychological burden of functional limitations and significantly improve quality of life among older adults. Additionally, addressing underlying sociodemographic inequalities in healthcare access and support systems is crucial to ensuring that interventions reach the most vulnerable groups, including those in rural or low-income areas, who often experience compounded challenges related to both physical impairments and limited social resources (34).
The extensive evidence linking functional limitations and depressive symptoms among older adults, while well-documented, highlights the need for further exploration of sociodemographic moderators that could refine our understanding of this connection (35, 36, 59). Variables such as gender, age, education, and socioeconomic status have shown potential as moderators of the effects of functional limitations on depressive symptoms. Understanding how these factors interact with functional limitations to influence depressive symptoms could offer valuable insights into the mental health disparities observed among older adults (37). For example, educational attainment might equip individuals with better coping strategies and greater awareness of available resources, potentially mitigating some of the depressive symptoms associated with functional limitations. Similarly, individuals with higher socioeconomic status may experience fewer psychological burdens associated with functional impairments due to enhanced access to healthcare services, assistive devices, and social support networks. This study investigates the moderating effects of sociodemographic factors selected through a tripartite ecological framework encompassing individual (age group), familial (living arrangement), and societal (urban-rural region) levels on the association between functional limitations and depressive symptoms among Chinese older adults (22).
This study aims to examine the moderating effects of sociodemographic factors on the relationship between functional limitations and depressive symptoms among older Chinese adults. By investigating these interactions, we seek to identify specific subgroups that may be at greater risk of experiencing depressive symptoms in the presence of functional limitations. The findings from this research are expected to deepen our understanding of the complex interactions between physical health, sociodemographic characteristics, and mental well-being in aging populations. This knowledge will be instrumental in developing culturally and contextually appropriate interventions and healthcare policies, ultimately improving mental health outcomes for vulnerable subgroups within the older adult population.
By addressing the role of sociodemographic factors, this study contributes to a more comprehensive understanding of the multifaceted influences on depressive symptoms among older adults facing functional limitations. Through insights gained from this research, healthcare providers, policymakers, and caregivers will be better equipped to design targeted interventions that recognize and address the unique needs of this population. Such interventions are critical in enhancing the quality of life, promoting mental well-being, and ensuring equitable access to care and support for older adults, particularly in the context of an aging society where functional limitations and mental health issues are increasingly prevalent.
2 Methods
2.1 Data and study population
We utilized data from the Chinese Longitudinal Healthy Longevity Survey (CLHLS), a large-scale, ongoing prospective cohort study that covers 23 of China’s 31 provinces. The CLHLS was established in 1998 to investigate factors influencing healthy aging and longevity among the Chinese population, making it one of the most comprehensive longitudinal studies on aging in China. This cohort study has had subsequent follow-ups and participant recruitment waves in 2000, 2002, 2005, 2008, 2011, 2014, and 2018. Detailed information on the study design, sampling, and methodology has been documented extensively in prior publications (38).
For the present analysis, we included data from the most recent follow-up wave in 2018, which allowed us to examine the transitions in health and well-being over this four-year period. The CLHLS collects a wide array of data, including sociodemographic characteristics, lifestyle factors, cognitive and physical health assessments, and functional and psychological well-being, thus providing a robust foundation for analyzing factors that influence aging outcomes in older Chinese adults.
This study received approval from the Research Ethics Committee of Peking University (IRB00001052-13074), and all participants or their legal representatives provided informed consent through a signed form, confirming their willingness to participate in the baseline and follow-up surveys.
After excluding participants with missing data, a final sample of 9,354 older adults aged 65 years and above was included in this analysis. This large sample enhances the statistical power of our study and allows for a more precise estimation of associations related to aging and health outcomes in the Chinese population.
2.2 Measurements
2.2.1 Dependent variable
The dependent variable was depressive symptoms measured using the 10-item Center for Epidemiologic Studies Depression Scale (CES-D-10) (39). This scale is a widely used survey tool to measure depressive symptoms among Chinese older adults, with good validity and reliability. All items are rated on a four-point scale, from “rarely” to “on some days” (1–2 days), “occasionally” (3–4 days), or “most of the time” (5–7 days). We scored the responses of “rarely,” “on some days” (1–2 days), “occasionally” (3–4 days), and “most of the time” (5–7 days) as 0, 1, 2, and 3, respectively, after we reversely coded the responses to two positive questions— “I was happy” and “I felt hopeful about the future.” The total range of CES-D-10 scores is 0–30, with higher scores indicating a greater severity of depressive symptoms. The well-validated cutoff value is 10 in measuring depressive symptoms among Chinese older populations (40, 41); therefore, participants with a score ≥ 10 on the CES-D-10 were considered to have depressive symptoms.
2.2.2 Independent variable
In this study, the independent variable is functional limitations, which refer to reductions in the capacity to engage in activities of daily living (ADLs) or instrumental activities of daily living (IADLs) due to physical, cognitive, or emotional challenges. Within the CLHLS questionnaire, participants’ ADLs were evaluated based on their reported difficulty in performing tasks such as dressing, bathing/showering, eating, getting into or out of bed, using the toilet, and controlling urination and defecation. For each of these six tasks, participants were provided with the following response options: (1) no, I do not have any difficulty; (2) I have difficulty but can still manage; (3) yes, I have difficulty and require assistance; (4) I am unable to perform the task. Consistent with the approach employed by Zhang et al. (60), We scored the responses of “(1) no, I do not have any difficulty,” “(2) I have difficulty but can still manage”, “(3) yes, I have difficulty and require assistance”, and “(4) I am unable to perform the task” as 0, 1, 2, and 3. By aggregating responses to these six tasks, we obtained ADL limitations ranging from 0-18. Regarding IADLs, participants were queried about their difficulty in preparing hot meals, shopping for groceries, making phone calls, taking medication, and managing money. Following the same operationalization as ADLs, we obtained IADL limitations ranging from 0-15. We collectively refer to ADL and IADL limitations as functional limitations, with a range from 0 to 33.
2.2.3 Moderating variables
This study examines three key sociodemographic moderating factors—age group, living arrangement, and region—that reflect individual, familial, and society relevant to aging outcomes. By categorizing age into “young-old” (65–74), “old-old” (75-84) and “oldest old” (85+), differentiating living arrangements between those living alone versus with family, and distinguishing between urban and rural regions, the study seeks to reveal how these contextual variables shape health and well-being among older adults.
2.2.4 Control variables
Control variables in this study included a range of demographic factors such as age, gender, marital status, household income, and perceived social stratification. Age, gender, and marital status provide insights into basic sociodemographic profiles that can influence health outcomes and psychological well-being. Household income, a crucial socioeconomic indicator, reflects the material resources available to individuals and can impact access to healthcare, social services, and general quality of life among older adults. Perceived social stratification was assessed through a single-item measure that captures an individual’s self-reported economic standing relative to others in their neighborhood. Respondents were asked, “How would you rate your economic status compared to other people in your neighborhood?” with responses ranging from 1 (“very rich”) to 5 (“very poor”). This self-assessment allows for the examination of subjective socioeconomic status, which has been shown to be a meaningful predictor of health outcomes, as it often reflects perceived social inequality and related stressors (42, 43). Including these control variables helps to account for underlying demographic and socioeconomic influences that may affect the primary variables under study, thus improving the robustness of the analysis.
2.3 Data analysis
The present study was primarily carried out to investigate the effect of functional limitations on depressive symptoms among older Chinese adults, and the potential moderating role of sociodemographic factors were also explored (Figure 1). To accomplish this, statistical analysis was conducted using STATA 17 software. Specifically, a three-step analytical approach was employed. Firstly, descriptive analysis was performed to illustrate the general characteristics of the study population, generating a summary of the relevant demographic and clinical variables, such as age, gender, region, and marital status. Secondly, correlation analysis was utilized to examine the relationships between the key study variables, namely functional limitations, depressive symptoms, and sociodemographic factors, so as to assess the strength and direction of these relationships, and to identify any potential confounding factors that might affect the main study outcomes. Finally, regression analysis was employed to investigate the impact of interaction terms (i.e. moderating effects) on depressive symptoms, while controlling for potential confounding factors identified during the correlation analysis stage, for which, a series of regression models were constructed to examine the main and interactive effects of functional limitations, sociodemographic factors, and other relevant covariates on depressive symptoms. Overall, this analytical approach allowed for a thorough examination of the research questions and provided valuable insights into the role of functional limitations and sociodemographic factors in depressive symptoms among older Chinese adults.
3 Results
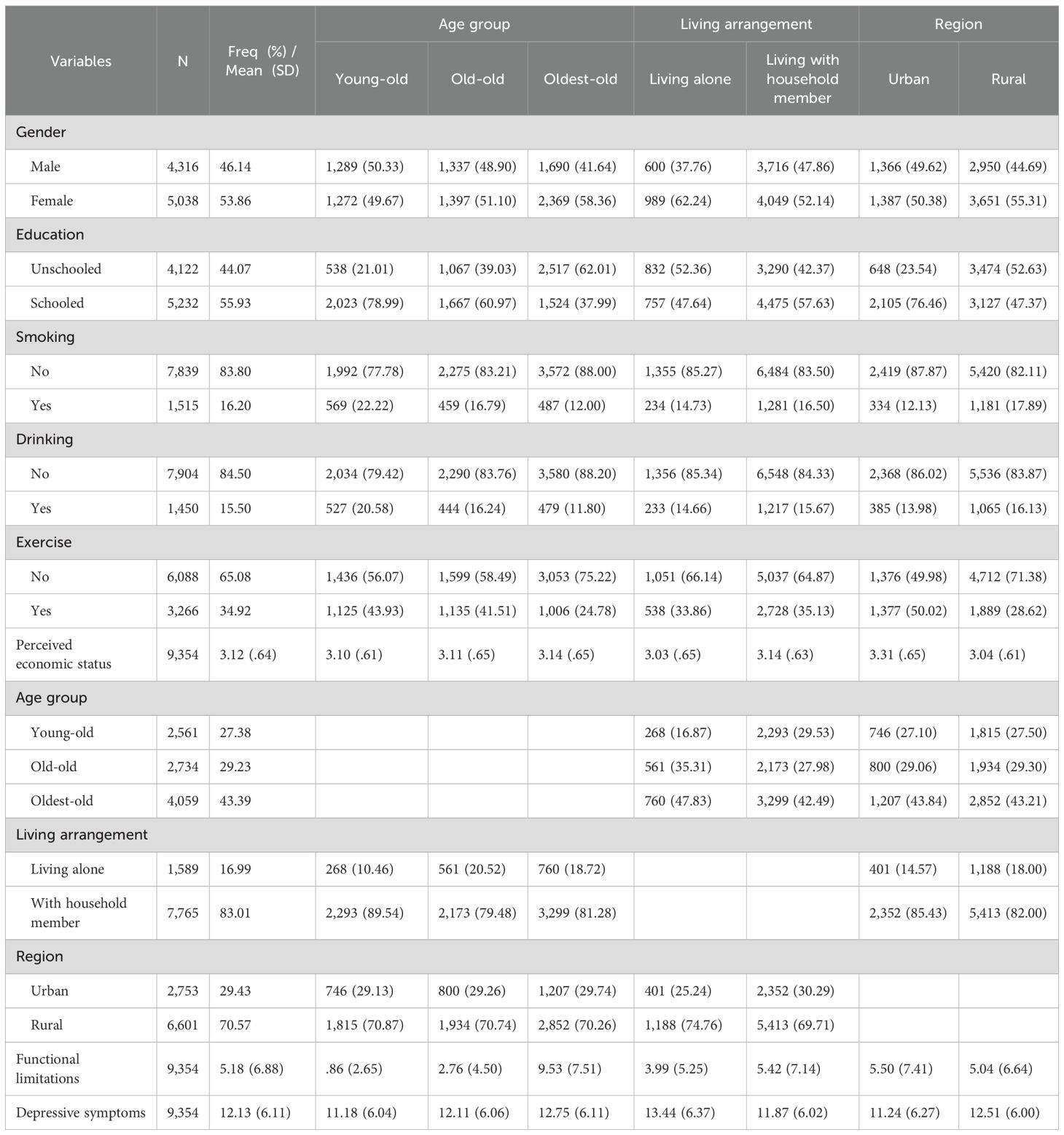
3.1 Characteristics of the study population
The sample characteristics in Table 1 reveal significant sociodemographic, health behavior, and health status variations among 9,354 older Chinese adults. The majority are female (53.86%) and “oldest-old” (43.39%), with women more likely to live alone, particularly in rural areas where functional limitations and depressive symptoms are more prevalent. Education levels differ substantially between age groups and regions; only 44.07% are unschooled, with a greater proportion of educated individuals in the younger elderly group and urban areas. Most participants are nonsmokers (83.80%) and nondrinkers (84.50%), with rural residents and younger elderly individuals more likely to report smoking and drinking. Regular exercise is reported by 34.92%, with higher rates among urban residents and the younger elderly. Perceived economic status, a key subjective socioeconomic indicator, is higher among urban residents and those living with family, while those living alone and rural participants report slightly lower perceived economic status. Functional limitations average 5.18, with higher levels among the old elderly and rural residents. Depression scores are similarly elevated in rural areas and among those living alone, emphasizing the health vulnerabilities within specific subgroups. These patterns underscore the importance of targeted health and support interventions for older Chinese adults, particularly those in rural settings or experiencing social isolation.
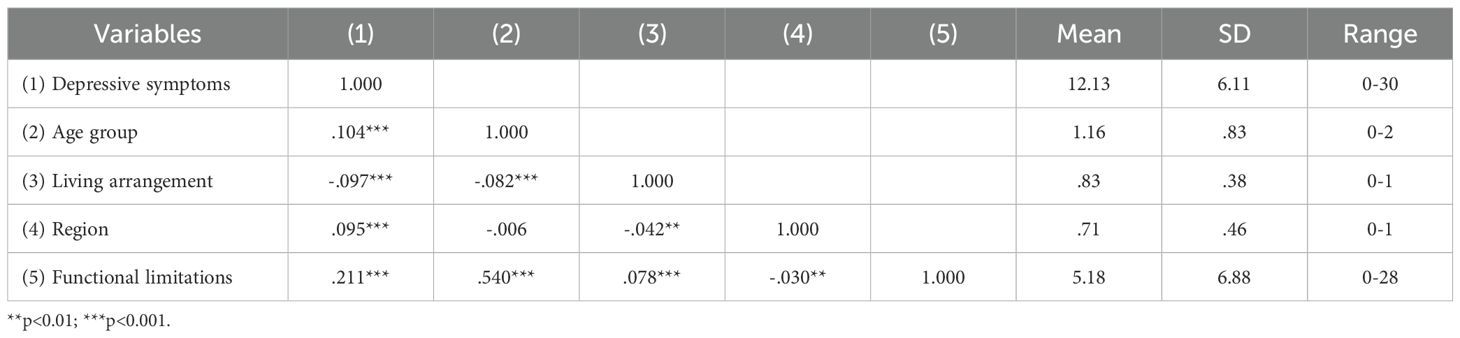
3.2 Correlation of the main variables
Table 2 presents the correlations between the main variables, including depressive symptoms, age group, living arrangement, region, and functional limitations. depressive symptoms show a positive correlation with both age group (r = 1.104, p <.001) and region (r = .095, p <.001), suggesting that depressive symptoms are slightly higher among the “oldest- old” (85+) and rural residents. depressive symptoms also demonstrate a moderate positive correlation with functional limitations (r = .211, p <.001), indicating that greater physical limitations are associated with higher depressive symptoms. Conversely, a negative correlation is observed between depressive symptoms and living arrangement (r = -.097, p <.001), implying that individuals living alone tend to report higher levels of depressive symptoms.
Functional limitations show the strongest correlation with age group (r = .540, p <.001), highlighting that physical limitations are more common among older participants. Functional limitations are also positively correlated with living arrangement (r = .078, p <.001) and negatively with region (r = -.030, p <.01), suggesting that limitations are more pronounced among those living alone and slightly lower among rural residents. Additionally, age group and living arrangement exhibit a negative correlation (r = -.082, p <.001), indicating that older participants are more likely to live with family members. Overall, the correlations suggest that age, living arrangement, region, and functional limitations are interrelated and may collectively impact depression levels among older adults.
3.3 Moderation model
Table 3 presents the moderation analysis of sociodemographic factors (age group, living arrangement, and region) on the relationship between functional limitations and depressive symptoms. The models progressively incorporate these moderators and their interaction effects, allowing for a nuanced examination of how sociodemographic factors influence the association between functional limitations and depressive symptoms. The F-values in Table 3 indicate the overall fit and statistical significance of each model in explaining the relationship between functional limitations and depressive symptoms, with sociodemographic moderators included. Each model displays a statistically significant F-value (p < 0.001), suggesting that the variables collectively explain a meaningful portion of the variance in depressive symptoms among older adults.
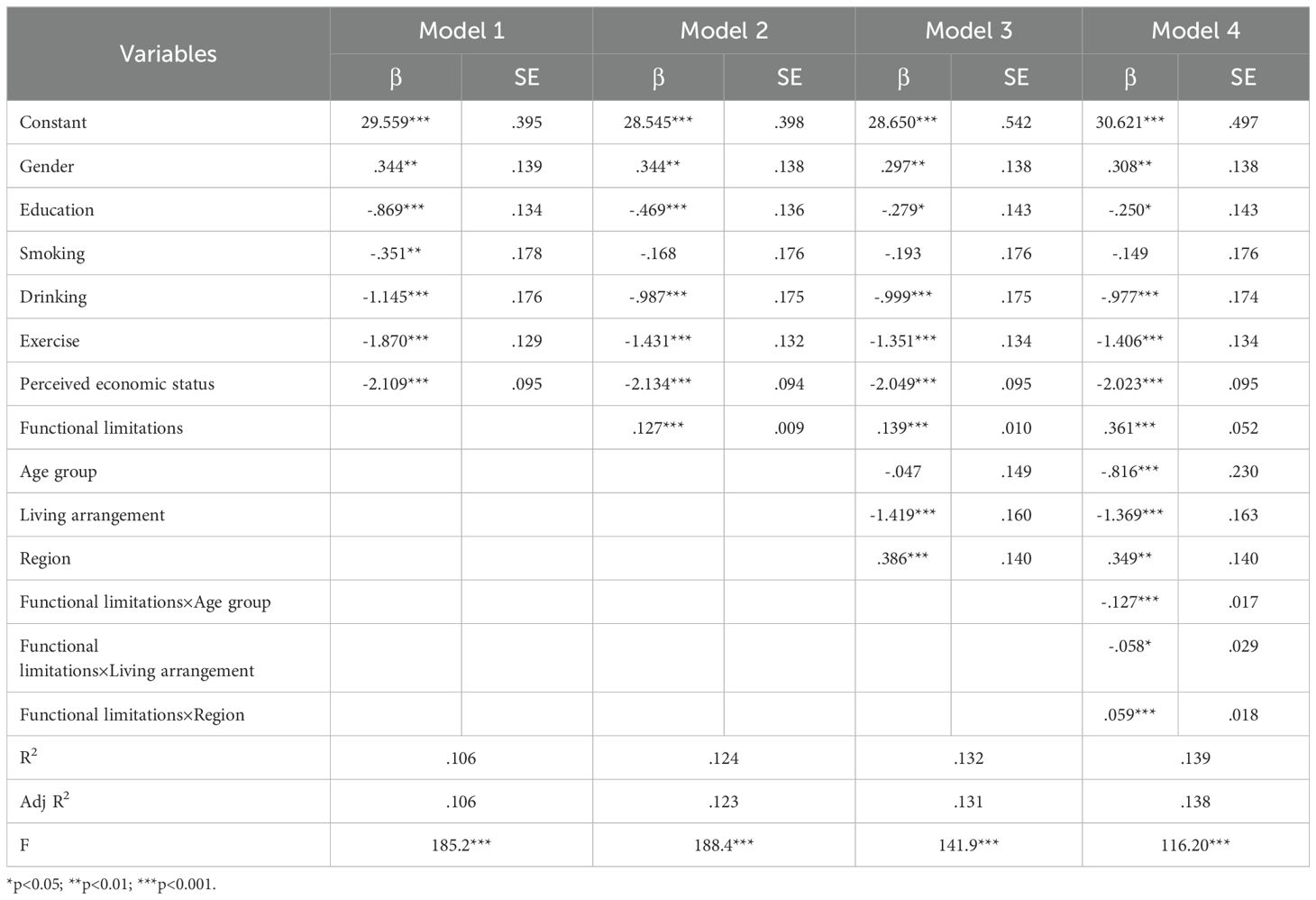
Table 3. Moderation analysis of sociodemographic factors on the relationship between functional limitations and depressive symptoms.
In Model 1, baseline demographic variables (gender, education, smoking, drinking, exercise, and perceived economic status) are included. Gender and perceived economic status show significant effects on depressive symptoms, with women and those perceiving a lower economic status reporting higher depression scores. Education, exercise, and drinking are negatively associated with depressive symptoms, suggesting that higher educational attainment, physical activity, and alcohol consumption are linked to lower levels of depressive symptoms. This model explains 10.6% of the variance in depression scores (R² = .106, p <.001).
In Model 2, functional limitations are added, demonstrating a significant positive association (β = .127, SE = .009, p <.001), indicating that higher levels of functional limitations are associated with increased depressive symptoms. This model slightly improves the explained variance (R² = .124).
Model 3 incorporates the sociodemographic factors age group, living arrangement, and region. The results reveal significant effects for living arrangement (β = -1.419, SE = .160, p <.001) and region (β = .386, SE = .140, p <.01). Older adults living alone report higher depression scores, while those in rural regions also show increased depressive symptoms. The inclusion of these moderators further increases the model’s explanatory power (R² = .132).
Finally, Model 4 includes interaction terms between functional limitations and each sociodemographic factor to test for moderation effects. The results confirm significant interaction effects between functional limitations and age group (β = -.127, SE = .017, p <.001), living arrangement (β = -.058, SE = .029, p <.01), and region (β = .059, SE = .018, p <.001). These interactions indicate that the impact of functional limitations on depressive symptoms varies by sociodemographic context: the association is stronger in younger elderly, those living alone, and individuals in rural regions. Model 4 explains the highest variance in depression scores, with an R² of.139.
The specific moderating effects are as follows. First, within the age group variable, functional limitations have a greater impact on depressive symptoms among the “young-old” compared to the “oldest-old,” as shown in Figure 2. Second, for living arrangements, the effect of functional limitations on depressive symptoms is more pronounced among older adults living alone than among those residing with family members, as illustrated in Figure 3. Finally, in terms of region, functional limitations have a stronger effect on depressive symptoms among rural older adults than their urban counterparts, as depicted in Figure 4. Overall, the findings suggest that sociodemographic factors such as age group, living arrangement, and region significantly moderate the relationship between functional limitations and depressive symptoms among older Chinese adults.
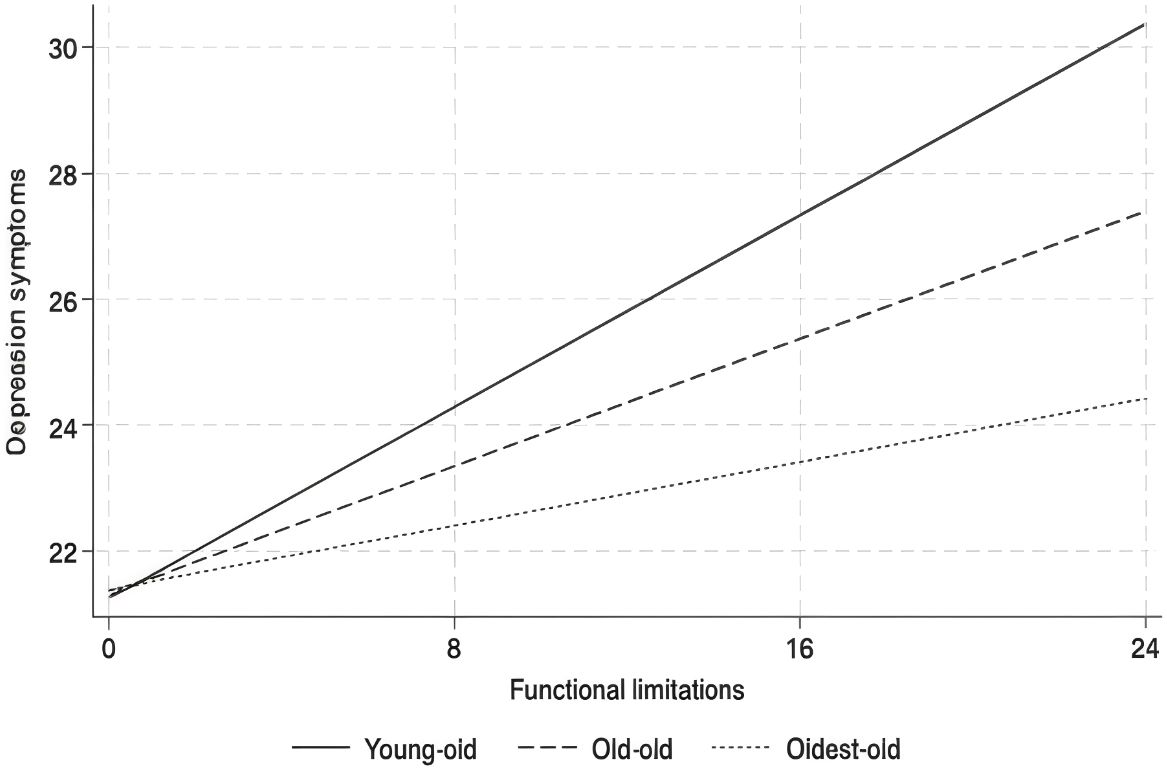
Figure 2. Moderation analysis of the interaction between functional limitations and age group on depressive symptoms.
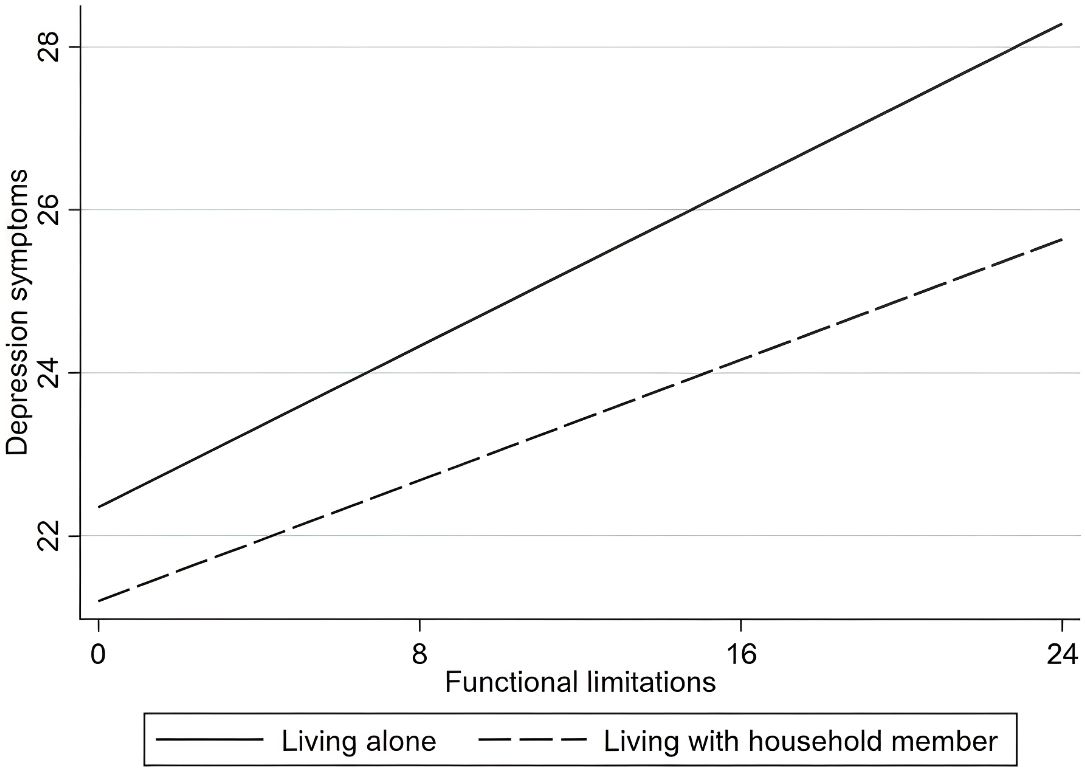
Figure 3. Moderation analysis of the interaction between functional limitations and living arrangement on depressive symptoms.
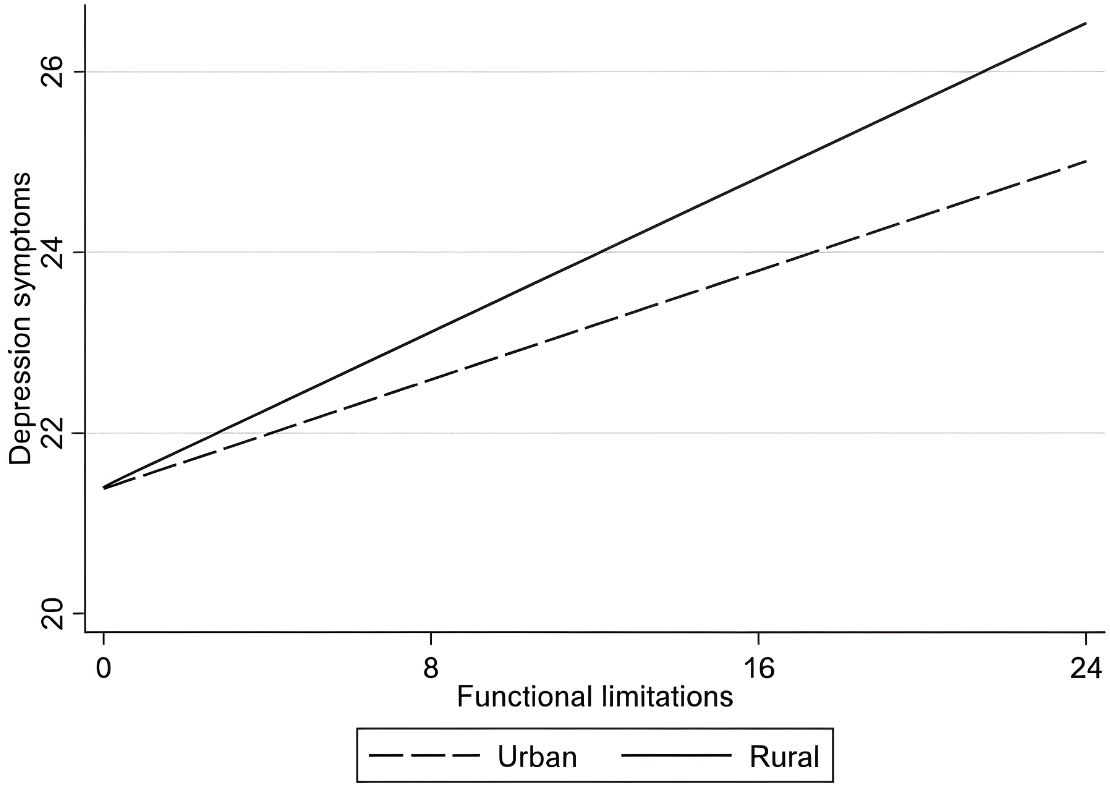
Figure 4. Moderation analysis of the interaction between functional limitations and region on depressive symptoms.
4 Discussion
This study investigates how sociodemographic factors—specifically age group, living arrangement, and region—moderate the relationship between functional limitations and depressive symptoms among older Chinese adults. The findings reveal nuanced interactions between these variables, demonstrating that sociodemographic contexts significantly shape how functional limitations influence depressive symptoms. Below, we discuss the implications of each moderating variable in the context of existing literature, the potential mechanisms driving these effects, and the broader implications for interventions and policy.
The results indicate that the impact of functional limitations on depressive symptoms is more pronounced among the “young-old” (65–74) compared to the “old-old” (75-84) and “oldest-old” (85+), aligning with evidence that younger older adults may experience greater psychological distress from functional decline due to a disruption of previously active lifestyles (44, 45). This contrast suggests that while the young-old often view these limitations as unexpected, the old-old and oldest-old may have adjusted to age-related changes, seeing physical decline as a natural part of aging and, therefore, experiencing less associated psychological distress (46, 47). This age-related moderation underscores the need for tailored interventions: younger older adults could benefit from initiatives focusing on preserving autonomy through physical rehabilitation, mobility aids, and assistive technologies designed to maintain independence (48). For the old-old, support should emphasize social and psychological resilience, helping them cope with age-related limitations while fostering emotional well-being through social support networks (49). Addressing these age-specific needs may optimize mental health outcomes for both age groups by recognizing and catering to their distinct perceptions and experiences of functional limitations.
The findings further reveal that functional limitations have a stronger impact on depressive symptoms among those living alone compared to those living with family (50). This result is consistent with prior research emphasizing the buffering effect of social support against depressive symptoms (51). Family members often provide practical assistance with daily tasks, emotional support, and companionship, all of which can mitigate the depressive impact of functional limitations (52). For older adults living alone, however, functional limitations may exacerbate feelings of loneliness, helplessness, and isolation, which are closely linked to depressive symptoms (53). This finding underscores the importance of social support systems and suggests that policies should focus on enhancing community and social services for older adults who live alone. Programs aimed at improving social interaction, such as volunteer and mentorship programs, could help reduce isolation and provide emotional support. Additionally, strengthening in-home care services and ensuring access to community centers for older adults living alone could alleviate the adverse effects of functional limitations on mental health.
Finally, the study highlights that functional limitations have a more substantial effect on depressive symptoms among rural older adults than urban ones. This finding can be attributed to disparities in healthcare infrastructure, accessibility to mental health resources, and social services between urban and rural areas in China (54). Rural residents may have fewer resources to manage physical limitations, limited access to mental health services, and reduced availability of community-based support, which together exacerbate the psychological toll of functional limitations. Addressing this regional disparity requires a focus on policy measures that enhance healthcare access and social support in rural areas. Policymakers should consider prioritizing rural healthcare funding, particularly for programs that target older adults with functional limitations. Community-based support networks and mobile healthcare units could bridge gaps in service delivery, bringing essential healthcare resources directly to rural communities. Additionally, telemedicine and mental health counseling services could provide accessible and affordable support for older adults in these areas, helping to mitigate the depressive effects associated with functional limitations.
The findings of this study have implications for theories that address the intersection of physical health and mental well-being in aging populations. The Life Course Theory, which emphasizes the influence of early life conditions and accumulated experiences on later-life health outcomes, may help explain why younger older adults exhibit greater distress in response to functional limitations than their older counterparts (55). For the young-old, functional limitations may signify a break from their previously active roles and aspirations, which can be psychologically unsettling. Resilience Theory further supports the idea that older adults living alone or in rural areas may lack the social and structural resources necessary to cope with the stress associated with functional decline, thereby heightening their risk of depressive symptoms (56, 57). These findings contribute to a nuanced understanding of how sociodemographic factors impact the association between physical limitations and depressive symptoms, suggesting that the relationship is not only a matter of individual health but is significantly shaped by social, familial, and environmental factors. Integrating these theories can provide a comprehensive framework for understanding the complex interactions between functional limitations and depressive symptoms in aging populations, particularly in culturally specific contexts like China.
From a practical perspective, this study highlights the need for targeted mental health interventions and social policies that address the sociodemographic diversity within the older adult population. First, healthcare practitioners working with Chinese older adults should consider the sociodemographic context when assessing and treating depressive symptoms in individuals with functional limitations. Tailored interventions that address specific needs based on age, living arrangement, and region can improve mental health outcomes and promote overall well-being (58, 60). For younger older adults with functional limitations, practitioners could focus on empowering strategies that maintain their sense of autonomy and prevent a decline in psychological well-being. For older adults living alone, building robust social support networks through community initiatives could help alleviate feelings of loneliness and reduce the risk of depressive symptoms. Lastly, for rural residents, expanding access to healthcare resources and strengthening local support services are critical steps toward reducing health disparities and improving mental health among older adults. Policymakers should prioritize healthcare accessibility in rural areas, increase funding for mental health services, and foster community-based programs that support independent living for older adults. Additionally, policies that promote age-friendly environments—such as accessible transportation, safe housing, and community centers—can play an essential role in fostering healthy aging and reducing the negative mental health impacts associated with functional limitations.
While this study provides valuable insights into the moderating effects of sociodemographic factors, there are some limitations. First, the study’s reliance on self-reported measures may introduce bias, as older adults may underreport depressive symptoms or functional limitations due to social desirability or memory constraints. Future research could incorporate more objective measures, such as clinical assessments, to obtain a more accurate understanding of the impact of functional limitations on mental health. Additionally, this study focuses on cross-sectional data, limiting the ability to draw causal conclusions about the relationship between functional limitations and depressive symptoms. Longitudinal research could provide further insight into how this relationship evolves over time and how sociodemographic factors may impact this trajectory. Furthermore, given the focus on Chinese older adults, it would be beneficial to replicate this study in other cultural settings to assess the generalizability of these findings. While this study focused on three multilevel moderators, future research could examine additional factors (e.g., gender, education) using advanced modeling techniques. Nevertheless, our findings provide actionable insights for policymakers to design stratified interventions across individual, familial, and societal dimensions.
In conclusion, this study sheds light on the complex interplay between functional limitations and depressive symptoms among Chinese older adults, with sociodemographic factors playing a significant moderating role. Age group, living arrangement, and region each influence the strength of the relationship between functional limitations and depressive symptoms, underscoring the need for targeted interventions that consider the individual, familial, and society of aging. By focusing on the unique needs of subgroups within the older adult population, healthcare providers and policymakers can better support mental health and enhance quality of life in this vulnerable population.
5 Conclusion
This study investigated the role of sociodemographic moderators—age group, living arrangement, and region—in the relationship between functional limitations and depressive symptoms among Chinese older adults. The findings underscore that functional limitations have a differentiated impact on depressive symptoms depending on these key sociodemographic factors. Specifically, functional limitations are more strongly associated with depressive symptoms in the “young-old” group than in the “oldest-old,” suggesting that younger older adults may experience a sharper decline in mental well-being as physical impairments arise. Additionally, older adults living alone show a greater vulnerability to the depressive effects of functional limitations compared to those residing with family members, likely due to reduced social support. Regionally, rural older adults exhibit a stronger association between functional limitations and depressive symptoms than urban residents, highlighting the role of limited healthcare access and support services in rural areas.
Overall, the results indicate that sociodemographic factors significantly shape the psychological impact of functional limitations. These insights emphasize the need for targeted interventions that consider age, living arrangement, and regional differences, which can improve mental health outcomes by addressing the specific needs of diverse subgroups within China’s aging population.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: China Longitudinal Healthy Longevity Survey, https://opendata.pku.edu.cn/dataverse/CHADS.
Ethics statement
The studies involving humans were approved by Research Ethics Committee of Peking University (IRB00001052-13074). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HH: Methodology, Conceptualization, Data curation, Formal Analysis, Investigation, Software, Visualization, Writing – original draft. JY: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Software, Visualization, Writing – original draft. YY: Funding acquisition, Methodology, Project administration, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rodda J, Walker Z, and Carter J. Depression in older adults. Bmj. (2011) 343:d5291. doi: 10.1136/bmj.d5219
2. Haigh EA, Bogucki OE, Sigmon ST, and Blazer DG. Depression among older adults: a 20-year update on five common myths and misconceptions. Am J Geriatric Psychiatry. (2018) 26:107–22. doi: 10.1016/j.jagp.2017.06.011
3. Schieman S and Plickert G. Functional limitations and changes in levels of depression among older adults: A multiple-hierarchy stratification perspective. Journals Gerontol Ser B: psychol Sci Soc Sci. (2007) 62:S36–42. doi: 10.1093/geronb/62.1.S36
4. Geerlings SW, Beekman ATF, Deeg DJH, Twisk JWR, and Van Tilburg W. The longitudinal effect of depression on functional limitations and disability in older adults: an eight-wave prospective community-based study. psychol Med. (2001) 31:1361–71. doi: 10.1017/S0033291701004639
5. Katz S, Downs TD, Cash HR, and Grotz RC. Progress in development of the index of ADL. gerontologist. (1970) 10:20–30. doi: 10.1093/geront/10.1_Part_1.20
6. Dunlop DD, Semanik P, Song J, Manheim LM, Shih V, and Chang RW. Risk factors for functional decline in older adults with arthritis. Arthritis Rheumatism. (2005) 52:1274–82. doi: 10.1002/art.20968
7. Hybels CF, Pieper CF, and Blazer DG. The complex relationship between depressive symptoms and functional limitations in community-dwelling older adults: the impact of subthreshold depression. psychol Med. (2009) 39:1677–88. doi: 10.1017/S0033291709005650
8. Covinsky KE, Yaffe K, Lindquist K, Cherkasova E, Yelin E, and Blazer DG. Depressive symptoms in middle age and the development of later-life functional limitations: The long-term effect of depressive symptoms. J Am Geriatrics Soc. (2010) 58:551–6. doi: 10.1111/j.1532-5415.2010.02723.x
9. Dunlop DD, Lyons JS, Manheim LM, Song J, and Chang RW. Arthritis and heart disease as risk factors for major depression: the role of functional limitation. Med Care. (2004) 6:502–11. doi: 10.1097/01.mlr.0000127997.51128.81
10. Ahn J and Kim BJ. The relationships between functional limitation, depression, suicidal ideation, and coping in older Korean immigrants. J immigrant minority Health. (2015) 17:1643–53. doi: 10.1007/s10903-015-0204-2
11. Fakoya OA, McCorry NK, and Donnelly M. Loneliness and social isolation interventions for older adults: a scoping review of reviews. BMC Public Health. (2020) 20:1–14. doi: 10.1186/s12889-020-8251-6
12. Hawkley LC and Cacioppo JT. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Ann Behav Med. (2010) 40:218–27. doi: 10.1007/s12160-010-9210-8
13. Cudjoe TK, Roth DL, Szanton SL, Wolff JL, Boyd CM, and Thorpe RJ Jr. The epidemiology of social isolation: National health and aging trends study. Journals Gerontol: Ser B. (2020) 75:107–13. doi: 10.1093/geronb/gby037
14. Idaiani S and Indrawati L. Functional status in relation to depression among elderly individuals in Indonesia: a cross-sectional analysis of the Indonesian National Health Survey 2018 among elderly individuals. BMC Public Health. (2021) 21:2332. doi: 10.1186/s12889-021-12260-z
15. Okun MA, August KJ, Rook KS, and Newsom JT. Does volunteering moderate the relation between functional limitations and mortality? Soc Sci Med. (2010) 71:1662–8. doi: 10.1016/j.socscimed.2010.07.034
16. Sánchez-Moreno E, Gallardo-Peralta L, Barrón López de Roda A, and Rivera Álvarez JM. Socioeconomic status, loneliness, and depression among older adults: a cross-sectional study in Spain. BMC geriatrics. (2024) 24:361. doi: 10.1186/s12877-024-04978-3
17. Zimmer Z, Wen M, and Kaneda T. A multi-level analysis of urban/rural and socioeconomic differences in functional health status transition among older Chinese. Soc Sci Med. (2010) 71:559–67. doi: 10.1016/j.socscimed.2010.03.048
18. Xu J, Wang J, King M, Liu R, Yu F, Xing J, et al. Rural–urban disparities in the utilization of mental health inpatient services in China: the role of health insurance. Int J Health economics Manage. (2018) 18:377–93. doi: 10.1007/s10754-018-9238-z
19. Cheng C, Yang CY, Inder K, and Wai-Chi Chan S. Urban–rural differences in mental health among Chinese patients with multiple chronic conditions. Int J Ment Health Nurs. (2020) 29:224–34. doi: 10.1111/inm.12666
20. Qin VM, McPake B, Raban MZ, Cowling TE, Alshamsan R, Chia KS, et al. Rural and urban differences in health system performance among older Chinese adults: cross-sectional analysis of a national sample. BMC Health Serv Res. (2020) 20:1–14. doi: 10.1186/s12913-020-05194-6
21. Reilly M. Health disparities and access to healthcare in rural vs. Urban areas. Theory Action. (2021) 14:6. doi: 10.3798/tia.1937-0237.2109
22. Bronfenbrenner U. The ecology of human development: Experiments by nature and design Vol. 352. Cambridge, Massachusetts: Harvard University Press (1979).
23. McLeroy KR, Bibeau D, Steckler A, and Glanz K. An ecological perspective on health promotion programs. Health Educ Q. (1988) 15:351–77. doi: 10.1177/109019818801500401
24. Krieger N. A glossary for social epidemiology. J Epidemiol Community Health. (2001) 55:693–700. doi: 10.1136/jech.55.10.693
25. Sallis JF, Owen N, and Fisher E. Ecological models of health behavior. In: Health behavior. (2015) 5:43–64. Burlington, Massachusetts, USA: Jones & Bartlett Learning.
26. Li LW, Liu J, Xu H, and Zhang Z. Understanding rural–urban differences in depressive symptoms among older adults in China. J Aging Health. (2016) 28:341–62. doi: 10.1177/0898264315591003
27. Ying M, Wang S, Bai C, and Li Y. Rural-urban differences in health outcomes, healthcare use, and expenditures among older adults under universal health insurance in China. PloS One. (2020) 15:e0240194. doi: 10.1371/journal.pone.0240194
28. Zhang X, Dupre ME, Qiu L, Zhou W, Zhao Y, and Gu D. Urban-rural differences in the association between access to healthcare and health outcomes among older adults in China. BMC geriatrics. (2017) 17:1–11. doi: 10.1186/s12877-017-0538-9
29. Sun J and Lyu S. Social participation and urban-rural disparity in mental health among older adults in China. J Affect Disord. (2020) 274:399–404. doi: 10.1016/j.jad.2020.05.091
30. Zhang Y, Liu Z, Zhang L, Zhu P, Wang X, and Huang Y. Association of living arrangements with depressive symptoms among older adults in China: a cross-sectional study. BMC Public Health. (2019) 19:1–10. doi: 10.1186/s12889-019-7350-8
31. Wu H and Liu Y. Association between living arrangements and psychological well-being among older adults in rural China: activities of daily living disability as a moderator. SAGE Open. (2023) 13:21582440231215635. doi: 10.1177/21582440231215635
32. Li M, Yang Y, Pang L, Wu M, Wang Z, Fu Y, et al. Gender-specific associations between activities of daily living disability and depressive symptoms among older adults in China: Evidence from the China Health and Retirement Longitudinal Study. Arch Psychiatr Nurs. (2019) 33:160–6. doi: 10.1016/j.apnu.2019.08.010
33. Djernes JK. Prevalence and predictors of depression in populations of elderly: a review. Acta Psychiatrica Scandinavica. (2006) 113:372–87. doi: 10.1111/j.1600-0447.2006.00770.x
34. Su D, Wu XN, Zhang YX, Li HP, Wang WL, Zhang JP, et al. Depression and social support between China’rural and urban empty-nest elderly. Arch gerontol geriatrics. (2012) 55:564–9. doi: 10.1016/j.archger.2012.06.006
35. Friedmann JM, Elasy T, and Jensen GL. The relationship between body mass index and self-reported functional limitation among older adults: a gender difference. J Am Geriatrics Soc. (2001) 49:398–403. doi: 10.1046/j.1532-5415.2001.49082.x
36. Prado L. D. D. S. D., Ramos MEK, Camargo JDC, Bertoncelo GL, Reginatto CC, and Siqueira LDO. Relationship between pain, functional limitations, dependence, depression and osteoarthritis in older adults. Fisioterapia em Movimento. (2023) 36:e36202. doi: 10.1590/fm.2023.36202
37. Agreli BF, Dias FA, dos Santos Ferreira PC, Gomes NC, and dos Santos Tavares DM. Functional disability and morbidities among the elderly people, according to socio-demographic conditions and indicative of depression. Investigación y educación en enfermería. (2017) 35:48–58. doi: 10.17533/udea.iee.v35n1a06
38. Zeng Y, Feng Q, Hesketh T, Christensen K, and Vaupel JW. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: a cohort study. Lancet. (2017) 389:1619–29. doi: 10.1016/S0140-6736(17)30548-2
39. Andresen EM, Malmgren JA, Carter WB, and Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. (1994) 10:77–84. doi: 10.1016/S0749-3797(18)30622-6
40. Cheng ST and Chan AC. The center for epidemiologic studies depression scale in older Chinese: thresholds for long and short forms. Int J Geriatric Psychiatry: A J Psychiatry late Life Allied Sci. (2005) 20:465–70. doi: 10.1002/gps.1314
41. Yao Y, Chen H, Chen L, Ju SY, Yang H, Zeng Y, et al. Type of tea consumption and depressive symptoms in Chinese older adults. BMC Geriatr. (2021) 21:331. doi: 10.1186/s12877-021-02203-z
42. Wang HX, Karp A, Winblad B, and Fratiglioni L. Late-life engagement in social and leisure activities is associated with a decreased risk of dementia: a longitudinal study from the Kungsholmen project. Am J Epidemiol. (2002) 155:1081–7. doi: 10.1093/aje/155.12.1081
43. Pei Z, Zhang J, Qin W, Hu F, Zhao Y, Zhang X, et al. Association between dietary patterns and depression in Chinese older adults: A longitudinal study based on CLHLS. Nutrients. (2022) 14:5230. doi: 10.3390/nu14245230
44. Kelley-Moore JA and Ferraro KF. A 3-D model of health decline: Disease, disability, and depression among Black and White older adults. J Health Soc Behav. (2005) 46:376–91. doi: 10.1177/002214650504600405
45. Everson-Rose SA, Skarupski KA, Bienias JL, Wilson RS, Evans DA, and De Leon CFM. Do depressive symptoms predict declines in physical performance in an elderly, biracial population? Psychosomatic Med. (2005) 67:609–15. doi: 10.1097/01.psy.0000170334.77508.35
46. Freyne A, Keogh F, Kelly M, and Wrigley M. A longitudinal study of depression in old age II: depression and physical disability. Irish J psychol Med. (2005) 22:94–100. doi: 10.1017/S0790966700009101
47. Van Gool CH, Kempen GI, Penninx BW, Deeg DJ, Beekman AT, and Van Eijk JTM. Impact of depression on disablement in late middle aged and older persons: results from the Longitudinal Aging Study Amsterdam. Soc Sci Med. (2005) 60:25–36. doi: 10.1016/j.socscimed.2004.04.021
48. Hamer M, Bates CJ, and Mishra GD. Depression, physical function, and risk of mortality: National Diet and Nutrition Survey in adults older than 65 years. Am J Geriatric Psychiatry. (2011) 19:72–8. doi: 10.1097/JGP.0b013e3181df465e
49. de Jonge P, Kempen GI, Sanderman R, Ranchor AV, van Jaarsveld CH, van Sonderen E, et al. Depressive symptoms in elderly patients after a somatic illness event: prevalence, persistence, and risk factors. Psychosomatics. (2006) 47:33–42. doi: 10.1176/appi.psy.47.1.33
50. Honjo K, Tani Y, Saito M, Sasaki Y, Kondo K, Kawachi I, et al. Living alone or with others and depressive symptoms, and effect modification by residential social cohesion among older adults in Japan: the JAGES longitudinal study. J Epidemiol. (2018) 28:315–22. doi: 10.2188/jea.JE20170065
51. Kim C, Chang EJ, and Kim CY. Regional differences in the effects of social relations on depression among Korean elderly and the moderating effect of living alone. J Prev Med Public Health. (2021) 54:441. doi: 10.3961/jpmph.21.337
52. De Ronchi D, Bellini F, Berardi D, Serretti A, Ferrari B, and Dalmonte E. Cognitive status, depressive symptoms, and health status as predictors of functional disability among elderly persons with low-to-moderate education: The Faenza Community Aging Study. Am J geriatric Psychiatry. (2005) 13:672–85. doi: 10.1097/00019442-200508000-00006
53. Lim EJ. Gender differences in the relationship between physical functioning and depressive symptoms in low-income older adults living alone. Nurs Health Sci. (2014) 16:381–6. doi: 10.1111/nhs.12119
54. Wang Y, Li Z, and Fu C. Urban-rural differences in the association between social activities and depressive symptoms among older adults in China: a cross-sectional study. BMC geriatrics. (2021) 21:1–11. doi: 10.1186/s12877-021-02541-y
55. Pudrovska T and Anikputa B. Early-life socioeconomic status and mortality in later life: an integration of four life-course mechanisms. . Journals Gerontol: Ser B. (2014) 69:451–60. doi: 10.1093/geronb/gbt122
56. Yang Y and Wen M. Psychological resilience and the onset of activity of daily living disability among older adults in China: A nationwide longitudinal analysis. Journals Gerontol Ser B: psychol Sci Soc Sci. (2014) 70:470–80. doi: 10.1093/geronb/gbu068
57. MacLeod S, Musich S, Hawkins K, Alsgaard K, and Wicker ER. The impact of resilience among older adults. Geriatric Nurs. (2016) 37:266–72. doi: 10.1016/j.gerinurse.2016.02.014
58. Luo J, Zhang X, Jin C, and Wang D. Inequality of access to health care among the urban elderly in northwestern China. Health Policy. (2009) 93:111–7. doi: 10.1016/j.healthpol.2009.06.003
59. Zhang S, Wang Q, Wang X, Qi K, Zhou Y, and Zhou C. Longitudinal relationship between sensory impairments and depressive symptoms in older adults: the mediating role of functional limitation. Depression Anxiety. (2022) 39:624–32. doi: 10.1002/da.23266
Keywords: functional limitations, depressive symptoms, age group, living arrangement, region, Chinese older adults
Citation: Hao H, Yue J and Yeo YH (2025) Sociodemographic moderators of the association between functional limitations and depressive symptoms among Chinese older adults. Front. Psychiatry 16:1509485. doi: 10.3389/fpsyt.2025.1509485
Received: 11 October 2024; Accepted: 22 July 2025;
Published: 13 August 2025.
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyReviewed by:
Alberto Sardella, University of Catania, ItalyCristiano Capurso, University of Foggia, Italy
Xuhong Li, City University of Hong Kong, Hong Kong SAR, China
Copyright © 2025 Hao, Yue and Yeo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yeong Hun Yeo, eWh5ZW8yQGdtYWlsLmNvbQ==
 Haijun Hao
Haijun Hao Junyue Yue
Junyue Yue Yeong Hun Yeo
Yeong Hun Yeo