- 1Department of Psychiatry, Psychotherapy and Psychosomatics, Psychiatric University Hospital, University of Zurich, Zurich, Switzerland
- 2Department of Psychiatry, University Hospitals Geneva, Geneva, Switzerland
- 3Faculty of Medicine, University of Geneva, Geneva, Switzerland
Introduction: Burnout among healthcare professionals is rising, exacerbated by increased workloads and the Covid-19 pandemic. Affected individuals face stress, depression, and anxiety, adversely impacting both personal well-being and patient care. Resilience has emerged as a key focus for targeted interventions, with online delivery gaining relevance due to the digital transformation and the need for flexibility in busy healthcare schedules.
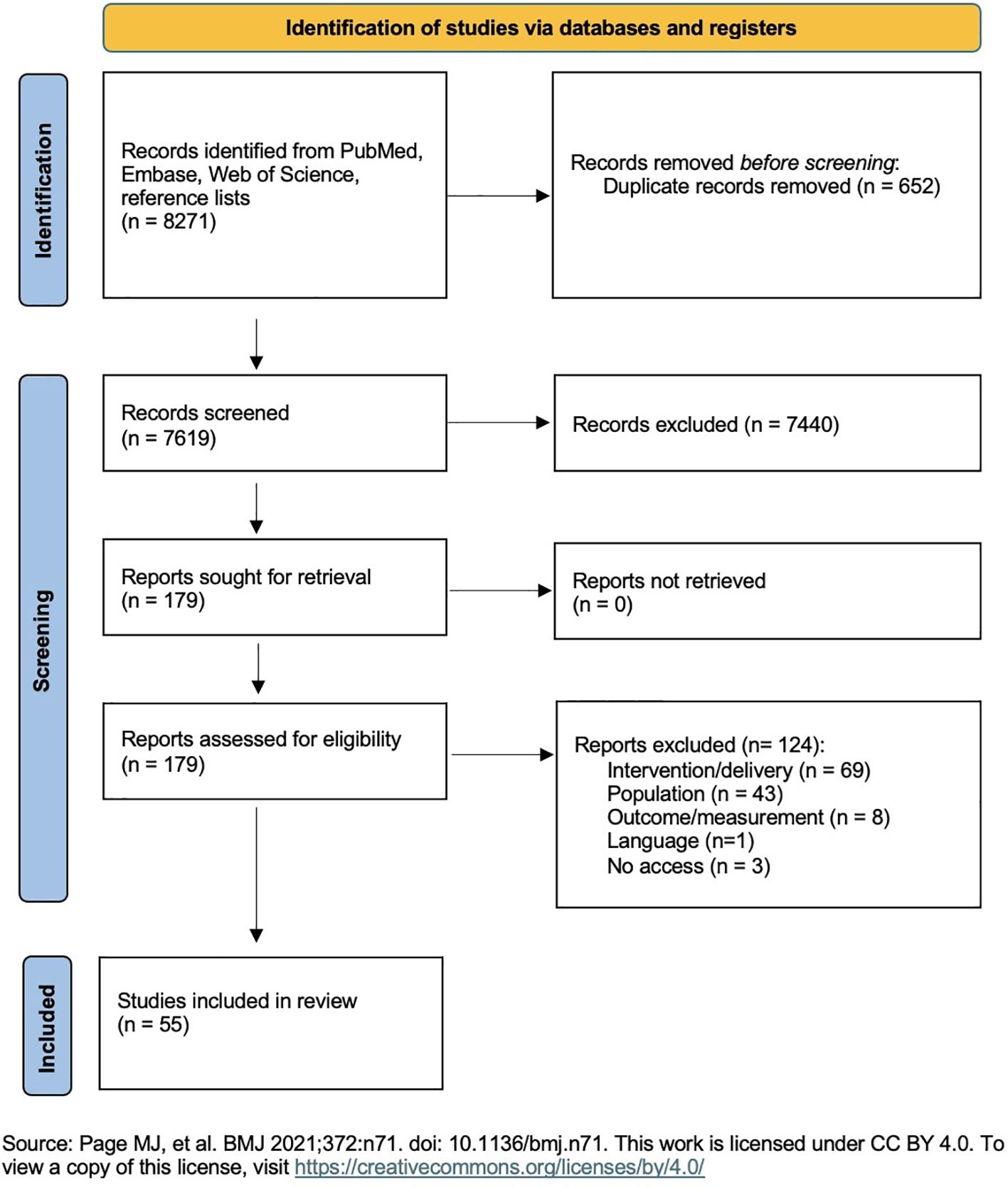
Methods: A systematic review was conducted by searching PubMed, Embase, and Web of Science for eligible studies from April 2014 to April 2024, using search terms related to resilience, online/blended interventions, and healthcare professionals. A total of 7,619 records were identified and screened by two independent reviewers (ML, AM). Final inclusion was based on predefined criteria for online or blended interventions aimed at enhancing resilience in healthcare professionals. The Effective Public Health Practice Project (EPHPP) assessed risk of bias. PRISMA guidelines were followed.
Results: Fifty-five studies were selected, employing various interventions such as psychoeducation, meditation, mindfulness, and elements of cognitive-behavioral therapy (CBT) and acceptance and commitment therapy (ACT). Interventions were delivered online through websites, apps, audio files, etc. or in blended formats complementing in-person sessions. Most studies reported significant improvements in resilience, alongside reductions in stress, burnout, depression, and anxiety. However, only three studies in the online group involving mindfulness or CBT interventions received a strong global rating in the risk of bias assessment by fulfilling the methodological quality criteria. Among these, mindfulness, compared to a waitlist control or a psychoeducational brochure, significantly improved resilience and reduced burnout, while the CBT intervention, compared to bibliotherapy, led to a significant reduction in stress. Compared to the other studies, these three stood out due to minimal selection bias, low attrition rates, a robust study design, and at least partial blinding.
Discussion: This review indicates that digital interventions may enhance resilience and associated factors in healthcare personnel. However, caution is advised due to the heterogeneity of interventions and varied measurement methods. Only three studies met methodological quality criteria, limiting the reliability of other findings. Future research should standardize resilience concepts and adhere to methodological criteria to ensure valid conclusions.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD42024542758 PROSPERO, identifier CRD42024542758.
1 Introduction
Burnout, defined by emotional exhaustion (EE), depersonalization (DP), and reduced sense of accomplishment (PA), is a well-described and increasing issue in the healthcare sector worldwide. Various studies indicate burnout prevalence of 50% and higher in healthcare settings (1–4), a significantly higher rate compared to the general population (4–6).
Factors such as increasing workloads, extended working hours, demanding situations, personnel shortages, escalating bureaucracy, and the added impact of the COVID-19 pandemic, contribute to these challenging circumstances. Symptoms of overload and burnout are increasingly being reported, manifesting as depression, anxiety, fractured relationships, a rise in substance abuse and even an increased likelihood of subsequent suicidal ideation (7–9).
Burnout also has physical consequences, including heart disease, chronic pain, gastrointestinal issues, and even mortality (2) and further leads to absenteeism, resignations, turnover in personnel and a generally decreased job satisfaction (10).
However, it is not only the healthcare workers who are affected. Studies show that these issues also impact patient well-being and safety, leading to lower quality of care, reduced patient satisfaction, and higher rates of medical errors (2, 11).
Organizationally, declining productivity and increased employee absenteeism exacerbate the shortage of skilled professionals, further straining the remaining workforce. This is compounded by elevated turnover rates and reduced productivity, leading to financial consequences for healthcare institutions.
These impacts highlight the importance of mental health for healthcare employees. Consequently, there has been a rapid increase in interest in interventions aimed at preserving and promoting mental health. As therapy is often resource-intensive and costly, there is a growing recognition of the value of preventive measures. Accordingly, various studies have explored multiple interventions to enhance mental well-being (12).
A concept that has gained prominence in this context is resilience. Currently, there is no consensus on a precise definition, making objective measurement challenging (Supplementary Figure 1 in Supplementary Material). In brief, resilience can be described as the ability to maintain psychological and physical health despite exposure to stressors, to rebound, recover, and grow when faced with adversity, and is influenced by genetic, epigenetic, developmental, neurochemical, and psychosocial factors (13, 14).
However, within organizational contexts, resilience is conceptualized at multiple levels, including individual, team, and organizational dimensions. Individual-focused models emphasize personal traits and coping mechanisms that enable employees to adapt to stress and adversity. These approaches highlight the importance of psychological resources such as self-efficacy and emotional regulation but may overlook the influence of organizational structures and culture. In contrast, organizational resilience frameworks consider systemic factors, such as leadership, communication, and adaptive capacity, recognizing that resilience emerges from the interaction between individuals and their work environment. While these models provide a broader understanding, they can be challenging to operationalize and measure. Integrating insights from both perspectives is essential for designing effective interventions that address the complex, multilevel nature of resilience in healthcare settings.
Several studies demonstrate the impact of resilience on mental health, showcasing its role in stress management and the prevention of burnout (3, 6, 15–19). As a result, numerous interventions have been developed to enhance resilience and psychological well-being. These include psychotherapeutic techniques, such as mindfulness-based therapy, emotional supportive coping, cognitive-behavioral therapy (CBT), acceptance and commitment therapy (ACT), attention and interpretation therapy, problem-solving therapy and coping strategies (15, 20, 21). Most interventions were delivered face-to-face in workshops and group-meetings. For instance, Kunzler et al. analyzed 44 randomized controlled trials on resilience-enhancing interventions, finding a positive effect on resilience and related outcomes. However, there was low certainty evidence for improvements, further limited by intervention heterogeneity (15). Another systematic review by Angelopoulou et al. included eleven studies on mindfulness techniques and emotional-supportive coping, showing small but significant positive effects on the resilience of physicians (21).
Although these interventions reported as effective in promoting mental well-being, scheduling in-person training within the already tight schedules of healthcare professionals can be challenging and may intensify stress. Additionally, online training is generally more cost-effective than in-person sessions (22–25). It also provides better accessibility, allowing healthcare workers to participate at their convenience, thus reducing barriers to access and participate. Therefore, offering an online intervention that can be conducted at preferred times is considered meaningful, efficient, and appreciated.
Several studies have examined interventions delivered through an online format. For example, Ladino et al. (20) investigated the effect of internet-based psychosocial interventions on professional burnout in a systematic review comprising four articles. In this review, findings could not demonstrate a significant post-intervention difference compared to the control group. Two studies underwent a meta-analysis, which failed to provide evidence of the interventions’ effectiveness in reducing burnout.
Another systematic review by Henshall et al. (26) explored the effectiveness of web-based interventions on the resilience of healthcare professionals, including eight studies indicating post-intervention enhancements in resilience. All eight studies demonstrated an improvement in resilience levels and associated symptoms following the web-based interventions.
Furthermore, a systematic review by Lopez-Del-Hoyo (27) investigated the effectiveness of eHealth interventions on stress reduction and improvement in the overall mental health of healthcare workers. In this review, 22 studies with different program types were compared, with 13 studies showing significant enhancements in stress, depression, anxiety, burnout, resilience, and mindfulness.
The aim of this study was to compile existing research on online resilience interventions in the healthcare sector and assess their effectiveness. Although there is already a wide variety of resilience interventions, unified approaches are lacking. By comparing different interventions and delivery formats, this review contributes to progress in this area.
By including the most current studies in this rapidly evolving field, this systematic review complements existing literature, further contributing to the preservation and promotion of resilience and overall mental health among healthcare professionals. Covering 55 studies that incorporate diverse psychological approaches and interventions across various healthcare professions, this review summarizes their impacts on resilience, stress, burnout, depression, anxiety, and well-being. It also compares purely digital delivery formats with blended versions to advance the implementation of these interventions.
2 Methods
This systematic review was conducted according to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) 2020 Checklist.
The systematic review protocol has been registered in the International Prospective Register of Systematic Reviews (PROSPERO) under registration number CRD42024542758.
2.1 Eligibility criteria
To be included, the studies should meet several criteria.
Regarding the population, all studies are included in which the intervention group (IG) consisted of individuals working in the healthcare sector, comprising physicians, nurses, paramedics, physiotherapists, and other unspecified healthcare professionals, along with students of healthcare sciences.
All studies incorporating an intervention, regardless of the presence of a control group (CG), whether randomized or non-randomized are included. The requirement is that both baseline and post-intervention data are collected.
The studies must be written in English or German.
Another criterion is that the studies involve interventions aiming at maintaining or promoting resilience or related factors. The specific content of the intervention is not predetermined.
All studies offering resilience interventions digitally or in a blended format incorporating both online and in-person aspects are taken into consideration.
An additional inclusion criterion concerns the measurements. Included are studies comprising quantitative measurements of resilience or related outcomes such as stress, burnout, depression, anxiety, or well-being.
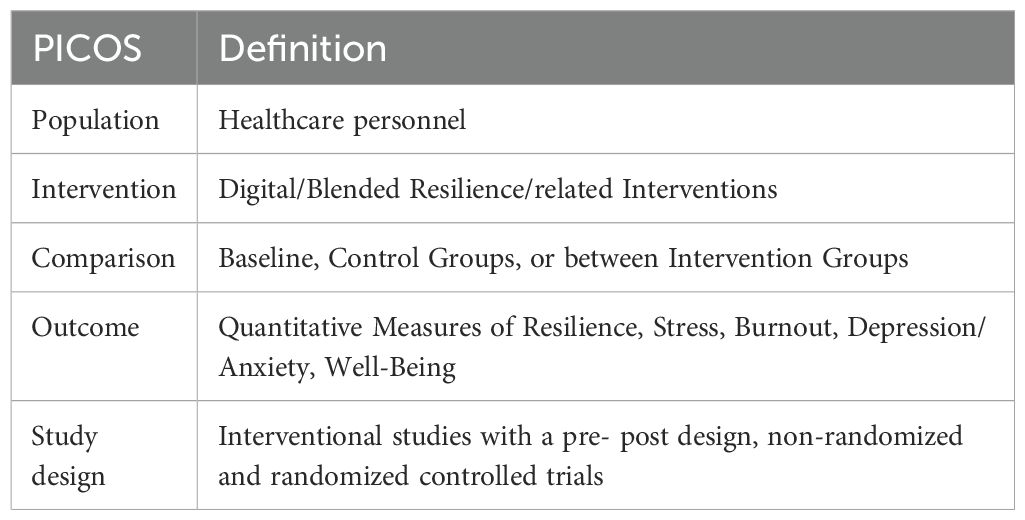
The eligibility criteria are summarized below according to the PICOS scheme (Table 1).
All studies that do not meet the above criteria are excluded. This encompasses studies with a target population that is either not further specified or not employed in the healthcare sector; all reviews, study protocols, or similar works lacking an intervention design; and studies published in languages other than English or German. Additionally, interventions that are unrelated to resilience or related symptoms, interventions exclusively offering in-person or remote training, and studies with only qualitative outcome assessments and lacking a quantitative measurement method are also excluded.
2.2 Search strategy and data sources
For the systematic literature search, three databases were explored: PubMed, Embase, and Web of Science. The search strategy was based on three key terms: health care, resilience, and online or blended interventions. All articles published until the end of April 2024 were considered. In total, the search yielded 8271 search results.
2.3 Screening and study selection
All articles found from the search were extracted to Endnote and duplicates were deleted. The remaining studies were classified by relevance using an algorithm and sorted accordingly in an Excel spreadsheet. The AI (artificial intelligence) algorithm is based on the AS Review program. It is a language model that categorizes and prioritizes studies in the dataset under investigation based on their likely relevance using titles, sentences, and words. Hand-selected studies meeting the inclusion criteria serve as the reference (28).
Based on title and abstract, the majority of irrelevant studies were excluded in a first step. In a second step, the remaining studies were screened using the full text and ultimately included if the inclusion criteria were met. The detailed protocol can be found in the appendix (screening protocol).
More studies that met the inclusion criteria were identified from the reference lists of relevant studies and were added to the study pool.
This analysis was performed by two independent authors (ML, AM) and subsequently discussed until a final list of included studies was generated on Excel by joint consensus.
2.4 Data extraction and analysis
During the data extraction process, included studies were divided into two groups. The first group consisted of studies with purely digital, asynchronous interventions. The second group comprised studies that offered interventions in blended formats, combining both digital and in-person components.
From all included studies, the key information was extracted and presented in an Excel spreadsheet. This included the publication details (title, authors, year of publication, journal, location), population (number of participants, profession, age, proportion of female participants, attrition), intervention (content, delivery, duration of the intervention, frequency), outcome (what are the outcomes, how and when are they measured), study design and control group, results (resilience, stress, burnout, depression, anxiety, well-being), and correlations if investigated.
Given the significant heterogeneity between the two groups (online vs. blended), a subgroup analysis was conducted for better comparability, focusing on study characteristics, sample size and population characteristics, and intervention characteristics. A descriptive analysis was then performed to summarize the effectiveness and significate of the measured outcomes.
2.5 Risk of bias assessment
To assess the risk of bias, The Effect Public Health Practice Project (EPHPP) has been utilized. This involved considering selection bias, the study design, confounders, the blinding, the data collection method, and withdrawals and dropouts.
After capturing all the aforementioned factors, a global rating was created to illustrate the risk of bias.
2.6 Ethics
Ethics approval was not required for this study, as no primary data were utilized, and neither humans nor animals were directly involved.
3 Results
3.1 Search outcomes
See Figure 1 for flow chart.
3.2 Online group
In total, 39 studies were assigned to the online intervention group (29–67).
3.2.1 Study characteristics
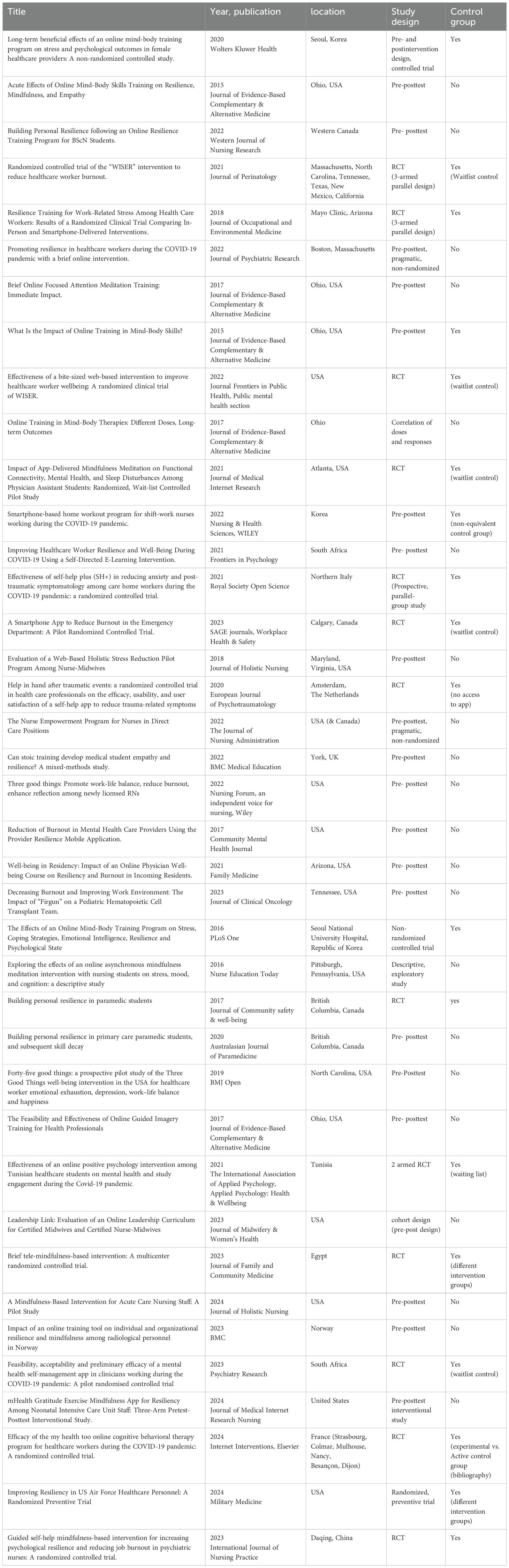
The included studies, published between 2015 and 2024, comprised
14 randomized controlled trials (29, 41, 43–45, 48, 50, 51, 55, 59, 63–65, 67), 4 controlled trials (30, 35, 38, 42), and 20 with a pre-posttest design (31–34, 36, 37, 39, 46, 47, 49, 52–54, 56–58, 60–62, 66). One study focused solely on correlations post-intervention (40) (Table 2).
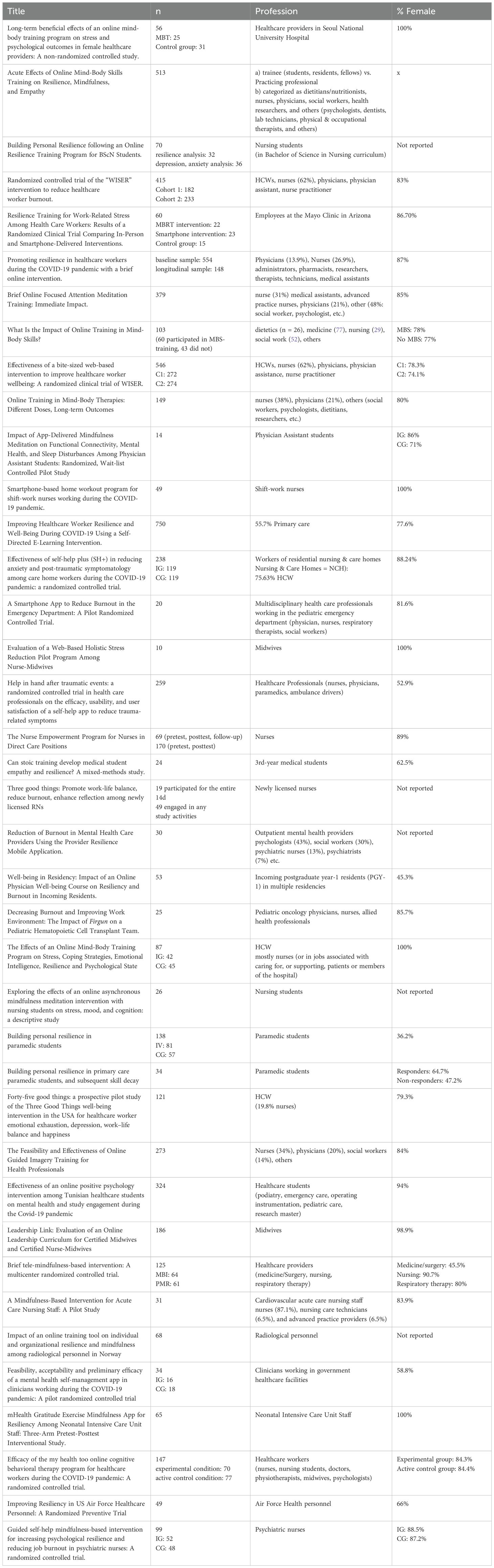
3.2.2 Sample size and population characteristics
Across all studies, nearly 10’000 participants provided baseline data, with around 6600 of them receiving interventions. Post-intervention surveys were completed by approximately 3800 individuals, and around 2200 provided follow-up data. Most participants were women, primarily doctors, nurses, and students in these fields. Other professions included midwives, paramedics, social workers, psychologists, nutritionists, dentists, pharmacists, and physiotherapists (Table 3).
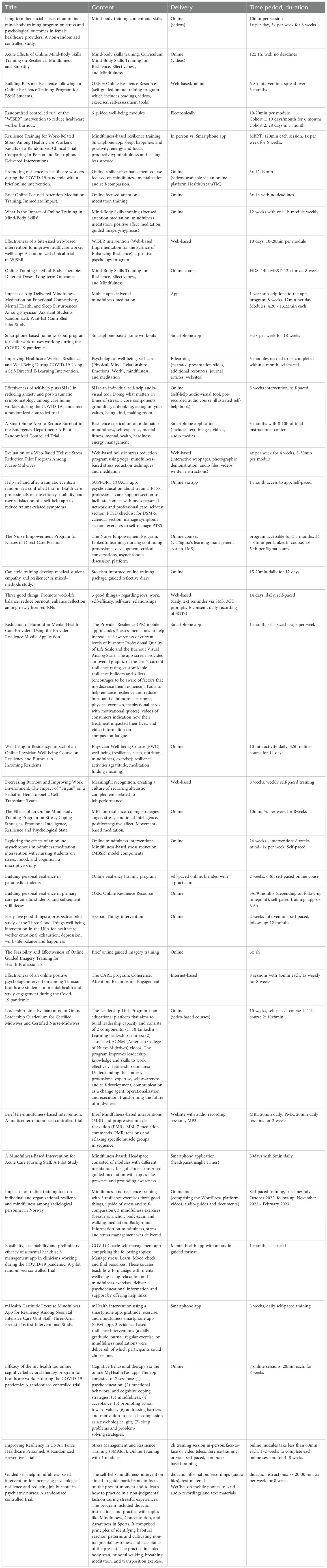
3.2.3 Intervention characteristics
The interventions varied significantly in terms of content, format, duration, frequency, and intensity, reflecting the broad and complex nature of resilience. Generally, they aimed to enhance resilience and address symptoms like stress, burnout, depression, anxiety, and improve overall well-being. Participants were introduced to resilience concepts through educational materials, taught coping strategies, and engaged in practice-based learning to strengthen mental health.
Many studies emphasized mindfulness and mind-body skills using meditation, breathing exercises, relaxation, guided imagery, autogenic training, journaling, and yoga. Common themes included gratitude, kindness, social support, relationships, sleep, productivity, positivity, compassion, hardiness, and empathy.
The interventions, delivered online, utilized various resources like educational materials, quizzes, videos, audio files, podcasts, and self-paced workshops.
Fourteen interventions were entirely self-paced (29, 33, 36, 48, 49, 52, 53, 55–57, 61, 62, 64, 66), allowing individuals to decide the intensity of their practice. Fifteen interventions were pre-designed modules with a specified length that needed to be completed (31, 34, 37–39, 41–43, 45, 46, 50, 51, 58, 63, 65), and ten studies recommended a specific duration or frequency of training over a defined period (30, 32, 35, 40, 44, 47, 54, 59, 60, 67) (Table 4).
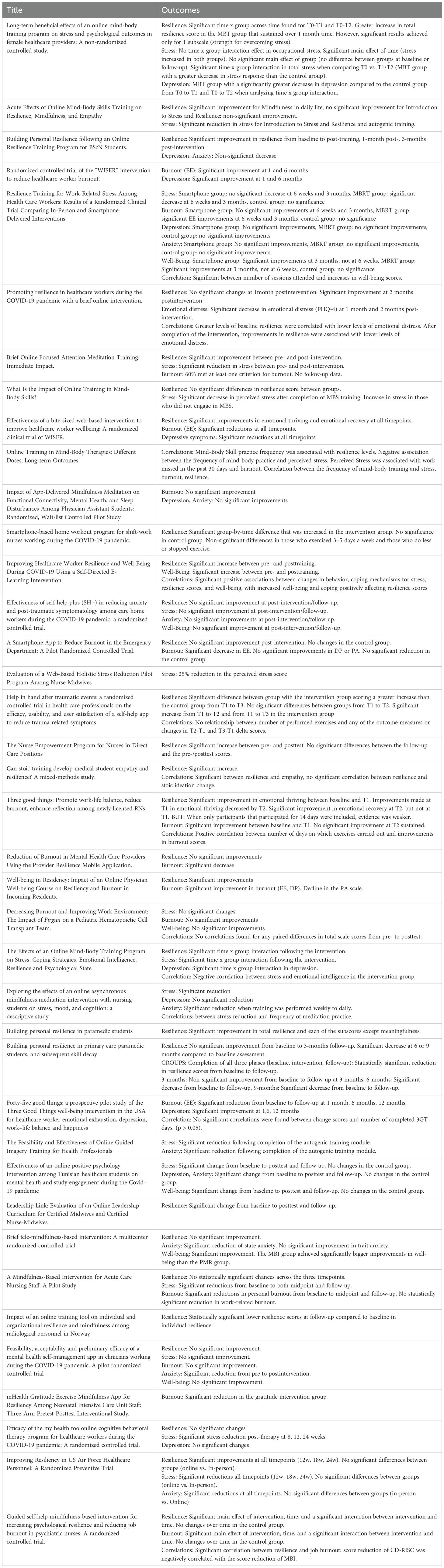
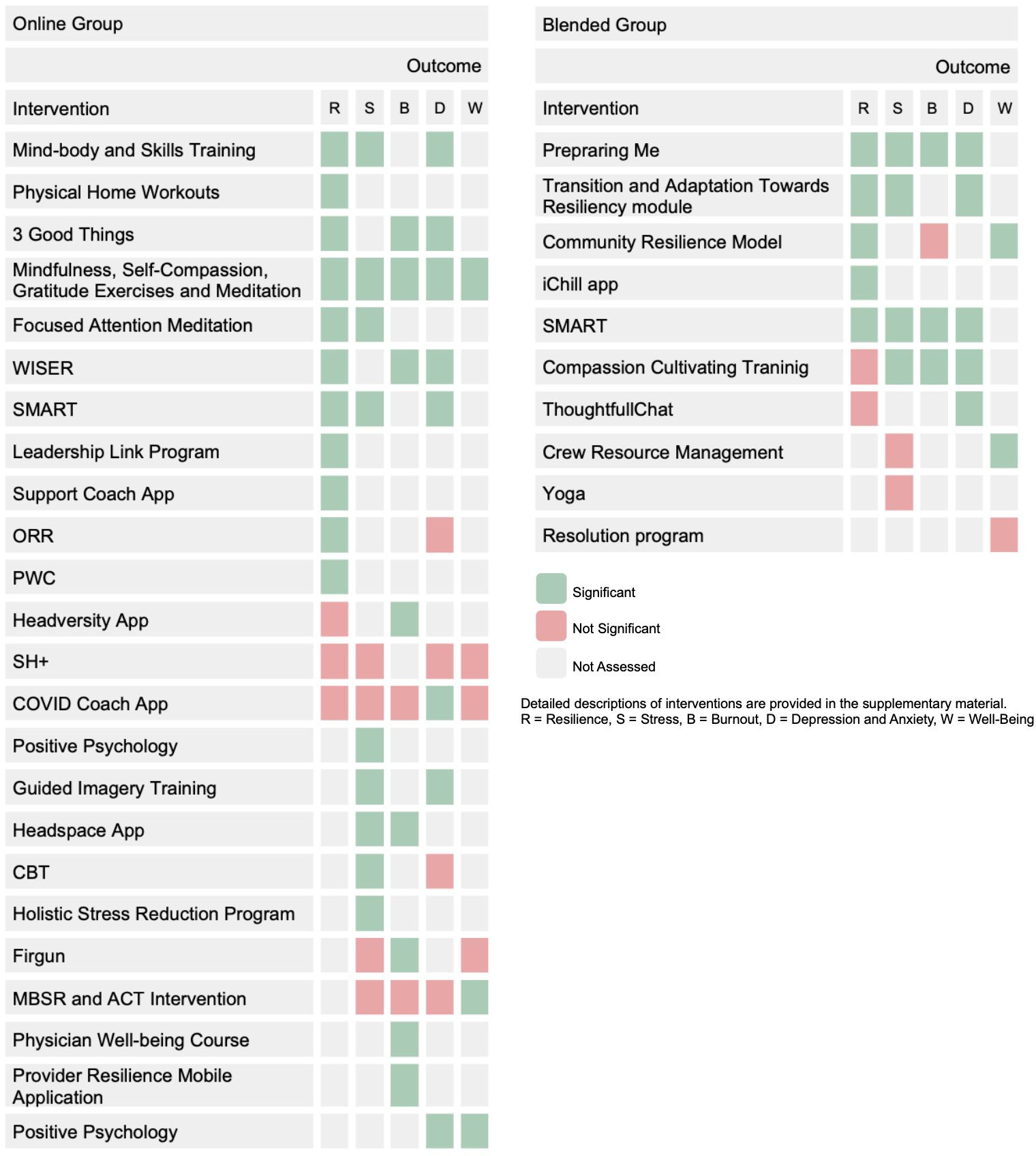
3.2.4 Outcomes
The following table summarizes the results of individual studies on resilience, stress, burnout, depression, anxiety, and well-being, including any investigated correlations (Table 5). In each study, a p-value < 0.05 was considered significant.
3.2.4.1 Resilience
A total of 29 studies ( (29–40, 42, 44, 47, 48, 50, 54–57, 59–65, 67) examined resilience as an outcome. Of these, 19 studies (29–37, 39, 42, 47, 50, 54, 55, 61–63, 67) achieved significant results, while 10 (38, 44, 48, 56, 57, 59, 60, 64, 65) did not. One study focused solely on correlations and provided no numerical data (40). Three studies demonstrated a significant time x group interaction (30, 35, 42) following mind-body training or home workouts.
Post-intervention, 16 studies (29–33, 35–37, 39, 42, 47, 50, 55, 61, 63, 67) showed significant improvements in resilience, while five did not (44, 48, 60, 64, 65). Long-term follow-ups revealed significant results in eight studies (33, 42, 50, 54, 55, 61–63), but three did not show sustained improvements (31, 48, 65). One study found significant results for a resilience enhancement course only after two months, with no significance at one month (34). Another study utilizing the Online Resilience Resource (ORR) intervention achieved non-significant improvements after three months, with a decrease in resilience after six and nine months (56). The Nurse Empowerment Program achieved significance post-intervention, but results were not sustained at follow-up (31).
In summary, interventions such as mind-body and skills training, physical home workouts, 3 good things, mindfulness and self-compassion exercises, focused attention meditation and programs such as WISER, SMART, the Leadership Link program, the Support Coach app, the ORR course and the PWC course achieved significant results. Conversely, interventions like the headversity app, the Self-Help + (SH+) program or the COVID coach app did not show significant improvements.
Measurement tools included the Korean version of the Connor-Davidson Resilience Scale (CD-RISC) (42), Smith’s (6-item) Brief Resilience Scale (37–40), Resilience Scale for Adults (RSA) (54, 56), Connor-Davidson Resilience Scale (CD-RISC) (30, 31, 35, 36, 44, 47, 48, 57, 59, 61–65, 67), Brief Resilience Scale (BRS) (32, 34, 60), Resilience Evaluation Scale (55), 8-item Resilience Scales (emotional thriving, emotional recovery) (33), Dispositional Resilience Scale (47), and the Resilience scale (RS) (29).
3.2.4.2 Stress
17 studies (35, 37–43, 46, 48, 52, 53, 58, 60, 63–65) examined stress, with 12 reporting significant results (35, 37–39, 41, 42, 46, 52, 58, 60, 63, 65), and four not achieving significance (43, 48, 53, 64). One study only examined correlations and did not provide any numerical data (40). Two studies showed a significant group x time interaction (35, 42) with mind-body training.
Post-intervention, 11 studies reported significant stress reductions (37–39, 41, 42, 46, 52, 58, 60, 63, 65), 4 did not (43, 48, 53, 64). Among seven studies that examined follow-up results (41–43, 48, 52, 63, 65), five achieved significant results (41, 42, 52, 63, 65), two did not (43, 48).
Overall, mind-body and skills training, positive psychology, focused attention and mindfulness meditation, guided imagery training, mindfulness via the Headspace app, CBT, as well as the care program, Stress Management and Resilience Training (SMART) program, and the holistic stress reduction program, all brought significant improvements in stress. Conversely, SH+ and Firgun, the COVID coach app, as well as MBSR (Mindfulness-based stress reduction) and ACT intervention, did not achieve significant stress reduction. Long-term success in stress reduction was observed with the Care program, CBT, SMART, mind-body training, and mindfulness meditation.
Measurement tools included the Korean Occupational Stress Scale (KOSS) (35, 42), Stress Response Inventory (Stress, depression) (42), Perceived Stress scale (PSS) (37, 39, 46, 48, 52, 53, 58, 60, 63–65), and the Cohen’s 10-item Perceived Stress Scale (38, 40).
3.2.4.3 Burnout
16 studies (33, 39, 40, 43–45, 47, 49–51, 53, 57, 60, 64, 66, 67) recorded the outcome burnout. 11 studies achieved significant relevance (33, 44, 45, 47, 49, 50, 53, 57, 60, 66, 67), 3 did not (43, 51, 64). One study measured burnout numerically only once, preventing comparisons (39), and another focused solely on correlations without numerical data (40).
Post-intervention, nine studies showed statistically relevant results (33, 44, 47, 49, 50, 53, 57, 60, 66, 67), two did not (51, 64). Two studies (headversity app and Firgun intervention) achieved significant improvements only in EE, with DP and PA remaining non-significant (44, 53). In follow-up surveys, three studies showed significant relevance (45, 49, 50), two did not (33, 43). One study implementing the 3 good things intervention showed relevance post-interventional, but the effect could not be maintained until follow-up (33).
In conclusion, the headversity app, the WISER intervention, the three good things (3GT) intervention, mindfulness and gratitude exercises, the physician well-being course, the Firgun program, the Headspace app and the Provider Resilience Mobile Application all achieved significant improvements in burnout. In contrast, a MBSR and ACT intervention, the COVID coach app, as well as a mindfulness meditation intervention, did not result in significant burnout reduction.
Measurement tools included the Maslach Burnout Inventory (EE, DP, PA) (34, 39, 44, 45, 47, 49, 50, 53, 67), MBI-Human Services Survey (MBI-HSS) (43), EE (33), 7-item Mayo Clinic Physician Well-Being Index (PWBI) (40), School Burnout Inventory (51), Professional Quality of Life Scale (ProQOL) (57, 66), Copenhagen Burnout Inventory (CBI) (60, 64).
3.2.4.4 Depression/anxiety
17 studies (34, 35, 41–43, 45, 46, 48–52, 54, 59, 63–65) measured depression and/or anxiety, with 12 achieving statistical significance (34, 35, 41, 42, 45, 46, 49, 50, 52, 59, 63, 64) and 5 not (43, 48, 51, 54, 65). Two studies utilizing positive psychology or resilience interventions focusing on mindfulness, meditation, and self-compassion, showed significant reductions in depressive and anxious symptoms (34, 41). Five studies reported significant improvement in depressive symptoms (35, 42, 45, 49, 50), and 5 in anxiety symptoms (46, 52, 59, 63, 64). Two studies analyzing mind-body training found a significant time x group interaction in depression (35, 42).
Post-intervention, seven studies reached statistical significance (35, 42, 46, 50, 52, 63, 64), three did not (43, 48, 51, 65). One study achieved a significant improvement in state anxiety following a brief mindfulness intervention, whereas trait anxiety showed no significant change (59). In the follow-up surveys, eight studies achieved statistical relevance (34, 41, 42, 45, 49, 50, 52, 63), four did not (43, 48, 54, 65).
Overall, interventions such as positive psychology, the WISER intervention, the SMART program, the COVID coach app, mind-body training, guided imagery training, 3GT, mindfulness meditation, and a mindfulness, mentalization, and self-compassion program yielded significant reductions in symptoms of depression and anxiety. Specifically, the WISER intervention, mind-body training, and 3GT brought about improvements in depressive symptoms, while guided imagery training and mindfulness meditation showed an effect on anxiety. The SH+, ORR, CBT, and MBSR interventions did not have a significant effect on depression or anxiety.
Measurement tools included the Generalized Anxiety Disorder 7-items (GAD-7) (48, 54, 63), The Patient Health Questionnaire (PHQ) (34, 54, 65), Center for Epidemiological Studies Depression Scale 10-item version (CES-D10) (45, 49, 50, 64), Depression, Anxiety and Stress Scale (DASS-21) (41, 43, 51), The Hospital Anxiety and Depression scale (HADS) (52), Patient Reported Outcomes Measurement Information System – Anxiety Scale (46), Stress Response Inventory (depression) (35), and the State-Trait Anxiety Scale (59, 64).
3.2.4.5 Well-being
7 studies (36, 41, 43, 48, 53, 59, 64) measured the outcome well-being, with four reporting significance (36, 41, 43, 59) and three not (48, 53, 64).
Post-interventional, 2 studies showed significant improvements (36, 59), 3 did not (48, 53, 64). 2 studies achieved significant relevance in the follow-up measurements (41, 43), one of which was relevant after 3 months, but the results were not yet significant at 6 weeks (43). Another study did not reach statistical significance at follow-up (48).
Interventions that demonstrated a significant positive influence on well-being included positive psychology, a MBSR and ACT intervention, and a mindfulness and meditation intervention. The SH+, the COVID coach app and Firgun interventions remained without a significant relevance.
Measurement tools included the WHO-5 Well-Being Index (WHO-5) (36, 43, 48, 53, 59, 64) and the Warwick-Edinburgh Mental Well-being Scale (WEMWBS) (41).
In summary, the WISER program could improve resilience and reduce burnout, the SMART program demonstrated significant stress reduction and improved resilience, and the Leadership Link program showed effectiveness in enhancing resilience. The Three Good Things (3GT) intervention led to improvements in both resilience and burnout, while mindfulness practices and self-compassion exercises were effective in enhancing resilience as well. The Headspace app significantly reduced stress and burnout, but the Headversity app, Self-Help + (SH+), and the COVID Coach did not show significant improvements in any outcomes. Mind-body training and guided imagery effectively improved resilience, as well as symptoms of depression and anxiety. The Firgun intervention failed to achieve significant benefits across the measured outcomes.
These findings are based on studies that predominantly employed quantitative tools to assess resilience, such as various versions of the Connor-Davidson Resilience Scale (CD-RISC), the Brief Resilience Scale (BRS), and the Resilience Scale for Adults (RSA). While these instruments differ somewhat in conceptual orientation, most assess resilience as a dynamic, modifiable capacity rather than a fixed trait. For instance, the CD-RISC and BRS conceptualize resilience as an individual’s current ability to adapt and recover from stress, which can be enhanced through targeted interventions. In contrast, measures such as the Dispositional Resilience Scale also incorporate more stable trait-like elements, capturing a person’s general predisposition to cope with adversity. Overall, the use of primarily state-oriented measurement tools aligns with the interventions’ goals of promoting improvements in psychological adaptability and recovery.
A detailed table with the results for each outcome is located in the appendix (Supplementary Table 10).
3.2.4.6 Correlations
In 13 studies (31–36, 40, 43, 49, 52, 53, 55, 67), various correlations were analyzed. Significant relationships were found between outcomes such as the number of sessions attended, and improvements in well-being scores (43), stress (40, 52), burnout (33, 40) and resilience (40). Resilience was also linked emotional distress (34) and empathy (32). Positive associations were observed between changes in resilience and well-being, as well as coping mechanisms for stress and improvements in well-being and resilience (36). Additionally, a positive correlation was found between job demand and perceived stress, while stress negatively correlated with emotional intelligence (35). Lastly, resilience was linked to job burnout (67).
3.2.4.7 Students
Seven (29, 32, 37, 41, 52, 54, 65) out of nine studies (29, 32, 37, 41, 51, 52, 54, 56, 65) examining the effects of interventions on students found that mind-body skills, psychoeducation, CBT, and positive psychology had a positive impact on resilience, burnout, stress, depression, anxiety, and well-being.
3.3 Blended group
A total of 16 studies were allocated to the blended group (68–83).
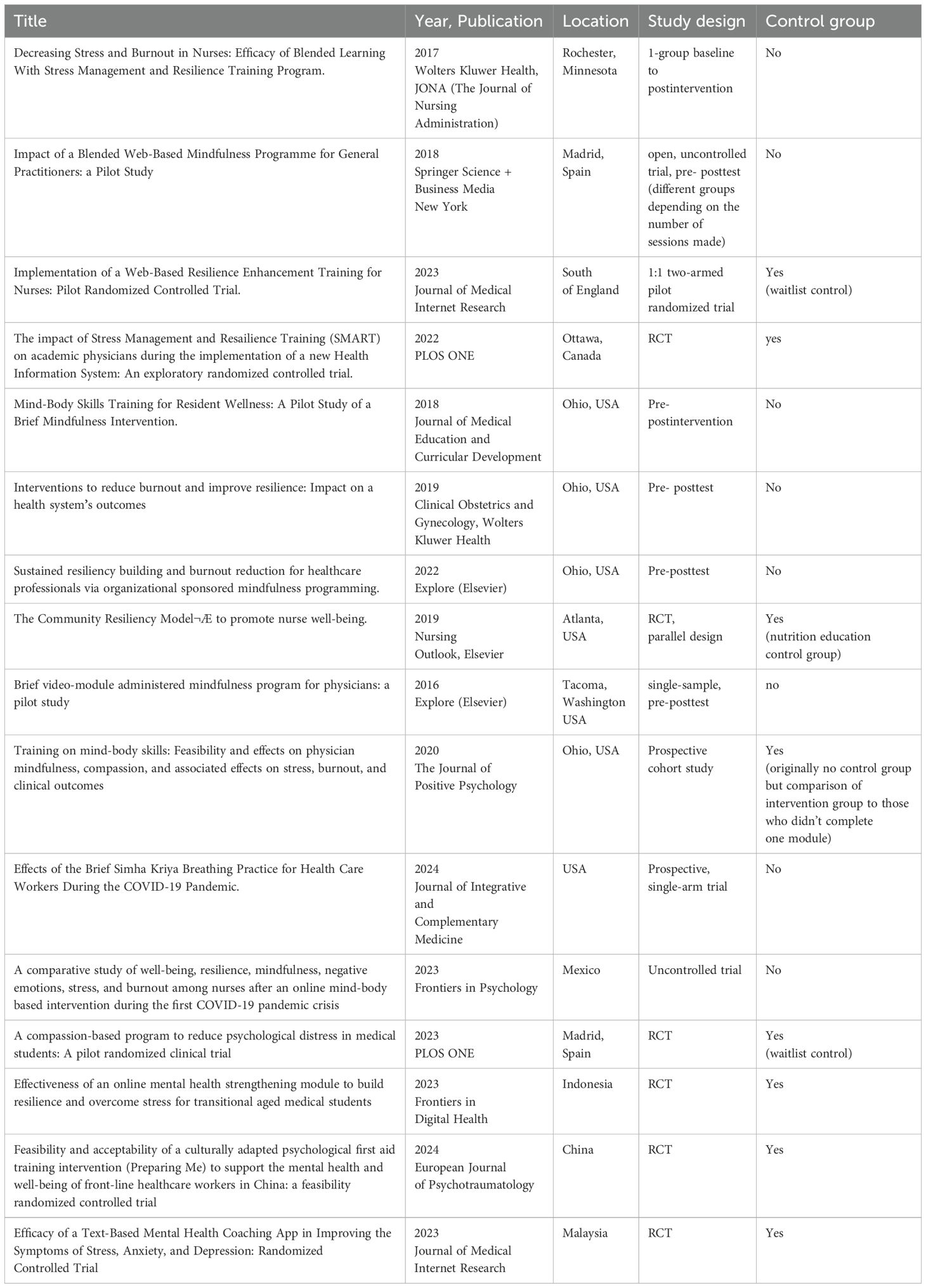
3.3.1 Study characteristics
All included studies were published between 2016 and 2024, comprising 7 randomized controlled trials (68, 69, 77, 79–81, 83), one uncontrolled trial (78), and 8 studies with a pre-posttest interventional design (70–76, 82) (Table 6).
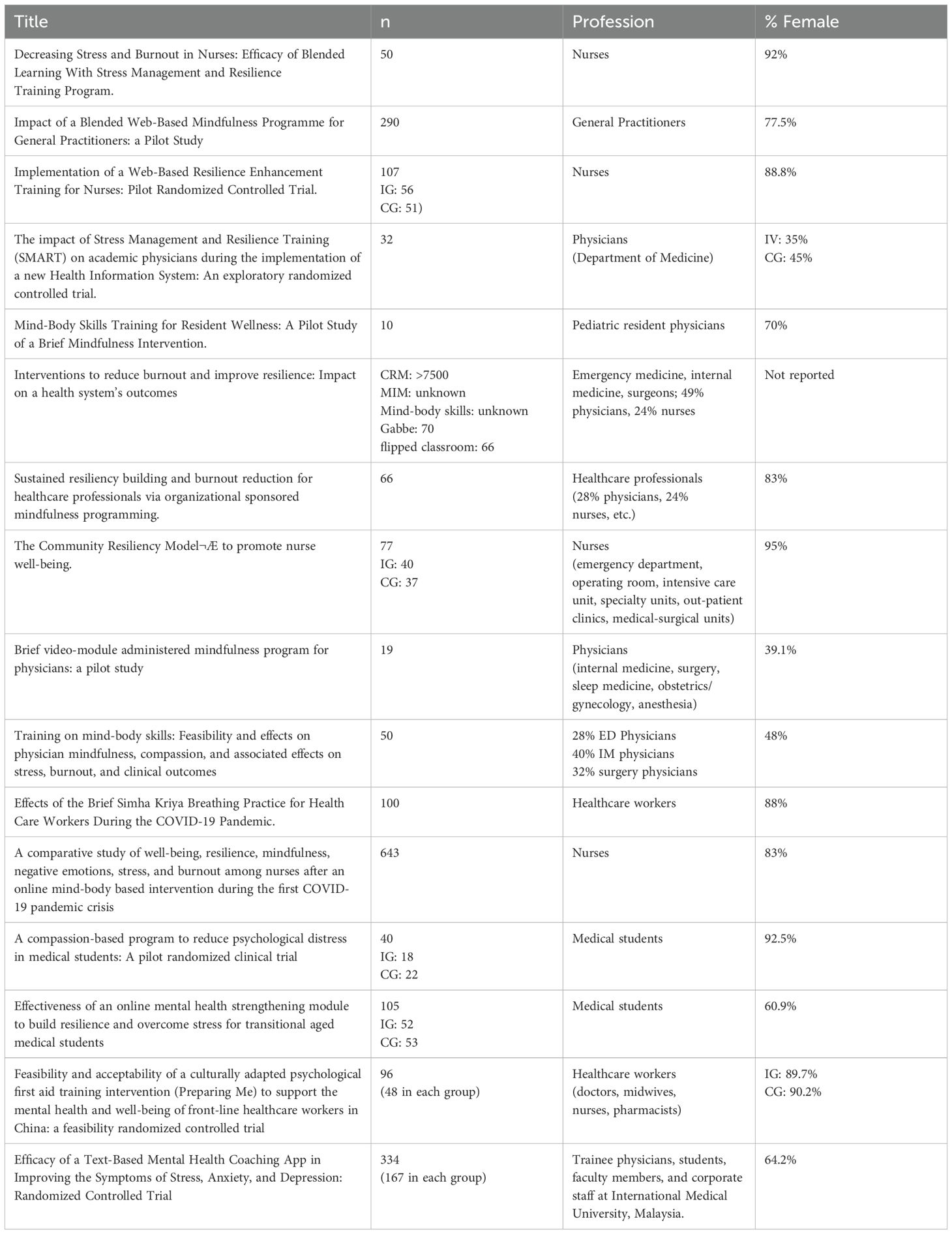
3.3.2 Sample size and population characteristics
In total, over 2800 individuals provided baseline data, with nearly 2400 participating in the intervention and about 1500 submitting post-intervention or follow-up data.
Most participants were nurses and physicians, and two studies exclusively involved medical students (79, 81). The majority of participants across the studies were female (Table 7).
3.3.3 Intervention characteristics
The included studies offered interventions focused on stress management, mindfulness and awareness, mind-body skills, meditation, and yoga as resilience training, delivered in a blended format. All studies featured an online, asynchronous component for independent completion, alongside workshops conducted in-person or remotely via platforms like Zoom, providing content explanations, addressing questions, facilitating practice exercises, and enabling group discussions. The online components varied in duration, intensity, and frequency; five studies supplemented in-person interventions with self-paced online content (68, 70, 71, 78, 79), while eight combined in-person training with structured online modules (69, 72–76, 81, 83). Two studies provided online training with remote support (80, 82), and one made online training entirely optional (77) (Table 8).
3.3.4 Outcomes
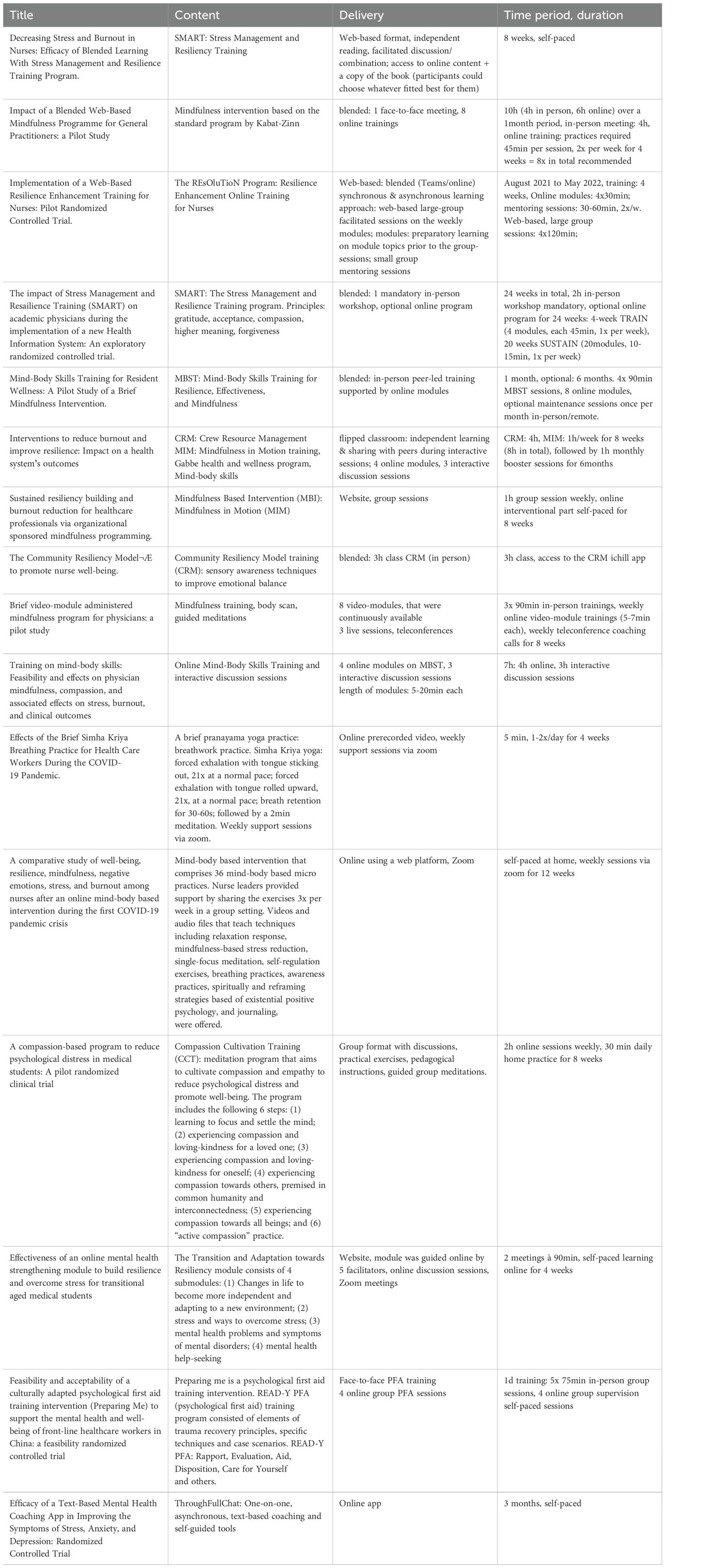
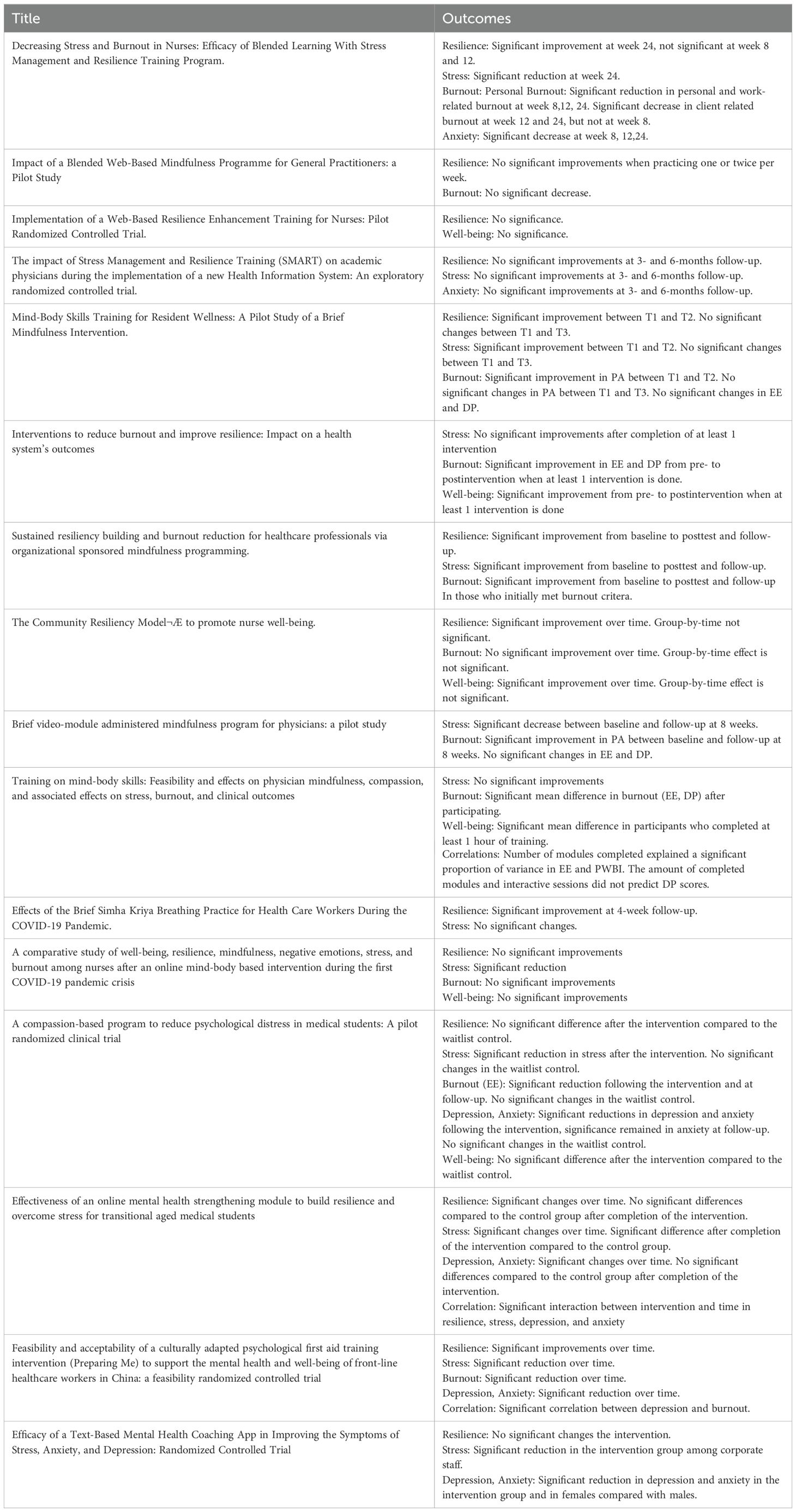
The following table summarizes the outcomes for each study, with a significance level set at p<0.05 (Table 9).
3.3.4.1 Resilience
Seven studies (68–71, 73, 76, 77) measured resilience, with four studies achieving statistical relevance (68, 70, 71, 76), three did not (69, 73, 77).
Post-intervention, one study showed a significant improvement in resilience (76), whereas four did not (69, 71, 73, 77). At follow-up, two studies reached significance (70, 71), two did not (76, 77). One study failed to significantly improve resilience postintervention and after four weeks but achieved it at 16 weeks follow-up (71). Another study demonstrated significant results immediately after the intervention but lost effects at the six months follow-up (76).
In summary, significant increases in resilience were found in studies involving mindfulness and mind-body skills training, as well as programs like “Preparing Me”, the “Transition and Adaptation Towards Resiliency module”, the “Community Resilience Model”, and the “iChill app”. The SMART program showed significant improvement in one of two studies, while “Compassion Cultivating Training” and “ThoughfullChat” did not yield significant changes.
Measurement tools included the CD-RISC (68, 70, 71, 73, 77), Brief Resilience Scale (69), and the Smith’s Brief Resilience Scale (76).
3.3.4.2 Stress
Seven studies examined the outcome of stress (70–72, 74–77), with four achieving significant results (70, 71, 75, 76), and three not (72, 74, 77). Five studies measured perceived stress post- intervention (71, 72, 74–76), of which two reported significant reductions (75, 76). At follow-up, two studies showed significant improvements (70, 71), whereas two did not (76, 77). One study examining effects of mind-body skills achieved significant stress reduction post-intervention but could not sustain it at follow-up (76).
Overall, interventions incorporating mindfulness and mind-body skills achieved significant stress reductions, as did the “Compassion Cultivating Training”, the “Transition and Adaptation towards Resiliency” module, and the “Preparing Me” program. The SMART intervention reached significance in one of two studies, with only a non-significant trend in the other. The “Crew Resource Management” program and a yoga intervention did not yield significant results.
The Perceived Stress Scale (70–72, 74–77) was used to measure changes in stress.
3.3.4.3 Burnout
Eight studies assessed burnout symptoms (68, 70–76), with six reporting significant reductions (70–72, 74–76), and two did not (68, 73).
Immediately after the intervention, five studies achieved significant reductions in burnout (71, 72, 74–76), while two did not (68, 73). Among the four studies that measured over an extended period (68, 70, 71, 76), three studies realized statistically significant improvement at follow-up (70, 71, 76). Romcevich et al. measured burnout subthemes EE, DP, and PA (76) following a mind-body skills intervention. While no significant reduction could be achieved in EE immediately after the intervention or at the follow-up, a significant improvement in DP was observed between baseline and follow-up. A significant increase in PA was also achieved between baseline and post-intervention, but this improvement was not sustained until the follow-up. Pflugeisen et al. could achieve significant improvements in PA between baseline and postintervention survey using a mindfulness intervention. However, decreases in EE and DP between baseline and postintervention remained non-significant (75).
A significant reduction in burnout symptoms was achieved by the SMART intervention, mindfulness and mind-body skills trainings, as well as the “Compassion Cultivating Training” and the “Preparing Me” program. The “Community Resilience Training” did not result in a significant reduction in burnout symptoms.
Measurement tools included the Burnout Inventory (68, 71), Burnout Clinical Subtype Questionnaire (BSCQ-12) (73), and the Maslach Burnout Inventory (70, 72, 74–76).
3.3.4.4 Depression, anxiety
Two studies evaluated symptoms of depression and anxiety (71, 77). One study significantly reduced anxiety symptoms at postintervention and at follow-ups (71), while the other did not (77).
A significant reduction in depression and anxiety was achieved through the “Compassion Cultivating Training”, the “Transition and Adaptation Towards Resiliency” module, the “Preparing Me” program, and “ThoughtfullChat”. The SMART intervention reached significant in one of two studies, with a non-significant trend in the other.
The Generalized Anxiety Scale (71, 77) was used for measurement.
3.3.4.5 Well-being
Four studies focused on the outcome of well-being (68, 69, 72, 74).
Henshall et al. could show a trend towards improvement; however, results could not reach statistical significance (69). In another study, significant improvements in well-being were made when training was performed at least once (72). Grabbe et al. succeeded to significantly improve well-being over time (68). When at least one hour of training was done, significant increases in well-being could be seen in the study of Nguyen et al. (74).
The “Crew Resource Management” training, mindfulness and mind-body skills training interventions, and the “Community Resiliency Model” achieved a significant increase in well-being. The Resolution program, on the other hand, showed only a non-significant trend toward improvement.
Measurement tools included the Warwick-Edinburgh Mental Wellbeing Scale (69), Physician Well-Being Index (PWI) (72, 74), and the WHO-5 Well-being Index (WHO-5) (68).
A detailed table with the results for each outcome is located in the appendix (Supplementary Table 11).
3.3.4.6 Correlations
Three studies investigated various variables and their interrelationships (74, 79, 83). One study found a correlation between the number of completed modules and changes in EE and well-being scores (74). Another study demonstrated a significant interaction between time and intervention regarding outcomes such as resilience, stress, depression, and anxiety (79). Additionally, a connection was observed between depression and burnout (83).
3.3.4.7 Students
Three studies (79–81) reported an effect on stress (79, 81), burnout (79), and depression and anxiety (79, 80) through the Use of the Transition and Adaptation towards Resiliency module, the ThoughFullChat intervention, and the Compassion Cultivating Training.
All outcomes of the included interventions, along with their reported significance, are visually summarized in the heatmap (Figure 2).
3.4 Risk of bias assessment
The Effect Public Health Practice Project (EPHPP) was used to assess the risk of bias.
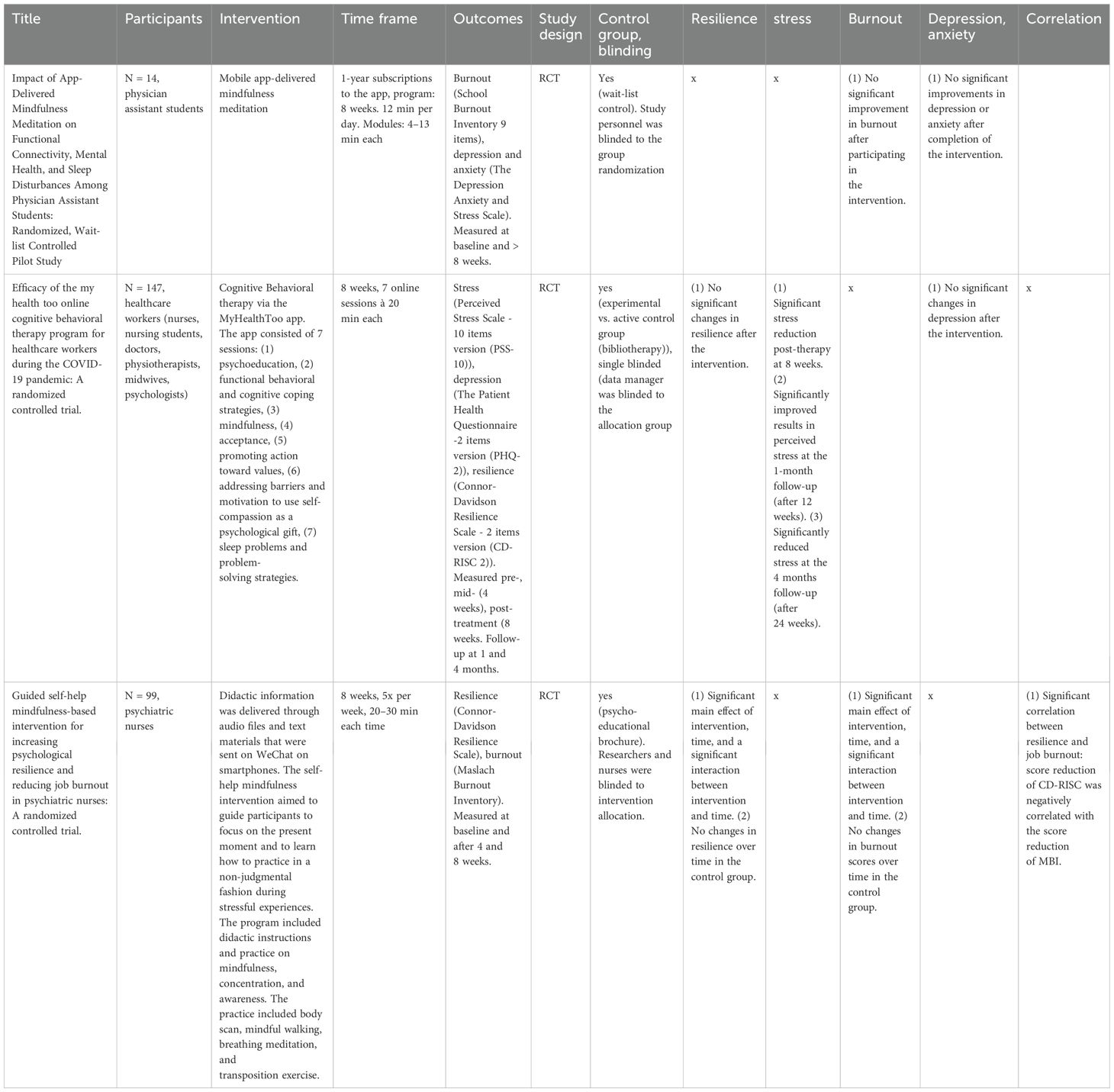
Among the 55 included studies, only three studies achieved a strong global rating, while at least 12 attained a moderate global rating.
Regarding Selection Bias, all studies included a population likely to be representative of the target population, as this was an inclusion criterion from the outset. However, certain studies received a weak rating since only a specific portion of the initially approached individuals ultimately participated.
According to the inclusion criteria, all studies with an intervention design were included, regardless of whether they were randomized controlled trials (RCTs), uncontrolled trials, or pre-post intervention studies. As a result, only 23 studies received a strong rating in the study design section, as they were the only ones conducted as RCTs. The remaining studies, being either uncontrolled trials or using pre-post intervention designs, did not achieve the same rating.
Several studies were assessed as weak in the Confounders section, particularly if the study was designed with only one group, making an assessment in this regard impossible. The same applied to the Blinding section. In the Data Collection Methods, all studies demonstrated strength, as the use of a valid and quantitative measurement method was a criterion for inclusion. In the Dropouts section, one-third of all included studies had to be rated as weak.
Detailed results of the EPHPP are provided in the appendix (Effective Public Health Practice Project (EPHPP) Risk of bias assessment).
The three studies that achieved a strong global rating are summarized in the following table (Table 10).
All three studies were conducted as randomized controlled trials and performed moderately to strongly in the blinding section due to single or double blinding. A large proportion of the initially approached participants were recruited for the intervention and were likely to be representative of the target population, leading to strong performance in the selection bias section. Additionally, the attrition rate was low in all three studies, which was methodologically solid. Due to the relatively high number of participants in two out of these three studies, their findings are more robust and generalizable. In terms of content, the CBT intervention achieved a significant reduction in stress, while one of the two mindfulness interventions led to improvements in resilience and burnout.
4 Discussion
4.1 Summary of main findings
This systematic review screened existing literature on how to foster resilience in healthcare and finally included 55 studies that examined the effects of various online and blended interventions on resilience and related outcomes, designed as (randomized) controlled trials and cohort studies.
Overall, 7898 healthcare workers comprised of doctors, nurses, allied health personnel and healthcare students were able to receive interventions incorporating cognitive-behavioral therapy, acceptance and commitment therapy, mindfulness, mind-body skills, gratitude, meditation, leadership, support, positive psychology, guided imagery, and physical activities. Most studies reported immediate and significant improvements in various mental health outcomes, indicating that these resilience interventions have meaningful and lasting effects on well-being.
Some studies highlighted correlations between the frequency and time invested in training, and the extent of improvement in well-being, resilience, stress, and burnout. Furthermore, a relationship emerged between resilience and emotional distress, well-being, and empathy. This demonstrates how interconnected resilience is and how an improvement in it can influence other outcomes as well.
One strength of this review is the inclusion of student populations from diverse health disciplines. Findings suggest that fostering resilience during academic years may improve coping with stress in professional life, highlighting the interventions potential long-term benefits.
4.2 Comparison of blended vs. online group
Both studies that conducted interventions purely online and those that used a blended format were able to achieve significant results in the five outcomes examined.
A significant advantage of conducting the intervention purely online is that it allows participants to engage at their own pace and at a place and time of their choosing, seamlessly integrating into their individual schedules. Furthermore, there is no need to provide a location or instructors, which represents a financial advantage.
However, the added personal component in blended interventions was appreciated. For instance, participants appreciated the personal interaction and exchange with other participants. Furthermore, the instruction of interventions could be better explained, and any open questions were promptly addressed.
Generally, the comparatively higher attrition rate in pure online intervention studies (84–88) was also evident in this review where the blended group scored higher in the risk of bias assessment regarding withdrawals and dropouts compared to the online group.
In conclusion, both online and blended interventions significantly improve psychological outcomes, each offering distinct advantages. The choice of format should depend on factors like time constraints, location, needs, and costs.
4.3 Comparison with previous work
There has been previous work conducted regarding web-based resilience interventions in healthcare professions.
Three other systematic reviews were found that examined the effects of online interventions to enhance mental health in physicians, nurses, and allied healthcare staff.
Ladino et al. (20) conducted a systematic review involving four articles to examine the effects of internet-based psychosocial interventions on professional burnout. Despite a meta-analysis of two articles suggesting no significant reduction in professional burnout, and even though post-interventionally no significant differences compared to the control group could be observed, the review highlighted psychoeducation as a promising intervention for addressing this issue. It was also demonstrated in this review that psychoeducation is a way to improve mental health (29, 34, 41, 44, 45, 51, 55).
In a similar vein, Henshall et al. (26) conducted a systematic review encompassing eight studies, revealing a positive impact of web-based interventions on resilience and associated symptoms in health professionals in clinical practice settings. These results largely align with the findings of this review and illustrate the impact that online interventions can have not only on resilience, but on various psychological outcomes.
Further insights were gained from Lopez-Del-Hoyo et al. (27), who included 27 studies in their review to assess the effectiveness of eHealth interventions in reducing stress and promoting mental health. Thirteen studies reported a significant post-intervention reduction in stress, along with improvements in depression, anxiety, burnout, resilience, and mindfulness. Nevertheless, the study’s conclusions were constrained by the observed heterogeneity in the interventions. This study, which encompassed a similar volume of research, yielded comparable results to this review. However, what stood out with the inclusion of a larger number of studies, as observed in this review, is the challenge posed by the heterogeneity of interventions and measurement methods, highlighting the need for standardization to enhance comparability.
The present review contributes to the current research on interventions aimed at preserving psychological health across various healthcare professions to further progress in this rapidly evolving subject. The potential of these interventions was demonstrated through significant improvements in resilience, well-being, and the reduction of symptoms related to burnout, stress, depression, and anxiety.
4.4 Methodological quality
In the risk of bias assessment, only three out of the 55 included studies received a strong global rating. The three strong studies demonstrated that CBT and mindfulness interventions could improve resilience, stress, and burnout. Twelve studies achieved a moderate rating, while the remaining studies were rated as weak. Consequently, the findings from the majority of studies cannot be reliably analyzed, and even statistically significant results should be interpreted with serious caution.
Notably, all studies that received a strong rating were in the online group, suggesting that the results from the blended group are only partially reliable. This reduced reliability may stem from greater difficulties in implementing blinding for in-person components, the presence of confounding factors between groups, and selection bias.
The three studies with strong ratings achieved high methodological quality using randomized controlled trial (RCT) designs, single or double blinding, low attrition rates, and minimal selection bias. In contrast, the remaining studies faced various methodological issues. Although the study populations across all studies were representative of the target population according to the inclusion criteria, some studies struggled to recruit sufficient participants, with only a fraction of the initially approached individuals participating in the intervention and consequently received lower ratings. Additionally, some studies experienced higher attrition rates, further affecting their reliability.
The data collection methods were consistently rated as strong, as they met the criteria for inclusion. Regarding study designs, all intervention studies were included, with RCTs performing better than pre-post intervention designs. Blinding, particularly in psychological or behavioral interventions, was often not feasible due to the nature of the interventions, resulting in many studies receiving a weak rating in the blinding section. The lack of effective blinding may have contributed to performance bias, where various factors, such as participants’ awareness of the intervention or the mere attention from a professional, may influenced the participants’ behavior or reported outcomes. As a result, improvements cannot be clearly attributed to the intervention itself, complicating the assessment of its true efficacy. This raises the possibility that the strong effect sized reported in some studies may be inflated by placebo effects or participant expectations rather than reflecting the genuine impact of the intervention.
4.5 Limitations and implications for future research
Until today, there is no uniform definition of resilience. As a result, there are still no universally valid measurements methods for this. The included studies have used various tools to objectify resilience. Related symptoms such as stress, burnout, anxiety, and depression have been used as proxy indicators for resilience, which further complicates the interpretation.
This problem is accompanied by a further limitation. Due to the versatility of resilience, the included studies have implemented a variety of interventions with diverse content.
Additionally, the timing of measured changes following interventions varied significantly across the studies (post-intervention vs. follow-up). This variability suggests the possibility that some changes may have been missed if measurements were taken only after a certain period. While other studies may not provide insights into the long-term effects of the interventions. All this leads to challenges in the general interpretation and comparability of the studies. In the future, efforts should be made to establish a universally accepted definition of resilience and develop standardized, objective measurement tools. Such consensus is crucial to enhance the comparability of studies, particularly regarding the timing of assessments, which currently varies widely. A unified conceptual framework and consistent measurement would allow researchers to more accurately capture changes in resilience, compare intervention outcomes across different studies, and identify which interventions are most effective. Furthermore, standardized tools would facilitate meta-analyses and evidence synthesis, ultimately supporting the optimal design and tailoring of interventions specifically aimed at improving resilience in diverse populations.
An additional constraint to generalizability is the composition of the study populations. In the vast majority of studies, a significant proportion of participants are female. Given the findings of a recent study that approximately 77% of nurses worldwide are female (89), this is not surprising, considering that nurses constitute the largest proportion of all professions in this review. However, this gender distribution does not reflect all healthcare professions, many of which have a more balanced or different gender ratio. As a result, the findings of this review have limited generalizability across the broader range of healthcare workers and are even less applicable to the general population. To draw more robust and widely applicable conclusions about the effectiveness of resilience interventions, future studies should include samples that are more balanced and diverse in terms of gender and professional background, since intervention effects observed primarily in predominantly female nursing populations may not apply to other healthcare professions or demographic groups. Differences in occupational roles, stressors, and coping strategies could lead to varying outcomes, so caution is necessary when extrapolating these results beyond the studies groups.
Furthermore, several studies lacked a control group, which limits the conclusiveness regarding intervention effectiveness. Future studies should therefore be designed and conducted as randomized controlled trials.
The relatively high attrition rate is another limitation. Although many individuals could be initially reached, some were lost until follow-up surveys. Attrition is a well-known phenomenon especially in online interventions (90) and should be minimized in future studies.
Lastly, a significant limitation is the methodological quality constraints of many studies. Due to high attrition rates, selection bias, study designs, and challenges with blinding, only three studies achieved a strong global rating in the risk of bias assessment. Consequently, only the findings from these studies are considered decisive.
Overall, the previously mentioned heterogeneity among the studies continues to be a challenge, limiting full comparability.
To improve the validity of future studies, it is critical to address these methodological weaknesses to enhance the reliability and significance of their findings. Ensuring higher recruitment rates and lower attrition would help provide more representative results. Incorporating blinding techniques where feasible could reduce bias and lead to more reliable findings. Without these improvements, even statistically significant outcomes must be interpreted with caution, as they may be influenced by uncontrolled biases and limitations inherent in the study design.
Due to mentioned limitations, the results should be interpreted with caution until replicated.
4.6 Broader implications
As demonstrated in this review, numerous resilience interventions have shown a significant improvement in multiple mental health outcomes. This contributes to strengthening individual resilience and acts as a strategy against burnout symptoms and other manifestations related to stress.
Beyond structured training programs, there are various other individual-level workplace interventions that may contribute to strengthening resilience (91–96). These include, for example, employer-provided access to physical activity facilities such as on-site gyms, which may help employees enhance their mental well-being through exercise. Similarly, the availability of quiet or relaxation rooms can offer staff opportunities for mental rest and recovery during demanding workdays. Other supportive measures include designated contact persons or anonymous hotlines, which allow employees to express concerns and receive guidance in times of distress. However, such interventions tend to be reactive rather than preventive in nature and may lack the lasting effects that targeted resilience interventions aim to achieve. Moreover, their overall impact is often limited to the individual level and does not necessarily translate into broader organizational change.
However, as mentioned at the outset, there are organizational factors that cannot be solely influenced by individual actions and necessitate a broader approach. Employers and large institutions are thus encouraged to take measures, such as avoiding prolonged working hours, offering psychological support when needed, and emphasizing overall employee well-being as part of the institutional culture to contribute further to the preservation of the mental health of their workforce.
For future considerations, it is advisable to address the issue in two ways: firstly, through individual training sessions aimed at strengthening the resilience of individual persons, as seen in the included studies, and secondly, through organizational changes on the part of employers that can further positively influence mental health at the organizational level. Such measures may include implementing clear and manageable working hours, ensuring reasonable workload distribution, promoting supportive leadership and effective communication, providing access to psychological support services, and fostering a workplace culture that prioritizes employee well-being and work-life balance.
This review focused exclusively on assessing the impact of resilience interventions within healthcare personnel. It would be intriguing for future research to expand the investigation to the entire workforce, thereby revealing the potential for preserving and enhancing resilience and mental health, particularly in today’s world marked by pervasive shortages of skilled personal in various fields.
5 Conclusions
In summary, findings of this review suggest a positive impact of the analyzed interventions on overall resilience, consequently leading to a positive effect on symptoms of depression, anxiety, better coping with occupational stress, and a significant contribution to the maintenance and promotion of general well-being. The inclusion of long-term follow-up results also demonstrated the likely sustainability of the effects with a longer duration.
These comprehensive results emphasize the relevance of resilience promotion within interventions aimed at improving the mental health of healthcare professionals.
Future research is warranted to establish a universally applicable definition and measurement methodology for resilience, which would facilitate the development of more standardized interventions, promoting comparability across studies.
Further considerations for future studies include addressing limitations such as the composition of the study populations, study designs and attrition rates. Additionally, expanding the study population across diverse occupational domains is recommended to enhance the generalizability of findings. Moreover, institutional measures are imperative to contribute at the organizational level and address the issue comprehensively. Lastly, ensuring high methodological quality in future studies is essential to produce interpretable and meaningful results.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
ML: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration. DH: Writing – review & editing, Investigation, Methodology, Software. MK: Writing – review & editing, Conceptualization, Formal analysis, Methodology, Project administration, Supervision, Validation. ES: Writing – review & editing, Conceptualization, Formal analysis, Methodology, Supervision, Project administration, Validation. AM: Writing – review & editing, Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript. Generative AI was utilized solely for the enhancement of linguistic style in this document. It contributed no content-related insights or information.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1519670/full#supplementary-material
References
1. Ghahramani S, Lankarani KB, Yousefi M, Heydari K, Shahabi S, and Azmand S. A systematic review and meta-analysis of burnout among healthcare workers during COVID-19. Frontiers. Psychiatry. (2021) 12:758849. doi: 10.3389/fpsyt.2021.758849
2. Jun J, Ojemeni MM, Kalamani R, Tong J, and Crecelius ML. Relationship between nurse burnout, patient and organizational outcomes: Systematic review. Int J Nurs Stud. (2021) 119:103933. doi: 10.1016/j.ijnurstu.2021.103933
3. West CP, Dyrbye LN, and Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. (2018) 283:516–29. doi: 10.1111/joim.12752
4. Kansoun Z, Boyer L, Hodgkinson M, Villes V, Lançon C, and Fond G. Burnout in French physicians: A systematic review and meta-analysis. J Affect Disord. (2019) 246:132–47. doi: 10.1016/j.jad.2018.12.056
5. De Hert S. Burnout in healthcare workers: prevalence, impact and preventative strategies. Local Reg Anesth. (2020) 13:171–83. doi: 10.2147/LRA.S240564
6. Rahimi B, Baetz M, Bowen R, and Balbuena L. Resilience, stress, and coping among Canadian medical students. Can Med Educ J. (2014) 5:e5–e12. doi: 10.36834/cmej.36689
7. Dyrbye LN, Thomas MR, Massie FS, Power DV, Eacker A, Harper W, et al. Burnout and suicidal ideation among U. S. Med students. Ann Intern Med. (2008) 149:334–41. doi: 10.7326/0003-4819-149-5-200809020-00008
8. Horsfall S. Doctors who commit suicide while under GMC fitness to practise investigation.pdf. Gen Med Counsil. (2014) 1–51.
9. Meltzer H, Griffiths C, Brock A, Rooney C, and Jenkins R. Patterns of suicide by occupation in England and Wales: 2001-2005. Br J Psychiatry. (2008) 193:73–6. doi: 10.1192/bjp.bp.107.040550
10. Shanafelt TD, Sloan JA, and Habermann TM. The well-being of physicians. Am J Med. (2003) 114:513–9. doi: 10.1016/S0002-9343(03)00117-7
11. Salyers MP, Bonfils KA, Luther L, Firmin RL, White DA, Adams EL, et al. The relationship between professional burnout and quality and safety in healthcare: A meta-analysis. J Gen Intern Med. (2017) 32:475–82. doi: 10.1007/s11606-016-3886-9
12. Michaelsen MM, Graser J, Onescheit M, Tuma MP, Werdecker L, Pieper D, et al. Mindfulness-based and mindfulness-informed interventions at the workplace: A systematic review and meta-regression analysis of RCTs. Mindfulness (N Y). (2023) 14:1–34. doi: 10.1007/s12671-023-02130-7
13. de Terte I, Stephens C, and Huddleston L. The development of a three part model of psychological resilience. Stress Health. (2014) 30:416–24. doi: 10.1002/smi.2625
14. McAllister SJ, Vincent A, Hassett AL, Whipple MO, Oh TH, Benzo RP, et al. Psychological resilience, affective mechanisms and symptom burden in a tertiary-care sample of patients with fibromyalgia. Stress Health. (2015) 31:299–305. doi: 10.1002/smi.2555
15. Kunzler AM, Helmreich I, Chmitorz A, König J, Binder H, Wessa M, et al. Psychological interventions to foster resilience in healthcare professionals. Cochrane Database Systematic Rev. (2020) 2020(7):CD012527. doi: 10.1002/14651858.CD012527.pub2
16. Wang M, Li J, Yan G, Lei T, Rong W, and Sun L. The relationship between psychological resilience, neuroticism, attentional bias, and depressive symptoms in college Chinese students. Front Psychol. (2022) 13. doi: 10.3389/fpsyg.2022.884016
17. Sullivan V, Hughes V, and Wilson DR. Nursing burnout and its impact on health. Nurs Clin North Am. (2022) 57:153–69. doi: 10.1016/j.cnur.2021.11.011
18. García-León MÁ, Pérez-Mármol JM, Gonzalez-Pérez R, MdC García-Ríos, and Peralta-Ramírez MI. Relationship between resilience and stress: Perceived stress, stressful life events, HPA axis response during a stressful task and hair cortisol. Physiol Behavior. (2019) 202:87–93. doi: 10.1016/j.physbeh.2019.02.001
19. Li Z-S and Hasson F. Resilience, stress, and psychological well-being in nursing students: A systematic review. Nurse Educ Today. (2020) 90:104440. doi: 10.1016/j.nedt.2020.104440
20. Ladino MDM, Bolaños C, Ramírez VAC, Giraldo EJS, Álzate JP, Cubides A, et al. Effects of internet-based, psychosocial, and early medical interventions on professional burnout in health care workers: Systematic literature review and meta-analysis. Internet Interv. (2023) 34:100682. doi: 10.1016/j.invent.2023.100682
21. Angelopoulou P and Panagopoulou E. Resilience interventions in physicians: A systematic review and meta-analysis. Appl Psychol Health Well Being. (2022) 14:3–25. doi: 10.1111/aphw.12287
22. Aspvall K, Sampaio F, Lenhard F, Melin K, Norlin L, Serlachius E, et al. Cost-effectiveness of internet-delivered vs in-person cognitive behavioral therapy for children and adolescents with obsessive-compulsive disorder. JAMA Netw Open. (2021) 4::e2118516. doi: 10.1001/jamanetworkopen.2021.18516
23. Griffiths F, Lindenmeyer A, Powell J, Lowe P, and Thorogood M. Why are health care interventions delivered over the internet? A systematic review of the published literature. J Med Internet Res. (2006) 8:e10. doi: 10.2196/jmir.8.2.e10
24. Donker T, Blankers M, Hedman E, Ljótsson B, Petrie K, and Christensen H. Economic evaluations of Internet interventions for mental health: a systematic review. Psychol Med. (2015) 45:3357–76. doi: 10.1017/S0033291715001427
25. Mitchell LM, Joshi U, Patel V, Lu C, and Naslund JA. Economic evaluations of internet-based psychological interventions for anxiety disorders and depression: A systematic review. J Affect Disord. (2021) 284:157–82. doi: 10.1016/j.jad.2021.01.092
26. Henshall C, Ostinelli E, Harvey J, Davey Z, Aghanenu B, Cipriani A, et al. Examining the effectiveness of web-based interventions to enhance resilience in health care professionals: systematic review. JMIR Med Educ. (2022) 8:e34230. doi: 10.2196/34230
27. López-Del-Hoyo Y, Fernández-Martínez S, Pérez-Aranda A, Barceló-Soler A, Bani M, Russo S, et al. Effects of eHealth interventions on stress reduction and mental health promotion in healthcare professionals: A systematic review. J Clin Nurs. (2023) 32:5514–33. doi: 10.1111/jocn.16634
28. van de Schoot R, de Bruin J, Schram R, Zahedi P, de Boer J, Weijdema F, et al. An open source machine learning framework for efficient and transparent systematic reviews. Nat Mach Intelligence. (2021) 3:125–33. doi: 10.1038/s42256-020-00287-7
29. Anderson G, Vaughan A, and Mills S. Building personal resilience in paramedic students. J Community Saf Well-being. (2017) 2:51–4. doi: 10.35502/jcswb.44
30. Baek Y, Han K, Kim J, and Yoo HY. Smartphone-based home workout program for shift-work nurses working during the COVID-19 pandemic. Nurs Health Sci. (2022) 24:708–16. doi: 10.1111/nhs.12969
31. Bard K, Cornell JA, Cunningham SD, Madigan EA, and Solomon J. The nurse empowerment program for nurses in direct care positions. J Nurs Adm. (2022) 52:542–8. doi: 10.1097/NNA.0000000000001196
32. Brown MEL, MacLellan A, Laughey W, Omer U, Himmi G, LeBon T, et al. Can stoic training develop medical student empathy and resilience? A mixed-methods study. BMC Med Education. (2022) 22:340. doi: 10.1186/s12909-022-03391-x
33. Cline M, Roberts P, Werlau T, Hauser P, and Smith-Miller C. Three good things: Promote work-life balance, reduce burnout, enhance reflection among newly licensed RNs. Nurs Forum. (2022) 57:1390–8. doi: 10.1111/nuf.12830
34. DeTore NR, Sylvia L, Park ER, Burke A, Levison JH, Shannon A, et al. Promoting resilience in healthcare workers during the COVID-19 pandemic with a brief online intervention. J Psychiatr Res. (2022) 146:228–33. doi: 10.1016/j.jpsychires.2021.11.011
35. Jung YH, Ha TM, Oh CY, Lee US, Jang JH, Kim J, et al. The effects of an online mind-body training program on stress, coping strategies, emotional intelligence, resilience and psychological state. PloS One. (2016) 11:e0159841. doi: 10.1371/journal.pone.0159841
36. Kelly F, Uys M, Bezuidenhout D, Mullane SL, and Bristol C. Improving healthcare worker resilience and well-being during COVID-19 using a self-directed E-learning intervention. Front Psychol. (2021) 12:748133. doi: 10.3389/fpsyg.2021.748133
37. Kemper KJ and Khirallah M. Acute effects of online mind-body skills training on resilience, mindfulness, and empathy. J Evid Based Complementary Altern Med. (2015) 20:247–53. doi: 10.1177/2156587215575816
38. Kemper KJ, Lynn J, and Mahan JD. What is the impact of online training in mind-body skills? J Evid Based Complementary Altern Med. (2015) 20:275–82. doi: 10.1177/2156587215580882
39. Kemper KJ and Rao N. Brief online focused attention meditation training: immediate impact. J Evid Based Complementary Altern Med. (2017) 22:395–400. doi: 10.1177/2156587216663565
40. Kemper KJ, Rao N, Gascon G, and Mahan JD. Online training in mind-body therapies: different doses, long-term outcomes. J Evid Based Complementary Altern Med. (2017) 22:696–702. doi: 10.1177/2156587217701857
41. Krifa I, Hallez Q, van Zyl LE, Braham A, Sahli J, Ben Nasr S, et al. Effectiveness of an online positive psychology intervention among Tunisian healthcare students on mental health and study engagement during the Covid-19 pandemic. Appl Psychol Health Well Being. (2022) 14:1228–54. doi: 10.1111/aphw.12332
42. Lee D, Lee WJ, Choi SH, Jang JH, and Kang DH. Long-term beneficial effects of an online mind-body training program on stress and psychological outcomes in female healthcare providers: A non-randomized controlled study. Med (Baltimore). (2020) 99:e21027. doi: 10.1097/MD.0000000000021027
43. Mistretta EG, Davis MC, Temkit M, Lorenz C, Darby B, and Stonnington CM. Resilience training for work-related stress among health care workers: results of a randomized clinical trial comparing in-person and smartphone-delivered interventions. J Occup Environ Med. (2018) 60:559–68. doi: 10.1097/JOM.0000000000001285
44. Monfries N, Sandhu N, and Millar K. A smartphone app to reduce burnout in the emergency department: A pilot randomized controlled trial. Workplace Health Saf. (2023) 71:181–7. doi: 10.1177/21650799221123261
45. Profit J, Adair KC, Cui X, Mitchell B, Brandon D, Tawfik DS, et al. Randomized controlled trial of the “WISER” intervention to reduce healthcare worker burnout. J Perinatol. (2021) 41:2225–34. doi: 10.1038/s41372-021-01100-y
46. Rao N and Kemper KJ. The feasibility and effectiveness of online guided imagery training for health professionals. J Evid Based Complementary Altern Med. (2017) 22:54–8. doi: 10.1177/2156587216631903
47. Ricker M, Brooks AJ, Bodine S, Lebensohn P, and Maizes V. Well-being in residency: impact of an online physician well-being course on resiliency and burnout in incoming residents. Fam Med. (2021) 53:123–8. doi: 10.22454/FamMed.2021.314886
48. Riello M, Purgato M, Bove C, Tedeschi F, MacTaggart D, Barbui C, et al. Effectiveness of self-help plus (SH+) in reducing anxiety and post-traumatic symptomatology among care home workers during the COVID-19 pandemic: a randomized controlled trial. R Soc Open Sci. (2021) 8:210219. doi: 10.1098/rsos.210219
49. Sexton JB and Adair KC. Forty-five good things: a prospective pilot study of the Three Good Things well-being intervention in the USA for healthcare worker emotional exhaustion, depression, work-life balance and happiness. BMJ Open. (2019) 9:e022695. doi: 10.1136/bmjopen-2018-022695
50. Sexton JB, Adair KC, Cui X, Tawfik DS, and Profit J. Effectiveness of a bite-sized web-based intervention to improve healthcare worker wellbeing: A randomized clinical trial of WISER. Front Public Health. (2022) 10:1016407. doi: 10.3389/fpubh.2022.1016407
51. Smith JL, Allen JW, Haack CI, Wehrmeyer KL, Alden KG, Lund MB, et al. Impact of app-delivered mindfulness meditation on functional connectivity, mental health, and sleep disturbances among physician assistant students: randomized, wait-list controlled pilot study. JMIR Form Res. (2021) 5:e24208. doi: 10.2196/24208
52. Spadaro KC and Hunker DF. Exploring The effects Of An online asynchronous mindfulness meditation intervention with nursing students On Stress, mood, And Cognition: A descriptive study. Nurse Educ Today. (2016) 39:163–9. doi: 10.1016/j.nedt.2016.02.006
53. Stein J, Madni A, Moody K, Kramer D, Vaughn D, Bhatia S, et al. Decreasing burnout and improving work environment: the impact of firgun on a pediatric hematopoietic cell transplant team. JCO Oncol Pract. (2023) 19:e365–e76. doi: 10.1200/OP.22.00299
54. Stoliker BE, Vaughan AD, Collins J, Black M, and Anderson GS. Building personal resilience following an online resilience training program for BScN students. West J Nurs Res. (2022) 44:755–64. doi: 10.1177/01939459211017240
55. van der Meer CAI, Bakker A, van Zuiden M, Lok A, and Olff M. Help in hand after traumatic events: a randomized controlled trial in health care professionals on the efficacy, usability, and user satisfaction of a self-help app to reduce trauma-related symptoms. Eur J Psychotraumatol. (2020) 11:1717155. doi: 10.1080/20008198.2020.1717155
56. Vaughan AD, Stoliker BE, and Anderson GS. Building personal resilience in primary care paramedic students, and subsequent skill decay. Australas J Paramedicine. (2020) 17:1–8. doi: 10.33151/ajp.17.803
57. Wood AE, Prins A, Bush NE, Hsia JF, Bourn LE, Earley MD, et al. Reduction of burnout in mental health care providers using the provider resilience mobile application. Community Ment Health J. (2017) 53:452–9. doi: 10.1007/s10597-016-0076-5
58. Wright EM. Evaluation of a web-based holistic stress reduction pilot program among nurse-midwives. J Holist Nurs. (2018) 36:159–69. doi: 10.1177/0898010117704325
59. AlQarni AM, Elfaki A, Abdel Wahab MM, Aljehani Y, Alkhunaizi AA, Alex J, et al. Brief tele-mindfulness-based intervention: A multicenter randomized controlled trial. J Family Community Med. (2023) 30:180–7. doi: 10.4103/jfcm.jfcm_82_23
60. Brouwer KR, Melander S, Walmsley LA, Norton J, and Okoli C. A mindfulness-based intervention for acute care nursing staff: A pilot study. J Holist Nurs. (2024) 42:24–33. doi: 10.1177/08980101231181004
61. Clark E, Solomon J, Cunningham SD, Bard K, and Storey AS. Leadership link: evaluation of an online leadership curriculum for certified midwives and certified nurse-midwives. J Midwifery Womens Health. (2023) 68:627–36. doi: 10.1111/jmwh.13508
62. Gransjøen AM. Impact of an online training tool on individual and organizational resilience and mindfulness among radiological personnel in Norway. BMC Res Notes. (2023) 16:373. doi: 10.1186/s13104-023-06659-7
63. Hernandez SHA, Killian J, Parshall MB, Reno J, and Zhu Y. Improving resiliency in U.S. Air force healthcare personnel: A randomized preventive trial. Mil Med. (2024) 189:e250–e8. doi: 10.1093/milmed/usad303
64. Kirykowicz K, Jaworski B, Owen J, Kirschbaum C, Seedat S, and van den Heuvel LL. Feasibility, acceptability and preliminary efficacy of a mental health self-management app in clinicians working during the COVID-19 pandemic: A pilot randomised controlled trial. Psychiatry Res. (2023) 329:115493. doi: 10.1016/j.psychres.2023.115493
65. Mengin AC, Nourry N, Severac F, Berna F, Bemmouna D, Costache ME, et al. Efficacy of the my health too online cognitive behavioral therapy program for healthcare workers during the COVID-19 pandemic: A randomized controlled trial. Internet Interv. (2024) 36:100736. doi: 10.1016/j.invent.2024.100736
66. Peterson NE, Thomas M, Hunsaker S, Stewart T, and Collett CJ. mHealth gratitude exercise mindfulness app for resiliency among neonatal intensive care unit staff: three-arm pretest-posttest interventional study. JMIR Nurs. (2024) 7:e54561. doi: 10.2196/54561
67. Wang Q, Luan Y, Liu D, Dai J, Wang H, Zhang Y, et al. Guided self-help mindfulness-based intervention for increasing psychological resilience and reducing job burnout in psychiatric nurses: A randomized controlled trial. . Int J Nurs Pract. (2024) 30:e13204. doi: 10.1111/ijn.13204
68. Grabbe L, Higgins MK, Baird M, Craven PA, and San Fratello S. The Community Resiliency Model® to promote nurse well-being. Nurs Outlook. (2020) 68:324–36. doi: 10.1016/j.outlook.2019.11.002
69. Henshall C, Davey Z, Srikesavan C, Hart L, Butcher D, and Cipriani A. Implementation of a web-based resilience enhancement training for nurses: pilot randomized controlled trial. J Med Internet Res. (2023) 25:e43771. doi: 10.2196/43771
70. Klatt M, Westrick A, Bawa R, Gabram O, Blake A, and Emerson B. Sustained resiliency building and burnout reduction for healthcare professionals via organizational sponsored mindfulness programming. Explore (NY). (2022) 18:179–86. doi: 10.1016/j.explore.2021.04.004
71. Magtibay DL, Chesak SS, Coughlin K, and Sood A. Decreasing stress and burnout in nurses: efficacy of blended learning with stress management and resilience training program. J Nurs Adm. (2017) 47:391–5. doi: 10.1097/NNA.0000000000000501
72. Moffatt-Bruce SD, Nguyen MC, Steinberg B, Holliday S, and Klatt M. Interventions to reduce burnout and improve resilience: impact on a health system’s outcomes. Clin Obstet Gynecol. (2019) 62:432–43. doi: 10.1097/GRF.0000000000000458
73. Montero-Marin J, Gaete J, Araya R, Demarzo M, Manzanera R, Mon M, et al. Impact of a blended web-based mindfulness programme for general practitioners: a pilot study. Mindfulness. (2018) 9:129–39. doi: 10.1007/s12671-017-0752-8
74. Nguyen MC, Gabbe SG, Kemper KJ, Mahan JD, Cheavens JS, and Moffatt-Bruce SD. Training on mind-body skills: Feasibility and effects on physician mindfulness, compassion, and associated effects on stress, burnout, and clinical outcomes. J Positive Psychol. (2020) 15:194–207. doi: 10.1080/17439760.2019.1578892
75. Pflugeisen BM, Drummond D, Ebersole D, Mundell K, and Chen D. Brief video-module administered mindfulness program for physicians: A pilot study. Explore (NY). (2016) 12:50–4. doi: 10.1016/j.explore.2015.10.005
76. Romcevich LE, Reed S, Flowers SR, Kemper KJ, and Mahan JD. Mind-body skills training for resident wellness: A pilot study of a brief mindfulness intervention. J Med Educ Curric Dev. (2018) 5:2382120518773061. doi: 10.1177/2382120518773061
77. Spilg EG, Kuk H, Ananny L, McNeill K, LeBlanc V, Bauer BA, et al. The impact of Stress Management and Resailience Training (SMART) on academic physicians during the implementation of a new Health Information System: An exploratory randomized controlled trial. PloS One. (2022) 17:e0267240. doi: 10.1371/journal.pone.0267240
78. Cepeda-Lopez AC, Solís Domínguez L, Villarreal Zambrano S, Garza-Rodriguez IY, Del Valle AC, and Quiroga-Garza A. A comparative study of well-being, resilience, mindfulness, negative emotions, stress, and burnout among nurses after an online mind-body based intervention during the first COVID-19 pandemic crisis. Front Psychol. (2023) 14:848637. doi: 10.3389/fpsyg.2023.848637
79. Kaligis F, Ismail RI, Wiguna T, Prasetyo S, Gunardi H, Indriatmi W, et al. Effectiveness of an online mental health strengthening module to build resilience and overcome stress for transitional aged medical students. Front Digit Health. (2023) 5:1207583. doi: 10.3389/fdgth.2023.1207583
80. Lim YS, Quek JH, Ching XW, Lim DTR, Lim KG, Thuraisingham C, et al. Efficacy of a text-based mental health coaching app in improving the symptoms of stress, anxiety, and depression: randomized controlled trial. JMIR Form Res. (2023) 7:e46458. doi: 10.2196/46458
81. Rojas B, Catalan E, Diez G, and Roca P. A compassion-based program to reduce psychological distress in medical students: A pilot randomized clinical trial. PloS One. (2023) 18:e0287388. doi: 10.1371/journal.pone.0287388
82. Wagner RW, Mallaiah S, Anderson CR, Engle R, Vasu V, Bruera E, et al. Effects of the brief simha kriya breathing practice for health care workers during the COVID-19 pandemic. J Integr Complement Med. (2024) 30(10):970–7. doi: 10.1089/jicm.2023.0692
83. Wang L, Norman I, Xiao T, Li Y, Li X, Liu T, et al. Feasibility and acceptability of a culturally adapted psychological first aid training intervention (Preparing Me) to support the mental health and well-being of front-line healthcare workers in China: a feasibility randomized controlled trial. Eur J Psychotraumatol. (2024) 15:2299195. doi: 10.1080/20008066.2023.2299195
84. Meyerowitz-Katz G, Ravi S, Arnolda L, Feng X, Maberly G, and Astell-Burt T. Rates of attrition and dropout in app-based interventions for chronic disease: systematic review and meta-analysis. J Med Internet Res. (2020) 22:e20283. doi: 10.2196/20283
85. Helander E, Kaipainen K, Korhonen I, and Wansink B. Factors related to sustained use of a free mobile app for dietary self-monitoring with photography and peer feedback: retrospective cohort study. J Med Internet Res. (2014) 16:e109. doi: 10.2196/jmir.3084
86. Guertler D, Vandelanotte C, Kirwan M, and Duncan MJ. Engagement and nonusage attrition with a free physical activity promotion program: the case of 10,000 steps Australia. J Med Internet Res. (2015) 17:e176. doi: 10.2196/jmir.4339
87. Bennett GG and Glasgow RE. The delivery of public health interventions via the Internet: actualizing their potential. Annu Rev Public Health. (2009) 30:273–92. doi: 10.1146/annurev.publhealth.031308.100235
89. Kharazmi E, Bordbar N, and Bordbar S. Distribution of nursing workforce in the world using Gini coefficient. BMC Nurs. (2023) 22:151. doi: 10.1186/s12912-023-01313-w
90. Barrett K and Stewart I. A preliminary comparison of the efficacy of online Acceptance and Commitment Therapy (ACT) and Cognitive Behavioural Therapy (CBT) stress management interventions for social and healthcare workers. Health Soc Care Community. (2021) 29:113–26. doi: 10.1111/hsc.13074
91. Chu AH, Koh D, Moy FM, and Müller-Riemenschneider F. Do workplace physical activity interventions improve mental health outcomes? Occup Med (Lond). (2014) 64:235–45. doi: 10.1093/occmed/kqu045
92. Hinzmann D, Forster A, Koll-Krüsmann M, Schießl A, Schneider F, Sigl-Erkel T, et al. Calling for help-peer-based psychosocial support for medical staff by telephone-A best practice example from Germany. Int J Environ Res Public Health. (2022) 19(23):15453. doi: 10.3390/ijerph192315453
93. Joyce S, Modini M, Christensen H, Mykletun A, Bryant R, Mitchell PB, et al. Workplace interventions for common mental disorders: a systematic meta-review. Psychol Med. (2016) 46:683–97. doi: 10.1017/S0033291715002408
94. Martland RN, Ma R, Paleri V, Valmaggia L, Riches S, Firth J, et al. The efficacy of physical activity to improve the mental wellbeing of healthcare workers: A systematic review. Ment Health Phys Activity. (2024) 26:100577. doi: 10.1016/j.mhpa.2024.100577
95. Prendergast V, Elmasry S, Juhl NA, and Chapple KM. Resilience room use and its effect on distress among nurses and allied staff. J Neurosci Nurs. (2023) 55:80–5. doi: 10.1097/JNN.0000000000000701
Keywords: resilience, mental health, digital intervention, healthcare workers, healthcare students
Citation: Larsson M, Ho DM, Kirschner M, Seifritz E and Manoliu A (2025) Digital resilience interventions for healthcare workers: a systematic review. Front. Psychiatry 16:1519670. doi: 10.3389/fpsyt.2025.1519670
Received: 30 October 2024; Accepted: 21 July 2025;
Published: 10 September 2025.
Edited by:
Mansoor Malik, Johns Hopkins Medicine, United StatesReviewed by:
Praag Bhardwaj, All India Institute of Medical Sciences, IndiaMaria Armaou, ICON plc, United Kingdom
Copyright © 2025 Larsson, Ho, Kirschner, Seifritz and Manoliu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Malin Larsson, bWFsaW4ubGFyc3NvbkB1emguY2g=
 Malin Larsson
Malin Larsson Dominic M. Ho
Dominic M. Ho Matthias Kirschner
Matthias Kirschner Erich Seifritz
Erich Seifritz Andrei Manoliu
Andrei Manoliu