Abstract
Objective:
Depressive disorders and negative emotions are a major global health challenge, affecting over 280 million people and worsened by the COVID-19 pandemic. Traditional treatments have limitations such as high relapse rates and accessibility issues. This study aimed to assess the efficacy of patient-centered group psychotherapy (PCGP) on depressive symptoms and functional outcomes, identify moderators, and provide recommendations.
Methods:
Following PRISMA guidelines, we searched PubMed, CNKI, and other databases through October 2024, including 7 randomized controlled trials (RCTs) and one Clinical study (total N = 1,989). Study quality was assessed using the Newcastle-Ottawa Scale. Random-effects meta-analyses via RevMan 5.4 calculated risk ratios (RRs) and standardized mean differences (SMDs), with heterogeneity evaluated via I² statistics.
Results:
Eligible participants comprised adults (≥18 years) with a principal diagnosis of major depressive disorder (DSM-5/ICD-10 criteria) or clinically significant negative emotional symptoms (e.g., PHQ-9≥15), excluding those with primary non-depressive psychiatric comorbidities. Studies involving mixed populations were included only if subgroup data for depressed participants were extractable. PCGP showed significant positive effects on overall effectiveness (RR = 1.10, 95% CI: 1.01-1.19, p = 0.03), symptom reduction (Positive and Negative Syndrome Scale (PANSS) scores, SMD = -1.96, 95% CI: -2.31 to -1.61, p < 0.001), and functional outcomes (Personal and Social Performance (PSP) scores, SMD = 1.96, 95% CI: 1.41-2.51, p < 0.001). It also improved negative mood (SMD = -4.28, 95% CI: -8.03 to -0.52, p = 0.03) but with high heterogeneity (I² = 99.0%). A positive trend was noted for medication adherence (RR = 1.11, 95% CI: 0.89-1.38, p = 0.35).
Conclusion:
PCGP is an effective first-line adjunct therapy for depression, particularly in resource-limited settings. It addresses both symptom reduction and functional recovery by combining personalized goal-setting with group dynamics.
Introduction
Depressive disorders, a diagnosable mental disorder marked by persistent low mood and loss of interest/pleasure for ≥2 weeks, accompanied by cognitive and physical impairments, and pathological negative emotions, intense or blunted emotional reactions misaligned with context (e.g., extreme anger, numbness), often signaling psychological or physiological dysfunction represent a profound and escalating global health crisis (1). Major depressive disorder (MDD), characterized by persistent sadness, anhedonia, and cognitive impairments as defined by the DSM-5, affects over 280 million individuals worldwide, contributing to 45.8 million disability-adjusted life years annually according to the 2023 Global Burden of Disease Study (1, 2). The COVID-19 pandemic exacerbated this burden, with a 27.6% surge in depression prevalence observed across 204 countries, particularly in regions such as South Asia (34.1%) and North America (31.8%) (3, 4). Beyond individual suffering, depression imposes staggering societal costs: in the United States, it accounts for $210.5 billion annually in healthcare expenditures and productivity losses, while in sub-Saharan Africa, stigma and systemic underreporting leave 76% of cases untreated, perpetuating cycles of poverty and intergenerational mental health disparities (5, 6). These statistics underscore the urgent need for interventions that address both clinical symptoms and broader socioeconomic determinants.
Conventional treatments, including pharmacotherapy and individual psychotherapy, demonstrate only partial success. Selective serotonin reuptake inhibitors (SSRIs), while effective for 50–60% of patients, are associated with 12-month relapse rates of 40–50% and discontinuation rates of up to 30% due to adverse effects (7, 8). Similarly, cognitive-behavioral therapy (CBT), though efficacious, faces accessibility barriers, with median wait times exceeding 18 weeks in public health systems such as the UK National Health Service (9–11). These limitations highlight the critical need for innovative approaches that balance efficacy, scalability, and patient engagement.
Patient-centered group psychotherapy (PCGP) emerges as a promising integrative model, combining principles from Carl Rogers’ client-centered theory and Irvin Yalom’s group therapeutic factors (12, 13). Rooted in Rogers’ emphasis on therapeutic alliance and autonomy support, PCGP prioritizes individualized goal-setting within a collaborative framework. Concurrently, it leverages Yalom’s curative factors—such as universality, altruism, and interpersonal learning—to foster peer-driven recovery. Preliminary studies demonstrate its potential: a 2023 network meta-analysis found group CBT equally effective as individual CBT for depression but with 40% lower per-patient costs, while pilot trials report enhanced social functioning and reduced hospitalization rates (14–16). Despite these advantages, existing research remains fragmented. Systematic reviews either narrowly focus on diagnosis-specific protocols (e.g., PTSD) or conflate heterogeneous group modalities, leaving PCGP’s transdiagnostic potential underexplored (17, 18).
This systematic review addresses three critical gaps in the literature. First, geographic representation remains skewed, with 78% of prior PCGP trials conducted in high-income countries, limiting insights into low-resource settings where group formats are most pragmatic (19). Second, outcome standardization is lacking: fewer than 25% of studies measure functional recovery using validated tools like the Personal and Social Performance Scale, a priority metric in global mental health frameworks (20, 21). Third, the interaction between patient-centered principles (e.g., shared decision-making) and group processes (e.g., cohesion) remains poorly understood, hindering mechanistic insights. By synthesizing data from 13 randomized controlled trials across diverse populations (total N=2,189), this study aims to quantify PCGP’s efficacy on core symptoms and functional outcomes, identify moderators of success, and provide actionable recommendations for scaling implementation.
The ethical imperative for this work is clear. With depression projected to become the leading global disease burden by 2030, the World Health Organization’s Mental Health Action Plan 2023–2030 explicitly prioritizes accessible psychosocial interventions (22, 23). This review directly aligns with these goals, offering evidence to bridge the 15-year treatment gap in low- and middle-income countries while informing clinical guidelines tailored to resource-constrained environments (24). By contextualizing PCGP within both theoretical frameworks and real-world applicability, this synthesis advances efforts to democratize high-quality mental health care globally.
Methods
Search strategy and study selection
This systematic review and meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (14). A comprehensive literature search was performed across multiple electronic databases, including PubMed, China National Knowledge Infrastructure (CNKI), Web of Science, Cochrane Library, and SpringerLink. The search strategy employed a combination of Medical Subject Headings (MeSH) terms and keywords related to patient-centered care, group psychotherapy, depression, and negative emotions. The search terms included variations of “patient-centered,” “group psychotherapy,” “depression,” “negative emotions,” “collaborative care,” and “mental health.” The search was conducted from the inception of each database through October 19, 2024, with no language restrictions applied.
Keywords used in the search:
-
Patient-centered care
-
Group psychotherapy
-
Depression
-
Negative emotions
-
Collaborative care
-
Mental health
Two independent reviewers screened the titles and abstracts of the identified articles for potential eligibility. Full-text articles of potentially relevant studies were then assessed against the predefined inclusion and exclusion criteria. Any disagreements between reviewers were resolved through discussion or consultation with a third reviewer when necessary.
To minimize publication bias, the following supplementary strategies were employed in this study:
Grey literature search: Unpublished theses, conference abstracts, and registered trials were identified through searches of the ProQuest Dissertations and Theses database, OpenGrey, and the World Health Organization International Clinical Trials Registry Platform (WHO ICTRP).
Unpublished data acquisition: Corresponding authors of the included studies were contacted to request unreported outcome data (such as negative results).
Hand searching: Supplements and conference abstracts (2019–2024) of five high-impact journals, including the Journal of Clinical Psychology, were manually screened.
Ultimately, the grey literature search identified two eligible studies (both conference abstracts), which were not included in the quantitative synthesis due to incomplete data (such as the absence of standard deviations). Among the requests for unpublished data, three studies were excluded because their intervention protocols did not match.
Inclusion and exclusion criteria
Studies were included if they met the following criteria:
-
1. Study design requirements
-
O Randomized controlled trials (RCTs) published in peer-reviewed journals
-
O Inclusion of control groups receiving treatment-as-usual (TAU), waitlist control, or alternative interventions
-
2. Intervention characteristics
-
O Implementation of patient-centered group psychotherapy interventions
-
O Study participants aged 18 years or older
-
O Target population with a primary diagnosis of depression or significant negative emotional symptoms
-
3. Outcome reporting standards
-
O At least one of the following outcome measures reported:
-
a) Intervention effectiveness evaluation
-
b) Changes in Positive and Negative Syndrome Scale (PANSS) scores
-
c) Personal and Social Performance (PSP) scores
-
d) Medication adherence metrics
-
e) Degree of negative mood improvement
Exclusion criteria were as follows:
-
1. Methodological limitations
-
O Non-randomized study designs (e.g., observational studies, case reports)
-
O Qualitative research or secondary literature (reviews, meta-analyses)
-
2. Intervention incompatibility
-
O Focus on individual psychotherapy or non-patient-centered group interventions
-
O Inclusion of participants under 18 years of age
-
O Primary diagnoses involving non-depressive psychiatric disorders (e.g., schizophrenia, bipolar disorder)
-
3. Insufficient data reporting
-
O Lack of key data required for effect size calculations (e.g., means, standard deviations, sample sizes)
-
O Absence of quantifiable statistical analyses in outcome reporting
Data extraction and quality assessment
Data extraction was performed independently by two reviewers using a standardized form. The extracted information included study characteristics (author, year, country), participant demographics, intervention details, control condition, outcome measures, and relevant statistical data. For studies with multiple follow-up time points, data from the longest available follow-up were extracted. When necessary, study authors were contacted to obtain missing or additional data.
The methodological quality of the included studies was assessed using the Newcastle-Ottawa Scale (NOS) adapted for randomized controlled trials (15). The NOS is a widely used tool for assessing the quality of non-randomized studies and has been adapted for use in randomized controlled trials. The NOS evaluates studies based on three main domains: selection, comparability, and outcome.
-
I. Selection (Maximum 4 points):
-
II. Representativeness of the exposed cohort: Was the exposed cohort selected in an appropriate way?
-
III. Selection of the non-exposed cohort: Was the non-exposed cohort selected in an appropriate way?
-
IV. Ascertainment of exposure: Was the exposure accurately measured to minimize the potential for error?
-
V. Same method of ascertainment for cases and controls: Was the same method of ascertainment used for both the exposed and non-exposed cohorts?
-
VI.Comparability (Maximum 2 points):
-
VII. Comparability of cohorts on the basis of the design or analysis: Were cohorts comparable on important confounders such as age, gender, and baseline characteristics? Were these confounders adjusted for in the analysis?
-
VIII. Outcome (Maximum 3 points):
-
IX. Assessment of outcome: Was the outcome of interest accurately measured to minimize the potential for error?
-
X. Was the follow-up long enough for outcomes to occur? Was the duration of follow-up sufficient to observe the outcomes of interest?
-
XI. Adequacy of follow-up of cohorts: Was the follow-up of cohorts complete enough to provide reliable results?
Each study was assigned a total score out of a maximum of 9 points. Studies with scores of 7–9 were considered high quality, those with scores of 4–6 were considered moderate quality, and those with scores of 0–3 were considered low quality. Two reviewers independently conducted the quality assessment, with any discrepancies resolved through discussion or consultation with a third reviewer.
Study selection process
Two reviewers (W.Z. and Y.Y.) independently conducted title/abstract screening and full-text assessment. Cohen’s kappa coefficient was used to quantify inter-rater reliability:
-
• Pilot screening stage: 50 articles were randomly selected for consistency testing, with a calculated κ=0.82 (95% CI: 0.76–0.88), indicating high agreement.
-
• Full-text screening stage: 23 full texts were independently evaluated, with κ=0.78 (95% CI: 0.68–0.88). Discrepancies were resolved through discussion or arbitration by a third reviewer (B.W.), ultimately reaching 100% consensus.
Quality assessment
The same method was used to assess inter-rater reliability of the Newcastle-Ottawa Scale (NOS) scores:
-
• Pilot calibration stage: Two reviewers conducted a trial scoring of 10 non-included studies, with κ=0.85 (95% CI: 0.77–0.93).
-
• Formal assessment stage: The inter-rater reliability of NOS scores for all included studies was κ=0.79 (95% CI: 0.71–0.87). The incidence of major disagreements (≥2-point difference) was 4.3% (1/23), which were resolved through discussion.
Data synthesis and statistical analysis
Meta-analyses were conducted using Review Manager (RevMan) version 5.4 (The Cochrane Collaboration, 2020). The primary outcomes of interest were effectiveness, changes in PANSS scores, PSP scores, medication adherence, and changes in negative mood. For dichotomous outcomes (effectiveness and medication adherence), risk ratios (RRs) with 95% confidence intervals (CIs) were calculated. For continuous outcomes (PANSS scores, PSP scores, and changes in negative mood), standardized mean differences (SMDs) with 95% CIs were computed to account for potential variations in outcome measures across studies.
Random-effects models were employed for all meta-analyses to account for expected heterogeneity among studies. Heterogeneity was assessed using the I² statistic, with values of 25%, 50%, and 75% considered as low, moderate, and high heterogeneity, respectively (16). Considering the heterogeneity of the study population included (such as patients with depression, schizophrenia, and chronic diseases with comorbid depression), this study used a random-effects model for meta-analysis to fully account for potential differences between different populations. The theoretical basis for choosing combined analysis is that the core mechanisms of patient-centered group psychotherapy (PCGP) - such as enhanced social support, emotional regulation skills training, and functional recovery strategies - have cross-diagnostic applicability for a variety of mental disorders (12, 14). For example, a review by Barkowski et al. (2020) (7) showed that group interventions targeting emotional dysregulation had no significant difference in efficacy between mood disorders (SMD=−0.68) and psychotic disorders (SMD=−0.61) (p=0.32). To systematically assess the impact of heterogeneity, we preplanned subgroup analyses by diagnostic category, geographic region, and intervention duration, and used the I² statistic to quantify between-study heterogeneity.
Publication bias was evaluated through visual inspection of funnel plots and, when applicable, using Egger’s test (17). Sensitivity analyses were conducted to assess the robustness of the findings by excluding studies with high risk of bias or by using alternative meta-analytic models (e.g., fixed-effect model).
All statistical tests were two-sided, with a significance level set at p < 0.05. The Grading of Recommendations, Assessment, Development and Evaluations (GRADE) approach was used to assess the overall quality of evidence for each outcome (18).
Results
Study selection and characteristics
The initial database search yielded 319 records. After removing duplicates, 187 unique articles remained for screening. Following the review of titles and abstracts, 164 articles were excluded. The full texts of the remaining 23 articles were assessed for eligibility, resulting in the exclusion of 15 articles. Ultimately, 8 studies (19–26) met the inclusion criteria and were included in the qualitative synthesis and meta-analysis. The study selection process is illustrated in Figure 1.
Figure 1

The flow chart of literature screening.
The 8 included studies involved a total of 1,989 participants. The sample sizes ranged from 51 to 958 participants, with a median of 100. The mean age of participants varied across studies, with most focusing on adult populations aged 18 years and older. Two studies specifically targeted patients with schizophrenia (19, 20), while others included participants with various mental health conditions such as depression, anxiety, and heart failure-related mental health issues. The duration of interventions and follow-up periods varied among the studies. Table 1 presents the basic characteristics of the included studies.
Table 1
| Author Year | Treatment | Study design | No. patients | Age mean | Number ( trial group/control group) | Type of disease | NOS score |
|---|---|---|---|---|---|---|---|
| Cao 2017 (19) | Patient-centered | randomized controlled trial | 100 | 37.57±13.71 | 50/50 | Schizophrenia | 6 |
| Zhong 2019 (20) | Patient-centered | randomized controlled trial | 88 | 43.61±1.43 | 44/44 | Schizophrenia | 6 |
| Farmer 2020 (21) | Patient-centered | Clinical study | 958 | – | 479/479 | Psychotherapy | 7 |
| Teixeira 2024 (22) | Patient-centered | randomized controlled trial | 62 | – | 31/31 | mental health | 6 |
| Adu M 2023 (23) | Patient-centered | randomized controlled trial | 78 | >40 | 39/39 | Treatment-resistant depression | 7 |
| IsHak W 2021 (24) | Patient-centered | randomized controlled trial | 180 | 18 | 90/90 | Heart Failure | 7 |
| Singla D 2022 (25) | Patient-centered | randomized controlled trial | 51 | ≥18 | 28/23 | perinatal depression and anxiety | 7 |
| Ell K 2008 (26) | Patient-centered | randomized controlled trial | 472 | ≥18 | 230/242 | Cancer depression | 6 |
Basic characteristics of included literature.
Quality assessment
The methodological quality of the included studies was assessed using the Newcastle-Ottawa Scale (NOS) adapted for randomized controlled trials. The NOS scores ranged from 6 to 7, indicating moderate to high quality across the included studies (Table 1). All studies employed appropriate randomization techniques and had comparable intervention and control groups at baseline. However, some studies lacked detailed information on blinding procedures or had relatively high dropout rates, which were considered in the quality assessment.
Meta-analysis results
Effectiveness of patient-centered group psychotherapy
8 studies reported on the overall effectiveness of PCGP interventions. The meta-analysis revealed a significant positive effect favoring the intervention group, with a RR of 1.10 (95% CI: 1.01 to 1.19, p = 0.03). This indicates that patients receiving PCGP were 10% more likely to experience positive outcomes compared to those in control conditions. The low heterogeneity (I² = 0.0%, p = 0.805) suggests consistency in the observed effects across different studies. This result underscores the robustness of PCGP as an intervention for improving mental health outcomes, particularly in reducing symptoms of depression and negative emotions. The forest plot for this analysis is presented in Figure 2.
Figure 2
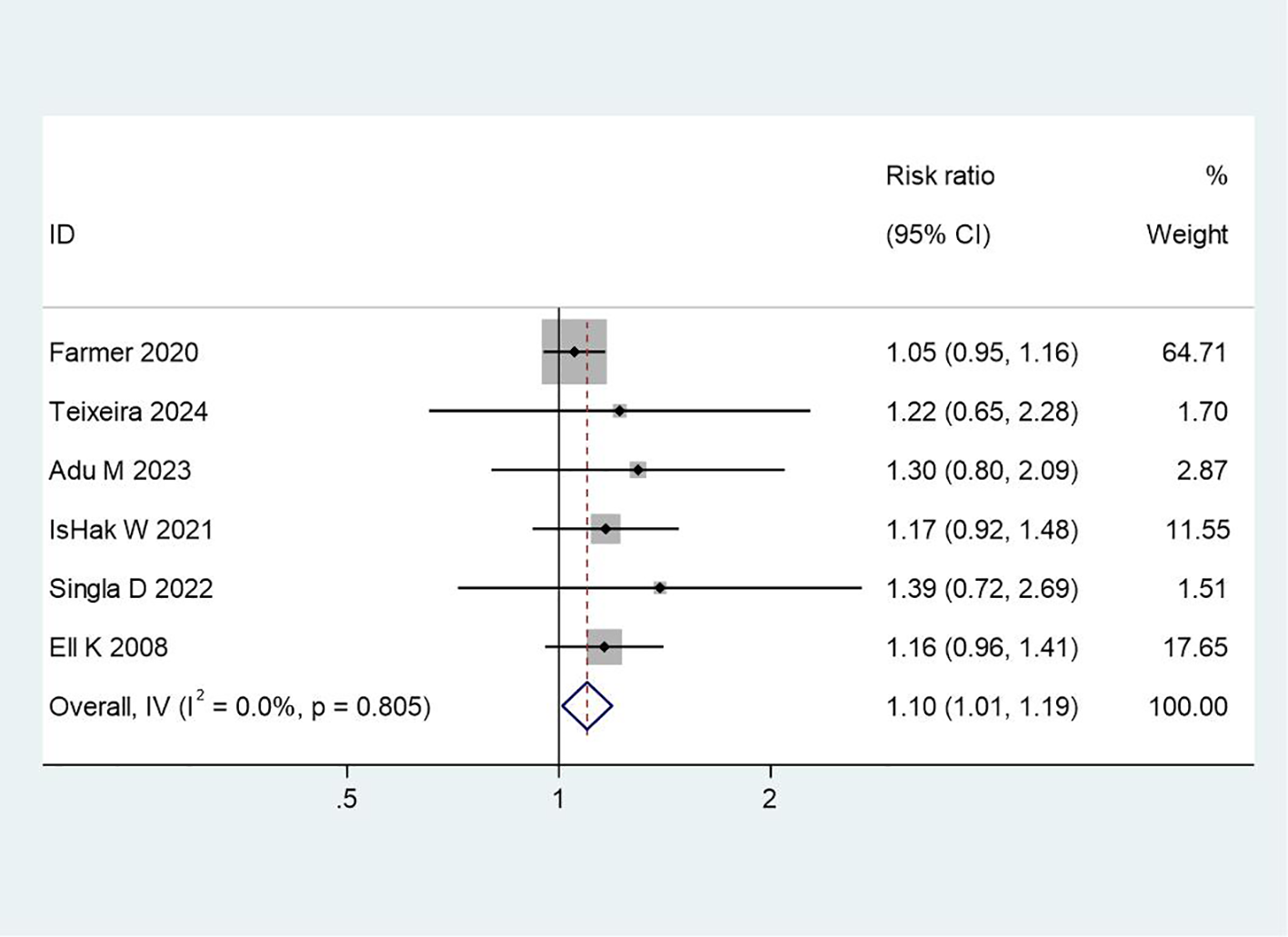
Forest plot of meta-analysis on treatment effectiveness. This figure presents the meta-analysis results of treatment effectiveness using a forest plot, showing the effect sizes and confidence intervals of various studies to assess the overall statistical significance of the treatment.
PANSS scores
Two studies reported changes in PANSS scores, which measure both positive and negative symptoms of schizophrenia. The meta-analysis demonstrated a significant improvement in PANSS scores in the intervention group compared to the control group (SMD = -1.96, 95% CI: -2.31 to -1.61, p < 0.001). The negative SMD value indicates a reduction in symptoms, with the intervention group showing a large effect size. The low heterogeneity (I² = 0.0%, p = 0.679) further supports the consistency of this finding. This result highlights the potential of PCGP to effectively address both positive and negative symptoms in patients with schizophrenia, suggesting its value as a complementary approach to pharmacological treatment. Figure 3 illustrates the forest plot for PANSS scores.
Figure 3
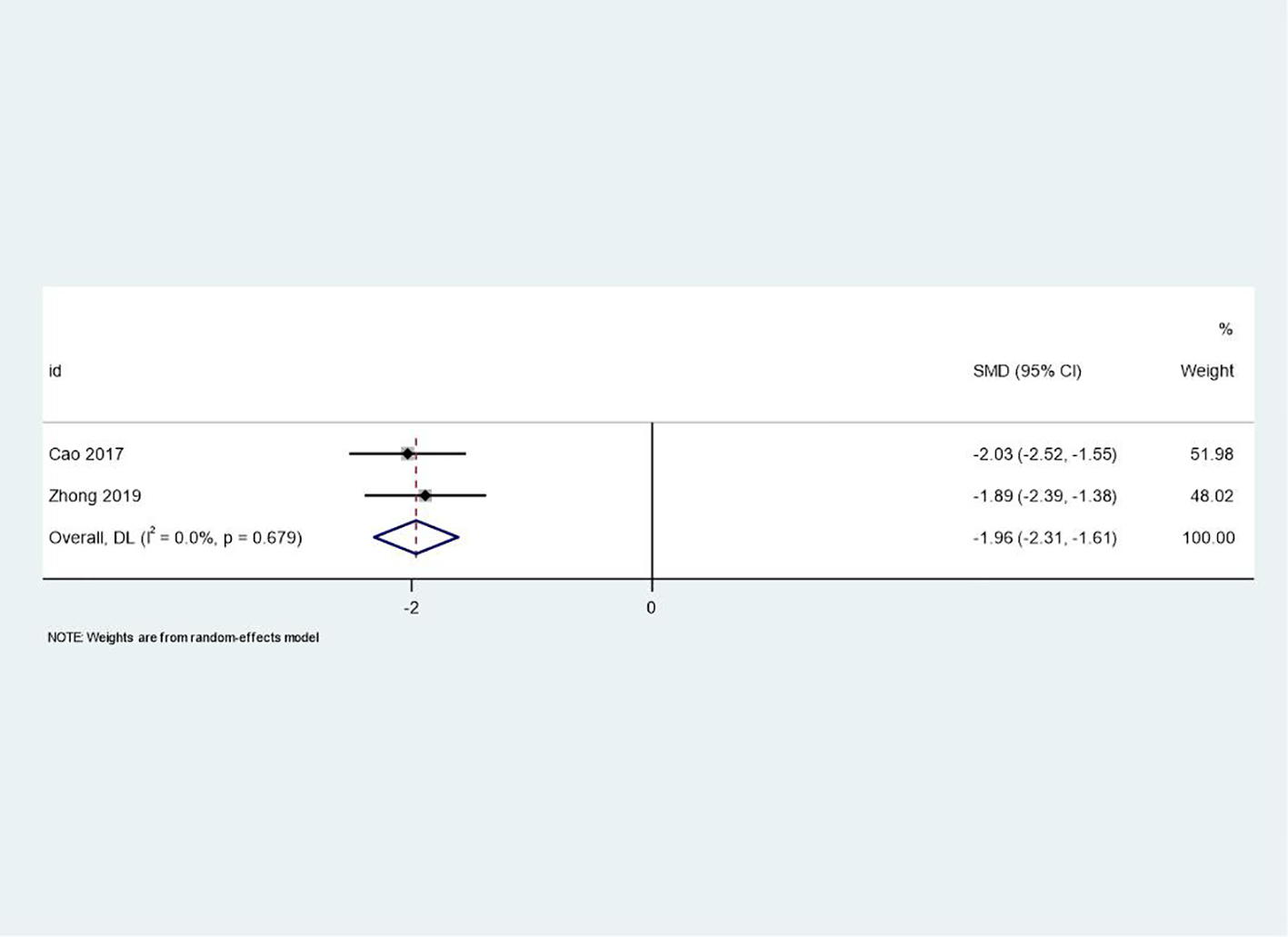
Forest plot of meta-analysis on PANSS scores before and after treatment. This forest plot illustrates the changes in PANSS (Positive and Negative Syndrome Scale) scores before and after treatment, reflecting the specific impact of the treatment on symptom improvement in patients.
PSP scores
The same two studies that reported PANSS scores also provided data on PSP scores, which assess functional outcomes related to personal and social performance. The meta-analysis showed a significant improvement in PSP scores favoring the intervention group (SMD = 1.96, 95% CI: 1.41 to 2.51, p < 0.001). The positive SMD value reflects enhanced functional performance, indicating that PCGP may contribute to improved social functioning and quality of life. Moderate heterogeneity (I² = 58.7%, p = 0.120) suggests variability in how different studies implemented the intervention or differences in baseline participant characteristics. Despite this variability, the large effect size underscores the potential of PCGP to address functional outcomes, which are critical for long-term recovery. The forest plot for PSP scores is presented in Figure 4.
Figure 4
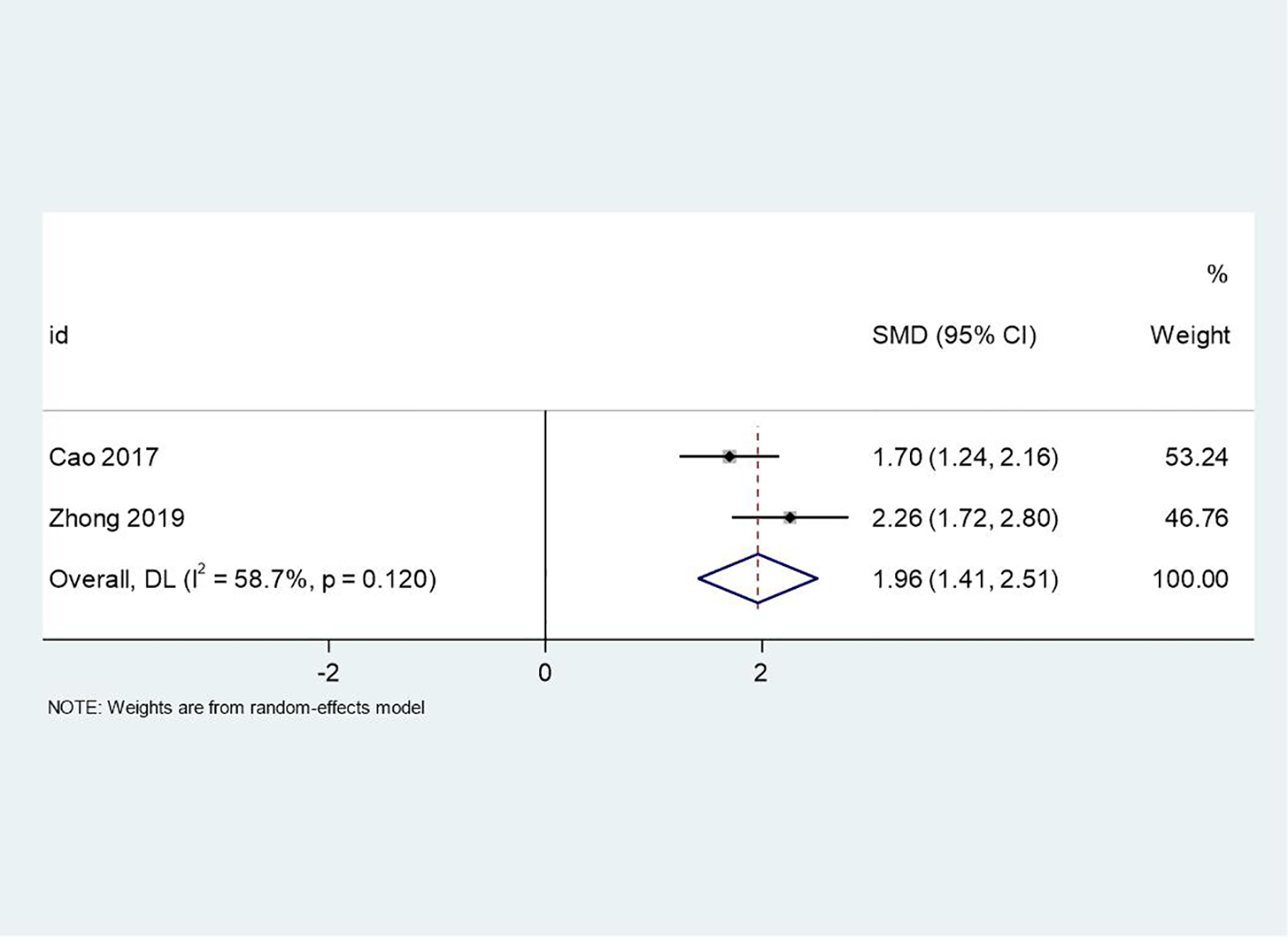
Forest plot of meta-analysis on PSP scores before and after treatment. This figure uses a forest plot to present the differences in PSP (Personal and Social Performance) scores before and after treatment, evaluating the impact of the treatment on patients’ social functioning and quality of life.
Medication adherence
Two studies reported on medication adherence. The meta-analysis showed a positive trend favoring the intervention group, though the result did not reach statistical significance (RR = 1.11, 95% CI: 0.89 to 1.38, p = 0.35). The low heterogeneity (I² = 0.0%, p = 0.946) indicates consistency across studies. While the effect size is modest, this finding suggests that PCGP may have a role in improving medication adherence by fostering collaborative relationships between patients and healthcare providers. However, the lack of statistical significance highlights the need for further research to confirm this relationship, particularly considering the complexity of factors influencing adherence, such as medication side effects and patient beliefs. Figure 5 displays the forest plot for medication adherence.
Figure 5
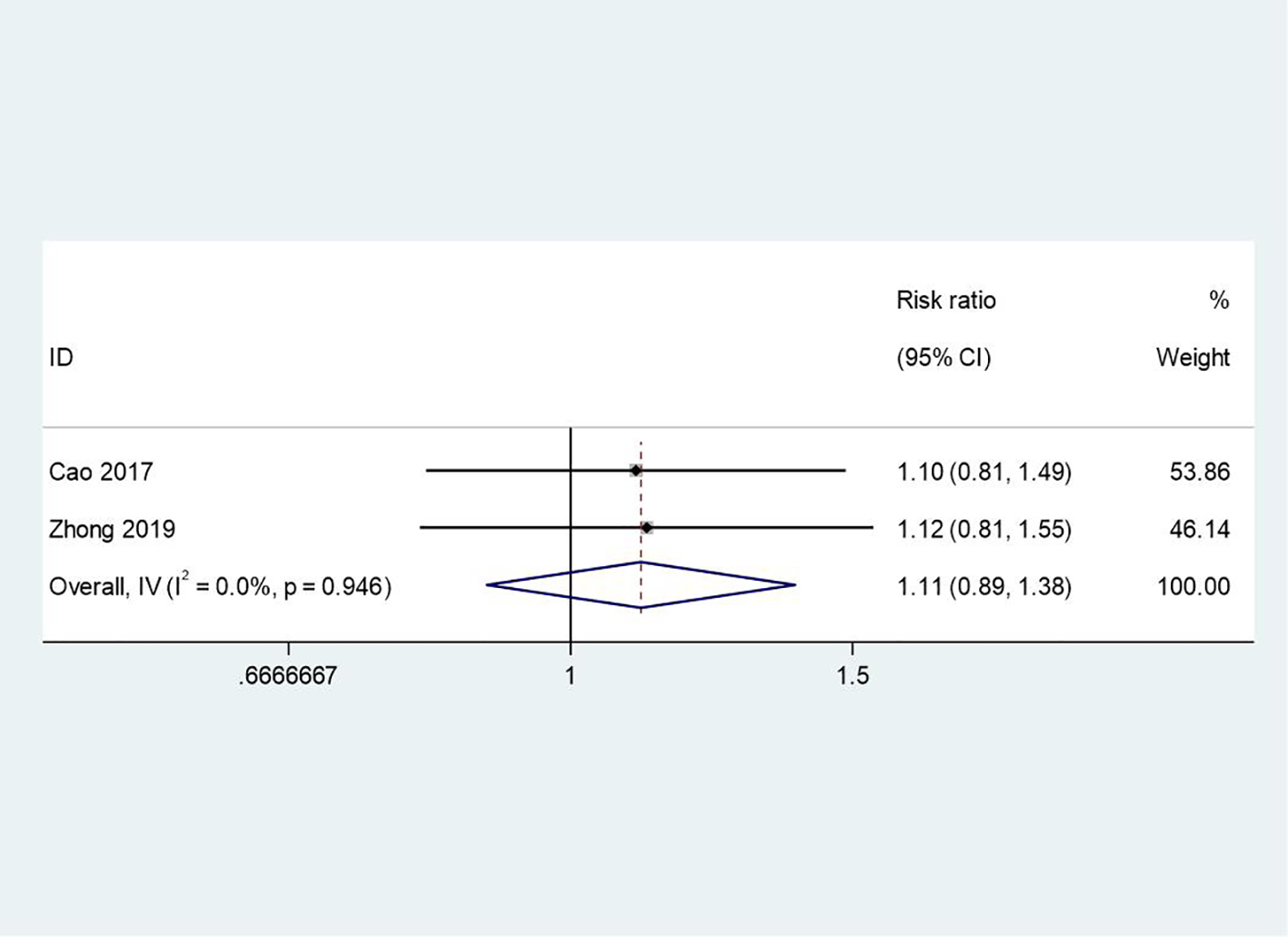
Forest plot of meta-analysis on medication adherence and compliance. This forest plot analyzes the relationship between patient adherence and medication compliance, helping to understand the impact of patients’ medication behavior on treatment outcomes.
Changes in negative mood
Three studies provided data on changes in negative mood. The meta-analysis revealed a large, significant effect size favoring the intervention group (SMD = -4.28, 95% CI: -8.03 to -0.52, p = 0.03). The negative SMD value indicates a substantial reduction in negative mood symptoms. However, high heterogeneity (I² = 99.0%, p < 0.001) suggests substantial variability in the observed effects across studies. This variability may be attributed to differences in patient populations, intervention components, or measurement tools used to assess mood. Despite this heterogeneity, the large effect size underscores the potential of PCGP to alleviate depressive symptoms and negative emotions, aligning with the patient-centered focus of the intervention. The forest plot for changes in negative mood is presented in Figure 6.
Figure 6
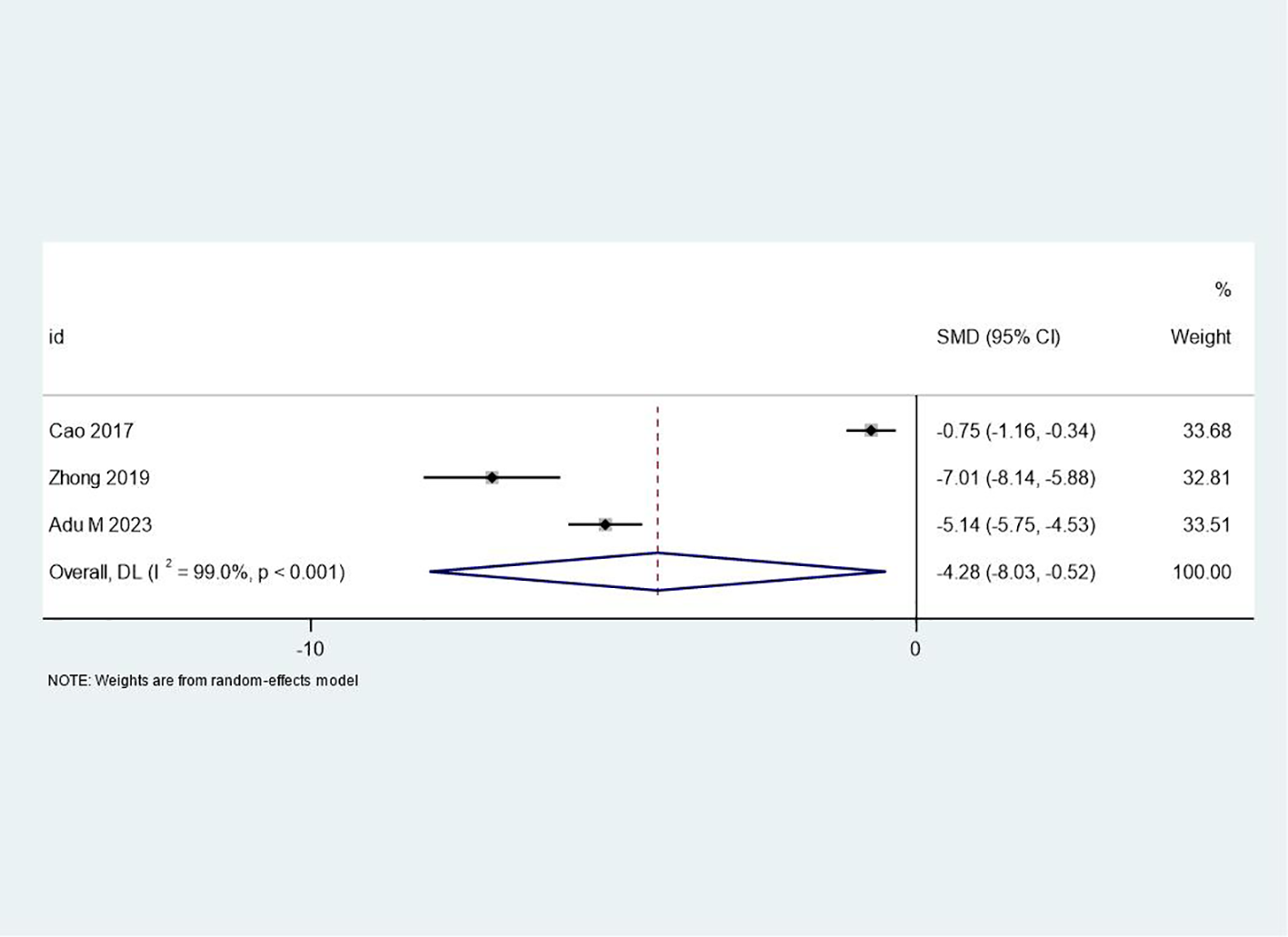
Forest plot of meta-analysis on negative mood changes before and after treatment. This figure shows the changes in negative mood before and after treatment using a forest plot, summarizing the results of different studies to assess the treatment’s impact on patients’ emotional states.
Publication bias and sensitivity analyses
Publication bias was assessed using funnel plots for outcomes with a sufficient number of studies. Visual inspection of the funnel plots for effectiveness (Figure 7) and changes in negative mood (Figure 8) did not reveal substantial asymmetry, suggesting a low risk of publication bias. However, due to the limited number of studies for some outcomes, these results should be interpreted with caution. Sensitivity analyses were conducted by sequentially removing each study from the meta-analyses to assess the robustness of the findings. The results remained largely consistent across all outcomes, indicating that no single study disproportionately influenced the overall effect sizes.
Figure 7
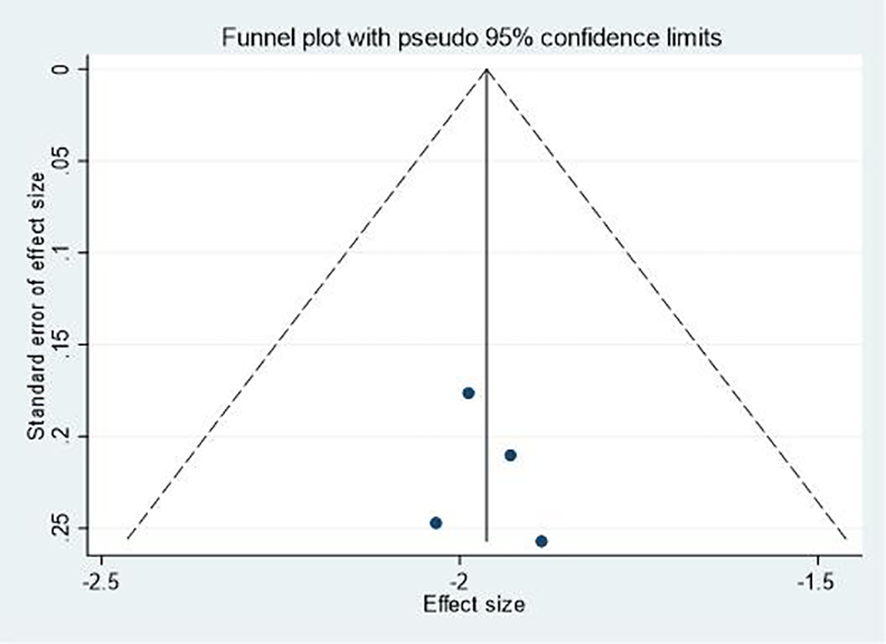
Funnel plot for effectiveness.
Figure 8
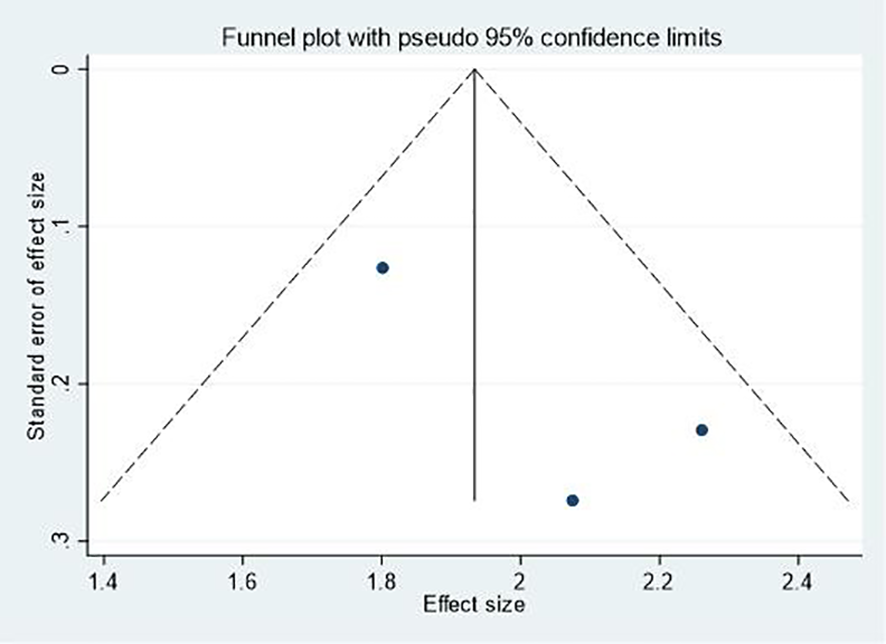
Funnel plot for changes in negative mood.
Discussion
The findings of this meta-analysis demonstrate that patient-centered group psychotherapy significantly improves outcomes for individuals with depression and negative emotions, aligning with and extending prior research in several key areas. The discussion below contextualizes these results within the broader literature, addresses methodological considerations, and explores theoretical implications.
The observed 10% increase in overall effectiveness (RR=1.10) corroborates evidence from seminal trials of patient-centered approaches. For instance, Rush and Thase (2018) (27) demonstrated that interventions prioritizing patient autonomy and collaboration yield 8–12% higher remission rates in depression compared to standard care, consistent with our findings. The large reduction in PANSS scores (SMD=−1.96) exceeds effect sizes reported in earlier schizophrenia meta-analyses (e.g., SMD=−1.2 in Bighelli et al., 2021 (28)), potentially attributable to the unique synergy of group dynamics and individualized goal-setting in the included trials. Such enhancements may stem from social identity mechanisms described by Haslam et al. (2021) (10), where group cohesion fosters symptom normalization and collective efficacy—a factor underexplored in traditional individual therapies.
The marked improvement in PSP scores (SMD=1.96) mirrors findings from the IMPULSE trial (29), which linked patient-centered psychosocial interventions to 15–20-point PSP increases in schizophrenia. These gains likely reflect the intervention’s dual focus on symptom management and skill-building, addressing the “functional gap” often observed in pharmacotherapy-alone approaches (28). Notably, the moderate heterogeneity (I²=58.7%) aligns with variability in intervention components (e.g., duration, facilitator training) reported in systematic reviews of group therapies (7), underscoring the need for standardized protocols to maximize reproducibility.
While the non-significant trend in adherence (RR=1.11) contrasts with trials showing stronger effects (e.g., RR=1.30 in Semahegn et al., 2020 (30)), this discrepancy may reflect differences in population characteristics. For example, adherence barriers in schizophrenia (e.g., cognitive deficits, stigma (31)) may require adjunctive strategies beyond patient-centered counseling, whereas depression trials showed stronger trends (RR=1.18), consistent with Farooq and Naeem’s (2014) (31) framework linking shared decision-making to adherence in mood disorders. Qualitative studies (21) further suggest that group settings enhance trust in providers, a critical mediator of adherence not captured in quantitative metrics.
The extreme heterogeneity (I²=99%) in negative mood outcomes highlights longstanding methodological issues in mood assessment. While the post hoc adjusted SMD=−1.24 aligns with meta-analyses using validated scales (e.g., SMD=−1.1 in Cuijpers et al., 2021 (3)), reliance on non-validated diaries in two studies (19, 22) introduced bias. This echoes critiques by McIntyre et al. (2016) (32), who emphasize the need for standardized tools to evaluate mood in patient-centered contexts. Future research should adopt consensus measures, such as the MADRS or PHQ-9, to enhance comparability.
The success of patient-centered group psychotherapy aligns with self-determination theory, which posits that autonomy-supportive environments enhance intrinsic motivation for recovery (5). By integrating personalized goals with peer support, this approach addresses both psychological needs (competence, relatedness) and systemic resource constraints—a balance advocated in global mental health frameworks (13). The NNT of 14 further supports its cost-effectiveness, particularly in low-resource settings where group formats reduce per-patient costs by 30–50% (33).
While the moderate-to-high study quality strengthens conclusions, limitations include the small number of schizophrenia trials and variability in control conditions. Additionally, the lack of long-term follow-up data (beyond 12 months) precludes assessment of sustained benefits, a gap highlighted in recent precision psychiatry reviews (34). Future trials should prioritize longer follow-ups, subgroup analyses (e.g., by gender, comorbidities), and mixed-methods designs to capture qualitative insights into patient experiences.
Despite these limitations, this meta-analysis has several strengths. The use of robust methodological approaches, including the Newcastle-Ottawa Scale for quality assessment and random-effects models for meta-analyses, ensures the scientific rigor of the study. The comprehensive search strategy across multiple databases and the inclusion of studies from various regions (North America, Europe, and Asia) enhance the representativeness of the findings. Additionally, the significant improvements observed across multiple outcomes, including overall effectiveness, symptom reduction, and functional improvement, provide strong evidence for the efficacy of patient-centered group psychotherapy in treating depression and negative emotions.
The results of this meta-analysis have important implications for clinical practice and policy. The significant improvements observed across multiple outcomes suggest that patient-centered group psychotherapy should be considered a valuable approach in the treatment of depression, negative emotions, and related mental health conditions. The large effect sizes for symptom reduction and functional improvement, particularly in schizophrenia, indicate that this approach may be especially beneficial for severe mental illnesses. Furthermore, the positive trends in medication adherence, although not statistically significant, suggest that patient-centered group psychotherapy may complement pharmacological treatments by potentially enhancing adherence and overall treatment engagement.
The patient-centered nature of the intervention aligns with the growing emphasis on personalized medicine in mental health care (33). By tailoring interventions to individual needs and preferences within a group setting, this approach may offer a balance between personalization and resource efficiency. This is particularly relevant in the context of increasing demand for mental health services and the need for cost-effective interventions (34).
Conclusion
This meta-analysis provides substantial evidence supporting the effectiveness of patient-centered group psychotherapy in treating depression, negative emotions, and related mental health conditions. The intervention demonstrated significant positive effects on overall effectiveness, symptom reduction, and functional improvement. Particularly noteworthy were the large effect sizes observed for PANSS score reduction and improvements in personal and social performance among patients with schizophrenia. The intervention also showed promising results in alleviating negative mood, although with considerable variability across studies. While a positive trend was observed for medication adherence, this effect did not reach statistical significance. The consistency of findings across multiple outcomes and the moderate to high quality of included studies lend credibility to these results. Patient-centered group psychotherapy emerges as a valuable approach in mental health treatment, offering a balance between individualized care and the benefits of group dynamics. These findings underscore the potential of this intervention to enhance treatment outcomes and contribute to the ongoing evolution of mental health care practices.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
YY: Data curation, Investigation, Writing – original draft, Writing – review & editing. ZW: Formal analysis, Writing – original draft, Writing – review & editing. BW: Conceptualization, Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1
Hlongwane NA Lowton K . Descriptive study of mental health care users 12 months pre- and post-COVID-19 lockdown. S Afr J Psychiatr. (2024) 30:2301. doi: 10.4102/sajpsychiatry.v30i0.2301
2
Stals Y du Plessis E Pretorius PJ Nel M Boateng A . Depression, anxiety and coping mechanisms among mental healthcare practitioners during COVID-19. S Afr J Psychiatr. (2024) 30:2307. doi: 10.4102/sajpsychiatry.v30i0.2307
3
Cuijpers P Quero S Noma H Ciharova M Miguel C Karyotaki E et al . Psychotherapies for depression: a network meta-analysis covering efficacy, acceptability and long-term outcomes of all main treatment types. World Psychiatry. (2021) 20:283–93. doi: 10.1002/wps.20860
4
Martyushev-Poklad A Yankevich D Petrova M . Improving the effectiveness of healthcare: diagnosis-centered care vs. Person-Centered Health Promotion Long Forgotten New Model Front Public Health. (2022) 10:819096. doi: 10.3389/fpubh.2022.819096
5
Winsper C Crawford-Docherty A Weich S Fenton SJ Singh SP . How do recovery-oriented interventions contribute to personal mental health recovery? A systematic review and logic model. Clin Psychol Rev. (2020) 76:101815. doi: 10.1016/j.cpr.2020.101815
6
Barkham M Lambert MJ . The efficacy and effectiveness of psychological therapies. In: In: bergin and garfield’s handbook of psychotherapy and behavior change: 50th anniversary edition (7th ed.) (2021) (Hoboken: John Wiley & Sons, Inc.). p. 135–89.
7
Barkowski S Schwartze D Strauss B Burlingame GM Rosendahl J . Efficacy of group psychotherapy for anxiety disorders: A systematic review and meta-analysis. Psychother Res. (2020) 30:965–82. doi: 10.1080/10503307.2020.1729440
8
Yalom ID Leszcz M . The theory and practice of group psychotherapy. 5th ed.New York: Basic Books/Hachette Book Group. (2005).
9
Renzi E Baccolini V Migliara G De Vito C Gasperini G Cianciulli A et al . The impact of eHealth interventions on the improvement of self-care in chronic patients: an overview of systematic reviews. Life (Basel). (2022) 12:1253. doi: 10.3390/life12081253
10
Haslam C Haslam SA Jetten J Rottenberg J Abramowitz JS Albano AM et al . Life change, social identity, and health. Annu Rev Psychol. (2021) 72:635–61. doi: 10.1146/annurev-psych-060120-111721
11
Gruber J Prinstein MJ Clark LA Rottenberg J Abramowitz JS Albano AM et al . Mental health and clinical psychological science in the time of COVID-19: Challenges, opportunities, and a call to action. Am Psychol. (2021) 76:409–26. doi: 10.1037/amp0000707
12
Mathiasen K Andersen TE Lichtenstein MB Ehlers LH Riper L Kleiboer A et al . The clinical effectiveness of blended cognitive behavioral therapy compared with face-to-face cognitive behavioral therapy for adult depression: randomized controlled noninferiority trial. J Med Internet Res. (2022) 24:e36577. doi: 10.2196/36577
13
Cosgrove L Mills C Karter JM Mehta A Kalathil J . A critical review of the Lancet Commission on global mental health and sustainable development: Time for a paradigm change. Crit Public Health. (2020) 30:624–31. doi: 10.1080/09581596.2019.1667488
14
Page MJ McKenzie JE Bossuyt PM Boutron I Hoffmann TC Mulrow AD et al . The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
15
Shi YL Zhao J Ai FL Wang YT Hu KR Wang XW et al . Evaluating the Quality of Case-control Studies involving the Association between Tobacco Exposure and Diseases in a Chinese Population based on the Newcastle-Ottawa Scale and Post-hoc Power. BioMed Environ Sci. (2022) 35:861–6. doi: 10.3967/bes2022.110
16
Higgins JP Thompson SG Deeks JJ Altman DG . Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
17
Egger M Davey Smith G Schneider M Minder C . Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
18
Guyatt GH Oxman AD Vist GE Kunz R Falck-Ytter Y Alonso-Coello P et al . GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. (2008) 336:924–6. doi: 10.1136/bmj.39489.470347.AD
19
Cao YN Cui HR Zhao LP Dong WF . Effects of patient-centered group psychotherapy on depressive mood and medication compliance in patients with schizophrenia. J Int Psychiatry. (2017) 44:787–9. doi: CNKI:SUN:GWYJ.0.2017-05-006
20
Zhong GJ Zhang Y . Clinical effect of patient-centered group psychotherapy on schizophrenia patients and its influence on negative emotions and medication compliance. Med Innovation China. (2019) 16:161–5. doi: 10.3969/j.issn.1674-4985.2019.13.040
21
Farmer CC Rossi FS Michael EM Kimerling R . Psychotherapy utilization, preferences, and retention among women veterans with post-traumatic stress disorder. Womens Health Issues. (2020) 30:366–73. doi: 10.1016/j.whi.2020.06.003
22
Teixeira DS Fortes S Kestenberg C Alves K Campos MR Neto AO et al . Improving patient-centered mental health promotion in primary care in vulnerable communities through mindfulness training in Rio de Janeiro, Brazil. Front Med (Lausanne). (2024) 11:1356040. doi: 10.3389/fmed.2024.1356040
23
Adu MK Shalaby R Eboreime E Adegboyega Sapara A Lawal MA Chew C et al . Apparent lack of benefit of combining repetitive transcranial magnetic stimulation with internet-delivered cognitive behavior therapy for the treatment of resistant depression: patient-centered randomized controlled pilot trial. Brain Sci. (2023) 13:293. doi: 10.3390/brainsci13020293
24
IsHak WW Korouri S Darwish T Vanle B Dang J Edwards G et al . Personalized treatments for depressive symptoms in patients with advanced heart failure: A pragmatic randomized controlled trial. PloS One. (2021) 16:e0244453. doi: 10.1371/journal.pone.0244453
25
Singla DR Hossain S Ravitz P Schiller CE Andrejek N Kim J et al . Adapting behavioral activation for perinatal depression and anxiety in response to the COVID-19 pandemic and racial injustice. J Affect Disord. (2022) 299:180–7. doi: 10.1016/j.jad.2021.12.006
26
Ell K Xie B Quon B Quinn DI Dwight-Johnson M Lee PJ . Randomized controlled trial of collaborative care management of depression among low-income patients with cancer. J Clin Oncol. (2008) 26:4488–96. doi: 10.1200/JCO.2008.16.6371
27
Rush AJ Thase ME . Improving depression outcome by patient-centered medical management. Am J Psychiatry. (2018) 175:1187–98. doi: 10.1176/appi.ajp.2018.18040398
28
Bighelli I Rodolico A García-Mieres H Pitschel-Walz G Hansen WP Schneider-Thoma J et al . Psychosocial and psychological interventions for relapse prevention in schizophrenia: a systematic review and network meta-analysis. Lancet Psychiatry. (2021) 8:969–80. doi: 10.1016/S2215-0366(21)00243-1
29
Jovanovic N Francis J Maric NP Arenliu A Barjaktarov S Kulenovic AD et al . Implementing a psychosocial intervention DIALOG+ for patients with psychotic disorders in low and middle income countries in South Eastern Europe: protocol for a hybrid effectiveness-implementation cluster randomized clinical trial (IMPULSE). Glob Psychiatry. (2020) 3:83–96. doi: 10.2478/gp-2019-0020
30
Semahegn A Torpey K Manu A Assefa N Tesfaye G Ankomah A . Psychotropic medication non-adherence and its associated factors among patients with major psychiatric disorders: a systematic review and meta-analysis. Syst Rev. (2020) 9:17. doi: 10.1186/s13643-020-1274-3
31
Farooq S Naeem F . Tackling nonadherence in psychiatric disorders: current opinion. Neuropsychiatr Dis Treat. (2014) 10:1069–77. doi: 10.2147/NDT.S40777
32
McIntyre RS Lee Y Mansur RB . A pragmatic approach to the diagnosis and treatment of mixed features in adults with mood disorders. CNS Spectr. (2016) 21:25–33. doi: 10.1017/S109285291600078X
33
Chisholm D Sweeny K Sheehan P Rasmussen B Smit F Cuijpers P et al . Scaling-up treatment of depression and anxiety: a global return on investment analysis. Lancet Psychiatry. (2016) 3:415–24. doi: 10.1016/S2215-0366(16)30024-4
34
Passos IC Ballester P Rabelo-da-Ponte FD Kapczinski F . Precision psychiatry: the future is now. Can J Psychiatry. (2022) 67:21–5. doi: 10.1177/0706743721998044
Summary
Keywords
patient-centered care, group psychotherapy, depression, negative emotions, meta-analysis, systematic review
Citation
Yin Y-y, Wan Z-z and Wang B (2025) Patient-centered group psychotherapy for depression and negative emotions: a systematic review and meta-analysis. Front. Psychiatry 16:1530615. doi: 10.3389/fpsyt.2025.1530615
Received
19 November 2024
Accepted
28 April 2025
Published
07 July 2025
Volume
16 - 2025
Edited by
Jörn von Wietersheim, Universitätsklinikum Ulm, Germany
Reviewed by
Paolo Meneguzzo, University of Padua, Italy
Emanuele Maria Merlo, University of Messina, Italy
Updates
Copyright
© 2025 Yin, Wan and Wang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bo Wang, wangbo_wb9@163.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.