- 1Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 2Department of Substance Dependence, Third People's Hospital of Fuyang, Fuyang, China
- 3Department of Psychiatry, The Affiliated Brain Hospital of Nanjing Medical University, Nanjing, Jiangsu, China
Introduction: The escalating severity of gambling issues in China highlights the need for culturally adapted assessment tools. The Yale-Brown Obsessive Compulsive Scale for Pathological Gambling (PG-YBOCS) is recognized for its ability to assess both the severity and compulsive features of gambling disorder.
Methods: Given its emphasis on the compulsive features of gambling disorder, this study aimed to validate the Chinese version (PG-YBOCS-C) in clinical assessment. The 10-item PG-YBOCS-C was developed through translation and expert review. A total of 116 individuals with gambling disorder were recruited.
Results: Reliability was assessed using Cronbach’s α coefficient (0.958) and test-retest reliability (0.722). The content validity index was 0.912, with item-level indices ranging from 0.778 to 1.000. Bartlett’s test of sphericity yielded X2 = 1123.86, P<0.001, and the KMO measure was 0.93. Exploratory factor analysis identified a single principal component accounting for 72.8% of the variance.
Discussion: The reliability and validity of PG-YBOCS-C have been demonstrated, establishing it as a dependable tool for evaluating the severity of gambling symptoms in Chinese individuals.
1 Introduction
Gambling Disorder (GD), according to the DSM-5, is characterized by persistent and recurrent gambling behavior causing significant psychological distress or social impairment (1). The World Health Organization (WHO) reports that approximately 0.1% to 6% of adults worldwide suffer from this disorder (2). GD affects mental health, causing anxiety, depression, and suicidal ideation. It also leads to financial crises, social isolation, family breakdowns, and criminal behavior, increasing public health burdens and social instability (3).
According to a 2021 report by the United Nations Office on Drugs and Crime (UNODC), the illegal sports betting market sees annual wagers of up to $1.7 trillion (UN 4). This figure unequivocally highlights the significant risks and potential harms associated with gambling. Additionally, internet gambling has proliferated with the rapid development of the digital age due to its convenience, interactivity, and anonymity. It has become the fastest-growing mode of gambling, fundamentally changing how gamblers participate and making gambling behavior more difficult to regulate and control (5, 6).
In China, small-scale gambling is often seen as a form of entertainment deeply rooted in cultural traditions. In recent years, the prevalence of gambling has surged, surpassing levels seen in many other countries, and this situation has been further exacerbated by the rise of online gaming, which has become the dominant form of gambling in China (7). Despite laws prohibiting all forms of gambling, societal tolerance remains high, contributing to the popularity of gambling, particularly during major festivals (3, 8). However, social acceptance of gambling does not extend to an understanding of GD, which is often stigmatized and attributed to moral failings (9). This complex legal and cultural context leads to individuals with GD hiding their problems and being reluctant to seek help due to fear of legal consequences and stigma (10). Studies credited by Slutske (11) indicated that only 10% of individuals with GD seek treatment.
Assessing the severity of gambling is crucial for the treatment of GD, helping to determine individual risk levels and formulate targeted treatment plans. Currently, various scales for measuring GD have been developed internationally. Among these, self-report scales such as the Canadian Problem Gambling Index (CPGI) and the South Oaks Gambling Screen (SOGS) are widely used (12). However, these tools primarily rely on self-reports. In clinical studies, self-reported outcomes from individuals with GD may be biased due to their awareness of having received an intervention, particularly in terms of reported gambling behaviors and perceptions. Conversely, outcomes measured by an independent, blinded professional would have a lower risk of bias when assessing treatment effect (13). Additionally, individuals with GD may underestimate or deny the severity of their problems due to social pressure or distorted self-perception (14). Studies have shown that the self-reports of people with GD often indicate lower severity than those observed by third parties (10).
Observer rating scales, such as the Yale-Brown Obsessive Compulsive Scale for Pathological Gambling (PG-YBOCS), may provide a more objective method of assessment, combining observation and questioning, which may increase diagnostic reliability when examining treatment effects (15, 16). Moreover, GD shares significant neurocognitive characteristics with obsessive-compulsive disorder (OCD), including ritualized behaviors, intrusive thoughts, and diminished impulse control (16). The PG-YBOCS developed by Pallanti et al. (16) specifically targets gambling-related thoughts and behaviors, measuring the severity of obsessive-compulsive disorder, especially for obsessions and compulsions. Multiple studies confirmed that PG-YBOCS can effectively distinguish different severity levels of GDs and has been widely used as a primary measure of treatment efficacy (17–20). PG-YBOCS has been translated into several languages, such as Japanese (21), demonstrating its cross-cultural applicability and importance in global addiction research.
In China, several self-report tools for GD exist, including the Chinese Version of the Canadian Problem Gambling Index, the South Oaks Gambling Screen and the Chinese Gambling Urge Scale (22–24). An observer rating scale administered by a professional, such as a psychologist or a clinical tester in clinical assessment has not been developed. Given the gap in GD assessment, the objective and standardized PG-YBOCS can effectively measure the severity of GDs. Localizing and validating the Chinese Version of PG-YBOCS (PG-YBOCS-C) is crucial for assessing and treating GDs in China, promoting clinical research in this field.
2 Methods
2.1 Participants
From September 2023 to June 2024, 116 male individuals with GD in the Department of Addiction Treatment at Shanghai Mental Health Center in Mainland China were recruited. The average age was 30.63 years (SD = 6.33, range: 22-55), the average education duration was 14.69 years (SD = 6.88, range: 6-19), and the average duration of gambling was 7.72 years(SD = 4.97, range: 1-30).
Inclusion criteria: Individuals who met the diagnostic criteria for GD in DSM-5 (≥4); had sufficient cognitive ability to complete all assessments and related clinical examinations required for this study; and exhibited normal hearing and vision.
Exclusion criteria: IQ < 70; had taken medications that promoted cognitive functions in recent months; had other physical diseases or cognitive impairments besides GD, such as schizophrenia; other situations deemed unsuitable for participation in the study by the researchers.
2.2 Procedure
The adaptation of PG-YBOCS for the Chinese context involved a rigorous and meticulous process to ensure linguistic accuracy and cultural relevance. The PG-YBOCS-C was translated from the original scale into Chinese by two experts in GD, and the initial Chinese version was formed after review. Subsequently, a bilingual expert who had not previously been exposed to the original scale translated the initial Chinese version into English to ensure translation accuracy. An expert committee then reviewed the translation to ensure content and conceptual equivalence between the original and the Chinese version. To validate and refine the scale, the initial Chinese version was first pretested on 30 individuals with GD, and revisions and cross-cultural wording adjustments were made based on feedback. Ultimately, after multiple rounds of correction and optimization, the PG-YBOCS-C used in this study was finalized.
Individuals with GD who met the experimental criteria were required to complete the assessment. Before the formal assessment, they read and signed the informed consent form and completed the PG-YBOCS-C rating by others as well as other related questionnaires under the guidance of trained professional assessors. The PG-YBOCS-C assessment took approximately 10 minutes, conducted through interviews with each individual by professional assessors, without direct contact with the test items by the individuals. Other questionnaires were completed by themselves. The PG-YBOCS-C retest rating by others was completed two weeks later through telephone interviews conducted by professional assessors. All assessors received standardized training in PG-YBOCS-C interview techniques by experienced clinicians, using a scoring manual to ensure consistency in administration and rating. In total, 55 individuals with GD completed the retest.
2.3 Measures
The evaluation scores of the Gambling Symptom Assessment Scale (G-SAS) for GD reflect the specific severity of GD, which is consistent with the measurement direction of the rating tool aimed to be revised in this study. The score of the Gambling Eagerness Scale (GES) indicates the level of immediate gambling eagerness. Therefore, the G-SAS and the GES for GD are used as the primary criterion for measurement in this study. Additionally, GD has significant associations with traits such as motor impulsivity, decision-making impulsivity, and individual self-control ability (25). Therefore, this study also measured the Barratt Impulsiveness Scale (BIS-11) and the Chinese Version of the Self Control Scale (SCS) as criteria (26).
2.3.1 DSM-5 criteria for gambling disorder
The DSM-5 provides a comprehensive diagnostic framework for identifying GD. According to the assessment standards of DSM-5 (1), a score over 4 was considered indicative of GD. The total score ranged from 4 to 9, with 1 point assigned for meeting each diagnostic criterion. A higher score indicated more pronounced manifestations and severe symptoms of GD. Individuals who meet the diagnostic criteria for GD will be included in this study. DSM-5 is regarded as the gold standard for diagnosing GD due to its high reliability and validity (27).
2.3.2 Pathological Gambling Adaptation of the Yale-Brown Obsessive Compulsive Scale
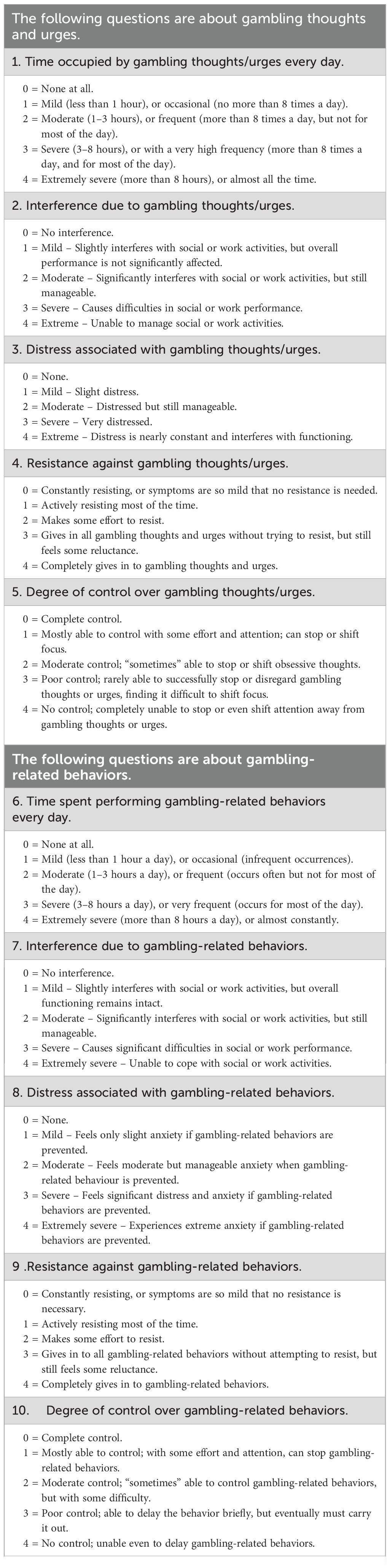
The PG-YBOCS consists of 10 items of clinician-administered questions, primarily measuring gambling thoughts and impulses as well as gambling behaviors. The scale is divided into two sections: the first five items target gambling urges and thoughts while the remaining five focus on the behavioral component of the disorder. Both components assess key domains including time spent on gambling activities, functional impairment, emotional distress, resistance attempts, and perceived control over gambling behavior. It employs a Likert 5-point scale (0-4), assessing the severity of GD during the most recent time interval (usually within the past week). Each question is scored separately, with a total score obtained by summing both. A higher total score indicates a more severe level of GD. The severity is classified as subclinical, mild, moderate, severe, and extreme levels of GD according to the score. Specific scale items are presented in Table 1. Previous research has shown that the Japanese version of PG-YBOCS has good reliability and validity in clinical samples, with a Cronbach’s α of 0.85 (Yokomitsu et al., 2020).
2.3.3 Gambling Symptom Assessment Scale
As a self-report scale, G-SAS is designed to assess the severity of symptoms among GD (28). The scale consists of 12 items that measure gambling symptoms over one week, including gambling urges, gambling thoughts, and actual gambling behaviors. The total score ranges from 0 to 48, with higher scores indicating more severe symptoms. The score is defined as follows: a score below 8 indicates no gambling symptoms; a score of 8–20 indicates mild symptoms; a score of 21–30 indicates moderate symptoms; a score of 31–40 indicates severe symptoms; and a score above 40 indicates extreme gambling symptoms. The Cronbach’s α of G-SAS in this study was 0.926 (29).
2.3.4 Gambling Eagerness Scale
The Gambling eagerness Scale is designed to measure the current level of gambling urges among individuals, requiring individuals with GD to rate their gambling urges based on their immediate feelings (30). This scale is a single-item rating scale ranging from 0 to 10, with 0 representing ‘no eagerness for gambling’ and 10 representing ‘extreme high eagerness for gambling’.
2.3.5 Barratt Impulsiveness Scale Version 11
BIS-11, including 30 items, reflects individuals’ impulsivity levels and is used to assess the likelihood of impulse control disorders. A higher score indicates a greater likelihood of impulse control disorders and more pronounced impulsive characteristics. The Cronbach’s α of BIS-11 in this study was 0.761 (31).
2.3.6 Self-control Scale
The SCS primarily assesses the ability of individuals with GD to exert self-control. The scale consists of 19 items and employs a Likert 5-point scoring system. A higher total score indicates a greater degree of self-control. Analysis in this study revealed that the Cronbach’s α of the SCS in this study was 0.671 (32).
2.4 Statistical analysis
IBM SPSS 23.0 was used for analysis. For item analysis, individuals were ranked in descending order with the top 27% and bottom 27% classified into high and low score groups, respectively. An independent samples t-test was employed to determine the cut-off value. The internal consistency reliability of the scale was assessed by Cronbach’s α, while the test-retest reliability over two weeks was determined through Pearson’s correlation coefficient. Additionally, the content validity of the scale was evaluated by expert consultation at both the item and scale levels. Exploratory factor analysis was conducted to identify the factor structure of the PG-YBOCS-C, with the Kaiser Meyer Olkin (KMO) measure and Bartlett’s test of sphericity ensuring the suitability of factor analysis. The principal component analysis method and varimax rotation were used to explore the factor structure of the scale.
3 Results
3.1 Item analysis
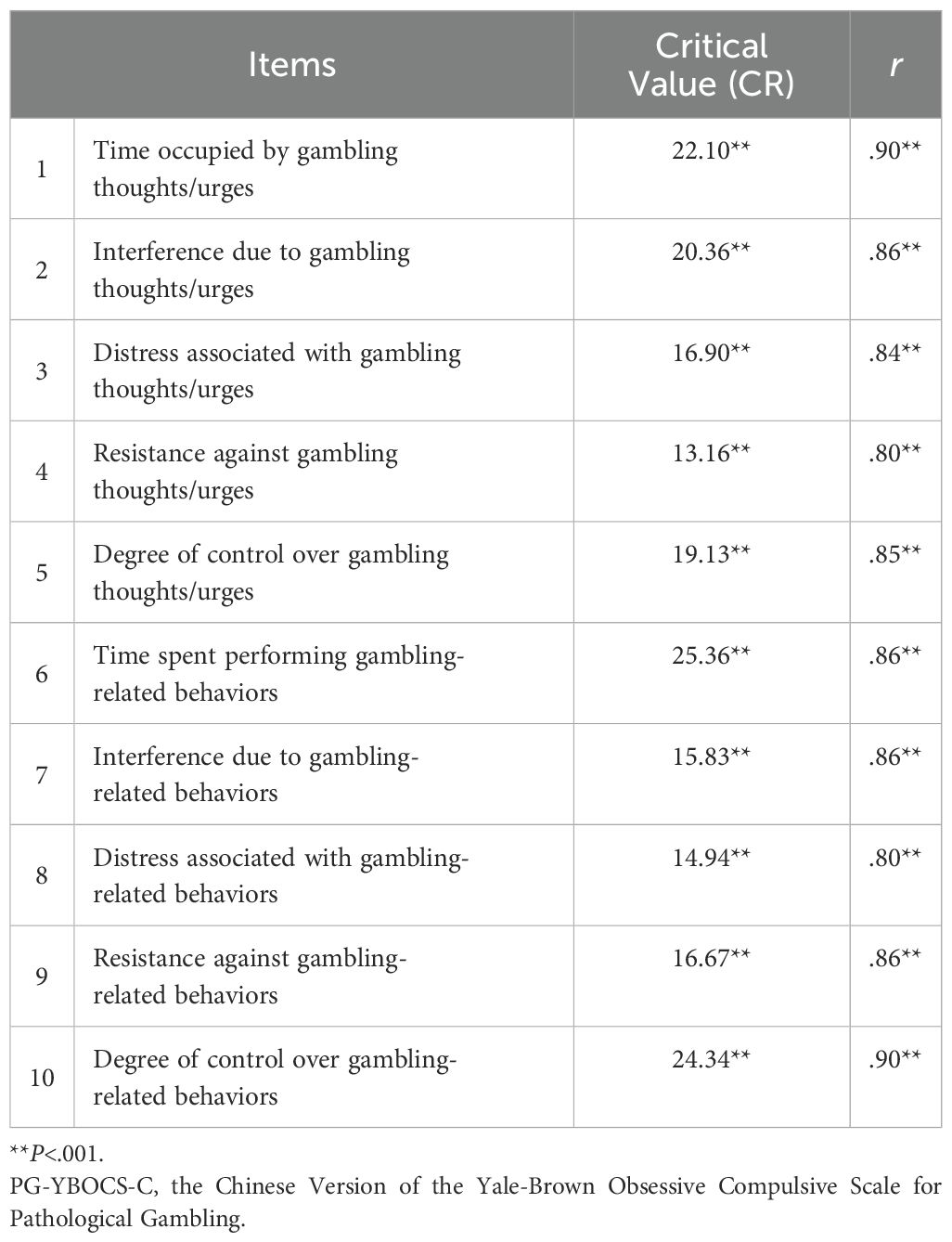
The item analysis revealed that the critical values (CR) of each item ranged from 13.16 to 25.36, with significant differences in scores between the high score and low score groups across all items (P < 0.001). In addition, the Pearson correlation analysis was used to analyze the correlation between individual item scores on the PG-YBOCS-C and the total score. The results showed that each item score was positively correlated with the total scale score at a significant level (Table 2).
3.2 Reliability analysis
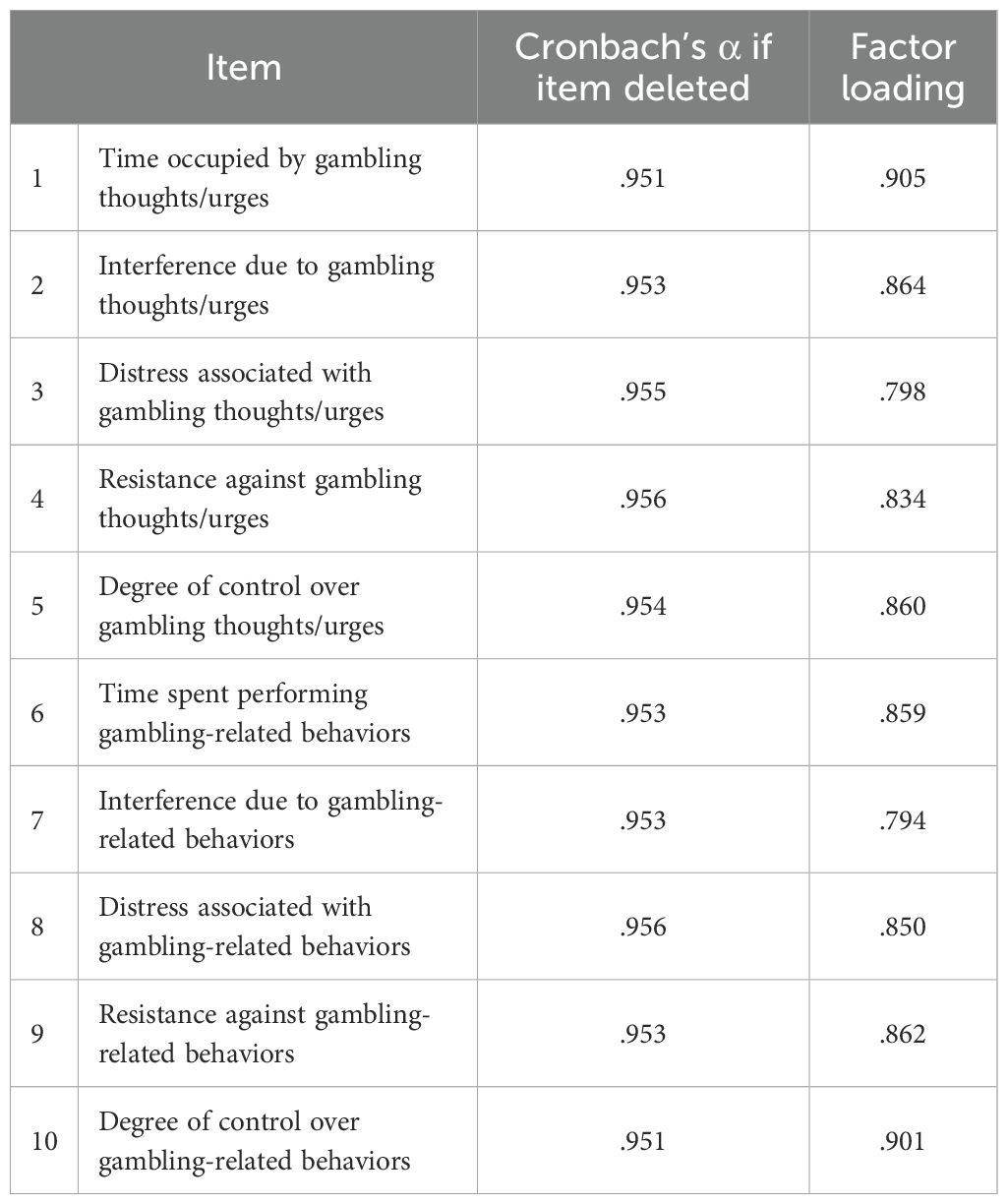
For reliability analysis, the PG-YBOCS-C exhibited strong internal consistency overall with a Cronbach’s α of 0.958. The Cronbach’s α values for each item are detailed in Table 3. Additionally, test-retest reliability was assessed over a two-week interval with a subset of 55 participants. The test-retest reliability of the PG-YBOCS-C was 0.722, with P<0.01, which is statistically significant. The result indicates that the PG-YBOCS-C scale exhibits good stability across time, demonstrating high consistency and reliability.
3.3 Validity analysis
For content validity, the item content validity index (ICVI) and the scale content validity index (SCVI) were evaluated. Nine experts in psychology and psychiatry were invited to rate the appropriateness, comprehensibility, and representativeness of each item on the scale using 5-point scale (1 = very poor, 5 = very good). The ICVI was calculated as the proportion of experts who rated an item as 5, divided by the total number of experts, while the SCVI was derived as the mean of the experts’ ratings. The results showed that ICVI ranged from 0.778 to 1. The SCVI of the PG-YBOCS-C was 0.912, indicating a good content validity of PG-YBOCS-C.
Regarding structural validity, the result indicated that the scale was suitable for subsequent factor analysis (KMO=0.95, Bartlett’s Test of Sphericity X2 = 1123.86, P=0.000<0.01). Based on this, exploratory factor analysis was performed on 116 valid datasets using principal component analysis and varimax rotation, with factors extracted based on eigenvalues greater than 1. This analysis revealed that the PG-YBOCS-C has a unidimensional structure, explaining 72.811% of the total variance. All item factor loadings exceeded 0.4, suggesting strong factor loadings, with the factor loadings detailed in Table 3. These results demonstrate that the PG-YBOCS-C exhibits good structural fit and high structural validity.
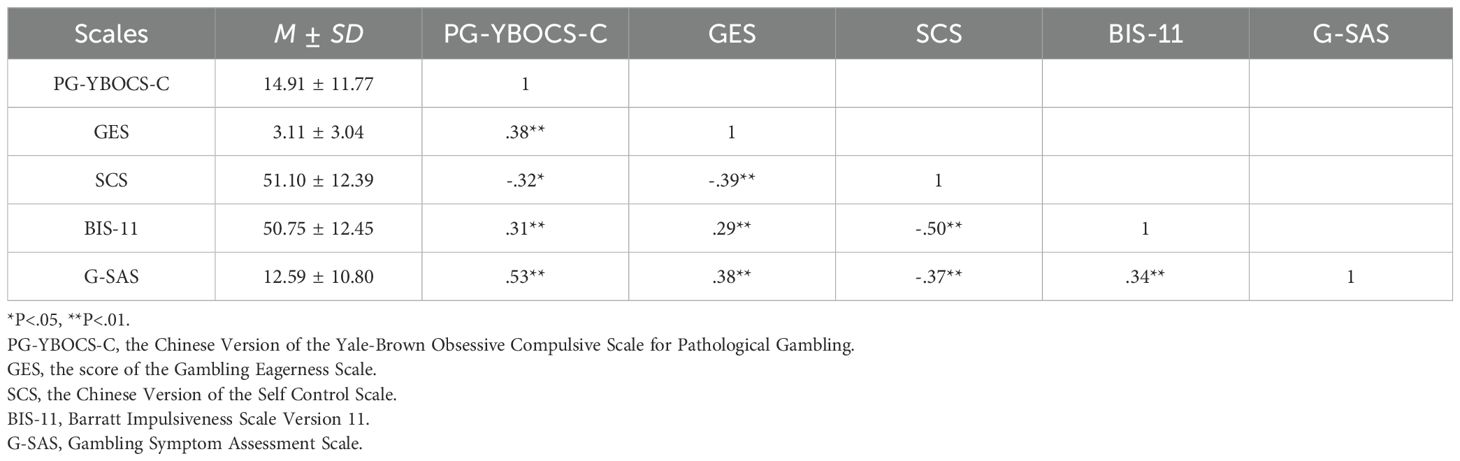
Regarding criterion validity, correlation analysis between the PG-YBOCS-C and other variables(G-SAS, GES, SCS, BIS-11) was conducted. Results about indicators of GD severity showed that the PG-YBOCS-C was significantly correlated with the GES (r=.38, p<.01) and the G-SAS (r=.53, p<.01). Other indicators demonstrated a negative correlation between the PG-YBOCS-C and the SCS (r=-.32, p<.01), while a positive correlation was found with the BIS-11 (r=.31, p<.01) (Table 4).
4 Discussion
To our knowledge, this is the first study to focus on the reliability and validity of an observer rating scale for GD in Chinese mainland. The results confirm that PG-YBOCS-C is a reliable tool for assessing symptom severity in Chinese individuals with GD. This tool effectively fills the gap in the current research on GDs, providing the instrument for clinical assessment, and will help clinical staff to evaluate and develop treatment plans.
In this study, item analysis revealed that PG-YBOCS-C have good discrimination, indicating significant power in differentiating individuals with varying symptom severity. The scale showed high internal consistency with a Cronbach’s α of 0.965. Each of the 10 items demonstrated good discriminatory ability, and all item scores correlated significantly with the total score, further validating the scale’s internal consistency. Test-retest reliability over two weeks showed a coefficient of 0.722, emphasizing the scale’s stability and repeatability. The content validity index (SCVI) was 0.912, confirming expert agreement on the relevance of these items to gambling symptoms. This highlights the scale’s applicability and professionalism in the field of gambling research, supported by its robust content validity. The findings are consistent with the findings of Yokomitsu et al. (2020) in Japan.
Many researchers have proposed that impulse control disorder is a core symptom of addictive behavior, including GD. Addictive behavior is often described as compulsive (33). Given the similarities between OCD and GD (16), particularly in terms of ritual behavior and the compelling urge to gamble, as well as the correlations between OCD-like symptoms and gambling severity (34), the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) (35) has been adapted for pathological gambling (PG-YBOCS) (16). Contrary to the two-dimensional structure of Y-BOCS (obsessive thoughts and compulsions) (36), Pallanti et al. (16) identified a unidimensional structure for the PG-YBOCS. This also proves that compulsive behaviors in OCD tend to be more complex and specific, often disconnected from direct impulses (37). Our findings align with this unidimensional model, indicating that addictive behavior is intrinsically linked to the urge itself, making the two inseparable (e.g. gambling behavior may intensify corresponding urges, creating a vicious cycle) (38).
To examine the effectiveness of PG-YBOCS-C in assessing the severity of GD, the G-SAS was employed, a tool that has been proven reliable and effective in measuring symptom severity and monitoring treatment progress (28). The significant positive correlations between PG-YBOCS-C and G-SAS indicated that PG-YBOCS-C is an effective measure of GD severity, as further evidenced by its significant positive correlation with a single-item GES scale measuring gambling eagerness. Furthermore, consistent with previous findings, the significant positive correlations between PG-YBOCS-C and BIS-11 suggested that higher impulsivity levels are associated with more severe GDs (25). The significant negative correlation between PG-YBOCS-C and SCS (39) suggested that individuals with low self-control are less able to inhibit impulses for immediate gratification, making them more susceptible to engaging in risky behaviors, including GDs.
This study highlighted the practicality and effectiveness of the PG-YBOCS-C in the Chinese cultural context, providing a reliable observer rating tool for assessing GD symptoms in Chinese clinical practice. It addressed the need for gambling assessment tools to be adapted to the unique social and cultural landscape (7). As a clinician-administered tool, it reduces the tendency to underreport gambling behaviors due to shame or bias, thereby enhancing the accuracy and reliability of assessments. Owing to its concise and structured format, the PG-YBOCS-C is well-suited for application in clinical triage, risk screening, and symptom monitoring. It can also be combined with other tools to provide a more comprehensive assessment (such as self-report scales).
Although this study validated PG-YBOCS-C as an effective clinical tool, there were some limitations of the study. First, despite efforts to recruit a broad participant base, the sample size remained relatively small, potentially limiting the generalizability of the results. Given the limited sample size, this study only conducted EFA to examine the structural validity of the scale. While the EFA results suggested a strong unidimensional structure explaining 72.8% of the total variance, the use of EFA alone may carry certain limitations, such as potential overfitting and reduced generalizability of the factor structure. Additionally, the sample consisted exclusively of men, which may lead to gender biases. Furthermore, as the sample was drawn solely from mainland China, the applicability of the findings to other regions, such as Hong Kong and Macau, may be constrained due to differing sociopolitical contexts. Even so, the results of this study still provided a favorable tool for clinical research in the area of GD in the Chinese Mainland. To enhance the diversity and representativeness of the findings, future studies should include more diverse samples from various regions.
5 Conclusion
In conclusion, the results of the present study indicate that the PG-YBOCS-C is a reliable and valid measure for assessing the severity of GD in the Chinese mainland. Our findings validate that the scale is a reliable observer rating tool for assessing the severity of gambling symptoms in these individuals.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study protocol was approved by the Ethics Committee of the Shanghai Mental Health Center in China (Approval No. 2022-18), and written informed consent was obtained from the participants to participate in this study.
Author contributions
DF: Writing – original draft, Conceptualization, Formal Analysis. XZ: Data curation, Formal Analysis, Investigation, Writing – original draft. SS: Data curation, Formal Analysis, Writing – review & editing. JL: Data curation, Writing – review & editing. YW: Writing – review & editing. GS: Methodology, Writing – review & editing. YiZ: Data curation, Writing – review & editing. YuZ: Data curation, Writing – review & editing. JS: Data curation, Writing – review & editing. XC: Data curation, Writing – review & editing. GZ: Conceptualization, Methodology, Writing – review & editing. JD: Conceptualization, Funding acquisition, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Funding for this study was supported by the National Key R&D Program of China (2023YFC3304204, 2019HY320001); National Nature Science Foundation (82130041, 82171484, 81871045); Shanghai Jiao Tong University Medical Engineering Cross Research (YG2023ZD25).
Acknowledgments
We express our deepest gratitude to all the contributors who made this article possible. Special thanks to Mr. Guoqi Si for their help in data collection.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM-5. Washington, DC: American Psychiatric Association (2013).
2. Abbott MW. The changing epidemiology of gambling disorder and gambling-related harm: public health implications. Public Health. (2020) 184:41–5. doi: 10.1016/j.puhe.2020.04.003
3. Ukhova D, Marionneau V, Nikkinen J, and Wardle H. Public health approaches to gambling: a global review of legislative trends. Lancet Public Health. (2024) 9:e57–67. doi: 10.1016/s2468-2667(23)00221-9
4. News U. Illegal bets add up to 1.7 trillion dollars each year: new UN report (2021). Available online at: https://news.un.org/en/story/2021/12/1107472 (Accessed October 15, 2023).
5. Gainsbury SM. Online gambling addiction: the relationship between internet gambling and disordered gambling. Curr Addict Rep. (2015) 2:185–93. doi: 10.1007/s40429-015-0057-8
6. Tabri N, Xuereb S, Cringle N, and Clark L. Associations between financial gambling motives, gambling frequency and level of problem gambling: a meta-analytic review. Addiction. (2022) 117:559–69. doi: 10.1111/add.15642
7. Zhong G, Du J, and Zhao M. Understanding and addressing the challenges of online gambling addiction in mainland China. Gen Psychiatr. (2024) 37:e101477. doi: 10.1136/gpsych-2023-101477
8. Wu AM and Lau JT. Gambling in China: socio-historical evolution and current challenges. Addiction. (2015) 110:210–6. doi: 10.1111/add.12710
9. Loo JM, Raylu N, and Oei TP. Gambling among the Chinese: a comprehensive review. Clin Psychol Rev. (2008) 28:1152–66. doi: 10.1016/j.cpr.2008.04.001
10. Raylu N and Oei TP. Role of culture in gambling and problem gambling. Clin Psychol Rev. (2004) 23:1087–114. doi: 10.1016/j.cpr.2003.09.005
11. Slutske WS. Natural recovery and treatment-seeking in pathological gambling: results of two U.S. national surveys. Am J Psychiatry. (2006) 163:297–302. doi: 10.1176/appi.ajp.163.2.297
12. Lesieur HR and Blume SB. The South Oaks Gambling Screen (SOGS): a new instrument for the identification of pathological gamblers. Am J Psychiatry. (1987) 144:1184–8. doi: 10.1176/ajp.144.9.1184
13. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Bmj. (2011) 343:d5928. doi: 10.1136/bmj.d5928
14. Luquiens A, Miranda R, Benyamina A, Carré A, and Aubin HJ. Cognitive training: A new avenue in gambling disorder management? Neurosci Biobehav Rev. (2019) 106:227–33. doi: 10.1016/j.neubiorev.2018.10.011
15. Cuijpers P, Li J, Hofmann SG, and Andersson G. Self-reported versus clinician-rated symptoms of depression as outcome measures in psychotherapy research on depression: a meta-analysis. Clin Psychol Rev. (2010) 30:768–78. doi: 10.1016/j.cpr.2010.06.001
16. Pallanti S, DeCaria CM, Grant JE, Urpe M, and Hollander E. Reliability and validity of the pathological gambling adaptation of the Yale-Brown Obsessive-Compulsive Scale (PG-YBOCS). J Gambl Stud. (2005) 21:431–43. doi: 10.1007/s10899-005-5557-3
17. Blanco C, Potenza MN, Kim SW, Ibáñez A, Zaninelli R, Saiz-Ruiz J, et al. A pilot study of impulsivity and compulsivity in pathological gambling. Psychiatry Res. (2009) 167:161–8. doi: 10.1016/j.psychres.2008.04.023
18. Bodor D, Ricijaš N, and Filipčić I. Treatment of gambling disorder: review of evidence-based aspects for best practice. Curr Opin Psychiatry. (2021) 34:508–13. doi: 10.1097/yco.0000000000000728
19. Grant JE, Odlaug BL, and Chamberlain SR. Gambling disorder, DSM-5 criteria and symptom severity. Compr Psychiatry. (2017) 75:1–5. doi: 10.1016/j.comppsych.2017.02.006
20. Kovanen L, Basnet S, Castrén S, Pankakoski M, Saarikoski ST, Partonen T, et al. A randomised, double-blind, placebo-controlled trial of as-needed naltrexone in the treatment of pathological gambling. Eur Addict Res. (2016) 22:70–9. doi: 10.1159/000435876
21. Okamoto Y, Katsumata Y, Baba S, Kawaguchi Y, and Harigai M. Validation of the Japanese version of the Lupus Damage Index Questionnaire in a large observational cohort: A two-year prospective study. Modern rheumatology. (2021) 31(4):834–842. doi: 10.1080/14397595.2020.1829341
22. Loo JM, Oei TP, and Raylu N. Psychometric evaluation of the Problem Gambling Severity Index-Chinese version (PGSI-C). J Gambl Stud. (2011) 27:453–66. doi: 10.1007/s10899-010-9221-1
23. Yu-ping YANG, D.-x. W, and Han-gui LI. Reliability and validity of chinese version of gambling urge scale. Chin J Public Health. (2012) 28:1310–2. doi: 10.11847/zgggws2012-28-10-16
24. Zhou Y, Cui Y, Shi S, Liu J, Wei Y, Zhang X, et al. Chinese south oaks gambling screen: A study on reliability and validity in mainland China. Asian J Soc Health Behav. (2025) 8:9–14. doi: 10.4103/shb.shb_250_24
25. Ioannidis K, Hook R, Wickham K, Grant JE, and Chamberlain SR. Impulsivity in Gambling Disorder and problem gambling: a meta-analysis. Neuropsychopharmacology. (2019) 44:1354–61. doi: 10.1038/s41386-019-0393-9
26. Mazhari S. Association between problematic internet use and impulse control disorders among Iranian university students. Cyberpsychology Behavior Soc Networking. (2012) 15:270–3. doi: 10.1089/cyber.2011.0548
27. Yau YH and Potenza MN. Gambling disorder and other behavioral addictions: recognition and treatment. Harv Rev Psychiatry. (2015) 23:134–46. doi: 10.1097/hrp.0000000000000051
28. Kim SW, Grant JE, Potenza MN, Blanco C, and Hollander E. The Gambling Symptom Assessment Scale (G-SAS): a reliability and validity study. Psychiatry Res. (2009) 166:76–84. doi: 10.1016/j.psychres.2007.11.008
29. Ong HSR, Chao-Xu P, Asharani. VP, and Guo S. Factor structure of the Gambling Symptom Assessment Scale among treatment-seeking adults in Singapore. Int Gambling Stud. (2016) 16:442–54. doi: 10.1080/14459795.2016.1223149
30. Heller GZ, Manuguerra M, and Chow R. How to analyze the Visual Analogue Scale: Myths, truths and clinical relevance. Scand J Pain. (2016) 13:67–75. doi: 10.1016/j.sjpain.2016.06.012
31. Li X-Y, Phillips MR, Xu D, Zhang Y-L, Yang S-J, Tong Y-S, et al. Reliability and validity of an adapted Chinese version of Barratt Impulsiveness Scale. Chin Ment Health J. (2011) 25:610–5.
32. Tan S-h and Guo Y-y. Revision of Self-Control Scale for Chinese college students. Chin J Clin Psychol. (2008) 16:468–70.
33. Heather N. Is the concept of compulsion useful in the explanation or description of addictive behaviour and experience? Addictive Behav Rep. (2017) 6:15–38. doi: 10.1016/j.abrep.2017.05.002
34. Cocker PJ and Winstanley CA. Animal Models of Gambling-Related Behaviour. In: Heinz A, Romanczuk-Seiferth N, and Potenza MN, editors. Gambling Disorder. Springer International Publishing (2019). p. 101–25. doi: 10.1007/978-3-030-03060-5_6
35. Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. (1989) 46:1006–11. doi: 10.1001/archpsyc.1989.01810110048007
36. McKay D, Danyko S, Neziroglu F, and Yaryura-Tobias JA. Factor structure of the Yale-Brown Obsessive-Compulsive Scale: a two dimensional measure. Behav Res Ther. (1995) 33:865–9. doi: 10.1016/0005-7967(95)00014-o
37. Starcevic V and Janca A. Obsessive-compulsive spectrum disorders: still in search of the concept-affirming boundaries. Curr Opin Psychiatry. (2011) 24:55–60. doi: 10.1097/YCO.0b013e32833f3b58
38. Moritz S, Bücker L, Wittekind C, Gawęda Ł, and Gehlenborg J. The dimensional structure of the Yale-Brown Obsessive-Compulsive Scale for pathological gambling: Functional differences between true compulsions and compulsive behavior. Int Gambling Stud. (2021) 21:92–102. doi: 10.1080/14459795.2020.1808045
Keywords: Yale-Brown Obsessive Compulsive Scale, gambling disorder, validity, reliability, pathological gambling
Citation: Fan D, Zhang X, Shi S, Liu J, Wei Y, Song G, Zhou Y, Zhu Y, Shi J, Cai X, Zhong G and Du J (2025) Validation of the Chinese version of the Yale-Brown Obsessive Compulsive Scale for Pathological Gambling for individuals with gambling disorder in Mainland China. Front. Psychiatry 16:1535332. doi: 10.3389/fpsyt.2025.1535332
Received: 27 November 2024; Accepted: 29 April 2025;
Published: 29 May 2025.
Edited by:
Feten Fekih-Romdhane, Tunis El Manar University, TunisiaReviewed by:
Zhou Xu Hui, Second People’s Hospital of Hunan Province, ChinaJia-jun Xu, Sichuan University, China
Yong-guang Wang, Hangzhou Seventh Peoples Hospital, China
Copyright © 2025 Fan, Zhang, Shi, Liu, Wei, Song, Zhou, Zhu, Shi, Cai, Zhong and Du. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiang Du, ZHVqaWFuZ2RvdUAxNjMuY29t; Gangliang Zhong, emhvbmdnYW5nbGlhbmdAaG90bWFpbC5jb20=
†These authors share first authorship
 Dongli Fan1,2†
Dongli Fan1,2† Siyao Shi
Siyao Shi Yicheng Wei
Yicheng Wei Jiang Du
Jiang Du