- 1Department of Psychology, Institute of Population Health, University of Liverpool, Liverpool, United Kingdom
- 2Department of Women & Children’s Health, School of Life Course & Population Sciences, King’s College London, London, United Kingdom
- 3Department of Psychological Medicine, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, London, United Kingdom
- 4Division of Methodologies, Florence Nightingale Faculty of Nursing, Midwifery & Palliative Care, King’s College London, London, United Kingdom
- 5School of Health Sciences, College of Medicine and Health, Bangor University, Bangor, United Kingdom
- 6Division of Psychology and Mental Health, School of Health Sciences, The University of Manchester, Manchester, United Kingdom
- 7PETALS: The Baby Loss Counselling Charity, Cambridge, United Kingdom
- 8Patient and Participant Involvement and Engagement Group for Perinatal Bereavement, Trauma, and Loss, King’s College London, London, United Kingdom
- 9Fetal Medicine Unit, Liverpool Women’s NHS Foundation Trust, Liverpool, United Kingdom
- 10Fetal Medicine Unit, St. George’s University Hospitals NHS Foundation Trust, University of London, London, United Kingdom
Introduction: Nearly three quarters of stillbirths and neonatal deaths occur in infants born prematurely. The mothers of these children may be at increased risk of developing mental health difficulties as a result of their premature labour and/or subsequent loss.
Methods: This systematic review was conducted to understand the psychological experiences of mothers who gave birth prematurely to a baby who subsequently dies as a result of an intrapartum stillbirth or a neonatal death. Ten databases were searched. Any studies which included women who had suffered a perinatal bereavement as a result of preterm labour and birth, in any country, and in any language were eligible to be included. Studies focusing on antepartum stillbirth or in utero death were excluded due to not having the element of preterm labour and/or birth within the studies. Risk of bias was to be assessed using the Critical Appraisal Skills Programme.
Results: Following the screening of citations, no studies were eligible for inclusion in the review. The majority of studies were excluded due to a lack of distinction in terms of intrapartum or antepartum stillbirth, or grouping of types of perinatal loss. Had the inclusion criteria been less stringent and the three most common reasons for exclusion been removed, 19 studies would have been eligible for inclusion in the review, and we present a brief summary of these findings.
Discussion: These review findings highlight the need for more research into the psychological experiences of mothers of preterm infants whose baby subsequently dies, whereby future studies should consider routine reporting of gestational age. To address the identified gaps, future research should consider alternative methods or broader inclusion criteria to capture relevant data. Emphasising the importance of reporting gestational age and distinguishing between types of perinatal loss will enhance the specificity of research findings.
1 Introduction
Preterm birth and perinatal bereavement continue to be neglected public health issues. Birth at <37 weeks’ gestation (‘preterm birth’) (1) is one of the leading causes of mortality worldwide in children under five (2). In the United Kingdom, prematurity is the leading cause of neonatal death (death of a live born infant within the first 28 completed days of life) (3), accounting for 73% of all infant mortality in 2021 (4). Although rates have been declining, predominantly due to increased medical advances in neonatal care, the downward trajectory is not stable, showing recent rises once again in 2021 (4).
The birth of a preterm baby can be psychologically traumatic for mothers. There is a well-documented increased risk of developing depression (5), anxiety (6, 7), and post-traumatic stress disorder (8), amongst mothers of premature infants, compared with those who deliver at term. Mental distress may be exacerbated further in women who give birth to extremely premature infants (e.g., <28 weeks’ gestation), due to increased health concerns associated with earlier gestational age (9). Mothers of premature infants commonly experience thanatophobic (extreme fear of death or the dying process) anxieties (10). Furthermore, the unexpectedness of the birth often renders mothers feeling unprepared for parenthood (11), whilst they face financial burdens and social isolation associated with the baby’s prematurity, which can persist well after birth (12). Intangible costs resulting from stillbirth such as grief and anxiety, as well as those more tangible such as financial difficulties, can be severe and long-lasting (13). These experiences may be exacerbated amongst those women whose infants require extended periods of time in neonatal care (7).
Prematurity remains the leading cause of stillbirth and neonatal death. Recent estimates suggest ≈75% of stillbirths and ≈73% of neonatal deaths occur in babies born prematurely (4); yet despite high prevalence rates, the psychological consequences of perinatal bereavement remain under-explored and under-reported (12). When the infant has a prolonged stay in hospital and their death is expected, mothers may experience feelings of fear and anticipatory grief (14). These psycho-emotional responses can often be difficult to communicate, because women simultaneously grieve the loss of their ‘normal’ pregnancy, alongside fearing for their infant’s life, and/or grieving following the death of their baby (13).
Despite the severe and long-lasting psychological consequences of both preterm birth and perinatal bereavement, there is no synthesis of the evidence outlining the psychological consequences for mothers who labour prematurely and whose preterm infant subsequently dies. Given that a review in this area had never been conducted, we kept the aim broad in scope. Thus, the current review aimed to understand the psychological experiences of women who went into preterm labour whose babies subsequently died due to an intrapartum stillbirth or a neonatal death, through a systematic review of both qualitative and quantitative literature.
2 Methods
2.1 Registration
This systematic review was registered with PROSPERO in April 2024 (CRD42024516271) (15), and is reported according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses [PRISMA] 2020 guidelines (16) (see Figure 1).
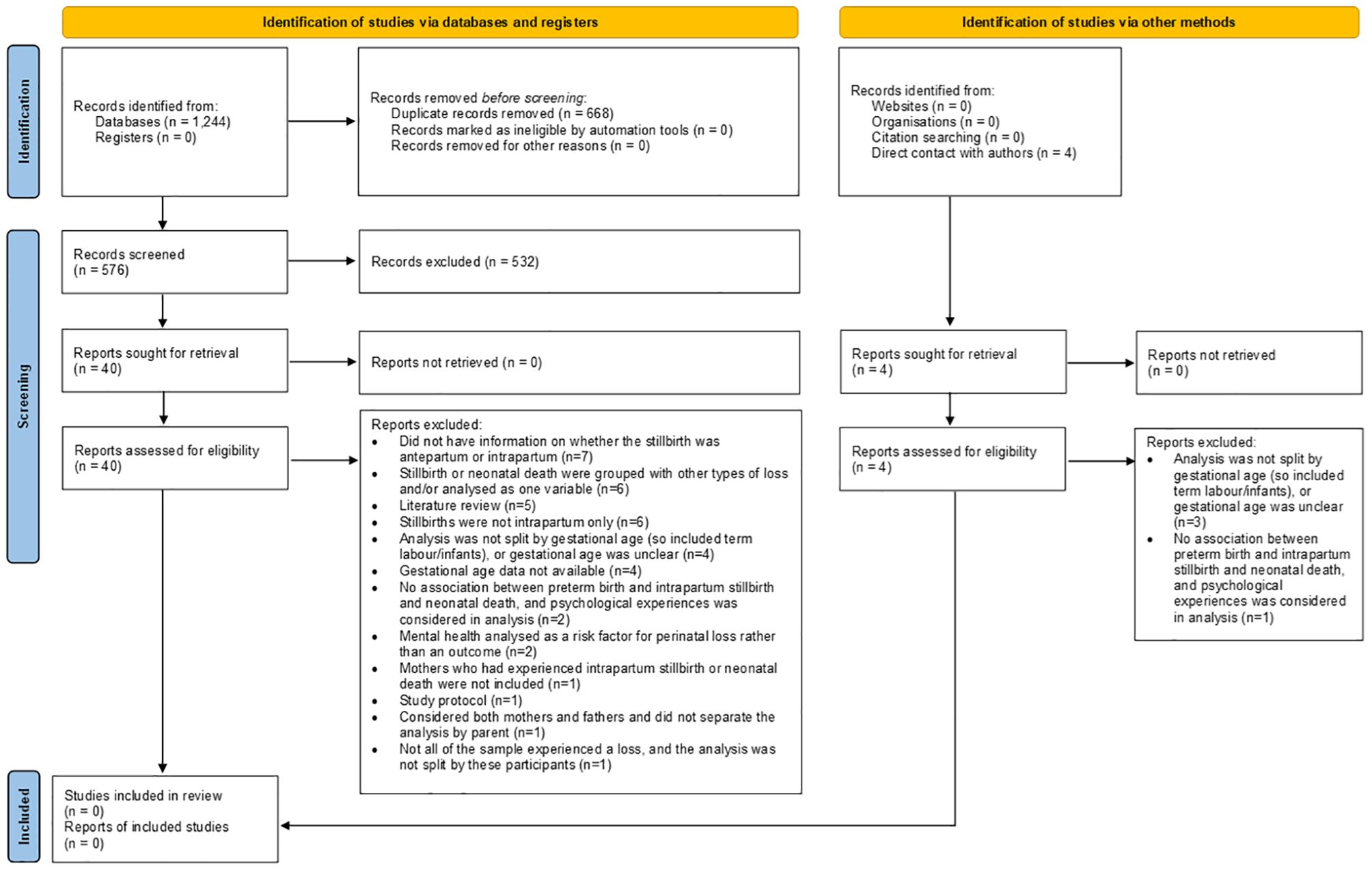
Figure 1. PRISMA 2020 flow diagram for new systematic reviews which included searches of databases, registers and other sources.
2.2 Patient and public involvement and engagement
The protocol for this systematic review was outlined and discussed at the Patient and Participant Involvement and Engagement [PPIE] Group for Perinatal Bereavement, Trauma, and Loss at King’s College London (18 March 2024). This group comprises experts by experience, members of third sector and charitable organisations, academics, researchers, clinicians, and policy makers. Through this engagement we sought and received feedback on the aim of the review from both lay and expert stakeholders, including members of the public, those with lived experience, health and social care professionals, researchers, and policy makers. They fully supported the rationale for the review and suggested we should augment the aim to also include stillbirth, as well as the originally intended inclusion of neonatal death in the review. These changes were incorporated before the PROSPERO registration.
2.3 Eligibility criteria
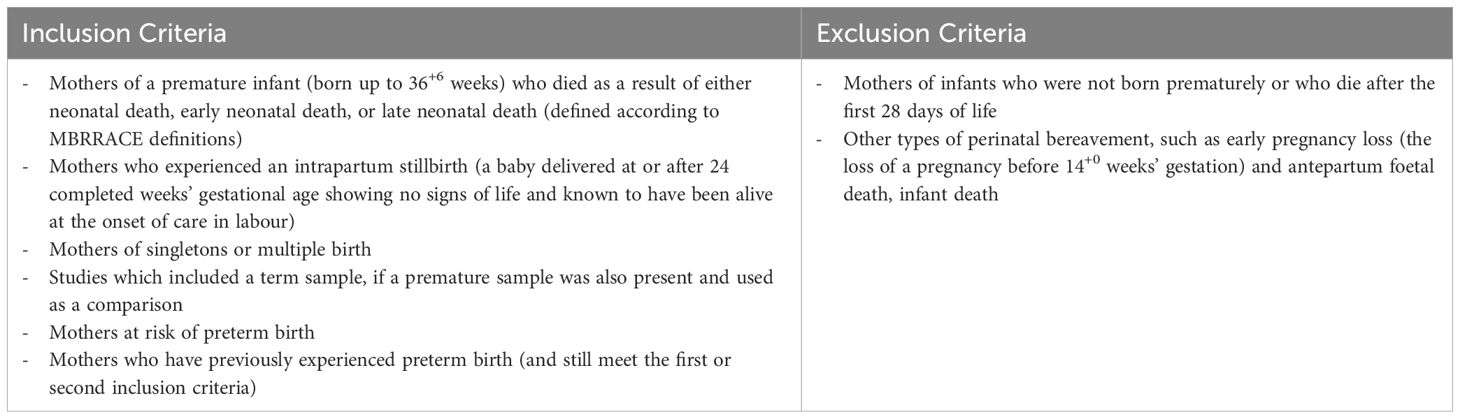
Studies were to be included if they reported a sample of women who laboured prematurely (up to 36+6 weeks’ gestation) and whose baby had subsequently died as a result of either an intrapartum stillbirth (a baby delivered at or after 24 completed weeks’ gestational age showing no signs of life and known to have been alive at the onset of care in labour) or a neonatal death (including early and late neonatal death) according to Mothers and Babies: Reducing Risk through Audits and Confidential Enquiries across the UK [MBRRACE] definitions (4). We also aimed to include studies of mothers at risk of preterm birth or those who had previously experienced preterm birth. Other types of perinatal bereavement, such as early pregnancy loss, in utero death, antepartum stillbirth, or infant death, were ineligible as perinatal bereavement experiences are known to be different (17), and the focus of this review was perinatal bereavement as a result of a preterm labour and birth. No studies were excluded on the basis of design or language. Reviews (be they critical, narrative, scoping, or systematic) were excluded, although the reference lists of relevant reviews were hand-searched for any missed references. For a full list of inclusion and exclusion criteria, please see the published protocol (15) or Table 1.
2.4 Information sources
Searches included both peer-reviewed literature as well as grey literature and theses/dissertations. All databases (British Library EThOS; Cochrane Library; CINAHL; MEDLINE (Ovid); OPENGREY; ProQuest; PsycArticles; PsycINFO; PubMed; Scopus) were searched from inception to 5 April 2024, and included psychological, medical, and clinical databases (initially we also had intended to search on Embase, however Scopus includes all articles covered by Embase, rendering a separate search unnecessary) (15). The initial search strategy published on PROSPERO was expanded because the initial strategy was deemed too narrow after searches were conducted; the expanded strategy was added as a revision to the initial protocol (15) and can also be found in Supplementary Table 1.
2.5 Selection process
Searches were conducted by one author [SW] and exported to Rayaan (18), a commonly used web-tool to assist with the screening of articles against inclusion and exclusion criteria. All results were screened by title, abstract, and full text by two authors [SW, OP]. Any conflicts which could not be resolved between the screening authors were referred to a third author [SAS].
2.6 Data collection process and data items
Full data extraction for all reports was conducted via a pre-prepared Microsoft Excel spreadsheet, containing sub-headings to extract information. For the sub-headings, please see the published protocol (15).
2.7 Synthesis methods
Quantitative studies were to be synthesised using a convergent integrated approach (19), whereby data would be transformed into a compatible format to be analysed. The attribution of codes and/or themes to quantitative data is less likely to produce errors compared to assigning numerical values to qualitative data (i.e., ‘qualitizing’ the quantitative) (20). Studies were then to be synthesised and presented using narrative synthesis (21).
Qualitative studies were also to be synthesised and presented using narrative synthesis (21). An inductive multi-stage approach was to be used to collate narrative findings of each study, once exported to NVivo15. Results would be coded according to their meaning and content. Descriptive themes would be developed, and a hierarchical structure was to be built, by considering similarities and differences between codes, with the aim of developing analytical themes in a consultative and iterative way.
2.8 Reporting bias assessment
All eligible studies were to be independently assessed using the Critical Appraisal Skills Programme [CASP] Tool (22). CASP includes various checklists for a range of study designs, including quantitative, qualitative and case control studies. Reports and articles are rated on a ‘yes’, ‘no’, and ‘can’t tell’ system, with the ability to add further comments. No studies would be excluded based on a low rating. Bias assessment was to be used to aid data synthesis and interpretation and weighting of results.
3 Results
3.1 Screening
In total, 1,244 citations were extracted from the databases (see Figure 1). Suspected duplicates were identified automatically in Rayaan and verified by one author [SW]. Of the 576 articles reviewed at title and abstract stage, only 44 articles were reviewed as full text. Of these, seventeen were longitudinal studies (23–39), five were qualitative studies (40–44), twelve were cross-sectional or case control studies (45–56), five were literature reviews (57–61) and one was a study protocol (62). When contacting for further clarification, the author of the study protocol identified four further articles (63–66) that were published following the protocol which were reviewed at full-text stage, that used data from a cohort study.
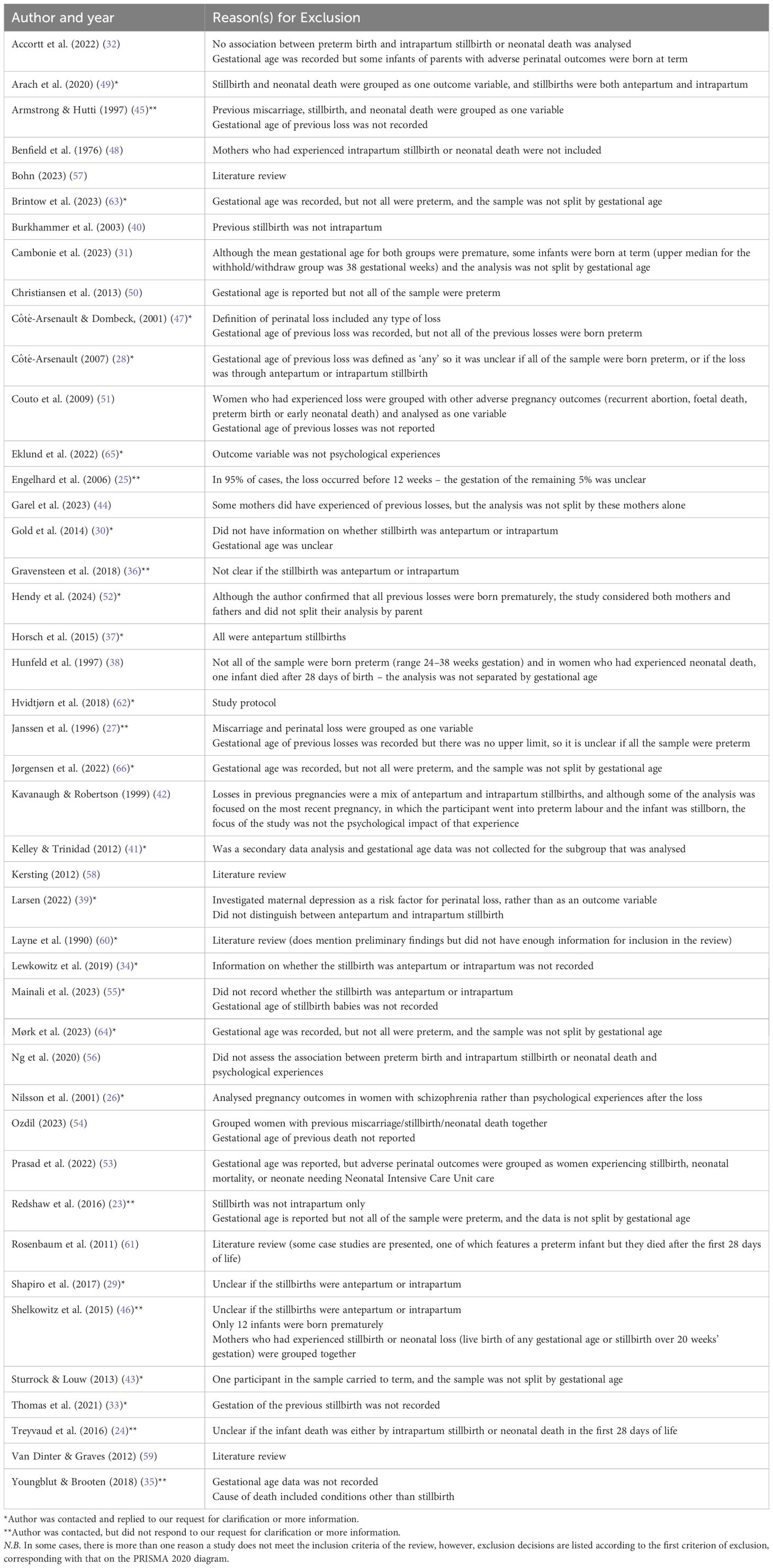
No studies were eligible for inclusion in the review, rendering it an empty review. When there was a lack of clarity in the published article and so a decision on eligibility could not be made with certainty, one author [SW] contacted the authors of the original paper to provide further information. Initially, contact was made via e-mail if available, which was done throughout August and September 2024. Each author was contacted at least three times. When e-mail addresses were unavailable, other methods of contact were attempted, including via ResearchGate, and other members of the authorship team, or wider research teams, if their e-mails were also available. No study was excluded solely on the basis of the author not responding to our contact; in most cases it was that no information on type of stillbirth or gestational age was recorded, which they informed us via e-mail. One article was translated from German to English (58). The most common reasons for exclusion included: no information on whether the stillbirth was intrapartum or antepartum (n=7) (24, 28–30, 34, 46, 55), stillbirth or neonatal death were grouped with other types of loss and/or analysed as one variable (n=6) (27, 45, 47, 51, 53, 54,) stillbirths were not intrapartum only (n=6) (23, 36, 37, 40, 42, 49). For a full list of all studies and the reason for exclusion, see Table 2.
3.2 Reconciling the ‘empty’ systematic review
Despite no studies being eligible for inclusion in the review, they can still provide useful information. As it was not possible to answer the original research questions, in a deviation from the protocol, we applied less stringent criteria and extracted data from 19 of the above studies (23, 24, 27–30, 34, 36, 37, 40, 42, 45–47, 49, 51, 53–55), based on the most common reasons for exclusion: no information regarding stillbirth being intrapartum or antepartum (n=7), stillbirth or neonatal death were grouped with other types of loss and/or analysed as one variable (n=6), stillbirths were not intrapartum only (n=6); in order to provide information on psychological outcomes following perinatal bereavement. Where reported, studies were predominantly conducted in the USA (24, 28), and UK (23, 37), with the exact locations of other studies not being reported.
When combined, these studies indicated that the psychological impacts of perinatal loss could be pronounced up to 18 months after the loss, but inconsistent control for confounders and heterogeneity in timing of measure might limit the interpretation. The methodological quality of the studies was generally high, although more consistent reporting of gestational age in particular is needed for future studies. For full data extraction and critical appraisal of these studies, please see Supplementary Tables 2-6.
One study (24) investigated women with multiple birth whose children had died between two and seven years after birth. However, it was not included because there was no information on whether the stillbirth was intrapartum or antepartum. Nevertheless, the authors (24) demonstrated maternal mental health was similar in both mothers of multiples compared to singletons, but those who had experienced bereavement were 3.6 times more likely to have anxiety and depressive symptoms when their surviving child was seven years old. Similarly, another study (52) was excluded because both mothers and fathers were included in the analysis, and it was not split by parent. Nevertheless, it demonstrated parents who previously suffered a neonatal death and who had an infant in the Neonatal Intensive Care Unit [NICU] had significantly higher stress levels compared to those who had not suffered one (OR=3.21, 95%CI 0.96 to 10.73, p=.0470), although the sample size is small and the wide confidence intervals limit the interpretation of the findings.
Although excluded because all stillbirths were antepartum, one study (37) considering stillbirth also showed levels of PTSD were highest in the three months following a stillbirth. Furthermore, although excluded as the type of stillbirth was unclear, another study (34) highlighted within one year of stillbirth at >23 weeks’ gestation, women were nearly 2.5 times more likely to be re-admitted to hospital due to psychiatric morbidity (OR=2.47, 95%CI 2.20 to 2.77). Alongside this, the risks for postpartum psychiatric illness were highest within four months of suffering a stillbirth (aHR=3.26, 95%CI 2.63-4.04) (34). Similarly, despite being excluded in part because stillbirths were both antepartum and intrapartum, one study (49) found that over half (62.3%) of women who had experienced a perinatal death were classified as having probable depression based on an Edinburgh Postnatal Depression Scale [EPDS] cut-off of >14. Although excluded because there was no information on the type of stillbirth or gestational age, another study (30), found that in the adjusted analysis bereaved mothers had more than twice the odds for GAD (OR=2.39, CI(1.10-5.18), p=.28) and social phobia (OR=2.32, CI=1.52-3.54), p<.0005, but not panic disorder (p=.214) or OCD (p=.112). Further, despite the type of stillbirth being unclear, it has been found that following a previous stillbirth women in their current pregnancy were more likely to have anxiety compared with the previous live birth group (aOR=5.47, 95%CI= 2.90-10.32, p<.001) and the previously nulliparous group (aOR=4.97, 95%CI 2.68-9.24, p<.001) after adjusting for demographic factors (36). Additionally, they were significantly more depressed (aOR=1.91, 95%CI= 1.11-3.27, p=.019) than the previous live birth and the nulliparous group (aOR=1.91, 95%CI=1.11-3.36, p=.026) after adjusting for demographic factors (36). Finally, despite being excluded because the type of stillbirth was unclear, one study (29) found that after adjusting for all variables, prior stillbirth was not significantly associated with pregnancy anxiety in the first (β=0.30, 95%CI=0.10-0.70), p=.13), or second (β=0.24, 95%CI=0.08-0.57, p=.14) trimester, but was in the third trimester (β=0.40, 95%CI-0.05-0.74, p=.025).
4 Discussion
4.1 Main findings
The aim of this systematic review was to understand the psychological experiences of mothers who begin labour prematurely and whose babies subsequently died. Inclusion criteria aimed to identify women who had experienced intrapartum stillbirth or neonatal death with a preterm baby. No studies met criteria for inclusion in the review. Whilst frustrating to have a systematic review rendered empty, this demonstrates two needs from the field of research. Firstly, this empty systematic review demonstrates the need to accurately document data on the gestational age at which a baby was stillborn or died. Secondly, research must ensure perinatal bereavements are not grouped, but documented separately and accurately (17). Finally, this empty systematic review can be used as a call for future research conducted with women who go into labour prematurely to ensure psychometric measures of psychological health and experiential qualitative data are captured when including women who subsequently experience a perinatal bereavement.
4.2 Interpretation of findings
It is well established that women who experience stillbirth, regardless of gestational age, are more likely to experience poor mental health for a prolonged period after the death (67). However, the results of the review highlight that women who go into preterm labour with a baby who dies during active labour (i.e., intrapartum stillbirth) are an under researched group. Seven studies were excluded from the review because there was no information on whether the stillbirth was intrapartum or antepartum (24, 28–30, 34, 46, 55), and six studies were excluded because stillbirth or neonatal death were grouped with other types of loss and/or analysed as one variable (27, 45, 47, 51, 53, 54). This is surprising given preterm delivery has been identified as an independent risk factor for intrapartum foetal death (68). Grouping stillbirth and neonatal death with other types of loss, such as earlier pregnancy losses, is problematic in the context of preterm birth as women may experience these differently (69). Other types of in utero death, such as pregnancy losses of all kinds and antepartum stillbirths, present distinctly different lived experiences, as no labour and birth to a live infant is part of the pregnancy and birthing journey. Furthermore, stillbirth has been associated with feelings of ‘failure’ and guilt surrounding the self (70) whereas neonatal death has also been associated with increased anxiety surrounding the fragility of the infant, which is already well established in the context of preterm birth (71). Although in some cases this was the aim of the studies, it is important in future studies to further distinguish between stillbirth and other types of loss in the first instance, but also between antepartum and intrapartum stillbirth, particularly as the two can have differing incidence and causes (72), so psychological outcomes may vary. A recent study (73) examining stillbirth using gestational age in a sample of over 125 million births indicated approximately 74% of stillbirths were preterm, but also called for greater granularity in assessing risk, including by gestational age categories and labour types to provide greater understanding.
Four studies (25, 31, 38, 50) were excluded from the review because the analysis was not split by gestational age or the gestational age was unclear. Another four studies (33, 35, 41, 43) were excluded because gestational age data were not available. The disparity in reporting of gestational age, both in the case of stillbirth and neonatal death means that, despite the increased risk of perinatal loss associated with preterm birth, this group is underrepresented, and in some cases completely missed, in current research. It is already well known that the birth of a preterm baby can lead to an increased likelihood of developing maternal mental health difficulties, and can lead to feelings of detachment towards the infant, anxiety surrounding their health, and fear surrounding their survival (74). Coping with these emotions whilst dealing with the increased likelihood of the loss of an infant, or the ambiguity surrounding potential end-of-life decisions, alongside complex medical difficulties may lead to difficulties expressing these emotions (75). Studies have found that parents who feel more involved in their infant’s care whilst in the NICU may help families to navigate their grief (76). Although the majority of admissions to the NICU are for term infants (77), mothers of premature infants are a particularly important group to consider because their experiences may be further compounded by the unexpectedness, and potentially traumatic nature, of the birth (78). Future studies considering experiences of stillbirth or neonatal death should consider routine reporting of gestational age to enable greater understanding of the experiences of mothers who give birth preterm to a baby who then subsequently dies.
4.3 Strengths, limitations, and future directions
This comprehensive systematic review searched a range of clinical, psychological, and medical databases, with all screening decisions assessed independently by two reviewers, ensuring robustness. Despite potential criticisms that empty systematic reviews result from overly niche topics, we expanded the initial search strategy following patient and public involvement and engagement consultation, as well as preliminary searches, to broaden the focus.
An empty systematic review, whilst initially appearing unproductive, holds substantial significance in the scientific community by highlighting critical gaps in the existing literature (79, 80). Rather than merely indicating a lack of data, it highlights areas where evidence is lacking, guiding researchers to design studies that address these deficiencies and informing funding agencies about the importance of investing in under-researched topics. Empty reviews influence various stakeholders by encouraging researchers to conduct studies addressing the identified gaps, thus preventing duplication of effort and fostering a cumulative knowledge-base (80). For clinicians, awareness of the lack of evidence informs practice, highlighting the need for caution or alternative approaches when evidence is insufficient (79). Policymakers can identify areas where guidelines may need development or revision, ensuring that policies are based on comprehensive and current evidence.
Additionally, conducting research with vulnerable populations, such as women who have experienced preterm labour resulting in intrapartum stillbirth or neonatal death, presents ethical challenges (81, 82). Emotional distress, fear of re-living trauma, and protective gatekeeping can hinder participant recruitment. To overcome these barriers, researchers should emphasise beneficence by ensuring that the research is designed to provide potential benefits to participants or contribute valuable knowledge (81). In practice, this could be done by implementing sensitive consent processes which use compassionate communication strategies as respecting the emotional state of participants is crucial (82). Engaging with support groups and patient advocates, as demonstrated in the process of conducting this review, can build trust and facilitate recruitment by collaborating with organisations that support bereaved mothers. It has been recently identified that whilst mothers who have experienced a loss are generally very keen to take part in research, a key barrier is not understanding how they can take part or if their reasons for taking part will be appreciated (83). As such, similar to other studies, researchers could consider developing guides for taking part in research surrounding perinatal loss, to encourage participation and open up dialogue between researchers and participants (83).
To address the identified gaps, future research should consider alternative methods or broader inclusion criteria to capture relevant data. Expanding criteria to include various gestational ages or related experiences is also necessary to gather more comprehensive data. Emphasising the importance of reporting gestational age and distinguishing between types of perinatal loss will enhance the specificity of research findings. By addressing these limitations and implementing alternative approaches, future research can effectively fill the gaps identified by this empty review, ultimately contributing to better support and interventions for bereaved mothers.
5 Conclusion
This systematic review aimed to understand the psychological experience of mothers who gave birth prematurely to a baby who subsequently died. Whilst preterm birth only occurs in approximately 10% of cases, it is the leading cause of neonatal death in the UK. No studies were eligible for inclusion in the review. Reasons for exclusion included lack of clarity or distinction between antepartum and intrapartum stillbirth, or disparity in reporting of gestational age. Therefore, this review highlights the lack of research and understanding surrounding experiences of mothers who experience the loss of a premature baby and emphasises the need for greater research and reporting of gestational age in this context.
6 Definitions
Gestational Age: The number of weeks of age of the foetus or newborn infant, based on the time from the mother’s last menstrual period until the present date. Perinatal Period: The time between conception and up until the end of the first postpartum year. Perinatal Bereavement: Any form of pregnancy loss or perinatal death (including stillbirth and neonatal death). Thanatophobia: Extreme fear of death or the dying process. Preterm Birth: Birth at less than 37 weeks’ gestation. Extremely Preterm: Birth at less than 28 weeks’ gestation. Very Preterm: Birth at 28 to less than 32 weeks’ gestation. Moderate to Late Preterm: Birth at 32 to 37 weeks’ gestation. Stillbirth: A baby delivered at or after 24 completed weeks’ gestational age showing no signs of life, irrespective of when the death occurred. Antepartum Stillbirth: A baby delivered at or after 24 completed weeks’ gestational age showing no signs of life and known to have died before the onset of care in labour. Intrapartum Stillbirth: A baby delivered at or after 24 completed weeks’ gestational age showing no signs of life and known to have been alive at the onset of care in labour. Neonatal Death: A liveborn baby (born at 20 completed weeks’ gestational age or later, or with a birthweight of 400g or more where an accurate estimate of gestation is not available), who died before 28 completed days after birth. Early Neonatal Death: A liveborn baby (born at 20 completed weeks’ gestational age or later, or with a birthweight of 400g or more where an accurate estimate of gestation is not available) who died before 7 completed days after birth. Late Neonatal Death: A liveborn baby (born at 20 completed weeks’ gestational age or later, or with a birthweight of 400g or more where an accurate estimate of gestation is not available) who died after 7 completed days but before 28 completed days after birth.
Author contributions
SW: Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Visualization, Writing – original draft, Conceptualization, Funding acquisition. EP: Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. REF: Formal analysis, Validation, Writing – original draft. OP: Formal analysis, Investigation, Methodology, Software, Writing – review & editing. NHC: Conceptualization, Validation, Writing – review & editing. JC: Conceptualization, Validation, Writing – review & editing. AW: Conceptualization, Data curation, Methodology, Validation, Writing – review & editing. KB: Conceptualization, Validation, Writing – review & editing. CS: Conceptualization, Validation, Writing – review & editing. LAM: Conceptualization, Methodology, Validation, Writing – review & editing. PvD: Conceptualization, Methodology, Validation, Writing – review & editing. PC: Conceptualization, Data curation, Methodology, Project administration, Resources, Supervision, Validation, Writing – review & editing. VF: Conceptualization, Project administration, Resources, Supervision, Validation, Writing – review & editing. AK: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Resources, Supervision, Validation, Writing – review & editing. SAS: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Funding acquisition, Software, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We would like to acknowledge the support and input of the Patient and Public Involvement and Engagement Group for Perinatal Bereavement, Trauma, & Loss at King’s College London and the ongoing support and input of PETALS: The Baby Loss Counselling Charity. We would like to acknowledge that since completion of our empty systematic review, the Critical Appraisal Skills Programme (CASP) has subsequently published a Cross-Sectional Study Checklist. Whilst it may have been more appropriate for some of the 19 studies to have been assessed using this checklist, this would not have affected the quality appraisal and nor would it have rendered the review not empty.
Conflict of interest
SAS is one of the Topic Editors, and EP and REF are the Topic Coordinators of the Frontiers in Psychiatry Research Topic on ‘Perinatal Bereavement, Trauma, & Loss’ to which this article was submitted and accepted.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1544485/full#supplementary-material
Abbreviations
CASP, Critical Appraisal Skills Programme; EPDS, Edinburgh Postnatal Depression Scale; MBRRACE, Mothers and Babies, Reducing Risk through Audits and Confidential Enquiries across the UK; NICU, Neonatal Intensive Care Unit; PPIE, Patient and Participant Involvement and Engagement; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
References
1. National Health Service. Premature labour and birth. London, United Kingdom: NHS England. Available at: https://www.nhs.uk/pregnancy/labour-and-birth/signs-of-labour/premature-labour-and-birth/ (Accessed October 31, 2024).
2. World Health Organization. Preterm birth. Geneva, Switzerland: WHO. Available at: https://www.who.int/news-room/fact-sheets/detail/preterm-birth (Accessed October 31, 2024).
3. Pathirana J, Muñoz FM, Abbing-Karahagopian V, Bhat N, Harris T, Kapoor A, et al. Neonatal death: Case definition & guidelines for data collection, analysis, and presentation of immunization safety data. Vaccine. (2016) 34:6027–37. doi: 10.1016/j.vaccine.2016.03.040
4. Draper ES, Gallimore ID, Smith LK, Matthews RJ, Fenton AC, Kurinczuk JJ, et al. MBRRACE-UK Perinatal Mortality Surveillance, UK Perinatal Deaths for Births from January to December 2021: State of the Nation Report. Leicester: The Infant Mortality and Morbidity Studies, Department of Population Health Sciences, University of Leicester (2023).
5. de Paula Eduardo JA, de Rezende MG, Menezes PR, and Del-Ben CM. Preterm birth as a risk factor for postpartum depression: A systematic review and meta-analysis. J Affect Disord. (2019) 259:392–403. doi: 10.1016/j.jad.2019.08.069
6. Bouras G, Theofanopoulou N, Mexi-Bourna P, Michopoulos I, Tassiopoulou I, Daskalaki A, et al. Preterm birth and maternal psychological health. J Health Psychol. (2013) 11):1388–96. doi: 10.1177/1359105313512353
7. Worrall S, Christiansen P, Khalil A, Silverio SA, and Fallon V. Associations between prematurity, postpartum anxiety, neonatal intensive care unit admission, and stress. Front Psychiatry. (2024) 15:1323773. doi: 10.3389/fpsyt.2024.1323773
8. Hall EO, Kronborg H, Aagaard H, and Brinchmann BS. The journey towards motherhood after a very preterm birth: mothers' experiences in hospital and after home-coming. J Neonatal Nursing. (2013) 19:109–13. doi: 10.1016/j.jnn.2012.08.002
9. Worrall S, Silverio SA, and Fallon VM. The relationship between prematurity and maternal mental health during the first postpartum year. J Neonatal Nursing. (2023) 29:511–8. doi: 10.1016/j.jnn.2022.10.002
10. Barr P. Guilt, shame and fear of death predict neonatal intensive care unit-related parental distress. J Reprod Infant Psychol. (2015) 33:402–13. doi: 10.1080/02646838.2015.1043624
11. Hamon E, Bourdin B, and Le Driant B. Parental representations after preterm birth: a narrative review. Front Psychol. (2023) 14:1114418. doi: 10.3389/fpsyg.2023.1114418
12. Heazell AE, Siassakos D, Blencowe H, Burden C, Bhutta ZA, Cacciatore J, et al. Stillbirths: economic and psychosocial consequences. Lancet. (2016) 387:604–16. doi: 10.1016/S0140-6736(15)00836-3
13. Leahy-Warren P, Coleman C, Bradley R, and Mulcahy H. The experiences of mothers with preterm infants within the first-year post discharge from NICU: social support, attachment and level of depressive symptoms. BMC Pregnancy Childbirth. (2020) 20:1–0. doi: 10.1186/s12884-020-02956-2
14. Lenington K, Dudding KM, Fazeli PL, Dick T, and Patrician P. Palliative care in the neonatal intensive care unit: an evolutionary concept analysis of uncertainty in anticipated loss. Adv Neonatal Care. (2024) 19:10–97. doi: 10.1097/ANC.0000000000001143
15. Worrall S, Pike O, Carlisle N, Carter J, Fallon V, Christiansen P, et al. PROSPERO (2024). Available online at: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=516271 (Accessed October 31, 2024).
16. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surgery. (2021) 88:105906. doi: 10.1016/j.ijsu.2021.105906
17. Silverio SA, Easter A, Storey C, Jurković D, Sandall J, and on behalf of the PUDDLES Global Collaboration. Preliminary findings on the experiences of care for parents who suffered perinatal bereavement during the COVID-19 pandemic. BMC Pregnancy Childbirth. (2021) 21:1–13. doi: 10.1186/s12884-021-04292-5
18. Rayyan. Rayyan – Intelligent Systematic Review (2022). Available online at: https://www.rayyan.ai/ (Accessed October 31, 2024).
19. Stern C, Lizarondo L, Carrier J, Godfrey C, Rieger K, Salmond S, et al. Methodological guidance for the conduct of mixed methods systematic reviews. JBI Evidence Synthesis. (2020) 18:2108–18. doi: 10.11124/JBISRIR-D-19-00169
20. Lovell H, Silverio SA, Story L, Skelton E, and Matthew J. Factors which influence ethnic minority women’s participation in maternity research: A systematic review of quantitative and qualitative studies. PLoS One. (2023) 18:e0282088. doi: 10.1371/journal.pone.0282088
21. Rodgers M, Sowden A, Petticrew M, Arai L, Roberts H, Britten N, et al. Testing methodological guidance on the conduct of narrative synthesis in systematic reviews: effectiveness of interventions to promote smoke alarm ownership and function. Evaluation. (2009) 15:49–73. doi: 10.1177/1356389008097871
22. Critical Appraisal Skills Programme. CASP checklist (2023). Available online at: https://casp-uk.net/ (Accessed October 31, 2024).
23. Redshaw M, Hennegan JM, and Henderson J. Impact of holding the baby following stillbirth on maternal mental health and well-being: findings from a national survey. BMJ Open. (2016) 6:e010996. doi: 10.1136/bmjopen-2015-010996
24. Treyvaud K, Aldana AC, Scratch SE, Ure AM, Pace CC, Doyle LW, et al. The influence of multiple birth and bereavement on maternal and family outcomes 2 and 7 years after very preterm birth. Early Hum Dev. (2016) 100:1–5. doi: 10.1016/j.earlhumdev.2016.04.005
25. Engelhard IM, Van Den Hout MA, and Schouten EG. Neuroticism and low educational level predict the risk of posttraumatic stress disorder in women after miscarriage or stillbirth. Gen Hosp Psychiatry. (2006) 28:414–7. doi: 10.1016/j.genhosppsych.2006.07.001
26. Nilsson E, Lichtenstein P, Cnattingius S, Murray RM, and Hultman CM. Women with schizophrenia: pregnancy outcome and infant death among their offspring. Schizophr Res. (2002) 58:221–9. doi: 10.1016/S0920-9964(01)00370-X
27. Janssen HJ, Cuisinier MC, Hoogduin KA, and de Graauw KP. Controlled prospective study of the mental health of women following pregnancy loss. Obstetrical Gynecological Survey. (1996) 51:512–4. doi: 10.1097/00006254-199609000-00004
28. Côté-Arsenault D. Threat appraisal, coping, and emotions across pregnancy subsequent to perinatal loss. Nurs Res. (2007) 56:108–16. doi: 10.1097/01.NNR.0000263970.08878.87
29. Shapiro GD, Séguin JR, Muckle G, Monnier P, and Fraser WD. Previous pregnancy outcomes and subsequent pregnancy anxiety in a Quebec prospective cohort. J Psychosomatic Obstetrics Gynecology. (2017) 38:121–32. doi: 10.1080/0167482X.2016.1271979
30. Gold KJ, Boggs ME, Muzik M, and Sen A. Anxiety disorders and obsessive compulsive disorder 9 months after perinatal loss. Gen Hosp Psychiatry. (2014) 36:650–4. doi: 10.1016/jgenhosppsych.2014.09.008
31. Cambonie G, Desage C, Thaller P, Lemaitre A, de Balanda KB, Combes C, et al. Context of a neonatal death affects parental perception of end-of-life care, anxiety and depression in the first year of bereavement. BMC Palliative Care. (2023) 22:58. doi: 10.1186/s12904-023-01183-8
32. Accortt E, Mirocha J, Jackman S, Coussons-Read M, Dunkel Schetter C, and Hobel C. Association between diagnosed perinatal mood and anxiety disorders and adverse perinatal outcomes. J Maternal-Fetal Neonatal Medicine. (2022) 35:9066–70. doi: 10.1080/14767058.2021.2014450
33. Thomas S, Stephens L, Mills TA, Hughes C, Kerby A, Smith DM, et al. Measures of anxiety, depression and stress in the antenatal and perinatal period following a stillbirth or neonatal death: a multicentre cohort study. BMC Pregnancy Childbirth. (2021) 21:1–9. doi: 10.1186/s12884-021-04289-0
34. Lewkowitz AK, Rosenbloom JI, Keller M, López JD, Macones GA, Olsen MA, et al. Association between stillbirth≥ 23 weeks gestation and acute psychiatric illness within 1 year of delivery. Am J Obstetrics Gynecology. (2019) 221:491–e1. doi: 10.1016/j.ajog.2019.06.027
35. Youngblut JM and Brooten D. Comparison of mothers and grandmothers physical and mental health and functioning within 6 months after child NICU/PICU death. Ital J Pediatrics. (2018) 44:1–0. doi: 10.1186/s13052-018-0531-8
36. Gravensteen IK, Jacobsen EM, Sandset PM, Helgadottir LB, Rådestad I, Sandvik L, et al. Anxiety, depression and relationship satisfaction in the pregnancy following stillbirth and after the birth of a live-born baby: a prospective study. BMC Pregnancy Childbirth. (2018) 18:1–0. doi: 10.1186/s12884-018-1666-8
37. Horsch A, Jacobs I, and McKenzie-McHarg K. Cognitive predictors and risk factors of PTSD following stillbirth: A short-term longitudinal study. J Traumatic Stress. (2015) 28:110–7. doi: 10.1002/jts.21997
38. Hunfeld JA, Wladimiroff JW, and Passchier J. The grief of late pregnancy loss. Patient Educ Counseling. (1997) 31:57–64. doi: 10.1016/S0738-3991(97)01008-2
39. Larsen AM. Perinatal Depression and Adverse Infant Outcomes among Kenyan Mother-Infant Pairs. United States – Washington: University of Washington (2022). Available at: https://www.proquest.com/dissertations-theses/perinatal-depression-adverse-infant-outcomes/docview/2717795645/se-2 (Accessed October 31, 2024).
40. Burkhammer MD, Anderson GC, and Chiu SH. Grief, anxiety, stillbirth, and perinatal problems: healing with kangaroo care. J Obstetric Gynecologic Neonatal Nursing. (2004) 33:774–82. doi: 10.1177/0884217504270594
41. Kelley MC and Trinidad SB. Silent loss and the clinical encounter: parents’ and physicians’ experiences of stillbirth–a qualitative analysis. BMC Pregnancy Childbirth. (2012) 12:1–5. doi: 10.1186/1471-2393-12-137
42. Kavanaugh K and Robertson PA. Recurrent perinatal loss: A case study. OMEGA-Journal Death Dying. (1999) 39:133–47. doi: 10.2190/X65F-ENLV-VALG-F7AG
43. Sturrock C and Louw J. Meaning-making after neonatal death: narratives of Xhosa-speaking women in South Africa. Death Stud. (2013) 37:569–88. doi: 10.1080/07481187.2012.673534
44. Garel M, Bahuaud M, and Blondel B. Consequences for the family of a very preterm birth two months after discharge. Results of the EPIPAGE qualitative study. Arch Pédiatrie. (2004) 11:1299–307. doi: 10.1016/j.arcped.2004.06.022
45. Armstrong D and Hutti M. Pregnancy after perinatal loss: the relationship between anxiety and prenatal attachment. J Obstetric Gynecologic Neonatal Nursing. (1998) 27:183–9. doi: 10.1111/j.1552-6909.1998.tb02609.x
46. Shelkowitz E, Vessella SL, O’Reilly P, Tucker R, and Lechner BE. Counseling for personal care options at neonatal end of life: a quantitative and qualitative parent survey. BMC Palliative Care. (2015) 14:1–1. doi: 10.1186/s12904-015-0063-6
47. Côté-Arsenault D and Dombeck MT. Maternal assignment of fetal personhood to a previous pregnancy loss. Health Care Women Int. (2001) 22:649–65. doi: 10.1080/07399330127171
48. Benfield DG, Leib SA, and Reuter J. Grief response of parents after referral of the critically ill newborn to a regional center. New Engl J Medicine. (1976) 294:975–8. doi: 10.1056/NEJM197604292941803
49. Arach AA, Nakasujja N, Nankabirwa V, Ndeezi G, Kiguli J, Mukunya D, et al. Perinatal death triples the prevalence of postpartum depression among women in Northern Uganda: A community-based cross-sectional study. PLoS One. (2020) 15:e0240409. doi: 10.1371/journal.pone.0240409
50. Christiansen DM, Elklit A, and Olff M. Parents bereaved by infant death: PTSD symptoms up to 18 years after the loss. Gen Hosp Psychiatry. (2013) 35:605–11. doi: 10.1016/j.genhosppsych.2013.06.006
51. Couto ER, Couto E, Vian B, Gregório Z, Nomura ML, Zaccaria R, et al. Quality of life, depression and anxiety among pregnant women with previous adverse pregnancy outcomes. Société Française de Pédiatrie. (2009) 127:185–9. doi: 10.1590/S1516-31802009000400002
52. Hendy A, El-Sayed S, Bakry S, Mohammed SM, Mohamed H, Abdelkawy A, et al. The stress levels of premature infants’ Parents and related factors in NICU. SAGE Open Nursing. (2024) 10:23779608241231172. doi: 10.1177/23779608241231172
53. Prasad M, Joshi A, and Saxena A. Comparison of EPDS scores among women with good neonatal outcomes and adverse neonatal outcomes. J Obstetrics Gynecology India. (2023) 73:552–4. doi: 10.1007/s13224-022-01650-x
54. Ozdil M. Postpartum depression among mothers of infants hospitalized in the neonatal intensive care unit during the COVID-19 pandemic. Cureus. (2023) 15:1–8. doi: 10.7759/cureus.44380
55. Mainali A, Infanti JJ, Thapa SB, Jacobsen GW, and Larose TL. Anxiety and depression in pregnant women who have experienced a previous perinatal loss: a case-cohort study from Scandinavia. BMC Pregnancy Childbirth. (2023) 23:111. doi: 10.1186/s12884-022-05318-2
56. Ng QJ, Koh KM, Tagore S, and Mathur M. Perception and feelings of antenatal women during COVID-19 pandemic: a cross-sectional survey. Ann Acad Med Singap. (2020) 49:543–52. doi: 10.47102/annals-acadmedsg.
57. Bohn JA. When words fail:“Miscarriage,” referential ambiguity, and psychological harm. J Med Philosophy: A Forum Bioethics Philosophy Med. (2023) 48:265–82. doi: 10.1093/jmp/jhad013
58. Kersting A. Peripartale Depressionen und Trauer nach Schwangerschaftsverlusten. Der Nervenarzt. (2012) 83:1434–41. doi: 10.1007/s00115-012-3663-x
59. Van Dinter MC and Graves L. Managing adverse birth outcomes: helping parents and families cope. Am Family Physician. (2012) 85:900–4.
60. Layne LL. Motherhood lost: Cultural dimensions of miscarriage. Women Health. (1990) 16:69–98. doi: 10.1300/J013v16n03_05
61. Rosenbaum JL, Smith JR, and Zollfrank R. Neonatal end-of-life spiritual support care. J Perinatal Neonatal Nursing. (2011) 25:61–9. doi: 10.1097/JPN.0b013e318209e1d2
62. Hvidtjørn D, Prinds C, Bliddal M, Henriksen TB, Cacciatore J, and O’Connor M. Life after the loss: protocol for a Danish longitudinal follow-up study unfolding life and grief after the death of a child during pregnancy from gestational week 14, during birth or in the first 4 weeks of life. BMJ Open. (2018) 8:e024278. doi: 10.1136/bmjopen-2018-024278
63. Brintow MB, Prinds C, O’Connor M, Möller S, Henriksen TB, Mørk S, et al. Continuing bonds in parents after a loss in pregnancy, or a death at or shortly after birth: A population-based study. Death Stud. (2023) 23:1–3. doi: 10.1080/07481187.2023.2297059
64. Mørk S, Hvidtjørn D, Möller S, Henriksen TB, O'Connor M, and Bonanno GA. Grief trajectories after loss in pregnancy and during the neonatal period. J Psychiatr Res. (2023) 168:293–9. doi: 10.1016/j.jpsychires.2023.10.052
65. Eklund MV, Prinds C, Mørk S, Damm M, Möller S, and Hvidtjørn D. Parents’ religious/spiritual beliefs, practices, changes and needs after pregnancy or neonatal loss—A Danish cross-sectional study. Death Stud. (2022) 46:1529–39. doi: 10.1080/07481187.2020.1821260
66. Jørgensen ML, Prinds C, Mørk S, and Hvidtjørn D. Stillbirth–transitions and rituals when birth brings death: Data from a danish national cohort seen through an anthropological lens. Scandinavian J Caring Sci. (2022) 36:100–8. doi: 10.1111/scs.12967
67. Campbell-Jackson L and Horsch A. The psychological impact of stillbirth on women: A systematic review. Illness Crisis Loss. (2014) 22:237–56. doi: 10.2190/IL.22.3.d
68. Davidesko S, Levitas E, Sheiner E, Wainstock T, and Pariente G. Critical analysis of risk factors for intrapartum fetal death. Arch Gynecology Obstetrics. (2023) 308:1239–45. doi: 10.1007/s00404-022-06811-x
69. Smith LK, Dickens J, Bender Atik R, Bevan C, Fisher J, and Hinton L. Parents’ experiences of care following the loss of a baby at the margins between miscarriage, stillbirth and neonatal death: a UK qualitative study. BJOG: Int J Obstetrics Gynaecology. (2020) 127:868–74. doi: 10.1111/1471-0528.16113
70. Gold KJ, Sen A, and Leon I. Whose fault is it anyway? Guilt, blame, and death attribution by mothers after stillbirth or infant death. Illness Crisis Loss. (2018) 26:40–57. doi: 10.1177/1054137317740800
71. Janvier A, Bourque CJ, Pearce R, Thivierge E, Duquette LA, Jaworski M, et al. Fragility and resilience: parental and family perspectives on the impacts of extreme prematurity. Arch Dis Childhood-Fetal Neonatal Edition. (2023) 108:575–80. doi: 10.1136/archdischild-2022-325011
72. Shanker O, Saini V, and Gupta M. Stillbirths: incidence, causes and surrogate markers of intrapartum and antepartum fetal deaths. Int J Innovative Res Med Sci (IJIRMS). (2020) 5. doi: 10.23958/ijirms/vol05-i08/927
73. Okwaraji YB, Suárez-Idueta L, Ohuma EO, Bradley E, Yargawa J, Pingray V, et al. Stillbirths: Contribution of preterm birth and size-for-gestational age for 125.4 million total births from nationwide records in 13 countries, 2000–2020. BJOG: Int J Obstetrics Gynaecology. (2023). doi: 10.1111/1471-0528.17653
74. Acharya S, Bhandari S, Bhattarai S, and Gaire H. Experiences of mothers having preterm infants admitted in neonatal intensive care unit: a qualitative study. J Chitwan Med College. (2021) 11:4–8. doi: 10.54530/jcmc.454
75. Baum N, Weidberg Z, Osher Y, and Kohelet D. No longer pregnant, not yet a mother: giving birth prematurely to a very-low-birth-weight baby. Qual Health Res. (2012) 22:595–606. doi: 10.1177/1049732311422899
76. Lakhani J, Mack C, Kunyk D, and van Manen M. Exploring and supporting parents’ stories of loss in the NICU: A narrative study. Qual Health Res. (2023) 33:1279–90. doi: 10.1177/10497323231201023
77. Neonatal Medicine Research Group - Neonatal Data Analysis Unit. Neonatal Data Analysis. London, United Kingdom: Imperial College London (2024). Available at: https://www.imperial.ac.uk/neonatal-data-analysis-unit/neonatal-data-analysis-unit/ (Accessed October 31, 2024).
78. Lasiuk GC, Comeau T, and Newburn-Cook C. Unexpected: an interpretive description of parental traumas’ associated with preterm birth. BMC Pregnancy Childbirth. (2013) 13:1–0. doi: 10.1186/1471-2393-13-S1-S13
79. Yaffe J, Montgomery P, Hopewell S, and Shepard LD. Empty reviews: a description and consideration of Cochrane systematic reviews with no included studies. PLoS One. (2012) 7:e36626. doi: 10.1371/journal.pone.0036626
80. Lang AT, Edwards N, and Fleiszer A. Empty systematic reviews: hidden perils and lessons learned. J Clin Epidemiol. (2007) 60:595–7. doi: 10.1016/j.jclinepi.2007.01.005
81. Blehar MC, Spong C, Grady C, Goldkind SF, Sahin L, and Clayton JA. Enrolling pregnant women: issues in clinical research. Women's Health Issues. (2013) 23:e39–45. doi: 10.1016/j.whi.2012.10.003
82. Macklin R. Enrolling pregnant women in biomedical research. Lancet. (2010) 375:632–3. doi: 10.1016/S0140-6736(10)60257-7
Keywords: preterm birth, neonatal death, intrapartum stillbirth, gestational age, perinatal mental health, empty systematic review
Citation: Worrall S, Payne E, Fellows RE, Pike O, Carlisle NH, Carter J, Wittkowski A, Burgess K, Storey C, Magee LA, von Dadelszen P, Christiansen P, Fallon V, Khalil A and Silverio SA (2025) Women’s psychological experiences of preterm labour and birth which results in an intrapartum stillbirth or a neonatal death: an empty systematic review. Front. Psychiatry 16:1544485. doi: 10.3389/fpsyt.2025.1544485
Received: 12 December 2024; Accepted: 19 May 2025;
Published: 05 June 2025.
Edited by:
Laura Orsolini, Marche Polytechnic University, ItalyReviewed by:
Soudabeh Givrad, NewYork-Presbyterian, United StatesGiulio Longo, Marche Polytechnic University, Italy
Copyright © 2025 Worrall, Payne, Fellows, Pike, Carlisle, Carter, Wittkowski, Burgess, Storey, Magee, von Dadelszen, Christiansen, Fallon, Khalil and Silverio. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sergio A. Silverio, Uy5BLlNpbHZlcmlvQGxpdmVycG9vbC5hYy51aw==
†These authors share senior authorship
‡ORCID: Semra Worrall, orcid.org/0000-0002-6587-9306
Elana Payne, orcid.org/0009-0001-6214-6641
Rebecca E. Fellows, orcid.org/0009-0005-6909-6498
Olivia Pike, orcid.org/0009-0002-8703-132X
Naomi H. Carlisle, orcid.org/0000-0001-8943-8700
Jenny Carter, orcid.org/0000-0003-2550-6465
Anja Wittkowski, orcid.org/0000-0003-3806-0183
Karen Burgess, orcid.org/0000-0001-6256-116X
Claire Storey, orcid.org/0000-0002-5428-9909
Laura A. Magee, orcid.org/0000-0002-1355-610X
Peter von Dadelszen, orcid.org/0000-0003-4136-3070
Paul Christiansen, orcid.org/0000-0001-7534-0948
Victoria Fallon, orcid.org/0000-0002-7350-2568
Asma Khalil, orcid.org/0000-0003-2802-7670
Sergio A. Silverio, orcid.org/0000-0001-7177-3471
 Semra Worrall
Semra Worrall Elana Payne
Elana Payne Rebecca E. Fellows
Rebecca E. Fellows Olivia Pike1‡
Olivia Pike1‡ Anja Wittkowski
Anja Wittkowski Laura A. Magee
Laura A. Magee Peter von Dadelszen
Peter von Dadelszen Paul Christiansen
Paul Christiansen Victoria Fallon
Victoria Fallon Asma Khalil
Asma Khalil Sergio A. Silverio
Sergio A. Silverio