- 1Department of Psychiatry, Alan and Marlene Norton College of Medicine, SUNY Upstate Medical University, Syracuse, NY, United States
- 2Keck School of Medicine, University of Southern California, Los Angeles, CA, United States
Schemas are affective-cognitive conceptual models of self, others and the world, derived from life experience. Predictive Coding theory proposes schema are created from perceptual input as follows: Based on previous similar experiences, the brain generates schema, with “predictions,” expectations of future sensory experiences. Discrepancy between predicted versus actual experience produces a “prediction error.” Exposure to prediction errors considered more certain than the predictions of a schema prompts the hippocampus to update and revise the schema. Hypothesized underlying mechanisms include memory reconsolidation, extinction and pattern separation. Depression is characterized by negative schemas predicting helplessness, hopelessness and worthlessness. Early maladaptive schemas, from childhood, are implicated in mediating the greater risk of depression from childhood maltreatment. Prominent examples include the Defectiveness/Shame self-schema, predicting a flawed, unlovable self and the Social Isolation/Alienation schema, predicting isolation. Predictive Coding offers the following biopsychosocial hypothesis explaining how childhood maltreatment promotes depressogenic early maladaptive schema, and how psychotherapy can help: Schema can be difficult to change because of an attention/memory bias away from schema-incongruent information that generate prediction errors prompting schema revision. Childhood maltreatment exacerbates this learning bias. Maladaptive coping styles associated with childhood maltreatment, decrease exposure to experiences contradicting depressogenic schema. Biological changes from childhood maltreatment, including inflammation, interfere with hippocampal updating of schema. Finally, impaired socio-occupational function, associated with childhood maltreatment, reinforces depressogenic schema. By targeting factors associated with childhood maltreatment, which reinforce depressogenic early maladaptive schema or diminish prediction errors, psychotherapy can facilitate revision of depressogenic schema.
Child maltreatment, early maladaptive schemas, and predictions
A history of child maltreatment (CM), involving abuse (emotional, physical, or sexual) or neglect, increases the risk for depression incidence, severity, and treatment resistance (1–5). Predictive coding, a prominent neuroscience hypothesis, may explain how early maladaptive schemas (EMS) from CM promote depression and are addressed by psychotherapy.
Schemas are mental models, characterizing broad, core affective and cognitive beliefs about self, others, and the world (6). By organizing and filtering information for attention, interpretation, and memory, schemas can facilitate learning and decision making (7–9). Importantly, schemas generate predictions of cognitive, affective, and perceptual states typically characterizing different contexts (6). Thus, predictions from schemas offer guidance for future navigation of such contexts.
Childhood schemas can have long-standing psychological consequences (10). Bowlby proposed that “attachment styles,” reflecting child–parent relationships, substantially influence adult schemas of self (self-schemas), and of others (10). Emotionally attuned parenting facilitates the development of a “secure” attachment style (11). Securely attached adults generally “predict” being a lovable, competent self, and trustworthy and accepting close others (11). Such positive schemas of self/others are understood to foster social support and psychological health (11–13). In contrast, CM promotes EMS of self/others (14), and insecure attachment (15), which substantially contributes to psychopathology (15–17).
Depression, early maladaptive schema, and interlocking self-reinforcing feedback loops
Depression is characterized by negative schemas, predicting helplessness, hopelessness, and worthlessness (18, 19). Depressogenic EMS are implicated in increased depression risk from CM (20). In a recent metanalysis, the Defectiveness/Shame and Social Isolation/Alienation EMS were most strongly associated with depression. The Defectiveness/Shame self-schema predicts an inferior, unlovable self. The Social Isolation/Alienation self-schema predicts not belonging (21). Shame appears particularly important in perpetuating depression, through maladaptive styles of coping with shame, including avoidance (flight), overcompensation (fight), and surrender (freeze) (21, 22).
Surrendering to the Defectiveness/Shame EMS involves accepting shame, harsh self-criticism, and predicting failure and social rejection (22). Shame-prone persons often conceal personal “defectiveness,” even from themselves (23, 24). Overcompensation coping involves hostile, grandiose defensive denials of shame. Avoidance coping minimizes consciousness of shame by diverting attention, through compulsive reward-seeking (addiction), self-injury, and experiential avoidance (suppression) of distress (25).
Securely attached persons characteristically acknowledge and process distress with self-compassion and by seeking social support (11–13). In contrast, CM is associated with harsh self-criticism (26), the Defectiveness/Shame EMS (14), avoidant coping (27) and insecure attachment (15), which all promote depression (20, 28–32).
Impaired occupational function (33) and loneliness (34, 35) associated with CM may be mediated by insecure attachment, shame, and maladaptive shame-coping strategies (36–41). Interpersonal difficulties appear to mediate the association of childhood adversities with depression (42–44). Low social connectedness promotes depression risk, severity, and treatment resistance (45–47). Social support (48) is protective.
The Defectiveness/Shame and Social Isolation/Alienation EMS appear to negatively impact interpersonal function among persons with CM (49). The adverse impact is attributed to impaired mentalization, the ability to understand mental states in self/others (50, 51). Avoidance of self-disclosure in shame-prone persons, which promotes social disconnection, may also contribute (52).
Socio-occupational disappointments would, reasonably, be expected to confirm depressogenic schema (53), including the Shame/Defectiveness and Social Isolation/Alienation EMS. These schemas support self-sustaining feedback loops (Figure 1) underlying depression.
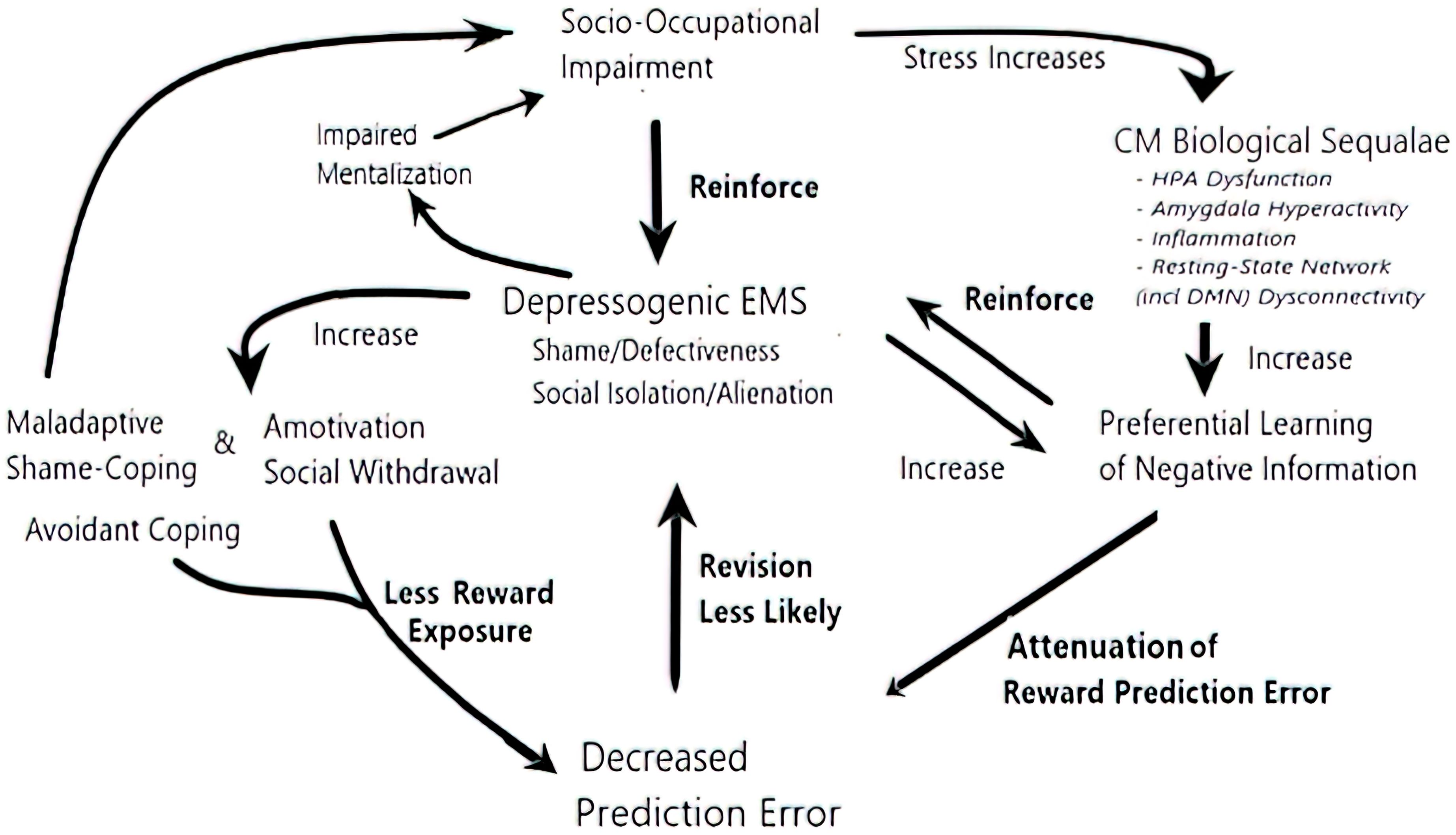
Figure 1. The self-sustaining feedback loops underlying depression. CM exacerbates all the elements driving the loops. In one loop, psychological sequelae of CM, including shame, maladaptive shame-coping, mentalization difficulties, social withdrawal, and a motivation, all impair socio-occupational function (36–41). In turn, repeated socio-occupational disappointments can confirm EMS of Defectiveness/Shame and Social Isolation/Alienation, reinforcing their certainty and resistance to schema-incongruent information (53, 54). In another interlocked recursive loop, CM sequelae diminish exposure to and learning from reward prediction errors, which could have revised depressogenic EMS: For example, avoidant coping decreases social/occupational engagement, thus reducing opportunities for reward prediction errors. When rewarding experiences do arise, their impact is decreased by biological sequelae of CM: amygdala hyperactivity, HPA axis dysfunction, and inflammation promote preferential learning of negative information (55–59), through attenuated reward prediction error, negative overgeneralized memory, and negative memory/attention biases socio-occupational stress further exacerbates the biological sequelae (60–62), completing the loop.
An introduction to predictive coding
Predictive coding offers a biopsychosocial framework, explaining how CM promotes depressogenic EMS and how psychotherapy can help. Principles underlying predictive coding were first characterized in sensory processing, explaining how the brain constructs reality from perception.
Predictive coding theory proposes that the brain creates predictions of reality from schemas and perceptual input as follows (63–67): based on schemas, derived from repeated associative memory patterns (see below), the brain generates “predictions,” expectations of future sensory experiences. Discrepancies between the prediction and actual experience produce “prediction errors,” signaling mismatch. The brain minimizes prediction errors, through “active inference,” a process that optimizes the match between actual and predicted experience. Active inference involves either updating the pre-existing prediction or, instead, suppressing the prediction error.
Predictions and prediction errors are inherently uncertain, derived from statistically “noisy” environmental signals. Predictions cannot be perfectly accurate. The level of certainty in predictions, relative to prediction error, determines if, and how much, the prediction is updated following an experience (68).
When an experience that is incongruent with the prediction is considered more accurate than the prediction, the prediction error is more certain than the pre-existing prediction. The prediction, consequently, is updated (68). Prediction errors, from information considered as less certain than the prior prediction, are instead suppressed by changing neural input to match the prediction (68, 69). Commonly, attention is redirected away from the perceptions generating the prediction error. By ignoring unexpected sensory information, the prediction error is dismissed. Thus, the pre-existing prediction is maintained rather than being updated (70, 71).
Highly certain predictions are harder to update because, comparatively, prediction errors appear less certain and are, therefore, suppressed. Disregarding prediction errors, reflecting anomalous, “noisy,” incongruent information, is adaptive when the prior prediction is, indeed, more accurate. However, ignoring unexpected perceptions (dismissing “prediction errors”) that better reflect reality than pre-existing predictions is maladaptive.
Predictive coding in perceptual processing is better understood than in processing memory and schemas. Nonetheless, emerging research shows clear parallels in the principles of predictive coding in perception, memory and schemas (71–75). Hypotheses suggest that psychotherapy often promotes “prediction errors” from unexpected experiences, which then revise maladaptive schemas of self/others, derived from autobiographical memories of childhood adversity (71–75).
Schemas
Autobiographical memories are believed to be represented by neural networks, with distributed nodes across brain regions bound together through Hebbian plasticity (76). Specialized nodes represent different elements of memory, such as the sensations, emotions, and spatiotemporal context. Over time, ventromedial prefrontal cortex (vmPFC)—hippocampus interactions “schematize,” or transform, memories into schemas (77). When schemas generate faulty predictions, the prediction error can prompt hippocampal updates to memories and schema (78–80).
The hippocampus creates memories by rapidly connecting associated experiences (80). Over time, vmPFC-hippocampal interactions are hypothesized to extract patterns of common, recurrent associations, thereby creating conceptual structures of cognitive-affective knowledge or schemas (67, 80). Schematization allows information reflecting memory commonalities to be condensed, organized, and recalled efficiently (67, 77, 81–84). Unique details become less accessible (7). Schemas also generate predictions, since common, repeated associations (“statistical regularities”) generally recur.
For example, seasoned travelers predict the common, repeated aspects of airport travel, involving typical sequences, tasks, emotions, and so forth. Recurrent, common aspects of airport memories become incorporated into airport travel schema, and associated predictions, while excluding unique features, such as flight numbers.
Cognitive-affective schema after childhood trauma and depression
EMS in the Disconnection/Rejection Domain, such as the Defectiveness/Shame and Social Isolation/Alienation EMS, are proposed to develop from schematization of repeated childhood experiences of unmet core emotional needs from attachment figures (85, 86).
Depressogenic EMS is proposed to arise from extracting common, repeated experiences of CM, woven together with schema of self/others. Children may respond to harsh parenting with habitual submission (86, 87). Repeated appeasement of belittling, dominant others can lead to an internalized shame-based self-schema, consistent with the Defectiveness/Shame EMS (86, 87). Recurrent parental maltreatment is believed to lead to schema of others as rejecting (Social Isolation/Alienation EMS) (11, 86, 88).
Depressogenic early maladaptive schema—neurodevelopmental hypotheses
CM-induced neurodevelopmental changes to the circuitry are hypothesized to promote vulnerability to EMS (85). Mapping the underlying circuity or changes from CM promoting EMS remains preliminary. Research challenges are attributed to heterogeneous timing and type of CM and genetic susceptibility (89).
CM-induced changes in the structure, function, and connectivity of brain areas in prefrontal-subcortical circuits (90), such as the mPFC, hippocampus, limbic areas, Default-Mode Network (DMN), involved in self-referential processing (91, 92), and mentalizing network (93), are hypothesized to increase vulnerability to maladaptive schema of self/others (85). Amygdala hyper-reactivity (2, 94, 95), altered amygdala connectivity with DMN, and mentalizing network nodes (2, 96) and hippocampal volume reduction (2) are proposed to increase cognition, salience, and recall of negative self-characteristics. Blunted striatal reward activity (97) and increased threat-related insula and amygdala activity (98) associated with CM may contribute to impaired self-efficacy (99, 100). CM-induced changes to mentalizing networks are suggested to play a role in schema predicting untrustworthy others (101).
In summary, CM-induced neurodevelopmental changes are hypothesized to promote negative schema of rejecting/untrustworthy others and self-schema involving negative self-characteristics. These negative self-/other schemas are consistent with the Defectiveness/Shame and Social Isolation/Alienation EMS. Established depressogenic EMS are self-reinforcing: vmPFC-hippocampal interactions boost engagement toward schema-congruent information (7, 67). CM-induced cognitive bias toward negative information provides further confirmation.
Child maltreatment promotes preferential learning of negative information
Overgeneralization, pattern completion, and impaired pattern separation
Sensory, affective, and cognitive aspects of predictions are encoded by diverse specialized neural areas, or nodes, interconnected within an auto-associative network. A partial cue activating several nodes can activate the entire network. For example, packing luggage can instantiate a schema of airport travel, with characteristic sensory, cognitive, and emotional aspects. Instantiating a prediction from a partial cue is termed “Pattern Completion.” (102).
Pattern Completion is counterbalanced by Pattern Separation, a neurocomputational process that encodes new memories distinctly from old memories in prior contexts, thereby minimizing interference (103). When Pattern Separation is impaired, Pattern Completion can become maladaptive, promoting overgeneralization (104). Overgeneralized learning extrapolates associations from isolated experiences to inappropriate, unrelated contexts (105): for example, a depressed patient may receive mild criticism about performance in an atypical circumstance. This partial cue of isolated criticism, in a narrow, atypical context, can instantiate a childhood schema of self-denigration, related to harsh parenting (105). Thus, overgeneralization can reinforce the Defectiveness/Shame EMS.
Negative memory overgeneralization likely mediates the association of CM with pessimism and harsh self-criticism (106). Hippocampal neurogenesis is implicated in Pattern Separation (103, 107, 108). CM-induced inflammation and hypercortisolemia can suppress neurogenesis (103, 109), thereby interfering with Pattern Separation. Such pathophysiological changes are believed to underlie increased overgeneralization in CM (103).
Negative attention and memory bias
In addition to their role in schematization, vmPFC—hippocampus interactions are proposed to underlie a top-down attention/memory bias toward schema-congruent information (7, 67): new information, congruent with a schema, is easier to attend and recall than schema-incongruent information (67).
The learning bias against schema-incongruent information may reflect skepticism of anomalous data. Skepticism about data that is inconsistent with statistical regularities embedded in schemas can be adaptive. However, bias against schema-incongruent information is maladaptive when the schema is held with unwarranted certainty.
CM biases attention and memory toward negative (over positive) information. Examples include angry over happy faces or negative (over positive) self-descriptive words (110, 111). Negative attention bias predicts increased depression severity (112). Negative memory bias is associated with rumination, which in turn, exacerbates depression (113). Biological sequelae attributed to CM, including amygdala hyperactivity, resting-state network (including DMN) dysconnectivity (114), HPA axis dysfunction, and increased inflammation (2, 55, 95, 115), are implicated in negative attention and memory bias (56–58, 95, 116, 117).
Attenuated reward prediction errors, child maltreatment and preferential learning of negative information—interim summary
Prediction errors from unexpected rewards would be expected to prompt revision of depressogenic schema (78, 79). Growing evidence indicates that CM diminishes reward prediction errors, thereby disrupting learning from positive experiences (97). In support of this connection, attenuated reward prediction errors are linked to anhedonia and a higher depression risk (118).
CM likely promotes preferential learning of negative information through diminished reward prediction errors, overgeneralized memory, and negative learning biases, thereby promoting depression (106, 110, 113).
Preferentially attending to and remembering failure and rejection, while minimizing socio-occupational rewards, promotes a motivation and social withdrawal. Furthermore, these learning disruptions confirm depressogenic EMS, such as Defectiveness/Shame and Social Isolation/Alienation. The mutual reinforcement of depressogenic schema and negative learning biases creates another positive feedback loop in depressed patients with CM (Figure 1).
Child maltreatment and interlocking self-reinforcing feedback loops promote depressive early maladaptive schema
Many forms of psychopathology, including depression, are proposed to result from maladaptive predictions carrying excessive certainty over prediction errors, rendering them resistant to update by new incongruent information (54, 119–121).
CM exacerbates interlocking self-reinforcing feedback loops proposed to maintain depression (53) (Figure 1). Repeated life disappointments can confirm EMS of Defectiveness/Shame and Social Isolation/Alienation, increasing their certainty and resistance to schema-incongruent information (53, 54). CM exacerbates this feedback loop, in which socio-occupational dysfunction and excessive certainty in depressogenic EMS, such as the Defectiveness/Shame and Social/Isolation/Alienation EMS, cumulatively reinforce each other.
Both biological and psychological sequelae of CM promote and reinforce depressogenic EMS (2, 122): for example, harsh self-criticism, impaired mentalization, and negative cognitive biases amplify the impact of aversive experiences, while avoidant coping diminishes exposure to, and learning from, prediction errors generated by social/occupational rewards (2, 122). Finally, biological sequelae of CM also amplify learning reinforcing depressogenic EMS, while attenuating reward prediction error (55–62).
Prediction updating by psychotherapy
Neuroscience hypotheses of therapeutic change
The relative imperviousness of EMS to schema-incongruent information effectively impairs learning impeding therapeutic change in persons with CM.
Neural processes proposed to mediate prediction updating in psychotherapy include memory reconsolidation, extinction, and pattern separation (123–125). These processes are currently understood as follows: Prediction errors, sent to the hippocampus, appear to prompt updates to neural networks that encode predictions (126, 127). Memory reconsolidation involves erasing existing maladaptive associations and creating new associations (123, 124, 128). Extinction involves creating a new memory that competes with the old maladaptive memory (123). Pattern separation encodes a new adaptive memory in a distinct context, separate from the prior context, to counteract overgeneralization (125, 129).
In summary, extinction and pattern separation lead to coexisting old and new predictions. Memory reconsolidation replaces old predictions with new ones.
EMS disrupt therapeutic relationships
The therapeutic alliance is the chief predictor of successful psychotherapy adherence (130) and outcomes (131). CM sequelae, including shame/harsh self-criticism (132–134) and insecure attachment (15, 135, 136), can disrupt the therapeutic bond. This disruption likely contributes to treatment resistance in persons with CM (4, 5).
The Defectiveness/Shame EMS may disrupt the therapeutic alliance in several ways. When patients cope with shame through denial, withdrawal, self-criticism, or hostility, therapists may respond by distancing (137). Furthermore, shame induces the urge to avoid self-disclosure (24). Shame-prone persons reveal less in psychotherapy (138, 139).
The therapeutic alliance and prediction errors
A “corrective emotional experience” is an unexpected experience with a therapist, which challenges maladaptive schemas, and is believed to generate a prediction error (140–143). This “corrective emotional experience” is considered an important mechanism of change in psychotherapy (123, 140, 144). For example, feeling safety, support, and connection with a therapist is incongruent with depressogenic EMS predicting inadequacy and rejection (145). “Attachment security priming,” in which a therapist is experienced as a safe, secure attachment figure (146), contributes substantially to the healing benefit of the therapeutic alliance (145).
Attachment security priming alleviates many factors driving self-reinforcing feedback loops underlying depression. Security priming increases feelings of self-compassion, self-acceptance, and belonging (145). These feelings can generate prediction errors, directly counteracting the EMS of Defectiveness/Shame and Social Isolation/Alienation, of a flawed, inferior, unlovable self (21).
Security priming may improve receptivity to schema-incongruent information, particularly in persons with CM, given their higher prevalence of insecure attachment (147). Insecurely attached persons characteristically ignore or defend against new schema-incongruent information (11), which would be expected to diminish exposure to prediction errors. Security priming has been proposed to promote epistemic trust, the willingness to consider new perspectives from a therapist as trustworthy, generalizable, and self-relevant (148). Security priming also increases cognitive openness to new information (145). Epistemic trust and cognitive openness both likely support receptivity to schema-incongruent information and revision of maladaptive schema.
Psychotherapy targets elements of self-reinforcing feedback loops
Psychological interventions may improve biological sequelae of CM. Amygdala hyperactivity and inflammation, which are implicated in negative learning bias (56, 57, 59, 117, 149, 150), improve with security priming and cognitive behavioral therapy (CBT), respectively (149–151).
Different psychotherapy approaches target different elements of the self-reinforcing feedback loop (Figure 2). Interpersonal therapy facilitates social engagement over withdrawal (152). CBT challenges preferential learning of negative information and anhedonia/social withdrawal by encouraging engagement with rewarding experiences (153). Attitudes of acceptance, mindfulness, self-compassion, and committed action in Acceptance and Commitment Therapy counteract avoidant coping and the Defectiveness/Shame EMS (154, 155).
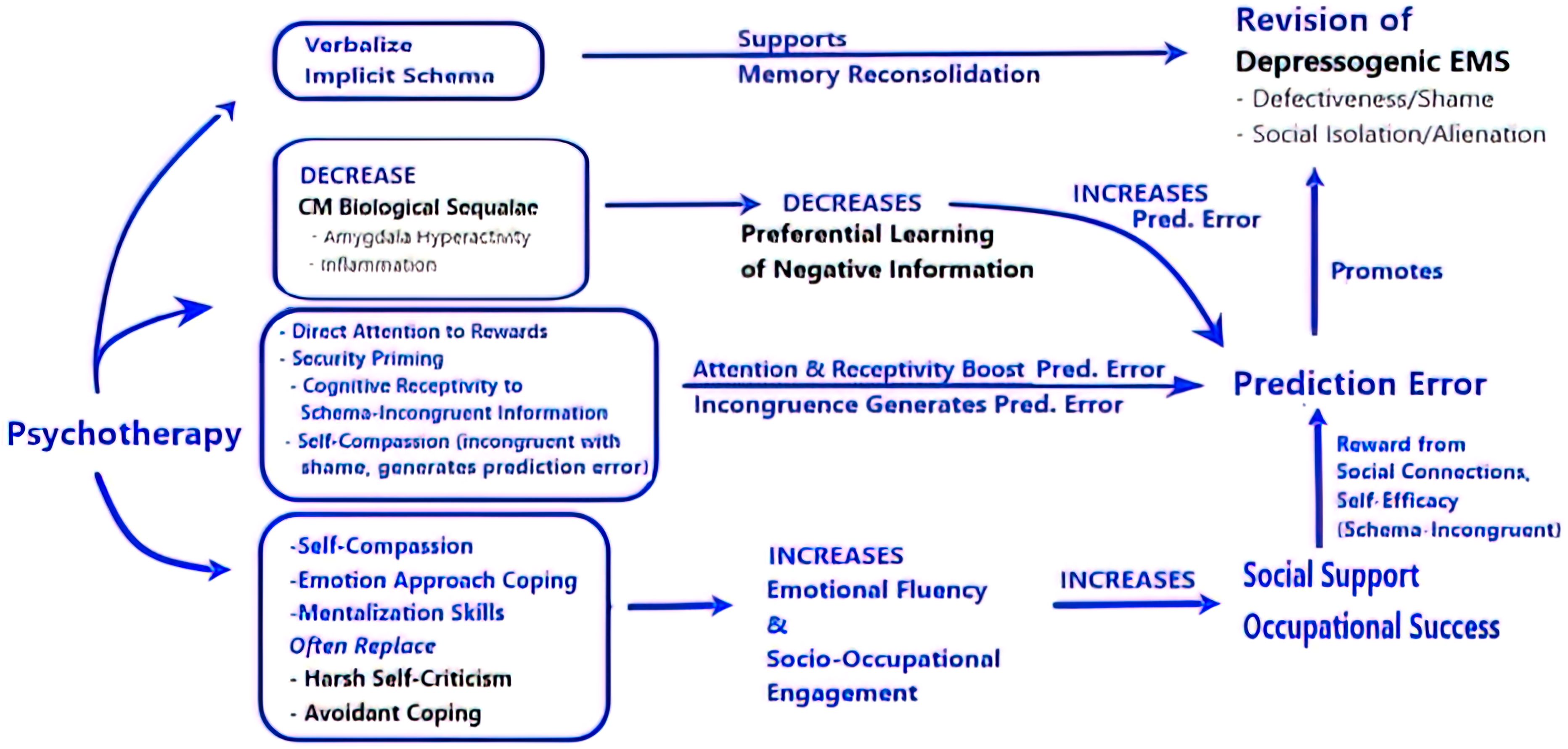
Figure 2. Psychotherapy targets elements promoting EMS and boosts factors supporting revision of depressogenic early maladaptive schema. The figure illustrates hypothetical pathways explaining how psychotherapy targets vulnerability factors (in black) promoting depression/depressogenic and boosts factors (in blue) supporting EMS revision. (1) Verbalizing implicit schema supports memory reconsolidation. (2) Psychotherapy (security priming & CBT) improves CM biological sequelae that would otherwise attenuate prediction error. (3) Prediction error prompting EMS revision is boosted by directing attention and improving cognitive receptivity to schema-incongruent information. Security priming also promotes self-compassion, which is incongruent with the Defectiveness/Shame EMS, and thus generates a prediction error. (4) Self-compassion, emotion approach coping, and Mentalization skills counteract harsh self-criticism and avoidant coping, support emotional fluency, and facilitate socio-occupational engagement.
Psychotherapy revises EMS
Several psychotherapy schools, including CBT, schema therapy and many psychodynamic approaches directly target maladaptive schemas for revision and updating. One first step involves helping patients verbalize implicit maladaptive schemas. This may support memory reconsolidation (128): memory reconsolidation does not impact inactive predictions stored in memory but rather affects actively recalled predictions. Explicitly articulating EMS may support active recall, thereby facilitating reconsolidation.
Prediction error appears important for hippocampal prediction updating (156), and thus, important for revising EMS. Indeed, pretreatment reward prediction errors predict depression responsiveness to CBT (157). Exposure to prediction errors appears diminished by both avoidant coping and preferential learning of negative information, which are targets of psychotherapy (153, 154). Attention to schema-incongruent information, by CBT and psychodynamic therapies (74, 158–160), may instead boost the neural encoding of prediction errors (161).
Summary: experiential avoidance, impaired socio-occupational function and depressogenic EMS are mutually reinforcing, and key targets of psychotherapy
The Defectiveness/Shame EMS is hypothesized to reflect the maladaptive persistence of an appeasement strategy toward harsh parents, accompanied by experiential avoidance of anger and grief (87). Experiential avoidance can be understood as a maladaptive prediction, that anger and grief are so shameful, dangerous, and/or intolerable that suppression is the only solution (162). Many psychotherapy approaches encourage “emotion approach coping,” attending to and processing emotions, instead of suppression (153, 154, 163, 164).
In psychotherapy, patients may discover they can tolerate their anger and grief. This prediction error would be expected to revise habitual experiential avoidance to a new prediction: attention to affective information is meaningful and useful.
Access to a wider emotional range can expand a patient’s repertoire to include acknowledging and communicating distress, improved mentalization, assertiveness, and social engagement. Greater self-compassion and emotional fluency enable social and occupational success, which decreases amygdala activity (165) and inflammation (166) and leads to further positive experiences (reward prediction errors). Psychotherapy can thus facilitate a virtuous self-reinforcing cycle of more positive self-schema, adaptive coping strategies and improving function.
Author contributions
GR: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. AC: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Nelson J, Klumparendt A, Doebler P, Ehring T. Childhood maltreatment and characteristics of adult depression: meta-analysis. Br J Psychiatry. (2017) 210:96–104. doi: 10.1192/bjp.bp.115.180752
2. Kuzminskaite E, Penninx B, van Harmelen AL, Elzinga BM, Hovens J, Vinkers CH. Childhood trauma in adult depressive and anxiety disorders: an integrated review on psychological and biological mechanisms in the NESDA cohort. J Affect Disord. (2021) 283:179–91. doi: 10.1016/j.jad.2021.01.054
3. Jaworska-Andryszewska P, Rybakowski JK. Childhood trauma in mood disorders: Neurobiological mechanisms and implications for treatment. Pharmacol Rep. (2019) 71:112–20. doi: 10.1016/j.pharep.2018.10.004
4. Lippard ETC, Nemeroff CB. The devastating clinical consequences of child abuse and neglect: increased disease vulnerability and poor treatment response in mood disorders. Am J Psychiatry. (2020) 177:20–36. doi: 10.1176/appi.ajp.2019.19010020
5. Teicher MH, Gordon JB, Nemeroff CB. Recognizing the importance of childhood maltreatment as a critical factor in psychiatric diagnoses, treatment, research, prevention, and education. Mol Psychiatry. (2022) 27:1331–8. doi: 10.1038/s41380-021-01367-9
6. Young JEK, Weishaar JS, Marjorie E. Schema Therapy: Conceptual Model. In: Schema Therapy: A Practitioner’s Guide. New York, NY, USA: Guilford Press (2006). p. 1–62.
7. Gilboa A, Marlatte H. Neurobiology of schemas and schema-mediated memory. Trends Cognit Sci. (2017) 21:618–31. doi: 10.1016/j.tics.2017.04.013
8. Hales RE, Yudofsky SC, Gabbard GO, American Psychiatric Publishing. The American Psychiatric Publishing textbook of psychiatry. 5th ed Vol. xxxi. . Washington, DC: American Psychiatric Pub (2008). p. 1786.
9. McQuaid JR, Thase ME. Mood Disorders: Psychotherapy. In: Kaplan and Sadocks Comprehensive Textbook of Psychiatry, Tenth Edition. Wolters Kluwer Health, Philadelphia (2017).
10. Bretherton I, Munholland KA. Internal Working Models in Attachment Relationships Elaborating a Central Construct in Attachment Theory 2008. In: Handbook of Attachment: Theory, Research, and Clinical Applications, 2nd ed. (2008) New York, NY, USA: Guilford Publications Kindle Edition.
11. Shaver PR, Mikulincer M. Attachment-related psychodynamics. Attach Hum Dev. (2002) 4:133–61. doi: 10.1080/14616730210154171
12. Deylyen M, Greenberg M. Attachment and Psychopathology in Childhood 2008. In: Handbook of Attachment, Second Edition: Theory, Research, and Clinical Applications, Kindle Edition. 2nd. Guilford Publications, New York. p. 1020.
13. Mikulincer M, Shaver PR. An attachment and behavioral systems perspective on social support. J Soc Pers Relations. (2009) 26:7–19. doi: 10.1177/0265407509105518
14. May T, Younan R, Pilkington PD. Adolescent maladaptive schemas and childhood abuse and neglect: A systematic review and meta-analysis. Clin Psychol Psychother. (2022) 29:1159–71. doi: 10.1002/cpp.v29.4
15. Nivison MD, Facompre CR, Raby KL, Simpson JA, Roisman GI, Waters TEA. Childhood abuse and neglect are prospectively associated with scripted attachment representations in young adulthood. Dev Psychopathol. (2021) 33:1143–55. doi: 10.1017/S0954579420000528
16. van-Wijk-Herbrink MF, Bernstein DP, Broers NJ, Roelofs J, Rijkeboer MM, Arntz A. Internalizing and externalizing behaviors share a common predictor: the effects of early maladaptive schemas are mediated by coping responses and schema modes. J Abnorm Child Psychol. (2018) 46:907–20. doi: 10.1007/s10802-017-0386-2
17. Roelofs J, Onckels L, Muris P. Attachment quality and psychopathological symptoms in clinically referred adolescents: the mediating role of early maladaptive schema. J Child Fam Stud. (2013) 22:377–85. doi: 10.1007/s10826-012-9589-x
18. Trincas R, Ottaviani C, Couyoumdjian A, Tenore K, Spitoni G, Mancini F. Specific dysphoric symptoms are predicted by early maladaptive schemas. ScientificWorldJournal. (2014) 2014:231965. doi: 10.1155/2014/231965
19. Wright MO, Crawford E, Del Castillo D. Childhood emotional maltreatment and later psychological distress among college students: the mediating role of maladaptive schemas. Child Abuse Negl. (2009) 33:59–68. doi: 10.1016/j.chiabu.2008.12.007
20. Li ET, Luyten P, Midgley N. Psychological mediators of the association between childhood emotional abuse and depression: A systematic review. Front Psychiatry. (2020) 11:559213. doi: 10.3389/fpsyt.2020.559213
21. Bishop A, Younan R, Low J, Pilkington PD. Early maladaptive schemas and depression in adulthood: A systematic review and meta-analysis. Clin Psychol Psychother. (2022) 29:111–30. doi: 10.1002/cpp.v29.1
22. Brockman RN, Simpson S, Hayes C, Wijngaart Rvd, Smout M. From Core Emotional Needs to Schemas, Coping Styles, and Schema Modes The Conceptual Model of Schema Therapy. In: Cambridge Guide to Schema Therapy (Cambridge Guides to the Psychological Therapies). Cambridge University Press. Kindle Edition, Melbourne, Australia (2023). p. 1–15.
23. Wurmser L. Primary shame, mortal wound and tragic circularity: Some new reflections on shame and shame conflicts. Int J Psychoanal. (2015) 96:1615–34. doi: 10.1111/1745-8315.12470
24. Tangney JP, Stuewig J, Mashek DJ. Moral emotions and moral behavior. Annu Rev Psychol. (2007) 58:345–72. doi: 10.1146/annurev.psych.56.091103.070145
25. Farr J, Ononaiye M, Irons C. Early shaming experiences and psychological distress: The role of experiential avoidance and self-compassion. Psychol Psychother. (2021) 94:952–72. doi: 10.1111/papt.12353
26. Jina Pagura BJC, Sareen J, Enns MW. Childhood adversities associated with self-criticism in a nationally representative sample. Pers Individ Diff. (2006) 41:1287–98. doi: 10.1016/j.paid.2006.05.003
27. Korem N, Ben-Zion Z, Spiller TR, Duek OA, Harpaz-Rotem I, Pietrzak RH. Correlates of avoidance coping in trauma-exposed U.S. military veterans: Results from the National Health and Resilience in Veterans Study. J Affect Disord. (2023) 339:89–97. doi: 10.1016/j.jad.2023.07.036
28. Holahan CJ, Moos RH, Holahan CK, Brennan PL, Schutte KK. Stress generation, avoidance coping, and depressive symptoms: a 10-year model. J Consult Clin Psychol. (2005) 73:658–66. doi: 10.1037/0022-006X.73.4.658
29. Martin F, Scheel C, Legenbauer T. Shame coping strategies amplify certain psychopathologies. Psychopathology. (2021) 54:305–14. doi: 10.1159/000517767
30. Castilho P, Pinto-Gouveia J, Duarte J. Two forms of self-criticism mediate differently the shame-psychopathological symptoms link. Psychol Psychother. (2017) 90:44–54. doi: 10.1111/papt.2017.90.issue-1
31. Carvalho S, Dinis A, Pinto-Gouveia J, Estanqueiro C. Memories of shame experiences with others and depression symptoms: the mediating role of experiential avoidance. Clin Psychol Psychother. (2015) 22:32–44. doi: 10.1002/cpp.v22.1
32. Barnhofer T, Brennan K, Crane C, Duggan D, Williams JM. A comparison of vulnerability factors in patients with persistent and remitting lifetime symptom course of depression. J Affect Disord. (2014) 152-154:155–61. doi: 10.1016/j.jad.2013.09.001
33. Bunting L, Davidson G, McCartan C, Hanratty J, Bywaters P, Mason W, et al. The association between child maltreatment and adult poverty - A systematic review of longitudinal research. Child Abuse Negl. (2018) 77:121–33. doi: 10.1016/j.chiabu.2017.12.022
34. Landry J, Asokumar A, Crump C, Anisman H, Matheson K. Early life adverse experiences and loneliness among young adults: The mediating role of social processes. Front Psychol. (2022) 13:968383. doi: 10.3389/fpsyg.2022.968383
35. Zamir O. Childhood maltreatment and relationship quality: A review of type of abuse and mediating and protective factors. Trauma Viol. Abuse. (2022) 23:1344–57. doi: 10.1177/1524838021998319
36. Zuroff DC, Koestner R, Powers TA. Self-criticism at age 12: A longitudinal study of adjustment. Cogn Ther Res. (1994) 18:367–85. doi: 10.1007/BF02357511
37. Ypsilanti A, Lazuras L, Powell P, Overton P. Self-disgust as a potential mechanism explaining the association between loneliness and depression. J Affect Disord. (2019) 243:108–15. doi: 10.1016/j.jad.2018.09.056
38. Ypsilanti A. Lonely but avoidant—the unfortunate juxtaposition of loneliness and self-disgust. Palgrave Commun. (2018) 4:144. doi: 10.1057/s41599-018-0198-1
39. Srivastava S, Tamir M, McGonigal KM, John OP, Gross JJ. The social costs of emotional suppression: a prospective study of the transition to college. J Pers Soc Psychol. (2009) 96:883–97. doi: 10.1037/a0014755
40. Michaeli Y, Kalfon Hakhmigari M, Dickson DJ, Scharf M, Shulman S. The role of change in self-criticism across young adulthood in explaining developmental outcomes and psychological wellbeing. J Pers. (2019) 87:785–98. doi: 10.1111/jopy.12433
41. Dodge KA. How a defensive mindset develops from early adverse experiences and guides antisocial outcomes. Dev Psychopathol. (2024) 36(5):2585–2591. doi: 10.1017/S0954579424000348
42. Panagou C, MacBeth A. Deconstructing pathways to resilience: A systematic review of associations between psychosocial mechanisms and transdiagnostic adult mental health outcomes in the context of adverse childhood experiences. Clin Psychol Psychother. (2022) 29:1626–54. doi: 10.1002/cpp.v29.5
43. Hammen C. Risk factors for depression: an autobiographical review. Annu Rev Clin Psychol. (2018) 14:1–28. doi: 10.1146/annurev-clinpsy-050817-084811
44. Sheets ES, Craighead WE. Comparing chronic interpersonal and noninterpersonal stress domains as predictors of depression recurrence in emerging adults. Behav Res Ther. (2014) 63:36–42. doi: 10.1016/j.brat.2014.09.001
45. Mann F, Wang J, Pearce E, Ma R, Schlief M, Lloyd-Evans B, et al. Loneliness and the onset of new mental health problems in the general population. Soc Psychiatry Psychiatr Epidemiol. (2022) 57:2161–78. doi: 10.1007/s00127-022-02261-7
46. Wang J, Mann F, Lloyd-Evans B, Ma R, Johnson S. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry. (2018) 18:156. doi: 10.1186/s12888-018-1736-5
47. Wickramaratne PJ, Yangchen T, Lepow L, Patra BG, Glicksburg B, Talati A, et al. Social connectedness as a determinant of mental health: A scoping review. PloS One. (2022) 17:e0275004. doi: 10.1371/journal.pone.0275004
48. Gariepy G, Honkaniemi H, Quesnel-Vallee A. Social support and protection from depression: systematic review of current findings in Western countries. Br J Psychiatry. (2016) 209:284–93. doi: 10.1192/bjp.bp.115.169094
49. Janovsky T, Rock AJ, Thorsteinsson EB, Clark GI, Murray CV. The relationship between early maladaptive schemas and interpersonal problems: A meta-analytic review. Clin Psychol Psychother. (2020) 27:408–47. doi: 10.1002/cpp.v27.3
50. Csukly G, Telek R, Filipovits D, Takacs B, Unoka Z, Simon L. What is the relationship between the recognition of emotions and core beliefs: Associations between the recognition of emotions in facial expressions and the maladaptive schemas in depressed patients. J Behav Ther Exp Psychiatry. (2011) 42:129–37. doi: 10.1016/j.jbtep.2010.08.003
51. Hayden MC, Mullauer PK, Gaugeler R, Senft B, Andreas S. Improvements in mentalization predict improvements in interpersonal distress in patients with mental disorders. J Clin Psychol. (2018) 74:2276–86. doi: 10.1002/jclp.2018.74.issue-12
52. Gilbert P. Shame, humiliation, guilt, and social status. In: Compassion Focused Therapy: Clinical Practice and Applications, vol. 1. Routledge, New York, NY (2022).
53. Smith R, Alkozei A, Killgore WDS, Lane RD. Nested positive feedback loops in the maintenance of major depression: An integration and extension of previous models. Brain Behav Immun. (2018) 67:374–97. doi: 10.1016/j.bbi.2017.09.011
54. Kube T, Schwarting R, Rozenkrantz L, Glombiewski JA, Rief W. Distorted cognitive processes in major depression: A predictive processing perspective. Biol Psychiatry. (2020) 87:388–98. doi: 10.1016/j.biopsych.2019.07.017
55. Murphy F, Nasa A, Cullinane D, Raajakesary K, Gazzaz A, Sooknarine V, et al. Childhood trauma, the HPA axis and psychiatric illnesses: A targeted literature synthesis. Front Psychiatry. (2022) 13:748372. doi: 10.3389/fpsyt.2022.748372
56. Harrison NA, Voon V, Cercignani M, Cooper EA, Pessiglione M, Critchley HD. A neurocomputational account of how inflammation enhances sensitivity to punishments versus rewards. Biol Psychiatry. (2016) 80:73–81. doi: 10.1016/j.biopsych.2015.07.018
57. De Raedt R, Koster EH. Understanding vulnerability for depression from a cognitive neuroscience perspective: A reappraisal of attentional factors and a new conceptual framework. Cognit Affect Behav Neurosci. (2010) 10:50–70. doi: 10.3758/CABN.10.1.50
58. Ellenbogen MA, Schwartzman AE, Stewart J, Walker CD. Stress and selective attention: the interplay of mood, cortisol levels, and emotional information processing. Psychophysiology. (2002) 39:723–32. doi: 10.1111/psyp.2002.39.issue-6
59. Jiang Y. A theory of the neural mechanisms underlying negative cognitive bias in major depression. Front Psychiatry. (2024) 15:1348474. doi: 10.3389/fpsyt.2024.1348474
60. Zhang X, Ge TT, Yin G, Cui R, Zhao G, Yang W. Stress-induced functional alterations in amygdala: implications for neuropsychiatric diseases. Front Neurosci. (2018) 12:367. doi: 10.3389/fnins.2018.00367
61. Slavich GM, Irwin MR. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol Bull. (2014) 140:774–815. doi: 10.1037/a0035302
62. Herman JP, McKlveen JM, Ghosal S, Kopp B, Wulsin A, Makinson R, et al. Regulation of the hypothalamic-pituitary-adrenocortical stress response. Compr Physiol. (2016) 6:603–21. doi: 10.1002/cphy.c150015
63. O'Callaghan C, Kveraga K, Shine JM, Adams RB Jr., Bar M. Predictions penetrate perception: Converging insights from brain, behaviour and disorder. Cons. Cogn. (2017) 47:63–74. doi: 10.1016/j.concog.2016.05.003
64. Kaye AP, Krystal JH. Predictive processing in mental illness: Hierarchical circuitry for perception and trauma. J Abnorm Psychol. (2020) 129:629–32. doi: 10.1037/abn0000628
65. Shipp S. Neural elements for predictive coding. Front Psychol. (2016) 7:1792. doi: 10.3389/fpsyg.2016.01792
66. Nadel L. What Is a Memory That It Can Be Changed? In: Neuroscience of Enduring Change: Implications for Psychotherapy. Oxford University Press. Kindle Edition, New York, NY (2020).
67. Ghosh VE, Gilboa A. What is a memory schema? A historical perspective on current neuroscience literature. Neuropsychologia. (2014) 53:104–14. doi: 10.1016/j.neuropsychologia.2013.11.010
68. Friston K. Does predictive coding have a future? Nat Neurosci. (2018) 21:1019–21. doi: 10.1038/s41593-018-0200-7
69. Pezzulo G, Parr T, Friston K. Active inference as a theory of sentient behavior. Biol Psychol. (2024) 186:108741. doi: 10.1016/j.biopsycho.2023.108741
70. Yon D, Heyes C, Press C. Beliefs and desires in the predictive brain. Nat Commun. (2020) 11:4404. doi: 10.1038/s41467-020-18332-9
71. Holmes J, Nolte T. Surprise" and the Bayesian Brain: Implications for Psychotherapy Theory and Practice. Front Psychol. (2019) 10:592. doi: 10.3389/fpsyg.2019.00592
72. Holmes J. Friston's free energy principle: new life for psychoanalysis? BJPsych. Bull. (2022) 46:164–8. doi: 10.1192/bjb.2021.6
73. Chekroud AM. Unifying treatments for depression: an application of the Free Energy Principle. Front Psychol. (2015) 6:153. doi: 10.3389/fpsyg.2015.00153
74. Ecker B. Erasing Problematic Emotional Learnings Psychotherapeutic Use of Memory Reconsolidation Research 2020. In: Neuroscience of Enduring Change: Implications for Psychotherapy. (2020) Oxford University Press. Kindle Edition, New York.
75. Solms M. New project for a scientific psychology: General scheme. Neuropsychoanalysis. (2020) 22:5–35. doi: 10.1080/15294145.2020.1833361
76. Miry O, Li J, Chen L. The quest for the hippocampal memory engram: from theories to experimental evidence. Front Behav Neurosci. (2020) 14:632019. doi: 10.3389/fnbeh.2020.632019
77. Moscovitch M, Cabeza R, Winocur G, Nadel L. Episodic memory and beyond: the hippocampus and neocortex in transformation. Annu Rev Psychol. (2016) 67:105–34. doi: 10.1146/annurev-psych-113011-143733
78. Moscovitch DA, Moscovitch M, Sheldon S. Neurocognitive model of schema-congruent and -incongruent learning in clinical disorders: application to social anxiety and beyond. Perspect Psychol Sci. (2023) 18:1412–35. doi: 10.1177/17456916221141351
79. Sinclair AH, Manalili GM, Brunec IK, Adcock RA, Barense MD. Prediction errors disrupt hippocampal representations and update episodic memories. Proc Natl Acad Sci U S A. (2021) 118. doi: 10.1073/pnas.2117625118
80. Yu LQ, Wilson RC, Nassar MR. Adaptive learning is structure learning in time. Neurosci Biobehav Rev. (2021) 128:270–81. doi: 10.1016/j.neubiorev.2021.06.024
81. Josselyn SA, Tonegawa S. Memory engrams: Recalling the past and imagining the future. Science. (2020) 367. doi: 10.1126/science.aaw4325
82. Summerfield C, de Lange FP. Expectation in perceptual decision making: neural and computational mechanisms. Nat Rev Neurosci. (2014) 15:745–56. doi: 10.1038/nrn3838
83. Teufel C, Fletcher PC. Forms of prediction in the nervous system. Nat Rev Neurosci. (2020) 21:231–42. doi: 10.1038/s41583-020-0275-5
84. de Sousa AF, Chowdhury A, Silva AJ. Dimensions and mechanisms of memory organization. Neuron. (2021) 109:2649–62. doi: 10.1016/j.neuron.2021.06.014
85. Tottenham N. Neural meaning making, prediction, and prefrontal-subcortical development following early adverse caregiving. Dev Psychopathol. (2020) 32:1563–78. doi: 10.1017/S0954579420001169
86. Brockman RN, Simpson S, Hayes C, van der Wijngaart R, Smout M. Research Supporting the Schema Therapy. In: Cambridge Guide to Schema Therapy (Cambridge Guides to the Psychological Therapies). Cambridge University Press. Kindle Edition, Cambridge, UK (2023). p. 16–38.
87. Gilbert P, Simos G. Compassion focused therapy: clinical practice and applications. Milton Park, Abingdon, Oxon; New York, NY: Taylor and Francis. Kindle Edition (2022).
88. Brockman RN, Simpson S, Hayes C, van der Wijngaart R, Smout M. Case Conceptualisation and Mode Mapping in Schema Therapy. In: Cambridge Guide to Schema Therapy (Cambridge Guides to the Psychological Therapies). Cambridge University Press. Kindle Edition, Cambridge, UK (2023). p. 86–95.
89. Teicher MH, Samson JA. Annual Research Review: Enduring neurobiological effects of childhood abuse and neglect. J Child Psychol Psychiatry. (2016) 57:241–66. doi: 10.1111/jcpp.2016.57.issue-3
90. Tomoda A, Nishitani S, Takiguchi S, Fujisawa TX, Sugiyama T, Teicher MH. The neurobiological effects of childhood maltreatment on brain structure, function, and attachment. Eur Arch Psychiatry Clin Neurosci (2024).
91. Dixon ML, Moodie CA, Goldin PR, Farb N, Heimberg RG, Zhang J, et al. Frontoparietal and default mode network contributions to self-referential processing in social anxiety disorder. Cognit Affect Behav Neurosci. (2022) 22:187–98. doi: 10.3758/s13415-021-00933-6
92. Kim H. A dual-subsystem model of the brain's default network: self-referential processing, memory retrieval processes, and autobiographical memory retrieval. Neuroimage. (2012) 61:966–77. doi: 10.1016/j.neuroimage.2012.03.025
93. Arioli M, Cattaneo Z, Ricciardi E, Canessa N. Overlapping and specific neural correlates for empathizing, affective mentalizing, and cognitive mentalizing: A coordinate-based meta-analytic study. Hum Brain Mapp. (2021) 42:4777–804. doi: 10.1002/hbm.v42.14
94. Silva RC, Maffioletti E, Gennarelli M, Baune BT, Minelli A. Biological correlates of early life stressful events in major depressive disorder. Psychoneuroendocrinology. (2021) 125:105103. doi: 10.1016/j.psyneuen.2020.105103
95. Duyser FA, Vrijsen JN, van Oort J, Collard RM, Schene AH, Tendolkar I, et al. Amygdala sensitivity for negative information as a neural marker for negative memory bias across psychiatric diagnoses. Psychiatry Res Neuroimag. (2022) 323:111481. doi: 10.1016/j.pscychresns.2022.111481
96. Samson JA, Newkirk TR, Teicher MH. Practitioner Review: Neurobiological consequences of childhood maltreatment - clinical and therapeutic implications for practitioners. J Child Psychol Psychiatry. (2024) 65:369–80. doi: 10.1111/jcpp.13883
97. Hanson JL, Williams AV, Bangasser DA, Pena CJ. Impact of early life stress on reward circuit function and regulation. Front Psychiatry. (2021) 12:744690. doi: 10.3389/fpsyt.2021.744690
98. Hein TC, Monk CS. Research Review: Neural response to threat in children, adolescents, and adults after child maltreatment - a quantitative meta-analysis. J Child Psychol Psychiatry. (2017) 58:222–30. doi: 10.1111/jcpp.2017.58.issue-3
99. Shany O, Gurevitch G, Gilam G, Dunsky N, Reznik Balter S, Greental A, et al. A corticostriatal pathway mediating self-efficacy enhancement. NPJ Ment Health Res. (2022) 1:6. doi: 10.1038/s44184-022-00006-7
100. Muller-Pinzler L, Czekalla N, Mayer AV, Schroder A, Stolz DS, Paulus FM, et al. Neurocomputational mechanisms of affected beliefs. Commun Biol. (2022) 5:1241. doi: 10.1038/s42003-022-04165-3
101. van Schie CC, van Harmelen AL, Hauber K, Boon A, Crone EA, Elzinga BM. The neural correlates of childhood maltreatment and the ability to understand mental states of others. Eur J Psychotraumatol. (2017) 8:1272788. doi: 10.1080/20008198.2016.1272788
102. Liu KY, Gould RL, Coulson MC, Ward EV, Howard RJ. Tests of pattern separation and pattern completion in humans-A systematic review. Hippocampus. (2016) 26:705–17. doi: 10.1002/hipo.22561
103. Lecei A, van Winkel R. Hippocampal pattern separation of emotional information determining risk or resilience in individuals exposed to childhood trauma: Linking exposure to neurodevelopmental alterations and threat anticipation. Neurosci Biobehav Rev. (2020) 108:160–70. doi: 10.1016/j.neubiorev.2019.11.010
104. Ghasemi M, Navidhamidi M, Rezaei F, Azizikia A, Mehranfard N. Anxiety and hippocampal neuronal activity: Relationship and potential mechanisms. Cognit Affect Behav Neurosci. (2022) 22:431–49. doi: 10.3758/s13415-021-00973-y
105. Markowitz JC, Milrod BL. Mood Disorders: Intrapsychic and Interpersonal Aspects. In: Kaplan & Sadock's concise textbook of clinical psychiatry, 4th ed, vol. xvi. Wolters Kluwer, Philadelphia (2017). p. 1008.
106. Dehghan Manshadi Z, Neshat-Doost HT, Jobson L. Cognitive factors as mediators of the relationship between childhood trauma and depression symptoms: the mediating roles of cognitive overgeneralisation, rumination, and social problem-solving. Eur J Psychotraumatol. (2024) 15:2320041. doi: 10.1080/20008066.2024.2320041
107. Rolls ET. The mechanisms for pattern completion and pattern separation in the hippocampus. Front Syst Neurosci. (2013) 7:74. doi: 10.3389/fnsys.2013.00074
108. Bakker A, Kirwan CB, Miller M, Stark CE. Pattern separation in the human hippocampal CA3 and dentate gyrus. Science. (2008) 319:1640–2. doi: 10.1126/science.1152882
109. Brenhouse HC. Points of divergence on a bumpy road: early development of brain and immune threat processing systems following postnatal adversity. Mol Psychiatry. (2023) 28:269–83. doi: 10.1038/s41380-022-01658-9
110. Vrijsen JN, van Amen CT, Koekkoek B, van Oostrom I, Schene AH, Tendolkar I. Childhood trauma and negative memory bias as shared risk factors for psychopathology and comorbidity in a naturalistic psychiatric patient sample. Brain Behav. (2017) 7:e00693. doi: 10.1002/brb3.2017.7.issue-6
111. Pechtel P, Pizzagalli DA. Effects of early life stress on cognitive and affective function: an integrated review of human literature. Psychopharmacol (Berl). (2011) 214:55–70. doi: 10.1007/s00213-010-2009-2
112. Disner SG, Shumake JD, Beevers CG. Self-referential schemas and attentional bias predict severity and naturalistic course of depression symptoms. Cognit Emot. (2017) 31:632–44. doi: 10.1080/02699931.2016.1146123
113. Wisco BE, Gilbert KE, Marroquin B. Maladaptive processing of maladaptive content: rumination as a mechanism linking cognitive biases to depressive symptoms. J Exp Psychopathol. (2014) 5:329–50. doi: 10.5127/jep.038213
114. Miao H, Zhong S, Liu X, Lai S, He J, Zhu Y, et al. Childhood trauma history is linked to abnormal brain metabolism of non-medicated adult patients with major depressive disorder. J Affect Disord. (2022) 302:101–9. doi: 10.1016/j.jad.2021.12.103
115. Belleau EL, Treadway MT, Pizzagalli DA. The impact of stress and major depressive disorder on hippocampal and medial prefrontal cortex morphology. Biol Psychiatry. (2019) 85:443–53. doi: 10.1016/j.biopsych.2018.09.031
116. Luo Q, Chen J, Li Y, Wu Z, Lin X, Yao J, et al. Aberrant brain connectivity is associated with childhood maltreatment in individuals with major depressive disorder. Brain Imaging Behav. (2022) 16:2021–36. doi: 10.1007/s11682-022-00672-3
117. Maydych V. The interplay between stress, inflammation, and emotional attention: relevance for depression. Front Neurosci. (2019) 13:384. doi: 10.3389/fnins.2019.00384
118. Pizzagalli DA. Toward a better understanding of the mechanisms and pathophysiology of anhedonia: are we ready for translation? Am J Psychiatry. (2022) 179:458–69. doi: 10.1176/appi.ajp.20220423
119. Linson A, Friston K. Reframing PTSD for computational psychiatry with the active inference framework. Cognit Neuropsych. (2019) 24:347–68. doi: 10.1080/13546805.2019.1665994
120. Paulus MP. Driven by pain, not gain: computational approaches to aversion-related decision making in psychiatry. Biol Psychiatry. (2020) 87:359–67. doi: 10.1016/j.biopsych.2019.08.025
121. Kinley I, Amlung M, Becker S. Pathologies of precision: A Bayesian account of goals, habits, and episodic foresight in addiction. Brain Cogn. (2022) 158:105843. doi: 10.1016/j.bandc.2022.105843
122. McCrory EJ, Gerin MI, Viding E. Annual Research Review: Childhood maltreatment, latent vulnerability and the shift to preventative psychiatry - the contribution of functional brain imaging. J Child Psychol Psychiatry. (2017) 58:338–57. doi: 10.1111/jcpp.2017.58.issue-4
123. Levy I, Schiller D. Neural computations of threat. Trends Cognit Sci. (2021) 25:151–71. doi: 10.1016/j.tics.2020.11.007
124. Huppert JD, Fradkin I, Cahill SP. CBT for Anxiety Disorders: Memory Reconsolidation Theory and Its Relationship to Cognitive, Emotional Processing, and Inhibitory Models 2020. In: Neuroscience of Enduring Change: Implications for Psychotherapy. (2020) Oxford University Press. Kindle Edition, New York, NY.
125. Bein O, Gasser C, Amer T, Maril A, Davachi L. Predictions transform memories: How expected versus unexpected events are integrated or separated in memory. Neurosci Biobehav Rev. (2023) 153:105368. doi: 10.1016/j.neubiorev.2023.105368
126. Iordanova MD, Yau JO, McDannald MA, Corbit LH. Neural substrates of appetitive and aversive prediction error. Neurosci Biobehav Rev. (2021) 123:337–51. doi: 10.1016/j.neubiorev.2020.10.029
127. Milton AL, Das RK, Merlo E. The challenge of memory destabilisation: From prediction error to prior expectations and biomarkers. Brain Res Bull. (2023) 194:100–4. doi: 10.1016/j.brainresbull.2023.01.010
128. Goldman R, Fredrick-Keniston A. Memory Reconsolidation as a Common Change Process. In: Lane RD, Lynn N, editors. Neuroscience of Enduring Change: Implications for Psychotherapyâ. Oxford University Press. Kindle Edition, New York, NY (2020). p. 328–59.
129. Leal SL, Yassa MA. Integrating new findings and examining clinical applications of pattern separation. Nat Neurosci. (2018) 21:163–73. doi: 10.1038/s41593-017-0065-1
130. Sharf J, Primavera LH, Diener MJ. Dropout and therapeutic alliance: a meta-analysis of adult individual psychotherapy. Psychother (Chic). (2010) 47:637–45. doi: 10.1037/a0021175
131. Baier AL, Kline AC, Feeny NC. Therapeutic alliance as a mediator of change: A systematic review and evaluation of research. Clin Psychol Rev. (2020) 82:101921. doi: 10.1016/j.cpr.2020.101921
132. Gong J, Chan RCK. Early maladaptive schemas as mediators between childhood maltreatment and later psychological distress among Chinese college students. Psychiatry Res. (2018) 259:493–500. doi: 10.1016/j.psychres.2017.11.019
133. Lassri D, Gewirtz-Meydan A. Self-compassion moderates the mediating effect of self-criticism in the link between childhood maltreatment and psychopathology. J Interpers Viol. (2022) 37:NP21699–NP722. doi: 10.1177/08862605211062994
134. Black RS, Curran D, Dyer KF. The impact of shame on the therapeutic alliance and intimate relationships. J Clin Psychol. (2013) 69:646–54. doi: 10.1002/jclp.21959
135. Howard R, Berry K, Haddock G. Therapeutic alliance in psychological therapy for posttraumatic stress disorder: A systematic review and meta-analysis. Clin Psychol Psychother. (2022) 29:373–99. doi: 10.1002/cpp.v29.2
136. Bernecker SL, Levy KN, Ellison WD. A meta-analysis of the relation between patient adult attachment style and the working alliance. Psychother Res. (2014) 24:12–24. doi: 10.1080/10503307.2013.809561
137. Zaslav MR. Shame-related states of mind in psychotherapy. J Psychother Pract Res. (1998) 7:154–66.
138. Farber BA. Patient self-disclosure: a review of the research. J Clin Psychol. (2003) 59:589–600. doi: 10.1002/jclp.10161
139. Brown B. Shame resilience theory: A grounded theory study on women and shame. Families Society. (2006) 87:43–52. doi: 10.1606/1044-3894.3483
140. Castonguay LG, Hill CE. Transformation in psychotherapy: corrective experiences across cognitive behavioral, humanistic, and psychodynamic approaches. 1st ed Vol. xiii. . Washington, DC: American Psychological Association (2012). p. 390.
141. Nakamura K, Iwakabe S. Corrective emotional experience in an integrative affect-focused therapy: Building a preliminary model using task analysis. Clin Psychol Psychother. (2018) 25:322–37. doi: 10.1002/cpp.v25.2
142. McLean L, Steindl SR, Bambling M. Compassion-focused therapy as an intervention for adult survivors of sexual abuse. J Child Sex Abus. (2018) 27:161–75. doi: 10.1080/10538712.2017.1390718
143. Lane RD, Smith R. Neuroscience of Enduring Change and Psychotherapy Summary, Conclusions, and Future Directions. In: Neuroscience of Enduring Change. New York, NY, USA: Oxford University Press. Kindle Edition (2020).
144. Alexander F, French TM. Psychoanalytic Therapy: Principles and Application. New York: Ronald Press (1946).
145. Gillath O, Karantzas GC, Romano D, Karantzas KM. Attachment security priming: A meta-analysis. Pers Soc Psychol Rev. (2022) 26:183–241. doi: 10.1177/10888683211054592
146. Farber BA, A.Metzger J. The Therapist as a Secure Base. In: Obegi JH, Berant E, editors. Attachment theory and research in clinical work with adults, vol. xii . Guilford Press, New York (2009). p. 529.
147. Barnett JE, Howe TR. Multiple maltreatment and adverse childhood experiences: exploring cumulative threats to attachment quality. Viol. Vict. (2021) 36:214–32. doi: 10.1891/VV-D-19-00158
148. Fonagy P, Allison E. The role of mentalizing and epistemic trust in the therapeutic relationship. Psychother (Chic). (2014) 51:372–80. doi: 10.1037/a0036505
149. Wang B, Peng X, Gao F, Zhang K, Zhang J, Wu L. Attachment security priming delayed negative information-related attentional disengagement among anxiously attached individuals: evidence from behavioral and functional MRI experiments. Front Psychol. (2022) 13:913805. doi: 10.3389/fpsyg.2022.913805
150. Norman L, Lawrence N, Iles A, Benattayallah A, Karl A. Attachment-security priming attenuates amygdala activation to social and linguistic threat. Soc Cognit Affect Neurosci. (2015) 10:832–9. doi: 10.1093/scan/nsu127
151. Lopresti AL. Cognitive behaviour therapy and inflammation: A systematic review of its relationship and the potential implications for the treatment of depression. Aust N Z J Psychiatry. (2017) 51:565–82. doi: 10.1177/0004867417701996
152. Rajhans P, Hans G, Kumar V, Chadda RK. Interpersonal psychotherapy for patients with mental disorders. Indian J Psychiatry. (2020) 62:S201–S12. doi: 10.4103/psychiatry.IndianJPsychiatry_771_19
153. Beck AT, John RA, Shaw BF, Gary E, DeRubeis Robert J, Hollon SD. Application of Behavioral Techniques. In: Cognitive Therapy of Depression. Guilford Publications. Kindle Edition, New York, NY (2024). p. 73–94.
154. Dindo L, Van Liew JR, Arch JJ. Acceptance and commitment therapy: A transdiagnostic behavioral intervention for mental health and medical conditions. Neurotherapeutics. (2017) 14:546–53. doi: 10.1007/s13311-017-0521-3
155. Jason B Luoma MGP. Shame, self-criticism, self-stigma, and compassion in Acceptance and Commitment Therapy. Curr Opin Psychol. (2015) 2:97–101. doi: 10.1016/j.copsyc.2014.12.016
157. Queirazza F, Fouragnan E, Steele JD, Cavanagh J, Philiastides MG. Neural correlates of weighted reward prediction error during reinforcement learning classify response to cognitive behavioral therapy in depression. Sci Adv. (2019) 5:eaav4962. doi: 10.1126/sciadv.aav4962
158. Beck AT, John RA, Shaw BF, Gary E, DeRubeis Robert J, Hollon SD. Integrating Cognitive Techniques. In: Cognitive Therapy of Depression. Guilford Publications. Kindle Edition, New York (2024). p. 95–119.
159. Brockman RN, Simpson S, Hayes C, van der Wijngaart R, Smout M. Intervention Strategies for Schema Healing 3 Experiential Techniques. In: Cambridge Guide to Schema Therapy (Cambridge Guides to the Psychological Therapies). Cambridge University Press. Kindle Edition, New York, NY (2023). p. 150–84.
160. Mendes I, Ribeiro AP, Angus L, Greenberg LS, Sousa I, Goncalves MM. Narrative change in emotion-focused psychotherapy: a study on the evolution of reflection and protest innovative moments. Psychother Res. (2011) 21:304–15. doi: 10.1080/10503307.2011.565489
161. Smout CA, Tang MF, Garrido MI, Mattingley JB. Attention promotes the neural encoding of prediction errors. PloS Biol. (2019) 17:e2006812. doi: 10.1371/journal.pbio.2006812
162. Hayes SC, Wilson KG, Gifford EV, Follette VM, Strosahl K. Experimental avoidance and behavioral disorders: a functional dimensional approach to diagnosis and treatment. J Consult Clin Psychol. (1996) 64:1152–68. doi: 10.1037/0022-006X.64.6.1152
163. Hoyt MA, Llave K, Wang AW, Darabos K, Diaz KG, Hoch M, et al. The utility of coping through emotional approach: A meta-analysis. Health Psychol. (2024) 43:397–417. doi: 10.1037/hea0001364
164. Greenberg LS. Emotion–focused therapy. Clin Psychol Psychother.: Int J Theory Prac. (2004) 11:3–16.
165. Sato W, Kochiyama T, Uono S, Sawada R, Yoshikawa S. Amygdala activity related to perceived social support. Sci Rep. (2020) 10:2951. doi: 10.1038/s41598-020-59758-x
Keywords: early maladaptive schemas (EMS), depression, predictive coding, child maltreatment (CM), psychotherapy
Citation: Ramamurthy G and Chen A (2025) Early maladaptive schemas from child maltreatment in depression and psychotherapeutic remediation: a predictive coding framework. Front. Psychiatry 16:1548601. doi: 10.3389/fpsyt.2025.1548601
Received: 19 December 2024; Accepted: 25 March 2025;
Published: 29 April 2025.
Edited by:
Asle Hoffart, Modum Bad Psychiatric Center, NorwayReviewed by:
Sooah Jang, Yonsei University, Republic of KoreaCopyright © 2025 Ramamurthy and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gita Ramamurthy, cmFtYW11cmdAdXBzdGF0ZS5lZHU=
 Gita Ramamurthy
Gita Ramamurthy Alan Chen2
Alan Chen2