- 1Department of Public Health, College of Medicine and Health Science, Mizan-Tepi University, Mizan-Aman, Ethiopia
- 2Department of Statistics, College of Natural and Computational Science, Mizan-Tepi University, Tepi, Ethiopia
- 3Faculty of Health Science, Health Research Institute, University of Canberra, Bruce, ACT, Australia
- 4Department of Psychiatry, College of Medicine and Health Science, Mizan-Tepi University, Mizan-Aman, Ethiopia
Background: Depression and HIV/AIDS are common mental health problems in people living in refugee camps under stressful conditions. When both conditions occur together in an already vulnerable population living in a deprived situation, they lead to severe health outcomes and complicate patient care. However, there is a shortage of data on the magnitude of depression and related factors among displaced populations living with HIV/AIDS in refugee camps. Therefore, this study aimed to assess the prevalence and factors associated with depression among HIV/AIDS patients living in the Okugu Refugee Camp, Ethiopia.
Methods: A health facility-based cross-sectional study was conducted among a sample of 382 adults living with HIV/AIDS who were on highly active antiretroviral therapy (HAART) at the Okugu Refugee Camp. Data were collected using a structured, interviewer-administered questionnaire and medical chart review based on a standard checklist. The Patient Health Questionnaire-9 (PHQ-9) was used to assess depression. Data were coded and entered into EpiData version 4.6.0.6 and analyzed using SPSS version 23. Descriptive statistics and bivariate and multivariable binary logistic regression analysis were performed. Variables with a p-value less than 0.05 in the final model were considered statistically significantly associated with depression.
Results: A total of 380 study participants took part in the study, with a response rate of 99.4%. More than half of the study participants (58.2%) were female, and the mean age of respondents was 32.71 (SD=7.42). The prevalence of depression among the displaced South Sudanese population living with HIV/AIDS in the Ethiopia Okugu Refugee Camp was 56.8% (95% CI: 51.8%–61.9%). Female sex (AOR = 2.6; 95% CI: 1.24, 6.28), opportunistic infections (AOR = 3.00; 95% CI: 1.75, 7.06), a CD4 count < 200 cells/mm3 (AOR = 2.40; 95% CI: 1.78, 8.23), and poor social support (AOR = 4.70; 95% CI: 1.98, 9.79) were significantly associated with depression among the refugees.
Conclusions: The magnitude of depression among refugees living with HIV/AIDS was significantly high. Therefore, regular screening of people living with HIV for depression through integration of mental health services with routine ART services and equipping healthcare providers with essential supplies to deal with the problems of refugees are crucial.
Introduction
According to the United Nations High Commissioner for Refugees (UNHCR) report, approximately 117.3 million people were forcibly displaced worldwide by the end of 2023, and approximately 75% of them were hosted in low- and middle-income countries, where health systems and other basic services are already overwhelmed (1). These forcibly displaced people are at a higher risk for HIV (2–4), mental health problems (5–7), and social and psychological problems (8, 9).
By the end of 2023, the World Health Organization (WHO) estimated 39.9 million people were living with HIV, and approximately 20.5 million and 1.4 million HIV cases were women and children, respectively. Moreover, the report showed that 26.0 million people living with HIV (PLHIV) in 2023 were from the African region, and the virus has claimed almost 42.3 million lives thus far (10). Studies have shown that the prevalence of HIV is higher among refugees and migrants than in host populations (2, 11, 12). Moreover, migrants experience delayed entry into HIV care and have poorer HIV-related outcomes when compared to native-born populations in their host country due to different barriers (4).
Migrants and refugees are exposed to various stressors that exacerbate pre-existing mental health conditions or contribute to the development of new ones. Depression is the most common mental disorder that affects migrants and refugees (5, 6). It is a mental health problem that presents with a depressed mood, loss of interest or pleasure, decreased energy, feelings of guilt, disturbed sleep or appetite, and poor concentration (13). Globally, it is estimated that 350 million individuals, or approximately 4.4% of the global population, suffer from depression (13, 14). The co-morbidity of depression is nearly twice as prevalent among people living with HIV in Africa as compared to the general population (15). In sub-Saharan countries, 1.57 million people living with HIV/AIDS, or approximately 50% to 60%, are affected by depression (16).
The co-occurrence of depression and HIV/AIDS could result in poor health outcomes due to obstacles to treatment and the deterioration of medical outcomes, including treatment resistance, increased morbidity, and higher mortality rates. Depression among PLHIV is also associated with poor health-related quality of life, poor adherence to antiretroviral therapy (ART), and unsatisfactory viral load suppression (17–19). In addition, depression contributes to loss of productivity and increases both the direct and indirect costs of medical care (20).
Ethiopia has committed to ending the HIV/AIDS epidemic by 2030 (21). To achieve this goal, the health system must adopt innovative strategies that address previously overlooked or neglected challenges (22). Therefore, identifying and treating depression has the potential to improve various HIV-related outcomes, including adherence to ART (23).
Being a forced migrant or refugee and living with HIV is an extremely stressful condition that can hugely contribute to the development or worsening of pre-existing mental health disorders, including depression. However, the burden of depression in migrants or refugees living with HIV and how being a forced migrant and living with HIV contributes to the development or exacerbation of pre-existing mental conditions are not well-documented globally. Furthermore, there is a lack of integrated care and routine mental health screening in refugee camps, leading to missed opportunities for health professionals to identify depression and other mental health problems among migrants or refugees living with HIV/AIDS. Therefore, this study aimed to assess the magnitude of depression and its associated factors among refugees living with HIV/AIDS in the Okugu Refugee Camp, Ethiopia.
Methods
Study setting and study design
A facility-based cross-sectional study design was conducted from 20 April to 30 May 2023, among the population displaced from South Sudan due to civil war and residing in the Okugu Refugee Camp, located in the Dimma District, Gambella Regional State, Western Ethiopia. The camp was established in 2013 following the outbreak of violence between confronting parties, which led to the displacement of a significant number of South Sudanese to neighboring countries, including Ethiopia. The majority of inhabitants of the Okugu Refugee Camp are from Jonglei State in South Sudan. Currently, approximately 13,645 people live in the camp, of whom 64% belong to the Anyuak ethnic group and the remaining 36% to the Murle ethnic group. According to the Okugu Refugee Camp Health Center report, 790 adolescents are living with HIV/AIDS, and receiving ART drugs from the health center. In total, 20 healthcare providers are working in the camp’s health center. The health center provides ART clinic services through a separate clinic specifically for people living with HIV/AIDS.
Population
The study was done among randomly selected adults aged 18 years or older who were receiving highly active ART (HAART) at the ART clinic of the Okugu Refugee Camp Health Center for HIV/AIDS treatment. Patients who were severely ill during data collection and unable to respond were excluded from the study.
Sample size and sampling procedure
The sample size was determined using Epi Info version 7.1 with the following parameters: statistical power=80%, confidence level =95%, a ratio of exposed to non-exposed 1:1, and an odds ratio of 1.89, which was obtained from a previous study (24). A 5% contingency was added for non-responses, resulting in a final sample size of 382.
The study participants were selected using a systematic sampling technique. The sample frame was generated using medical registration numbers obtained from the ART registry book of the Okugu Refugee Camp Health Centre, after excluding illegible registrations. The sampling interval was calculated by dividing the total population by the total sample size of 382, resulting in a kth interval of two. The first person was selected using a lottery method, and then patients were interviewed every two intervals until the required sample was achieved. The data collection was done by waiting for the sampled patients at the ART clinic when they came for different services.
Study variables
The dependent variable of the study was depression, categorized as either having depression or not having depression. The independent variables include sociodemographic characteristics (age, sex, marital status, religion, occupation, education status, and income), clinically related factors [opportunistic infections, WHO clinic stage, viral load, ART regimen, duration of illness, CD4 count, adherence to ART, and body mass index (BMI)], social support, perceived stigma, loss of relatives during the conflict, alcohol drinking, cigarette smoking, and khat chewing.
Data collection tool and procedure
Data were collected using a structured questionnaire through an interview-administered method and medical chart review using a data extraction checklist. The data collection tools were adapted from various similar studies conducted in different parts of the world and modified to fit the local context (25–27). The questionnaire was translated from English into the local languages, Agnuak and Murle, and then back-translated into English by different individuals to ensure consistency. The questionnaire included sections on sociodemographic characteristics, clinically related factors, psychosocial factors, and behavioral factors. Before the actual data collection, the tool was pre-tested on 5% of the sample size among patients who were not part of the main study, and modifications were made accordingly. The data collection was carried out by trained BSc nurses, and the process was supervised by MPH professionals.
Depression was measured using the Patient Health Questionnaire (PHQ-9). The PHQ-9 is a reliable and validated tool in Ethiopia and has demonstrated strong internal consistency (Cronbach’s alpha of 0.85) (25). It has nine items to which participants respond with four scales: not at all (0), several days (1), more than half the days (2), and nearly every day (3). Finally, the responses were summed, and participants were categorized as having depression if they scored 10 or more, otherwise, they were categorized as not having depression (25).
Social support was measured using the Oslo Social Support Scale (Oslo-3), which consists of three items. Based on the total score, respondents were categorized as having poor social support (score 3–8), moderate social support (score 9–11), or strong social support (score 12–14).
Adherence to HAART was determined based on the patient’s recall of their compliance with the prescribed doses over the days preceding the interview. Adherence was calculated by dividing the number of pills taken by the number of pills prescribed to be taken during that period. Then, based on the WHO guideline for measuring optimal treatment adherence, patients who had taken 95% or more of the prescribed pills were considered adherent, while those who had taken less than 95% were classified as non-adherent (28).
Perceived HIV-related stigma was measured using the HIV-Related Stigma Scale (HSS), which consists of eight items. Respondents who scored equal to or above the mean total score were considered to have perceived stigma, while those who scored below the mean were considered not to have perceived stigma (29).
Patients who had at least one of the following opportunistic infections or AIDS-defining cancers: herpes simplex, Salmonella infection, tuberculosis, candidiasis, toxoplasmosis, cytomegalovirus infection, histoplasmosis, cryptosporidiosis, and Kaposi’s sarcoma, either at baseline or after initiation of HAART, were considered to have opportunistic infections or cancers; otherwise, not (29). Alcohol drinkers were defined as those who consumed alcohol more than twice per week, and khat chewers were defined as participants who chewed khat more than twice per week (30).
Data processing and analysis
The completeness of the data was checked manually before being entered into EpiData software version 4.0.4.6 and subsequently exported to SPSS version 23 for analysis. Descriptive analysis such as frequencies and percentages were calculated. Bivariate binary logistic regression analysis was performed to assess the association of each independent factor with depression. Candidate variables with p-values less than 0.25 in the bivariate analysis were entered into multivariable binary logistic regressions to identify independent factors associated with depression. A backward likelihood ratio with a 0.1 probability of removal was used to develop the model. The goodness of fit of the final model was assessed using the Hosmer–Lemeshow test, and the result indicated a good model fit (p-value=0.789). Variables with a p-value of less than 0.05 in the final multivariable binary logistic regression model were considered statistically significant predictors of depression. Adjusted odds ratios (AORs) with 95% confidence intervals (CIs) were used to estimate the strength of the association. The results are presented in narrative descriptions, tables, and graphs.
Results
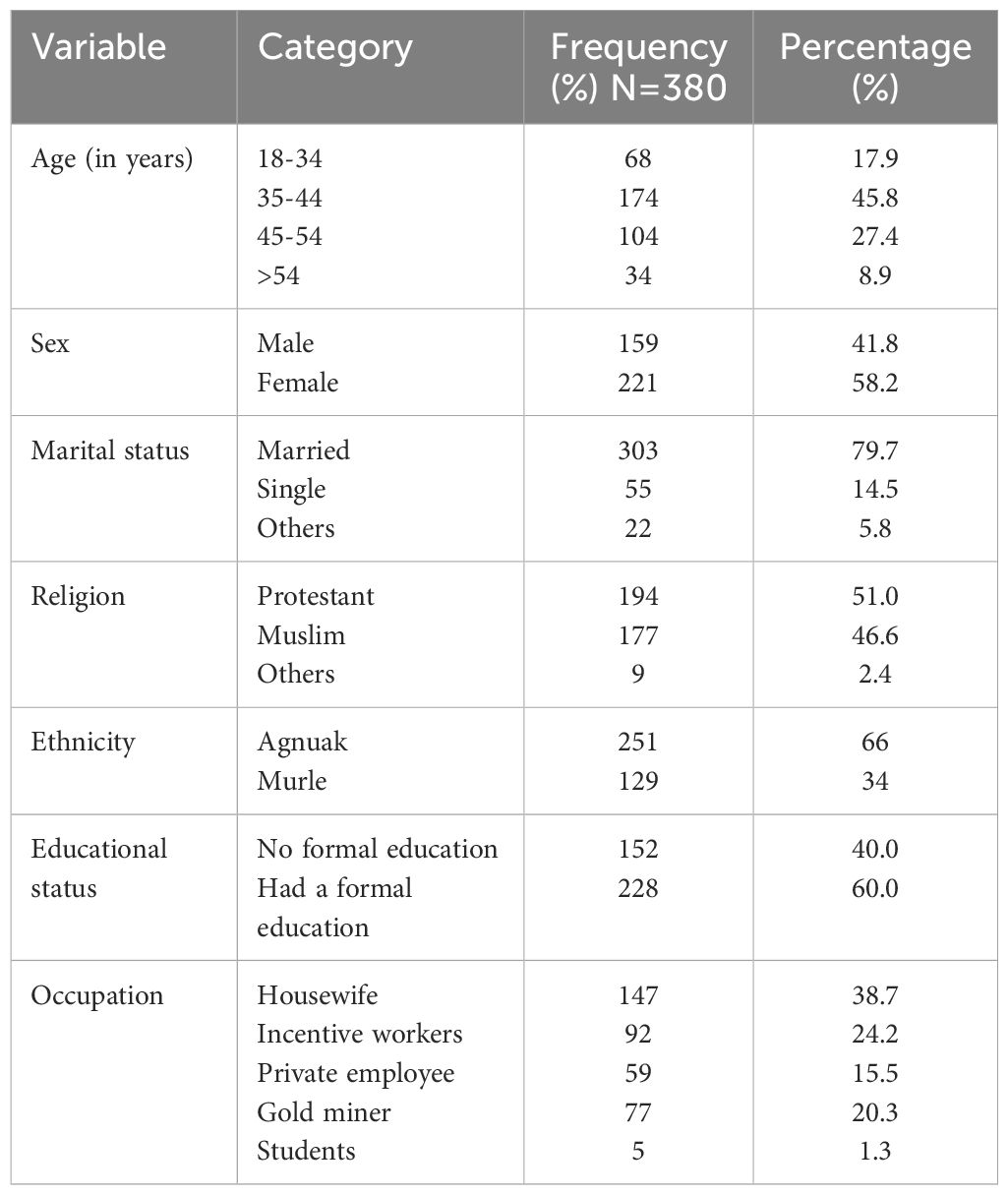
Sociodemographic characteristics
A total of 380 participants took part in the study, with a response rate of 99.4%. The mean age of the respondents was 32.71 with a standard deviation (SD) of 7.42. More than half of the respondents (58.2%) were female. Regarding religion, the majority (51.0%) were Protestant Christians followed by Muslims (46.6%) (Table 1).
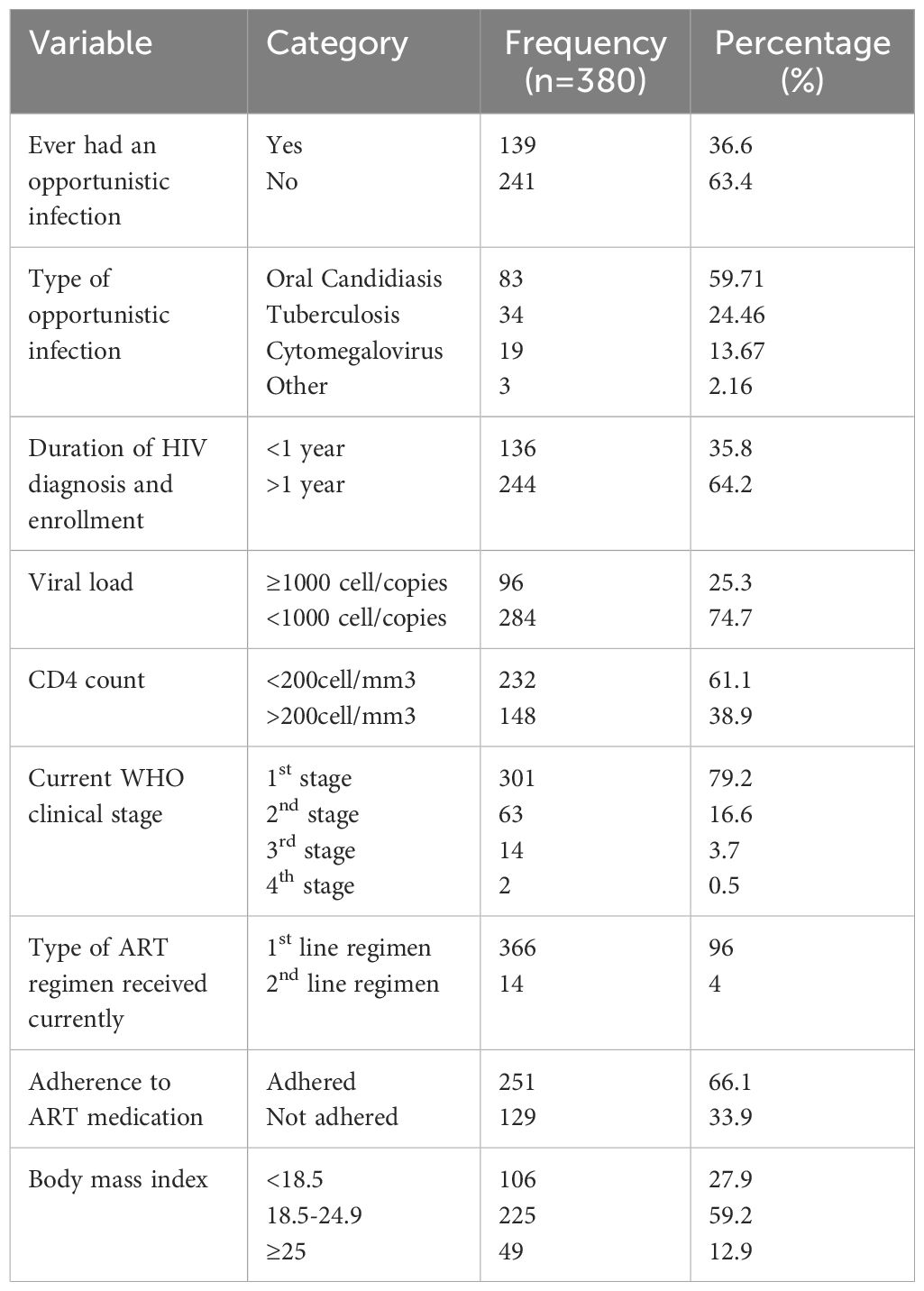
Clinical condition of the patients
The CD4 count of 61.1% of the study participants was below 200 cells/mm3, and 36.6% of the participants had experienced opportunistic infections. Furthermore, 25.3% of study participants had a viral load of greater than 1,000 copies/ml. Regarding the WHO clinical stage of HIV/AIDS, 27.19% were in stage III, and 9.69% were in stage IV. Finally, 251 participants (66.1%) adhered to their ART (Table 2).
Social support, perceived stigma, and behavior
According to the standard Oslo-3 item classification, 172 respondents (45.2%) had moderate social support. Nearly half (54.2%) of the participants had not experienced perceived stigma. Regarding substance use, 68.7% of respondents consumed alcohol, 26.6% chewed khat, and 69.7% smoked cigarettes (Table 3).
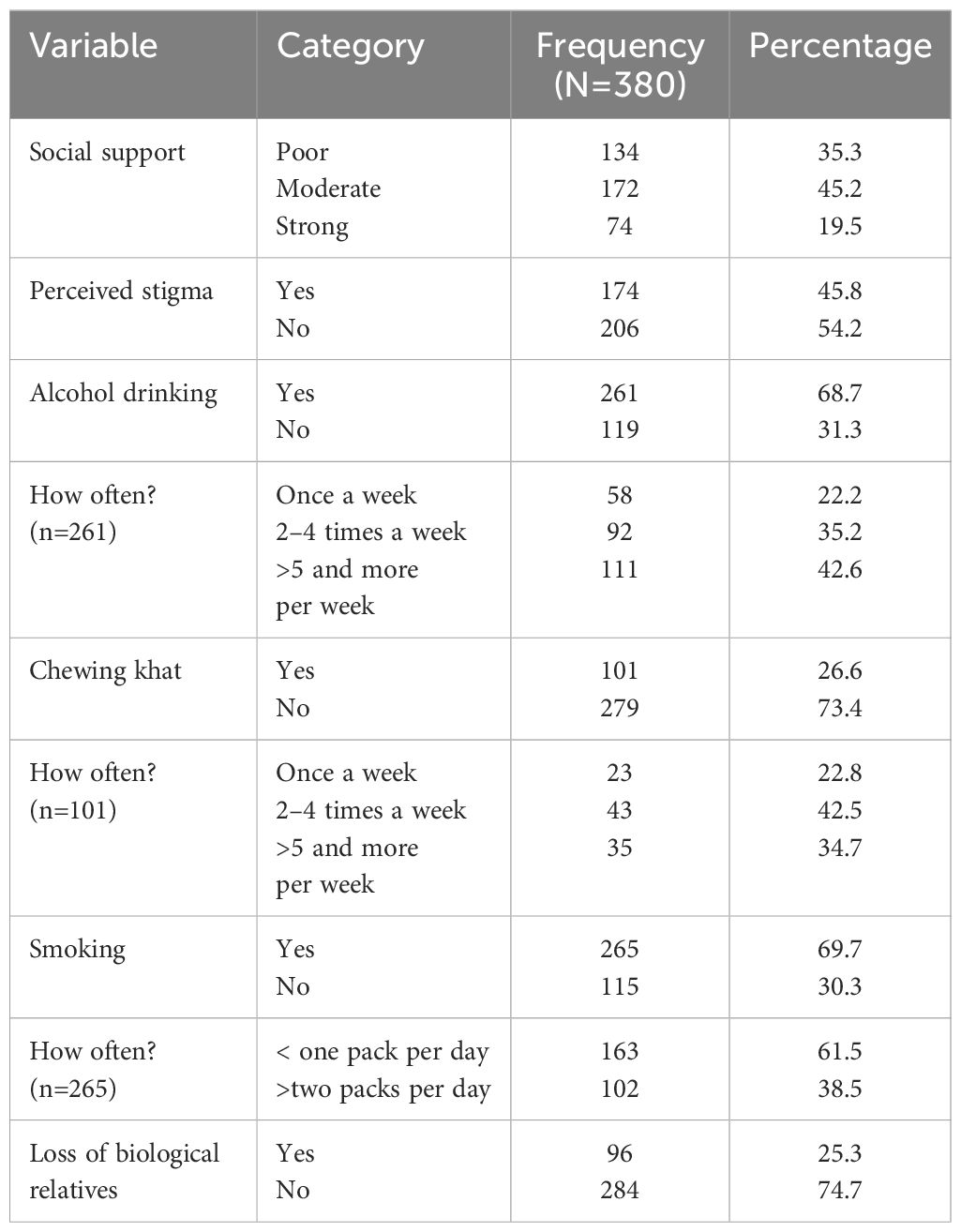
Table 3. Social support, perceived stigma, and behavior-related factors among adults on HAART at Okugu Refugee Camp Health Center, 2023.
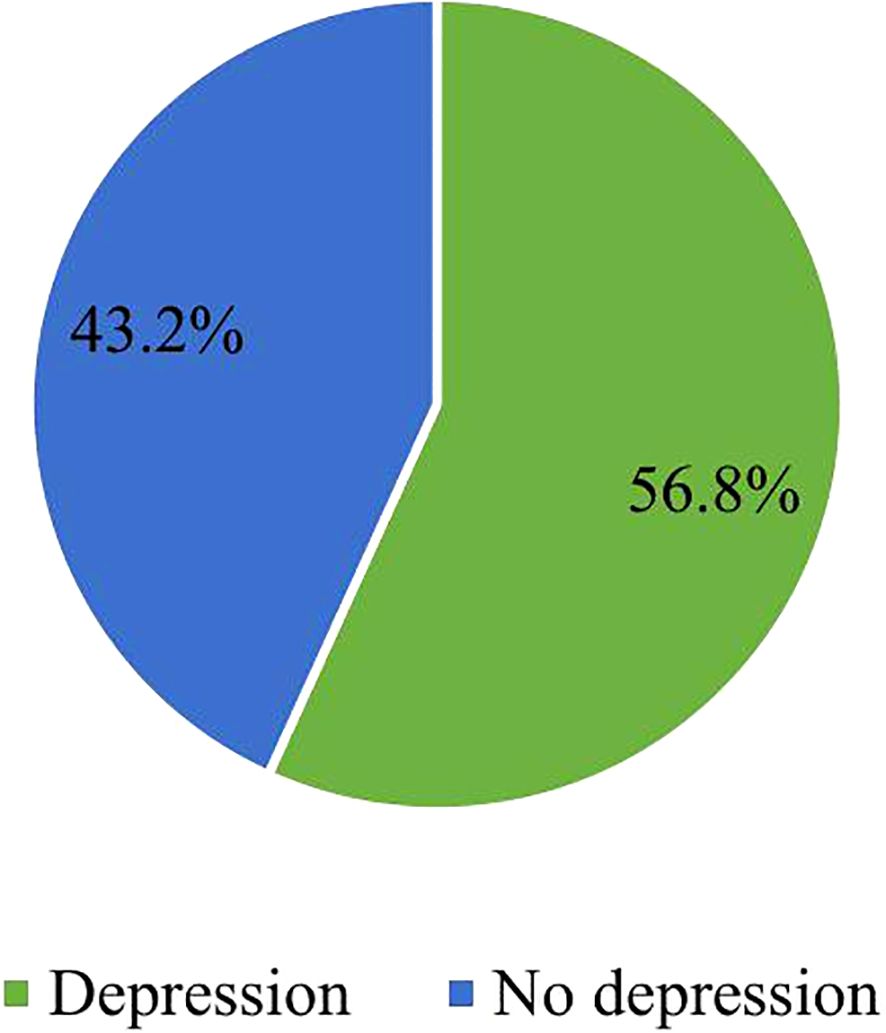
Prevalence of depression
The prevalence of depression among the refugees on HAART at Okugu Refugee Camp Health Center was 56.8% (95% CI: 51.8%–61.9%) (Figure 1).
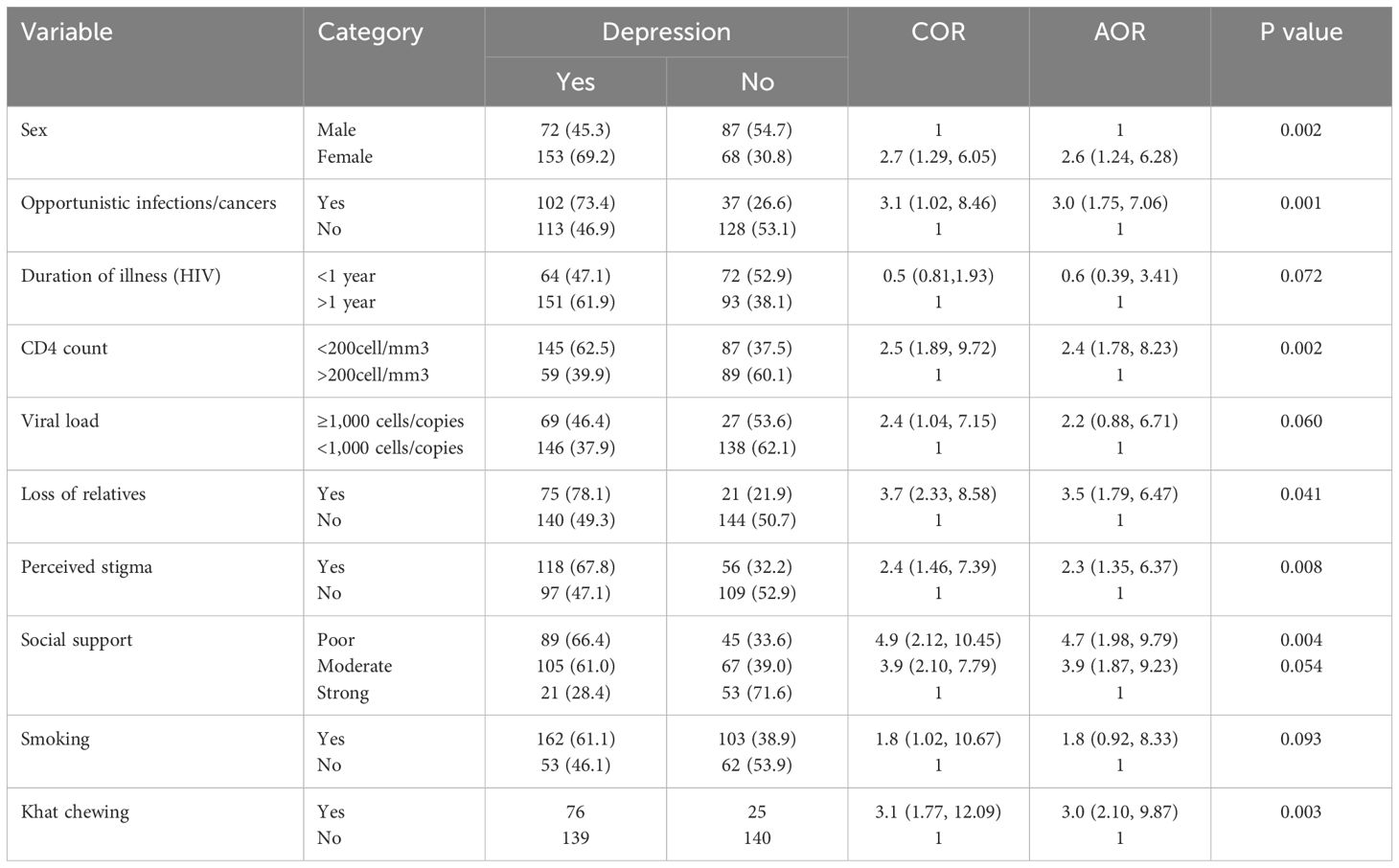
Factors associated with depression
In the bivariable analysis, variables including sex, presence of opportunistic infections or cancers, current CD4 count, viral load, duration since HIV diagnosis, loss of biological relatives, perceived stigma, social support, smoking, and khat chewing had p-values less than 0.25. These variables were included in the multivariable binary logistic regression to control for potential confounders and identify independent determinants of depression among adult HIV/AIDS patients living in the refugee camp. The multivariate binary logistic regression model revealed that sex, opportunistic infection, CD4 count, and level of social support were statistically significantly associated with depression in patients on HAART at Okugu Refugee Camp (p-value <0.05).
In this study, female patients had 2.6 times higher odds of having depression as compared to male patients (AOR=2.6: 95% CI; 1.24, 6.28). Moreover, patients with HIV/AIDS who had suffered opportunistic infections or cancers were three times more likely to experience depression compared to those who had not suffered opportunistic infections or cancers (AOR=3.0; 95% CI; 1.75, 7.06). In addition, individuals with a CD4 count of less than 200 cells/mm3 had 2.4 times higher odds of suffering depression than those with a CD4 count greater than or equal to 200 cells/mm3 (AOR=2.4: 95% CI, 1.78, 8.23). The refugees who had poor social support were 4.7 times more likely to be affected by depression as compared to those who had strong social support (AOR=4.7: 95% CI; 1.98, 9.79) (Table 4).
Discussion
This study aimed to assess the magnitude of depression and its associated factors among people living with HIV/AIDS on HAART in Okugu Refugee Camp. The study showed that sex, opportunistic infections or AIDS-defining cancers, CD4 count, and social support were significantly associated with depression. The prevalence of depression was 56.8% (95% CI: 51.8%–61.9%).
This finding is consistent with similar studies conducted in India (31) and North Central Nigeria (32) with 58.75% and 56.7%, respectively. However, it is higher than the prevalence reported in rural South Africa (42.4%) (33) and Malawi (18.9%) (34), and studies carried out in three areas of Ethiopia: Bale (44.9%), Hawassa (48.6%), and Harar (45.8%) (26, 29, 35). The higher prevalence observed in this study could be because the current study was conducted among a refugee population that may have suffered numerous stressors that cause or exacerbate mental health conditions, including depression. The refugees and migrants living with HIV are susceptible to a number of traumatic events including the loss of loved ones, lack of social support, stigma from the host community, rape and other sexual assaults, and limited access to mental health services at camps. Moreover, variations in measurement and sample size may also have accounted for the observed differences.
This study showed that female patients living with HIV were more likely to experience depression compared to their male counterparts. The finding is congruent with other studies conducted in South Africa (36); Khartoum, Sudan (37); and Debre Birhan, Ethiopia (38). Related to sex, there are unique biological factors, hormonal variation, and exposure to several psychosocial burdens that could make women more likely to suffer worry, stress, and depression (39). Moreover, women in refugee settings tend to be exposed to sexual harassment and violence in the household and in the broader community, which can further exacerbate their mental health challenges (40).
The odds of depression were significantly higher in individuals with a CD4 cell count below 200 cells/mm3 compared to those with 200 cells/mm3 or more. This finding is consistent with studies conducted in Malawi (34) and Ethiopia (38). One possible explanation is that depression can negatively impact the immune system by reducing immunoglobulin, lymphocyte activity, and natural killer cell function (41). Additionally, depression among patients with HIV is often associated with poor adherence to ART medication, which may lead to unsatisfactory viral load suppression and inadequate CD4 cell recovery (17–19).
We found that recent opportunistic infections or AIDS-defining cancers were associated with an increased occurrence of depression. This finding aligns with previous studies conducted in Addis Ababa and South Wollo, Ethiopia (22, 42). A possible explanation is that opportunistic infections worsen the quality of life among people living with HIV, which can consequently lead to poor mental health outcomes. These infections are often linked to hospitalization and diminished functional capacity, which may impact a patient’s psychosocial wellbeing.
This study indicates that individuals who had poor social support had a higher risk of depression. This finding is supported by a study conducted in the Mecha district, Northwest Ethiopia (43). Social interaction among family members and their ability to respond constructively to life transitions play a crucial role in reassuring individuals and maintaining social cohesion (44). People without families to disclose their problems to are unable to receive care and may have increased depressive symptoms (45). Moreover, when social connectedness is lost, the individual may feel isolated and experience heightened feelings of depression.
Conclusion
This study suggests that the prevalence of depression among refugees living with HIV in the Okugu Refugee Camp is high. Being female and having opportunistic infections or AIDS-defining cancers, a CD4 count of less than 200 cells/mm3, and poor social support were identified as significant predictors of depression among people living with HIV attending the ART clinic in the camp. To mitigate the effect of this prevalent mental health condition, healthcare providers should be trained to routinely screen for depression in people living with HIV, with particular attention paid to the identified risk factors. Additionally, integrating mental health services into existing HAART programs should be considered in refugee camps. Moreover, special emphasis should be given to strengthening social support systems for forcibly displaced individuals residing in camps.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board (IRB) of Mizan-Tepi University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. The animal study was approved by Institutional Review Board (IRB) of Mizan-Tepi University. The study was conducted in accordance with the local legislation and institutional requirements.
Author contributions
AA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. BH: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. ZA: Validation, Visualization, Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision. NS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. WS: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. GM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We would like to express our heartfelt gratitude to Mizan-Tepi University for supporting this research project. We also extend our thanks to the administration of the Okugu Refugee Camp health and ART clinic workers for their cooperation in providing us valuable information needed to undertake this research project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AOR, adjusted odds ratio; HAART, highly active antiretroviral therapy; ART, antiretroviral therapy; BMI, body mass index; CI, confidence interval; COR, crude odds ratio; HIV, human immunodeficiency virus; PLWH, people living with HIV; RRS, refugee and returnee services; WHO, World Health Organization; WMH, World Mental Health; UNHCR, United Nations High Commissioner for Refugees.
References
1. McAuliffe M and Oucho LA. World Migration Report 2024 [Internet]. Geneva, Switzerland: International Organization for Migration (2024). Available at: https://creativecommons.org/licenses/by-nc-nd/3.0/igo/legalcode (Accessed December, 2024).
2. Santoso D, Asfia SKBM, Mello MB, Baggaley RC, Johnson CC, Chow EPF, et al. HIV prevalence ratio of international migrants compared to their native-born counterparts: A systematic review and meta-analysis. eClinicalMedicine. (2022) 53:1–14. doi: 10.1016/j.eclinm.2022.101661
3. Suphanchaimat R, Sommanustweechai A, Khitdee C, Thaichinda C, Kantamaturapoj K, Leelahavarong P, et al. HIV/AIDS health care challenges for cross-country migrants in low- and middle-income countries: A scoping review. HIV/AIDS - Res Palliat Care. (2014) 6:19–38. doi: 10.2147/HIV.S56277
4. Arora AK, Ortiz-Paredes D, Engler K, Lessard D, Mate KKV, Rodriguez-Cruz A, et al. Barriers and facilitators affecting the HIV care cascade for migrant people living with HIV in organization for economic co-operation and development countries: A systematic mixed studies review. AIDS Patient Care STDS. (2021) 35:288–307. doi: 10.1089/apc.2021.0079
5. Marquez PV. Mental health among displaced people and refugees: making the case for action at the world bank group. Mental Health Among Displaced People and Refugees. Washington, DC: World Bank (2017). doi: 10.1596/25854
6. Morina N, Akhtar A, Barth J, and Schnyder U. Psychiatric disorders in refugees and internally displaced persons after forced displacement: A systematic review. Front Psychiatry. (2018) 9. doi: 10.3389/fpsyt.2018.00433
7. Grasser LR. Addressing mental health concerns in refugees and displaced populations: is enough being done? Risk Manag Healthc Policy. (2022) 15:909–22. doi: 10.2147/RMHP.S270233
8. Ciaramella M, Monacelli N, and Cocimano LCE. Promotion of resilience in migrants: A systematic review of study and psychosocial intervention. J Immigr Minor Heal. (2022) 24:1328–44. doi: 10.1007/s10903-021-01247-y
9. James P, Iyer A, and Webb TL. The impact of post-migration stressors on refugees’ emotional distress and health: A longitudinal analysis. Eur J Soc Psychol. (2019) 49:1359–67. doi: 10.1002/ejsp.v49.7
10. WHO. Epidemiological Fact Sheet: HIV statistics, globally and by WHO region, 2024. HIV Data and Statistics. (2024). Available online at: https://cdn.who.int/media/docs/default-source/hq-hiv-hepatitis-and-stis-library/j0294-who-hiv-epi-factsheet-v7.pdf?sfvrsn=5cbb3393_7 (Accessed December, 2024).
11. Schousboe C and Wejse C. Hiv prevalence in migrant groups based on country of origin: A systematic review on data obtained between 1993 and 2020. Sustain. (2021) 13:1–18. doi: 10.3390/su132111642
12. Panchenko S, Gabster A, Mayaud P, and Erausquin JT. Sexual health challenges in migrant, immigrant, and displaced populations 2022–2023. Curr Opin Infect Dis. (2024) 37(1):46–52. doi: 10.1097/QCO.0000000000000990
13. Marcus M, Yasamy MT, van Ommeren M, Chisholm D, and Saxena S. Depression, a global public health concern. PsycEXTRA Dataset. (2012). doi: 10.1037/e517532013-004
14. Pandey A and Galvani AP. The global burden of HIV and prospects for control. Lancet HIV. (2019) 6:e809–11. doi: 10.1016/S2352-3018(19)30230-9
15. Duko B, Toma A, Asnake S, and Abraham Y. Depression, anxiety and their correlates among patients with HIV in South Ethiopia: An institution-based cross-sectional study. Front Psychiatry. (2019) 10:1–7. doi: 10.3389/fpsyt.2019.00290
16. Lofgren SM, Bond DJ, Nakasujja N, and Boulware DR. Burden of depression in outpatient HIV-infected adults in sub-saharan africa; systematic review and meta-analysis. AIDS Behav. (2020) 24:1752–64. doi: 10.1007/s10461-019-02706-2
17. Tran BX, Dang AK, Truong NT, Ha GH, Nguyen HLT, Do HN, et al. Depression and quality of life among patients living with HIV/AIDS in the era of universal treatment access in Vietnam. Int J Environ Res Public Health. (2018) 15:1–14. doi: 10.3390/ijerph15122888
18. Logie CH, Okumu M, Malama K, Mwima S, Hakiza R, Kiera UM, et al. Examining the substance use, violence, and HIV and AIDS (SAVA) syndemic among urban refugee youth in Kampala, Uganda: Cross-sectional survey findings. BMJ Glob Heal. (2022) 7:e006583. doi: 10.1136/bmjgh-2021-006583
19. Heath K, Levi J, and Hill A. The Joint United Nations Programme on HIV/AIDS 95 – 95–95 targets : worldwide clinical and cost benefits of generic manufacture. AIDS. (2021) 35(Suppl 2):S197–S203. doi: 10.1097/QAD.0000000000002983
20. World Health Organization and Columbia University. Group Interpersonal Therapy (IPT) for Depression (WHO generic field-trial version 1.0) Geneva: WHO (2016).
21. Assefa Y, Gilks CF, Dean J, Tekle B, Lera M, Balcha TT, et al. Towards achieving the fast-track targets and ending the epidemic of HIV/AIDS in Ethiopia: Successes and challenges. Int J Infect Dis. (2019) 78:57–64. doi: 10.1016/j.ijid.2018.10.022
22. Tesfaw G, Ayano G, Awoke T, Assefa D, Birhanu Z, Miheretie G, et al. Prevalence and correlates of depression and anxiety among patients with HIV on-follow up at Alert Hospital, Addis Ababa, Ethiopia. BMC Psychiatry. (2016) 16:368. doi: 10.1186/s12888-016-1037-9
23. Gloria Kang GJ, Ewing-Nelson SR, Mackey L, Schlitt JT, Marathe A, and Abbas KM SS. Effects of depression alleviation on ART adherence and HIV clinic attendance in Uganda, and the mediating roles of self- efficacy and motivation. AIDS Behav. (2017) 21:1655–64. doi: 10.1007/s10461-016-1500-0
24. Beyamo A, Bashe T, Facha W, and Moshago T. Depression and associated factors among adult HIV/AIDS patients attending antiretroviral therapy at Wolaita Sodo University teaching and referral hospital, Southern Ethiopia. HIV/AIDS - Research and Palliative Care (2020), 707–15. doi: 10.2147/HIV.S278794
25. Gelaye B, Williams MA, Lemma S, Deyessa N, Bahretibeb Y, Shibre T, et al. Validity of the Patient Health Questionnaire-9 for Depression Screening and Diagnosis in East Africa. Psychiatry Res. (2013) 210(2):653–61. doi: 10.1016/j.psychres.2013.07.01
26. Duko B, Geja E, Zewude M, and Mekonen S. Prevalence and associated factors of depression among patients with HIV/AIDS in Hawassa, Ethiopia, cross-sectional study. Ann Gen Psychiatry. (2018) 17:4–9. doi: 10.1186/s12991-018-0215-1
27. Abadiga M. Depression and its associated factors among HIV/AIDS patients attending ART clinics at Gimbi General hospital, West Ethiopia, 2018. BMC Res Notes. (2019) 12:1–8. doi: 10.1186/s13104-019-4553-0
28. Kemigisha E, Zanoni B, Bruce K, Menjivar R, Kadengye D, Atwine D, et al. Prevalence of depressive symptoms and associated factors among adolescents living with HIV/AIDS in South Western Uganda. AIDS Care. (2019) 31:1297–303. doi: 10.1080/09540121.2019.1566511
29. Desta F, Tasew A, Tekalegn Y, Zenbaba D, Sahiledengle B, Assefa T, et al. Prevalence of depression and associated factors among people living with HIV/AIDS in public hospitals of Southeast Ethiopia. BMC Psychiatry. (2022) 22:1–10. doi: 10.1186/s12888-022-04205-6
30. Kibret GD and Salilih SZ. Prevalence and associated factors of depression among HIV infected patients in Debre Markos town northwest Ethiopia. Int J Emerg Ment Health. (2015) 17:714–6.
31. Bhatia MS and Munjal S. Prevalence of depression in people living with HIV/AIDS undergoing ART and factors associated with it. J Clin Diagn Res. (2014) 8:WC01–4. doi: 10.7860/JCDR/2014/7725.4927
32. Shittu RO, Issa BA, Olanrewaju GT, Mahmoud AO, Odeigah LO, Salami AK, et al. Prevalence and correlates of depressive disorders among people living with HIV/AIDS, in north central Nigeria. J AIDS Clin Res. (2013) 4:1–7. doi: 10.4172/2155-6113.1000251
33. Pappin M, Wouters E, and Booysen FLR. Anxiety and depression amongst patients enrolled in a public sector antiretroviral treatment programme in South Africa: A cross-sectional study. BMC Public Health. (2012) 12:244. doi: 10.1186/1471-2458-12-244
34. Kim MH, Mazenga AC, Yu X, Devandra A, Nguyen C, Ahmed S, et al. Factors associated with depression among adolescents living with HIV in Malawi. BMC Psychiatry. (2015) 15:1–12. doi: 10.1186/s12888-015-0649-9
35. Bezatu Mengistie MM. Prevalence of Depression and Associated Factors among HIV Patients Seeking Treatments in ART Clinics at Harar Town, Eastern Ethiopia. J AIDS Clin Res. (2015) 06:1–6. doi: 10.4172/2155-6113.1000474
36. Nyirenda M, Chatterji S, Rochat T, Mutevedzi P, and Newell ML. Prevalence and correlates of depression among HIV-infected and -affected older people in rural South Africa. J Affect Disord. (2013) 151:31–8. doi: 10.1016/j.jad.2013.05.005
37. Elbadawi A and Mirghani H. Depression among hiv/aids Sudanese patients: A cross-sectional analytic study. Pan Afr Med J. (2017) 26:1–8. doi: 10.11604/pamj.2017.26.43.10919
38. Asmare Eshetu D and Meseret S. Prevalence of Depression and Associated Factors among HIV/AIDS Patients Attending ART Clinic at Debrebirhan Referral Hospital, North Showa, Amhara Region, Ethiopia. Clin Psychiatry. (2015) 1:1–7. doi: 10.21767/2471-9854.100003
39. Albert PR. Why is depression more prevalent in women? J Psychiatry neuroscience : Jpn Canada;. (2015) 40:219–21. doi: 10.1503/jpn.150205
40. Noubani A, Diaconu K, Ghandour L, El Koussa M, Loffreda G, and Saleh S. A community-based system dynamics approach for understanding factors affecting mental Health and Health seeking behaviors in Beirut and Beqaa regions of Lebanon. Global Health. (2020) 16:1–13. doi: 10.1186/s12992-020-00556-5
41. Leonard BE. The concept of depression as a dysfunction of the immune system. Curr Immunol Rev. (2010) 6:205–12. doi: 10.2174/157339510791823835
42. Seid S, Abdu O, Mitiku M, and Tamirat KS. Prevalence of depression and associated factors among HIV/AIDS patients attending antiretroviral therapy clinic at Dessie referral hospital, South Wollo, Ethiopia. Int J Ment Health Syst. (2020) 14:1–8. doi: 10.1186/s13033-020-00389-0
43. Mekonen T, Belete H, and Fekadu W. Depressive symptoms among people with HIV/AIDS in Northwest Ethiopia: Comparative study. BMJ Open. (2021) 11:1–7. doi: 10.1136/bmjopen-2021-048931
44. Wouters E, Masquillier C, and le Roux Booysen F. The importance of the family: A longitudinal study of the predictors of depression in HIV patients in South Africa. AIDS Behav. (2016) 20:1591–602. doi: 10.1007/s10461-016-1294-0
Keywords: depression, mental health, refugees, refugee camp, HIV-AIDS, HAART
Citation: Asefa A, Hirpesa B, Asaye Z, Shifera N, Sheferaw WE and Mesafint G (2025) Prevalence of depression and associated factors among HIV/AIDS Patients on HAART in Okugu Refugee Camp, Gambella, Ethiopia. Front. Psychiatry 16:1550488. doi: 10.3389/fpsyt.2025.1550488
Received: 23 December 2024; Accepted: 22 April 2025;
Published: 23 May 2025.
Edited by:
Felix Khuluza, Kamuzu University of Health Sciences (formerly College of Medicine-University of Malawi), MalawiReviewed by:
Addisu Girma, Dr.Bogalech Gebre Memorial General Hospital, EthiopiaKim Madundo, KCMC University, Tanzania
Copyright © 2025 Asefa, Hirpesa, Asaye, Shifera, Sheferaw and Mesafint. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Adane Asefa, YWRhbmU3NzlAZ21haWwuY29t
 Adane Asefa
Adane Asefa Belay Hirpesa1
Belay Hirpesa1 Zufan Asaye
Zufan Asaye Nigusie Shifera
Nigusie Shifera Wegayehu Enbeyle Sheferaw
Wegayehu Enbeyle Sheferaw Gebremeskel Mesafint
Gebremeskel Mesafint