- 1Department of Child and Adolescent Psychiatry, Medical University of Warsaw, Warsaw, Poland
- 2Department of Paediatrics, Medical University of Warsaw, Warsaw, Poland
- 3Faculty of Medicine, Medical University of Warsaw, Warsaw, Poland
Parents of children with autism often experience unique challenges that can impact their emotional wellbeing. The aim of this study was to validate the Polish adaptation of the Quality of Life in Autism Survey (QoLA) and to examine the factors influencing quality of life (QoL) among parents of children with autism spectrum disorder (ASD). The survey was administered to 372 participants, predominantly mothers, and assessed QoL using the QoLA-A and QoLA-B scales alongside established tools such as the Beck Depression Inventory and WHOQOL-BREF. Results showed high reliability for the QoLA-A scale, supported by Cronbach's alpha (0.93) and omega coefficients, and confirmed an 8-factor model consistent with Schalock's domains of QoL. The scale showed strong correlations with psychological health, social relationships and environmental factors, validating its criterion and construct reliability. Conversely, QoLA-B showed limitations, capturing only five dimensions and explaining less than 50% of the variance. Important predictors of parental QoL included employment status, material well-being and depressive symptoms, with externalising behaviours in children having a significant negative influence. Intellectual and communication disabilities, although a significant challenge, were not strongly correlated with parental QoL. The findings highlight the need to address socio-economic and mental health support for caregivers, with an emphasis on tailored interventions that enhance parental wellbeing, rather than exclusively targeting child-specific therapies. This comprehensive validation highlights the utility of the QoLA-A and the nuanced factors that influence caregiver QoL.
1 Introduction
1.1 Autism and parental quality of life
Autism spectrum disorder (ASD) is a complex neurodevelopmental condition. It is characterized by challenges with social interaction, and communication, as well as the presence of restricted, repetitive patterns of behaviour and interests (1). The prevalence of ASD has increased over time and currently affects approximately 1 in 36 children worldwide by the age of 8 years, with boys being significantly more affected than girls (2). Autism affects not only the individual, but also places significant challenges on their families and caregivers. A review of the literature on the quality of life of parents of children diagnosed with ASD reveals a consistent trend of lower satisfaction compared to parents of typically developing children (3). According to a recent meta-analysis involving 27,942 individuals, siblings of those diagnosed with ASD are more likely to experience adverse outcomes compared to siblings of individuals without ASD or with other disabilities (4). These outcomes include a higher likelihood of internalizing behavioural problems, limitations in social functioning, and symptoms of anxiety and depression compared to siblings of children with Down syndrome or those without disabilities.
In addition to reporting a lower quality of life in general, parents of children with ASD face specific challenges and elevated levels of stress compared to parents of typically developing children or those with other disabilities (5). These challenges include difficulties in accessing appropriate services and resources, managing problematic behaviours, navigating social interactions and relationships, and coping with the daily demands of parenting a child with ASD. Some studies have suggested that the stress experienced by these parents can negatively impact their overall mental and physical health (6). It is therefore unsurprising that viewing the family as an integrated unit and addressing their needs alongside those of the child can significantly enhance the effectiveness of therapy and improve overall family functioning (7).
1.2 Quality of life of parents of autistic children in Poland
Recent studies conducted in Poland confirm that parents of children with autism spectrum disorder report significantly lower quality of life across multiple domains. For example, research comparing parents of children with ASD to parents of neurotypical children revealed substantial differences in general health, mental health, social functioning, and vitality, with the ASD group scoring consistently lower (8). Similar findings were observed in studies analysing family functioning and stress coping strategies, which demonstrated reduced psychosocial well-being among parents of children with ASD (9). Moreover, a cross-cultural study comparing parents from Poland, Belarus, and France revealed that Polish parents reported the lowest overall quality of life according to the WHOQOL-BREF scale (10). These findings highlight the importance of using culturally sensitive and linguistically adapted tools for assessing parental quality of life in families affected by autism.
1.3 Measurement of quality of life
As crucial as it is, the concept of quality of life is often difficult to measure in a specific and consistent manner. Some authors even argue that it is not possible to measure comprehensively (11). However, researchers looking for useful models to provide effective care for individuals with ASD and their families are well aware that these must go beyond a focus on ASD symptomatology. Examples include Family Quality of Life (FQOL) (12–15) and ABCX (16–18), both of which consider parental quality of life as an integral component of treatment planning. Regarding the quality of life, researchers emphasize the importance of factors such as happiness, meaning, self-esteem, physical and mental health, social relationships, and goal attainment (19). There are various dimensions within the quality of life, ranging from four to eight or even more (20). In recent years, Shalock’s 8-factor framework (21), which includes domains such as self-determination, social inclusion, interpersonal relationships, rights, material well-being, emotional well-being, physical well-being, and personal development, has gained increasing prominence in studies of QoL among people with intellectual disabilities (20, 22–24), people with visual impairments (25), residents of group homes (26) and other populations.
Of the many quality-of-life assessments available worldwide, only a few are specifically tailored to individuals with ASD or their caregivers. Even fewer have been translated into Polish and psychometrically validated. The currently available translated questionnaires do not focus on individuals with ASD and fail to address the core symptoms of ASD or the challenges experienced by their families. Therefore, there is a significant need for a well-validated Polish-language tool specifically designed to assess the quality of life of families caring for patients with ASD.
1.4 Quality of life in autism questionnaire
The Quality of Life in Autism Questionnaire was developed to assess the quality of life experienced by parents of children diagnosed with ASD, aged 2 to 18 (27). It consists of two sections, comprising 48 items, and utilizes a Likert scale for responses. Part A includes 28 items evaluating the parent’s own quality of life and emotional well-being, while Part B contains 20 items assessing the degree of difficulty the parent experiences with specific autism-related behaviours in their child. Although both sections contribute to a comprehensive understanding of the parental experience, they address distinct psychological constructs related to different individuals (parent vs. child) and are therefore typically analysed separately. This questionnaire has shown good psychometric properties and has been validated in several languages, making it a reliable tool for assessing the impact of ASD on parents’ quality of life.
1.5 Aims of this study
The first validation was conducted for the English version. This research aims to adapt the original QoLA questionnaire to Polish conditions and to validate the new adaptation using a sample of parents of children diagnosed with ASD. In addition to examining the factorial structure and reliability of the instrument, we seek to assess its concurrent and criterion validity. Based on the existing literature, we formulated several hypotheses. First, we expected a strong negative correlation between parental quality of life (QoLA-A scores) and depressive symptoms, as measured by the Beck Depression Inventory. Second, we hypothesized that quality of life would be lower among single, unemployed parents of children with disabilities who are nonverbal. Finally, we anticipated that lower QoLA-A scores would correlate with reduced material well-being.
2 Materials and methods
2.1 Translation procedure
The study was approved by the Bioethics Committee of the Medical University of Warsaw (approval number AKBE/232/2023). In accordance with the World Health Organization (WHO) guidelines for the translation and adaptation of psychometric instruments (28), two independent researchers performed the initial forward translation of the questionnaire. Both were native Polish speakers with proficiency in English and familiarity with the relevant terminology in the field. Subsequently, a discussion of the translations was held among the three authors of this manuscript (ŁK, MK, and JŁ), resulting in a single, final version of the questionnaire. In the third step, two translators, both native English speakers fluent in Polish, back-translated the instrument into English. ŁK, MK, and JŁ then reviewed the back translations to identify discrepancies between them and the original tool, leading to the agreement on the final Polish version of the questionnaire.
2.2 Participants
Parents of children with ASD, aged 2 to 18 years, participated in the survey. The questionnaire was distributed online through websites and social media platforms that gathered a community of families of children with ASD.
2.3 The instrument
The Quality of Life in Autism questionnaire consists of two parts (27). Part A contains 28 questions that assess a parent’s quality of life, with responses recorded on a 5-point Likert scale. Part B lists 20 typical behaviours observed in children with ASD and evaluates how difficult these behaviours are for the parent, using a 5-point Likert scale. The total score of the QoLA questionnaire ranges from 48 to 240 and can also be analysed separately for parts A and B.
To assess the psychometric properties of the QoLA-A scale, we included two additional standardized measures. The Beck Depression Inventory (BDI) was administered to parents to assess depressive symptoms, which are known to impact perceived quality of life. This allowed us to examine the criterion validity of the QoLA-A. In addition, we used the WHOQOL-BREF questionnaire to assess convergent validity, by comparing QoLA-A scores with a general, widely validated measure of quality of life. These instruments were selected to ensure that the scale demonstrates validity both in relation to established psychological constructs and to broader well-being outcomes.
The WHOQOL-BREF, a shortened version of the WHOQOL-100 questionnaire, was developed to assess quality of life (29). It consists of 26 questions covering four domains: physical health, psychological health, social relationships, and environment. Responses are given on a 5-point Likert scale. Calculated and converted scores in each domain range from 4 to 20 points.
The Beck Depression Inventory (BDI) is a self-report questionnaire used to assess the severity of depressive symptoms in adults (30). It consists of 21 closed-ended questions covering hopelessness, irritability, guilt, lack of satisfaction, and somatic symptoms. Responses are scored on a scale from 0 to 3, with higher scores indicating more severe depressive symptoms.
Both measures have been previously translated into Polish and validated. All instruments were completed by the parents; no questionnaires were administered to the children.
2.4 Statistical analysis
R, was used to statistically analyze the collected data. Descriptive statistics were used to summarise the demographic characteristics and responses of the participants. In addition, both exploratory factor analyses (EFA) and confirmatory factor analyses (CFA) were conducted using the R psych and lavaan packages to assess the construct validity of the QoLA questionnaire. Cronbach’s alpha coefficients were calculated to assess the internal consistency of QoLA-A and QoLA-B (31). However, as we assumed a multidimensional structure of the inventories, omega h and omega total statistics were also calculated, as they are more appropriate for multidimensional questionnaires (32). To further investigate the nature of the variables influencing the quality of life, structured equation modeling was performed using the R lavaan package. Exploratory factor analysis with Promax rotation was used to examine the structural dimensions of QoLA. Four different methods were used to determine the number of factors: eigenvalues greater than 1 (resulting in 7 factors), Cattell’s scree plot (6 factors), variances accounting for 80% of the variance (13 factors), and the minimum number of factors required for a non-significant chi-square test of model fit (10 factors). In line with Shallock’s model of quality of life, which suggests 8 domains, we aimed for an 8-factor model accounting for 67% of the variance. Items entering the 8 factors are compared against their corresponding Shallock’s domains in Table 1.
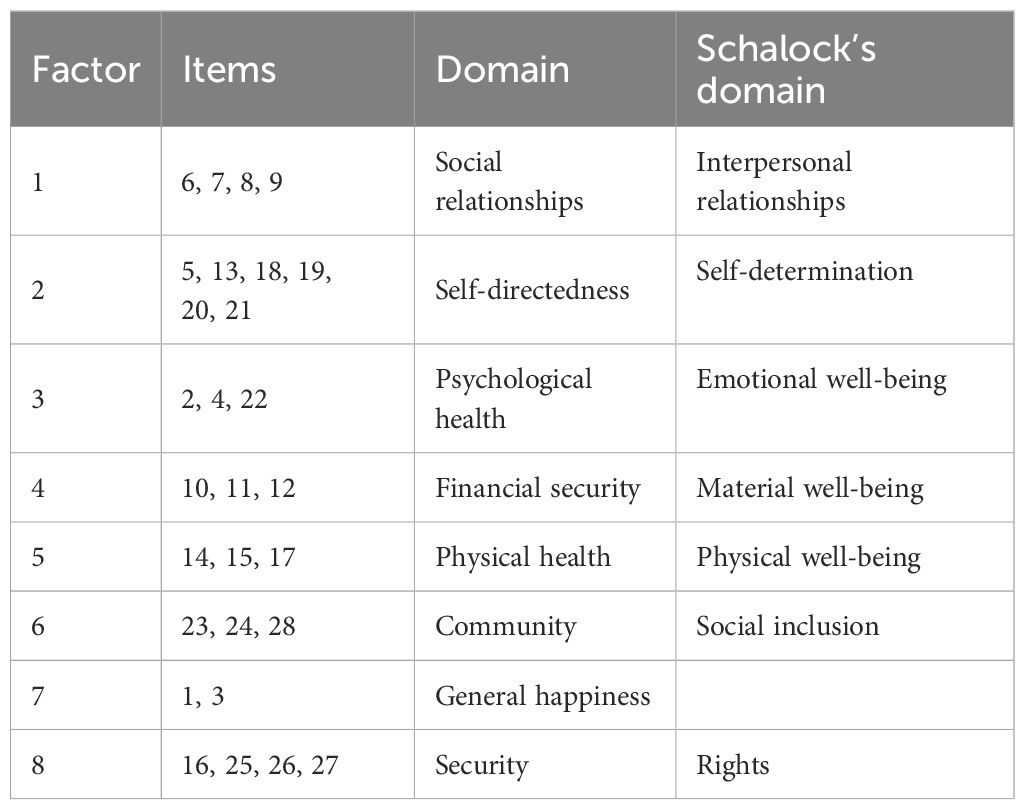
Table 1. Comparison of our CFA 8-factor structure of the QoLA-A and Schalock’s 8 domains of quality of life.
3 Results
3.1 Sociodemographic characteristics of the sample
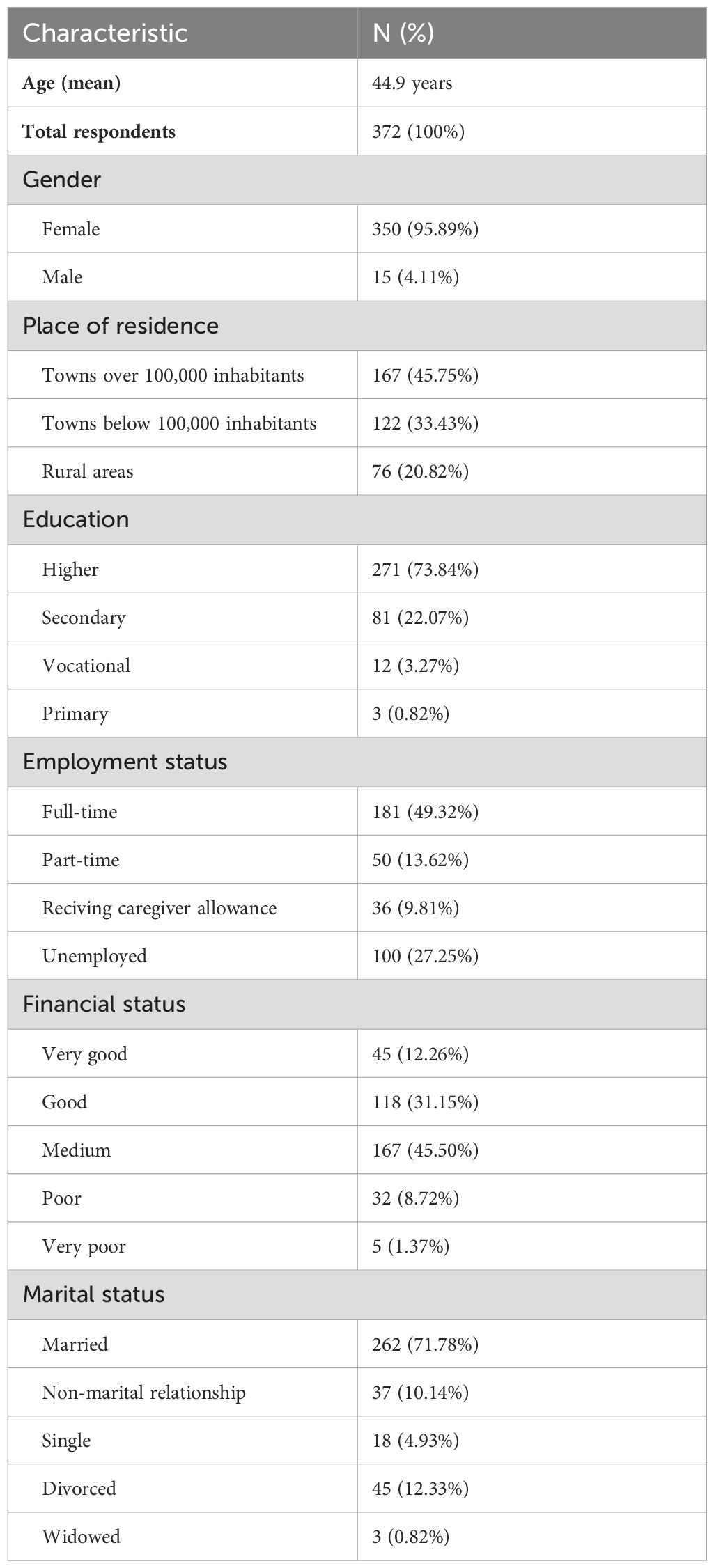
The study sample consisted of 372 respondents, predominantly mothers, with an average age of 44.9 years. Table 2 below summarizes key demographic and socioeconomic characteristics, including place of residence, education level, employment status, financial situation, and marital status.
Descriptive analyses were conducted to characterize the study population in terms of demographic, clinical, and psychological variables. Most children in the sample were boys, and the average age was approximately 10 years. Nearly half of the respondents had two children. A large majority of the children communicated using words, while approximately one in five were reported to have an intellectual disability. More than half of the responding parents had received an autism spectrum disorder (ASD) diagnosis themselves.
Mean quality of life scores as measured by the QoLA-A and QoLA-B scales are presented in Figure 1, along with WHOQOL-BREF domain scores. The distribution of parental depressive symptoms is also summarized.
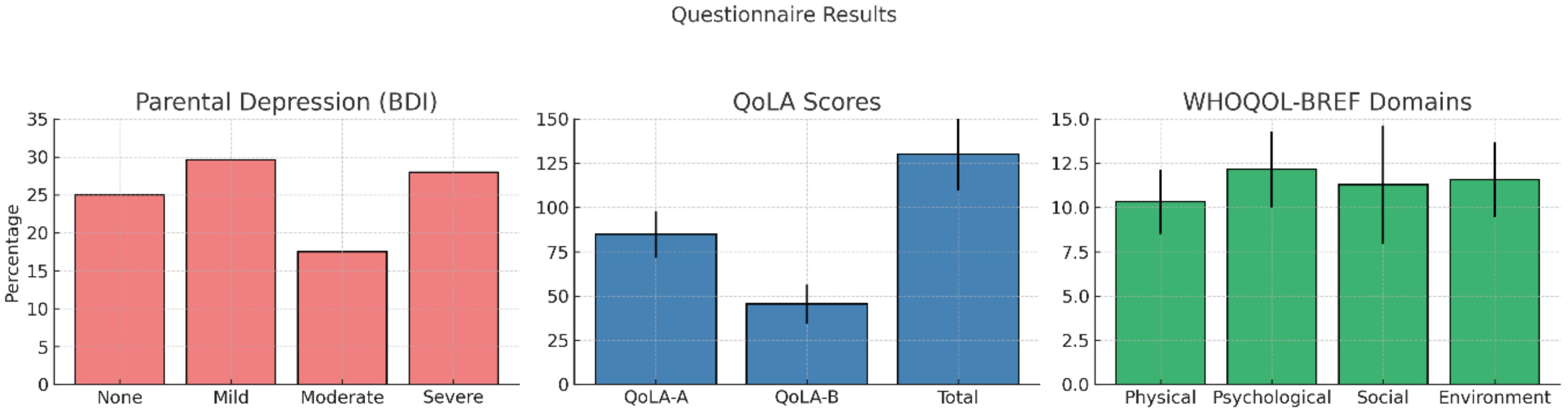
Figure 1. Mean scores on the QoLA-A and QoLA-B scales, WHOQOL-BREF domains, and levels of depressive symptoms (BDI) among participating parents. Error bars represent standard deviations.
3.2 QoLA part A
3.2.1 Validity
A number of analyses were carried out to provide comprehensive evidence of the QoLA questionnaire’s construct validity.
To confirm the 8-factor model, a Confirmatory Factor Analysis was conducted. The model displayed satisfactory fit measures: Root Mean Square Error of Approximation = 0.056 and Comparative Fit Index = 0.92. The resultant model, illustrated in Figure 2, covers all the factors proposed by Shalock except for “Personal growth,” which was replaced with “General well-being.” In general, the factor analysis suggested that the Polish version of QoLA part A is a tool that evaluates at least seven out of eight domains of quality of life. The correlations between the latent variables were moderate to high, indicating a common underlying factor and allowing for total score calculations (see Reliability section). The CFA findings are presented in Table 3.
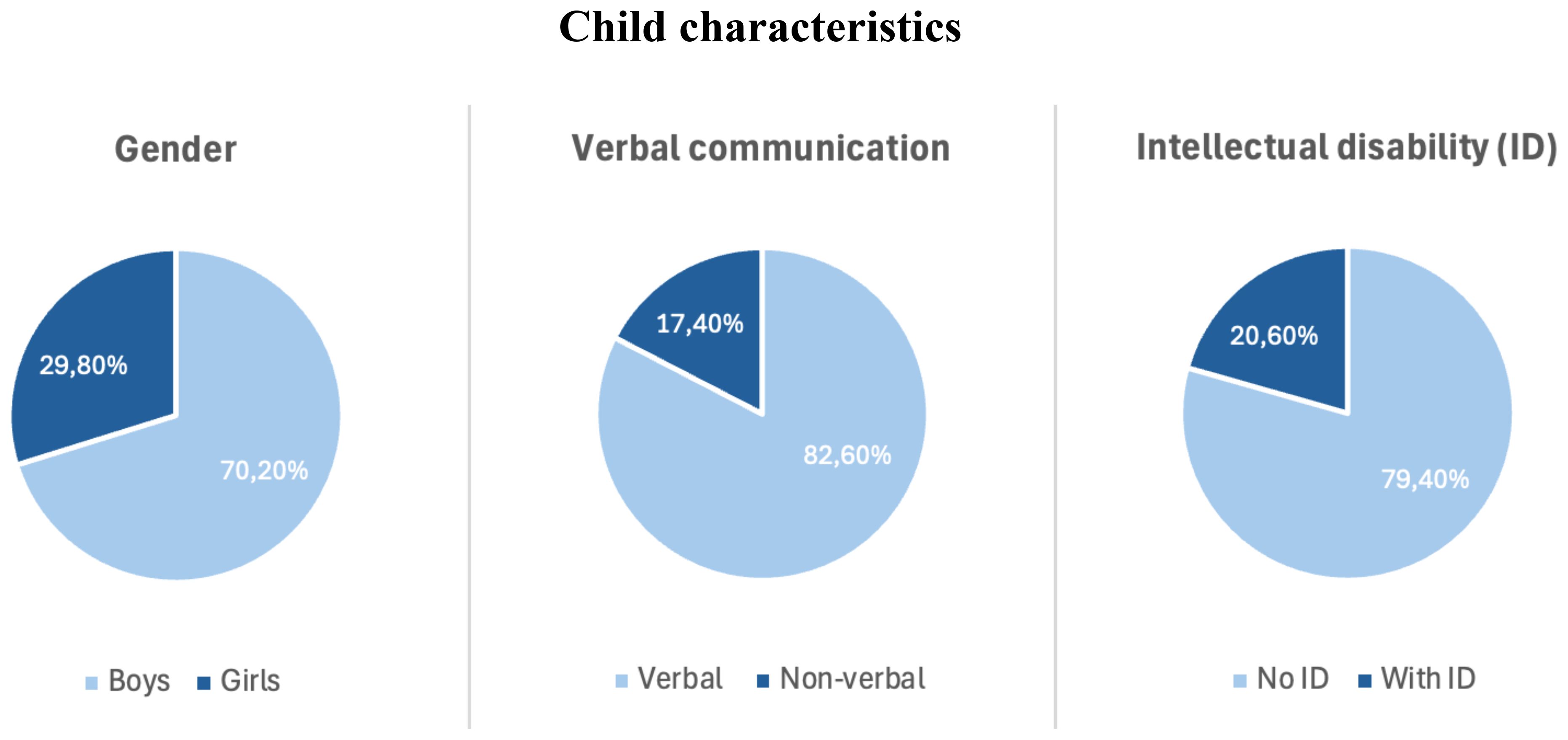
Figure 2. Distribution of child characteristics in the sample, including gender, verbal communication, and presence of intellectual disability.
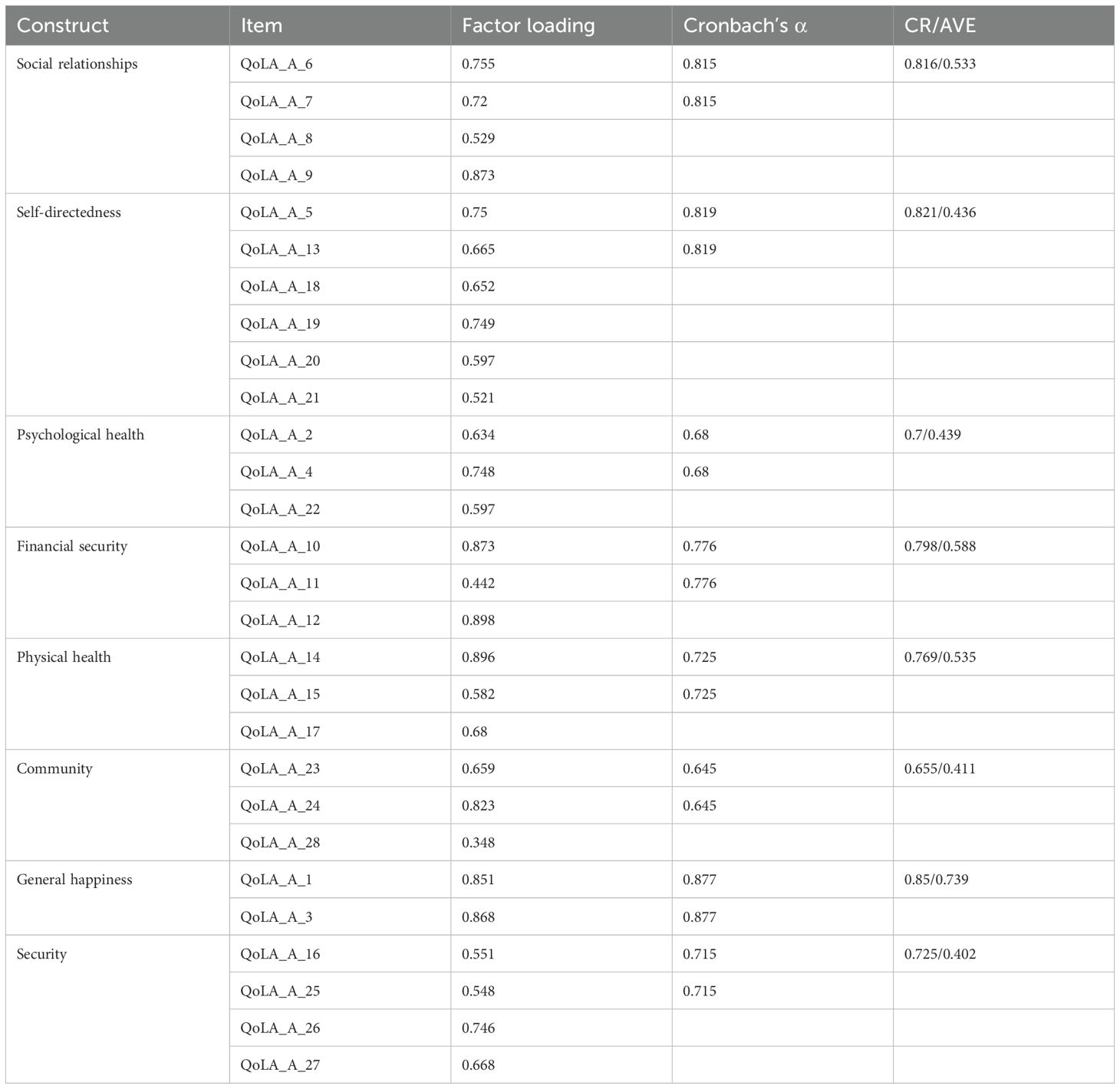
Table 3. Factor loadings of the 8-dimensional CFA model of QoLA-A, CR, Composite Reliability; AVE, Average Variance Extracted.
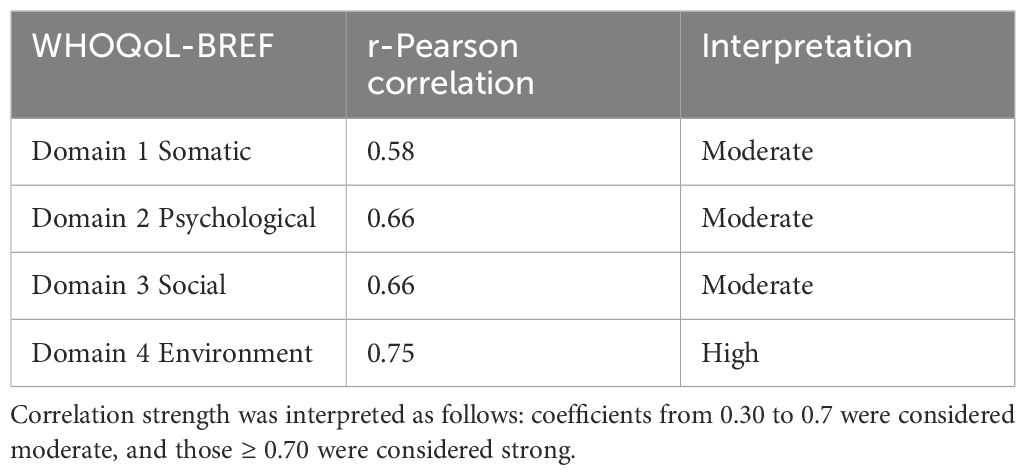
R-Pearson correlation values of QoLA part A and four domains of WHOQoL-BREF are shown in Table 4.
The moderate to high correlations between QoLA-A scores and the four domains of the WHOQoL-BREF suggest good criterion validity. A moderate positive correlation was found between QoLA-A scores and domains related to social relationships, somatic health, and psychological well-being. In addition, a high positive correlation was observed between QoLA-A scores and the environmental domain. These correlations suggest that the QoLA-A effectively measures constructs similar to those of the WHOQoL-BREF in assessing quality of life, validating its use as a reliable tool for assessing individuals’ well-being across domains.
To test concurrent validity, the correlation between QoLA-A scores and the Beck Depression Inventory (BDI) was examined. As expected, the correlation coefficient was –0.71, indicating a strong negative relationship between parental quality of life and depressive symptoms. This finding supports the scale’s criterion validity by demonstrating its sensitivity to psychological distress, a well-established factor associated with reduced wellbeing in parents of children with ASD.
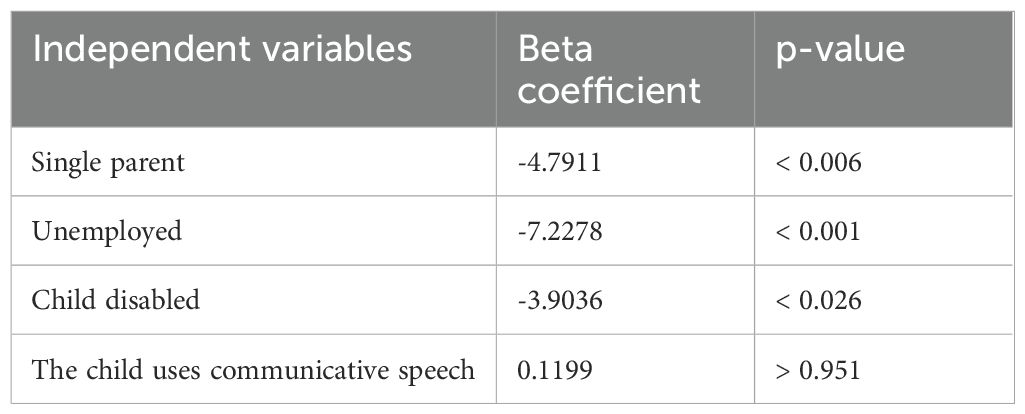
In addition, regression analysis was conducted to assess the relationship between QoLA-A scores and sociodemographic characteristics. The results showed that single parenthood reduced QoLA-A scores by 4.8 points, unemployment by 7.22 points, and having a child with an intellectual disability by 3.9 points. Notably, having a child who could not communicate verbally did not have a statistically significant effect on the QoLA-A score. These results are consistent with theoretical expectations and support the scale’s validity in reflecting the impact of known risk factors on parental quality of life.
3.2.2 Reliability
The reliability of the QoLA part A was found to be high, as indicated by a Cronbach’s alpha coefficient of 0.93. There was no effect on the alpha value when any item was excluded. To take account of the multidimensional nature of the QoLA part A, we also assessed its reliability using the hierarchical omega coefficient (omega h), which was 0.77 - slightly lower than the alpha coefficient but still within an acceptable range (above 0.7). The common factor explained 47% of the total variance. The total omega was 0.95. These results confirm that the QoLA Part A has satisfactory reliability and can effectively measure the quality of life of parents of autistic children, both as a single construct and as an 8-dimensional model. Based on these findings, using the total score as a measure of quality of life is reasonable.
3.3 QoLA part B
3.3.1 Validity
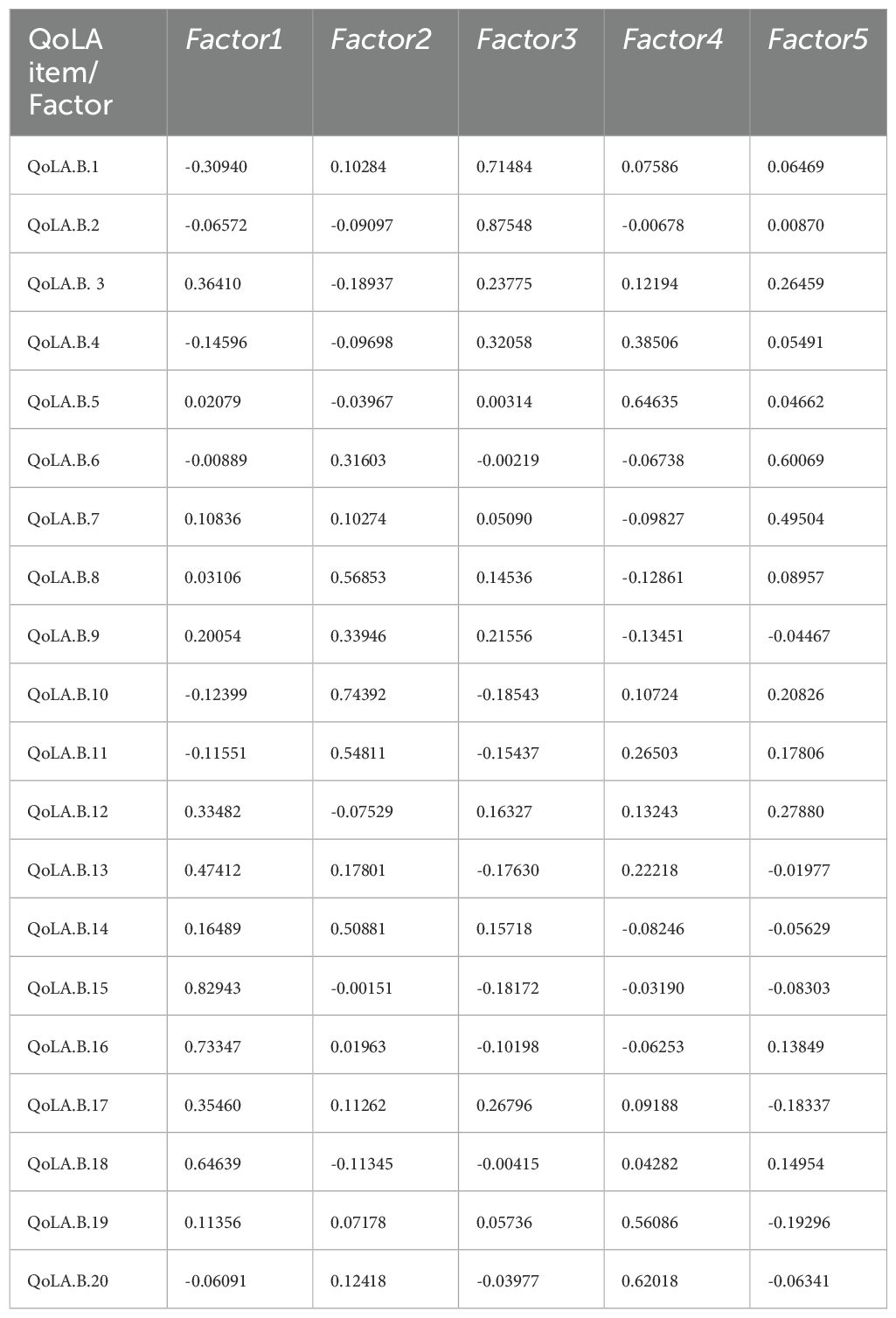
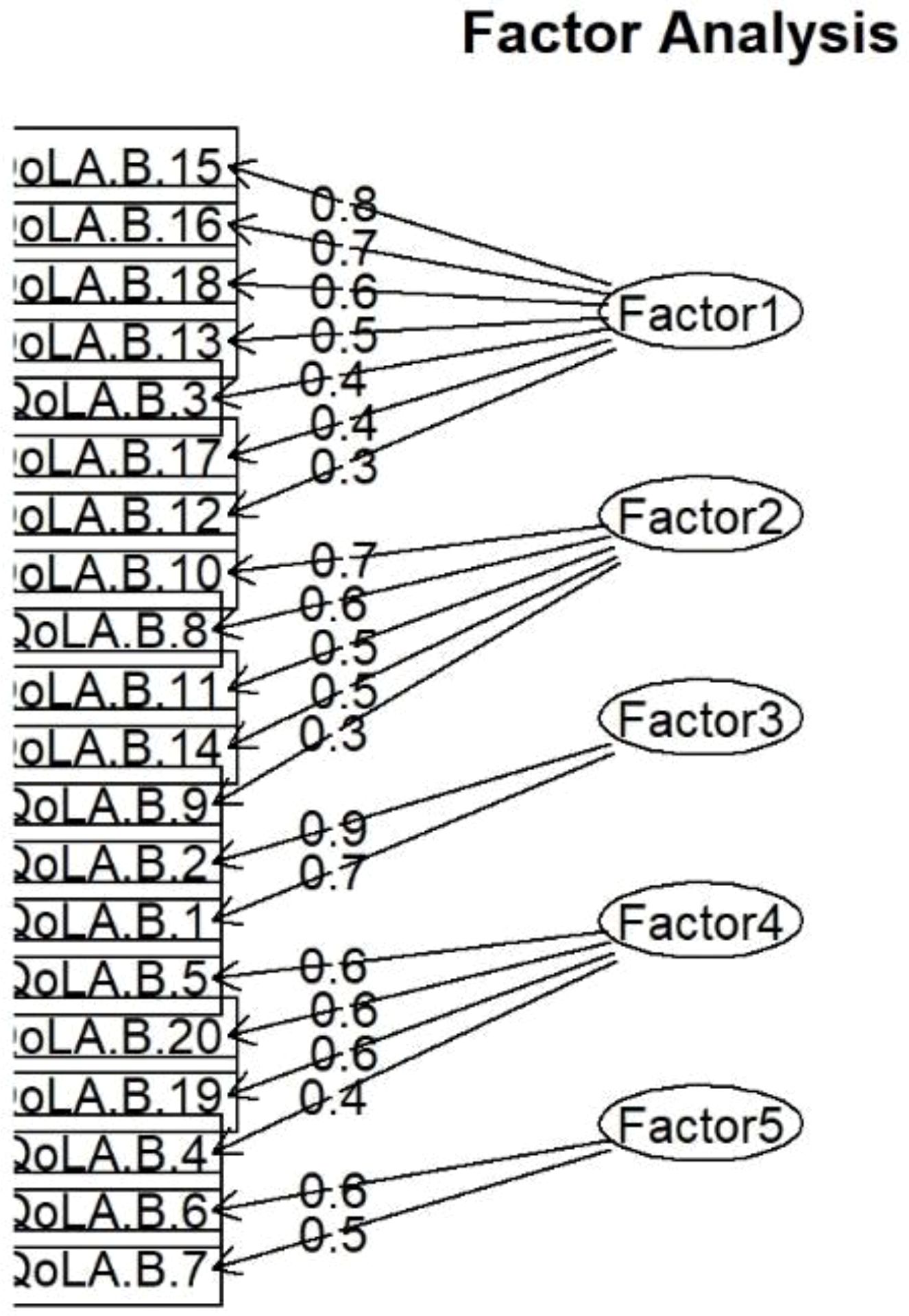
The second part’s exploratory factor analysis resulted in a five-dimensional model with an RMSEA of 0.044, which is below the threshold of 0.05 (Table 5). Models with fewer dimensions are also needed to fit the data adequately. The five-dimensional model accounted for only 42.7% of the variance, so even these dimensions were insufficient to explain most of the variance in the scores. Based on the data and findings, there was no compelling need to conduct a confirmatory factor analysis.
The analysis suggests that the validity of the second part of the QoLA is unsatisfactory, as it covers different aspects of autism spectrum disorder but accounts for only a limited amount of score variability.
3.3.2 Reliability
The reliability of the QoLA part B was assessed using Cronbach’s alpha coefficient, which was 0.86. The removal of one item did not affect the reliability. The calculated omega h was 0.55, below the accepted threshold of 0.7. On the other hand, the total omega (i.e., the five factors plus the general factor) was 0.9, which is very good.
Following the guidelines of authors who suggest using omega total rather than Cronbach’s alpha for multidimensional scales (33), we conclude that the QoLA Part B is a reliable measure of a 5-dimensional construct but a weak measure of a single construct.
3.4 QoLA – B: externalizing behaviours
Although QoLA-B did not prove to be an adequate measure of the impact of ASD symptoms on quality of life in general, we decided to extract items from Factor 1 (see Figure 3), which covers externalizing behaviors, for further analysis. Cronbach’s alpha coefficient estimated its reliability at 0.79, justifying its use to measure externalizing behaviors.
3.5 Comparisons and regression models
Comparison of means revealed that parents who were married, employed full-time, and reported a higher material status tended to report higher levels of quality of life. Similarly, parents of verbally communicative children and those without an intellectual disability in the child also reported higher QoLA-A scores (see Table 6). These findings are consistent with intuition and prior research and provide further support for the construct validity of the instrument. Notably, widowed participants (N = 3) reported relatively high QoLA-A scores; however, this subgroup was extremely small, and the high standard deviation suggests substantial variability. Therefore, this result should be interpreted with caution, as it may reflect individual characteristics or random variation rather than a systematic pattern. The comparisons are presented in Figure 4.
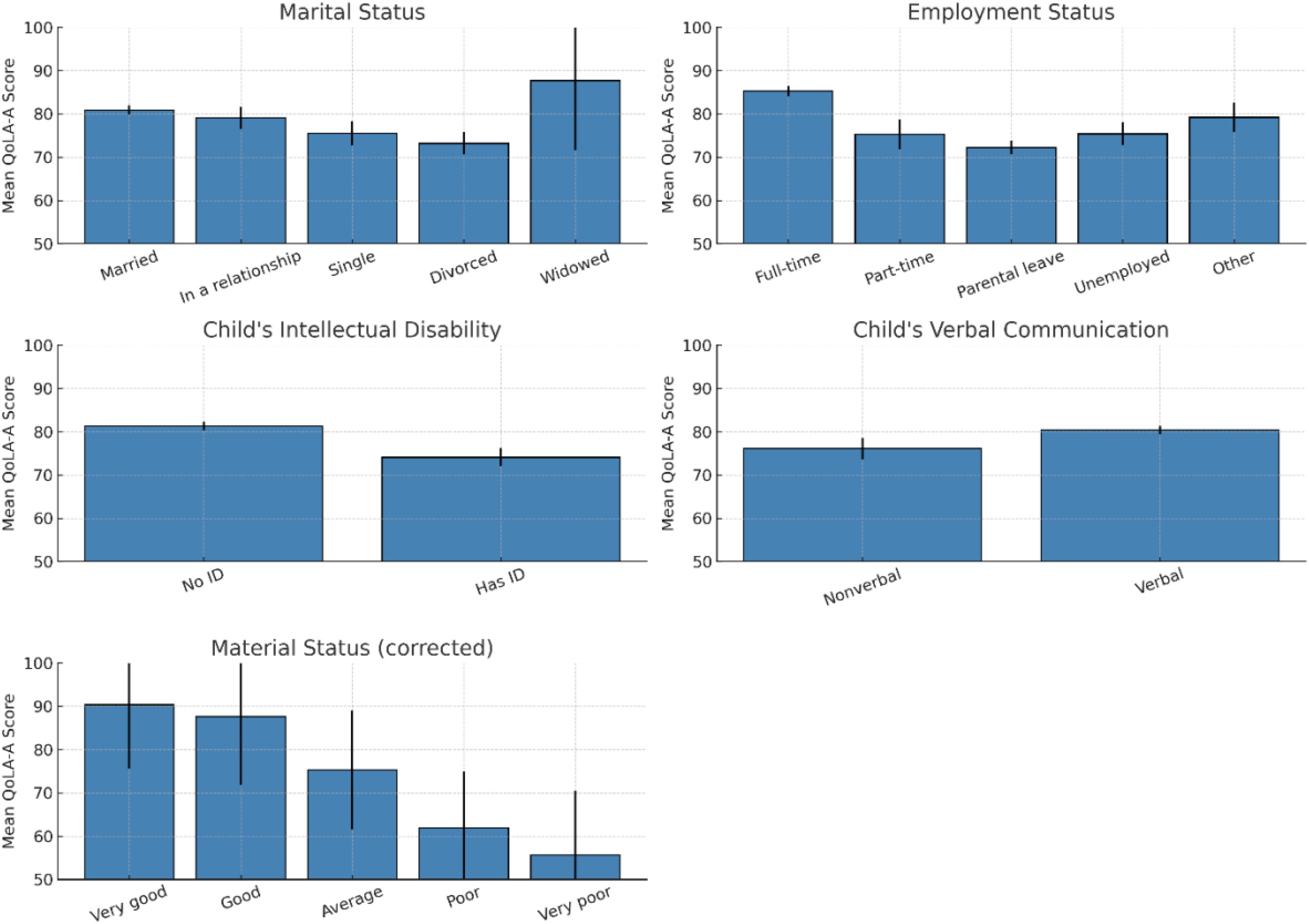
Figure 4. Comparisons of mean QoLA-A score by groups. Error bars represent standard errors of the mean.
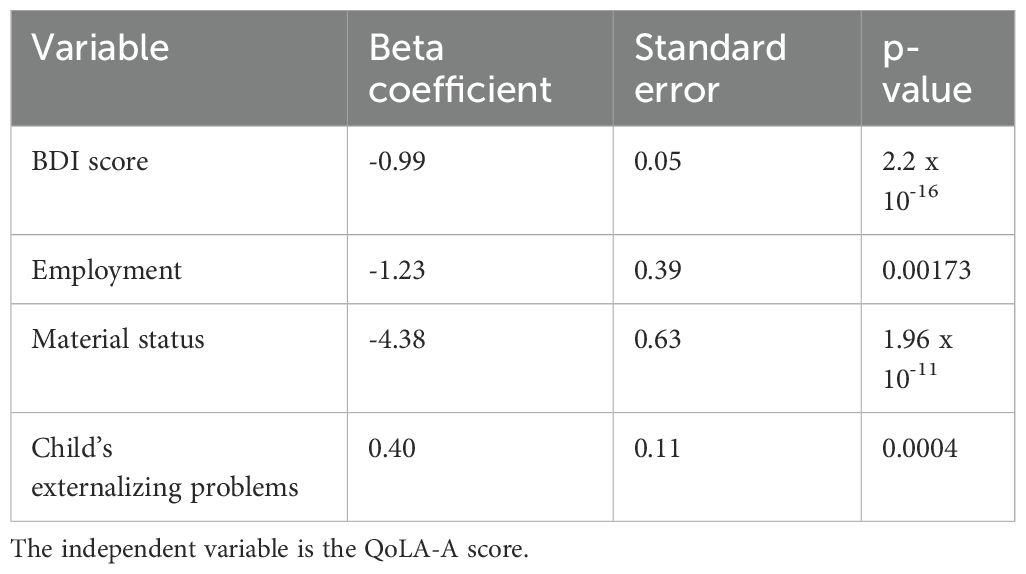
A number of regression models were used to further elucidate the factors influencing the quality of life of the participants in our study. A backward stepwise multiple regression analysis, which systematically removes variables that do not contribute significantly to the model, was applied to the initial set of nine explanatory variables. Initially including nine explanatory variables - the presence of communicative speech in the child, the presence of intellectual disability, Beck Depression Scale scores, parental age, child age, number of children living in the household, employment status, marital status, and externalizing behaviors exhibited by the child - the analysis eventually reduced the model to include only four variables: Beck Depression Scale scores, employment status, material status, and externalizing behaviors exhibited by the child. The relevant coefficients of this model are shown in Table 7. The final model was statistically significant, F = 189.1, df(4, 356), p < 2.2 x 10-16, and explained 68% of the variance in the scores (R2 = 0.68, adj. R2 = 0.68).
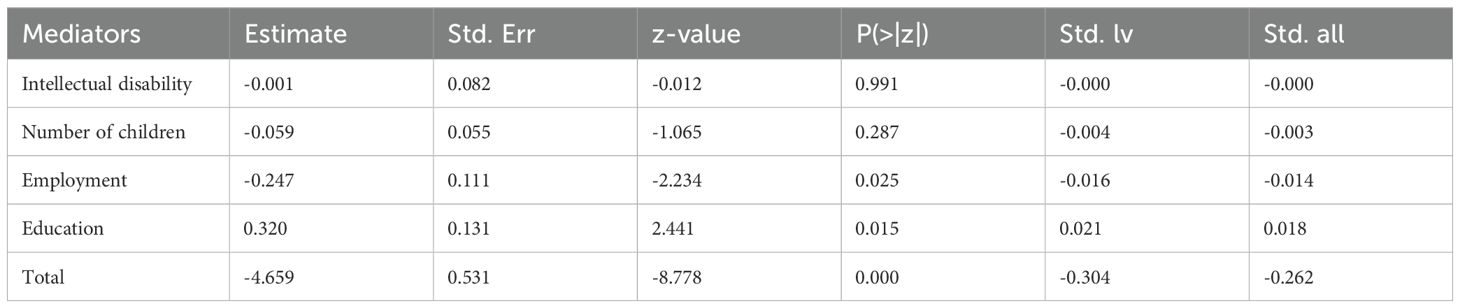
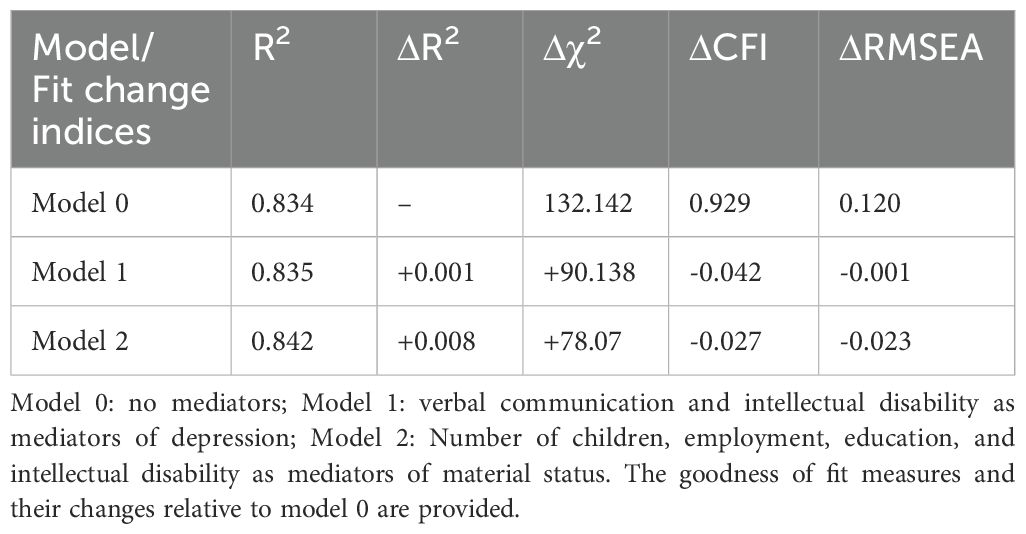
We then used this model as the basis for structured equation modeling, where a latent variable, ‘quality of life,’ was defined as a composite of QoLA-A and WHOQOL dimensions 1,2,3 and 4 scores. Model 0 included the four explanatory variables obtained by stepwise regression. Model 1 included verbal communication and intellectual disability as mediators of parental depression. Model 2 included the number of children in the household, parental education, intellectual disability, and employment as mediators of material status. Material status was positioned as a higher-order variable based on both theoretical and empirical considerations. Conceptually, financial well-being is an upstream determinant of key life circumstances, such as educational attainment, employment status, and family size. These factors are, in turn, known to influence parental quality of life. By modeling material status as an exogenous variable with potential mediating pathways, we aimed to better understand the mechanisms through which financial conditions shape well-being. This structure was further supported by the results of the structural equation modeling, which identified employment and education as significant mediators of the material status–quality of life relationship. In model 1, no significant mediators were found; in model 2, the mediating effects of employment and education on the effect of material status on quality of life were statistically significant (see Table 8). The other mediators were not significant.
Model 2 provided the greatest increase in R2 and the greatest decrease in RMSEA, bringing it below 0.1, which is considered acceptable for a model, while keeping CFI slightly above 0.9, which is still considered acceptable (see Table 9). Therefore, we chose model 2 as the best representation of the data obtained. Moreover, Model 2 demonstrated the best overall fit among the three tested models. This suggests that placing material status in a higher-level position provides a more accurate representation of the data. Table 8 lists the 4 mediation effects of the model, 2 of which were statistically significant.
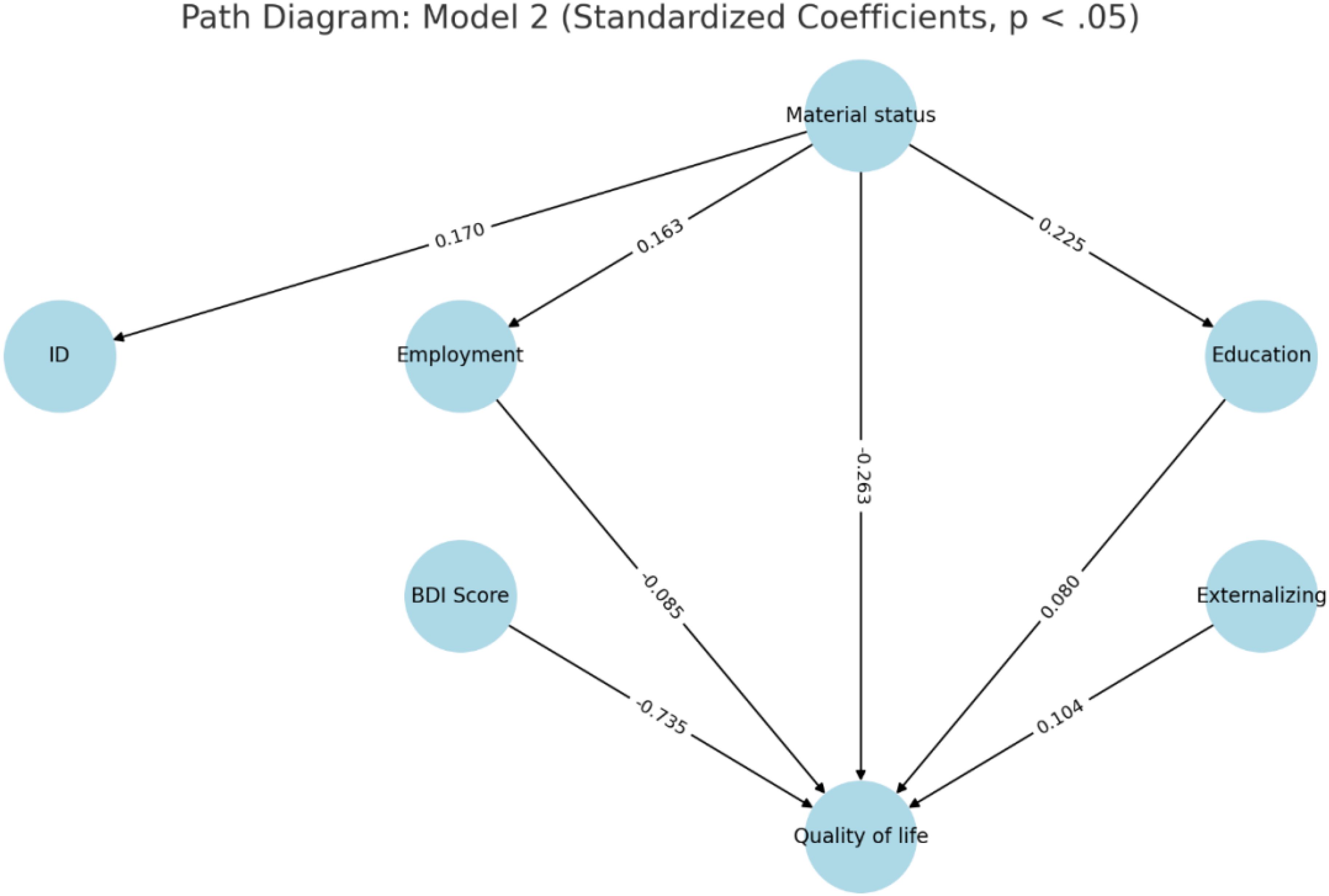
Figure 5. Path diagram of Model 2 with standardized coefficients of statistically significant effects (p <.05). Model 2 tested the mediating role of employment, education, intellectual disability (ID), and number of children in the household in the relationship between material status and parental quality of life (QoL). Only paths with p-values below.05 are shown. Material status was modeled as an exogenous variable based on both theoretical rationale and empirical model fit improvements ΔR², .008; ΔRMSEA, –.023). BDI, Beck Depression Inventory.
In model 2, QoL is directly predicted by BDI scores, child externalizing problems, parental education, employment, and material status. Indirectly, poorer material status predicts lower education and employment, which worsens quality of life. The poorer material status also predicts intellectual disability, but this variable did not affect the quality of life. The mediation paths are presented in Figure 5 and coefficients are listed in Table 10.
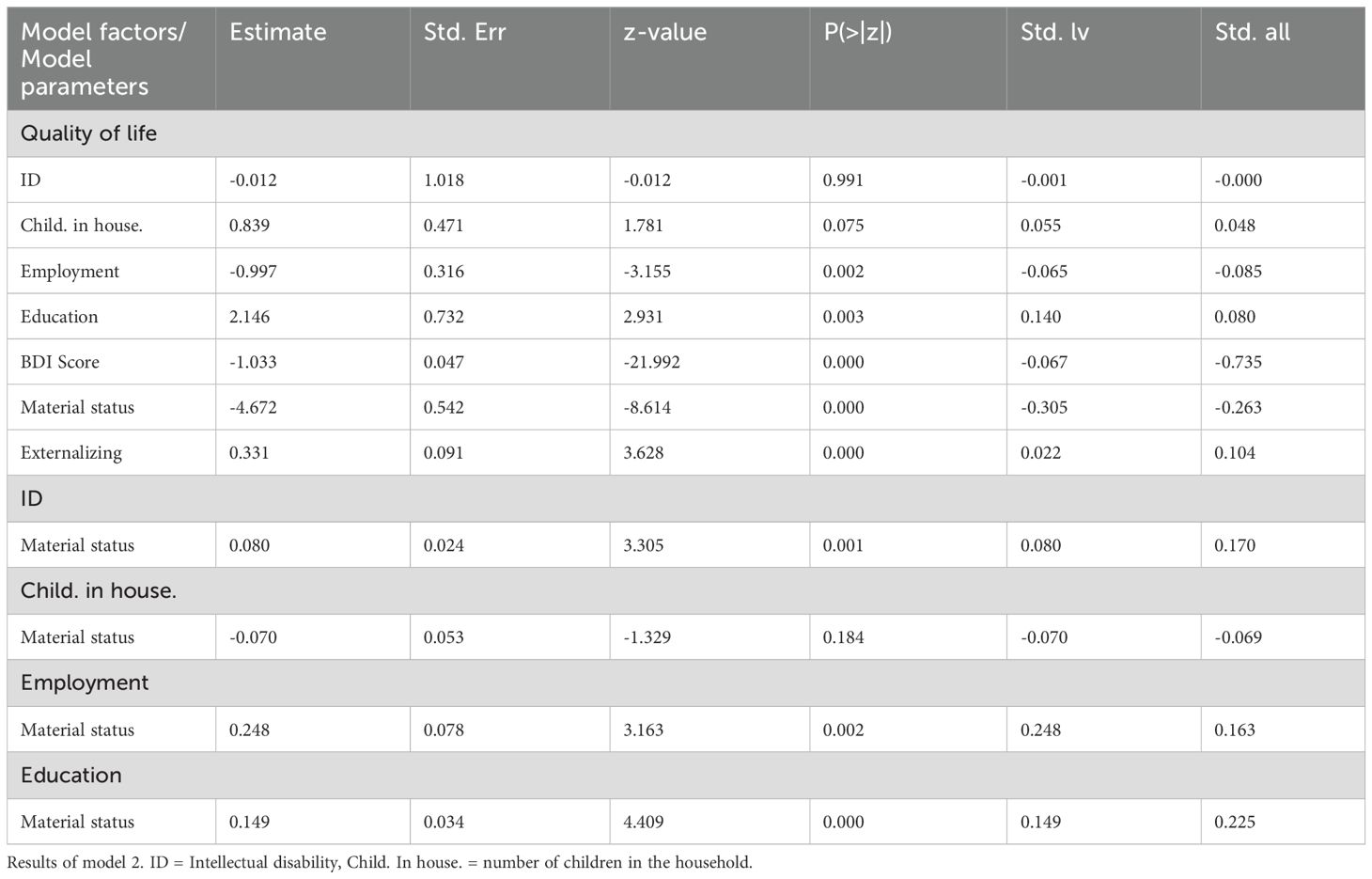
Table 10. Path analysis of model 2 with standardized coefficients of statistically significant effects (p <.05).
4 Discussion
4.1 Summary of findings
In this study, we conducted several analyses to evaluate the measurement properties of the QoLA questionnaire using a sample of parents of children with ASD. In addition, we aimed to identify factors that influence their quality of life.
Part A of the questionnaire showed satisfactory reliability as measured by Cronbach’s alpha, omega h, and omega total. To investigate the structure of QoLA-A, we used exploratory factor analysis and explored different methods to determine the number of factors. Ultimately, an 8-factor model aligned with Schalock’s quality of life domains was confirmed by confirmatory factor analysis, which showed satisfactory goodness of fit. Criterion validity was established by assessing correlations between QoLA Part A scores and the WHOQOL-BREF and the Beck Depression Inventory. The results showed moderate to high correlations, supporting its relevance for different aspects of well-being. Based on the results, it is concluded that the QoLA-Part A is a valid and reliable measure of quality of life in people with autistic spectrum disorders. The scores also correlated moderately to strongly with established predictors of QoL, such as depression, marital status, material status, and unemployment. This is consistent with the questionnaire adaptations from Turkey (34), Iran (35), Bangladesh (36), and Malaysia (37).
Part B’s reliability was confirmed, but exploratory factor analysis revealed a 5-dimensional structure that explained less than 50% of the variance in scores, failing to prove that the questionnaire measures ASD symptomatology as commonly described. This contrasts findings from Turkey (34) and transcultural studies (38), where a three-dimensional structure explaining over 60% of score variance is consistently reported. This suggests that cultural differences may play a role in parents’ perceptions of ASD symptoms in their children. Indeed, this has been confirmed in a cross-cultural comparison showing that culture plays an important role in reporting symptoms related to repetitive behaviors, with Polish and US parents more likely to endorse these items than parents from other countries (39). This may have led to items related to these behaviors being split into multiple dimensions. Nevertheless, caution should be exercised when using the QoLA Part B to assess parent-reported ASD symptomatology in Poland.
Although the overall Cronbach’s alpha and omega coefficients justify the use of the QoLA-B as a reliable measure of the five dimensions, the low omega h value, the failure to capture the predicted dimensionality, and the low explanatory power of the questionnaire’s five-dimensional model raise serious doubts about the use of the inventory to measure the impact of ASD symptoms on quality of life in Poland.
4.2 Child-related factors of parental quality of life
Our results showed that of the child-related variables included in the study - intellectual disability, lack of verbal communication, child’s age, gender, and externalizing problems - only the latter was a statistically significant predictor of parents’ quality of life. This seemed puzzling, as intellectual disability and lack of verbal communication could potentially be a major burden for carers. However, other researchers have also found that in families of children with ASD, externalizing problems such as oppositional defiant disorder and aggression are more strongly associated with poorer quality of life scores than communication difficulties (40). Similarly, ASD subtype or severity was not found to influence maternal distress (41) or quality of life (42) when child behavioral problems were taken into account. Other data also suggest a limited or no effect of child-related variables on parental QoL (43). Intellectual disability had a limited or no effect on parental QoL in some studies (41, 44, 45). Physical disability did not worsen maternal QoL (46). Communication problems were found to hurt QoL, but parental optimism may act as a mediator (47). A meta-regression study found neither IQ nor ASD severity predicted adult QoL, but social functioning did (48). On the other hand, some studies report a negative impact of autism severity on family quality of life (17, 49–51) (but only for mothers, fathers reported an inverse relationship), even compared to other disabilities, including neurological ones (52). The reason for these conflicting results may be that intellectual disability (ID) is a spectrum ranging from mild to severe, with 85% of those diagnosed being mildly impaired (1, 53). We did not ask respondents to indicate the level of intellectual disability of their children, but we can assume that most were mildly impaired. In one paper, we found that parents of mildly mentally disabled children reported a quality of life similar to that of neurotypical children, in contrast to parents of moderately intellectually disabled children (12). Another plausible explanation for this phenomenon is that psychiatric diagnoses may be less able to accurately predict parents’ quality of life than functional diagnoses and the child’s level of autonomy. This assertion implies that factors related to the individual’s functional abilities and the degree of independence they can exercise may have greater predictive power in determining overall quality of life, as suggested by existing research (51, 52). Finally, our respondents were almost exclusively mothers, which means that child-related variables may have a greater impact on fathers’ quality of life.
4.3 Social factors of parental quality of life
Our model, including the social variables, explained over 80% of the variance, which is very high. It should be noted, however, that this high percentage may be influenced by the fact that some QoLA-A questions deal with material status, which contributes to an inflated covariance. This implies that the social variables included in our model play a crucial role in predicting parents’ quality of life. We found that lower material status, employment status, and educational attainment predicted lower quality of life.
In our univariate analyses, single parenthood was initially found to predict lower quality of life. However, when additional variables were included in the analysis, this effect was attenuated, suggesting a mediating influence of these additional factors. This observation aligns with findings from previous studies in which single parenthood was similarly dependent on a range of socioeconomic factors (52). This suggests that while single mothers may have a lower reported quality of life, this outcome is predominantly due to a lack of material resources and support from a partner rather than their marital status per se.
The presence of additional offspring had no significant effect on the outcome, which differs from previous studies suggesting that an increased number of children correlates with improved quality of life (53). This finding is consistent with existing research (18, 54). The potential influence of neurodevelopmental diagnoses in siblings warrants consideration in this context.
Although some studies do not report on the influence of material status on quality of life (54, 55), most do (13, 15, 56–58). A Greek study comparing the influence of the COVID-19 pandemic and the financial crisis of 2014–5 provides interesting insights, showing that the economic crisis worsened parental quality of life more than the pandemic, highlighting the role of financial stability (59). This is in line with the findings of other studies.
4.4 Maternal depression and mother-related variables
We measured levels of depression in our sample and found 28% of the respondents were experiencing severe depression and only 25% had no symptoms. Additionally, maternal depression deteriorated their quality of life even when socio-economic variables were taken into an account. This is in line with other evidence showing that the prevalence of depression in mothers of autistic children is high and affects their quality of life as well as ASD symptom severity in children (52, 60). A study conducted among 409 parents of children with ASD in China, revealed that 18.8% exhibited significant depressive symptoms, with notably higher occurrence observed among families experiencing high economic burden, caring for a child with limited verbal communication, expressing dissatisfaction with their current marital status and facing unemployment (58).
We did not find any moderators of the influence of maternal depression on quality of life, however other studies point to personality traits like neuroticism (61). Spousal support may serve as a significant factor (62, 63) although findings exhibit variability (62). It is plausible that beyond the mere presence of a spouse, the quality of the interpersonal relationship within the dyad plays a critical role (13). Perception of the child by immediate neighbours has also been shown to affect maternal depression (64). Extensive investigation has been dedicated to examining maternal coping mechanisms. Research indicates that a task-oriented approach and ego-resiliency, loosely defined as the ability to withstand stress, are robust predictors of enhanced maternal quality of life, whereas an emotion-focused coping style demonstrates a contrary effect (63).
4.5 Strengths and limitations of our study
A key strength of our survey is the relatively large sample size, which increases our findings’ statistical power and generalisability. However, as the survey was distributed online via social media platforms, it reached a limited demographic group. This distribution method may have yet to capture a broad and diverse cross-section of the population, potentially bias our results and limiting the scope of our conclusions. Future studies should include a higher representation of fathers and participants with a more diverse educational status. In addition, eligibility in our questionnaire was based only on parental reports of ASD. It is possible that not all families had children diagnosed with ASD using scientifically accepted methods.
5 Conclusions
In conclusion, the validation of the questionnaire showed that the QoLA Part A is suitable for use in Polish settings and well reflects the quality of life of parents of children with ASD. However, Part B should be used cautiously when measuring ASD-related quality of life.
Based on the results of the multivariate analysis, we suggest that policymakers focus on improving the material status of families raising children with ASD as a key pathway to enhancing parental quality of life. In addition to direct financial assistance, such as targeted benefits or tax relief, this could include active measures such as subsidized employment opportunities, flexible work arrangements, and access to vocational training—particularly for mothers, who often bear the greatest caregiving burden. In addition, early screening for signs of depression in parents and appropriate psychological and medical support should be provided. In addition, behavioral therapy and parent counseling for externalizing and internalizing problems should be offered. Increasing the child’s autonomy and facilitating their participation in a normal school environment is also recommended, as parents with a child who attended school and those with a child who had leisure activities in a normal environment reported less stress and a better quality of life (60).
On the other hand, we found no compelling evidence, either in this study or in the literature, to recommend increasing the amount of ASD-specific therapeutic activities as a means of improving maternal quality of life. An over-concentration of individual work with the child to alleviate ASD symptoms may decrease parents’ quality of life (64). Some research has found that attending autism support groups and parent training had no significant effect on quality of life (57) or that parents who attended reported lower quality of life than those who did not (45).
Another reason to focus on parents’ quality of life is that data suggests that while behavior does not influence maternal well-being, the reverse is true (54). Parents who attend autism support groups report lower quality of life.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Bioethics Committee of the Medical University of Warsaw (approval number AKBE/232/2023). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
LK: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MK: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. JL: Investigation, Resources, Validation, Writing – original draft, Writing – review & editing. PR: Formal Analysis, Resources, Software, Writing – original draft, Writing – review & editing. TW: Formal analysis, Funding acquisition, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We want to thank the SYNAPSIS Foundation for helping us distribute the survey and all the parents who participated in the study. We also want to thank Professor Valsamma Eapen for allowing us to conduct the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be constructed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lai MC, Lombardo MV, and Baron-Cohen S. Autism. Lancet. (2014) 383:896–910. doi: 10.1016/S0140-6736(13)61539-1
2. Maenner MJ, Warren Z, Williams AR, Amoakohene E, Bakian AV, Bilder DA, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2020. MMWR Surveill Summ. (2023) 72:1–14. doi: 10.15585/mmwr.ss7202a1
3. Vasilopoulou E and Nisbet J. The quality of life of parents of children with autism spectrum disorder: A systematic review. Res Autism Spectr Disord. (2016) 23:36–49. doi: 10.1016/j.rasd.2015.11.008
4. Arya Y, Mishra D, Juneja M, and Gupta A. Factors affecting quality of life in adolescent siblings of children with autism spectrum disorder. Indian Pediatr. (2023) 60:739–43. doi: 10.1007/s13312-023-2988-3
5. Ilias K, Cornish K, Kummar AS, Park MS, and Golden KJ. Parenting stress and resilience in parents of children with autism spectrum disorder (ASD) in Southeast Asia: A systematic review. Front Psychol. (2018) 9:280. doi: 10.3389/fpsyg.2018.00280
6. Gau S, Chou M-C, Chiang H-L, Lee J-C, Wong C-C, Chou W-J, et al. Parental adjustment, marital relationship, and family function in families of children with autism. Res Autism Spectr Disord. (2012) 6:263–70. doi: 10.1016/j.rasd.2011.05.007
7. McConachie H and Diggle T. Parent implemented early intervention for young children with autism spectrum disorder: a systematic review. J Eval Clin Pract. (2007) 13:120–9. doi: 10.1111/j.1365-2753.2006.00674.x
8. Sikorska I and Pisula E. Jakość życia rodziców dzieci z autyzmem w porównaniu z rodzicami dzieci rozwijających się typowo. Psychiatr Pol. (2008) 42:713–22.
9. Stefańska-Klar R. Funkcjonowanie rodzin z dziećmi z ASD – przegląd literatury i ujęcie empiryczne. Niepełnosprawność – Dyskursy Pedagog Spec. (2021) 40):93–106.
10. Ślifirczyk A, Głowacka MD, and Ślifirczyk M. Quality of life of parents of children with autism – a comparative study in Poland, France and Belarus. Prog Health Sci. (2016) 6:102–7. doi: 10.5604/01.3001.0010.1918
11. Veenhoven R. The four qualities of life: ordering concepts and measures of the good life. J Happiness Stud - J HAPPINESS Stud. (2000) 1:1–39. doi: 10.1023/A:1010072010360
12. Dizdarevic A, Memisevic H, Osmanovic A, and Mujezinovic A. Family quality of life: perceptions of parents of children with developmental disabilities in Bosnia and Herzegovina. Int J Dev Disabilities. (2022) 68:274–80. doi: 10.1080/20473869.2020.1756114
13. Borilli MC, Germano CMR, de Avó L, Pilotto RF, and Melo DG. Family quality of life among families who have children with mild intellectual disability associated with mild autism spectrum disorder. Arq Neuropsiquiatr. (2022) 80:360–7. doi: 10.1590/0004-282x-anp-2020-0537
14. McStay RL, Trembath D, and Dissanayake C. Stress and family quality of life in parents of children with autism spectrum disorder: parent gender and the double ABCX model. J Autism Dev Disord. (2014) 44:3101–18. doi: 10.1007/s10803-014-2178-7
15. Schlebusch L, Dada S, and Samuels AE. Family quality of life of South African families raising children with autism spectrum disorder. J Autism Dev Disord. (2017) 47:1966–77. doi: 10.1007/s10803-017-3102-8
16. Pisula E and Porębowicz-Dörsmann A. Family functioning, parenting stress and quality of life in mothers and fathers of Polish children with high functioning autism or Asperger syndrome. PloS One. (2017) 12:e0186536. doi: 10.1371/journal.pone.0186536
17. Pozo P, Sarriá E, and Brioso A. Family quality of life and psychological well-being in parents of children with autism spectrum disorders: a double ABCX model. J Intellect Disabil Res. (2014) 58:442–58. doi: 10.1111/jir.2014.58.issue-5
18. Volgyesi-Molnar M, Gyori M, Eapen V, Borsos Z, Havasi A, Jakab Z, et al. Quality of life in hungarian parents of autistic individuals. J Autism Dev Disord. (2024) 55:1122–37. doi: 10.1007/s10803-024-06243-3
19. Dedhiya S and Kong SX. Quality of life: an overview of the concept and measures. Pharm World Sci. (1995) 17:141–8. doi: 10.1007/BF01879707
20. Claes C, Van Hove G, van Loon J, Vandevelde S, and Schalock RL. Quality of life measurement in the field of intellectual disabilities: eight principles for assessing quality of life-related personal outcomes. Soc Indic Res. (2010) 98:61–72. doi: 10.1007/s11205-009-9517-7
21. Schalock RL, Bradley VJ, and Gardner JF. Quality of Life for People with Intellectual and Other Developmental Disabilities: Applications Across Individuals, Organizations, Communities, and Systems. Washington, DC, USA: American Association on Intellectual and Developmental Disabilities. (2006).
22. Verdugo MÁ, de Urríes FdBJ, CJ Río, Escribano CC, and Crespo M. Quality of life of workers with an intellectual disability in supported employment. J Appl Res Intellect Disabil. (2006) 19(4):309–16. doi: 10.1111/j.1468-3148.2006.00277.x
23. Maes B, Geeraert L, and Van den Bruel B. Developing a model for quality evaluation in residential care for people with intellectual disability. J Intellect Disabil Res. (2000) 44:544–52. doi: 10.1046/j.1365-2788.2000.00266.x
24. Rapley M and Beyer S. Daily activity community participation and quality of life in an ordinary housing network: A two-year follow-up. J Appl Res Intellect Disabil. (1998) 11(1):34–43. doi: 10.1111/j.1468-3148.1998.tb00032.x
25. Verdugo M, Prieto G, Caballo C, and Peláez A. Factorial structure of the quality of life questionnaire in a Spanish sample of visually disabled adults. Eur J psychol Assess - Eur J Psychol ASSESS. (2005) 21:44–55. doi: 10.1027/1015-5759.21.1.44
26. Bigby C, Knox M, Beadle-Brown J, and Bould E. Identifying good group homes: qualitative indicators using a quality of life framework. Intellect Dev Disabil. (2014) 52:348–66. doi: 10.1352/1934-9556-52.5.348
27. Eapen V, Crnčec R, Walter A, and Tay KP. Conceptualisation and development of a quality of life measure for parents of children with autism spectrum disorder. Autism Res Treat. (2014) 2014:160783. doi: 10.1155/2014/160783
28. Available online at: https://www.who.int/substance_abuse/research_tools/translation/en/WHOWHOPotaaoi (Accessed April 19, 2024).
29. World Health Organization and Division of Mental Health. WHOQOL-BREF: introduction a, scoring and generic version of the assessment: field trial version, December 1996. Geneva, Switzerland: World Health Organization (1996). Available online at: https://iris.who.int/handle/10665/63529 (Accessed April 19, 2024).
30. Beck AT, Ward CH, Mendelson M, Mock J, and Erbauch J. Beck Depression Inventory (BDI) [Database record]. APA PsycTests. Washington, DC: American Psychological Association. (1961). doi: 10.1037/t00741-000
31. Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. (1951) 16:297–334. doi: 10.1007/BF02310555
32. Rodriguez A, Reise SP, and Haviland MG. Evaluating bifactor models: Calculating and interpreting statistical indices. Psychological Methods. (2016) 21(2):137–50. doi: 10.1037/met0000045
33. Dunn TJ, Baguley T, and Brunsden V. From alpha to omega: a practical solution to the pervasive problem of internal consistency estimation. Br J Psychol. (2014) 105:399–412. doi: 10.1111/bjop.2014.105.issue-3
34. Gürbüz Özgür B, Aksu H, and Eser E. Turkish validity and reliability of quality of life in autism questionnaire-parent version. Anadolu Psikiyatri Dergisi. (2017) 18:344–52. doi: 10.5455/apd.249390
35. Hosseini S-S, Beheshti S, Eapen V, Almasi-Hashiani A, and Maroufizadeh S. Reliability and Validity of the Persian Version of the Quality of Life in Autism Questionnaire (QoLA) - Parent Version in Iranian Mothers. Research Square [Preprint]. (2021).
36. Azad SMA, Shilvy N, and Rabby A. Adaptation of the quality of life in autism scale for use in Bangladesh. Biores Communications. (2021) 7:960–6. doi: 10.3329/brc.v7i1.54250
37. Shamsudin ID, M-l Yu, and Brown T. Translation, cross-cultural adaptation and validation of the quality of life in autism questionnaire (QoLA) from english into the Malay language. J Occup Therapy Schools Early Intervention. (2018) 12:253 – 72. doi: 10.1080/19411243.2018.1538842
38. Eapen V, Karlov L, John JR, Beneytez C, Grimes PZ, Kang YQ, et al. Quality of life in parents of autistic children: A transcultural perspective. Front Psychol. (2023) 14:1022094. doi: 10.3389/fpsyg.2023.1022094
39. Matson JL, Matheis M, Burns CO, Esposito G, Venuti P, Pisula E, et al. Examining cross-cultural differences in autism spectrum disorder: A multinational comparison from Greece, Italy, Japan, Poland, and the United States. Eur Psychiatry. (2017) 42:70–6. doi: 10.1016/j.eurpsy.2016.10.007
40. Lecavalier L, Leone S, and Wiltz J. The impact of behavior problems on caregiver stress in young people with autism spectrum disorders. J Intellect Disabil Res. (2006) 50:172–83. doi: 10.1111/j.1365-2788.2005.00732.x
41. Peters-Scheffer N, Didden R, and Korzilius H. Maternal stress predicted by characteristics of children with autism spectrum disorder and intellectual disability. Res Autism Spectr Disord. (2012) 6:696–706. doi: 10.1016/j.rasd.2011.10.003
42. Lichtlé J, Devouche E, Dialahy IZ, de Gaulmyn A, Amestoy A, Coutelle R, et al. Development, psychometric evaluation, and factor analysis of an instrument measuring quality of life in autistic preschoolers. Int J Methods Psychiatr Res. (2023) 33:e2002. doi: 10.1002/mpr.2002
43. Ten Hoopen LW, de Nijs PFA, Duvekot J, Greaves-Lord K, Hillegers MHJ, Brouwer WBF, et al. Caring for children with an autism spectrum disorder: factors associating with health- and care-related quality of life of the caregivers. J Autism Dev Disord. (2022) 52:4665–78. doi: 10.1007/s10803-021-05336-7
44. Baghdadli A, Pry R, Michelon C, and Rattaz C. Impact of autism in adolescents on parental quality of life. Qual Life Res. (2014) 23:1859–68. doi: 10.1007/s11136-014-0635-6
45. Vernhet C, Michelon C, Dellapiazza F, Rattaz C, Geoffray MM, Roeyers H, et al. Perceptions of parents of the impact of autism spectrum disorder on their quality of life and correlates: comparison between mothers and fathers. Qual Life Res. (2022) 31:1499–508. doi: 10.1007/s11136-021-03045-3
46. Yıldız A, Tarakcı D, Hajebrahimi F, and Mutluay F. Disabled children’s functionality and maternal quality of life and psychological status. Pediatr Int. (2016) 58:1291–6. doi: 10.1111/ped.13020
47. Wisessathorn M, Chanuantong T, and Fisher EB. The impact of child’s severity on quality-of-life among parents of children with autism spectrum disorder: the mediating role of optimism. J Med Assoc Thai. (2013) 96:1313–8.
48. Kim SY and Bottema-Beutel K. A meta regression analysis of quality of life correlates in adults with ASD. Res Autism Spectr Disord. (2019) 63:23–33. doi: 10.1016/j.rasd.2018.11.004
49. Harrop C, McBee M, and Boyd BA. How are child restricted and repetitive behaviors associated with caregiver stress over time? A parallel process multilevel growth model. J Autism Dev Disord. (2016) 46:1773–83. doi: 10.1007/s10803-016-2707-7
50. Zablotsky B, Anderson C, and Law P. The association between child autism symptomatology, maternal quality of life, and risk for depression. J Autism Dev Disord. (2013) 43:1946–55. doi: 10.1007/s10803-012-1745-z
51. Cappe É, Poirier N, Sankey C, Belzil A, and Dionne C. Quality of life of French Canadian parents raising a child with autism spectrum disorder and effects of psychosocial factors. Qual Life Res. (2018) 27:955–67. doi: 10.1007/s11136-017-1757-4
52. Mugno D, Ruta L, D’Arrigo VG, and Mazzone L. Impairment of quality of life in parents of children and adolescents with pervasive developmental disorder. Health Qual Life Outcomes. (2007) 5:22. doi: 10.1186/1477-7525-5-22
53. Einfeld SL and Tonge BJ. Population prevalence of psychopathology in children and adolescents with intellectual disability: II. Epidemiological findings. J Intellect Disabil Res. (1996) 40:99–109. doi: 10.1046/j.1365-2788.1996.768768.x
54. Totsika V, Hastings RP, Emerson E, Lancaster GA, Berridge DM, and Vagenas D. Is there a bidirectional relationship between maternal well-being and child behavior problems in autism spectrum disorders? Longitudinal analysis of a population-defined sample of young children. Autism Res. (2013) 6:201–11. doi: 10.1002/aur.2013.6.issue-3
55. Alasiri RM, Albarrak DA, Alghaith DM, Alsayari OS, Alqahtani YS, Bafarat AY, et al. Quality of life of autistic children and supported programs in Saudi Arabia: A cross-sectional study. Cureus. (2024) 16:e51645. doi: 10.7759/cureus.51645
56. Abd-Alnabi AL and Sachet KR. Assessment of quality of life among parents with autistic child. Pakistan J Med Health Sci. (2022) 16:964–7. doi: 10.53350/pjmhs22163964
57. Calonge-Torres MVJB, Reyes AL, Avendaño EL, Conducto CC, and Bautista ML. Quality of life of parents of children with autism spectrum disorder aged 3 to 18 years living in an urban area. Arch Dis Childhood. (2017) 102:A197–A8. doi: 10.1136/archdischild-2017-313087.491
58. Chen X, Tong J, Zhang W, Wang X, Ma S, Shi D, et al. Factors predicting depressive symptoms in parents of children with autism spectrum disorder in eastern China. BMC Public Health. (2024) 24:226. doi: 10.1186/s12889-024-17731-7
59. Papanikolaou K, Ntre V, Gertsou IM, Tagkouli E, Tzavara C, Pehlivanidis A, et al. Parenting children with autism spectrum disorder during crises: differential responses between the financial and the COVID-19 pandemic crisis. J Clin Med. (2022) 11:1–14. doi: 10.3390/jcm11051264
60. Cappe T. Effect of social and school inclusion on adjustment and quality of life of parents with a child having an autism spectrum disorder. Annales Medico-Psychologiques. (2012) 170:471–5. doi: 10.1016/j.amp.2012.06.015
61. Naheed A, Islam MS, Hossain SW, Ahmed HU, Uddin MMJ, Tofail F, et al. Burden of major depressive disorder and quality of life among mothers of children with autism spectrum disorder in urban Bangladesh. Autism Res. (2020) 13:284–97. doi: 10.1002/aur.v13.2
62. Samson AC, Phillips JM, Parker KJ, Shah S, Gross JJ, and Hardan AY. Emotion dysregulation and the core features of autism spectrum disorder. J Autism Dev Disord. (2014) 44:1766–72. doi: 10.1007/s10803-013-2022-5
63. Yamada A, Kato M, Suzuki M, Suzuki M, Watanabe N, Akechi T, et al. Quality of life of parents raising children with pervasive developmental disorders. BMC Psychiatry. (2012) 12:1–8. doi: 10.1186/1471-244X-12-119
Keywords: autism, parents, wellbeing, quality of life, children
Citation: Konowałek Ł, Kotowska-Bąbol M, Łukasik J, Remiszewski P and Wolańczyk T (2025) Quality of life among parents of autistic children: questionnaire validation study and multivariate analysis of associated factors. Front. Psychiatry 16:1554368. doi: 10.3389/fpsyt.2025.1554368
Received: 13 January 2025; Accepted: 14 April 2025;
Published: 09 July 2025.
Edited by:
Shuliweeh Alenezi, King Saud University, Saudi ArabiaReviewed by:
Shushan Liu, Shandong University, ChinaNeelam Muthu Lakshmi, Sri Padmavati Mahila Visvavidyalayam, India
Copyright © 2025 Konowałek, Kotowska-Bąbol, Łukasik, Remiszewski and Wolańczyk. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Piotr Remiszewski, czA5MDgzNkBzdHVkZW50Lnd1bS5lZHUucGw=
†These authors have contributed equally to this work
‡ORCID: Tomasz Wolańczyk, orcid.org/0000-0002-3223-5467
Jan Łukasik, orcid.org/0000-0002-9385-857X
 Łukasz Konowałek
Łukasz Konowałek Maja Kotowska-Bąbol
Maja Kotowska-Bąbol Jan Łukasik2‡
Jan Łukasik2‡ Piotr Remiszewski
Piotr Remiszewski