- 1Infection Control Office, Xi’an Public Health Center (Xi’an Emergency Medical Center), Xi’an, Shaanxi, China
- 2Virology Department, Ningxia Hui Autonomous Region Center for Disease Control and Prevention, Yinchuan, Ningxia, China
- 3Endemic Disease Control Division, Lianhu District Center for Disease Control and Prevention, Xi’an, Shaanxi, China
- 4Occupational Health Department, Weiyang District Center for Disease Control and Prevention, Xi’an, Shaanxi, China
- 5Preventive Healthcare Department, Yanta District Traditional Chinese Medicine Hospital, Xi’an, Shaanxi, China
Long COVID (LC) refers to a multisystem condition that persists after infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus responsible for coronavirus disease 2019 (COVID-19). In addition to physical symptoms, the psychological impact is particularly pronounced. This review summarizes the manifestations, potential mechanisms, epidemiological characteristics, and current interventions related to psychological disorders in LC. Drawing on domestic and international literature, it highlights anxiety, depression, cognitive dysfunction, and post-traumatic stress disorder (PTSD) as the primary psychological symptoms. These symptoms may be associated with neuroinflammation, immune abnormalities, vascular dysfunction, and psychosocial stress. Although research in this area is still developing, psychotherapy, pharmacotherapy, neuromodulation, and lifestyle interventions show promise as treatment approaches. This review aims to provide insights that can inform future research on clinical treatments and psychological care for individuals with LC.
1 Introduction
Since the outbreak of coronavirus disease 2019 (COVID-19) in 2019, hundreds of millions of people worldwide have been infected. Although the initial symptoms often subside within weeks for the majority of patients, 10%–20% of people encounter enduring or recurring symptoms, ultimately progressing to long COVID (LC) (1). A meta-analysis reported that 45% of COVID-19 survivors continue to experience unresolved symptoms after recovery (2). LC is a chronic, infection-related condition that manifests post-COVID-19, last for a minimum of three months, and is distinguished by a cycle of ongoing relapse and remission or escalating deterioration. It may impact one or more organ systems (3). Although COVID-19 is primarily considered a respiratory disease, it also invades the central and peripheral nervous systems, making it closely associated with various neuropsychiatric manifestations (4, 5). Additionally, it is often associated with significant psychological symptoms: around 30% of patients with LC have psychological symptoms such as exhaustion, while nearly 20% endure psychological disorders like despair, anxiety, and post-traumatic stress disorder (PTSD) (6, 7). Individuals with LC often experience high levels of anxiety and depression, which may result not only from persistent physical symptoms but also as a direct consequence of the initial SARS-CoV-2 infection (8). A systematic review and meta-analysis found that the prevalence of at least one symptom during follow-up was 52.6% among hospitalized patients and 34.5% among non-hospitalized patients (2). According to a study conducted in Wuhan, China, more than 55% of previously disorders COVID-19 patients continued to report symptoms two years after discharge (9). Another systematic review and meta-analysis indicated that three years after infection, the most common unresolved psychological symptoms in COVID-19 patients were fatigue and anxiety. This population tends to have poorer health-related quality of life (HRQoL), reduced physical function, more post-discharge psychological symptoms, and increased healthcare utilization, thereby imposing a substantial burden on both individuals and national healthcare systems (10).
Since the onset of the COVID-19 pandemic, the public has been facing unprecedented challenges and pressure related to psychological health (11). Psychological problems not only compromise patients’ quality of life and exacerbate physical illness but can also have significant economic and psychosocial implications (12). On December 7, 2022, China optimized its COVID-19 prevention and control policies, and from January 8, 2023, reclassified COVID-19 as a Category B infectious disease managed with Category B measures (13, 14). Since then, addressing LC and supporting recovery have become pressing issues in China. In a Lancet article entitled “China needs a scientific long COVID recovery-support platform,” Chinese scholars pointed out that there is currently no publicly accessible and authoritative platform in China to explain LC symptoms. As a result, the public lacks access to reliable scientific information, leading to insufficient understanding and awareness of LC. The absence of an official, credible source of information or support platform for LC patients may prolong or worsen their symptoms and contribute to psychological distress due to a lack of timely guidance (15).
To date, much of the focus on COVID-19 has centered on physical symptoms and outcomes. However, there is a growing recognition of the pandemic’s impact on psychological health and an urgent need for appropriate psychological health services to provide psychological support. Therefore, systematically reviewing the research progress on psychological symptoms in LC patients and exploring underlying mechanisms and intervention strategies is of great importance for improving psychological health outcomes and quality of life.
2 Stigmatization and psychological disorders in LC
2.1 Stigmatization
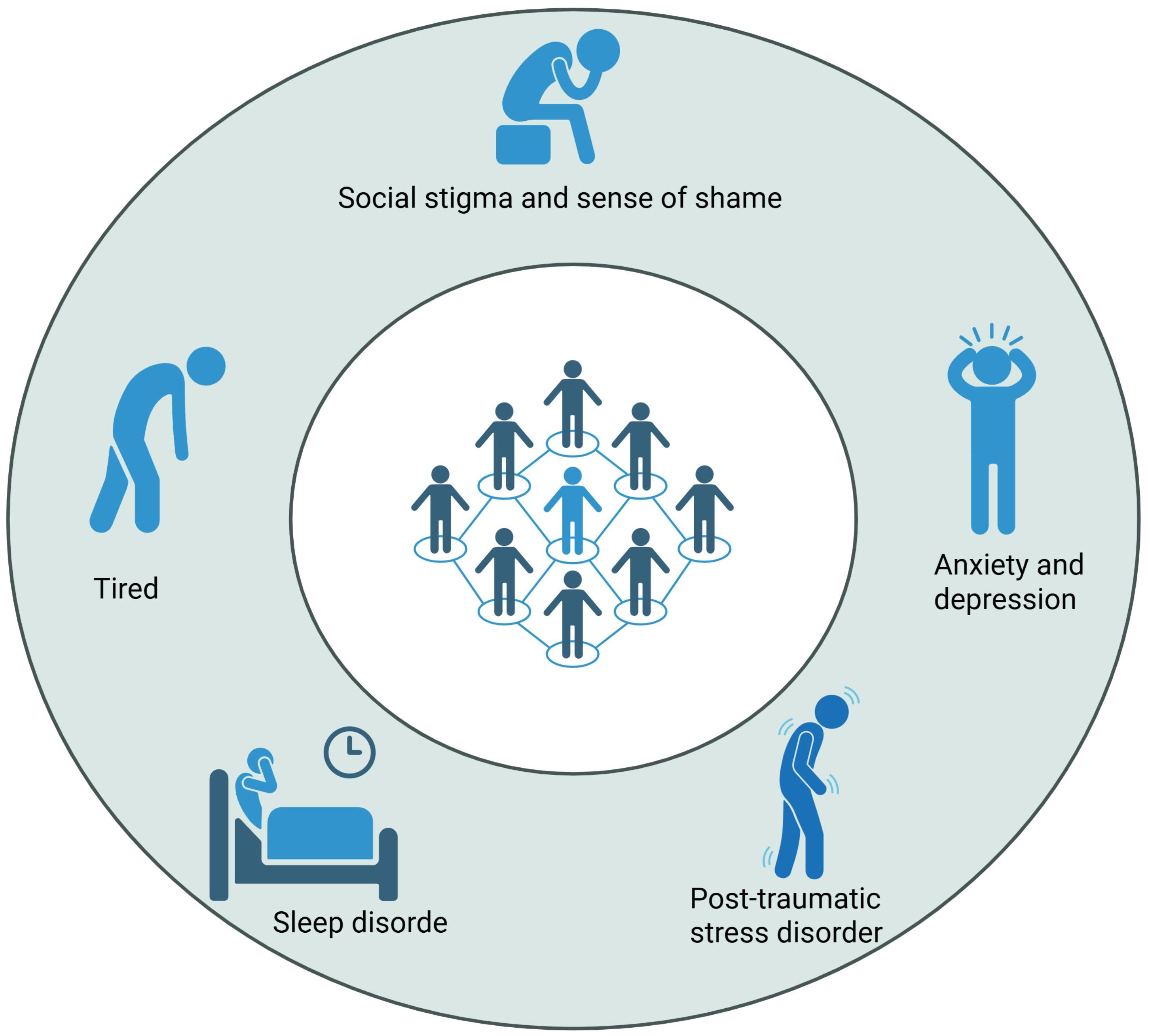
The stigmatization of psychological health issues can be subdivided into two dimensions: social stigma and illness-related shame. Social stigma refers to the negative attitudes and discrimination commonly faced by individuals suffering from health conditions and unexplained physical symptoms (16). During the COVID-19 pandemic and in the context of LC symptoms, the impact of social stigma on psychological health has been widely documented (17–19). Illness-related shame triggered by COVID-19 and LC rarely exists in isolation and is often accompanied by other forms of stigma. These stigmatizing experiences adversely affect individuals’ physical health and quality of life. The impact of social shame surrounding psychological health issues is a contributing factor to the deterioration of psychological well-being among LC patients. Shame can inhibit individuals from seeking help and sharing their experiences, potentially exacerbating feelings of isolation and distress (20). The spectrum of psychological problems associated with LC complicates recovery and intensifies the stigma related to psychological health (21). To reduce stigma and shame faced by individuals with long COVID, health education targeting the sources of social stigma and efforts to increase public awareness and understanding of the condition may represent an effective strategy (22).
2.2 Anxiety and depression
Anxiety and depression are the most common psychological disorders among LC patients (23). Anxiety symptoms typically include persistent worry, tension, irritability, inability to stop or control worrying, and feelings of nervousness and anxiety, which are among the most frequently reported symptoms. Depression primarily manifests as fatigue or lack of energy, low mood, sadness, or hopelessness, and in some cases, suicidal ideation (24). Some patients may also experience feelings of despair and diminished self-worth. Survivors exhibiting higher levels of anxiety and depression tend to more frequently express fear of COVID-19-related sequelae and report more symptoms post-discharge, especially fatigue and sleep disturbances (25, 26). A large body of literature has revealed that the challenges faced by COVID-19 survivors extend beyond physiological aspects, encompassing psychological stressors such as uncertainty related to the illness, social isolation, and financial burdens during recovery. Anxiety and depression symptoms may persist even after COVID-19 recovery, lasting up to 24 months (27).
2.3 Post-traumatic stress disorder
PTSD refers to a group of conditions triggered by trauma or other life stressors. COVID-19-related PTSD can result from both direct effects (the illness itself) and indirect consequences (living under stress, uncertainty, and changes in daily life), with PTSD symptoms potentially exacerbating other psychological disorders (28, 29). COVID-19 patients, particularly within months after hospital discharge, may experience PTSD symptoms (30). Some patients develop PTSD following intensive care treatment for severe COVID-19 or after losing loved ones. PTSD symptoms in LC patients can manifest in various ways, with commonly reported symptoms including intrusive thoughts related to the traumatic experience of COVID-19, increased anxiety, emotional numbness, and hyperarousal (31, 32). These symptoms significantly impair patients’ daily functioning and psychological health (33).
2.4 Fatigue
Fatigue is one of the most common symptoms of LC and can be defined as a decline in physical and/or mental performance caused by alterations in central, psychological, and/or peripheral factors related to COVID-19 (34). It is mainly characterized by fatigue that is not significantly relieved by rest, often accompanied by heterogeneous symptoms such as generalized body, muscle, and joint aches, mood disturbances, and sleep difficulties. Physical and laboratory examinations usually show no obvious abnormalities (35). While fatigue is a common and unavoidable symptom in daily life, LC patients experience a markedly increased burden of fatigue (36). Persistent fatigue is often associated with other symptoms such as dyspnea and cognitive impairment, which significantly impact the affected individuals’ quality of life and functional status (37).
2.5 Sleep disorders
Sleep disorders have become a major problem among LC patients. The types of sleep disturbances reported by LC patients are diverse, including insomnia, nightmares, excessive daytime sleepiness, and disrupted sleep architecture. Insomnia is one of the most common symptoms in LC patients, typically presenting as difficulty initiating sleep, frequent nocturnal awakenings, or early morning awakenings. Excessive daytime sleepiness is also a frequent neuropsychiatric manifestation; some LC patients experience difficulty maintaining wakefulness during the day, and some may meet diagnostic criteria for idiopathic hypersomnia or type 2 narcolepsy according to international sleep disorder classifications (38). LC patients often complain of poor sleep quality and feeling exhausted upon waking, with insufficient restoration of energy (39). Moreover, the relationship between sleep disorders and other neuropsychiatric symptoms such as anxiety and depression is well established. Sleep problems may be not only a direct consequence of viral infection but also closely related to psychological health (40).
2.6 Cognitive dysfunction
Cognitive dysfunction in LC patients is characterized by a range of symptoms, including memory decline, attention deficits, executive dysfunction, and reduced language fluency, often accompanied by psychological distress (41). A case-control study using the Addenbrooke’s Cognitive Examination III screening test found that the overall cognitive function of LC patients was significantly lower than that of recovered controls. Additionally, 48% of LC patients exhibited episodic memory deficits, with 27% showing overall cognitive impairment, particularly in attention, working memory, processing speed, and language fluency (41). Cognitive symptoms are often accompanied by other behavioral manifestations such as anxiety, depression, and sleep disorders, which collectively exacerbate the cognitive burden (42). Cognitive dysfunction related to LC is relatively common and persistent, affecting individuals across all age groups (43). The duration of cognitive impairment varies among patients; some experience symptom improvement after several weeks, whereas others suffer long-term cognitive problems that severely impact daily life and work performance (44, 45) (Figure 1).
3 Mechanisms of psychological disorders in LC
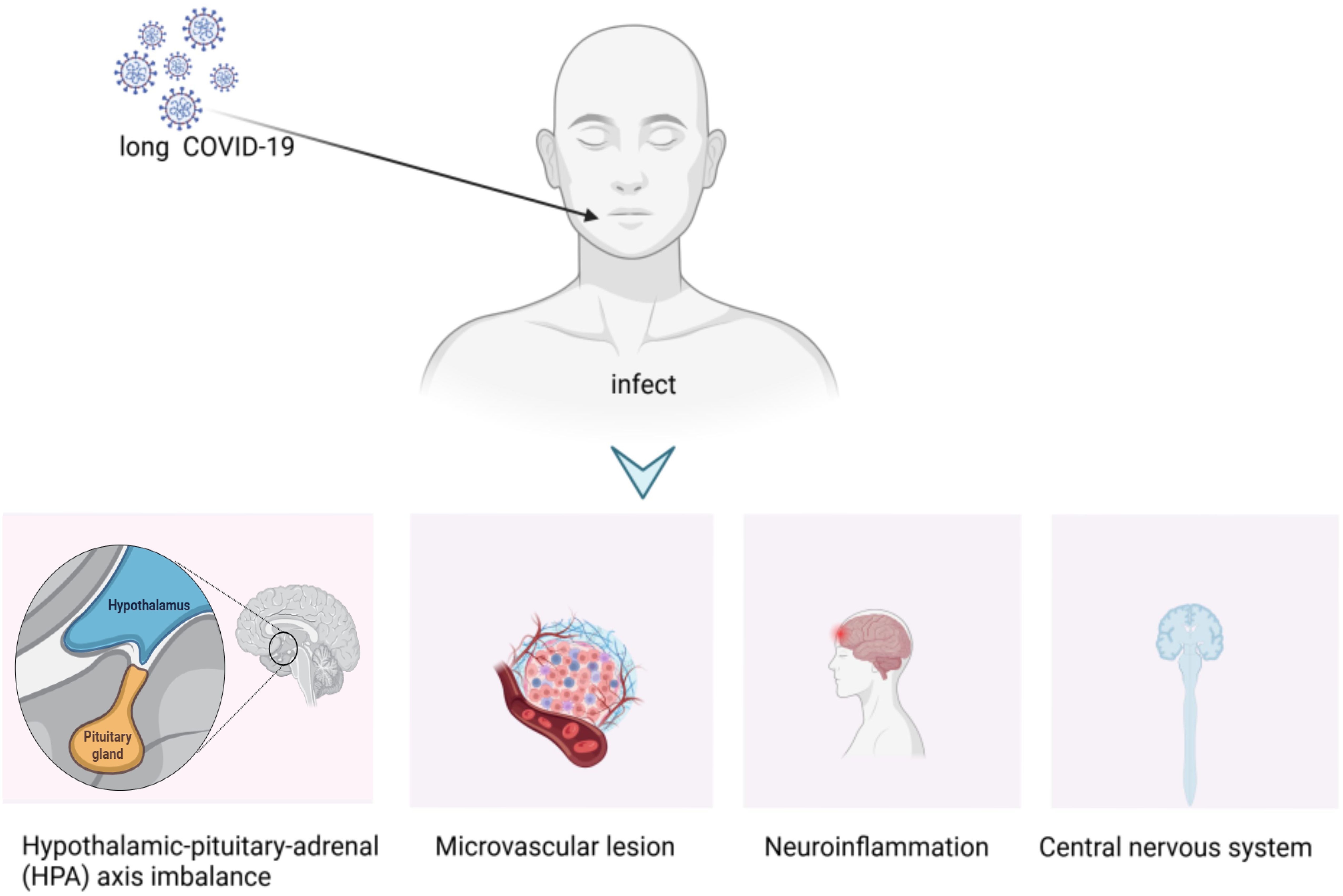
3.1 Direct viral invasion
Studies suggest that SARS-CoV-2 may persistently reside in tissue reservoirs within LC patients, triggering immune responses that contribute to symptom persistence (46–48). SARS-CoV-2 can enter the central nervous system (CNS) via multiple routes, including trans-synaptic transfer, the olfactory nerve, the blood-brain barrier, and hematogenous spread, leading to direct neuronal injury (49). This direct damage may contribute to the development of neuropsychiatric symptoms such as anxiety and depression, which are commonly observed in LC patients. Moreover, the continued presence of viral particles or remnants within the CNS may exacerbate inflammation, causing demyelination and neurodegenerative changes (50, 51), which in turn may trigger neuroinflammation and mental health issues (52, 53).
3.2 Immune dysregulation
Research has demonstrated that COVID-19 induces an overactive immune response, with increased cytokine release associated with various psychiatric disorders (54, 55). Depression and COVID-19 share similar immune functional patterns, particularly a pro-inflammatory state characterized by elevated cytokines including IL-6, TNFα, and IL-1β (56). Immune activation can impair neuronal function and affect brain plasticity (56). Prolonged immune activation is likely to disrupt brain function, especially in regions controlling emotion and cognition, such as the prefrontal cortex and hippocampus, leading to symptoms including depression, anxiety, and cognitive impairment. Recent studies support the long-term impairment of cognitive functions—especially executive function—and their association with inflammatory markers (57).
3.3 Neuroinflammation
Neuroinflammation results from the interaction between the virus and the immune system, causing the release of pro-inflammatory cytokines that affect brain function and emotional regulation. The immune response to SARS-CoV-2 may directly impact psychological health (58, 59). This inflammatory response can persist long after the acute phase of infection, contributing to chronic psychological issues observed in LC patients (60). Neuroinflammation is a prominent feature of LC, with studies demonstrating significant in vivo neuroinflammatory responses in LC patients (61). Widespread neuroinflammation in LC patients, which was associated with cognitive decline and structural brain changes such as cortical thinning and reductions in gray matter volume over time (58, 59). This neuroinflammatory state is thought to be driven by the immune response to the initial viral infection, leading to microglial activation and release of pro-inflammatory cytokines that can damage neuronal cells and disrupt synaptic function (62). Elevated levels of inflammatory markers in the cerebrospinal fluid of LC patients further support the role of neuroinflammation in the pathogenesis of neurological symptoms (63).
3.4 Vascular dysfunction
Vascular dysfunction contributes to the development of mood disorders because the brain’s ability to regulate emotions is closely linked to its vascular health. SARS-CoV-2 may directly affect the vascular system, causing endothelial dysfunction and microvascular injury, thereby exacerbating psychological disorders (64). Studies indicate that SARS-CoV-2 can trigger systemic vascular problems, especially in severely infected patients, where endothelial dysfunction and microvascular pathology are common. Inflammation-induced signaling caused by SARS-CoV-2 and endothelial cell dysfunction promotes a hypercoagulable state (65, 66). Microvascular thrombosis impairs oxygen exchange, and widespread cellular hypoxia may contribute to LC symptoms such as sleep disturbances, anxiety, and depression (67, 68).
3.5 Hypothalamic-pituitary-adrenal axis dysregulation
The physiological mechanisms of LC, particularly psychological disorders, may be closely related to dysregulation of the HPA axis. This dysregulation is a key neuroendocrine aspect of the stress and inflammatory response. Research shows that the HPA axis plays a critical role in the human stress response. SARS-CoV-2 can induce increased systemic inflammation, especially elevated levels of pro-inflammatory cytokines such as IL-6 and TNF-α, which may lead to hyperactivation of the HPA axis. Activation of the HPA axis results in the release of glucocorticoids, which are crucial for regulating immune responses and maintaining homeostasis (69). Cortisol levels influence brain regions involved in emotional regulation, and sustained high cortisol may be associated with the development of psychological symptoms such as anxiety and depression, which may partially explain the presence of such symptoms in LC patients (70, 71).
3.6 Psychosocial stress
Beyond biological mechanisms, psychosocial factors also play a significant role in the psychological symptoms experienced by LC patients (72). The experience of COVID-19 itself can cause substantial psychological stress, which may trigger or exacerbate pre-existing psychological issues. Studies show that individuals with a history of mental illness are at higher risk of developing new psychological problems post-infection, with factors such as social isolation, stigma, and stress related to coping with health uncertainty playing key roles (73, 74). The psychological impact of the COVID-19 pandemic, including fear of illness and disruptions to daily life, may contribute to disorders such as PTSD, anxiety, and depression (75, 76) (Figure 2).
4 Epidemiological characteristics of psychological symptoms in LC
4.1 Prevalence
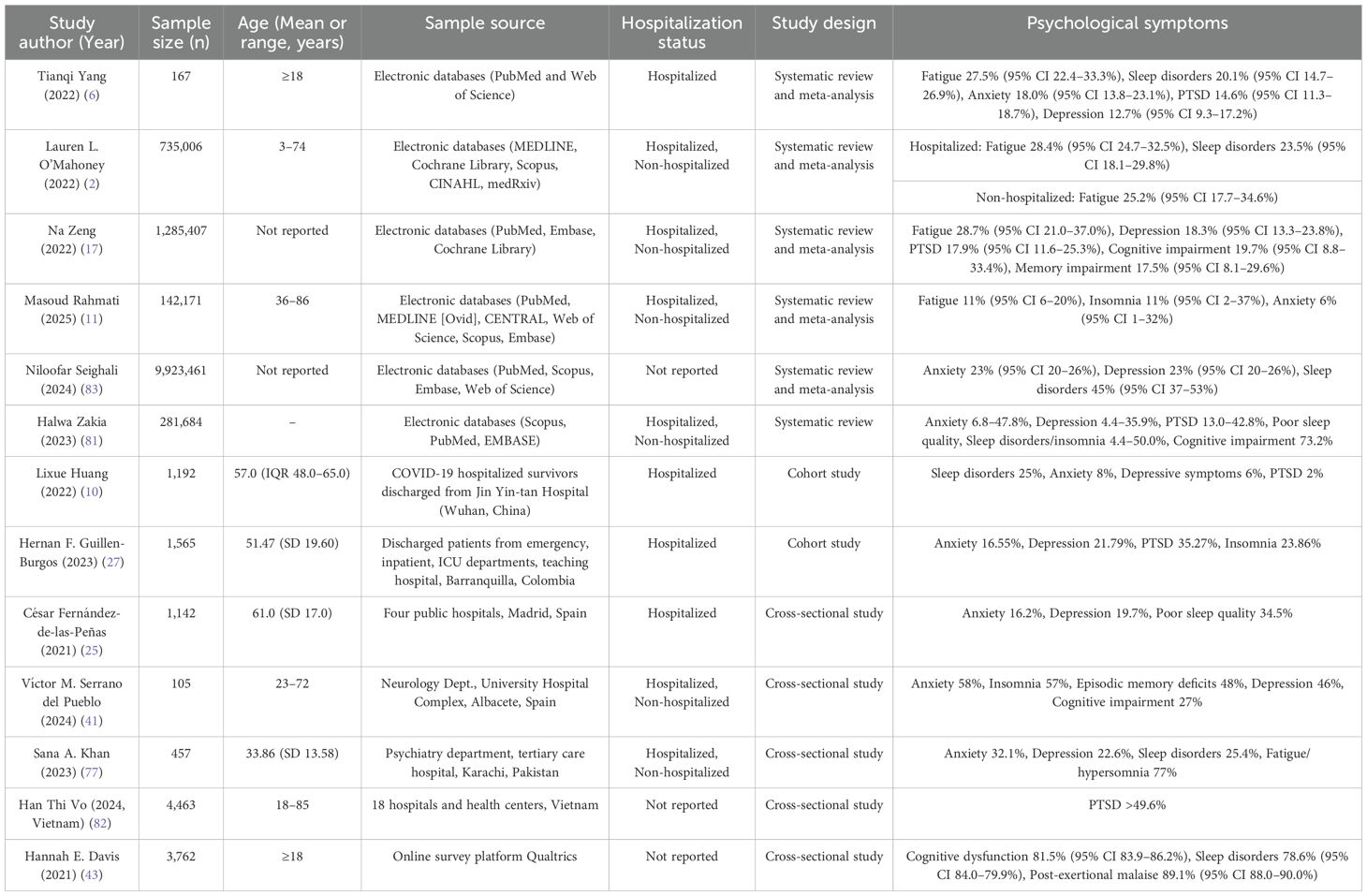
The occurrence of psychological symptoms is significantly higher among LC patients worldwide (77, 78). Studies reveal that approximately 30% of LC patients exhibit psychological symptoms. One survey found that the vast majority of LC patients have experienced some form of social exclusion, with 95.4% encountering social stigma at least occasionally and 75.9% experiencing it frequently (79). Due to heterogeneity in study populations and neuropsychological assessments, prevalence estimates vary considerably. Two meta-analyses estimated the overall prevalence of cognitive impairment to range between 14% and 22% (35, 80). The prevalence of anxiety symptoms ranges from 6.8% to 47.8%; depression from 4.4% to 35.9%; PTSD from 13.0% to 42.8%; and sleep disorders from 4.4% to 50.0% (81). Recent studies indicate that a substantial proportion of LC patients exhibit PTSD symptoms, with an estimated over 49% meeting diagnostic criteria for PTSD (82). A systematic review integrating data from 165 studies involving 9,923,461 patients showed that among COVID-19 survivors, the prevalence rates for depression and anxiety were both 23%, and sleep disorders 45% (83) (Table 1). An online survey including 3,726 participants from 56 countries reported a 78.6% prevalence of sleep disturbances over more than seven months of follow-up, including insomnia (60%), night sweats (41%), awakening with breathing difficulty (36%), restless legs syndrome (18%), and sleep apnea (10%) (43). Variability in reported prevalence rates of psychological symptoms across studies may be attributed to differences in study design, assessment methods, sociocultural contexts, viral variants, and demographic characteristics. Furthermore, different systematic reviews and meta-analyses include varying ranges of literature, contributing to discrepancies in prevalence estimates. The duration of psychological symptoms in LC varies individually; most patients experience symptom improvement within months post-infection, but some persist beyond six months, even exceeding 24 months, with relapsing episodes (10).
4.2 Risk factors
Among demographic factors, female sex is consistently identified as an important risk factor. Research shows that females are more likely than males to develop psychological symptoms such as anxiety and depression. A prospective cohort study on females with LC found that the proportion of females experiencing most physical symptoms and all psychological symptoms was higher than males (84). This difference may be attributed to social expectations, the psychological burden of caregiving roles typically assumed by women, and hormonal influences (20, 85). However, some studies have shown that anxiety symptoms in male LC patients are higher than in females, which may be due to the small male sample size and limited representativeness in that particular study (20), individuals with a history of psychological health disorders such as anxiety or depression have a significantly higher risk of developing psychological problems in LC (86). During the pandemic, older adults faced more severe physical symptoms, whereas younger individuals appeared to be at higher risk for poor psychological functioning (87). This may be related to the emotional advantages associated with older age, which declined during the COVID-19 pandemic but still persisted (20). COVID-19 may trigger or worsen common chronic conditions in the elderly, such as cardiovascular disease, respiratory illness, neurodegenerative diseases, and functional decline; they may also have experienced bereavement during the pandemic, leading to physical and psychological frailty (88). Some studies suggest that younger populations may be more susceptible to the cognitive and psychosocial impacts of COVID-19 (72), and compared with older adults, younger individuals may have poorer capacity to regulate negative emotions related to the pandemic (89). Moreover, lower educational attainment and socioeconomic status have been associated with increased risk of psychological problems after the COVID-19 pandemic (90). Clinically, survivors with a history of mental illness or substance use are particularly prone to anxiety and depression symptoms post-infection (91). Patients with severe COVID-19 symptoms, especially those requiring hospitalization or intensive care, have a higher risk of developing psychological symptoms, notably PTSD (92). The coexistence of chronic diseases exacerbates psychological distress, as individuals must cope with both physical and psychological health challenges (90). Furthermore, COVID-19-related stigma has been recognized as a novel risk factor, inducing anxiety and distress among survivors (93). Regarding environmental factors, the context of the COVID-19 pandemic has been a significant contributor to psychological symptoms associated with LC (94). The widespread social isolation and lockdown measures have increased feelings of loneliness and anxiety among various populations (95).
5 Measures to improve psychological symptoms of LC
5.1 Psychotherapy
Cognitive Behavioral Therapy (CBT) is a common psychotherapeutic approach that alleviates psychological distress by identifying and modifying negative thought patterns and behaviors (96). CBT is widely applied and has shown good efficacy in the intervention of psychological symptoms in LC (97, 98). Studies indicate that CBT can effectively reduce anxiety, depression, insomnia, and fatigue symptoms in LC patients (99, 100). By altering patients’ negative cognitive patterns, CBT helps them adopt a more positive attitude toward illness and recovery. Additionally, other psychotherapies such as mindfulness therapy (101), meditation, and relaxation training have demonstrated beneficial effects. However, it is important to avoid repeated recounting of traumatic experiences to prevent secondary trauma (102). For patients with severe psychiatric disorders, early psychiatric specialist intervention is recommended. Moreover, enhancing the inclusivity of social support is an important strategy to improve the psychological health of LC patients (103).
5.2 Pharmacotherapy
For patients with more severe symptoms, pharmacological treatment can complement psychotherapy (104). Pharmacological approaches to treating psychological symptoms in LC typically involve antidepressants and anxiolytics. Selective serotonin reuptake inhibitors (SSRIs) and other classes of antidepressants have been shown to effectively treat common depression and anxiety symptoms in this population (105). Short-term use of anxiolytics, such as benzodiazepines, may be helpful for patients with prominent anxiety symptoms (106). The link between inflammation and psychological health is well established, with elevated pro-inflammatory cytokines (e.g., IL-6 and TNF-α) implicated in the pathogenesis of mood disorders; thus, adjunctive anti-inflammatory treatments may be an important strategy for managing psychiatric conditions (107). Nevertheless, long-term use of medications should be cautious and conducted under professional medical supervision.
5.3 Neuromodulation therapy
Non-invasive brain stimulation (NIBS) plays a significant role in improving psychological symptoms in LC. Neuromodulation techniques such as transcranial magnetic stimulation (TMS), deep brain stimulation (DBS), and vagus nerve stimulation (VNS) have demonstrated efficacy in treating anxiety and depression and are applicable in LC health management (108). TMS, which uses magnetic fields to stimulate specific brain regions and enhance neuroplasticity, has been used to treat treatment-resistant depression. TMS effectively improves depressive symptoms and cognitive impairment in LC patients (109). Transcutaneous auricular VNS exerts anti-inflammatory, analgesic, and antidepressant effects, showing beneficial impact on fatigue syndrome in LC patients (110). These techniques modulate neural activity in targeted brain areas, thereby influencing neural circuits involved in emotion and physiological responses, and are particularly suitable for patients resistant to pharmacotherapy (111).
5.4 Hyperbaric oxygen therapy
HBOT involves treatment with 100% oxygen at pressures exceeding one absolute atmosphere (ATA), enhancing oxygen delivery to tissues, reducing inflammation, and promoting healing (112, 113). HBOT is used for various medical conditions, including trauma, hypoxia, infections, and certain chronic diseases. Recently, HBOT has been explored as a potential treatment for some LC-related symptoms (114). HBOT can alleviate several symptoms associated with LC, including depression, fatigue, and cognitive dysfunction (113, 115). Its safety and efficacy have been well established, making it a feasible option for LC treatment (116).
5.5 Lifestyle interventions
Lifestyle interventions have been identified as potential means to improve psychological symptoms associated with LC (117). Exercise and diet, as adjunctive treatments, play roles in alleviating psychological symptoms in LC patients. Moderate physical activity, especially aerobic exercise, helps improve mood and cognitive function (118). Maintaining regular sleep routines also benefits anxiety, depression, and stress (119). A balanced diet rich in antioxidants and anti-inflammatory compounds may help reduce neuroinflammation and alleviate psychological symptoms. Sleep disturbances related to LC are associated with inflammation, and nutrients such as zinc, vitamins C and D, and polyphenols may improve inflammation and sleep quality, thereby reducing symptoms (120). Coenzyme Q10 and alpha-lipoic acid, alone or combined with acetyl-L-carnitine as part of dietary interventions, have shown efficacy in reducing fatigue (121, 122). In summary, lifestyle interventions—including physical activity, sleep management, and nutritional support—are critical for mitigating psychological symptoms associated with LC.
5.6 Social support and rehabilitation programs
The establishment of social support systems is crucial for alleviating psychological symptoms in LC patients. Communities and families should provide emotional support to help patients cope positively with life’s challenges (123). Additionally, personalized rehabilitation programs should be developed, focusing not only on physical recovery but also integrating psychological support tailored to individual experiences and needs, assisting patients in gradually rebuilding a normal life (124). These programs are recommended to be designed by multidisciplinary teams, including psychiatrists, psychologists, and psychiatric nurses (125). Ongoing research is needed to evaluate the effectiveness of digital solutions and tailor them to the unique needs of long COVID patients (126). A combined approach of pharmacotherapy and psychological intervention is generally advised to address the multifaceted nature of LC. One study showed that combining cognitive behavioral therapy with pharmacotherapy (including non-benzodiazepine sedatives) significantly improved patients’ psychological health outcomes (8). The combination of NIBS and aerobic exercise therapy has also been used to improve the quality of life and reduce fatigue in LC patients (127).
With the continuous mutation of the novel coronavirus and the rising number of COVID-19 cases worldwide, many individuals have suffered from persistent long-term symptoms (128, 129). Notably, psychological symptoms often last longer than physical symptoms (130, 131). Research on psychological symptoms related to LC is gradually deepening, but many challenges remain, such as inconsistent diagnostic criteria, lack of long-term follow-up studies, and insufficient treatment strategies (43, 132). Given the prolonged duration and high prevalence of LC-related psychological symptoms, integrating psychological health care into comprehensive LC treatment plans is essential (133). Existing evidence suggests that psychotherapy, pharmacological interventions, and social support can effectively improve patients’ psychological health (134).
The psychological impact of LC is multidimensional and complex, involving a broad spectrum of symptoms, underlying pathophysiological mechanisms, and unique epidemiological characteristics. This review systematically summarized LC-associated psychological symptoms, including social stigma and shame, anxiety and depression, PTSD, fatigue, sleep disturbances, and cognitive dysfunction, all of which significantly reduce patients’ quality of life and social functioning. The underlying mechanisms may involve the interplay of direct viral invasion of the central nervous system, immune dysregulation and neuroinflammation, vascular dysfunction, HPA axis dysregulation, and psychosocial stress.
Current integrated interventions for these psychological symptoms include psychotherapy (e.g., cognitive behavioral therapy), pharmacotherapy (e.g., antidepressants), neuromodulation techniques (e.g., transcranial magnetic stimulation), hyperbaric oxygen therapy, lifestyle modifications (e.g., exercise and sleep management), and social support and rehabilitation programs. However, the long-term efficacy of existing treatments requires further validation, and the development of individualized intervention strategies is particularly important. Future research should further explore the deeper connections among these mechanisms to develop more personalized and refined intervention approaches, ultimately helping patients achieve better recovery.
Author contributions
SS: Writing – original draft, Writing – review & editing. XZ: Writing – original draft, Writing – review & editing. JP: Investigation, Writing – review & editing. BW: Investigation, Writing – review & editing. JHo: Investigation, Writing – review & editing. RC: Investigation, Writing – review & editing. YG: Writing – review & editing. FL: Writing – review & editing. JHa: Writing – review & editing. ZW: Conceptualization, Writing - review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. Medical Research Fund of Xi’an Science and Technology Bureau (22YXYJ0073); Scientific Research Project of Xi’an Health Commission (2023yb27). Ningxia Natural Science Foundation: (No: 2024AAC03734).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wulf Hanson S, Abbafati C, Aerts JG, Al-Aly Z, Ashbaugh C, Ballouz T, et al. Estimated global proportions of individuals with persistent fatigue, cognitive, and respiratory symptom clusters following symptomatic COVID-19 in 2020 and 2021. Jama. (2022) 328:1604–15. doi: 10.1001/jama.2022.18931
2. O’Mahoney LL, Routen A, Gillies C, Ekezie W, Welford A, Zhang A, et al. The prevalence and long-term health effects of Long Covid among hospitalised and non-hospitalised populations: A systematic review and meta-analysis. EClinicalMedicine. (2023) 55:101762. doi: 10.1016/j.eclinm.2022.101762
3. Greenhalgh T, Sivan M, Perlowski A, and Nikolich J. Long COVID: a clinical update. Lancet. (2024) 404:707–24. doi: 10.1016/S0140-6736(24)01136-X
4. Doyle MF. Central nervous system outcomes of COVID-19. Transl Res. (2022) 241:41–51. doi: 10.1016/j.trsl.2021.09.002
5. Lin LC, Hollis B, and Hefti MM. Neuropathology of COVID-19. Indian J Pathol Microbiol. (2022) 65:S146–s52. doi: 10.4103/ijpm.ijpm_1103_21
6. Yang T, Yan MZ, Li X, and Lau EHY. Sequelae of COVID-19 among previously hospitalized patients up to 1 year after discharge: a systematic review and meta-analysis. Infection. (2022) 50:1067–109. doi: 10.1007/s15010-022-01862-3
7. Zeng N, Zhao YM, Yan W, Li C, Lu QD, Liu L, et al. A systematic review and meta-analysis of long term physical and mental sequelae of COVID-19 pandemic: call for research priority and action. Mol Psychiatry. (2023) 28:423–33. doi: 10.1038/s41380-022-01614-7
8. Fancourt D, Steptoe A, and Bu F. Psychological consequences of long COVID: comparing trajectories of depressive and anxiety symptoms before and after contracting SARS-CoV-2 between matched long- and short-COVID groups. Br J Psychiatry. (2023) 222:74–81. doi: 10.1192/bjp.2022.155
9. Rahmati M, Udeh R, Kang J, Dolja-Gore X, McEvoy M, Kazemi A, et al. Long-term sequelae of COVID-19: A systematic review and meta-analysis of symptoms 3 years post-SARS-coV-2 infection. J Med Virol. (2025) 97:e70429. doi: 10.1002/jmv.70429
10. Huang L, Li X, Gu X, Zhang H, Ren L, Guo L, et al. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: a longitudinal cohort study. Lancet Respir Med. (2022) 10:863–76. doi: 10.1016/S2213-2600(22)00126-6
11. Greenwood DC, Mansoubi M, Bakerly ND, Bhatia A, Collett J, Davies HE, et al. Physical, cognitive, and social triggers of symptom fluctuations in people living with long COVID: an intensive longitudinal cohort study. Lancet Reg Health Eur. (2024) 46:101082. doi: 10.1016/j.lanepe.2024.101082
12. Schäfer IC, Krehbiel J, Adler W, Borho A, Herold R, Greiner B, et al. Three-month follow-up of the post-COVID syndrome after admission to a specialised post-COVID centre-A prospective study focusing on mental health with patient reported outcome measures (PROMs). Int J Environ Res Public Health. (2024) 21(8):1076. doi: 10.3390/ijerph21081076
13. Agency XN. The Joint Prevention and Control Mechanism of the State Council Issued the “Notice on Further Optimizing and Implementing COVID-19 Prevention and Control Measures” (2022). Available online at: https://www.gov.cn/xinwen/2022-12/07/content_5730475.htm. (Accessed June 21, 2025).
14. Agency XN. Major Adjustment! COVID-19 Infection Classification Adjusted from “Category B Management as Category A” to “Category B Management” (2022). Available online at: https://www.gov.cn/xinwen/2022-12/27/content_5733672.htm. (Accessed June 21, 2025).
15. Tan H, Liu J, and Zeng F. China needs a scientific long COVID recovery-support platform. Lancet. (2023) 401:344–5. doi: 10.1016/S0140-6736(23)00138-1
16. Van de Vyver J, Leite AC, and Alwan NA. Navigating the social identity of long covid. Bmj. (2021) 375:n2933. doi: 10.1136/bmj.n2933
17. Yuan K, Huang XL, Yan W, Zhang YX, Gong YM, Su SZ, et al. A systematic review and meta-analysis on the prevalence of stigma in infectious diseases, including COVID-19: a call to action. Mol Psychiatry. (2022) 27:19–33. doi: 10.1038/s41380-021-01295-8
18. Macpherson K, Cooper K, Harbour J, Mahal D, Miller C, and Nairn M. Experiences of living with long COVID and of accessing healthcare services: a qualitative systematic review. BMJ Open. (2022) 12:e050979. doi: 10.1136/bmjopen-2021-050979
19. Koller JE, Villinger K, Lages NC, Brünecke I, Debbeler JM, Engel KD, et al. Stigmatization of Chinese and Asian-looking people during the COVID-19 pandemic in Germany. BMC Public Health. (2021) 21:1296. doi: 10.1186/s12889-021-11270-1
20. Schröder D, Schmachtenberg T, Heinemann S, Müllenmeister C, Roder S, El-Sayed I, et al. Parenting and gender as impact factors for social participation, quality of life, and mental health in long COVID. J Prim Care Community Health. (2024) 15:21501319241255592. doi: 10.1177/21501319241255592
21. Saltzman LY, Longo M, and Hansel TC. Long-COVID stress symptoms: Mental health, anxiety, depression, or posttraumatic stress. Psychol Trauma. (2024) 16:1169–78. doi: 10.1037/tra0001567
22. Stangl AL, Earnshaw VA, Logie CH, van Brakel W, CS L, Barré I, et al. The Health Stigma and Discrimination Framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. (2019) 17:31. doi: 10.1186/s12916-019-1271-3
23. Ruiyin W, Qi J, Tingting W, Yuqin Y, Yan J, and Kun P. Long COVID outcomes following omicron wave in non-hospital population. Front Public Health. (2024) 12:1377866. doi: 10.3389/fpubh.2024.1377866
24. Martins S, Ferreira AR, Fernandes J, Vieira T, Fontes L, Coimbra I, et al. Depressive and anxiety symptoms in severe COVID-19 survivors: A prospective cohort study. Psychiatr Q. (2022) 93:891–903. doi: 10.1007/s11126-022-09998-z
25. Fernández-de-Las-Peñas C, Gómez-Mayordomo V, de-la-Llave-Rincón AI, Palacios-Ceña M, Rodríguez-Jiménez J, Florencio LL, et al. Anxiety, depression and poor sleep quality as long-term post-COVID sequelae in previously hospitalized patients: A multicenter study. J Infect. (2021) 83:496–522. doi: 10.1016/j.jinf.2021.06.022
26. Shanbehzadeh S, Tavahomi M, Zanjari N, Ebrahimi-Takamjani I, and Amiri-Arimi S. Physical and mental health complications post-COVID-19: Scoping review. J Psychosom Res. (2021) 147:110525. doi: 10.1016/j.jpsychores.2021.110525
27. Guillen-Burgos HF, Galvez-Florez JF, Moreno-Lopez S, Gonzalez I, Guillen M, and Anaya JM. Factors associated with mental health outcomes after COVID-19: A 24-month follow-up longitudinal study. Gen Hosp Psychiatry. (2023) 84:241–9. doi: 10.1016/j.genhosppsych.2023.08.009
28. Mazza MG, Palladini M, De Lorenzo R, Magnaghi C, Poletti S, Furlan R, et al. Persistent psychopathology and neurocognitive impairment in COVID-19 survivors: Effect of inflammatory biomarkers at three-month follow-up. Brain Behav Immun. (2021) 94:138–47. doi: 10.1016/j.bbi.2021.02.021
29. Poyraz B, Poyraz CA, Olgun Y, Gürel Ö, Alkan S, Özdemir YE, et al. Psychiatric morbidity and protracted symptoms after COVID-19. Psychiatry Res. (2021) 295:113604. doi: 10.1016/j.psychres.2020.113604
30. Huang L, Xu X, Zhang L, Zheng D, Liu Y, Feng B, et al. Post-traumatic stress disorder symptoms and quality of life of COVID-19 survivors at 6-month follow-up: A cross-sectional observational study. Front Psychiatry. (2021) 12:782478. doi: 10.3389/fpsyt.2021.782478
31. Janiri D, Carfì A, Kotzalidis GD, Bernabei R, Landi F, and Sani G. Posttraumatic stress disorder in patients after severe COVID-19 infection. JAMA Psychiatry. (2021) 78:567–9. doi: 10.1001/jamapsychiatry.2021.0109
32. Liu D, Baumeister RF, Veilleux JC, Chen C, Liu W, Yue Y, et al. Risk factors associated with mental illness in hospital discharged patients infected with COVID-19 in Wuhan, China. Psychiatry Res. (2020) 292:113297. doi: 10.1016/j.psychres.2020.113297
33. Marchi M, Grenzi P, Serafini V, Capoccia F, Rossi F, Marrino P, et al. Psychiatric symptoms in Long-COVID patients: a systematic review. Front Psychiatry. (2023) 14:1138389. doi: 10.3389/fpsyt.2023.1138389
34. Rudroff T, Fietsam AC, Deters JR, Bryant AD, and Kamholz J. Post-COVID-19 fatigue: potential contributing factors. Brain Sci. (2020) 10(12):1012. doi: 10.3390/brainsci10121012
35. Ceban F, Ling S, Lui LMW, Lee Y, Gill H, Teopiz KM, et al. Fatigue and cognitive impairment in Post-COVID-19 Syndrome: A systematic review and meta-analysis. Brain Behav Immun. (2022) 101:93–135. doi: 10.1016/j.bbi.2021.12.020
36. Koleničová V, Vňuková MS, Anders M, Fišerová M, Raboch J, and Ptáček R. A review article on exercise intolerance in long COVID: unmasking the causes and optimizing treatment strategies. Med Sci Monit. (2023) 29:e941079. doi: 10.12659/MSM.941079
37. Righi E, Mirandola M, Mazzaferri F, Dossi G, Razzaboni E, Zaffagnini A, et al. Determinants of persistence of symptoms and impact on physical and mental wellbeing in Long COVID: A prospective cohort study. J Infect. (2022) 84:566–72. doi: 10.1016/j.jinf.2022.02.003
38. Morelli-Zaher C, Vremaroiu-Coman A, Coquoz N, Genecand L, Altarelli M, Binkova A, et al. Post-COVID central hypersomnia, a treatable trait in long COVID: 4 case reports. Front Neurol. (2024) 15:1349486. doi: 10.3389/fneur.2024.1349486
39. Hoang HTX, Yeung WF, Truong QTM, Le CT, Bui ATM, Bui QV, et al. Sleep quality among non-hospitalized COVID-19 survivors: a national cross-sectional study. Front Public Health. (2023) 11:1281012. doi: 10.3389/fpubh.2023.1281012
40. Paranhos ACM, Dias ARN, Bastos TDR, Rodrigues AN, Santana KHY, Dias LHA, et al. Persistent olfactory dysfunction associated with poor sleep quality and anxiety in patients with long COVID. Front Neurosci. (2023) 17:1161904. doi: 10.3389/fnins.2023.1161904
41. Serrano Del Pueblo VM, Serrano-Heras G, Romero Sánchez CM, Landete PP, Rojas-Bartolome L, Feria I, et al. Brain and cognitive changes in patients with long COVID compared with infection-recovered control subjects. Brain. (2024) 147:3611–23. doi: 10.1093/brain/awae101
42. Taube M. Depression and brain fog as long-COVID mental health consequences: Difficult, complex and partially successful treatment of a 72-year-old patient-A case report. Front Psychiatry. (2023) 14:1153512. doi: 10.3389/fpsyt.2023.1153512
43. Davis HE, Assaf GS, McCorkell L, Wei H, Low RJ, Re’em Y, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine. (2021) 38:101019. doi: 10.1016/j.eclinm.2021.101019
44. Leitner M, Pötz G, Berger M, Fellner M, Spat S, and Koini M. Characteristics and burden of acute COVID-19 and long-COVID: Demographic, physical, mental health, and economic perspectives. PloS One. (2024) 19:e0297207. doi: 10.1371/journal.pone.0297207
45. Schild AK, Scharfenberg D, Regorius A, Klein K, Kirchner L, Yasemin G, et al. Six-month follow-up of multidomain cognitive impairment in non-hospitalized individuals with post-COVID-19 syndrome. Eur Arch Psychiatry Clin Neurosci. (2024) 274:1945–57. doi: 10.1007/s00406-024-01863-3
46. Proal AD, VanElzakker MB, Aleman S, Bach K, Boribong BP, Buggert M, et al. Author Correction: SARS-CoV-2 reservoir in post-acute sequelae of COVID-19 (PASC). Nat Immunol. (2023) 24:1778. doi: 10.1038/s41590-023-01646-3
47. Desimmie BA, Raru YY, Awadh HM, He P, Teka S, and Willenburg KS. Insights into SARS-coV-2 persistence and its relevance. Viruses. (2021) 13(6):1025. doi: 10.3390/v13061025
48. Jacobs JJL. Persistent SARS-2 infections contribute to long COVID-19. Med Hypotheses. (2021) 149:110538. doi: 10.1016/j.mehy.2021.110538
49. Bougakov D, Podell K, and Goldberg E. Multiple neuroinvasive pathways in COVID-19. Mol Neurobiol. (2021) 58:564–75. doi: 10.1007/s12035-020-02152-5
50. Tang SW, Leonard BE, and Helmeste DM. Long COVID, neuropsychiatric disorders, psychotropics, present and future. Acta Neuropsychiatr. (2022) 34:109–26. doi: 10.1017/neu.2022.6
51. Thye AY, Law JW, Tan LT, Pusparajah P, Ser HL, Thurairajasingam S, et al. Psychological symptoms in COVID-19 patients: insights into pathophysiology and risk factors of long COVID-19. Biol (Basel). (2022) 11(1):61. doi: 10.3390/biology11010061
52. Abdel Hafez SMN. Can Covid-19 attack our nervous system? J Chem Neuroanat. (2021) 117:102006. doi: 10.1016/j.jchemneu.2021.102006
53. Wan D, Du T, Hong W, Chen L, Que H, Lu S, et al. Neurological complications and infection mechanism of SARS-COV-2. Signal Transduct Target Ther. (2021) 6:406. doi: 10.1038/s41392-021-00818-7
54. Raony Í, de Figueiredo CS, Pandolfo P, Giestal-de-Araujo E, Oliveira-Silva Bomfim P, and Savino W. Psycho-neuroendocrine-immune interactions in COVID-19: potential impacts on mental health. Front Immunol. (2020) 11:1170. doi: 10.3389/fimmu.2020.01170
55. Bower JE, Radin A, and Kuhlman KR. Psychoneuroimmunology in the time of COVID-19: Why neuro-immune interactions matter for mental and physical health. Behav Res Ther. (2022) 154:104104. doi: 10.1016/j.brat.2022.104104
56. Perlmutter A. Immunological interfaces: the COVID-19 pandemic and depression. Front Neurol. (2021) 12:657004. doi: 10.3389/fneur.2021.657004
57. He D, Yuan M, Dang W, Bai L, Yang R, Wang J, et al. Long term neuropsychiatric consequences in COVID-19 survivors: Cognitive impairment and inflammatory underpinnings fifteen months after discharge. Asian J Psychiatr. (2023) 80:103409. doi: 10.1016/j.ajp.2022.103409
58. Rothstein TL. Cortical Grey matter volume depletion links to neurological sequelae in post COVID-19 “long haulers. BMC Neurol. (2023) 23:22. doi: 10.1186/s12883-023-03049-1
59. Douaud G, Lee S, Alfaro-Almagro F, Arthofer C, Wang C, McCarthy P, et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. (2022) 604:697–707. doi: 10.1038/s41586-022-04569-5
60. Kumar S, Veldhuis A, and Malhotra T. Neuropsychiatric and cognitive sequelae of COVID-19. Front Psychol. (2021) 12:577529. doi: 10.3389/fpsyg.2021.577529
61. Phetsouphanh C, Darley DR, Wilson DB, Howe A, Munier CML, Patel SK, et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat Immunol. (2022) 23:210–6. doi: 10.1038/s41590-021-01113-x
62. Müller L and Di Benedetto S. Aged brain and neuroimmune responses to COVID-19: post-acute sequelae and modulatory effects of behavioral and nutritional interventions. Immun Ageing. (2023) 20:17. doi: 10.1186/s12979-023-00341-z
63. Wei ZD, Liang K, and Shetty AK. Role of microglia, decreased neurogenesis and oligodendrocyte depletion in long COVID-mediated brain impairments. Aging Dis. (2023) 14:1958–66. doi: 10.14336/AD.2023.10918
64. Kempuraj D, Aenlle KK, Cohen J, Mathew A, Isler D, Pangeni RP, et al. COVID-19 and long COVID: disruption of the neurovascular unit, blood-brain barrier, and tight junctions. Neuroscientist. (2024) 30:421–39. doi: 10.1177/10738584231194927
65. Li T, Yang Y, Li Y, Wang Z, Ma F, Luo R, et al. Platelets mediate inflammatory monocyte activation by SARS-CoV-2 spike protein. J Clin Invest. (2022) 132. doi: 10.1172/JCI150101
66. Fard MB, Fard SB, Ramazi S, Atashi A, and Eslamifar Z. Thrombosis in COVID-19 infection: Role of platelet activation-mediated immunity. Thromb J. (2021) 19:59. doi: 10.1186/s12959-021-00311-9
67. Zuin M, Engelen MM, Barco S, Spyropoulos AC, Vanassche T, Hunt BJ, et al. Incidence of venous thromboembolic events in COVID-19 patients after hospital discharge: A systematic review and meta-analysis. Thromb Res. (2022) 209:94–8. doi: 10.1016/j.thromres.2021.11.029
68. Pretorius E, Vlok M, Venter C, Bezuidenhout JA, Laubscher GJ, Steenkamp J, et al. Persistent clotting protein pathology in Long COVID/Post-Acute Sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin. Cardiovasc Diabetol. (2021) 20:172. doi: 10.1186/s12933-021-01359-7
69. Iadecola C, Anrather J, and Kamel H. Effects of COVID-19 on the nervous system. Cell. (2020) 183:16–27.e1. doi: 10.1016/j.cell.2020.08.028
70. Elder GJ, Altena E, Palagini L, and Ellis JG. Stress and the hypothalamic-pituitary-adrenal axis: How can the COVID-19 pandemic inform our understanding and treatment of acute insomnia? J Sleep Res. (2023) 32:e13842. doi: 10.1111/jsr.13842
71. Haucke M, Golde S, Saft S, Hellweg R, Liu S, and Heinzel S. The effects of momentary loneliness and COVID-19 stressors on hypothalamic-pituitary adrenal (HPA) axis functioning: A lockdown stage changes the association between loneliness and salivary cortisol. Psychoneuroendocrinology. (2022) 145:105894. doi: 10.1016/j.psyneuen.2022.105894
72. Henneghan AM, Lewis KA, Gill E, and Kesler SR. Cognitive impairment in non-critical, mild-to-moderate COVID-19 survivors. Front Psychol. (2022) 13:770459. doi: 10.3389/fpsyg.2022.770459
73. Yuan K, Zheng YB, Wang YJ, Sun YK, Gong YM, Huang YT, et al. A systematic review and meta-analysis on prevalence of and risk factors associated with depression, anxiety and insomnia in infectious diseases, including COVID-19: a call to action. Mol Psychiatry. (2022) 27:3214–22. doi: 10.1038/s41380-022-01638-z
74. Kataoka M, Hazumi M, Usuda K, Okazaki E, and Nishi D. Association of preexisting psychiatric disorders with post-COVID-19 prevalence: a cross-sectional study. Sci Rep. (2023) 13:346. doi: 10.1038/s41598-023-27405-w
75. Hao F, Tam W, Hu X, Tan W, Jiang L, Jiang X, et al. A quantitative and qualitative study on the neuropsychiatric sequelae of acutely ill COVID-19 inpatients in isolation facilities. Transl Psychiatry. (2020) 10:355. doi: 10.1038/s41398-020-01039-2
76. Sykes DL, Holdsworth L, Jawad N, Gunasekera P, Morice AH, and Crooks MG. Post-COVID-19 symptom burden: what is long-COVID and how should we manage it? Lung. (2021) 199:113–9. doi: 10.1183/13993003.congress-2021.OA4189
77. Khan SA, Ashkar R, Kumari S, Khenhrani RR, Ullah S, Rajpar R, et al. Long COVID syndrome: psychological and sexual dysfunction among survivors of COVID-19 infection. Ann Med Surg (Lond). (2023) 85:4788–93. doi: 10.1097/MS9.0000000000001153
78. Kubota T, Kuroda N, and Sone D. Neuropsychiatric aspects of long COVID: A comprehensive review. Psychiatry Clin Neurosci. (2023) 77:84–93. doi: 10.1111/pcn.13508
79. Pantelic M, Ziauddeen N, Boyes M, O’Hara ME, Hastie C, and Alwan NA. Long Covid stigma: Estimating burden and validating scale in a UK-based sample. PloS One. (2022) 17:e0277317. doi: 10.1371/journal.pone.0277317
80. Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, and Mukherjee B. Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: A meta-analysis and systematic review. J Infect Dis. (2022) 226:1593–607. doi: 10.1093/infdis/jiac136
81. Zakia H, Pradana K, and Iskandar S. Risk factors for psychiatric symptoms in patients with long COVID: A systematic review. PloS One. (2023) 18:e0284075. doi: 10.1371/journal.pone.0284075
82. Vo HT, Dao TD, Duong TV, Nguyen TT, Do BN, Do TX, et al. Impact of long COVID-19 on posttraumatic stress disorder as modified by health literacy: an observational study in Vietnam. Osong Public Health Res Perspect. (2024) 15:33–44. doi: 10.24171/j.phrp.2023.0261
83. Seighali N, Abdollahi A, Shafiee A, Amini MJ, Teymouri Athar MM, Safari O, et al. The global prevalence of depression, anxiety, and sleep disorder among patients coping with Post COVID-19 syndrome (long COVID): a systematic review and meta-analysis. BMC Psychiatry. (2024) 24:105. doi: 10.1186/s12888-023-05481-6
84. Bai F, Tomasoni D, Falcinella C, Barbanotti D, Castoldi R, Mulè G, et al. Female gender is associated with long COVID syndrome: a prospective cohort study. Clin Microbiol Infect. (2022) 28:611.e9–.e16. doi: 10.1016/j.cmi.2021.11.002
85. Leone V, Freuer D, Goßlau Y, Kirchberger I, Warm T, Hyhlik-Dürr A, et al. Symptom clusters in acute SARS-coV-2 infection and long COVID fatigue in male and female outpatients. J Pers Med. (2024) 14(6):602. doi: 10.3390/jpm14060602
86. Gómez Bravo R, Infanti A, Billieux J, Ritzen M, Vögele C, and Benoy C. The psychological syndrome associated with Long-COVID: A study protocol. Front Epidemiol. (2023) 3:1193369. doi: 10.3389/fepid.2023.1193369
87. Kavčič T, Avsec A, and Zager Kocjan G. Psychological functioning of slovene adults during the COVID-19 pandemic: does resilience matter? Psychiatr Q. (2021) 92:207–16. doi: 10.1007/s11126-020-09789-4
88. Mansell V, Hall Dykgraaf S, Kidd M, and Goodyear-Smith F. Long COVID and older people. Lancet Healthy Longev. (2022) 3:e849–e54. doi: 10.1016/S2666-7568(22)00245-8
89. Knepple Carney A, Graf AS, Hudson G, and Wilson E. Age moderates perceived COVID-19 disruption on well-being. Gerontologist. (2021) 61:30–5. doi: 10.1093/geront/gnaa106
90. Babicki M, Szewczykowska I, and Mastalerz-Migas A. Mental health in the era of the second wave of SARS-coV-2: A cross-sectional study based on an online survey among online respondents in Poland. Int J Environ Res Public Health. (2021) 18(5):2522. doi: 10.3390/ijerph18052522
91. Silva Moreira P, Ferreira S, Couto B, MaChado-Sousa M, Fernández M, Raposo-Lima C, et al. Protective elements of mental health status during the COVID-19 outbreak in the portuguese population. Int J Environ Res Public Health. (2021) 18. doi: 10.3390/ijerph18041910
92. Ahmed H, Patel K, Greenwood DC, Halpin S, Lewthwaite P, Salawu A, et al. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: A systematic review and meta-analysis. J Rehabil Med. (2020) 52:jrm00063. doi: 10.2340/16501977-2694
93. Barin B, Yoldascan BE, Savaskan F, Ozbalikci G, Karaderi T, and Çakal H. Joint investigation of 2-month post-diagnosis igG antibody levels and psychological measures for assessing longer term multi-faceted recovery among COVID-19 cases in northern Cyprus. Front Public Health. (2020) 8:590096. doi: 10.3389/fpubh.2020.590096
94. Shi L, Lu ZA, Que JY, Huang XL, Lu QD, Liu L, et al. Long-term impact of COVID-19 on mental health among the general public: A nationwide longitudinal study in China. Int J Environ Res Public Health. (2021) 18(16):8790. doi: 10.3390/ijerph18168790
95. Cai Z, Cui Q, Liu Z, Li J, Gong X, Liu J, et al. Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. J Psychiatr Res. (2020) 131:132–7. doi: 10.1016/j.jpsychires.2020.09.007
96. Huey SJ Jr., Park AL, Galán CA, and Wang CX. Culturally responsive cognitive behavioral therapy for ethnically diverse populations. Annu Rev Clin Psychol. (2023) 19:51–78. doi: 10.1146/annurev-clinpsy-080921-072750
97. Arch JJ, Eifert GH, Davies C, Plumb Vilardaga JC, Rose RD, and Craske MG. Randomized clinical trial of cognitive behavioral therapy (CBT) versus acceptance and commitment therapy (ACT) for mixed anxiety disorders. J Consult Clin Psychol. (2012) 80:750–65. doi: 10.1037/a0028310
98. van Loenen I, Scholten W, Muntingh A, Smit J, and Batelaan N. The effectiveness of virtual reality exposure-based cognitive behavioral therapy for severe anxiety disorders, obsessive-compulsive disorder, and posttraumatic stress disorder: meta-analysis. J Med Internet Res. (2022) 24:e26736. doi: 10.2196/26736
99. Kuut TA, Müller F, Csorba I, Braamse A, Aldenkamp A, Appelman B, et al. Efficacy of cognitive-behavioral therapy targeting severe fatigue following coronavirus disease 2019: results of a randomized controlled trial. Clin Infect Dis. (2023) 77:687–95. doi: 10.1093/cid/ciad257
100. Liu Z, Qiao D, Xu Y, Zhao W, Yang Y, Wen D, et al. The efficacy of computerized cognitive behavioral therapy for depressive and anxiety symptoms in patients with COVID-19: randomized controlled trial. J Med Internet Res. (2021) 23:e26883. doi: 10.2196/26883
101. Zhang D, Lee EKP, Mak ECW, Ho CY, and Wong SYS. Mindfulness-based interventions: an overall review. Br Med Bull. (2021) 138:41–57. doi: 10.1093/bmb/ldab005
102. Buchholz JL and Abramowitz JS. The therapeutic alliance in exposure therapy for anxiety-related disorders: A critical review. J Anxiety Disord. (2020) 70:102194. doi: 10.1016/j.janxdis.2020.102194
103. Ju N, Yang X, Ma X, Wang B, Fu L, Hu Y, et al. Hospitalization, interpersonal and personal factors of social anxiety among COVID-19 survivors at the six-month follow-up after hospital treatment: the minority stress model. Eur J Psychotraumatol. (2022) 13:2019980. doi: 10.1080/20008198.2021.2019980
104. Jansen van Vuren E, Steyn SF, Brink CB, Möller M, Viljoen FP, and Harvey BH. The neuropsychiatric manifestations of COVID-19: Interactions with psychiatric illness and pharmacological treatment. BioMed Pharmacother. (2021) 135:111200. doi: 10.1016/j.biopha.2020.111200
105. Butzin-Dozier Z, Ji Y, Deshpande S, Hurwitz E, Anzalone AJ, Coyle J, et al. SSRI use during acute COVID-19 and risk of long COVID among patients with depression. BMC Med. (2024) 22:445. doi: 10.1186/s12916-024-03655-x
106. Wang Y, Su B, Xie J, Garcia-Rizo C, and Prieto-Alhambra D. Long-term risk of psychiatric disorder and psychotropic prescription after SARS-CoV-2 infection among UK general population. Nat Hum Behav. (2024) 8:1076–87. doi: 10.1038/s41562-024-01853-4
107. Renner V, Joraschky P, Kirschbaum C, Schellong J, and Petrowski K. Pro- and anti-inflammatory cytokines Interleukin-6 and Interleukin-10 predict therapy outcome of female patients with posttraumatic stress disorder. Transl Psychiatry. (2022) 12:472. doi: 10.1038/s41398-022-02230-3
108. Baptista AF, Baltar A, Okano AH, Moreira A, Campos ACP, Fernandes AM, et al. Applications of non-invasive neuromodulation for the management of disorders related to COVID-19. Front Neurol. (2020) 11:573718. doi: 10.3389/fneur.2020.573718
109. Noda Y, Sato A, Shichi M, Sato A, Fujii K, Iwasa M, et al. Real world research on transcranial magnetic stimulation treatment strategies for neuropsychiatric symptoms with long-COVID in Japan. Asian J Psychiatr. (2023) 81:103438. doi: 10.1016/j.ajp.2022.103438
110. Badran BW, Huffman SM, Dancy M, Austelle CW, Bikson M, Kautz SA, et al. A pilot randomized controlled trial of supervised, at-home, self-administered transcutaneous auricular vagus nerve stimulation (taVNS) to manage long COVID symptoms. Res Sq. (2022) 8(1):13. doi: 10.21203/rs.3.rs-1716096/v1
111. Guo B, Zhang M, Hao W, Wang Y, Zhang T, and Liu C. Neuroinflammation mechanisms of neuromodulation therapies for anxiety and depression. Transl Psychiatry. (2023) 13:5. doi: 10.1038/s41398-022-02297-y
112. Katz AA, Wainwright S, Kelly MP, Albert P, and Byrne R. Hyperbaric oxygen effectively addresses the pathophysiology of long COVID: clinical review. Front Med (Lausanne). (2024) 11:1354088. doi: 10.3389/fmed.2024.1354088
113. Robbins T, Gonevski M, Clark C, Baitule S, Sharma K, Magar A, et al. Hyperbaric oxygen therapy for the treatment of long COVID: early evaluation of a highly promising intervention. Clin Med (Lond). (2021) 21:e629–e32. doi: 10.7861/clinmed.2021-0462
114. Kjellberg A, Hassler A, Boström E, El Gharbi S, Al-Ezerjawi S, Kowalski J, et al. Hyperbaric oxygen therapy for long COVID (HOT-LoCO), an interim safety report from a randomised controlled trial. BMC Infect Dis. (2023) 23:33. doi: 10.1186/s12879-023-08002-8
115. Banerjee I, Robinson J, and Sathian B. Treatment of Long COVID or Post COVID syndrome: A Pharmacological approach. Nepal J Epidemiol. (2022) 12:1220–3. doi: 10.3126/nje.v12i3.48532
116. Wilmshurst P, Bewley S, and Murray P. Hyperbaric oxygen therapy for the treatment of long COVID. Clin Med (Lond). (2023) 23:99–100. doi: 10.7861/clinmed.Let.23.1.2
117. Miao Y, Ren R, Shen Z, Li Y, Zhang W, Bai J, et al. Quantifying the adverse effects of long COVID on individuals’ Health after infection: A propensity score matching design study. Risk Manag Healthc Policy. (2024) 17:701–13. doi: 10.2147/RMHP.S446321
118. Jacob L, Tully MA, Barnett Y, Lopez-Sanchez GF, Butler L, Schuch F, et al. The relationship between physical activity and mental health in a sample of the UK public: A cross-sectional study during the implementation of COVID-19 social distancing measures. Ment Health Phys Act. (2020) 19:100345. doi: 10.1016/j.mhpa.2020.100345
119. Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. (2020) 17(11):4065. doi: 10.3390/ijerph17114065
120. Pak VM and Lee J. Examining the role of micronutrients on improving long COVID sleep-related symptoms. J Clin Nurs. (2022). doi: 10.1111/jocn.16326
121. Barletta MA, Marino G, Spagnolo B, Bianchi FP, Falappone PCF, Spagnolo L, et al. Coenzyme Q10 + alpha lipoic acid for chronic COVID syndrome. Clin Exp Med. (2023) 23:667–78. doi: 10.1007/s10238-022-00871-8
122. Helbing DL, Dommaschk EM, Danyeli LV, Liepinsh E, Refisch A, Sen ZD, et al. Conceptual foundations of acetylcarnitine supplementation in neuropsychiatric long COVID syndrome: a narrative review. Eur Arch Psychiatry Clin Neurosci. (2024) 274:1829–45. doi: 10.1007/s00406-023-01734-3
123. Zhou T, Guan R, Rosenthal SL, Moerdler S, Guan Z, and Sun L. Supporting health-care workers and patients in quarantine wards: evidence from a survey of frontline health-care workers and inpatients with COVID-19 in wuhan, China. Front Public Health. (2021) 9:705354. doi: 10.3389/fpubh.2021.705354
124. Hawke LD, Nguyen ATP, Sheikhan NY, Strudwick G, Rossell SL, Soklaridis S, et al. Swept under the carpet: a qualitative study of patient perspectives on Long COVID, treatments, services, and mental health. BMC Health Serv Res. (2023) 23:1088. doi: 10.1186/s12913-023-10091-9
125. Roy A, Singh AK, Mishra S, Chinnadurai A, Mitra A, and Bakshi O. Mental health implications of COVID-19 pandemic and its response in India. Int J Soc Psychiatry. (2021) 67:587–600. doi: 10.1177/0020764020950769
126. Rinn R, Gao L, Schoeneich S, Dahmen A, Anand Kumar V, Becker P, et al. Digital interventions for treating post-COVID or long-COVID symptoms: scoping review. J Med Internet Res. (2023) 25:e45711. doi: 10.2196/45711
127. Laguarta-Val S, Varillas-Delgado D, Lizcano-Álvarez Á, Molero-Sánchez A, Melian-Ortiz A, Cano-de-la-Cuerda R, et al. Effects of aerobic exercise therapy through nordic walking program in lactate concentrations, fatigue and quality-of-life in patients with long-COVID syndrome: A non-randomized parallel controlled trial. J Clin Med. (2024) 13(4):1035. doi: 10.3390/jcm13041035
128. Lovaglio PG, Borgonovo F, Manzo Margiotta A, Mowafy M, Colaneri M, Bandera A, et al. Estimating long COVID-19 prevalence across definitions and forms of sample selection. Front Epidemiol. (2025) 5:1597799. doi: 10.3389/fepid.2025.1597799
129. Yagi K, Kondo M, Terai H, Asakura T, Kimura R, Takemura R, et al. Impact of long COVID on the health-related quality of life of Japanese patients: A prospective nationwide cohort study. Respir Investig. (2025) 63:610–6. doi: 10.1016/j.resinv.2025.05.001
130. Li Y, Lam LT, Xiao Y, Qiu Z, and Zhang Y. The association between Long-COVID symptomology, perceived symptom burden and mental health in COVID-19 patients in Shijiazhuang, China: a population-based health survey. Front Psychiatry. (2024) 15:1332066. doi: 10.3389/fpsyt.2024.1332066
131. Gómez Bravo R, Infanti A, Billieux J, Ritzen M, Nischwitz S, Erhardt A, et al. Unmasking the psychological landscape of long COVID: A cluster-analytical approach. Biopsychosoc Sci Med. (2025) 87:162–72. doi: 10.1097/PSY.0000000000001380
132. Surapaneni KM, Singhal M, Saggu SR, Bhatt A, Shunmathy P, and Joshi A. A scoping review on long COVID-19: physiological and psychological symptoms post-acute, long-post and persistent post COVID-19. Healthcare (Basel). (2022) 10(12):2418. doi: 10.3390/healthcare10122418
133. Aiyegbusi OL, Hughes SE, Turner G, Rivera SC, McMullan C, Chandan JS, et al. Symptoms, complications and management of long COVID: a review. J R Soc Med. (2021) 114:428–42. doi: 10.1177/01410768211032850
Keywords: long COVID, psychological symptoms, mechanisms, epidemiology, interventions
Citation: Shen S, Zhao X, Pei J, Wang B, Hou J, Chai R, Guo Y, Li F, Hao J and Wu Z (2025) Exploring the psychological impact of long COVID: symptoms, mechanisms, and treatments. Front. Psychiatry 16:1555370. doi: 10.3389/fpsyt.2025.1555370
Received: 06 January 2025; Accepted: 25 July 2025;
Published: 19 August 2025.
Edited by:
Veena Kumari, Brunel University London, United KingdomReviewed by:
Krupa Vakani, Imperial College, United KingdomCopyright © 2025 Shen, Zhao, Pei, Wang, Hou, Chai, Guo, Li, Hao and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhonglan Wu, d3V6aG9uZ2xhbkAxNjMuY29t
†These authors have contributed equally to this work
 Shi Shen
Shi Shen Xin Zhao
Xin Zhao Jianxin Pei2†
Jianxin Pei2† Zhonglan Wu
Zhonglan Wu