- 1Department of Epidemiology and Biostatistics, School of Public Health, College of Health Sciences and Medicine, Wolaita Sodo University, Sodo, Ethiopia
- 2University of Gondar, Gondar, Amhara, Ethiopia
- 3Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: Childhood maltreatment increases the risk of substance use and substance use disorder (SUD) in adolescence and adulthood, with social support potentially mitigating this relationship. However, research in Ethiopia on mediating factors remains limited. This study uses structural equation modeling (SEM) to evaluate the influence of childhood maltreatment on substance use and the mediating role of social support among students in Gondar Town, Northwest Ethiopia.
Method: A cross-sectional study was conducted from April 18 to May 9, 2023, among 1,235 preparatory and public high school students in Gondar Town who were selected via simple random sampling. Childhood maltreatment was assessed using the Childhood Trauma Questionnaire (CTQ), which yields a total score ranging from 28 to 140. For descriptive analysis, scores were categorized as “none” for values between 25 and 36 or as “some form of childhood maltreatment” for scores above 37. Substance use was measured using the Tobacco, Alcohol, Prescription Medication, and Other Substance Use (TAPS-1) tool. Problematic substance use was defined as any response greater than “never” within the past 12 months. Social support was evaluated using the Multidimensional Scale of Perceived Social Support (MSPSS). Structural equation modeling analyzed the relationships, calculating the mediation proportion.
Results: The median age was 17 years, with 63.24% female participants. Of the students, 85.42% reported a history of childhood maltreatment, 23.48% had problematic alcohol use, and 10.04% had problematic drug use in the past 12 months. Childhood maltreatment significantly increased substance use (β = 1.181, 95% CI (lower, upper): 0.223–1.821). Specific maltreatment types—physical abuse (β = 1.422, 95% CI (lower, upper): 0.590–2.423), sexual abuse (β = 0.653, 95% CI (lower, upper): 0.652–1.320), emotional abuse (β = 2.252, 95% CI (lower, upper): 1.402–4.307), physical neglect (β = 4.101, 95% CI (lower, upper): 1.042–0.904), and emotional neglect (β = 1.513, 95% CI (lower, upper): 0.831–3.059)—were positively associated with substance use. Social support negatively mediated 28.30% of this relationship, reducing the effect of maltreatment on substance use.
Conclusion: Physical abuse, sexual abuse, emotional abuse, physical neglect, and emotional neglect all increase the likelihood of substance use. However, social support mitigates the relationship between childhood maltreatment and substance use. These findings highlight the need for interventions strengthening social support to mitigate the impact of maltreatment on substance use in Ethiopia.
Introduction
Both childhood maltreatment and substance use disorder (SUD) are significant public health concerns with profound implications, particularly in low- and middle-income countries (1, 2). Substance use, defined as the improper or risky consumption of psychoactive substances including alcohol, tobacco, prescription medications, and illicit drugs, contributes to a global burden of 35 million people experiencing risky drug use or dependence in 2022, as reported by the World Health Organization (WHO) (3). In Sub-Saharan Africa (SSA), substance use remains a growing challenge, with limited regional data indicating high prevalence rates among youth; approximately 31.2%–44.6% of adolescents in SSA engage in problematic alcohol or drug use (4). Among university students in Addis Ababa, Ethiopia, 56.8% consumed alcohol, 40.2% used khat, 14.1% smoked cigarettes, and 16.2% actively used illicit drugs (5). In Bahir Dar, Ethiopia, the prevalence of problematic substance use was 55.8% (6). These figures highlight the urgent need for targeted interventions in resource-limited settings like Ethiopia.
Adolescents and adults with SUD often have a history of childhood maltreatment, encompassing physical abuse, sexual abuse, emotional abuse, physical neglect, and emotional neglect (7, 8). Research has indicated that such maltreatment types disrupt emotional regulation and increase vulnerability to maladaptive coping mechanisms, including substance use (9). Moreover, childhood maltreatment can erode social support systems, which are critical protective factors (10, 11). Higher levels of social support encompassing family, peers, and other significant sources are associated with reduced substance use, potentially buffering the adverse effects of maltreatment (8). This protective role highlights social support as a potential mediator, an area needing further exploration, particularly in less-developed contexts.
Previous studies have often combined different types of childhood maltreatment into cumulative scores, limiting the ability to examine their independent effects (12). This approach overlooks the distinct impacts of, for example, emotional neglect versus physical abuse, which may differentially influence substance use outcomes. Additionally, many studies have treated latent variables like social support as observed, reducing analytical depth (13). Most investigations rely on classical models to assess direct effects, with scant attention to mediating pathways in settings like Ethiopia (14). Thus, this study investigated the role of social support in the relationship between childhood maltreatment and substance use using structural equation modeling (SEM) among adolescents and adults of Gondar Town. By focusing on a less-developed country context, this research aimed to provide evidence for tailored interventions to mitigate SUD among maltreated youth.
Materials and methods
Research design and period
This study employed an institution-based cross-sectional design to assess the relationship between childhood maltreatment, social support, and substance use. This design was chosen to capture data at a specific point in time, allowing for an in-depth examination of associations between key variables in a real-world setting. The study was conducted from April 18 to May 9, 2023, among students in public high schools and preparatory schools in Gondar Town. Gondar Town serves as the capital of the North Gondar Zone in the Amhara Regional State. This research was carried out as an independent study to contribute to the growing body of knowledge on childhood maltreatment’s influence among adolescents and young adults in Ethiopia.
Inclusion and exclusion criteria
The source population consisted of all Gondar Town public high school and preparatory school students, while the study population consisted of all students who registered for the second semester of the 2023 academic year. This survey included all Gondar Town public high and preparatory school students registered for the second semester of the 2023 academic year. Students from night prep schools and night high schools were not included in the study.
Sampling
This study used the practical recommendation on sample size for structural equation modeling a 10:1 ratio of a sample size to the number of free parameters (15). According to the hypothetical model (Figure 1), there are six covariances between latent variables, 35 observed endogenous variables, 27 loadings (because seven of them fixed to one to give latent measurement scale), 35 indicators’ error term variance, three latent variables’ error variance, and 13 path coefficients, resulting in 119 parameters that need to be estimated in total.

Figure 1. A hypothesized causal pathway shows the effect of childhood maltreatment and social support on substance use. Key: CM, childhood maltreatment; PA, physical abuse; EN, emotional neglect; PN, physical neglect; SA, sexual abuse; EA, emotional abuse. A simple random sampling technique was used to select study participants. There are 12 public high schools and preparatory schools, with an overall enrolment of 23,524. The list of student ID numbers served as a sampling frame for the computer-generated random number selection process.
Therefore, by adding a 5% non-respondent rate, our final sample size should be 1,250. The required sample size was estimated to be 1,250. The current analysis took into account the entire sample of 1,279 individuals, as this study was carried out in support of another research objective, and the full sample was utilized for the psychological wellbeing analysis.
Data collection tool
Childhood Trauma Questionnaire
The short version of the Childhood Trauma Questionnaire (CTQ-SF) (16) was used in this study to assess childhood maltreatment, including physical abuse, sexual abuse, emotional abuse, physical neglect, and emotional neglect. This 28-item questionnaire, originally in English and translated into Amharic for this study, includes five subscales (five items each) and three Minimization/Denial Scale items to detect false-negative reporting. The CTQ-SF demonstrates strong psychometric properties, with test–retest reliability of 0.85 and internal consistency (Cronbach’s alpha) ranging from 0.63 to 0.96 among adolescents and adults (17–20). The Childhood Trauma Questionnaire has a total of 28 to 140 scores; for descriptive purposes, childhood maltreatment was categorized as none if the score is 25 to 36 or as some forms of childhood maltreatment if it is greater than 37 (21).
Tobacco, Alcohol, Prescription Medication, and Other Substance Use tool
The Tobacco, Alcohol, Prescription Medication, and Other Substance Use (TAPS-1) tool (22) measured substance use, including tobacco, alcohol, prescription medications, and other drugs (e.g., marijuana, cocaine, and heroin). This tool, originally in English and translated into Amharic, uses a 5-point Likert scale (0 = never, 1 = less than monthly, 2 = monthly, 3 = weekly, and 4 = daily) to assess use over the past 12 months. Problematic use was defined as any response greater than “never”. Validation studies have confirmed its effectiveness in identifying moderate- to high-risk use for tobacco, alcohol, and prescription opioids (23, 24). Cigarette smoking, alcohol consumption, non-medical use of medications, and other substance use were assessed using the TAPS-1 tool. Any response greater than “never” within the past 12 months was considered indicative of problematic use (24). Non-medical use of prescription medications refers to use “just for the feeling”, in amounts greater than prescribed, or use of medications not prescribed to the respondent behaviors that are categorized as prescription drug misuse and are classified under substance use.
Multidimensional Scale of Perceived Social Support
The Multidimensional Scale of Perceived Social Support (MSPSS) was employed to evaluate social support, encompassing peer, family, and other significant support. Having four items each, each dimension has a Likert scale from 1 to 7. The mean scale score is divided into three categories: low support (scores of 1 to 2.9), moderate support (scores of 3 to 5), and great support (scores of 5.1 to 7) (25).
Data collection
A self-administered, structured questionnaire was used to gather data. Four skilled data collectors with a public health officer first degree were given the task of gathering data. Based on the recommended appropriate sample size for the pilot study, 200 public high and preparatory school students from Negus Teklehaimanot Secondary and High School in Debre Markos Town participated in an external pilot study to verify the processes of data collection, administration, and analysis (26). The pilot study additionally enabled us to assess how different participants understood each questionnaire, and we were able to make any necessary modifications for the final study based on their comments. For respondents who were unavailable when the data were collected, repeated trials were taken into consideration. Data were entered into EpiData after being coded. Missing value management was taken into account after data entry.
Model building and analysis
The completeness of the data was manually verified before analysis. The dataset was entered into EpiData version 3.6, and initial data handling was conducted and subsequently exported to STATA version 17 for further statistical analysis. SEM was conducted using AMOS version 24. Descriptive and summary statistics were presented in text, figures, and tables. Reliability and validity were assessed using Cronbach’s alpha (>0.7) and average variance extracted (AVE) or composite reliability (>0.5) (27, 28). Mardia’s coefficients confirmed non-normal data distribution, addressed using 1,000-sample bootstrap maximum likelihood estimation. The Mahalanobis distance identified 76 outliers (p< 0.001), which were re-included after verifying data entry accuracy. Unstandardized coefficients with 95% confidence intervals and 5% significance levels were reported.
Ethical considerations
All methods were conducted in compliance with national regulations and the Declaration of Helsinki. Ethical approval was obtained from the Institutional Review Board (IRB) of the University of Gondar College of Medicine and Health Sciences (Reference No. IPH/2489/08/2023). Written informed consent was obtained from all participants, and for those under 18, consent was obtained from their parents or legal guardians, along with participant assent.
To ensure privacy and confidentiality, all data were stored securely in a locked cabinet accessible only to the investigators. Personal identifiers were not included in the dataset, and the collected information was used exclusively for research purposes. Given the sensitivity of childhood maltreatment and substance use, participants were informed of their right to withdraw at any time without consequences. Additionally, referral information for psychological and social support services was made available; however, no participants reported experiencing distress or requiring further assistance during the study.
Results
Socio-demographic characteristics of the respondents
Out of 1,309 randomly selected students, a total of 1,235 respondents completed the questionnaires, resulting in a response rate of 94.3%. A majority of 781 (63.24%) participants were identified as female. The median age of the respondents was 17 years (IQR, 3 years). A majority of 991 (80.24%) respondents reported that both their mother and father served as their primary caregivers. Approximately 241 (19.51%) of the participants reported low levels of peer support, 205 (16.60%) experienced low levels of family support, and 197 (15.95%) reported low levels of other significant support (Table 1). Approximately 290 (23.48%) of the respondents had problematic alcohol use in the last 12 months. Of the students, 85.42% reported a history of childhood maltreatment to varying degrees, 290 (23.48%) had problematic alcohol use, and 124 (10.04%) had problematic drug use in the past 12 months (Figure 2).
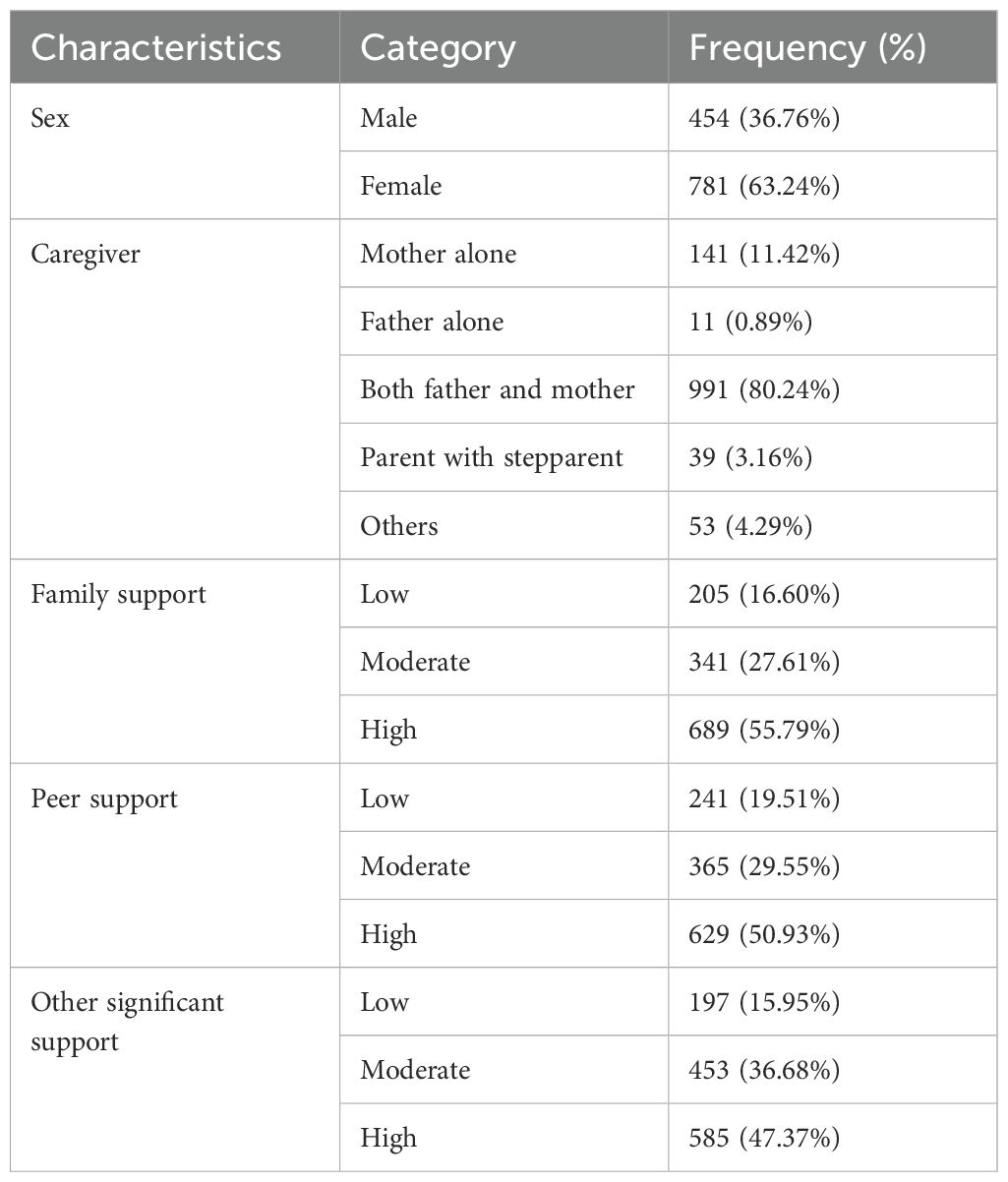
Table 1. Socio-demographic and psychosocial characteristics of high and preparatory school students in Gondar Town, Northwest Ethiopia, 2023 (n = 1,235).
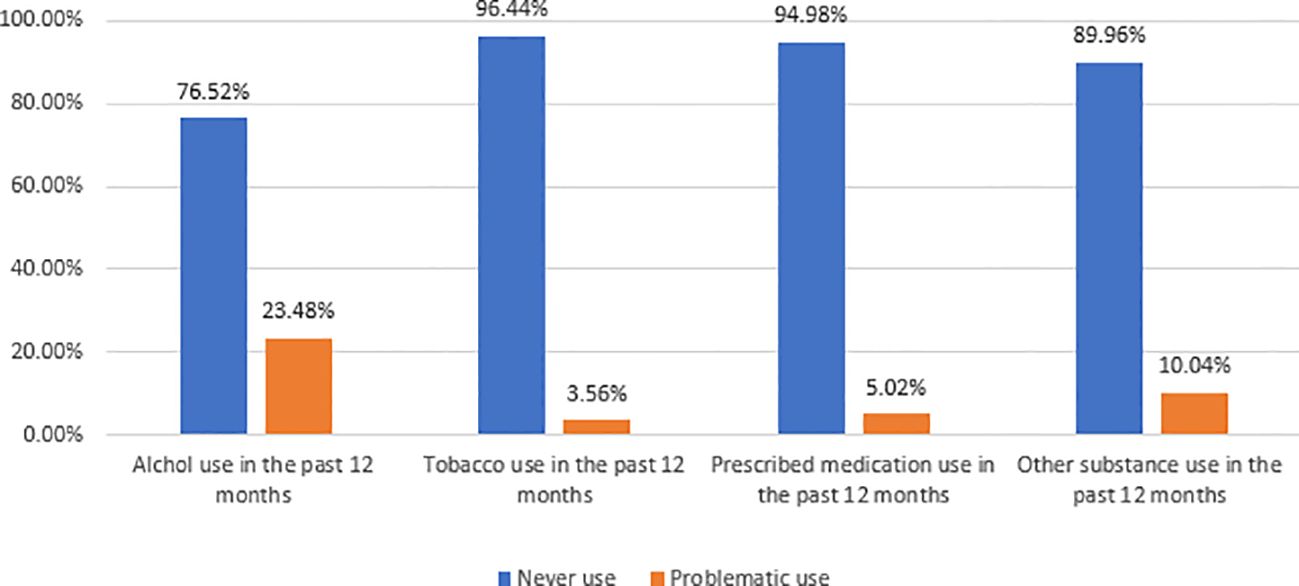
Figure 2. Magnitude of substance use among high and preparatory school students in Gondar Town, Northwest Ethiopia, 2023 (n = 1,235).
Correlation between childhood maltreatment, social support, and substance use
Childhood maltreatment had a moderate correlation (0.5 > r > 0.3, p< 0.01) with social support and substance use. A weak correlation (r< 0.3, p< 0.01) was observed between social support and substance use (Table 2).
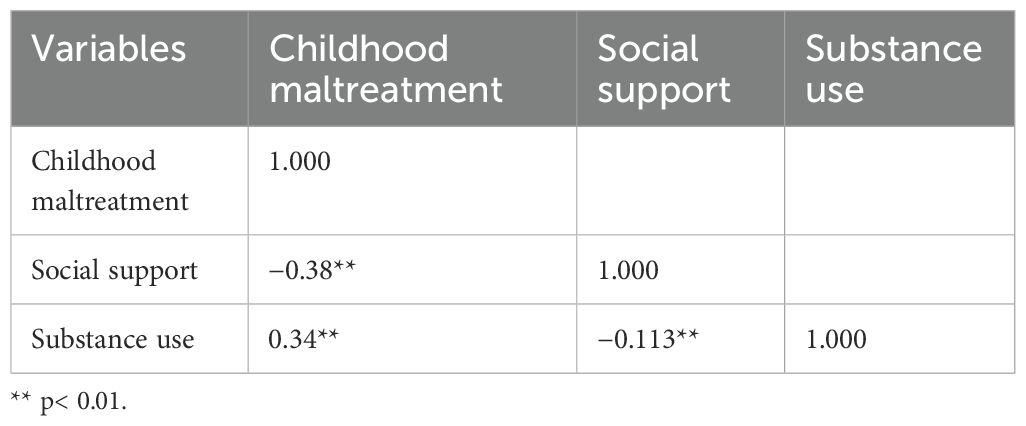
Table 2. Spearman’s correlation between childhood maltreatment, social support, and substance use of high and preparatory school students in Gondar Town, Northwest Ethiopia 2023 (n = 1,235).
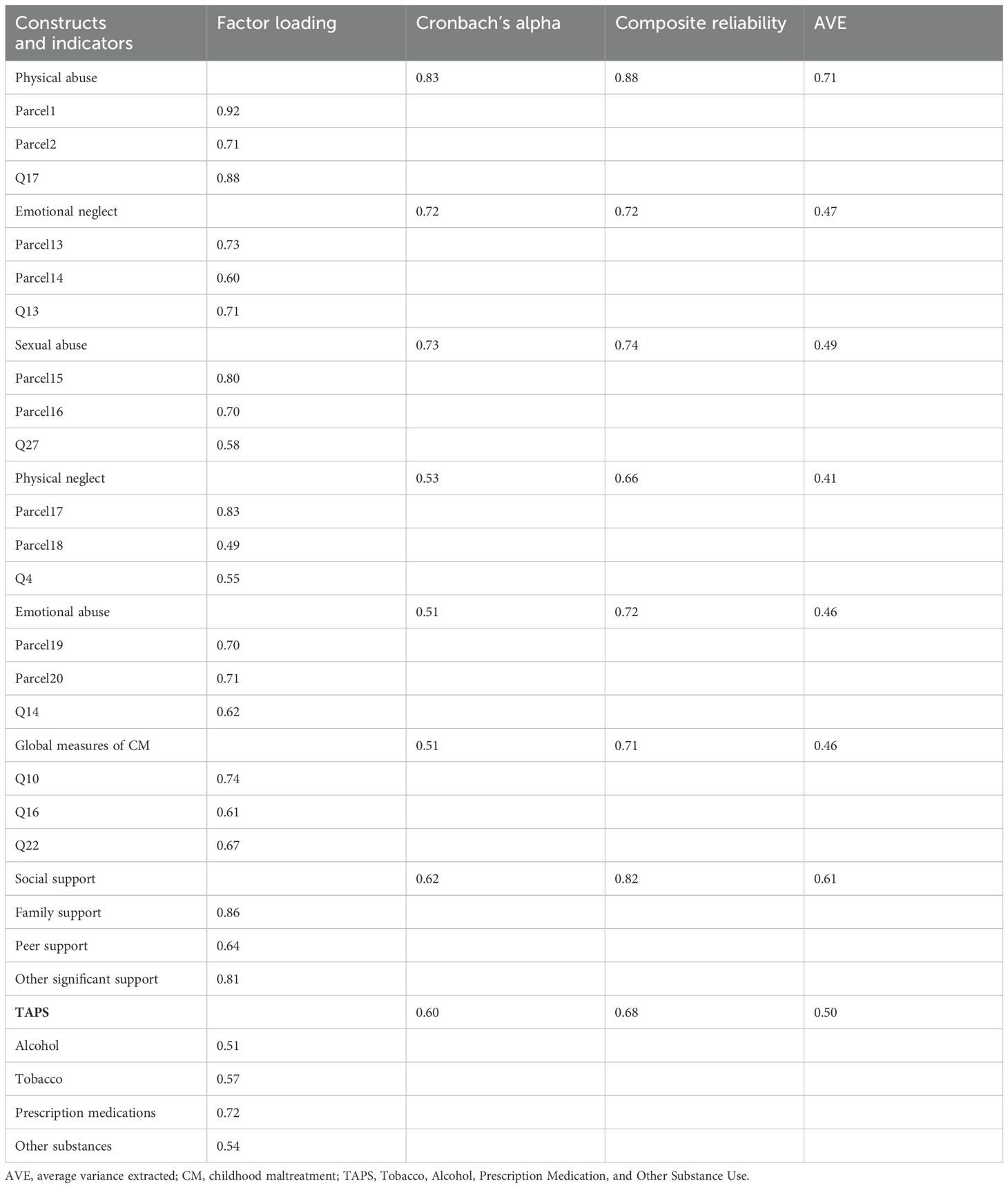
Measurement model
The measurement model in Figure 3 shows how latent variables are measured through observed variables, using a confirmatory factor analysis model for grouping multiple indicators into some constructs (29, 30). Overall fit indices were satisfactory [root mean square error of approximation (RMSEA) = 0.05, goodness-of-fit index (GFI) = 0.91, comparative fit index (CFI) = 0.93].
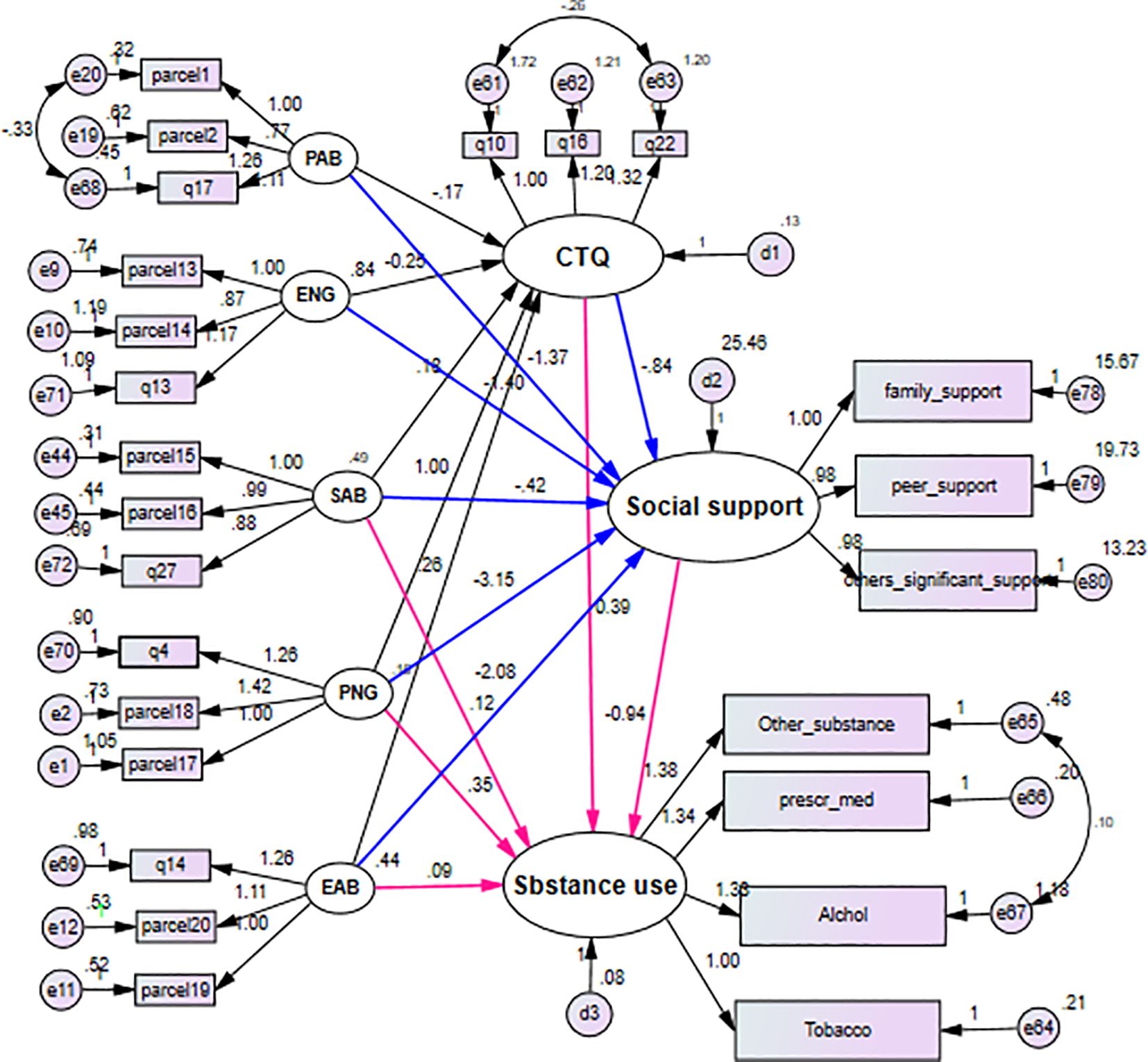
Figure 3. SEM diagram with unstandardized coefficient showing the effect of childhood maltreatment on substance use among high and preparatory school students of Gondar Town, Northwest Ethiopia, 2023. SEM, structural equation modeling.
The AVE for emotional neglect, physical neglect, sexual abuse, emotional abuse, and total childhood maltreatment ranged from 0.41 to 0.49, below the 0.5 threshold. However, composite reliability supported adequate convergent validity despite variance explained by error (Table 3).
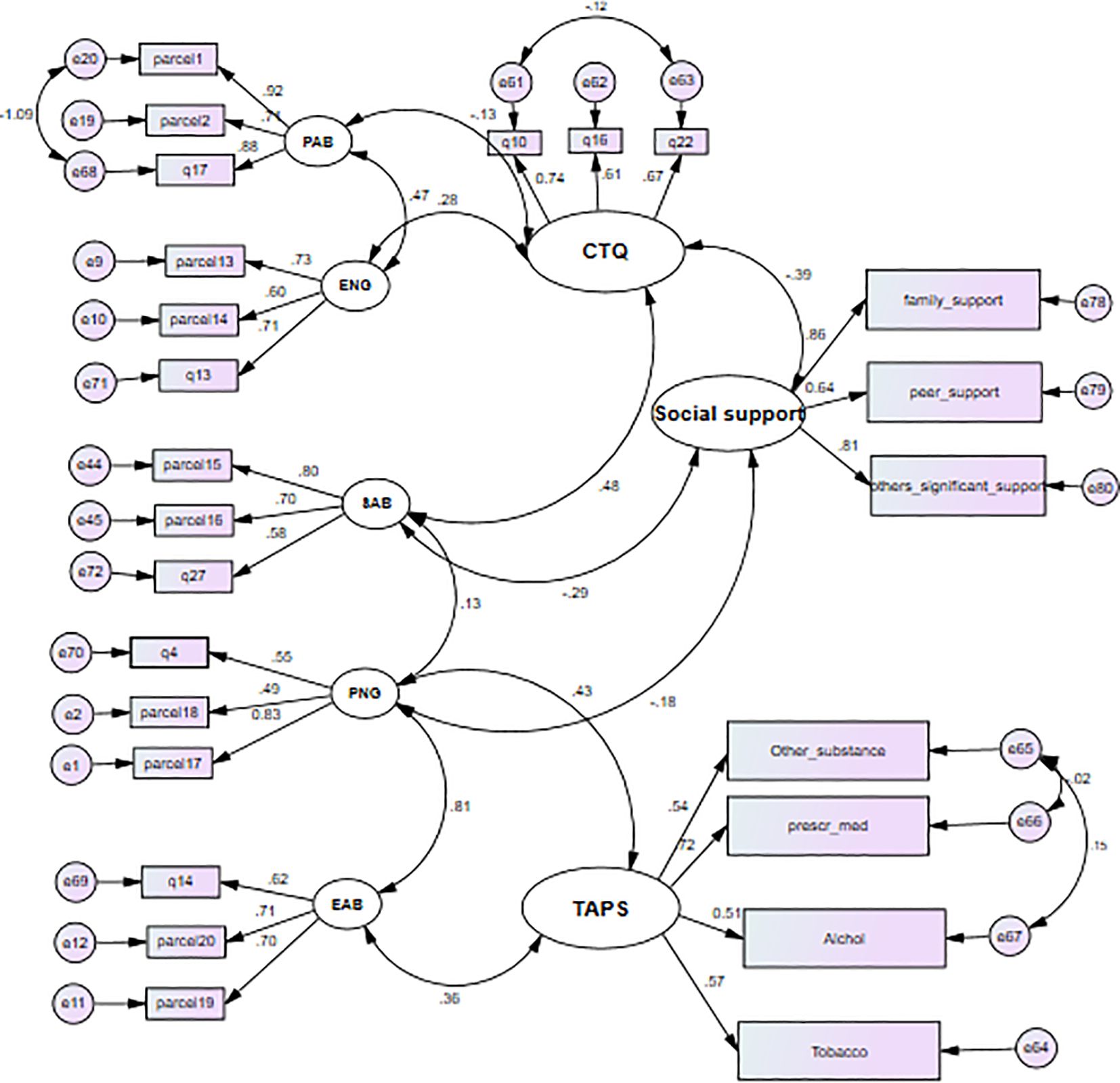
The effect of childhood maltreatment on substance use among adolescents and adults in Gondar Town
The final model, integrating structural (relationships among latent variables) and measurement components (relationships between latent variables and items), is presented in Figure 4 and Table 4. All path coefficients were statistically significant at an alpha level of 0.05. The model fit was optimal [χ2/df = 1.76, p< 0.001, RMSEA = 0.053, Tucker–Lewis Index (TLI) = 0.90, CFI = 0.93], comprising 25 indicator variables (10 parcels of 20 items), five unobserved exogenous variables, and three unobserved endogenous variables.
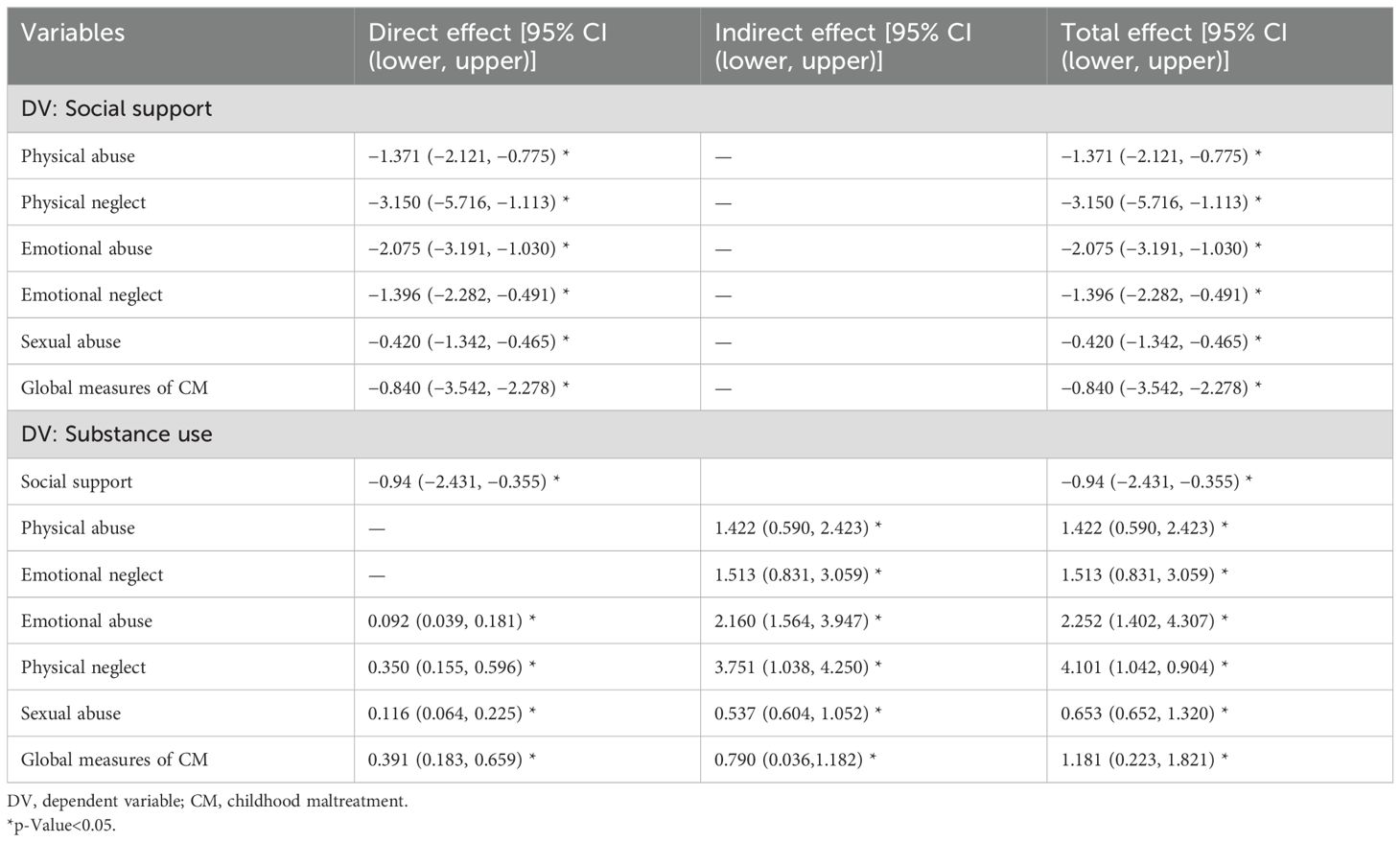
Table 4. Unstandardized estimate shows the effect of childhood maltreatment on substance use of high and preparatory school students in Gondar Town, Northwest Ethiopia 2023 (n = 1,235).
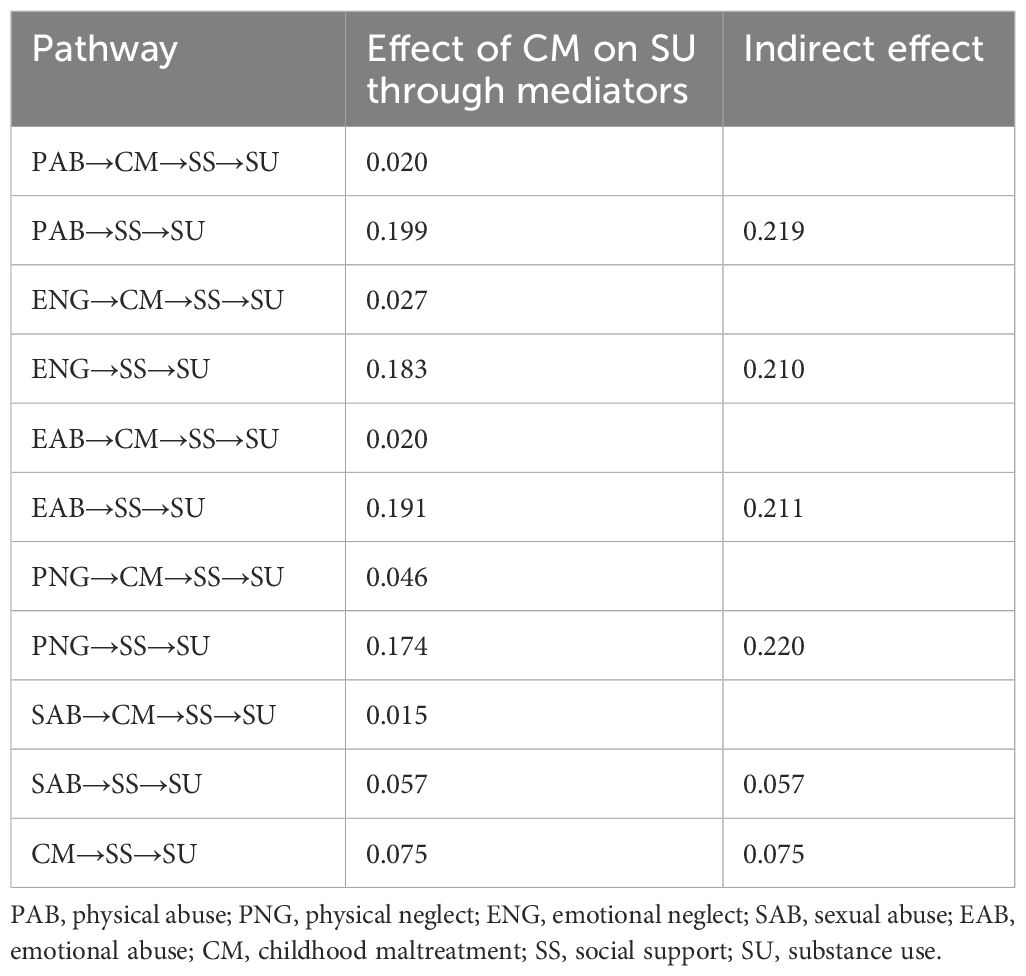
Physical abuse had an indirect positive effect (β = 1.422, 95% CI (lower, upper) (0.590, 2.423)) on substance use. Sexual abuse had a direct positive effect (β = 0.116, 95% CI (lower, upper) (0.064, 0.225)) and an indirect positive effect (β = 0.537, 95% CI (lower, upper) (0.604, 1.052)) on substance use, giving a total positive effect of β = 0.653, 95% CI (lower, upper) (0.652, 1.320). Childhood maltreatment had a direct positive effect (β = 0.391, 95% CI (lower, upper) (0.183, 0.659)) and an indirect effect (β = 0.790, 95% CI (lower, upper) (0.036, 1.182)) on substance use, yielding a total positive effect of β = 1.181, 95% CI (0.223, 1.821). These indicate that both social support and global measures of childhood maltreatment mediated the relationship between all forms of maltreatment and substance use outcomes. The total effect of physical abuse, sexual abuse, emotional abuse, physical neglect, and emotional neglect was mediated by global measures of childhood maltreatment and social support. The indirect standardized effect of childhood maltreatment on substance use through social support was β = 0.075, p< 0.05. The mediated effect of physical abuse through social support alone was β = 0.199, p< 0.05, and the mediated effect of physical abuse through global childhood maltreatment and social support was β = 0.020, p< 0.05 (Tables 4, 5).
The mediating variable social support had a negative direct effect (β = −0.83, p< 0.05) on substance use. The standardized direct effect of overall childhood maltreatment on substance use was β = 0.19, p< 0.05, with an indirect effect of β = 0.075, p< 0.05, yielding a total effect of β = 0.265, p< 0.05 (Table 4).
The mediation proportion (MP) is given as follows: .
The mediation proportion of social support on the association between overall childhood maltreatment and substance use was 28.30%.
Discussion
This study utilized SEM to effectively account for measurement errors while exploring the direct and mediated effects of childhood maltreatment on substance use through social support. The results indicated that except for physical and emotional abuse, all other types of childhood maltreatment had a direct and significant influence on substance use. Although physical and emotional abuse did not directly impact substance use, their effects were mediated by social support. Notably, social support played a crucial role, mediating 28.30% of the relationship between overall childhood maltreatment and substance use. These findings highlight the essential buffering effect of social support in reducing the negative consequences of childhood maltreatment on substance use.
The current study unequivocally demonstrated, consistent with prior research, that childhood maltreatment was directly associated with an increased risk of substance use among school-aged adolescents and adults (8, 31–33). Both directly and through social support, sexual abuse had increased effects on substance use. This finding is consistent with a study carried out in the United States (34). As physical neglect increases, substance use also increases, resulting from both a direct effect and a mediated effect through social support. This finding is consistent with studies conducted in the United States (35, 36). Emotional abuse had positive direct and indirect effects on substance use. This aligns with previous research (37, 38). Emotional neglect had an indirect effect on substance use, mediated through social support. This finding supports studies conducted in Germany (36) and Turkey (39). A possible explanation for this is that children who experience abuse and neglect may have more difficulty managing their emotional responses, which could make it harder for them to cope with distressing situations in healthy ways (40). As a result, maltreated individuals may turn to substances as a coping mechanism to manage the psychological and emotional pain caused by maltreatment. This aligns with the broader literature, which suggests that childhood maltreatment can disrupt emotional regulation and contribute to maladaptive coping strategies, including substance use (41). The association between childhood maltreatment and substance use was mediated by social support (8, 42). This finding is convergent with studies from the Midwestern metropolitan area (10) and Ireland (11). This indicates social support serves as a buffer in the relationship between childhood maltreatment and substance use. The possible explanation for this may be that individuals with maltreatment seem less emotionally mature than their peers because childhood maltreatment could make it harder to grow a trusting relationship with their own emotions. Therefore, those with a history of childhood maltreatment may have limited access to the necessary supportive networks or resources to buffer these adverse effects. Moreover, this results in a higher frequency of emotional problems, and to cope with this stress, they may turn to substances.
However, while these patterns are common across different international settings, it is essential to recognize the local factors that may influence the relationship between maltreatment and substance use in Ethiopia. For example, young people in Ethiopia may face unique challenges, such as limited access to mental health services, cultural stigmas surrounding both substance use and abuse, and the availability of certain substances. These contextual differences can shape how childhood maltreatment impacts substance use and complicate efforts to provide interventions that work in other settings.
The findings of this study not only enhance the international understanding of the relationship between childhood maltreatment and substance use but also underscore the importance of context-sensitive interventions. While international benchmarks offer valuable comparisons, it is crucial for future research and intervention programs to consider the unique challenges faced by Ethiopian youth. Policies should be adapted to address local needs while also drawing on global best practices to ensure their effectiveness. Moreover, the results emphasize the critical role of social support in mitigating the negative consequences of childhood maltreatment on substance use. These findings suggest that interventions and prevention strategies must prioritize the promotion of mental health and the strengthening of social support networks to prevent substance use among maltreated children. It is essential for future programs to not only focus on direct substance use prevention but also address the emotional and psychological impact of maltreatment particularly in settings like Ethiopia, where access to mental health resources may be limited.
Strengths and limitations of the study
To the best of our knowledge, this is the first study in Ethiopia to investigate the relationships between childhood maltreatment and substance use mediated by social support among high school and preparatory school students. Childhood maltreatment was assessed using the CTQ, a standardized and validated tool applicable in both developed and developing countries. Additionally, this study employed SEM, which allowed for the simultaneous assessment of both direct and indirect effects of multiple predictors on outcome variables, enhancing the robustness of the findings. Despite these strengths, the study has certain limitations. The sample was restricted to adolescents and adults attending public schools, which may limit the generalizability of the findings to the broader population, including those in private schools or out-of-school adolescents. A significant limitation is the reliance on self-reported data, which may be subject to recall bias or social desirability effects. This could affect the accuracy of prevalence estimates and the strength of observed associations. Future studies should consider adopting longitudinal designs to establish causality and reduce bias over time.
Conclusion
This study underscores the significant relationship between childhood maltreatment, substance use, and the role of social support in mitigating these effects. The findings suggest that social support plays a critical role in buffering the adverse consequences of childhood maltreatment on substance use. These results provide valuable insights that can inform the development of interventions and prevention strategies aimed at addressing the complex issue of substance use among adolescents and young adults who have experienced maltreatment. While this study emphasizes the importance of social support in this context, it is important to note that other factors, such as direct substance use prevention and emotional and psychological support, must also be considered in developing comprehensive strategies.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board (IRB) of the University of Gondar College of Medicine and Health Sciences (reference number: IPH/2489/08/2023). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
AA: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AT: Conceptualization, Methodology, Supervision, Validation, Visualization, Writing – review & editing. MM: Conceptualization, Data curation, Methodology, Resources, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We extend our thanks to the University of Gondar for providing us with the ethical approval needed to carry out this research. We sincerely appreciate the participants’ time and helpful cooperation during the data collection process, as well as the teachers and directors of the public high and preparatory schools in Gondar Town.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. American public health association. Substance misuse . Available online at: https://www.apha.org/topics-and-issues/substance-misuse:~:text=Substance%20misuse%20is%20a%20serious,is%20harmful%20to%20our%20health (Accessed July 15, 2024).
2. World health organization. Child maltreatment (2022). Available online at: https://www.who.int/news-room/fact-sheets/detail/child-maltreatment:~:text=Child%20maltreatment%20has%20often%20severe,infections%20(STIs)%20including%20HIV (Accessed July 15, 2024).
3. World Health Organization. Drugs (psychoactive) (2023). Available online at: https://www.who.int/health-topics/drugs-psychoactivetab=tab_1 (Accessed July 15, 2024).
4. Marsiglia FF, Huang C-K, Williams JH, Munyuwiny S, Makunyane L, Molobe DI, et al. Substance use among adolescents in sub-saharan Africa: A narrative review of epidemiological data. Afr J Alcohol Drug Abuse. (2024) 12:80–111. doi: 10.4314/ajada.v12i1.5
5. Shegute T and Wasihun Y. Prevalence of substance use in university students, Ethiopia. Subst Abuse: Res Treat. (2021) 15:11782218211003558. doi: 10.1177/11782218211003558
6. Shegaw M, Fekadu W, Beka M, Menberu M, Yohannes K, Yimer S, et al. Problematic substance use and its associated factors among street youth in Bahir Dar city, Ethiopia. Front Psychiatry. (2022) 13:930059. doi: 10.3389/fpsyt.2022.930059
7. Cicchetti D and Rogosch FA. A developmental psychopathology perspective on substance use: Illustrations from the research on child maltreatment. In: Alcohol use disorders: A developmental science approach to etiology. Oxford, UK: Oxford University Press (2018). p. 17–29.
8. Cicchetti D and Handley ED. Child maltreatment and the development of substance use and disorder. Neurobiol stress. (2019) 10:100144. doi: 10.1016/j.ynstr.2018.100144
9. Su Y, Meng X, Yang G, and D’Arcy C. The relationship between childhood maltreatment and mental health problems: coping strategies and social support act as mediators. BMC Psychiatry. (2022) 22:359. doi: 10.1186/s12888-022-04001-2
10. Sperry DM and Widom CS. Child abuse and neglect, social support, and psychopathology in adulthood: a prospective investigation. Child Abuse Negl. (2013) 37:415–25. doi: 10.1016/j.chiabu.2013.02.006
11. Lagdon S, Ross J, Robinson M, Contractor AA, Charak R, and Armour C. Assessing the mediating role of social support in childhood maltreatment and psychopathology among college students in Northern Ireland. J Interpersonal Violence. (2021) 36:NP2112–36NP. doi: 10.1177/0886260518755489
12. Bryce I and Collier S. A systematic literature review of the contribution accumulation makes to psychological and physical trauma sustained through childhood maltreatment. Trauma Care. (2022) 2:307–29. doi: 10.3390/traumacare2020026
13. Brown SM and Shillington AM. Childhood adversity and the risk of substance use and delinquency: The role of protective adult relationships. Child Abuse Neglect. (2017) 63:211–21. doi: 10.1016/j.chiabu.2016.11.006
14. Newsom JT. Structural equation modeling (2020). Available online at: https://web.pdx.edu/~newsomj/semclass/ho_moderation.pdf (Accessed July 15, 2024).
15. Bentler PM and Chou C-P. Practical issues in structural modeling. Sociological Methods Res. (1987) 16:78–117. doi: 10.1177/0049124187016001004
16. Mathews B, Pacella R, Dunne MP, Simunovic M, and Marston C. Improving measurement of child abuse and neglect: A systematic review and analysis of national prevalence studies. PloS One. (2020) 15:e0227884. doi: 10.1371/journal.pone.0227884
17. Paivio SC and Cramer K. Factor structure and reliability of the childhood trauma questionnaire in a Canadian undergraduate student sample. Child Abuse Negl. (2004) 28: 889–904. doi: 10.1016/j.chiabu.2004.01.011
18. Garrusi B and Nakhaee N. Validity and reliability of a Persian version of the Childhood Trauma Questionnaire. psychol Rep. (2009) 104:509–16. doi: 10.2466/PR0.104.2.509-516
19. Wu Z, Liu Z, Jiang Z, Fu X, Deng Q, Palaniyappan L, et al. Overprotection and overcontrol in childhood: An evaluation on reliability and validity of 33-item expanded Childhood Trauma Questionnaire (CTQ-33), Chinese version. Asian J Psychiatry. (2022) 68:102962. doi: 10.1016/j.ajp.2021.102962
20. Saini S, Hoffmann C, Pantelis C, Everall I, and Bousman C. Systematic review and critical appraisal of child abuse measurement instruments. Psychiatry Res. (2018) 272:330–45. doi: 10.1016/j.psychres.2018.12.068
21. Bernstein DP and Fink L. Childhood Trauma Questionnaire: A Retrospective Self-report. San Antonio, TX: Harcourt Brace & Company (1998).
22. National Institutes of Health. Tobacco, alcohol, prescription medication, and other substance use Tool . Available online at: https://nida.nih.gov/taps2/ (Accessed August 20, 2024).
23. Carter G, Yu Z, Aryana Bryan M, Brown JL, Winhusen T, and Cochran G. Validation of the tobacco, alcohol, prescription medication, and other substance use (TAPS) tool with the WHO alcohol, smoking, and substance Involvement screening test (ASSIST). Addict Behav. (2022) 126:107178. doi: 10.1016/j.addbeh.2021.107178
24. Gryczynski J, McNeely J, Wu L-T, Subramaniam GA, Svikis DS, Cathers LA, et al. Validation of the TAPS-1: a four-item screening tool to identify unhealthy substance use in primary care. J Gen Internal Med. (2017) 32:990–6. doi: 10.1007/s11606-017-4079-x
25. social workers tool box. Multidimensional scale of perceived social support (MSPSS). Available online at: http://www.socialworkerstoolbox.com/multidimensional-scale-perceived-social-support-mspss/ (Accessed December 15, 2024).
26. Linked in. How do you choose the best sample size and method for your pilot test? (2023). Available online at: https://www.linkedin.com/advice/0/how-do-you-choose-best-sample-size-method-your (Accessed December 15, 2024).
27. Analysis INN. Average variance extracted (AVE) (2020). Available online at: https://www.analysisinn.com/post/average-variance-extracted-ave/ (Accessed December 15, 2024).
28. UCLA stastical method and data analytics. What does Cronbach’s alpha mean? (2021). Available online at: https://stats.oarc.ucla.edu/spss/faq/what-does-cronbachs-alpha-mean/ (Accessed December 15, 2024).
29. Kline RB. Principles and practice of structural equation modeling. New York, NY: Guilford publications (2015).
30. Kang H and Ahn J-W. Model setting and interpretation of results in research using structural equation modeling: A checklist with guiding questions for reporting. Asian Nurs Res. (2021) 15:157–62. doi: 10.1016/j.anr.2021.06.001
31. Strathearn L, Giannotti M, Mills R, Kisely S, Najman J, and Abajobir A. Long-term cognitive, psychological, and health outcomes associated with child abuse and neglect. Pediatrics. (2020) 146. doi: 10.1542/peds.2020-0438
32. Kirsch DE, Tretyak V, Radpour S, Weber WA, Nemeroff CB, Fromme K, et al. Childhood maltreatment, prefrontal-paralimbic gray matter volume, and substance use in young adults and interactions with risk for bipolar disorder. Sci Rep. (2021) 11:123. doi: 10.1038/s41598-020-80407-w
33. Abajobir AA, Najman JM, Williams G, Strathearn L, Clavarino A, and Kisely S. Substantiated childhood maltreatment and young adulthood cannabis use disorders: A pre-birth cohort study. Psychiatry Res. (2017) 256:21–31. doi: 10.1016/j.psychres.2017.06.017
34. Levine EC, Martinez O, Mattera B, Wu E, Arreola S, Rutledge SE, et al. Child sexual abuse and adult mental health, sexual risk behaviors, and drinking patterns among Latino men who have sex with men. J Child sexual abuse. (2018) 27:237–53. doi: 10.1080/10538712.2017.1343885
35. Dubowitz H, Roesch S, Arria AM, Metzger R, Thompson R, Kotch JB, et al. Timing and chronicity of child neglect and substance use in early adulthood. Child Abuse Neglect. (2019) 94:104027. doi: 10.1016/j.chiabu.2019.104027
36. Duprey EB, Oshri A, and Caughy MO. Childhood neglect, internalizing symptoms and adolescent substance use: does the neighborhood context matter? J Youth adolescence. (2017) 46:1582–97. doi: 10.1007/s10964-017-0672-x
37. Barahmand U, Khazaee A, and Hashjin GS. Emotion dysregulation mediates between childhood emotional abuse and motives for substance use. Arch Psychiatr Nursing. (2016) 30:653–9. doi: 10.1016/j.apnu.2016.02.007
38. Kepple NJ. Does parental substance use always engender risk for children? Comparing incidence rate ratios of abusive and neglectful behaviors across substance use behavior patterns. Child Abuse neglect. (2018) 76:44–55. doi: 10.1016/j.chiabu.2017.09.015
39. Kurtuluş C and Elemo AS. Childhood emotional neglect and risks of substance misuse: meaning and purpose of life as a mediator. Int J Ment Health Addict. (2023) 21:1–14. doi: 10.1007/s11469-023-01096-w
40. psychCentral. What are the effects of emotional abuse? (2022). Available online at: https://psychcentral.com/health/effects-of-emotional-abuserelationship-impacts (Accessed December 24, 2024).
41. Augustyn MB, Thornberry TP, and Henry KL. The reproduction of child maltreatment: An examination of adolescent problem behavior, substance use, and precocious transitions in the link between victimization and perpetration. Dev psychopathol. (2019) 31:53–71. doi: 10.1017/S0954579418001633
42. Wiss DA, Prelip ML, Upchurch DM, von Ehrenstein OS, Tomiyama AJ, and Shoptaw SJ. Perceived social support moderates the association between household dysfunction adverse childhood experiences (ACEs) and self-reported drug use among men who have sex with men in Los Angeles, California. Int J Drug Policy. (2022) 110:103899. doi: 10.1016/j.drugpo.2022.103899
Keywords: child abuse, child neglect, substance-related disorders, social support, structural equation modeling, mediation analysis, Ethiopia
Citation: Asnake AA, Taddese AA and Merid MW (2025) The influence of childhood maltreatment on substance use among students in Gondar Town, Northwest Ethiopia: the mediating role of social support. Front. Psychiatry 16:1559939. doi: 10.3389/fpsyt.2025.1559939
Received: 13 January 2025; Accepted: 26 May 2025;
Published: 17 June 2025.
Edited by:
Eduardo Fernández-Jiménez, European University of Madrid, SpainReviewed by:
Sarah-Jane Hannah Fenton, University of Birmingham, United KingdomMohammadreza Shalbafan, Iran University of Medical Sciences, Iran
Copyright © 2025 Asnake, Taddese and Merid. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Angwach Abrham Asnake, YW5nd2FjaGFicmhhbUBnbWFpbC5jb20=
†Present address: Asefa Adimasu Taddese, Academy of Wellness and Human Development, Faculty of Arts and Social Sciences, Hong Kong Baptist University, Hong Kong SAR, China
 Angwach Abrham Asnake
Angwach Abrham Asnake Asefa Adimasu Taddese
Asefa Adimasu Taddese Mehari Woldemariam Merid
Mehari Woldemariam Merid