Abstract
The detection of Generalized Anxiety Disorder (GAD) in indigenous populations poses a challenge due to their holistic approach to health, which significantly contrasts with the Western biomedical model. Moreover, conventional assessment tools often overlook cultural particularities, compromising their effectiveness in these contexts.
Objective:
Therefore, this study aimed to analyze the diagnostic accuracy of the GAD-7 in the Quechua indigenous population of the Peruvian Andes.
Method:
To address this issue, we conducted a case-control study to evaluate the clinical accuracy of the Generalized Anxiety Disorder Test (GAD-7) in rural Quechua communities of the Peruvian Andes. We included 147 GAD patients and 322 controls. The study involved four stages: cultural adaptation of the GAD-7, door-to-door evaluation, blind psychiatric and neuropsychological assessments, and application of the Quechua GAD-7. The adaptation used the Delphi method, focus groups, and bilingual judges. Factor analyses, reliability assessments, and diagnostic utility evaluations were performed.
Results:
The Quechua GAD-7 showed high content validity (Aiken’s V > 0.85), strong internal consistency (α = 0.912, ω = 0.85), and an area under the curve of 0.93. With a cutoff score of 11, it achieved 91.3% sensitivity and 86.1% specificity.
Conclusions:
This is the first study to validate a Western test for GAD in indigenous populations.
1 Introduction
Generalized anxiety disorder (GAD) is a mental health condition characterized by excessive and uncontrollable worry (1). Its etiology is multifactorial, but chronic stress has been shown to predispose individuals to its development and amplify the associated emotional and physiological burden (2–4). Currently, GAD is one of the most challenging problems worldwide (5–7); Due to the complexity of GAD symptoms and their interaction with daily life, affected individuals often experience somatic and cognitive problems, such as motor restlessness, muscle tension, sleep disturbances, difficulty concentrating, fatigue, and irritability (8). Additionally, it often coexists with other psychiatric disorders, such as bipolar disorder, depression, and substance use (9–14). In some cases, GAD can even increase the risk of suicide, significantly impacting occupational and functional performance (15–17).
In Peru, the COVID-19 pandemic exacerbated the burden of anxiety, with rates ranging between 13.1% and 41.8% during this period (18–23); This phenomenon is well documented in the general population (24–31). However, knowledge about GAD in rural Indigenous communities, both globally and in Peru, remains limited (32, 33). In this regard, available evidence suggests that Indigenous populations face significant barriers to accessing appropriate medical and mental health services (34–38). This is due to factors such as geographical barriers (37), cultural differences, the lack of preparation among healthcare professionals, and economic aspects (39–41). Additionally, the symptoms of GAD often overlap with other mental disorders, complicating the diagnostic process (7). Finally, there are few validated clinical instruments available to detect anxiety symptoms in culturally diverse populations (42–46). This combination of factors hinders the early detection and treatment of GAD (47, 48). This underscores the need to develop and validate useful instruments for rural and indigenous populations in the country.
The GAD-7 is a self-assessment test, developed by Spitzer et al. in 2006 (49), to assess symptoms of generalized anxiety over the past two weeks. It has been widely used around the world because of its high sensitivity, simplicity, and ease of administration. The test consists of seven items that are statements about worry or somatic symptoms, rated on a four-point Likert scale. Factor analyses have shown that the GAD-7 has adequate psychometric indicators, explaining between 60% and 70% of the variance, with adequate fit indices (RMSEA = 0.080; CFI = 0.995; SRMR = 0.053) and high internal consistency, with a Cronbach’s alpha of 0.920, indicating high reliability for the detection of GAD symptoms, as demonstrated in various studies (50–55).
However, global evidence shows that most studies analyzing the statistical or clinical indicators of the GAD-7 have been conducted primarily in Western contexts and urban communities (50, 56–60); with some studies conducted in rural settings (61, 62). To our knowledge, the clinical utility of the GAD-7 has not been evaluated in indigenous communities living in culturally indigenous settings, such as rural contexts. Evaluating the diagnostic utility of the GAD-7 in a sample of Indigenous adults is critical to ensure that the test accurately captures the specific cultural manifestations of anxiety in this population. Since expressions of anxiety can vary significantly between urban and Indigenous contexts, validation of the GAD-7 in this setting will ensure that the language is understandable, the relevant symptoms are appropriately measured, and the scoring norms reflect the cultural realities of Indigenous populations. This is essential for improving diagnostic accuracy, ensuring the clinical relevance of the test, and designing mental health interventions that are culturally sensitive and effective. Therefore, the aim of this study was to analyze the diagnostic accuracy of the GAD-7 in the Quechua Andean Indigenous population of Peru.
2 Materials and method
Cross-sectional case-control study with blinded diagnostic assessment to analyze the diagnostic accuracy of a clinical scale for detecting generalized anxiety in a non-probabilistic sample of 147 patients with a medical diagnosis of GAD and 322 healthy controls; all participants were middle-aged adults, bilingual rural Quechua Indigenous individuals from the Peruvian highlands. Measurements were conducted between 2023 and 2024.
The sampling was carried out in two successive phases. First, through purposive door-to-door community sampling, bilingual Quechua Indigenous adults from rural areas of the Peruvian Andes were identified. Subsequently, targeted clinical sampling was applied, which allowed the selection of participants based on a blinded medical diagnosis of GAD or its absence. This non-probabilistic, clinically contrasted sampling strategy is common in diagnostic accuracy studies, particularly in contexts where there are limitations in clinical records and access to health services is limited(63). The combination of both phases allowed for the construction of a balanced and culturally relevant sample to evaluate the diagnostic accuracy of the GAD-7 in this context.
2.1 Procedure
The study was conducted in four stages (Figure 1: Study flowchart). First, a linguistic adaptation of the GAD-7 items into Quechua was carried out using the Delphi method as a strategy to achieve community consensus. This process was developed by two members of the research team (IQR and CQA), together with a panel composed of eight bilingual community members, native Quechua speakers fluent in Spanish. The first round consisted of the individual review of the preliminary item translation, analyzing semantic clarity, conceptual equivalence, and cultural appropriateness. A second round was then held as an in-person group discussion (focus group), in which particularly sensitive terms—such as “anxiety” and “nervousness”—were collectively explored, and culturally relevant linguistic adjustments were proposed. This stage enabled consensus on the final wording of the items, respecting the Indigenous worldview, the principles of functional equivalence, and the criteria of community acceptability and comprehension.
Figure 1

Study flowchart.
Then, using the Quechua version of the GAD-7, the content of the test items was analyzed based on the judgment of four experts—specialists in psychiatry and mental health—with cultural and linguistic ties to Quechua. The experts provided valuable suggestions that contributed to improving the adaptation of specific terms and the response options of the GAD-7. Additionally, using the Typeform platform, and based on a specification table, the semantic definition and construct components of each item on the scale were analyzed. The judges followed the 5 criteria of Osterlind to complete the content validity (63).
Secondly, a door-to-door invitation was carried out targeting middle-aged adults from rural areas of the Peruvian Andes (Ayacucho, Apurímac, and Huancavelica); identified as Quechua Indigenous individuals, native Quechua speakers and bilingual in Spanish, with the aim of evaluating the effects of the post-COVID-19 pandemic on the mental health of this population. A total of 1,873 individuals responded to a brief initial questionnaire, which included 3 demographic questions (sex, age, and years of formal education); 3 cultural questions (whether Quechua was their mother tongue, whether they identified as part of the indigenous community, and whether they engaged in associated cultural practices); and a brief checklist on generalized anxiety symptoms, along with 2 clinical questions (symptoms of mood disorders before, during, and after the pandemic, and what illnesses or disorders they had).
Third, 890 of the 1,873 respondents underwent a psychiatric and neuropsychological evaluation using medical criteria and specialized scales to assess mood and neurocognitive disorders. Specialists did not have access to the door-to-door survey information. Based on the interdisciplinary evaluation and consensus, participants were assigned to two diagnostic groups (cases: 265 and healthy controls: 467). A total of 158 participants were excluded due to the presence of other conditions concurrent with GAD, findings of mild neurocognitive disorder, neuropsychiatric disorder, major depression, failure to complete the clinical evaluation or dropout.
Finally, the selected subjects (n=732) were referred to psychologists with mental health training who administered the GAD-7 in a blinded fashion. A total of 263 individuals did not attend the second appointment, resulting in a final sample of 469 assessed patients. Upon completing the assessment, the medical team met with the scientific team to analyze the results.
2.2 Instrument
The GAD-7 is a widely used scale for assessing Generalized Anxiety Disorder over the past two weeks, according to the DSM-5 (64). It contains 7 items, each scored on a 4-point Likert scale indicating the frequency of symptoms, ranging from 0 (not at all) to 3 (almost every day). The total GAD-7 score can range from 0 to 21, with a score of ≥10 indicating generalized anxiety disorder. The original study reported adequate sensitivity (0.92) and specificity (0.83) (58). Since then, good psychometric properties of the instrument have been reported worldwide (56, 65), and it is widely used in various mental health contexts (66, 67).
Based on the adapted version of the GAD-7 for the Spanish-speaking Peruvian population (68), we made the linguistic and cultural adaptations for the Quechua population (Supplementary Data: Quechua GAD-7 Test). In addition, a training program was designed for the field team that conducted the door-to-door surveys. This training included theoretical and practical sessions aimed at strengthening communication and interviewing skills and using the virtual platform for data collection. In addition, the field staff and the professionals conducting the blind evaluations were trained in mental health, emotional support techniques, and intercultural clinical assessment.
2.3 Data analysis
Content and linguistic validity were obtained using Aiken’s V confidence interval for each item of the instrument, using the Icaiken software (69). This confidence interval makes it possible to check whether the magnitude of the coefficient obtained is more significant than a predetermined minimally acceptable level (70–72). Its value ranges from 0 to 1, with a value of 1 indicating perfect agreement between the judges regarding the maximum validity score of the content evaluated.
Next, an analysis of the psychometric properties of the GAD-7 was conducted for the rural Quechua population of Peru. An exploratory factor analysis (EFA) was performed according to the KMO and sphericity criteria using the non-orthogonal oblimin method. For the confirmatory factor analysis (CFA), the weighted least squares mean, and variance adjusted (WLSMV) method was used. The following metrics were used for goodness-of-fit criteria: root mean square error of approximation (RMSEA) with an acceptable fit value, goodness-of-fit index (GFI), and standardized root mean square residual (SRMR). Reliability was then analyzed using the omega index, Cronbach’s alpha coefficient, and item-total correlation based on the final items of the instrument.
Finally, a diagnostic utility analysis was performed by comparing the performance of the GAD-7 with expert medical criteria using the aROC curve methodology. Due to the cultural characteristics of the population studied, the cutoff score suggested in the literature (≥10 points) was not selected to detect GAD symptoms. Instead, the cutoff score was chosen where the sensitivity (S) and specificity (S) values of the GAD-7 test were best balanced. Statistical analyses were performed using the R program, version 1.3.1056.
2.4 Ethical considerations
Informed consent was obtained from the study participants, who were informed about the objective of the research. All procedures were followed to comply with national and international ethical standards related to human research under the 1975 Helsinki Declaration, revised in 2008, for those subjects whose results indicated mood disorders, psychotherapy, and comprehensive clinical care were offered. This research is part of an international study aimed at analyzing mental health in the adult and elderly populations of Latin America and the Caribbean. The protocol was approved by the Ethics Committee of Universidad Nacional Autónoma Altoandina de Tarma, Perú (Ref. 01-2024)
3 Results
Table 1 presents the content validity analysis of the GAD-7 items adapted for the Quechua population of Peru. All 7 items of the instrument showed adequate content validity (Aiken’s V), above 50%; making significant adjustments to the item statements unnecessary. Additionally, 6 out of 7 items demonstrated excellent inter-judge consensus, except for item 6, which was still very good, with over 75% global consensus.
Table 1
| Items GAD | Osterlin Criterion | Judges | ME | Aiken | % Consensus | Confidence Interval | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | L Upper | L Lower | |||||
| 1 | Rep | 4 | 4 | 4 | 4 | 4 | 1 | 0,89% | .70 | .92 |
| Pert | 4 | 2 | 4 | 4 | 3,5 | 0,87 | ||||
| Comp | 4 | 4 | 4 | 3 | 3,8 | 0,93 | ||||
| Inter | 4 | 4 | 4 | 3 | 3,8 | 0,93 | ||||
| Clar | 4 | 3 | 3 | 4 | 2,5 | 0,72 | ||||
| 2 | Rep | 4 | 4 | 4 | 4 | 4 | 1 | 0,91% | .72 | .94 |
| Pert | 4 | 4 | 4 | 3 | 3,8 | 0,93 | ||||
| Comp | 4 | 4 | 4 | 4 | 4 | 1 | ||||
| Inter | 4 | 3 | 4 | 3 | 3.5 | 0,87 | ||||
| Clar | 4 | 2 | 4 | 3 | 3,2 | 0,75 | ||||
| 3 | Rep | 4 | 3 | 4 | 4 | 4 | 1 | 0,93% | .85 | .95 |
| Pert | 4 | 4 | 3 | 4 | 3,8 | 0,93 | ||||
| Comp | 4 | 3 | 4 | 4 | 4 | 0,93 | ||||
| Inter | 4 | 4 | 3 | 4 | 3,8 | 0,93 | ||||
| Clar | 2 | 4 | 4 | 4 | 3,5 | 0,87 | ||||
| 4 | Rep | 4 | 4 | 4 | 4 | 4 | 1 | 0,98% | .91 | .99 |
| Pert | 4 | 4 | 4 | 4 | 4 | 1 | ||||
| Comp | 4 | 4 | 4 | 4 | 4 | 1 | ||||
| Inter | 4 | 4 | 4 | 3 | 3,8 | 0,93 | ||||
| Clar | 4 | 4 | 4 | 4 | 4 | 1 | ||||
| 5 | Rep | 4 | 4 | 4 | 4 | 4 | 1 | 0,89% | .79 | .92 |
| Pert | 4 | 4 | 3 | 3 | 3,5 | 0,87 | ||||
| Comp | 3 | 4 | 3 | 3 | 3,3 | 0,82 | ||||
| Inter | 4 | 3 | 3 | 3 | 3,3 | 0,82 | ||||
| Clar | 4 | 4 | 4 | 3 | 3,8 | 0,95 | ||||
| 6 | Rep | 3 | 4 | 3 | 4 | 3,5 | 0,7 | 0,76% | .65 | .79 |
| Pert | 3 | 4 | 4 | 3 | 3,8 | 0,76 | ||||
| Comp | 4 | 4 | 4 | 4 | 4 | 1 | ||||
| Inter | 3 | 3 | 3 | 4 | 3,3 | 0,66 | ||||
| Clar | 3 | 3 | 4 | 3 | 3,3 | 0,66 | ||||
| 7 | Rep | 4 | 4 | 3 | 3 | 3,5 | 0,7 | 0,80% | .74 | .84 |
| Pert | 3 | 4 | 3 | 2 | 3 | 0,6 | ||||
| Comp | 4 | 4 | 4 | 4 | 1 | 1 | ||||
| Inter | 3 | 3 | 4 | 4 | 3,5 | 0,7 | ||||
| Clar | 4 | 4 | 4 | 4 | 4 | 1 | ||||
Evaluation of the Quechua GAD-7 items.
Rep, Representativity; Pert, Pertinence; Comp, Comprehension; Inter, Interpretation; Clar, Clarity; ME, Mean; Lower. P, Lower Limit; Upper. L, Upper Limit.
In Table 2, the descriptive statistics and exploratory factor analyses of the items from the GAD-7 test are shown. The results of the EFA revealed a unidimensional structure that explained 66.11% of the data variance. Upon reviewing the factor loadings, it was determined that all 7 items of the test met the criteria to be part of the unidimensional structure (KMO = .900; p <.000). The factor loadings for the items exceeded.720, adhering to the recommendations of (67).
Table 2
| Items | ME | DS | kurtosis | Skewness | Confidence Intervals | Factor 1 | Communality | |
|---|---|---|---|---|---|---|---|---|
| Lower Limit | Upper Limit | |||||||
| 1 | 1,29 | 0,92 | -0,79 | 0,23 | 1,22 | 1,35 | 0,85 | 0,73 |
| 2 | 0,99 | 0,88 | -0,23 | 0,67 | 0,92 | 1,05 | 0,88 | 0,78 |
| 3 | 1,28 | 0,96 | -1,04 | 0,10 | 1,21 | 1,36 | 0,89 | 0,79 |
| 4 | 1,46 | 0,98 | -1,02 | 0,07 | 1,38 | 1,53 | 0,89 | 0,79 |
| 5 | 0,95 | 0,86 | -0,34 | 0,60 | 0,89 | 1,01 | 0,84 | 0,71 |
| 6 | 1,25 | 0,94 | -0,72 | 0,37 | 1,18 | 1,33 | 0,71 | 0,50 |
| 7 | 1,18 | 1,05 | -1,00 | 0,45 | 1,10 | 1,26 | 0,76 | 0,58 |
Descriptive statistics and exploratory factor analysis of the Quechua GAD-7.
ME, Mean; DS, Standard Deviation.
A confirmatory factor analysis was conducted. The global fit indices indicated an adequate model fit (RMSEA = .059; GFI = .996; AGFI = .989; SRMR = .032). The incremental indices also met the established criteria (NFI = .996; RFI = .994), with values ≥.950 as recommended (70). The parsimony indices were acceptable (PNFI = .664; PGFI = .532), exceeding the standard criterion of ≥.500. Table 3 presents the factor loadings and item communalities based on the analysis performed.
Table 3
| In the past 15 days, have you felt or experienced: | Factor 1 | Communality |
|---|---|---|
| 1. A feeling of nervousness, anxiety, or being on edge? | 0,85 | 0,73 |
| 2. Inability to avoid or control worrying? | 0,88 | 0,78 |
| 3. Excessive worry about different things or situations? | 0,89 | 0,79 |
| 4. Difficulty relaxing? | 0,89 | 0,79 |
| 5. Restlessness to the extent that it is hard to stay still? | 0,84 | 0,71 |
| 6. Easily annoyed or irritable? | 0,71 | 0,50 |
| 7. Fear, as if something awful might happen? | 0,76 | 0,58 |
Exploratory factor analysis.
Figure 2 shows the factor loadings for the 7 items on their respective scales. The factor has loadings ranging from.70 to.90. Finally, the correlation between the factors is low, which does not affect the discriminant validity of the instrument for detecting the theoretical construct (generalized anxiety) in the Quechua population of Peru.
Figure 2
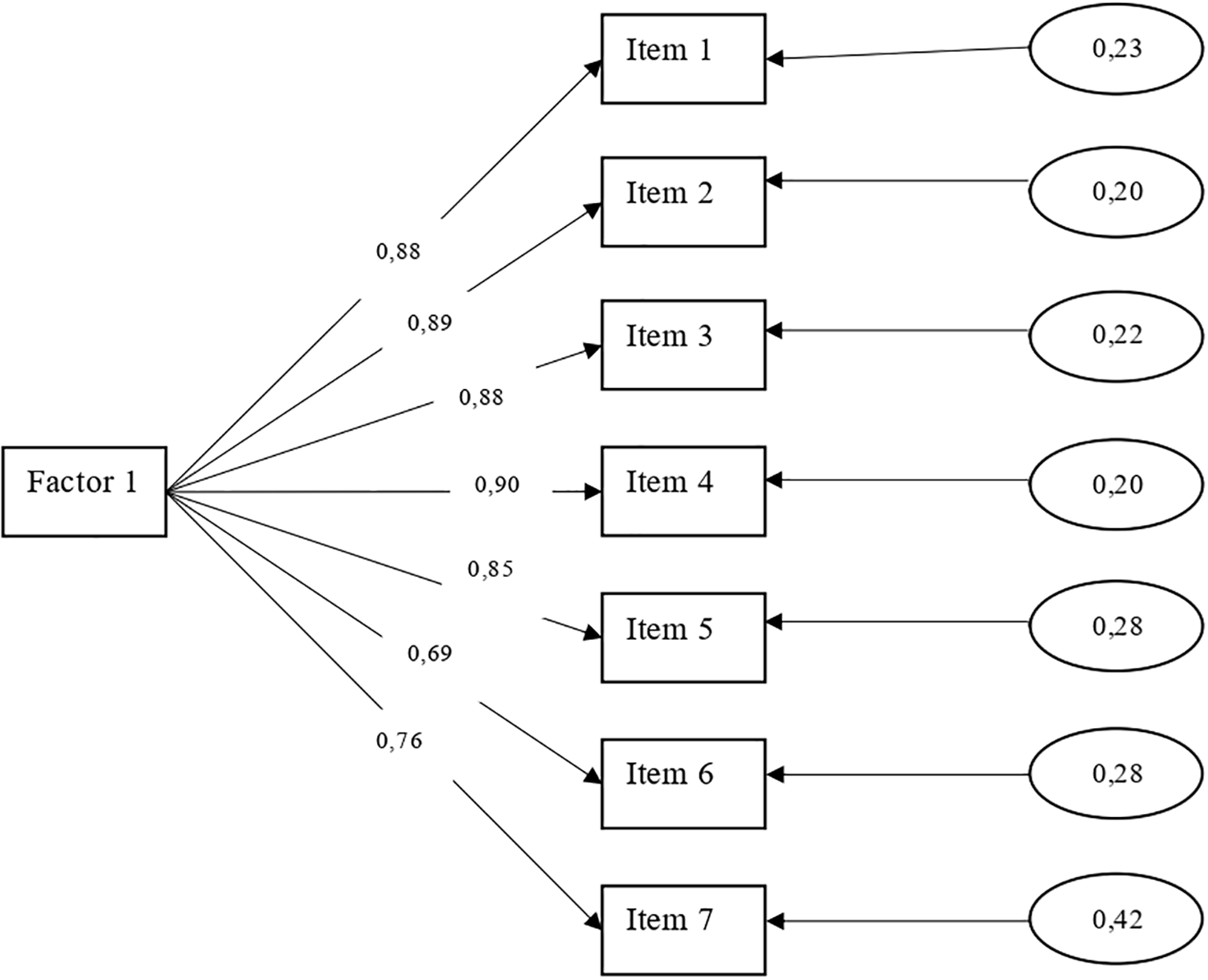
Unidimensional characteristic of the GAD-7 Test.
Additionally, the 7 items of the GAD-7 were subjected to an internal consistency analysis to determine the reliability index of the scale. The Cronbach’s Alpha coefficient (α: 0.912) and the Omega index (ω: 0.85) were used for this. These results showed high reliability of the scale.
Finally, ROC curve analysis was conducted to compare the diagnostic utility of the Quechua version of the GAD-7 with the expert psychiatric medical diagnosis (Figure 3). The area under the curve for the medical criterion was high (aROC:.90), with the test slightly higher (aROC:.93). To establish the optimal cut-off point, the Youden index was used, selecting the value that simultaneously maximized sensitivity and specificity—that is, the point at which both parameters showed the best balance. With a cutoff score of ≥11 points, the GAD-7 exhibited Sensitivity (91.3) and Specificity (86.1) values higher than those shown by the medical criterion (S: 85.5; E: 80.6) for identifying generalized anxiety symptoms in general.
Figure 3
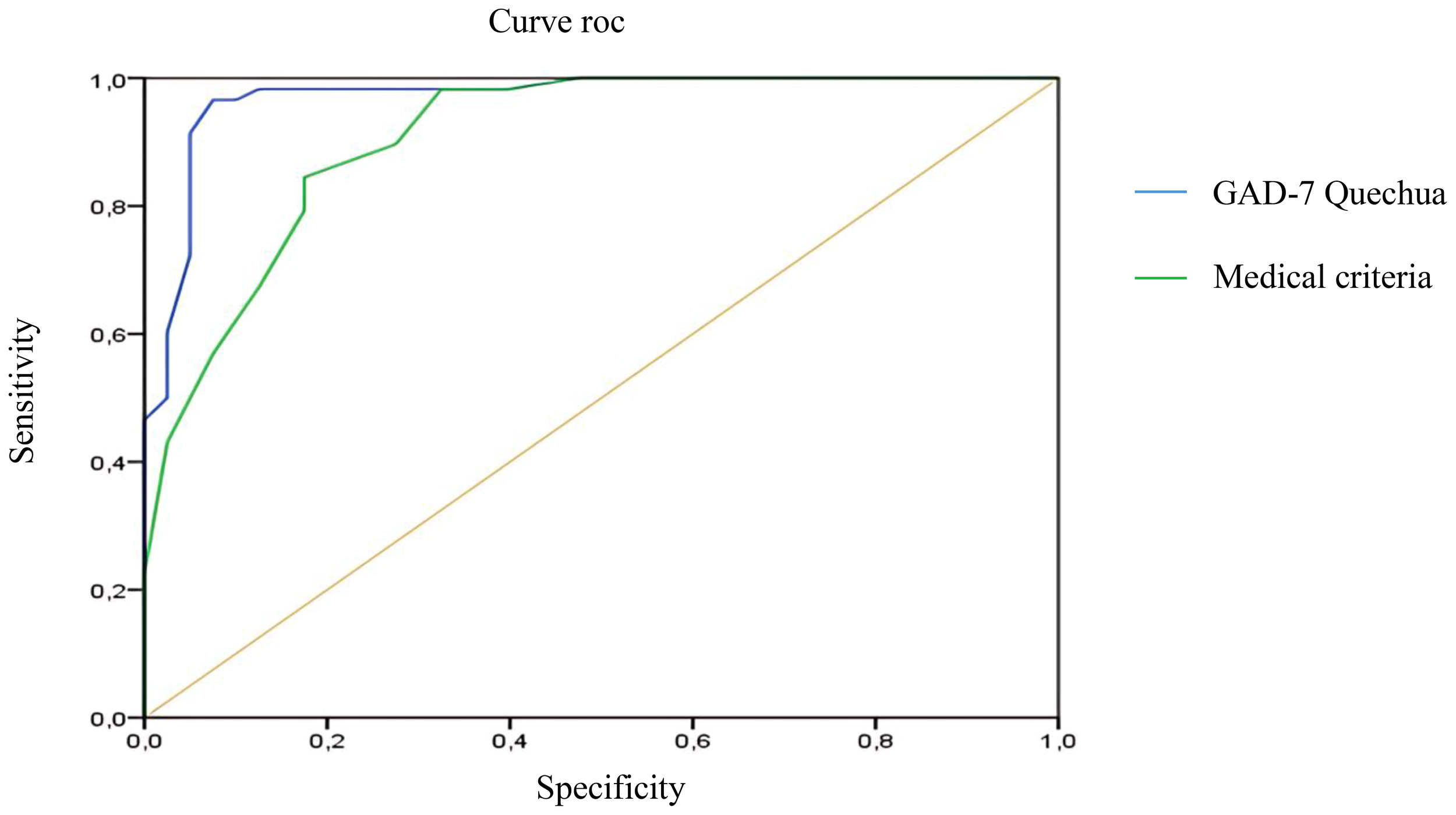
Compared ROC curve.
4 Discussion
We analyzed the diagnostic utility of the GAD-7 in Quechua-speaking populations of the Peruvian highlands, addressing its cultural adaptation, psychometric analysis, and diagnostic accuracy against the expert clinical criterion, using the area under the curve method.
In linguistic and cultural terms, the test the test showed adequate content values (Aiken’s V), with more than 50% consensus among the bilingual expert judges who reviewed the 7 items of the Quechua GAD-7. Thus, few linguistic adjustments were necessary, except for item 1, where the words “anxiety” and “nervousness” were problematic. These terms are rare or have no linguistic equivalents in Quechua as they are spoken in the highlands. It is important to note that Quechua does not have precise terms for concepts such as ‘fear’ and ‘nervousness’; emotions in this language are expressed through situational and bodily descriptions rather than abstract terms. According to Mannheim and Salas Carreño (73, 74), Quechua terms for emotions are deeply tied to bodily experience and social relationships, complicating the direct translation of Western psychological concepts such as ‘anxiety.’ Similarly, previous studies by Lévi-Strauss (75), showed that Indigenous languages tend to describe emotional states through concrete and situational references, reflecting a worldview in which emotions are linked to the environment and community relationships. In addition, Quechua is characterized as an agglutinative action language, where a single word has the potential to signify and express different emotions.
Thus, two perspectives come into conflict when assessing emotional states in Indigenous communities. The Western perspective, used when the goal is to ensure that participants understand precisely what is being measured, follows Western mental health terminology as recently described (76). This study used the terms “phutisk’alla/ansiedad nisqhawan.” This choice combines a Quechua term (“phutisk’alla”) with an additional explanation in Spanish (“ansiedad nisqhawan”). This approach is used to ensure that the concept of anxiety is adequately understood, as there may not be an exact equivalent in Quechua that fully captures the notion of “anxiety” as it is understood in Western psychiatry.
On the other hand, the term “ancha mancharisqha” (nervousness) also uses terms adapted or translated from Spanish into Quechua. In this case, the expression “mancharisqa” implies a reaction of alarm or fear, which is how nervousness could be understood in these contexts. This expression would be more easily understood and accepted by the target population (76).
In contrast, our study’s anthropological or community-based perspective focuses on respecting the indigenous worldview by using terms that correspond to emotions as they are understood in Quechua communities. In this sense, we used the term “llaquiska” (fear), which refers to intense worry or sadness, a relevant emotional concept in the Indigenous worldview. We also used the term “manchakusqachu” (nervousness), which refers to being frightened or alarmed. This aligns well with the concept of nervousness, especially when nervousness is perceived as a response to a perceived threat.
The Cjuno et al. (76), version of the GAD-7 combines Quechua and Spanish to ensure that clinical concepts are fully understood, which is helpful for accurate diagnosis within a medical-psychological framework. This approach is appropriate for use with Indigenous individuals living in either community or urban settings. In contrast, our version maintains greater fidelity to the language and Indigenous perspective, which may be more appropriate for rural Indigenous communities. However, it requires more context or explanation during the assessment (especially for item 1) to fully capture clinical nuances.
Moreover, Indigenous communities understand health, illness, and well-being differently from the Western perspective, integrating personal well-being with community, the land, and oral traditions (77–80). This makes it difficult to incorporate these perspectives into the individualistic model of Western health (81–83). Some clinical conceptualizations may lose meaning if they lack linguistic equivalents or intragroup acceptance from an Indigenous perspective (84–86). Furthermore, terms such as “distress,” “anxiety,” “nervousness,” or “depression” are either not used or are interpreted differently in these communities (85–87).
Therefore, to reduce cultural bias in the measurement of mental health issues, it is crucial to conduct cross-cultural adaptations with the active participation of Indigenous peoples, paying particular attention to integrating the holistic intercultural perspective of well-being from these communities (88, 89) as was done in our study and is reflected in the available evidence (90, 91). This may involve adapting or removing items from a test (52, 92–94); or, in some cases, creating new items (95, 96). This approach makes the standard Western test more culturally appropriate and usable in Indigenous contexts to assess mode (97–99); as described in a recent meta-analysis that analyzed the extent of tests used to screen for depression and anxiety in Indigenous adults worldwide (100). However, from an anthropological perspective on health, especially from an ethnological epistemology, it would be most appropriate for Indigenous communities to define mental health criteria and conduct measurements, analyses, interpretations, and decisions based on their cultural frameworks (101–104).
After cultural adaptation, we performed exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) on the Quechua version of the GAD-7 used in our study. The EFA revealed a unidimensional structure that explained 66.11% of the variance in the data, with factor loadings ranging from 0.71 to 0.89, as recently reported in a study of a Quechua Collao-speaking population (76); this is a variant of Quechua. In this study, sedimentation or parallel analysis showed the presence of a single latent factor; similarly, KMO analyses (0.88, p = 0.01) confirmed these results, considering the linguistic and cross-cultural adaptations built into the test, showing adequate factor weights (0.64 - 0.85) (76).
Although there are very few studies using the GAD-7 or analyzing its psychometric properties in Indigenous populations, our results are consistent with the limited evidence available (76). In this context, a recent global meta-analysis shows that studies of anxiety and depression in indigenous populations have focused more on analyzing depression symptoms than anxiety, often using the PHQ-9 or shorter versions of it (100). In other cases, some studies have equated generalized anxiety disorder (GAD) with depression for analysis in Indigenous communities (86, 100). Exceptions include two studies that examined mental health indicators, including GAD, among Aboriginal people in Alberta, Canada (105) and South Dakota, USA (106), using a 2-item version of the GAD.
Nevertheless, the findings of unidimensionality in our analyses are consistent with previous studies that have validated the GAD-7 in culturally diverse societies, such as Japanese (107), Korean (108), Chinese (109, 110) and African (43, 111) populations. In addition, the GAD-7 is invariant concerning gender, level of education, and membership in culturally diverse communities (54, 112–114); suggesting that these variables do not influence test scores (62, 115). Similarly, these psychometric indicators have been confirmed in various Western populations (49, 51, 56, 58, 116); providing robust evidence for the test’s unidimensionality.
On the other hand, the CFA showed adequate fit indices, with an RMSEA of 0.100, a CFI of 0.996, and an SRMR of 0.056, supporting the robustness of the factorial structure in the Quechua Peruvian population. These fit indices are comparable to those obtained in a recent study with Indigenous populations (76) and in global multicultural contexts, such as in China (110) and Russia (117).
In addition, reliability analyses of the GAD-7 showed optimal values for Cronbach’s alpha (α: 0.912) and omega (Ω: 0.85). This is consistent with similar findings in multicultural populations worldwide (37, 45, 50, 52, 104, 106, 110, 114–119, 128–131), where internal consistency values (α: between 0.82 - 0.94; Ω: between 0.894 - 0.90) like ours have been reported, although most studies were conducted in culturally and linguistically diverse populations, with only one focusing on indigenous peoples (76). These results suggest that the 7 items of the GAD-7 are consistent and correlate with each other, ensuring the integrity of the test to accurately measure the construct despite the cultural and racial differences in which it has been tested.
Finally, we analyzed the diagnostic utility of the GAD-7 by comparing it to the psychiatric expert criterion. In this regard, the Quechua version of the GAD-7 (aROC:.93) showed greater diagnostic accuracy than the psychiatric evaluation (aROC:.90) for detecting symptoms of generalized anxiety disorder (GAD). Recently, our research group (120), conducted a phase 1 case-control study, reporting high diagnostic utility of the GAD-7 (aROC: 0.91) in a clinical Quechua Indigenous sample. Apart from these two studies, there are no similar studies in Indigenous populations in the current literature, although there are some in rural communities speaking Latvian and Russian (62) and in China (121); where AUC values were reported to range between 0.76, 0.86, and 0.97, respectively. These indicators reflect the clinical benefit of using the GAD-7 in diverse and geographically remote settings. Additionally, it is worth noting the existence of a 2-item version of the test, which has been analyzed in rural areas (122, 123); showing AUC ranges varying between 0.69 and 0.954.
Moreover, by balancing sensitivity and specificity values, our study selected a cut-off score of 11 points to identify GAD symptoms. With one point more than in the original study (49), a sensitivity of 90.3% and specificity of 84.1% were achieved-both higher than those reported using the medical criterion (S: 85.5%; E: 80.6%). This cut-off point of ≥11 had already been proposed in a previous study conducted by our team, in which we reported sensitivity (92.56%) and specificity (89.35%) values of comparable magnitude (120), as this threshold offered a better balance between sensitivity and specificity in our sample, optimizing diagnostic performance according to the Youden Index. where we reported similar sensitivity (92.56%) and specificity (89.35%) values. Taken together, these results strengthen the evidence supporting the cross-cultural applicability of the GAD-7 as an effective screening tool in Indigenous populations.
However, we are struck by the diversity of cut-off scores (5–10) and wide ranges of sensitivity (56-94%) and specificity (46-94.4%) available in the literature. In this regard, Mughal et al. (124), conducted a systematic review of GAD screening tools in low- and middle-income countries and confirmed this variability. They reported that the GAD-7 was one of the most widely used and accurate diagnostic tests for detecting anxiety disorders; however, it showed a wide range of sensitivity (57-94%) and specificity (53-94%). This variability was associated with the region in which it was administered, participant characteristics, and methodological aspects.
An example of these variations in AUC values for the GAD-7 is the study by Vrublevska et al. (62); who validated the GAD-7 in urban and rural primary care settings in Latvia, a country with cultural and linguistic ties to Russia. In this study, two versions of the GAD-7 were analyzed. The cut-off score (≥5) and the sensitivity (0.70) and specificity (0.79) values for the Latvian version differed from those obtained for the Russian version (cut-off ≥7; S: 73.3 and E: 84.1). These findings highlight the importance of adapting GAD-7 cutoff points to specific populations and show that the optimal score may vary significantly between different cultural and linguistic groups. They also confirm the clinical utility of the GAD-7 as a tool for the detection of generalized anxiety disorder in multicultural contexts.
Despite these findings, our study has several limitations that should be considered. First, probabilistic sampling of participants was not used, which may limit the generalizability of the findings to other indigenous populations in the country. However, a rigorous double-blind selection and assessment process was used, which is rarely seen in similar studies and enhances the quality of the analyses. Second, although a thorough cultural adaptation of the GAD-7 was carried out, it is possible that some linguistic and cultural nuances were not fully captured, especially since only one variant of Quechua was considered. In addition, it has been challenging to reconcile the indigenous perspective on mental health with the Western perspective. Therefore, we believe continuing with studies that convey these cultural specificities is necessary. Finally, a gold standard test could not be used for convergent analysis with the GAD-7 due to its non-existence. These limitations suggest the need for future studies that address these aspects, as such studies are very scarce worldwide.
Considering these points, we can conclude that the Quechua version of the GAD-7 is appropriate, reliable, and effective in identifying mood variation in rural indigenous communities in Peru and overcoming cultural barriers. It has adequate clinical utility indicators for the detection of generalized anxiety disorder symptoms. This is the first study in the world to compare the accuracy of the GAD-7 test with expert medical criteria for detecting GAD in a rural indigenous population. This is excellent news for community health settings, especially in remote areas of a country where access to medical services is often limited. Therefore, having a quick to administer, easy to score and interpret clinically and culturally validated test is an excellent strategy for early and transcultural detection of mental health problems in multicultural settings (125–127). Additionally, it helps increase health coverage indicators in rural and indigenous contexts within the country.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study was approved by the Ethics Committee of Universidad Nacional Autónoma Altoandina de Tarma, Perú (Ref. 01-2024). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
NC: Conceptualization, Funding acquisition, Investigation, Project administration, Resources, Writing – original draft, Writing – review & editing. CQ-A: Resources, Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Software, Supervision. J-CC: Writing – original draft, Writing – review & editing, Conceptualization, Investigation, Methodology, Project administration, Resources. LC-A: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Methodology, Resources. DS: Writing – original draft, Writing – review & editing, Conceptualization, Formal analysis, Funding acquisition, Methodology, Resources. BM-A: Data curation, Writing – review & editing, Conceptualization. DR-C: Data curation, Formal analysis, Writing – original draft, Writing – review & editing, Software, Supervision, Validation. RQ-A: Data curation, Software, Supervision, Writing – original draft, Writing – review & editing, Project administration, Resources. JC-V: Writing – original draft, Writing – review & editing, Conceptualization, Formal Analysis, Project administration, Resources, Supervision. LC: Conceptualization, Data curation, Formal analysis, Project administration, Resources, Writing – original draft, Writing – review & editing. KA-F: Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Methodology, Resources, Validation. EL-C: Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Investigation, Resources, Supervision. RV-A: Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Methodology, Supervision, Validation. CC: Writing – original draft, Writing – review & editing, Data curation, Resources, Software, Supervision, Visualization. PG: Writing – original draft, Writing – review & editing, Conceptualization, Formal analysis, Investigation, Methodology, Resources. IQ-R: Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Investigation, Resources, Validation. EM-R: Writing – original draft, Writing – review & editing, Conceptualization, Methodology, Resources, Software, Visualization. AP-R: Conceptualization, Data curation, Formal analysis, Resources, Supervision, Writing – original draft, Writing – review & editing. IF-P: Data curation, Funding acquisition, Resources, Software, Supervision, Writing – original draft, Writing – review & editing. JH-P: Conceptualization, Funding acquisition, Investigation, Methodology, Resources, Writing – original draft, Writing – review & editing. NL: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was approved and funded by the Universidad Santo Tomás (Chile), Universidad de La Costa (Colombia) and Universidad Nacional Autónoma Altoandina de Tarma (Perú). Project reference: (INV.140-02-007-15).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1565895/full#supplementary-material
Supplementary Data S1GAD-7 test in Quechua.
References
1
Munir S Takov V . Generalized Anxiety Disorder. Isla del Tesoro (FL: StatPearls Publishing (2025).
2
Manzar MD Salahuddin M Pandi-Perumal SR Bahammam AS . Insomnia may mediate the relationship between stress and anxiety: A cross-sectional study in university students. Nat Sci Sleep. (2021) 13:31–8. doi: 10.2147/NSS.S278988
3
Ibrahim D Ahmed RM Mohammad AZ Ibrahim B Mohammed T Mohamed ME et al . Prevalence and correlates of generalized anxiety disorder and perceived stress among Sudanese medical students. BMC Psychiatry. (2024) 24:68. doi: 10.1186/s12888-024-05510-y
4
Patriquin MA Mathew SJ . The neurobiological mechanisms of generalized anxiety disorder and chronic stress. Chronic Stress. (2017) 1:1–10. doi: 10.1177/2470547017703993
5
Mohammadi MR Pourdehghan P Mostafavi SA Hooshyari Z Ahmadi N Khaleghi A . Generalized anxiety disorder: Prevalence, predictors, and comorbidity in children and adolescents. J Anxiety Disord. (2020) 73:102234. doi: 10.1016/j.janxdis.2020.102234
6
Kiviruusu O Haravuori H Lindgren M Therman S Marttunen M Suvisaari J et al . Generalized anxiety among Finnish youth from 2013 to 2021—Trend and the impact of COVID-19. J Affect Disord. (2023) 330:267–74. doi: 10.1016/j.jad.2023.03.010
7
Matsuyama S Otsubo T Nomoto K Higa S Takashio O . Prevalence of generalized anxiety disorder in Japan: A general population survey. Neuropsychiatr Dis Treat. (2024) 20:1355–66. doi: 10.2147/NDT.S456272
8
Zhou Y Luo Y Zhang N Liu S . Ten years of researches on generalized anxiety disorder (GAD): a scientometric review. Curr Psychol. (2024) 43:21393–408. doi: 10.1007/s12144-024-05872-2
9
Zech JM Patel TA Cougle JR . Correlates of treatment-seeking in DSM-5 generalized anxiety disorder: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions-III. J Anxiety Disord. (2024) 106:102909. doi: 10.1016/j.janxdis.2024.102909
10
Hajek A König HH . The prevalence and correlates of probable major depressive disorder and probable generalized anxiety disorder during the COVID-19 pandemic. Results of a nationally representative survey in Germany. Int J Environ Res Public Health. (2021) 18:12302. doi: 10.3390/ijerph182312302
11
Soraya S Mahdavi M Saeidi M Seddigh R Nooraeen S Sadri M et al . Prevalence of anxiety disorders and its co-occurrence with substance use disorder: a clinical study. Middle East Curr Psychiatry. (2022) 29:30. doi: 10.1186/s43045-022-00197-x
12
Macdonald-Gagnon G Stefanovics EA Potenza MN Pietrzak RH . Generalized anxiety and mild anxiety symptoms in U.S. military veterans: Prevalence, characteristics, and functioning. J Psychiatr Res. (2024) 171:263–70. doi: 10.1016/j.jpsychires.2024.02.013
13
Onaemo VN Fawehinmi TO D’Arcy C . Comorbid cannabis use disorder with major depression and generalized anxiety disorder: A systematic review with meta-analysis of nationally representative epidemiological surveys. J Affect Disord. (2021) 281:467–75. doi: 10.1016/j.jad.2020.12.043
14
Wang Y Liu J Zhang R Luo G Sun D . Untangling the complex relationship between bipolar disorder and anxiety: a comprehensive review of prevalence, prognosis, and therapy. J Neural Transm. (2025) 132(4):567–78. doi: 10.1007/s00702-024-02876-x
15
Escobar-Agreda S Romero Albino Z Contreras PJ Cuba-Fuentes MS . Complicated grief and its relationship with anxiety, depression, and suicidal ideation in older adults in the context of the COVID-19 pandemic in Peru: a cross-sectional analysis. BMC Psychiatry. (2023) 23:908. doi: 10.1186/s12888-023-05412-5
16
Ben Thabet J Turki M Mezghani M Guermazi A Mâalej M Charfi N et al . Prevalence of the generalized anxiety disorder in Tunisia: A study of 707 primary care outpatients. Int J Psychiatry Med. (2024) 60(2):187–202. doi: 10.1177/00912174241263235
17
Brunett KM Kinstley C Howard K Perrotte J Deason R Cordaro M . Generalized anxiety disorder in college students during the COVID-19 pandemic: the importance of screening and early detection during traumatic stressor events. J Coll Student Ment Health. (2024) 38:445–59. doi: 10.1080/87568225.2023.2191880
18
Caycho-Rodríguez T Tomás JM Vilca LW Carbajal-León C Cervigni M Gallegos M et al . Socio-demographic variables, fear of COVID-19, anxiety, and depression: prevalence, relationships and explanatory model in the general population of seven latin american countries. Front Psychol. (2021) 12. doi: 10.3389/fpsyg.2021.695989
19
Santabárbara J Lasheras I Lipnicki DM Bueno-Notivol J Pérez-Moreno M López-Antón R et al . Prevalence of anxiety in the COVID-19 pandemic: An updated meta-analysis of community-based studies. Prog Neuropsychopharmacol Biol Psychiatry. (2021) 109:110207. doi: 10.1016/j.pnpbp.2020.110207
20
Espinoza-Ascurra G Gonzales-Graus I Meléndez-Marón M Cabrera R . Prevalencia y Factores Asociados con Depresión en Personal de Salud Durante la Pandemia de SARS-CoV-2 en el Departamento de Piura, Perú. Rev Colomb Psiquiatr. (2021) 53:63–72. doi: 10.1016/j.rcp.2021.11.005
21
Sánchez Carlessi HH Yarlequé Chocas LA Alva LJ Nuñez LLacuachaqui ER Arenas Iparraguirre C Matalinares Calvet ML et al . Anxiety, depression, somatization and experiential avoidance indicators in Peruvian university students in quarantine by COVID-19. Rev la Facultad Medicina Humana. (2021) 21:346–53. doi: 10.25176/RFMH.v21i2.3654
22
Uribe-Hernández Y Ruiz-Tejada J Meneses-Claudio B Gonzalez-Cordero N . Impacto Psicológico por la pandemia COVID-19 en los Profesionales de la Salud de la provincia de Cañete-Perú. UCV-SCIENTIA. (2021) 13:19–28. doi: 10.18050/ucvs.v.13i1.02
23
Landaeta-Díaz L Agüero SD Vinueza-Veloz MF Arias VC Cavagnari BM Ríos-Castillo I et al . Anxiety, Anhedonia, and related food consumption at the beginning of the COVID-19 quarantine in populations of Spanish-speaking Ibero-American countries: An online cross-sectional survey study. SSM Popul Health. (2021) 16:100933. doi: 10.1016/j.ssmph.2021.100933
24
Valladares-Garrido MJ Picón-Reátegui CK Zila-Velasque JP Grados-Espinoza P Vera-Ponce VJ Pereira-Victorio CJ et al . Depression and anxiety in Peruvian military personnel during the pandemic context: a cross-sectional study. BMC Public Health. (2023) 23:691. doi: 10.1186/s12889-023-15612-z
25
Mamani-Benito O Carranza Esteban RF Castillo-Blanco R Lingán-Huamán SK Gálvez-Díaz N del C Huancahuire-Vega S et al . Worry effect for COVID-19 transmission over depression, anxiety, and satisfaction with studies in Peruvian university students. Front Educ (Lausanne). (2023) 8. doi: 10.3389/feduc.2023.1149765
26
Huarcaya-Victoria J Alarcon-Ruiz CA Barzola-Farfán W Cruzalegui-Bazán C Cabrejos-Espinoza M Aspilcueta-Montoya G et al . One-year follow-up of depression, anxiety, and quality of life of Peruvian patients who survived COVID-19. Qual Life Res. (2023) 32:139–49. doi: 10.1007/s11136-022-03208-w
27
Valladares-Garrido D Quiroga-Castañeda PP Berrios-Villegas I Zila-Velasque JP Anchay-Zuloeta C Chumán-Sánchez M et al . Depression, anxiety, and stress in medical students in Peru: a cross-sectional study. Front Psychiatry. (2023) 14. doi: 10.3389/fpsyt.2023.1268872
28
Morales J Basilio-Rojas MR Solano-Canchaya GN Torres-Malca JR Lindo-Cano EF Garcia-Monge VA . Depression, anxiety, and insomnia among Peruvian university students during the COVID-19 pandemic. Int J Health Sci (Qassim). (2022) 15:8988–9001. doi: 10.53730/ijhs.v6nS4.10714
29
Zegarra-López AC Luna-Victoria G Romero-Montenegro D Florentino-Santisteban B Prieto-Molinari DE Montoya-Cuadrao M . Prevalence and predictors of somatization in Peruvian undergraduate students during the COVID-19 pandemic. Int J Environ Res Public Health. (2022) 19:15576. doi: 10.3390/ijerph192315576
30
Yáñez JA Afshar Jahanshahi A Alvarez-Risco A Li J Zhang SX . Anxiety, distress, and turnover intention of healthcare workers in Peru by their distance to the epicenter during the COVID-19 crisis. Am J Trop Med Hyg. (2020) 103:1614–20. doi: 10.4269/ajtmh.20-0800
31
Porter C Favara M Hittmeyer A Scott D Sánchez Jiménez A Ellanki R et al . Impact of the COVID-19 pandemic on anxiety and depression symptoms of young people in the global south: evidence from a four-country cohort study. BMJ Open. (2021) 11:e049653. doi: 10.1136/bmjopen-2021-049653
32
Rondón MB . Salud mental: un problema de salud pública en el Perú. Rev Peru Med Exp Salud Publica. (2006) 23:237–8.
33
Lewis-Fernández R Hinton DE Laria AJ Patterson EH Hofmann SG Craske MG et al . Culture and the anxiety disorders: recommendations for DSM-V. Focus (Madison). (2011) 9:351–68. doi: 10.1176/foc.9.3.foc351
34
Anticona Huaynate CF Pajuelo Travezaño MJ Correa M Mayta Malpartida H Oberhelman R Murphy LL et al . Diagnostics barriers and innovations in rural areas: insights from junior medical doctors on the frontlines of rural care in Peru. BMC Health Serv Res. (2015) 15:454. doi: 10.1186/s12913-015-1114-7
35
Calderón M Alvarado-Villacorta R Barrios M Quiroz-Robladillo D Guzmán Naupay DR Obregon A et al . Health need assessment in an indigenous high-altitude population living on an island in Lake Titicaca, Perú. Int J Equity Health. (2019) 18:94. doi: 10.1186/s12939-019-0993-3
36
Dawson AZ Walker RJ Campbell JA Davidson TM Egede LE . Telehealth and indigenous populations around the world: a systematic review on current modalities for physical and mental health. Mhealth. (2020) 6:30–0. doi: 10.21037/mhealth.2019.12.03
37
Page IS Leitch E Gossip K Charlson F Comben C Diminic S . Modelling mental health service needs of Aboriginal and Torres Strait Islander peoples: a review of existing evidence and expert consensus. Aust N Z J Public Health. (2022) 46:177–85. doi: 10.1111/1753-6405.13202
38
Smye V Browne AJ Josewski V Keith B Mussell W . Social suffering: indigenous peoples’ Experiences of accessing mental health and substance use services. Int J Environ Res Public Health. (2023) 20:3288. doi: 10.3390/ijerph20043288
39
Hualparuca-Olivera L . Cultural lenses of the utility of the ICD-11-PD model: Integrating the Peruvian context. Front Psychiatry. (2022) 13. doi: 10.3389/fpsyt.2022.1016471
40
Oliveira T de S Pereira AMM . Expressions of inequalities in access to health services in Latin America: a scoping review. Cien Saude Colet. (2024) 29:e04932024. doi: 10.1590/1413-81232024297.04932024
41
Aviles Gonzalez CI Cerchiaro Fernandez DM Guerra Munoz ME Romero Ramirez R Abarca Arias YM Brasesco MV et al . Mental health professionals’ Perception of respect for human rights and organizational well-being in three countries of south america. Int J Environ Res Public Health. (2024) 21:214. doi: 10.3390/ijerph21020214
42
Caycho-Rodríguez T Valencia PD Vilca LW Carbajal-León C Vivanco-Vidal A Saroli-Araníbar D et al . Cross-cultural validation of the new version of the Coronavirus Anxiety Scale in twelve Latin American countries. Curr Psychol. (2023) 42:30612–29. doi: 10.1007/s12144-021-02563-0
43
Nyongesa MK Mwangi P Koot HM Cuijpers P Newton CRJC Abubakar A . The reliability, validity and factorial structure of the Swahili version of the 7-item generalized anxiety disorder scale (GAD-7) among adults living with HIV from Kilifi, Kenya. Ann Gen Psychiatry. (2020) 19:62. doi: 10.1186/s12991-020-00312-4
44
Parkerson HA Thibodeau MA Brandt CP Zvolensky MJ Asmundson GJG . Cultural-based biases of the GAD-7. J Anxiety Disord. (2015) 31:38–42. doi: 10.1016/j.janxdis.2015.01.005
45
Sawaya H Atoui M Hamadeh A Zeinoun P Nahas Z . Adaptation and initial validation of the Patient Health Questionnaire – 9 (PHQ-9) and the Generalized Anxiety Disorder – 7 Questionnaire (GAD-7) in an Arabic speaking Lebanese psychiatric outpatient sample. Psychiatry Res. (2016) 239:245–52. doi: 10.1016/j.psychres.2016.03.030
46
Villarreal-Zegarra D Paredes-Angeles R Mayo-Puchoc N Arenas-Minaya E Huarcaya-Victoria J Copez-Lonzoy A . Psychometric properties of the GAD-7 (General Anxiety Disorder-7): a cross-sectional study of the Peruvian general population. BMC Psychol. (2024) 12:183. doi: 10.1186/s40359-024-01688-8
47
Graham-LoPresti JR Abdullah T Calloway A . Culturally responsive assessment and treatment of generalized anxiety disorder. In: Handbook of Cultural Factors in Behavioral Health, vol. p. Springer International Publishing, Cham (2020). p. 231–45.
48
Basile VT Newton-John T Wootton BM . Treatment histories, barriers, and preferences for individuals with symptoms of generalized anxiety disorder. J Clin Psychol. (2024) 80:1286–305. doi: 10.1002/jclp.23665
49
Spitzer RL Kroenke K Williams JBW Löwe B . A brief measure for assessing generalized anxiety disorder. Arch Intern Med. (2006) 166:1092. doi: 10.1001/archinte.166.10.1092
50
Cotiga AC Zanfirescu ŞA Iliescu D Ciumăgeanu M Gotca I Popa CO . Psychometric characteristics of the Romanian adaptation of the GAD-7. J Psychopathol Behav Assess. (2023) 45:691–701. doi: 10.1007/s10862-023-10062-8
51
Camargo L Herrera-Pino J Shelach S Soto-Añari M Porto MF Alonso M et al . Escala de ansiedad generalizada GAD-7 en profesionales médicos Colombianos durante pandemia de COVID-19: validez de constructo y confiabilidad. Rev Colomb Psiquiatr. (2023) 52:245–50. doi: 10.1016/j.rcp.2021.06.003
52
Johnson SU Ulvenes PG Øktedalen T Hoffart A . Psychometric properties of the general anxiety disorder 7-item (GAD-7) scale in a heterogeneous psychiatric sample. Front Psychol. (2019) 10. doi: 10.3389/fpsyg.2019.01713
53
Porto MF Ocampo-Barba N Flores-Valdivia G Caldichoury N López N . Propiedades psicométricas del GAD-7 para detectar ansiedad generaliza en profesionales sanitarios de Bolivia. Rev Peru Med Exp Salud Publica. (2022) 39:115–6. doi: 10.17843/rpmesp.2022.391.8620
54
Bolgeo T Di Matteo R Simonelli N Dal Molin A Lusignani M Bassola B et al . Psychometric properties and measurement invariance of the 7-item General Anxiety Disorder scale (GAD-7) in an Italian coronary heart disease population. J Affect Disord. (2023) 334:213–9. doi: 10.1016/j.jad.2023.04.140
55
Plummer F Manea L Trepel D McMillan D . Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. (2016) 39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005
56
Garcia-Campayo J Zamorano E Ruiz MA Pardo A Perez-Paramo M Lopez-Gomez V et al . Cultural adaptation into Spanish of the generalized anxiety disorder-7 (GAD-7) scale as a screening tool. Health Qual Life Outcomes. (2010) 8:8. doi: 10.1186/1477-7525-8-8
57
Donker T van Straten A Marks I Cuijpers P . Quick and easy self-rating of Generalized Anxiety Disorder: Validity of the Dutch web-based GAD-7, GAD-2 and GAD-SI. Psychiatry Res. (2011) 188:58–64. doi: 10.1016/j.psychres.2011.01.016
58
Hinz A Klein AM Brähler E Glaesmer H Luck T Riedel-Heller SG et al . Psychometric evaluation of the Generalized Anxiety Disorder Screener GAD-7, based on a large German general population sample. J Affect Disord. (2017) 210:338–44. doi: 10.1016/j.jad.2016.12.012
59
Sousa TV Viveiros V Chai MV Vicente FL Jesus G Carnot MJ et al . Reliability and validity of the Portuguese version of the Generalized Anxiety Disorder (GAD-7) scale. Health Qual Life Outcomes. (2015) 13:50. doi: 10.1186/s12955-015-0244-2
60
Krizova K Halamová J Strnádelová B Baránková M . Psychometric analysis of the GAD-7 questionnaire in Slovak helping professionals. J Affect Disord Rep. (2024) 17:100803. doi: 10.1016/j.jadr.2024.100803
61
Yu Y Liu ZW Zhou W Zhao M Qiu D Li YL et al . Cutoff of the Zarit Burden Interview in predicting depression and anxiety. Qual Life Res. (2019) 28:2525–33. doi: 10.1007/s11136-019-02208-7
62
Vrublevska J Renemane L Kivite-Urtane A Rancans E . Validation of the generalized anxiety disorder scales (GAD-7 and GAD-2) in primary care settings in Latvia. Front Psychiatry. (2022) 13. doi: 10.3389/fpsyt.2022.972628
63
Osterlind SJ . Constructing test items. 2nd ed Vol. 47. . Dordrecht: Springer Dordrecht (1998). Evaluation in Education and Human Services. doi: 10.1007/0-306-47535-9
64
American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American: Editosdsaqrial Médica Panamericana (2013).
65
Masuyama A Shinkawa H Kubo T . Validation and psychometric properties of the Japanese version of the fear of COVID-19 scale among adolescents. Int J Ment Health Addict. (2022) 20:387–97. doi: 10.1007/s11469-020-00368-z
66
Muñoz-Navarro R Cano-Vindel A Moriana JA Medrano LA Ruiz-Rodríguez P Agüero-Gento L et al . Screening for generalized anxiety disorder in Spanish primary care centers with the GAD-7. Psychiatry Res. (2017) 256:312–7. doi: 10.1016/j.psychres.2017.06.023
67
Seo JG Park SP . Validation of the Generalized Anxiety Disorder-7 (GAD-7) and GAD-2 in patients with migraine. J Headache Pain. (2015) 16:97. doi: 10.1186/s10194-015-0583-8
68
Zhong QY Gelaye B Zaslavsky AM Fann JR Rondon MB Sánchez SE et al . Diagnostic validity of the generalized anxiety disorder - 7 (GAD-7) among pregnant women. PloS One. (2015) 10:e0125096. doi: 10.1371/journal.pone.0125096
69
Soto CM Segovia JL . Intervalos de confianza asimétricos para el índice la validez de contenido: Un programa Visual Basic para la V de Aiken (2009). Available online at: https://revistas.um.es/analesps/article/view/71631 (Accessed February 12, 2024).
70
Aiken LR . Content validity and reliability of single items or questionnaires. Educ Psychol Meas. (1980) 40:955–9.
71
Aiken LR . Three coefficients for analyzing the reliability and validity of ratings. Educ Psychol Meas. (1985) 45:131–42. doi: 10.1177/0013164485451012
72
Aiken LR . Tests psicológicos y evaluación. Mexico: Pearson Educación (2003). p. 528.
73
Mannheim B . The Language of the Inka since the European Invasion. New York, USA: University of Texas Press (1991).
74
Mannheim B Salas Carreño G . Wak’as: Entifications of the Andean Sacred. In: The Archaeology of Wak’as: Explorations of the Sacred in the Pre-Columbian Andes. Boulder, CO: University Press of Colorado (2015). p. 47–72.
75
Lévi-Strauss C . Totemism. Boston: Beacon Press (1971).
76
Cjuno J Villegas-Mejía RA Coronado-Fernández J . Adaptación y análisis psicométrico del cuestionario de ansiedad generalizada (GAD-7) al Quechua Collao en Perú. Rev Peru Med Exp Salud Publica. (2024) 41:121–8. doi: 10.17843/rpmesp.2024.412.13373
77
Muller L . Indigenous Research into Mainstream Australian Culture. London: Routledge (2023).
78
Boksa P Joober R Kirmayer LJ . Mental wellness in Canada’s Aboriginal communities: striving toward reconciliation. J Psychiatry Neurosci. (2015) 40:363–5. doi: 10.1503/jpn.150309
79
Gall A Anderson K Howard K Diaz A King A Willing E et al . Wellbeing of indigenous peoples in Canada, aotearoa (New zealand) and the United States: A systematic review. Int J Environ Res Public Health. (2021) 18:5832. doi: 10.3390/ijerph18115832
80
Gould B MacQuarrie C O’Connell ME Bourassa C . Mental wellness needs of two Indigenous communities: Bases for culturally competent clinical services. Can Psychol. (2021) 62:213–26. doi: 10.1037/cap0000247
81
Simonds VW Christopher S . Adapting western research methods to indigenous ways of knowing. Am J Public Health. (2013) 103:2185–92. doi: 10.2105/AJPH.2012.301157
82
Browne AJ Varcoe C Lavoie J Smye V Wong ST Krause M et al . Enhancing health care equity with Indigenous populations: evidence-based strategies from an ethnographic study. BMC Health Serv Res. (2016) 16:544. doi: 10.1186/s12913-016-1707-9
83
Fijal D Beagan BL . Indigenous perspectives on health: Integration with a Canadian model of practice. Can J Occup Ther. (2019) 86:220–31. doi: 10.1177/0008417419832284
84
Kirmayer LJ Sehdev M Whitley R Dandeneau SF Isaac C . Community resilience: models, metaphors and measures. Int J Indig Health. (2009) 5:62–117.
85
Snodgrass JG Lacy MG Upadhyay C . Developing culturally sensitive affect scales for global mental health research and practice: Emotional balance, not named syndromes, in Indian Adivasi subjective well-being. Soc Sci Med. (2017) 187:174–83. doi: 10.1016/j.socscimed.2017.06.037
86
Brinckley MM Calabria B Walker J Thurber KA Lovett R . Reliability, validity, and clinical utility of a culturally modified Kessler scale (MK-K5) in the Aboriginal and Torres Strait Islander population. BMC Public Health. (2021) 21:1111. doi: 10.1186/s12889-021-11138-4
87
Kohrt BA Rasmussen A Kaiser BN Haroz EE Maharjan SM Mutamba BB et al . Cultural concepts of distress and psychiatric disorders: literature review and research recommendations for global mental health epidemiology. Int J Epidemiol. (2014) 43:365–406. doi: 10.1093/ije/dyt227
88
Newton D Day A Gillies C Fernandez E . A review of evidence-based evaluation of measures for assessing social and emotional well-being in indigenous Australians. Aust Psychol. (2015) 50:40–50. doi: 10.1111/ap.12064
89
Martínez-Radl FB Hinton DE Stangier U . Susto as a cultural conceptualization of distress: Existing research and aspects to consider for future investigations. Transcult Psychiatry. (2023) 60:690–702. doi: 10.1177/13634615231163986
90
Bazo-Alvarez JC Aparicio ARO Robles-Mariños R Julca-Guerrero F Gómez H Bazo-Alvarez O et al . Cultural adaptation to Bolivian Quechua and psychometric analysis of the Patient Health Questionnaire PHQ-9. BMC Public Health. (2024) 24:129. doi: 10.1186/s12889-023-17566-8
91
Carranza Esteban RF Mamani-Benito O Cjuno J Tito-Betancur M Caycho-Rodríguez T Vilca LW et al . Adaptación y validación de la Patient Health Questionnaire for Depression and Anxiety (PHQ-4) en una muestra de quechua hablantes Peruanos. Medicina Clínica y Social. (2024) 8:63–74. doi: 10.52379/mcs.v8i1.361
92
Uysal-Bozkir Ö Parlevliet JL de Rooij SE . Insufficient cross-cultural adaptations and psychometric properties for many translated health assessment scales: A systematic review. J Clin Epidemiol. (2013) 66:608–18. doi: 10.1016/j.jclinepi.2012.12.004
93
Jain M Tandon S Sharma A Jain V Rani Yadav N . Cross-Cultural adaption, validity and reliability of a Hindi versionof the Corah’s Dental Anxiety Scale. Health Promot Perspect. (2018) 8:120–6. doi: 10.15171/hpp.2018.15
94
Yang M Seon Q Gomez Cardona L Karia M Velupillai G Noel V et al . Safe and valid? A systematic review of the psychometric properties of culturally adapted depression scales for use among Indigenous populations. Cambridge Prisms: Global Ment Health. (2023) :10:e60. doi: 10.1017/gmh.2023.52
95
Demes KA Geeraert N . Measures matter. J Cross Cult Psychol. (2014) 45:91–109. doi: 10.1177/0022022113487590
96
Ribeiro Santiago PH Nielsen T Smithers LG Roberts R Jamieson L . Measuring stress in Australia: validation of the perceived stress scale (PSS-14) in a national sample. Health Qual Life Outcomes. (2020) 18:100. doi: 10.1186/s12955-020-01343-x
97
Getting it Right Collaborative Group Hackett ML Teixeira-Pinto A Farnbach S Glozier N Skinner T et al . Getting it Right: validating a culturally specific screening tool for depression (aPHQ -9) in Aboriginal and Torres Strait Islander Australians. Med J Aust. (2019) 211:24–30. doi: 10.5694/mja2.50212
98
Gallardo-Peralta LP Sánchez-Moreno E Rodríguez-Rodríguez V . Strangers in their own world: exploring the relation between cultural practices and the health of older adults in native communities in Chile. Br J Soc Work. (2019) 49:920–42. doi: 10.1093/bjsw/bcz045
99
Sánchez-Moreno E Gallardo-Peralta LP Leyton C . The social gradient in mental health and well-being for indigenous older adults living in rural areas: A cross-sectional comparison with rural non-indigenous population in Chile. J Aging Health. (2021) 33:287–99. doi: 10.1177/0898264320979201
100
Meldrum K Andersson E Webb T Quigley R Strivens E Russell S . Screening depression and anxiety in Indigenous peoples: A global scoping review. Transcult Psychiatry. (2023) 0(0):1–16. doi: 10.1177/13634615231187257
101
Kohrt BA Mendenhall E Brown PJ . How anthropological theory and methods can advance global mental health. Lancet Psychiatry. (2016) 3:396–8. doi: 10.1016/S2215-0366(16)00046-8
102
Jain S Orr DMR . Ethnographic perspectives on global mental health. Transcult Psychiatry. (2016) 53:685–95. doi: 10.1177/1363461516679322
103
Cianconi P Lesmana CBJ Ventriglio A Janiri L . Mental health issues among indigenous communities and the role of traditional medicine. Int J Soc Psychiatry. (2019) 65:289–99. doi: 10.1177/0020764019840060
104
Organizacion Mundial de la salud . Global plan of action for health of indigenous peoples (2024). Available online at: https://www.who.int/initiatives/global-plan-of-action-for-health-of-indigenous-peoples (Accessed November 25, 2024).
105
Lee C Wozniak LA Soprovich AL Sharma V Healy B Samanani S et al . Mental health experiences with COVID-19 public health measures in an Alberta First Nations Community. Int J Ment Health Syst. (2022) 16:22. doi: 10.1186/s13033-022-00532-z
106
Warne D Dulacki K Spurlock M Meath T Davis MM Wright B et al . Adverse childhood experiences (ACE) among american Indians in south dakota and associations with mental health conditions, alcohol use, and smoking. J Health Care Poor Underserved. (2017) 28:1559–77. doi: 10.1353/hpu.2017.0133
107
Doi S Ito M Takebayashi Y Muramatsu K Horikoshi M . Factorial validity and invariance of the 7-item generalized anxiety disorder scale (GAD-7) among populations with and without self-reported psychiatric diagnostic status. Front Psychol. (2018) :9. doi: 10.3389/fpsyg.2018.01741
108
Ahn JK Kim Y Choi KH . The psychometric properties and clinical utility of the korean version of GAD-7 and GAD-2. Front Psychiatry. (2019) 10. doi: 10.3389/fpsyt.2019.00127
109
Sun J Liang K Chi X Chen S . Psychometric properties of the generalized anxiety disorder scale-7 item (GAD-7) in a large sample of chinese adolescents. Healthcare. (2021) 9:1709. doi: 10.3390/healthcare9121709
110
Gong Y Zhou H Zhang Y Zhu X Wang X Shen B et al . Validation of the 7-item Generalized Anxiety Disorder scale (GAD-7) as a screening tool for anxiety among pregnant Chinese women. J Affect Disord. (2021) 282:98–103. doi: 10.1016/j.jad.2020.12.129
111
Adjorlolo S . Generalised anxiety disorder in adolescents in Ghana: Examination of the psychometric properties of the Generalised Anxiety Disorder-7 scale. Afr J psychol Assess. (2019) 1(0):a10. doi: 10.4102/ajopa.v1i0.10
112
Zhang C Wang T Zeng P Zhao M Zhang G Zhai S et al . Reliability, validity, and measurement invariance of the general anxiety disorder scale among chinese medical university students. Front Psychiatry. (2021) 12. doi: 10.3389/fpsyt.2021.648755
113
Shevlin M Butter S McBride O Murphy J Gibson-Miller J Hartman TK et al . Measurement invariance of the Patient Health Questionnaire (PHQ-9) and Generalized Anxiety Disorder scale (GAD-7) across four European countries during the COVID-19 pandemic. BMC Psychiatry. (2022) 22:154. doi: 10.1186/s12888-022-03787-5
114
De Man J Absetz P Sathish T Desloge A Haregu T Oldenburg B et al . Are the PHQ-9 and GAD-7 suitable for use in India? A psychometric analysis. Front Psychol. (2021) 12. doi: 10.3389/fpsyg.2021.676398
115
Ip H Suen YN Hui CLM Wong SMY Chan SKW Lee EHM et al . Assessing anxiety among adolescents in Hong Kong: psychometric properties and validity of the Generalised Anxiety Disorder-7 (GAD-7) in an epidemiological community sample. BMC Psychiatry. (2022) 22:703. doi: 10.1186/s12888-022-04329-9
116
Löwe B Decker O Müller S Brähler E Schellberg D Herzog W et al . Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med Care. (2008) 46:266–74. doi: 10.1097/MLR.0b013e318160d093
117
Zolotareva AA . Adaptation of the Russian version of the generalized anxiety disorder-7. Couns Psychol Psychotherapy. (2023) 31:31–46. doi: 10.17759/cpp.2023310402
118
Dos Santos Silva L De Farias Leite M Lima Barros Feitosa A Faro A . Propriedades psicométricas da GAD-7 no Brasil. Psico. (2023) 54:e39902. doi: 10.15448/10.15448/1980-8623.2023.1
119
Zinchuk M Kustov G Rider F Pashnin E Voinova N Popova S et al . Psychometric properties of the Russian language version of the GAD-7 in patients with epilepsy. J Neurol Sci. (2021) 429:119186. doi: 10.1016/j.jns.2021.119186
120
López N Coronado JC Quispe-Ayala C García-Roncallo P Cárdenas-Valverde J Flórez Y et al . Clinical validation of the GAD-7 for the Peruvian Quechua population. Gen Hosp Psychiatry. (2024) 92:119–20. doi: 10.1016/j.genhosppsych.2024.10.008
121
Tong X An D McGonigal A Park SP Zhou D . Validation of the Generalized Anxiety Disorder-7 (GAD-7) among Chinese people with epilepsy. Epilepsy Res. (2016) 120:31–6. doi: 10.1016/j.eplepsyres.2015.11.019
122
Bhana A Mntambo N Gigaba SG Luvuno ZPB Grant M Ackerman D et al . Validation of a brief mental health screening tool for common mental disorders in primary healthcare. South Afr Med J. (2019) 109:278. doi: 10.7196/SAMJ.2019.v109i4.13664
123
Luo Z Li Y Hou Y Zhang H Liu X Qian X et al . Adaptation of the two-item generalized anxiety disorder scale (GAD-2) to Chinese rural population: A validation study and meta-analysis. Gen Hosp Psychiatry. (2019) :60:50–6. doi: 10.1016/j.genhosppsych.2019.07.008
124
Mughal AY Devadas J Ardman E Levis B Go VF Gaynes BN . A systematic review of validated screening tools for anxiety disorders and PTSD in low to middle income countries. BMC Psychiatry. (2020) 20:338. doi: 10.1186/s12888-020-02753-3
125
Janca A Lyons Z Balaratnasingam S Parfitt D Davison S Laugharne J . Here and Now Aboriginal Assessment: background, development and preliminary evaluation of a culturally appropriate screening tool. Australas Psychiatry. (2015) 23:287–92. doi: 10.1177/1039856215584514
126
Tennyson RL Kemp CG Rao D . Challenges and strategies for implementing mental health measurement for research in low-resource settings. Int Health. (2016) 8:374–80. doi: 10.1093/inthealth/ihw043
127
Russell SG Quigley R Thompson F Sagigi B Miller G LoGiudice D et al . Culturally appropriate assessment of depression and anxiety in older torres strait islanders: limitations and recommendations. Clin Gerontol. (2023) 46:240–52. doi: 10.1080/07317115.2022.2086090
128
Dhira TA Rahman MA Sarker AR Mehareen J . Validity and reliability of the Generalized Anxiety Disorder-7 (GAD-7) among university students of Bangladesh. PloS One. (2021) 16:e0261590. doi: 10.1371/journal.pone.0261590
129
Manzar MD Alghadir AH Anwer S Alqahtani M Salahuddin M Addo HA et al . Psychometric properties of the general anxiety disorders-7 scale using categorical data methods: A study in a sample of university attending Ethiopian young adults. Neuropsychiatr Dis Treat. (2021) 17:893–903. doi: 10.2147/NDT.S295912
130
Belus JM Muanido A Cumbe VFJ Manaca MN Wagenaar BH . Psychometric validation of a combined assessment for anxiety and depression in primary care in Mozambique (CAD-MZ). Assessment. (2022) 29:1890–900. doi: 10.1177/10731911211032285
131
Pheh KS Tan CS Lee KW Tay KW Ong HT Yap SF . Factorial structure, reliability, and construct validity of the Generalized Anxiety Disorder 7-item (GAD-7): Evidence from Malaysia. PloS One. (2023) 18:e0285435. doi: 10.1371/journal.pone.0285435
Summary
Keywords
clinical utility, case-control study, GAD-7 test, rural indigenous, Quechua
Citation
Caldichoury N, Quispe-Ayala C, Coronado J-C, Castellanos-Alvarenga LM, Salazar D, Morales-Asencio B, Ripoll-Córdoba D, Quincho-Apumayta R, Cárdenas-Valverde J, Camargo L, Alcos-Flores K, Layme-Condori E, Villalba-Arbañil R, Castellanos C, Gargiulo PA, Quispe-Rodríguez I, Muñoz-Romero E, Patiño-Rivera AR, Flores-Poma I, Herrera-Pino J and López N (2025) Clinical utility of the GAD-7 for detecting generalized anxiety in Quechua indigenous people. Front. Psychiatry 16:1565895. doi: 10.3389/fpsyt.2025.1565895
Received
23 January 2025
Accepted
13 May 2025
Published
30 May 2025
Volume
16 - 2025
Edited by
Marco Grados, Johns Hopkins University, United States
Reviewed by
Jose Livia, National University Federico Villareal, Peru
Haidong Song, Affiliated Mental Health Center Zhejiang University School of Medicine, China
Henrry Sánchez, Universidad Santo Tomás, Seccional Villavicencio, Colombia
Updates
Copyright
© 2025 Caldichoury, Quispe-Ayala, Coronado, Castellanos-Alvarenga, Salazar, Morales-Asencio, Ripoll-Córdoba, Quincho-Apumayta, Cárdenas-Valverde, Camargo, Alcos-Flores, Layme-Condori, Villalba-Arbañil, Castellanos, Gargiulo, Quispe-Rodríguez, Muñoz-Romero, Patiño-Rivera, Flores-Poma, Herrera-Pino and López.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Norman López, normanlopezve@santotomas.cl
†Deceased
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.