- 1Tobacco Settlement Endowment Trust (TSET) Health Promotion Research Center, The University of Oklahoma Health Sciences, Tulsa, OK, United States
- 2Department of Psychology, The University of Tulsa, Tulsa, OK, United States
- 3Department of Psychology, Oklahoma State University, Tulsa, OK, United States
- 4Department of Health Promotion Sciences, The University of Oklahoma Health Sciences, Tulsa, OK, United States
Background: Native Americans (NAs) experience higher rates of chronic pain than other U.S. ethnic/racial groups. This may be partly caused by stress from interpersonal discrimination, which promotes pain-related catastrophizing and anxiety, cognitive-emotional processes that amplify pain. Greater identification with NA culture has been shown to buffer against negative health outcomes for NA communities, therefore the present study examined whether greater identification with NA culture buffers against the harmful effects of discrimination on pain-related anxiety and catastrophizing.
Material and Methods: Participants were 153 healthy, chronic pain-free NAs enrolled in the Oklahoma Study of Native American Pain Risk (OK-SNAP). Identification with NA culture was assessed by the Native American Acculturation Scale (NAAS), which was reversed scored so that higher scores=greater identification. Interpersonal discrimination was assessed by the Everyday Discrimination Scale. Following laboratory pain tasks, situational pain catastrophizing was assessed with the Pain Catastrophizing Scale and pain-related anxiety was assessed with a visual analogue scale (VAS).
Results: A significant interaction was found between discrimination and identification with NA culture when predicting pain catastrophizing (ΔR2 = 0.034, p = 0.017). Greater identification with NA culture was associated with a significant positive relationship between discrimination and pain catastrophizing (p < 0.001), whereas less identification was associated with a non-significant relationship (p = 0.32). Although discrimination was associated with higher pain-related anxiety (p = 0.015), this was not moderated by identification with NA culture (ΔR2 = 0.009, p = 0.23), nor did identification with NA culture predict pain-related anxiety. An additional analysis found that NAs who identified more with NA culture experienced more discrimination (p = 0.012).
Conclusions: These findings suggest that the relationship between discrimination and pain catastrophizing is stronger for NAs who identify more strongly with NA culture, an effect that is likely due to these individuals having greater overall exposure to discrimination. Alternatively, the NAAS may not capture the full range of cultural processes that buffer against negative health outcomes for NAs. Future research should examine other facets of cultural resilience.
1 Introduction
Chronic pain is experienced by approximately 20% of adults in the United States and is associated with significant negative consequences (1), such as poorer occupational performance, psychological wellbeing, physical functioning, and sleep (2). Native Americans (NAs) exhibit alarmingly high chronic pain prevalence rates compared to other racial and ethnic communities in the United States – nearly 1 in 3 NAs experience chronic pain (3). The Oklahoma Study of Native American Pain Risk (OK-SNAP) found that healthy, pain-free NAs were 2.9 times more likely to develop chronic pain than non-Hispanic White (NHW) individuals within a 2-year period (4) and 4 times more likely to develop chronic pain within a 5-year period (5). This pain inequity is partly explained by experiences with interpersonal discrimination that promote pain-related anxiety and pain catastrophizing, cognitive-affective processes that amplify pain (4).
Interpersonal discrimination refers to a negative attitude or unfair treatment (e.g., harassment, exclusion, differential treatment) towards a group of people, and research has found it contributes to poorer health outcomes in underserved communities (6). NAs report experiencing interpersonal discrimination across many settings, including healthcare, police encounters, housing, and employment opportunities (7). Moreover, interpersonal discrimination is associated with higher blood pressure (8), depressive symptoms (9), and physical pain and impairment (10) for NAs. Research on non-NA populations has shown that both lifetime and daily interpersonal discrimination increases one’s likelihood of developing chronic pain (11) and our research has shown that interpersonal discrimination partially explains the higher rate of chronic pain in NAs (4, 5). Together, these findings highlight the importance of interpersonal discrimination as a potential contributor to the NA chronic pain inequity. The current manuscript aims to investigate if greater identification with NA culture buffers against the negative impact of interpersonal discrimination on pain related anxiety and pain catastrophizing.
Pain-related anxiety is a future-oriented, negative affective response to potential threats that enhances pain (12). Pain catastrophizing refers to cognitive processes involving pain magnification, rumination about pain, and feelings of helplessness, which work together to amplify the pain experience (13). Pain-related anxiety and catastrophizing are associated with lower heat pain threshold/tolerance (12, 14), heightened postoperative pain intensity (15), and increased risk for postsurgical chronic pain (16). Our previous work has shown that NAs report more pain-related anxiety and catastrophizing than NHWs in response to painful tasks (17), and these cognitive-affective pain amplifiers are associated with increased risk of prospectively developing chronic pain for NAs (5, 18, 19).
Given the detrimental impact of interpersonal discrimination and cognitive-affective pain amplifiers on chronic pain outcomes for NAs, it is important to find protective factors that ameliorate this pain disparity. Identification with NA culture is one potential factor. Indeed, Walters and Simoni introduced the Indigenist Stress Coping Model, which states that cultural processes such as identification with NA culture and spirituality are coping mechanisms for life stressors such as interpersonal discrimination and historical trauma (20). In their conceptualization, Ward & Szabó explain that cultural identification includes both enculturation and acculturation processes. Enculturation “refers to the process of being socialized into a particular culture” whereas acculturation refers to navigating the relationships between traditional and mainstream cultural identities (21, p. 268). Thus, NA cultural identification has been measured using enculturation and acculturation scales (22–24). For example, Garrett and Pichette developed the Native American Acculturation Scale (NAAS) to assess cultural identity along an acculturation continuum ranging from identification with traditional NA cultural practices to assimilated into mainstream American culture, with the midpoint representing bicultural identification (22).
Previous research has found that greater identification with NA culture is protective against alcohol use (25) and depressive symptoms (9) for NA adults. Additionally, Fetter and Thompson found that strong ethnic identity moderated (buffered) the relationship between historical loss and wellbeing in a sample of NA college students (26). Further studies with NA youth have demonstrated greater identification with NA culture is protective against suicidal ideation (27) and promotes academic success (28) and resilience (29). Moreover, a recent scoping review highlights identification with NA culture as a factor that protects against negative health outcomes because of enhanced resilience promoted by increased social support, wellbeing, and engagement with traditional practices (30). However, it has also been shown that greater identification with NA culture is associated with experiencing more interpersonal discrimination (25, 31, 32), and historical loss thinking (e.g., frequency of thinking about loss of land, people, and/or culture (25, 32);, both of which have negative health outcomes.
The current study is a secondary analysis of data collected from OK-SNAP. In OK-SNAP, healthy, pain-free NHW and NA adults were recruited to identify potential mechanisms contributing to the NA pain disparity before chronic pain had developed. Several pain tasks were administered to assess individual differences in pain sensitivity, central sensitization, and pain inhibition. However, these tasks also provided an ecologically-valid opportunity to assess pain-related anxiety and catastrophizing in response to pain – processes that amplify pain and increase chronic pain risk (33). For the present study, only data from NA participants in OK-SNAP were used, given that the study aim was to investigate whether identification with NA culture buffers against (moderates) the harmful effects of interpersonal discrimination. It was hypothesized that greater cultural identification would be associated with a weaker relationship between interpersonal discrimination and pain-related anxiety and pain catastrophizing.
2 Materials and methods
2.1 Participants
Participants included 153 healthy, pain-free NA individuals who participated in OK-SNAP. Participants were recruited from NA newspapers, fliers, personal communications with NA groups, email announcements, and online platforms (e.g., Facebook). OK-SNAP exclusion criteria were: (1) <18 years old, (2) history of cardiovascular, neuroendocrine, musculoskeletal, and neurological disorders, (3) reported chronic pain or acute pain problems, (4) BMI ≥ 35, (5) use of antidepressants, anxiolytic, analgesic, stimulant, or antihypertensive medication, (6) current psychotic symptoms or substance use problems, and/or (7) an inability to read and speak English. OK-SNAP data collection occurred from March 2014 to October 2018. Procedures were approved by the University of Tulsa, Cherokee Nation, and Indian Health Service Oklahoma City Area Office institutional review boards (IRBs). All participants provided informed consent and were able to withdraw from the study at any point. NA status was verified through Certificate of Degree of Indian Blood (CDIB) or tribal membership cards. NA participants represent tribal nations predominately from eastern Oklahoma and the southern plains, but tribal affiliation was not reported to respect tribal community confidentiality (33).
2.2 Procedures
OK-SNAP was performed over a 2-day testing period, lasting approximately 4 to 6 hours each testing day. A full description of study procedures is provided elsewhere (33). Screening for inclusion/exclusion criteria and informed consent were performed on the first testing day. One testing day consisted of pain sensitivity tasks including assessment of threshold and tolerance of cold, heat, ischemia, pressure, and electric pain. The other testing day assessed measures of central sensitization and pain inhibition. Central sensitization tasks consisted of nociceptive flexion response (NFR) threshold, temporal summation of NFR (TS-NFR), and temporal summation of heat pain (TS-Heat). Pain inhibition tasks included emotional controls of nociception (ECON) and conditioned pain modulation (CPM).
Situational pain catastrophizing and pain-related anxiety were assessed after each pain task. Each measure was averaged across tasks and used as the primary dependent variables in the present study. Participants were compensated $100 for each completed testing day or $10 an hour for non-completed days (33).
2.3 Questionnaires
2.3.1 Demographics
A custom-built demographics questionnaire was used to collect background information including age at enrollment, sex assigned at birth (male vs. female), race, marital status, highest level of completed education, employment status, annual household income, and body mass index (BMI). To be included in the current study, participants were required to have chosen American Indian/Alaskan Native or mixed race, including American Indian/Alaskan Native, which was verified by presentation of a CDIB or tribal identification card. Participant height and weight were measured using a medical scale and then used to calculate BMI in kg/m2 (4).
2.3.2 Interpersonal discrimination
The 9-item Everyday Discrimination Scale was used to assess the frequency of interpersonal discrimination experienced in daily life (34). Questions include, “You are treated with less courtesy than other people are,” “People act as if they think you are dishonest,” and “You are threatened or harassed.” Participants responded to “In your day-to-day life, how often do any of the following things happen to you?” to each of the 9 items on a 6-point Likert scale with ratings ranging from: 1 = “Almost every day,” 2 = “At least once a week,” 3 = “A few times a month,” 4 = “A few times a year,” 5 = “Less than once a year,” and 6 = “Never.” Responses were reverse scored and averaged. Thus, scores ranged from 1 to 6, with higher scores being indicative of more frequent experiences of interpersonal discrimination. A final question asked participants what they thought the main reason was for their interpersonal discrimination experiences (e.g., gender, race, age, weight, income level, sexual orientation). Cronbach’s alpha was 0.897 (4).
2.3.3 Situational pain catastrophizing
The 13-item Pain Catastrophizing Scale (PCS) was used to assess situational pain catastrophizing immediately following each pain task. The PCS assesses rumination, magnification, and helplessness in response to pain. Questions include, “I anxiously want the pain to go away,” “I become afraid that the pain may get worse,” and “I worry all the time about whether the pain will end.” Participants rated each of the 13 items on a 5-point Likert scale (0 = “Not at all,” 1 = “To a slight degree,” 2 = “To a moderate degree,” 3 = “To a great degree,” and 4 = “All the time”). The 13 items of the PCS were summed to provide a total score ranging from 0-52, with higher scores indicating greater pain catastrophizing (13). To assess situational catastrophizing, instructions were modified so that participants were asked to think back to the thoughts they experienced during each pain task. The 10 total PCS scores across the 10 pain tasks had a Cronbach’s alpha of 0.92, thus an overall situational pain catastrophizing score was created by averaging across the tasks (4).
2.3.4 Pain-related anxiety
A visual analog scale (VAS) was used to assess pain-related anxiety following each of the 10 pain tasks. Instructions to participants were, “Using this scale, rate how anxious the [insert pain test] made you feel.” Participants rated their pain-related anxiety on a scale that ranged from “not at all anxious” to “extremely anxious.” VAS responses were converted to scores ranging from 0 to 100, with higher scores representing more pain-related anxiety. Cronbach’s alpha for the 10 pain-related anxiety scores in response to the 10 pain tasks was 0.90, thus an overall pain-related anxiety score was created by averaging across the tasks (4).
2.3.5 Identification with Native American culture
The 20-item Native American Acculturation Scale (NAAS) was used to assess overall identification with NA culture on an acculturation continuum (22). The NAAS includes domains related to language, identity, friendships, behaviors, generational/geographic background, and attitudes. Questions on the NAAS include “What language can you speak?,” “How do you identify yourself?,” and “What contact have you had with Native American communities?” Participants’ responses were reverse scored so that higher scores would reflect greater identification with culture to ease interpretation. Scores were then averaged creating an overall score that ranged from 1 = “lower identification with NA culture” to 5 = “greater identification with NA culture,” with a midpoint score of 3 indicating bicultural identification. Cronbach’s alpha was 0.88 (33).
2.4 Data analysis
Before performing primary analyses, variable distributions were inspected using box plots, histograms, and tests of normality. Outlier values were identified using the MAD-median procedure with a recommended cutoff score of 2.24 (35) and winsorized with the nearest non-outlier value. Winsorized variables in the current study were interpersonal discrimination, identification with NA culture, and situational pain catastrophizing. Age was log-10 transformed to adjust for positive skew. The following variables had missing values: interpersonal discrimination (3.9%), identification with NA culture (3.9%), income (3.3%), BMI (2.6%), marital status (2.0%), employment status (1.3%), situational pain catastrophizing (1.3%), pain-related anxiety (1.3%), and highest level of completed education (0.7%). To avoid listwise deletion in regression models, the expectation-maximization (EM) algorithm in LISREL 8.80 (Scientific Software International, Chapel Hill, NC) was performed to impute missing values. Significance level was set at α<.05 (2-tailed) for all analyses.
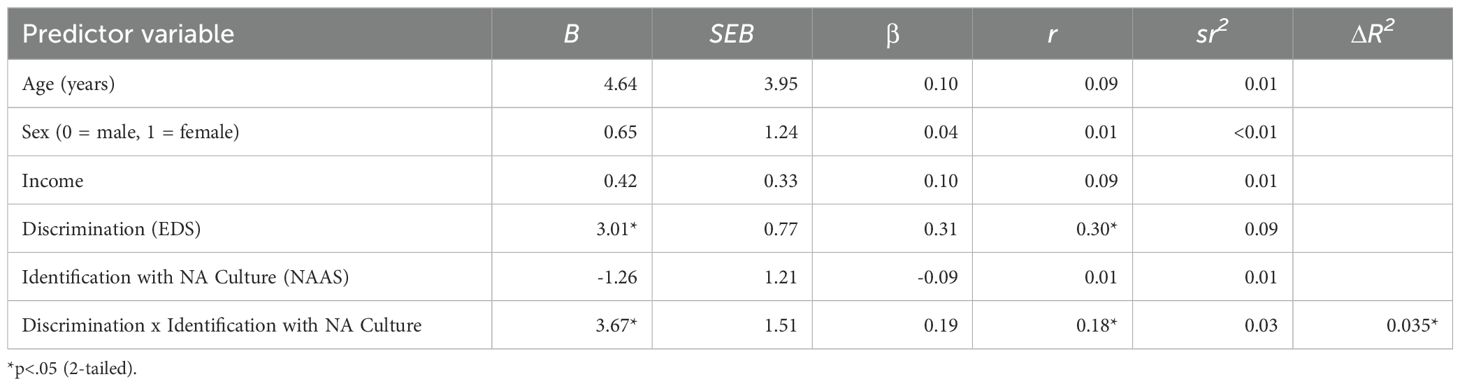
Two moderated regression analyses were performed using PROCESS v4.2 (36). In the first model, pain-related anxiety was the criterion variable. In the second model, situational pain catastrophizing was the criterion variable. Both models included the same predictors: interpersonal discrimination, identification with NA culture, and the interaction term between interpersonal discrimination and identification with NA culture. Primary analysis controlled for age, sex, and income given that epidemiological studies in the U.S. have found that older age, female sex, and lower socioeconomic position are chronic pain risk factors (37).
Before the creation of interaction terms, main effect variables were mean centered. Identification with NA culture was conceptualized as the moderator in both models. In the event of a significant interaction, simple effects were examined at -1SD, the mean, and +1SD of the moderator. To establish if there is a relationship between identification with NA culture and exposure to discrimination, a simple regression was conducted in SPSS v29 (IBM, Armonk, NY) with interpersonal discrimination as the criterion variable and identification with NA culture as the predictor.
3 Results
3.1 Sample characteristics
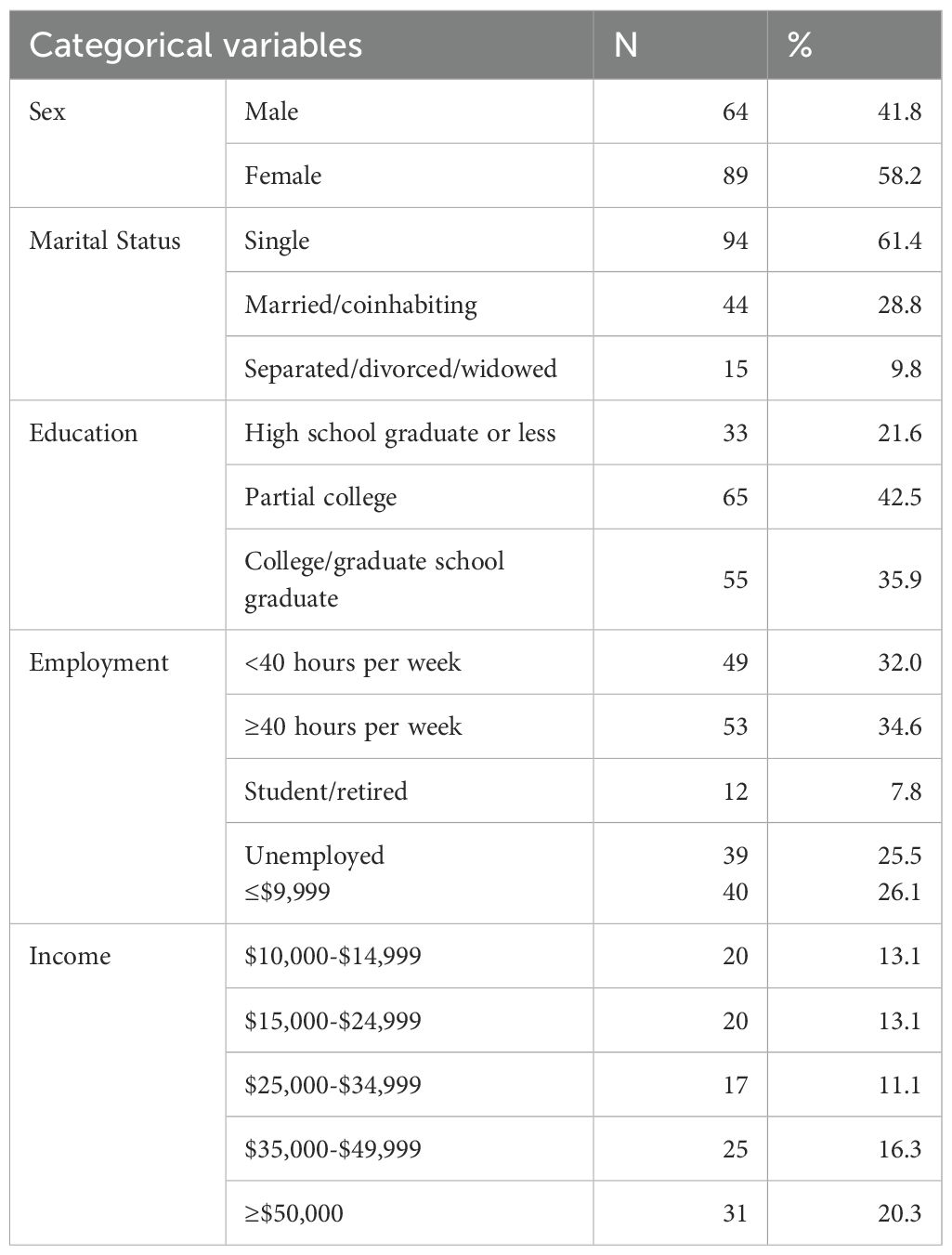
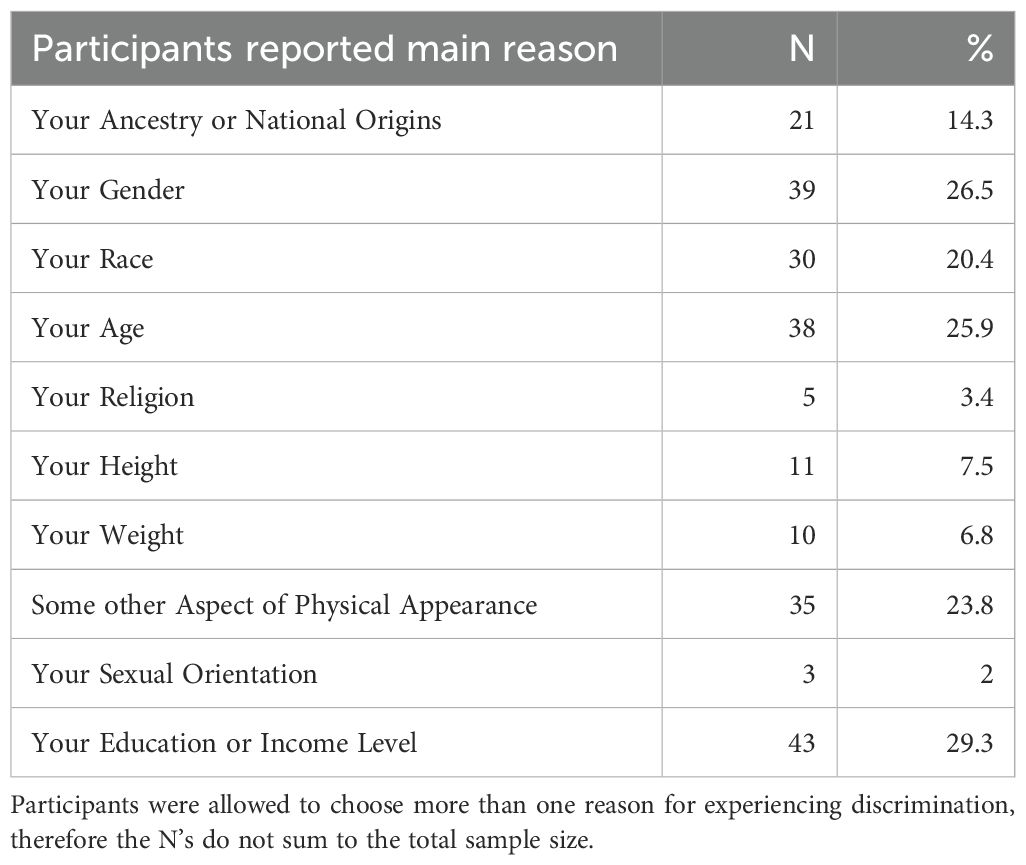
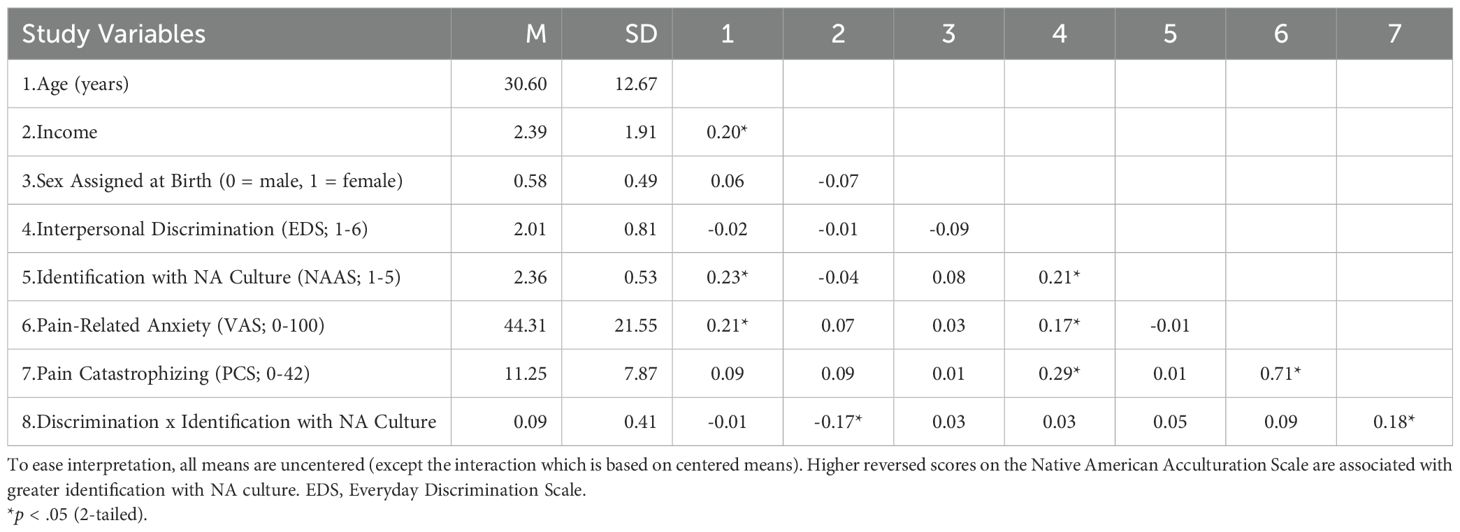
Table 1 displays the sample characteristics. Participants’ ages ranged from 18 to 63 years, with a mean age of 30.60 years (SD = 12.67). The sample was 58.2% female. Most participants reported their marital status as single (61.4%). Most participants (78.4%) reported some college experience (partial college or college graduate). Approximately a fourth of participants reported being unemployed (25.5%). Over half of participants reported earning less than $25,000 (52.3%), which is below the average per capita income in the state of Oklahoma (38). Participants’ BMI ranged from 16.60 to 35.00, with a mean BMI of 25.88 (SD = 4.43). Approximately 15% of participants scored above a 3 on the reverse scored NAAS indicating that most (85%) participants scored in the bicultural identification or lower identification with NA culture range. Participants’ cultural identification ranged from 1.37 to 3.45. As shown in Table 2, 34.7% of participants reported the main reason for their interpersonal discrimination experiences were their ancestry or race. Table 3 presents means, SDs, and intercorrelations among all variables used in regression models.
3.2 Predicting pain-related anxiety
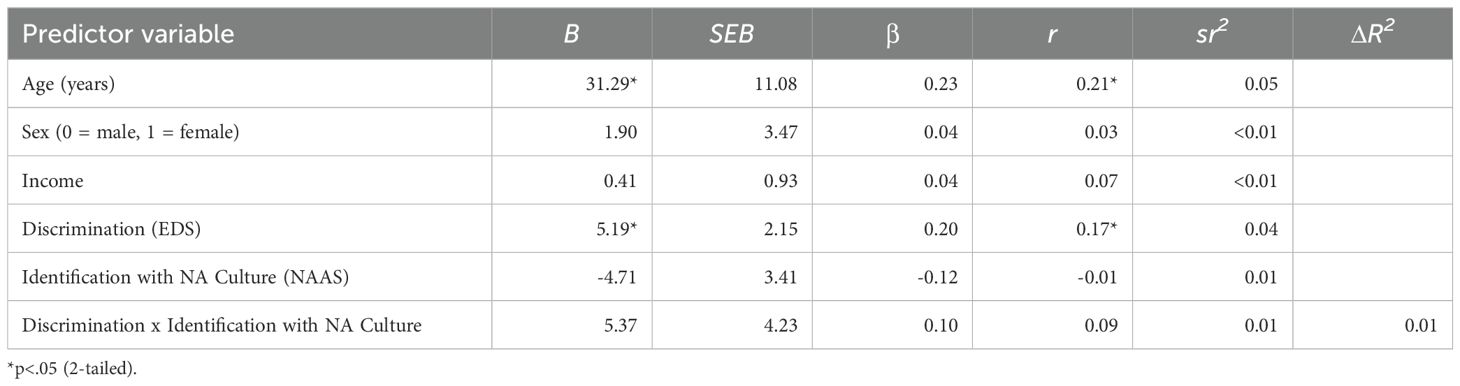
The overall model that included all predictors in the prediction of pain-related anxiety was significant [F(6,146) = 2.62, p = 0.019] and explained 9.73% of the variance. As shown in Table 4, there was a significant main effect for interpersonal discrimination, such that experiencing more unfair treatment was associated with experiencing higher pain-related anxiety (β = 0.20, p = 0.017). However, as shown in Figure 1, the interaction of interpersonal discrimination and identification with NA culture (higher scores=greater enculturation) was nonsignificant [F(1,146) = 1.61, p = 0.21] and only explained an additional 1.0% of the variance (ΔR2 = 0.010). There was a significant effect for age (β = 0.23, p = 0.005), but no other predictor was significant. These findings indicate greater experiences of interpersonal discrimination and higher age was associated with more pain-related anxiety.
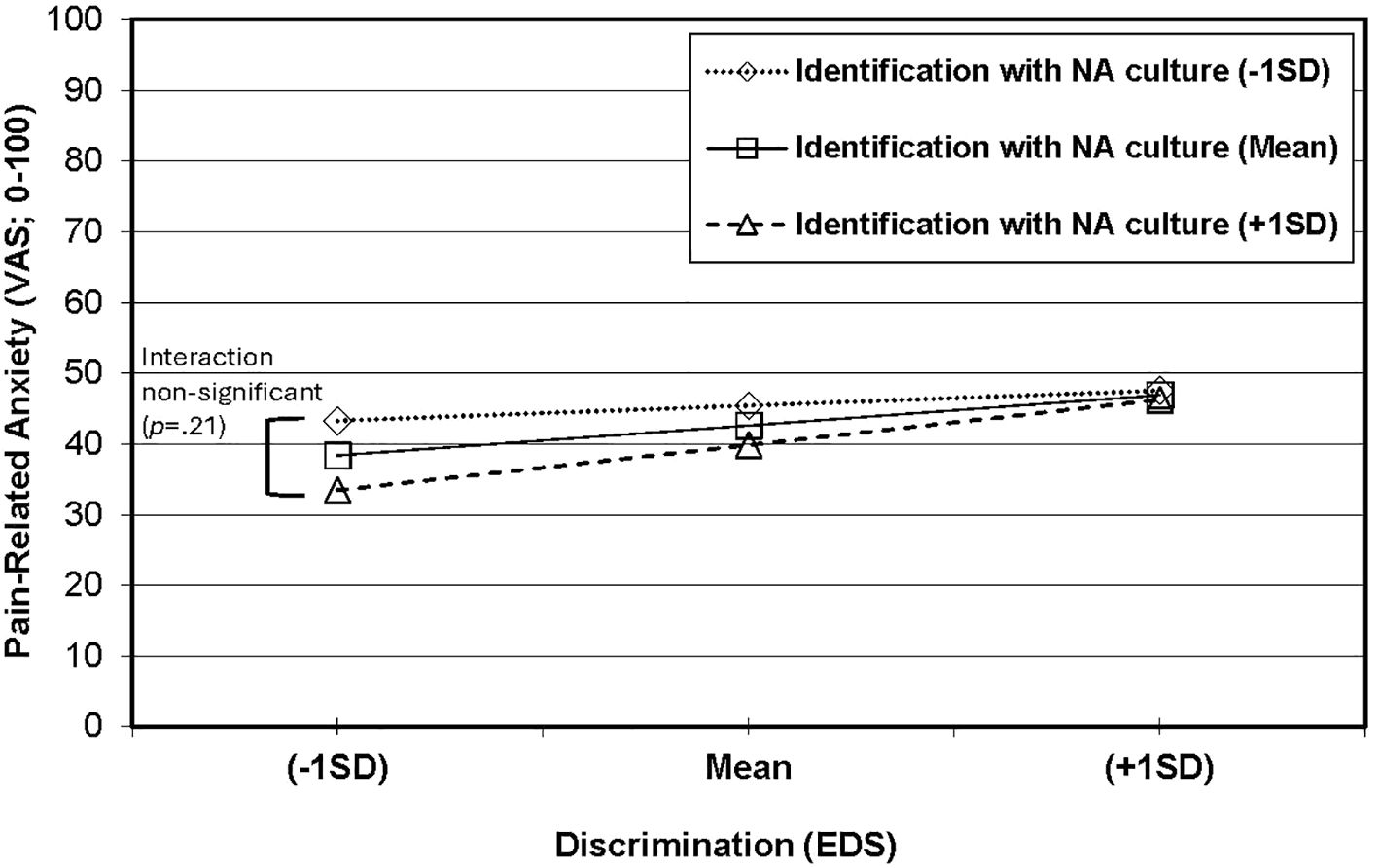
Figure 1. Non-significant interaction between identification with NA culture and interpersonal discrimination in the prediction of pain-related anxiety.
3.3 Predicting situational pain catastrophizing
The overall model that included all predictors in the prediction of situational pain catastrophizing was significant [F(6,146) = 4.01, p = 0.001] and explained 14.14% of the variance. As shown in Table 5, a significant interaction (p = 0.016) was found between interpersonal discrimination (higher scores=more frequent unfair treatment) and identification with NA culture (higher scores=greater enculturation) that explained an additional 3.5% of the variance (ΔR2 = 0.035). As shown in Figure 2, the simple effect for the relationship between interpersonal discrimination and situational pain catastrophizing was significant at +1SD of identification with NA culture (p < 0.0001) and with the mean of identification with NA culture (p = 0.0001), but not at -1SD (p = 0.34). No other predictor in the model was significant. Taken together, these results suggest greater identification with NA culture was associated with a stronger positive relationship between interpersonal discrimination and situational pain catastrophizing.
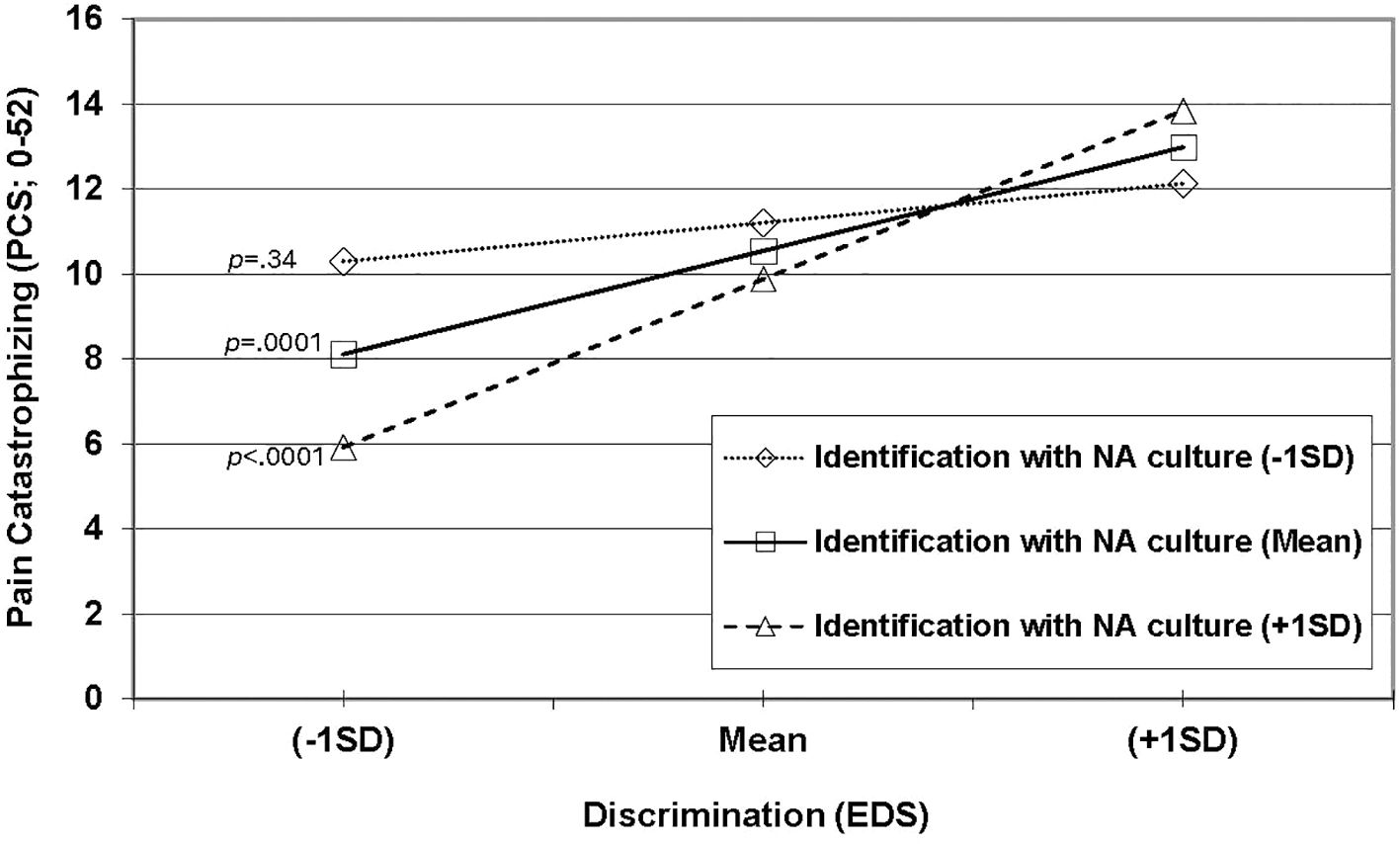
Figure 2. Significant interaction between identification with NA culture and interpersonal discrimination in the prediction of pain catastrophizing.
3.4 Relationship between interpersonal discrimination and identification with NA culture
Given that the moderating effect of identification with NA culture (higher scores=greater enculturation) was in the opposite direction as predicted, we examined whether identification with NA culture was associated with interpersonal discrimination (higher scores=more frequent unfair treatment) to help interpret the results. The model was significant (F[1,151] = 6.69, p = 0.011) and explained 4.2% of the variance. There was a significant positive relationship between identification with NA culture and interpersonal discrimination (β = 0.21), which suggests that greater identification with NA culture was associated with greater exposure to interpersonal discrimination.
4 Discussion
This study investigated whether identification with NA culture buffered against the harmful effects of interpersonal discrimination in a sample of healthy, pain free NA individuals. Interpersonal discrimination was positively associated with pain-related anxiety; however, this relationship was not moderated by identification with NA culture. By contrast, and surprisingly, greater identification with NA culture strengthened the relationship between interpersonal discrimination and pain catastrophizing. Additionally, greater identification with NA culture was associated with more reported experiences of interpersonal discrimination. Taken together, this highlights the ongoing devastating impact of experiencing interpersonal discrimination for NAs. These findings are discussed in the following sections.
4.1 Pain-related anxiety
The hypothesis that identification with NA culture would moderate (buffer) the relationship between interpersonal discrimination and pain-related anxiety was not supported. Although surprising, research has found some mixed results for the protective effects of identification with traditional culture. For example, greater participation in traditional practices buffers against the impact of discrimination on depressive symptoms for NA adults (9). Moreover, stronger identification with traditional Indigenous culture promotes happiness and is associated with less perceived stress for Yup’ik community members (39). This extends to cultural identification for other minoritized individuals too. For example, Cariello and colleagues found greater cultural identification buffered the indirect effect of anxiety through minority stressors (e.g., acculturative stress and discrimination) on physical health for Latinx immigrants (40). Conversely, Gonzalez and colleagues found that greater Indigenous cultural identification was associated with greater anxiety in Indigenous communities (41). Additionally, greater Latinx cultural identification has been found to be associated with a stronger relationship between experienced racism and anxiety for Latinx university students (42). However, it should be emphasized results from Latinx communities might not generalize to NA communities.
Age was positively related to pain-related anxiety and identification with NA culture. Thus, age could moderate the relationship between identification with NA culture and pain-related anxiety. We conducted an exploratory analysis to investigate this potential interaction (not presented), but the interaction was non-significant.
To our knowledge, this was the first study to examine whether identification with NA culture buffers the relationship between interpersonal discrimination and pain-related anxiety. In the current study, there was not a significant interaction between interpersonal discrimination and identification with NA culture when predicting pain-related anxiety. Moreover, there was an absence of a main effect for identification with NA culture when predicting pain-related anxiety, which is consistent with a prior study that found there was no association between ethnic identity and culturally related anxiety in Navajo college students (43). Our laboratory has previously found NAs experience greater pain-related anxiety than NHWs in response to pain tasks (17), thus it appears that interpersonal discrimination is associated with greater pain-related anxiety, regardless of cultural identification for participants in the current study.
4.2 Pain catastrophizing
Unlike pain-related anxiety, identification with NA culture did moderate the relationship between interpersonal discrimination and pain catastrophizing. As the degree of identification with NA culture increased, the relationship between interpersonal discrimination and pain catastrophizing grew stronger. This finding was surprising given the original hypothesis that greater identification with NA culture would buffer against the negative impact of interpersonal discrimination. Potential explanations for this finding are presented below.
Minoritized individuals who identify more with their traditional culture may have higher group identification, resulting in a greater threat appraisal in response to interpersonal discrimination. For example, Latinx students who had a greater degree of group identification appraised prejudice against other Latinx students as more personally threatening than participants with lower group identification (44). In turn, this led to greater depressed mood. Thus, NA individuals in the present study who reported greater identification with NA culture may have appraised experiences of interpersonal discrimination as more threatening towards their community and self-concept, thus leading to greater pain catastrophizing.
Acculturative stress could be another factor that contributes to the stronger relationship between interpersonal discrimination and pain catastrophizing in those reporting higher cultural identification. In a study with Indigenous Alaskans, it was found that discrimination was associated with higher Indigenous identification which was in turn associated with higher acculturative stress. However, this only held true for participants who reported higher identification with mainstream American culture. The authors argued that identity conflict stemming from the combined identification with American culture and Indigenous culture promoted the relationships between discrimination, Indigenous identification, and acculturative stress (45). So, given that NA participants in our sample who reported greater identification with NA culture also scored in the bicultural range of the NAAS, they may experience greater acculturative stress when experiencing interpersonal discrimination thus leading to greater pain catastrophizing. However, this hypothesis requires testing since we did not measure acculturative stress.
Another explanation might involve historical loss thinking. Tucker and colleagues (32) found that identification with NA culture and interpersonal discrimination were positively associated with historical loss thinking, which is associated with psychological distress (25, 32, 46). So, it might be that participants in the current study who identified more with NA culture engage in more historical loss thinking, creating an indirect pathway to increased pain catastrophizing. Future studies are needed to examine these potential explanations.
4.3 Limitations and future directions
The current study has several limitations. First, it used a cross-sectional design, thus analyses cannot determine causality or verify the temporal relationships of the effects. Second, only healthy, pain-free NA individuals were recruited because our goal was to identify variables that promote future chronic pain, so the relationships among the variables may not generalize to those experiencing chronic pain. Third, NA participants were predominately from tribal communities in Oklahoma, so results may not generalize to other NA communities. Fourth, we verified NA status from CDIB/tribal membership cards which excluded individuals who identify as NA but do not have these forms of identification. Fifth, given a majority of our sample scored below a 3 on the reverse scored NAAS (suggesting most were acculturated or bicultural in their NA cultural identification), we may not have been able to observe the protective effects of greater identification with NA culture. For example, Whitbeck and colleagues found that consistently engaging in NA traditional practices buffered the relationship between experienced discrimination and depressive symptoms (9). Thus, NA individuals who identify more with NA culture (scoring closer to a 5 on the reverse scored NAAS) may experience a greater buffering effect.
And finally, the NAAS largely focuses on acculturation processes associated with identification with NA culture. However, the NAAS does not assess for all NA spiritual beliefs/values that encompass identification with NA culture such as the interconnectedness of all things or expressing gratitude (47). Therefore, we might have missed other important facets of NA culture that buffer against the harmful effects of discrimination. Future studies should assess whether broader cultural processes like cultural connectedness or cultural continuity that include other facets such as other NA spiritual beliefs/values, engagement with elders, and intergenerational transmission of cultural values buffer against interpersonal discrimination. Cultural connectedness is defined as the degree of integration an individual has within their culture (48), whereas cultural continuity is defined as maintenance of intergenerational cultural connectedness through familial unity and elders who pass down cultural knowledge to younger generations (49). The maintenance of strong cultural connectedness by NA caregivers buffers the relationship between stressful life events and psychological distress for their children (50). Additionally, greater cultural continuity buffers the association between racial discrimination and allostatic load for Indigenous university students in Canada (51).
These findings have salient considerations for identifying cultural processes that could buffer against chronic pain risk factors. Specifically, our laboratory has found stress from interpersonal discrimination and allostatic load were both involved in indirect pathways predicting chronic pain development for NAs (4). Thus, future research should use measures that include facets of cultural connectedness and cultural continuity such as the Cultural Connectedness Scale (48) or the Native American Spirituality Scale (47) to investigate the potential buffering impact these cultural processes might have on chronic pain risk factors.
The potential mediating/moderating impact of historical loss thinking between interpersonal discrimination and chronic pain risk factors should also be explored in future studies. Interpersonal discrimination is positively associated with historical loss thinking and psychological distress (25, 32). Given that NA participants who identified more with NA culture report more interpersonal discrimination, historical loss thinking could also contribute to chronic pain risk. Lastly, acculturative stress could be explored regarding its impact on the relationship between interpersonal discrimination and chronic pain risk factors for NA individuals, especially those reporting bicultural identity (45).
5 Summary
This study examined identification with NA culture as a moderator between interpersonal discrimination and pain-related anxiety and pain catastrophizing among healthy, pain-free NA participants. Interpersonal discrimination was positively associated with pain-related anxiety and pain catastrophizing. Surprisingly, greater identification with NA culture was associated with a stronger relationship between interpersonal discrimination and pain catastrophizing. But we also noted that individuals who identified more with NA culture reported more experiences of interpersonal discrimination. This could explain why there was a stronger relationship between interpersonal discrimination and pain catastrophizing. To promote a strengths-based approach, other facets of identification with NA culture (e.g., cultural connectedness, cultural continuity) should be explored in future studies to identify cultural processes that protect against chronic pain risk.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by University of Tulsa, Cherokee Nation, and Indian Health Service Oklahoma City Area Office institutional review boards (IRBs). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
BJ: Writing – original draft, Writing – review & editing. HV: Formal analysis, Writing – review & editing. TB: Writing – review & editing. PK: Writing – review & editing. KT: Writing – review & editing. JS: Writing – review & editing. JR: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing, Funding acquisition, Project administration.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This research was supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number R01MD007807. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, Indian Health Service, or the Cherokee Nation.
Acknowledgments
The authors would like to thank Felicitas Huber, Tyler Toledo, Edward Lannon, Bethany Kuhn, Shreela Palit, Erin Street, Michael Payne, Cassandra Sturycz-Taylor, Natalie Hellman, Yvette Guereca, Mara Demuth, Burkhart Hahn, Heather Coleman, Kathryn Thompson, Jessica Fisher, Samuel Herbig, Ky’Lee Barnoski, Garrett Newsom, and Lucinda Chee for their help with data collection, as well as Dr. John Chaney for his consultation on the project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Yong RJ, Mullins PM, and Bhattacharyya N. Prevalence of chronic pain among adults in the United States. PAIN. (2022) 163:e328–32. doi: 10.1097/j.pain.0000000000002291
2. Kawai K, Kawai AT, Wollan P, and Yawn BP. Adverse impacts of chronic pain on health-related quality of life, work productivity, depression and anxiety in a community-based study. Family Practice. (2017) 34:656–61. doi: 10.1093/fampra/cmx034
3. Zajacova A, Grol-Prokopczyk H, and Fillingim R. Beyond Black vs White: racial/ethnic disparities in chronic pain including Hispanic, Asian, Native American, and multiracial US adults. PAIN. (2022) 163:1688–99. doi: 10.1097/j.pain.0000000000002574
4. Rhudy JL, Huber FA, Toledo TA, Kell PA, Street EN, and Shadlow JO. Psychosocial and cardiometabolic predictors of chronic pain onset in Native Americans: serial mediation analyses of 2-year prospective data from the Oklahoma study of Native American pain risk. PAIN. (2022) 163:e654–74. doi: 10.1097/j.pain.0000000000002458
5. Rhudy JL, Kell PA, Brown TV, Ventresca HM, Vore CN, Trevino K, et al. Mechanisms of the Native American pain inequity: predicting chronic pain onset prospectively at 5 years in the Oklahoma Study of Native American Pain Risk. PAIN. (2024) 166:936–55. doi: 10.1097/j.pain.0000000000003442
6. Pascoe EA, Lattanner MR, and Richman LS. Meta-analysis of interpersonal discrimination and health-related behaviors. Health Psychol. (2022) 41:319–31. doi: 10.1037/hea0001147
7. Findling MG, Casey LS, Fryberg SA, Hafner S, Blendon RJ, Benson JM, et al. Discrimination in the United States: experiences of native americans. Health Serv Res. (2019) 54:1431–41. doi: 10.1111/1475-6773.13224
8. Thayer ZM, Blair IV, Buchwald DS, and Manson SM. Racial discrimination associated with higher diastolic blood pressure in a sample of American Indian adults. Am J Phys Anthropology. (2017) 163:122–8. doi: 10.1002/ajpa.23190
9. Whitbeck LB, McMorris BJ, Hoyt DR, Stubben JD, and LaFromboise T. Perceived discrimination, traditional practices, and depressive symptoms among American Indians in the upper Midwest. J Health Soc Behavior. (2002) 43:400–18. doi: 10.2307/3090234
10. Chae DH and Walters KL. Racial discrimination and racial identity attitudes in relation to self-rated health and physical pain and impairment among two-ppirit American Indians/Alaska Natives. Am J Public Health. (2009) 99:S144–51. doi: 10.2105/AJPH.2007.126003
11. Brown TT, Partanen J, Chuong L, Villaverde V, Chantal Griffin A, and Mendelson A. Discrimination hurts: The effect of discrimination on the development of chronic pain. Soc Sci Med. (2018) 204:1–8. doi: 10.1016/j.socscimed.2018.03.015
12. Rhudy JL and Meagher MW. Fear and anxiety: divergent effects on human pain thresholds. Pain. (2000) 84:65–75. doi: 10.1016/S0304-3959(99)00183-9
13. Sullivan MJL, Bishop SR, and Pivik J. The pain catastrophizing scale: development and validation. psychol Assessment. (1995) 7:524–32. doi: 10.1037/1040-3590.7.4.524
14. Terry MJ, Moeschler SM, Hoelzer BC, and Hooten WM. Pain catastrophizing and anxiety are associated with heat pain perception in a community ample of adults with chronic pain. Clin J Pain. (2016) 32:875–81. doi: 10.1097/AJP.0000000000000333
15. Granot M and Ferber SG. The roles of pain catastrophizing and anxiety in the prediction of postoperative pain intensity: a prospective study. Clin J Pain. (2005) 21:439–45. doi: 10.1097/01.ajp.0000135236.12705.2d
16. Theunissen M, Peters M, Bruce J, Gramke H, and Marcus M. Preoperative anxiety and catastrophizing: a systematic review and meta-analysis of the association with chronic postsurgical pain. Clin J Pain. (2012) 28:819–41. doi: 10.1097/AJP.0b013e31824549d6
17. Rhudy JL, Lannon EW, Kuhn BL, Palit S, Payne MF, Sturycz CA, et al. Sensory, affective, and catastrophizing reactions to multiple stimulus modalities: results from the Oklahoma study of Native American pain risk. J Pain. (2019) 20:965–79. doi: 10.1016/j.jpain.2019.02.009
18. Rhudy JL, Huber F, Kuhn BL, Lannon EW, Palit S, Payne MF, et al. Pain-related anxiety promotes pronociceptive processes in Native Americans: bootstrapped mediation analyses from the Oklahoma study of Native American pain risk. Pain Rep. (2020) 5:1–9. doi: 10.1097/PR9.0000000000000808
19. Toledo TA, Kuhn BL, Payne MF, Lannon EW, Palit S, Sturycz CA, et al. The effect of pain catastrophizing on endogenous inhibition of pain and spinal nociception in Native Americans: results from the Oklahoma study of Native American pain risk. Ann Behav Med. (2020) 54:575–94. doi: 10.1093/abm/kaaa004
20. Walters KL and Simoni JM. Reconceptualizing native women’s health: An “Indigenist” stress-coping model. Am J Public Health. (2002) 92:520–4. doi: 10.2105/AJPH.92.4.520
21. Ward C and Szabó Á. Acculturation, cultural identity and well-being. Nat Rev Psychol. (2023) 2:267–82. doi: 10.1038/s44159-023-00171-2
22. Garrett MT and Pichette EF. Red as an apple: Native American acculturation and counseling with or without reservation. J Couns Development: JCD. (2000) 78:3–13. doi: 10.1002/j.1556-6676.2000.tb02554.x
23. Winderowd C, Montgomery D, Stumblingbear G, Harless D, and Hicks K. Development of the “American Indian enculturation scale” to assist counseling practice. Am Indian Alaska Native Ment Health Research: J Natl Center. (2008) 15:1–14. doi: 10.5820/aian.1502.2008.1
24. Zimmerman MA, Ramirez-Valles J, Washienko KM, Walter B, and Dyer S. The development of a measure of enculturation for Native American youth. Am J Community Psychol. (1996) 24:295–310. doi: 10.1007/BF02510403
25. Whitbeck LB, Chen X, Hoyt DR, and Adams GW. Discrimination, historical loss and enculturation: culturally specific risk and resiliency factors for alcohol abuse among American Indians. J Stud Alcohol. (2004) 65:409–18. doi: 10.15288/jsa.2004.65.409
26. Fetter AK and Thompson MN. The impact of historical loss on Native American college students’ mental health: The protective role of ethnic identity. J Couns Psychol. (2023) 70:486–97. doi: 10.1037/cou0000686
27. Yoder KA, Whitbeck LB, Hoyt DR, and LaFromboise T. Suicidal ideation among American Indian youths. Arch Suicide Res. (2006) 10:177–90. doi: 10.1080/13811110600558240
28. Whitbeck LB, Hoyt DR, Stubben JD, and LaFromboise T. Traditional culture and academic success among American Indian children in the upper Midwest. J Am Indian Education. (2001) 40:48–60. Available online at: https://www.jstor.org/stable/24398333.
29. LaFromboise TD, Hoyt DR, Oliver L, and Whitbeck LB. Family, community, and school influences on resilience among American Indian adolescents in the upper midwest. J Community Psychol. (2006) 34:193–209. doi: 10.1002/jcop.20090
30. John-Henderson NA, White EJ, and Crowder TL. Resilience and health in American Indians and Alaska Natives: a scoping review of the literature. Dev Psychopathol. (2023) 35:2241–52. doi: 10.1017/S0954579423000640
31. Jones ML and Galliher RV. Daily racial microaggressions and ethnic identification among Native American young adults. Cultural Diversity Ethnic Minority Psychol. (2015) 21:1–9. doi: 10.1037/a0037537
32. Tucker RP, Wingate LR, and O’Keefe VM. Historical loss thinking and symptoms of depression are influenced by ethnic experience in American Indian college students. Cultural Diversity Ethnic Minority Psychol. (2016) 22:350–8. doi: 10.1037/cdp0000055
33. Rhudy JL, Lannon EW, Kuhn BL, Palit S, Payne MF, Sturycz CA, et al. Assessing peripheral fibers, pain sensitivity, central sensitization, and descending inhibition in Native Americans: main findings from the Oklahoma study of Native American pain risk. PAIN. (2020) 161:388–404. doi: 10.1097/j.pain.0000000000001715
34. Williams DR, Yan Y, Jackson JS, and Anderson NB. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol. (1997) 2:335–51. doi: 10.1177/135910539700200305
35. Wilcox RR. Understanding and applying basic statistical methods using R. New Jersey: John Wiley & Sons (2016). p. 504.
36. Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York: The Guilford Press (2017). 732 p.
37. Dahlhamer J, Lucas J, Zelaya C, Nahin R, Mackey S, DeBar L, et al. Prevalence of chronic pain and high-impact chronic pain among adults — United States, 2016. Morbidity Mortality Weekly Rep. (2018) 67:1001–6. doi: 10.15585/mmwr.mm6736a2
38. U.S. Census Bureau. QuickFacts: Oklahoma. United States Census Bureau. Available online at: https://www.census.gov/quickfacts/fact/table/OK/AFN120217 (Accessed October 27, 2024).
39. Wolsko C, Lardon C, Mohatt GV, and Orr E. Stress, coping, and well-being among the Yup`ik of the Yukon-Kuskokwim delta: the role of enculturation and acculturation. Int J Circumpolar Health. (2007) 66:51–61. doi: 10.3402/ijch.v66i1.18226
40. Cariello AN, Perrin PB, Williams CD, Espinoza GA, Morlett-Paredes A, Moreno OA, et al. Moderating influence of enculturation on the relations between minority stressors and physical health via anxiety in Latinx immigrants. Cultural Diversity Ethnic Minority Psychol. (2020) 26:356–66. doi: 10.1037/cdp0000308
41. Gonzalez MB, Sittner KJ, and Walls ML. Cultural efficacy as a novel component of understanding linkages between culture and mental health in Indigenous communities. Am J Community Psychol. (2022) 70:191–201. doi: 10.1002/ajcp.12594
42. Alamilla SG, Kim BSK, and Lam NA. Acculturation, enculturation, perceived racism, minority status stressors, and psychological symptomatology among Latino/as. Hispanic J Behav Sci. (2010) 32:55–76. doi: 10.1177/0739986309352770
43. McNeil DW, Kee M, and Zvolensky MJ. Culturally related anxiety and ethnic identity in Navajo college students. Cultural Diversity Ethnic Minority Psychol. (1999) 5:56–64. doi: 10.1037/1099-9809.5.1.56
44. McCoy SK and Major B. Group identification moderates emotional responses to perceived prejudice. Pers Soc Psychol Bull. (2003) 29:1005–17. doi: 10.1177/0146167203253466
45. Mallett RK, Patrianakos J, and Swim J. Indigenous Alaskan and mainstream identification explain the link between perceived discrimination and acculturative stress. J Soc Psychol. (2021) 161:593–607. doi: 10.1080/00224545.2020.1867040
46. Whitbeck LB, Adams GW, Hoyt DR, and Chen X. Conceptualizing and measuring historical trauma among american Indian people. Am J Community Psychol. (2004) 33:119–30. doi: 10.1023/B:AJCP.0000027000.77357.31
47. Greenfield BL, Hallgren KA, Venner KL, Hagler KJ, Simmons JD, Sheche JN, et al. Cultural adaptation, psychometric properties, and outcomes of the Native American spirituality scale. Psychol Serv. (2015) 12:123–33. doi: 10.1037/ser0000019
48. Snowshoe A, Crooks CV, Tremblay PF, Craig WM, and Hinson RE. Development of a cultural connectedness scale for first nations youth. psychol Assessment. (2015) 27:249–59. doi: 10.1037/a0037867
49. Reading CL and Wien F. Health inequalities and the social determinants of Aboriginal peoples’ health. BC: National Collaborating Centre for Aboriginal Health Prince George (2009). Available online at: http://www.nccih.ca/docs/determinants/RPT-HealthInequalities-Reading-Wien-EN.pdf (Accessed August 20, 2024).
50. Tsethlikai M, Korous K, and Kim J. Strong cultural connectedness buffers urban American Indian children from the negative effects of stress on mental health. Child Dev. (2024) 95:1845–57. doi: 10.1111/cdev.14149
Keywords: ethnic differences, Native Americans, interpersonal discrimination, pain catastrophizing, pain anxiety, cultural identification
Citation: Jones BW, Ventresca HM, Brown TV, Kell PA, Trevino KN, Shadlow JO and Rhudy JL (2025) Relationships among discrimination, cognitive-affective pain amplifiers, and identification with Native American culture: results from the Oklahoma Study of Native American Pain Risk. Front. Psychiatry 16:1568450. doi: 10.3389/fpsyt.2025.1568450
Received: 29 January 2025; Accepted: 17 September 2025;
Published: 30 September 2025.
Edited by:
Zina Trost, Texas A and M University, United StatesReviewed by:
Brandon Boring, Kent State University, United StatesKhalid Walid Freij, University of Alabama at Birmingham, United States
Copyright © 2025 Jones, Ventresca, Brown, Kell, Trevino, Shadlow and Rhudy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jamie L. Rhudy, SmFtaWUtUmh1ZHlAb3UuZWR1
†These authors have contributed equally to this work
 Brandon W. Jones
Brandon W. Jones Hayden M. Ventresca2†
Hayden M. Ventresca2† Parker A. Kell
Parker A. Kell Jamie L. Rhudy
Jamie L. Rhudy