Abstract
Objective:
The aim of this study was to investigate the association between preoperative anxiety and depression and surgical outcome in patients with Müller-Weiss disease (MWD).
Methods:
This retrospective study included 41 patients diagnosed with MWD who underwent talonavicular joint fusion at the Foot and Ankle Surgery Department of Xi'an Honghui Hospital between April 2014 and September 2024. Patients were stratified into two groups based on preoperative anxiety and depression symptoms: Group A (symptomatic) and Group B (asymptomatic). Preoperative and final follow-up assessments included the Hospital Anxiety and Depression Scale (HADS), Visual Analogue Scale (VAS) for pain (0–100 mm), and American Orthopedic Foot and Ankle Society (AOFAS) score.
Results:
Among 41 patients with complete follow-up, 20 (49%) exhibited preoperative anxiety and depression symptoms. Both groups demonstrated significant improvement in clinical outcomes following talonavicular joint fusion; however, Group A showed inferior overall outcomes compared to Group B. There is a significant negative correlation between AOFAS score improvement and preoperative anxiety levels (r = -0.62, P < 0.05).
Conclusion:
In patients undergoing talonavicular fusion surgery the presence of high levels of depression and anxiety is associated with inferior post-operative outcomes; moreover the level of anxiety correlates with post-operative improvement in function, emphasizing the importance of addressing psychological factors in treatment planning.
1 Introduction
Muller-Weiss disease (MWD) is characterized by chronic dorsal foot pain, compression fracture of the navicular bone, transverse talar protrusion, and morphological changes in the hindfoot, often presenting idiopathically (1). Disease progression leads to foot deformity and debilitating pain (2). The pathogenesis of MWD remains unclear. Navicular osteonecrosis is classified into stages I-V based on the severity of Meary's horn and foot deformity (3). Surgical intervention is typically indicated for patients with stage III disease or above. However, given the absence of a definitive gold standard for MWD treatment, surgery may be necessary for patients who fail to achieve significant improvement after six months of conservative management (4).
Talonavicular joint fusion represents the primary surgical treatment (5). Reade et al. demonstrated that talonavicular joint fusion effectively restores medial column length, increases medial longitudinal arch height, corrects flatfoot deformity, and maintains midfoot and hindfoot stability (6). This procedure also significantly reduces complications such as nonunion and peripheral joint injury (7). Surgical outcomes are influenced by various factors, including comorbidities such as diabetes (8, 9), hypertension (10), and coronary heart disease (11). Additionally, patients' psychological state, including anxiety and depression, has been associated with surgical outcomes (12).
Severe navicular osteonecrosis results in foot deformities, debilitating pain, and functional impairment, significantly affecting daily activities including work, education, and social participation. This can diminish patients' quality of life and increase the likelihood of anxiety and depression, potentially hindering recovery following talonavicular joint fusion. Dydyk et al. found that patients with persistent chronic pain experience elevated levels of anxiety and depression, which negatively impact quality of life and may increase the risk of self-harm (13). Weinerman et al. demonstrated that anxiety and depression are predictive factors for poor surgical outcomes in orthopedic trauma patients (14), with negative psychological states affecting surgical prognosis (15–17). Nathaniel P.M et al. have demonstrated that mental health disorders adversely affect subjective outcomes and complications following total ankle arthroplasty (18). Shihang Cao et al. found that abnormal mental and psychological states such as anxiety and depression before surgery would reduce the surgical prognosis of patients with Hepple V osteochondral lesions of the talus (19).
Multiple studies have established that poor mental health adversely impacts functional outcomes following joint replacement (20–22). Therefore, appropriate psychological interventions may enhance surgical outcomes and improve overall quality of life.
Although surgical treatment for MWD is well-established clinically, the association between preoperative mental state and surgical outcomes remains unclear. This study aims to investigate the association between preoperative anxiety and depression and postoperative pain, functional recovery, and overall surgical outcomes in MWD patients through standardized questionnaire-based assessment. These findings will help elucidate the relationship between preoperative mental state and treatment outcomes, ultimately informing strategies to optimize patient selection and improve surgical efficacy.
2 Research methods
This retrospective study received institutional review board approval (approval number 202410012). Data were collected from MWD patients who underwent talonavicular joint fusion at the Foot and Ankle Surgery Department of Xi'an Honghui Hospital between April 2014 and September 2024. All patients provided informed consent.
Inclusion criteria: (1) MWD was diagnosed based on clinical symptoms (pain and tenderness over the navicular and naviculocuneiform joints, with potential medial longitudinal arch collapse in some patients) and weight-bearing anteroposterior and lateral radiographs of the foot; (2) failed conservative treatment for six months with persistent pain; (3) Maceira stage III disease or higher with closed epiphyseal plates; (4) talonavicular joint fusion as the surgical procedure; (5) minimum follow-up of 12 months and the follow-up period was from the surgery to the clinical assessment at the last follow-up. Exclusion criteria: (1) incomplete clinical data; (2) concomitant foot trauma; (3) concurrent foot pathology, including subtalar arthritis, bone tuberculosis, rheumatoid arthritis, or bone tumors; (4) Patients with a history of psychiatric disorders (including bipolar disorder, schizophrenia, depression, anxiety disorders, and other major psychiatric conditions). In this study, patients were contacted via telephone or the WeChat messaging platform.
All patients were treated by the same foot and ankle surgeon using standardized anesthesia and surgical techniques. Eligible patients were identified from medical records and subsequently contacted by telephone to invite participation in the study. Upon consent, baseline demographic and surgical data were extracted from medical records, while current functional outcomes, pain levels, and psychological status were assessed through standardized questionnaires administered during the follow-up contact.
Patient contact information was retrieved from the medical record system, and eligible patients were contacted and invited to participate. Demographic data were collected from enrolled patients, who completed questionnaires assessing subjective symptoms and functional status. The follow-up period was from the surgery to the clinical assessment at the last follow-up.
The Hospital Anxiety and Depression Scale (HADS) assessed anxiety and depression levels at baseline and final follow-up. The HADS comprises two subscales: HADS-A (anxiety) and HADS-D (depression), each containing seven items scored on a four-point scale (0-3). Scores of eight or higher indicate clinically significant anxiety or depression (23, 24). Pain intensity was evaluated using the Visual Analogue Scale (VAS) at baseline and final follow-up. The VAS consists of a 10-cm horizontal line anchored by "no pain" (0 mm) and "worst possible pain" (100 mm), with patients marking their perceived pain level (25). Functional status was assessed using the American Orthopedic Foot & Ankle Society (AOFAS) Midfoot Score at baseline and final follow-up. The AOFAS scoring system quantifies foot health status and monitors treatment progress. Trained evaluators ensured accurate scoring. All questionnaire responses and clinical data were entered into a standardized electronic database and anonymized to ensure accuracy and patient confidentiality.
Patients were stratified into two groups based on preoperative HADS scores: Group A (anxiety or depression symptoms present, score ≥8 on either subscale) and Group B (no anxiety or depression symptoms, score <8 on both subscales).
3 Statistical methods
Statistical analysis was conducted using SPSS 27.0 software. The Shapiro-Wilk test was performed to assess normality for all continuous variables. Normally distributed data were presented as mean ± standard deviation (SD), with between-group comparisons performed using independent samples t-tests. Effect sizes were reported as Cohen's d, along with 95% confidence intervals and mean differences. Within-group comparisons utilized paired samples t-tests. Non-normally distributed data were presented as median (first quartile, third quartile) [M (Q1, Q3)]. Between-group comparisons for non-parametric data employed the Mann-Whitney U test, with effect sizes reported as rank-biserial correlation coefficients (r), median differences, and 95% confidence intervals. Categorical variables were described as frequencies and percentages (%), with group comparisons performed using χ² tests.
For patients with anxiety and depression, independent samples t-tests were used to compare psychological status between genders. Pearson correlation analysis was performed to assess relationships between age, postoperative functional improvement, and anxiety/depression scores. All statistical tests were two-tailed with significance set at P < 0.05. Data visualizations were created using GraphPad Prism version 10.0.
4 Surgical methods
A medial anterior foot incision was made, and the talonavicular joint was exposed layer by layer. The necrotic bone and surrounding osteophytes were removed, and the joint was reduced to the appropriate position. Cancellous bone graft from the tibia/ilium was used, and the talonavicular joint was fixed with hollow nails/micro-plates. Stability of the fusion was confirmed by movement on the platform. C-arm fluoroscopy confirmed proper alignment of the talonavicular joint and internal fixation. The incision was closed layer by layer after irrigation.
A medial longitudinal incision was made over the talonavicular joint, which was exposed through sequential tissue dissection. Necrotic navicular bone and periarticular osteophytes were debrided, and the joint surfaces were prepared for fusion. Anatomical reduction of the talonavicular joint was achieved and maintained with autologous cancellous bone graft harvested from the tibia or ilium. Joint fusion was secured using either cannulated screws or low-profile plates. Construct stability was assessed through manual stress testing. Intraoperative fluoroscopy confirmed appropriate joint alignment and satisfactory hardware positioning. Following copious irrigation, the surgical site was closed in anatomical layers.
5 Postoperative rehabilitation protocol
Following surgery, we elevated the affected limb and implemented symptomatic management including anti-inflammatory measures and analgesic therapy. Prophylactic antibiotic therapy was administered for 72 hours postoperatively to prevent surgical site infection, with dressing changes performed every 48 hours. Suture removal occurred on postoperative day 14. Between 6 and 8 weeks postoperatively, patients initiated active and passive range-of-motion exercises for the toes and plantar joints under non-weight-bearing conditions. Partial weight-bearing ambulation commenced at 8–12 weeks postoperatively. Radiographic evaluation was performed at 6, 8, and 12 weeks postoperatively in the outpatient setting. Full weight-bearing ambulation was permitted only after radiographic and clinical evidence confirmed adequate bone healing.
6 Imaging data
The imaging data are shown in Figures 1 and 2.
Figure 1

Preoperative imaging of navicular avascular necrosis in Muller-Weiss disease. (A, B) Preoperative magnetic resonance imaging demonstrates lateral compression and collapse of the navicular bone with avascular necrosis, subchondral cystic changes, and bone marrow edema, confirming Muller-Weiss disease. (C, D) Preoperative weight-bearing radiographs showing characteristic navicular deformity and talonavicular joint incongruity.
Figure 2

Postoperative imaging demonstrating successful talonavicular joint fusion with hardware in situ. (A, B) Postoperative X-ray images. (C, D) Postoperative CT images. The images demonstrate good alignment of the talonavicular joint and internal fixation.
7 Results
7.1 Comparison of baseline data between groups
Of 56 enrolled patients, 41 completed full follow-up and were included in the final analysis. The cohort comprised seven males and 34 females with a median age of 51.00 (40.00, 59.00) years and mean follow-up of 51.83 ± 33.47 months.
Twenty patients demonstrated preoperative anxiety or depression (4 males, 16 females) with mean follow-up of 57.25 ± 32.30 months. Twenty-one patients without preoperative anxiety or depression (3 males, 18 females) had mean follow-up of 46.67 ± 34.53 months.
No significant between-group differences were observed for demographic variables, follow-up duration, or preoperative AOFAS and VAS scores (P > 0.05). As expected, preoperative HADS-A and HADS-D scores differed significantly between groups (P < 0.01). Detailed baseline characteristics are presented in Table 1, with preoperative score comparisons shown in Figure 3.
Table 1
| Variables | Group A(n=20) | Group B (n=21) | t/Z/χ² | P | Group difference (95% CI) | Effect size (95% CI) | ||
|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | |||||
| Sex | 4(20.00) | 16(80.00) | 3(14.28) | 18(85.71) | 0.70 | 0.47 | – | – |
| Age | 48.00(25.00,55.50) | 54.00(43.50,62.50) | -1.71 | 0.09 | Med diff:-7.50(-17.00,1.00) | r:-0.37(-0.66,-0.02) | ||
| Follow-uptime | 57.25 ± 32.30 | 46.67 ± 34.53 | 1.01 | 0.32 | MD:10.58(-10.56,31.73) | d:0.32(-0.30,0.93) | ||
| AOFAS | 48.35 ± 11.20 | 48.86 ± 9.29 | -0.16 | 0.88 | MD:-0.51(-6.99,5.98) | d:-0.05(-0.66,0.56) | ||
| VAS | 54.15 ± 6.57 | 52.24 ± 8.93 | 0.78 | 0.44 | MD:1.91(-3.06,6.88) | d:0.24(-0.37,0.86) | ||
| HADS-A | 14.00(10.25,16.00) | 6.00(4.00,7.00) | -5.51 | 0.00 | Med diff: 8.00(6.00,10.00) | r:-0.86(-0.93,-0.73) | ||
| HADS-D | 14.00(12.00,15.00) | 5.00(4.00,6.00) | -5.52 | 0.00 | Med diff: 8.00(7.00,9.00) | r:-0.86(-0.94,-0.75) | ||
Baseline characteristics of patients (Mean ± SD/Median [Q1, Q3]).
MD, Mean Difference; Med diff, Median difference (Hodges-Lehmann estimator).
d, Cohen's d; r, Rank-biserial correlation.
Figure 3
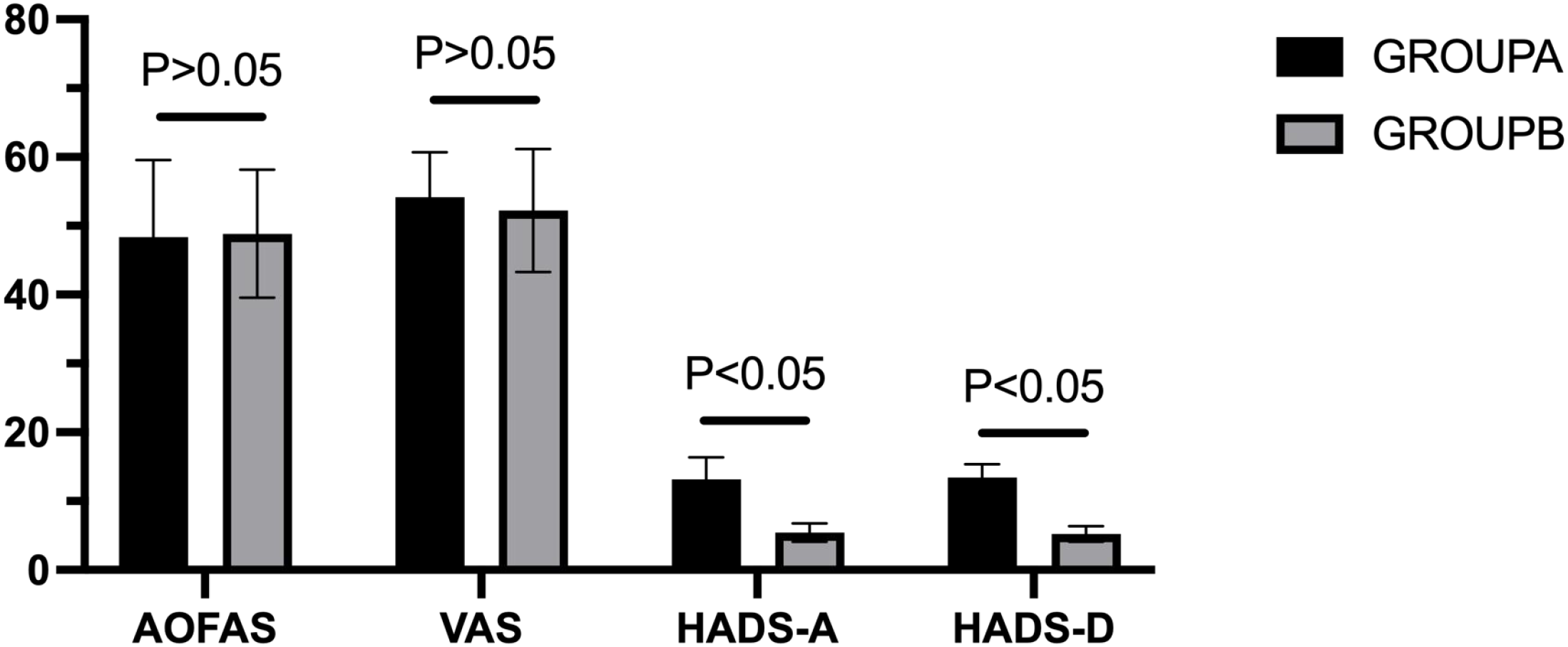
Comparison of preoperative evaluation indicators between groups.
7.2 Pre- and postoperative outcome measures
Following talonavicular joint fusion, both groups demonstrated significant improvements in all outcome measures: AOFAS scores, VAS pain ratings, and HADS-A and HADS-D scores (P < 0.01). Detailed results are presented in Table 2.
Table 2
| Variables | Pairing | t | P | Group difference (95% CI) | Effect size (95% CI) | ||
|---|---|---|---|---|---|---|---|
| Before operation | Last follow-up | ||||||
| Group A(n=20) | AOFAS VAS HADS-A HADS-D |
48.35 ± 11.20 | 70.50 ± 8.28 | -8.70 | 0.00 | MD:-22.15(-27.51,-16.79) | d:11.45(-2.68,-1.17) |
| 54.15 ± 6.57 | 18.15 ± 5.75 | 15.99 | 0.00 | MD:36.00(31.29,40.71) | d:3.58(2.36,4.78) | ||
| 14.00(10.25,16.00) | 6.00(6.00,7.00) | -3.93 | 0.00 | Meddiff:-6.50(-8.00,-5.00) | r:-0.67(-0.81, -0.49) | ||
| 14.00(12.00,15.00) | 6.25 ± 1.52 | -3.94 | 0.00 | Meddiff:-7.50(-8.50,-6.00) | r:-0.67(-0.81, -0.50) | ||
| Group B(n=21) | AOFAS VAS HADS-A HADS-D |
48.86 ± 9.29 | 86.24 ± 6.11 | -16.08 | 0.00 | MD:-37.38(-42.23,-32.53) | d:10.65(-4.66,-2.34) |
| 52.24 ± 8.93 | 4.67 ± 2.03 | 24.66 | 0.00 | MD:47.57(43.55,51.60) | d:8.84(3.67,7.08) | ||
| 6.00(4.00,7.00) | 1.00(0.50,2.00) | -3.97 | 0.00 | Meddiff:-4.00(-5.00,-3.50) | r:-0.67(-0.81, -0.50) | ||
| 5.00(4.00,6.00) | 2.00(1.00,3.00) | -4.07 | 0.00 | Meddiff:-3.00(-4.00,-3.00) | r:-0.68(-0.82, -0.51) | ||
Comparison of preoperative and final follow-up scores between groups (Mean ± SD).
MD, Mean Difference; Med diff, Median difference (Hodges-Lehmann estimator).
d, Cohen's d; r, Rank-biserial correlation.
7.3 Between-group postoperative outcomes
Significant between-group differences were observed in all postoperative outcome measures (P < 0.01). Patients without preoperative anxiety or depression (Group B) achieved superior functional and psychological outcomes compared to those with preoperative anxiety or depression (Group A), indicating that baseline psychological status significantly influences postoperative recovery (Figure 4). Detailed postoperative comparisons are presented in Table 3.
Figure 4
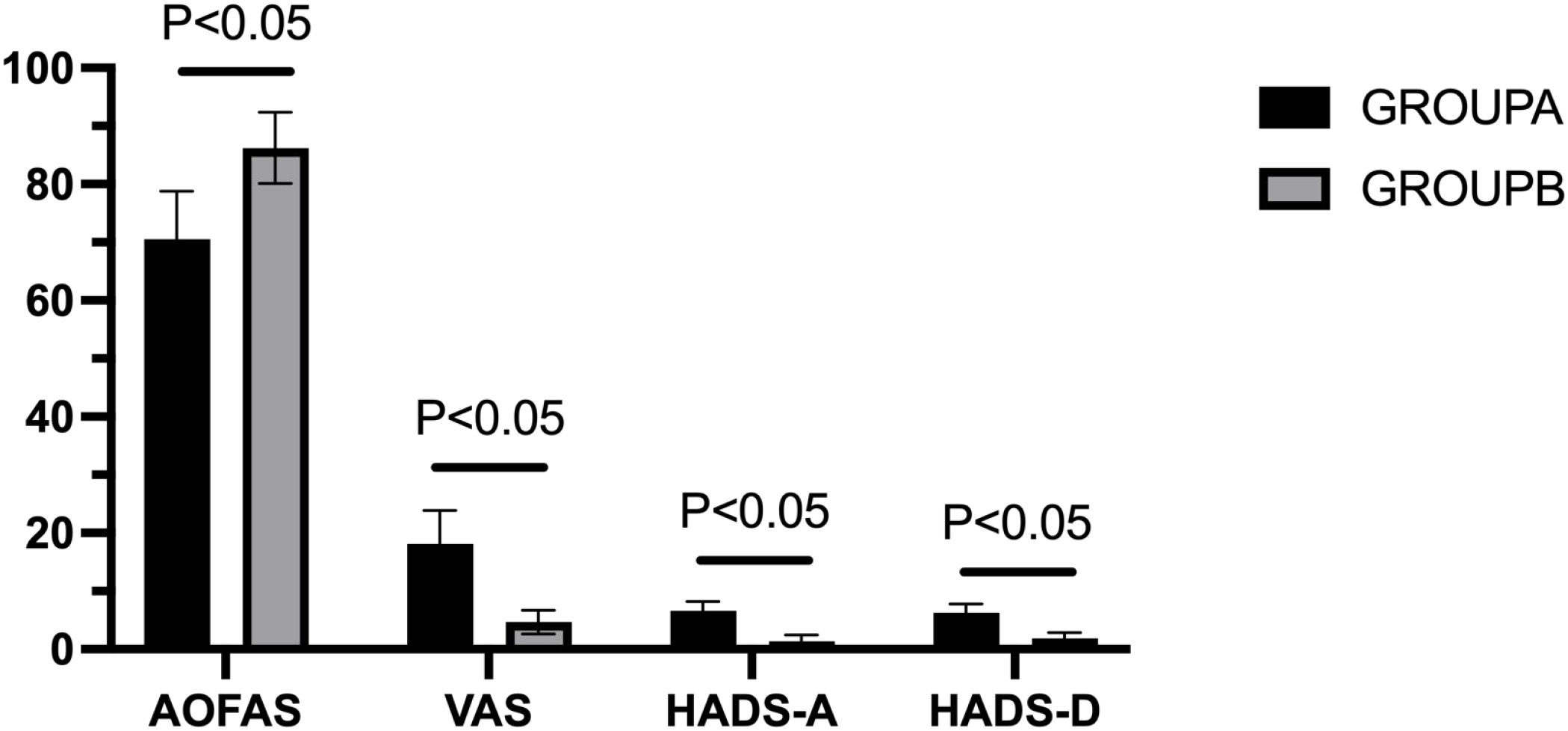
Comparison of postoperative evaluation indicators between groups.
Table 3
| Variables | AOFAS | VAS | HADS-A | HADS-D |
|---|---|---|---|---|
| Group A(n=20) | 70.50 ± 8.28 | 18.15 ± 5.75 | 6.00(6.00,7.00) | 6.25 ± 1.52 |
| Group B(n=21) | 86.24 ± 6.11 | 4.67 ± 2.03 | 1.00(0.50,2.00) | 2.00(1.00,3.00) |
| t | -6.95 | 9.91 | -5.53 | -5.45 |
| P | 0.00 | 0.00 | 0.00 | 0.00 |
| Group Difference (95% CI) | MD:-15.74(-20.32,-11.16) | MD:13.48(10.67,16.30) | Meddiff:5.00(4.00,6.00) | Meddiff:4.00(4.00,5.00) |
| Effect Size (95% CI) | d:-2.17(-2.94,-1.38) | d:4.27(2.22,4.08) | r: -0.86 (-0.93, -0.75) | r: -0.85 (-0.92, -0.73) |
Comparison of postoperative evaluation indicators between groups (Mean ± SD).
MD, Mean Difference; Med diff, Median difference (Hodges-Lehmann estimator).
d, Cohen's d; r, Rank-biserial correlation.
7.4 Comparison of pre- and postoperative changes in AOFAS, HADS-A, HADS-D, and VAS scores between groups
Statistical analysis demonstrated a statistically significant difference in AOFAS score changes between the two groups (P < 0.01), whereas no significant difference was observed in VAS score changes (P = 0.96). The differences between preoperative and final follow-up scores are presented in Table 4.
Table 4
| Variables | AOFAS changes | VAS changes | HADS-A changes | HADS-D changes |
|---|---|---|---|---|
| Group A(n=20) | 22.15 ± 11.45 | 36.00 ± 10.07 | 6.50 ± 3.35 | 7.15 ± 2.20 |
| Group B(n=21) | 37.38 ± 10.65 | 47.57 ± 8.84 | 3.86 ± 1.20 | 3.00(3.00,4.00) |
| t/Z | -4.29 | -3.92 | -4.12 | -4.63 |
| P | 0.00 | 0.00 | 0.00 | 0.00 |
| Group Difference (95% CI) | MD:-14.56(-21.43,-7.69) | MD:-11.57(-17.55,-5.59) | MD:3.00(2.00,5.00) | Meddiff:4.00(3.00,5.00) |
| Effect Size (95% CI) | d:-1.34(-2.01,-0.65) | d:-1.22(-1.89,-0.55) | d:1.71(1.14,2.28) | r:-0.72 (-0.83, -0.58) |
Comparison of changes in evaluation indicators between groups before and after surgery (Mean ± SD).
MD, Mean Difference; Med diff, Median difference (Hodges-Lehmann estimator).
d, Cohen's d; r, Rank-biserial correlation.
7.5 Correlation analysis between psychological status and clinical variables in group A
In Group A, no significant correlations were identified between age, gender, and preoperative anxiety or depression scores. However, a significant negative correlation was observed between AOFAS score improvement and preoperative anxiety levels (r = -0.62, P < 0.05), as shown in Figure 5. Preoperative depression levels demonstrated no significant correlation with functional outcomes in this analysis (r = 0.12, P > 0.05). Comprehensive results are presented in Tables 5 and 6.
Figure 5
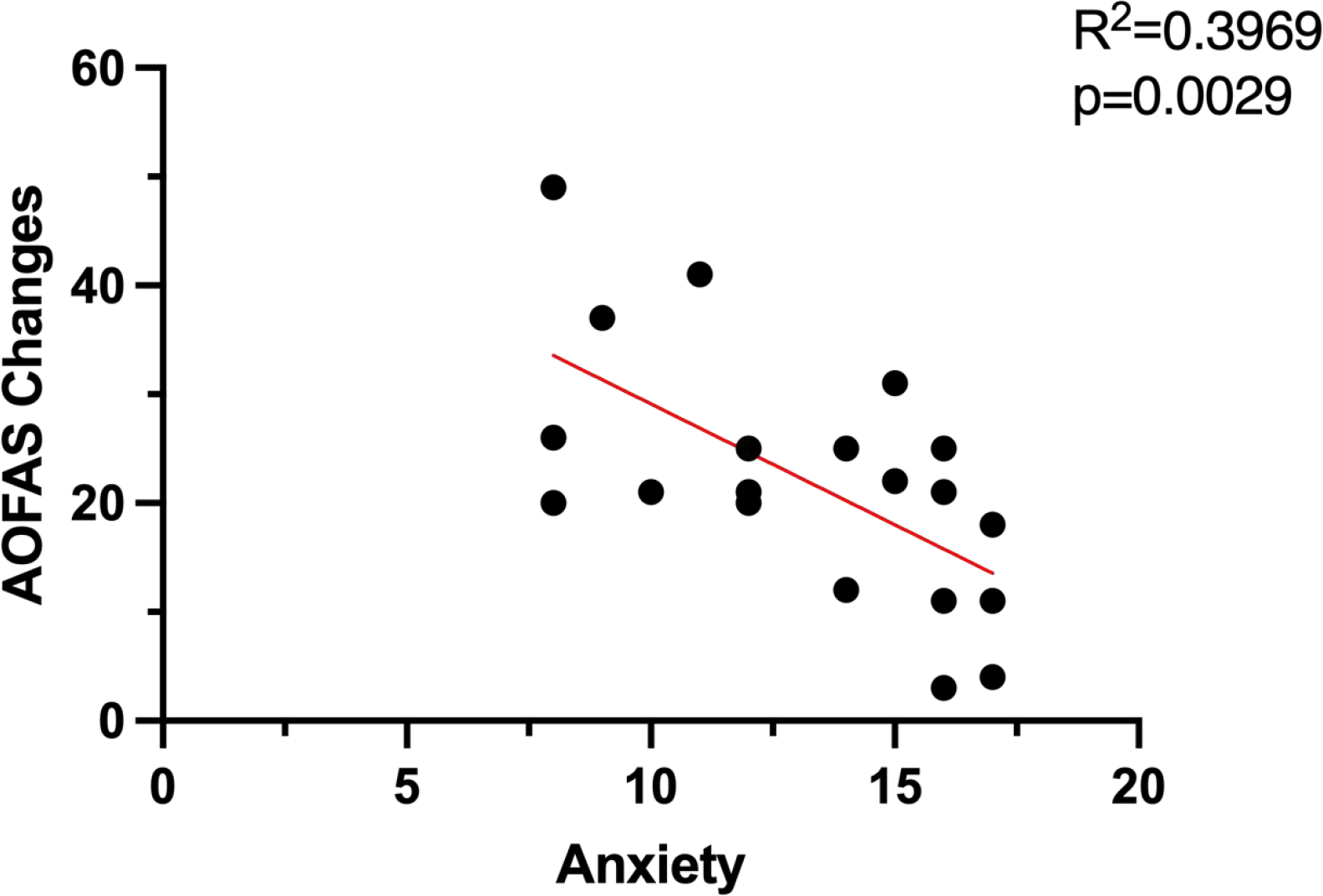
Correlation between postoperative improvement in AOFAS score and preoperative anxiety in group A.
Table 5
| Variables | Anxiety | Depression | |
|---|---|---|---|
| Age |
r
P |
0.48 | -0.24 |
| 0.05 | 0.32 | ||
| Sex |
r
P |
0.15 | -0.28 |
| 0.52 | 0.24 | ||
Correlation between age, gender, and preoperative anxiety and depression in group A.
Table 6
| Variables | Anxiety | Depression | |
|---|---|---|---|
| AOFAS difference |
r
P |
-0.62 | 0.12 |
| 0.00 | 0.62 | ||
| VAS difference |
r
P |
0.05 | -0.01 |
| 0.83 | 0.97 | ||
Correlation between postoperative improvement in AOFAS score and preoperative anxiety and depression in group A.
8 Discussion
Midfoot deformity with pain, also known as Brailsford disease (MWD), predominantly affects middle-aged women (40–60 years) and has a relatively low incidence (26). Cotchett et al. reported that negative emotions frequently accompany foot and ankle pain (27), adversely impacting surgical outcomes (28). According to Sharma et al., referral of patients with high-risk psychosocial factors could be essential to improve postoperative outcomes and satisfaction (29).
This study demonstrated significant postoperative improvements in functional activity, pain levels, and psychological status in both groups following talonavicular (TN) fusion. Hu et al. reported increased AOFAS scores from 43.5 ± 12.4 to 83.8 ± 9.1 and decreased VAS scores from 7.3 ± 1.5 to 1.0 ± 0.4 after TN fusion (30). Similarly, Liang Lu et al. found that in patients with MWD, AOFAS scores improved from a preoperative value of 43.4 ± 16.1 to 85.3 ± 6.2, further confirming the effectiveness of this surgical approach in enhancing foot and ankle function in MWD patients (31). The conclusions in this study are all greater than the minimal clinically important difference (MCID) in the relevant research literature, further confirming the effectiveness of this surgical method (32, 33). Our analysis of psychological status revealed significant improvements in postoperative HADS-A and HADS-D scores, with no adverse events such as wound infection or nonunion observed during follow-up. These findings suggest that TN fusion is an effective treatment modality for MWD and all subjects experience an improvement that is clinically and statistically significant, as seen by other authors.
Postoperative VAS and AOFAS scores differed significantly between the two groups. Preoperative anxiety or depression was associated with suboptimal pain management and functional recovery. This finding aligns with previous research indicating that poor preoperative psychological status is associated with diminished functional recovery and increased postoperative pain (34). Agarwalla et al. (35) and Lai (36) similarly reported that depression and poor mental health negatively affected outcomes after biceps tendon fixation and bunion surgery, respectively. Therefore, it appears that preoperative psychological status could influence postoperative outcomes.
The mean improvement in AOFAS scores was 22.15 ± 11.45 and the mean reduction in VAS scores was 36.00 ± 10.07 in Group A. These improvements were significantly smaller than those observed in Group B (AOFAS: 37.38 ± 10.65; VAS: 47.57 ± 8.84) (P < 0.05). Baseline demographic and clinical data (gender, age, preoperative AOFAS and VAS scores) showed no significant differences between groups. However, significant differences emerged in postoperative AOFAS and VAS scores despite both groups receiving identical surgical interventions. Although postoperative pain is common, patients with preoperative anxiety or depression experienced inferior functional outcomes and elevated pain levels compared to those without these conditions (37). This phenomenon may be attributed to reduced participation in postoperative rehabilitation programs. While preoperative AOFAS and VAS scores did not differ significantly between groups, Group A exhibited significantly higher postoperative VAS scores and lower AOFAS scores with greater variability than Group B (P < 0.05). Both groups demonstrated significant improvements in postoperative HADS-A and HADS-D scores. However, given that Group B had lower baseline anxiety and depression scores, their improvement was less pronounced than Group A. These findings suggest that preoperative psychological status significantly impacts postoperative pain management and functional recovery, as reflected in AOFAS and VAS scores.
In Group A patients, no significant correlations were identified between age or gender and levels of anxiety or depression. This finding may be attributed to the limited sample size and unequal gender distribution in this study. Among Group A patients, a significant negative correlation was observed between postoperative functional improvement and preoperative anxiety levels, whereas no significant correlation was found with preoperative depression. We hypothesize that elevated preoperative anxiety levels may impair patients' ability to cooperate fully with medical personnel before surgery, thereby compromising their confidence in the surgical team. Previous studies have demonstrated that patients with high preoperative anxiety often experience poor sleep quality, and the severity of sleep disorders is significantly negatively correlated with postoperative physical function (38). Patients with compromised sleep quality are at increased risk for fractures, falls, and other adverse events (39). Excessive activity of the affected limb may precipitate secondary injuries, thereby compromising surgical outcomes. Relevant studies have found that patients who experience anxiety before surgery often have higher levels of stress hormones such as cortisol, epinephrine, and norepinephrine, which in turn affects the surgical prognosis of the patients (40). Conversely, no significant correlation was observed between preoperative depression and postoperative prognosis. This may be because preoperative depression primarily intensifies patients' negative emotions without directly affecting physical activity levels. This study highlights the importance of assessing anxiety in patients undergoing surgery for MWD and the HADS questionnaire can be a useful tool for this purpose. This would allow for the implementation of strategies aimed at reducing anxiety levels, such as deep breathing (41), muscle relaxation (42), music therapy (43, 44), and guided imagery (45). What's more, it's possible to reduce the level of anxiety and depression of patients by proper nursing measures just like what Emily L. Zale et al. have reported (46). We also recommend that particular attention should be given to evaluating the psychological status of MWD patients, especially anxiety levels, to develop individualized treatment plans that enhance the clinical effectiveness of surgical intervention.
This study has several limitations: (1) a relatively small sample size; (2) subjective assessment methodologies for foot function and pain evaluation; (3) the potential influence of confounding variables such as occupation and living conditions on patient outcomes; (4) the impact of socioeconomic factors on foot and ankle functional recovery. Furthermore, the retrospective study design limits the ability to establish definitive causal relationships between variables; (5)variability in the timing of follow-up assessments may have introduced measurement bias. Future investigations should incorporate larger sample sizes to minimize the influence of confounding factors and, when feasible, conduct prospective studies to validate these findings.
9 Conclusion
In patients undergoing talonavicular fusion surgery the presence of high levels of depression and anxiety is associated with inferior post-operative outcomes; moreover the level of anxiety correlates with post-operative improvement in function. The findings of this study suggest that clinical management of similar patients should incorporate appropriate psychological interventions to mitigate preoperative anxiety and psychological distress. This comprehensive approach may optimize surgical outcomes, facilitate functional recovery, and ultimately improve patients' overall quality of life.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Red Society Hospital affiliated to Xi 'an Jiaotong University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
XL: Resources, Writing – original draft, Writing – review & editing. YP: Investigation, Resources, Supervision, Writing – review & editing. SC: Software, Supervision, Writing – review & editing. JL: Supervision, Writing – review & editing. JX: Funding acquisition, Resources, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1
Monteagudo M Maceira E . Management of müller-weiss disease. Foot Ankle Clin. (2019) 24:89–105. doi: 10.1016/j.fcl.2018.09.006
2
Mohiuddin T Jennison T Damany D . Müller-Weiss disease - review of current knowledge. Foot Ankle Surg. (2014) 20:79–84. doi: 10.1016/j.fas.2013.11.001
3
Bartolotta RJ McCullion JC Belfi LM Hentel KD . Mueller-Weiss syndrome: imaging and implications. Clin Imaging. (2014) 38:895–8. doi: 10.1016/j.clinimag.2014.06.012
4
Perisano C Greco T Vitiello R Maccauro G Liuzza F Tamburelli FC et al . Mueller-Weiss disease: review of the literature. J Biol Regul Homeost Agents. (2018) 32:157–62(6 Suppl. 1):157–162.
5
Maceira E Rochera R . Müller-Weiss disease: clinical and biomechanical features. Foot Ankle Clin. (2004) 9:105–25. doi: 10.1016/S1083-7515(03)00153-0
6
Reade B Atlas G Distazio J Kruljac S . Mueller-Weiss syndrome: an uncommon cause of midfoot pain. J Foot Ankle Surg. (1998) 37:535–9. doi: 10.1016/s1067-2516(98)80032-x
7
Ma S Jin D . Isolated talonavicular arthrodesis. Foot Ankle Int. (2016) 37:905–8. doi: 10.1177/1071100716641731
8
Tan DJH Yaow CYL Mok HT Ng CH Tai CH Tham HY et al . The influence of diabetes on postoperative complications following colorectal surgery. Tech Coloproctol. (2021) 25:267–78. doi: 10.1007/s10151-020-02373-9
9
Faramawi MF Delhey LM Chancellor JR Sallam AB . The influence of diabetes status on the rate of cataract surgery following pars plana vitrectomy. Ophthalmol Retina. (2020) 4:486–93. doi: 10.1016/j.oret.2019.09.011
10
Bramham K Parnell B Nelson-Piercy C Seed PT Poston L Chappell LC . Chronic hypertension and pregnancy outcomes: systematic review and meta-analysis. BMJ. (2014) 348:g2301. doi: 10.1136/bmj.g2301
11
Eagle KA Rihal CS Mickel MC Holmes DR Foster ED Gersh BJ . Cardiac risk of noncardiac surgery: influence of coronary disease and type of surgery in 3368 operations. CASS Investigators and University of Michigan Heart Care Program. Coronary Artery Surg Study. Circulation. (1997) 96:1882–7. doi: 10.1161/01.cir.96.6.1882
12
Tamate T Nishioka S Ry LD Weldon RH AS N Nakasone CK . The influence of mental health on early outcomes following total hip arthroplasty. Arch Orthop Trauma Surg. (2024) 144:1773–9. doi: 10.1007/s00402-023-05159-4
13
Dydyk AM Sizemore DC Fariba KA Sanghavi DK Porter BR . Florida controlled substance prescribing. In: StatPearls. StatPearls Publishing, Treasure Island (FL (2022).
14
Weinerman J Vazquez A Schurhoff N Shatz C Goldenberg B Constantinescu D et al . The impacts of anxiety and depression on outcomes in orthopaedic trauma surgery: a narrative review. Ann Med Surg (Lond). (2023) 85:5523–7. doi: 10.1097/MS9.0000000000001307
15
Wagener N Löchel J Hipfl C Perka C Hardt S Leopold VJ . Psychological status affects postoperative quality of life, function, and pain after periacetabular osteotomy. Bone Jt Open. (2023) 4:758–65. doi: 10.1302/2633-1462.410.BJO-2023-0104.R1
16
Maurer E Walter N Baumgartner H Histing T Alt V Rupp M . Quality of life after fracture-related infection of the foot. Foot Ankle Surg. (2022) 28:1421–6. doi: 10.1016/j.fas.2022.08.005
17
Althof JE Beasley BD . Psychosocial management of the foot and ankle surgery patient. Clin Podiatr Med Surg. (2003) 20:199–211. doi: 10.1016/S0891-8422(03)00003-X
18
Mercer NP Lezak BA Hedbany D Butler JJ Krebsbach S Bloom DA et al . The impact of mental health disorders on outcomes following total ankle arthroplasty: A systematic review. Foot Ankle Surg. (2025) 31:392–9. doi: 10.1016/j.fas.2025.01.005
19
Cao S Zan Q Lu J Li Y Li B Zhao H et al . Analysis of preoperative and postoperative depression and anxiety in patients with osteochondral lesions of the talus. Front Psychiatry. (2024) 15:1356856. doi: 10.3389/fpsyt.2024.1356856
20
Harmer JR Wyles CC Duong SQ Morgan Iii RJ Maradit-Kremers H Abdel MP . Depression and anxiety are associated with an increased risk of infection, revision, and reoperation following total hip or knee arthroplasty. Bone Joint J. (2023) 105-B:526–33. doi: 10.1302/0301-620X.105B5.BJJ-2022-1123.R1
21
Goh GS Khow YZ Tay DK Lo NN Yeo SJ Liow MHL . Preoperative mental health influences patient-reported outcome measures and satisfaction after revision total knee arthroplasty. J Arthroplasty. (2021) 36:2878–86. doi: 10.1016/j.arth.2021.03.026
22
Wong SE Colley AK Pitcher AA Zhang AL Ma CB Feeley BT . Mental health, preoperative disability, and postoperative outcomes in patients undergoing shoulder arthroplasty. J Shoulder Elbow Surg. (2018) 27:1580–7. doi: 10.1016/j.jse.2018.02.066
23
Julian LJ . Measures of anxiety: state-trait anxiety inventory (STAI), beck anxiety inventory (BAI), and hospital anxiety and depression scale-anxiety (HADS-A). Arthritis Care Res (Hoboken). (2011) 63 Suppl 11:S467–72. doi: 10.1002/acr.20561
24
Wang W Chair SY Thompson DR Twinn SF . A psychometric evaluation of the Chinese version of the Hospital Anxiety and Depression Scale in patients with coronary heart disease. J Clin Nurs. (2009) 18:1908–15. doi: 10.1111/j.1365-2702.2008.02736.x
25
He S Renne A Argandykov D Convissar D Lee J . Comparison of an emoji-based visual analog scale with a numeric rating scale for pain assessment. JAMA. (2022) 328:208–9. doi: 10.1001/jama.2022.7489
26
Hermena S Francis M . Clinical presentation, imaging features, and management of müller-weiss disease. Cureus. (2021) 13:e18659. doi: 10.7759/cureus.18659
27
Cotchett M Frescos N Whittaker GA Bonanno DR . Psychological factors associated with foot and ankle pain: a mixed methods systematic review. J Foot Ankle Res. (2022) 15:10. doi: 10.1186/s13047-021-00506-3
28
Baker M Albelo F Zhang T Schneider MB Foster MJ Aneizi A et al . PROMIS Depression and Anxiety in shoulder surgery patients. Bone Joint J. (2022) 104-B:479–85. doi: 10.1302/0301-620X.104B4.BJJ-2021-1089.R1
29
Sharma AK Elbuluk AM Gkiatas I Kim JM Sculco PK Vigdorchik JM . Mental health in patients undergoing orthopaedic surgery: diagnosis, management, and outcomes. JBJS Rev. (2021) 9(7). doi: 10.2106/JBJS.RVW.20.00169
30
Hu D Zhang Y Liang X Li Y Zhao H . Effectiveness of talonavicular arthrodesis for Müller-Weiss disease. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. (2017) 31:1434–7. doi: 10.7507/1002-1892.201703052
31
Lu L Liu B Zeng J Chen W Hu F Ma Q et al . Efficacy of triple and talonavicular arthrodesis for the treatment of III-V müller-weiss disease. Tohoku J Exp Med. (2022) 258:97–102. doi: 10.1620/tjem.2022.J062
32
Sutton RM McDonald EL Shakked RJ Fuchs D Raikin SM . Determination of minimum clinically important difference (MCID) in visual analog scale (VAS) pain and foot and ankle ability measure (FAAM) scores after hallux valgus surgery. Foot Ankle Int. (2019) 40:687–93. doi: 10.1177/1071100719834539
33
Hung M Baumhauer JF Licari FW Voss MW Bounsanga J Saltzman CL . PROMIS and FAAM minimal clinically important differences in foot and ankle orthopedics. Foot Ankle Int. (2019) 40:65–73. doi: 10.1177/1071100718800304
34
Yoo JS Hrynewycz NM Brundage TS Mogilevsky FA Shah HC Mehraban N et al . The influence of preoperative mental health on PROMIS physical function outcomes following minimally invasive transforaminal lumbar interbody fusion. Spine (Phila Pa 1976). (2020) 45:E236–43. doi: 10.1097/BRS.0000000000003236
35
Agarwalla A Lu Y Chang E Patel BH Cancienne JM Cole BJ et al . Influence of mental health on postoperative outcomes in patients following biceps tenodesis. J Shoulder Elbow Surg. (2020) 29:2248–56. doi: 10.1016/j.jse.2020.03.020
36
Lai SWH Tang CQY Graetz AEK Thevendran G . Preoperative mental health score and postoperative outcome after hallux valgus surgery. Foot Ankle Int. (2018) 39:1403–9. doi: 10.1177/1071100718794661
37
Park JH Rhee SM Kim HS Oh JH . Effects of anxiety and depression measured via the hospital anxiety and depression scale on early pain and range of motion after rotator cuff repair. Am J Sports Med. (2021) 49:314–20. doi: 10.1177/0363546520976574
38
Anwar FN Roca AM Medakkar SS Loya AC Snigur GA Sencaj JF et al . Correlation between anxiety, sleep disturbance and clinical outcomes in a lumbar decompression cohort. J Clin Neurosci. (2024) 127:110759. doi: 10.1016/j.jocn.2024.110759
39
Cauley JA Hovey KM Stone KL Andrews CA Barbour KE Hale L et al . Characteristics of self-reported sleep and the risk of falls and fractures: the women's health initiative (WHI). J Bone Miner Res. (2019) 34:464–74. doi: 10.1002/jbmr.3619
40
Mavros MN Athanasiou S Gkegkes ID Polyzos KA Peppas G Falagas ME . Do psychological variables affect early surgical recovery? PLoS One. (2011) 6:e20306. doi: 10.1371/journal.pone.0020306
41
Hu L Hua Y Wang L Mao Z Jia X Lei Z et al . Effect of short-term deep breathing exercises on perioperative anxiety and pain in pediatric orthopedic patients: A randomized controlled trial. J Perianesth Nurs. (2025) 40:69–75. doi: 10.1016/j.jopan.2024.03.009
42
Fang J Yu C Liu J Mao X Jia X Luo J et al . A systematic review and meta-analysis of the effects of muscle relaxation training vs. conventional nursing on the depression, anxiety and life quality of patients with breast cancer. Transl Cancer Res. (2022) 11:548–58. doi: 10.21037/tcr-22-428
43
Sayadi Mank-Halati M Rezaei M Farzaei MH Khatony A . Comparing the effects of rosemary aromatherapy and music therapy on anxiety levels in patients undergoing general surgery: A randomized controlled clinical trial. Explore (NY). (2024) 20:102976. doi: 10.1016/j.explore.2024.01.002
44
Abdul Hamid MR Mansor MB Zainal Abidin MF . Music therapy for reducing anxiety in patients undergoing total knee replacement surgery under subarachnoid anesthesia. J Orthop Surg (Hong Kong). (2022) 30:10225536221122347. doi: 10.1177/10225536221122347
45
Thomas KM Sethares KA . Is guided imagery effective in reducing pain and anxiety in the postoperative total joint arthroplasty patient? Orthop Nurs. (2010) 29:393–9. doi: 10.1097/NOR.0b013e3181f837f0
46
Zale EL Ring D Vranceanu AM . The future of orthopaedic care: promoting psychosocial resiliency in orthopaedic surgical practices. J Bone Joint Surg Am. (2018) 100:e89. doi: 10.2106/JBJS.17.01159
Summary
Keywords
Muller-Weiss disease, talonavicular joint fusion, mental state, surgical outcomes, relationship
Citation
Liu X, Pan Y, Cao S, Lu J and Xu J (2025) Preoperative psychological factors predict talonavicular fusion outcomes in Muller-Weiss disease. Front. Psychiatry 16:1571794. doi: 10.3389/fpsyt.2025.1571794
Received
06 February 2025
Accepted
11 September 2025
Published
30 September 2025
Volume
16 - 2025
Edited by
Lamyae Benzakour, University of Geneva, Switzerland
Reviewed by
Maryam Daghiani, Tehran University of Medical Sciences, Iran
Laura De Cristofaro, University of Molise, Italy
Updates
Copyright
© 2025 Liu, Pan, Cao, Lu and Xu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Junkui Xu, 568720818@qq.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.