- School of Physical Education, Hainan Normal University, Haikou, Hainan, China
Background: Aerobic exercise (AE), as a non-pharmacological therapy, is an effective supplement to conventional depression treatments. However, a comprehensive assessment of combined AE interventions remains insufficient. This study aims to systematically evaluate the intervention effects of different therapies combined with AE in depression patients via network meta-analysis (NMA).
Methods: Following the PICOS framework, literature was searched in PubMed, Web of Science, Cochrane Library, Embase, Scopus, CNKI, Wanfang, and CBM for randomized controlled trials (RCTs) until June 2024. Independent screening and data extraction were conducted. NMA utilized Stata 15.0 and R 4.4.1, with bias risk assessed by the Cochrane Risk of Bias tool and evidence quality assessed by CINeMA.
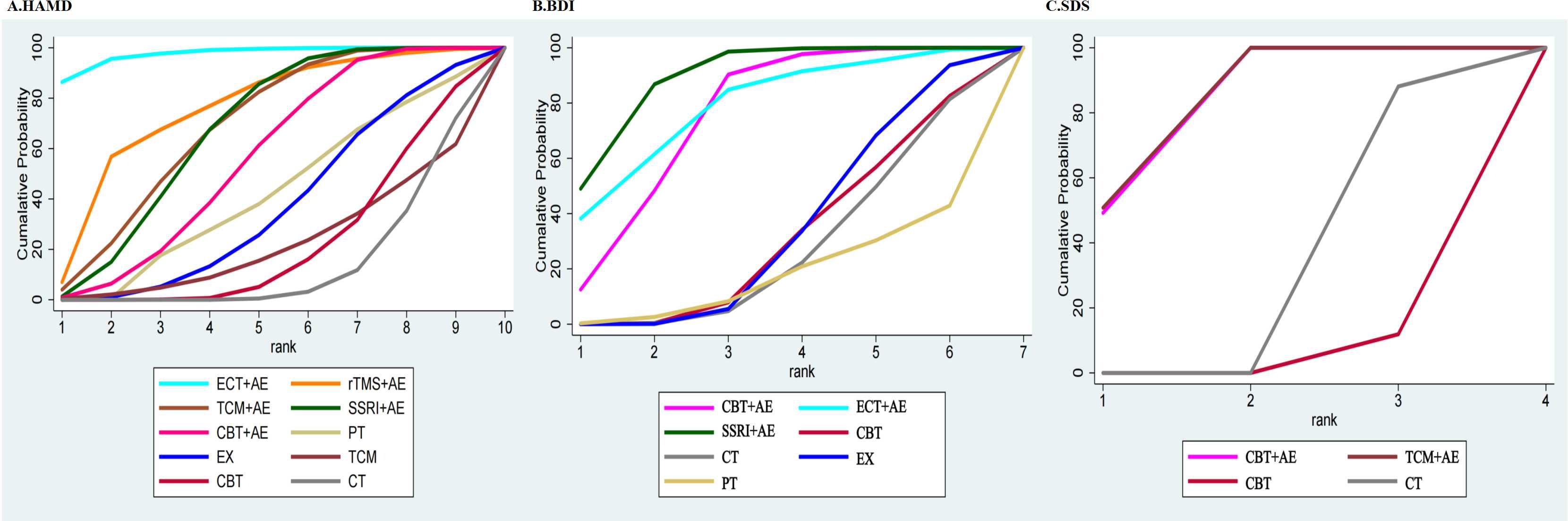
Results: A total of 37 RCTs involving 3,362 patients with depression were included, evaluating five combined AE interventions. Results based on the area under the cumulative ranking curve indicated: (1) Hamilton Depression Rating Scale (HAMD): Electroconvulsive therapy + AE (ECT+AE) > repetitive transcranial magnetic stimulation + AE (rTMS+AE) > Traditional Chinese Medicine + AE (TCM+AE) > Selective Serotonin Reuptake Inhibitors + AE (SSRI+AE) > Cognitive Behavioral Therapy + AE (CBT+AE) > Physical Therapy (PT) > Exercise (EX) > CBT > TCM > Control Treatment (CT); (2) Beck Depression Inventory (BDI): SSRI+AE > ECT+AE > CBT+AE > EX > CBT > CT > PT; (3) Self-rating Depression Scale (SDS): TCM+AE > CBT+AE > CT > CBT.
Conclusions: Current evidence suggests that combined aerobic exercise interventions are superior to monotherapy in the treatment of depression. Of these, SSRI+AE is the most recommended combination, with strong RCT evidence and high-quality evidence ratings. For other AE combination therapies, further validation in large, high-quality trials is necessary in the future.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/, identifier CRD42024594873.
1 Introduction
Depression is a common mental disorder that affects the mental health of hundreds of millions of people worldwide. According to the World Health Organization (WHO), depression has become one of the leading causes of disability in the world, severely affecting patients’ mood, cognition, and physiological functioning, and may even lead to an increase in suicidal behavior (1). With in-depth research on the pathophysiological mechanisms of depression, a variety of therapeutic modalities have been applied in clinical practice, including medication, psychotherapy, and physical therapy. However, these treatment modalities often face the limitations of poor compliance, many side effects, and high costs (2).
Exercise intervention, a non-pharmacological approach to depression management, has garnered significant attention owing to its cost-effectiveness, minimal side effects, and practical applicability (3). Research indicates that exercise exerts beneficial effects on individuals with depression through multiple mechanisms, such as elevating neurochemical levels, suppressing inflammatory responses, regulating the neuroendocrine system, and enhancing neuroplasticity (4). Network meta-analyses have also been used to compare the efficacy of different types of exercise on depression, showing that walking, jogging, yoga, and strength training are more effective than other exercises and that various types of exercise affect cognitive performance, back pain, and blood pressure (5).
Aerobic exercise (AE) refers to physical activity that improves oxygen utilization efficiency while fostering holistic physical and psychological health (6). Recent studies have established the therapeutic potential of aerobic exercise in alleviating depressive symptoms (7, 8). Evidence suggests that aerobic exercise ameliorates depressive symptoms through neurobiological modulation, including hippocampal upregulation of brain-derived neurotrophic factor (BDNF) levels. A regimen of moderate-intensity aerobic exercise (3-5 sessions weekly,≥30 minutes per session, sustained for 6-8 weeks) significantly reduces depressive symptoms in affected individuals (9). Growing experimental evidence supports the integration of aerobic exercise with other therapies to achieve synergistic benefits, thereby optimizing treatment efficacy and complementing conventional interventions (10–12).
Clinical guidelines from the United States, Australia, and New Zealand uniformly advocate integrating aerobic exercise into depression treatment protocols (13). The American Psychiatric Association endorses any aerobic exercise and resistance training as adjunct therapies, whereas Australian and New Zealand guidelines recommend ≥2-3 weekly high-intensity aerobic sessions combined with resistance training (14). However, existing research inadequately explores combination therapies involving aerobic exercise and fails to identify optimal integrated modalities for maximal therapeutic benefit. Furthermore, prior meta-analyses predominantly assessed aerobic exercise as a monotherapy (15–17), with limited investigation into its efficacy when combined with other treatments.
Therefore, this study used NMA to investigate the intervention effects of different treatment measures combined with aerobic exercise on patients with depression, with a view to identifying the most effective of these combined interventions, and to provide an evidence-based basis for treatment choices and nursing practice in depression.
2 Materials and methods
This study strictly adhered to the Priority Reporting Entries for Systematic Reviews and Meta-Analyses: a PRISMA Statement (18) and has been registered with the International Platform for the Registration of Systematic Reviews (PROSPERO) (registration number: CRD42024594873)1.
2.1 Data sources and search strategy
Based on the independent double-blind principle, two researchers followed the PICOS framework (19) and conducted computerized searches in PubMed, Web of Science, Cochrane Library, Embase, Scopus, CNKI, Wanfang Database, and China Biomedical Database. The researchers combined the corresponding subject terms and free text terms for each database, and the search timeframe was from the date of each database’s creation to June 6, 2024. The subject terms used in the literature search included “Exercise” AND “Combined Modality Therapy” AND “Depression” and “Randomized Controlled Trial”. Please refer to the Supplementary Material for details of the search strategy.
2.2 Selection and exclusion criteria
Inclusion criteria (1): Participants were patients with a confirmed diagnosis of depression according to the Diagnostic and Statistical Manual of Mental Disorders (DSM) (20), International Classification of Diseases (ICD) (21), or Chinese Classification of Mental Disorders (CCMD) (22), or patients with depression level scores above the threshold as determined by other clinical diagnostic methods and commonly used depression assessment scales (23–25). Comorbidity was not used as an exclusion criterion (2). The control group received conventional treatment, including medication, psychotherapy, physical therapy, or single-mode exercise therapy. The experimental group combines aerobic exercise (such as walking, jogging, dancing, etc.) with low to moderate intensity on a continuous basis, with the treatment of the control group (3). The results of this study were measured based on the severity of depressive symptoms, which were assessed using the HAMD, BDI, and SDS scores (4). The study type was RCT.
Exclusion criteria (1): studies in which diagnostic criteria were not clearly described (2); studies in which a single treatment measure was used in the test group (3); studies in which the full text was not available; and (4) studies in which information was incomplete and data could not be extracted.
2.3 Literature screening and data extraction
Two researchers conducted the inclusion and screening of the literature in an independent double-blind manner and carried out cross-checking. In case of any discrepancies during the inclusion process, a third researcher would be involved to make the final decision. Finally, literature management was carried out using EndNoteX9 software, and data were extracted step by step in accordance with a pre-designed table, including the first author of the literature, the title, the year of publication, the basic information of the research subjects, the interventions taken, and the main outcome measures.
2.4 Risk of bias evaluation of included studies
Based on the recommended risk of bias assessment tool in the Cochrane Handbook 5.1.0, the RevMan 5.4 software was used to evaluate the risk of bias in RCTs according to six aspects: random sequence generation, allocation concealment, blinding of participants and personnel, completeness of outcome data, selective reporting, and other bias (26). When all items were assessed as “low risk,” the study was classified as grade A. If some items were assessed as “low risk,” it was classified as grade B. If none were assessed as “low risk,” it was considered grade C (27).
2.5 Statistical analysis
In this study, NMA was performed using Stata 15.0 software. For the closed-loop structure in the network evidence graph, the node-split method was applied to test for consistency; a consistency model was used if P > 0.05, and an inconsistency model was used otherwise. Intervention ranking was assessed using the surface under the cumulative ranking curve (SUCRA; 0% to 100%, higher values indicate better efficacy). Publication bias was assessed using Egger’s test and funnel plots. Heterogeneity was evaluated using τ² and its p-value for qualitative assessment, alongside I² for quantitative estimation (I² < 25%: low; 25–50%: moderate; > 50%: substantial; > 75%: high heterogeneity). To address substantial heterogeneity (I² > 50%), NMA regression analyses were conducted using the R software gemtc package to explore potential sources (e.g., publication year, age, diagnostic tools, baseline symptoms, intervention duration, and frequency). Finally, the CINeMA framework was applied to assess the risk of bias and evidence quality (28).”
3 Results
3.1 Results of the literature search
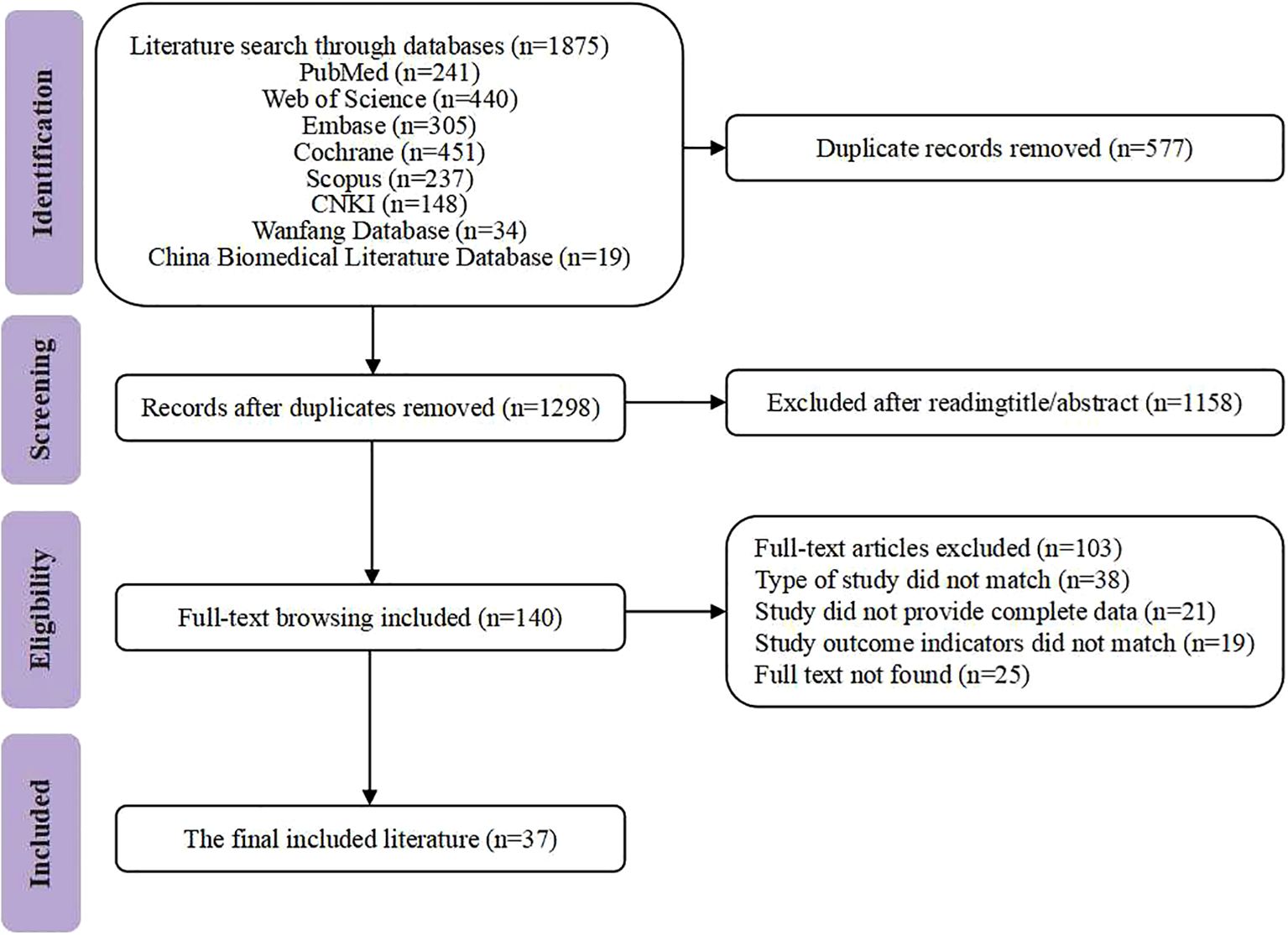
A comprehensive search of 8 databases yielded 1,875 articles relevant to the research topic. After merging and filtering with EndNote X9, 577 duplicates were removed. Then, 140 articles were preliminarily selected based on titles and abstracts. Finally, 37 RCTs were included after full-text reviews of the 140 articles. Figure 1 shows the literature screening process.
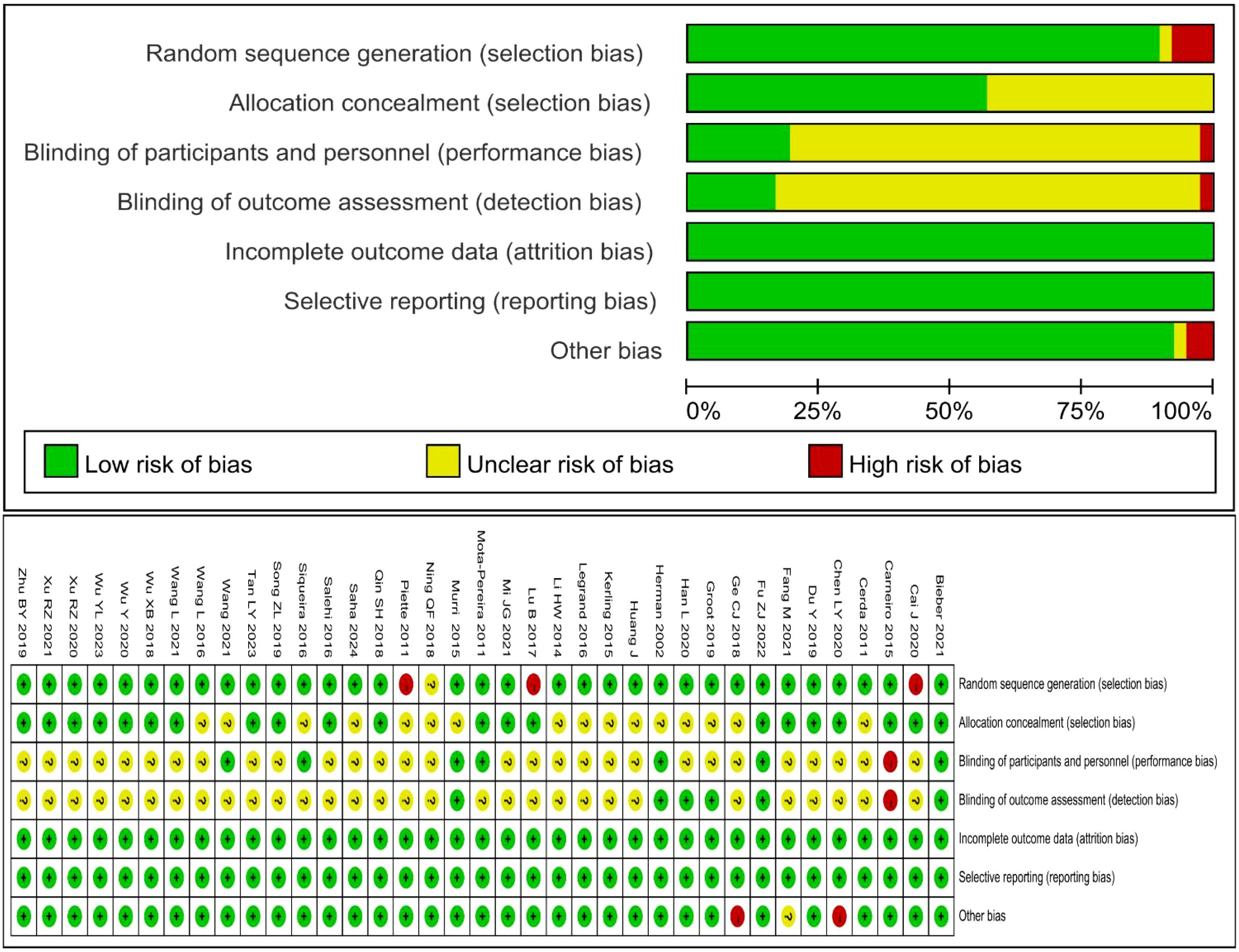
3.2 The characteristics of studies
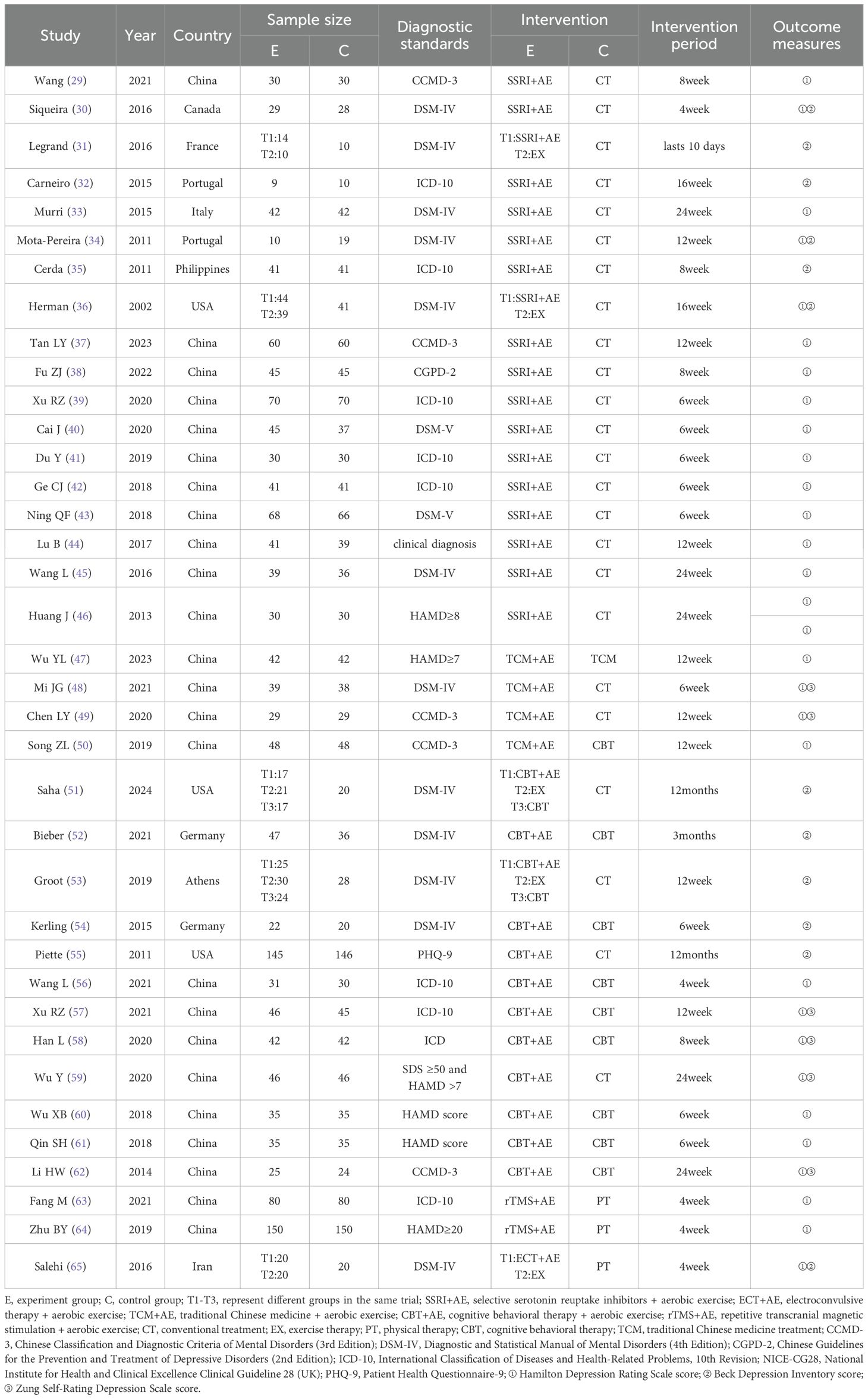
This study included a total of 37 articles (29–65), encompassing 3,362 patients with depression and evaluating five distinct combined aerobic exercise interventions. Among these, 19 studies investigated selective serotonin reuptake inhibitors combined with aerobic exercise (SSRI+AE), 12 studies examined cognitive behavioral therapy combined with aerobic exercise (CBT+AE), 4 studies focused on Traditional Chinese Medicine combined with aerobic exercise (TCM+AE), 2 studies assessed repetitive transcranial magnetic stimulation combined with aerobic exercise (rTMS+AE), and 1 study explored electroconvulsive therapy combined with aerobic exercise (ECT+AE). The baseline characteristics of the included studies are presented in Table 1.
3.3 Quality assessment
The quality of the included literature was evaluated; 2 were graded A (38, 52) and 35 were graded B (29–37, 39–51, 53–65). The quality of the included literature was assessed by a quality assessment. Of these, 35 used randomization sequences, 24 implemented allocation method concealment, 4 were blinded to both subjects and assessors, and all of the included literature reported on the primary outcome indicators. Detailed results are shown in Figure 2.
3.4 Results of reticulated meta-analysis
3.4.1 Web evidence map
The HAMD score, BDI score, and SDS score were used to compare the intervention effects of different interventions, and their network relationships are shown in Figure 3. The dots in the network evidence map represent the interventions for treating depression. The size of the dots reflects the sample size of the intervention, while the thickness of the lines between the dots indicates the number of related studies. The results demonstrated that SSRI+AE had the highest number of supporting studies compared to other interventions.
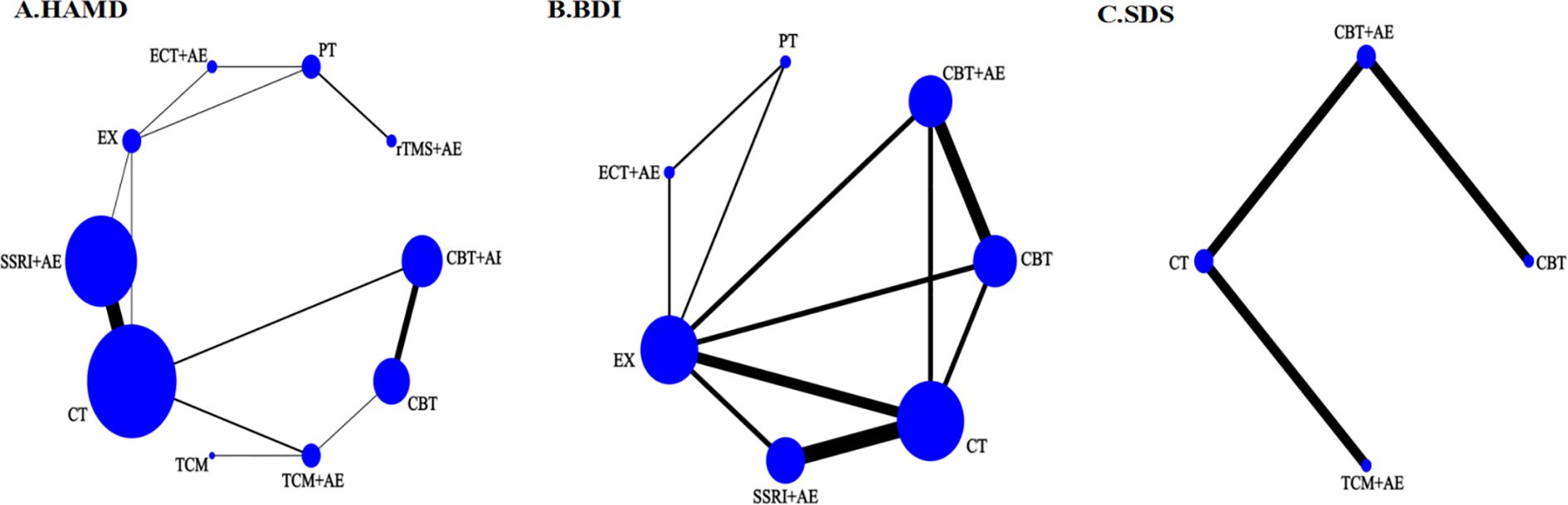
Figure 3. Network structure of different treatment measures. (A) Network structure diagram of HAMD outcomes; (B) Network structure diagram of BDI outcomes; (C) Network structure diagram of SDS outcomes.
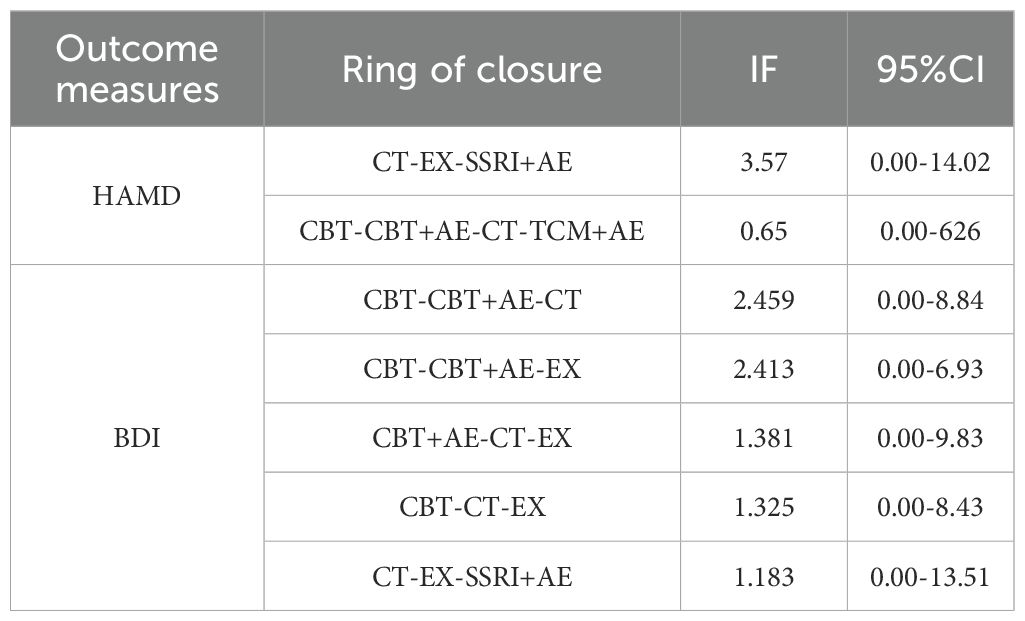
3.4.2 Inconsistency check
Inconsistency tests were performed on the closed loops formed by HAMD scores and BDI scores. The results showed that the inconsistency factor (IF) values of some closed loops were higher than 1, but the 95% CIs of all closed loops included 0, indicating no inconsistency in outcome indicators (see Table 2). Furthermore, the node-splitting method was used to perform global consistency and local consistency tests. All results showed P > 0.05, suggesting good global and local consistency. Therefore, the consistency model was adopted for the network meta-analysis in this study.
3.4.3 Comparative results for key indicators
Twenty-nine RCTs reported HAMD scores, involving 5 combined treatment measures. The results of NMA showed (Figure 4A) that compared with conventional treatment, ECT+AE (MD: -9.61, 95%CI: -15.85 to -3.38), TCM+AE (MD: -5.61, 95%CI: -9.37 to -1.85), SSRI+AE (MD: -5.39, 95%CI: -6.89 to -3.81), and CBT+AE (MD: -4.28, 95%CI: -7.88 to -0.69) were more effective. Compared with single CBT treatment, TCM+AE (MD: -4.16, 95%CI: -5.51 to -2.81), SSRI+AE (MD: -4.16, 95%CI: -5.51 to -2.81), and CBT+AE (MD: -4.16, 95%CI: -5.51 to -2.81) were more effective. It is worth noting that ECT+AE was superior to all single treatment measures.
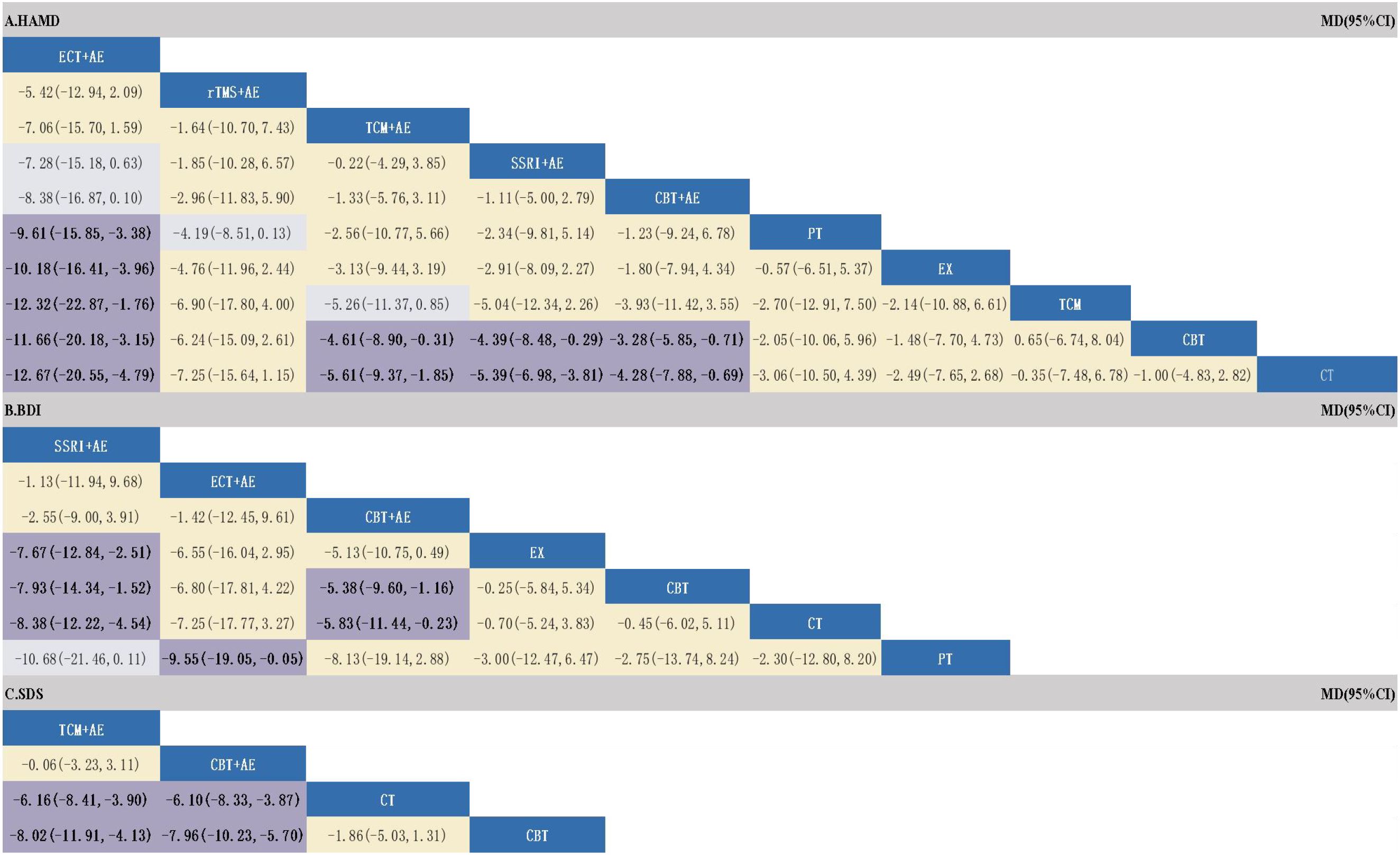
Figure 4. Results of a network meta-analysis of different treatment measures (MD95%CI). (A) ranking of different combinations for HAMD outcomes; (B) ranking of different combination treatments for BDI outcomes; (C) ranking of different combination treatments for SDS outcomes.
The SUCRA rankings of each treatment measure were ECT+AE (97.6%) > rTMS+AE (75.5%) > TCM+AE (68.4%) > SSRI+AE (67.3%) > CBT+AE (55.6%) > Physical Therapy (41.2%) > Exercise Therapy (36.5%) > CBT (22.1%) > TCM (22%) > CT (13.7%). However, it should be particularly noted that the top two ranked ECT+AE and rTMS+AE were contributed by only 1 and 2 studies, respectively. Although their SUCRA values were high, the evidence base was very weak, and interpretation should be extremely cautious. The cumulative probability comparison is shown in Figure 5A, and the detailed SUCRA ranking probabilities are shown in Supplementary Table 11.
3.4.4 Comparative results for secondary indicators
Twelve RCTs reported BDI scores, involving 3 combined treatment measures. The NMA results showed (Figure 4B) that SSRI+AE was superior to conventional treatment (MD: -8.38, 95%CI: -12.22 to -4.54), single EX (MD: -7.67, 95%CI: -12.84 to -2.51), and single CBT (MD: -7.93, 95%CI: -14.34 to -1.52). CBT+AE was superior to conventional treatment (MD: -5.83, 95%CI: -11.44 to -0.23) and single CBT (MD: -5.38, 95%CI: -9.60 to -1.16). ECT+AE was only superior to single PT (MD: -9.55, 95%CI: -19.05 to -0.05). The SUCRA rankings were SSRI+AE (88.8%) > ECT+AE (78.1%) > CBT+AE (75%) > EX (33.1%) > CBT (30.9%) > CT (26.6%) > PT (17.3%). The cumulative probability comparison is shown in Figure 5B, and the detailed SUCRA ranking probabilities are presented in Supplementary Table 12.
Six RCTs reported SDS scores, involving 2 combined treatment measures. The NMA results showed (Figure 4C) that TCM+AE was superior to conventional treatment (MD: -6.16, 95%CI: -8.41 to -3.90) and single CBT (MD: -8.02, 95%CI: -11.91 to -4.13). CBT+AE was also superior to conventional treatment (MD: -6.10, 95%CI: -8.33 to -3.87) and single CBT (MD: -7.96, 95%CI: -10.31 to -5.70). The SUCRA rankings were TCM+AE (83.6%) > CBT+AE (83.1%) > CT (29.4%) > CBT (4%). The cumulative probability comparison is shown in Figure 5C, and the detailed SUCRA ranking probabilities are presented in Supplementary Table 13.
3.4.5 Heterogeneity and regression analysis
Heterogeneity was assessed using τ², I², and Q statistics, indicating substantial heterogeneity across studies (Supplementary Table 14). We therefore conducted meta-regression to examine potential moderators: mean age, publication year, diagnostic criteria, baseline symptom severity, session duration, intervention frequency, and treatment duration. No significant moderating effects were identified for any covariate (Supplementary Table 15), indicating that the substantial heterogeneity persisted, but the main comparative findings of the NMA were not substantially altered by these factors.
3.4.6 Publication bias
The comparison-adjusted funnel plots for HAMD, BDI, and SDS scores showed asymmetrical scatter distribution, with some points outside the funnel, implying potential publication bias or small-sample effects. However, Egger’s test showed no significant publication bias (P > 0.05). See Figure 6.
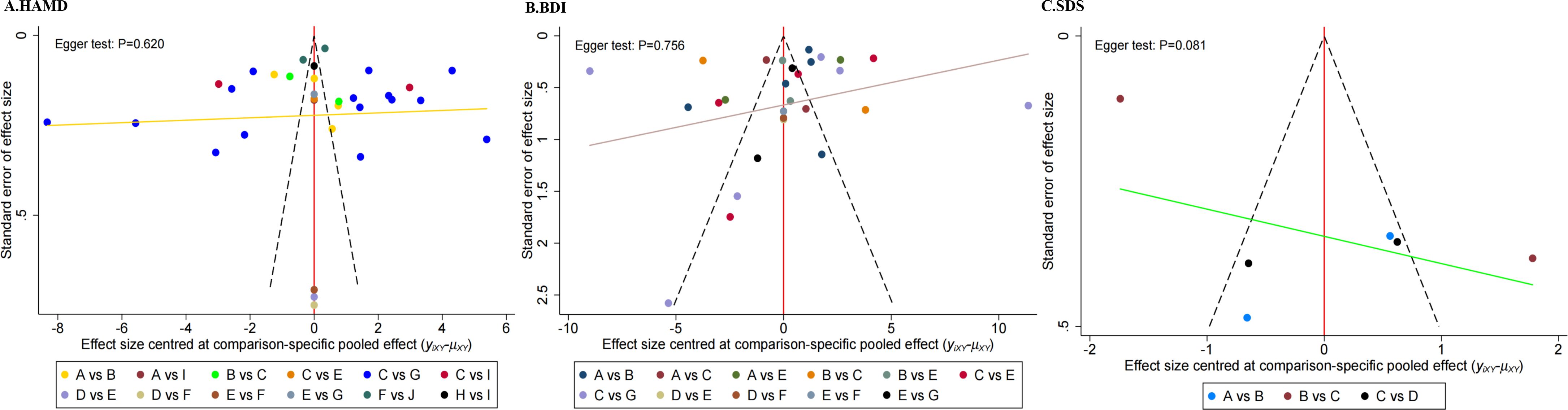
Figure 6. Funnel plot of publication bias for different outcome indicators. (A) Comparison-adjusted funnel plot for HAMD outcomes; (B) Comparison-adjusted funnel plot for BDI outcomes; (C) Comparison-adjusted funnel plot for SDS outcomes. A = CBT+AE; B = CT; C = ECT+AE; D = EX; E = SSRI+AE; F = TCM+AE; G = rTMS+AE.
3.4.7 Quality of evidence evaluation
According to the CINeMA evidence quality assessment results (Supplementary Table 16), only SSRI+AE was rated as having high confidence, while most of the other evidence had “low” confidence and a small portion had “very low” confidence. The reasons for this were significant limitations due to bias risk and imprecision. However, the directness of the research evidence and the low likelihood of publication bias provided assurance for the reliability of the study results.
4 Discussion
Depression is a mental disorder that significantly impacts the quality of life, with core symptoms including persistent low mood, diminished interest, and anhedonia (66). The variability in severity and clinical manifestations of depression poses challenges for treatment, and conventional monotherapies often yield suboptimal outcomes (67). Exercise therapy, particularly aerobic exercise, has emerged as a vital complementary approach to depression treatment due to its minimal side effects, cost-effectiveness, and ease of implementation (68). This study synthesized 37 RCTs from eight databases through a network meta-analysis. Pairwise comparisons of interventions combining aerobic exercise revealed that five therapeutic approaches (SSRI, TCM, rTMS, CBT, ECT) combined with aerobic exercise outperformed conventional monotherapies.
The NMA based on HAMD scores indicated that physical therapies combined with aerobic exercise (ECT+AE and rTMS+AE) demonstrated significant potential advantages in improving depressive symptoms, with SUCRA values reaching 97.6% and 75.5%, respectively. Mechanistically, ECT modulates neurotransmitter equilibrium and neural circuit reorganization in the cerebral cortex via electrical stimulation, restoring homeostasis in the excitatory-inhibitory system and thereby rapidly alleviating core depressive symptoms (69). As a non-invasive physical intervention, rTMS utilizes magnetic pulses to target and regulate neuronal activity in the dorsolateral prefrontal cortex, promoting neuroplasticity and enhancing emotional regulation (70). Aerobic exercise facilitates endorphin release, elevates BDNF levels, and concurrently improves cerebral perfusion and mitigates oxidative stress, creating a multimodal intervention targeting both neurobiological and psychological-behavioral pathways. Its synergistic effects with the aforementioned physical therapies may further enhance therapeutic outcomes (71). However, the current evidence base exhibits significant limitations: only one RCT supports the efficacy of ECT+AE, and only two RCTs support rTMS+AE. This extremely limited number of studies substantially increases the risk of small-study bias and overestimation of effect sizes. Furthermore, CINeMA evidence quality assessment rated their reliability lower than interventions supported by multiple studies (SSRI+AE). Consequently, although the SUCRA ranking suggests potential clinical promise for these combination physical therapies, the conclusion must be regarded as highly exploratory due to the fragility of the evidence. Large-scale, multi-center clinical trials are urgently required to validate their long-term efficacy and safety.
In interventions combining pharmacotherapy with aerobic exercise, TCM+AE showed a marginally higher SUCRA ranking than SSRI+AE, with SUCRA values of 68.9% and 67.1%, respectively. This marginal difference may suggest a potential advantage for TCM+AE, whose mechanism emphasizes personalized holistic regulation, potentially enhancing efficacy by improving the synergistic mind-body state (72). In contrast, SSRIs primarily improve mood by increasing synaptic serotonin concentrations but are limited by delayed onset and insufficient response in some patients (73). Aerobic exercise further amplifies the synergistic effects of both interventions by promoting neurotrophic factor release, enhancing neuroplasticity, and modulating oxidative stress-inflammatory pathways (74). However, it is crucial to emphasize caution: evidence supporting the efficacy of TCM+AE originates from only four RCTs, and its CINeMA evidence quality rating is lower than that of SSRI+AE due to insufficient sample sizes and methodological heterogeneity. This disparity in evidence quality may significantly diminish the clinical interpretability of the SUCRA ranking difference and even carries a risk of small-study bias overestimating the effect. Therefore, although TCM+AE shows potential based on theoretical mechanisms and preliminary data, the findings are insufficient to confirm its significant clinical superiority over SSRI+AE. It should rather be regarded as a potential optimization strategy requiring validation in large-scale, high-quality studies. Future research also urgently needs more rigorously designed clinical trials specifically investigating the synergistic mechanisms between TCM and exercise therapy.
Cognitive behavioral therapy combined with aerobic exercise (CBT+AE) demonstrated superior efficacy to monotherapy in SUCRA rankings across three depression scales, yet underperformed relative to other combined exercise interventions. This discrepancy may stem from inherent tensions between CBT+AE’s therapeutic characteristics and conventional assessment frameworks. As an individualized psychological intervention, CBT+AE’s effectiveness depends critically on therapist-patient engagement and requires sustained behavioral-cognitive restructuring, a process that typically necessitates an extended duration for stable therapeutic effects to manifest (75, 76). While aerobic exercise provides rapid mood improvement through endorphin release and neuroplasticity modulation, fluctuations in patient adherence to psychological interventions may compromise synergistic benefits (77). Notably, existing depression scales primarily capture somatic symptom improvement rather than psychological mechanisms targeted by CBT+AE, such as cognitive restructuring or behavioral activation (78). This measurement misalignment potentially obscures CBT+AE’s long-term advantages in short-term evaluations. Promisingly, emerging evidence suggests dose-response efficacy for CBT+AE in comorbid conditions, for example, OCD, and group-based exercise formats may enhance treatment adherence through social interaction (79). Future protocols should integrate motivational enhancement strategies and multidimensional assessment tools to fully realize this intervention’s clinical potential.
This study has the following limitations. First, although both Chinese and English literature were systematically searched and included, the absence of studies in other languages may compromise the comprehensiveness of the evidence, potentially omitting key findings from specific regions or cultural contexts. Second, significant clinical heterogeneity was present. Although a random-effects model was applied for adjustment and regression analyses were conducted, variations in treatment response across different populations could still confound the efficacy assessment. Third, the outcomes overly relied on depression scale scores, lacking multidimensional assessments such as patient-reported experiences, quality of life, and functional recovery, making it difficult to fully capture the interventions’ actual clinical value. Crucially, the number of studies investigating physical therapy combinations (only 1 for ECT+AE and 2 for rTMS+AE) and TCM combinations (only 4 for TCM+AE) was severely limited. This not only resulted in lower CINeMA evidence quality ratings but also introduced a risk of small-study bias in the SUCRA rankings, highlighting considerable uncertainty in the results. Additionally, the overall quality of the included studies was suboptimal, primarily due to inadequate allocation concealment and double-blinding, which constrained the robustness of the conclusions. Therefore, future research urgently needs to address these evidence gaps through standardized intervention protocols, multidimensional outcome assessments, and large-scale trials.
5 Conclusion
Based on the current evidence, aerobic exercise combination therapies demonstrate superior efficacy over monotherapy. Among these, SSRI+AE emerges as the most robustly supported intervention, with the highest volume of RCT evidence and CINeMA quality rating. Although ECT+AE and rTMS+AE show good SUCRA rankings, they have a limited number of studies and can only be used as exploratory findings. TCM+AE and CBT+AE exhibit potential but are constrained by methodological heterogeneity and assessment limitations. Future research should prioritize large multicenter trials with standardized protocols and multidimensional outcomes to evaluate physical therapy combinations long-term, alongside mechanistic studies on TCM-exercise synergy for precision therapy.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
LC: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AL: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. JZ: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. WC: Conceptualization, Data curation, Investigation, Methodology, Project administration, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. YK: Data curation, Investigation, Methodology, Software, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the National Social Science Foundation of China (21BTY074) and the Hainan Provincial Graduate Student Innovative Scientific Research Project (Qhys2024-374).
Acknowledgments
We thank Prof. Aichun Li, Prof. Junlai Zhou, and team members for their help in data collection and writing this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1573557/full#supplementary-material
Footnotes
- ^ https://www.crd.york.ac.uk/PROSPERO/
References
1. WHO. Word mental health report: transforming mental health for all. Geneva: World Health Organization (2022). Available online at: https://www.who.int/publications/i/item/9789240049338 (Accessed August 13, 2024).
2. Li R, Wang G, and Zhou J. Research progress on exercise intervention treatment for depression. Chin J Psychiatry. (2019) 522:4. doi: 10.3760/cma.j.issn.1006-7884.2019.02.011
3. Kvam S, Kleppe CL, Nordhus IH, and Hovland A. Exercise as a treatment for depression: A meta-analysis. J Affect Disord. (2016) 202:67–86. doi: 10.1016/j.jad.2016.03.063
4. Zhang S and Li C. Research progress on exercise treatment for depressive disorders. J Shanghai Jiao Tong Univ (Medical Science). (2023) 437:916–22. doi: 10.3969/j.issn.1674-8115.2023.07.014
5. Noetel M, Sanders T, Gallardo-Gómez D, Taylor P, del Pozo Cruz B, Van Den Hoek D, et al. Effect of exercise for depression: systematic review and network meta-analysis of randomised controlled trials. bmj. (2024) 3848417:17. doi: 10.1136/bmj-2023-075847
6. Shu JW, Lu TC, Tao BL, Chen HW, Sui HR, Wang LZ, et al. Effects of aerobic exercise on body self-esteem among Chinese college students: A meta-analysis. PloS One. (2023) 189:e0291045. doi: 10.1371/JOURNAL.PONE.0291045
7. Radovic S, Gordon MS, and Melvin GA. Should we recommend exercise to adolescents with depressive symptoms? A meta-analysis. J Paediatrics Child Health. (2017) 533:214–20. doi: 10.1111/jpc.13426
8. Wegner M, Amatriain-Fernández S, Kaulitzky A, Murillo-Rodriguez E, MaChado S, and Budde H. Systematic review of meta-analyses: exercise effects on depression in children and adolescents. Front Psychiatry. (2020) 11:81. doi: 10.3389/fpsyt.2020.00081
9. Pim C, Clara M, Mathias H, Yves PC, Marketa C, Davide P, et al. Psychological treatment of depression: A systematic overview of a ‘Meta-Analytic Research Domain. J Affect Disord. (2023) 335:141–51. doi: 10.1016/j.jad.2023.05.011
10. Recchia F, Leung CK, Chin EC, Fong DY, Montero D, Cheng CP, et al. Comparative effectiveness of exercise, antidepressants and their combination in treating non-severe depression: a systematic review and network meta-analysis of randomised controlled trials. Br J sports Med. (2022) 5623:1375–80. doi: 10.1136/bjsports-2022-105964
11. Singh B, Olds T, Curtis R, Dumuid D, Virgara R, Watson A, et al. Effectiveness of physical activity interventions for improving depression, anxiety and distress: an overview of systematic reviews. Br J sports Med. (2023) 5718:1203–9. doi: 10.1136/bjsports-2022-106195
12. Hu MX, Turner D, Generaal E, Bos D, Ikram MK, Ikram MA, et al. Exercise interventions for the prevention of depression: a systematic review of meta-analyses. BMC Public Health. (2020) 20:1–11. doi: 10.1186/s12889-020-09323-y
13. Gelenberg AJ, Freeman M, Markowitz J, Rosenbaum J, Thase M, Trivedi M, et al. American Psychiatric Association practice guidelines for the treatment of patients with major depressive disorder. Am J Psychiatry. (2010) 167Suppl 10:9–118.
14. Malhi GS, Bell E, Bassett D, Boyce P, Bryant R, Hazell P, et al. The 2020 Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders. Aust New Z J Psychiatry. (2021) 551:7–117. doi: 10.1177/0004867420979353
15. Xu H, Liu R, Wang X, and Yang J. Effectiveness of aerobic exercise in the prevention and treatment of postpartum depression: Meta-analysis and network meta-analysis. PloS One. (2023) 1811:e0287650. doi: 10.1371/JOURNAL.PONE.0287650
16. Li W, Liu Y, Deng J, and Wang T. Influence of aerobic exercise on depression in young people: a meta-analysis. BMC Psychiatry. (2024) 241:1–14. doi: 10.1186/S12888-024-06013-6
17. Wang X, Cai ZD, Jiang WT, Fang YY, Sun WX, and Wang X. Systematic review and meta-analysis of the effects of exercise on depression in adolescents. Child Adolesc Psychiatry Ment Health. (2022) 161:16. doi: 10.1186/S13034-022-00453-2
18. Brian H, David M, and Chris C. The PRISMA extension statement. J Ann Internal Med. (2015) 1637:566–7. doi: 10.7326/L15-5144-2
19. Li XY. PICOS principle in meta-analysis research design. Chin J Intervent Cardiol. (2016) 2411:611. doi: 10.3969/j.issn.1004-8812.2016.11.005
20. American Psychiatric Association D and American Psychiatric Association D. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American psychiatric association (2013).
21. Hong Y and Zeng ML. International classification of diseases (ICD). KO Knowledge Organ. (2023) 497:496–528. doi: 10.5771/0943-7444-2022-7-496
22. Chinese Society of Psychiatry. CCMD-3: Chinese Classification of Mental Disorders (3rd ed.) [M]CCMD-3: Chinese Classification of Mental Disorders (3rd ed.) [M]. Jinan: Shandong Science and Technology Press (2001).
23. Tang YH and Zhang MY. Hamilton Rating Scale for Depression (HAMD). Shanghai Arch Psychiatry. (1984) (2):61–4.
24. Wang Z, Yuan CM, Huang J, Li ZZ, Chen J, Zhang HY, et al. Reliability and validity of the Chinese version of Beck Depression Inventory-IIamong depression patients. Chin Ment Health J. (2011) 256:5. doi: 10.3969/j.issn.1000-6729.2011.06.014
25. Wang ZY and Chi YF. Self-Rating Depression Scale (SDS). Shanghai Arch Psychiatry. (1984) (2).
26. Gu HQ, Wang Y, and Li W. Application of Cochrane Risk of bias tool in meta-analysis of randomized controlled trials. Chin Circ J. (2014) 29002:147–8. doi: 10.3969/j.issn.1000-3614.2014.02.017
27. Fellow JP, Deeks JJ, and Altman DG. Special Topics in Statistics: Cochrane Handbook for Systematic Reviews of Interventions. Chichester, UK: Wiley-Blackwel. (2008) ch1. doi: 10.1002/9780470712184.ch1
28. Adriani N, T HJP, Theodoros P, Anna C, Cinzia DG, Matthias E, et al. CINeMA: An approach for assessing confidence in the results of a network meta-analysis. PloS Med. (2020) 174:e1003082. doi: 10.1371/journal.pmed.1003082
29. Wang J and Li Z. Effect of physical exercise on medical rehabilitation treatment of depression. Rev Bras Medicina do Esporte. (2022) 283:174–6. doi: 10.1590/1517-8692202228032021_0483
30. Siqueira CC, Valiengo LL, Carvalho AF, Santos-Silva PR, Missio G, Sousa RTD, et al. Antidepressant efficacy of adjunctive aerobic activity and associated biomarkers in major depression: A 4-week, randomized, single-blind, controlled clinical trial. PloS One. (2016) 115:e0154195. doi: 10.1371/journal.pone.0154195
31. Legrand FD and Neff EM. Efficacy of exercise as an adjunct treatment for clinically depressed inpatients during the initial stages of antidepressant pharmacotherapy: An open randomized controlled trial. J Affect Disord. (2016) 191:139–44. doi: 10.1016/j.jad.2015.11.047
32. Carneiro LSF, Fonseca AM, Vieira-Coelho MA, Mota MP, and Vasconcelos-Raposo J. Effects of structured exercise and pharmacotherapy vs. pharmacotherapy for adults with depressive symptoms: A randomized clinical trial. J Psychiatr Res. (2015) 71:48–55. doi: 10.1016/j.jpsychires.2015.09.007
33. Murri MB, Amore M, Menchetti M, Toni G, Neviani F, Cerri M, et al. Physical exercise for late-life major depression. Br J Psychiatry. (2015) 2073:235–42. doi: 10.1192/bjp.bp.114.150516
34. Mota-Pereira J, Silverio J, Carvalho S, Ribeiro JC, and Ramos J. Moderate exercise improves depression parameters in treatment-resistant patients with major depression disorder. J Psychiatr Res. (2011) 458:1005–11. doi: 10.1016/j.jpsychires.2011.02.005
35. Cerda PDL, Cervelló E, Cocca A, and Viciana J. Effect of an aerobic training program as complementary therapy in patients with moderate depression. Perceptual Motor Skills. (2011) 1123:761–9. doi: 10.2466/02.15.PMS.112.3.761-769
36. Herman S, Blumenthal JA, Babyak M, Khatri P, Craighead WE, Krishnan KR, et al. Exercise therapy for depression in middle-aged and older adults: predictors of early dropout and treatment failure. Health Psychol. (2002) 216:553. doi: 10.1037/0278-6133.21.6.553
37. Tan LY and Zhang TW. Therapeutic effect of escitalopram combined with aerobic exercise in depression. Healthy Friends. (2023) 7:245–7. doi: 10.3969/j.issn.1002-8714.2023.07.084
38. Fu ZJ, Xu MY, Wang TD, Chen XH, and Wang AH. Effects of aerobic exercise therapy combined with selective5-hydroxytryptamine reuptake inhibitor on the remissionof psychiatric symptoms and social function in adolescentpatients with depression. J Clin Pathological Sci. (2022) 4212:3047–54. doi: 10.3978/j.issn.2095-6959.2022.12.028
39. Xu RZ, Wang XJ, Chen QQ, and Tang YP. Analysis of the efficacy of aerobic exercise therapy on mild to moderate depression based on an exercise data monitoring model. Zhejiang Clin Med. (2020) 228:1143–4.
40. Cai J and Ling D. Efficacy of paroxetine combined with exercise behavior intervention in the treatment of depression and its effect on γ-aminobutyric acid. Int J Lab Med. (2020) 4120:2485–8. doi: 10.3969/j.issn.1673-4130.2020.20.013
41. Du Y, Wang L, Zhang XL, Liu BG, Dai J, Wu HL, et al. Control study of exercise’influence on depression’s symptom,cognitive function and GABA. Chin J Gen Pract. (2019) 179:1547–50. doi: 10.16766/j.cnki.issn.1674-4152.000994
42. Ge CJ and Li JH. Clinical efficacy of escitalopram combined with aerobic exercise in the treatment of depression. Health For Everyone. (2018) 2:71–136.
43. Ning QF, Zhang XL, and Zhou GZ. Clinical efficacy of antidepressants combined with aerobic exercise in the early treatment phase of depression. Shanxi Med J. (2018) 476:675–7. doi: 10.3969/j.issn.0253-9926.2018.06.022
44. Lu B, Wang X, and Ma Y. Effects of trazodone combined with aerobic exercise in treatment of climacteric depression. Southwest Defense Med. (2017) 274:374–6. doi: 10.3969/j.issn.1004-0188.2017.04.019
45. Wang L, Shou XL, Ren AH, Wang ZX, Yu EY, and Wu WZ. Effect of aerobic exercise combined with escitalopram on senile depressivepatients. Modern Chin doctors. (2016) 5435:78–81.
46. Huang J and Li CH. Comparison of quality of life in patients with chronic obstructive pulmonary disease combined with depression treated with haloperidol melittin combined with exercise training. Chin J Gerontology. (2014) 19:5453–5. doi: 10.3969/j.issn.1005-9202.2014.19.059
47. Wu YL, Lin JM, Lin LC, Yu CQ, and Yao BN. Clinical observation of exercise therapy combined with Wenpi-Jieyu decoction in the treatment of depression with spleen-yang deficiency syndrome. Yunnan J Traditional Chin Med. (2023) 4410:45–8. doi: 10.3969/j.issn.1007-2349.2023.10.009
48. Mi JG. Clinical effect of modified Chaihu Longgu Muli decoction combined withTai Chi exercise in treatment of depression: An analysis of 40 cases. Hunan J Traditional Chin Med. (2021) 372:6–9. doi: 10.16808/j.cnki.issn1003-7705.2021.02.002
49. Chen LY. The clinical study of “Motion-Sequential Eight Method” combined with exercise therapy on diabetes with depression. Chin Med Clin Res. (2020) 1236:63–5. doi: 10.3969/j.issn.1674-7860.2020.36.026
50. Song Z, Song Q, and Zheng C. Clearing dizziness and tranquilizing spirit soup combined with exercise intervention for treatment of liver-qi stagnation type elderly hypertension combined with depression in 48 cases. Zhejiang J Traditional Chin Med. (2019) 5411:808–9. doi: 10.3969/j.issn.0411-8421.2019.11.017
51. Saha CK, Shubrook JH, Hornsby WG, Yang Z, Pillay Y, Mather KJ, et al. Program ACTIVE II: 6- and 12-month outcomes of a treatment approach for major depressive disorder in adults with type 2 diabetes. J Diabetes Its Complications. (2024) 382:108666. doi: 10.1016/j.jdiacomp.2023.108666
52. Miriam B, Esra G, Daniela S, Kirsten Z, Semra E, Benedikt F, et al. Effects of body-oriented yoga: a RCT study for patients with major depressive disorder. Eur Arch Psychiatry Clin Neurosci. (2021) 2717:1–13. doi: 10.1007/s00406-021-01277-5
53. Groot MD, Shubrook JH, Hornsby WG, Pillay Y, and Saha C. Program ACTIVE II: outcomes from a randomized, multistate community-based depression treatment for rural and urban adults with type 2 diabetes. Diabetes Care. (2019) 427:1185–93. doi: 10.2337/dc18-2400
54. Kerling A, Tegtbur U, Gützlaff E, Kück M, Borchert L, Ates Z, et al. Effects of adjunctive exercise on physiological and psychological parameters in depression: A randomized pilot trial. J Affect Disord. (2015) 177:1–6. doi: 10.1016/j.jad.2015.01.006
55. Piette JD, Caroline R, Joseph H, Sonia D, Trissa T, Mark V, et al. A randomized trial of telephonic counseling plus walking for depressed diabetes patients. Med Care. (2011) 497:641–8. doi: 10.1097/MLR.0b013e318215d0c9
56. Wang L. Application of multimodal exercise combined with music-guided imagery in elderly patients with depression. (Master's thesis). Huzhou Normal University, Huzhou. (2021). doi: 10.27946/d.cnki.ghzsf.2021.000041
57. Xu RZ, Wang XJ, Chen QQ, and Tang YP. Effects of moderate-intensity aerobic exercise combined with cognitive be-havioral therapy on symptoms and quality of life in patients with mild tomoderate depression. Modern Doctors China. (2021) 5922:105–8.
58. Han L, Zhang H, and Guo H. Intervention effect of health education combined with aerobic exercise on adolescent depression. China School Health. (2020) 416:859–62. doi: 10.16835/j.cnki.1000-9817.2020.06.016
59. Wu Y, Zhao K, and Cheng SN. Exploring the efficacy of using rehabilitation exercises combined with five elements music therapy in elderly patients with Parkinson’s-complicated depression. Chin J Convalescent Med. (2020) 295:504–7. doi: 10.13517/j.cnki.ccm.2020.05.019
60. Wu XB and Lv B. Research on the effect of mental health education combined with aerobic exercise on the early intervention of college students’ psychological depression level. China Health Nutr. (2018) 281:185–6. doi: 10.3969/j.issn.1004-7484.2018.01.272
61. Qin SH. A study on the effect of mental health education combined with aerobic exercise on the intervention of early depression in college students. Psychologist. (2018) 2417:321–2.
62. Li HW. Kinetotherapy and psychagogy interventionof mild depression in undergraduate student. Sports Res Educ. (2014) 294:114–7.
63. Fang M. Effects of repetitive transcranial magnetic stimulation combined with exercise therapy on the level of cognitive functioning in patients with major depressive disorder. Huaihai Med. (2021) 395:495–7. doi: 10.14126/j.cnki.1008-7044.2021.05.016
64. Zhu BY and Yin XW. Effect of repetitive transcranial magnetic stimulation combinedwith exercise therapy on cognitive function and serum inflammatorycytokine levels in patients with depression. China J Modern Med. (2019) 2922:113–7. doi: 10.3969/j.issn.1005-8982.2019.22.023
65. Salehi I, Hosseini SM, Haghighi M, Jahangard L, Bajoghli H, Gerber M, et al. Electroconvulsive therapy (ECT) and aerobic exercise training (AET) increased plasma BDNF and ameliorated depressive symptoms in patients suffering from major depressive disorder. J Psychiatr Res. (2016) 76:1–8. doi: 10.1016/j.jpsychires.2016.01.012
66. Bao H and Liu YY. Progress in etiology and diagnosis of depression. Prog Clin Med. (2023) 134:5641–5. doi: 10.12677/acm.2023.134797
67. Wang XD, Qiao MQ, Zhang ZJ, Chen G, Chen JX, and Tu Y. Current status and outlook of research on depressive disorders in China. Chin J Psychiatry. (2015) 3:5. doi: 10.3760/cma.j.issn.1006-7884.2015.03.004
68. Jiang SW, Bo Y, He LG, Ren DR, Ya GC, and Hai BY. Research progress in exercise therapy for depression. Chin J Phys Med Rehabil. (2019) 413:3. doi: 10.3760/cma.j.issn.0254-1424.2019.03.019
69. Sun X, Di DC, and Zhang DJ. A study of the effect of drug combined MECT and rTMS treatment on cognitive function in patients with depression. Adv Psychol. (2024) 146:42–7. doi: 10.12677/ap.2024.146378
70. Yang J, Yang CX, Liu PH, and Sun N. Research progress of brain network mechanism of the anti-depressive effect of repetitive transcranial magnetic stimulation based on magnetic resonance imaging. Chin J Psychiatry. (2023) 562:144–9. doi: 10.3760/cma.j.cn113661-20220615-00155
71. George MS. Transcranial magnetic stimulation for the treatment of depression. Expert Rev Neurother. (2010) 1011:1761–72. doi: 10.1586/ern.10.95
72. Olav S and Bjrn M. Drug treatment of depression. Br Med J. (2021) 2:13–7. doi: 10.3760/cma.j.issn.1007-9742.1999.Z1.105
73. Lynn B, Fredrik H, Alexander L, Pim C, and Elias E. The complex clinical response to selective serotonin reuptake inhibitors in depression: a network perspective. Trans Psychiatry. (2023) 131:19–. doi: 10.1038/S41398-022-02285-2
74. Wang XH, Tang L, and Pan M. Exercise intervention in the treatment of depression. Int J Psychiatry. (2024) 5104:1023–5. doi: 10.13479/j.cnki.jip.2024.04.077
75. Wang JF, Li X, Wang Y, and Yuan J. Advances in research on the efficacy of cognitive-behavioral therapy for depression. China Med J. (2013) S1:2.
76. Wang L, Bai H, Wang FJ, Xu Y, Zhang J, and Huang YY. Comparative study on the effect of cognitive behavior therapy in patients with depression disorder. Int J Psychiatry. (2019) 4601:161–3 + 71. doi: 10.13479/j.cnki.jip.2019.01.048
77. Zhang QF. To explore the application value of cognitive behavioral therapy (CBT) inmaintenance treatment of depression. Psychol Monthly. (2021) 17:3. doi: 10.19738/j.cnki.psy.2021.17.015
78. Dunlop BW, Cole SP, Nemeroff CB, Mayberg HS, and Craighead WE. Differential change on depressive symptom factors with antidepressant medication and cognitive behavior therapy for major depressive disorder. J Affect Disord. (2018) 229:111–9. doi: 10.1016/j.jad.2017.12.035
Keywords: depression, aerobic exercise, combination therapy, network meta-analysis, systematic review
Citation: Chen L, Li A, Zhou J, Chen W and Kou Y (2025) Effectiveness of different therapeutic measures combined with aerobic exercise as an intervention in patients with depression: a systematic review and network meta-analysis. Front. Psychiatry 16:1573557. doi: 10.3389/fpsyt.2025.1573557
Received: 09 February 2025; Accepted: 30 June 2025;
Published: 25 July 2025.
Edited by:
Mirko Manchia, University of Cagliari, ItalyCopyright © 2025 Chen, Li, Zhou, Chen and Kou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aichun Li, bGFjMTA1QDE2My5jb20=
†These authors have contributed equally to this work
 Lei Chen
Lei Chen Aichun Li*†
Aichun Li*† Wenhao Chen
Wenhao Chen