- 1Department of Social Work and Social Administration, The University of Hong Kong, Hong Kong, Hong Kong SAR, China
- 2Department of Psychiatry, School of Clinical Medicine, LKS Faculty of Medicine, The University of Hong Kong, Hong Kong, China
- 3School of Nursing, LKS Faculty of Medicine, The University of Hong Kong, Hong Kong, Hong Kong SAR, China
- 4The State Key Laboratory of Brain and Cognitive Sciences, The University of Hong Kong, Hong Kong, Hong Kong SAR, China
- 5Centre for Youth Mental Health, Faculty of Medicine, Dentistry and Health Sciences, University of Melbourne, Parkville, VIC, Australia
- 6Orygen Youth Health, Parkville, VIC, Australia
Introduction: Breakfast skipping is common among young people, although previous work has suggested its negative influences on cognitive and executive functions and mental health outcomes. Whether reduced impulse control, particularly in the cognitive domain, would be a mechanism that links breakfast skipping to elevated psychiatric symptoms remains to be investigated.
Methods: We used data from 3154 young people (aged 15–25 years) in the Hong Kong Youth Epidemiological Study of Mental Health 2019–2022. Participants were asked about their general breakfast consumption habits, impulsivity (overall and its subdomains, using the Barratt Impulsiveness Scale–11), depressive symptoms (Patient Health Questionnaire–9), anxiety symptoms (Generalized Anxiety Disorder Scale–7), and functioning (reduced and lost productivity due to mental health problems, and the observer-rated Social and Occupational Functioning Assessment Scale). Impulsivity and its subdomains were tested for their potential mediating influences between breakfast skipping frequency and symptom outcomes. Sociodemographic variables, psychiatric history, and eating disorder symptoms were adjusted for in all mediation models.
Results: The weighted prevalence of daily breakfast consumption and breakfast skipping (defined as no breakfast consumption at all) was 33% and 14.2%, respectively. More frequent breakfast skipping was associated with higher levels of impulsivity, specifically in terms of attentional control (r=0.14) and self-control (r=0.13), and depressive symptoms (r=0.14), all p<0.001. Breakfast skipping frequency also showed significant associations with anxiety symptoms and poorer functioning, although their relationships were weak (r range=0.04–0.08). In a parallel mediation model, attentional impulsivity (B=0.21, SE=0.03, CI=0.15–0.27), but not self-control impulsivity (B=0.01, SE=0.01, CI=-0.02–0.03), significantly mediated the relationship between breakfast skipping and depressive symptoms and explained 34.2% of the total effect. All findings remained unchanged even when excluding those who reported rising at 12 pm or after.
Conclusion: Breakfast skipping is associated with elevated depressive symptoms in young people, with impaired attentional control being an important mechanism in this relationship. Encouraging young people to build regular breakfast habits may be incorporated as part of future lifestyle interventions for mental disorders and be further emphasised in public health policies.
1 Introduction
Breakfast constitutes one of the most important meals of the day (1). After an overnight fast, blood glucose concentration tends to be at its lowest upon waking, which could negatively affect daytime cognitive functions if not restored (2, 3). Cascades of biochemical reactions involving not only depleted blood glucose and impaired glucose homeostasis but also their related physiological mechanisms (e.g., insulin, cortisol, serotonin, and glutamate) can result due to breakfast skipping (4, 5). Irregular breakfast consumption has been shown to be linked to elevated risks of cardiovascular diseases (6), as well as mental health problems, particularly depressive symptoms (7–11), in a range of studies. Yet, skipping breakfast has become increasingly common in today’s society, particularly among young people (12–14).
While youth signifies a time of increased opportunities for social network building and the crystallisation of self-concepts (15), the marked neurobiological, social, physical, and psychological changes that take place during this life stage also make young people more vulnerable to the onset of mental disorders (16, 17). Despite the significant burden of disease associated with depression and anxiety in youth (18), mental health help-seeking remains a persistent challenge. In our previous youth epidemiological study in Hong Kong (19), we found that only 16.7% of those with a 12-month major depressive episode were utilising any psychiatric or psychological services, with financial costs and accessibility difficulties reported as two leading causes of non-utilisation. Similar observations of non-help-seeking among youths have been reported in other countries (20). In addition to enhancing youth-friendly and evidence-based services in the community, determining the possible benefits of building healthy habits, such as regular breakfast consumption, in mental health may offer more practical and low-stigma strategies for well-being in the population.
Among existing studies that have explored the effects of breakfast skipping on young people, the majority focused on cognitive performance deficits in school-aged children (4). A related systematic review found that children and adolescents who do not consume breakfast tend to show poorer cognitive performance of the brain, particularly in tasks involving attention, memory, and executive functions (4). The researchers, nevertheless, noted the relative scarcity of studies conducted on adolescent samples, thereby limiting the generalisability of findings to this age group. More recently, a meta-analysis has suggested that breakfast skipping is associated with elevated depressive and anxiety symptoms in adolescents, with no associations with anxiety symptoms observed in other age groups (7). These studies generally suggested that breakfast consumption plays a role in cognitive functions and mental health symptoms, although no study has yet simultaneously investigated the effects of breakfast skipping on both cognitive functions and mental health outcomes in young people, as well as their possible interrelationships.
Notably, an earlier national Japanese survey of high school students reported that those who skipped breakfast showed significantly higher levels of impulsivity (21). It is possible that breakfast skipping could be linked to deficits in inhibitory control processes [which are closely related to glucose imbalances (22)] and, in turn, affect mental well-being. Indeed, problems in the ability to focus attention and control impulses have long been linked to a vast range of mental health problems (23–26), particularly in young people (27). Whether reduced impulse control may serve as a mechanism that links breakfast skipping to mental health symptoms, even when adjusting for factors that might confound breakfast consumption patterns and their associations with mental health outcomes (e.g., pre-existing mental health problem, symptoms of eating restraints, and later rise time), warrants further investigation.
Extending observations in previous work, we conducted this study with three major aims: to determine the patterns of breakfast consumption in a population-representative household-based youth sample in Hong Kong; to investigate the associations between breakfast skipping, impulsivity, as well as depressive and anxiety symptoms and functioning outcomes; and to explore whether specific domains of impulsivity would mediate the effects of breakfast skipping on poorer mental health outcomes. We hypothesised that young people who more frequently skip breakfast would show poorer outcomes and that impulsivity, particularly in the cognitive and attentional domains, would mediate the effects of breakfast skipping on both depressive and anxiety symptoms.
2 Materials and methods
2.1 Participants and study design
Participants were from the Hong Kong Youth Epidemiological Study of Mental Health (HK-YES) (19, 28), which was, to date, the first territory-wide household-based study of mental health in Hong Kong specifically targeting young people aged 15–24 years in the city. As in previous large-scale epidemiological studies, a stratified multistage cluster sampling design was adopted to improve sample representativeness. Invitation letters were sent to randomly selected addresses obtained from the local government to all young people within the age group at the time of recruitment. All data were collected from May 2019 to June 2022 by trained research staff through face-to-face interviews or online video conferencing during COVID-19, following the same procedures. Details of the HK-YES have been reported (19, 28–30). Data collected regarding patterns of breakfast consumption habits, impulsivity, depressive and anxiety symptoms, functioning, sociodemographic factors, and plausible confounders in the HK-YES were analysed in the present study. Written informed consent was obtained from all participants in the HK-YES, with additional parental or guardian consent obtained from those below the age of 18 years. Ethical approval was granted by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster.
2.2 Measures
2.2.1 Breakfast consumption patterns
Breakfast consumption was assessed using the item “Which of the following best describes your general breakfast habit?”. The item was rated on a 4-point scale with the following options: “eat breakfast daily”, “often eat breakfast”, “rarely eat breakfast”, and “never eat breakfast”. A higher score reflects a habit of more frequent breakfast skipping.
2.2.2 Impulsivity
Impulsivity was assessed using the 30-item Barratt Impulsiveness Scale, version 11 (BIS-11) (31), which has been referred to as the gold standard in the measure of general impulse control (32). All items on the BIS-11 were rated on a 4-point Likert scale (from “rarely/never” to “almost always/always”) and were summed to generate a composite score, wherein a higher score reflects higher impulsiveness (range = 0–90). Aside from overall impulsivity, the BIS-11 comprises six first-order components reflecting various subdomains of impulse control, namely attention (e.g., “I concentrate easily” [reversed]) (range = 0–15); cognitive instability (e.g., “I have ‘racing’ thoughts”) (range = 0–9); motor (“I do things without thinking”) (range = 0–21); perseverance (e.g., “I can only think about one thing at a time”) (range = 0–12); cognitive complexity (e.g., “I like to think about complex problems” [reversed]) (range = 0–15); and self-control (e.g., “I plan tasks carefully”) (range = 0–18). The Chinese version of the BIS-11 has been validated in young people (33) and shows good internal consistency in our sample (α = 0.76).
2.2.3 Depressive and anxiety symptoms
Depressive and anxiety symptoms during the past two weeks were assessed using the Patient Health Questionnaire–9-item (PHQ-9) (34) and the Generalized Anxiety Disorder–7-item (GAD-7) (35), respectively. Items of the scales were developed based on the DSM-IV criteria, which correspond to symptoms of major depressive disorder and generalised anxiety disorder in the DSM-V. All items were rated on a 4-point Likert scale (from “not at all” to “nearly every day”) and were summed to generate composite scores of depressive and anxiety symptom severity, with higher scores reflecting greater symptom severity]) (PHQ-9 range = 0–27; GAD-7 range = 0–21). Both the PHQ-9 and GAD-7 have been validated in Hong Kong and youth populations (36–38).
2.2.4 Functioning
Three indicators of functioning were assessed, including two items which directly asked the participants the number of days during the past 30 days they have experienced reduced and lost productivity due to psychiatric symptoms, respectively (19) (range = 0–30), and the Social and Occupational Functioning Assessment Scale (SOFAS) (39), which is an interviewer-rated measure derived from the DSM (rated from 0 to 100). A higher score reflects more optimal social and occupational functioning on the SOFAS.
2.2.5 Covariates
Several additional variables were taken as covariates in the study. Sociodemographics include sex, age, socioeconomic status [as reflected by any governmental subsidy received (19)], and any history of a psychiatric disorder. Given possible influences of dietary, shape, and weight concerns in breakfast skipping, symptoms of eating disorders were also included as a plausible confounder, which was reflected by the mean score on the Eating Disorder Examination Questionnaire 6.0 (EDE-Q) (40, 41). Participants were also asked about their regular rising time, which was used to adjust for potential influences of breakfast skipping due to late rising in our sensitivity analyses.
2.3 Statistical analysis
The prevalence of breakfast consumption patterns of the general youth population in Hong Kong was first established with weighting adjustments applied according to sex and age data from the local 2019 Census. A series of independent t-tests or Chi-square tests (for continuous and categorical variables) were applied to explore differences across the various domains of impulsivity, depressive and anxiety symptoms, and functioning between those who at least consume breakfast sometimes and those who completely skip breakfast. A series of correlation analyses were then conducted to examine the degree of associations between breakfast skipping frequency, impulsivity (overall and subdomains), mental health symptoms, and functioning. Mediation models were applied to examine the potential mediating effects of impulsivity between breakfast skipping and symptom outcomes [only among variables showing a coefficient of ≥0.1 in the correlation analyses (42)], whilst adjusting for sociodemographic characteristics and eating disorder symptoms.
As a sensitivity analysis, we conducted the same set of analyses after excluding participants who reported regularly waking at 12 pm or after (late risers) to ensure the breakfast skipping was not the result of late rising time. All mediation effects were tested with a bootstrapping of 10,000 samples and a confidence interval of 95%. Analyses were conducted using SPSS version 29.0, with mediation analyses conducted using the PROCESS macro. The statistical significance was set at the p < 0.05 level for all analyses.
3 Results
3.1 Breakfast skipping: prevalence and associated factors
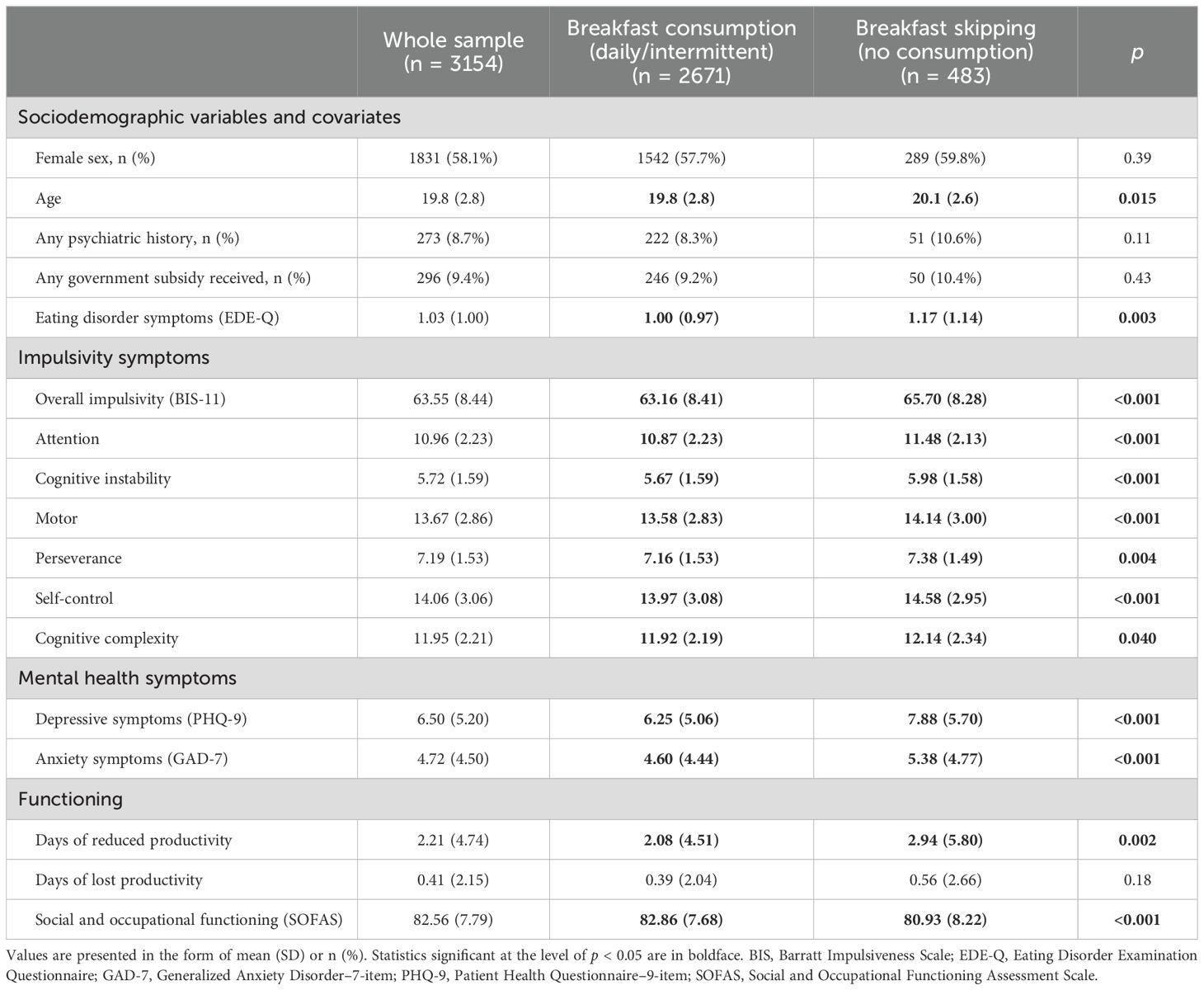
Table 1 presents the sample characteristics, with a detailed summary of the various psychiatric conditions reported by young people provided in Supplementary Table S1. With weighting adjustments applied, 33% of the youth population reported having a habit of consuming breakfast every day. 28.1% often consume breakfast, 24.1% rarely consume breakfast, and 14.8% completely skip breakfast.
Differences in sociodemographic variables, impulsivity, as well as mental health and functioning outcomes, between those who at least sometimes consume breakfast (rarely to daily) and those who completely skip breakfast are also shown in Table 1. Young people who skipped breakfast showed higher levels of overall impulsivity as compared with those who consumed breakfast (mean = 65.70 [SD = 8.28] vs 63.16 [8.41]), p < 0.001. The same pattern of findings was observed for each subdomain of impulsivity (Table 1). Those who skipped breakfast also showed higher levels of depressive symptoms (mean = 7.88 [SD = 5.70] vs 6.25 [5.06]) and anxiety symptoms (5.38 [4.77] vs 4.60 [4.44]), more days of reduced productivity (2.94 [5.80] vs 2.08 [4.51]), as well as poorer social and occupational functioning (80.93 [8.22] vs 82.86 [7.68]), all p < 0.01. They were also slightly older and reported more symptoms of eating disorders. Participant sex, psychiatric history, and socioeconomic status were not different between those who consumed and skipped breakfast, all p > 0.05 (Table 1).
Table 2 shows findings from the correlation analyses. Breakfast skipping frequency was associated with higher levels of overall impulsivity (BIS-11, r = 0.16), and specifically attentional (r = 0.14) and self-control (r = 0.13) impulsivity, all p < 0.001. The associations between breakfast skipping frequency and other subdomains of impulsivity were significant but very weak, with coefficients below 0.1. Breakfast skipping frequency, overall impulsivity, and both attention and self-control impulsivity were also significantly associated with depressive symptoms (r = 0.14; r = 0.33; r = 0.36; r = 0.21), respectively. Moderate degrees of associations were observed between impulsivity and anxiety symptoms and poorer functioning, while very weak associations of breakfast skipping frequency with these outcomes were observed (Table 2). Mediation analyses were thus conducted only on depressive symptoms as the outcome.
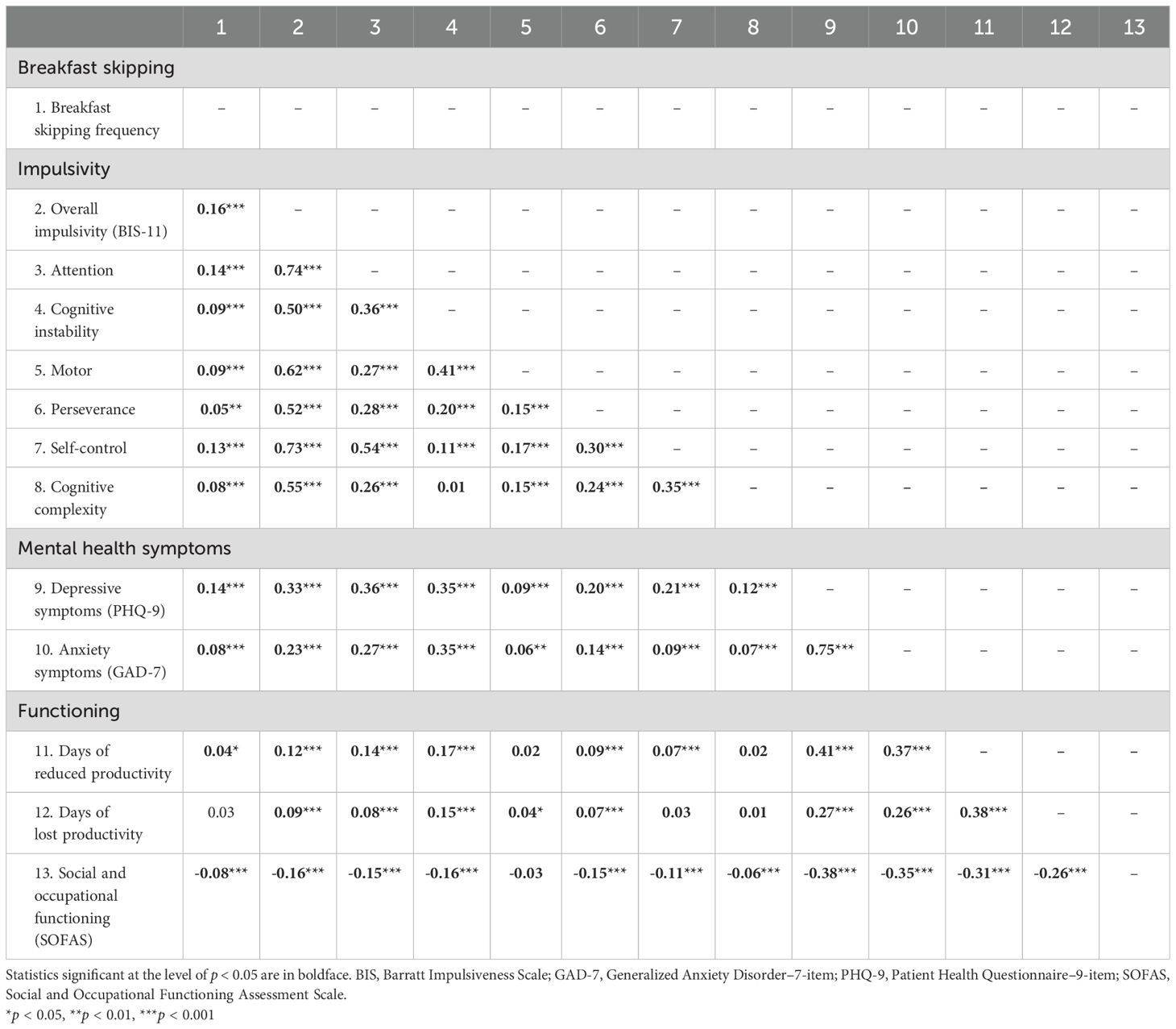
Table 2. Correlations between breakfast skipping frequency, impulsivity, mental health symptoms, and functioning.
3.2 Mediating effects of impulsivity between breakfast skipping and mood symptoms
Two separate mediation models were constructed to examine the potential mediating effects of (i) overall impulsivity, as well as (ii) attentional and self-control impulsivity, between breakfast skipping frequency and depressive symptoms. With sociodemographic characteristics and eating disorder symptoms accounted for, overall impulsivity significantly mediated the effect of breakfast skipping on overall mood symptoms (B = 0.21, SE = 0.03, CI = 0.16–0.26) and accounted for 34.4% of the total effect in the model (Figure 1a). In the second model, a parallel mediation analysis was applied with both attentional and self-control impulsivity (Figure 1b). Results showed significant mediating effects of attentional impulsivity (B = 0.21, SE = 0.03, CI = 0.15–0.27) but not self-control impulsivity (B = 0.01, SE = 0.01, CI = -0.02–0.03) in the model. The two variables altogether explained 35.6% of the total effect, with 34.2% being explained by attentional impulsivity (Figure 1b).
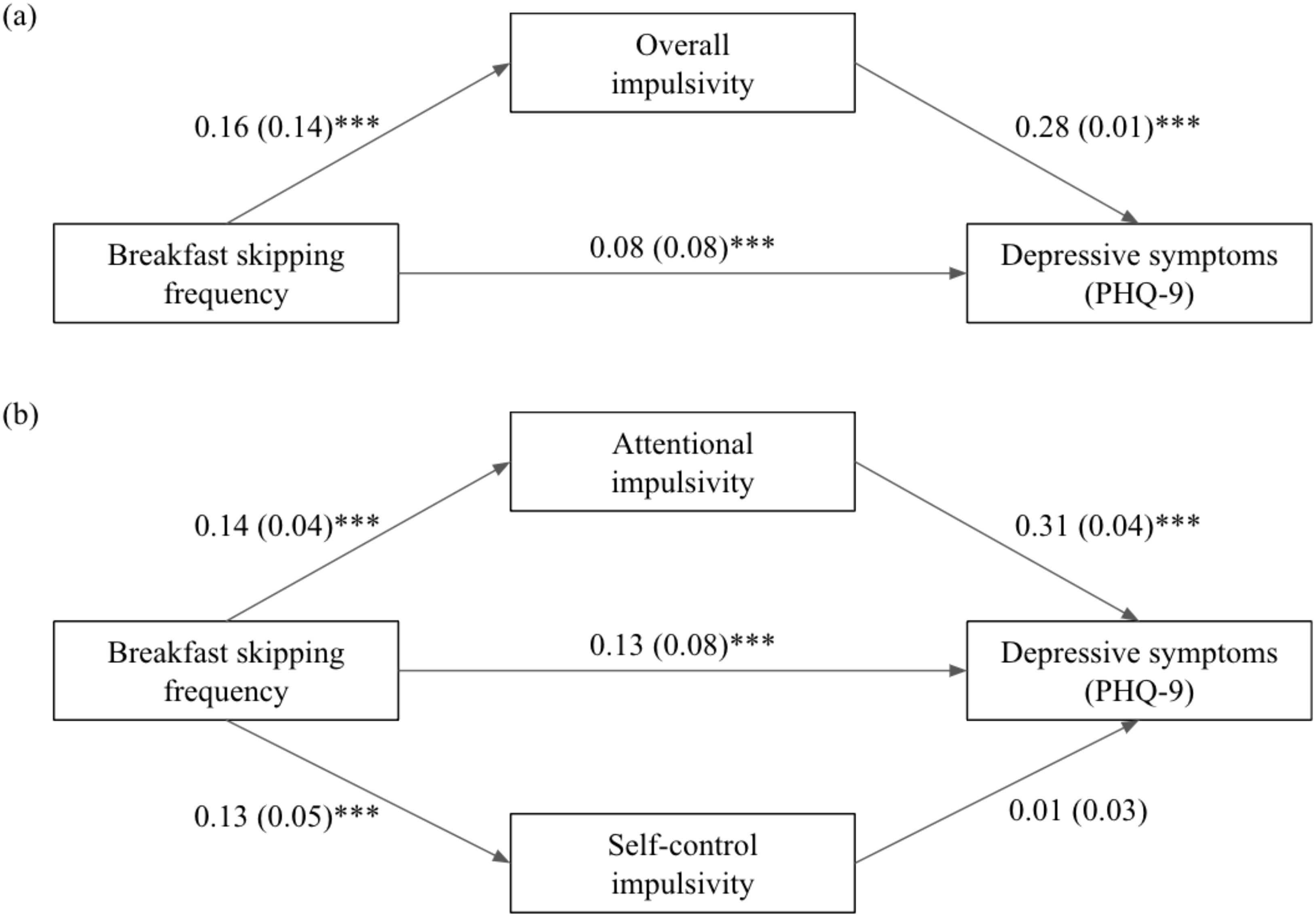
Figure 1. Diagram illustrating impulsivity as a putative mediator between breakfast skipping frequency and depressive symptoms, with (a) overall impulsivity, and specifically (b) attentional and self-control impulsivity, as the mediators. Sex, age, any psychiatric history, socioeconomic status, and symptoms of eating disorders were adjusted for in both models. Standardised coefficients are presented, with standard error in parentheses. PHQ-9 = Patient Health Questionnaire–9-item. ***p<0.001.
Diagram illustrating impulsivity as a putative mediator between breakfast skipping frequency and depressive symptoms, with (a) overall impulsivity, and specifically (b) attentional and self-control impulsivity, as the mediators. Sex, age, any psychiatric history, socioeconomic status, and symptoms of eating disorders were adjusted for in both models. Standardised coefficients are presented, with standard error in parentheses. PHQ-9 = Patient Health Questionnaire–9-item. ***p<0.001
3.3 Sensitivity analysis
Additional analyses were conducted in the youth sample after excluding the subgroup of late risers (n = 2781). Findings from all analyses overall remained unchanged and detailed in the Supplementary Material (Supplementary Tables S2–S4, Supplementary Figure S1).
4 Discussion
This study was the first initiative to examine breakfast consumption habits in a household-based epidemiological youth sample and the possible role of various impulsivity domains between breakfast skipping and mental health symptoms. We found that around one-third of young people (33%) in Hong Kong consume breakfast daily, while nearly 15% completely skip breakfast on a regular basis. Confirming previous studies, we found more frequent breakfast-skipping patterns to be associated with elevated depressive symptoms. Aside from its relationship with overall impulsivity, we found breakfast skipping to be specifically associated with greater attentional and self-control impulsivity, among which attentional impulsivity significantly mediated the relationship between breakfast skipping and depressive symptomatology in young people. These observations have implications for future research and practice.
Despite often being referred to as one of the most important meals of the day, skipping breakfast has become a common lifestyle in modern society (5). While it may be a possible approach to reducing overall energy intake (43), studies have shown the associations of breakfast skipping with elevated risks of adverse health outcomes (6). The importance of regular breakfast consumption has thus been emphasised by governments and organisations, including the World Health Organization (44). While further controlled longitudinal studies are needed to establish the effects of breakfast on the course of depression (e.g., onset, recurrence, and relapse) and its mechanisms, our present study provided a perspective to suggest that attentional impulsivity, in particular, plays a role in the relationships between breakfast skipping and depressive symptoms.
Attentional impulsivity, as assessed using the BIS-11, is generally defined as “an inability to focus attention or concentrate” (45) and covers items such as “don’t pay attention” and “can concentrate easily” (reversed). Indeed, attention is known to be a core building block of cognitive-perceptual functions, with the ability to sustain and control attention playing a crucial role in the manifestation of depressive and anxiety disorders (46, 47). There is also growing evidence in support of attention training (including mindfulness-based cognitive training) in reducing overall depressive and anxiety symptoms and repetitive negative thinking (i.e., rumination and worries) (48–51) – a major transdiagnostic mechanism identified to underly the onset and maintenance of the two internalising disorders (52, 53). The need to give more consideration to the different domains of attention in depressive disorders and other mental health problems has also recently been highlighted (26). Our study contributed to this line of inquiry by showing not only its influences on depressive and anxiety symptoms but also the negative effects (at least to a small degree) of breakfast skipping on attentional control. Whether this relationship is explained by related physiological and metabolic mechanisms or other factors remains to be investigated in future work.
The present study has multiple strengths. The use of an epidemiological design ensured the representativeness of the findings in the youth population, which were generally aligned with previous studies. We also accounted for the influences of major confounding factors, such as demographics, socioeconomic status, psychiatric history, eating disorder symptoms, as well as rising time, which add confidence to the robustness of findings. Together with previous observations, the findings suggest that incorporating breakfast consumption as part of existing clinical interventions (e.g., as a form of behavioural activation) and lifestyle intervention for mental disorders alongside other approaches [e.g., sleep-based interventions (54), and nature experiences (55)] could have beneficial effects. Investing in more rigorous controlled trial studies to evaluate its implications is encouraged.
We note several limitations. First, the cross-sectional nature of the study could not provide definite information on the direction of causality among the variables. With appetite change being a common symptom of depression, it is possible that depressive symptoms could have played a role in the patterns of breakfast skipping we observed in the youth sample. While a number of longitudinal studies have shown a relationship between breakfast skipping and prospective depressive symptoms in young people and adults (8, 9), it would be helpful for future work to build on our study to elucidate the longitudinal, causal pathways among breakfast consumption, impulsivity (particularly attentional impulsivity and control), and mental health outcomes using a combination of experimental and longitudinal observation study designs. Further, while the BIS-11 is a widely adopted self-reported measure of impulsivity, incorporating laboratory-based tests as complementary assessments may offer additional information about specific patterns of associations between breakfast consumption/skipping and the cognitive and behavioural domains of impulsivity, respectively (56).
Contrary to findings from a previous systematic review (7), we did not find breakfast skipping to be associated with anxiety symptoms. Given that the effect sizes in our study were generally weak overall, whether breakfast consumption would be similarly or differentially related to depressive and anxiety symptom dimensions cannot be firmly concluded. The use of a retrospective measure for breakfast consumption can contribute to potential recall bias and may be a reason for the weak effect sizes observed. Nevertheless, the current findings may serve as a basis for future work to replicate and test. Aside from longitudinal studies and randomised controlled trials, the experience sampling method may be considered to pinpoint whether daily breakfast consumption patterns would contribute to subsequent attentional control and mood states, whilst accounting for contextual factors in the real-world setting (57, 58). Qualitative studies should also be conducted to unravel the reasons behind breakfast skipping among young people and, in turn, to inform more personalised intervention approaches and improve intervention uptake. Given the challenges in health behaviour change (59), aside from designing theory and empirically informed interventions, co-creating approaches with young people to facilitate the building of breakfast-eating habits is warranted.
Lastly, we acknowledge that specific components of breakfast [e.g., energy intake, nutrients, portion sizes (1)] could moderate the associations between consumption and health outcomes. A single-item measure of breakfast, similar to previous work (5, 11), can be beneficial for large-scale population screening and in time-limited settings. Nevertheless, it would be worthwhile for future studies to elucidate how each of these components affects physical and mental health and whether differential attention, neurobiological, physiological, and metabolic pathways would mediate their respective associations. These findings would be helpful in informing more effective interventions and providing policymakers with more specific health promotion strategies.
Mental health problems, particularly depression, are among the leading causes of the global burden of disease faced by young people and have considerable implications at individual, interpersonal, and socioeconomic levels. Although additional research is needed to elucidate the pathways and mechanisms underlying breakfast skipping, given problems of service non-utilisation among youths and insufficient manpower in psychiatric or psychological settings, encouraging regular breakfast consumption among young people may act as a simple, low-stigma, low-cost, and scalable strategy with physical, cognitive, and mental health benefits.
Data availability statement
The de-identified raw data supporting the conclusions of this article will be made available by the authors upon reasonable request, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by all participants and from their parents/guardians for those below the age of 18 years.
Author contributions
SW: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. OC: Data curation, Formal analysis, Methodology, Writing – review & editing. YS: Investigation, Methodology, Project administration, Writing – review & editing. CH: Investigation, Methodology, Project administration, Supervision, Writing – review & editing. EL: Investigation, Supervision, Writing – review & editing. SC: Supervision, Investigation, Writing – review & editing. EC: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The study was partially funded by Phase I of the Commissioned Study on Mental Health Survey, Food and Health Bureau, HKSAR Government (Reference number: MHS-P1 (Part 2) to EC.
Acknowledgments
We are grateful to all youth participants of the HK-YES and research staff who contributed to this work. We would also like to thank the Food and Health Bureau, HKSAR Government for their support of the HK-YES.
Conflict of interest
EC received speaker honoraria from Johnson and Johnson and DKSH, which had no role in the present study.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1574119/full#supplementary-material
References
1. O’Neil CE, Byrd-Bredbenner C, Hayes D, Jana L, Klinger SE, and Stephenson-Martin S. The role of breakfast in health: definition and criteria for a quality breakfast. J Acad Nutr Diet. (2014) 114:S8–S26. doi: 10.1016/j.jand.2014.08.022
2. Benton D and Parker PY. Breakfast, blood glucose, and cognition. Am J Clin Nutr. (1998) 67:772S–8S. doi: 10.1093/ajcn/67.4.772S
3. Owens DS and Benton D. The impact of raising blood glucose on reaction times. Neuropsychobiology. (1994) 30:106–13. doi: 10.1159/000119146
4. Adolphus K, Lawton CL, Champ CL, and Dye L. The effects of breakfast and breakfast composition on cognition in children and adolescents: A systematic review. Adv Nutr. (2016) 7:590S–612S. doi: 10.3945/an.115.010256
5. Kim HM, Kang HJ, Lee DH, Jeong S-M, and Joh H-K. Association between breakfast frequency and metabolic syndrome among young adults in South Korea. Sci Rep. (2023) 13:16826. doi: 10.1038/s41598-023-43957-3
6. Rong S, Snetselaar LG, Xu G, Sun Y, Liu B, Wallace RB, et al. Association of skipping breakfast with cardiovascular and all-cause mortality. J Am Coll Cardiol. (2019) 73:2025–32. doi: 10.1016/j.jacc.2019.01.065
7. Zahedi H, Djalalinia S, Sadeghi O, Zare Garizi F, Asayesh H, Payab M, et al. Breakfast consumption and mental health: a systematic review and meta-analysis of observational studies. Nutr Neurosci. (2020) 25(6):1250–64. doi: 10.1080/1028415X.2020.1853411
8. Miki T, Eguchi M, Kuwahara K, Kochi T, Akter S, Kashino I, et al. Breakfast consumption and the risk of depressive symptoms: The Furukawa Nutrition and Health Study. Psychiatry Res. (2019) 273:551–8. doi: 10.1016/j.psychres.2019.01.069
9. Ren Z, Cao J, Cheng P, Shi D, Cao B, Yang G, et al. Association between breakfast consumption and depressive symptoms among Chinese college students: A cross-sectional and prospective cohort study. Int J Environ Res Public Health. (2020) 17:1571. doi: 10.3390/ijerph17051571
10. Ferrer-Cascales R, Sánchez-SanSegundo M, Ruiz-Robledillo N, Albaladejo-Blázquez N, Laguna-Pérez A, and Zaragoza-Martí A. Eat or skip breakfast? The important role of breakfast quality for health-related quality of life, stress and depression in spanish adolescents. Int J Environ Res Public Health. (2018) 15:1781. doi: 10.3390/ijerph15081781
11. Moller H, Sincovich A, Gregory T, and Smithers L. Breakfast skipping and cognitive and emotional engagement at school: a cross-sectional population-level study. Public Health Nutr. (2021) 25:1–10. doi: 10.1017/S1368980021004870
12. Australian Health Survey: Nutrition First Results - Foods and Nutrients. Australian bureau of statistics (2014). Available online at: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/Australian-health-survey-nutrition-first-results-foods-and-nutrients/latest-release (Accessed January 18, 2025).
13. Pendergast FJ, Livingstone KM, Worsley A, and McNaughton SA. Correlates of meal skipping in young adults: a systematic review. Int J Behav Nutr Phys Act. (2016) 13:125. doi: 10.1186/s12966-016-0451-1
14. Heo J, Choi W-J, Ham S, Kang S-K, and Lee W. Association between breakfast skipping and metabolic outcomes by sex, age, and work status stratification. Nutr Metab (Lond). (2021) 18:8. doi: 10.1186/s12986-020-00526-z
15. Sawyer SM, Azzopardi PS, Wickremarathne D, and Patton GC. The age of adolescence. Lancet Child Adolesc Health. (2018) 2:223–8. doi: 10.1016/S2352-4642(18)30022-1
16. Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. (2021) 27:281–95. doi: 10.1038/s41380-021-01161-7
17. Arain M, Haque M, Johal L, Mathur P, Nel W, Rais A, et al. Maturation of the adolescent brain. Neuropsychiatr Dis Treat. (2013) 9:449–61. doi: 10.2147/NDT.S39776
18. GBD. Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2019) 396:1204–22.
19. Wong SMY, Chen EYH, Suen YN, Wong CSM, Chang WC, Chan SKW, et al. Prevalence, time trends, and correlates of major depressive episode and other psychiatric conditions among young people amid major social unrest and COVID-19 in Hong Kong: a representative epidemiological study from 2019 to 2022. Lancet Reg Health West Pac. (2023) 40:100881. doi: 10.1016/j.lanwpc.2023.100881
20. Mitchell C, McMillan B, and Hagan T. Mental health help-seeking behaviours in young adults. Br J Gen Pract. (2017) 67:8–9. doi: 10.3399/bjgp17X688453
21. Itani O, Kaneita Y, Munezawa T, Ikeda M, Osaki Y, Higuchi S, et al. Anger and impulsivity among Japanese adolescents: A nationwide representative survey. J Clin Psychiatry. (2016) 77:e860–6. doi: 10.4088/JCP.15m10044
22. Gailliot MT, Baumeister RF, DeWall CN, Maner JK, Plant EA, Tice DM, et al. Self-control relies on glucose as a limited energy source: willpower is more than a metaphor. J Pers Soc Psychol. (2007) 92:325–36. doi: 10.1037/0022-3514.92.2.325
23. d’Acremont M and van der Linden M. How is impulsivity related to depression in adolescence? Evidence from a French validation of the cognitive emotion regulation questionnaire. J Adolesc. (2007) 30:271–82. doi: 10.1016/j.adolescence.2006.02.007
24. Granö N, Keltikangas-Järvinen L, Kouvonen A, Virtanen M, Elovainio M, Vahtera J, et al. Impulsivity as a predictor of newly diagnosed depression. Scand J Psychol. (2007) 48:173–9. doi: 10.1111/j.1467-9450.2007.00566.x
25. López Steinmetz LC, Godoy JC, and Fong SB. Altitude and latitude variations in trait-impulsivity, depression, anxiety, suicidal risk, and negative alcohol-related consequences in Argentinean adolescents. Heliyon. (2020) 6:e04529. doi: 10.1016/j.heliyon.2020.e04529
26. Keller AS, Leikauf JE, Holt-Gosselin B, Staveland BR, and Williams LM. Paying attention to attention in depression. Transl Psychiatry. (2019) 9:279. doi: 10.1038/s41398-019-0616-1
27. Moustafa AA, Tindle R, Frydecka D, and Misiak B. Impulsivity and its relationship with anxiety, depression and stress. Compr Psychiatry. (2017) 74:173–9. doi: 10.1016/j.comppsych.2017.01.013
28. Wong CS-M, Hui CL-M, Suen Y-N, Wong SM-Y, Chang W-C, Chan SK-W, et al. The Hong Kong youth epidemiological study of mental health (HK-YES)-A population-based psychiatric epidemiology study of youth mental health in Hong Kong: A study protocol. Early Interv Psychiatry. (2023) 17:702–7. doi: 10.1111/eip.13364
29. Hui CLM, Wong SMY, Yu TYT, Lau TTY, Choi O, Tsang S, et al. Visual-stress-related cortical excitability as a prospective marker for symptoms of depression and anxiety in young people. Eur Arch Psychiatry Clin Neurosci. (2022) 273:1051–60. doi: 10.1007/s00406-022-01469-7
30. Wong SMY, Ip CH, Hui CLM, Suen YN, Wong CSM, Chang WC, et al. Prevalence and correlates of suicidal behaviours in a representative epidemiological youth sample in Hong Kong: the significance of suicide-related rumination, family functioning, and ongoing population-level stressors. Psychol Med. (2023) 53:4603–13. doi: 10.1017/S0033291722001519
31. Patton JH, Stanford MS, and Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. (1995) 51:768–74. doi: 10.1002/1097-4679(199511)51:6<768::AID-JCLP2270510607>3.0.CO;2-1
32. Reise SP, Moore TM, Sabb FW, Brown AK, and London ED. The Barratt Impulsiveness Scale-11: reassessment of its structure in a community sample. Psychol Assess. (2013) 25:631–42. doi: 10.1037/a0032161
33. Hui-qin Y, Shu-qiao Y, Xiong-zhao Z, Auerbach R, Abela J, and Tong X. The Chinese version of the Barratt impulsiveness scale,11th version(BIS-11) in adolescents: Its reliability and validity. Chin J Clin Psychol. (2007) 15:4–6.
34. Kroenke K, Spitzer RL, and Williams JBW. The PHQ-9. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
35. Spitzer RL, Kroenke K, Williams JBW, and Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
36. Yu X, Tam WWS, Wong PTK, Lam TH, and Stewart SM. The Patient Health Questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong. Compr Psychiatry. (2012) 53:95–102. doi: 10.1016/j.comppsych.2010.11.002
37. Leung DYP, Mak YW, Leung SF, Chiang VCL, and Loke AY. Measurement invariances of the PHQ-9 across gender and age groups in Chinese adolescents. Asia Pac Psychiatry. (2020) 12:e12381. doi: 10.1111/appy.12381
38. Ip H, Suen YN, Hui CLM, Wong SMY, Chan SKW, Lee EHM, et al. Assessing anxiety among adolescents in Hong Kong: psychometric properties and validity of the Generalised Anxiety Disorder-7 (GAD-7) in an epidemiological community sample. BMC Psychiatry. (2022) 22:703. doi: 10.1186/s12888-022-04329-9
39. Morosini PL, Magliano L, Brambilla L, Ugolini S, and Pioli R. Development, reliability and acceptability of a new version of the DSM-IV Social and Occupational Functioning Assessment Scale (SOFAS) to assess routine social funtioning. Acta Psychiatr Scand. (2000) 101:323–9.
40. Fairburn CG. Cognitive behavior therapy and eating disorders. Guilford Press, New York, NY, USA (2008).
41. Chan CW and Leung SF. Validation of the Eating Disorder Examination Questionnaire: an online version. J Hum Nutr Diet. (2015) 28:659–65. doi: 10.1111/jhn.2015.28.issue-6
42. Schober P, Boer C, and Schwarte LA. Correlation coefficients: Appropriate use and interpretation. Anesth Analg. (2018) 126:1763–8. doi: 10.1213/ANE.0000000000002864
43. Levitsky DA and Pacanowski CR. Effect of skipping breakfast on subsequent energy intake. Physiol Behav. (2013) 119:9–16. doi: 10.1016/j.physbeh.2013.05.006
44. Regional Office for Europe WHO. Adolescents’ Dietary habits. World Health Organization. (2016) https://iris.who.int/bitstream/handle/10665/378549/WHO-EURO-2016-10468-50240-75716-eng.pdf?sequence=1&isAllowed=y (February 9, 2025).
45. Stanford MS, Mathias CW, Dougherty DM, Lake SL, Anderson NE, and Patton JH. Fifty years of the Barratt Impulsiveness Scale: An update and review. Pers Individ Dif. (2009) 47:385–95. doi: 10.1016/j.paid.2009.04.008
46. Chun MM, Golomb JD, and Turk-Browne NB. A taxonomy of external and internal attention. Annu Rev Psychol. (2011) 62:73–101. doi: 10.1146/annurev.psych.093008.100427
47. Eysenck MW, Derakshan N, Santos R, and Calvo MG. Anxiety and cognitive performance: attentional control theory. Emotion. (2007) 7:336–53. doi: 10.1037/1528-3542.7.2.336
48. Hsu KJ, Shumake J, Caffey K, Risom S, Labrada J, Smits JAJ, et al. Efficacy of attention bias modification training for depressed adults: a randomized clinical trial. Psychol Med. (2021) 52:3865–73. doi: 10.1017/S0033291721000702
49. Pettit JW, Rey Y, Marin CE, Bechor M, Lebowitz ER, Vasey MW, et al. Attention training as a low-intensity treatment for concerning anxiety in clinic-referred youth. Behav Ther. (2023) 54:77–90. doi: 10.1016/j.beth.2022.07.004
50. Timm C, Rachota-Ubl B, Beddig T, Zamoscik VE, Ebner-Priemer U, Reinhard I, et al. Mindfulness-based attention training improves cognitive and affective processes in daily life in remitted patients with recurrent depression: A randomized controlled trial. Psychother Psychosom. (2018) 87:184–6. doi: 10.1159/000488862
51. Wadlinger HA and Isaacowitz DM. Fixing our focus: training attention to regulate emotion. Pers Soc Psychol Rev. (2011) 15:75–102. doi: 10.1177/1088868310365565
52. Watkins ER. Depressive rumination and co-morbidity: evidence for brooding as a transdiagnostic process. J Ration Emot Cognit Behav Ther. (2009) 27:160–75. doi: 10.1007/s10942-009-0098-9
53. Wong SMY, Chen EYH, Lee MCY, Suen YN, and Hui CLM. Rumination as a transdiagnostic phenomenon in the 21st century: the flow model of rumination. Brain Sci. (2023) 13:1041. doi: 10.3390/brainsci13071041
54. Cheung FTW and Li SX. Editorial: What does the future hold for psychological treatments in youth? Long-term perspectives on sleep and circadian interventions. J Am Acad Child Adolesc Psychiatry. (2024) 64:321–2. doi: 10.1016/j.jaac.2024.08.003
55. Wong SMY, So MM, Suen Y-N, Hui CLM, and Chen EYH. Can a brief guided nature walk reduce distress and improve resilience, mindful attention, and sleep quality? Evidence from a pilot study with two-week follow-up. Int J Environ Health Res. (2025), 1–11. doi: 10.1080/09603123.2025.2455991
56. Lane SD, Cherek DR, Rhoades HM, Pietras CJ, and Tcheremissine OV. Relationships among laboratory and psychometric measures of impulsivity: Implications in substance abuse and dependence. Addict Disord Their Treat. (2003) 2:33–40. doi: 10.1097/00132576-200302020-00001
57. Verhagen SJW, Hasmi L, Drukker M, van Os J, and Delespaul PAEG. Use of the experience sampling method in the context of clinical trials. Evid Based Ment Health. (2016) 19:86–9. doi: 10.1136/ebmental-2016-102418
58. Myin-Germeys I, Schick A, Ganslandt T, Hajdúk M, Heretik A, Van Hoyweghen I, et al. The experience sampling methodology as a digital clinical tool for more person-centered mental health care: an implementation research agenda. Psychol Med. (2024) 54:2785–93. doi: 10.1017/S0033291724001454
Keywords: breakfast skipping, depressive symptoms, anxiety symptoms, attentional impulsivity, attentional control, youth mental health
Citation: Wong SMY, Choi O, Suen YN, Hui CLM, Lee EHM, Chan SKW and Chen EYH (2025) Breakfast skipping and depressive symptoms in an epidemiological youth sample in Hong Kong: the mediating role of reduced attentional control. Front. Psychiatry 16:1574119. doi: 10.3389/fpsyt.2025.1574119
Received: 10 February 2025; Accepted: 22 April 2025;
Published: 22 May 2025.
Edited by:
Federica Fogacci, University of Bologna, ItalyReviewed by:
Robert Waltereit, University Medical Center Göttingen, GermanyVictor J. Avila-Quintero, Yale University, United States
Copyright © 2025 Wong, Choi, Suen, Hui, Lee, Chan and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Stephanie Ming Yin Wong, c3RlcGgubXkud29uZ0BnbWFpbC5jb20=; Eric Yu Hai Chen, ZXloY2hlbi5oa0BnbWFpbC5jb20=
 Stephanie Ming Yin Wong
Stephanie Ming Yin Wong Olivia Choi
Olivia Choi Yi Nam Suen
Yi Nam Suen Christy Lai Ming Hui
Christy Lai Ming Hui Edwin Ho Ming Lee
Edwin Ho Ming Lee Sherry Kit Wa Chan
Sherry Kit Wa Chan Eric Yu Hai Chen
Eric Yu Hai Chen