- 1Department of Nephrology, Changhai Hospital, Naval Medical University, Shanghai, China
- 2Faculty of Psychology, Naval Medical University, Shanghai, China
- 3Department of Nephrology, Naval Medical Center of PLA, Naval Medical University, Shanghai, China
Background: This study investigated predictive factors and personality determinants of kinesiophobia (fear of movement) in dialysis patients. Methods: Using the Chinese versions of the Ten-Item Personality Inventory (TIPI-C) and Tampa Scale for Kinesiophobia Heart (TSK-SV heart), we assessed 329 patients from December 2022 to February 2023. The influencing factors of fear of movement were identified by univariate analysis and multiple linear regression.
Results: The mean score of fear of movement for dialysis patients was 45.128 (45.128 ± 7.023). Multiple linear regression revealed that advanced age,local medical insurance, and lower education significantly predicted higher kinesiophobia scores, while exercise habits, being married, alcohol and tobacco use served as protective factors. Personality analysis demonstrated that lower extraversion, emotional stability, and conscientiousness were associated with greater kinesiophobia.
Conclusions: Personality determinants were significantly associated with fear of movement. These findings emphasize the clinical utility of personality assessment in identifying high-risk patients and personalizing rehabilitation strategies for this vulnerable population.
1 Introduction
Physical activity constitutes a cornerstone of chronic disease management (1–4), with particular demonstrated efficacy across the continuum of renal disease (3, 5–9). For end-stage kidney disease (ESKD) patients undergoing dialysis, physical dysfunction represents a significant contributor to adverse clinical outcomes (10). Robust evidence confirms that structured exercise interventions yield clinically meaningful improvements in both physical capacity and health-related quality of life (HRQoL) in chronic kidney disease (CKD) patients (11–15), with multicenter studies (n=171 hemodialysis patients) documenting sustained benefits from resistance training (16) and randomized controlled trials validating comparable advantages from home-based programs in both hemodialysis and peritoneal dialysis populations (11). These therapeutic effects are mediated through measurable physiological adaptations including enhanced muscular strength (17) and improved blood pressure control (18, 19).
However, the implementation of exercise therapy faces a formidable psychological barrier in kinesiophobia - a pathological fear of movement (20) that perpetuates physical inactivity cycles (21). This phenomenon proves particularly pronounced in kidney transplant recipients(KTRs) exhibiting excessive graft-protective behaviors (22, 23). Contemporary psychological research reveals that temperament and personality traits fundamentally modulate behavioral responses to physical activity (24). Patients with kinesiophobia typically demonstrate pessimistic outcome expectations and harm-avoidant personality profiles (25), often displaying impaired self-assessment capabilities where exercise tolerance evaluations are disproportionately influenced by prior negative experiences rather than objective capacity (25–27). Emerging research further supports personality-mediated biases in self-reported exercise assessments (28).
Cultural health beliefs prioritizing rest over physical activity compound these psychological dimensions (29, 30). This cognitive-cultural confluence frequently manifests as exercise hypervigilance and subsequent avoidance (31–33), establishing kinesiophobia as a personality-anchored behavioral response specific to physical activity contexts (34). These observations align with broader clinical evidence that psychological factors - particularly depression, anxiety, and kinesiophobia - disproportionately influence rehabilitation outcomes compared to biological or social determinants (35–37), carrying significant implications for treatment adherence and quality of life (38–40).
The diathesis-stress model provides a theoretical framework for these phenomena, positing that pre-existing personality traits amplify during health stressors, predisposing individuals to maladaptive responses (41). Neuroticism exemplifies this mechanism through its established associations with: (1) catastrophic pain cognition, (2) subsequent kinesiophobia development, and (3) ultimately, impaired pain adaptation and depressive symptomatology (42, 43).
Given (1) the established efficacy of exercise therapy in dialysis populations (3), (2) the significant association between kinesiophobia and reduced physical activity (44, 45), and (3)growing recognition of personality’s role in health behavior modulation, this study systematically investigates personality determinants of kinesiophobia in dialysis patients. Addressing this knowledge gap represents a critical step in optimizing rehabilitation outcomes for this vulnerable population through targeted intervention strategies.
2 Materials and methods
2.1 Study design and participants
A prospective cohort study was conducted following a priori power analysis using G*Power 3.1.Based on one-way ANOVA calculations (effect size f = 0.25, α= 0.05, power = 0.8, 4 groups), the minimum required sample size was determined to be 180 participants. Additional analyses were performed for independent t-tests, Pearson correlation, and multiple linear regression to ensure comprehensive power assessment. We recruited 329 end-stage kidney disease patients undergoing maintenance dialysis at Changhai Hospital and Naval Medical Center of PLA between December 2022 and February 2023. Inclusion criteria comprised: (1) age≥18 years, (2) Chinese language fluency, and (3) current dialysis treatment. Exclusion criteria included severe cognitive impairment or diagnosed mental illness. After excluding incomplete responses, 329 participants (179 male, 150 female) were included in final analyses, yielding a 99.1% response rate.
The study was approved by the Research Ethics Commission of Naval Medical Center of PLA (protocol code 2022121903).
2.2 Measures
We collected comprehensive demographic data including age, gender, educational attainment, marital status, cohabitation with children, medical insurance coverage, and pre-diagnosis health behaviors (tobacco/alcohol use and exercise frequency). Clinical variables encompassed primary renal diagnosis, initial and current dialysis modalities, and treatment duration.
Personality characteristics were assessed using the Chinese Version of the Ten-Item Personality Inventory (TIPI-C), a validated adaptation of the original TIPI for Chinese populations. This 10-item instrument evaluates five core personality dimensions:Extraversion (Characterized by enthusiasm, positive emotionality, and sociability), Agreeableness(Reflecting compassion, cooperativeness, and trust), Conscientiousness(Indicating self-discipline, determination, and preference for planned behavior), Emotional Stability(Representing confidence and low emotional reactivity) and Openness(Encompassing creativity, imagination, and novelty-seeking). The TIPI-C has demonstrated satisfactory reliability and validity in Chinese cultural contexts (38, 39).
Emotional stability reflects psychological resilience, characterized by confidence, security, and reduced emotional reactivity in stressful situations. Its counterpart, neuroticism, indicates heightened vulnerability to emotional instability. Openness to experience captures cognitive flexibility and novelty-seeking tendencies, manifesting as creativity, inventiveness, and receptivity to unconventional ideas. Individuals with low openness typically demonstrate conventional attitudes and resistance to change. These personality dimensions were assessed using a standardized 7-point Likert scale (1 = strongly disagree to 7 = strongly agree). The Chinese version of the Ten-Item Personality Inventory (TIPI-C) was adapted from the original TIPI to assess personality traits in Chinese populations. Psychometric evaluations have confirmed its reliability and validity for this cultural context (46, 47).
For our primary outcome, kinesiophobia (fear of movement), we administered the validated Chinese version of the Tampa Scale for Kinesiophobia Heart (TSK-SV Heart). This 17-item instrument measures four domains:Danger (perception of disease risk), Fear (fear of adverse outcomes of exercise), Avoidance (avoidance of exercise due to heart problems), and Dysfunction (physical, psychological, and social dysfunction caused by fear of movement). All items employ a 4-point Likert scale (1 = strongly disagree to 4 = strongly agree), with higher scores indicating greater kinesiophobia severity (48).
2.3 Statistical analysis
All statistical analyses were performed with the use of SPSS 26.0 (Statistical Package for the Social Sciences) for Windows (SPSS, Chicago, IL).A two-sided P<0.05 was considered statistically significant.
For univariate analysis, statistical differences were analyzed using Student’s t-test or one-way ANOVA test. Pearson correlation analysis was used to analyze correlations between continuous variables.
Univariate analysis was conducted for each variable, and multivariate analysis was used for factors with P value<0.05 in univariate analysis. Multiple linear regression analysis using the stepwise procedure was conducted for detecting risk factors for danger, fear, avoidance, dysfunction and fear of movement total score.
3 Results
3.1 Baseline information
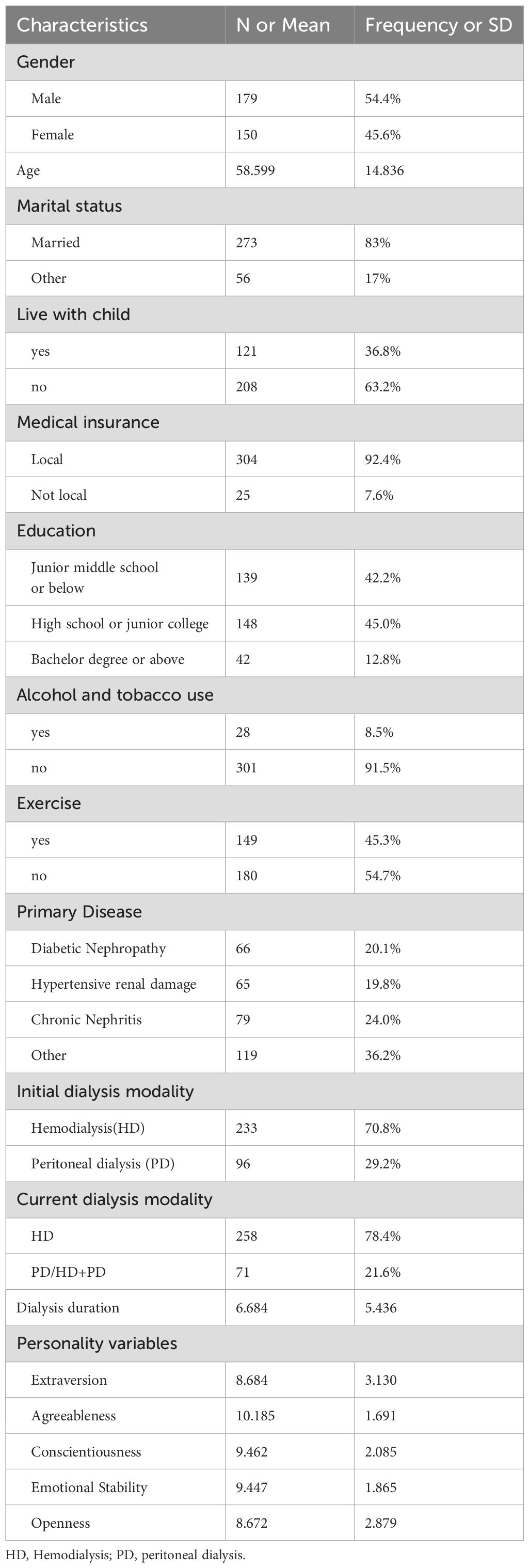
The study cohort comprised 329 dialysis-dependent patients with kidney disease (mean age = 58.599years; range: 22–97 years). Demographic characteristics revealed that 83% were married, 36.8% cohabitated with children, and 92.4% possessed local medical insurance. Educational attainment distribution included: 12.8% with bachelor’s degrees or higher, 45.0% with high school/junior college education, and 42.2% with middle school education or less. Current tobacco or/and alcohol use was reported by 28 participants(8.5%). Primary renal diagnoses were: diabetic nephropathy (20.1%), hypertensive nephropathy (19.8%), chronic nephritis (24.0%), and other etiologies (36.2%). Initial dialysis modalities included hemodialysis (70.8%) and peritoneal dialysis (29.2%), with current treatment distribution of 78.4% hemodialysis and 21.6% peritoneal dialysis/hemodialysis +peritoneal dialysis.The five personality traits of the patients are emotional stability (9.447 ± 1.865), extraversion (8.684 ± 3.130), openness (8.672 ± 2.879), agreeableness (10.185 ± 1.691), and conscientiousness (9.462 ± 2.085) (Table 1).
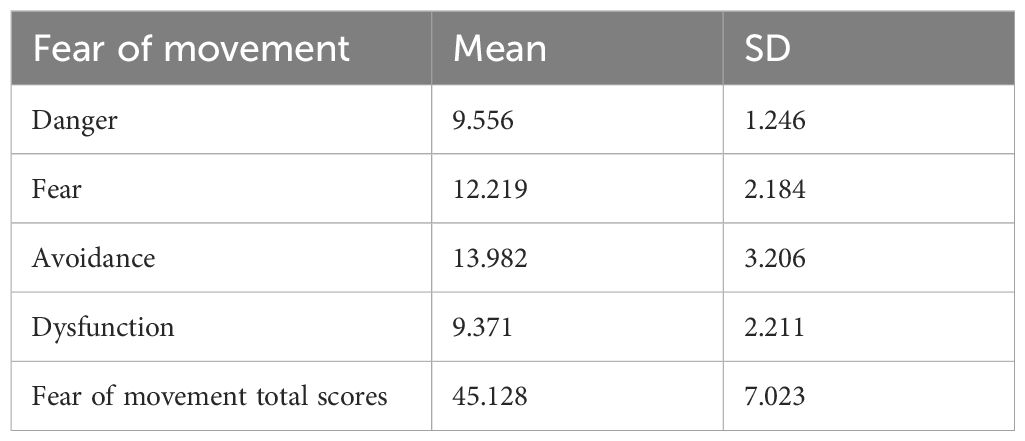
The TSK-SV heart scale measured participants’ scores on four fear of movement factors: Danger (9.556 ± 1.246), Fear (12.219 ± 2.184), Avoidance (13.982 ± 3.206), and Dysfunction (9.371 ± 2.211) (Table 2).
3.2 Danger, fear, avoidance, dysfunction and TSK-SV Heart total scores according to demographic variables and nephropathy variables
Significant differences in kinesiophobia scores emerged across sociodemographic and clinical subgroups (Table 3). Compared to married participants, unmarried individuals (single/divorced/widowed) demonstrated elevated danger scores (t=-2.474, p=0.014) but reduced fear scores (t=2.454, p=0.015). Participants with local medical insurance showed significantly greater fear (t=3.334, p=0.001), avoidance (t=3.604, p<0.001), and total kinesiophobia scores (t=2.789, p=0.006) than those without insurance. Age exhibited positive correlations with fear, avoidance, dysfunction, and total scores. Educational attainment significantly influenced fear (F=8.839, p<0.001), avoidance (F=7.565, p=0.001), and fear of movement total scores (F=7.817, p<0.001). Regular exercise was associated with substantially lower scores across all domains: danger (t=-4.869, p<0.001), fear (t=-8.617, p<0.001), avoidance (t=-10.883, p<0.001), dysfunction (t=-9.876, p<0.001), and fear of movement total scores (t=-12.600, p<0.001). Tobacco/alcohol users reported heightened fear (t=-2.660, p=0.008) and avoidance (t=-2.326, p=0.021) compared to non-users. In addition, primary disease etiology showed significant associations with danger and dysfunction scores, while both initial and current dialysis modalities correlated with fear, avoidance, and total kinesiophobia scores (Table 3).
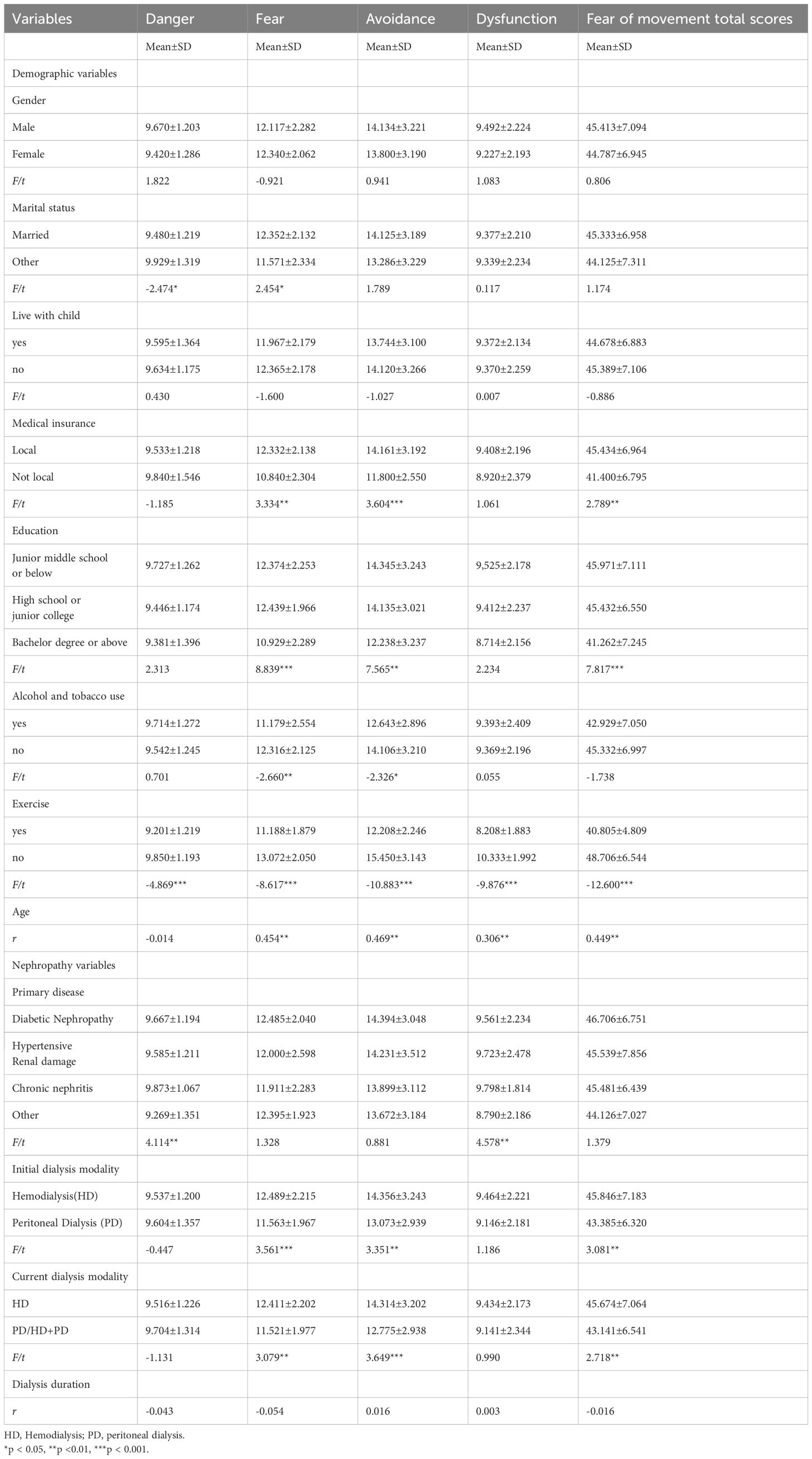
Table 3. Danger, fear, avoidance, dysfunction and TSK-SV Heart total scores according to demographic variables and nephropathy variables.
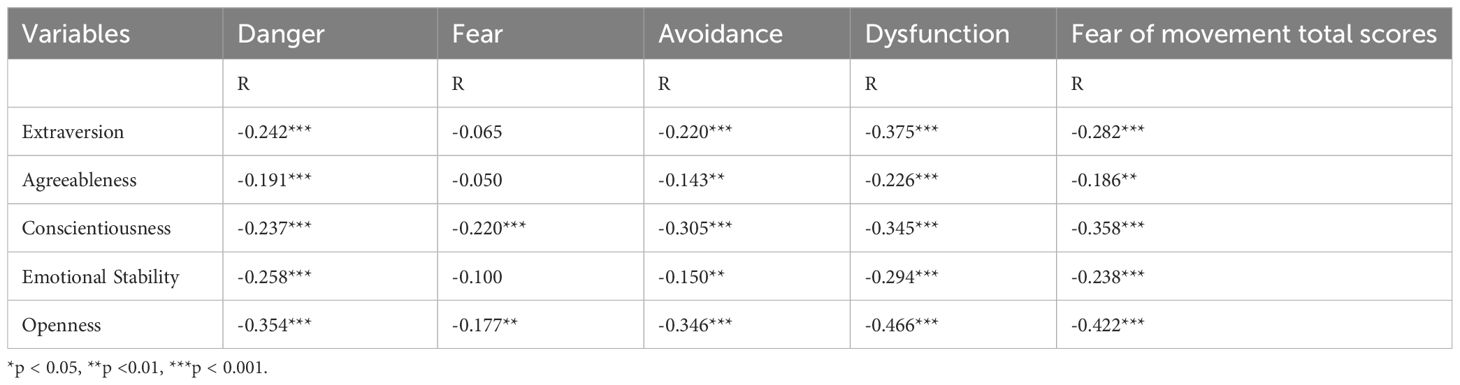
Five personality traits were all significantly associated with danger, avoidance, dysfunction, and fear of movement total score, however fear was significantly associated with conscientiousness and openness (Table 4).
3.3 Risk factors for fear of movement scores
Multiple linear regression analyses were conducted to identify risk factors for kinesiophobia subscales (danger, fear, avoidance, dysfunction) and total scores (Figure 1). Univariate analysis revealed significant associations between danger scores and marital status, exercise habits, primary disease diagnosis, and all five personality dimensions.
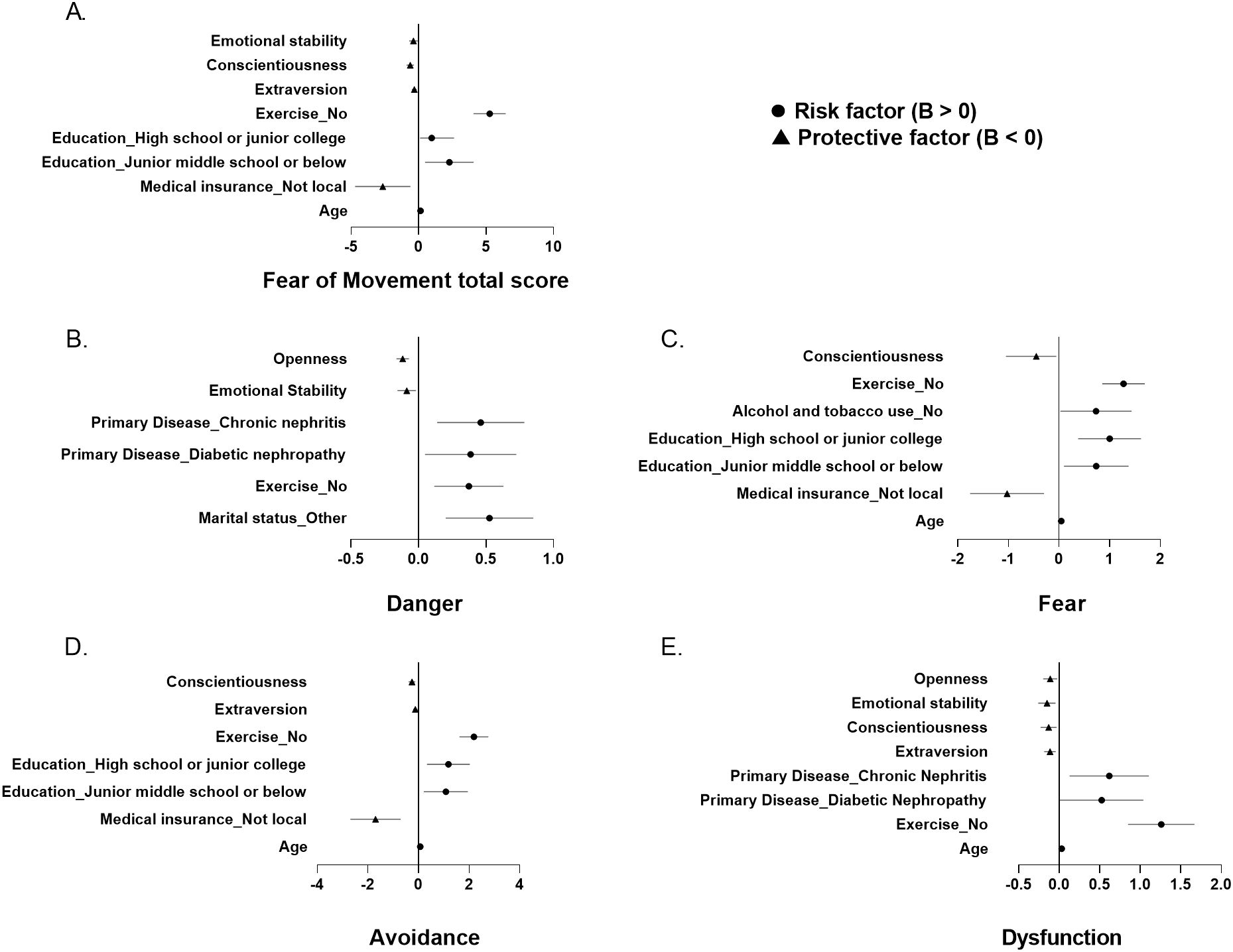
Figure 1. Forest plots of final multivariable linear regression models for (A) Fear of Movement total score and (B-E) its subscales. Unstandardized coefficients (B) with 95% confidence intervals are shown for significant predictors retained in the final model, selected from candidate variables with p<0.05 in univariate analyses. Continuous variables represent the change in outcome per unit increase (e.g., age: 1 year). Categorical variables are relative to reference groups: Education (ref: Bachelor degree or above), Exercise (ref: yes), Marital status (ref: Married), Medical insurance (ref: Local), Alcohol and tobacco use (ref: yes). The vertical line indicates null effect (B=0). Panel descriptions: (A) Fear of Movement total score. (B) Danger. (C) Fear. (D) Avoidance. (E) Dysfunction. Initial candidate variables not retained in the final model were included in model building but did not reach significance (p≥0.05).
The final regression model demonstrated that marital status (married), regular exercise, higher emotional stability, and greater openness served as protective factors against danger perceptions. Conversely, diabetic nephropathy and chronic nephritis emerged as significant clinical risk factors (Figure 1B; Supplementary Table S1).
The fear prediction model demonstrated statistically significant explanatory power (F = 26.508, p < 0.001), which explained 35.2% of the variation in the fear variable (adjusted R2 = 0.352). Significant risk factors included advanced age, local medical insurance coverage, lower educational attainment, and physical inactivity. Conversely, conscientiousness emerged as a protective factor (Figure 1C; Supplementary Table S2).
For avoidance behaviors, the regression model (adjusted R² = 0.442) identified age, local insurance, and education level as risk factors. Protective factors included regular exercise, extraversion, and conscientiousness (Figure 1D; Supplementary Table S3).
The linear regression had dysfunction as the dependent variable to be explained by several independent variables including age, habits of exercising, primary disease, extraversion, conscientiousness, emotional stability, and openness(adjusted R2 = 0.414). Participants with older age, no habit of exercising, and having diabetic nephropathy or chronic nephritis as a primary disease had higher levels of dysfunction. Those with higher levels of extraversion, conscientiousness, emotional stability, and openness had lower levels of dysfunction (Figure 1E; Supplementary Table S4).
The predictive model of the fear of movement total score was constructed using the multiple linear stepwise regression method of the linear regression model. The final multiple linear regression model was statistically significant (F = 43.131, p < 0.001). A total of 50.7% of changes in the dependent variable can be explained by changes in independent variables (adjusted R2 = 0.507). The risk factors of fear of movement total score were older age, having local medical insurance, and lower education level. While the protective factors were having habits of exercising, higher levels of extraversion, conscientiousness, and emotional stability (Figure 1A; Supplementary Table S5).
4 Discussion
This cross-sectional study examined demographic and personality predictors of kinesiophobia in dialysis patients, as measured by the Tampa Scale for Kinesiophobia Heart (TSK-SV). The mean kinesiophobia score (45.128 ± 7.023) significantly exceeded the clinical threshold of 37 (49), indicating pronounced movement-related fear in this population - a novel finding in dialysis research.
Regression analyses identified advanced age as a significant predictor of elevated kinesiophobia scores across all subscales (fear,avoidance and dysfunction). This association may reflect age-related physiological declines, including: (1) progressive physical impairment (50), (2) compounded exercise limitations from renal comorbidities (51), and (3) heightened health vigilance characteristic of older adults (52). Together, these factors likely contribute to increased activity avoidance and movement apprehension in elderly dialysis patients.
Interestingly, being married was identified as a protective factor against the perception of danger. Married individuals had significantly lower danger scores compared to those with other marital statuses. Higher social support, which married people tend to have, suggests lower risk perception (53). This pattern might help account for the observed link between marital status and reduced fear of movement.
Regular exercise habits were also found to be a protective factor against fear of movement and its subscales. Studies have indicated that dialysis patients without long-term exercise habits are more susceptible to the side effects of dialysis, such as fatigue, hypotension, and muscle cramps. These side effects might be more noticeable during exercise, potentially contributing to higher fear of movement scores (54, 55).
The findings further suggest that certain personality traits significantly influence the fear of movement in dialysis patients. This underscores the need for personality assessments to study factors related to individual vulnerability and resilience in exercise interventions. A personalized psychological framework can enable individualized, progressive treatment plans, helping patients maximize their function and quality of life.
According to the Five Factor Model (56), Extraversion is characterized by assertiveness, sociability, and positive emotionality. Studies in chronic pain patients have found that Extraversion is negatively related to anxious and depressive symptoms, as well as fear-avoidance (57). Consistent with these findings, our study found that higher extraversion was associated with lower fear of movement. Patients with high Extraversion tend to report more optimism and positive attitudes toward their condition, which might correlate with greater adherence to medical advice and understand the positive effects of exercise.
In contrast, high levels of Neuroticism reveal a tendency to experience ambiguous emotions and interpret ordinary situations as threatening, viewing minor setbacks as significant difficulties (56). Previous research has shown a positive relationship between Neuroticism and fear-avoidance (57), supporting our findings that high Neuroticism is significantly associated with higher levels of fear of movement in dialysis patients. These patients tended to report more catastrophic interpretations of physical activity as a threat to kidney health, viewing rehabilitation as hopelessly difficult.
Conscientiousness reflects an individual’s tendency toward self-discipline, diligence, organization, and determination (56). Our results indicated that Conscientiousness was inversely associated with fear of movement. Highly conscientious individuals generally exhibit stronger goal-setting and planning behaviors. A study of peritoneal dialysis patients found that lower Conscientiousness was correlated with higher peritonitis risk (58). It is plausible that dialysis patients with higher Conscientiousness might demonstrate better adherence to collaboratively set health goals and establish structured routines, potentially contributing to more adaptive coping strategies.
Openness to experience encompasses traits such as curiosity, imagination, novelty-seeking, and cognitive flexibility (56). A cross-sectional study in CKD patients reported that Openness was associated with fewer health-related symptoms (59). Similarly, our study found that Openness was negatively associated with fear of movement. Patients with higher Openness scores tended to show greater willingness to consider new perspectives on exercise, which coincided with lower reported fear of movement.
The current results demonstrate significant associations between personality determinants and fear of movement in dialysis patients, suggesting their potential role as obstacles or enablers in multidisciplinary treatment programs. These findings emphasize the clinical value of incorporating personality assessments in pretreatment screening to identify patients with specific trait profiles who may require personalized rehabilitation approaches. While our cross-sectional design shows covariation rather than causation, the observed personality-kinesiophobia relationships tentatively parallel broader temperamental mechanisms described in affective disorders research (60), where non-pathological predispositions influence clinical presentations. This conceptual alignment raises the possibility that shared psychological features (e.g., threat monitoring tendencies and emotion regulation patterns) might underlie both domains, though future studies are needed to investigate whether temperament-informed interventions could be adapted for medically complex populations. The converging evidence highlights the necessity of further research examining personality traits in dialysis patients, particularly regarding their potential to modulate rehabilitation outcomes.
Despite several significant findings, this study has some limitations. The cross-sectional design precludes causal inferences and fails to capture temporal dynamics in the relationship between personality traits and kinesiophobia. Reliance on self-reported measures introduces potential social desirability and recall biases, particularly for sensitive items related to fear expression. Cultural influences on pain-related stoicism may further limit the generalizability of our findings across diverse populations. The absence of physiological markers (e.g., cortisol, heart rate variability) and a healthy control group restricts mechanistic interpretations and normative comparisons. Future research should employ longitudinal designs to establish temporal precedence, integrate multimodal assessments (behavioral tasks, biomarkers) to overcome self-report limitations, conduct cross-cultural validations to disentangle cultural moderators, and develop targeted interventions addressing personality-specific fear mechanisms. These advances would substantially strengthen both theoretical models and clinical applications.
5 Conclusions
Our study identified several significant predictors of kinesiophobia among dialysis patients. Multiple regression analyses revealed that advanced age, lower educational attainment, and lack of local medical insurance were independently associated with elevated kinesiophobia scores. Conversely, marital status and higher levels of extraversion, conscientiousness, openness, and emotional stability served as protective factors. We strongly recommend that nephrology teams incorporate psychological professionals to develop interdisciplinary rehabilitation plans tailored to dialysis patients’ specific personality profiles, particularly for those exhibiting elevated fear of movement.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by The study was approved by the Research Ethics Commission of Naval Medical Center of PLA (protocol code 2022121903). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YZ: Methodology, Writing – original draft. RZ: Software, Writing – review & editing. XM: Validation, Writing – review & editing. LZ: Supervision, Validation, Writing – original draft. ML: Funding acquisition, Validation, Writing – original draft. LL: Project administration, Writing – original draft. YL: Supervision, Writing – original draft. QS: Formal Analysis, Writing – original draft. LD: Investigation, Writing – original draft. TS: Conceptualization, Resources, Visualization, Writing – review & editing. ZG: Conceptualization, Data curation, Writing – review & editing. NL: Conceptualization, Funding acquisition, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by NM.L. of the Excellent talent project of naval medical center of PLA, grant number 21TPZY3201, and the Shanghai Municipal Health Commission Medical and Health General Project, grant number 202240395; This research was funded by MT.L. of the China Postdoctoral Science Foundation Funded Project, grant number 2023M744289, and the Basic Medical Science Project of Naval Military Medical University, grant number 2023QN046.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1574232/full#supplementary-material
References
1. Pedersen BK and Saltin B. Evidence for prescribing exercise as therapy in chronic disease. Scandinavian J Med Sci sports. (2006) 16 Suppl 1:3–63. doi: 10.1111/j.1600-0838.2006.00520.x
2. Sallis RE. Exercise is medicine and physicians need to prescribe it! Br J sports Med. (2009) 43:3–4. doi: 10.1136/bjsm.2008.054825
3. Barcellos FC, Santos IS, Umpierre D, Bohlke M, and Hallal PC. Effects of exercise in the whole spectrum of chronic kidney disease: a systematic review. Clin Kidney J. (2015) 8:753–65. doi: 10.1093/ckj/sfv099
4. Pedersen BK and Saltin B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scandinavian J Med Sci sports. (2015) 25 Suppl 3:1–72. doi: 10.1111/sms.12581
5. Kosmadakis GC, Bevington A, Smith AC, Clapp EL, Viana JL, Bishop NC, et al. Physical exercise in patients with severe kidney disease. Nephron Clin Pract. (2010) 115:c7–c16. doi: 10.1159/000286344
6. Johansen KL and Painter P. Exercise in individuals with CKD. Am J Kidney Dis. (2012) 59:126–34. doi: 10.1053/j.ajkd.2011.10.008
7. Smith AC and Burton JO. Exercise in kidney disease and diabetes: time for action. J Renal Care. (2012) 38 Suppl 1:52–8. doi: 10.1111/j.1755-6686.2012.00279.x
8. Gould DW, Graham-Brown MP, Watson EL, Viana JL, and Smith AC. Physiological benefits of exercise in pre-dialysis chronic kidney disease. Nephrol (Carlton Vic). (2014) 19:519–27. doi: 10.1111/nep.12285
9. Heiwe S and Jacobson SH. Exercise training in adults with CKD: a systematic review and meta-analysis. Am J Kidney Dis. (2014) 64:383–93. doi: 10.1053/j.ajkd.2014.03.020
10. Tentori F, Elder SJ, Thumma J, Pisoni RL, Bommer J, Fissell RB, et al. Physical exercise among participants in the Dialysis Outcomes and Practice Patterns Study (DOPPS): correlates and associated outcomes. Nephrol dialysis Transplant. (2010) 25:3050–62. doi: 10.1093/ndt/gfq138
11. Manfredini F, Mallamaci F, D’Arrigo G, Baggetta R, Bolignano D, Torino C, et al. Exercise in patients on dialysis: A multicenter, randomized clinical trial. J Am Soc Nephrol: JASN. (2017) 28:1259–68. doi: 10.1681/ASN.2016030378
12. Hellberg M, Höglund P, Svensson P, and Clyne N. Randomized controlled trial of exercise in CKD-the RENEXC study. Kidney Int Rep. (2019) 4:963–76. doi: 10.1016/j.ekir.2019.04.001
13. Huang M, Lv A, Wang J, Xu N, Ma G, Zhai Z, et al. Exercise training and outcomes in hemodialysis patients: systematic review and meta-analysis. Am J nephrol. (2019) 50:240–54. doi: 10.1159/000502447
14. Salhab N, Karavetian M, Kooman J, Fiaccadori E, and El Khoury CF. Effects of intradialytic aerobic exercise on hemodialysis patients: a systematic review and meta-analysis. J nephrol. (2019) 32:549–66. doi: 10.1007/s40620-018-00565-z
15. Wilkinson TJ, Watson EL, Gould DW, Xenophontos S, Clarke AL, Vogt BP, et al. Twelve weeks of supervised exercise improves self-reported symptom burden and fatigue in chronic kidney disease: a secondary analysis of the ‘ExTra CKD’ trial. Clin Kidney J. (2019) 12:113–21. doi: 10.1093/ckj/sfy071
16. Bennett PN, Fraser S, Barnard R, Haines T, Ockerby C, Street M, et al. Effects of an intradialytic resistance training programme on physical function: a prospective stepped-wedge randomized controlled trial. Nephrol dialysis Transplant. (2016) 31:1302–9. doi: 10.1093/ndt/gfv416
17. Chan D, Green S, Fiatarone Singh M, Barnard R, and Cheema BS. Development, feasibility, and efficacy of a customized exercise device to deliver intradialytic resistance training in patients with end stage renal disease: Non-randomized controlled crossover trial. Hemodialysis Int Int Symposium Home Hemodialysis. (2016) 20:650–60. doi: 10.1111/hdi.12432
18. Tsuyuki K, Kimura Y, Chiashi K, Matsushita C, Ninomiya K, Choh K, et al. Oxygen uptake efficiency slope as monitoring tool for physical training in chronic hemodialysis patients. Ther apheresis dialysis: Off peer-reviewed J Int Soc Apheresis Japanese Soc Apheresis Japanese Soc Dialysis Ther. (2003) 7:461–7. doi: 10.1046/j.1526-0968.2003.00084.x
19. Toussaint ND, Polkinghorne KR, and Kerr PG. Impact of intradialytic exercise on arterial compliance and B-type natriuretic peptide levels in hemodialysis patients. Hemodialysis Int Int Symposium Home Hemodialysis. (2008) 12:254–63. doi: 10.1111/j.1542-4758.2008.00262.x
20. Vlaeyen JWS, Kole-Snijders AMJ, Boeren RGB, and van Eek H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain. (1995) 62:363–72. doi: 10.1016/0304-3959(94)00279-N
21. Cook AJ, Brawer PA, and Vowles KE. The fear-avoidance model of chronic pain: validation and age analysis using structural equation modeling. Pain. (2006) 121:195–206. doi: 10.1016/j.pain.2005.11.018
22. Zelle DM, Corpeleijn E, Klaassen G, Schutte E, Navis G, and Bakker SJ. Fear of movement and low self-efficacy are important barriers in physical activity after renal transplantation. PloS One. (2016) 11:e0147609. doi: 10.1371/journal.pone.0147609
23. Purnajo I, Beaumont JL, Polinsky M, Alemao E, and Everly MJ. Trajectories of health-related quality of life among renal transplant patients associated with graft failure and symptom distress: Analysis of the BENEFIT and BENEFIT-EXT trials. Am J Transplant. (2020) 20:1650–8. doi: 10.1111/ajt.15757
24. Wang Y, Sang W, Jia G, Qin N, Sun J, Wang D, et al. Causes of high level kinesiophobia in first-episode patients with acute myocardial infarction:a qualitative study. J Nurs Sci. (2022) 37:23–5,37.
25. Back M, Lundberg M, Cider A, Herlitz J, and Jansson B. Relevance of kinesiophobia in relation to changes over time among patients after an acute coronary artery disease event. J Cardiopulmonary Rehabil Prev. (2018) 38:224–30. doi: 10.1097/HCR.0000000000000265
26. Back M, Cider A, Herlitz J, Lundberg M, and Jansson B. The impact on kinesiophobia (fear of movement) by clinical variables for patients with coronary artery disease. Int J Cardiol. (2013) 167:391–7. doi: 10.1016/j.ijcard.2011.12.107
27. Demirci C, Oksul M, Ozer N, and Ozdemir L. Effect of mindfulness on fatigue, kinesiophobia and quality of life in patients with acute myocardial infarction. Ann Clin Analytical Med. (2023) 14:110–5. doi: 10.4328/ACAM.21365
28. Zhu Y, Wang Z, Su T, Fang Z, Pang X, and Tang X. Kinesophobia and its related factors in patients after percutaneous coronary intervention: A cross-sectional study. J Clin Nursing. (2024) 33:4692–707. doi: 10.1111/jocn.17126
29. Back M, Caldenius V, Svensson L, and Lundberg M. Perceptions of kinesiophobia in relation to physical activity and exercise after myocardial infarction: A qualitative study. Phys Ther. (2020) 100:2110–9. doi: 10.1093/ptj/pzaa159
30. Wang Z, Zhang Y, Wang Y, Liu L, and Zhang J. Kinesiophobia and its associated factors in patients with coronary heart disease: a cross-sectional study based on latent feature analysis. BMJ Open. (2023) 13:e072170. doi: 10.1136/bmjopen-2023-072170
31. Knapik A, Dabek J, and Brzek A. Kinesiophobia as a problem in adherence to physical activity recommendations in elderly polish patients with coronary artery disease. Patient Preference Adherence. (2019) 13:2129–35. doi: 10.2147/PPA.S216196
32. Ren P, Zhang Y, Ding L, Tang A, Dong L, Ge Y, et al. The Mediating Effect of Kinesophobia on Self-Efficacy and Exercise adherence in Patients with Acute Myocardial Infarction after PCI. Nurs J Chin People’s Liberation Army. (2022) 39:21–4.
33. Xiao J, Wang R, Xie M, Xia R, and Zhang J. Latent profiles of kinesiophobia and their relationships with physical activity among patients after percutaneous coronary intervention. J Nurs Sci. (2024) 39:42–6,67.
34. Kluszczynska M, Mlynarska A, and Mikulakova W. Influence of frailty syndrome on kinesiophobia according to the gender of patients after coronary artery bypass surgery. Healthcare. (2021) 9:730. doi: 10.3390/healthcare9060730
35. Hasenbring M, Hallner D, and Klasen B. Psychological mechanisms in the transition from acute to chronic pain: over- or underrated? Schmerz (Berlin Germany). (2001) 15:442–7. doi: 10.1007/s004820100030
36. Viniol A, Jegan N, Brugger M, Leonhardt C, Barth J, Baum E, et al. Even worse - risk factors and protective factors for transition from chronic localized low back pain to chronic widespread pain in general practice: A cohort study. Spine. (2015) 40:E890–9. doi: 10.1097/BRS.0000000000000980
37. Nordstoga AL, Nilsen TIL, Vasseljen O, Unsgaard-Tøndel M, and Mork PJ. The influence of multisite pain and psychological comorbidity on prognosis of chronic low back pain: longitudinal data from the Norwegian HUNT Study. BMJ Open. (2017) 7:e015312. doi: 10.1136/bmjopen-2016-015312
38. Westman A, Linton SJ, Ohrvik J, Wahlén P, and Leppert J. Do psychosocial factors predict disability and health at a 3-year follow-up for patients with non-acute musculoskeletal pain? A validation of the Orebro Musculoskeletal Pain Screening Questionnaire. Eur J Pain (London England). (2008) 12:641–9. doi: 10.1016/j.ejpain.2007.10.007
39. Thompson EL, Broadbent J, Bertino MD, and Staiger PK. Do pain-related beliefs influence adherence to multidisciplinary rehabilitation?: A systematic review. Clin J pain. (2016) 32:164–78. doi: 10.1097/AJP.0000000000000235
40. Luque-Suarez A, Martinez-Calderon J, and Falla D. Role of kinesiophobia on pain, disability and quality of life in people suffering from chronic musculoskeletal pain: a systematic review. Br J sports Med. (2019) 53:554–9. doi: 10.1136/bjsports-2017-098673
41. Dersh J, Polatin PB, and Gatchel RJ. Chronic pain and psychopathology: research findings and theoretical considerations. Psychosomatic Med. (2002) 64:773–86. doi: 10.1097/01.psy.0000024232.11538.54
42. Goubert L, Crombez G, and Van Damme S. The role of neuroticism, pain catastrophizing and pain-related fear in vigilance to pain: a structural equations approach. Pain. (2004) 107:234–41. doi: 10.1016/j.pain.2003.11.005
43. Wong WS, Lam HM, Chen PP, Chow YF, Wong S, Lim HS, et al. The fear-avoidance model of chronic pain: assessing the role of neuroticism and negative affect in pain catastrophizing using structural equation modeling. Int J Behav Med. (2015) 22:118–31. doi: 10.1007/s12529-014-9413-7
44. Nijs J, De Meirleir K, and Duquet W. Kinesiophobia in chronic fatigue syndrome: assessment and associations with disability. Arch Phys Med rehabilitation. (2004) 85:1586–92. doi: 10.1016/j.apmr.2003.12.033
45. Koho P, Orenius T, Kautiainen H, Haanpää M, Pohjolainen T, and Hurri H. Association of fear of movement and leisure-time physical activity among patients with chronic pain. J Rehabil Med. (2011) 43:794–9. doi: 10.2340/16501977-0850
46. Gosling SD, Rentfrow PJ, and Swann WB. A very brief measure of the Big-Five personality domains. J Res Personality. (2003) 37:504–28. doi: 10.1016/S0092-6566(03)00046-1
47. Li J. Psychometric properties of ten-item personality inventory in China. Chin J Health Psychol. (2013) 21:1688–92.
48. Lei M, Liu T, Xiong S, Sang M, and Jin C. Chinese translation and validation of the cardiac patients’ Fear of movement scale: reliability and validity assessment. Chin Nurs Management. (2019) 19:1637–42.
49. Brunetti ND, Guerra A, Ieva R, Correale M, Santoro F, Tarantino N, et al. Scared for the scar: fearsome impact of acute cardiovascular disease on perceived kinesiophobia (fear of movement). Clin Cardiol. (2017) 40:480–4. doi: 10.1002/clc.22682
50. Umbleja T, Brown TT, Overton ET, Ribaudo HJ, Schrack JA, Fitch KV, et al. Physical function impairment and frailty in middle-aged people living with human immunodeficiency virus in the REPRIEVE trial ancillary study PREPARE. J Infect Dis. (2020) 222:S52–s62. doi: 10.1093/infdis/jiaa249
51. Sánchez-Tocino ML, González-Parra E, Miranda Serrano B, Gracia-Iguacel C, de-Alba-Peñaranda AM, López-González A, et al. Evaluation of the impact of an intradialytic exercise programme on sarcopaenia in very elderly haemodialysis patients. Clin Kidney J. (2022) 15:1514–23. doi: 10.1093/ckj/sfac046
52. Alkerwi A, Pagny S, Lair ML, Delagardelle C, and Beissel J. Level of unawareness and management of diabetes, hypertension, and dyslipidemia among adults in Luxembourg: findings from ORISCAV-LUX study. PloS One. (2013) 8:e57920. doi: 10.1371/journal.pone.0057920
53. Kim ES, Hawes AM, and Smith J. Perceived neighbourhood social cohesion and myocardial infarction. J Epidemiol Community Health. (2014) 68:1020–6. doi: 10.1136/jech-2014-204009
54. Hu H, Chau PH, and Choi EPH. Physical activity, exercise habits and health-related quality of life in maintenance hemodialysis patients: a multicenter cross-sectional study. J nephrol. (2024) 37:1881–91. doi: 10.1007/s40620-024-01935-6
55. Hu H, Wu C, Chau PH, and Choi EPH. Availability of exercise program, perceived exercise benefits and barriers, and exercise habits in maintenance hemodialysis patients: A multicenter cross-sectional study. J Renal Nutr. (2025). S1051-2276(25):00084–6. doi: 10.1053/j.jrn.2025.03.009
56. Costa PT and McCrae RR. Four ways five factors are basic. Pers Individ Differences. (1992) 13:653–65. doi: 10.1016/0191-8869(92)90236-I
57. Ibrahim ME, Weber K, Courvoisier DS, and Genevay S. Big five personality traits and disabling chronic low back pain: association with fear-avoidance, anxious and depressive moods. J Pain Res. (2020) 13:745–54. doi: 10.2147/JPR.S237522
58. Komatsu S, Hara T, Hiratsuka M, and Yamada Y. Association between conscientiousness and peritoneal dialysis-related peritonitis. Nephrol (Carlton Vic). (2021) 26:999–1006. doi: 10.1111/nep.13952
59. Pugi D, Ferretti F, Galeazzi M, Gualtieri G, Lorenzi L, Pappalardo N, et al. Health-Related Quality of Life in pre-dialysis patients with chronic kidney disease: the role of Big-Five personality traits and illness denial. BMC Psychol. (2022) 10:297. doi: 10.1186/s40359-022-00992-5
Keywords: personality, extraversion, emotional stability, conscientiousness, openness to experience, dialysis
Citation: Zhang Y, Zhang R, Miao X, Li M, Zhang L, Li L, Liu Y, Shao Q, Ding L, Su T, Guo Z and Liu N (2025) Personality traits: an important factor affecting fear of movement in dialysis patients. Front. Psychiatry 16:1574232. doi: 10.3389/fpsyt.2025.1574232
Received: 10 February 2025; Accepted: 07 July 2025;
Published: 30 July 2025.
Edited by:
Domenico De Berardis, ASL 4, ItalyReviewed by:
Francesco Monaco, Azienda Sanitaria Locale Salerno, ItalyFabiola Raffone, Asl Napoli 1 Centro, Italy
Copyright © 2025 Zhang, Zhang, Miao, Li, Zhang, Li, Liu, Shao, Ding, Su, Guo and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nanmei Liu, MTM1ODU5OTYyNzVAMTYzLmNvbQ==; Zhiyong Guo, ZHJndW96aGl5b25nQDE2My5jb20=; Tong Su, c3V0b25nLTIwMDZAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 You Zhang1†
You Zhang1† Ruike Zhang
Ruike Zhang Xiaoyong Miao
Xiaoyong Miao Maoting Li
Maoting Li Lu Li
Lu Li Qing Shao
Qing Shao Tong Su
Tong Su Zhiyong Guo
Zhiyong Guo Nanmei Liu
Nanmei Liu