- 1Children’s Nutrition Research Center, Children’s Hospital of Chongqing Medical University, Chongqing Key Laboratory of Child Neurodevelopment and Cognitive Disorders, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, Chongqing, China
- 2Growth, Development, and Mental Health of Children and Adolescence Center, Children’s Hospital of Chongqing Medical University, Chongqing, China
Background: Social jet lag (SJL) is a form of circadian rhythm misalignment caused by the mismatch between social schedules and biological clocks, which is associated with cognition, behavior, and emotion in children. However, social jet lag among children with autism spectrum disorders (ASD) and its impacts are unknown.
Methods: This cross-sectional study recruited 2-7-year-old children with ASD from special education institutions and outpatient clinics. The Children’s Sleep Habits Questionnaire (CSHQ) assessed children’s sleep. SJL was calculated as |weekend sleep midpoint - weekday sleep midpoint|. Sleep adequacy was determined based on the National Sleep Foundation’s recommendations. Core symptoms were evaluated using the Childhood Autism Rating Scale (CARS), Social Responsiveness Scale (SRS), and Autism Behavior Checklist (ABC). Developmental level was assessed using the Gesell Developmental Scale.
Results: 1) The prevalence of sleep problems was 49.8% and the mean CSHQ total score was 48.04 in ASD. There are significant differences in sleep patterns between weekends and weekdays, characterized by later bedtimes, delayed wake-up times, increased total sleep duration, and reduced prevalence of sleep deficiency during weekends. 2) The 2-3-year-old group had the highest rates of sleep insufficiency (80.77% on weekdays; 82.17% on weekends). There were no significant differences in sleep duration across different age groups, with the median sleep duration ranging from 9.5 to 10 hours. 3) Median SJL in each age group was 0.25 h (2–3 years), 0.5 h (3–4 years), 0.42 h (4–5 years), and 0.5 h (≥5 years), respectively. In children aged 2–3 years, SJL was significantly positively correlated with core symptoms 4) SJL was observed to be weakly associated with developmental level of personal-social only in the ≥ 3-year-old group (r = 0.100, P = 0.042).
Conclusion: Our study found for the first time a correlation between SJL and core symptoms in 2-3-year-old children with ASD. This finding suggests that SJL may have a potentially negative impact on core symptoms in ASD. Therefore, it is crucial to emphasize the importance of regular routines for ASD, especially in younger children.
1 Introduction
Autism Spectrum Disorder (ASD) is a neurodevelopmental condition characterized by social communication deficits, restricted interests, and repetitive behaviors (1). Sleep disturbances, including delayed sleep onset, frequent nighttime awakenings, and circadian rhythm disruptions, are prevalent in ASD (2). There are two main mechanisms for sleep regulation: the biological clock (also known as circadian rhythm) and sleep homeostasis (3). Biological clock is located in the suprachiasmatic nucleus (SCN) of hypothalamus, which is the master clock that regulates life’s activities (4). Internal clock has to be synchronized with the rhythms of the external environment, and this is accomplished through light (5). There are social activities in human society, including work, study, etc., so individuals also need synchronize the internal biological clock with social activities. When they are not synchronized, social jet lag (SJL) occurs (6).
Social jet lag is an easily overlooked manifestation of circadian rhythm disorders, usually reflected in differences in sleep patterns between weekdays and weekends (SJL = |weekend sleep midpoint - weekday sleep midpoint|) (6). SJL affects mental and physical health, including metabolism, cardiovascular health, sleep, anxiety and depression (7–14). However, most of the relevant studies have been conducted in adults and adolescents, with fewer in children, especially in ASD. A large multicenter survey of preschool children in China showed that longer SJL was positively associated with children’s emotional and behavioral problems (15). In children with attention deficit and hyperactivity disorder (ADHD), SJL was positively correlated with their cognitive abilities and core symptoms (16). In ASD, a study that included 171 individuals aged 5–21 years investigated the correlation of SJL with age and sleep, but no further reports of SJL with core symptoms (17). Autistic children may experience more severe SJL-related consequences due to their inherent clinical characteristics, such as social impairments and difficulties in adapting to the environment. Currently, there is a limited number of reports on social jet lag in children with ASD, and the associations with the core symptoms have not yet been clarified, so related studies are needed.
This study has the following main objectives: 1) investigate the sleep patterns of children with ASD during weekdays and weekends, 2) examine the sleep patterns and the characteristics of social jet lag in children with ASD of different ages, 3) explore the correlation between social jet lag and the core symptoms, and developmental level of ASD. We hope that our study will enable more researchers to understand the characteristics the possible negative effects of social jet lag in children with ASD, and provide parents and clinicians with practical guidance suggestions to promote the establishment of a regular routine.
2 Methods
2.1 Participants
This cross-sectional study enrolled autistic children from Chongqing, China. Inclusion criteria: 1) 2–7 years old; 2) DSM-5-confirmed ASD diagnosis by developmental -behavioral pediatricians; 3) informed consent from caregivers. Exclusion criteria: 1) suffering from other serious diseases; 2) non-completion of questionnaires.
The study was approved by the Ethics Committee of Children’s Hospital of Chongqing Medical University (No. 121-1/2018) and registered at the Chinese Clinical Trial Registry (ChiCTR2000031194).
2.2 Clinical assessments
2.2.1 Sleep conditions
The Children’s Sleep Habits Questionnaire (CSHQ) was used to assess children’s sleep and consisted of 33 scored entries as well as a survey of bedtime and wake up time (18). Recent studies have suggested that using the original score of 41 to define sleep problems may be overestimated and that using a score of 48 may be more reasonable (19–21), so we used this as the cutoff in subsequent analyses. Sleep patterns were obtained from parents answering the following questions: bedtime and wake up time on weekdays/weekends. Sleep duration is the interval between bedtime and wake-up time. Sleep midpoint = wake up time - (sleep duration/2). SJL = |weekend sleep midpoint − weekday sleep midpoint| (22). Adequacy of sleep is determined based on the American Sleep Foundation’s recommended hours of sleep, which are 11–14 hours for toddlers, 10 hours for ages 3-6, and 9 hours for ages 6-14 (23).
2.2.2 Core symptoms
Core symptoms in children with ASD were assessed using the Childhood Autism Rating Scale (CARS), Social Responsiveness Scale (SRS), and Autism Behavior Checklist (ABC). The CARS is a 15-item scale that assesses the severity of autism (24). The SRS contains 65 items assessing the dimensions of social awareness, social cognition, social communication, social motivation, and autistic mannerisms, with a total score range of 0-195 (25). The ABC scale contains 57 items assessing 5 dimensions: sensory, relating, body and object use, language, and social and self-help, with a total score range of 0-158 (26).
2.2.3 Developmental level
The developmental level was assessed using the Gesell Developmental Scale (GDS), consisting of adaptive behavior, gross motor, fine motor, language, and personal-social (27). Total developmental quotient (DQ) is the mean of the five dimensions.
2.3 Statistical analysis
Data were analyzed using SPSS 25.0. Continuous variables were expressed as mean ± standard deviation (M ± SD) or Median (25th percentile to 75th percentile) [M (P25-P75)], group comparisons using one-way Analysis of Variance (ANOVA) or Kruskal-Wallis tests. Categorical variables were expressed as frequencies (percentages) [N (%)], group comparisons using chi-square tests. Paired t-tests, Wilcoxon signed-rank tests, and McNemar’s tests were employed for intra-group comparisons, with selection criteria based on data characteristics. Bonferroni correction was applied for multiple comparisons. Correlation analyses were performed based on data distribution. Pearson’s correlation coefficient was applied to variables meeting normality assumptions, while Spearman’s rank-order correlation was employed for non-normally distributed variables. Statistical significance was set at P < 0.05.
3 Results
3.1 Study population
A total of 701 children with ASD were included in this study, and 36 children were excluded because their questionnaires contained missing items (e.g., filled in the time of going to sleep, missing the time of waking up; filled in the sleep situation on weekdays, missing the weekend). Finally, 545 boys and 121 girls were included in this study, with an age distribution of 3.82 (3.13,4.61) years. The prevalence of sleep problems was 49.8% and the mean CSHQ total score was 48.04.
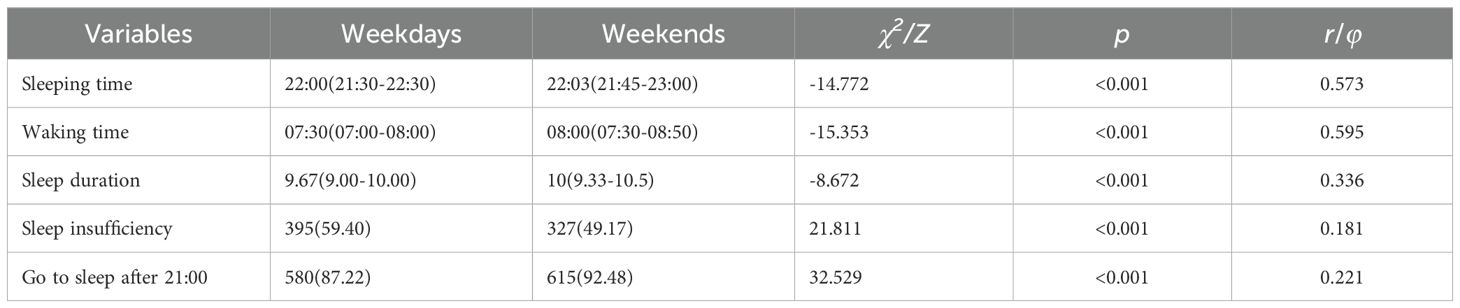
3.2 Sleep patterns during weekdays and weekends in children with ASD
As shown in Table 1, there were significant differences in the sleep patterns of children with ASD between weekdays and weekends. More children slept later, got up later, slept more hours, and had lower rates of sleep insufficiency on weekends than on weekdays (P < 0.05), suggesting that weekend routines may have compensated for weekday sleep insufficiency. Both the World Sleep Association and the National Health Commission of China recommend that children should go to bed before 21:00. In this survey, the percentage of autistic children went to bed after 21:00 on weekdays was 87.22%, which further increased to 92.48% on weekends (P < 0.05).
3.3 Comparison of sleep patterns and social jet lag in children with ASD in different age groups
As shown in Table 2, children in the ≥5 years group slept the earliest during weekdays and weekends compared to the other age groups, [21:30 (21:00, 22:07), P < 0.05] on weekdays and [22:00 (21:30, 22:30), P < 0.05] on weekends, but still 81.5% and 90.7% of them went to sleep after 21:00. It can be seen that the children with ASD had a higher incidence of late sleep in this investigation.
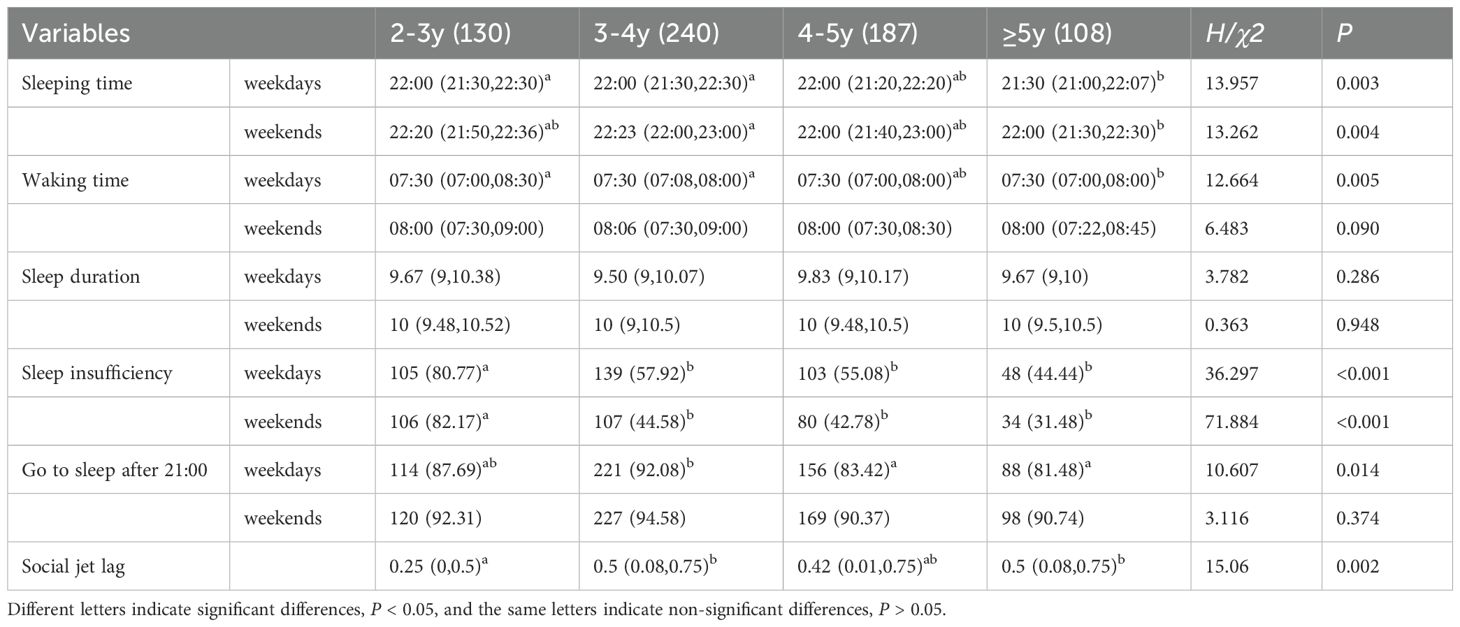
Table 2. Comparison of sleep patterns and social jet lag in children with ASD at different age groups.
Sleep insufficiency tended to decrease in older age groups, and was significantly higher in the 2-3-year-old group (P < 0.05), 80.77% on weekdays and 82.17% on weekends, compared to 44.44%-57.92% (weekdays) and 31.48%-44.58% (weekends) in other age groups. There was no difference in sleep duration between the groups, but the fact is that the younger the age, the more sleep is needed. According to the recommendations of the American Sleep Foundation, the recommended hours of sleep for children aged 2–3 years should be more than 11 hours, but here the P75 for sleep duration is 10.38 hours on weekdays and 10.52 hours on weekends.
The median of SJL was 0.5 h, 0.42 h, and 0.5 h for the 3-4, 4-5, and ≥5 year old groups, respectively, which were not significantly different from each other. The 2-3-year-old group had the shortest SJL of 0.25 (0, 0.5) h, which was significantly lower than that in 3–4 and ≥5 year old age groups (P < 0.05).
3.4 Correlations between social jet lag and core symptoms in children with ASD in different age groups
Since the social jet lag among the 3-4, 4-5, and ≥5-year-old groups was similar and showed no significant differences, we merged them into a single group. The association between SJL and core symptoms was assessed using Spearman’s rank-order correlation analysis. As shown in Table 3 below, in the 2-3-year-old group, SJL was positively correlated with the following scores: ABC relating (r = 0.178, P = 0.050), ABC language (r = 0.297, P = 0.001), ABC total score (r = 0.178, P = 0.050), SRS communication (r = 0.163, P = 0.065), SRS motivation (r = 0.181, P = 0.039), SRS autistic mannerisms (r = 0.215, P = 0.014), and SRS total score (r = 0.208, P = 0.018). In the ≥3 year old group, no correlation was found between SJL and core symptom scores.
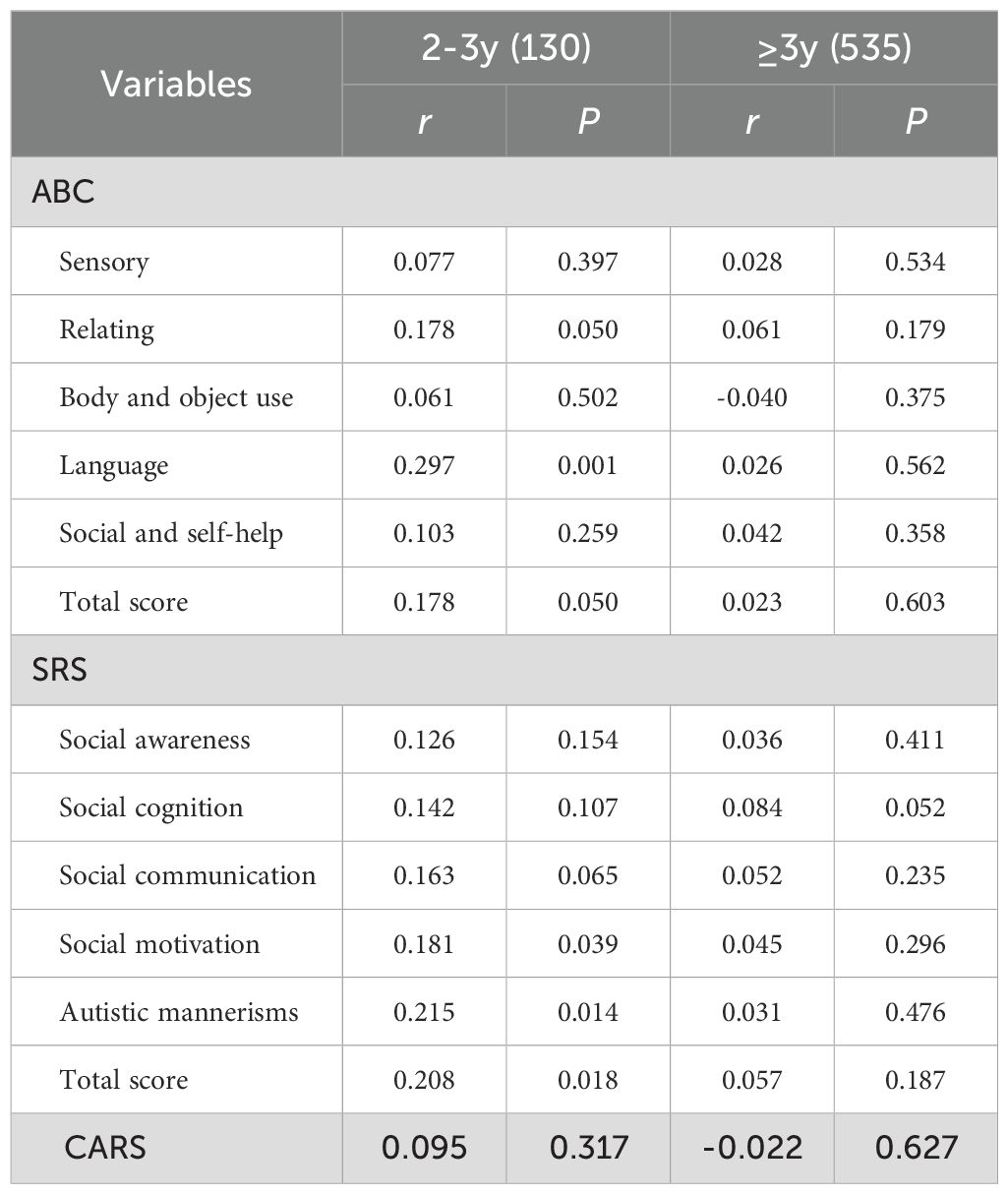
Table 3. Correlation between social jet lag and core symptoms in children with ASD at different age groups.
3.5 Correlations between social jet lag and developmental level in children with ASD in different age groups
The association between SJL and developmental level was assessed using Spearman’s rank-order correlation analysis. In Table 4, the ≥ 3-year-old group, the correlation between developmental level of personal-social and SJL was extremely weak (r = 0.100, P = 0.042) and can be considered irrelevant. Overall, no correlation between developmental level and social jet lag was found.

Table 4. Correlation between social jet lag and developmental level in children with ASD at different age groups.
4 Discussion
In this study, the median of bedtime for children with ASD by age ranged from 21:30 to 22:23, waking up time from 7:30 to 8:06, and sleep duration from 9.5 to 10 hours. This is generally consistent with previous reports. Zou’s (28) study showed that autistic children under 6 years old went to sleep at 22:30 on weekdays and 23:00 on weekends, woke up at 7:30 and 8:00, respectively, and slept for about 10 h. Among children aged 3–5 years with ASD, Li’s (29) survey showed that their average sleep duration on weekdays and weekends was 9.74 h and 9.99 h, respectively, and Iwamoto (30) reported a bedtime of 21:45 and a wake-up time of 7:25, with an average sleep duration of 8.85 h. In Anders’ (31) study, children with ASD aged 2-5.5 years went to bed at 21:00 and slept for approximately 10 h. Due to variations in sample sizes, survey instruments used, and cultural regions, the results of the surveys varied slightly.
Our study indicates that children with ASD exhibit significant differences in sleep patterns between weekends and weekdays, characterized by later bedtimes, delayed wake-up times, increased total sleep duration, and reduced prevalence of sleep deficiency during weekends. This may be associated with more relaxed schedules on weekends. Parents often grant children greater autonomy in time management, resulting in delayed sleep timing. However, while such compensatory sleep behavior partially alleviates weekday sleep deprivation, it may also induce circadian rhythm disruption and other adverse effects, potentially compromising overall sleep quality (32, 33). Several domestic and international guidelines recommend that children should be in bed before 21:00 (34, 35). However, our survey reveals that 81.48%-92.08% of ASD children across different age groups go to bed after 21:00 on weekdays, with this proportion further increasing to 90.37%-94.58% on weekends. These findings demonstrate that delayed bedtime is prevalent among ASD children of all ages. Future interventions should emphasize cultivating regular sleep-wake routines, including promoting early bedtimes, trying to follow consistent bedtime and wake-up times on weekdays and weekends, and so on.
In different age groups exhibit distinct characteristics in terms of sleep patterns and social jet lag, especially in the 2-3-year-old group. The prevalence of insufficient sleep is most severe in the 2-3-year-old group (80%), whereas it ranges from 31% to 58% in the other three older age groups. According to the recommendations of the National Sleep Foundation (34), children aged 2–3 years should have a sleep duration of more than 11 hours. However, the results of this survey show that the P75 sleep duration is 10.38 hours on weekdays and 10.52 hours on weekends. In addition, although the SJL in the 2-3-year-old group is the shortest compared with other age groups, its negative impact on core symptoms is the greatest, especially in terms of language and communication, indicating that younger ASD children are more sensitive to changes in daily routines. This may be related to the physiological and psychological developmental characteristics of this age group. Nervous system develops rapidly before the age of 3 (36). The Lancet has also emphasized the importance of development before the age of 3 in its series of articles on early child development (37–39). The period from conception to 3 years old is the time when children are most vulnerable to adverse exposures and when interventions are most beneficial. The latest Guidelines on Early Infant and Toddler Development Services issued by our Health Commission 2025 expresses a similar viewpoint, clearly stating that the period before the age of 3 is a critical period for children’s growth and development.
This is the first time we have reported the association between SJL and core symptoms in children with ASD aged 2–7 years. In a study involving 171 children with ASD aged 5–21 years, the overall SJL was 0.72 hours and was positively correlated with age, but the authors did not explore the relationship between social jet lag and core symptoms (17). Compared to this study, we had a larger sample size and investigated SJL in different age subgroups. In addition, we investigated the association between SJL and core symptoms and developmental levels in ASD, revealing its potential significance in this population. In a multicenter survey in China (40), longer SJL was associated with poorer psychological health in children and adolescents. Another study in preschool showed SJL was positively correlated with overall emotional and behavioral problems (15). In ADHD, SJL is considered an important predictor of ADHD symptoms (41). These studies reveal the important role of SJL in children’s emotion, behavior and so on from different populations, and indirectly support our research conclusions.
In the group of autistic children aged ≥3 years, the SJL is higher than that in the 2-3-year-old group. However, no correlation between SJL and core symptoms has been found yet. This may be related to the fact that more children with ASD receive behavioral interventions or enter kindergarten after the age of 3 (42). On one hand, fixed intervention programs and kindergarten routines can help children with ASD establish regular daily routines on weekdays. However, the more relaxed family environment on weekends leads to an increase in SJL. On the other hand, behavioral interventions may to some extent mitigate the negative impact of SJL on core symptoms. In addition, as the circadian rhythm regulation ability of older children is enhanced, their resistance to external disturbances may also be improved. However, this does not mean that sleep problems and circadian rhythm disorders in older children can be ignored.
Another noteworthy point is that the majority of autistic children in all age groups go to bed after 21:00, but in ≥5-year-old group the bedtime is the earliest. This indicates that late bedtime is not only caused by irregular daily routines, but may also be related to some physiological characteristics of ASD, involving deeper-level mechanism discussions, such as melatonin. It requires further research.
Based on the results of this study, we propose the following recommendations: 1) Families, institutions, and kindergartens should enhance communication to cultivate regular daily routines in children with ASD. 2) Children’s daily routines are closely related to parental sleep habits and parenting styles. Therefore, parents should be aware of their important role in shaping children’s sleep habits. On the one hand, parents should set a positive example for their children by adjusting their own sleep behavior; on the other hand, they need to create a good sleep environment for their children, set a reasonable sleep schedule and supervise the implementation. 3) For children with ASD aged 2–3 years, special attention should be paid to inconsistencies between weekday and weekend routines to alleviate the negative impacts of irregular sleep patterns.
Several limitations of this study should be noted. First, subjective questionnaire was used to survey the bedtime and wake-up time. In future studies, we plan to incorporate actigraphy to objectively assess children’s sleep patterns and expand data collection to include parental sleep profiles. Moreover, this study only preliminarily explored the social jet lag in children with ASD and its association with core symptoms. Further research is needed to comprehensively investigate the role of SJL in autism from multiple dimensions. For instance, functional magnetic resonance imaging (fMRI) could be employed to characterize the relationship between SJL and functional connectivity within social brain networks, as well as to explore the interaction between SJL and genes in children with ASD.
5 Conclusion
Our study found for the first time a correlation between SJL and core symptoms in 2-3-year-old children with ASD. This finding suggests that SJL may have a potentially negative impact on core symptoms in ASD. Therefore, it is crucial to emphasize the importance of regular routines for ASD, especially in younger children.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the ethics committee of the Children’s Hospital of Chongqing Medical University and registered in the Chinese Clinical Trial Registry. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
HC: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing. TY: Data curation, Methodology, Project administration, Supervision, Writing – review & editing. JC: Data curation, Project administration, Supervision, Writing – review & editing. YD: Supervision, Writing – review & editing. XX: Investigation, Writing – review & editing. QW: Investigation, Writing – review & editing. QM: Investigation, Writing – review & editing. BY: Investigation, Writing – review & editing. BH: Investigation, Writing – review & editing. DZ: Investigation, Writing – review & editing. DA: Investigation, Writing – review & editing. TL: Funding acquisition, Methodology, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This survey was supported by the National Natural Science Foundation of China (No. 81771223, 82372559, 82304119), and Chief Medical Expert Studio of Chongqing (No.YWBF[2018]263).
Acknowledgments
We would like to thank the families and children who contributed to this study. Thanks to the researchers who participated in the survey. It is because of your joint participation that we are able to work better on research related to children with autism spectrum disorders.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1574814/full#supplementary-material
References
1. Lord C, Elsabbagh M, Baird G, and Veenstra-Vanderweele J. Autism spectrum disorder. Lancet. (2018) 392:508–20. doi: 10.1016/S0140-6736(18)31129-2
2. Hirota T and King BH. Autism spectrum disorder: A review. JAMA. (2023) 329:157–68. doi: 10.1001/jama.2022.23661
3. Franken P and Dijk DJ. Sleep and circadian rhythmicity as entangled processes serving homeostasis. Nat Rev Neurosci. (2024) 25:43–59. doi: 10.1038/s41583-023-00764-z
4. Cable J, Schernhammer E, Hanlon EC, Vetter C, Cedernaes J, Makarem N, et al. Sleep and circadian rhythms: pillars of health-a Keystone Symposia report. Ann N Y Acad Sci. (2021) 1506:18–34. doi: 10.1111/nyas.14661
5. Daruwalla A, Choi EH, Palczewski K, and Kiser PD. Structural biology of 11-cis-retinaldehyde production in the classical visual cycle. Biochem J. (2018) 475:3171–88. doi: 10.1042/BCJ20180193
6. Wittmann M, Dinich J, Merrow M, and Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiol Int. (2006) 23:497–509. doi: 10.1080/07420520500545979
7. Komada Y, Breugelmans R, Drake CL, Nakajima S, Tamura N, Tanaka H, et al. Social jetlag affects subjective daytime sleepiness in school-aged children and adolescents: A study using the Japanese version of the Pediatric Daytime Sleepiness Scale (PDSS-J). Chronobiol Int. (2016) 33:1311–9. doi: 10.1080/07420528.2016.1213739
8. Kolomeichuk SN, Randler C, Morozov AV, Gubin DG, and Drake CL. Social jetlag and excessive daytime sleepiness from a sample of Russian children and adolescents. Nat Sci Sleep. (2021) 13:729–37. doi: 10.2147/NSS.S290895
9. Xu YX, Li J, Wan YH, Su PY, Tao FB, and Sun Y. Association between behavioral jet lag with subjective and objective circadian rhythm among Chinese young adults. Soc Sci Med. (2025) 366:117689. doi: 10.1016/j.socscimed.2025.117689
10. Duarte A, Martins S, Augusto C, Silva MJ, Lopes L, Santos R, et al. Associations between sleep opportunity, sleep problems, and social jetlag and toddlers' adiposity: A cross-sectional study. Sleep Med. (2025) 126:172–7. doi: 10.1016/j.sleep.2024.12.006
11. Lin MY, Kang YN, Apriliyasari RW, and Tsai PS. Association between social jetlag and components of metabolic syndrome: A systematic review and meta-analysis. J Nurs Res. (2024) 32:e354. doi: 10.1097/jnr.0000000000000628
12. Pompeia S, Panjeh S, Louzada FM, D'Almeida V, Hipolide DC, and Cogo-Moreira H. Social jetlag is associated with adverse cardiometabolic latent traits in early adolescence: an observational study. Front Endocrinol (Lausanne). (2023) 14:1085302. doi: 10.3389/fendo.2023.1085302
13. Baek SU, Lee YM, Won JU, and Yoon JH. Association between social jetlag and anxiety symptoms: Findings from a nationally representative sample of the Korean working population. Sleep Med. (2025) 126:300–6. doi: 10.1016/j.sleep.2024.12.029
14. Jung SM and Lee MR. Analyzing the effect of sleep duration, chronotype, and social jet lag on anxiety disorders and health-related quality of life: A cross-sectional study. PloS One. (2024) 19:e0314187. doi: 10.1371/journal.pone.0314187
15. Chao Y, Wang Y, Yang J, Guo K, Ma K, Ding P, et al. Associations of social jetlag and emotional and behavioral problems among Chinese preschoolers. Chronobiol Int. (2022) 39:1110–7. doi: 10.1080/07420528.2022.2071157
16. Qu X, Kalb LG, Holingue C, Rojo-Wissar DM, Pritchard AE, Spira APE, et al. Association of time in bed, social jetlag, and sleep disturbances with cognitive performance in children with ADHD. J Atten Disord. (2024) 28:99–108. doi: 10.1177/10870547231204010
17. Taylor BJ, Pedersen KA, Mazefsky CA, Lamy MA, Reynolds CF, Strathmann WR, et al. From alert child to sleepy adolescent: age trends in chronotype, social jetlag, and sleep problems in youth with autism. J Autism Dev Disord. (2024) 54:4529–39. doi: 10.1007/s10803-023-06187-0
18. Owens JA, Spirito A, and McGuinn M. The Children's Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. (2000) 23:1043–51. doi: 10.1093/sleep/23.8.1d
19. Reynolds AM, Soke GN, Sabourin KR, Hepburn S, Katz T, Wiggins LD, et al. Sleep problems in 2- to 5-year-olds with autism spectrum disorder and other developmental delays. Pediatrics. (2019) 143:e20180492. doi: 10.1542/peds.2018-0492
20. Ishii R, Obara H, Nagamitsu S, Matsuoka M, Suda M, Yuge K, et al. The Japanese version of the children's sleep habits questionnaire (CSHQ-J): A validation study and influencing factors. Brain Dev. (2022) 44:595–604. doi: 10.1016/j.braindev.2022.06.003
21. Deng Y, Zhang Z, Gui Y, Li W, Rong T, Jiang Y, et al. Sleep disturbances and emotional and behavioral difficulties among preschool-aged children. JAMA Netw Open. (2023) 6:e2347623. doi: 10.1001/jamanetworkopen.2023.47623
22. Barragán R, Fernández-Carrión R, Asensio-Márquez EM, Ortega-Azorín C, Álvarez-Sala A, Pérez-Fidalgo A, et al. Timing of meals and sleep in the mediterranean population: the effect of taste, genetics, environmental determinants, and interactions on obesity phenotypes. Nutrients. (2023) 15:708. doi: 10.3390/nu15030708
23. Paruthi S, Brooks LJ, D'Ambrosio C, Hall WA, Kotagal S, Lloyd RM, et al. Consensus statement of the american academy of sleep medicine on the recommended amount of sleep for healthy children: methodology and discussion. J Clin Sleep Med. (2016) 12:1549–61. doi: 10.5664/jcsm.6288
24. Garfin DG, McCallon D, and Cox R. Validity and reliability of the Childhood Autism Rating Scale with autistic adolescents. J Autism Dev Disord. (1988) 18:367–78. doi: 10.1007/BF02212193
25. Cen CQ, Liang YY, Chen QR, Chen KY, Deng HZ, Chen BY, et al. Investigating the validation of the Chinese Mandarin version of the Social Responsiveness Scale in a Mainland China child population. BMC Psychiatry. (2017) 17:51. doi: 10.1186/s12888-016-1185-y
26. Rellini E, Tortolani D, Trillo S, Carbone S, and Montecchi F. Childhood Autism Rating Scale (CARS) and Autism Behavior Checklist (ABC) correspondence and conflicts with DSM-IV criteria in diagnosis of autism. J Autism Dev Disord. (2004) 34:703–8. doi: 10.1007/s10803-004-5290-2
27. Wilson MG. Gesell developmental testing. J Pediatr. (1963) 62:162–4. doi: 10.1016/s0022-3476(63)80093-1
28. Hu JM, Liu XH, Deng HZ, Chen KY, and Zou XB. Investigation of sleep quality in children with autism spectrum disorder. J New Med. (2017) 48:99–103. doi: 10.3969/j.issn.0253-9802.2017.02.007
29. Li SY, Jin Y, Jing J, Huang LJ, and Zhou JX. Sleep behaviors in children with autism spectrum disorders. Chin Ment Health J. (2012) 26:471–5. doi: 10.3969/j.issn.1000-6729.2012.06.015
30. Iwamoto BK, Neece CL, Nair A, Rockwood NJ, Fenning RM, Krantz ML, et al. Exploring bidirectional relationships: child sleep duration, child behavior problems, and parenting stress in families of children with autism spectrum disorder. Res Autism Spectr Disord. (2023) 106:102197. doi: 10.1016/j.rasd
31. Anders T, Iosif AM, Schwichtenberg AJ, Tang K, and Goodlin-Jones B. Sleep and daytime functioning: a short-term longitudinal study of three preschool-age comparison groups. Am J Intellect Dev Disabil. (2012) 117:275–90. doi: 10.1352/1944-7558-117.4.275
32. Depner CM, Melanson EL, Eckel RH, Snell-Bergeon JK, Perreault L, Bergman BC, et al. Ad libitum Weekend Recovery Sleep Fails to Prevent Metabolic Dysregulation during a Repeating Pattern of Insufficient Sleep and Weekend Recovery Sleep. Curr Biol. (2019) 29:957–967.e4. doi: 10.1016/j.cub.2019.01.069
33. Wang X, Xu Y, Li X, Mansuri A, McCall WV, Liu Y, et al. Day-to-day deviations in sleep parameters and biological aging: Findings from the NHANES 2011-2014. Sleep Health. (2023) 9:940–6. doi: 10.1016/j.sleh
34. Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep Foundation's sleep time duration recommendations: methodology and results summary. Sleep Health. (2015) 1:40–3. doi: 10.1016/j.sleh.2014.12.010
35. Paruthi S, Brooks LJ, D'Ambrosio C, Hal WA, Kotagal S, Lloyd R, et al. Recommended amount of sleep for pediatric populations: A consensus statement of the american academy of sleep medicine. J Clin Sleep Med. (2016) 12:785–6. doi: 10.5664/jcsm.5866
36. Brown TT and Jernigan TL. Brain development during the preschool years. Neuropsychol Rev. (2012) 22:313–33. doi: 10.1007/s11065-012-9214-1
37. Black MM, Walker SP, Fernald LCH, Andersen CT, DiGirolamo AM, Lu C, et al. Early childhood development coming of age: science through the life course. Lancet. (2017) 389:77–90. doi: 10.1016/S0140-6736(16)31389-7
38. Richter LM, Daelmans B, Lombardi J, Heymann J, Boo FL, Behrman JR, et al. Investing in the foundation of sustainable development: pathways to scale up for early childhood development. Lancet. (2017) 389:103–18. doi: 10.1016/S0140-6736(16)31698-1
39. Lake A and Chan M. Putting science into practice for early child development. Lancet. (2015) 385:1816–7. doi: 10.1016/S0140-6736(14)61680-9
40. Li T, Liu X, Cao C, Yang F, Ding P, Xu S, et al. Association between screen time, homework and reading duration, sleep duration, social jetlag and mental health among Chinese children and adolescents. BMC Psychiatry. (2024) 24:781. doi: 10.1186/s12888-024-06233-w
41. McGowan NM, Voinescu BI, and Coogan AN. Sleep quality, chronotype and social jetlag differentially associate with symptoms of attention deficit hyperactivity disorder in adults. Chronobiol Int. (2016) 33:1433–43. doi: 10.1080/07420528.2016.1208214
Keywords: autism spectrum disorder, social jet lag, sleep patterns, core symptoms, circadian rhythm
Citation: Chen H, Yang T, Chen J, Ding Y, Xiang X, Wei Q, Mou Q, Yuan B, Hu B, Zhang D, Ai D and Li T (2025) Social jet lag is associated with core symptoms in 2-3-year-old children with autism spectrum disorders. Front. Psychiatry 16:1574814. doi: 10.3389/fpsyt.2025.1574814
Received: 11 February 2025; Accepted: 28 April 2025;
Published: 16 May 2025.
Edited by:
Magdalena Budisteanu, Prof. Dr. Alexandru Obregia Psychiatry Hospital, RomaniaReviewed by:
Jinchen Li, Central South University, ChinaSergio Serrada-Tejeda, Rey Juan Carlos University, Spain
Copyright © 2025 Chen, Yang, Chen, Ding, Xiang, Wei, Mou, Yuan, Hu, Zhang, Ai and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tingyu Li, dHlsaUB2aXAuc2luYS5jb20=
 Hongyu Chen1
Hongyu Chen1 Ting Yang
Ting Yang Yuan Ding
Yuan Ding Tingyu Li
Tingyu Li