- Center for Music Research, Florida State University, Tallahassee, FL, United States
Introduction: Complexities such as TBI and co-occurring conditions such as homelessness impact Veterans’ awareness and use of health care services offered in the VHA and the community. Thus, targeted interventions that engage and reduce barriers to care among Veterans with interconnected challenges are needed. Research has suggested that music therapy interventions are well received by both active-duty Service Members and Veterans, but little is available on music therapy-based programming to address the complex needs of Veterans with interconnected challenges.
Methods: The purpose of this project was to conduct a programmatic evaluation of a music therapist-led, community-based music program offered in a supportive housing complex to foster mental, emotional, and social health and wellbeing in Veterans encountering long-term and repeated homelessness, TBI, and other co-occurring conditions. We reviewed music therapist notes, attendance logs, participant demographic data, and unsolicited feedback from a 45-session music program grounded in a whole health and trauma-informed perspective to (a) identify the music interventions used and (b) explore how Veterans perceived the program. Demographic and attendance data were analyzed descriptively, and therapist notes and unsolicited feedback were examined thematically.
Results: Results showed Veterans preferred rock, country, blues, and folk music, and singing and instrument play were the most common music strategies implemented in the program. Session topics most often included music, recreation/leisure, and emotions. The most common therapist objectives included self-expression, building rapport, and group cohesion. Both therapist notes and Veteran comments suggested that the program was appreciated, and it created a space where challenges could be addressed.
Conclusion: This is one of the first music therapy programs presented in the literature to focus on Veterans experiencing homelessness and living in supportive housing. Results suggest that music therapy programming may be an innovative, well received option to engage Veterans with interconnected challenges. Results further suggest that sessions offered directly in supportive housing units and collaborating with Veterans on music planning may build trust and connection and empower them to take charge of their own health and wellbeing. Thus, music therapy-based programming may be uniquely positioned to address the needs of this marginalized population.
1 Background
The transition from active-duty military service to Veteran status is often a complex process not only for the Service Member, but for their family and support system as well. Stressors induced and exasperated by military service can place Veterans and their families at an increased risk for chronic health issues, often at a higher rate than their civilian counterparts (1). To address U.S. Veterans’ health and wellbeing needs, the Veterans Health Administration (VHA) provides medical care and social support services like readjustment counseling and outreach services for veterans (2). However, Veterans who use VHA services are a clinically complex group, and they can experience barriers to care (3). This is especially true for Veterans with interconnected challenges such as traumatic brain injuries (TBI) and co-occurring conditions like mental health conditions, substance use disorder, physical health conditions like pain, and social and transition issues like inadequate social support and homelessness (4). (Note: In alignment with language used by the U.S. Department of Veterans Affairs, the term ‘homeless’ is used throughout.)
To better address the complex needs of Veterans, the VHA has taken a whole health approach, moving away from a singular focus on disease-oriented care and empowering and equipping individuals to take charge of their health and wellbeing (5). As part of the whole health approach, the VHA now focuses on the full continuum of care, integrating non-clinical, wellbeing-oriented, and clinical services. Moreover, as Veterans have sought holistic and complementary treatment methods (6), the VHA has broadened its range of services to include evidence-based complementary/integrative approaches (7, 8).
Music therapy, an evidence-based integrative approach, has been recognized for its impact on military personnel across the clinic to community continuum (9). Music therapy services are currently offered across the VHA in group and individual format (10), both in person and via telehealth (11). Music therapy services for Veterans are provided to individuals with clinical, non-clinical, and wellbeing needs in a variety of settings including Veterans Affairs (VA) hospitals/clinics, VA Domiciliaries (12), permanent supportive housing, and VA living centers (13). Both active and receptive interventions like drumming (active) and song writing (receptive) have been used to improve functional outcomes (14), reduce stress and trauma (15), reduce isolation and increase socialization (16, 17), and promote community reintegration (15). Research has suggested that music therapy interventions are well received by both active-duty Service Members and Veterans (10), and there is emerging support for music-based interventions with Veterans with complex and interconnected needs (12). However, more research is needed to better understand how music therapy can support Veterans with interconnected challenges like mental health conditions, physical conditions, and homelessness.
The purpose of this project was to conduct a program evaluation of a music therapist-led, community-based music program offered in a supportive housing complex, designed to support and foster mental, emotional, and social health and wellbeing in Veterans encountering long-term and repeated homelessness, mental illness, and/or other health or transition issues. Our aim was to (a) identify the music interventions used in the program and (b) explore how Veterans perceived the music therapy interventions. To identify program characteristics, we explored the following questions as we evaluated the program:
● What types of Veterans were served in a music therapist-led, community-based music program?
● What music therapy informed interventions were used with Veterans who participated in a music therapist-led, community-based music program?
● Did Veteran participants prefer specific types of music, music interventions, or other elements implemented during the music therapist-led, community-based music program?
● What objectives were commonly addressed during the music therapist-led, community-based music program?
To explore the Veterans’ perceptions, we asked the following questions as we evaluated the program:
● How did Veterans perceive the music therapist-led, community-based music program?
● How did Veterans perceive their overall wellbeing while engaged in the music therapist-led, community-based music program?
2 Methods
2.1 Design
A descriptive, single unit, embedded case study design was used to evaluate the Sounds of Service music therapy program. We chose this observational, non-experimental design because it allowed us to evaluate Veterans’ experiences in music therapy within a real-life, single context using multiple sources of evidence (18, 19). This design also allowed us to maximize available resources while working within required privacy and confidentiality guidelines.
2.2 Participants
Veterans from all branches of the military ages 18 and older living in a U.S. Department of Housing and Urban Development-VA Supportive Housing ([HUD-VASH]; 20, 21) complex in a Northern Florida city were eligible to participate in the program. Veterans were eligible regardless of health status, time since transition out of active duty, VA service-connected eligibility status, or any demographic characteristic like sex or age.
2.3 Measurements and data analysis
Data were collected from two primary sources: the music therapist’s session notes and Veterans’ verbal and written program input. Attendance logs and music therapist session notes served as the primary sources of information. Attendance logs were used to track the total number of attendees per session. Session notes were used to collect data for each session on music genres used, and music therapy interventions implemented. Primary objectives targeted by the music therapist and topics addressed by the Veterans themselves were also tracked for each session. Additionally, the music therapist recorded narrative comments to address additional information not covered in the structured note. This included recording Veterans’ comments and other relevant clinical information.
To integrate the Veteran’s voice and input into the clinical program to the extent allowable within the required privacy and confidentiality guidelines, Veterans were asked to provide their military branch, preferred musical genres, and preferred ways to engage in music. This information was provided at the start of the program through a music use questionnaire; however, providing the information was voluntary and not required for participation in the program. Music use data were recorded in a spreadsheet and used to guide clinical programming. Veterans were asked to again provide their preferred music and preferred ways to engage in music at the end of the program. In addition to the music use data, narrative feedback was provided by two Veterans who chose to write notes in support of the program. These Veterans had verbalized support throughout the program and wanted to be sure their voices were included in the program evaluation.
All demographic and attendance data were analyzed descriptively to determine ranges, means, and standard deviations. Participants’ comments, taken from the therapist’s notes and Veterans’ feedback, were examined to determine if any common themes arose. To do this, we conducted a qualitative content analysis by coding and combining comments into thematic groups.
2.4 Theoretical conceptualization
Whole Health is a person-centered, evidence-informed approach that recognizes the relationship between the Veteran, their providers, and the community. Whole Health is rooted in the idea that engaging the whole person—physically, emotionally, mentally, and spiritually—is crucial to health and wellbeing (5). Whole Health aims to empower Veterans by offering personalized, proactive, patient-driven care guided by the Veteran’s values, goals, and vision for their own health and wellbeing (7). Currently, whole health is integrated in some VA sites; however, there have been calls for the Department of Veterans Affairs to scale the Whole Health system to fully transform care to be people-centered, comprehensive, and holistic (22). This would include providing care across a continuum and strengthening access to Complementary and Integrative Health (CIH) approaches like music therapy, which have been mandated as part of the standard VA medical benefits since 2017 (8).
In keeping with the Whole Health Model, we designed a group, music therapist-led music program to support and foster physical, mental, emotional, and social health and wellbeing among Veterans who successfully completed the HUDVASH program and engaged in music therapy treatment as part of their maintenance support. Our goal was to empower Veterans to take charge of their own health and wellbeing through Veteran-centered active and receptive music therapy interventions in a safe, familiar, and non-judgmental environment. We did this by focusing on whole person, personalized, proactive, Veteran driven care, and by including the Veterans themselves in constructing the structure of each session to foster collaboration with peers and the music therapist. We also focused on the core principles of trauma-informed care (safety, trustworthiness and transparency, peer support, collaboration and mutuality, empowerment, voice, and choice, and cultural, historical, and gender issues) (23), in part by integrating ongoing supervision by an experienced music therapist to ensure the music therapists leading sessions promoted ongoing safety, trust, and responsiveness to the Veterans.
2.5 Setting and program design
Sounds of Service was the title used for the duration of this program in 2019 and since has concluded. Sessions were offered in a HUD-VASH supportive housing complex located in a city in Northern Florida, USA. The housing complex provides housing for up to 50 homeless Veterans (24).
Sessions were led by music therapists from the music therapy private practice. One primary music therapist led the program, and in the event of the primary therapist’s absence, two additional music therapists served as substitutes. Additionally, a music therapy student was assigned to assist the board-certified music therapist during each session. The project was funded by the National Endowment for the Arts and the Florida Division of Cultural Affairs.
During the program, Veterans participated in active and receptive music therapy interventions including group music making (singing and group drumming), song discussion, lyric re-writing, and music-assisted relaxation. To promote trust and responsiveness, the Veterans also played an active role in determining the music experiences integrated in each session. Additional steps were taken to promote safety, trust, and responsiveness, including:
● The academic partner met with the VHA/HUD-VASH staff prior to the start of the program to ensure that the program’s design would be consistent with and responsive to the culture and needs of those who would be served. Communication continued throughout the project to support ongoing responsiveness to the Veterans’ needs and adapt to facility changes.
● The music therapy team actively consulted with HUD-VASH staff before, during, and after each session to promote Veteran safety.
● HUD-VASH/VHA staff worked with the music therapy team to ensure their policies and protocols were followed to facilitate Veterans’ safety and privacy.
● Sessions were offered directly in the HUD-VASH housing complex to increase accessibility for those without transportation. Sessions were also scheduled to maximize Veterans’ ability to participate.
● The MT-BC clinicians participated in regular supervision with the academic partner to address challenges and ensure ongoing responsiveness to the Veterans’ needs.
2.6 Session description
A basic session protocol was developed for structuring sessions. The protocol was intended to be a flexible guide rather than a directive session plan; as a result, each session was adapted by the music therapist based on who attended, the number of attendees, session location (location changed based on housing complex programming), and other factors. The session structure was also adapted based on input from and choices made by the Veterans. The protocol consisted of:
1. Introduction of therapist and participants.
2. Check in with participants. The music therapist and Veterans spent time discussing life events, changes since last time together, and other things Veterans chose to share.
3. Questions about music-related preferences and interventions. Veterans were asked about what music they had been listening to, instruments they wanted to play, music they wanted for the session, strategies they would like to participate in during the session, and so on.
4. Music therapist led re-creative music interventions: The music therapist led live singing and instrument play using preferred music options shared at the onset of the session or requested by Veterans during previous sessions. Re-creative interventions were selected because the Veterans “expressed their desire to play live music” (MT-BC session notes).
5. Veteran selected/led music interventions: Veterans selected and/or led music interventions like music listening, singing, and instrument play. Music selections included songs that had previously been introduced by the music therapist and/or music introduced by the Veterans. Veterans also brought their own recordings and/or instruments to the sessions.
6. Other music interventions: Other interventions were integrated when appropriate based on group and individual needs and requests from the Veterans. Interventions used included composition/songwriting, improvisation (primarily percussion based), and receptive interventions like song discussion.
7. Reflection and Feedback: Throughout the session, the music therapist created space for reflection, reminiscing, discussion, and feedback related to the music experiences during the session. Reflection questions were asked based on the music, group discussion, and comments shared by the Veterans. These questions were designed to elicit both Veterans’ input for future sessions and their insights and feelings. This approach allowed Veterans to shape future session content while also supporting emotional processing and personal reflection. Time was also spent summarizing the day’s experiences at the end of each session to provide closure before ending the session.
3 Results
3.1 Program characteristics
A total of 45 sessions occurred during the program. Of these, 42 were group music sessions, two were canvasing sessions, and one was a demonstration session. Canvasing sessions were focused on recruiting participants, and these occurred at the start of the program. Twenty people were engaged during the canvasing sessions, and a total of 21 unique individuals participated in the Sounds of Service program. Group size for the music sessions ranged from two to five individuals, with a cumulative total of 120 Veteran attendances. Veterans represented four branches of the U.S. military: the U.S. Army, U.S. Air Force, U.S. Marine Corps, and U.S. Navy. Among the participants, two Veterans identified as female, while the remaining individuals identified as male.
Veterans were asked, pre and post program, to indicate their preferred music therapy interventions. Live music listening and singing were identified as most preferred at both pre and post program. The music therapist also tracked music therapy interventions used in each session, and the most frequently utilized interventions included singing (82% of sessions), instrument play (69%), song discussion (53%), drumming (36%), and music listening (15%). Veterans were additionally asked to indicate their preferred music genres pre and post program; they indicated a preference for rock, country, blues, and folk music, with rock and country emerging as the most frequently utilized genres during sessions. Most frequently used genres were based on music therapist session notes. According to the pre and post data collected from the Veterans, musical preferences remained the same over the course of the program, and no reported changes were noted.
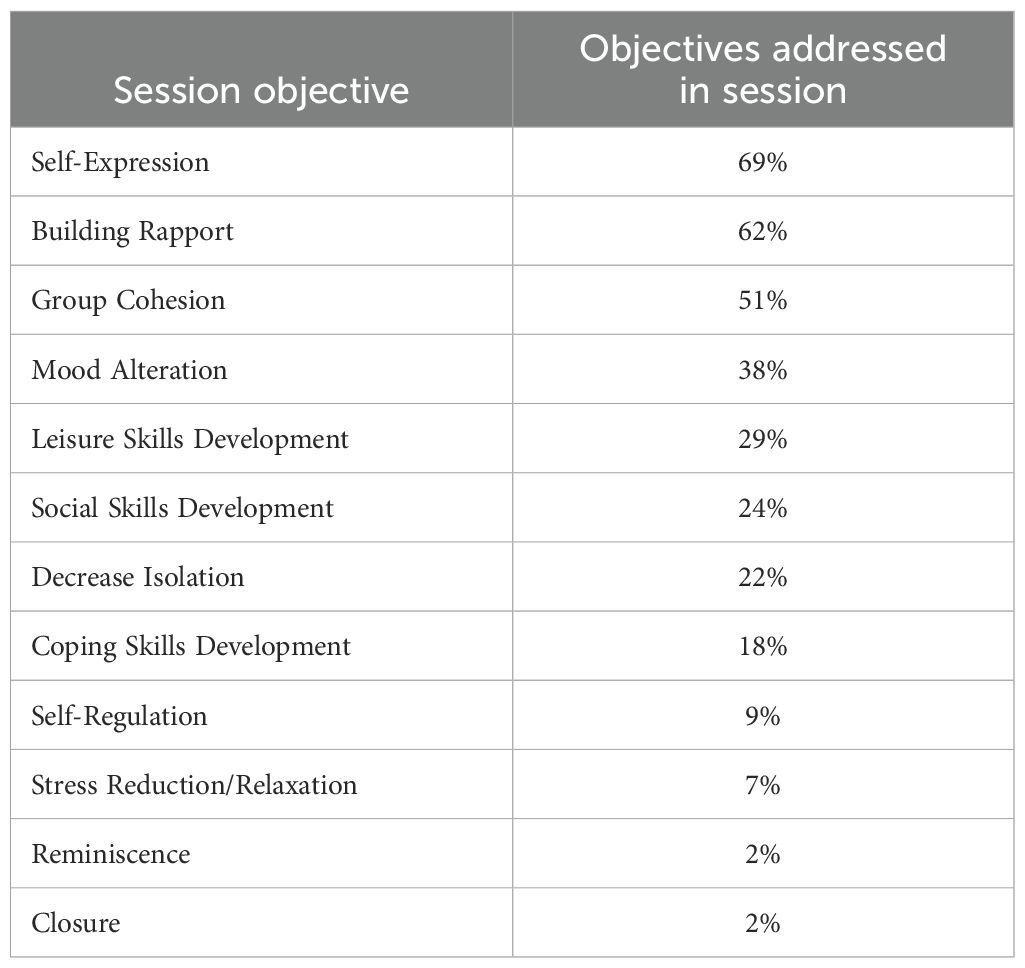
During each session, the music therapist tracked objectives. The three most frequently addressed objectives during the music therapy sessions were fostering self-expression (69%), building rapport (62%), and enhancing group cohesion (51%). Additional objectives addressed included mood enhancement (39%), developing leisure skills (29%), improving social skills (24%), reducing isolation (22%), and fostering coping skills (18%). Objectives such as self-regulation, stress reduction, and reminiscence were addressed at rates lower than 1%. Table 1 presents the distribution of primary objectives addressed across sessions.
Topics discussed during sessions were tracked by the music therapist, and the most often addressed topics related to music (84%), recreation and leisure (53%), emotions (51%), relationships (48%), and military service (46%). Other topics frequently discussed in sessions were coping, family, substance use disorder, finances and employment, and homelessness. Veteran verbal and musical engagement and group cohesion were assessed weekly by the music therapist using a standardized 5-point scale. To promote consistency across therapists, a shared rating guide was developed. Engagement was defined as observable participation in either verbal or musical activities during the session. Verbal engagement included behaviors such as responding to questions, sharing personal reflections, or contributing to group discussions. Musical engagement encompassed actively singing, playing instruments, improvising, or participating in music therapy interventions. Group cohesion was defined as the sense of connection, trust, and mutual support among group members, as demonstrated through active participation and positive interactions. Results showed verbal engagement (M = 4.2, SD = 1.0), musical engagement (M = 3.3, SD = 1.3), and group cohesion (M = 4.3, SD = 0.9).
3.2 Veterans’ comments
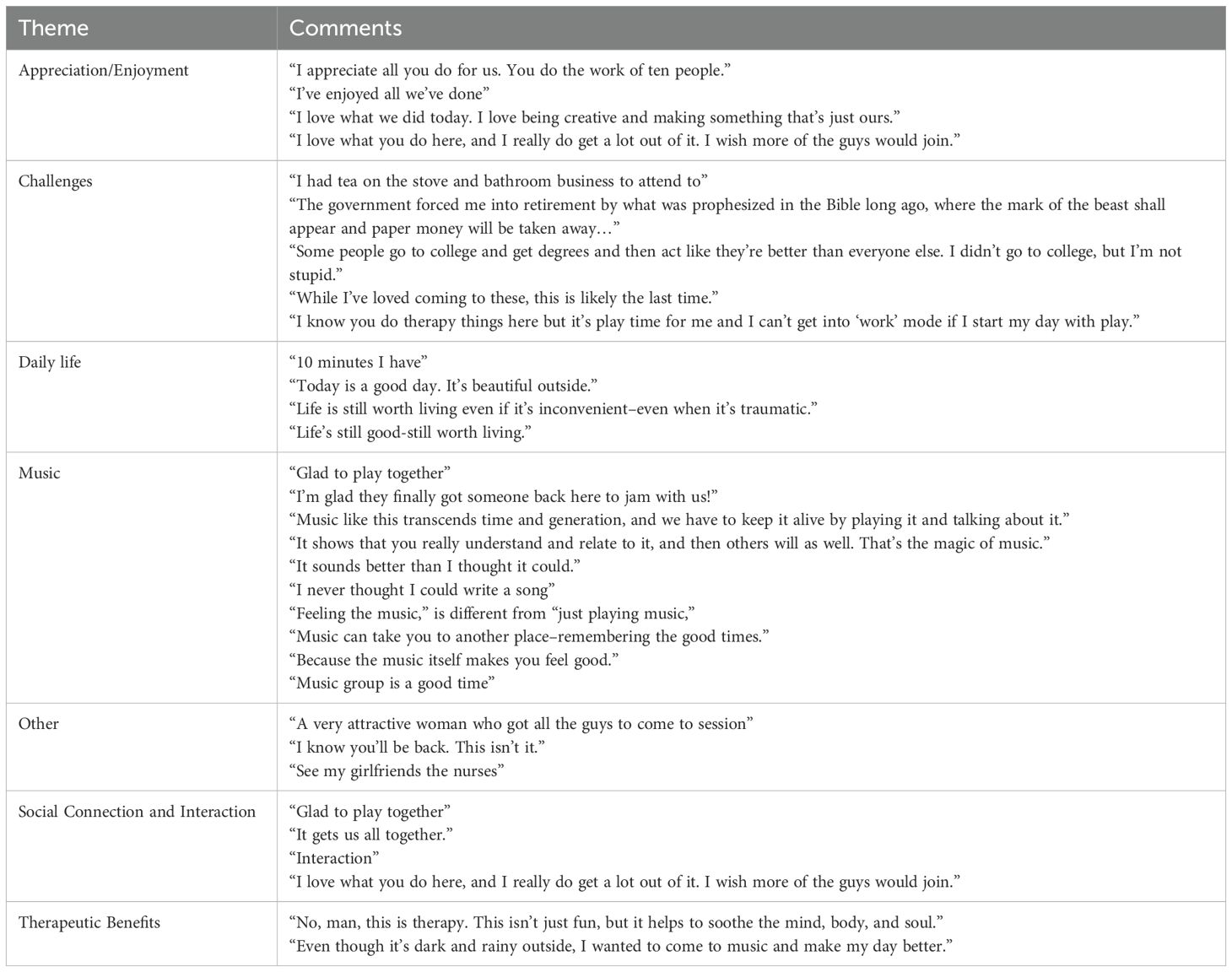
The authors conducted a qualitative content analysis on 30 comments shared by Veterans during sessions; these comments were obtained from session notes. Each comment was coded and combined into themes, which the team discussed and organized until agreement was reached. To enhance the trustworthiness of our thematic analysis, the authors conducted the coding process, and an additional researcher—who did not participate in the study—reviewed the session notes independently. Discrepancies were discussed and resolved through consensus to minimize bias.
Recurring keywords such as “together,” “therapy,” and “appreciate” were identified. Through open coding and collaborative discussions, six overarching themes emerged: Music (n =10), challenges (n = 6), daily life (n = 4), social connection and interaction (n = 4), appreciation and enjoyment (n = 4), therapeutic benefits (n = 2), and other (n = 3). Table 2 depicts the comments grouped by key themes from the Veterans’ comments.
3.3 Therapist notes
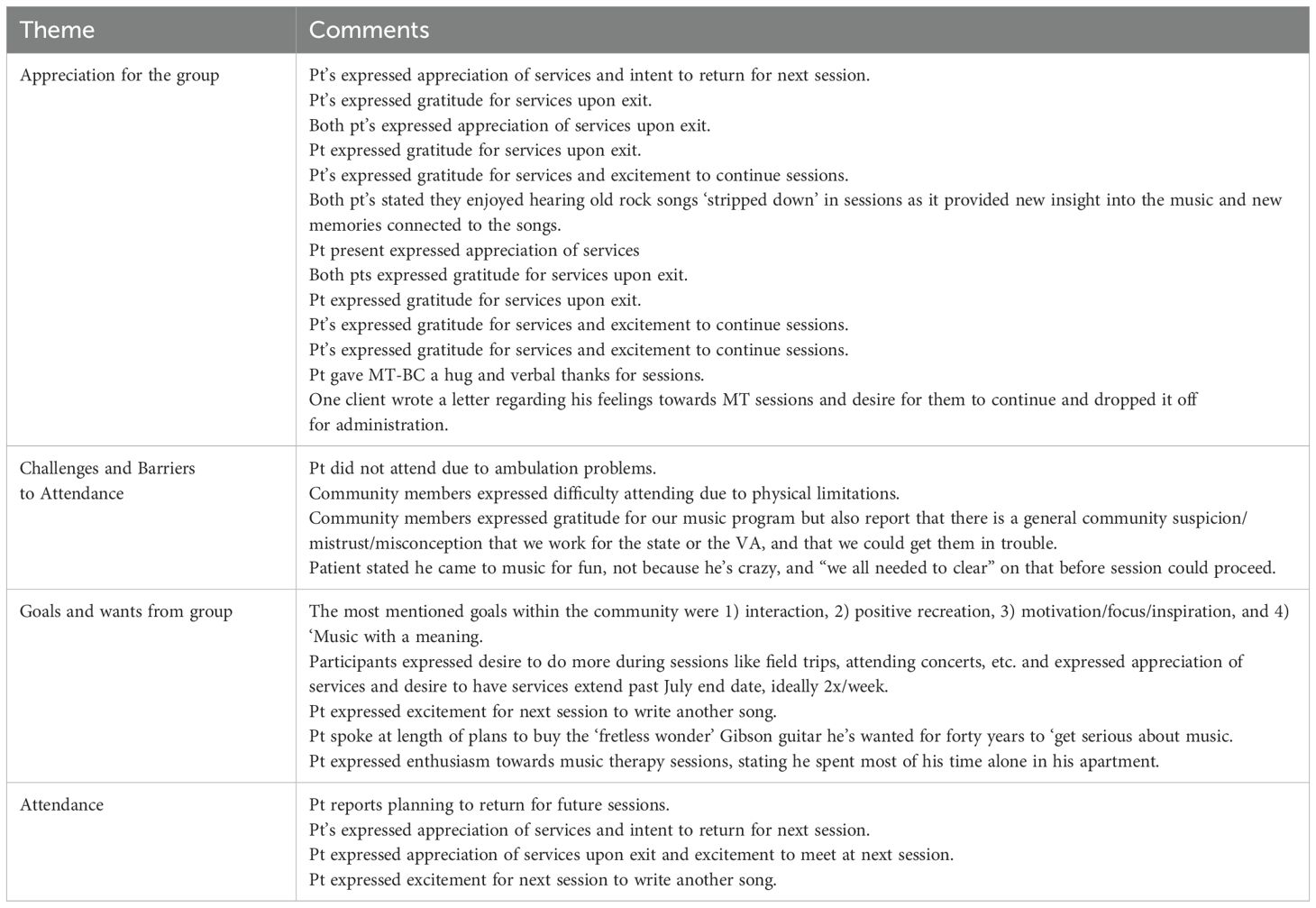
We followed the same process in analyzing 41 music therapist session notes as we did for the Veterans’ comments. Session notes were not recorded for the demonstration and canvasing sessions (n=3), and notes were missing for one session. This left a total of 41 notes for analysis. Our team identified four primary themes from the music therapist’s notes: (a) appreciation for the group (n = 13), (b) objectives and expectations for the group (n = 5), (c) challenges and barriers to attendance (n = 4), and (d) attendance (n = 4).
4 Discussion
The purpose of our study was to evaluate a music therapist-led, community-based music program offered in a supportive housing complex. This program was designed to support and foster mental, emotional, and social health and wellbeing in Veterans encountering long-term and repeated homelessness, mental illness, and/or other health or transition issues. To evaluate the program, we identified (a) Veterans served, (b) music therapy interventions implemented, (c) objectives addressed, and (d) Veterans’ perceptions of the program and their wellbeing as reported in music therapist session notes. Over the course of 45 sessions, we served 21 individuals from four branches of the military who largely identified as male. Singing and instrument play were the most common musical experiences, and rock and country were the most integrated musical genres. Per music therapist session notes, self-expression, building rapport, and group cohesion were the most addressed objectives. “Music” was the most discussed topic by the Veterans, and “appreciation and enjoyment” for the program was the most common topic identified by the music therapist. “Challenges and barriers” were identified by both the Veterans and the music therapist. Additional topics addressed included objectives (music therapist), social connection/interaction (Veterans), and daily life (Veterans).
Our findings illustrate the potential impact of music therapist-led music programming on Veterans, particularly in fostering the development of meaningful recreational/leisure skills while also providing a safe space—through music therapist-led experiences—for Veterans with complex needs to express themselves, build connection, and discuss challenges. Comments like “glad to play together,” “It shows that you really understand and relate to it, and then others will as well.” “The magic of music,” “It gets us all together,” and “I love what you do here, and I really do get a lot out of it. I wish more of the guys would join” highlight the Veterans’ perceptions that the program promoted the development of healthy leisure experiences, addressed social isolation, and promoted a sense of community (Table 3). Vetro-Kalseth et al. (25) found similar results in their work using a phased music therapy group to support Veterans’ reintegration. In that project, Veterans highlighted benefits of participating in music therapy groups like having skill-building opportunities, bolstering peer connections, decreasing isolation, enhancing camaraderie, and increasing social connections. Thus, engaging in music therapist-led group music therapy interventions appears to be a well received, promising option to address the needs of both Veterans transitioning (25) into the community and those living in the community with more expansive needs.
4.1 Considerations regarding program characteristics
Based on our results, it appears that the Veterans enjoyed engaging in and with music, mainly through active music making (e.g., singing, drumming) or through song discussion (verbal processing of the musical and verbal elements of a song). Previous research has shown that Veterans reported music listening as their most frequent leisure activity (26) and that Veterans have found opportunities to connect with others, build coping skills, and grow through music (27). Veterans who participated in the Sounds of Service program had similar responses, sharing “Glad to play together,” “I never thought I could write a song,” and “This isn’t just fun, but it helps to soothe the mind, body, and soul.” These comments suggest that the Veterans who participated in our project not only enjoyed the program, but also had opportunities to connect, build coping skills, and grow.
In designing our program, we intentionally tailored the program to meet the unique needs of those who would be participating. This included working collaboratively with the Veterans to determine what interventions would be integrated into the sessions. This appeared to be a positive approach, as illustrated by one Veteran who stated, “I love being creative and making something that’s just ours”. Their comment underscores the importance of tailored music therapy interventions and highlights the need to collaboratively engage Veterans in music programming.
Equally important, one Veteran shared “I’m glad they finally got someone back here to jam with us,” highlighting the importance and need to make therapy-based experiences accessible for Veterans, particularly those facing barriers to services. Offering Sounds of Service directly in the supportive housing unit appeared to support participation as well as create connections among the housing community residents (“It gets us all together”). Thus, it appears that group, music-therapy based programming should be structured to be (a) inclusive of both active (i.e., making) and receptive (i.e., responding to) music interventions, (b) collaborative and tailored to the Veteran participants, and (c) accessible. Additional research is needed to explore how specific interventions can better support Veterans facing complex and interconnected challenges such as Post Traumatic Stress Disorder (PTSD), depression, chronic pain, and homelessness.
4.2 Considerations regarding veterans’ and music therapist’s perception
Music therapy has been found to be well received by Veterans (10), potentially creating a path to address participants’ interconnected needs when more traditional approaches are viewed with distrust. According to Bradt et al. (28), music therapy may not be associated with the same stigma as other therapies, may be more accepted, and may lower barriers, particularly in terms of mental health care. Because music therapy services for Veterans emphasize evidence-based, person-centered interventions that promote the whole health of the individual (29), music therapy may increase accessibility and reduce barriers to participation when integrated into the holistic, “whole health” approach used to serve Veterans from the clinic to the community.
Trauma-informed care (TIC), which emphasizes safety, trustworthiness, peer support, collaboration, and empowerment (23), has been endorsed with military-connected populations (30). Music therapy naturally integrates these principles by creating a supportive environment that acknowledges the impact of trauma while fostering resiliency and recovery. By incorporating the TIC tenets along with the core principles of whole health, music therapists can provide emotional safety, encourage trust-building, and empower Veteran’s health journey (31, 32).
Veterans’ comments collected during the program highlighted the significant emotional and personal value participants placed on the music therapy sessions. Veterans expressed gratitude for the sessions and enthusiasm for future attendance, demonstrating strong engagement with the program. Participants also reported forming personal connections and gaining new insights through the experience. For example, some noted that hearing classic rock songs in a stripped-down format provided them with a fresh perspective and deeper emotional connection. This impact was further emphasized by two Veterans who wrote and delivered an unsolicited letter detailing the benefits of the music therapy program and underscoring the value of these sessions as a vital resource for Veterans. They also expressed a strong desire for a dedicated staff member to support and sustain the program. Additionally, participants’ goals for expanded activities and continued sessions further underscore the program’s importance in their lives, emphasizing the need for ongoing support and development.
Congruent with the Veteran’s perceptions expressed in the notes they wrote to support the program; music therapist’s session notes showed the Veterans’ appreciation and value for the services provided. According to these notes, participants articulated several goals for their engagement in music therapy, with the most common being social interaction, positive recreation, motivation, and finding personal meaning in music. Some participants expressed enthusiasm for expanding program activities, including field trips, attending concerts, and extending sessions beyond the initial timeframe, ideally increasing frequency to twice per week. Individual goals also emerged, such as writing new songs in future sessions and pursuing personal musical aspirations, such as purchasing a long-desired instrument to deepen musical practice. These responses underscore the program’s role in fostering both individual and group development, suggesting that expanding opportunities for engagement could further enhance participant outcomes. Future efforts should focus on sustaining and developing these services to meet the evolving needs of this community (33, 34, 35).
4.3 Other considerations for future programming
Financial, personal, and physical obstacles, confidence in the VA healthcare system, and privacy and security have all been identified as barriers to care among Veterans (36, 37). Veterans who participated in Sounds of Service expressed similar challenges and barriers to their participation. For example, physical challenges such as ambulation problems prevented some Veterans from attending. Additionally, community mistrust posed a barrier, as some individuals expressed concerns about the program’s affiliation with the state or the VA. There was also evidence of stigma surrounding therapy, with one participant clarifying they attended for enjoyment rather than because they were “crazy.” Comments like these highlight the need for increased accessibility and community education to address misconceptions and reduce barriers to participation.
5 Conclusion
Sounds of Service is one of the first music therapy programs presented in the literature to focus on homeless Veterans who are living in supportive housing. Our group-based, music therapist-led music program was designed from a whole health and trauma-informed perspective to address the unique needs of this marginalized population. We offered sessions directly in the housing complex to increase accessibility, and we collaborated with the Veterans, integrating their preferences and values to build trust and connection and empower them to take charge of their own health and wellbeing. Veterans appeared to both enjoy and benefit from the program, and the data collected suggest the potential of this type of program to meet the needs of Veterans with interconnected challenges.
We believe Sounds of Service is an important first step in expanding our understanding of music therapy with Veteran populations with complex, interconnected needs living in the community. It provides guidance on and a model for evidence-based clinical practice, academic research, and community connection. It also provides additional evidence on the benefits of music therapy treatment in supporting the clinic-to-community continuum. Future research and clinical learning are needed to explore the sustainability of programs such as this, but we hope this study demonstrates the feasibility of music therapy treatment in partnership with local community entities and a large health system.
Data availability statement
The datasets presented in this article are not readily available because data was not approved for public accessibility. Requests to access the datasets should be directed to LG,bGdvb2RpbmdAZnN1LmVkdQ==.
Ethics statement
The studies involving humans were approved by Florida State University Office for Human Subjects Protection (OHSP) and Institutional Review Board (IRB). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LG: Conceptualization, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. FH: Writing – original draft, Writing – review & editing. DL: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This project is sponsored in part by the Department of State, Division of Cultural Affairs, the Florida Council of Arts and Culture and the State of Florida and the National Endowment for the Arts.” (Section 286.25, Florida Statutes). This work was also supported in part by Creative Forces®: NEA Military Healing Arts Network, an initiative of the National Endowment for the Arts in partnership with the U.S. Departments of Defense and Veterans Affairs that seeks to improve the health, well-being, and quality of life for military and veteran populations exposed to trauma, as well as their families and caregivers. Creative Forces is managed in partnership with the Henry M. Jackson Foundation for the Advancement of Military Medicine, and Mid-America Arts Alliance.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Olenick M, Flowers M, and Diaz VJ. US Veterans and their unique issues: Enhancing health care professional awareness. Adv Med Educ Pract. (2015) 6:635–9. doi: 10.2147/AMEP.S89479
2. U.S. Department of Veterans Affairs. Veterans Health Administration. Washington, DC: VA.gov Veterans Affairs (2025). Available at: https://www.va.gov/health/aboutvha.asp (Accessed January 25, 2025).
3. Rasmussen P and Farmer CM. The promise and challenges of VA community care: veterans' Issues in focus. Rand Health Q. (2023) 10:9.
4. Oster C, Morello A, Venning A, Redpath P, and Lawn S. The health and wellbeing needs of Veterans: A rapid review. BMC Psychiatry. (2017) 17:414. doi: 10.1186/s12888-017-1547-0
5. Kligler B. Whole health in the veterans health administration. Global Adv Health Med. (2022) 11:2164957X221077214. doi: 10.1177/2164957X221077214
6. Woodward L and Otto D. Music therapy in the Department of Veterans Affairs. In: Vaudreuil R, editor. Music therapy with military and veteran populations. Philadelphia, PA: Jessica Kingsley Publishers (2021). p. 65.
7. Krejci LP, Carter K, and Gaudet T. Whole Health: The vision and implementation of personalized, proactive, patient-driven health care for Veterans. Med Care. (2014) 52:S5–S8. Available online at: https://journals.lww.com/lww-medicalcare/fulltext/2014/12001/whole_health:the_vision_and_implementation_of.4.aspx.
8. Kligler B, Khung M, Schult T, and Whitehead A. What we have learned about the implementation of Whole Health in the Veterans Administration. J Integr Complement Med. (2023) 29:774–80. doi: 10.1089/jicm.2022.0753
9. Vaudreuil R, Bronson H, and Bradt J. Bridging the clinic to community: Music performance as social transformation for Military Service Members. London, UK: Frontiers in Psychology (2019). doi: 10.3389/fpsyg.2019.00119
10. Gooding LF and Langston DG. Music therapy with military populations: A scoping review. J Music Ther. (2019) 56:315–47. doi: 10.1093/jmt/thz010
11. Vaudreuil R, Langston DG, Magee WL, Betts D, Kass S, and Levy C. Implementing music therapy through telehealth: Considerations for military populations. Disabil Rehabil Assist Technol. (2022) 17:201–10. doi: 10.1177/0305735614566841
12. Wasmuth S, Rattray NA, Cheng P, Crow S, Myers J, Burns DS, et al. A developmental formative evaluation of a pilot participatory music program for Veterans with housing insecurity. BMC Public Health. (2023) 23:1583. doi: 10.1186/s12889-023-16427-8
13. Ehmling AE. People experiencing homelessness within music therapy settings: A descriptive study (2018) University of Kentucky, Lexington, KY. Available at: https://uknowledge.uky.edu/music_etds/106 (Accessed January 20, 2025).
14. Bronson H, Vaudreuil R, and Bradt J. Music therapy treatment of active duty military: An overview of intensive outpatient and longitudinal care programs. Music Ther Perspect. (2018) 36:195–206. doi: 10.1093/mtp/miy006
15. American Music Therapy Association. Music therapy and military populations: A status report and recommendations on music therapy treatment, programs, research, and practice policy. Silver Springs, MD: American Music Therapy Association (AMTA (2014). Available online at: https://www.musictherapy.org/research/music_therapy_and_military_populations/ (Accessed January 13, 2025).
16. Peden AR. Music: Making the connection with persons who are homeless. J Psycho Nurs Ment Health Serv. (1993) 31:17–20. doi: 10.3928/0279-3695-19930701-07
17. Powers JS, Heim D, Grant B, and Rollins J. Music therapy to promote movement from isolation to community in homeless veterans. Tennessee med: J Tennessee Med Assoc. (2012) 105:38–9.
19. Yin RK. Case study research: Design and methods. In: Applied social research methods series, 3rd, vol. 5. Thousand Oaks, CA: SAGE Publications (2003).
20. U.S. Department of Veterans Affairs VHA Office of Mental Health. VA Homeless Programs. Washington, DC: VA.gov Veterans Affairs (2024). Available online at: https://www.va.gov/homeless/hud-vash.asp (Accessed January 25).
21. VA/U.S. Department of Veterans Affairs. Homeless Veteran care (2024). Available online at: https://www.va.gov/north-florida-health-care/health-services/homeless-veteran-care/ (Accessed January 25, 2025).
22. National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Health Care Services, and Committee on Transforming Health Care to Create Whole Health. Achieving whole health: A new approach for veterans and the nation. Meisnere M, South-Paul J, and Krist &AH, editors. Washington, DC: National Academies Press (2023). Available at: https://www.ncbi.nlm.nih.gov/books/NBK591727/.
23. Substance Abuse and Mental Health Service Administration [SAMHSA]. SAMHSA’s concept of trauma and guidance for trauma-informed approach (2014). Available online at: https://library.samhsa.gov/product/samhsas-concept-trauma-and-guidance-trauma-informed-approach/sma14-4884 (Accessed January 13, 2025).
24. Leon County. Community resources. Available online at: https://cms.leoncountyfl.gov/Government/Departments/Human-Services-Community-Partnerships/Veteran-Services/Community-Resources (Accessed January 13, 2025).
25. Vetro-Kalseth D, Vaudreuil R, and Segall LE. Treatment description and case series report of a phased music therapy group to support Veteran reintegration. Milit Psychol. (2021) 33:446–52. doi: 10.1080/08995605.2021.1962194
26. Zoteyeva V, Forbes D, and Rickard NS. Military veterans’ use of music-based emotion regulation for managing mental health issues. Psychol Music. (2016) 44:307–23. doi: 10.1177/0305735614566841
27. Liebowitz M, Tucker MS, Frontz M, and Mulholland S. Participatory choral music as a means of engagement in a Veterans’ mental health and addiction treatment setting. Arts Health. (2015) 7:137–50. doi: 10.1080/17533015.2014.999246
28. Bradt J, Biondo J, and Vaudreuil R. Songs created by military service members in music therapy: A retrospective analysis. Creative Arts Ther Milit. (2019) 62:19–27. doi: 10.1016/j.aip.2018.11.004
29. Davis WB and Else BA. Music therapy with service members and Veterans. In: Kraaz SM, editor. Music and War in the United States. London, UK: Routledge (2018). p. 291–307.
30. Herzog JR, Whitworth JD, and Scott DL. Trauma informed care with military populations. J Hum Behav Soc Environ. (2019) 30:265–78. doi: 10.1080/10911359.2019.1679693
31. Clay RA. Serving the underserved. Mon Psychol. (2010) 41:70. Available online at: https://www.apa.org/monitor/2010/12/underserved.
32. Weber J, Lee RC, and Martsolf D. Understanding the health of Veterans who are homeless: A review of the literature. Public Health Nurs. (2017) 34:505–11. doi: 10.1111/phn.12338
33. Byrne T, Montgomery AE, and Fargo JD. Unsheltered homelessness among Veterans: Correlates and profiles. Community Ment Health J. (2016) 52:148–57. doi: 10.1007/s10597-015-9922-0
34. Kinney RL, Szymkowiak D, and Tsai J. Growing concern about unsheltered homelessness among Veterans: Clinical characteristics and engagement in health care services. Public Health Rep. (2024) 139:582–90. doi: 10.1177/00333549241227155
35. Nichter B, Tsai J, and Pietrzak RH. Prevalence, correlates, and mental health burden associated with homelessness in U.S. Milit Vet psychol Med. (2023) 53:3952–62. doi: 10.1017/S0033291722000617
36. Cheney AM, Koenig CJ, Miller CJ, Zamora K, Wright P, Stanley R, et al. Veteran-centered barriers to VA mental healthcare services use. BMC Health Serv Res. (2018) 18:591. doi: 10.1186/s12913-018-3346-9
Keywords: music therapy, veterans, homelessness, community, military
Citation: Gooding LF, Hernandez FdC and Langston DG (2025) Sounds of Strength: a programmatic evaluation of a music therapist led community-based program for Veterans in supportive housing. Front. Psychiatry 16:1581291. doi: 10.3389/fpsyt.2025.1581291
Received: 21 February 2025; Accepted: 02 June 2025;
Published: 14 July 2025.
Edited by:
Jay M. Uomoto, Henry M Jackson Foundation for the Advancement of Military Medicine (HJF), United StatesReviewed by:
Bronwen Landless, Shenandoah University, United StatesLeslie Henry, Alverno College, United States
Copyright © 2025 Gooding, Hernandez and Langston. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lori F. Gooding, bGdvb2RpbmdAZnN1LmVkdQ==
 Lori F. Gooding
Lori F. Gooding Flor del Cielo Hernandez
Flor del Cielo Hernandez Diane G. Langston
Diane G. Langston