- 1Department of Psychiatry, Chongqing Mental Health Center, Chongqing, China
- 2School of Nursing, Zunyi Medical University, Zunyi, China
- 3Department of Nursing, Chengdu Fifth People’s Hospital, Chengdu, China
- 4Department of Nursing, Chongqing Mental Health Center, Chongqing, China
Background: Non-suicidal self-injury (NSSI) in adolescents represents a significant global public health challenge, with lifetime prevalence rates demonstrating a consistent upward trajectory. Current evidence indicates that NSSI conveys elevated risks for both physical complications and psychological comorbidities, while simultaneously imposing a substantial burden on primary caregivers.
Objective: This study applied latent profile analysis (LPA) to classify distinct caregiver burden profiles among adolescents with NSSI, identify modifiable determinants, and establish an empirical foundation for developing precision interventions stratified by burden type.
Method: From August 2022 to May 2023, 385 caregivers of adolescents with NSSI in Sichuan Province, China, were selected as respondents and systematically assessed using six validated instruments: General Information Questionnaire, Family Burden Scale of Disease, Social Support Rating Scale, Generalized Anxiety Disorder 7-Item Scale, Patient Health Questionnaire-9, and Internalized Stigma of Mental Illness Scale. LPA with maximum likelihood estimation identified distinct caregiver burden profiles, and multinomial logistic regression to determine predictors of profile membership.
Results: The caregiver burden among adolescents with NSSI can be identified into three profiles: low burden-family vulnerability profile (34.5%), moderate burden-mental health priority profile (36.6%), and high burden-economic preponderance profile (28.9%). Female caregivers (OR = 3.760, p = 0.005), rural residents (OR = 3.666, p = 0.027), diminished social support (OR = 0.884, p = 0.016), and elevated anxiety severity (OR = 1.183, p = 0.027) exhibited heightened vulnerability to the moderate burden-mental health priority profile. Heightened depression symptoms (OR = 1.130, p = 0.037) and stronger illness-related stigma (OR = 1.063, p = 0.001) were disproportionately represented in both moderate burden-mental health priority profile and high burden-economic preponderance profile.
Conclusions: This study delineates three distinct caregiver burden profiles among adolescents with NSSI, alongside sociodemographic and clinical predictors of profile membership. Tailored interventions, such as rapid mental health service linkage for high-burden subgroups and family-centered psychoeducation, can mitigate these burdens through stratified support mechanisms.
1 Introduction
Adolescence is a critical developmental window of heightened neuroplasticity and psychopathological vulnerability. Non-suicidal self-injury (NSSI) is a prevalent mental health concern within this population, operationally defined as the deliberate, self-inflicted destruction of bodily tissue without suicidal intent (1). Clinical presentations typically involve cutaneous cutting, severe scratching, and intentional burning (2, 3). Global data reveal a rising prevalence trend, with meta-analytic estimates indicating a 22.0% lifetime incidence in community adolescent cohorts (4). Notably, a Chinese epidemiological study demonstrated elevated rates, with 24.7% of adolescents reporting at least one NSSI episode within the preceding 12-month period (5). The behavior frequently exhibits chronicity and behavioral reinforcement patterns, with a longitudinal investigation identifying addictive characteristics in 22.1% of recurrent cases (6). Moreover, the clinical gravity of NSSI extends beyond its diagnostic categorization, functioning both as a transdiagnostic marker of psychological distress and the strongest identifiable predictor of subsequent suicidality (7, 8). Meta-analytic evidence indicates that over 50% of adolescents with NSSI exhibit clinically elevated suicide risk profiles (9). These converging lines of evidence position NSSI as an urgent global public health.
NSSI constitutes a significant threat to both physical and psychological well-being in affected individuals, while simultaneously imposing multidimensional burdens on familial systems. The protracted treatment requirements for adolescents with NSSI frequently result in substantial disruptions to caregivers’ occupational functioning, daily routines, and long-term life planning (10). Prolonged caregiving strains both physical and mental health, lowering caregivers’ quality of life and disrupting family well-being (11). This chain of effects creates a severe caregiver burden, marked by economic instability and long-term health impacts.
Caregiver burden refers to the challenges or adverse effects of the patient’s illness on the caregiver and their family, encompassing physical, psychological, emotional, interpersonal, and financial domains (12). A cross-sectional survey revealed that 25.2% of caregivers of adolescents with NSSI reported moderate-to-severe or severe burden (13). Epidemiological evidence shows elevated burden levels correlate strongly with poorer psychosocial outcomes (14). Chronic caregiving stress directly impairs care quality, undermining treatment efficacy through caregiver burnout. Furthermore, caregiver burden transcends clinical impacts to disrupt fundamental life domains, including educational pursuits, occupational performance, recreational activities, and daily functioning for patients and families (15). Crucially, this burden undermines family functioning through three pathways: impaired collaborative problem-solving, weakened collective resource management, and disrupted social support mobilization (16). In addition, some caregiver-related factors, such as anxiety (17), depression (18), low social support (19), and stigma (20), were associated with higher levels of caregiver burden.
Current research on caregiver burden in adolescents with NSSI remains notably limited. Existing studies primarily employ standardized scales to assess caregiver burden, potentially neglecting clinically meaningful heterogeneity among individuals (21). Latent profile analysis (LPA), a person-centered statistical approach, addresses this limitation by identifying latent subgroups through continuous indicator variables (22). This methodology classifies study populations into distinct profiles based on observed variable patterns, enabling systematic comparison of inter-group differences in key outcomes and characteristic identification (23). Applied to caregiver burden in NSSI adolescents, LPA facilitates: (a) identification of distinct burden phenotypes, (b) estimation of subtype prevalence rates, and (c) demographic profiling across profiles. Notably, no prior studies have implemented LPA to investigate caregiver burden among Chinese adolescents with NSSI. This study first applies LPA to identify burden profiles in this population and analyze associated predictors. This finding aims to offer clinicians an evidence-based framework for caregiver burden stratification, targeted intervention design, and personalized support delivery, effectively alleviating caregiver distress.
2 Methods
2.1 Participants
A total of 385 questionnaires were distributed in this study, with 374 valid responses retained, yielding an effective response rate of 98.9%. Inclusion criteria comprised (1) adolescents with clinician-confirmed Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) NSSI; (2) adolescents aged 13–18 years; and (3) participants who are the primary caregivers, legal guardians, or direct financial sources for the patients. The exclusion criteria comprised (1) adolescents with severe somatic disorders (which may introduce unrelated pathophysiological factors affecting self-injury assessment); (2) caregivers with severe health conditions (which could compromise caregiving capacity and introduce reporting biases); and (3) those experiencing major traumatic events unrelated to the adolescents’ condition (to isolate NSSI-specific triggers from external stressors), thereby ensuring homogeneity in evaluating caregiver burden associated with adolescent NSSI.
2.2 Procedures
Participants comprised caregivers of adolescent inpatients with NSSI recruited from a psychiatric care setting. Data collection occurred via secured electronic questionnaires administered on discharge day following standardized protocols. Prior to study enrollment, prospective participants were provided with a two-day deliberation period to review study protocols and determine their willingness to participate. All participants provided written informed consent and completed the official Chinese version of the FBS, the SSRS, the GAD-7, the PHQ-9, and the ISMI. To ensure data validity, questionnaires were completed anonymously through a dedicated research platform. The median completion duration ranged from 20–30 minutes. This study received ethical clearance from the Institutional Review Board of Chengdu Fourth Hospital (Approval No: [2022] Lun Shen Zi 71) and was prospectively registered with the Chinese Clinical Trial Registry (ChiCTR2300072081).
2.3 Measures
2.3.1 Socio-demographic information
The socio-demographic information was collected in two domains: caregiver characteristics and corresponding adolescent profiles with NSSI. Data collected from participants included gender, age, residential status, parental status (number of dependent children), educational attainment, marital status, occupational category, monthly household income, health literacy, health insurance coverage type, and family composition. Adolescent records specifically documented the frequency of NSSI episodes during the 30-day observation period, which was determined by the clinical data recorded by psychiatrists at the latest consultation.
2.3.2 Family burden scale of disease
The Family Burden Scale of Disease (FBS) (24), developed to measure the multidimensional impact of patients’ illnesses on both patients and caregivers, encompassing physical, psychological, emotional, interpersonal, and economic domains. This instrument comprises 24 items organized into six dimensions: economic burden, daily activity disruption, recreational activity limitation, family relationship strain, physical health deterioration, and psychological distress. Responses were captured using a 3-point Likert scale (0 = strongly disagree to 2 = strongly agree), with higher composite scores reflecting greater perceived family burden. Following standardized scoring procedures (total dimension score divided by number of items), scores ≥ 1 were categorized as indicating moderate-to-severe burden. The FBS has been validated and widely utilized by previous studies in the study of mental disorders (25). In the present cohort, the Chinese version of the scale demonstrated excellent internal consistency (Cronbach’s α = 0.953).
2.3.3 Social support rating scale
The Social Support Rating Scale (SSRS) (26), developed to measure individuals’ perceived social support through three domains: subjective support, objective support, and support utilization. This 10-item instrument generates a composite score ranging from 12 to 66 by summating all item scores. Social support levels were classified as low (≤ 22), moderate (23–44), or high (45–66). The Chinese version has been used in a wide range of Chinese populations (27). In the present study, the scale demonstrated acceptable internal consistency (Cronbach’s α = 0.740).
2.3.4 Generalized anxiety disorder-7 items
The Generalized Anxiety Disorder 7-item scale (GAD-7), developed by Spitzer (28), assesses anxiety symptoms through self-reported measures of emotional states during the preceding two-week period. This instrument contains seven items rated on a 4-point Likert scale (0 = never to 3 = nearly every day), with total scores ranging from 0 to 21. Higher total scores correspond to greater anxiety severity, with established clinical thresholds as follows: 0–4 (minimal/no anxiety), 5–9 (mild anxiety), 10–14 (moderate anxiety), and 15–21 (severe anxiety). It has shown good validity and reliability in the Chinese population (29). In the present study, the scale demonstrated excellent reliability (Cronbach’s α = 0.905).
2.3.5 Patient health questionnaire-9 items
The Patient Health Questionnaire-9 (PHQ-9), developed by Kroenke (30), is a validated self-report instrument for assessing depressive symptom severity. This 9-item measure employs a 4-point Likert scale (0 = not at all to 3 = nearly every day). Higher total scores reflect greater depressive symptom severity, categorized clinically as: 0–4 (minimal depressive symptoms), 5–9 (mild depression), 10–14 (moderate depression), 15–19 (moderately severe depression), and 20–27 (severe depression). The Chinese version of the PHQ-9 has been demonstrated to be a reliable and valid measurement (29). In the current sample, the instrument demonstrated strong internal consistency (Cronbach’s α = 0.913).
2.3.6 Internalized stigma of mental illness scale
The Internalized Stigma of Mental Illness Scale (ISMI), originally developed by Ritsher (31), evaluates stigma perception among individuals with mental disorders and their caregivers. This 29-item instrument assesses five core dimensions: alienation, stereotyping, discrimination, social withdrawal, and stigma resistance. Responses are recorded using a 4-point Likert scale, with higher composite scores indicating greater stigma internalization. Standardized scores (total dimension score divided by number of items per dimension) stratify stigma severity into four categories: ≤ 2 (no stigma), 2–2.5 (mild), 2.5–3 (moderate), and > 3 (severe). This scale has shown good internal consistency in the Chinese subject population (32). In the current study, the scale demonstrated excellent reliability (Cronbach’s α = 0.913).
2.4 Data analyses
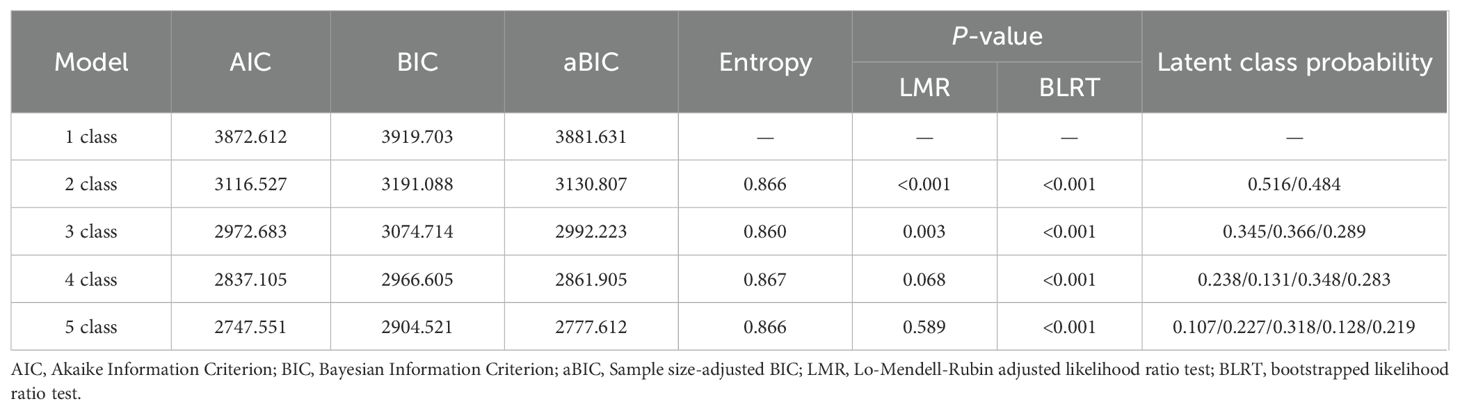
Given the varying metric ranges of the FBS dimensions (1–6), standardized scores were computed across all six domains to facilitate the interpretation of LPA results. The LPA classification model was constructed using Mplus 8.3 software. Model selection was guided by evaluating model fit indices and clinical interpretability. Comparative fit indices included the Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), and sample size-adjusted BIC (aBIC). The AIC quantifies model fit while penalizing parameter complexity, whereas the BIC and aBIC incorporate both model parameters and sample size. As information-theoretic model selection criteria, lower values of AIC, BIC, and aBIC indicate superior model fit. Entropy values (0–1) assessed classification accuracy, with values>0.8 suggesting distinct profile separation. The Lo-Mendell-Rubin adjusted likelihood ratio test (LMRT) and bootstrapped likelihood ratio test (BLRT) statistically compared model improvements between successive class solutions, where significant p-values (p < 0.05) favored the k-class model over the k-1 solution. Following latent profile classification of caregiver burden severity, data were analyzed using SPSS Statistics version 27.0. Variables demonstrating statistical significance in univariate analyses (p < 0.05) were entered as independent predictors in a multinomial logistic regression model, the continuous numerical variables and total scale scores were used as covariates, and the results of potential profile analysis of caregiver burden served as the dependent variable. The variance inflation factor (VIF) checked potential multicollinearity between predictor variables, with VIF > 5 indicating collinearity. Statistical significance was determined at p < 0.05.
3 Results
3.1 Assessment of multicollinearity
To ensure no redundancy among predictors, the Variance Inflation Factor (VIF) was employed to assess multicollinearity. The results indicated that all VIF values were below 5, with the maximum value being 3.312.
3.2 Latent profiles determination
Fit indices for 1–5 class solutions are summarized in Table 1. The AIC, BIC, and aBIC values showed progressive decreases with increasing class solutions, demonstrating diminishing model improvement. The three-class solution demonstrated acceptable classification accuracy (entropy = 0.860), supported by statistically significant LMRT and BLRT results (p < 0.05). However, the four-class model showed non-significant LMRT improvement (p > 0.05). Although the four-class model showed slightly higher entropy (0.867 vs. 0.860), its fourth profile exhibited overlapping burden dimensions with clinically indistinct features, reducing practical applicability for targeted interventions. The three-class solution aligns with the clinically validated tri-level framework (low/moderate/high burden), ensuring clearer alignment with stepped-care protocols. Statistical parsimony (non-significant LMRT for four-class) further supported this choice. Thus, the three-class model balances statistical rigor and clinical translatability.
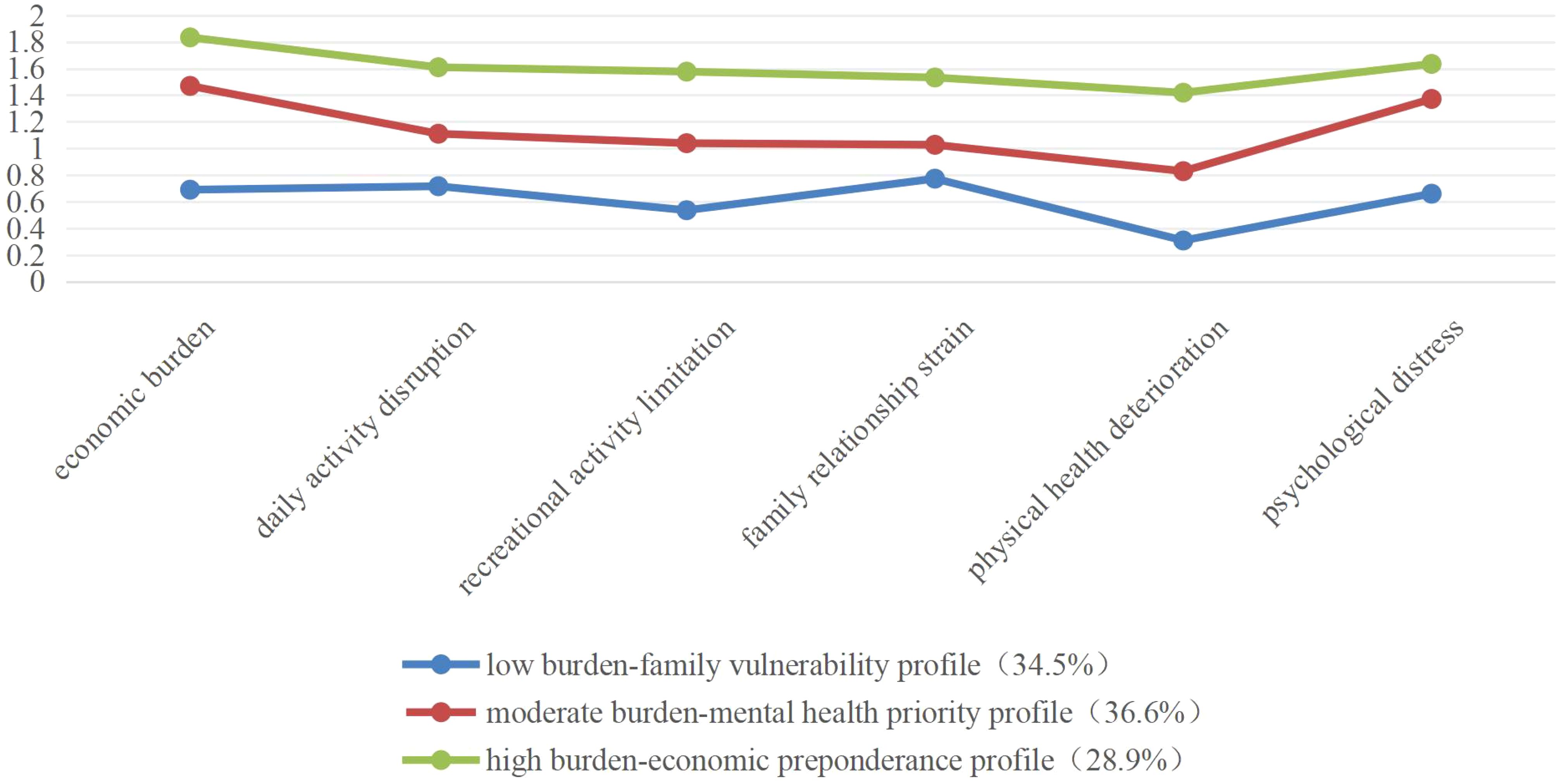
Figure 1 illustrates the three distinct caregiver burden profiles identified via LPA across six measurement domains. Class 1 accounted for 34.5% of the sample, followed by Class 2 (36.6%) and Class 3 (28.9%).
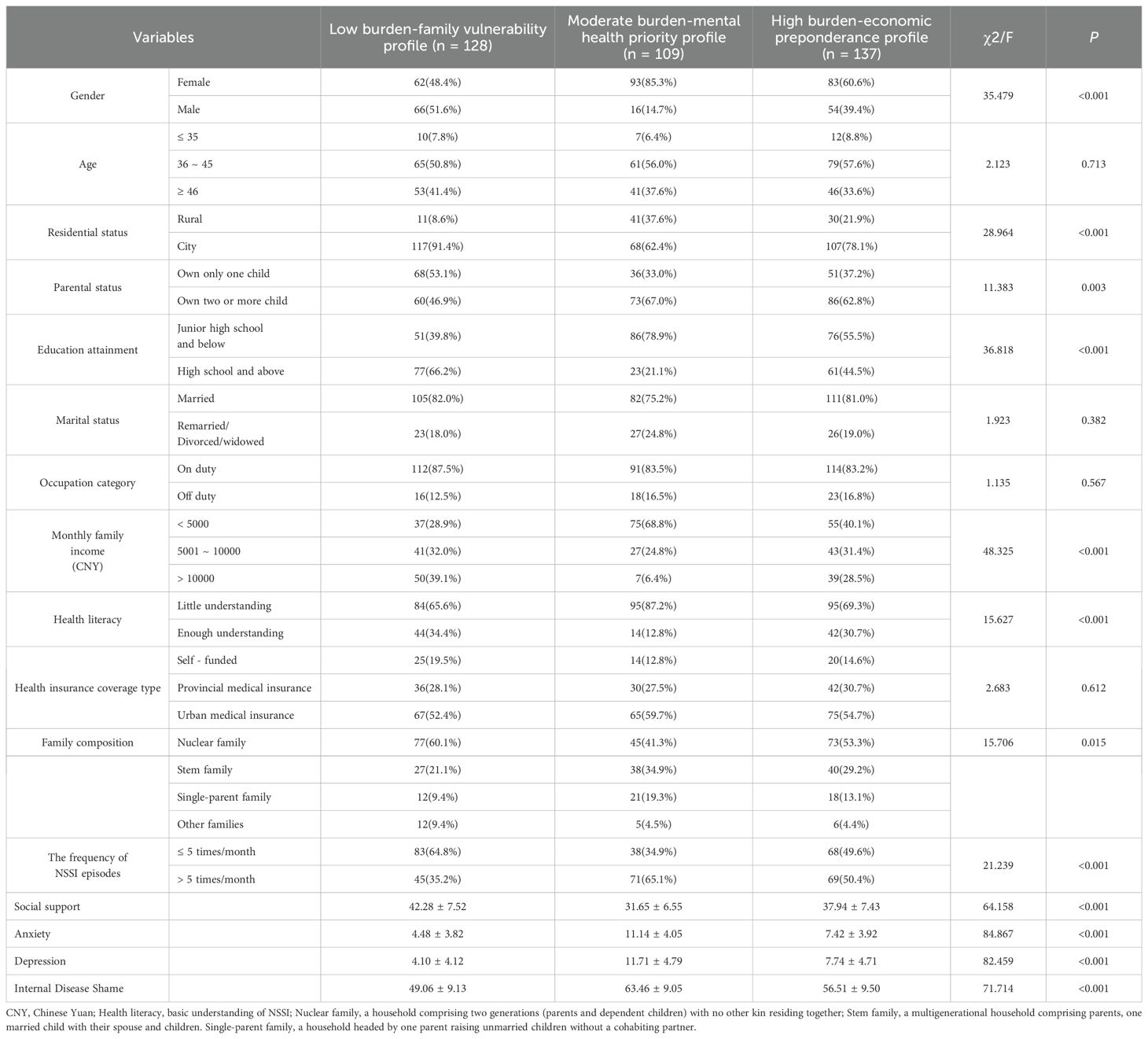
3.3 Socio-demographic characteristics of the participants
Analysis of 374 completed questionnaires revealed a caregiver cohort predominantly female (63.6%, n = 238), with 92.2% aged ≥ 35 years. The majority reported multiparous status (58.6% with ≥ 2 children) and urban residency (53.5%). Twelve variables, including demographic characteristics (gender, residential status, parental status, educational attainment, monthly household income, health literacy, family composition, and the frequency of NSSI episodes) and mental health indicators (social support, anxiety, depression, and internalized stigma), showed statistically significant differences among the three caregiver burden classes (p < 0.05), while other variables showed no statistical differences (p > 0.05), as shown in Table 2.
Profile nomenclature was derived from standardized scoring patterns across classes: Class 1 (n = 128) showed uniformly low domain scores except elevated family relationship strain, designated as “low burden-family vulnerability profile”. Class 2 (n = 109) presented a moderate overall burden with prominent psychological distress scores, labeled “moderate burden-mental health priority profile”. Class 3 (n = 137) exhibited clinically elevated burdens across all domains, particularly economic strain, categorized as “high burden-economic predominance profile”.
3.4 Predictor of latent profile membership
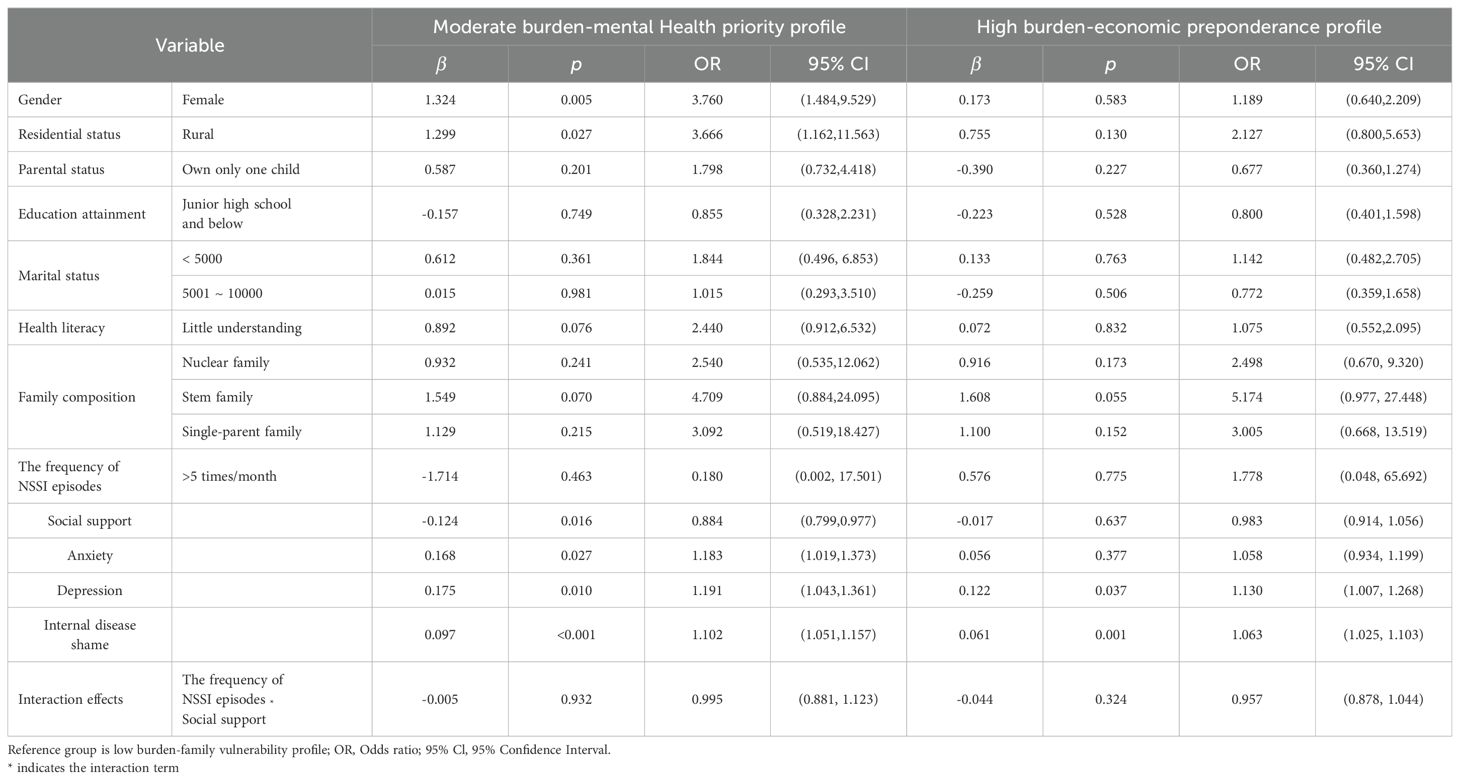
Using the profiles of latent classes of caregiver burden as the dependent variable, the low burden-family vulnerability profile as the reference, and the statistically significant factors in the univariate analysis as the independent variables. Multiple logistic regression analyses (Table 3) revealed significant associations between caregiver burden profiles and both demographic characteristics (gender, residential status) and mental health indicators (social support, anxiety, depression, internal disease shame) (all p < 0.05). Female caregivers, rural residents, diminished social support, and caregivers with higher anxiety were more likely to belong to the moderate burden profile. Heightened depression symptoms and stronger illness-related stigma were more likely to belong to both the moderate burden-mental health priority profile and the high burden-economic preponderance profile. Additionally, the stress-buffering hypothesis (33) posits that social support attenuates the psychological impacts of chronic stressors. It was hypothesized that caregivers’ social support would modify the association between adolescent NSSI frequency and caregiver burden. The NSSI frequency * social support interaction was tested across latent classes, the result showed no significant effects in either the moderate burden-mental health priority profile or the high burden-economic preponderance profile (p>0.05).
4 Discussion
LPA identified three distinct burden profiles among caregivers of adolescents with NSSI: low burden-family vulnerability profile (34.5%), moderate burden-mental health priority profile (36.6%), and high burden-economic preponderance profile (28.9%). This typology demonstrates substantial heterogeneity in caregiver burden manifestation, with 65.5% of caregivers of adolescents with NSSI experiencing moderate-to-severe burden levels, significantly exceeding the 38.2% prevalence observed in schizophrenia caregiver populations (34). The elevated burden may reflect the developmental specificities of adolescent care recipients, who concurrently face academic pressures and extended treatment durations (35).
This study revealed that female caregivers were more likely to belong to the moderate burden-mental health priority profile, consistent with existing evidence demonstrating that mothers of adolescents with NSSI report elevated depression, anxiety, and stress scores (36). Gender-based differences in personality traits may contribute to this pattern, as women generally demonstrate heightened emotional sensitivity and greater susceptibility to irritability compared to men (37). Furthermore, research indicates that female relational strengths foster stronger therapeutic alliances with adolescents, enhancing empathy-driven responses in NSSI care (37). These intensified emotional connections may predispose female caregivers to elevated anxiety and depressive symptoms secondary to caregiving stressors, thereby exacerbating familial burden (38). However, traditional Confucian values in China, which emphasize a gendered division of labor conceptualized as men dominate outside, and women dominate inside, continue to shape the distribution of economic pressures (39). Consequently, female caregivers are underrepresented in high burden-economic preponderance profile. These findings underscore the necessity for gender-specific psychological support interventions, particularly targeted emotion regulation training for female caregivers to mitigate negative affective states and optimize caregiving outcomes.
This study demonstrated that rural caregivers were more likely to belong to the moderate burden-mental health priority profile, aligning with findings reported by Siddiqui (40). This disparity may stem from systemic healthcare challenges in rural settings, including resource scarcity, underdeveloped healthcare infrastructure, and insufficient primary care personnel (41). Additionally, rural caregivers generally demonstrate lower educational attainment, constraining their capacity to obtain condition-specific knowledge and access evidence-based interventions (42). Heightened NSSI-related stigmatization in these populations may further predispose caregivers to anxiety, depression, and comorbid psychological distress (43). However, emerging evidence shows that China’s Rural Cooperative Medical Insurance system reduces out-of-pocket medical costs by 40%, effectively lowering caregivers’ financial stress (44). Consequently, rural caregivers are underrepresented in high burden-economic preponderance profile. These findings highlight the need for multisectoral approaches to improve early case detection and care. Coordinated implementation could reduce caregiver distress through timely adolescent mental health services and family support programs.
Social support was more likely to belong to the moderate burden-mental health priority profile. The social buffering theory (33) asserts that perceived social support mitigates stress responses by enhancing individuals’ adaptive capacities to societal challenges. From a family systems perspective, externally derived social support attenuates the disruptive effects of stressors on family dynamics. Robust social networks not only foster psychological resilience and somatic health maintenance but also reinforce self-efficacy and goal-directed behaviors through positive cognitive reinforcement (45). Consequently, implementing multidimensional support systems proactively reduces caregiver burden (46). Empowering caregivers to mobilize community resources, engage in peer support networks, and adopt help-seeking behaviors is critical (47). Concurrently, systemic integration of caregiver support into national healthcare frameworks further ensures sustainable burden alleviation through institutionalized assistance mechanisms.
This study revealed that elevated anxiety scores were more likely to belong to the moderate burden-mental health priority profile. Emerging neurobehavioral evidence links NSSI to addiction-like neuroplasticity, characterized by chronic engagement-induced dysregulation of hippocampal-amygdala circuits in adolescents, underlying both heightened suicide risk and caregiver distress potentiation (48). Mechanistically, recurrent NSSI episodes create cyclical caregiving crises through progressive symptom escalation requiring intensified monitoring and the emergence of treatment-resistant behavioral patterns (49). These clinical trajectories synergistically compound caregiver anxiety through anticipatory vigilance and resource depletion (50). This pathophysiology underscores the imperative for Multidisciplinary care models integrating trauma-informed psychotherapy with caregiver psychoeducation (51).
This study demonstrated that elevated caregiver depression scores were more likely to be both the moderate burden-mental health priority profile and the high burden-economic preponderance profile. Caregivers’ persistent concerns about NSSI’s impact on adolescent development trajectories, particularly regarding academic performance, vocational prospects, and interpersonal relationships, were found to progressively induce physical exhaustion, emotional distress, and impaired social functioning (45). Chronic exposure to these biopsychosocial stressors established cyclical patterns of depressive symptomatology, which amplified familial disease burden through psychosomatic mechanisms (10). The clinical complexity of NSSI when comorbid with psychiatric disorders (e.g., major depressive disorder, borderline personality disorder) necessitates multimodal interventions, particularly psychotherapy as a core therapeutic component (52). Within China’s healthcare system, the exclusion of psychotherapeutic services from national health insurance coverage creates substantial financial burdens for families through out-of-pocket payments (53). This economic strain is intensified when caregivers require extended leave or employment termination to accommodate treatment schedules, generating compounded financial and psychological consequences. These findings highlight the necessity for implementing standardized caregiver mental health screening protocols and evidence-based support systems.
This study demonstrated that the elevated caregiver internalized stigma levels were more likely to be categorized in both the moderate burden-mental health priority profile and the high burden-economic preponderance profile. Caregivers of adolescents with NSSI frequently develop chronic self-blame and shame due to recurrent symptom relapse cycles and pervasive societal stigma (54). This internalized stigma initiates a self-perpetuating cycle of social withdrawal, progressively eroding social support networks through avoidance behaviors (11). Stigmatized caregivers often demonstrate a pathological denial of adolescent psychopathology, actively resisting professional interventions to avoid perceived social judgment. Such maladaptive coping perpetuates unresolved distress and inadvertently reinforces NSSI behaviors via emotional contagion mechanisms (46). Multisector interventions should integrate psychoeducational programs targeting NSSI neurobiological mechanisms and psychosocial risk factors. Furthermore, empirical evidence demonstrates that caregivers derive substantial benefits from structured support networks, including family, friends, and peer support. Evidence from randomized trials indicates that structured peer support networks reduce internalized stigma and enhance adaptive coping strategies (55). Qualitative data further elucidate how caregiver peer alliances facilitate practical strategy exchange and cognitive restructuring of caregiving challenges (56), while fostering empowerment through collective resilience-building (57, 58).
Cultural contexts profoundly influence caregiver burden dynamics in adolescents with NSSI. In collectivist societies such as China, multigenerational households magnify caregiving responsibilities through filial piety traditions, while simultaneously exacerbating family shame associated with mental health stigma (59). Under patriarchal norms prevalent in China, female caregivers disproportionately internalize self-blame for NSSI through attribution to familial inadequacy, thereby compounding psychological distress (60).
5 Limitations
While this investigation provides notable insights, three constraints warrant acknowledgment. Primarily, the cross-sectional design precludes causal inferences regarding observed associations, and reliance on self-reported data introduces potential biases. Future studies could employ longitudinal designs with objective measures to delineate comprehensive burden trajectories. Secondly, the exclusive focus on caregivers within Sichuan Province raises concerns about geographical generalizability. Future studies should conduct multi-regional sampling across diverse geographical settings to validate findings beyond Sichuan Province. Furthermore, participant recruitment was restricted to caregivers of hospitalized adolescents, thereby potentially overlooking critical burden dimensions in community-dwelling caregivers who have not accessed clinical services. Future studies should expand recruitment to include non-clinical community-based caregivers of adolescents to capture underrepresented burden profiles.
6 Conclusion
This study demonstrates the heterogeneity of caregiver burden among adolescents with NSSI through LPA, identifying three distinct profiles: low burden-family vulnerability, moderate burden-mental health priority, and high burden-economic preponderance. These findings underscore the need for profile-specific interventions to address multidimensional burden drivers. Mental health professionals are encouraged to prioritize anxiety management and stigma reduction initiatives tailored for families. Policymakers may explore rural-focused partnerships while embedding caregiver psychosocial evaluations into NSSI care protocols. Caregivers may benefit from accessing digital peer-support platforms through real-time resource sharing. Future research should translate these findings into precision care models that address both psychological distress and structural disparities.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board of Chengdu Fourth Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
YQ: Data curation, Investigation, Writing – original draft. JL: Data curation, Formal Analysis, Investigation, Writing – original draft. JD: Resources, Supervision, Validation, Writing – review & editing. BY: Conceptualization, Supervision, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Cummings J. Nonsuicidal self-injury. Am J Nurs. (2023) 123:44–7. doi: 10.1097/01.NAJ.0000938732.60723.b9
2. De Luca L, Pastore M, Palladino BE, Reime B, Warth P, and Menesini E. The development of Non-Suicidal Self-Injury (NSSI) during adolescence: a systematic review and Bayesian meta-analysis. J Affect Disord. (2023) 339:648–59. doi: 10.1016/j.jad.2023.07.091
3. Plener PL, Kaess M, Schmahl C, Pollak S, Fegert JM, and Brown RC. Nonsuicidal self-injury in adolescents. Dtsch Arztebl Int. (2018) 115:23–30. doi: 10.3238/arztebl.2018.0023
4. Xiao Q, Song X, Huang L, Hou D, and Huang X. Global prevalence and characteristics of non-suicidal self-injury between 2010 and 2021 among a non-clinical sample of adolescents: a meta-analysis. Front Psychiatry. (2022) 13:912441. doi: 10.3389/fpsyt.2022.912441
5. Qu D, Wen X, Liu B, Zhang X, He Y, Chen D, et al. Non-suicidal self-injury in Chinese population: a scoping review of prevalence, method, risk factors and preventive interventions. Lancet Reg Health West Pac. (2023) 37:100794. doi: 10.1016/j.lanwpc.2023.100794
6. Liu X, Liu ZZ, and Jia CX. Repeat self-harm among Chinese adolescents: 1-year incidence and psychosocial predictors. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:1979–92. doi: 10.1007/s00127-021-02085-x
7. Hawton K, Bale L, Brand F, Townsend E, Ness J, Waters K, et al. Mortality in children and adolescents following presentation to hospital after non-fatal self-harm in the Multicentre Study of Self-harm: a prospective observational cohort study. Lancet Child Adolesc Health. (2020) 4:111–20. doi: 10.1016/S2352-4642(19)30373-6
8. Liu RT, Walsh R, Sheehan AE, Cheek SM, and Sanzari CM. Prevalence and correlates of suicide and nonsuicidal self-injury in children: a systematic review and meta-analysis. JAMA Psychiatry. (2022) 79:718–26. doi: 10.1001/jamapsychiatry.2022.1256
9. Duarte TA, Paulino S, Almeida C, Gomes HS, Santos N, and Gouveia-Pereira M. Self-harm as a predisposition for suicide attempts: a study of adolescents' deliberate self-harm, suicidal ideation, and suicide attempts. Psychiatry Res. (2020) 287:112553. doi: 10.1016/j.psychres.2019.112553
10. Wang X, Huang X, Huang X, and Zhao W. Parents' lived experience of adolescents' repeated non-suicidal self-injury in China: a qualitative study. BMC Psychiatry. (2022) 22:70. doi: 10.1186/s12888-022-03715-7
11. Fu X, Yang J, Liao X, Lin J, Peng Y, Shen Y, et al. Parents' Attitudes toward and experience of non-suicidal self-injury in adolescents: a qualitative study. Front Psychiatry. (2020) 11:651. doi: 10.3389/fpsyt.2020.00651
12. Utz RL and Warner EL. Caregiver burden among diverse caregivers. Cancer. (2022) 128:1904–6. doi: 10.1002/cncr.34171
13. Dada MU, Okewole NO, Ogun OC, and Bello-Mojeed MA. Factors associated with caregiver burden in a child and adolescent psychiatric facility in Lagos, Nigeria: a descriptive cross sectional study. BMC Pediatr. (2011) 11:110. doi: 10.1186/1471-2431-11-110
14. Spatuzzi R, Giulietti MV, Ricciuti M, Merico F, Fabbietti P, Raucci L, et al. Exploring the associations between spiritual well-being, burden, and quality of life in family caregivers of cancer patients. Palliat Support Care. (2019) 17:294–9. doi: 10.1017/S1478951518000160
15. Ribé JM, Salamero M, Pérez-Testor C, Mercadal J, Aguilera C, and Cleris M. Quality of life in family caregivers of schizophrenia patients in Spain: caregiver characteristics, caregiving burden, family functioning, and social and professional support. Int J Psychiatry Clin Pract. (2018) 22:25–33. doi: 10.1080/13651501.2017.1360500
16. Chien SC, Chang YH, Yen CM, Onthoni DD, Wu IC, Hsu CC, et al. Exploring concepts and trends in informal caregiver burden: systematic review using citation network and content analysis. Aging Clin Exp Res. (2023) 35:2873–85. doi: 10.1007/s40520-023-02582-w
17. Del-Pino-Casado R, Priego-Cubero E, López-Martínez C, and Orgeta V. Subjective caregiver burden and anxiety in informal caregivers: a systematic review and meta-analysis. PLoS One. (2021) 16:e0247143. doi: 10.1371/journal.pone.0247143
18. Baykal S, Karakurt MN, çakır M, and Karabekiroğlu K. An examination of the relations between symptom distributions in children diagnosed with autism and caregiver burden, anxiety and depression levels. Community Ment Health J. (2019) 55:311–7. doi: 10.1007/s10597-018-0343-8
19. Yu SH, Wang LT, Szutu WJ, Huang LC, Shen CC, and Chen CY. The caregivers' dilemma: Care burden, rejection, and caregiving behaviors among the caregivers of patients with depressive disorders. Psychiatry Res. (2020) 287:112916. doi: 10.1016/j.psychres.2020.112916
20. Shi Y, Shao Y, Li H, Wang S, Ying J, Zhang M, et al. Correlates of affiliate stigma among family caregivers of people with mental illness: a systematic review and meta-analysis. J Psychiatr Ment Health Nurs. (2019) 26:49–61. doi: 10.1111/jpm.12505
21. Kunwar D, Lamichhane S, Pradhan N, Shrestha B, Khadka S, Gautam K, et al. The study of burden of family caregivers of patients living with psychiatric disorders in remote area of Nepal. Kathmandu Univ Med J (KUMJ). (2020) 18:144–8. doi: 10.3126/kumj.v18i2.33224
22. Naldi L and Cazzaniga S. Research techniques made simple: latent class analysis. J Invest Dermatol. (2020) 140:1676–80. doi: 10.1016/j.jid.2020.05.079
23. Sinha P, Calfee CS, and Delucchi KL. Practitioner's guide to latent class analysis: methodological considerations and common pitfalls. Crit Care Med. (2021) 49:e63–79. doi: 10.1097/CCM.0000000000004710
24. Pai S and Kapur RL. The burden on the family of a psychiatric patient: development of an interview schedule. Br J Psychiatry. (1981) 138:332–5. doi: 10.1192/bjp.138.4.332
25. Huang J, Wei WX, Zheng PP, Tang T, Zhang PH, Long MY, et al. Factor analysis of the relationship between PANSS score and family burden of patients with schizophrenia. Brain Behav. (2021) 11:e2229. doi: 10.1002/brb3.2229
26. Xiao SY and Yang DS. Effects of social support on physical and mental health. Chin J Ment Health. (1987) 4:183–7.
27. Wu Y, Yan Z, Fornah L, Zhao J, and Wu S. The mediation effect of social support between stigma and social alienation in patients with stroke. Front Public Health. (2023) 11:1290177. doi: 10.3389/fpubh.2023.1290177
28. Spitzer RL, Kroenke K, Williams JB, and Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
29. Zhou Z, Wang Y, Feng P, Li T, Tebes JK, Luan R, et al. Associations of caregiving knowledge and skills with caregiver burden, psychological well-being, and coping styles among primary family caregivers of people living with schizophrenia in China. Front Psychiatry. (2021) 12:631420. doi: 10.3389/fpsyt.2021.631420
30. Kroenke K, Spitzer RL, and Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
31. Ritsher JB, Otilingam PG, and Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res. (2003) 121:31–49. doi: 10.1016/j.psychres.2003.08.008
32. Liu X, Yin M, Li Z, and Wang D. Psychosocial correlates of internalized stigma among Chinese individuals with severe mental illness. J Psychosoc Nurs Ment Health Serv. (2024) 62:37–44. doi: 10.3928/02793695-20230726-05
33. Cohen S and Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. (1985) 98:310–57. doi: 10.1037/0033-2909.98.2.310
34. Rahmani F, Roshangar F, Gholizadeh L, and Asghari E. Caregiver burden and the associated factors in the family caregivers of patients with schizophrenia. Nurs Open. (2022) 9:1995–2002. doi: 10.1002/nop2.1205
35. Zhao YL, Liu ZH, Li YY, Liu DL, and Yi JN. The lived experiences of parents providing care to young people who self-harm: a meta-aggregative synthesis of qualitative studies. Int J Ment Health Nurs. (2023) 32:402–19. doi: 10.1111/inm.13095
36. Tschan T, Schmid M, and In-Albon T. Parenting behavior in families of female adolescents with nonsuicidal self-injury in comparison to a clinical and a nonclinical control group. Child Adolesc Psychiatry Ment Health. (2015) 9:17. doi: 10.1186/s13034-015-0051-x
37. Compère L, Sperduti M, Gallarda T, Anssens A, Lion S, Delhommeau M, et al. Sex differences in the neural correlates of specific and general autobiographical memory. Front Hum Neurosci. (2016) 10:285. doi: 10.3389/fnhum.2016.00285
38. Gromatsky MA, Waszczuk MA, Perlman G, Salis KL, Klein DN, and Kotov R. The role of parental psychopathology and personality in adolescent non-suicidal self-injury. J Psychiatr Res. (2017) 85:15–23. doi: 10.1016/j.jpsychires.2016.10.013
39. Liu AY, Tong X, and Fu W. Gender division of household labor in dual-earner families: Economic dependence, gender ideology, or emotional expression. Society. (2015) 35(02):109–36. doi: 10.15992/j.cnki.31-1123/c.2015.02.006
40. Siddiqui S and Khalid J. Determining the caregivers' burden in caregivers of patients with mental illness. Pak J Med Sci. (2019) 35:1329–33. doi: 10.12669/pjms.35.5.720
41. Jaffe DH, Balkaran BL, Yue L, Mulhern-Haughey S, and Anjo J. The burden of caring for adults with depression and suicidal ideation in five large European countries: analysis from the 2020 National Health and Wellness Survey. BMC Psychiatry. (2021) 21:550. doi: 10.1186/s12888-021-03511-9
42. Tang J, Li G, Chen B, Huang Z, Zhang Y, Chang H, et al. Prevalence of and risk factors for non-suicidal self-injury in rural China: Results from a nationwide survey in China. J Affect Disord. (2018) 226:188–95. doi: 10.1016/j.jad.2017.09.051
43. Zhou SC, Zhou Z, Tang Q, Yu P, Zou H, Liu Q, et al. Prediction of non-suicidal self-injury in adolescents at the family level using regression methods and machine learning. J Affect Disord. (2024) 352:67–75. doi: 10.1016/j.jad.2024.02.039
44. Wang J, Chen L, Ye T, Zhang Z, and Ma J. Financial protection effects of modification of China's New Cooperative Medical Scheme on rural households with chronic diseases. BMC Health Serv Res. (2014) 14:305. doi: 10.1186/1472-6963-14-305
45. Mughal F, Troya MI, Dikomitis L, Tierney S, Corp N, Evans N, et al. The experiences and needs of supporting individuals of young people who self-harm: a systematic review and thematic synthesis. EClinicalMedicine. (2022) 48:101437. doi: 10.1016/j.eclinm.2022.101437
46. Whitlock J, Lloyd-Richardson E, Fisseha F, and Bates T. Parental secondary stress: the often hidden consequences of nonsuicidal self-injury in youth. J Clin Psychol. (2018) 74:178–96. doi: 10.1002/jclp.22488
47. Boritz TZ, Sheikhan NY, Hawke LD, Mcmain SF, and Henderson J. Evaluating the effectiveness of the Family Connections program for caregivers of youth with mental health challenges, part I: a quantitative analysis. Health Expect. (2021) 24:578–88. doi: 10.1111/hex.13205
48. Pang X, Wu D, Wang H, Zhang J, Yu Y, Zhao Y, et al. Cortical morphological alterations in adolescents with major depression and non-suicidal self-injury. NeuroImage Clin. (2024) 44:103701. doi: 10.1016/j.nicl.2024.103701
49. Peng B, Wang R, Zuo W, Liu H, Deng C, Jing X, et al. Distinct correlation network of clinical characteristics in suicide attempters having adolescent major depressive disorder with non-suicidal self-injury. Transl Psychiatry. (2024) 14:134. doi: 10.1038/s41398-024-02843-w
50. Xia Q, Zhang Y, and Huang X. Psychological well-being and associated factors among parents of adolescents with non-suicidal self-injury: a cross-sectional study. Front Psychiatry. (2023) 14:1253321. doi: 10.3389/fpsyt.2023.1253321
51. Featherston R, Barlow J, Song Y, Haysom Z, Loy B, Tufford L, et al. Mindfulness-enhanced parenting programmes for improving the psychosocial outcomes of children (0 to 18 years) and their parents. Cochrane Database Syst Rev. (2024) 1:CD012445. doi: 10.1002/14651858.CD012445.pub2
52. Bahji A, Pierce M, Wong J, Roberge JN, Ortega I, and Patten S. Comparative efficacy and acceptability of psychotherapies for self-harm and suicidal behavior among children and adolescents: a systematic review and network meta-analysis. JAMA Netw Open. (2021) 4:e216614. doi: 10.1001/jamanetworkopen.2021.6614
53. Yue JL, Li N, Que JY, Hu SF, Xiong NN, Deng JH, et al. Workforce situation of the Chinese mental health care system: results from a cross-sectional study. BMC Psychiatry. (2022) 22:562. doi: 10.1186/s12888-022-04204-7
54. Curtis S, Thorn P, Mcroberts A, Hetrick S, Rice S, and Robinson J. Caring for young people who self-harm: a review of perspectives from families and young people. Int J Environ Res Public Health. (2018) 15(5):950. doi: 10.3390/ijerph15050950
55. Burke EM, Pyle M, Machin K, and Morrison AP. Providing mental health peer support 2: Relationships with empowerment, hope, recovery, quality of life and internalised stigma. Int J Soc Psychiatry. (2018) 64:745–55. doi: 10.1177/0020764018810307
56. Qin Y, Wu D, Liu J, Peng J, and Li C. Perspectives of parents of adolescents with repeated non-suicidal self-injury on sharing their caretaking experiences with peers: a qualitative study. Front Psychiatry. (2023) 14:1237436. doi: 10.3389/fpsyt.2023.1237436
57. Nguyen J, Goldsmith L, Rains LS, and Gillard S. Peer support in early intervention in psychosis: a qualitative research study. J Ment Health. (2022) 31:196–202. doi: 10.1080/09638237.2021.1922647
58. King AJ and Simmons MB. The Best of Both Worlds": Experiences of young people attending groups co-facilitated by peer workers and clinicians in a youth mental health service. Early Interv Psychiatry. (2023) 17:65–75. doi: 10.1111/eip.13293
59. Meheli S and Banerjee D. Revisiting social stigma in non-suicidal self-injury: a narrative review. Consort Psychiatr. (2022) 3:6–18. doi: 10.17816/CP196
Keywords: non-suicidal self-injury, adolescents, caregivers, caregiver burden, latent profile analysis
Citation: Qin Y, Liu J, Duan J and Yang B (2025) Profiles of caregiver burden among adolescents with non-suicidal self-injury: a latent profile analysis. Front. Psychiatry 16:1581640. doi: 10.3389/fpsyt.2025.1581640
Received: 22 February 2025; Accepted: 24 April 2025;
Published: 19 May 2025.
Edited by:
Shin-ichi Ishikawa, Doshisha University, JapanReviewed by:
Yuko Mori, University of Turku, FinlandMohd Radzi Tarmizi A. Halim, University of Malaysia Terengganu, Malaysia
Copyright © 2025 Qin, Liu, Duan and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiming Duan, MTA1OTAxNzY5OEBxcS5jb20=; Bo Yang, MTM3NjI1NTM5MUBxcS5jb20=
‡ORCID: Yuan Qin, orcid.org/0000-0001-5544-159X
 Yuan Qin
Yuan Qin Jiao Liu2,3
Jiao Liu2,3