Abstract
Background:
Personality pathology and childhood trauma are known to be associated with substance use disorders (SUDs) in general and opioid use disorders (OUDs) in particular but the complex relationship is only partially understood. Investigating personality functioning in patients with OUD is crucial for gaining a deeper understanding of the emergence and course of illness as well as for planning appropriate treatment strategies.
Aims:
To empirically investigate personality functioning in a sample of patients in opioid substitution treatment and to examine the associations between personality functioning, injecting drug use (IDU) and childhood trauma.
Methods:
In a cross-sectional design, 31 patients with OUDs currently in an opioid substitution treatment program were assessed with the revised Structured Interview for Personality Organization, the Structured Clinical Interview for DSM-5, the Addiction Severity Index – Lite and the Childhood Trauma Questionnaire. The sample consisted of 80.6% male and 19.4% female patients.
Results:
The large majority (93.5%) of participants were diagnosed with severe impairment of personality functioning. Impaired personality functioning and higher rates of reported childhood trauma were associated with a younger age of onset of IDU and a greater number of years of IDU. Level of personality functioning showed a stronger statistical association with both IDU and the number of diagnosed personality disorders than reported childhood trauma.
Conclusions:
OUDs are associated with severely impaired personality functioning. Assessment of personality functioning can provide important information for treatment strategies in addition to categorical psychiatric diagnoses and trauma history.
1 Introduction
Opioid use disorders (OUDs) are serious, often chronic mental disorders characterized by problematic opioid use leading to significant impairment, distress, high mortality risk and substantial impacts on individual health and national healthcare systems (1–3).
In many cases, OUDs are connected to polysubstance use and injecting drug use (IDU) (2, 4). The complex etiology of substance use disorders (SUDs) include biological, genetic, sociocultural and psychological factors (5, 6).
Among the psychological factors, early adverse experiences, particularly childhood trauma, have been increasingly recognized as a critical factor in the development of severe mental disorders, including SUDs (7).
Patients with SUDs frequently describe experiences of severe childhood traumatization (8) and for OUDs, research suggests that more severe childhood trauma is associated with a higher risk of earlier onset of opioid use and IDU (9–12).
In this context, personality pathology has emerged as key psychological factor in SUDs, with growing evidence suggesting an association between certain personality traits and disorders and the occurrence and persistence of substance use disorders (11, 13–17).
Research on co-morbidity of SUDs and other mental disorders has shown elevated prevalence rates of Antisocial and Borderline Personality Disorder (PD) among OUD patients (11, 13, 14). Furthermore, studies examining personality traits in this population revealed higher scores in facets of Neuroticism and lower scores in facets of Conscientiousness, Extraversion, and Agreeableness (15, 16).
Against this background, the concept of “personality functioning” (PF) has gained increasing relevance as a dimensional approach to understanding personality-related vulnerability in psychopathology in general (18, 19), also offering a more nuanced framework for assessing the underlying psychological mechanism in patients with SUDs.
The importance of this concept was underscored by the introduction of the Alternative Model for Personality Disorders in DSM-5 and the revised PD classification in ICD-11, both of which define disturbances in self (identity and self-direction) and interpersonal (intimacy and empathy) functioning as the core features of personality pathology (18, 19).
These models of PF converge with long-standing psychodynamic conceptualizations (20) as in the object relations model developed by Kernberg and colleagues.
Kernberg’s model of personality organization (= functioning) offers a developmentally informed psychodynamic framework for understanding manifestations of personality pathology, particularly in light auf early traumatic experiences. Central to this model is the notion that early relational experiences play a critical role in the internalization of “object relations” and the organization of the self. When early attachment relationships – particularly those involving neglectful, abusive or in other ways traumatic experiences – fail to support the integrations of intense affective experiences, individuals may rely on “primitive” defense mechanisms, such as splitting, leading to impairments in identity integration (identity diffusion), in the perception of the self and others and consequently to difficulties in building healthy relationships and deficits in affect regulation. Kernberg’s theory provides an in-depth understanding of how early trauma and relational disruptions can shape patterns of impaired psychological functioning (21, 22).
The model comprises three basic levels of PF: neurotic, borderline, and psychotic personality organization (23, 24). These levels of personality organization (i.e., PF) are distinguished by differences in identity integration, maturity of defense mechanisms, the capacity for reality testing, and the integration of aggression and moral values. A neurotic level of PF is defined by an integrated identity, relatively mature defense mechanisms (e.g. anticipation), and intact reality testing. Borderline personality organization is characterized by an unintegrated identity (identity diffusion) and the use of primitive defense mechanisms (mainly splitting and projective identification) with intact capacity for reality testing. Based on Kernberg’s model of PF, the “Structured Interview for Personality Organization” (STIPO) was developed, a semi-structured Interview allowing an in-depth assessment of personality pathology (25, 26). A revised and shortened version, the STIPO-R, was subsequently introduced (26). Studies investigating personality pathology among opioid and polysubstance use samples found severe impairments across domains of PF [27, 28, 29). In a study by Fuchshuber et al. (30) deficits in PF were found to mediate the relationship between childhood trauma and addictive behaviors. Moreover, a greater number of comorbid PDs was found to be associated with more severe impairment in PF (9, 29, 31).
The concept of PF provides a scientifically grounded and clinically meaningful framework for examining personality pathology in patients with SUDs and related behaviors (e.g., IDU). It allows for a more comprehensive assessment of psychological functioning that extends beyond descriptive diagnoses and reports of childhood trauma.
2 Aims
The main aim of this study is to empirically investigate PF using the STIPO-R in individuals with OUDs currently in a substitution program and to examine the associations between PF, IDU and childhood trauma. We expected significant correlations between all STIPO-R domains, childhood trauma severity and age of the first IDU, as well as number of years of IDU. Moreover, we investigated the extent to which deficits in PF and childhood trauma are independently associated with IDU and with the number of diagnosed PDs via hierarchical multiple regression analysis.
3 Methods
The study employed a cross-sectional design. The study project was approved by the Ethics Commission of the Medical University of Vienna. Written informed consent was obtained by all participants.
All interviews were conducted by certified psychotherapists or psychotherapists in advanced stages of psychotherapy training, who received specific training in the administration of each interview. Prior to the beginning of data collection, each interviewer completed a supervised training case involving the full interview process. The results and the procedure were then reviewed and discussed within the research group to ensure consistency in administration and standardized application of all instruments.
The interview process lasted 4 to 5 hours and was divided into 2 to 3 sessions, depending on the participant’s preferences. Breaks were provided whenever needed.
3.1 Participants
31 patients in opioid substitution treatment were recruited at “Suchthilfe Wien” in Vienna. Participants had to meet the following inclusion criteria: over 18 years old, DSM-5 diagnosis of OUD, sufficient German language skills, and cognitive ability to understand the interviews and questionnaires. Patients with psychotic disorders, current intoxication, or significant cognitive impairment were excluded. Psychotic disorders were assessed using the SCID-5. Acute intoxication was evaluated through conversation and clinical observation at the start of the interview. If intoxication was evident, the interview session was rescheduled or terminated to ensure valid participation. Cognitive impairment was informally screened during consent and early interview stages, with difficulties in understanding or engagement indicating possible impairment. Given the sample’s characteristics (OUDs with frequent polysubstance use), some residual substance effects were expected. Exclusion criteria focused pragmatically on acute impairment that would compromise ethical and valid participation.
Sampling followed a referral-based approach: social workers at Suchthilfe Wien were informed about the study and referred patients who appeared to meet the inclusion criteria. A total of 68 individuals were referred and initially agreed to participate in the study. Of these, 30 participants (44.12%) fully completed both the interviews and questionnaires, while one participant (1.47%) completed the interview but not the questionnaires. 15 individuals (22.06%) either lost interest in participation or were unavailable, for example due to hospitalization. 8 participants (11.76%) did not appear for their first scheduled appointment. In ten cases (14.71%), participants did not return after their first appointment and dropped out of the interview process. Additionally, in four instances (5.88%), interviewers determined that the inclusion criteria were not actually met – due to reasons such as active psychosis, not being enrolled in an opioid substitution program, intoxication, or being too adversely affected by the interview process. Demographic data were collected using a brief, self-constructed questionnaire.
Each participant received a 50 Euro voucher as compensation, balancing acknowledgment of their time without exerting undue influence on their decision to participate.
3.2 Measures
3.2.1 Structured interview for personality organization-revised
The Structured Interview for Personality Organization (STIPO) is a semi-structured interview assessing personality functioning based on Kernberg’s object relations model (25, 26). The most recent version, the revised STIPO (STIPO-R), consists of 55 items and assesses the following domains and sub-domains: 1. Identity: 1.A. Capacity to invest, 1.B. Sense of self - Coherence and continuity, 1.C. Representation of others; 2. Object relations: 2.A. Interpersonal relationships, 2.B. Intimate relationships and sexuality, 2.C. Internal working model of relationships, 3. Defense: 3.A. Primitive defenses, 3.B. Higher-level defenses; 5. Aggression: 5.A. Self-directed aggression, 5.B. Other-directed aggression 6. Moral values. It also includes a rating of narcissism. The single-item rating is made by the interviewer on a three-point scale with operationalized descriptions for each rating. For each (sub)dimension a clinical rating can be made on a 1-to-5 scale, allowing for a clinical assessment based on operationalizations of the domains. From the clinical ratings, an overall level of personality organization can be determined. Six different levels of personality organization are provided for the overall rating, ranging from a normal level to severely impaired PF: (1) Normal, (2) Neurotic 1, (3) Neurotic 2, (4) Borderline 1, (5) Borderline 2, and (6) Borderline 3 (26). For this study, the 1–5 clinician ratings across the six main domains, along with the overall rating of level of PF (scale range: 1–6), were used for statistical analysis.
Satisfactory reliability and validity have been demonstrated for the STIPO (32–34). For this study, the intraclass correlation coefficient (ICC) among the interviewers for the overall STIPO level was.90.
3.2.2 Structured clinical interview for DSM-V
The Structured Clinical Interview for DSM-5 (SCID-5) is the official instrument for the diagnosis of psychiatric disorders according to DSM-5. The semi-structured interview contains questions addressing every single diagnostic criterion of the psychiatric disorders of the DSM-5 (35, 36). For the present study, the German versions of SCID-5-PD and SCID-5-CV were used (37, 38). The variable ‘number of PDs’ was obtained using the SCID-5-PD by summing the categorical PD diagnoses for each participant.
3.2.3 Addiction severity index-lite
The Addiction Severity Index-Lite (ASI-Lite) is a shortened version of the Addiction Severity Index (ASI), a semi-structured interview that assesses substance use-related behaviors and problems over a lifetime and the past 30 days (39). The English ASI-Lite has psychometric properties similar to the original ASI (40). A slightly abbreviated German version was used, including an added section on IDU from the original ASI (41). Participants’ reports on IDU were utilized for statistical analyses.
3.2.4 Childhood trauma questionnaire
The Childhood Trauma Questionnaire (CTQ), in its short version (42), is the most widely used self-report instrument for assessing childhood trauma, consisting of 28 items across five scales: Emotional Abuse, Physical Abuse, Sexual Abuse, Emotional Neglect, and Physical Neglect. The German translation has validated psychometric properties (43). Each subscale score ranges from 5 to 25, based on five items rated on a 5-point scale Likert scale. The total score ranges from 25 to 125, summing the five abuse/neglect subscales (minimization items are excluded from the total score).
Internal consistency was excellent for the CTQ total score (Cronbach’s α = .95), and excellent to good for the Emotional Abuse (α = .90), Physical Abuse (α = .98), Sexual Abuse (α = .89) and Emotional Neglect (α = 0.90) subscales. The Physical Neglect subscale showed lower internal consistency (α = .50). This finding is consistent with previous research indicating that the Physical Neglect subscale tends to show lower internal consistency compared to the other subscales (44, 45).
3.3 Statistics
Spearman-Rho-Correlation analyses were conducted to explore the relationship between PF and childhood trauma, PF and IDU and childhood trauma and substance use (one-sided). Multiple hierarchical regression analyses were conducted to examine the predictive value of PF and the CTQ score as independent variables for years of IDU, age of first IDU and total number of PD diagnoses. Multicollinearity was tested using Variance Inflation Factors (VIF). Independence of errors was assessed with the Durbin-Watson-test. All assumptions were met. Analyses were carried out with SPSS 27.
4 Results
4.1 Sample characteristics
The sample consisted of 31 participants aged between 29 and 66 years (mean = 42.84, SD = 10.05). 80.6% of participants identified as male, 19.4% as female. 90.3% of participants were born in Austria. Most of the sample reported being unemployed (87.1%) and not having a high school diploma (93.5%). More than half of the participants reported being single (64.5%) or divorced (16.1%) at the time of interviewing, 35.5% reported having children.
4.2 SCID-5 diagnoses
All participants fulfilled criteria for OUD, and 87.10% of participants were diagnosed with one or more PDs. A detailed list of all SCID-5 diagnoses is shown in Table 1.
Table 1
| SCID-5 Diagnoses | n | % |
|---|---|---|
| Substance Use Disorders | ||
| Opioids (total) | 31 | 100 |
| severe | 31 | 100 |
| Alcohol (total) | 7 | 22.58 |
| mild | 2 | 6.45 |
| moderate | 3 | 9.68 |
| severe | 2 | 6.45 |
| Sedatives, Tranquilizers, Hypnotics (total) | 4 | 12.90 |
| severe | 4 | 12.90 |
| Cannabis (total) | 12 | 38.71 |
| mild | 3 | 9.68 |
| moderate | 5 | 16.13 |
| severe | 4 | 12.90 |
| Stimulants (total) | 10 | 32.26 |
| mild | 2 | 6.45 |
| moderate | 7 | 22.58 |
| severe | 1 | 3.23 |
| Hallucinogens (total) | 1 | 3.23 |
| severe | 1 | 3.23 |
| Depressive Disorders & Bipolar and Related Disorders | ||
| Major Depressive Disorder (MDD) | 6 | 19.35 |
| MDD partial remission | 4 | 12.90 |
| MDD full remission | 6 | 19.35 |
| Bipolar 1 Disorder (current episode: hypomanic) | 1 | 3.23 |
| Anxiety Disorders & Trauma- and Stressor-Related Disorders | ||
| Panic Disorder | 1 | 3.23 |
| Social Anxiety Disorder | 3 | 9.68 |
| Generalized Anxiety Disorder | 5 | 16.13 |
| Posttraumatic Stress Disorder | 13 | 41.94 |
| current | 9 | 29.03 |
| Past | 4 | 12.90 |
| Personality Disorders | ||
| Avoidant | 4 | 12.90 |
| Dependent | 1 | 3.23 |
| Obsessive-Compulsive | 1 | 3.23 |
| Paranoid | 3 | 9.68 |
| Schizoid | 3 | 9.68 |
| Narcissistic | 1 | 3.23 |
| Borderline | 8 | 25.81 |
| Antisocial | 9 | 29.03 |
| Other specified PD | 11 | 35.48 |
| Of those: with antisocial traits | 8 | 25.81 |
| Total number of PD diagnoses | ||
| 0 | 4 | 12.90 |
| 1 | 16 | 51.61 |
| 2 | 8 | 25.81 |
| 3 | 3 | 9.68 |
SCID-diagnoses.
4.3 Substance use
All participants were in opioid substitution treatment. 16.13% of patients were treated with levomethadone, 3.23% with methadone, and 80.65% with extended-release morphine. There is a relatively high prevalence of polysubstance use in the study sample (cf. Table 1). On average, participants used more than one substance per day over a period of 14.58 years (SD = 11.10), and on 17.77 days out of the last 30 days (SD = 13.24). Substances most used in the last 30 days were sedatives/tranquilizers/hypnotics (mean = 19.28 days, SD = 14.60), followed by cannabinoids (mean = 13.35 days, SD = 13.26). The mean age of the first consumption of heroin was 19.17 (SD = 4.38).
Concerning the issue of IDU (referring to the intravenous consumption of any substance, including substitution medications), only 4 participants (12.90%) reported having never injected any substance, the majority (n = 27, 87.10%) confirmed engaging in IDU. The mean age of the first drug injection was 21.67 (SD = 6.13), with an average duration of IDU of 13.90 years (SD = 11.23). Over the last 30 days, participants reported an average of 11.85 days with IDU (SD = 2.52).
4.4 Level of PF
Most participants were diagnosed with a borderline level of PF (93.50%): 32.30% with “Borderline 1”, 35.50% with “Borderline 2” and 25.80% with “Borderline 3”. Only two participants (6.50%) were diagnosed with “Neurotic 2”. Mean values for the STIPO-R domains are shown in Figure 1.
Figure 1
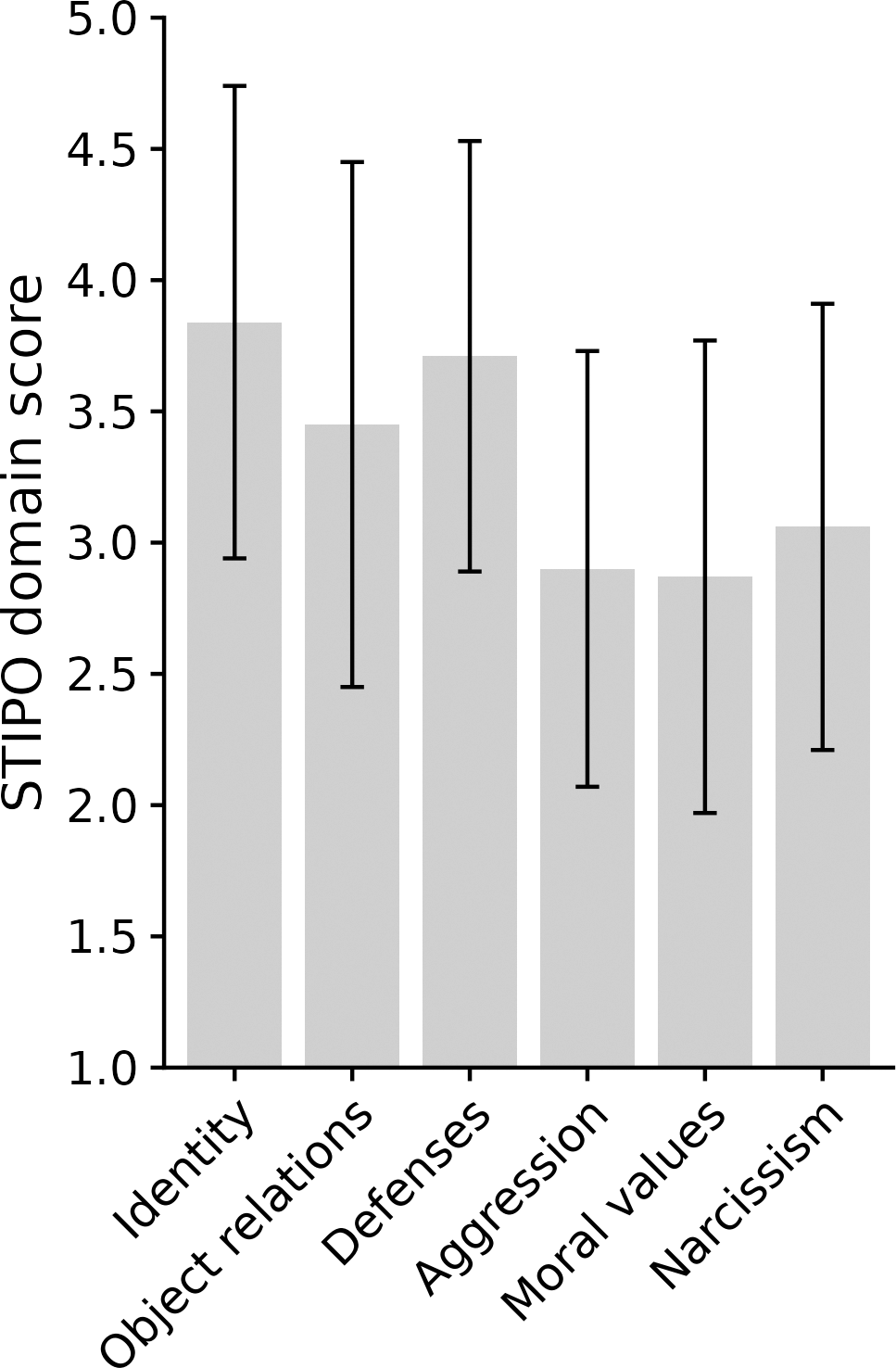
Mean values for the STIPO-R domains (scale-range = 1-5) with standard deviations shown as error bars with 95 % confidence intervals are displayed. Higher values indicate higher levels of pathology.
4.5 Childhood trauma
Results concerning (remembered) childhood traumatization are shown in Table 2. Scores in the different subdomains are grouped into four categories: no traumatization, low to moderate, moderate to severe, and severe to extreme traumatization (42).
Table 2
| CTQ Scale | None | Low - moderate | Moderate-severe | Severe-extreme | |
|---|---|---|---|---|---|
| M (SD) | n (%) | n (%) | n (%) | n (%) | |
| Emotional Abuse | 13.27 (6.23) | 11 (35.48) | 3 (9.67) | 5 (16.13) | 11 (35.48) |
| Physical Abuse | 10.67 (7.39) | 18 (58.10) | 0 (0) | 1 (3.23) | 11 (35.48) |
| Sexual Abuse | 7.13 (3.50) | 20 (64.52) | 1 (3.23) | 5 (16.13) | 4 (12.90) |
| Emotional Neglect | 13.97 (5.47) | 7 (22.58) | 10 (32.33) | 4 (12.90) | 9 (29.03) |
| Physical Neglect | 10.37 (3.71) | 8 (25.81) | 5 (16.13) | 9 (29.03) | 8 (25.81) |
| CTQ Total Score | 55.40 (22.17) |
CTQ subdomain scores and distribution across CTQ categories for trauma severity.
Missing: n =1.
When summarizing data categorized “low/moderate to extreme” as positive exposure to childhood traumatization, 61.28% of the participants report emotional abuse, 38.71% physical abuse, 32.26% sexual abuse, 74.26% emotional neglect and 70.97% physical neglect.
4.6 The relationship between levels of PF and childhood trauma
The overall level of PF (higher ratings indicating higher levels of pathology) showed moderate to strong significant positive correlations with the CTQ total score and almost all subdomains of the CTQ, except for “emotional neglect” (detailed results are given in Table 3).
Table 3
| Emotional abuse | Physical abuse | Sexual abuse | Emotional neglect | Physical neglect | CTQ total score | |
|---|---|---|---|---|---|---|
| Level of PF | .41* | .54** | .34* | .19 | .47** | .41* |
| Identity | .42* | .51** | .32* | .22 | .48** | .42* |
| Object Relations | .41* | .40* | .37* | .20 | .41* | .40* |
| Defenses | .36* | .42* | .29 | .16 | .48** | .38* |
| Aggression | .42* | .48** | .25 | .15 | .25 | .34* |
| Moral Values | .28 | .47** | .40* | -.10 | .17 | .24 |
| Narcissism | .37* | .43** | .30 | .03 | .31* | .32* |
Spearman-Rho correlations between STIPO-R domains and CTQ scales.
** ≤ 0.01, * ≤ 0.05 (one-sided).
4.7 The relationship between levels of PF and IDU
The overall Level of PF (higher values indicating higher levels of pathology) was significantly negatively correlated with “age at first IDU” (r = -.52, p <.01) and significantly positively correlated with “years of IDU” (r = .49, p <.01).
Regarding the STIPO-R dimensions, results revealed significant negative correlations between “age at first IDU” and increased pathology in the domain of “identity” (r = -.48, p <.05) and between “age at first IDU” and deficits in the domain of “moral values” (r = -.47, p <.05).
“Years of IDU” showed a significant positive correlation with higher levels of pathology in the following domains: “identity” (r = .45, p <.05), “defenses” (r = .40, p <.05) “aggression” (r = .42, p <.05) and “narcissism” (r = .39, p <.05). Correlations between the other STIPO-R domains and the IDU variables were non-significant.
4.8 The relationship between childhood trauma and IDU
“Age at first IDU” showed significant negative correlations with the CTQ total score (r = -.36, p <.05), “physical abuse” (r = -.43, p <.05), “sexual abuse” (r = -.43, p <.05), and with “physical neglect” (r = -.35, p <.05).
“Years of IDU” positively correlated with the CTQ total score (r = .33, p <.05), “physical abuse” (r = .43, p <.01) and “emotional abuse” (r = .35, p <.05).
“IDU in the last 30 days” only sowed a positive correlation with “emotional neglect” (r = .37, p <.05). Correlations between the other CTQ scales and the IDU variables were non-significant.
4.9 Regression models of “years of IDU” and “age at first IDU”
Two hierarchical multiple regression analyses were conducted to assess the predictive value of PF and CTQ scores for years of IDU and age at first IDU (Table 4). In both models, PF proved to be the stronger predictor for the respective IDU variables than childhood trauma.
Table 4
| Years of injecting drug use | Age of first injecting drug use | |||||
|---|---|---|---|---|---|---|
| Models and predictor variables | β | R2 | ΔR | β | R2 | ΔR2 |
| Regression Model 1 | .13* | .13* | .07 | .07 | ||
| CTQ Total Score | .36* | -.26 | ||||
| Regression Model 2 | .29* | .16* | .23* | .16* | ||
| CTQ Total Score | .17 | -.10 | ||||
| STIPO-R Level of PF | .44* | -.43* | ||||
Regression analyses summary.
* ≤ 0.05.
4.10 Number of PDs
The total number of PD diagnoses showed a significant positive correlation with level of PF (r = .77, p <.05). In a multiple regression analysis, PF was shown to be a stronger predictor of the number of PD diagnoses than childhood trauma (cf. Table 5).
Table 5
| Models and predictor variables | B | SE B | β | R2 | ΔR2 |
|---|---|---|---|---|---|
| Regression Model 1** | .24** | .24** | |||
| (Intercept) CTQ total score |
.30 .02 |
.37 .01 |
.49** |
||
| Regression Model 2** | .59** | .35** | |||
|
-2.03 .01 .61 |
.56 .01 .13 |
.20 .66** |
Regression analysis predicting number of PDs.
** ≤ 0.01, * ≤ 0.05.
5 Discussion
The results of this study demonstrate that IDU is associated with childhood trauma as well as impairments in PF as measured by the STIPO-R.
Consistent with studies assessing PF in SUD, and especially OUD or polysubstance use samples, most of the participants of this study showed moderate to severe deficits in PF (27–29).
Also, high rates of PDs, especially Antisocial PD and Borderline PD, were observed, alongside elevated reports of childhood trauma, consistent with other findings in SUD patients (46). In line with previous research, a greater number of PDs was associated with increased impairment in PF (29, 31).
Results of the present study show that a younger age at the onset of IDU and a greater number of years of IDU are associated with higher rates of reported childhood trauma and with higher levels of personality pathology. However, in multiple regression analyses, PF demonstrated a stronger statistical association with IDU and the number of diagnosed PDs, accounting for a greater proportion of explained variance than the CTQ score. This finding corresponds to results by Fuchshuber et al. which suggested a mediating role of PF (assessed with the IPO) in the association between childhood trauma and addictive behaviors (30).
In the present study, PF was operationalized with the STIPO-R, an interview based on psychoanalytic object relations theory. Following the central premises of this theory, psychological functioning develops in interactions with early “objects”, i.e. significant others.
Traumatic experiences, defined as overwhelming events that disrupt the psyche’s protective barriers and coping mechanisms, can distort internalized images of self and others and lead to maladaptive defense strategies (23, 24, 47). Severe childhood trauma fosters the internalization of dysfunctional object relations, negatively impacting development and resulting in deficits in PF (23, 24, 48). These deficits are associated with the manifestation of symptoms and mental disorders (31, 49–51).
The STIPO-R domains allow for a nuanced understanding of personality pathology in OUDs. Deficits in the domain of “identity” are associated with an unstable and poorly integrated sense of self and significant others and corresponding disturbances in affect regulation. Substance use might help in the regulation of self-perception and self-worth and in dealing with intense and overwhelming emotional states (23, 52, 53). Disturbances in the dimension of “object relations” point to unstable, fragmented, and negative internal representations of others, leading to severe difficulties in building and maintaining relationships (23, 24). Substance use can function as a coping strategy in the face of disappointments stemming from human interactions, defending against unbearable wishes for and fear of dependency. Severe personality pathology is associated with the use of primitive defense mechanisms like denial, splitting, idealization/devaluation, or projective identification (24, 54). Especially the mechanisms of denial of internal and external reality and of splitting have been emphasized in psychodynamic literature on substance use (51, 55). Furthermore, these defense mechanisms can be reinforced by the pharmacological effects of drugs (55). As has been pointed out in the “self-medication-hypothesis”, substance use can be understood as a mean to alleviate painful affective states, providing a sense of control (52). Considering the STIPO-R domain of “aggression”, drug use and its consequences can also be understood as a form of self-destructive behavior, leading to serious health problems and severe self-neglect (23, 56). The relation between substance use and aggression directed towards others is complex: some substances, but also severe craving and withdrawal symptoms can lead to disinhibition and increased display of aggressive behaviors. However, some individuals among SUD samples seem to show a low control of impulses and high readiness for aggressive actions as part of their personality organization (23). These considerations also touch the domain of “moral values” assessed by the STIPO-R. Because many substances are illegal, maintaining a socially accepted drug addiction is impossible, and being labeled a ‘drug addict’ is stigmatized, often leading to a downward social spiral. It seems crucial to not only assess observable behavioral aspects of illicit actions but to obtain information about the underlying dimensions of PF (e.g., information on the ability to reflect on behavior and articulate and tolerate feelings of guilt).
From psychodynamic perspectives, opioid use in particular has been linked to regressive tendencies, such as the desire for a symbiotic state due to unmet basic needs for safety and closeness, and has been discussed as a defense against cruel self-judgment, resulting feelings of guilt and shame, and potential psychotic disintegration (17).
Considering the application of drugs, IDU takes on a special position: due to its considerable risks, it can be viewed as a form of self-destructive behavior, but it can also be understood as serving a very “existential” purpose: like self-harming behaviors such as cutting, it may be used to release unbearable tension, solidify a sense of self and identity and provide a feeling of control and safety (57, 58).
Regarding the age of onset of IDU, it is important to note that distinct etiological pathways may be involved. Adolescence and early adulthood are sensitive neurodevelopmental periods during which vulnerabilities – such as impulsivity, difficulties with executive functioning or emotional dysregulation – can increase risk-taking behaviors, including early substance use (59). These behaviors may disrupt developmental trajectories and contribute to a more severe course of addiction. In contrast, late-onset IDU may be linked to psychosocial stressors or traumatic events in adulthood, that overwhelm an individual’s emotional regulation and coping capacities.
Additionally, while impaired PF may contribute to substance use, it is furthermore important to consider that prolonged opioid use may itself negatively impact personality functioning. As substance use becomes a central aspect of an individual’s life, it can further erode the sense of self, impair emotional regulation and the ability to build and maintain interpersonal relationships and strengthen maladaptive defense mechanisms. These effects may reinforce and interact with pre-existing vulnerabilities and contribute to a cycle of psychological dysfunction and continued substance use.
Lastly, complementing the psychoanalytic framework, neurobiological models offer important insights by highlighting how repeated substance use alters brain neurochemistry and circuits involved in reward, stress and executive control – especially within the mesolimbic dopamine system and extended amygdala (59). These changes impair emotion regulation, impulse control and decision-making while increasing sensitivity to drug-related cues and stress, leading to craving, withdrawal, and compulsive use (59).
Behavioral models of substance use disorders emphasize the role of reinforcement in the development and maintenance of addictive behaviors, focusing on the pleasurable effects of substance use (positive reinforcement) and the relief from distress or withdrawal (negative reinforcement). Over time, these reinforcement processes strengthen substance use patterns, making them increasingly resistant to change and contributing to an erosion of alternative coping strategies (60).
Although psychodynamic, neurobiological and behavioral models offer different perspectives – focusing on internal conflicts, brain circuitry or learned reinforcement patterns – they each capture distinct facets of addiction. Across these models, substance use is understood as serving a crucial function within an individual’s psychological – and neurobiological – systems, often associated with the compensation of deficits in affect regulation, coping or reward processing.
5.1 Implications for treatment and prevention strategies
In the treatment of patients with OUDs, both diagnostic assessment and psychotherapeutic interventions should take facets of PF into account. Integrating PF assessment into treatment planning may help identify individuals at higher risk for treatment dropout, poor adherence, or difficulties in establishing therapeutic alliance – factors known to impact treatment outcomes. Moreover, assessing PF can guide clinical decision-making by identifying specific impairments in mental functioning that may serve as targets for therapeutic interventions (61–65). Longitudinal research is needed to further examine the predictive value of PF for various treatment outcomes and to evaluate the efficacy of therapeutic approaches informed by PF assessment.
Given the complex pathogenesis of OUDs, a multiprofessional treatment approach is required, combining psychotherapy, social work and medical care. Since childhood trauma is a major risk for mental health issues, prevention strategies should prioritize not only restricting access to illegal drugs but also fostering supportive social networks and ensuring accessible healthcare for families and children in challenging circumstances.
5.2 Limitations
Limitations of this study include its cross-sectional design and the relatively low sample size due to the time-consuming interview process. Childhood trauma was assessed using a self-report questionnaire, which may be subject to various biases (e.g. recall bias, limited insight into one’s own traumatic experiences). Additionally, the sample primarily consisted of male patients, reflecting the common overrepresentation of males in this population (66) preventing the consideration of gender differences.
Another limitation concerns the risk of inflated Type I error due to multiple statistical comparisons. Formal corrections for multiple testing were not applied, a decision based on the exploratory nature of the study and the limited sample size, a consequence of the time-intensive and resource-demanding interview procedure. Applying strict correction methods could have reduced statistical power and potentially obscured meaningful patterns for further research. Nevertheless, the lack of correction increases the likelihood of false-positive findings, and the results should therefore be interpreted with appropriate caution. Replication in larger, more statistically powered samples is needed to confirm the robustness of the observed results.
Finally, it should be emphasized that causality cannot be inferred due to the cross- sectional study design. While significant associations between personality functioning and substance use were observed, the direction of these effects cannot be determined. It seems plausible that impairments in personality functioning contribute to substance use disorder pathology, but also that prolonged substance use may negatively impact personality functioning.
6 Conclusion
OUDs are associated with severely impaired PF. A younger age at the onset of IDU and a greater number of years of IDU use are associated with higher levels of personality pathology and reports of childhood trauma. A greater number of PDs was associated with more severe impairment of PF. When compared, PF accounts for a greater proportion of explained variance in IDU and the number of diagnosed PDs than self-reported childhood trauma. Assessment of PF can provide important information for preventive and treatment strategies in addition to categorical psychiatric diagnoses and trauma history anamnesis and enhances our understanding of the complex relationship between substance use, childhood trauma and personality pathology.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Commission of the Medical University of Vienna (Decision reference number: 1718/2020). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LW: Conceptualization, Data curation, Formal Analysis, Investigation, Writing – original draft, Writing – review & editing. SH: Conceptualization, Investigation, Project administration, Resources, Writing – review & editing. DB-E: Investigation, Writing – review & editing. JF: Formal Analysis, Writing – review & editing. SH-S: Writing – review & editing. KM: Investigation, Writing – review & editing. LO: Data curation, Software, Writing – review & editing. KR: Writing – review & editing. VB: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1
Bolshakova M Bluthenthal R Sussman S . Opioid use and misuse: Health impact, prevalence, correlates, and interventions. Psychol Health. (2019) 34:1105–39. doi: 10.1080/08870446.2019.1622013
2
Cicero TJ Ellis MS Kasper ZA . Polysubstance use: A broader understanding of substance use during the opioid crisis. Am J Public Health. (2020) 110:244–50. doi: 10.2105/AJPH.2019.305412
3
Hedegaard H Bastian BA Trinidad JP Spencer M Warner M . Drugs most frequently involved in drug overdose deaths: United States, 2011–2016. Natl Vital Stat Rep. (2018) 69.
4
Hser YI Evans E Grella C Ling W Anglin D . Long-term course of opioid addiction. Harvard Rev Psychiatry. (2015) 23:76–89. doi: 10.1097/HRP.0000000000000052
5
Koob GF Volkow ND . Neurobiology of addiction: A neurocircuitry analysis. Lancet Psychiatry. (2016) 3:760–73. doi: 10.1016/S2215-0366(16)00104-8
6
Stone AL Becker LG Huber AM Catalano RF . Review of risk and protective factors of substance use and problem use in emerging adulthood. Addictive Behav. (2012) 37:747–75. doi: 10.1016/j.addbeh.2012.02.014
7
Kessler RC McLaughlin KA Green JG Gruber MJ Sampson NA Zaslavsky AM et al . Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry. (2010) 197:378–85. doi: 10.1192/bjp.bp.110.080499
8
Daigre C Rodríguez-Cintas L Tarifa N Rodríguez-Martos L Grau-López L Berenguer M et al . History of sexual, emotional, or physical abuse and psychiatric comorbidity in substance-dependent patients. Psychiatry Res. (2015) 229:743–9. doi: 10.1016/j.psychres.2015.07.059
9
Darke S Torok M . The association of childhood physical abuse with the onset and extent of drug use among regular injecting drug users. Addiction. (2014) 109:610–6. doi: 10.1111/add.12428
10
Guarino H Mateu-Gelabert P Quinn K Sirikantraporn S Ruggles KV Syckes C et al . Adverse childhood experiences predict early initiation of opioid use behaviors. Front Sociology. (2021) 6:620395. doi: 10.3389/fsoc.2021.620395
11
Santo T Campbell G Gisev N Martino-Burke D Wilson J Colledge-Frisby S et al . Prevalence of mental disorders among people with opioid use disorder: A systematic review and meta-analysis. Drug Alcohol Depend. (2022) 238:109551. doi: 10.1016/j.drugalcdep.2022.109551
12
Taplin C Saddichha S Li K Krausz MR . Family history of alcohol and drug abuse, childhood trauma, and age of first drug injection. Subst Use Misuse. (2014) 49:1311–6. doi: 10.3109/10826084.2014.901383
13
Scamaldo KM Tull MT Gratz KL . Motives for opioid use explain the relation between borderline personality disorder pathology and opioid use problems. Psychiatry Res. (2021) 296:113609. doi: 10.1016/j.psychres.2020.113609
14
Wojciechowski T . Antisocial personality disorder as a risk factor for opioid use: The dual mediating roles of antisocial attitudes and self-control. J Drug Issues. (2021) 51:268–83. doi: 10.1177/0022042620979630
15
Kornør H Nordvik H . Five-factor model personality traits in opioid dependence. BMC Psychiatry. (2007) 7:1–6. doi: 10.1186/1471-244X-7-37
16
Terracciano A Löckenhoff CE Crum RM Bienvenu OJ Costa PT . Five-factor model personality profiles of drug users. BMC Psychiatry. (2008) 8:1–10. doi: 10.1186/1471-244X-8-22
17
Blatt SJ McDonald C Sugarman A Wilber C . Psychodynamic theories of opiate addiction: New directions for research. Clin Psychol Rev. (1984) 4:159–89. doi: 10.1016/0272-7358(84)90027-8
18
American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC, USA: American Psychiatric Association Publishing (2013).
19
Mulder R Tyrer P . Diagnosis and classification of personality disorders: Novel approaches. Curr Opin Psychiatry. (2019) 32:27–31. doi: 10.1097/YCO.0000000000000461
20
Blüml V Doering S . ICD-11 personality disorders: A psychodynamic perspective on personality functioning. Front Psychiatry. (2021) 12:654026. doi: 10.3389/fpsyt.2021.654026
21
Kernberg OF . What is personality? J Pers Disord. (2016) 30:145–56. doi: 10.1521/pedi.2106.30.2.145
22
Kernberg OF . Some implications of new developments in neurobiology for psychoanalytic object relations theory. Neuropsychoanalysis. (2022) 24:3–12. doi: 10.1080/15294145.2021.1995609
23
Kernberg OF . Borderline conditions and pathological narcissism. New York, NY, USA: Jason Aronson (1975).
24
Kernberg OF . Severe personality disorders. New Haven, CT, USA: Yale University Press (1984).
25
Clarkin JF Caligor E Stern B Kernberg OF . Structured interview of personality organization (STIPO). Weill Medical College of Cornell University: Personality Disorders Institute (2004).
26
Clarkin JF Caligor E Stern B Kernberg OF . Structured interview of personality organization - revised (STIPO-R) [Unpublished manuscript]. Weill Medical College of Cornell University: Personality Disorders Institute (2016).
27
Atanassov N Savov S . Mentalization and personality organization in heroin addicted patients: A narrative analysis. Lang Psychoanalysis. (2016) 5:14–30. doi: 10.7565/landp.v5i1.1552
28
Di Pierro R Preti E Vurro N Madeddu F . Dimensions of personality structure among patients with substance use disorders and co-occurring personality disorders: A comparison with psychiatric outpatients and healthy controls. Compr Psychiatry. (2014) 55:1398–405. doi: 10.1016/j.comppsych.2014.04.005
29
Rentrop M Zilker T Lederle A Birkhofer A Hörz S . Psychiatric comorbidity and personality structure in patients with polyvalent addiction. Psychopathology. (2014) 47:133–40. doi: 10.1159/000351784
30
Fuchshuber J Hiebler-Ragger M Kresse A Kapfhammer HP Unterrainer HF . Depressive symptoms and addictive behaviors in young adults after childhood trauma: The mediating role of personality organization and despair. Front Psychiatry. (2018) 9:318. doi: 10.3389/fpsyt.2018.00318
31
Hörz S Rentrop M Fischer-Kern M Schuster P Kapusta N Buchheim P et al . Strukturniveau und klinischer Schweregrad der Borderline-Persönlichkeitsstörung. Z für Psychosomatische Med und Psychotherapie. (2010) 56:136–49. doi: 10.13109/zptm.2010.56.2.136
32
Doering S Burgmer M Heuft G Menke D Bäumer B Lübking M et al . Reliability and validity of the German version of the Structured Interview of Personality Organization (STIPO). BMC Psychiatry. (2013) 13:210. doi: 10.1186/1471-244X-13-210
33
Hörz S . Das strukturierte interview zur persönlichkeitsorganisation (STIPO). In: DoeringSHörzS, editors. Handbuch der strukturdiagnostik: konzepte, instrumente, praxis. Stuttgart, Germany: Schattauer (2012). p. 52–86.
34
Stern BL Caligor E Clarkin JF Critchfield KL Horz S MacCornack V et al . Structured Interview of Personality Organization (STIPO): Preliminary psychometrics in a clinical sample. J Pers Assess. (2010) 92:514–22. doi: 10.1080/00223891.2010.502382
35
First MB Williams JBW Karg RS Spitzer RL . Structured clinical interview for DSM-5 disorders—Clinician version (SCID-5-CV). Washington, DC, USA: American Psychiatric Association Publishing (2016).
36
First MB Williams JBW Karg RS Spitzer RL . Structured clinical interview for DSM-5 personality disorders (SCID-5-PD). Washington, DC, USA: American Psychiatric Association Publishing (2016).
37
Beesdo-Baum K Zaudig M & Wittchen HU eds. Strukturiertes klinisches interview für DSM-5-störungen – klinische version. Göttingen, Germany: Hogrefe (2019).
38
Beesdo-Baum K Zaudig M & Wittchen HU eds. Strukturiertes klinisches interview für DSM-5-störungen – persönlichkeitsstörungen. Göttingen, Germany: Hogrefe (2019).
39
McLellan AT Luborsky L Woody GE O’Brien CP . An improved diagnostic evaluation instrument for substance abuse patients: The Addiction Severity Index. J Nervous Ment Dis. (1980) 168:26–33. doi: 10.1097/00005053-198001000-00006
40
Cacciola JS Alterman AI McLellan AT Lin YT Lynch KG . Initial evidence for the reliability and validity of a “Lite” version of the Addiction Severity Index. Drug Alcohol Depend. (2007) 87:297–302. doi: 10.1016/j.drugalcdep.2006.09.002
41
Schäfer I . Deutsche version des addiction severity index lite. Universität Hamburg: Zentrum für Interdisziplinäre Suchtforschung (ZIS (2012).
42
Bernstein DP Stein JA Newcomb MD Walker E Pogge D Ahluvalia T et al . Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. (2003) 27:169–90. doi: 10.1016/s0145-2134(02)00541-0
43
Karos K Niederstrasser N Abidi L Bernstein DP Bader K . Factor structure, reliability, and known groups validity of the German version of the Childhood Trauma Questionnaire (Short-form) in Swiss patients and nonpatients. J Child Sexual Abuse. (2014) 23:418–30. doi: 10.1080/10538712.2014.896840
44
Peng C Cheng J Rong F Wang Y Yu Y . Psychometric properties and normative data of the childhood trauma questionnaire-short form in Chinese adolescents. Front Psychol. (2023) 14:1130683. doi: 10.3389/fpsyg.2023.1130683
45
Hoeboer CM Bodor N Oprel DA de Kleine RA Schoorl M van Minnen A et al . Validation of the childhood trauma questionnaire (CTQ) in the context of trauma-focused treatment. Child Maltreatment. (2025), 10775595251328611. doi: 10.1177/10775595251328611
46
Zhang S Lin X Liu J Pan Y Zeng X Chen F et al . Prevalence of childhood trauma measured by the short form of the Childhood Trauma Questionnaire in people with substance use disorder: A meta-analysis. Psychiatry Res. (2020) 294:113524. doi: 10.1016/j.psychres.2020.113524
47
Kernberg OF . Neurobiological correlates of object relations theory: The relationship between neurobiological and psychodynamic development. Int Forum Psychoanalysis. (2015) 24:38–46. doi: 10.1080/0803706X.2014.912352
48
Kernberg OF Caligor EA . Psychoanalytic theory of personality disorders. In: LenzenwegerMFClarkinJF, editors. Major theories of personality disorder, 2nd ed. New York, NY, USA: Guilford Press (2005). p. 114–56.
49
Doering S Blüml V Parth K Feichtinger K Gruber M Aigner M et al . Personality functioning in anxiety disorders. BMC Psychiatry. (2018) 18:294. doi: 10.1186/s12888-018-1870-0
50
Fischer-Kern M Kapusta ND Doering S Horz S Mikutta C Aigner M . The relationship between personality organization and psychiatric classification in chronic pain patients. Psychopathology. (2011) 44:21–6. doi: 10.1159/000317271
51
Kernberg OF . Borderline personality organization. J Am Psychoanalytic Assoc. (1967) 15:641–85. doi: 10.1177/000306516701500309
52
Khantzian EJ . The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Rev Psychiatry. (1997) 4:231–44. doi: 10.3109/10673229709030550
53
Morgenstern J Leeds J . Contemporary psychoanalytic theories of substance abuse: A disorder in search of a paradigm. Psychotherapy: Theory Research Practice Training. (1993) 30:194. doi: 10.1037/0033-3204.30.2.194
54
Caligor E Kernberg OF Clarkin JF Yeomans FE . Psychodynamic therapy for personality pathology: Treating self and interpersonal functioning. Washington, DC, USA: American Psychiatric Association Publishing (2018).
55
Rosenfeld HA . On drug addiction. Int J Psychoanalysis. (1960) 41:467–75.
56
Clarkin JF Lenzenweger MF Yeomans F Levy KN Kernberg OF . An object relations model of borderline pathology. J Pers Disord. (2007) 21:474–99. doi: 10.1521/pedi.2007.21.5.474
57
Voigtel R . Sucht. Gießen, Germany: Psychosozial-Verlag (2015).
58
Yakeley J Burbridge-James W . Psychodynamic approaches to suicide and self-harm. BJPsych Adv. (2018) 24:37–45. doi: 10.1192/bja.2017.6
59
Volkow ND Boyle M . Neuroscience of addiction: relevance to prevention and treatment. Am J Psychiatry. (2018) 175:729–40. doi: 10.1176/appi.ajp.2018.17101174
60
Skewes MC Gonzalez VM . The biopsychosocial model of addiction. In: MillerPM, editor. Principles of addiction. Amsterdam, Netherlands: Elsevier (2013). p. 61–70.
61
Clarkin JF Meehan KB De Panfilis C Doering S . Empirical developments in transference-focused psychotherapy. Am J Psychother. (2023) 76:39–45. doi: 10.1176/appi.psychotherapy.20220017
62
Kernberg OF . New developments in transference focused psychotherapy. Int J Psychoanalysis. (2016) 97:385–407. doi: 10.1111/1745-8315.12289
63
Ingenhoven TJ Duivenvoorden HJ Passchier J van den Brink W . Treatment duration and premature termination of psychotherapy in personality disorders: predictive performance of psychodynamic personality functioning. J Psychiatr Practice®. (2012) 18:172–86. doi: 10.1097/01.pra.0000415074.43744.29
64
Bach B Simonsen S . How does level of personality functioning inform clinical management and treatment? Implications for ICD-11 classification of personality disorder severity. Curr Opin Psychiatry. (2021) 34:54–63. doi: 10.1097/YCO.0000000000000658
65
Papamalis FE . Examining the relationship of personality functioning and treatment completion in substance misuse treatment. Subst Abuse: Res Treat. (2020) 14:1178221820951777. doi: 10.1177/1178221820951777
66
Hoffman KA Ponce Terashima J McCarty D . Opioid use disorder and treatment: Challenges and opportunities. BMC Health Serv Res. (2019) 19:1–5. doi: 10.1186/s12913-019-4751-4
Summary
Keywords
personality functioning, substance use disorders, opioid use disorders, injecting drug use, childhood trauma
Citation
Waschulin L, Hofner S, Bildstein-Ebner D, Fuchshuber J, Hörz-Sagstetter S, Michlmayr K, Ohse L, Riegel KD and Blüml V (2025) The role of personality functioning and childhood trauma in patients in opioid substitution treatment. Front. Psychiatry 16:1584143. doi: 10.3389/fpsyt.2025.1584143
Received
26 February 2025
Accepted
27 May 2025
Published
18 June 2025
Volume
16 - 2025
Edited by
Liana Fattore, CNR Neuroscience Institute (IN), Italy
Reviewed by
Karl Haller, Charité – University Medicine Berlin, Germany
Rebeka Javor, University of Pécs, Hungary
Updates
Copyright
© 2025 Waschulin, Hofner, Bildstein-Ebner, Fuchshuber, Hörz-Sagstetter, Michlmayr, Ohse, Riegel and Blüml.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Victor Blüml, victor.blueml@meduniwien.ac.at
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.