- 1School of Physical Education, Southwest University, Chongqing, China
- 2College of Horticulture and Landscape Architecture, Southwest University, Chongqing, China
Objective: This systematic review and meta-analysis aimed to evaluate the overall efficacy of school-based interventions (SBIs) in promoting resilience in children and adolescents and to provide evidence for advancing mental health care for children and adolescents.
Methods: A search was conducted in seven electronic databases, including PubMed, Embase, EBSCOhost, Scopus, Web of Science, APA PsycINFO, and Google Scholar. The Revised Cochrane risk-of-bias tool for randomized trials (RoB 2) was used for the quality appraisal. The standardized mean difference (SMD; Cohen’s d) combined with 95% confidence intervals (CIs) was used to pool the effect sizes.
Results: A total of 38 RCTs involving 15,730 participants were included in the systematic review, 21 of which were selected for inclusion in the meta-analysis. In terms of quality appraisal, the included trials were classified as having low risk, some concerns, or high risk, with proportions of 5.2%, 71.1%, and 23.7%, respectively. The pairwise meta-analyses indicated that SBIs significantly enhanced resilience in children and adolescents compared to the control group (SMD = 0.17, 95% Cl 0.06–0.29, p < 0.01).
Conclusions: SBIs have a positive effect on the resilience of children and adolescents. In the context of limited medical resources, SBIs could serve as a promising approach to promote the ability of children and adolescents to adapt to stressors. Given the considerable heterogeneity identified, SBIs should be personalized on the basis of variations in demographic characteristics, intervention implementation, and actual dose-response to improve the overall well-being of children and adolescents and reduce the risk of maladaptive psychological and behavioral responses.
1 Introduction
Resilience refers to an individual’s ability to cope and recover effectively in the face of setbacks and adversity and maintain normal physiological function and psychological health (1, 2). Resilience is a dynamic process for adapting to stressful situations, characterized by continuous development over time (3–5). The level of resilience is a crucial indicator for assessing an individual’s physical and mental development in response to stressors (6). Children and adolescents are in a critical stage of physical and mental development, making them susceptible to stressors from family, school, and peers, including parental divorce (7), academic pressure (8), teacher-student relationships (9), and school bullying (10, 11). Resilience can effectively help them overcome stressful situations, maintain psychological balance, and promote their positive development. According to the American Medical Association, approximately 293 million children and adolescents worldwide suffer from at least one mental disorder, such as anxiety, depression, and schizophrenia (12). To address this challenge, developing resilience is considered a promising approach (2, 13, 14). Evidence suggests that children and adolescents with higher resilience levels tend to respond positively to stressful situations by adopting adaptive coping strategies. This helps them reduce the risk of developing negative emotions such as anxiety and depression and promotes their overall mental health and welfare (15–17). By contrast, children and adolescents with lower resilience levels are more likely to exhibit problem behaviors, including smartphone addiction (18), violent tendencies (19), attention deficit hyperactivity disorder (20), illicit drug use, and smoking and alcohol abuse (21). The findings suggest that resilience, as an important psychological resource, can effectively reduce the negative impact of stressors on the growth process of children and adolescents, thereby promoting their physical and mental health development and enhancing their ability to adapt to and cope with stressful situations.
Interventions to promote resilience have been developed in a variety of settings to reduce mental health problems in children and adolescents, including families (22), communities (23), and hospitals (24). Family-based interventions aimed to improve family cohesion by strengthening positive communication between students and parents, thereby enhancing students’ resilience and reducing the occurrence of mental health disorders and issues during adolescence (22). Community-based interventions aimed to improve family economic conditions and provide children and adolescents with a stronger social support network, thereby promoting the development of their resilience (23). Hospital-based interventions aimed at helping patients build resilience through the care provided by healthcare professionals, enabling them to cope more effectively with stressors (25). However, interventions implemented in these environments may struggle to reach every child and adolescent. In this context, one of the most powerful tools for addressing the inequality in access to interventions is the implementation of school-based interventions (SBIs) to promote the physical and mental health of children and adolescents. SBIs are defined as any program, intervention, or strategy applied within the school environment aimed at regulating and improving students’ emotional, behavioral, or social functioning (26). To our knowledge, five systematic reviews or meta-analyses have examined the effectiveness of resilience programs on the mental health of children or adolescents (13, 14, 27–29). In terms of improving resilience, four studies reported effect sizes ranging from 0.23 to 0.58, while one study did not address this outcome (13). However, these studies have certain limitations. For example, three studies had incomplete search strategies regarding interventions or outcomes (14, 28, 29), and two studies included mixed populations (27, 28). Notably, only one study focused on interventions implemented in school environments (29), which means that the effectiveness of SBIs in improving resilience in children and adolescents still lacks high-quality evidence. The school system possesses sufficient foundational conditions to identify mental health issues effectively in children and adolescents and provide timely onsite interventions (30, 31). Specifically, this system can effectively identify early signs of mental health issues in children and adolescents by implementing universally applicable policies, ensuring access to high-quality educators, and establishing school-based clinics (32). Effective identification is made possible through strong collaboration among healthcare professionals, educators, and school administrators, enabling prompt interventions when these early warning signs emerge. In this way, SBIs not only help alleviate emotional and behavioral disorders in children and adolescents but also ensure that students who have difficulty accessing mental health care receive attention and support (26). Therefore, SBIs play an important role and significance in fostering resilience in children and adolescents.
The protective possibilities framework of resilience suggests that SBIs can promote students’ resilience by providing opportunities for development, as well as emotional, motivational, and strategic support (33). Key elements within the school environment—including teacher behaviors and support in the classroom, peer relationships, and family support and expectations—collectively form a supportive ecosystem that helps students better cope with challenges and stress, thereby enhancing their resilience. Over the past two decades, a series of studies have confirmed the significant efficacy of SBIs in promoting resilience in children and adolescents. For example, a program to support students exposed to trauma was proposed by Amin et al. (34), which includes 10 structured sessions designed to promote resilience by reducing students’ posttraumatic stress disorder symptoms (34). On the basis of the P-A-G-E framework, Cheng et al. (35) proposed the Digital Netizen Alliance program to increase students’ positive coping ability and resilience through the development of positive mental skills (35). Khalsa et al. (36) proposed a yoga program implemented within the school environment, which effectively improved students’ resilience by promoting mindfulness and developing cognitive skills related to self-awareness (36). However, evidence for SBIs in this field is not consistent, with some studies indicating that these interventions have not demonstrated significant efficacy in promoting resilience in children and adolescents (37, 38). In addition, previous studies have indicated that the efficacy of SBIs for children and adolescents may vary depending on population characteristics and intervention implementation. Differences in cognitive abilities, emotional needs, and brain development at various stages of childhood and adolescence may lead to different dose-response relationships in intervention implementation (39). Similarly, factors such as age, cultural background, and socioeconomic status may also contribute to variations in resilience levels (40, 41). Therefore, it is essential to investigate the differential efficacy of interventions based on variations in population characteristics and intervention implementation through moderator analyses. This approach enables the customization of SBIs to accommodate these variations, ensuring more tailored and effective adjustments. In summary, although SBIs can promote the development of resilience in children and adolescents to some extent, the overall efficacy of these interventions in this regard still lacks consistency. For children and adolescents exposed to many stressors, fostering resilience helps them cope positively with stressful situations and enhances their overall well-being (42). Given this, it is necessary to review previous evidence to examine the overall efficacy of SBIs on resilience in children and adolescents. The methodologies used in published related randomized controlled trials (RCTs) vary, resulting in differences in the effect sizes of SBIs on resilience in children and adolescents. This systematic review and meta-analysis aimed to evaluate the overall efficacy of SBIs in promoting resilience in children and adolescents and to provide evidence for advancing mental health care for children and adolescents.
2 Methods
This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines (43) and has been registered in the International Prospective Register of Systematic Reviews (PROSPERO) with the registration number: CRD420251009149.
2.1 Search methods
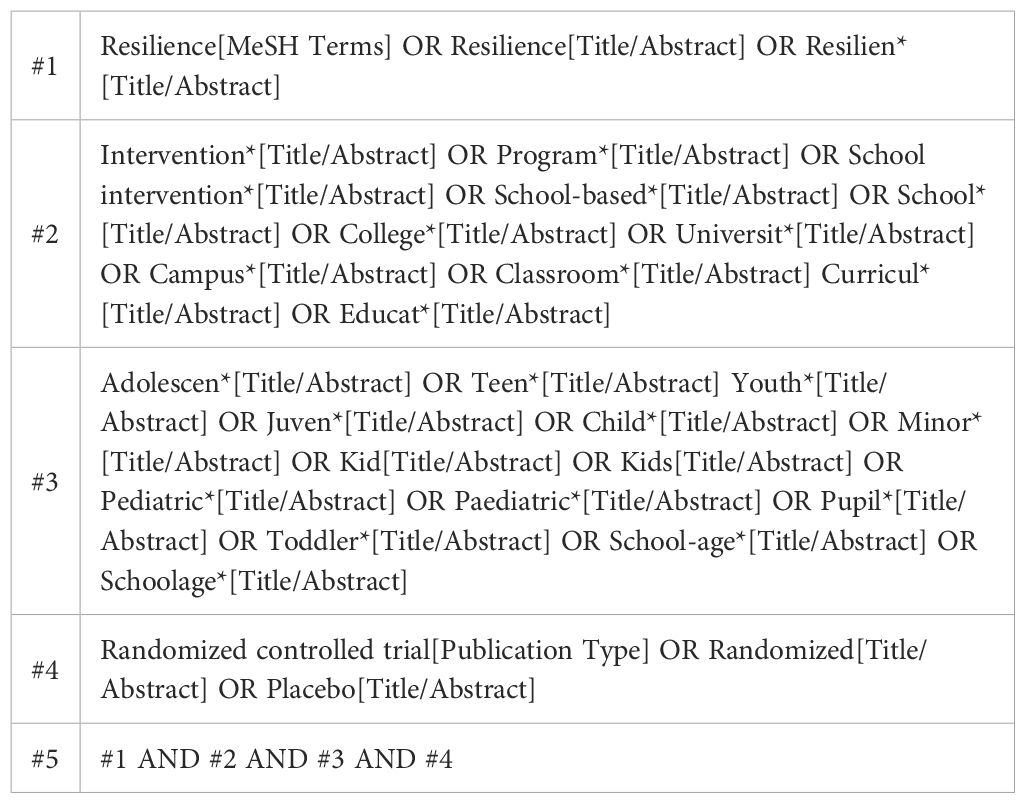
A search was conducted in six electronic databases via Medical Subject Headings and free-text terms: PubMed, Embase, EBSCOhost, Scopus, Web of Science, and APA PsycINFO. In addition, relevant references were manually searched on Google Scholar. The search period ranged from the creation of each database to January 2025. Notably, the included studies must be published in English and have been peer-reviewed. Grey literature is excluded from the literature search, as it may lack rigorous peer review and standardized reporting. The search methods followed the PICOS principles: (P) Population—children or adolescents (age range: 6—19 years); (I) Intervention—school-based interventions (e.g., classroom-based social and emotional learning program, school-based resilience intervention program, school-based emotion regulation program, school-based mindfulness training); (C) Comparator—control groups receiving routine education, wait-list, no-intervention, or active control; (O) Outcome—any assessment for resilience, including trials where it was a primary or secondary outcome; (S) Study design—all types of randomized controlled trials. The search methods of PubMed are presented in Table 1. The complete search methods for all electronic databases are detailed in Supplementary material Table 1.
2.2 Inclusion and exclusion criteria
The inclusion and exclusion criteria are presented in Table 2.
2.3 Study selection and data extraction
The study selection and data extraction were performed by two independent researchers (CYC and ZYM). Following the literature search, all records that fulfilled the predetermined inclusion and exclusion criteria were imported into EndNote 20.6, with duplicates removed. The titles, abstracts, and full texts of the remaining records were independently screened by two researchers. The extracted data included (a) basic information, including the first author, country, and year of publication; (b) participant characteristics, including the type and risk profile of population, mean age (standard deviation), sample size, and percentage of males; (c) details of the interventions and controls; and (d) outcome and measure. Any disagreements arising during the study selection and data extraction processes were addressed through consultation with the corresponding author (SL).
2.4 Quality appraisal
The quality appraisal was performed by two independent researchers (CYC and ZYM) via the Revised Cochrane risk-of-bias tool for randomized trials (RoB 2) (44). The RoB 2 examined included studies for potential sources of bias, including the randomization process, deviations from intended interventions, mising outcome data, measurement of the outcome, and selection of the reported result. The quality of the included studies was categorized into three levels: low risk, some concerns, and high risk. Any disagreements arising during the quality appraisal process were addressed through consultation with the corresponding author (SL).
2.5 Data synthesis
Given the variations in scales employed in different RCTs and given that the outcome in this study was a continuous variable, the standardized mean difference (SMD; Cohen’s d) combined with 95% confidence intervals (CIs) was used to pool the effect sizes (45). The differences in efficacy between the experimental and control groups were compared via forest plots, and heterogeneity of the pooled results was evaluated via the chi-square test, which is based on the Q test and I2 statistic (46). When significant heterogeneity was observed (I2 > 50%, p < 0.10), a random-effects model with the DerSimonian-Laird method was employed to pool the effect sizes. In the absence of significant heterogeneity (I2 < 50%, p > 0.10), a fixed-effects model with the inverse variance method was employed to pool the effect sizes (45). The sources of heterogeneity in the pooled results were explored through meta-regression (for continuous variables) and subgroup analysis (for categorical variables) (47, 48). After studies at high risk were excluded, a sensitivity analysis was performed via a stepwise elimination method to evaluate the robustness of the pooled results (45). Publication bias was assessed based on a visual inspection of the funnel plot and Egger’s test (49, 50). The trim-and-fill method was used to further evaluate the robustness of the pooled results in the presence of significant publication bias (51). The Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) guidelines were used for the certainty of evidence in the following areas: risk of bias, inconsistency, indirectness, imprecision, and publication bias (52). All data syntheses were conducted using Stata 18.0.
3 Results
3.1 Search outcomes
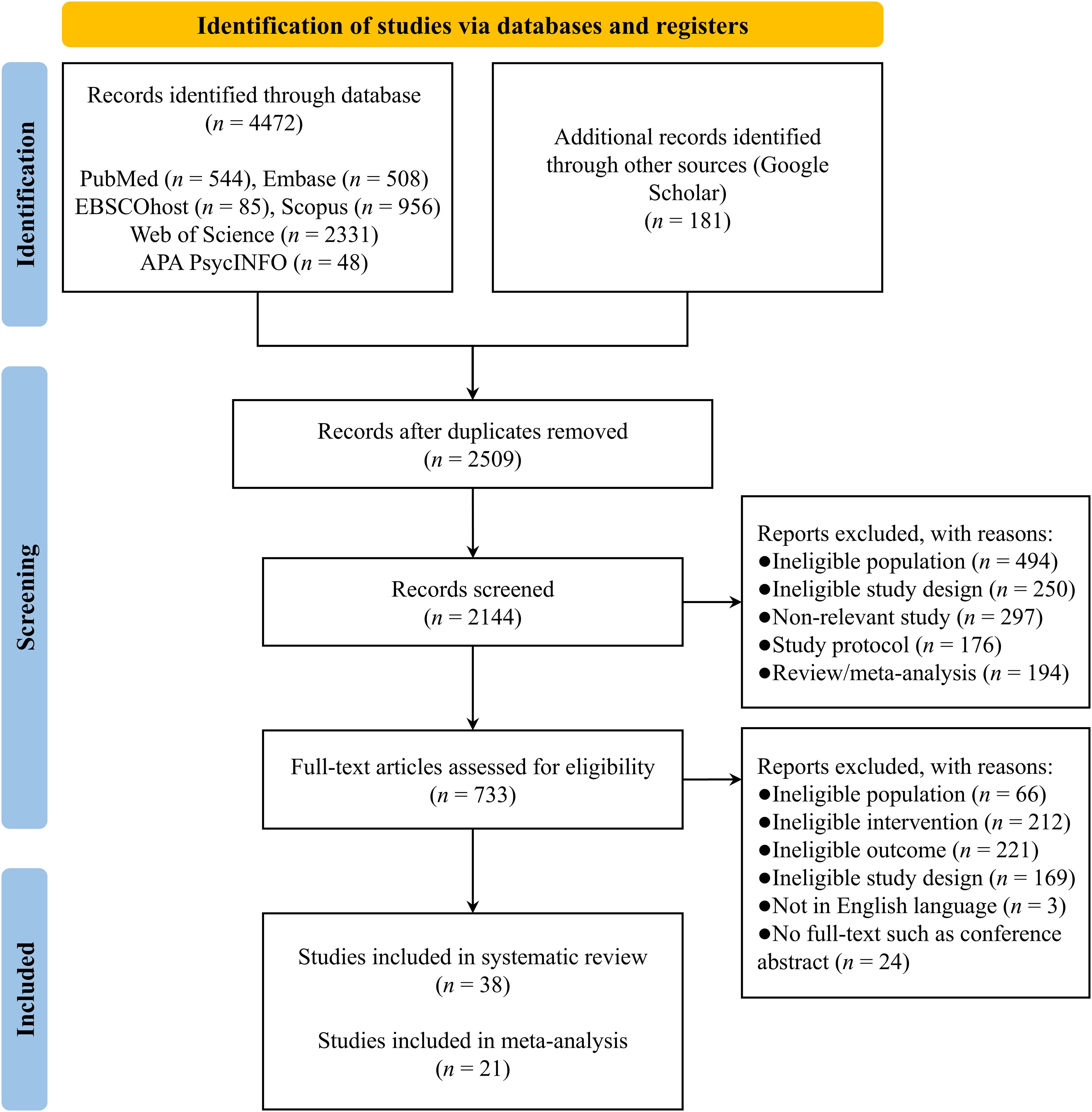
Seven electronic databases were searched, yielding a total of 4,653 records. A systematic identification and manual screening process removed 2,510 duplicates, leaving 2,143 records. A total of 1,411 records were excluded on the basis of titles and abstracts, and 695 records were excluded on the basis of full-text review. Thirty-eight studies were included in the systematic review, with twenty-one studies included in the meta-analysis. Seventeen studies were excluded from the meta-analysis due to a lack of available data (34–38, 53–85) (see Figure 1).
3.2 Study characteristics
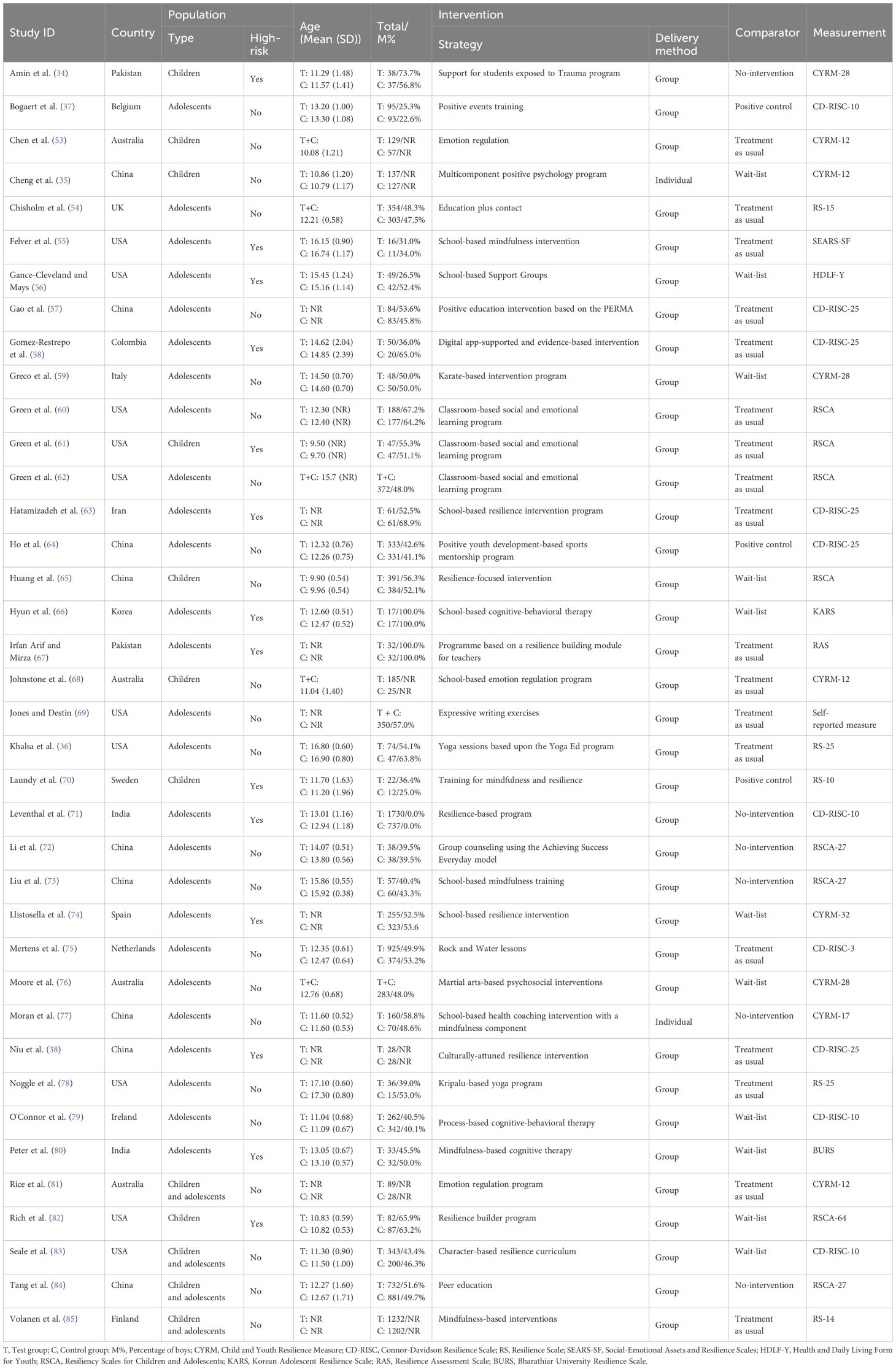
The included studies were published between 2008 and 2024. These studies were conducted in the United States (n = 10), China (n = 9), Australia (n = 4), Pakistan (n = 2), India (n = 2), and one study each in the United Kingdom, Colombia, Belgium, Italy, Iran, South Korea, Sweden, the Netherlands, Ireland, Spain, and Finland. In terms of population characteristics, 26 studies focused on adolescents, 8 studies focused on children, and the remaining 4 studies included mixed populations. In terms of the risk profile of population, participants in 14 studies came from high-risk groups, which may face additional challenges and difficulties in various aspects, such as lower socioeconomic status, physical and mental health issues, or identities as minority and marginalized groups. The remaining 24 studies involved participants who did not belong to high-risk groups. The experimental group consisted of 8,869 participants, ranging in age from 9.50 to 17.10 years. The control group included a total of 6,861 participants, ranging in age from 9.70 to 17.30 years. In terms of the delivery method of interventions, 36 studies used a group intervention model, while 2 studies employed an individual intervention model. Furthermore, 18 studies employed treatment-as-usual controls, 11 utilized wait-list controls, 6 incorporated no-intervention controls, and 3 applied positive controls (see Table 3).
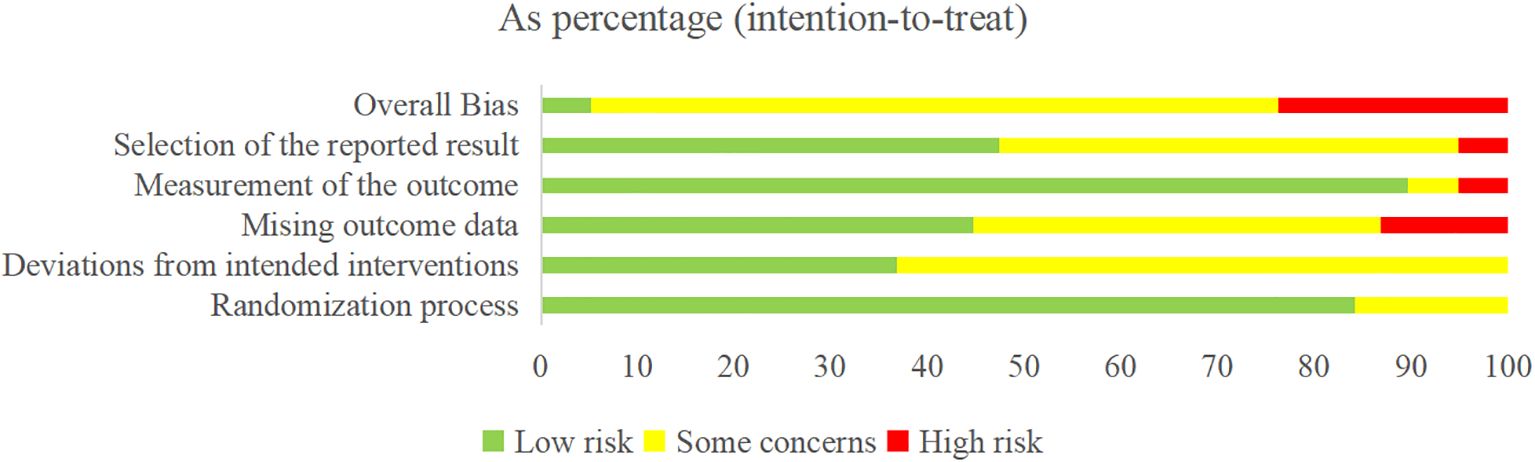
3.3 Quality appraisal
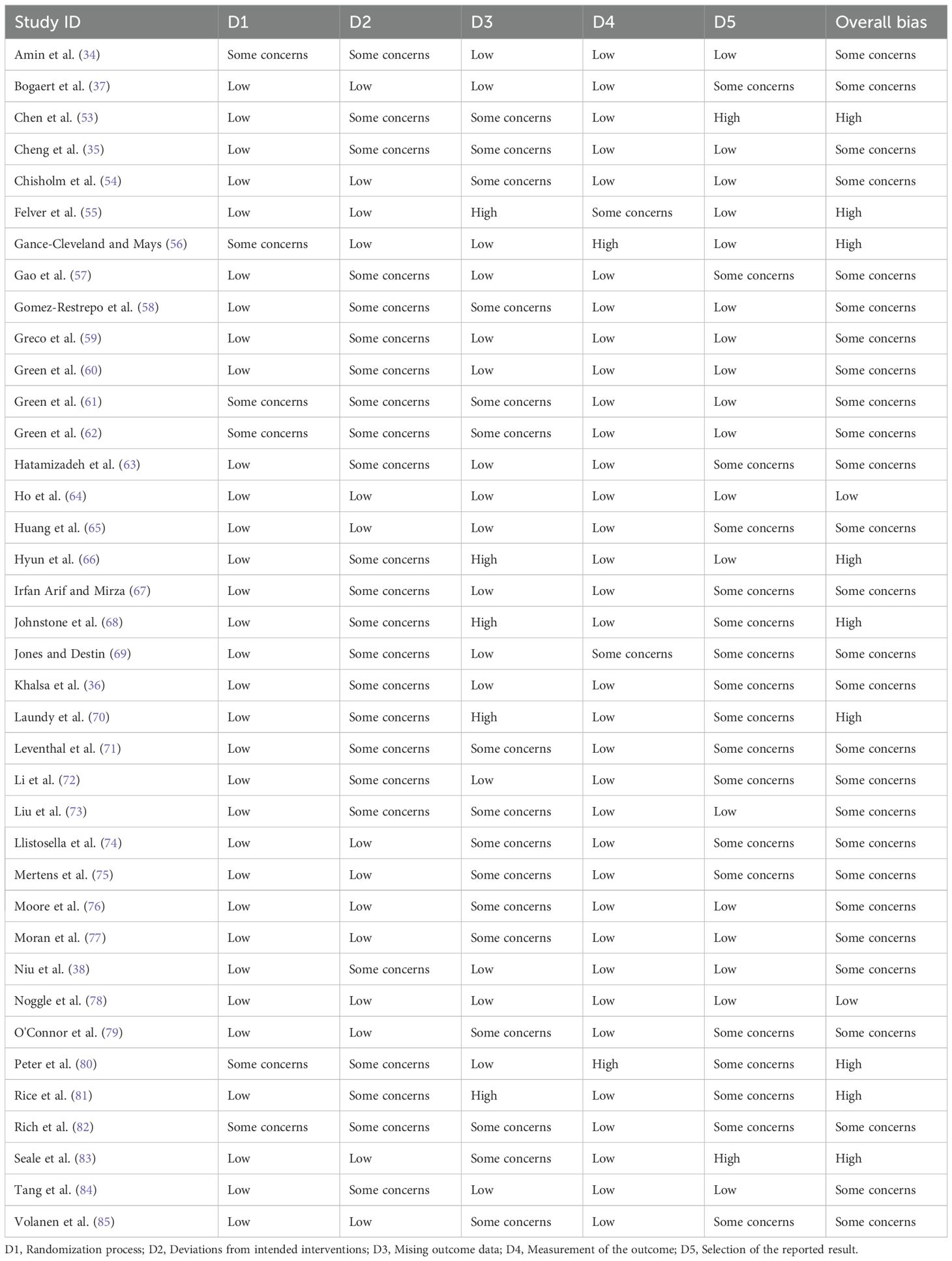
The risk of bias ranged from low to high (see Figure 2, Table 4). For the randomization process, 6 studies were assessed as having some concerns due to baseline differences, while the remaining studies as being of low risk. For the deviations from intended interventions, 24 studies were assessed as having some concerns due to the use of inappropriate analysis to estimate the effect of assignment to intervention, while the remaining studies as being of low risk. For the mising outcome data, 21 studies were assessed as having some concerns or high risk due to missing data for some participants and a lack of evidence that the result was not biased by missing outcome data, while the remaining studies as being of low risk. For the measurement of the outcome, 4 studies were assessed as having some concerns or high risk due to the method of measuring the outcome inappropriate, while the remaining studies as being of low risk. For the selection of the reported result, 20 studies were assessed as having some concerns or high risk due to multiple eligible outcome measurements within the outcome domain, while the remaining studies as being of low risk.
3.4 Pairwise meta-analyses
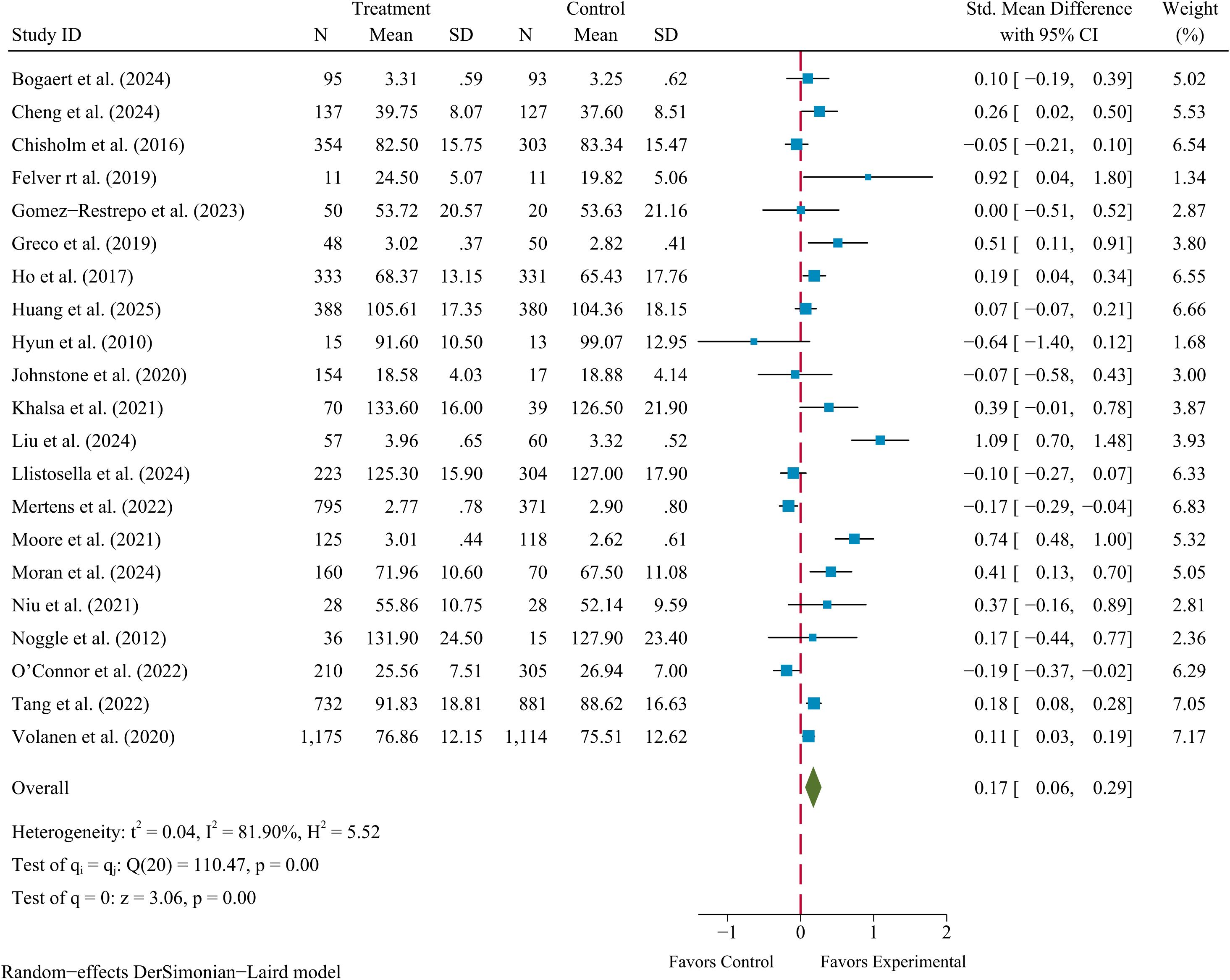
The pairwise meta-analyses included 21 RCTs with available data. Evidence for a small effect of SBIs on resilience in children and adolescents observed (SMD = 0.17, 95% Cl 0.06–0.29, p < 0.01), with considerable heterogeneity identified (I2 = 81.90%, Q = 110.47, p < 0.01). The corresponding forest plot for the pooled results is presented in Figure 3.
3.5 Moderator analyses
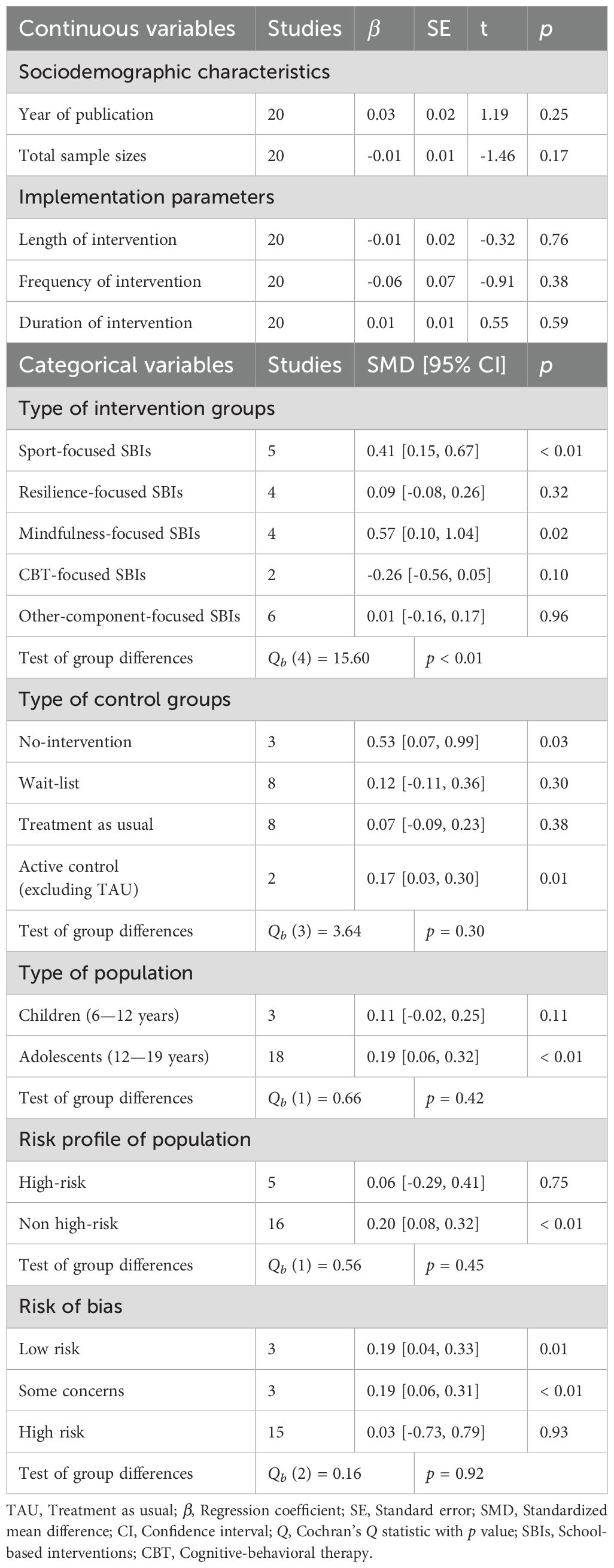
Based on meta-regression to test the moderating effects, the results indicated that year of publication (p = 0.25), total sample size (p = 0.17), length of intervention (p = 0.76), frequency of intervention (p = 0.38), and duration of intervention (p = 0.59) did not moderate the overall efficacy of SBIs on resilience in children and adolescents. Based on subgroup analysis to test the moderating effects, the results indicated that the type of intervention groups exhibited significant differences in the pooled results (Qb (4) = 15.60, p < 0.01). In contrast, no significant differences were observed in the pooled results with respect to the type of control groups (Qb (3) = 3.64, p = 0.30), type of population (Qb (1) = 0.66, p = 0.42), risk profile of population (Qb (1) = 0.56, p = 0.45), and risk of bias (Qb (2) = 0.16, p = 0.92) (see Table 5).
3.6 Sensitivity analyses
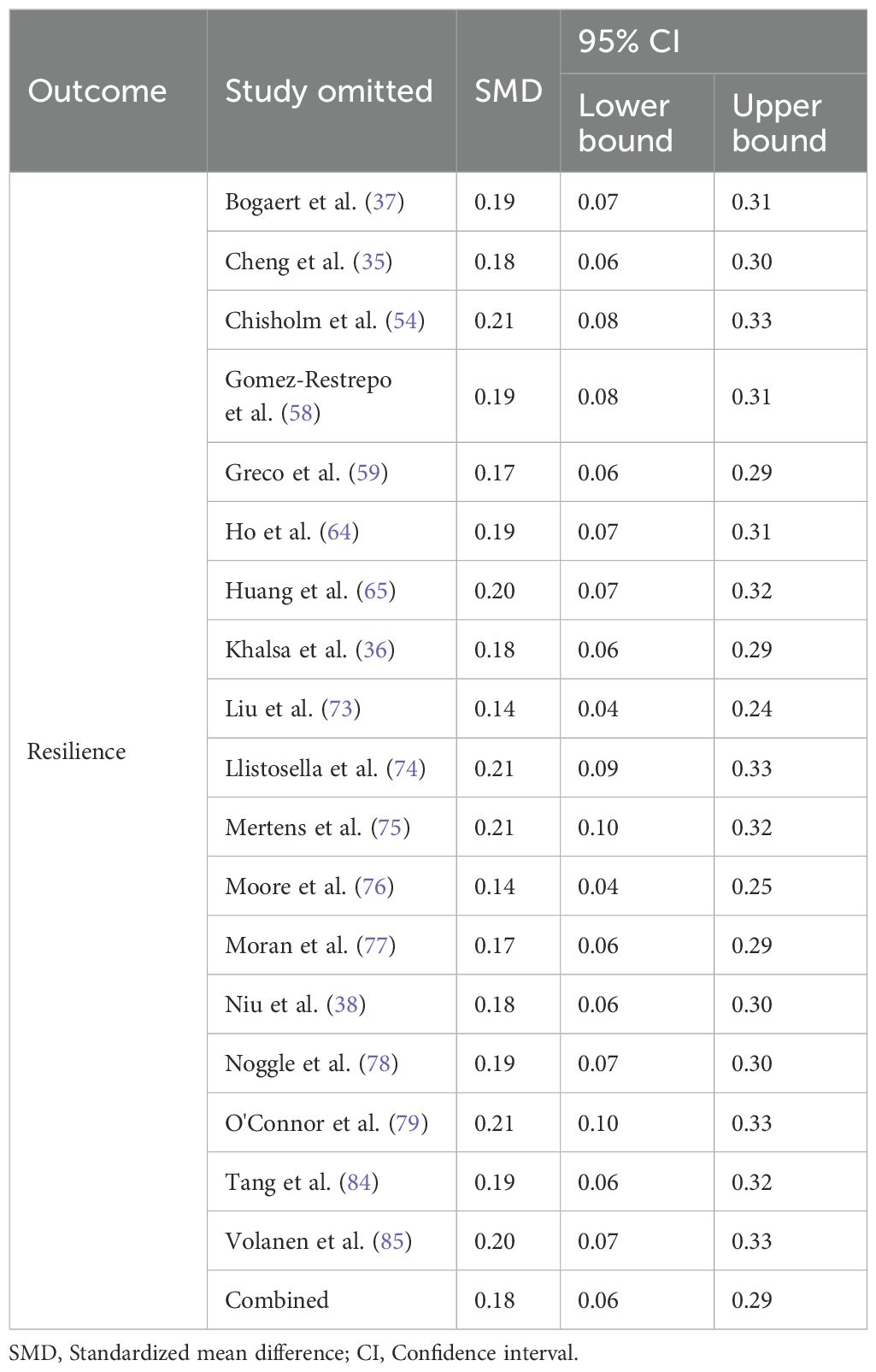
After studies at high risk were excluded, sensitivity analyses were performed via a stepwise elimination method. The results indicated that of the pooled results remained consistent despite variations in study selection, suggesting that the overall efficacy of SBIs on resilience in children and adolescents was robust, with an effect size ranging from 0.14 to 0.21 (see Table 6).
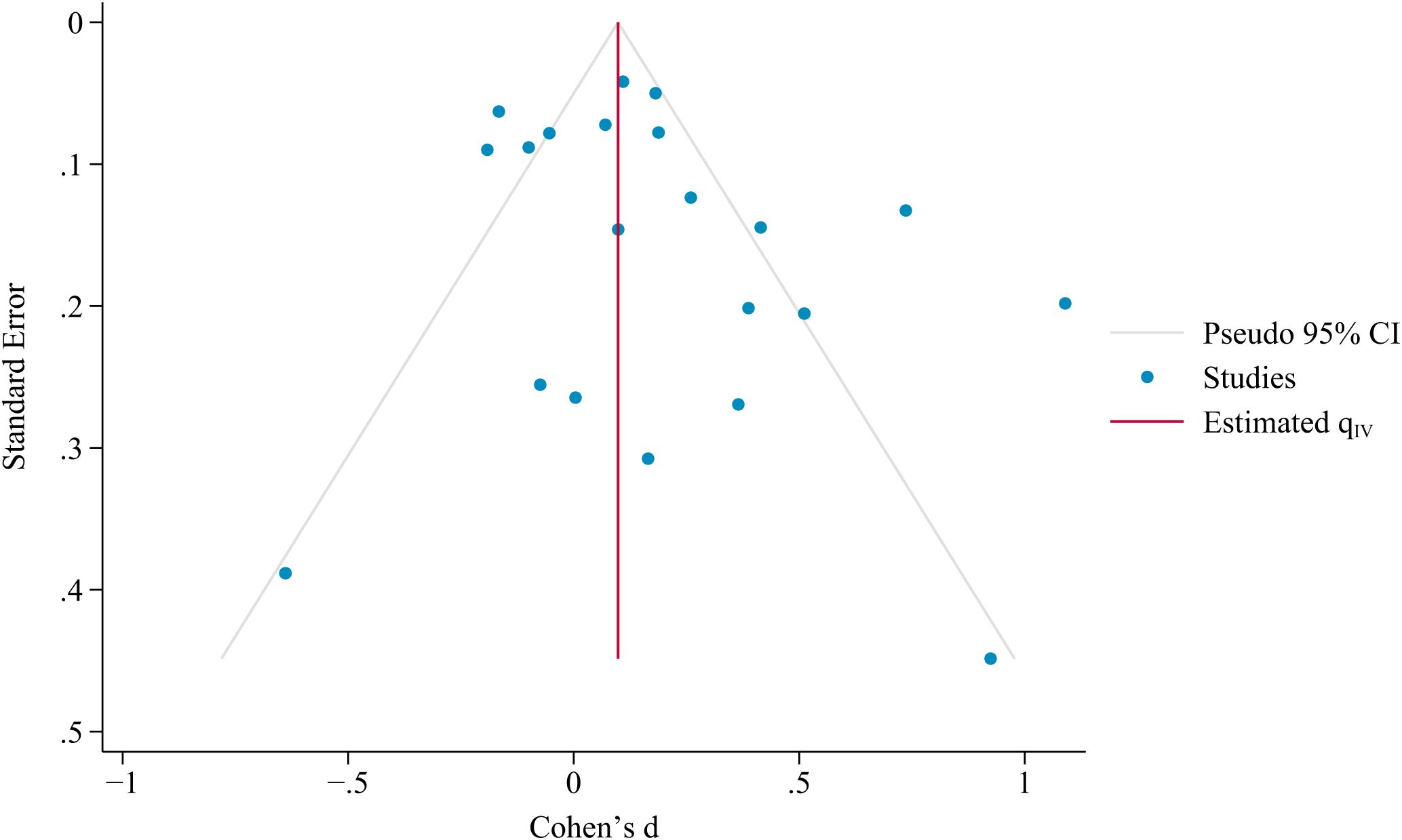
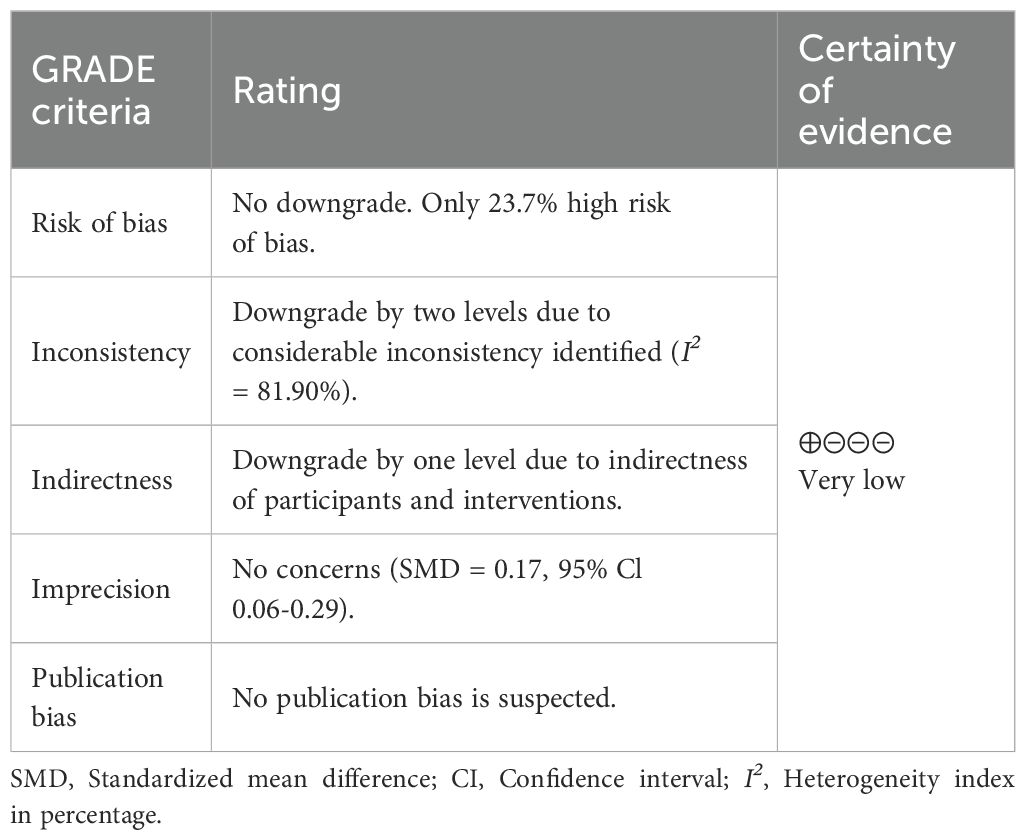
3.7 Publication bias and certainty of evidence
Publication bias was assessed based on a visual inspection of the funnel plot and Egger’s test. The results indicated that the included studies were evenly distributed on both sides of the funnel plot (see Figure 4), with an Egger’s test p of 0.1292. This finding indicates that publication bias has no influence on this study, and there is no significant systematic association between effect sizes and standard errors. According to the GRADE ratings, the certainty of evidence for resilience was very low (see Table 7).
4 Discussion
Children and adolescents often face various stressors as they grow up and may experience cognitive, emotional, and behavioral disorders, particularly when encountering trauma or adversity. Fostering resilience in children and adolescents helps them adapt positively and effectively cope with stressful situations, reducing the risk of maladaptive psychological and behavioral responses and thereby promoting the development of their physical and mental health (86). This systematic review and meta-analysis aimed to evaluate the overall efficacy of SBIs in promoting resilience in children and adolescents and to provide evidence for advancing mental health care for children and adolescents. The pairwise meta-analyses indicated that SBIs significantly enhanced resilience in children and adolescents compared to the control group (SMD = 0.17, 95% Cl 0.06–0.29, p < 0.01). The certainty of evidence for resilience was very low on the basis of the GRADE ratings (52). This finding is supported by previous systematic reviews and meta-analyses (29, 87).
Globally, 10—20% of children and adolescents are experiencing mental health issues (88), and only a minority of these children and adolescents have access to medical-level care due to limited medical resources. These findings suggest that non-pharmacological interventions may have important potential in addressing these challenges. Schools are environments that children and adolescents rely on for their development. Implementing interventions within the school environment can effectively reduce various barriers, including family financial burdens, caregiver burdens, transportation needs, and limited insurance coverage, without requiring significant additional time and human resources. More importantly, schools provide a familiar environment for students, along with support from teachers and peers, which is particularly important for promoting children’s and adolescents’ acceptance and adaptation to interventions (89–91). Furthermore, SBIs are especially crucial for children and adolescents from impoverished or minority communities, as they may be academically disadvantaged compared to children from non-poor or white families. Fostering resilience through SBIs provides these groups with higher-quality and more comprehensive educational experience, helping to prevent inequities in interventions caused by certain disparities (92).
In terms of pairwise meta-analyses, the pooled results indicated that SBIs significantly enhanced resilience in children and adolescents. The robustness of this finding was confirmed by sensitivity analyses, but it was accompanied by considerable heterogeneity. Although this study was unable to identify the sources of heterogeneity in the pooled results through meta-regression and subgroup analyses, this heterogeneity may reflect differences in population characteristics and intervention implementation. On the one hand, the differential efficacy of SBIs may be due to different health challenges or school environments experienced by children and adolescents. On the other hand, the specific processes, measures, and dosage of intervention implementation may also contribute to variations in efficacy. More importantly, the high heterogeneity may reveals a critical issue in the design of current interventions—namely, the lack of standardized procedures, theory-driven, and scalability. The absence of these elements not only limits the comparability and replicability of research findings, but also undermines the potential for SBIs to be effectively scaled and implemented in real educational settings. Researchers and practitioners should strive to develop clear intervention manuals and operational guidelines tailored to the specific conditions of each school, covering key elements such as goal setting, activity content, intervention arrangements, and required resources. The protective possibilities framework of resilience may hold promise in addressing this challenge (33). Future research could establish a unified intervention process and indicator system based on this framework, which would help ensure quality control in intervention implementation. In term of the scalability of SBIs, priority should be given to their cost-effectiveness, feasibility, and adaptability. Although the overall effect size of this study is small, its clinical efficacy may be influenced by population characteristics and intervention implementation. It is recommended to involve educational practitioners (e.g., teachers) during the intervention development stage to ensure that the intervention content aligns with students’ realities and provides implementation willingness and local adaptability. For children and adolescents facing multiple stressors, identifying promising and targeted interventions to enhance their resilience is particularly crucial. In light of this, the differential efficacy of SBIs should be further explored in enhancing resilience in children and adolescents, and identify the most effective SBI should be identified on the basis of the specific conditions of children and adolescents. This will help maximize the efficacy of SBIs in enhancing resilience in children and adolescents in the context of limited medical resources.
The findings of this study should be interpreted with consideration of its limitations. First, the outcome of this study focused only on resilience and did not address other potential outcomes similar to resilience, such as mental toughness and grittiness, although SBIs may have a homogenous effect on these outcomes. Second, this study primarily examined the overall efficacy of SBIs on resilience in children and adolescents and did not identify the most promising interventions. It is recommended that future research should build on existing evidence by conducting more high-quality RCTs and network meta-analyses to explore the differential efficacy of various SBIs in enhancing resilience in children and adolescents. Finally, although this study conducted moderator analyses, the results did not reveal potential sources of heterogeneity. Future research could explore the heterogeneity of the pooled results by incorporating more comprehensive information on demographic characteristics and intervention implementation. This helps further expand insights into the role of SBIs in enhancing resilience, especially in contexts with limited medical resources.
5 Conclusions
In conclusion, the results of this study suggest that SBIs have a positive effect on the resilience of children and adolescents. In the context of limited medical resources, SBIs could serve as a complementary or alternative therapy to promote the ability of children and adolescents to adapt to stressors. Given the considerable heterogeneity identified, clinical practice should prioritize the selection and implementation of interventions that take into account the demographic characteristics of children and adolescents. These interventions should be personalized on the basis of actual dose-response to improve the overall well-being of children and adolescents and reduce the risk of maladaptive psychological and behavioral responses.
Author contributions
CC: Data curation, Conceptualization, Writing – original draft, Methodology, Software, Writing – review & editing, Investigation. ZM: Writing – original draft, Conceptualization, Writing – review & editing, Investigation, Validation, Data curation. ZW: Visualization, Writing – review & editing, Validation. SL: Funding acquisition, Supervision, Project administration, Writing – review & editing, Methodology.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by the National Social Science Fund of China (project 24BTY098).
Acknowledgments
The research team would like to thank Southwest University for the support of this research, and also thank SL for the help in developing the research programme.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1594658/full#supplementary-material
References
1. Gupta S and McCarthy PJ. The sporting resilience model: A systematic review of resilience in sport performers. Front Psychol. (2022) 13:1003053. doi: 10.3389/fpsyg.2022.1003053
2. Mei Z, Jiang W, Zhang Y, Luo S, and Luo S. Mind-body therapies for resilience in adolescents: A systematic review of randomized controlled trials. Gen Hosp Psychiatry. (2024) 91:43–51. doi: 10.1016/j.genhosppsych.2024.08.014
3. Anderson K and Priebe S. Concepts of resilience in adolescent mental health research. J Adolesc Health. (2021) 69:689–95. doi: 10.1016/j.jadohealth.2021.03.035
4. Hill Y, Den Hartigh RJ, Meijer RR, De Jonge P, and Van Yperen NW. The temporal process of resilience. Sport Exercise Performa Psychol. (2018) 7:363–70. doi: 10.1037/spy0000143
5. Métais C, Burel N, Gillham JE, Tarquinio C, and Martin-Krumm C. Integrative review of the recent literature on human resilience: From concepts, theories, and discussions towards a complex understanding. Europe's J Psychol. (2022) 18:98–119. doi: 10.5964/ejop.2251
6. IJntema RC, Schaufeli WB, and Burger YD. Resilience mechanisms at work: The psychological immunity-psychological elasticity (PI-PE) model of psychological resilience. Curr Psychol. (2023) 42:4719–31. doi: 10.1007/s12144-021-01813-5
7. Forehand R, Middleton K, and Long N. Adolescent functioning as a consequence of recent parental divorce and the parent-adolescent relationship. J Appl Dev Psychol. (1987) 8:305–15. doi: 10.1016/0193-3973(87)90006-2
8. Grant KE, Compas BE, Thurm AE, McMahon SD, and Gipson PY. Stressors and child and adolescent psychopathology: Measurement issues and prospective effects. J Clin Child Adolesc Psychol. (2004) 33:412–25. doi: 10.1207/s15374424jccp3302_23
9. Keane K, Evans RR, Orihuela CA, and Mrug S. Teacher–student relationships, stress, and psychosocial functioning during early adolescence. Psychol Schools. (2023) 60:5124–44. doi: 10.1002/pits.23020
10. Vanaelst B, De Vriendt T, Huybrechts I, Rinaldi S, and De Henauw S. Epidemiological approaches to measure childhood stress. Paedia Perinatal Epidemiol. (2012) 26:280–97. doi: 10.1111/j.1365-3016.2012.01258.x
11. Knack JM, Jensen-Campbell LA, and Baum A. Worse than sticks and stones? Bullying is associated with altered HPA axis functioning and poorer health. Brain Cognit. (2011) 77:183–90. doi: 10.1016/j.bandc.2011.06.011
12. Kieling C, Buchweitz C, Caye A, Silvani J, Ameis SH, Brunoni AR, et al. Worldwide prevalence and disability from mental disorders across childhood and adolescence: evidence from the global burden of disease study. JAMA Psychiatry. (2024) 81:347–56. doi: 10.1001/jamapsychiatry.2023.5051
13. Dray J, Bowman J, Campbell E, Freund M, Wolfenden L, Hodder RK, et al. Systematic review of universal resilience-focused interventions targeting child and adolescent mental health in the school setting. J Am Acad Child Adolesc Psychiatry. (2017) 56:813–24. doi: 10.1016/j.jaac.2017.07.780
14. Pinto TM, Laurence PG, Macedo CR, and Macedo EC. Resilience programs for children and adolescents: a systematic review and meta-analysis. Front Psychol. (2021) 12:754115. doi: 10.3389/fpsyg.2021.754115
15. Finch J, Farrell LJ, and Waters AM. Searching for the HERO in youth: Does psychological capital (PsyCap) predict mental health symptoms and subjective wellbeing in Australian school-aged children and adolescents? Child Psychiatry Hum Dev. (2020) 51:1025–36. doi: 10.1007/s10578-020-01023-3
16. Skrove M, Romundstad P, and Indredavik MS. Resilience, lifestyle and symptoms of anxiety and depression in adolescence: the Young-HUNT study. Soc Psychiatry Psychiatr Epidemiol. (2013) 48:407–16. doi: 10.1007/s00127-012-0561-2
17. Hjemdal O, Vogel PA, Solem S, Hagen K, and Stiles TC. The relationship between resilience and levels of anxiety, depression, and obsessive–compulsive symptoms in adolescents. Clin Psychol Psychother. (2011) 18:314–21. doi: 10.1002/cpp.719
18. Ma A, Yang Y, Guo S, Li X, Zhang S, and Chang H. Adolescent resilience and mobile phone addiction in Henan Province of China: Impacts of chain mediating, coping style. PLoS One. (2022) 17:e0278182. doi: 10.1371/journal.pone.0278182
19. Fergus S and Zimmerman MA. Adolescent resilience: A framework for understanding healthy development in the face of risk. Annu Rev Public Health. (2005) 26:399–419. doi: 10.1146/annurev.publhealth.26.021304.144357
20. Regalla MA, Guilherme P, Aguilera P, Serra-Pinheiro MA, and Mattos P. Attention deficit hyperactivity disorder is an independent risk factor for lower resilience in adolescents: a pilot study. Trends Psychiatry Psychother. (2015) 37:157–60. doi: 10.1590/2237-6089-2015-0010
21. Ali MM, Dwyer DS, Vanner EA, and Lopez A. Adolescent propensity to engage in health risky behaviors: The role of individual resilience. Int J Environ Res Public Health. (2010) 7:2161–76. doi: 10.3390/ijerph7052161
22. Kuo C, Mathews C, Giovenco D, Atujuna M, Beardslee W, Hoare J, et al. Acceptability, feasibility, and preliminary efficacy of a resilience-oriented family intervention to prevent adolescent HIV and depression: a pilot randomized controlled trial. AIDS Educ Prevent. (2020) 32:67–81. doi: 10.1521/aeap.2020.32.1.67
23. Mampane MR. The effect of a community-based social support programme on the resilience of children from vulnerable families. Early Child Dev Care. (2020) 190:1638–53. doi: 10.1080/03004430.2019.1670653
24. Lee S, Lee J, and Choi JY. The effect of a resilience improvement program for adolescents with complex congenital heart disease. Eur J Cardiovasc Nurs. (2017) 16:290–8. doi: 10.1177/1474515116659836
26. Rones M and Hoagwood K. School-based mental health services: A research review. Clin Child Family Psychol Rev. (2000) 3:223–41. doi: 10.1023/A:1026425104386
27. Ang WHD, Lau ST, Cheng LJ, Chew HSJ, Tan JH, Shorey S, et al. Effectiveness of resilience interventions for higher education students: A meta-analysis and metaregression. J Educ Psychol. (2022) 114:1670–94. doi: 10.1037/edu0000719
28. Liu JJ, Ein N, Gervasio J, Battaion M, Reed M, and Vickers K. Comprehensive meta-analysis of resilience interventions. Clin Psychol Rev. (2020) 82:101919. doi: 10.1016/j.cpr.2020.101919
29. Llistosella M, Goni-Fuste B, Martín-Delgado L, Miranda-Mendizabal A, Franch Martinez B, Pérez-Ventana C, et al. Effectiveness of resilience-based interventions in schools for adolescents: A systematic review and meta-analysis. Front Psychol. (2023) 14:1211113. doi: 10.3389/fpsyg.2023.1211113
30. Katz DL. School-based interventions for health promotion and weight control: not just waiting on the world to change. Annu Rev Public Health. (2009) 30:253–72. doi: 10.1146/annurev.publhealth.031308.100307
31. Kazdin AE and Johnson B. Advances in psychotherapy for children and adolescents: Interrelations of adjustment, development, and intervention. J School Psychol. (1994) 32:217–46. doi: 10.1016/0022-4405(94)90016-7
32. Rava J, Hotez E, and Halfon N. The role of social capital in resilience among adolescents with adverse family environments. Curr Prob Pediatr Adolesc Health Care. (2023) 53:101436. doi: 10.1016/j.cppeds.2023.101436
33. Morrison GM and Allen MR. Promoting student resilience in school contexts. Theory into Pract. (2007) 46:162–9. doi: 10.1080/00405840701233172
34. Amin R, Nadeem E, Iqbal K, Asadullah MA, and Hussain B. Support for students exposed to trauma (SSET) program: An approach for building resilience and social support among flood-impacted children. School Ment Health. (2020) 12:493–506. doi: 10.1007/s12310-020-09373-y
35. Cheng C, Li S, and Chen S. Evaluation of a multicomponent positive psychology program to prevent gaming disorder and enhance mental wellness in primary pupils: A randomized controlled trial. J Behav Addict. (2024) 13:871–83. doi: 10.1556/2006.2024.00052
36. Khalsa SBS, Hickey-Schultz L, Cohen D, Steiner N, and Cope S. Evaluation of the mental health benefits of yoga in a secondary school: A preliminary randomized controlled trial. J Behav Health Serv Res. (2012) 39:80–90. doi: 10.1007/s11414-011-9249-8
37. Bogaert L, Hallford D, Loyen E, D'Argembeau A, and Raes F. Recalling and anticipating positive events to improve the positive affect and mental health of adolescents: A cluster randomized controlled trial in secondary schools. Behav Res Ther. (2024) 179:104543. doi: 10.1016/j.brat.2024.104543
38. Niu Y, Jiang X, Ashong Z, Hou J, Bai Y, Bai G, et al. Developing a resilience intervention approach for adolescents living with natural hazards risks: A pilot randomized controlled trial. Int J Disas Risk Reduct. (2021) 58:102190. doi: 10.1016/j.ijdrr.2021.102190
39. Porter B, Oyanadel C, Sáez-Delgado F, Andaur A, and Peñate W. Systematic review of mindfulness-based interventions in child-adolescent population: A developmental perspective. Eur J Invest Health Psychol Educ. (2022) 12:1220–43. doi: 10.3390/ejihpe12080085
40. Sun J and Stewart D. Age and gender effects on resilience in children and adolescents. Int J Ment Health promot. (2007) 9:16–25. doi: 10.1080/14623730.2007.9721845
41. Prabhu SG and Shekhar R. The role of socio-economic status in adolescent resilience and self-esteem. Indian J Health Wellbeing. (2017) 8:985–9.
42. Zolkoski SM and Bullock LM. Resilience in children and youth: A review. Children Youth Serv Rev. (2012) 34:2295–303. doi: 10.1016/j.childyouth.2012.08.009
43. Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Internal Med. (2015) 162:777–84. doi: 10.7326/M14-2385
44. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:1–9. doi: 10.1136/bmj.d5928
45. Deeks JJ, Higgins JP, Altman DG, and Group CSM. Analysing data and undertaking meta-analyses. In: Higgins J, Thomas J, Chandler J, Cumpston M, Li TPM, and Welch V, editors. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons, Hoboken (2019). p. 241–84.
46. Higgins JP, Thompson SG, Deeks JJ, and Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
47. Jackson D, Riley R, and White IR. Multivariate meta-analysis: potential and promise. Stat Med. (2011) 30:2481–98. doi: 10.1002/sim.4172
48. Harbord RM and Higgins JP. Meta-regression in stata. Stata J. (2008) 8:493–519. doi: 10.1177/1536867X0800800403
49. Egger M, Smith GD, Schneider M, and Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
50. Tang J-L and Liu JL. Misleading funnel plot for detection of bias in meta-analysis. J Clin epidemiol. (2000) 53:477–84. doi: 10.1016/S0895-4356(99)00204-8
51. Duval S and Tweedie R. Trim and fill: a simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics. (2000) 56:455–63. doi: 10.1111/j.0006-341X.2000.00455.x
52. Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, and Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. (2011) 64:380–2. doi: 10.1016/j.jclinepi.2010.09.011
53. Chen J, Johnstone KM, and Kemps E. A randomised controlled trial evaluating two universal prevention programs for children: Building resilience to manage worry. J Affect Disord. (2022) 297:437–46. doi: 10.1016/j.jad.2021.10.079
54. Chisholm K, Patterson P, Torgerson C, Turner E, Jenkinson D, and Birchwood M. Impact of contact on adolescents' mental health literacy and stigma: the SchoolSpace cluster randomised controlled trial. BMJ Open. (2016) 6:1–11. doi: 10.1136/bmjopen-2015-009435
55. Felver JC, Clawson AJ, Morton ML, Brier-Kennedy E, Janack P, and DiFlorio RA. School-based mindfulness intervention supports adolescent resiliency: A randomized controlled pilot study. Int J School Educ Psychol. (2019) 7:111–22. doi: 10.1080/21683603.2018.1461722
56. Gance-Cleveland B and Mays MZ. School-based support groups for adolescents with a substance-abusing parent. J Am Psychiatr Nurs Associat. (2008) 14:297–309. doi: 10.1177/1078390308321223
57. Gao J, Roslan S, Soh KG, and Zaremohzzabieh Z. Effects of positive education intervention on growth mindset and resilience among boarding middle school adolescents in China: a randomized controlled trial. Front Psychol. (2024) 15:1446260. doi: 10.3389/fpsyg.2024.1446260
58. Gomez-Restrepo C, Sarmiento-Suarez MJ, Alba-Saavedra M, Calvo-Valderrama MG, Rincon-Rodriguez CJ, Bird VJ, et al. Development and implementation of DIALOG+S in the school setting as a tool for promoting adolescent mental well-being and resilience in a post-armed conflict area in Colombia: exploratory cluster randomized controlled trial. JMIR Formative Res. (2023) 7:e46757. doi: 10.2196/46757
59. Greco G, Cataldi S, and Fischetti F. Karate as anti-bullying strategy by improvement resilience and self-efficacy in school-age youth. J Phys Educ Sport. (2019) 19:1863–70. doi: 10.7752/jpes.2019.s5276
60. Green AL, Ferrante S, Boaz TL, Kutash K, and Wheeldon-Reece B. Social and emotional learning during early adolescence: Effectiveness of a classroom-based SEL program for middle school students. Psychol Schools. (2021) 58:1056–69. doi: 10.1002/pits.22487
61. Green AL, Ferrante S, Boaz TL, Kutash K, and Wheeldon-Reece B. Evaluation of the SPARK child mentoring program: A social and emotional learning curriculum for elementary school students. J Primary Prevent. (2021) 42:531–47. doi: 10.1007/s10935-021-00642-3
62. Green AL, Ferrante S, Boaz TL, Kutash K, and Wheeldon-Reece B. Effects of the SPARK teen mentoring program for high school students. J Child Family Stud. (2022) 31:1982–93. doi: 10.1007/s10826-022-02298-x
63. Hatamizadeh N, Adibsereshki N, Kazemnejad A, and Sajedi F. Randomized trial of a resilience intervention on resilience, behavioral strengths and difficulties of mainstreamed adolescent students with hearing loss. Int J Pediatr Otorhinolaryngol. (2020) 128:109722. doi: 10.1016/j.ijporl.2019.109722
64. Ho FKW, Louie LHT, Hing-Sang Wong W, Chan KL, Tiwari A, Chow CB, et al. A sports-based youth development program, teen mental health, and physical fitness: An RCT. Pediatrics. (2017) 140:e20171543. doi: 10.1542/peds.2017-1543
65. Huang W, Wu P, Li J, Zhou Y, Xiong Z, Su P, et al. Effectiveness of a universal resilience-focused intervention for children in the school setting: A randomized controlled trial. J Affect Disord. (2025) 368:695–703. doi: 10.1016/j.jad.2024.09.120
66. Hyun MS, Nam KA, and Kim MA. Randomized controlled trial of a cognitive-behavioral therapy for at-risk korean male adolescents. Arch Psychiatr Nurs. (2010) 24:202–11. doi: 10.1016/j.apnu.2009.07.005
67. Irfan Arif M and Mirza MS. Effectiveness of an Intervention Program in Fostering Academic Resilience of Students at Risk of Failure at Secondary School Level. Bull Educ Res. (2017) 39:251–64.
68. Johnstone KM, Middleton T, Kemps E, and Chen J. A pilot investigation of universal school-based prevention programs for anxiety and depression symptomology in children: A randomized controlled trial. J Clin Psychol. (2020) 76:1193–216. doi: 10.1002/jclp.22926
69. Jones BK and Destin M. Effects of positive versus negative expressive writing exercises on adolescent academic achievement. J Appl Soc Psychol. (2021) 51:549–59. doi: 10.1111/jasp.12756
70. Laundy K, Friberg P, Osika W, and Chen Y. Mindfulness-based intervention for children with mental health problems: a 2-year follow-up randomized controlled study. Mindfulness. (2021) 12:3073–85. doi: 10.1007/s12671-021-01771-w
71. Leventhal KS, Gillham J, DeMaria L, Andrew G, Peabody J, and Leventhal S. Building psychosocial assets and wellbeing among adolescent girls: A randomized controlled trial. J Adolesc. (2015) 45:284–95. doi: 10.1016/j.adolescence.2015.09.011
72. Li CX, Ma C, Li P, and Liang ZJ. The effect of model-based group counseling on the resiliency of disadvantaged adolescents from poor areas of China: A single-blind randomized controlled study. School Ment Health. (2022) 14:550–67. doi: 10.1007/s12310-021-09479-x
73. Liu X, Lei L, Zheng Y, Deng Y, and Chen J. Alleviating learning burnout of Chinese middle school students by school-based mindfulness training: The mediating role of psychological resilience. Psychol Schools. (2024) 61:1034–53. doi: 10.1002/pits.23101
74. Llistosella M, Castellvi P, Garcia-Ortiz M, Lopez-Hita G, Torne C, Ortiz R, et al. Effectiveness of an Intervention Program in Fostering Academic Resilience of Students at Risk of Failure at Secondary School Level. Front Psychol. (2024) 15:1478424. doi: 10.3389/fpsyg.2024.1478424
75. Mertens ECA, Dekovic M, van Londen M, and Reitz E. Parallel changes in positive youth development and self-awareness: the role of emotional self-regulation, self-esteem, and self-reflection. Prev Sci. (2022) 23:502–12. doi: 10.1007/s11121-022-01345-9
76. Moore B, Woodcock S, and Dudley D. Well-being warriors: A randomized controlled trial examining the effects of martial arts training on secondary students' resilience. Br J Educ Psychol. (2021) 91:1369–94. doi: 10.1111/bjep.12422
77. Moran MJ, Aichele S, Shomaker LB, Lucas-Thompson RG, Heberlein E, Chandrasekhar JL, et al. Supporting youth mental health through a health coaching intervention with a mindfulness component: A pilot randomized controlled trial during COVID-19. Child Youth Care Forum. (2024) 53:645–66. doi: 10.1007/s10566-023-09764-7
78. Noggle JJ, Steiner NJ, Minami T, and Khalsa SBS. Benefits of yoga for psychosocial well-being in a US high school curriculum: A preliminary randomized controlled trial. J Dev Behav Pediatr. (2012) 33:193–201. doi: 10.1097/DBP.0b013e31824afdc4
79. O'Connor M, O'Reilly G, Murphy E, Connaughton L, Hoctor E, and McHugh L. Universal process-based CBT for positive mental health in early adolescence: A cluster randomized controlled trial. Behav Res Ther. (2022) 154:104120. doi: 10.1016/j.brat.2022.104120
80. Peter A, Srivastava R, Agarwal A, and Singh AP. The effect of mindfulness-based cognitive therapy on anxiety and resilience of the school going early adolescents with anxiety. J Indian Assoc Child Adolesc Ment Health. (2022) 18:176–85. doi: 10.1177/09731342221127959
81. Rice KJ, Chen J, Kemps E, Roberts RM, Edwards S, and Johnstone K. Two universal school-based prevention programs for depression and anxiety: 24-Month follow-up of an RCT. J Behav Ther Exp Psychiatry. (2024) 85:101985. doi: 10.1016/j.jbtep.2024.101985
82. Rich BA, Starin NS, Senior CJ, Zarger MM, Cummings CM, Collado A, et al. Improved resilience and academics following A school-based resilience intervention: A randomized controlled trial. Evidence-Based Pract Child Adolesc Ment Health. (2023) 8:252–68. doi: 10.1080/23794925.2022.2025630
83. Seale JP, Seale DM, Pande Y, Lewis TM, Manda W, Kasanga L, et al. GROW Zambia: A pilot cluster-randomized trial of a spiritually-based character strengths training curriculum to enhance resilience among Zambian youth. J Positive Psychol. (2022) 17:596–609. doi: 10.1080/17439760.2021.1913640
84. Tang Y, Diao H, Jin F, Pu Y, and Wang H. The effect of peer education based on adolescent health education on the resilience of children and adolescents: A cluster randomized controlled trial. PLoS One. (2022) 17:e0263012. doi: 10.1371/journal.pone.0263012
85. Volanen SM, Lassander M, Hankonen N, Santalahti P, Hintsanen M, Simonsen N, et al. Healthy learning mind – Effectiveness of a mindfulness program on mental health compared to a relaxation program and teaching as usual in schools: A cluster-randomised controlled trial. J Affect Disord. (2020) 260:660–9. doi: 10.1016/j.jad.2019.08.087
86. Richards M, Lewis G, Cornelli Sanderson R, Deane K, and Quimby D. Introduction to special issue: Resilience-based approaches to trauma intervention for children and adolescents. J Child Adolesc Trauma. (2016) 9:1–4. doi: 10.1007/s40653-016-0081-4
87. Zenner C, Herrnleben-Kurz S, and Walach H. Mindfulness-based interventions in schools—a systematic review and meta-analysis. Front Psychol. (2014) 5:603. doi: 10.3389/fpsyg.2014.00603
88. Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, et al. Child and adolescent mental health worldwide: evidence for action. Lancet. (2011) 378:1515–25. doi: 10.1016/S01406736(11)60827-1
89. Fusick L and Bordeau WC. Counseling at-risk Afro-American youth: An examination of contemporary issues and effective school-based strategies. Prof School Counsel. (2004) 8:102–15.
90. Owens JS and Murphy CE. Effectiveness research in the context of school-based mental health. Clin Child Family Psychol Rev. (2004) 7:195–209. doi: 10.1007/s10567-004-6085-x
91. Pandey A, Hale D, Das S, Goddings A-L, Blakemore S-J, and Viner RM. Effectiveness of universal self-regulation–based interventions in children and adolescents: A systematic review and meta-analysis. JAMA Pediatr. (2018) 172:566–75. doi: 10.1001/jamapediatrics.2018.0232
Keywords: school-based interventions, resilience, children, adolescents, mental health
Citation: Cai C, Mei Z, Wang Z and Luo S (2025) School-based interventions for resilience in children and adolescents: a systematic review and meta-analysis of randomized controlled trials. Front. Psychiatry 16:1594658. doi: 10.3389/fpsyt.2025.1594658
Received: 16 March 2025; Accepted: 14 April 2025;
Published: 19 May 2025.
Edited by:
Yibo Wu, Peking University, ChinaReviewed by:
Mar Diaz, University of Jaén, SpainYuhan Hu, Erasmus University Rotterdam, Netherlands
Jose Angel Vera Noriega, University of Sonora, Mexico
Copyright © 2025 Cai, Mei, Wang and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shi Luo, bHVvc2hpMDYwNEAxMjYuY29t
†These authors have contributed equally to this work
 Chenyi Cai
Chenyi Cai Zhengyang Mei
Zhengyang Mei Zirui Wang2
Zirui Wang2 Shi Luo
Shi Luo