- 1Department of Anesthesiology, The First People’s Hospital of Kunshan Affiliated with Jiangsu University, Kunshan, China
- 2Kunshan Biomedical Big Data Innovation Application Laboratory, Jiangsu, China
- 3Kunshan Cancer Pain Prevention and Treatment Key Laboratory, Jiangsu, China
Objective: The complex interplay between visceral adiposity and mental health outcomes, particularly suicidal ideation, remains a critical yet understudied area.
Methods: This cross-sectional analysis utilized data from the National Health and Nutrition Examination Survey (NHANES 2005-2018), examining 11,931 adults aged ≥20 years. Visceral adiposity index (VAI) was calculated using sex-specific equations. Suicidal ideation was assessed using item 9 of the Patient Health Questionnaire-9 (PHQ-9). We employed multivariable logistic regression models, generalized additive models (GAM), threshold effect analysis using segmented regression, and mediation analysis via fasting blood glucose (FBG) with 5,000 bootstrap resamples.
Results: A significant non-linear association between VAI and suicidal ideation was identified, with a threshold effect at VAI=6.81 (likelihood ratio test, P=0.006). Below this threshold, each unit increase in VAI was associated with 9.4% higher odds of suicidal ideation (OR=1.094, 95% CI: 1.028-1.163, P=0.005), while no significant association was observed above the threshold. FBG mediated 31.74% (95% CI: 4.43%-181.74%) of this relationship. The association was particularly pronounced among older adults (≥60 years), females, and individuals with diabetes or hypertension.
Conclusions: These findings highlight the importance of considering visceral adiposity in mental health assessments, especially among vulnerable populations, and suggest potential metabolic pathways linking adiposity to mental health outcomes through glucose metabolism.
Introduction
Suicide ideation represents a significant global public health concern, with depression being one of its primary contributing factors. According to the World Health Organization (WHO), approximately 800,000 individuals die by suicide annually, corresponding to a global mortality rate of 11.4 per 100,000 population, with suicide accounting for 1% of all deaths worldwide (1). The prevalence of depression, a major risk factor for suicide ideation, exhibits significant variation across diverse populations and regions. Global epidemiological data indicate that depression affects approximately 300 million people, with a worldwide prevalence of 4.4% (2). In the United States, the lifetime prevalence of depression is estimated at 16% (3), while in China, the prevalence of depressive symptoms among middle-aged and elderly adults reaches 35.19% (3, 4).
Recent epidemiological studies have yielded comprehensive insights into the prevalence of suicidal behaviors. A systematic review of the European general population revealed annual prevalence rates of 3.6%, 1.6%, and 0.5% for suicidal thoughts, plans, and attempts, respectively (5). These findings are corroborated by regional studies, such as one conducted in Andalusia, which reported point prevalence rates of 2.4% for suicidal ideation, 1.1% for suicide plans, and 0.6% for suicide attempts (5).
Beyond epidemiological data, understanding the underlying mechanisms is crucial. The relationship between adiposity and mental health outcomes, including suicide ideation, likely involves both biological and psychological pathways. From a biological perspective, visceral adipose tissue functions as an active endocrine organ that secretes pro-inflammatory cytokines which may induce neuroinflammation and affect neurotransmitter systems implicated in mood regulation (6–8). Visceral adiposity is also associated with insulin resistance and hypothalamic-pituitary-adrenal axis dysregulation, potentially affecting brain regions involved in emotional processing (7). Psychologically, individuals with obesity often experience weight stigma, discrimination, and reduced quality of life, which may contribute to depressive symptoms and, in some cases, suicidal thoughts (9, 10).
Emerging research indicates that insulin resistance, frequently observed with visceral obesity, leads to chronically elevated fasting blood glucose (FBG). Elevated FBG can disrupt neuronal energy metabolism, increase oxidative stress, and promote neuroinflammation—factors known to impair emotion regulation and contribute to increased risk of depression and suicidal behavior (11). Chronic hyperglycemia has also been associated with hippocampal and cortical dysfunction in neuroimaging studies (12), providing a plausible mechanistic link between metabolic syndrome and psychiatric outcomes. Consequently, FBG may function as a pivotal metabolic mediator, establishing a connection between visceral adiposity and suicidal ideation.
The Visceral Adiposity Index (VAI) has emerged as a novel biological indicator for assessing visceral fat accumulation and associated metabolic risks. Unlike traditional anthropometric measures such as the Body Mass Index (BMI), the VAI offers distinct advantages in evaluating fat distribution, particularly visceral adiposity, by incorporating multiple parameters including waist circumference, weight, height, and biochemical indicators. Recent research has demonstrated significant associations between VAI and various health conditions, including type 2 diabetes (13), cardiovascular diseases (14), and depression (15). Furthermore, VAI has shown superior predictive capability compared to BMI in discriminating different types of adiposity and associated health risks.
However, the relationship between VAI and suicide ideation remains largely unexplored. While extant research has identified associations between VAI and certain psychological parameters, such as impulsive behaviors in severely obese individuals, the specific mechanisms and extent of these relationships require further investigation (16). Earlier studies have indicated that individuals with BMI ≥25 demonstrate higher proportions of suicide ideation, suggesting a potential link between adiposity measures and suicide risk (17). Furthermore, the established role of VAI as a predictor of cardiovascular disease and metabolic syndrome suggests the possibility of indirect effects on suicide ideation through its impact on quality of life and psychological well-being.
The present study aims to investigate the potential relationship between visceral adiposity, as measured by VAI, and suicidal ideation, with particular focus on identifying any non-linear patterns or threshold effects. Additionally, we explore the potential mediating role of fasting blood glucose and examine effect modification by demographic and clinical subgroups. Using data from the National Health and Nutrition Examination Survey (NHANES), this research seeks to enhance our understanding of how metabolic factors may influence mental health outcomes, potentially informing more comprehensive approaches to suicide risk assessment.
2 Methods
2.1 Study design and population
This cross-sectional study utilized data from NHANES, a nationally representative survey designed to assess the health and nutritional status of the U.S. population. Data were collected from 2005 to 2018, encompassing 70,190 individuals. After excluding participants under 20 years of age and those with missing data, a total of 11,931 subjects were included in the final analysis.
All participants provided written informed consent, and the study protocol was approved by the National Center for Health Statistics Research Ethics Review Board. The inclusion and exclusion criteria are outlined in detail in Supplementary Figure 1.
2.2 Assessment of variables
2.2.1 Exposure variable
The VAI was utilized as the primary exposure variable and calculated using sex-specific equations:
For males, the following equation was used: VAI = (WC/[39.68 + (1.88 × BMI)] × (TG/1.03) × (1.31/HDL).
Females: VAI = (WC/[36.58 + (1.89 × BMI)] × (TG/0.81) × (1.52/HDL) where WC is waist circumference (cm), BMI is body mass index (kg/m²), TG is triglycerides (mmol/L), and HDL is high-density lipoprotein cholesterol (mmol/L). VAI has been demonstrated to reflect visceral fat deposition, with higher scores indicating greater visceral adiposity (18–20). To facilitate analysis, VAI values were stratified into three tertiles: low (0.134–1.285), middle (1.286–2.514), and high (2.515–135.673).
2.2.2 Outcome variables
The primary outcomes were suicidal ideation:
Depressive symptoms over the past two weeks were evaluated using the full Patient Health Questionnaire-9 (PHQ-9), which assesses nine core symptoms of depression, including low mood, sleep disturbances, fatigue, appetite changes, and concentration difficulties. The total score ranges from 0 to 27, with scores ≥10 indicating the presence of depressive symptoms (21–23).
The assessment of suicidal ideation entailed the utilization of item 9 of the PHQ-9, which specifically evaluates thoughts of self-harm or death over the past two weeks. Responses to this item were scored on a 4-point scale (0 = “not at all” to 3 = “nearly every day”), with scores ≥1 classified as suicidal ideation. Participants were then categorized into two distinct groups based on the presence or absence of suicidal ideation.
2.2.3 Covariates
In the analysis, potential confounding factors were adjusted for, including demographic characteristics, socioeconomic factors, lifestyle factors, clinical measurements, and medical conditions. The demographic characteristics encompassed age, sex (male/female), race/ethnicity (Mexican-American, non-Hispanic Black, non-Hispanic White, Hispanic, and other), educational attainment (below high school, high school graduate, some college, or college graduate), and marital status (married, living with a partner, never married, divorced, widowed, or separated). Socioeconomic factors included the family income-to-poverty ratio. The lifestyle factors considered in this study included smoking status, defined as a lifetime consumption of at least 100 cigarettes, and alcohol consumption, defined as a minimum of 12 alcoholic drinks in any given year. Clinical measurements included fasting glucose (mmol/L), systemic immune-inflammation index (SII), and laboratory parameters, including total cholesterol. The medical conditions encompassed hypertension and diabetes mellitus, both of which were self-reported based on physician diagnosis.
2.3 Statistical analysis
The participants were grouped into two categories, suicide ideation and non-suicide ideation, based on their responses to item 9 of the PHQ-9. The statistical analyses for baseline characteristics took into account the complex survey design of NHANES by incorporating appropriate sampling weights, as recommended by NHANES guidelines and procedures. For continuous variables, data were presented as survey-weighted means with 95% confidence intervals (CIs) and compared using survey-weighted t-tests. Categorical variables were expressed as survey-weighted percentages with 95% CIs and compared using chi-square tests.
The association between VAI and suicide ideation was assessed using multiple logistic regression models. Three models were constructed to account for potential confounders: The first model was unadjusted. Model 2: Adjusted for demographic characteristics, including age, sex, race/ethnicity, education level, and marital status. The third model was additionally adjusted for lifestyle factors (smoking status and alcohol consumption), socioeconomic status (family income-to-poverty ratio), and medical conditions (hypertension and diabetes).
In order to explore potential non-linear relationships between VAI and suicide ideation, a generalized additive model (GAM) was employed. This approach enabled the visualization of non-linear associations and the identification of potential inflection points. To this end, a threshold effect analysis was conducted to ascertain the inflection point in the relationship between VAI and suicide ideation. In this analysis, segmented regression models were applied to quantify associations on either side of the threshold.
Mediation analysis was performed to evaluate the indirect effect of fasting blood glucose (FBG) on the association between VAI and suicide ideation. The proportion of the total effect mediated by FBG was calculated using the product-of-coefficients method, with bootstrapping (5,000 resamples) employed to estimate 95% CIs for the mediated effect.
Subgroup analyses were conducted to assess potential effect modification by age, sex, smoking status, drinking status, hypertension, and diabetes. Interaction terms were incorporated into the logistic regression models to ascertain the statistical significance of effect modification.
A sensitivity analysis was performed by excluding pregnant women, resulting in a final sample size of 11,713 participants. The robustness of the results was then tested using multivariate regression, curve fitting, and threshold saturation effect analysis. Gender-stratified subgroup analyses were also conducted to evaluate whether the effects of the main variables differed by sex.
All statistical analyses were performed using R software (version 4.1.0; R Foundation for Statistical Computing, Vienna, Austria). Two-sided p-values less than 0.05 were considered statistically significant. It is imperative to note that all statistical tests were two-sided, with a significance level set at p<0.05.
3 Results
3.1 Baseline characteristics
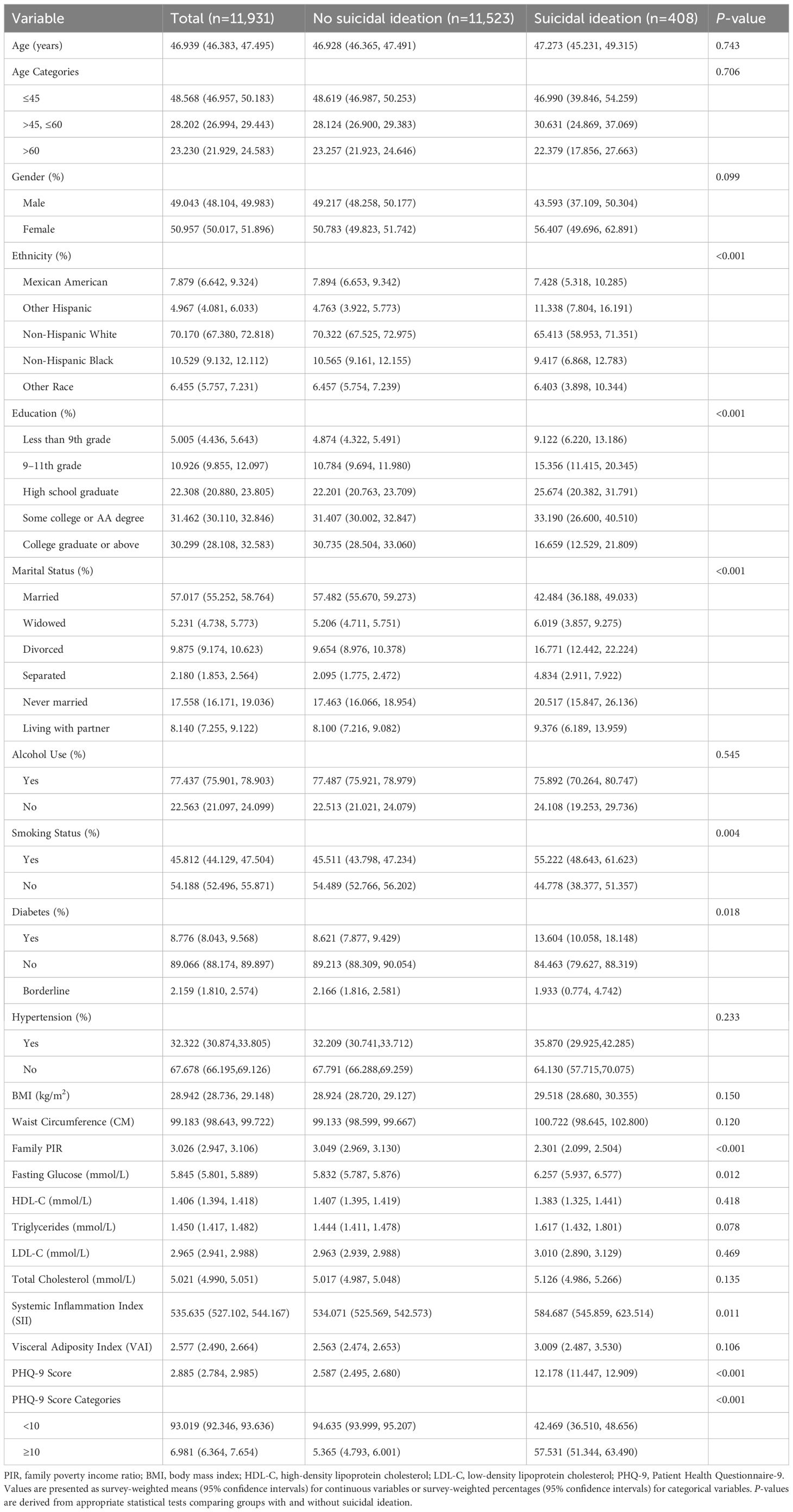
The present study encompassed a total of 11,931 participants, of whom 408 (3.42%) exhibited suicidal ideation and 11,523 (96.58%) did not (Table 1). The mean age of participants was 46.94 years (95% CI: 46.38–47.50), with no significant difference between groups (P=0.743). Individuals who reported suicidal ideation exhibited significantly higher PHQ-9 scores (12.18 vs. 2.59, P<0.001) and lower family income-to-poverty ratios (2.30 vs. 3.05, P<0.001) compared to those without suicidal ideation.
A statistically significant disparity in marital status was observed between the groups (P<0.001). The suicidal ideation group exhibited a lower proportion of married individuals (42.48% vs. 57.48%) and higher rates of divorce (16.77% vs. 9.65%) and widowhood (4.83% vs. 2.10%). While no significant differences were observed in alcohol consumption (P=0.545), BMI (P=0.150), waist circumference (P=0.120), or VAI (P=0.106), participants with suicidal ideation exhibited significantly elevated fasting glucose levels (6.26 vs 5.83 mmol/L, P=0.012) and systemic immune-inflammation index (584.69 vs 534.07, P=0.011). The prevalence of diabetes was found to be significantly higher in the suicidal ideation group compared to the control group (13.60% vs. 8.62%, P=0.018). A statistically significant difference was observed in educational attainment and racial distribution between the two groups (both P<0.001). The suicidal ideation group exhibited a higher proportion of smokers (55.22% vs. 45.51%, P=0.004).
3.2 Association between visceral adiposity index and suicidal ideation
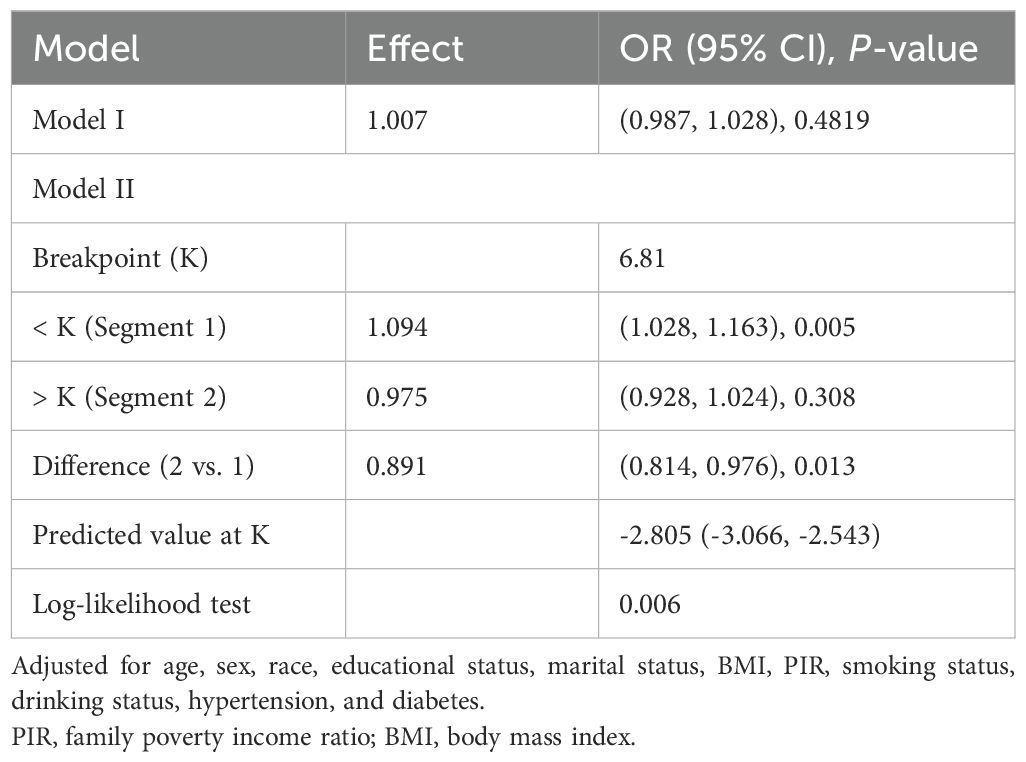
The association between VAI and suicidal ideation was examined using multiple logistic regression models (Table 2). When VAI was analyzed as a continuous variable, the unadjusted model demonstrated a marginally significant association (OR=1.018, 95% CI: 1.000–1.037, P=0.045). However, this association was attenuated and became non-significant after adjusting for potential confounders (fully adjusted OR=1.007, 95% CI: 0.987–1.028, P=0.482).
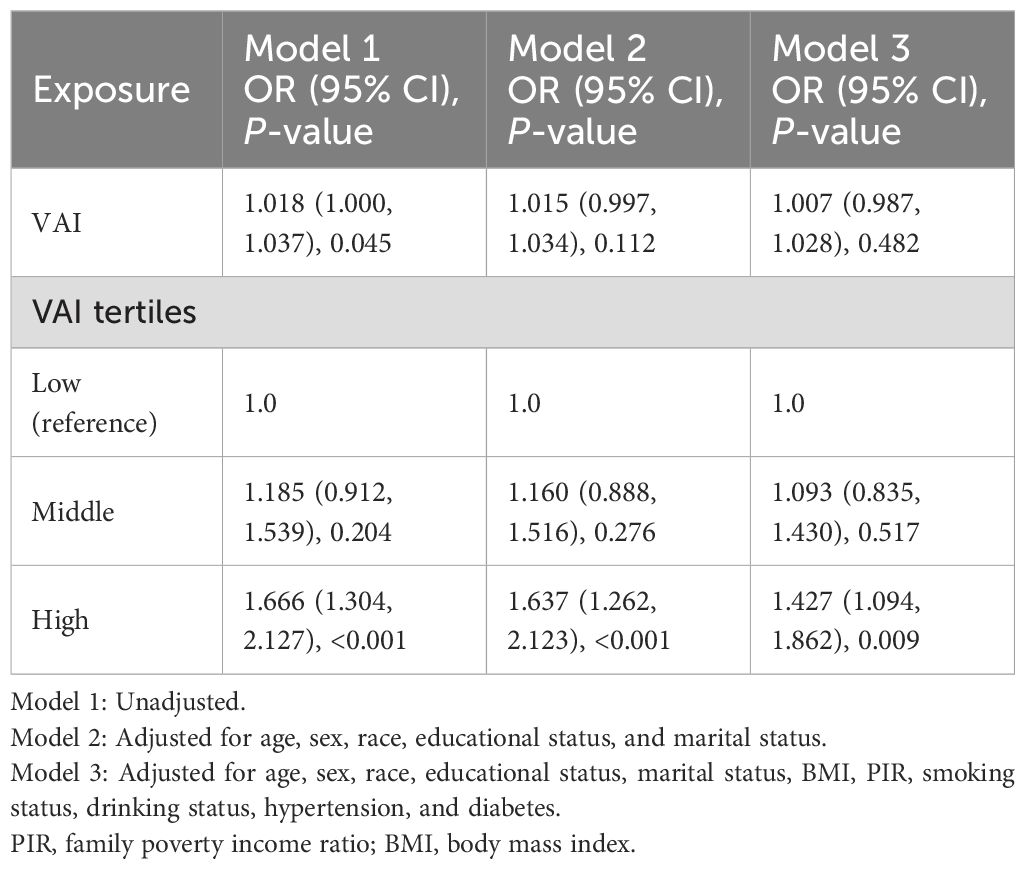
Table 2. Multivariate logistic regression analysis of visceral adiposity index and suicidal ideation.
When VAI was categorized into tertiles, a robust association was observed between elevated VAI levels and an increased risk of suicidal ideation. Compared with the lowest tertile, participants in the highest VAI tertile demonstrated significantly higher odds of suicidal ideation across all models. This association remained significant even after full adjustment for demographic characteristics, lifestyle factors, and comorbidities (OR=1.427, 95% CI: 1.094–1.862, P=0.009), indicating a 42.7% higher risk of suicidal ideation in the high VAI group. No significant association was observed in the middle VAI tertile compared to the lowest tertile (fully adjusted OR=1.093, 95% CI: 0.835–1.430, P=0.517).
3.3 Threshold effect analysis
GAM and threshold effect analysis revealed a significant non-linear relationship between VAI and suicidal ideation (likelihood ratio test, P=0.006), with a turning point identified at VAI=6.81 (Figure 1; Table 3). For VAI values below 6.81, a significant positive association with suicidal ideation was observed (OR=1.094, 95% CI: 1.028–1.163, P =0.005), indicating that each unit increase in VAI was associated with 9.4% higher odds of suicidal ideation. However, this association was not observed for VAI values above 6.81 (OR=0.975, 95% CI: 0.928–1.024, P=0.308).
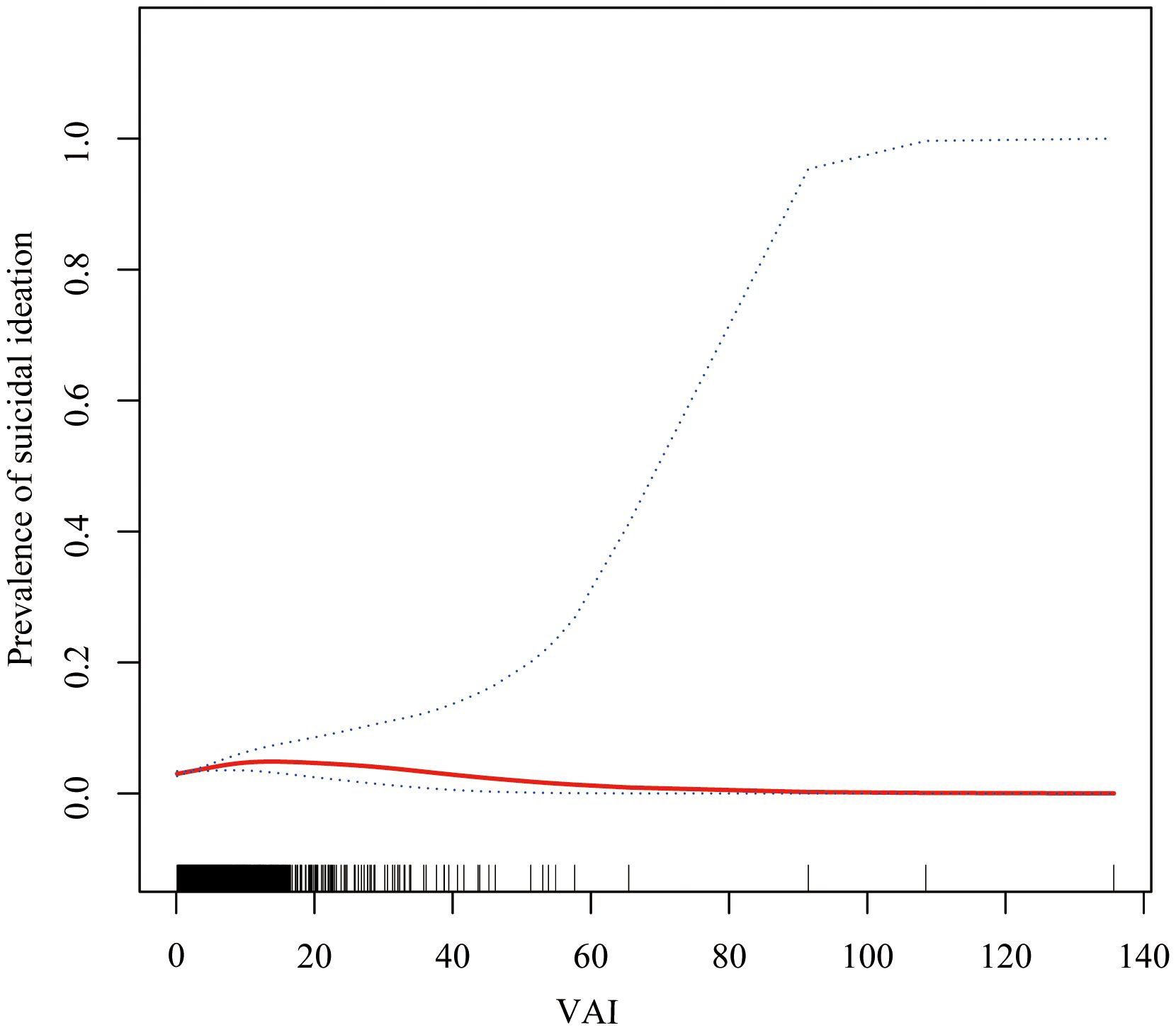
Figure 1. Non-linear relationship between visceral adiposity index (VAI) and risk of suicide ideation. The smooth curve fitting analysis shows the adjusted relationship between VAI and suicide ideation. The solid line represents the estimated probability of suicide ideation, and the dashed lines represent the 95% confidence interval. The analysis was adjusted for age, sex, race/ethnicity, educational level, marital status, alcohol consumption, smoking status, family poverty-income ratio, hypertension, and diabetes.
3.4 Subgroup analysis
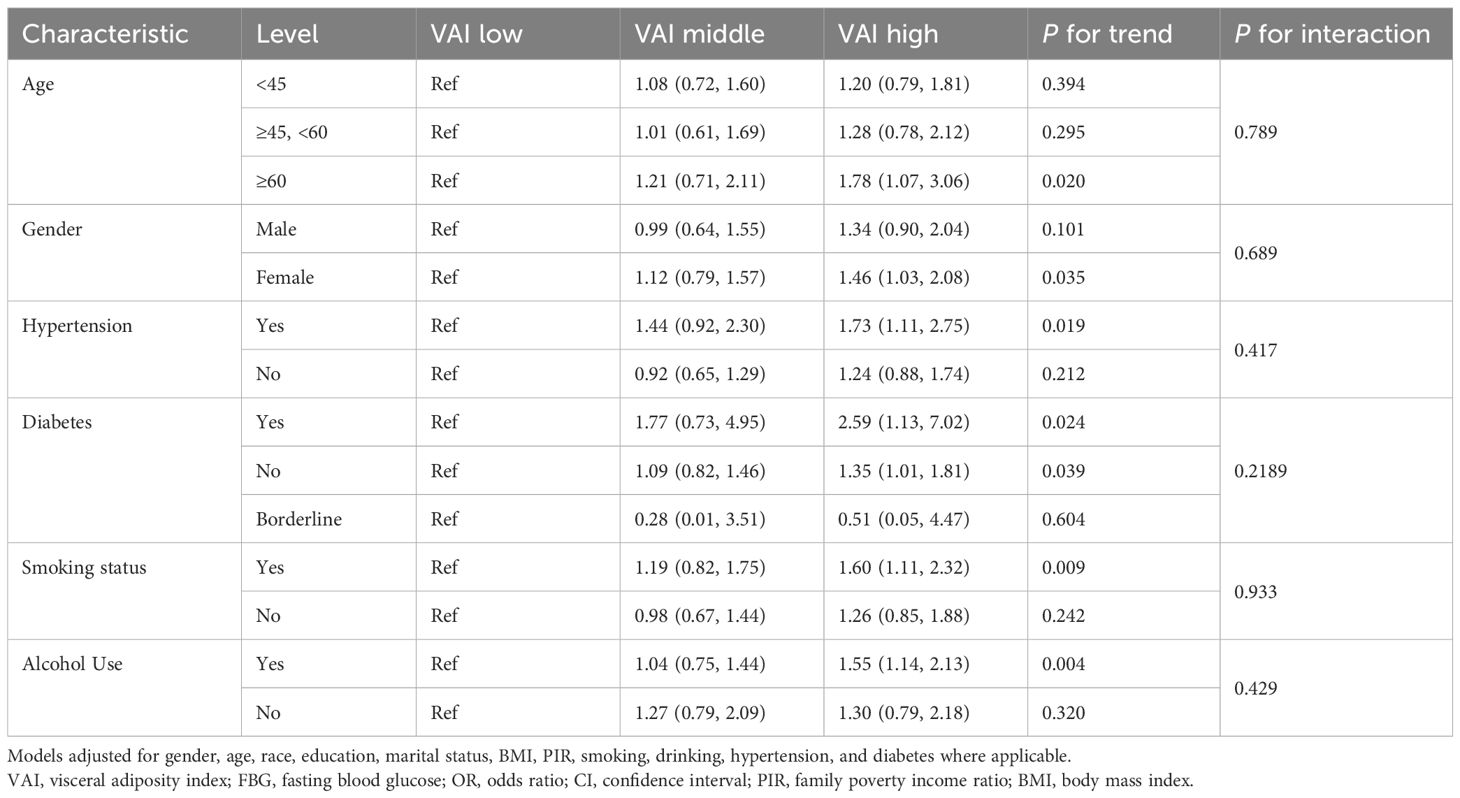
Subgroup analyses revealed notable patterns, despite the absence of statistically significant interactions across stratified analyses (all p for interaction >0.05) (Table 4). The association between VAI and suicidal ideation was more pronounced among older adults (aged ≥60 years), with participants in the highest VAI tertile demonstrating a 78% increased risk (OR=1.78, 95% CI: 1.07–3.06, p for trend = 0.020). Among females, those in the highest VAI tertile demonstrated a 46% higher risk (OR=1.46, 95% CI: 1.03–2.08, p for trend=0.035). Furthermore, individuals diagnosed with hypertension who were in the highest VAI tertile exhibited a 73% increased risk (OR=1.73, 95% CI: 1.11–2.75, p for trend=0.019). Individuals diagnosed with diabetes demonstrated the strongest association, exhibiting a 2.59-fold increased risk (OR=2.59, 95% CI: 1.13–7.02, p for trend=0.024). The influence of lifestyle factors on the observed associations was also significant, with notable trends observed among current smokers (OR=1.60, 95% CI: 1.11–2.32, p for trend = 0.009) and alcohol consumers (OR=1.55, 95% CI: 1.14–2.13, p for trend = 0.004).
3.5 Sensitivity analysis
A sensitivity analysis was conducted, with the exclusion of pregnant women resulting in a final sample of 11,713 participants (Supplementary Tables 1–3; Supplementary Figure 2). Subsequently, a series of analytical procedures were executed on this subset. These procedures included multivariate regression analysis, curve fitting, and threshold saturation effect analysis. Furthermore, gender-stratified subgroup analyses were carried out. The findings from these analyses were consistent, indicating the robustness and stability of the results.
3.6 Mediation analysis
Mediation analysis further revealed that fasting blood glucose (FBG) significantly mediated the relationship between VAI and suicidal ideation (Table 5). The total effect of VAI on suicidal ideation was found to be significant (β=0.001305, 95% CI: 0.000139–0.002752, P=0.032), with FBG accounting for 31.74% (95% CI: 4.43%–181.74%, P=0.042) of the total effect. The average mediation effect of FBG was 0.000414 (95% CI: 0.000110–0.000748, P=0.010), while the direct effect of VAI on suicidal ideation became non-significant after accounting for FBG (β=0.000891, 95% CI: -0.000331–0.002279, P=0.156).
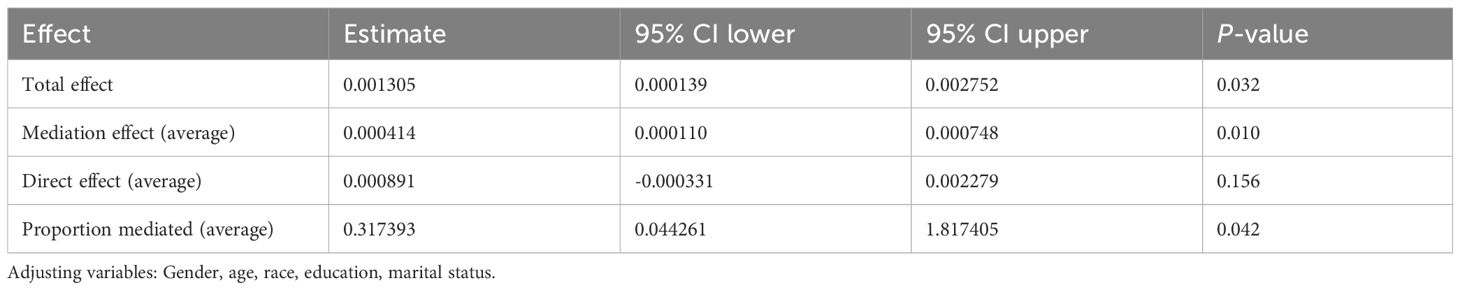
Table 5. Causal mediation analysis of visceral adiposity index on suicidal ideation via fasting blood glucose.
4 Discussion
This cross-sectional study examined the relationship between VAI and suicidal ideation using a nationally representative sample of 11,931 NHANES participants. The findings revealed a significant non-linear association with a threshold effect at VAI=6.81, below which each unit increase in VAI was associated with 9.4% higher odds of suicidal ideation (OR=1.094, 95% CI: 1.028–1.163, P=0.005). This relationship was particularly pronounced among older adults (≥60 years), females, and individuals with comorbidities such as hypertension or diabetes.
Our findings align with and extend previous research on visceral adiposity and mental health outcomes. Kim et al. (24) demonstrated in a Korean population (n=7,238) that higher VAI levels were significantly associated with depressive symptoms, with each 1 cm² increase in visceral fat associated with a 1.006-fold increase in depression risk, particularly among women. However, our study advances this field by: (1) examining the more severe outcome of suicidal ideation rather than depressive symptoms alone; (2) utilizing a larger, more diverse U.S. population; and (3) identifying a critical threshold effect that reveals the non-linear nature of this relationship. Supporting evidence indicates that elevated triglyceride levels significantly increase depression and suicidal tendencies risk, while low HDL-C levels correlate with higher suicide attempt likelihood (25–27), consistent with our VAI-based findings.
The observed association likely operates through multiple interconnected pathways. Visceral adipose tissue secretes pro-inflammatory cytokines (TNF-α, IL-6) while reducing adiponectin, potentially triggering neuroinflammation and disrupting serotonergic systems critical for mood regulation (28, 29). Additionally, VAT-associated insulin resistance may affect emotional regulation through neuroinflammation and HPA axis dysregulation (30).
The pronounced gender differences observed align with prior research showing VAT’s stronger association with depressive symptoms in middle-aged women (31, 32). This may reflect hormonal influences unique to women, including menopause-related changes that affect emotional regulation (33, 34). Neuroimaging studies demonstrate that women with high VAI exhibit reduced gray matter density in the ventral anterior cingulate cortex, potentially impairing emotional and cognitive regulation (16).
VAI offers significant advantages over conventional visceral fat measurement methods (CT/MRI) as a cost-effective, clinically practical mathematical model based on readily available anthropometric and biochemical parameters (35). Unlike traditional obesity metrics (BMI, waist circumference), VAI specifically reflects metabolic dysfunction and adipose tissue endocrine function (28). The identification of VAI=6.81 as a threshold value holds significant clinical relevance, enabling improved risk stratification with distinct management strategies. For individuals with VAI <6.81, the linear relationship (9.4% increased suicidal ideation risk per unit) supports proactive interventions including lifestyle modification, metabolic health optimization, and routine mental health screening integration into metabolic assessments. For individuals with VAI ≥6.81, where the association plateaus, more intensive evaluation is warranted through coordinated metabolic-psychiatric management and integrated care pathways.
Our mediation analysis revealed that FBG accounts for 31.74% of the VAI-suicidal ideation association, indicating substantial but incomplete mediation. While the wide confidence interval (4.43%–181.74%) reflects cross-sectional analysis limitations, the point estimate provides valuable clinical insight into metabolic mechanisms connecting visceral adiposity to mental health outcomes. The remaining 68.26% suggests multiple parallel pathways: inflammatory mechanisms involving cytokine-mediated neuroinflammation; lipid metabolism disruption affecting neuronal membrane composition and neurotransmitter function; HPA axis dysregulation increasing psychiatric vulnerability through altered cortisol secretion; and psychosocial factors including weight stigma and reduced quality of life. Additionally, behavioral clustering of risk factors (smoking, alcohol use, physical inactivity) among high-VAI individuals may contribute through non-glucose-mediated pathways.
It is imperative to acknowledge the limitations of this study. Firstly, as a cross-sectional investigation, it is only possible to establish associations between VAI and suicidal ideation without inferring causality. Furthermore, the absence of longitudinal data precludes examination of temporal relationships between VAI changes and the development of suicidal ideation. Secondly, VAI, while it is practical as an anthropometric surrogate, may introduce measurement bias compared to gold-standard imaging methods (CT/MRI), which could potentially attenuate observed associations. Furthermore, the assessment of suicidal ideation was predominantly based on self-reported questionnaires, as opposed to the utilization of structured clinical interviews, a practice that has the potential to engender recall bias. Thirdly, although the analysis employed representative NHANES data, it should be noted that the findings may not be generalizable to populations with different racial compositions, dietary patterns, or lifestyle factors. Despite adjustments being made for a number of confounding variables, unmeasured variables such as genetic predisposition, family psychiatric history, and psychological stress sources remain unaccounted for. Fourthly, the present mediation analysis demonstrates inherent limitations due to its cross-sectional design, with wide confidence intervals (4.43%–181.74%) reflecting statistical uncertainty when temporal precedence cannot be established. The relatively low prevalence of suicidal ideation (8.4%) and the absence of multiple comparison corrections in exploratory subgroup analyses may contribute to instability in the estimation process and to inflation of Type I error. In conclusion, it is evident that the development of prospective longitudinal designs incorporating validated imaging-based adiposity measures, in conjunction with appropriate statistical corrections, is imperative to address the identified methodological limitations.
5 Conclusion
This cross-sectional study identified a non-linear association between VAI and suicidal ideation, with a threshold at 6.81, which was partially mediated by fasting blood glucose (31.74%). The association was found to be more pronounced among older adults and individuals diagnosed with diabetes or hypertension.
In view of the limitations inherent in cross-sectional designs, these findings indicate associations rather than causality and should be regarded as preliminary evidence requiring prospective validation. Nevertheless, the results of the study highlight the potential value of considering metabolic parameters in mental health assessment. It is evident that further longitudinal studies employing imaging-based adiposity measures are required in order to elucidate the underlying causal mechanisms and to ascertain whether metabolic interventions have the potential to complement psychological approaches in the context of suicide prevention.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
All participants provided written informed consent, and the study protocol was approved by the National Center for Health Statistics Research Ethics Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
LZ: Writing – original draft, Writing – review & editing, Formal Analysis. WZ: Writing – original draft, Methodology. LH: Funding acquisition, Conceptualization, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. LZ reports funding from the Project of Suzhou Science and Technology (No. SKY2022079), the Kunshan Science and Technology Development Fund (No. KS2311), Medical Health Science and Technology Project of Kunshan First People’s Hospital (KSKFQYLWS2023022) and Key Laboratory of Clinical Laboratory Medicine of Jiangsu Province (JSKLM-Y-2024-016). LHH was financed by the Medical Scientific Research Project of Jiangsu Provincial Health Commission in 2021 (M2021072), Suzhou Applied Basic Research (medical and health) of Science and Technology Innovation Project (SYWD2024021), the Clinical Medicine Science and Technology Development Fund of Jiangsu University (JLY2021063), Kunshan High-level Medical Talents Project (Ksgccrc2004), and Medical Health Science and Technology Project of Kunshan First People’s Hospital (CXTD24-B03, KSKFQYLWS2023005, KRY-YN007).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2025.1598411/full#supplementary-material
References
1. Gebremeskel TG, Berhe M, Tesfahunegn TB, Gesesew HA, and Ward PR. Prevalence and factors associated with suicidal ideation among adult Eritrean refugees in northern Ethiopia. Front Public Health. (2022) 10:841848. doi: 10.3389/fpubh.2022.841848
2. Pearce M, Garcia L, Abbas A, Strain T, Schuch FB, Golubic R, et al. Association between physical activity and risk of depression: A systematic review and meta-analysis. JAMA Psychiatry. (2022) 79:550–9. doi: 10.1001/jamapsychiatry.2022.0609
3. Zhou S, Jin L, Liu X, Ding X, and Zhu X. Developmental trajectory of depressive symptoms in Chinese college students: latent classes and gender effect. Int J Environ Res Public Health. (2022) 19(6):3508. doi: 10.3390/ijerph19063508
4. Zheng X, Zhang Y, Chen Y, and Fang X. Internal migration experience and depressive symptoms among middle-aged and older adults: evidence from China. Int J Environ Res Public Health. (2021) 19(1):303. doi: 10.3390/ijerph19010303
5. Ramos-Martín J, Gómez Sánchez-Lafuente C, Martínez-García AI, Castillo-Jiménez P, Guzmán-Parra J, and Moreno-Küstner B. Suicidal behavior in persons attended in out-of-hospital emergency services in Spain. Front Psychiatry. (2023) 14:1235583. doi: 10.3389/fpsyt.2023.1235583
6. Liu H, Dong H, Zhou Y, Jin M, Hao H, Yuan Y, et al. The association between Metabolic Score for Visceral Fat and depression in overweight or obese individuals: evidence from NHANES. Front Endocrinol (Lausanne). (2024) 15:1482003. doi: 10.3389/fendo.2024.1482003
7. Alosaimi N, Sherar LB, Griffiths P, and Pearson N. Clustering of diet, physical activity and sedentary behavior and related physical and mental health outcomes: a systematic review. BMC Public Health. (2023) 23:1572. doi: 10.1186/s12889-023-16372-6
8. Al-Kuraishy HM, Al-Gareeb AI, Alsayegh AA, Hakami ZH, Khamjan NA, Saad HM, et al. A potential link between visceral obesity and risk of Alzheimer’s disease. Neurochem Res. (2023) 48:745–66. doi: 10.1007/s11064-022-03817-4
9. Guo S, Qing G, Chen Q, and Yang G. The relationship between weight-adjusted-waist index and suicidal ideation: evidence from NHANES. Eat Weight Disord. (2024) 29:37. doi: 10.1007/s40519-024-01666-4
10. Gerend MA, Sutin AR, Terracciano A, and Maner JK. The role of psychological attribution in responses to weight stigma. Obes Sci Pract. (2020) 6:473–83. doi: 10.1002/osp4.437
11. Liu J, Zhang G, Jia F, Yuan H, Wang Q, Li C, et al. U-shaped association between fasting blood glucose and suicide attempts in Chinese patients with first-episode drug-naïve major depressive disorder. BMC Psychiatry. (2024) 24:382. doi: 10.1186/s12888-024-05818-9
12. Qi S, Xu Y, Zeng K, Li Y, and Ma J. Incidence and factors associated with hyperglycemia in patients with first hospitalization for major depression disorder: A large cross-sectional sample. Neuropsychiatr Dis Treat. (2023) 19:1809–18. doi: 10.2147/NDT.S421984
13. Ejtahed HS, Kelishadi R, Hasani-Ranjbar S, Angoorani P, Motlagh ME, Shafiee G, et al. Discriminatory ability of visceral adiposity index as an indicator for modeling cardio-metabolic risk factors in pediatric population: the CASPIAN-V study. J Cardiovasc Thorac Res. (2019) 11:280–6. doi: 10.15171/jcvtr.2019.46
14. Ding Y, Gu D, Zhang Y, Han W, Liu H, and Qu Q. Significantly increased visceral adiposity index in prehypertension. PLoS One. (2015) 10:e0123414. doi: 10.1371/journal.pone.0123414
15. Zhou H, Li T, Li J, Zheng D, Yang J, and Zhuang X. Association of visceral adiposity index with hypertension (NHANES 2003-2018). Front Cardiovasc Med. (2024) 11:1341229. doi: 10.3389/fcvm.2024.1341229
16. Iceta S, Dadar M, Daoust J, Scovronec A, Leblanc V, Pelletier M, et al. Association between visceral adiposity index, binge eating behavior, and grey matter density in caudal anterior cingulate cortex in severe obesity. Brain Sci. (2021) 11(9):1158. doi: 10.3390/brainsci11091158
17. Ju YJ, Han KT, Lee TH, Kim W, Park JH, and Park EC. Association between weight control failure and suicidal ideation in overweight and obese adults: a cross-sectional study. BMC Public Health. (2016) 16:259. doi: 10.1186/s12889-016-2940-1
18. Ferguson CC, Knol LL, and Ellis AC. Visceral adiposity index and its association with Dietary Approaches to Stop Hypertension (DASH) diet scores among older adults: National Health and Nutrition Examination Surveys 2011-2014. Clin Nutr. (2021) 40:4085–9. doi: 10.1016/j.clnu.2021.02.008
19. Lei J, Luo Y, Xie Y, and Wang X. Visceral adiposity index is a measure of the likelihood of developing depression among adults in the United States. Front Psychol. (2022) 13:772556. doi: 10.3389/fpsyg.2022.772556
20. He Q, Liu S, Feng Z, Li T, Chu J, Hu W, et al. Association between the visceral adiposity index and risks of all-cause and cause-specific mortalities in a large cohort: Findings from the UK biobank. Nutr Metab Cardiovasc Dis. (2022) 32:2204–15. doi: 10.1016/j.numecd.2022.05.020
21. Ajele KW and Idemudia ES. Charting the course of depression care: a meta-analysis of reliability generalization of the patient health questionnaire (PHQ- 9) as the measure. Discov Ment Health. (2025) 5:50. doi: 10.1007/s44192-025-00181-x
22. Perlis RH, Gunning FM, Santillana M, Baum MA, Druckman JN, Ognyanova K, et al. Derivation of a 3-item patient health questionnaire as a shortened survey to capture depressive symptoms. JAMA Netw Open. (2025) 8:e2522036. doi: 10.1001/jamanetworkopen.2025.22036
23. Chen X, Luo H, and Ye M. Depressive symptoms were associated with an elevated prevalence of gallstones among adults in the United States: A cross-sectional analysis of NHANES 2017-2020. Prev Med Rep. (2024) 43:102771. doi: 10.1016/j.pmedr.2024.102771
24. Cho SJ, Lee HJ, Rhee SJ, Kim EY, Kim KN, Yoon DH, et al. The relationship between visceral adiposity and depressive symptoms in the general Korean population. J Affect Disord. (2019) 244:54–9. doi: 10.1016/j.jad.2018.09.046
25. Lee K, Kim S, and Jo JK. The relationships between abnormal serum lipid levels, depression, and suicidal ideation according to sex. J Clin Med. (2022) 11(8):2119. doi: 10.3390/jcm11082119
26. Cho H, Shin J, and Choi JK. Serum lipid levels and suicidal ideation of adults: A cross-sectional study using the Korea national health and nutrition examination survey. J Clin Med. (2023) 12(13):4285. doi: 10.3390/jcm12134285
27. Zhou S, Zhao K, Shi X, Sun H, Du S, Miao X, et al. Serum lipid levels and suicide attempts within 2 weeks in patients with major depressive disorder: is there a relationship? Front Psychiatry. (2021) 12:676040. doi: 10.3389/fpsyt.2021.676040
28. Brown JC, Harhay MO, and Harhay MN. Visceral adipose tissue dysfunction and mortality among a population-based sample of males and females. Diabetes Metab. (2016) 42:382–5. doi: 10.1016/j.diabet.2016.05.001
29. Heeran AB, McCready J, Dunne MR, Donlon NE, Nugent TS, Bhardwaj A, et al. Opposing Immune-Metabolic Signature in Visceral Versus Subcutaneous Adipose Tissue in Patients with Adenocarcinoma of the esophagus and the esophagogastric Junction. Metabolites. (2021) 11(11):768. doi: 10.3390/metabo11110768
30. Kahn D, Macias E, Zarini S, Garfield A, Zemski Berry K, MacLean P, et al. Exploring visceral and subcutaneous adipose tissue secretomes in human obesity: implications for metabolic disease. Endocrinology. (2022) 163(11):bqac1409. doi: 10.1210/endocr/bqac140
31. Murabito JM, Massaro JM, Clifford B, Hoffmann U, and Fox CS. Depressive symptoms are associated with visceral adiposity in a community-based sample of middle-aged women and men. Obes (Silver Spring). (2013) 21:1713–9. doi: 10.1002/oby.20130
32. Everson-Rose SA, Lewis TT, Karavolos K, Dugan SA, Wesley D, and Powell LH. Depressive symptoms and increased visceral fat in middle-aged women. Psychosom Med. (2009) 71:410–6. doi: 10.1097/PSY.0b013e3181a20c9c
33. Freeman EW, Sammel MD, Boorman DW, and Zhang R. Longitudinal pattern of depressive symptoms around natural menopause. JAMA Psychiatry. (2014) 71:36–43. doi: 10.1001/jamapsychiatry.2013.2819
34. Kornstein SG, Young EA, Harvey AT, Wisniewski SR, Barkin JL, Thase ME, et al. The influence of menopause status and postmenopausal use of hormone therapy on presentation of major depression in women. Menopause. (2010) 17:828–39. doi: 10.1097/gme.0b013e3181d770a8
Keywords: visceral adiposity index, suicidal ideation, NHANES, mediation analysis, mentalhealth
Citation: Zhang L, Zhang W and Hang L (2025) Threshold effect of visceral adiposity index on suicidal ideation: a mediation analysis through fasting blood glucose. Front. Psychiatry 16:1598411. doi: 10.3389/fpsyt.2025.1598411
Received: 23 March 2025; Accepted: 23 September 2025;
Published: 07 October 2025.
Reviewed by:
Ivan Antonio Garcia-Montalvo, National Institute of Technology of Mexico, MexicoSakir Ozgur Keskek, Alanya Alaaddin Keykubat University, Türkiye
Ming Gao, Shanxi Medical University, China
Copyright © 2025 Zhang, Zhang and Hang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lihua Hang, MTgwMTMyNzMxNjlAMTYzLmNvbQ==
 Li Zhang
Li Zhang Wenhao Zhang1
Wenhao Zhang1 Lihua Hang
Lihua Hang