- 1Children Psychiatry Unit, Specialized Psychiatric Health Care Centre in Lodz, Lodz, Poland
- 2Department of Environmental Psychiatry, Faculty of Life Sciences, Medical University of Warsaw, Warsaw, Poland
- 3Department of Public Health, Medical University of Warsaw, Warsaw, Poland
- 4Department of Population Health, Centre of Postgraduate Medical Education, Warsaw, Poland
Introduction: Currently, there are no nationwide cross-sectional studies on public awareness of mental disorders in Poland. This study aimed to identify factors associated with the awareness of mental disorders and their risk factors through a nationwide cross-sectional survey of adults in Poland.
Methods: This cross-sectional study was conducted between March 8 and 10, 2025, using the computer-assisted web interview (CAWI) technique. The questionnaire included questions on self-reported awareness of mental health, awareness of 9 mental disorders, and 12 mental disorder risk factors.
Results: The study population comprised 1114 adults aged 18–96 years, with 54.7% being female. The majority of respondents (47.2%) reported a moderate level of awareness of mental disorders. Depression (82.6%) was the most recognized mental disorder among adults in Poland. Traumatic experiences in the past (76.8%) were the most commonly recognized risk factor for mental disorders, followed by genetic predisposition (64.5%) and difficulties in family relationships (64.5%). Factors significantly associated with a rather good/very good level of awareness of mental disorders included being under 60 years of age (p<0.05), living in cities with more than 20,000 residents (p<0.05), having higher education (aOR=1.77 [1.23-2.55]; p=0.002), and having a family history of mental disorders (aOR=2.69 [1.86-3.89]; p<0.001).
Conclusions: The level of awareness of mental disorders among adults in Poland is low, and significant differences in awareness were observed based on sociodemographic variables. Understanding these disparities is crucial for tailoring effective public health campaigns and informing national mental health strategies aimed at early detection, destigmatization, and equitable access to care.
1 Introduction
According to the World Health Organization (WHO), health is the complete physical, mental and social well-being of a person, and not just the absence of disease or disability (1). Mental health is at the forefront in the global and European context as one of the pillars of public health, economic stability and social well-being. At the same time, it remains a fact that mental health problems constitute a significant burden for individuals, their relatives, the health care system and the entire society (2). In Poland, the results of a comprehensive epidemiological study on the mental health of society and its determinants conducted before the COVID-19 pandemic (EZOP II) showed that 26.46% of Polish men and women struggled with a mental disorder at least once in their life, of which 16.07% with neurotic disorders and 4.65% with mood disorders (3). According to the Global Burden of Disease Study (GBD), Poland loses 1,259 healthy life years per year due to mental illness (per 100,000 inhabitants), with the two most common conditions being anxiety disorders and depression, responsible for 3,082.5 and 1,192.1 cases per 100,000 inhabitants, respectively (4). The WHO European Health Equity Status Report 2019 showed that there is a significant relationship between socio-economic factors and mental health disorders as well as mental health inequalities (2). Similarly, poor mental health adversely affects productivity, the ability to achieve one’s life goals, and the economic situation.
A recent WHO report revealed that around 1 in 8 people worldwide are living with a mental disorder, with anxiety and depressive disorders being the most prevalent (5). Depression is expected to be a major contributor to the global burden of disease by 2030. Depression currently causes more disability in young people aged 10 to 24 than any other disease (5). Around 7.3% of the global burden of disease is attributed to mental and behavioral disorders. Most of this burden is attributed to unipolar depressive disorders, as well as anxiety, psychotic and substance use disorders (4, 6). Currently, around 450 million people suffer from mental disorders, and it is predicted that one in four people worldwide will be affected by a mental disorder at some point in their life (6). Mental disorders are one of the leading causes of ill health and disability worldwide (7). People with mental disorders experience disproportionately higher rates of disability and mortality (8). People with major depressive disorder and schizophrenia had a 40 to 60% higher risk of premature death than the general population (9). Between 1990 and 2019, the global number of disability-adjusted life years (DALYs) attributable to mental disorders increased from 80.8 million to 125.3 million (10). The share of global DALYs attributable to mental disorders increased from 3.1% to 4.9%. Mental disorders remain a leading cause of global health burden. Rates of burden measured in disability-adjusted life years (DALYs) were evident across all age groups. They occurred before the age of five in people with intellectual disabilities and autism spectrum disorders, and in older age in people with depression, anxiety disorders, and schizophrenia. Moreover, after considering the impact of the COVID-19 pandemic on population health (among the 25 leading causes), since 2010, age-standardized DALY rates have increased the most for anxiety disorders – by 16.7%; depressive disorders – by 16.4%; and diabetes – by 14.0% (11).
Mental health literacy, defined as “knowledge and attitudes about mental disorders that help in their recognition, treatment and prevention” is low worldwide, but particularly low in developing countries (12). Mental disorders are complex health problems that are influenced by biological, psychological and environmental factors. Understanding the risks associated with these disorders can help in their prevention and early recognition of symptoms. Researchers emphasize that lack of sufficient knowledge about mental disorders increases the risk of negative effects of developing conditions, delays effective help-seeking and treatment, and increases the risk of stigmatization (13). Currently, there are no nationwide cross-sectional studies among adults in Poland assessing awareness of mental disorders and risk factors. Raising awareness of risk factors associated with mental disorders is crucial for preventing their development and improving the quality of life of people struggling with mental problems. The National Mental Health Program for 2023–2030 is being implemented in Poland and is a strategic framework for actions aimed at improving the mental health of society (14). One of the key elements of the program is prevention, i.e. preventing the occurrence of mental disorders and promoting mental health. The implementation of the National Mental Health Program aims not only to reduce the number of new cases of mental disorders, but also to improve the quality of life of people struggling with these problems and their integration into society.
Nationwide cross-sectional surveys on public awareness of mental disorders and risk factors for mental disorders may inform healthcare professionals and policymakers on the level of knowledge on mental disorders and point out further educational needs.
Therefore, this study aimed to identify factors associated with the awareness of mental disorders and their risk factors in a nationwide cross-sectional survey among adults in Poland.
2 Material and methods
2.1 Study design and population
This study was carried out following a cross-sectional model, with data collected between 8 and 10 March 2025 using the Computer-Assisted Web Interview (CAWI) technique. To ensure a nationwide representation of adults in Poland, the study contracted a public opinion survey company [Arianda Poland’s Research Panel (15)] to collect data. The online questionnaire was hosted on a research platform managed by the company, and invitations to participate were sent via e-mail and text message to verified respondents from a pool of over 100,000 individuals. Each respondent received an invitation to participate in the survey via e-mail and text message.
While the sampling strategy was stratified by gender, age, and size of residence, ensuring demographic diversity, it is important to note that the use of CAWI may limit participation from groups without internet access, including older adults, rural populations, and those with limited digital literacy. The sampling method enabled the selection of a nationally representative group, based on demographic data from Statistics Poland (GUS), the central institution responsible for official statistical reporting (16). However, given that over 93% of households in Poland have internet access (17) and the sampling design accounted for key demographic variables such as age, the risk of systematic underrepresentation of digitally excluded individuals—particularly older adults—is minimal. The study was thus designed to be as inclusive as possible within the CAWI framework.
Participation in this survey was voluntary and anonymous. The study procedures followed the ethical and scientific standards expressed in the Helsinki Declaration. Ethical approval of the Ethics Committee of the Medical University of Warsaw was obtained (decision AKBE/38/2025 as of 24 Feb 2025).
2.2 Measures
The study questionnaire was prepared based on a literature review (1–5). A series of questions on public awareness of mental disorders and their risk factors were addressed. Respondents were asked to select all mental disorders and risk factors they were aware of. However, to minimize confusion, participants were provided with clear instructions to select all that applied to their knowledge, rather than only the most relevant items. Similar methodology was presented in other studies (17–21).
Self-reported level of knowledge of mental disorders was assessed based on a 5-point Likert scale. Respondents were asked about awareness of 9 different groups of mental disorders using the following question: “Have you ever heard of mental disorders listed below? (please indicate all you have heard of)”, with a response of yes/no to each mental disorder listed. A list of the 12 most common risk factors for mental disorders was prepared and the following question was addressed to the respondents: “What do you think are the risk factors for mental disorders? (please indicate all that apply)”, with a response yes/no to each risk factor listed.
Moreover, a set of questions on sociodemographic characteristics was addressed, including gender, age, place of residence, educational level, professional status (active – employed or self-employed; passive – unemployed, retired, student), relationship status, having children, living conditions, self-declared household financial status (based on self-declared assessment, as the question on monthly income resulted in the high number of missed answers). Question on the history of mental disorders in the family was also addressed: “Does any member of your immediate family (parent, sibling, child, partner) have or has had a diagnosis of a mental disorder?” (yes/no).
2.3 Statistical analysis
Data were analyzed with IBM SPSS version 29 (Armonk, NY, USA). The distribution of categorical variables was presented with frequencies and proportions. Cross-tables with chi-squared tests were used to compare categorical variables. A logistic regression model was used to identify factors associated with self-reported level of knowledge on mental disorders. In bivariable logistic regression, each sociodemographic variable was considered separately. In the multivariable logistic model, each variable statistically significant in the bivariable analysis was used in the multivariable model. The strength of associations was presented with odds ratio (OR) and 95% confidence intervals (95%CI). The statistical significance level was set at p<0.05.
3 Results
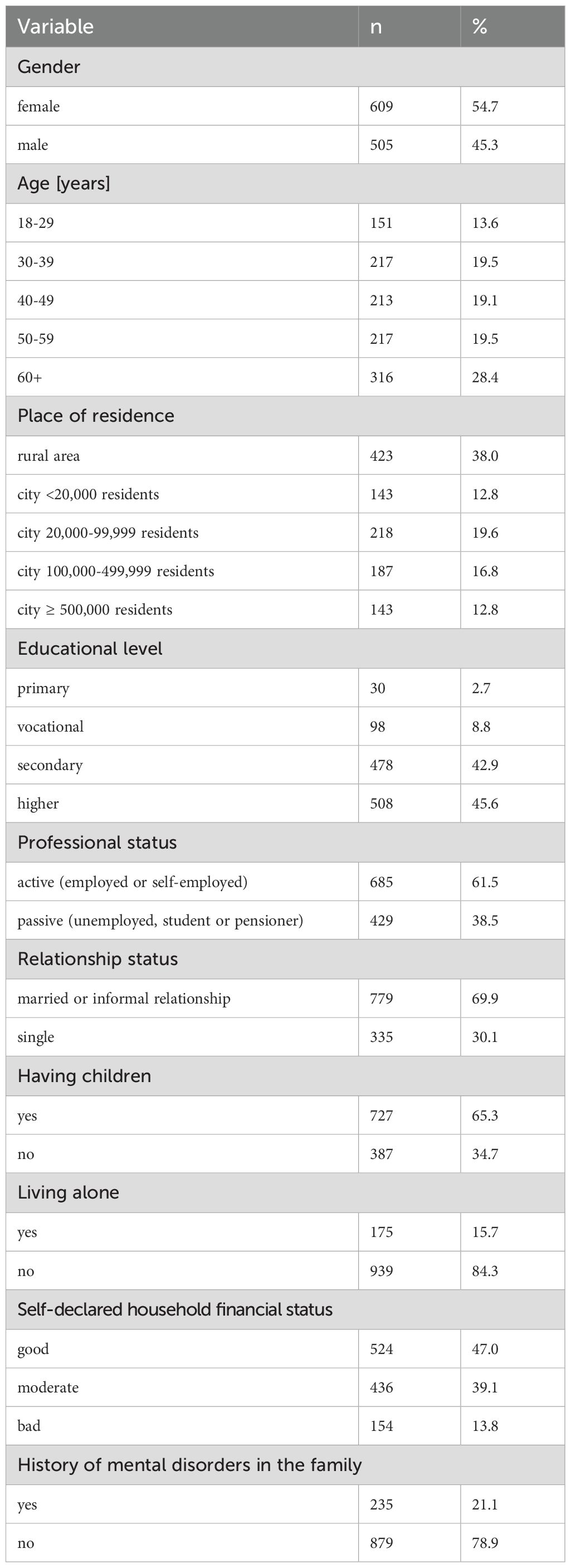
The study population included 1114 adults aged 18–96 years, 54.7% were females. Details are presented in Table 1.
3.1 Public awareness of mental disorders and their risk factors among adults in Poland
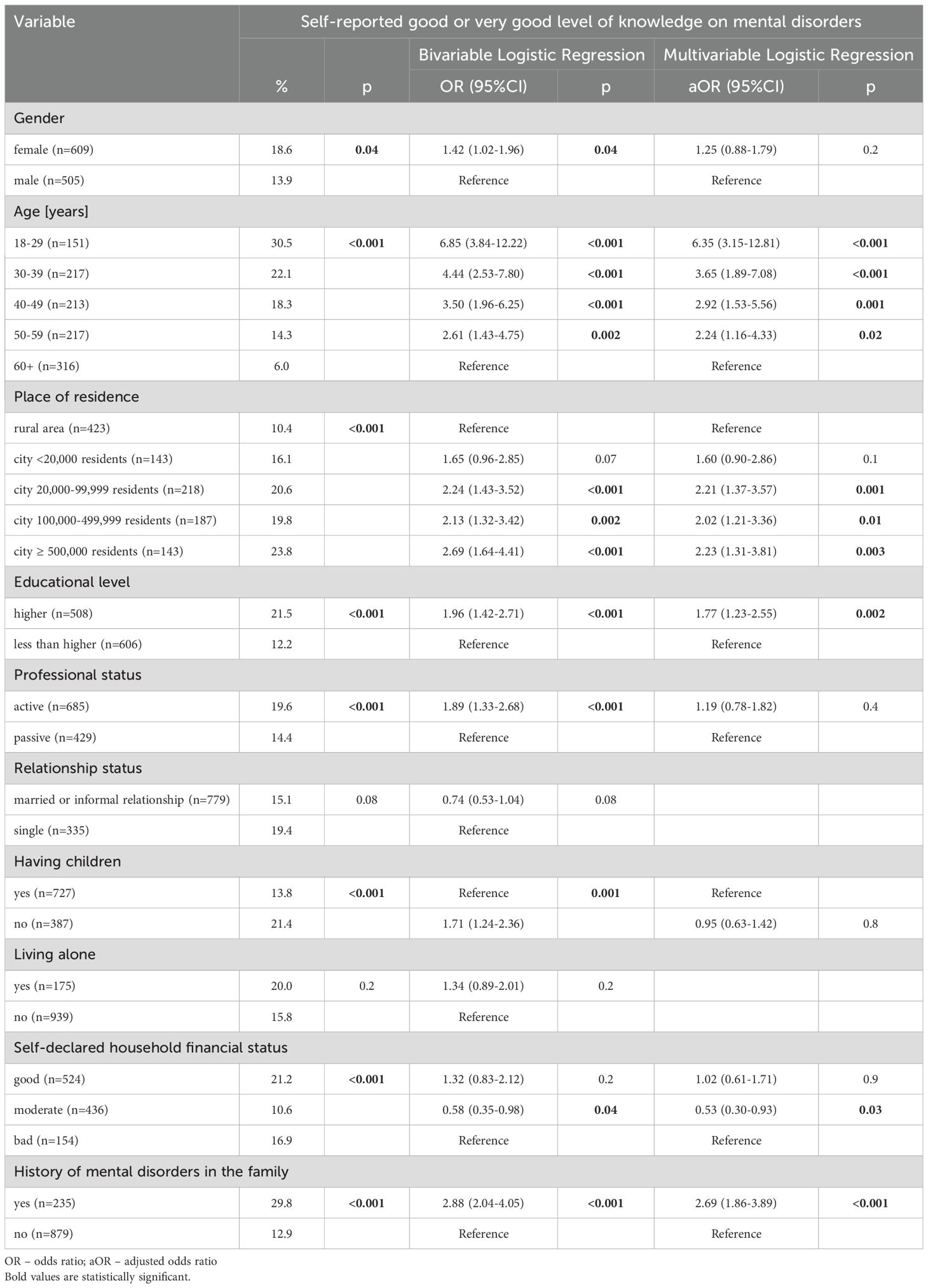
Most of the respondents (47.2%) declared a moderate level of knowledge of mental disorders (Table 2). In this study, a “moderate” level of knowledge was defined as a self-reported score of 3 on a 5-point Likert scale, where 1 indicated “very poor” and 5 “very good” knowledge. This level reflects general familiarity with mental disorders without in-depth understanding or recognition of a wide range of conditions. Only 2.7% of respondents declared a very good level of knowledge and 13.7% declared a rather good level of knowledge of mental disorders. Out of 9 different mental disorders analyzed in this study, depression (82.6%) was the most recognized mental disorder among adults in Poland. Moreover, over half of respondents declared awareness of addictions (74.7%), anxiety disorders (62.8%), neurodevelopmental disorders (61%), suicidal behavior (57.1%), obsessive-compulsive disorder (53.7%) and bipolar disorder (52.1%). Out of 12 different mental disorder risk factors, traumatic experiences in the past (76.8%) were the most recognized risk factors for mental disorders (Table 2). Moreover, over half of respondents declared that genetic predisposition (64.5%) or difficulties in family relationships (64.5%) are risk factors for mental disorders. Environmental pollution was the least (12.1%) recognized risk factor for mental disorders (Table 2).
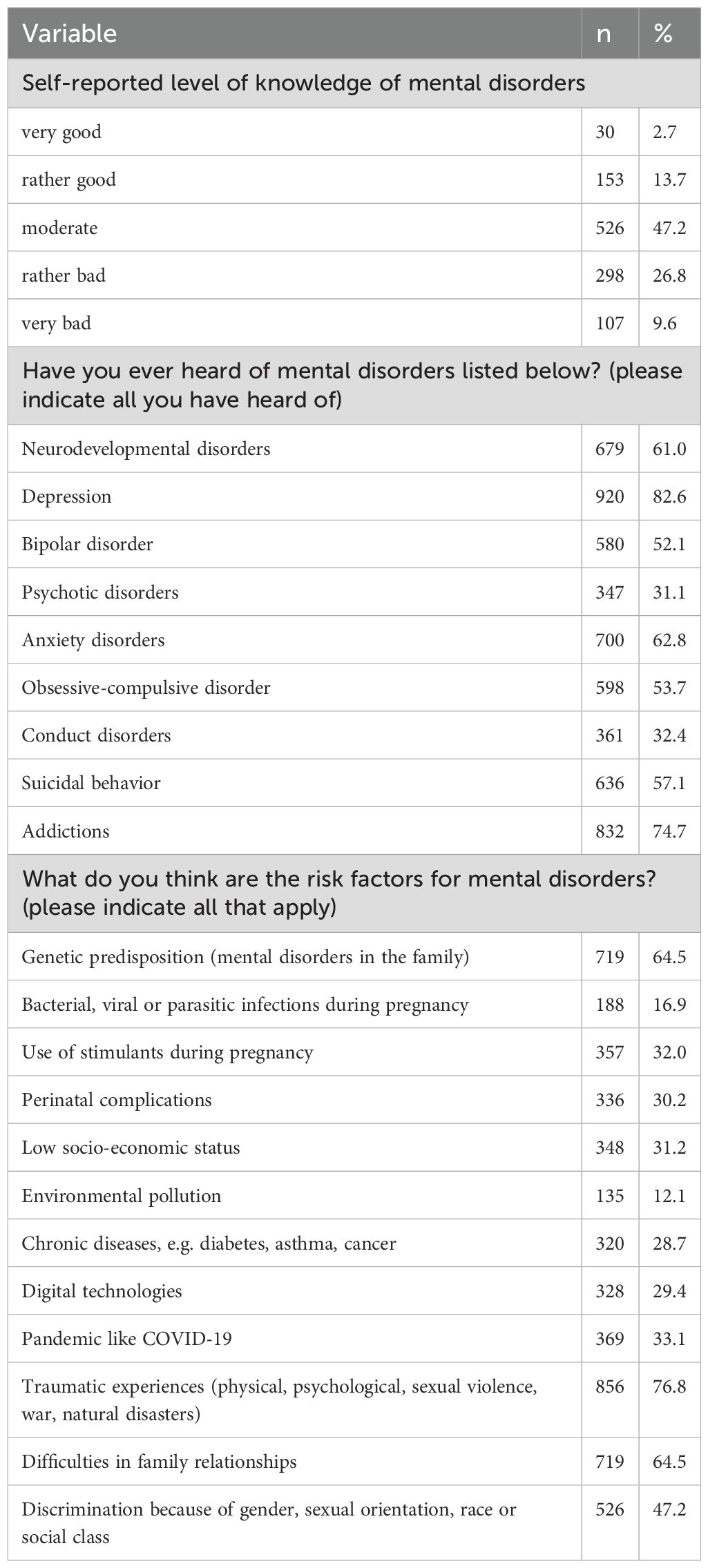
Table 2. Public awareness of mental disorders and their risk factors among adults in Poland (n=1114).
3.2 Sociodemographic differences in public awareness of mental disorders and their risk factors among adults in Poland
There were statistically significant differences (p<0.05) in public awareness of mental disorders, mostly by gender, age, place of residence, educational level, self-reported financial household status, and the history of mental disorders in the family (Tables 3, 4). Moreover, there were statistically significant differences (p<0.05) in public awareness of mental disorder risk factors: Women were more likely than men to recognize several key risk factors, including genetic predisposition (p<0.001), low socioeconomic status (p=0.006), traumatic experiences (p<0.001), difficulties in family relationships (p=0.003), and discrimination (p=0.005). Younger adults, particularly those under 40, more frequently identified digital technologies (p<0.001), the COVID-19 pandemic (p=0.002), and social discrimination (p=0.02). Respondents from larger cities showed higher recognition of genetic predisposition (p=0.002), use of stimulants during pregnancy (p=0.02), and traumatic experiences (p=0.05) compared to those from rural areas. Higher educational attainment was consistently associated with greater awareness of nearly all assessed risk factors, including genetic predisposition (p<0.001), environmental pollution (p=0.01), traumatic experiences (p<0.001), and discrimination (p=0.01). Those reporting good household financial status and individuals with a family history of mental disorders also demonstrated significantly higher awareness across multiple domains (p<0.05 for all listed factors) (Tables 5, 6).
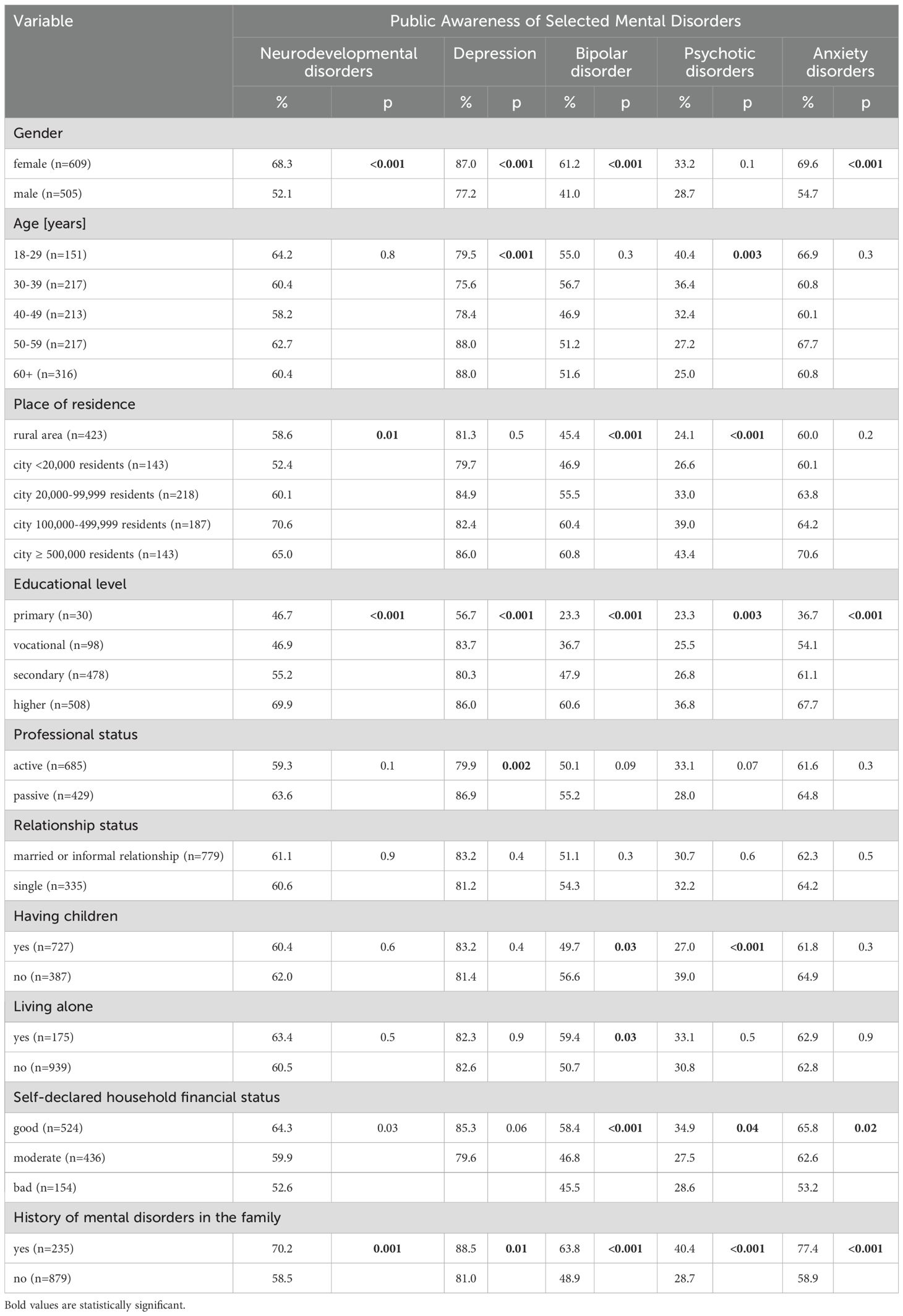
Table 3. Public awareness of selected mental disorders by sociodemographic factors (n=1114) – part 1.
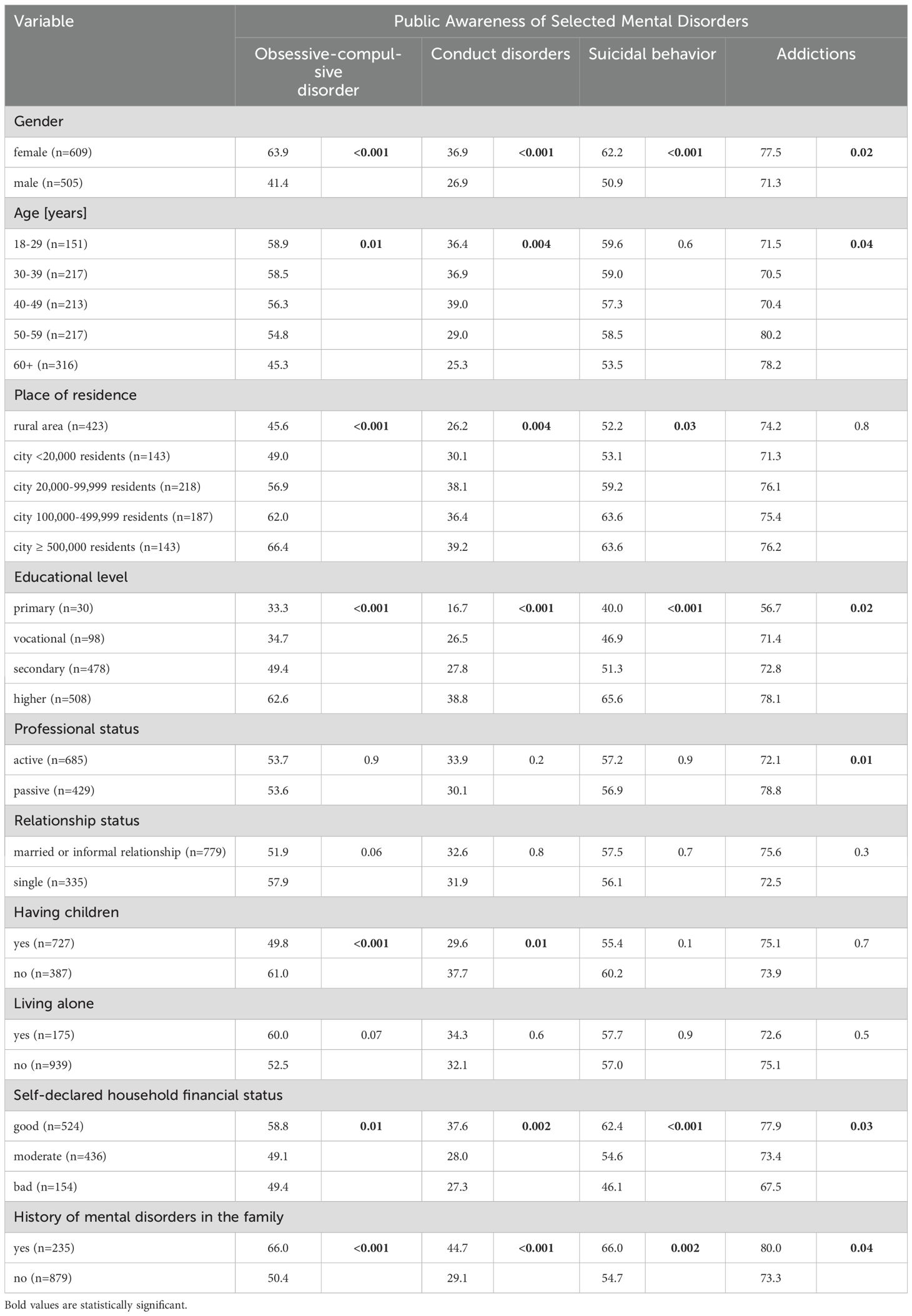
Table 4. Public awareness of selected mental disorders by sociodemographic factors (n=1114) – part 2.
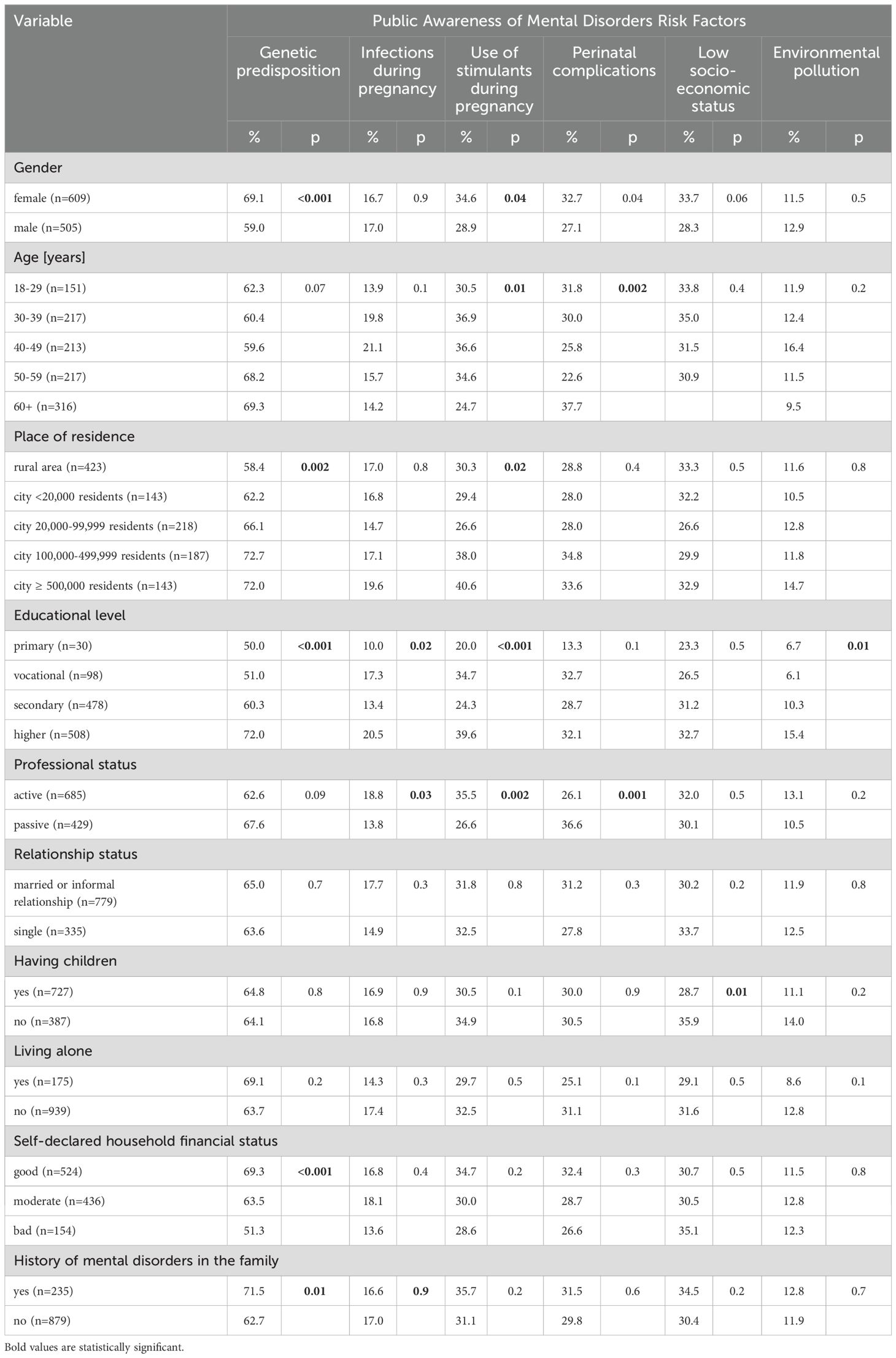
Table 5. Sociodemographic differences in public awareness of mental disorders risk factor (n=1114) – part 1.
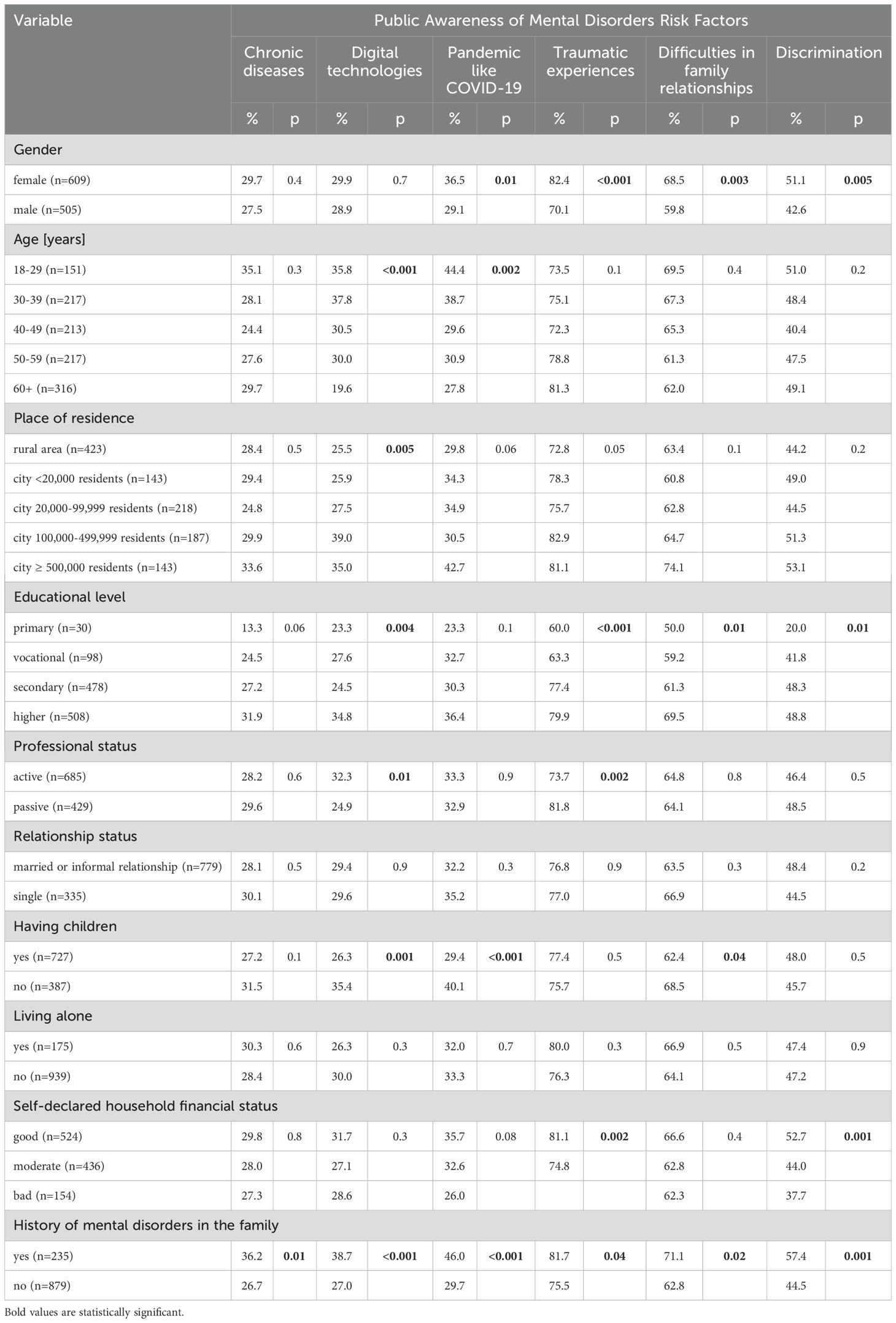
Table 6. Sociodemographic differences in public awareness of mental disorders risk factor (n=1114) – part 2.
3.3 Factors associated with the level of knowledge of mental disorders
A clear urban–rural gradient was observed, with respondents living in rural areas being least likely to report good knowledge of mental disorders, potentially due to reduced access to mental health information and services. In multivariable logistic regression (Table 7), age <60 years (p<0.05), living in cities over 20,000 residents (p<0.05), having higher education (aOR=1.77 [1.23-2.55]; p=0.002) and history of mental disorders in the family (aOR=2.69 [1.86-3.89]; p<0.001) were significantly associated with rather good/very good level of knowledge on mental disorders. Lower awareness among individuals with moderate household economic status may reflect limited health literacy, fewer contacts with mental health professionals, and lower exposure to public health campaigns, particularly outside urban centers. Respondents with moderate economic status were less likely to declare very good/rather good level of knowledge on mental disorders (aOR=0.53 [0.30-0.93]; p=0.03). There was no significant (p>0.05) impact of gender, professional status, relationship status, having children, and living conditions on self-reported level of knowledge on mental disorders. (Table 7).
4 Discussion
This is the first nationwide cross-sectional survey on public awareness of mental disorders and their risk factors among adults in Poland. Findings from this study revealed significant gaps in public knowledge on mental disorders. Depression was the most recognized mental disorder. Traumatic experiences like physical, psychological, sexual violence, war, or natural disasters were the most recognized risk factors for mental disorders, with low recognition of lifestyle-related mental disorders risk factors. Out of 10 different sociodemographic variables included in multivariable regression analysis, age, place of residence, educational level and family history of mental disorders were the only factors associated with higher levels of knowledge on mental disorders.
Building public awareness of mental disorders is an important element of national mental health strategies and translates into the possibility of early referral to psychiatric facilities for people suspected of having a mental disorder (22). People who are aware of mental disorders may be more likely to seek professional help at the early stage of a mental crisis. Moreover, people with a high level of awareness of mental disorders may be more likely to their relatives, friends, or co-workers who are affected by mental disorders or mental crises.
In this study, only 16.4% of respondents declared a very good or rather good level of knowledge on mental disorders. This observation may result from the fact that the National Mental Health Program in Poland, is mostly focused on the organization of mental health services, with a limited number of nationwide educational programs (14). Depression was the most recognized mental disorder which may result from the fact, that significant part of the educational campaigns on mental disorders, carried out by public organizations or NGOs in Poland was focused on depression (23). Moreover, talks on depression and its symptoms are often presented in mass media.
Awareness of risk factors of mental disorders is necessary to modify lifestyle behaviors and decrease the risk of mental disorders. Moreover, people who are at higher risk of mental disorders due to non-modifiable risk factors (like genetic predisposition or experiences in the past) may be more likely to seek help at an early stage of mental health deterioration, as they are more aware of their potential mental disorder risks. Lack of awareness of mental disorders among adults in Poland may also lead to misunderstanding and false social perception of people with mental disorders. For example, people with chronic diseases like diabetes are at higher risk of depression, but due to low awareness of the risk factors for mental disorders, relatives and friends of patients with chronic diseases may not be aware that chronic diseases may evoke changes in behaviors and mental disorders like diabetes (24). Environmental pollution was the least recognized risk factor for mental disorders. Numerous studies have shown that environmental pollutants have an impact on human mental health through different biological pathways (25). In numerous cities in Poland, air pollution levels exceed WHO air quality standards (26). Lack of awareness of the link between environmental factors and mental health requires implementation of urgent educational activities.
Urban areas contribute to higher awareness of mental disorders through multiple mechanisms that differ significantly from those available in rural settings. One major factor is the greater accessibility of mental health services in cities, owing to the higher concentration of healthcare facilities and trained professionals (27). Additionally, urban environments often host more educational programs and public awareness campaigns, frequently supported by NGOs and public health initiatives (28). Urban design also plays a role; interventions aimed at creating restorative environments can enhance mental health literacy and offer psychosocial support (29). Moreover, tele-psychiatry is more accessible in urban areas, facilitating timely diagnosis and treatment, in contrast to its limited availability in rural regions (30). Finally, urban populations typically exhibit higher levels of education and income, both of which are positively correlated with improved knowledge of and attitudes toward mental health issues (31).
Out of 10 different sociodemographic factors, only 4 were significantly associated with a higher level of knowledge of mental disorders. Individuals <60 years of age were more likely to declare a higher level of knowledge of mental disorders. This observation may result from the fact that younger generations are more likely to focus on mental health and well-being. This observation may result from the fact that younger generations are more likely to focus on mental health and well-being (32). Moreover, younger adults may be more likely to hear about mental health on social media or in the workplace (33, 34). Living in cities with > 20 thousand residents was also associated with a higher level of knowledge of mental disorders. This observation suggests that current educational campaigns on mental disorders do not sufficiently reach the inhabitants of villages and small towns. This observation may also impact the social perception of people with mental disorders who live in small local communities (35). Moreover, those who live in rural areas or small towns may be less likely to seek professional health during a mental health crisis. Local governments should urgently address this gap through educational and information campaigns targeted at local communities. Educational levels often affect health disparities (36). In general, those with higher education often present higher health literacy skills (37). Findings from this study also confirmed that higher education was associated with a higher level of knowledge of mental disorders. In this study also the family history of mental disorders was associated with a higher level of knowledge of mental disorders. The presence of disease in the family and personal history related to relatives with mental disorders may impact individual attitudes toward mental disorders.
There is a lack of other studies on public awareness of mental disorders in Poland, so direct comparisons are difficult. Uddin et al. showed that awareness of mental health conditions in a rural district in Bangladesh appeared to be very limited and the lowest knowledge on mental disorders was among females, older adults, people with low socioeconomic status and primary levels of education (38). More nationwide studies on public awareness of mental disorders are needed.
The study has several practical implications. First, nationwide data on public awareness of mental disorders and their risk factors may be used by healthcare professionals and policy makers to implement educational campaigns and may be included in the national mental health strategy. Second, sociodemographic differences in public awareness of mental disorders and their risk factors point out groups with the lowest level of knowledge on mental disorders, that should be targeted during the educational activities. Third, this study showed that there is an urgent need to educate adults in Poland on lifestyle-related risk factors for mental disorders, that may result in increase of adults who implement mental disorders prevention measures.
This cross-sectional survey has several limitations. Data were self-declared so recall bias may occur. The level of knowledge on mental disorders was based on one simple question with 5-point Likert scale and was not verified in more advanced tests or scales. This study was limited to 9 different mental disorders and 12 most common risk factors, so only selected mental disorders were assessed in this study. Data on mental disorders in the family were self-declared and was not crossed with medical documentation. CAWI method was used so only respondents with Internet access could participate in this study. The psychometric properties of the self-reported questionnaire used in this study, including its reliability and validity, have not been formally assessed, however, the pilot restudy was conducted on eight adults who completed the questionnaire twice, with a one-week interval. Based on the results of this pilot, one question and three response options were modified to improve the consistency and clarity of the questionnaire.
5 Conclusions
The level of knowledge on mental disorders among adults in Poland is low. Significant gaps in awareness of most common mental disorders and their risk factors (especially lifestyle-related risk factors) were found. Educational campaigns on mental disorders should be particularly targeted at older adults, citizens of rural areas of small cities, and those without higher education.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee at the Medical University of Warsaw, Poland (approval number: AKBE/38/2025 as of 24 Feb 2025). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AL: Writing – review & editing, Resources, Formal Analysis, Writing – original draft, Methodology, Visualization, Data curation, Investigation, Validation, Conceptualization, Project administration, Supervision. AS: Formal Analysis, Conceptualization, Writing – review & editing, Investigation, Writing – original draft. PM-T: Formal Analysis, Writing – review & editing, Writing – original draft, Visualization, Investigation, Conceptualization. AD-Z: Writing – original draft, Investigation, Conceptualization, Writing – review & editing. MJ: Conceptualization, Writing – review & editing, Methodology, Writing – original draft, Formal Analysis. MG: Investigation, Writing – review & editing, Conceptualization, Supervision, Writing – original draft, Methodology.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization (WHO). Health 2020: Education and health through the life-course. Geneva: World Health Organization (2015). Available at: https://iris.who.int/bitstream/handle/10665/363218/WHO-EURO-2015-6161-45926-66190-eng.pdf?sequence=1.
2. World Health Organization Regional Office for Europe (WHO Europe). The WHO european health equity status report 2019 . Available online at: https://health-inequalities.eu/jwddb/healthy-prosperous-lives-for-all-the-european-health-equity-status-report/ (Accessed 24 March 2024).
3. Institute of Psychiatry and Neurology. Comprehensive study of the mental health of society and its determinants (EZOP II) . Available online at: https://ezop.edu.pl/ (Accessed 24 March 2024).
4. GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. (2022) 9:137–50. doi: 10.1016/S2215-0366(21)00395-3
5. World Health Organization (WHO). World mental health report: transforming mental health for all . Available online at: https://www.who.int/publications/i/item/97892400493381 (Accessed 24 March 2024).
6. Arias D, Saxena S, and Verguet S. Quantifying the global burden of mental disorders and their economic value. EClinicalMedicine. (2022) 54:101675. doi: 10.1016/j.eclinm.2022.101675
7. Kieling C, Buchweitz C, Caye A, Silvani J, Ameis SH, Brunoni AR, et al. Worldwide prevalence and disability from mental disorders across childhood and adolescence: evidence from the global burden of disease study. JAMA Psychiatry. (2024) 81:347–56. doi: 10.1001/jamapsychiatry.2023.5051
8. Ferrari AJ, Somerville AJ, Baxter AJ, Norman R, Patten SB, Vos T, et al. Global variation in the prevalence and incidence of major depressive disorder: a systematic review of the epidemiological literature. Psychol Med. (2013) 43:471–81. doi: 10.1017/S0033291712001511
9. Saxena S, Funk M, and Chisholm D. World health assembly adopts comprehensive mental health action plan 2013-2020. Lancet. (9882) 2013:8;381. doi: 10.1016/S0140-6736(13)61139-3
10. GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. (2022) 9:137–50. doi: 10.1016/S2215-0366(21)00395-3
11. GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. (2024) 403:2133–61. doi: 10.1016/S0140-6736(24)00757-8
12. Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, and Pollitt P. Mental health literacy”: a survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med J Aust. (1997) 166:182–6. doi: 10.5694/j.1326-5377.1997.tb140071.x
13. Ndetei DM, Khasakhala LI, Mutiso V, and Mbwayo AW. Knowledge, attitude and practice (KAP) of mental illness among staff in general medical facilities in Kenya: practice and policy implications. Afr J Psychiatry (Johannesbg). (2011) 14:225–35. doi: 10.4314/ajpsy.v14i3.6
14. Journal of laws. Regulation of the council of ministers on the national mental health protection programme for 2023–2030 (item 2480) . Available online at: https://isap.sejm.gov.pl/isap.nsf/download.xsp/WDU20230002480/O/D20232480.pdf (Accessed 24 March 2024).
15. Arianda Poland’s Research Panel. About the panel . Available online at: https://panelariadna.com/ (Accessed 24 March 2024).
16. Statistics Poland. Demographic yearbook of Poland 2024. . Available online at: https://stat.gov.pl/en/topics/statistical-yearbooks/statistical-yearbooks/demographic-yearbook-of-Poland-2024,3,18.html (Accessed 24 March 2024).
17. Wrześniewska-Wal I, Grudziąż-Sękowska J, Pinkas J, and Jankowski M. Public knowledge and beliefs regarding pharmacy-based immunization in Poland-A nationwide cross-sectional study, 2024. Vaccines (Basel). (2024) 12:835. doi: 10.3390/vaccines12080835
18. Mularczyk-Tomczewska P, Lewandowska A, Kamińska A, Gałecka M, Atroszko PA, Baran T, et al. Patterns of energy drink use, risk perception, and regulatory attitudes in the adult polish population: results of a cross-sectional survey. Nutrients. (2025) 17:1458. doi: 10.3390/nu17091458
19. Kamińska A, Jankowski M, Rejdak MB, Ostrowski J, Rejdak R, and Pinkas J. An online questionnaire-based survey of 1076 individuals in Poland to identify the prevalence of ophthalmic symptoms in autumn 2022. Med Sci Monit. (2023) 29:e939622. doi: 10.12659/MSM.939622
20. Grudziąż-Sękowska J, Sękowski K, Pinkas J, and Jankowski M. Preferred sources of information on diabetes prevention programmes: a population-based cross-sectional study in Poland. BMJ Open. (2024) 14:e083362. doi: 10.1136/bmjopen-2023-083362
21. Jankowski M, Grudziąż-Sękowska J, Kamińska A, Sękowski K, Wrześniewska-Wal I, Moczeniat G, et al. A 2024 nationwide cross-sectional survey to assess the prevalence of cigarette smoking, e-cigarette use and heated tobacco use in Poland. Int J Occup Med Environ Health. (2024) 37:271–86. doi: 10.13075/ijomeh.1896.02402
22. Kutcher S, Wei Y, and Coniglio C. Mental health literacy: past, present, and future. Can J Psychiatry. (2016) 61:154–8. doi: 10.1177/0706743715616609
23. Toczyski P. The Local Awareness-Raising of Public Mental Health in the Capital City of Poland through Launch of Local Alliance against Depression. Int J Environ Res Public Health. (2023) 20:3892. doi: 10.3390/ijerph20053892
24. Chireh B, Li M, and D’Arcy C. Diabetes increases the risk of depression: A systematic review, meta-analysis and estimates of population attributable fractions based on prospective studies. Prev Med Rep. (2019) 14:100822. doi: 10.1016/j.pmedr.2019.100822
25. Catapano P, Luciano M, Cipolla S, D'Amico D, Cirino A, Della Corte MC, et al. What is the relationship between exposure to environmental pollutants and severe mental disorders? A systematic review on shared biological pathways. Brain Behav Immun Health. (2024) 43:100922. doi: 10.1016/j.bbih.2024.100922
26. Zgłobicki W and Baran-Zgłobicka B. Air pollution in major Polish cities in the period 2005-2021: Intensity, effects and attempts to reduce it. Environ Res. (2024) 240. doi: 10.1016/j.envres.2023.117497
27. Zolotor AJ and Yorkery B. Public policy approaches to population health. Prim Care. (2019) 46:575–86. doi: 10.1016/j.pop.2019.07.015
28. Bhave SY, Sovani AV, and Shah SR. Role of psychologist in adolescent medicine. Pediatr Clin North Am. (2022) 69:847–64. doi: 10.1016/j.pcl.2022.05.001
29. Müller H, Rehn-Groenendijk J, and Wasmer A. Small-scale urban design interventions: a framework for deploying cities as resource for mental health and mental health literacy. Front Psychol. (2023) 14:1112209. doi: 10.3389/fpsyg.2023.1112209
30. Khan S and Ramtekkar U. Child and adolescent telepsychiatry education and training. Psychiatr Clin North Am. (2019) 42:555–62. doi: 10.1016/j.psc.2019.08.010
31. Cong A, Shang L, Yan F, Zhao Y, Qi H, Huang Q, et al. Knowledge of and attitude towards depression among urban and rural residents in Beijing: a cross-sectional study. BMJ Open. (2024) 14:e083374. doi: 10.1136/bmjopen-2023-083374
32. Steptoe A, Deaton A, and Stone AA. Subjective wellbeing, health, and ageing. Lancet. (9968) 2015:385. doi: 10.1016/S0140-6736(13)61489-0
33. Luberenga I, Kasujja R, Vasanthan LT, Nyende A, Tumwebaze E, Henry Joseph LJ, et al. Mental health awareness programmes to promote mental well-being at the workplace among workforce in the low-income and middle-income countries: a scoping review protocol. BMJ Open. (2023) 13:e073012. doi: 10.1136/bmjopen-2023-073012
34. Hahn JS, Chua KC, Jones R, and Henderson C. The Every Mind Matters campaign: changes in mental health literacy and its associations with campaign awareness. Eur J Public Health. (2023) 33:1008–13. doi: 10.1093/eurpub/ckad145
35. Knutson D, Irgens MS, Flynn KC, Norvilitis JM, Bauer LM, Berkessel JB, et al. Associations between primary residence and mental health in global marginalized populations. Community Ment Health J. (2023) 59:1083–96. doi: 10.1007/s10597-023-01088-z
36. Zajacova A and Lawrence EM. The relationship between education and health: reducing disparities through a contextual approach. Annu Rev Public Health. (2018) 39:273–89. doi: 10.1146/annurev-publhealth-031816-044628
37. van der Heide I, Wang J, Droomers M, Spreeuwenberg P, Rademakers J, and and Uiters E. The relationship between health, education, and health literacy: results from the Dutch Adult Literacy and Life Skills Survey. J Health Commun. (2013) 18 Suppl 1:172–84. doi: 10.1080/10810730.2013.825668
Keywords: mental health, mental disorders, awareness, knowledge, risk factors
Citation: Lewandowska A, Silczuk A, Mularczyk-Tomczewska P, Duda-Zalewska A, Jankowski M and Gujski M (2025) Awareness of mental disorders and their risk factors - a nationwide cross-sectional survey among adults in Poland. Front. Psychiatry 16:1599683. doi: 10.3389/fpsyt.2025.1599683
Received: 25 March 2025; Accepted: 07 May 2025;
Published: 26 May 2025.
Edited by:
Pv AshaRani, Institute of Mental Health, SingaporeReviewed by:
Sonia Celedonia Huyhua Gutierrez, Universidad Nacional Toribio Rodríguez de Mendoza de Amazonas, PeruNurul Fajriyah Prahastuti, Sunan Kalijaga State Islamic University Yogyakarta, Indonesia
Copyright © 2025 Lewandowska, Silczuk, Mularczyk-Tomczewska, Duda-Zalewska, Jankowski and Gujski. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andrzej Silczuk, YW5kcnplai5zaWxjenVrQHd1bS5lZHUucGw=
 Aleksandra Lewandowska1
Aleksandra Lewandowska1 Andrzej Silczuk
Andrzej Silczuk Paulina Mularczyk-Tomczewska
Paulina Mularczyk-Tomczewska Mateusz Jankowski
Mateusz Jankowski Mariusz Gujski
Mariusz Gujski