- 1Research Center for Green Chemistry and Ecological Environment Technology, Guizhou Industry Polytechnic College, Guiyang, China
- 2State Key Laboratory Breeding Base of Green Pesticide and Agricultural Bioengineering, Key Laboratory of Green Pesticide and Agricultural Bioengineering, Ministry of Education, Guizhou University, Guiyang, China
- 3Drug Identification Center, Guiyang Municipal Public Security Bureau, Guiyang, China
The abuse of new psychoactive substances and narcotic drugs as drug substitutes poses a serious threat to public health and safety. This study outlines the effective use and negative abuse of drug substitutes and outlines associated criminal behaviors to help readers understand the potential risks of such substances. By summarizing the technical bottlenecks in the analysis and detection of criminal cases, this study highlights their impact on case discrimination, which in turn can limit or even render policy implementation ineffective. Finally, based on database analysis and the current regulatory system, flexible control strategies were proposed to address the constantly emerging “new” substances, providing a reference for relevant control guidelines to be formulated.
1 Introduction
With the rapid development of social economy, drug abuse has become an increasingly prominent issue posing a serious threat to social security and the physical and mental health of individuals. In recent years, the scale of drug supply, consumption, and abuse has continued to decline due to factors such as zero tolerance and high-pressure crackdowns on drug-related crimes by the international community. However, drug substitutes abuse has gradually increased, and new dynamics and trends have emerged in the field internationally. Drug substitutes are substances with effects similar to those of the original addictive substance that are sought by drug users for convenience and to satisfy their addiction due to an imbalance between supply and demand. These substances offer users convenience and a means to satisfy their addiction. Drug substitutes can be divided into the following categories according to their chemical composition, abuse methods, and effects: synthetic substitutes, natural plant substitutes, drug abuse substitutes, and new psychoactive substances. These substitutes often have addictive properties and can simulate or enhance the effects of traditional drugs in certain aspects while avoiding drug legislation (1–3). These compounds are popular worldwide because of their ease of purchase, lack of legal regulations, and incomplete safety assessment (4).
However, experimental, clinical, and epidemiological studies have shown that certain drug substitutes may cause chronic or acute health problems and pose unpredictable risks to human health (3–8). Abuse of drug substitutes by drug users can easily lead to mental abnormalities, hallucinations, or manic symptoms, posing a risk of accidents and even nonfatal and fatal poisoning hazards (5, 9, 10). Furthermore, in recent years, there has been a surge in the number of offenses involving drug substitutes, such as illegal manufacturing and distribution (11), involvement in narcotic-related sexual assaults (12, 13), accidental or intentional intoxication (6, 14–16), and recreational drugs abuse (16–19). However, in forensic and law enforcement departments, unlisted or newly emerging drug substitutes are excluded from standard drug screening protocols, and these may go undetected. Therefore, detecting new drugs in clinical and forensic setting is a complex task since traditional detection methods, such as mass spectrometry and chromatography, are reliant on known standard database that are difficult to update in real time. Simultaneously, other challenges such as sample complexity and matrix interference, trace detection and sensitivity limitations, and limitations of on-site rapid detection further complicate the analysis of certain drug substitutes. faces multiple challenges in the detection process. These analytical challenges are scientific in nature and directly affect the law enforcement, judicial system, and public health departments in their goal of prevention and control.
Drug traffickers use chemical modifications to synthesize alternative drugs and constantly challenge regulatory systems (such as the United States Federal Analogues Act) that are based primarily on chemical formulas. This force countries to explore more flexible policies to balance control accuracy with the need for quick response. In 1986, the United States revised the “Analogues Control Act” to explicitly state that substances sharing a parent structure or pharmacological similarity with a scheduled drug should be classified as a controlled analog (20). The purpose of this bill was to combat “underground scientists” who chemically modify the structure of listed substances, setting a precedent for the “skeletons control”. Subsequently, the UK followed suit by enacting the “Psychotropic Substances Act” in 2016, which established a parallel legislative response to address the rapid growth and increasing abuse of new substances. The “China Drug Situation Report 2019” (21) first proposed the concept of drug substitutes and mentioned their abuse in subsequent years. However, there was no mention of an explicit proposition of appropriate management policies for drug substitutes. These ambiguities in the formulation of laws and policies may affect case assessment and weaken the power of the law. Therefore, China may achieve collaborative innovation through the “China’s plan” and through international experience via “selective reference + localization transformation”. To break the vicious cycle of “ineffective control → accelerated diffusion” and build a more resilient drug control system.
Drug substitute abuse is becoming an increasingly serious issue and represents a key area for breaking the vicious circle of “regulation - variation - reregulation.” However, current research on drug substitutes is limited, lacking systematic understanding and in-depth research. This study provides an overview of the current trends and developments related to drug substitutes from several perspectives: explaining their pros and cons (knowing), analyzing their criminal effects (understanding), examining analytical detection methods (mastering), and prevention and control strategies (prevention). This study provides a valuable reference for drug abuse prevention and control efforts in China and contributes to the promotion of social harmony and stable development.
2 Duality of drug substitutes - benefits
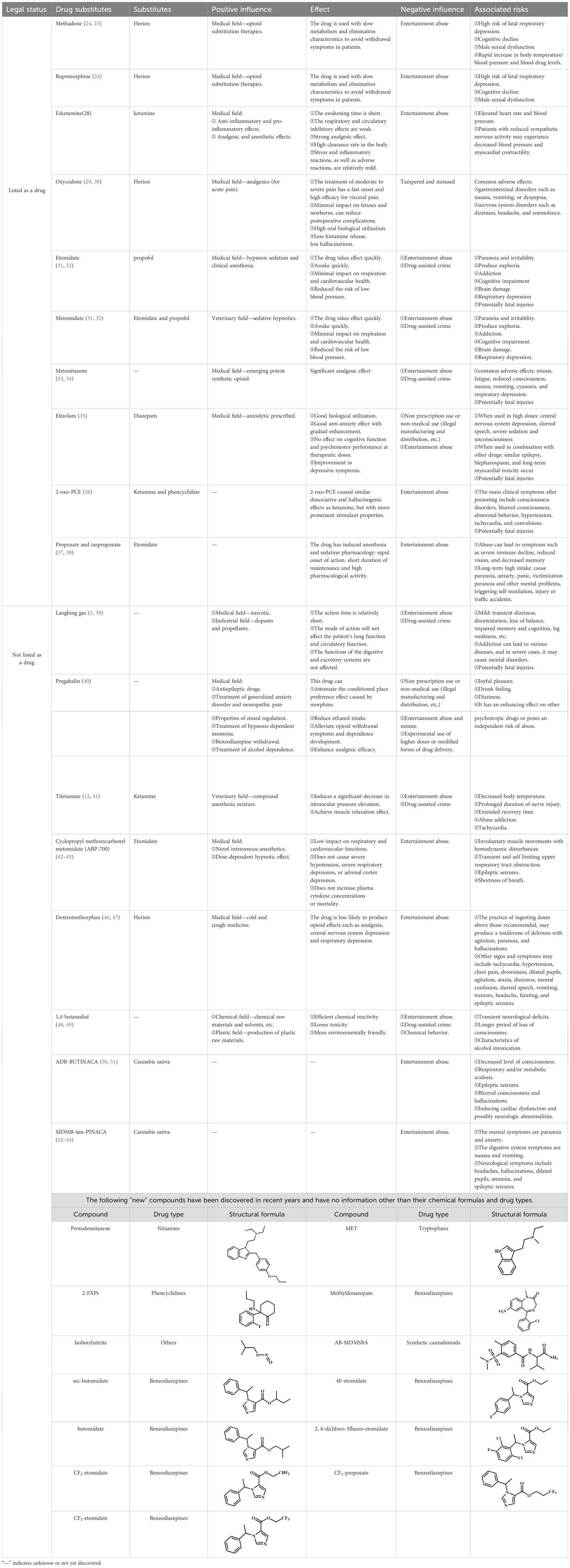
Psychoactive substances or psychotropic drugs are chemical substances that affect human function as well as mental and behavioral states (22). Certain psychotropic substances have been reported to be relatively safe, inexpensive, readily available, of consistent quality (23), and highly effective (17). These characteristics highlight their potential antitoxic nature and value as alternative substances. Prior study findings have demonstrated that methadone or buprenorphine can be used as maintenance therapy to reduce mortality (24, 25); acetylfentanyl and butyrylfentanyl can rapidly inhibit morphine withdrawal symptoms in rhesus monkeys, with butyrylfentanyl demonstrating a morphine replacement effect (26); esketamine, the right-handed isomer of ketamine, with strong analgesic effects, a short awakening time, and weak inhibition of respiration and circulation, is widely used in the clinic (27, 28); oxycodone is used medically as an opioid analgesic and has the advantages of oral bioavailability, rapid onset of action, high efficacy in visceral pain, and fewer hallucinations (29, 30); etomidate compounds are used clinically for hypnotic sedation and anesthesia with rapid drug onset, rapid awakening, minimal respiratory and cardiovascular effects and reduced risk of hypotension (31, 32). In addition to this, some of the other drug substitutes with positive effects are shown in Table 1.
Certain substances may have antitoxicity and alternative therapeutic properties. However, several experimental, clinical, and epidemiological studies have shown that most drug substitutes are associated with certain complications, including functional disorders, cognitive loss, multiorgan damage, poisoning, and high mortality rates (9, 10). Certain piperazine derivatives, with specific functional groups or substituents are used as anticancer drugs and exhibit good antitumor activity and low cytotoxicity in normal human liver cells, besides significantly inducing apoptosis, making them effective in an anticancer role (55, 56). As antipsychotic drugs too, piperazine derivatives exhibit strong activity to certain receptors. These antipsychotic effects are greatly enhanced when different heterocyclic groups are attached to the core piperazine structure or its rings (57, 58). However, piperazine analogs pose risks to humans as well such as life-threatening serotonin syndrome, hepatotoxicity, neurotoxicity, psychopathology, and potential abuse (4, 8, 59). “Laughing gas” is used medically as an anaesthetic (5), appreciated for its anxiolytic effects, and serves as an effective dopant in many industries (39). The industrial application of laughing gas constitutes a remarkable part of the national economy. However, its side effects include dizziness, disorientation, loss of balance, impaired memory and cognition, and leg weakness (5). Addiction to laughing gas can lead to various diseases, and, in severe cases, mental disorders and life-threatening complications.
The effects of drug substitutes on the body depend on single or multidrug intoxication (60, 61), route of administration (62), the person’s medical history (63), overdose, and medication purposes (64–66). To mitigate adverse events, it is essential to understand the pharmacological properties and common uses of drug substitutes prior to application, as well as ensure strict supervision and standardized guidelines are being followed during use. In summary, based on the progress in basic and clinical medical research, it is necessary to transform societal knowledge, attitudes and behaviors toward various types of drug substitutes. A comprehensive understanding of the relationship between drug substitutes and individuals, society, and countries should be considered at different levels and in varied perspectives. Strengthening the management of drug substitutes by updating the drug catalog can ensure their safe and effective use while maximizing their potential benefits.
3 Duality of drug substitutes - risks
Drug substitutes have been of use in the material sciences world for a long time and were originally intended to promote the development of this field (24–33). However, due to its traditional drug like effects, easy access, and gray areas in legal regulation, this type of substance has gradually become the focus of attention for drug traffickers. In recent years, drug substitutes have been found in suspected drug-related crimes; however, the degree of abuse is relatively mild (67, 68) and involves substances such as benzodiazepines, hypnotics, sedatives, and anesthetics. Initially, the emergence of these substitutes was likely driven by a lack of awareness of their potential harm and a desire for the effects these psychoactive substances provided. With changes in society and the strengthening of drug control measures, the supply of these addictive substances became insufficient and expensive. This led drug traffickers to seek drug substitutes with similar effects for sale or to commit crimes (11–19).
Drug substitutes are not confined to a closed range, and any addictive substance has the potential to become a substitute for abuse. This highlights the diversity and complexity of criminal targets, the interconnected and varied forms of criminal organization forms and the globalization and internationalization of crime-related regions. According to the United Nations Office on Drugs and Crime, a high proportion of new psychoactive substances-related deaths reported in 2019 were related to kratom, which has opioid and stimulant properties and contains pharmacologically active alkaloids. Between 2017 and 2019, the US Toxicology Portal reported 47 cases of kratom infection. Of these, 29 individuals died, 16 consumed it under the influence of alcohol, 1 was sexually assaulted, and 1 incident occurred in public places (69). Studies have indicated that xylazine (a veterinary drug) can also be used as a drug substitute in humans. Xylazine misuse has been linked to both accidental and intentional poisoning (6, 14, 15), recreational use, and use as a recreational drug admixture (18, 19). When administered to humans, it may cause central nervous system and respiratory depression, bradycardia, hypotension, and death. In addition, certain drug substitutes listed as illicit drugs are used for other illicit incidents, including drug trafficking (11), narcotic-related crimes (12, 13), lethal injections (15), recreational abuse (16, 17), and use as sedatives for animals reared for food and as stimulants for sports animals (19, 70). In addition, according to the results of the analysis of biological samples (hair, urine, and tobacco oil) conducted by the Drug Identification Center of the Guiyang Municipal Public Security Bureau in recent years, it was found that Pregabalin (41), ABP-700 (42–45), Dextromethorphan (46, 47), ADB-BUTINACA (50, 51), MDMB-4en-PINACA (52–54) and protodesnitazene were not included in the prohibited list, and the detection rate continued to increase. The relevant information on these drug substitutes is provided in Table 1.
Regarding the constantly emerging “new” substances and “new” crimes, White et al. (71) and Goldstein et al. (72) argue that drugs induce psychoactive effects that reduce natural inhibitions, thereby altering the drug user’s perception of the risks and consequences of crime. From an economic standpoint, drug users commit crimes as a means to finance their drug use. This trade in illegal drugs constitutes a crime and can lead to other criminal activities. In other words, if drug substitute usage lead to criminal behavior, then this criminal behavior creates further demand, sustaining the market for such substances. When existing laboratory analysis techniques fail to detect “new” drug substitutes circulating in the market or when legal loopholes exist, traditional regulatory measures become ineffective. This highlights the urgent need to develop cutting-edge analysis methods capable of rapidly identifying these substances, tracing their criminal use, and supporting judicial efforts. Such innovations are essential for providing scientific evidence that can disrupt the chain of the criminal behavior associated with drug substitute crimes.
4 Technical bottlenecks in the analysis of drug substitutes
According to the World Drug Report 2023 published by the United Nations Office on Drugs and Crime, new psychoactive substances are being continuously added globally in recent years, with only a few identified in laboratories within a short period (73). This lag in detection technology can undermine the reliability of scientific evidence, delay legal responses, exacerbate resource allocation imbalances, and, ultimately, result in limited or ineffective policy implementation. Laboratory testing currently focuses on the challenges of samples, instruments, and standards.
Appropriate biological samples are fundamental to the scientific and legal effectiveness of drug analysis. Such robust samples enable qualitative identification of substances present in drug users and provide targeted, highly accurate quantitative information about one or multiple drug substitutes (74). For general drug abuse cases, blood, urine, hair, and saliva are commonly used samples as they reduce the impact on the examinee In the case of collection of samples following death, peripheral blood, cardiac blood, spleen tissue, injection site tissue, and stomach tissue as well as the contents of the stomach are collected to provide a more comprehensive analysis of the type, duration, and form of substance abuse in the deceased’s body (15, 75). If necessary to determine whether alcohol has been consumed, ocular vitreous fluid should be collected simultaneously (75). Due to the high rates of sexual crimes worldwide, Amanda et al. (76) collected semen samples from crime scenes or victims as biological samples for testing. This method overcomes the limitations of traditional testing and provides support for criminal investigations. In addition, with the further optimization of modern analytical tools, the choice of biological samples has become wider. As Drolet’s et al. research has shown, dried blood spot and dried urine strip methodologies are minimally invasive sample collection methods that allow for ease of sample collection at minimal cost (77). The selection of samples must be comprehensively evaluated and considered based on the purpose of detection, toxicokinetic characteristics, legality of sample collection, and suitability of technical methods.
From the perspective of production methods, most drug substitutes produce new substances with structures similar to those of the original substances by modifying certain groups in the chemical structure (78–85). When these drug substitutes and their metabolites have similar chemical structures to those of their prototype drugs, simple test plates can be used to test positivity; however, these can lead to false-positive results (11, 86). Therefore, the detection and analysis of drug substitutes with similar structures typically require high-precision instruments such as mass spectrometry and liquid chromatography. Tiletamine and telazol have structures similar to those of ketamine, which can easily lead to false-positive immunoassay results. In such cases, advanced testing methods can be used; such as the case where He et al. (12) and Quail et al. (17) used GC-QTOF-MS and gas chromatography-mass spectrometry for detection and provided accurate mass numbers post-analysis. Previous studies have shown that the detection of etomidate and/or etomidate acids in biological samples is indicative of drug abuse since etomidate acid is a common metabolite of etomidate and its analogs (31, 32). However, etomidate analogs currently available on the market are not listed in Table 1. Tang et al. (31, 32) used high-resolution liquid chromatography-mass spectrometry to analyze specific metabolites and track prototype compounds to avoid misjudgment of drug abuse cases. This provides a reference for analyzing these substances. However, the dependence on high-end equipment, regional capacity differences, and imbalanced allocation of mass spectrometry parameter setting resources among countries have led to marked differences in the technical level of forensic toxicology analysis among laboratories. At the same time, drug testing, analysis, and identification in various countries are mainly concentrated in the National Drug Laboratory and a few qualified appraisal institutions. Most research institutions with the necessary capabilities are currently unable to perform relevant analyses and identifications, hindering the rapid development of detection and analysis.
Laboratory analysis results are highly dependent on the availability of standards and databases. However, both are subject to delayed update cycles. The emergence of new alternatives to detection and re-listing follows three steps: submission of applications, risk assessment, and formal listing (87, 88). During this time lag, the market share of these drug substitutes expands sufficiently to support the next round of structural variation. Currently, only a few foreign companies can provide standard substances for newly identified substances, and these are often expensive and limited in variety; therefore, many laboratories are unable to obtain high-quality reference substances (86), possibly leading to the misclassification of legal drugs as substitutes and weakening of the public trust in antidrug policies. However, many substitutes are metabolized into unknown compounds within the human body, making it difficult to trace them back to the original substance using existing technologies or standards. In legal proceedings, if the court requires clear evidence linking drug ingestion to individual behavior but the metabolites do not correspond to the original substance, the case may be dismissed due to insufficient evidence. This may lead to a cycle of “detection lag or insufficient evidence → regulatory delay → market diffusion → technology catch-up”.
Therefore, it is necessary to continuously expand the scope of drug substitute testing and improve, update, and optimize the screening and analysis processes internally. When the iteration speed of drug substitutes exceeds the cognitive boundary of traditional detection technologies, innovation in analytical methods is no longer merely a technical proposition of the laboratory.
5 Loopholes in the current control system and the proposal of new control ideas
The “structural escape” strategy designed by drug traffickers—exploiting delays in mass spectrometry databases—constantly challenges regulatory systems that rely on chemical formulas as the control. This has forced policymakers to find a new balance between “precise legislation” and “flexible control”. When a new substitute emerges in the drug market, legislators request a risk assessment by the World Health Organization’s drug expert committee on the relevant substance (87). If the assessment shows that the substance pose a risks that outweighs its potential therapeutic value, it may be added to the International Drug Control Convention for Regulation. For a period of time, legal restrictions on the sale of gamma hydroxybutyric acid in the UK have actually led to an increase in the use of the drug GBL (89, 90), and subsequent legislation targeting GBL contributed to the emergence of substitutes with higher side effects. The prohibition of methamphetamine has led to the rapid and widespread popularity of its legal substitutes such as BZP (78) and U-47700 (79). After a period of time, both were listed as controlled drugs, leading to the rapid emergence of D2PM and mephedrone (91) as substitutes of unknown toxicity. Furthermore, substitutes for substances such as ketamine, heroin, and morphine, such as isoflurane (80), fentanyl (81), 4-fluoroamphetamine (82, 83), and cassia seed (84, 85), have been in widespread use for some time now. Subsequently, due to reports of poisoning and death from these alternative drugs, these alternatives were added to the list of controlled drugs.
However, when these harmful substances disappear from the drug market, alternative substances that cause greater harm may emerge (3, 92). This poses a new problem, as the user group knows little about these compounds and is almost unaware of the risks posed by these new drugs. This leads to the question of whether this is a good strategy to drive all drug substitutes to the market immediately. Another approach proposed by foreign policymakers to address this issue is to accept reality, formulate policies, tolerate substances with the least risk, and prevent user groups from shifting from one substance to another, thereby reducing the risk of substance use (93). While considering systematic solutions, it is good to create favorable policies that align with local culture, background, and politics (94).
Based on existing international and domestic management regulations and social development needs, this study proposes the following hypotheses. First, in light of China’s national conditions, a temporary control system should be established, drawing on the practices of the United States, United Kingdom, Russia, and other countries (95). When a new type of substance that poses a serious risk to public health emerges in the a country, it may be subjected to temporary scheduling for a period of 1–2 years, during which a risk assessment can be conducted before deciding whether to officially list it. At the same time, after the activity and effects of the substance have been assessed by a judicial appraisal agency or scientific researchers, the information currently available will be made public; therefore, the public can become aware of the substance and reduce its use to minimize the risks involved. Second, after formal listing, relevant departments should issue judicial interpretations to establish standards for prosecuting and convicting individuals involved in the manufacture and trafficking of such substances. Subsequently, an authoritative identification agency should be established at the national level; a library of standard substances and analytical charts should be established; analytical methods based on common laboratory instruments should be developed; and analytical methods for biological samples suitable for on-site law enforcement testing should be developed to enhance the level of awareness and detection capabilities. Finally, supervision of the production and distribution of drug substitutes should be increased. The distribution of synthetic raw materials for medicines is controlled, and enterprises that produce, process, and sell new active substances without obtaining registration certificates should be dealt with in accordance with the law. Strengthening internet monitoring, timely deletion of websites containing the content of selling and trafficking drug substitutes, and dealing with relevant websites is also of utmost importance. Regardless of the approach taken, it will need to change over time to deal with this dynamic market and the increasing number of innovative attempts to circumvent regulations.
To strengthen the control of drug substitutes, it is necessary to work simultaneously on aspects of prevention, monitoring, and enforcement. First, demand-side interventions should be carried out for high-risk groups based on the trend of abuse to eliminate the possibility of abuse on this side. Simultaneously, monitoring and testing should be strengthened to accurately determine the properties of suspicious substances. It is necessary to strengthen the fight against illegal production, transport, sale, and possession of these substances. Finally, it is important to understand the degree of control required to prevent criminals from shifting their attention to compounds with higher risks. In other words, the management of drug substitutes should be based on the premise of “necessity” and should be undertaken without affecting economic and social development to achieve a balance between “necessary management” and “legitimate use”.
6 Conclusion
This study revealed the duality of current drug substitutes, including the effective use of medical and industrial drugs and the negative effects of illegal abuse and crime. The continuous emergence of drug substitutes leads to criminal cases, presenting multiple challenges for forensic investigations and laboratory analysis. These analytical challenges complicate law enforcement efforts and policy responses, ultimately weakening public confidence in antidrug policies. We also analyzed the unintended spread of more harmful new alternatives following prohibition measures of the older substances and proposed solutions informed by current regulatory management and social development needs to help mitigate this. In summary, this study aimed to systematically understand drug substitutes to reduce the risk of exposure. Moreover, it provides an analysis of the current situation of drug substitutes for public security organizations, enabling them to better respond to changes in the drug environment and maximize the effectiveness of combating drug substitute–related crimes.
Author contributions
SB: Conceptualization, Funding acquisition, Project administration, Supervision, Writing – review & editing. ML: Supervision, Writing – review & editing, Conceptualization, Project administration. ST: Conceptualization, Supervision, Investigation, Writing – review & editing. SW: Conceptualization, Investigation, Supervision, Writing – review & editing, Validation. RW: Conceptualization, Supervision, Resources, Software, Writing – review & editing. LC: Conceptualization, Supervision, Writing – review & editing, Project administration. FW: Supervision, Funding acquisition, Writing – original draft, Writing – review & editing. SL: Conceptualization, Funding acquisition, Investigation, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported, in part, by the Science and Technology Planning Project of Guozhou Province under Grant (Qian Ke He Zhi Cheng (2022) Yi Ban 279); Guizhou Industry Polytechnic College Faculty-level Research Project (Grant No. 2024zk18); the Opening Foundation of the Key Laboratory of Green Pesticide and Agricultural Bioengineering, the Ministry of Education, Guizhou University under Grant (2020GDGP0105); High-Level Talent Initial Funding of Guizhou Industry Polytechnic College under Grant (2023-RC-01); and Guizhou Industry Polytechnic College Science and Technology Innovation Team Project (Grant No. 2023CXTD03).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscriptBH
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Reuter P and Pardo B. New psychoactive substances: are there any good options for regulating new psychoactive substances? Int J Drug Policy. (2017) 40:117–22. doi: 10.1016/j.drugpo.2016.10.020
2. De Castro JS, Rodrigues CHP, and Bruni AT. In silico infrared characterization of synthetic cannabinoids by quantum chemistry and chemometrics. J Chem Inf Model. (2020) 60:2100–14. doi: 10.1021/acs.jcim.9b00871
3. Winstock AR and Ramsey JD. Legal highs and the challenges for policy makers. Addiction. (2010) 105:1685–7. doi: 10.1111/j.1360-0443.2010.02934.x
4. Welz A and Koba M. Piperazine derivatives as dangerous abused compounds. Acta Pharmaceut. (2020) 70:423–41. doi: 10.2478/acph-2020-0035
5. Fan TT, Han M, Liang Y, Cao GH, and Song GD. Application effects of nitrous oxide and oxygen mixed inhalation technology on analgesia and sedation during debridement and dressing change in children with moderate or severe burns. Publishing House Chin Med Assoc. (2022) 39:248–55. doi: 10.3760/cma.j.cn501225-20220308-00051
6. KrongvorakulL J, Auparakkitanon S, Trakulsrichai S, Sanguanwit P, Sueajai J, Noumjad N, et al. Use of xylazine in drug-facilitated crimes. J Forensic Sci. (2017) 63:1325–30. doi: 10.1111/1556-4029.13684
7. Cerveny SN, D’Agostino JJ, Davis MR, and Payton ME. Comparison of laryngeal mask airway use with endotracheal intubation during anesthesia of western lowland gorillas (Gorilla gorilla gorilla). J Zoo Wildlife Med. (2012) 43:759–67. doi: 10.1638/2011-0081r.1
8. Arbo MD, Bastos ML, and Carmo HF. Piperazine compounds as drugs of abuse. Drug Alcohol Depen. (2012) 122:174–85. doi: 10.1016/j.drugalcdep.2011.10.007
9. Shevyrin V, Melkozerov V, Nevero A, Eltsov O, Shafran Y, Morzherin Y, et al. Identification and analytical characteristics of synthetic cannabinoids with an indazole-3-carboxamide structure bearing a N-1-methoxycarbonylalkyl group. Anal Bioanal. Chem. (2015) 407:6301–15. doi: 10.1007/s00216-015-8612-7
10. Kasper MA, Ridpath AD, and Arnold JK. Notes from the field: severe illness associated with reported use of synthetic cannabinoids–mississippi, April 2015. Centers Dis Control Prev. (2015) 64:1121–2. doi: 10.15585/mmwr.mm6439a7
11. Hamby D, Burnett A, Jablonsky M, Twamley B, Kavanagh PV, and Gardner EA. Identification of 2-(ethylamino)-1-(4-methylphenyl)-1-pentanone (4-MEAP), a new “Legal high” Sold by an internet vendor as 4-methyl pentedrone. J Forensic Sci. (2015) 60:721–6. doi: 10.1111/1556-4029.12712
12. He SY, Gong FJ, and Lian R. Identification of tiletamine, zolazepam and their metabolites in drug facilitated sexual assault by GC-QTOF-MS. J Forensic Med. (2019) 35:581–5. doi: 10.12116/j.issn.1004-5619.2019.05.013
13. Kintz P. Bioanalytical procedures for detection of chemical agents in hair in the case of drug-facilitated crimes. Anal Bioanal. Chem. (2007) 388:1467–74. doi: 10.1007/s00216-007-1209-z
14. Ruiz-Colón K, Chavez-Arias C, Díaz-Alcalá JE, and Martínez MA. Xylazine intoxication in humans and its importance as an emerging adulterant in abused drugs: A comprehensive review of the literature. Forensic Sci Int. (2014) 240:1–8. doi: 10.1016/j.forsciint.2014.03.015
15. Chung H, Choi H, Kim E, Jin W, Lee H, and Yoo YA. Fatality due to injection of tiletamine and zolazepam. J Anal Toxicol. (2000) 240:305–8. doi: 10.1093/jat/24.4.305
16. Zuba D, Adamowicz P, and Byrska B. Detection of buphedrone in biological and non-biological material–Two case reports. Forensic Sci Int. (2013) 227:15–20. doi: 10.1016/j.forsciint.2012.08.034
17. Quail MT, Weimersheimer P, Woolf AD, and Magnani B. Abuse of telazol: an animal tranquilizer. J Toxicol.: Clin Toxicol. (2001) 39:399–402. doi: 10.1081/clt-100105161
18. Capraro AJ, Wiley JF, and Tucker JR. Severe intoxication from xylazine inhalation. Pediatr Emerg Care. (2001) 17:447–8. doi: 10.1097/00006565-200112000-00012
19. Teoh WK, Md Muslim NZ, Chang KH, and Abdullah AFL. Abuse of xylazine by human and its emerging problems: a review from forensic perspective. Malaysian J Med Health Sci. (2022) 18:190–201. doi: 10.47836/mjmhs18.4.26
20. Shimomura H, Dangott LJ, and Garbers DL. Covalent coupling of a resact analogue to guanylate cyclase. J Biol Chem. (1986) 261:15778–82. doi: 10.1016/S0021-9258(18)66786-9
21. China drug situation report 2019. Ministry of Public Security of the People’s Republic of China (2025). Available online at: https://www.mps.gov.cn/n6557558/c7257139/content.html (Accessed May 2025).
22. Amanollahi A, Shadnia S, Mehrabi Y, and Etemad K. Association between intoxication with psychoactive substances and adverse effects occurrence in consumers. Front Public Health. (2023) 11:1228854. doi: 10.3389/fpubh.2023.1228854
23. Carhart-Harris RL, King LA, and Nutt DJ. A web-based survey on mephedrone. Drug Alcohol Depend. (2011) 118:19–22. doi: 10.1016/j.drugalcdep.2011.02.011
24. Noble F and Marie N. Management of opioid addiction with opioid substitution treatments: beyond methadone and buprenorphine. Front Psychiatry. (2019) 9:742. doi: 10.3389/fpsyt.2018.00742
25. Guillery SPE, Hellweg R, Enge S, Bohr U, Kunte H, and Kronenberg G. Patients’ perceptions of opioid replacement therapy: a comparison of diamorphine and methadone/levomethadone. Int J Ment Health Ad. (2021) 19:2194–203. doi: 10.1007/s11469-020-00313-0
26. Aceto MD, Harris LS, and May EL. Dependence studies of new compounds in the rhesus monkey, rat, and mouse. Problems Drug Depend. (1996) 1998):338.
27. Schwenk ES, Pradhan B, and Nalamasu R. Ketamine in the past, present, and future: mechanisms, metabolites, and toxicity. Curr Pain Headache R. (2021) 25:57. doi: 10.1007/s11916-021-00977-w
28. Tu W, Yuan H, and Zhang S. Influence of anesthetic induction of propofol combined with esketamine on perioperative stress and inflammatory responses and postoperative cognition of elderly surgical patients. Am J Transl Res. (2021) 13:1701–9.
29. Piirainen P, Kokki H, and Kokki M. Epidural oxycodone for acute pain. Pharmaceuticals. (2022) 15:643. doi: 10.3390/ph1505064
30. Webster LR, Kinzler ER, Pantaleon C, Iverson M, and Aigner S. Relative oral bioavailability of an abuse-deterrent, immediate-release formulation of oxycodone, oxycodone ARIR in a randomized study. Adv Ther. (2019) 36:1730–40. doi: 10.1007/s12325-019-00963-0
31. Zhong SH, Qin SY, Wang YF, Li H, Wang XY, Chai TRM, et al. Identification and characterization of etomidate and metomidate metabolites in zebrafish, HLMs and S9 fraction by quadrupole-orbitrap LC-MS/MS for drug control. J Chromatogr B. (2025) 1250:124374. doi: 10.1016/j.jchromb.2024.124374
32. Tang YL, Xu LH, Zhao JB, Qian XY, Qiang HS, Xiang P, et al. Metabolic profile of etomidate and its three analogs in Zebrafish, human liver microsomes, human urine and hair samples using UHPLC-Q exactive orbitrap-HRMS. Drug Test Anal. (2025) 0:1–13. doi: 10.1002/dta.3869
33. Krotulski AJ, Papsun DM, Walton SE, and Logan BK. Metonitazene in the United States—Forensic toxicology assessment of a potent new synthetic opioid using liquid chromatography mass spectrometry. Drug Test Anal. (2021) 13:1697–1711. doi: 10.1002/dta.3115
34. Taoussi O, Berardinelli D, Zaami S, Tavoletta F, Basile G, Kronstrand R, et al. Human metabolism of four synthetic benzimidazole opioids: isotonitazene, metonitazene, etodesnitazene, and metodesnitazene. Arch Toxicol. (2024) 98:2101–16. doi: 10.1007/s00204-024-03735-0
35. Nielsen S and Mcauley A. Etizolam: A rapid review on pharmacology, non-medical use and harms. Drug Alcohol Rev. (2020) 39:330–6. doi: 10.1111/dar.13052
36. Tang MHY, Chong YK, Chan CY, Ching CK, Lai CK, Li YK, et al. Cluster of acute poisonings associated with an emerging ketamine analogue, 2-oxo-PCE. Forensic Sci Int. (2018) 290:238–43. doi: 10.1016/j.forsciint.2018.07.014
37. Gleadall IG. The effects of prospective anaesthetic substances on cephalopods: Summary of original data and a brief review of studies over the last two decades. J Exp Mar Biol Ecol. (2013) 447:23–30. doi: 10.1016/j.jembe.2013.02.008
38. Hansen MK, Nymoen U, and Horsberg TE. Pharmacokinetic and pharmacodynamic properties of metomidate in turbot (Scophthalmus maximus) and halibut (Hippoglossus hippoglossus). J Vet Pharmacol Ther. (2003) 26:95–103. doi: 10.1046/j.1365-2885.2003.00454.x
39. Liu DY, Tang K, Zhu SM, Zhang R, Zheng YD, and Gu SL. Effects of oxygen/nitrogen co-incorporation on regulation of growth and properties of boron-doped diamond films. Chin Physic B. (2023) 32:118102. doi: 10.1088/1674-1056/ace4b7
40. Schjerning O, Rosenzweig M, Pottegård A, Damkier P, and Nielsen J. Abuse potential of pregabalin: a systematic review. CNS Drugs. (2016) 30:9–25. doi: 10.1007/s40263-015-0303-6
41. McIver KA, Boveland SD, Clark-Price SC, and Hofmeister EH. Effects of tiletamine-zolazepam vs. propofol on peri-induction intraocular pressure in dogs: A randomized, masked crossover study. Front Vet Sci. (2023) 10:1061755. doi: 10.3389/fvets.2023.1061755
42. Peter S, Ervin P, Yan F, Wei C, and Douglas ER. Cyclopropyl-methoxycarbonyl metomidate studies in a lipopolysaccharide inflammatory model of sepsis. Anesthesiology. (2015) 123:368–76. doi: 10.1097/aln.0000000000000721
43. Valk BI, Absalom AR, Meyer P, Meier S, den Daas I, van Amsterdam K, et al. Safety and clinical effect of i.v. infusion of cyclopropyl-methoxycarbonyl etomidate (ABP-700), a soft analogue of etomidate, in healthy subjects. Brit. J Anaesth. (2018) 120:1401–11. doi: 10.1016/j.bja.2018.01.038
44. Beatrijs V, Megan M, Dario L, Brad Z, John M, and Douglas R. Toxicologic and inhibitory receptor actions of the etomidate analog ABP-700 and its metabolite CPM-acid. Anesthesiology. (2019) 131:287–304. doi: 10.1097/ALN.0000000000002758
45. Michel S, Beatrijs V, Douglas E, Anthony A, Peter M, and Sascha M. A phase 1, single-center, double-blind, placebo-controlled study in healthy subjects to assess the safety, tolerability, clinical Effects, and pharmacokinetics–pharmacodynamics of intravenous cyclopropyl-methoxycarbonylmetomidate (ABP-700) after a single ascending bolus dose. Anesthesiology. (2017) 127:20–35. doi: 10.1097/ALN.0000000000001662
46. Storck M, Black L, and Liddell M. Inhalant abuse and dextromethorphan. Child Adolesc Psychiatr Clinics North America. (2016) 25:497–508. doi: 10.1016/j.chc.2016.03.007
47. Stanciu CN, Penders TM, and Rouse EM. Recreational use of dextromethorphan, “Robotripping”—A brief review. Am J Addict. (2016) 25:374–7. doi: 10.1111/ajad.12389
48. Stefani M and Roberts DM. 1,4-Butanediol overdose mimicking toxic alcohol exposure. Clin Toxicol. (2020) 58:204–7. doi: 10.1080/15563650.2019.1617419
49. Dufayet L, Bargel S, Bonnet A, Boukerma AK, Chevallier C, Evrard M, et al. Gamma-hydroxybutyrate (GHB), 1,4-butanediol (1,4BD), and gamma-butyrolactone (GBL) intoxication: A state-of-the-art review. Regul Toxicol Pharm. (2023) 142:105435. doi: 10.1016/j.yrtph.2023.105435
50. King A, Hill SL, Pucci M, Bailey G, Keating L, Macfarlane R, et al. Clinical features associated with ADB-BUTINACA exposure in patients attending emergency departments in England. Clin Toxicol. (2022) 60:1094–8. doi: 10.1080/15563650.2022.2101469
51. Fan YL, Huang YY, Zhou Y, Ke X, Tian YM, Zheng S, et al. Unraveling the liver metabolomic profile of ADB-BUTINACA-induced hepatotoxicity. Ecotox. Environ Safe. (2024) 288:117375. doi: 10.1016/j.ecoenv.2024.117375
52. Goncalves R, Labadie M, Chouraqui S, Peyré A, Castaing N, Daveluy A, et al. Involuntary MDMB-4en-PINACA intoxications following cannabis consumption: clinical and analytical findings. Clin Toxicol. (2022) 60:458–63. doi: 10.1080/15563650.2021.1994144
53. Ahmad MA, Ghaleb SS, Hassan DAE, Sharkawi SMZ, Abdelghany AK, Mostafa AM, et al. Robust congregation influences of AB-PINACA and MDMB-4en-PINACA inhalation on neurobehavioral and cardiac disorders in mice. Beni-Suef. Univ J Basic. Appl Sci. (2024) 13:19. doi: 10.1186/s43088-024-00479-9
54. Lorenzo G, Tracy W, Daniel I, Alex K, Barry L, Ilaria T, et al. MDMB-4en-PINACA–related deaths in cook county jail awareness and preventive measures. Am J Forensic Med Pathol. (2025) 46:87–91. doi: 10.1097/paf.0000000000000966
55. Schumacher TJ, Sah N, Palle K, Rumbley J, and Mereddy VR. Synthesis and biological evaluation of benzofuran piperazine derivatives as potential anticancer agents. Bioorg. Med Chem Lett. (2023) 93:129425. doi: 10.1016/j.bmcl.2023.129425
56. Gao H, Zhang X, Pu XJ, Zheng X, Liu B, Rao GX, et al. 2-Benzoylbenzofuran derivatives possessing piperazine linker as anticancer agents. Bioorg. Med Chem Lett. (2019) 29:806–10. doi: 10.1016/j.bmcl.2019.01.025
57. Rathore A, Asati V, Kashaw SK, Agarwal S, Parwani D, Bhattacharya S, et al. The recent development of piperazine and piperidine derivatives as antipsychotic agents. Mini-Rev. Med Chem. (2021) 21:362–79. doi: 10.2174/1389557520666200910092327
58. Huang L, Gao L, Zhang X, Yin L, Hu J, Song T, et al. Synthesis and pharmacological evaluation of piperidine (piperazine)-amide substituted derivatives as multi-target antipsychotics. Bioorg. Med Chem Lett. (2020) 30:127506. doi: 10.1016/j.bmcl.2020.127506
59. Maurer HH, Kraemer T, Springer D, and Staack RF. Chemistry, pharmacology, toxicology and hepatic metabolism of designer drugs of the amphetamine (ecstasy), piperazine, and pyrrolidinophenone types. Ther Drug Monit. (2004) 26:127–31. doi: 10.1097/00007691-200404000-00007
60. Darke S. Opioid overdose and the power of old myths: What we thought we knew, what we do know and why it matters. Drug Alcohol Rev. (2014) 33:109–14. doi: 10.1111/dar.12108
61. Gossop M, Stewart D, Treacy S, and Marsden J. A prospective study of mortality among drug misusers during a 4-year period after seeking treatment. Addiction. (2002) 97:39–47. doi: 10.1046/j.1360-0443.2002.00079.x
62. Araújo AM, Carvalho F, Bastos ML, de Pinho PG, and Carvalho M. The hallucinogenic world of tryptamines: an updated review. Arch Toxicol. (2015) 89:1151–73. doi: 10.1007/s00204-015-1513-x
63. Kaewput W, Thongprayoon C, Petnak T, Chewcharat A, Boonpheng B, and Bathini T. Inpatient burden and mortality of methanol intoxication in the United States. Am J Med Sci. (2021) 361:69–74. doi: 10.1016/j.amjms.2020.08.014
64. Andersson L, Håkansson A, Krantz P, and Johnson B. Investigating opioid-related fatalities in southern Sweden: contact with care-providing authorities and comparison of substances. Harm Reduction J. (2020) 17:5–11. doi: 10.1186/s12954-019-0354-y
65. Tjagvad C, Skurtveit S, Linnet K, Andersen LV, Christoffersen DJ, and Clausen T. Methadone-related overdose deaths in a liberal opioid maintenance treatment programme. Eur Addict. Res. (2016) 22:249–58. doi: 10.1159/000446429
66. Wikner BN, Öhman I, Seldén T, Druid H, Brandt L, and Kieler H. Opioid-related mortality and filled prescriptions for buprenorphine and methadone. Drug Alcohol Rev. (2014) 33:491–8. doi: 10.1111/dar.12143
67. Wells D. Drug administration and sexual assault: sex in a glass. Sci Justice. (2001) 41:197–9. doi: 10.1016/S1355-0306(01)71890-4
68. Hindmarch I, Elsohly M, Gambles J, and Salamone S. Forensic urinalysis of drug use in cases of alleged sexual assault. J Clin Forensic Med. (2001) 8:197–205. doi: 10.1054/jcfm.2001.0513
69. United Nations Office on Drugs and Crime. Current NPS threats Volume II (2020). Available online at: https://www.unodc.org/documents/scientific/Current_NPS_Threats_Volume_II_Web.pdf (Accessed Nov 15, 2021).
70. Laitem L, Bello I, and Gaspar P. Gas chromatographic determination of tranquillizer residues in body fluids and in the meat of slaughtered animals. J Chromatogr A. (1978) 156:327–9. doi: 10.1016/s0021-9673(00)88322-3
71. White HR and Gorman DM. Dynamics of the drug-crime relationship. Criminal Justice. (2000) 1:1–218.
72. Goldstein PJ. The drugs/violence nexus: a tripartite conceptual framework. J Drug Issues. (1985) 15:493–506. doi: 10.1177/002204268501500406
73. World drug report. Office on Drugs and Crime (2023). Available online at: https://www.unodc.org/res/WDR-2023/2314940C.pdf (Accessed May 2025).
74. Tang YL, Xu LH, Liu W, Xiang P, Xu LL, and Yan H. Types and application of biological materials involved in the analysis of new psychoactive substances. J Pharm Anal. (2023) 43:1271–6. doi: 10.16155/j.0254-1793.2023.08.01
75. Drummer OH. Good practices in forensic toxicology. Curr Pharm Design. (2017) 23:5437–41. doi: 10.2174/1381612823666170704123836
76. Nascimento ALA, Costa FMS, Passos MLC, Santos JCC, and Saraiva MLMFS Automatic flow system for sequential detection of zinc and acid phosphatase in forensic samples. Microchem. J. (2025) 213:113781. doi: 10.1016/j.microc.2025.113781
77. Drolet J, Tolstikov V, Williams BA, Greenwood BP, Hill C, Vishnudas VK, et al. Integrated metabolomics assessment of human dried blood spots and urine strips. Metabolites. (2017) 7:35. doi: 10.3390/metabo7030035
78. Gee P, Richardson S, Woltersdorf W, and Moore G. Toxic effects of BZP-based herbal party pills in humans: a prospective study in Christchurch, New Zealand. New Z Med J. (2005) 118:1227.
79. Fleming SW, Cooley JC, Johnson L, Frazee CC, Domanski K, Kleinschmidt K, et al. Analysis of U-47700, a novel synthetic opioid, in human urine by LC–MS–MS and LC-QToF. J Anal Toxicol. (2016) 41:173–80. doi: 10.1093/jat/bkw131
80. Woodward WR, Choi D, Grose J, Malmin B, Hurst S, Pang J, et al. Isoflurane is an effective alternative to ketamine/xylazine/acepromazine as an anesthetic agent for the mouse electroretinogram. Doc Ophthalmol. (2007) 115:187–201. doi: 10.1007/s10633-007-9079-4
81. Burns SM, Cunningham CW, and Mercer SL. DARK classics in chemical neuroscience: fentanyl. ACS Chem Neurosci. (2018) 9–10:2428–37. doi: 10.1021/acschemneuro.8b00174
82. Dolan SB, Forster MJ, and Gatch MB. Discriminative stimulus and locomotor effects of para -substituted and benzofuran analogs of amphetamine. Drug Alcohol Depen. (2017) 180:39–45. doi: 10.1016/j.drugalcdep.2017.07.041
83. Linsen F, Koning RPJ, van Laar M, Niesink RJM, Koeter MW, and Brunt TM. 4-Fluoroamphetamine in the Netherlands: more than a one-night stand. Addiction. (2015) 110:1138–43. doi: 10.1111/add.12932
84. Adamowicz P. Blood concentrations of synthetic cathinones. Clin Toxicol. (2021) 59:648–54. doi: 10.1080/15563650.2020.1848100
85. Soares J, Costa VM, de L Bastos M, Carvalho F, and Capela JP. An updated review on synthetic cathinones. Arch Toxicol. (2021) 95:2895–940. doi: 10.1007/s00204-021-03083-3
86. Skaugen JM, Scoccimarro A, Pizon AF, Rymer JA, Giannoutsos S, Ekins S, et al. Novel ketamine analogues cause a false positive phencyclidine immunoassay. Ann Clin Biochem. (2019) 56:598–607. doi: 10.1177/0004563219858125
87. Word Health Organization. Essential medicines and health products (2025). Available online at: https://www.who.int/medicines/access/controlled-substances/ (Accessed May 2025).
89. Liechti ME, Kunz I, Greminger P, Speich R, and Kupferschmidt H. Clinical features of gamma-hydroxybutyrate and gamma-butyrolactone toxicity and concomitant drug and alcohol use. Drug Alcohol Depen. (2006) 81:323–6. doi: 10.1016/j.drugalcdep.2005.07.010
90. Wood DM, Warren-Gash C, Ashraf T, Greene SL, Shather Z, Trivedy C, et al. Medical and legal confusion surrounding gamma-hydroxybutyrate (GHB) and its precursors gamma-butyrolactone (GBL) and 1,4-butanediol (1,4BD). QJM. (2007) 101:23–9. doi: 10.1093/qjmed/hcm117
92. Angerer V, Mogler L, Steitz JP, Bisel P, Hess C, Schoeder CT, et al. Structural characterization and pharmacological evaluation of the new synthetic cannabinoid cumyl-pegaclone. Drug Test Anal. (2017) 10:597–603. doi: 10.1002/dta.2237
93. Scholten W. European drug report 2017 and opioid-induced deaths. Eur J Hosp. Pharm. (2017) 24:256–7. doi: 10.1136/ejhpharm-2017-001347
94. Holder HD. Substance abuse treatment as part of a total system of community response. Nord. Stud Alcohol Dr. (2010) 27:550–63. doi: 10.1177/145507251002700601
Keywords: drug substitutes, benefits, risks, analysis of technical bottlenecks, management strategies
Citation: Bai S, Li M, Tang S, Wan S, Wu R, Chen L, Wang F and Liu S (2025) Drug substitutes − Insights on benefits, risks, detection methods, and management strategies: a systematic review. Front. Psychiatry 16:1600212. doi: 10.3389/fpsyt.2025.1600212
Received: 27 March 2025; Accepted: 27 June 2025;
Published: 17 July 2025.
Edited by:
Styliani (stella) Vlachou, Dublin City University, IrelandReviewed by:
Samer El Hayek, American Center for Psychiatry and Neurology, United Arab EmiratesGeorge Panagis, University of Crete, Greece
Copyright © 2025 Bai, Li, Tang, Wan, Wu, Chen, Wang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fang Wang, d2YxOTk3MDkwOEAxNjMuY29t; Shan Liu, bGxzczA3MDFAc2luYS5jb20=
 Song Bai
Song Bai Miao Li1
Miao Li1 Fang Wang
Fang Wang